The Newborn Examination Karen Montgomery-Reagan, D.O. OUCOM Department of Pediatrics
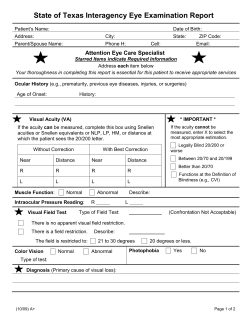
The Newborn Examination Karen Montgomery-Reagan, D.O. OUCOM Department of Pediatrics Overview • Review birth Hx and VS • Listen to heart while infant quiet: Cardiovascular- inspection, palpation, and auscultation • Start from top: Head and Neck – head, face, ears, eyes, nose, mouth, and neck • Chest and Lungs • Abdomen – inspection, palpation, and auscultation • Genitourinary – kidneys and genitalia • Orthopedic – spine, upper and lower extremities Vital Signs – Heart Rate (rates/min) • Awake 85-205 • Sleeping 80-160 – Respiratory Rate (breaths/min) • 30-60 – Systolic Blood Pressure (SBP) • • • • Infant SBP: 80 Age 12 hours: 50-70 / 25-45 Age 96 hours: 60-90 / 20-60 Hypotension defined in neonate to 28 days <60 APGAR Score Score Heart Rate Respiratory effort Muscle tone Reflex irritability (nose suction) Color 0 1 2 Absent <100bpm >100bpm Absent, irregular Slow, crying Good Limp Some flexion of extremities Active motion No response Grimace Cough or sneeze Blue, pale Acrocyanosis Completely pink Dubowitz/Ballard Score • External Characteristics – To be done within few hrs of birth – Edema – Skin texture, color, and opacity – Lanugo – Plantar creases – Nipples and breasts – Ear form and firmness – Genitals • Neuromuscular Score – To be done within 24 hrs – – – – – – Posture Square Window Arm recoil Popliteal angle Scarf sign Heel to ear Small for Gestational Age • Symmetric – HC, length, weight all <10 percentile – 33% of SGA infants – Cause: Infection, chromosomal abnormalities, inborn errors of metabolism, smoking, drugs • Asymmetric – Weight <10 percentile, HC and length normal – 55% of SGA infants – Cause: Uteroplacental insufficiency, Chronic hypertension or disease, Preeclampsia, Hemoglobinopathies, altitude, Placental infarcts or chronic abruption • Combined – Symmetric or asymmetric – 12% of SGA infants – Cause: Smoking, drugs, Placental infarcts or chronic abruption, velamentous insertion, circumvallate placenta, multiple gestation Large for Gestational Age • Etiologies – Infants of diabetic mothers – Beckwith-Wiedemann Syndrome • characterized by macroglossia, visceromegaly, macrosomia, umbilical hernia or omphalocele, and neonatal hypoglycemia – Hydrops fetalis – Large mother Skin • Color – – – – – Pallor: associated with low hemoglobin Cyanosis: associated with hypoxemia Plethora: associated with polycythemia Jaundice: elevated bilirubin Slate grey color: associated with methemoglobinemia Skin • Jaundice – Total and direct bilirubin levels should be measured in newborns with jaundice. – Causes can be related to increased unconjugated hyperbilirubinemia (physiologic, breastfeeding, increased production, decreased hepatic uptake/conjugation) or conjugated (hepatobiliary disorders, ductal disturbances) – The AAP has published guidelines on the management of hyperbilirubinemia in the newborn. Skin • Lanugo – Fine hair on shoulders and back – More common in preemies – Usually disappears in 2-4 weeks • Vernix Caseosa – Cheesy white covering Skin Lesions • Petechiae – On scalp and face after vertex delivery • Sucking blister – Develops from infant sucking on skin in utero. – Disappears as infant progress with feeding. • Hemangiomas – Usually enlarges in 1st year of life. – Large facial hemangiomas may be associated with posterior fossa malformations. – MC benign tumor of infancy – Most require no intervention Skin Lesions • Telangiectatic Nevi – Also called salmon patches or stork bite nevi – Flat, pink lesion found on upper eyelids, forehead, nape of neck – Fade by 1-2 years old except those on nape of neck which may persist • Cutis Marmorata – Transient mottling of the skin – Occurs when baby is exposed to the cold Skin Lesions • Milia – Pinpoint white papules of keratogenous material. – Usually on nose, cheeks and forehead. – Can last for several weeks. Skin Lesions • Miliaria – Obstructed eccrine sweat ducts. – Pinpoint vesicles on forehead, scalp, and skinfolds. – Usually clears within one week. Skin Lesions • Transient Neonatal Pustular Melanosis – Small vesicopustules, generally present at birth. – Contain WBCs and no organisms. – Intact vesicle ruptures to reveal a pigmented macule surrounded by a thin skin ring. Skin Lesions • Erythema Toxicum Neonatorum – Most common newborn rash. – Lesions are firm, yellow or white pustules on a red and swollen base. – Lesions may be found in face, trunk and limbs. – Lasts about 5-7 days. – Wright Stain shows eosinophil sheets. Skin Lesions • Café au lait spots – Suspect nuerofibromatosis if there are many large spots Skin Lesions • Mongolian spots – Well demarcated symmetric bluish gray to deep brown to black skin markings – Common among people of Asian, East Indian, African, and Latino heritage. – Often on the base of the spine, on the buttocks and back – Generally fade in a few years and disappear by puberty. Neurological Exam • Posture – Term infants normal posture is hips abducted and partially flexed, with knees flexed. – Arms are abducted and flexed at the elbow. – Fists are often clenched, with the fingers covering the thumb • Tone – To test, support the infant with one hand under the chest. Neck extensors should be able to hold head in line for 3 seconds – There should be no more than 10% head lag when moving from supine to sitting positions. Neurological Reflexes • Ensure symmetrical • Biceps jerk C5-C6, knee jerk L2-L4, ankle jerk S1-S2, anal wink S4S5, truncal incurvation reflex T2-S1. • Primitive reflexes are present: Babinski, Moro, Galant, palmer and plantar grasps, sucking, rooting, placing/stepping, and asymmetric tonic neck reflex (Fencer’s pose). Neurological Exam • Cranial Nerve Exam – CN II: Pupillary reflex – Oculocephalic Reflex (doll’s eyes) • CN III, IV, and VI • If Brainstem intact: – Eyes deviate contralaterally – Look away from direction of rotation – CNV and VII: Corneal, sucking, and rooting reflexes – CN VIII: Response to Noise – CN IX and X : Gag reflex Macrocephaly • Causes – Familial with autosomal dominant inheritance – Hydrocephalus – Other conditions • • • • • • • Achondroplasia (skeletal dysplasia) Sotos' Syndrome (Cerebral Gigantism) Alexander's Disease Canavan's Disease Gangliosidoses Glutaric aciduria Type I Neurofibromatosis Type I Microcephaly • Causes – Familial – Trisomy 13, 18, 21 – Cornelia de Lange, Rubinstein-Taybi, Smith-Lemli-Opitz, Prader-Willi – Teratogen Exposure • Fetal Alcohol Syndrome • Radiation exposure in utero (<15 weeks gestation) • Fetal Hydantoin – TORCH Virus congenital infection • Cytomegalovirus, Rubella, Toxoplasmosis – Other causes • • • • Meningitis/Encephalitis Gestational Diabetes Maternal hyperphenylalaninemia Hypoxic-ischemic encephalopathy Head Examination • Head – Check overriding sutures, number and size of fontanelles • Molding • Over-riding of cranial bones • Normal finding at delivery • Resolves spontaneously over first 5 days of life Head Trauma • Cephalohematoma – Not as common, but can occur after prolonged labor and instrumentation use. – Rupture of blood vessels that traverse skull to the periosteum – Fluctuant swelling, does not cross suture lines – No overlying discoloration, but possible fracture – Uncomplicated resolves in 2 weeks to 3 months, if fracture, Xray in 4-6 weeks to ensure closure, depressed fractures require neurosurgical consult. Head Trauma • Caput seccedaneum – Common after prolonged labor. – Accumulation of blood above periosteum. – Soft tissue swelling that crosses suture lines with overlying petechiae, purpura or bruising. – Usually resolves spontaneously over several days. Fontanelles • Anterior – Junction of coronal suture and sagittal suture – Mean newborn size: 2.1 cm (larger in black infants) – Often enlarges in first few months of life – Closes between 4 to 26 months (median 13.8 months) – Closes by 3 months in 1% of infants – Closes by 24 months in 96% of infants • Posterior – Junction of lambdoidal suture and sagittal suture – Mean newborn size: 0.5 to 0.7 cm – Closes by 2 months Fontanelles • Exam of anterior fontanelle – Palpate fontanelle with infant sitting upright quietly – Auscultate for bruit (suggests AV malformation) – Macewen's Sign (percussion of fontanelle) • Dull cracked-pot sound suggests increased ICP Fontanelles • Bulging fontanelle • Crying, coughing or vomiting • Increased intracranial pressure: Hydrocephalus, Meningitis/encephalitis, Hypoxic-ischemic injury, Intracranial hemorrhage, Dermoid tumors of the scalp • Sunken fontanelle • Decreasedintracranial pressure (dehydration) • Large fontanelle or delayed closure • Congenital hypothyroidism,Trisomy 21, Rickets, Achondroplasia, Increased Intracranial Pressure Head Examination • Craniosynostosis – Premature closing of cranial sutures – Results in growth restriction perpendicular to affected suture and compensatory overgrowth in unrestricted regions. – If accompanied by restricted brain growth or hydrocephalus, neurosurgical intervention is needed. Facial Examination • Facial Nerve Paralysis – Usually caused by compression of the facial nerve against the sacral promontory or by trauma of a forceps delivery. – The nasolabial fold on the affected side is not present, the corner of the mouth droops and the affected eye is unable to close. – Infant will have difficulty with feeding, drooling from the paralyzed side. – Most palsies resolved spontaneously within days. Ear Examination Assess for asymmetry or irregular shape – Note presence of auricular or pre-auricular pits, fleshy appendages, lipomas, or skin tags. – Low set ears • Below lateral canthus of eye • Associated with genitourinary anomalies, because these areas develop at similar times. – Malformed ears • Can be associated with Downs or Turners Syndromes Eye Examination • Normal Eye findings following delivery – Red reflex • Hold opthalmoscope 6-8” from eye. • Should transmit a clear red color back. – Equal pupil size and reactivity to light – Retinal or Subconjunctival Hemorrhages • Common after vaginal delivery • Clears spontaneously in 1-2 weeks – Lid edema • Force applied to open the eye often results in lid eversion • Examination should be postponed until the edema resolves – Eye Color • Permanent eye color usually not attained until age 6 months. Eye Examination • Conjunctivitis – Relatively common in newborns. – Chemical • Silver nitrate prophylaxis given at delivery • Requires no treatment, • resolves within 48 hours – Gonorrheal • 24-48 hours old • Profound edema, purulent exudate • Tx – Penicillin G, Rocephin, or Claforan – Chlamydial • Occurs within 7-10 days • Watery discharge changes to copious/purulent • Tx – Erythromycin – HSV • Occurs within 2 weeks • Keratitis, cataracts, chorioretinitis • Tx – Topical and systemic antivirals Eye Examination • Abnormal Funduscopic Exam – Lens opacity • Indicates congenital cataract • Associated with TORCH Virus infection • If monocular or dense cataract, newborn is at risk for developing amblyopia. – Leukocoria (White reflex or Cat’s eye reflex) • Suggests lens, vitreous or fundus abnormality • Evaluate for Retinoblastoma • Requires Opthalmologic Referral Eye Examination • Coloboma (ocular tissue defect) – Eyelid margin defect: Treacher Collins Syndrome – Aniridia (absent iris) • Usually occurs bilaterally • Associated with poor visual acuity and nystagmus – Iris and retina defect: CHARGE association • • • • • • Coloboma Heart disease Choanal Atresia Postnatal growth retardation Genital hypoplasia Ear Abnormality • Requires Opthalmologic Referral Nose Examination • Babies are obligate nose breathers until 4 months old. • Check patency with stethoscope (listen over nares). • Look for nasal flaring as a sign of increased respiratory effort. • Choanal Atresia – Small NG tube unable to pass through nares. – Normally should meet no resistance. – Bilateral atresia • Cyanosis that is relieved with crying. • Is an emergency in the newborn. • Requires an oral airway and surgical repair Mouth Examination • Observe the size and shape of the mouth – Microstomia – seen in Trisomy 18 and 21 – Macrostomia – seen in mucopolysaccharidoses – Fish mouth – seen in Fetal Alcohol Syndrome – Macroglossia – associated with hypothyroidism and mucopolysaccharidoses – Small Chin – associated with Pierre Robin Mouth Examination Epstein pearls Natal Teeth • small white cysts which contain keratin • frequently found on either side of the median raphe of the palate. • Resolves in 1-2 months • Occurs 1 in 2,000 births • Location is most often the lower incisors. • Risk of aspiration if loosely attached, most require removal. • More often present in newborns with cleft palate. Mouth • Ranulas – small bluish-white swellings of variable size on the floor of the mouth representing benign mucous gland retention cysts Mouth • Cleft Lip – – – – • Incidence 1 in 750 (Caucasian) Can be seen with or without cleft palate Common in Trisomy 13 Repair is usually at 3 months of age Cleft Palate – – – – Incidence 1 in 2500 (Caucasian) Midline defect starts at uvula May involve soft and hard palate and incisive foramen Repair is usually before age 1 for normal speech Neck Examination • Palpation – Palpate all neck muscles – Webbed neck • Associated with Turner’s and Noonan’s Syndromes – Lymph Nodes • Unusual at birth, presence usually indicates congenital infection – Torticollis • Sternocleidomastoid muscle injury from birth trauma. • Hematoma and fibrosis results in muscle shortening. • Muscle adaptation from abnormal intrauterine position. Neck Examination • Most common neck masses: – vascular malformations, abnormal lymphatic tissue, teratomas, and dermoid cysts • Cystic hygromas – Most common neck mass • Thyroglossal duct cysts – Typically midline and inferior to hyoid bone – Surgical consultation is required Chest/Lung Examination • Inspection – Supernumerary breast or nipple is common (10%) – Breast enlargement secondary to maternal hormones – Unilateral absence or hypoplasia of pectoralis major • Poland's Syndrome (Poland's Sequence) – Widely spaced nipples • Turner's Syndrome • Noonan Syndrome Chest/Lung Examination • Inspection – Chest Deformity • Pectus Carinatum – Much less common than Pectus Excavatum – More common in males by ratio of 4:1 – Narrow thorax with increased anteroposterior diameter • Pectus Excavatum – Gender predominance: Boys (3:1 ratio) – Mild: Oval pit near infrasternal notch – Severe: Sinking of entire lower sternum Chest/Lungs • Observe – Respiratory pattern • Brief periods apnea are normal in transition, called “periodic breathing” – Chest movement • Symmetry • Retractions and Tracheal tugging • Ascultation – Audible stridor, grunting – Wheeze, rales, rhonchi Cardiovascular • Inspection – Check for pallor, cyanosis, or plethora • Palpation – Check capillary refill • Should be less than 3 seconds – Precordium • Feel for increased activity and thrill – Pulses • Ipsilateral femoral (postductal) and brachial (preductal) pulses should be equal in timing and intensity • Decreased femoral = coarctation of aorta • Bounding pulses often indicated PDA Cardiovascular • Auscultation – Rhythm • Gallup Rhythms • Split S2 is Normal • Split S2 absent – Aortic or pulmonic valvular atresia or stenosis – Results in high pulmonary vascular resistance – Rate • Regular, irregular – Murmur • Quality, radiation, location of intensity Abdominal Inspection • Abdominal Shape – Flat: Seen with decreased tone, Diaphragmatic hernia - abdominal contents in chest, Abnormal abdominal musculature – Distended: Consider obstruction, Excess air inside or outside the bowel, Fluid in the peritoneal cavity (ascites), Enlarged viscus Abdominal Examination • Abdominal wall defects – Usually diagnosed prenatally. • Omphalocoele – Covered with membrane unless it has ruptured. – Cord attachment at apex of defect. – 67% have an associated abnormality. • Gastroschisis – Not covered with a membrane. – Defect is to right of umbilicus. – Cord attachment to abdominal wall. – Management – immediate surgical consultation • Abdominal Auscultation – Normoactive bowel sounds all four quadrants Abdominal Palpation • Abdominal Localized Mass – • Gastrointestinal Duplications, Meconium ileus, Mesenteric or omental cyst, Pyloric stenosis, Volvulus, Wilms tumor, Neuroblastoma, Renal vein thrombosis Liver – – Usually palpable 2 cm below costal margin Hepatomegaly – • Many causes depending on presence or absence of hyperbilirubinemia (direct or indirect) and associated splenomegaly Spleen – – Not usually palpable Splenomegally • • Etiology can be infectious or extramedullary hematopoeisis Kidneys – Length vertically should be 4.5-5.0 cm in full term infant. Umbilicus • Umbilical Cord – Count number of vessels • 3 vessel cord is normal (1 vein and 2 arteries) – A single umbilical artery is present in up to 1%, which may be associated with asymptomatic renal anomalies • Umbilicus – Check for signs of bleeding, infection, granuloma, or abnormal communication with the intra-abdominal organs • Examine for umbilical hernias Male Genitourinary Examination • Inspection – Check glans, urethral opening, prepuce and shaft • Term normal length is 3.5 +/- 0.7 cm • Term normal diameter is 1.1 +/- 0.2 cm • Abnormally small penis – Reduced androgen effect or reduced growth hormone in 2nd and 3rd semester – Normally it is difficult to completely retract the foreskin. – Circumcised infants should be checked for edema, bleeding or complications at the incision site. – Full term infants should have brownish pigmentation and fully rugated scrotums Male Genitourinary Examination • Hypospadias • A proximally displaced urethral meatus. • Wide variation from mild glanular to severe perineal. • Chordee • Ventral curvature of the penis. • May accompany hypospadias. • Can be due to skin tethering or a short urethra. • Circumcision should be delayed in these infants. Male Genitourinary Examination • Communicating Hydrocele • • • • Incomplete obliteration of processus vaginalis Painless, tense, fluctuant scrotal mass that transilluminates. Withold surgery until after first year of life Most will resolve spontaneously • Inguinal Hernia • Soft, nontender, reducible bulge in inguinal canal, especially at time of increased intra-abdominal pressure. • Becomes tender and tense with discoloration of overlying skin if incarcerated. • Requires elective surgical repair as soon as possible. Male Genitourinary Examination • Palpation of Testes – If not palpable must determine if it is retractile, ectopic or cryptorchid. – Unilateral retracted testicle • Testicle may be brought down into scrotum. • Follow-up examinations in the clinic. – Unilateral palpable ectopic or undescended testicle • Observe for descent. • Surgical correction at 6 month to 1 year. – Unilateral nonpalpable testicle (15% of cases) • Laparoscopy at 6 months to 1 year for evaluation. • Testicle found on laparoscopy in 50% of cases. • Orchiopexy brings testis into scrotum (98% efficacy). Female Genitourinary Examination • Inspection – Check labia, clitoris, urethral opening and external vaginal vault – Common normal findings • Prominent labia minora and clitoris – Clitoris can have a relatively prominent appearance, especially if the labia are underdeveloped or the infant is premature. – Clitoromegaly may be a sigh of masculinization or a virilizing tumor. – Can also be caused by increased androgen production or drug use. • Vaginal/hymenal skin tag • Mucoid/whitish discharge • Small amount of vaginal bleeding – Secondary to withdrawal of maternal hormones. Ambiguous Genitalia • Newborns with ambigious genitalia: require rapid diagnosis and treatment! • Potential clinical manifestations: hypoglycemia, hyperpigmentation, apneic episodes, seizures, hyperkalemia, dehydration, hypotension, vascular collapse, shock • Also social emergency: Refer to the infant as “your baby” or “your child,” delay naming the child/birth certificate until sex is determined Rectum and Anus • Anus patent and not ectopic – Assess with probe or small finger • No fistulas present • Pilonidal dimple/cyst – pit or sinus in the sacral area – pilonidal dimple may also be a deep tract, rather than a shallow depression, leading to a sinus that may contain hair. – During adolescence the pilonidal dimple or tract may become infected forming a cyst-like structure called a pilonidal cyst. These pilonidal cysts may require surgical drainage or total excision to prevent reinfection • Meconium passed within 48 hours of birth Spinal Dysraphism • Spina Bifida Occulta – • No abnormality of meninges, spinal cord or nerve roots Spinal Meningocele – – – – Meninges herniate through posterior vertebral arches Spinal cord and nerve roots are not involved. Most often occurs in low back Anterior herniation at sacrum may also occur • – May result in constipation or bladder abnormality Usually asymptomatic and covered by full layer skin Spinal Dysraphism • Myelomeningocele – – – – Meninges, spinal cord and nerve roots are involved Lumbosacral region in 75% of cases Associated with dysfunction of multiple organ systems Signs • • – Flaccid paralysis of lower extremities Deep Tendon Reflexes absent Associated Conditions • • • • Hydrocephalus and Chiari II Malformation (80% of cases) Neurogenic bladder Urinary Incontinence Stool Incontinence Spinal Dysraphism • Spinal Dysraphism – – – Dermatologic signs seen in 50-90% of cases Skin findings may be only signs of occult lesion Findings • Hypertrichosis – • • • Increased vellus Hair » Non-pigmented fine "peach fuzz" hair covering body Lipoma Midline Hemangioma Large midline dimple above gluteal crease – – – Do not probe dimple Small sacral dimple within gluteal crease is normal Not worrisome if bottom of dimple can be visualized UE Orthopedic Examination Clavicle • May Fracture from Birth Trauma • Most common newborn orthopedic injury, especially large infants • Pain with movement and Moro reflex • Pseudoparalysis of extremity on fracture side • Sternocleidomastoid muscle spasm on affected side • Deformity or discoloration may be possible • Crepitus at fracture site • Palpable bony irregularity at fracture site UE Orthopedic Examination • Digits (Fingers and Toes) – Supernumerary Digit • • • • • – Occur more often in black infants. Tends to be hereditary Frequently lateral to the 5th digit of hand or foot. Extra digit may have a nail, attached by small pedicle. Ligature around the digit allows it to fall off in several days. Polydactyly • • • • Extra-digit is located more often on the foot. Bone is palpable within the extra-digit. The digit may have voluntary movement. Amputation of digit when child is > 1 year old. UE Orthopedic Examination • Digits – Syndactyly • Simple – involves soft tissue attachment only • Complex – involves fusion of bone or nail • Partial - web extends from base partially • Complete - web from base to tip of finger • Radiographs needed to determine degree of fusion. • Should refer to orthopedics. UE Orthopedic Examination • Upper Extremities – Single Palmar Crease • Seen in Down's Syndrome • Seen in 4% of normal babies – Ulnar or radial bone absence UE Orthopedic Examination • Upper Extremity – Brachial Plexus Injuries • Results from excessive traction of C5-T3 spinal nerve roots. • Erb-Duchenne palsy – Most common injury, involves C5-C7 – Arm adducted, internally rotated, elbow extended, arm pronated, wrist flexed, “waiter’s tip if C7 involved. • Klumpke’s palsy – Incidence is rare, involves C8-T1. – Hand is paralyzed, no voluntary motion. LE Orthopedic Examination • Lower Extremities – Bowing of legs is normal variation – Positional deformities of foot • Foot should be easily replaced to normal position – Talipes Equinovarus (Clubfoot) • Heel inversion (varus) with internal rotation • Forefoot inverted and adducted (soles face each other) • Plantar flexion with inability to dorsiflex • Leg internal rotation • Refer immediately for serial casts • Severe clubfoot requires surgery LE Orthopedic Examination • Metatarsus Adductus (InToeing) – Forefoot rotated inwardly – Banana shaped or C-shaped foot – Lateral border of foot convex – Medial border of foot concave – Base of fifth metatarsal (styloid) prominent – Both feet are inverted (face each other) – Mild or flexible improves during first 3 months of life – Full resolution spontaneously in 85% of cases – Rigid deformity requires treatment LE Orthopedic Examination • Calcaneovalgus Deformity – Foot has up and out appearance – Foot dorsiflexes easily (long heel cord, ligaments lax) – Limited plantar flexion (less than 90 degrees) – Lateral Sole deviation (banana shaped) – Feet are everted (facing away from each other) – Heel position is valgus (medial malleoli are closer) LE Orthopedic Examination • Congenital hip dislocation – Ortolani test • Attempts to dislocate hip • Hip clunk felt on exam • Must distinguish from a hip click which is benignl – Galeazzi's Sign • Compare the 2 femur lengths – Barlow's Test • Attempts to sublux unstable hip – Perform with caution Resources • • • • • • • http://dermatlas.med.jhmi.edu http://www.fpnotebook.com http://health.allrefer.com http://health-pictures.com/index.htm www.neonatolgy.org Nelson’s Textbook of Pediatrics American Family Physician, “The Newborn Examination: Parts I and II” January 2002.
© Copyright 2026