Perioperative Nursing: An unfolding Case study by Gerry Altmiller,EdD, MSN, APRN
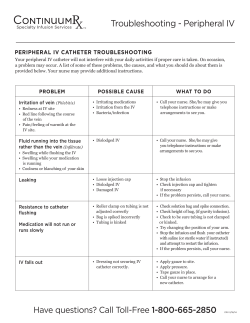
Perioperative Nursing: An unfolding Case study by Gerry Altmiller,EdD, MSN, APRN The Case: • John Egan, 53, has a history of Type I diabetes mellitus, cigarette smoking 40 pack years, CAD, and PVD. Six weeks ago, he developed a wound of his left heel which measured 4cm by 2cm when he discovered it. Despite IV antibiotics and chemical debridement, the wound developed a gangrene infection. He is scheduled for a BKA of the left lower extremity tomorrow at 10:00am. His meds include daily insulin, aspirin 325mg/day, Pletal 100mg BID. He has an advanced directive and NKDA. Identify the priority nursing care for Mr. Egan: Identify the priority nursing care for Mr. Egan: • • • • • • Complete pre-operative testing/Preparation Maintain normal glucose levels Ensure informed consent Ensure correct surgical site Prevent post-op infection Complete pre-operative teaching to prevent complications • Address psychological comfort What preoperative testing is appropriate for Mr. Egan? Pre-surgical Screening Tests • Chest x-ray • Electrocardiography for > 40 yrs • Complete blood count • Electrolyte levels • Urinalysis • X-ray left lower extremity When completing a medication reconciliation for Mr. Egan the evening before surgery, which orders increase the nurse’s concern? • Insulin 6 units Regular with 15 unit NPH subcutaneous q am. • Aspirin 325mg PO q d. • Pletal 100mg PO BID • Ativan 0.5mg IVP on call to OR in AM. – http://www.jointcommission.org • Insulin 6 units Regular with 15 unit NPH subcutaneous q am. (High Alert Med) (NPO after Midnight) • Aspirin 325mg PO q d. (Do not use abbrev) (bleeding potential) • Pletal 100mg PO BID (bleeding potential) Dr. Damon is Mr. Egan’s surgeon and Dr. Riley is Mr. Egan’s anethesiologist. Both come to see him and discuss the surgery the evening before. How does the nurse ensure informed consent? What must the patient consent to for the procedure to be done? Informed Consent for Surgery & Blood Transfusion 3 requirements: • Adequate disclosure of diagnosis-purpose, risks, and consequences of treatment, probability of success, prognosis if not instituted • Understanding & comprehension -patient must be drug free prior to signing consent • Consent given voluntarily -patient must not be persuaded or coerced to undergo the procedure Informed Consent Information • Description of procedure and alternative therapies • Underlying disease process and its natural course • Name and qualifications of person performing procedure • Explanation of risks and how often they occur • Explanation that patient has the right to refuse treatment or withdraw consent Informed Consent Information • Patient must be 18 years old to sign own consent or be an emancipated minor • Parent signs for dependent children as legally responsible • Patient must be deemed competent to sign own consent • Patient must be alert & oriented; Consent may not be signed by patient after receiving narcotics or sedatives • Not necessary if threat to life and patient or legally authorized person unavailable Informed Consent for Surgery, Anesthesia & Blood Transfusion • Part of legal preparation for surgery • Active, shared decision making process between provider and recipient of care • Protects patient, surgeon, hospital and its employees • Nurses role: advocate, witness, appropriate person signs • Medical emergency and consent- 2 physicians write it is necessity in chart • What does it mean that Mr. Egan has an advance directive? How will it apply to his surgical procedure? Advance Directives • Living wills – Patient is usually a full code for 24 hours following surgery – Allows family to know patient wishes in the event of serious intraoperative complication • Durable power of attorney for healthcare During the admission assessment, the nurse questions Mr. Egan to determine if there is a latex allergy or sensitivity. Why is this essential to the patient’s safety? What symptoms would the nurse question Mr. Egan about in order to determine this? Latex Allergy/Sensitivity • At Risk: – Genetic predisposition – Children with spina bifida – Urogenital abnormalities – Spinal cord injuries – Hx of multiple surgeries – Health care professionals Latex Allergy/Sensitivity • S&S – Urticaria – Rhinorrhea – Bronchospasm – Compromised respiratory status – Circulatory collapse & Death • Management – Identify those at risk – Latex free environment – Latex free equipment Preventing complications of surgery is an important part of all surgical patient’s care. What pre-operative teaching does Mr. Egan require in order to prevent complications? Preparing the Patient Through Teaching • Surgical events and sensations • Surgical site preparation • Pain management • Physical activities • Deep breathing • Coughing • Incentive spirometry • Leg exercises • Turning in bed What measures should be taken during this pre-operative phase to ensure the patient’s safety? • Patient Safety Solutions - Joint Commission Resources - Intranet • Mr. Egan is very restless the evening before. He verbalizes to his wife that he is “scared to death” and worried about losing his foot. She asks the nurse what can be done to help him. How will the nurse address the psychological comfort of Mr. Egan? Nursing Interventions to Meet Psychological Needs of Surgical Patients • Establish therapeutic relationship and allow Mr. Egan to verbalize fears and concerns. • Use touch to demonstrate genuine empathy and caring. • Be prepared to respond to Mr. Egan’s questions about surgery and the postoperative and rehabilitative experience. • Ensure a sleep aid is ordered for Mr. Egan for the evening before. • On the morning of the surgery, the OR calls for Mr. Egan to be brought to the OR holding room. What are the responsibilities of the nurse caring for Mr. Egan at this time? Nursing Responsibilities during immediate preoperative period • Accurate Identification of Mr. Egan – 2 patient identifiers • • • • • • Known last meal for patient Safe transport to OR via stretcher with side rails up Psychosocial support for Mr. Egan and his family Patent IV with D5.45NS infusing at 50cc/hr Mr. Egan voids before pre-operative medications Pre-operative dose of Ativan 0.5 mg IV given once on stretcher • Signed consent form is in the chart • OR Checklist completed and on the front of the chart • Accurate identification of patient, surgical procedure & site – Done in holding room with physician present Pre-operative Checklist • Form that lists requirements to be ascertained before patient goes to OR • Documents diagnostic tests complete • Documents pre-op medication given • Documents VS • Documents safety data – ID band in place; 2 identifiers – Jewelry removed – Last void – Dentures removed – Informed consent verified – Patient Allergies In the OR Holding Room, Mr. Egan is delivered into the care of the holding room nurse. Using SBAR technique, discuss the safe hand-off of the patient between the unit nurse and the OR Holding Room Nurse. Dr. Damon meets with Mr. Egan in the OR Holding Room. What final safety checks will be made at this time? While Mr. Egan is in the Operating Room, what considerations will be taken to ensure Mr. Egan’s safety and positive outcome? Time Out Intra-operative Safety • • • • • • Maintenance of sterile technique Continuous patient monitoring Instrument count Sponge count Breaks for personnel TeamSTEPPS Instructor Guide: Video Training Tools Post-operatively, Mr. Egan goes to the Post Anesthesia Care Unit (PACU) where he is extubated and begins to awaken from surgery. His EBL is 50 cc. He has an IV in right arm infusing D5.45 at 100 cc/hr. Post operative labs are drawn and sent. His vital signs remain stable and his dressing remains dry with a hemovac drain at the site. He is discharged back to his med-surg bed after a two hour PACU stay. Using SBAR communication strategy, how does the PACU nurse provide a safe hand off of Mr. Egan to the unit nurse? Mr. Egan’s post operative medication orders include the following: • Insulin 6 units Regular with 15 unit NPH subcutaneous q am. • Aspirin 325mg PO q d. • Pletal 100mg PO BID. • Morphine 2mg IVP q 3 hour for incisional pain. After receiving report, the med-surg unit nurse escorts Mr. Egan to his room via stretcher. He is drowsy but arousable. The unlicensed personnel assists the nurse in transferring Mr. Egan into his bed. What post-operative assessments and immediate post-operative interventions should be performed for Mr. Egan? Postoperative Assessments and Interventions • • • • Vital signs Continuous Pulse ox Telemetry monitoring Color and temperature of skin • Level of consciousness • Intravenous fluids • Surgical site management • • • • Other tubes Comfort Position and safety Report on Fluid intake, output and estimated blood loss (EBL) • Monitor lab values • NPO until bowel sounds return In Caring for Mr. Egan, the nurse recognizes that the highest priority in the post-operative phase is the preventions of complications. What complications is Mr. Egan at risk for following general anesthesia and a below the knee amputation (BKA)? • Hint: Remember Mr. Egan is a smoker, has heart disease and diabetes type 1 as well as PVD Common Post-operative Complications • • • • • • • • • Pain Hypovolemic Shock Thrombophlebitis-DVT Pulmonary embolus Fluid Overload Atelectasis Pneumonia Airway Obstruction Surgical site infection (SSI) What interventions can the nurse implement to prevent respiratory complications? Interventions to Prevent Respiratory Complications • • • • • • • • • Monitoring vital signs Implementing deep breathing Coughing Incentive spirometry Turning in bed; OOB to chair Ambulating Maintaining hydration Avoiding positioning that decreases ventilation Monitoring responses to narcotic analgesics Prevent Atelectasis Splinting Wound While Coughing when patient’s have abdominal surgery What interventions can the nurse implement to prevent cardio-vascular complications? Interventions to Prevent Deep Vein Thrombosis (DVT) • OOB to chair early and often • While on bed rest: Dorsiflex, change position frequently, rotate ankles • TED hose • Intermittent Compression boots • Prophylactic SC heparin BID Leg Exercises to Prevent Venous Stasis What interventions can the nurse implement to prevent surgical site infections? What measures can be taken to prevent surgical site infection (SSI)? • Appropriate use of prophylactic antibiotics • Appropriate surgical site hair removal before surgery • Maintaining glycemic control • Maintaining normal body temperature The laboratory personnel calls the med-surg unit and asks to speak with Mr. Egan’s nurse. She explains that she has a critical value report. What is the procedure to be followed for a critical lab value? Which of the following does the nurse identify as abnormal? Na 132 Chloride 99 Glucose 186 Potassium 5.3 Carbon Dioxide 25 BUN 20 Creatinine 0.9 Calcium 9.7 Magnesium 1.8 Phosphorus 3.8 Critical Lab Values Na 132 Chloride 99 Glucose 186 Potassium 5.3 Carbon Dioxide 25 BUN 20 Creatinine 0.9 Calcium 9.7 Magnesium 1.8 Phosphorus 3.8 While the nurse is on the phone with the lab, Mrs. Egan comes to the nurse’s station to tell the nurse that Mr. Egan is complaining of pain in his left foot. The nurse goes to Mr. Egan’s room to assess and determines he is having phantom limb pain. The nurse goes to the medication cabinet and selects meperidine 50 mg dose, places it in a carpuject and wastes 25mg in the presence of another nurse. As she is walking to Mr. Egan’s room, she stops and takes a time out. What does she discover? What is the nursing responsibility for this near miss? What is the red rule regarding medication administration? What is the nursing responsibility for this near miss? Discard meperidine with a witness Complete incident/occurrance report Report near miss to immediate supervisor Medicate Mr. Egan with correct medication and dose What is the red rule regarding narcotic administration? Never administer medications without reviewing MAR first; 3 checks of medication Incident/Occurrence Reports • Used to document any unusual occurrence that results in or has potential to result in harm to a patient, employee, or visitor • Should not be referred to in nursing notes • Used for quality improvement to identify risks • Records facts about an incident in case of litigation • May be used in court as evidence After medicating Mr. Egan for pain, the nurse addresses the critical lab values, notifying the surgical resident. What could be possible contributing factors to the lab abnormalities? What treatments would be most appropriate to correct the abnormalities? Later that evening, the nurse is called to the phone for an inquiry about Mr. Egan. The caller identifies herself as Mr. Egan’s sister. She wants to know his condition. What should the nurse tell the caller? Confidentiality • Protecting & maintain privacy of all patient information whether spoken, written or saved in computer • Includes confirmation that a patient is admitted to institution • Health Insurance Portability and Accountability Act (HIPAA) – Disclosure requires signed authorization from patient HIPAA Incidental Disclosure Permitted Disclosure • Public health activities for infectious disease or danger • Law enforcement and judicial proceedings • Deceased individuals • Use of sign in sheets • Overheard conversation provided attempt at privacy made • Use of White boards • X-ray light boards seen by passers-by • Calling out names in waiting room • Leaving appointment reminders on voicemail To prevent circulatory complication in the immediate post-operative period for a patient who has had an abdominal hysterectomy, which nursing action is of the highest priority? a. Administer pain medication b. Apply anti-embolism stockings c. Encourage coughing and deep breathing every two hours d. Monitor vital signs every hour until stable The nurse is completing a pre-operative checklist for a 27 year old female scheduled for a bowel resection. Which of the following interventions must be done prior to this patient being sent to the OR? Select all that apply. a. Operative consent signed b. Allergy and ID bands in place c. Removal of gown d. Removal of nail polish e. Removal of jewelry f. Evidence of advanced directive g. Completed H & P h. EKG results i. Anesthesia consent signed j. Results of preoperative diagnostic tests An 18 year old patient who is unconscious and hypotensive and who has sustained serious injury in an MVA in brought to the ED via ambulance. Which is true of the treatment for this patient? a. Next of kin needs to be notified prior to treatment beginning b. Advanced directive and durable power of attorney should be reviewed prior to treatment c. The life-threatening injuries warrant immediate emergent treatment d. The client can be treated after consent is given
© Copyright 2026