Lymphocytic progenitor cell origin and clonal evolution of human B-
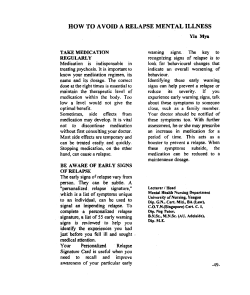
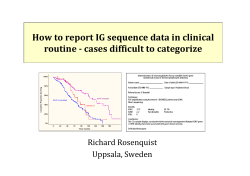
From www.bloodjournal.org by guest on November 10, 2014. For personal use only. 1996 88: 609-621 Lymphocytic progenitor cell origin and clonal evolution of human Blineage acute lymphoblastic leukemia F Davi, C Gocke, S Smith and J Sklar Updated information and services can be found at: http://www.bloodjournal.org/content/88/2/609.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved. From www.bloodjournal.org by guest on November 10, 2014. For personal use only. Lymphocytic Progenitor Cell Origin and Clonal Evolution of Human B-Lineage Acute Lymphoblastic Leukemia By Frederic Davi, Christopher Gocke, Stephen Smith, and Jeffrey Sklar At presentation, bone marrow specimens from over 25% of B-lineageacute lymphoblastic leukemias (ALL) display more than two clonal rearrangements of immunoglobulin heavy chain (IgHJgenes in Southern blot analyses. Nucleotide sequence analysis has shown predominantly different VHDJH junctions among these genes, leading t o the frequent description of such cases as oligoclonal leukemias. In the present study, we have analyzed the IgH genes from four patients whose leukemic cells contained different patterns of IgH gene rearrangementsbetween presentation and relapse. Nucleotide sequence analysis of the IgH genes showed that three mechanisms could account for these differences: de novo V H D J H rearrangement, VH to DJH recombination, and VHreplacement. In all cases, more than two totally different VHWH rearrangements appeared during evolution of the dis- ease, formally consistent with the conclusion that these tumors were composed of apparently unrelated clones. However, the retention of some of the antigen receptor gene rearrangements, as well as the persistence of a chromosomal marker in two cases, indicated that these leukemias had a monoclonal origin. These findings support the hypothesis that some ALLs arise from a lymphoid progenitor cell at a stage of lymphocyte development before the onset of IgH gene rearrangement. These leukemic lymphocyte progenitors generate malignant daughter cells capable of an in vivo maturation that involves the completion of multiple different IgH rearrangements as well as the modification of preexisting rearrangements by VH t o DJH recombination or by a VH replacement. 0 1996 by The American Society of Hematology. A loci in the germline configuration and spawns progeny cells in which de novo VHDJH joining occurs as the neoplasm evolves.739 Finally, truly bi- or oligoclonal tumors might arise from independent transformation events in separate progenitor We have evaluated the possible mechanisms for apparent oligoclonality and clonal evolution of ALL in four patients by sequencing IgH gene rearrangements. Our results suggest the origin of these tumors from a transformed lymphocyte progenitor cell, the progeny of which are capable of continuing de novo gene rearrangement and additional recombination events such as VHto DJH gene joining and VHreplacements. NTIGEN RECEPTOR gene rearrangements have been widely used as markers of clonality in human lymphoid neoplasms.’,*During B-cell ontogeny, the genes that encode immunoglobulins (Ig) are rearranged by recombination of discontinuous DNA segments that have been termed variable (V), diversity (D), and joining (J). This process occurs most often in a sequential order: heavy (H) chain genes before light (L) chain genes, and K light chain genes before A light chain genes. Among the IgH genes, the first event is generally the joining of a D segment to a JH segment, followed by the addition of a VH segment to the DJH join. Further diversity is created by the insertion of random nucleotides (the so-called N-regions) and/or the deletion of short stretches of sequence from the ends of the participating segments at the time of DJH and VHD joining, thereby creating a unique genetic marker for the cell and any progeny that cell may produce. Multiple studies using iso-en~ymes,~ karyotype: Ig idiotype,5 and gene rearrangement’.’ analyses have suggested that leukemia represents the clonal expansion of a single transformed hematopoietic cell. Nevertheless, Southern blot analysis has shown that at least 25% of early B-lineage acute lymphoblastic leukemias (ALLs) contain more than two IgH Furthermore, sequential follow-up of some patients has shown that the pattern of IgH gene rearrangement can change over the course of the disease.l’-I3 Therefore, many ALLs appear to be oligoclonal with respect to these markers. Several mechanisms could account for this observation. First, biclonality might be artificially created by hyperploidy of chromosome 14 with independent IgH rearrangements present in each chromosome.6 Second, apparent oligoclonality could be the result of evolution within the tumor clone by modification of a preexisting IgH gene rearrangement through at least four types of processessomatic mutation of immunoglobulin gene DNA,14 the replacement of a rearranged VH segment by a more 5’ unrearranged VH ~ e g m e n t , ’ ~the . ’ joining ~ of a VHsegment to an incomplete DJH rearrangement,17and by an “open and shut” mechanism with deletion and addition of junctional nucleotides.” Third, oligoclonality could also occur by transformation of an early lymphoid precursor cell that had retained Ig Blood, VOI 88, NO 2 (July 15). 1996 pp 609-621 MATERIALS AND METHODS Patients, samples, and cell lines. All tissues were obtained with the informed consent of patients. Malignant cells were obtained from patients with ALL at the time of presentation and at relapse. In each case, bone marrow aspirates and peripheral blood samples contained >80% leukemic cells. Diagnosis of ALL was established by standard morphological, cytochemical, and immunophenotypic methods. The precursor B phenotype was based on the presence of malignant cells positive for TdT, CD19, and HLA-DR (null ALL), or for TdT, From the Division of Molecular Oncology, Department of Pathology, Brigham & Women’s Hospital and Harvard Medical School, Boston, MA: the Department of Pathology, Pennsylvania State University School of Medicine. Hershey, PA: and the Division of Pediarric Hematology-Oncology, The University of Chicago Medical Center, Chicago, IL. Submitted December 4, 1995; accepted March 11, 19%. Supported by Grants No. PO1 CA34183 and ROI CAS8621 from the National Institutes of Health to J.S. F.D. was the recipient of a fellowship from The Lady Tata Memorial Trust. Address reprint requests to Jefiey Sklar, MD, Department of Pathology, Brigham and Women’s Hospital, 75 Francis St, Boston, MA 02115. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1996 by The American Society of Hematology. OOO6-4971/96/8802-O1$3.00/0 609 From www.bloodjournal.org by guest on November 10, 2014. For personal use only. DAVl ET AL 610 Table 1. Sequence of Oligonucleotides Primers Used for IgH PCR Outer Primers 5' Inner Primers 3' GCTGAGGTGAAGAAGCCTGGG CAGGTCACCTTGAGIAGGAGTCTGG AGGTGCAGCTGGTGCIGAGTCTGG AGGTGCAGCTGCAGGAGTCGGG GTGTCTCCCNCCACAGGTIAGTCTTIGTG AGGTACAGCTGCAGCAGTCAGGT ACCTGAGGAGACGGTGACCNGGRGITGT 5' 3' TCGGATCCTCNGGTGANGGGTCflTCCTGC GAAGATCTCACACTGACCTGCACCTIGTC GAAGATCTCTCCTGTGCAGCCTCTGG GTGGATCCTGTCCCTCACCTGCNGTICTG CCAGATCTCCTGTAAGGGTTCTGG GAAGATCTCTCACTCACCTGTGCCATC TGGAATTCCAGflGGTGICKCCTCITGGCCCCAG The BamHI, 69,II, and EcoRl restriction sites are underlined. CDIO, CD19, and HLA-DR (common ALL), or for TdT, CDIO, CD19, HLA-DR and cytoplasmic 1.1 chains (pre-B ALL). Establishment of cell lines, as well as their cytogenetic analysis, was performed using techniques previously described." Normal bone marrow was obtained from donors for allogeneic bone marrow transplantation. Normal blood was obtained from healthy volunteers. Southern blot anulysis. High molecular weight DNA was isolated and analyzed using the Southem blot hybridization procedure, as previously described.' Probes used for hybridization consisted of cloned DNA fragments containing human J,, C,, Chz regions of the IgH genes and the J, regions,*' the J, regions," and Jo region2" of the T-cell receptor (TCR) genes. The following restriction enzymes were used for analyses of the various genes: IgH-BumHI, EcoRI, Hind111 and Bgl 11; IgK-BamHI; IgX---EcoRI; TCR 0-BurnH1, HindII1, and EcoRI; TCR y-BumHI and Bgl 11; TCR b-ButnHI. EcoR1, and HindlI1. Polymerase chuin reuction (PCR). Amplification of IgH gene rearrangements using the PCR was performed in a two-part procedure. In the first step, 50 ng to I pg of DNA was amplified for 20 ro 25 cycles with a set of Vwfamily-specific primers and a consensus Jtl primer. Ten percent of this amplified material was then reamplified for 15 to 20 cycles using a second set of nested VH family-specific and consensus J H primers. PCR was performed using nucleotides, buffer, and enzyme provided in the Perkin-Elmer Cetus Gene Amp Kit (Perkin-Elmer Cetus, Nonvalk, CT), according to the manufacturer's specifications. All reactions contained IS0 ng of each primer and were performed in a 50-pL volume. Each amplification cycle consisted of a denaturation step at 94°C for I minute (3 minutes in the first cycle), a primer annealing step at a temperature ranging from 45°C to 55°C for 1 minute, and a primer extension step at 72°C for I minute (and 7 minutes in the last cycle). Negative controls were prepared by performing amplifications on samples lacking DNA or containing DNA from polyclonal specimens (bone marrow or blood from normal individuals). Precautions to avoid contamination with amplified material were followed. a s described in Kwock et al" and Sarkar et aLzx PCR products were analyzed by electrophoresis in I .2% agarose and 6% polyacrylamide gels. Oligonucleoride primers. Design of the 5' primers was based on sequence homology within the framework I region of each VtI family, according to the published human germline V,, genes."' '' The 3' antisense primers were chosen to match consensus sequences within the six human J H genes.'"-'' Restriction sites were incorporated into the set of nested primers to facilitate the ligation of the PCR products into vectors for cloning in Escherichiu coli. The sequences of the VtI and the .I,, primers are given in Table I . Clone-specific oligonucleotides were designed to correspond to the N-regions of clonal IgH rearrangements found within the leukemic cells of individual patients. All primers were constructed with an automated DNA synthesizer (Applied Biosystems, Foster City, CA). DNA sequencing. PCR products were digested with the restriction enzymes EcoRI and BumHI or Bgl I1 (BRL, Gaithersburg, MD). After purification in low melting point agarose, the fragments were ligated into DNA of the M I 3 sequencing vector. Multiple M I 3 clones grown in E coli were isolated and subjected to sequence analysis using the Sequanase Kit (US Biochemical Corp, Cleveland. OH). Only sequences found repeatedly in at least four MI3 clones were considered to represent clonal rearrangements. The specific identity of individual V, segments was not determined. N-oligonucleotide hybridization. PCR products amplified from tumor DNA, dilutions of tumor DNA in control DNA (bone marrow from normal individuals), and control DNA by itself, were separated by electrophoresis on I .2% agarose gel and transferred to Genatran nylon membranes (Plasco, Wobum, MA). Alternatively, the PCR products were directly applied to the membrane using a slotted manifold apparatus (Schleicher and Schuell, Keene, NH). Membranes were hybridized for 4 hours at 46°C in 5X SSPE (1 X SSPE is 0. I 5 mol1L sodium chloride, 10 mmol/L sodium phosphate, I mmol1L EDTA) and 0.5% SDS (sodium dodecyl sulfate) with clone-specific oligonucleotide probes which had been 5' end-labeled with '?P. After hybridization, membranes were washed twice in 2X SSPE, 0. I% SDS for 2 minutes at room temperature, and then once in 5 X SSPE. 0.1% SDS for 15 minutes at 2°C below the melting point of the oligonucleotide sequence. Blots were exposed on Kodak XAR-5 film (Eastnian Kodak, Rochester. NY) for 2 to 16 hours. RESULTS Patient 1. Patient 1 (Figs 1 and 2 ) was diagnosed with pre-B ALL containing the Philadelphia chromosome (Ph'). Two cell lines, SUP-B13 and SUP-B15, were established from cells collected at the time of first and second bone marrow relapses, 2 years and 26 months, respectively, after initial diagnosis.jx F o r this and all other cases except one (patient 3), digestion of DNA with Hind111 restriction enzyme, rather than with BamHI or EcoRI, seemed to display a greater number of bands in Southem blot analyses of the IgH genes. Using HindIII, the presentation bone marrow from this case showed a germline band, an equally intense rearranged band, and a second weakly hybridizing band, which probably also represented a clonally rearranged gene (this weakly hybridizing band occurred at the position of a minor cross-hybridizing germline band; the interpretation that this band may have represented a rearrangement in the presentation specimen was based on its relative increased intensity). At both the first and second relapses (bone marrow was analyzed for the first relapse and blood for the second) and in each cell line, the intense rearranged band was lost and a new, strongly hybridizing nongermline band appeared. A band at the position of the weakly hybridizing rearranged band was retained, From www.bloodjournal.org by guest on November 10, 2014. For personal use only. 611 ORIGIN AND EVOLUTION OF B-ALL I I I I I -G > > - Gf Fig 1. Southern blot analysis of leukemic cells from patient 1 at presentation, relapse, and call lines. DNA was digested with Hind 111 and the blot was hybridized with a JH probe. G shows the position of the germline band and G' the position of a weakly cross-hybridizing band; arrows indicate clonally rearranged bands. BM, bone marrow; PB, peripheral blood. > but it was not possible to distinguish it from the minor crosshybridizing germline band. The germline band, still present in the marrow relapse. was not seen in the cell lines and only faintly hybridized in the analysis of blood from the second relapse. Other antigen receptor genes displayed the same pattern of rearrangement in both marrow samples, the peripheral blood sample, and the SUP-B 13 cell line. This pattern consisted of the germline configuration for immunoglobulin light chain genes (IgL) and beta T-cell receptor genes (TCR /3), deletion of delta T-cell receptor chain genes (TCR 6). and apparent biallelic rearrangement of the gamma T-cell receptor genes (TCR 7 ) .The SUP-B 15 cell line showed one detectable kappa immunoglobulin light chain (Iglc) gene rearrangement and one weakly hybridizing rearranged band with each of the lambda immunoglobulin light chain (IgX) and TCR /3 probes, as well as an additional TCR y rearrangement. The Ph' chromosome was detected cytogenetically in all samples. At relapse, some cells had a more complex karyotype: 46,XY,t(9;22)(q34;qI 1 ),t( I ;4)(p22;q33),der( 14q),16p+. Both cell lines had only this karyotype in all cells. Amplification of IgH DNA in the presentation bone marrow repeatedly yielded three bands, two generated with the VHI-family primers, one with the VH3-family primers. The first VH1rearrangement involved a vH1 segment (VHIa), the DLR3 segment, and the JH4 segment, all joined in frame. The second VH1 rearrangement used a different VH1 segment (VHlb)joined out of frame to the DLRl segment and the JH6 segment. The vH3 rearrangement consisted of an inframe joining of a vH3segment (VH3a) directly to the JH6 segment, without any obvious D segment. In the samples obtained at relapse and in both cell lines, a single band was obtained, and only using VJ-family primers. This rearrangement had a partial homology with the original V H l b rearrangement identified in the presentation specimen, as both rearrangements shared the same D-N-JH region. However, the VH segment in this new rearrangement segment (VJb) and the N-region between VI, and D segments differed completely from that of the original rearrangement. This could be due to either two different VH segments rearranging to the same DJH joint, or the replacement of the VHI b gene by the VH3bgene. The later process, well characterized in mice, has been shown to occur in cultures of virally It intransformed pre-B cells and in B-cell volves a recombination process mediated through a heptamer sequence located in the 3' portion of most VI, genes.'" Theoretically, the sequences amplified from the blood or bone marrow in this patient could correspond with rearrangements of nonmalignant lymphocytes cells admixed with tumor cells rather than to bona fide clonal rearrangements contained in leukemic cell populations. To confirm the origin of these sequences from tumor cells, the frequencies of the sequences obtained were roughly quantitated within the specimens by hybridization studies using oligonucleotides specific for the individual rearrangements. Radiolabeled oligonucleotides (N-oligonucleotides) complementary to the sequences of the N-regions for each of the four rearrangements amplified in this case were hybridized to IgH DNA amplified from the total specimen DNA before or after dilution of that DNA with the DNA of normal bone marrow. Each oligonucleotide hybridized to product amplified from DNA of the appropriate specimen and not to product from normal DNA or from the DNA of specimens from the patient in which the rearrangement could not be detected by PCR (data not shown; similar results are illustrated for patient 3 below). Moreover, the hybridization occurred to product amplified from specimen DNA that had been diluted several orders of magnitude before amplification. The results indicate that the rearrangements represented by the N-oligonucleotides were relatively abundant within the specimens and probably reflected a significant clonal proliferation of cells containing the rearrangements. Although the VH3brearrangement was presumably generated by modification of a preexisting rearrangement (DJHor VHDJH), the tumor contains at least two apparently distinct clonal lines because three different VHDJH recombinations and a germline band were present in the presentation specimen. These clonal lines may have originated from a leukemic progenitor with both IgH alleles in the germline configuration. Alternatively, these lines may represent subclones that were derived from a tumor cell having one common rearranged allele, but which diverged as a result of different rearrangements on the second germline allele. Purient 2. Patient 2 (Fig 3) was diagnosed with a pre-B ALL containing a t ( l ; 19)(q23;p13). A cell line, SUP-B27, was derived from bone marrow obtained at relapse I year later. Southern blot analysis of the DNA from the presentation marrow after digestion with Hind 111 and hybridization with a JH probe showed a germline and four rearranged bands. The two more intense rearranged bands were conserved at relapse and in the cell line. The relapse marrow also From www.bloodjournal.org by guest on November 10, 2014. For personal use only. DAVl ET AL 612 P r e s e n t a t i o n (BM) - - - - Relapse 1(BM) Relapse 2 (PB) 1 Gt1R c 1 ~ ~ 1 G+2R G+lR G G G G G+2R G+2R de 1 de 1 de 1 de 1 de 1 G G G G G+lR 2 1R G G G+lR G G G+lR G+2R IJUNCTIOHAL 1R ~ Cellp line ~ 2 ~ (SUP-B15) 2 G+2R 2 c--) G+3R SEQUENCES~ VH3a JH6 TACTGTGCaagagggtcggagcccaACTACTACTACGGTATGGACGT ---__----___--____--_ VHla DLR3 JH4 TACTGTGCaacagccagtgaggaGGTGGTGACTGCTATTCagTTTGACTA _---____--_____-_____ VHlb DLRl .................... Cell l i n e s 1&2 (+) JH 6 TACTGTGCGAGAgaGGTGGTGTATGCTATACCggTACTACTACTACGGTATG~CGT Relapses 1&2 (+) (-) IIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIIII VH3b TACTGTACGAGAgttgccagggGGTGGTGTATGCTATACCggTACTACTACTACGGTATGGACGT ..................... (+) Fig 2. Patient 1: Summary of immunogenotype and IgH gene rearrangement junctional sequences. (A) Pattern of antigen receptor gene rearrangements by Southem blot analysis. BM, bone marrow; PB, peripheral blood; G, germline; R, rearranged; del, deleted. Arrows indicate identity balween rearranged bands; the number above the arrow indicates the number of rearranged bands that were identical. (B) Regions identified as VH, D, and Jn gene segments are overlined. The specific identity of individual VHsegments was not determined. N-regions are in small characters. Hatched bars, N-oligonudeotide probes. Vertical parallel bars, identical nucleotides between two rearrangements. (+I, in frame; (-1, out of frame. had a germline IgH band and two additional rearrangements, while the cell line showed no germline band. Light chain genes were in the germline configuration in the presentation marrow, while one Igrc and one Igh rearrangement appeared at relapse and were retained in the cell line. The cell line had four additional Igrc rearrangements, which appeared as bands with much lower intensities. TCR y genes were in the germline configuration in all samples. A germline and a rearranged band at the similar position were detected with a TCR 6 probe in the presentation and relapse marrows, the latter having two additional rearrangements. The cell line had a different TCR 6 rearrangement, and over time in culture acquired a second TCR 6 rearrangement. Finally, hybridization with a TCR 0 probe showed a germline and a rearranged band in the presentation marrow, while the relapse marrow and the cell line displayed only the germline configuration of this gene. Amplification of IgH rearrangements using VH3-family primers yielded the same two products from each sample, likely corresponding to the two conserved bands seen on the Southem blot analysis. One was an in-frame rearrangement of a vH3 segment (vH3c) to the DXP, segment, which in tum was joined to the JH6segment. This rearrangement may account for the cytoplasmic Igp chain produced by the leukemic cells in this case. The other IgH rearrangement amplified was out-of-frame and involved a different vH3 segment (VH3d),the DXP’1 segment, and the J& segment. In addition, VH6-familyprimers amplified an in-frame vH6-JH4rearrangement from the presentation marrow. On the other hand, a VHl-DXP’1-JJb rearrangement was amplified solely from the relapse marrow. Therefore, although Southem blot analysis displayed four rearrangements in both presentation and relapse samples, only three of them could be amplified from any specimen in this case. Absence of ampli- ~ ~ From www.bloodjournal.org by guest on November 10, 2014. For personal use only. ORIGIN AND EVOLUTION OF E-ALL 613 - - Presentation 1gH G+4R I9K G G TCR7 G TCR~ G+lR TCR~ G+lR Cell line (SUP-BZ7) Re1 apse 2 G+4R 2 2R G+lR 1 G+5R G+lR 1 G+lR G 1 G+3R G G G+lR f----t 1 2R G JUNCTIONAL SEQUENCES Presentation I- TATTGTGCAAGAGtgttgggtgttacccaTGACTA _---___-----__----- vH3c JH6 .................... Re 1apse Relapse DXP4 TACTGTGCGAGAGAagtggGTATTACGATTTTTGGAGTGGcttcgcggtggTACTACGGTATGGACGT presentation Cell line JH4 - VH6 r vH3d DXP'I JH4 1 TACTGTGCGAcctaatcaggcGTATTACTATGGTTCGGGGAGcctatagggggaaTTGACTA r1 DXP ' 1 JH5b vH1c TACTGTGCGAGAcaggggcagccgctTGGTTCGGGGAGTTAatgacttcgcggtcgtAAAACTGGTTCGACCC ..................... Fig 3. Patient 2: Summary of immunogenotype and IgH gene rearrangement junctional sequences. fication could be explained by the presence of a partial DJH rearrangement, which lacked a rearranged VH segment. Alternatively, insufficient complementarity between rearranged target VHor JH sequences and the consensus oligonucleotides used may have prevented amplification of additional, complete VHDJH rearrangements. The origin of each of the amplified rearrangements from clonal cell populations was confirmed by hybridization with N-oligonucleotides. These results suggest that this case contains several clonal lines, with one predominant line that is present at presentation and at relapse and is also represented by the in vitro cell line. In vivo, as well as in vitro, evolution within this line is demonstrated by rearrangements of the IgL and TCR 6 genes. At least one additional line at presentation and one at relapse, each bearing different IgH, TCR 6 and p rearrangements, were also present. All of these lines appear totally unrelated, at least with regard to their IgH genes. Because three separate leukemogenic transformation events seem unlikely in a single patient, the most plausible explanation for the findings in this case is a common B-lineage committed leukemic progenitor that had its antigen receptor genes in the germline configuration, but could undergo further maturation to the pre-B-cell stage. Patient 3. Patient 3 (Fig 4) was diagnosed with common ALL. Bone marrow from this patient was analyzed at presentation and at relapse 2 years later. Southern blot analyses performed on an EcoRI digest of DNA from the presentation marrow showed two rearranged IgH genes, as well as a band in the germline position. At relapse the germline band and one rearranged band persisted, while two less intense new rearranged bands also appeared. The patterns of bands in the analyses of IgL genes were identical in both samples and consisted of the deletion of both Igrc alleles, and one Igh rearrangement. Similarly, the TCR y gene pattern of a germline and two rearranged bands was unchanged between the two specimens. One of the two TCR 6 rearranged bands found at presentation was lost at relapse and one rearranged TCR p band was acquired at relapse. Amplification of IgH DNA from the presentation bone marrow yielded PCR products with vH2 and V& primers. One product consisted of a vH2 segment (VH2a)joined in frame to a D-D fusion (DK4 and DM2 segments), which, was in turn, joined to the JH6csegment. The second product consisted of a vH4 segment (V&a), parts of the DM 1 and DLR 5 segments and a JH segment that could not be precisely identified because of extensive 5' deletion. Two contiguous From www.bloodjournal.org by guest on November 10, 2014. For personal use only. DAVl ET AL 614 - Presentation G+2R de 1 G+1R G+2R Re 1apse 1 G+3R de 1 1 G+lR 2 G+2R 4----t G+2R G+lR G G+lR I JUNCTIONAL SEQUENCES I Presentation Presentation [ rL r Re 1apse VH2 a I DK4 DM2 - JH6c ---_-------------- TACTGTGCacGGATACAGCGGAACTACTACTACATGGACGT DLR5 CACGGCTGTGTATTACTGTGCGAGAggcgggtTGGAAgtcctatgATAGTACggt cccccgc VH4a DM1 ..................... VH4b CACGGCC. . ---e-- (+) (-) llllllllllllllllllllllllllllllllll . . . . . . . . . . . . .--------------cggggagggtTGGAAgtcctatgATAGTACggtcccccgc VH5b JH6 TACTGTGCaagagggtcggagcccaACTACTACTACGGTATGGACGT ------------------ (-) (+) Fig 4. Patient 3: Summary of immunogenotype and IgH gene rearrangement junctional sequences. Dotted line indicates a l&bp deletion within the 3' end of the VH4b gene. stop codons in the DLR5 segments interrupted the reading VHreplacement, when exonucleolytic digestion of rearranging gene segments, as in de novo V-D joining, commonly frame of this rearrangement. The vH4 rearrangement was occurs. Figure 5 illustrates the results of N-oligonucleotide also found at relapse, while the VH2 rearrangement was not detected. Instead, a vH5 and a different V d rearrangement hybridization in this case. Therefore, it appears that the bone marrow of patient 3 were amplified. The v H 5 rearrangement contained the VH5b segment joined in frame to the JH6 segment. The second contained a leukemic clone bearing a vH4 rearrangement that persisted through the course of the disease, but underwent a V& rearrangement was clearly related to the rearrangement VHreplacement event within a subclone. At different times, previously detected, as they shared the same N-D-N-JH rethe leukemic cells in this patient also possessed additional gion, but the vH4 segment used in this case (V&b) was IgH rearrangements, including the vH2 rearrangement found different (substitutions of nucleotides at 10 separate positions at presentation and the vH5 rearrangement found at relapse. distinguished the portions of the rearrangements amplified). These must have been produced by a VHDJH recombination This IgH modification most likely reflects a VHreplacement, in a precursor neoplastic clone with germline IgH genes. in which there is retention of sequences located 3' to the Whether both alleles were in the germline configuration in conserved internal VH gene heptamer (TACTGTG) recognized as the signal for VH to VH r e c ~ m b i n a t i o n . ' ~ An . ~ ~ . ~ ~this precursor, or only one allele was germline and the other had already undergone the vH4 rearrangement cannot be alternative explanation for these observations is a gene conresolved, although the deletion of IgK genes at both presentaversion event within the VH sequence; however, the 18-bp tion and relapse favors the latter interpretation. deletion found within the rearrangement at the 3' end of the Patient 4. Patient 4 (Figs 6 and 7) was an infant diagV&b segment, is more likely to have been generated during From www.bloodjournal.org by guest on November 10, 2014. For personal use only. 615 ORIGIN AND EVOLUTION OF B-ALL N-region specific probe Presentstion IO' I to-' 10-'10-~ I I I Normal - Relapse '01 I IC'16' lom31 I I I I i VHZa VH4b Additionally, the second relapse marrow showed another IgA rearrangement. A common TCR y rearrangement was found in all samples, while the second relapse marrow had an additional rearrangement. After prolonged exposure, four more faint bands appeared in analyses of the presentation sample and the first relapse sample, only two of which migrated at the same position. Four TCR 6 rearrangements were detected in the presentation sample, but only a single shared rearranged band was observed in both relapse samples. Exclusively germline configurations of TCR 0 genes were detected in all samples from this case. Four IgH rearrangements were amplified from the DNA of the presentation marrow. Three of these had similar DN-JH regions composed of the DN4 segment joined to the J ~ 3 bsegment. However, the VH-N regions were different and involved either a vH2 (VH2b),a VH5(VH%), or the VH6 segment. The fourth rearrangement had a totally unrelated sequence, created by a vH3 segment (VH3e)joined to the JH4segment. All four rearrangements were out of frame. In both relapse samples, a rearrangement was amplified that displayed partial homology with the first rearrangement detected in the presentation bone marrow; it had the same DN4-JH3b recombination identified previously, but this sequence was joined in frame to a vH4 segment (vH4c). Two additional rearrangements were obtained from the first re- Presentation VHSb FmP I Fig 5. Detection of leukemic cells from patient 3 bearing a clonal IgH gene rearrangement with a N-region clone-specific probe. DNA from tumor at presentation or relapse, 10-fold dilutions of tumor DNA in normal bone marrow (BM) or normal B M DNA were amplified with VHfamily-specific and JHconsensus oligonucleotides. PCR products were applied t o a nylon membrane using a slot-blot apparatus and hybridized with a N-region specific probe. The rearrangements from which the probes are derived are indicated on the left of each panel (see Fig 4 for sequence of the probes). A common rearrangement involving the VH4a segment is detected in both presentation and relapse samples, although the number of cells bearing this rearrangement is about 5 t o 10 times more abundant in the former than the latter. A specific product for the VH2a, VH4b, and the VH5b rearrangements is only detected in the sample from which this rearrangement was originally amplified. Relapse 2 mw '? > > > i. 8 . y * > -------- * *- G m nosed with a null ALL. Six IgH rearranged bands, in addition to a germline band, were identified in Southern blot autoradiograms of a Hind111 digest of DNA from his presentation bone marrow. In a first relapse, I year later, a germline band and two strongly hybridizing rearranged bands were present, one of which had already been detected in the previous sample. Furthermore, three faint rearranged bands could also be seen. In the second relapse, 8 months later, the bone marrow displayed only two IgH rearranged bands, identical to the two intensity hybridizing bands seen on the first reThe 'gK genes remained in the germline 'Onlapse figuration throughout the disease, while one IgA rearranged band appeared at the same position among all three samples. - Relapse 1 -4 --------* > ?. > Fig 6. Southern blot analysis of bone marrow samples from patient 4. DNA was digested with Hidl11 and the blot was hybridized with a JH probe. G shows the position of the germline band and arrows indicate clonally rearranged bands. From www.bloodjournal.org by guest on November 10, 2014. For personal use only. DAW ET AL 616 lapse marrow. One involved a vH3 segment (VH3f) joined directly to the J Hsegment; ~ the other, a v H 1segment (VHld) joined in frame to the DLR2 segment and the JH5bsegment. In the second relapse marrow, only one rearrangement could be amplified despite the detection of two IgH rearrangements by Southem blot analysis of this specimen. As mentioned in the discussion of patient 2, this could be due to a partial DJH recombination or to a mismatch between primers and target sequences. Hybridizations to PCR products derived from the DNA of the various specimens in this case were performed using an N-oligonucleotide probe specific for the junctional sequence each rearrangement. As expected, the N-oligonucleotides hybridized to product from amplified DNA and DNA dilutions of the appropriate specimens. An Presentation G+6R N-oligonucleotide for the V& rearrangement yields a strong hybridization signal in both relapse samples, but B negative signal in the presentation marrow (data not shown). Therefore, the common IgH rearranged band seen on the Southern blot analysis in all three samples seems to correspond to a nonamplifiable sequence. In this patient with a complex pattern of antigen receptor gene rearrangements, four IgH rearrangements were clearly related and came from a common allele bearing a DN4-JH3b recombination. Although it could be possible that multiple VH replacements occurred, it seems more likely that these rearrangements arose in the progeny of a cell containing a partial DJH joining and that several distinct VH segments were subsequently rearranged in different subclones de- Relapse 1 1 f--) G+5R G Relapse 2 c2-) G G G+lR 1 c--) 3 G+5R 2R G+lR G+5R G+4R G+lR G G 1 c--) & & G+2R G+2R G+lR G VH3e JH4 ..................... TACTGTtcttccccccctACTACTTTGACTA VH6 DN4 JH3b ------------------ TACTGTGCAAGAGgggATAGCAGCTCGTCCggATGCTTTTGATAT lllllllllllllllllllllllllllll llllllllllllllllllllllllll .................... I/III/II1lII/0IIIIII/ll/ .................... VH5c TACTGTGCGAGAccgtATAGCAGCTCGTCCggATGCTTTTGATAT ------------------ VH2b TACTGTGCacgggccttgagGCAGCTCGTCCggATGCTTTTGATAT Relapses 1 & 2 vH4c TACTGTGCGAGCggtggggttaggaCAGCTCGTCCggATGCTTTTGATAT DLR2 VHld .................... JH5b TACTGTGCaacagcactccttaataGTAGTGGTccctACkCC ( +) Fig 7. Patient 4 Summary of immunogonotype and IgH gene rearrangement junctional sequences. From www.bloodjournal.org by guest on November 10, 2014. For personal use only. ORIGIN AND EVOLUTION OF BALL scended from that cell. The presence of other totally unrelated sequences suggests that the original leukemic clone had other antigen receptor genes in the germline configuration. This inference is consistent with the intense germline band in the Southern blot autoradiogram of DNA from the presentation marrow. Therefore, evolution of the leukemic clone in this patient may have occurred by a series of steps: (1) a committed B-cell precursor with germline IgH genes gave rise to different lines with distinct rearrangements, as seen the the presentation specimen; ( 2 ) one of these lines, in which a DJH recombination had occurred, gave rise to subclones represented by the two relapse specimens in which VH to DJH rearrangement was completed; and (3) a cell having fully rearranged both IgH alleles at first relapse underwent additional rearrangement of the second Igh allele and TCR y genes before clonally expanding to produce the second relapse. DISCUSSION In this study we have analyzed antigen receptor genes to characterize the origins and evolution of ALL. This work relied heavily on PCR amplification to isolate and sequence IgH gene rearrangements. Previous studies have used single consensus oligonucleotides to 3’ VH and JH sequences and have shown IgH rearrangements could be amplified in 60% to 90% of In our hands, this method had failed to amplify multiple rearrangements in oligoclonal tumors; in general, only one or sometimes two bands were obtained. This could be due to the preferential amplification of sequences having better matches with the consensus VHprimer or to more efficient amplification of rearrangements that are more abundant within the sample. In view of these problems, we used VH-family specific primers. This approach enabled us to amplify many more IgH rearrangements. However, the number of sequences obtained by PCR did not strictly correspond with the number of bands detected on Southern blot analyses. Some sequences might not be amplified because they were partial DJH recombinations or were partially mismatched with the primers. Conversely, some sequences amplified were not seen on Southern blot analyses. This reflects the greater sensitivity of PCR techniques over Southern blot analysis for detection of less abundant but still clonal rearrangements, as discussed by Deane et al.43 The interpretation that an amplified IgH rearrangement was tumor-related and did not come from background lymphocytes was supported by the following considerations: (1) all sequences were found in multiple M13 clones obtained from independent amplifications; ( 2 ) amplification of polyclonal cells (bone marrow or blood from normal individuals) was always performed in parallel and generated a smear of PCR products assayed by polyacrylamide gel electrophoresis, while clonal populations showed one or sometimes two discrete bands (data not shown); and (3) slot blot hybridization of these PCR products with clone-specific N-region oligonucleotide probes showed that the specific sequences could be detected only in the relevant samples and not in control normal bone marrows. Furthermore, rough quantitation indicated that the amplified sequence was present in multiple copies within the tumor sample and did not arise 617 Table 2. Summary of IgH Gene Rearrangement Modifications in the Evolution of Precursor-B ALL Loss of IgH Rearrangement Patient Patient Patient Patient 3 + + + 4 f 1 2 VH to DJ. De Novo VHDJH VH Replacement Recombination Rearrangement + + or + + + + + from the amplification of a single background lymphocyte. It should be noted, however, that quantitation by this assay is only approximate and that the extent of dilution at which clonal IgH rearrangements were still detected might not exactly reflect the true abundance of cells with these rearrangements, since many factors, such as the degree of homology with the VHprimers, may affect the efficiency of amplification. The four patients presented in this study had a pattern of IgH gene rearrangements that differed between diagnosis and relapse (Table 2). In three of these patients (patients 2 to 4), a common IgH rearrangement was conserved, indicating a straightforward clonal relationship. This was further supported by the presence of a common rearrangement for some other antigen receptor gene, and in one case by the persistence of a chromosomal translocation t( 1;19) (patient 2). In one patient (patient l), there was no definite conserved IgH rearrangement, but the presence of an identical DJH joining, as well as the conserved configurations of TCR y and 6 genes and the persistence of the Ph’ chromosome leads to a similar conclusion. Three different mechanisms were responsible for shifting patterns of Ig gene rearrangement observed over time among the cases in our study (Table 2). (1) Loss of rearrangements. Loss of IgH gene rearrangements was seen in all four patients. Loss of TCR gene rearrangements was also detected for three of them: TCR y gene rearrangements for one patient (patient 4),TCR 6 gene rearrangements for two patients (patients 2, 3, and 4), and TCR p gene rearrangements for one patient (patient 2 ) . Loss of Ig and TCR gene rearrangements was probably related, at least in some instances, to the loss of the clonal lines bearing these sequences. The disappearance of subclones between presentation and relapse may have been related to their elimination by chemotherapy. On the other hand, certain cells containing a subset of rearrangements observed earlier in the case may have become resistant to chemotherapy andor acquired mutations leading to a selective growth advantage and overwhelming of competing subclones. A comparable phenomenon took place during the establishment in culture of the in vitro cell line developed for patient 2. ( 2 ) ModiJcation of apreexisting rearrangement. Modification of a preexisting rearrangement by a VHreplacement clearly occurred in one case (patient 3) and possibly in another (patient 1). Rearrangements of distinct VH genes to a common DJH joining could also account for IgH gene modification in one case (patient 4) and possibly in one other (patient 1). Therefore, in all but one patient (patient 2 ) , clonal From www.bloodjournal.org by guest on November 10, 2014. For personal use only. DAW ET AL 618 evolution involved, at least for some IgH rearrangements, modification of a preexisting rearrangement by VH replacement or VH to DJH joining, as reported by other investigator~.--~~ Two other mechanisms responsible for modification of preexisting rearrangements have also been described: somatic mutations and “open and shut” events. Somatic mutations occur frequently during evolution of some mature Bcell tumors such as follicular lymphoma,I4 similar to the process by which postrearrangement diversification of Ig gene sequences takes place during the normal immune response. Recent studies have also shown that somatic mutations may also occur at low frequency in precursor B leukemic cells- and can modify IgH rearrangements between diagnostic and relap~e.~’ In any event, somatic mutation is probably not responsible for the IgH gene alterations detected by Southern blot in our patients, as the sequences of PCR products amplified from the tumors show far greater differences than can be explained by somatic mutation. Junctional sequences can be changed by an “open and shut” mechanism.” In this process, new N-region nucleotides are generated after the rearrangement has reopened and closed following previous deletion and addition of nucleotides. This mechanism has been observed in artificial recombination substrates introduced into murine early B cells” and more recently in human ALL.@However, these types of modification were not seen in our study. ( 3 ) De novo rearrangements. De novo rearrangements were observed for three patients (patients 2 to 4). The fourth patient (patient 1) had three different VHDJH recombinations at presentation. Therefore in all cases, more than two totally unrelated VHDJH sequences appeared during the evolution of these ALL, formally consistent with oligoclonality of the tumors. Several explanations could account for this apparent oligoclonality in ALL. (1) Extra chromosome 14 may be present in a monoclonal tumor, as has been shown to occur in some ALL.‘ Cytogenetic data were available for two of our patients and did not show any evidence of additional copies of chromosome 14. Nevertheless, we cannot rule out this possibility for the two other patients. (2) Oligoclonality might result from independent transformation of separate lymphoid cells. Indeed, there is a group of tumors, particularly among those arising in immunosuppressed patients, in which independent lines of tumor cells are present, as confirmed by study of polymorphism in Epstein-Barr viral genome commonly found in these tumors.” Therefore, true multiclonality cannot be excluded a priori. (3) Transformation of a single progenitor lymphoid cell with unrearranged Ig genes, followed by the emergence of subclones with independent diverse IgH rearrangements, has been proposed to occur in some lymphocytic Considered in aggregate, our data best fits this overall mechanism for apparent oligoclonality of the ALL cases in our study. Thus, our analysis strongly supports the hypothesis of a transformed lymphocyte progenitor cell that undergoes distinct IgH rearrangements within different subclones. These subclones can further differentiate by completing VH to DJH rearrangements, VH replacement, and also IgL rearrangements, the Table 3. IgH Gene RearrangementSequences as Targets for Minimal Residual Disease Analysis Loss Patient 1 Patient 2 Patient 3 Patient 4 Partial (D-N-JHl Conservation + + + + + + Total (V,-N-D-N-J,) Conservation t latter being observed for three patients (patients I , 2, and 4). Maturation of the leukemic cells in the form of Ig gene rearrangements appearing over the course of the disease would seem to reflect the physiologic differentiation of their benign conterpart during normal B-cell de~elopment.~” However, rearrangements of TCR ?, 6, and p genes acquired over time may or may not be a property shared by normal developing B cells. Our results confirm those of some previous studies of oligoclonal B-lineage ALL.’,’ In contrast, Wasserman et al” have recently suggested that evolution of the immunogenotype in B-lineage ALL is most often related to VH replacement or VHto DJH recombination, ie, modification of a preexisting rearrangement rather than de novo rearrangement. This discrepancy might be due to the usage of different primers for DNA amplification, as we found that VHfamily-specific primers could amplify more diverse IgH rearrangements within oligoclonal tumors than the single VH consensus primer. Other investigators have reported that only a single pattern of ongoing rearrangement (ie, VHreplacement or VHto DJH recombination or complete de novo rearrangement) occurred in an individual patient.45These results suggested that the type of ongoing rearrangement was restricted depending on the development stage and IgH status of the precursor cells at the time of malignant transformation. Our data differ in showing that distinct ongoing IgH rearrangements processes can coexist within the same tumor. Our study suggests that despite an appearance of biclonality or oligoclonality, all the ALL analyzed here were monoclonal tumors and represented the leukemic transformation of lymphoid progenitors that yield progeny cells in which rearrangements of Ig genes continued well after primary transformation events had already taken place. A similar situation has been found in mice, where pre-B-cell tumors induced by Abelson murine leukemia virus could undergo clonal evolution and exhibit multiple IgH and L rearrangements. ‘ 7 5 2 Furthermore, continuing rearrangement of antigen receptor genes is not a phenomenon confined to leukemic cells in vivo; rearrangement of genes may also proceed in vitro (as in the cell line SUP-B27). All of these examples illustrate that transformation does not preclude further maturation and that the concept of tumor cells “frozen” at a specific stage of differentiation has limited relevance. Thus, despite the fact that acute leukemias consist of proliferating cells that fail to fully mature beyond certain stages of differentiation, this stage does not represent the stage at which transformation occurred. Transformation of a lymphocyte progenitor cell followed by clonal evolution has been well From www.bloodjournal.org by guest on November 10, 2014. For personal use only. ORIGIN AND EVOLUTION OF B-ALL 619 application of these gene rearrangements as markers for the documented in some cases of ALL,53of acute myelogenous detection of minimal residual disease. leukemia," and in chronic myelogenous leukemia." Some bilineage leukemia might also originate from transformation ACKNOWLEDGMENT of a pluripotent progenitor Therefore, partial maturation of transformed cells appears to be a common feature of We thank S. Schaflhausen for help in preparation of the manuleukemia, although the reasons why cells cannot continue to script. develop beyond certain immature stages is unclear. Two of our patients (patients 1 and 2) had a pre-B ALL, REFERENCES one had a common ALL (patient 3), and one had a null ALL 1. Arnold A, Cossman J, Bakhshi A, Jaffe E, Waldmann TA, (patient 4). Therefore, clonal evolution is not restricted to Korsmeyer S: Immunoglobulin-gene rearrangements as unique clonal markers in human lymphoid neoplasms. N Engl J Med a specific subtype of B-lineage ALL. Myeloid-associated 309:1593, 1983 antigens such as CD13, CD15, and CD33 were also detected 2. Cleary ML, Choa J, Warnke R, Sklar J: Immunoglobulin gene on the leukemic cells of two of our patients (patients 1 and rearrangement as a diagnostic criterion of B cell lymphoma. hoc 4). These findings add further evidence for the lymphocytic Natl Acad Sci USA 81:593, 1984 progenitor cell origin of these leukemias and suggest 3. Dow LW, Martin P, Moohr J, Greenberg M, Macdougall LG, involvement of a pluripotential stem cell in some instances. Najfield V, Fialkow PJ: Evidence for clonal development of childPrevious studies have shown preferential usage of certain hood acute lymphoblastic leukemia. Blood 66:902, 1985 VH,DH, and JH gene segments in human ALL. Though the 4. Yunis JJ: The chromosomal basis of human neoplasia. Science number of IgH rearrangements sequenced in our study was 221:227, 1983 small, similar findings were made. VH gene segments from 5. Mayumi M, Jubagawa H, Omura GA, Gathings WE, Kearney JF, Cooper MD: Studies on the clonal origin of human B cell leukefamilies vH4 (15.8%), vH5 (10.5%), and VH6(10.5%)were mia using monoclonal anti-idiotype antibodies. J Immunol 129:904, overrepresented compared with the expected frequencies 1982 based on the size of each family (respectively, lo%, 1%, 6. Kitchingman GR, Mirro J, Stass S, Rovigatti U, Melvin SL, and < 1 %), as previously reported.57The two most frequently Williams DL, Raimondi SC, Murphy SB: Biologic and prognostic used D segments belonged to the DLR and DXP families significance of presence of more than two p heavy-chain genes in (30% each), as already noted by Kiyoi et al.47 Finally, the childhood acute lymphoblastic leukemia of B precursor cell origin. JH4 and JH6 genes were the most frequently found (38.5% Blood 67:698, 1986 each) as previously shown by several investigator~.4~.~~ 7. Bird J, Galili N, Link M, Stites D, Sklar J: Continuing rearTherefore, ALLs with unstable IgH gene rearrangements do rangement but absence of somatic hypermutation in immunoglobulin not display any specific type of repertoire and cannot be genes of human B cell precursor leukemia. J Exp Med 168:229, distinguished from other ALLs based on their use of certain 1988 8. Katz F, Ball L, Gibbons B, Chessells J: The use of DNA probes gene segments. to monitor minimal residual disease in childhood acute lymphoblasDetection of minimal residual disease in B-ALL by PCR tic leukaemia. Br J Haematol 73:173, 1989 using clone-specific probes for the N-region of the IgH genes 9. Carter M, Neale GAM, Kitchingman GR: Characterization of has become increasingly widely used in recent years.4042.58.59 immunoglobulin heavy chain genes from an acute lymphocytic leuThis approach to monitoring of disease after therapy assumes kemia with four rearrangements. Leukemia 5:668, 1991 stability of the rearrangement over the course of the disease. 10. Beishuizen A, H2hlen K, Hagemeijer A, Verhoeven M-AJ, In our study, all cases had lost one or more IgH rearrangeHooijkaas H, Adriaansen HJ, Wolvers-Tetter0 ILM, van Wering ER, ments, and more importantly the associated N-regions, bevan Dongen JJM: Multiple rearranged immunoglobulin genes in tween presentation and relapse. However, one IgH rearrangechildhood acute lymphoblastic leukemia of precursor B-cell origin. ment was at least partially conserved among samples at Leukemia 5:657, 1991 1 1. Raghavachar A, Thiel E, Bartram CR: Analyses of phenotype various stages during the disease (Table 3). Because it is and genotype in acute lymphoblastic leukemias at first presentation impossible to predict which rearrangement may disappear and in relapse. Blood 70:1079, 1987 and which may persist, the most accurate assay would re12. Wright JJ, Poplack DG, Bakhshi A, Reaman G, Cole D, Jenquire use of a specific probe for each rearrangement. While sen JP, Korsmeyer SJ: Gene rearrangements as markers of clonal this strategy may be impractical, the DJH junction seems variation and minimal residual disease in acute lymphoblastic leukeoverall more often conserved than the VHD junction, and it mia. J Clin Oncol 5:735, 1987 would seem reasonable to choose this region as a target for 13. Bunin NJ, Raimondi SC, Mirro Jr. J, Behm FG, Goorha R, minimal residual disease analysis. TCR y , which is freKitchingman GR: Alterations in immunoglobulin or T cell receptor quently rearranged in B-ALL, has been suggested as a more gene rearrangement at relapse: Involvement of 1lq23 and changes in immunophenotype. Leukemia 4:727, 1990 stable marker." Indeed, three of the cases in our study had 14. Cleary ML, Meeker TC, Levy S, Lee E, Trela M, Sklar J, TCRy rearrangements that were apparently not modified Levy R: Clustering of extensive somatic mutations in the variable over time. Nevertheless, one case (patient 4) had lost some region of an immunoglobulin heavy chain gene from a human B of the TCRy rearrangements. Similarly, Tycko et a16' have cell lymphoma. Cell 44:97, 1986 reported a case with totally different TCRy rearrangements 15. Kleinfield R, Hardy RR, Tarlinton D, Dangl J, Herzenberg at diagnosis and relapse, while IgH rearrangements remained LA, Weigert M: Recombination between an expressed immunoglobidentical. Taken together, these data indicate the instability ulin heavy-chain gene and a germline variable gene segment in a of antigen receptor gene rearrangement in some cases of Ly 1' B-cell lymphoma. Nature 322:843, 1986 ALL represents a potentially important complication in the 16. Reth M, Gehmann P, Petrac E, P. W: A novel VH to VHDJH From www.bloodjournal.org by guest on November 10, 2014. For personal use only. 620 joining mechanism in heavy-chain-negative (null) pre-B cells results in heavy-chain production. Nature 322:840, 1986 17. Reth MG, Jacson S, Alt FW: VHDJH formation and DJH replacement during pre-B differentiation: Non-random usage of gene segments. EMBO J 5:2131, 1986 18. Lewis SM, Hesse JE, Mizuuchi K, Gellert M: Novel strand exchanges in V(D)J recombination. Cell 55: 1099, 1988 19. Sklar J, Cleary ML, Thielemans K, Gralow J, Wamke R, Levy R: Biclonal B-cell lymphoma. N Engl J Med 331:20, 1984 20. van Dongen JJM, Hooijkaas H, Michiels JJ, Grosveld G, de Klein A, van der Kwast TH, Prins MEF, Abels J, Hagemeijer A: Richter’s syndrome with different immunoglobulin light chains and different heavy chain gene rearrangements. Blood 64:571, 1984 21. Downing JR, Grossi CE, Smedberg CT, Burrows PD: Diffuse large cell lymphoma in patient with hairy cell leukemia: Immunoglobulin gene analysis reveals separate clonal origins. Blood 67:739, 1986 22. Cleary ML, Nalesnick MA, Shearer WT, Sklar J: Clonal analysis of transplant-associated lymphoproliferations based on the structure of the genomic termini of the Epstein-Barr virus. Blood 72:349, 1988 23. Smith SD, Morgan R, Link MR, McFall P, Hecht F: Cytogenetic and immunophenotypic analysis of cell lines established from patients with T cell leukemidlymphoma. Blood 67:650, 1986 24. Weiss LE, Hu E, Wood GS, Moulds C, Cleary ML, Wamke R, Sklar J: Clonal rearrangements of T-cell receptor genes in mycosis fungoides and dermatopathic lymphadenopathy. N Engl J Med 315:539, 1985 25. Lefranc MP, Rabbits T: Two tandemly organized human genes encoding the T-cell gamma constant region sequences show multiple rearrangements in different T-cell types. Nature 3 1 6:464, 1985 26. Hata S, Brenner MB, Krangel MS: Identification of putative human T cell receptor 6 complementary DNA clones. Science 238:678, 1987 27. Kwock S, Higushi R: Avoiding false positive with PCR. Nature 339:237, 1989 28. Sarkar G, Sommer SS: Shedding light on PCR contamination. Nature 343:27, 1990 29. Kodaira M, Kinashi T, Umemura I, Matsuda F, Noma T, Ono Y, Honjo T: Organization and evolution of variable region genes of the human immunoglobulin heavy chain. J Mol Biol 190:529, 1986 30. Lee KH, Matsuda F, Kinashi T, Kodaira M, Honjo T: A novel family of variable region genes of the human immunoglobulin heavy chain. J Mol Biol 195:761, 1987 31. Schroeder HWJ, Hillson JL, Perlmutter RM: Early restriction of the human antibody repertoire. Science 238:791, 1987 32. Humphries CG, Shen A, Kuziel WA, Capra JD, Blattner FR, Tucker PW: A new human immunoglobulin VHfamily preferentially rearranged in immature B-cell tumours. Nature 331:446, 1988 33. Berman JE, Mellis SJ, Pollock R, Smith CL, Suh H, Heinke B, Kowal C, Surti U, Chess L, Cantor CR, Alt FW: Content and organization of the human Ig VH locus: Definition of three new VH families and linkage to the Ig CHlocus. EMBO J 7:727, 1988 34. Sanz I, Kelly P, Williams C, Scholl S, Tucker P, Capra JD: The smaller human VHgene families display remarkably little polymorphism. EMBO J 8:3741, 1989 35. van Dijk KW, Mortari F, Kirkam PM, Schroeder Jr. HW, Milner ECB: The human immunoglobulin VH7 gene family consists of a small, polymorphic group of six to eight gene segments dispersed throughout the VH locus. Eur J Immunol 23:832, 1993 36. Ravetch JV, Sibenlist U, Korsmeyer S, Waldmann T, Leder P: Structure of the human immunoglobulin p locus: Characterization of embryonic and rearranged J and D genes. Cell 27:583, 1981 37. Yamada M, Wasserman R, Reichard BA, Shane S, Caton AJ, DAVl ET AL Rovera G: Preferential utilization of specific immunoglobulin heavy chain diversity and joining segments in adult human peripheral blood lymphocytes. J Exp Med 173:395, 1991 38. Naumovski L, Morgan R, Hecht F, Link MP, Glader BE, Smith SD: Philadelphia chromosome-positive acute lymphoblastic leukemia cell lines without classical breakpoint cluster region rearrangement. Cancer Res 48:2876, 1988 39. Covey LR, Ferrier P, Alt FW:VH to VHDJH rearrangement is mediated by the internal V, heptamer. Int Immunol 2:579, 1990 40. Yamada M, Hudson S, Toumay 0, Bittenbender S, Shane SS, Lange B, Tsujimoto Y, Caton AJ, Rovera G: Detection of minimal disease in hematopoietic malignancies of the B-cell lineage by using third-complementarity-determining region (CDR-111)-specific probes. Proc Natl Acad Sci USA 86:5123, 1989 41. Brisco MJ, Tan LW, Orsbom AM, Morley AA: Development of a highly sensitive assay, based on the polymerase chain reaction, for rare B-lymphocyte clones in a polyclonal population. Br J Haematol 75: 163, 1990 42. Jonsson OG, Kitchens RL, Scott FC, Smith RG: Detection of minimal residual disease in acute lymphoblastic leukemia using immunoglobulin hypervariable region specific oligonucleotide probes. Blood 76:2072, 1990 43. Deane M, Pappas H, Norton JD: Immunoglobulin heavy chain gene fingerprinting reveals widespread oligoclonality in B-lineage acute lymphoblastic leukaemia. Leukemia 5:832, 1991 44. Kitchingman GR: Immunoglobulin heavy chain gene VH-D junctional diversity at diagnosis in patients with acute lymphoblastic leukemia. Blood 81:775, 1993 45. Steenbergen EJ, Verhagen OJHM, van Leeuwen EF, von dem Borne AEG, van der Schoot CE: Distinct ongoing Ig heavy chain rearrangement processes in childhood B-precursor acute lymphoblastic leukemia. Blood 82:581, 1993 46. Steward CG, Goulden NJ, Katz F, Baines D, Martin PG, Langlands K, Potter MN, Chessels JM, Oakhill A: A polymerase chain reaction study of the stability of Ig heavy-chain and T-cell receptor b gene rearrangements between presentation and relapse of childhood B-lineage acute lymphoblastic leukemia. Blood 83:1355, 1994 47. Kiyoi H, Naoe T, Horibe K, Ohno R: Characterization of the immunoglobulin heavy chain complementarity determining region (CDR)-111sequences from human B cell precursor acute lymphoblastic leukemia cells. J Clin Invest 89:739, 1992 48. Cleary ML, Galili N, Trela M, Levy R, Sklar J: Single cell origin of bigenotypic and biphenotypic B-cell proliferations in human follicular lymphomas. J Exp Med 167:582, 1988 49. Potter MN, Steward CG, Oakhill A: Clonal instability in early B-lineage acute lymphoblastic leukemia. Blood 80:1630, 1992 (letter) 50. Rolink A, Melchers F: Molecular and cellular origins of B lymphocyte diversity. Cell 66:1081, 1991 51. Wasserman R, Yamada M, Ito Y, Finger LR, Reichard BA, Shane S, Lange B, Rovera G: VH gene rearrangement events can modify the immunoglobulin heavy chain during progression of Blineage acute lymphoblastic leukemia. Blood 79:223, 1992 52. Whitlock CA, Ziegler SF, Treiman LJ, Stafford JI, Witte ON: Differentiationof cloned populations of immature B cells after transformation with Abelson murine leukemia virus. Cell 3 2 9 3 , 1983 53. Tachibana N, Raimondi SC, Lauer SJ, Satain P, Dow LW: Evidence for a multipotential stem cell disease in some childhood Philadelphia chromosome-positive acute lymphoblastic leukemia. Blood 70:1458, 1987 54. Fialkow PH, Singer JW, Raskind WH, Adamson JW, Jacobson RJ, Bemstien ID, Dow LW, Najfeld V, Veith R: Clonal development, stem-cell differentiation, and clinical remissions in acute nonlymphocytic leukemia. N Engl J Med 317:468, 1987 55. Fialkow PJ, Jacobson RJ, Papayannopoulou T: Chronic my- From www.bloodjournal.org by guest on November 10, 2014. For personal use only. ORIGIN AND EVOLUTION OF BALL elocytic leukemia: Clonal origin in a stem cell common to the granulocyte, erythrocyte, platelet and monccyte/macrophage. Am J Med 63:125, 1977 56. Gale RP, Ben Hassat I: Hybrid acute leukemia. Br J Haematol 65261, 1987 57. Deane M, Norton JD: Immunoglobulin heavy chain variable region family usage is independent of tumor cell phenotype in human B lineage leukemias. Eur J Immunol 20:2209, 1990 58. Yamada M, Wasserman R, Lange B, Reichaxd BA, Womer RB, Rovera G: Minimal residual disease in childhood B-lineage lymphoblastic leukemia. Persistence of leukemic cells during the first 18 months of treatment. N Engl J Med 323:448, 1990 59. Billadeau D, Blackstadt M, Greipp P, Kyle RA, Oken MM, 62 1 Kay N, Van Ness B: Analysis of B-lymphoid malignancies using allele-specific polymerase chain reaction: A technique for sequential quantitation of residual disease. Blood 78:3021, 1991 60.Tycko B, Palmer JD, Link MP, Smith SD, Sklar J: Polymerase chain reaction amplification of rearranged antigen receptor genes using junction-specific oligonucleotides: Possible application for detection of minimal residual disease in acute lymphoblastic leukemia. Cancer Cells 7:47, 1989 61. Tycko B, Ritz J, Sallan S, Sklar J: Changing antigen receptor gene rearrangements in a case of early pre-B cell leukemia: Evidence for a tumor progenitor cell with stem cell features and implications for monitoring residual disease. Blood 79:481, 1992
© Copyright 2026