OligOmetastases: a NeW take ON MetaStatiC diSeaSe
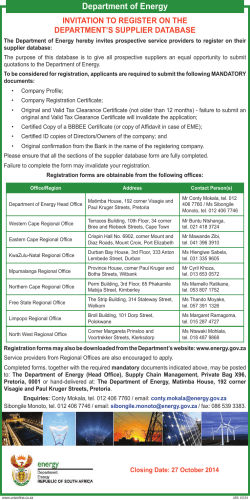
Rebecca Wong MBChB, MSc, FRCPC 2014. issue 1.volume 5 Radiation Medicine Program, Princess Margaret Cancer Centre, University Health Network 2013. issue 1.volume 4 Oligometastases: A New Take on Metastatic Disease Rebecca Wong MBChB, MSc, FRCPC Radiation Oncologist Professor, University of Toronto, Department of Radiation Oncology (UTDRO) Metastasis has historically been perceived as a systemic and incurable process for most adult solid tumours; this view has shaped our understanding of why cancer is difficult to beat. The concept of oligometastases challenges this paradigm and may provide the key to conquering cancer in our lifetime. Oligometastasis — a term coined by Hellman and Weichselbaum in 1995 — describes a state in which distant relapse is observed in only a limited number of locations. This intermediate state between localized and systemic disease may present an opportunity to cure. While the underlying mechanism remains uncertain, the “seed and soil” phenomenon and the interaction between cancer cells and our immune response, likely play critical roles in maintaining this state. For a subgroup of patients who present with a few metastatic lesions, local ablative therapies may provide prolonged disease-free and overall survival. The abscopal effect (shrinkage of tumours remote from the site of radiotherapy) provides further evidence that local ablative therapies, such as stereotactic body radiation therapy (SBRT), can modulate the immune system and influence the metastatic disease process. Continued on page 2. Oligometastases: A New Take on Metastatic Disease page 1 REBECCA WONG MBChB, MSc, FRCPC DID YOU KNOW? Page 3 Adult Radiation Late Effects Clinic (ARLEC): Improving Care Beyond Cure WILFRED LEVIN MBChB, FRCPC Clinical Trial HIGHLIGHT page 3 Rebecca Wong MBChB, MSc, FRCPC How to find us page 4 Recognition of Distinguished Service Dr. Mary Gospodarowicz was awarded the American Society for Radiation Oncology (ASTRO) Gold Medal, the Society’s highest honour in September 2014. The Gold Medal recognizes individuals who have made exceptional contributions and impact within the field of Radiation Oncology through their research, clinical care, teaching and service. Dr. Gospodarowicz is only the 5th Canadian to receive the ASTRO Gold Medal. The previous recipients include Drs. Bernard Cummings (2011), Walter Rider (1986), Harold Johns (1980) and Vera Peters (1979), all from the Princess Margaret Cancer Centre. Mary Gospodarowicz MD, FRCPC, FRCR(Hon) Radiation Oncologist, Professor, UTDRO “From the first consultation with Dr. Wong to the completion of radiation treatment, less than a month had elapsed. I find that incredibly reassuring — that all that can be done is being done!” —Doris Sonnenberg OLIGOMETASTASES continued Doris Sonnenberg had been feeling well since her initial diagnosis Doris Sonnenberg “I was immediately struck by Dr. Wong’s compassionate and caring nature. I thought this is someone I can trust to see me through this crisis.” —Doris Sonnenberg 2014. ISSUE 1. VOLUME 5 produced by the Radiation Medicine Program at Princess Margaret Cancer Centre Editor John Kim MD ISSUE EDITOR Stephen Breen PhD Editorial Board Andrea Bezjak MD Anthony Brade MD Caroline Chung MD Nicole Harnett MRT(T) Emma Ito PhD Richard Tsang MD and treatment of breast cancer over 17 years ago. However, lower back pain led to repeated diagnostic imaging, revealing two bone metastases in her pelvis. A course of ablative stereotactic radiotherapy to her pelvis was recommended, and six years later, Doris remains disease-free. She continues to be on hormone therapy. “The cancer is stable, I feel great and I’m able to look after three grandchildren on a regular basis. My husband and I celebrated our 50th wedding anniversary in Hawaii this year with all the children and grandchildren.” Doris’ case illustrates the effectiveness of SBRT — the precise delivery of a few very high doses of radiation to the tumour — in managing oligometastatic disease. The Princess Margaret Cancer Centre is a world leader in SBRT. It is one of the few centres worldwide offering SBRT to lung, liver and paraspinal cancer patients since 2005. Last year, the Radiation Medicine Program (RMP) opened its first Phase II clinical trial for multisite oligometastases (see Clinical Trial Highlight), examining the efficacy and safety of treating up to five metastatic lesions with SBRT. The effects of hypoxia on clinical outcome, the immune response of SBRT, as well as molecular biomarkers of the oligometastatic state are also being investigated. The findings from this study will be critical to unraveling the mysteries of the oligometastatic state. Answers to key questions, such as “How do we identify patients who are truly in the oligometastatic state?”, “What is the most effective way of achieving ablation of all metastases and maintenance of a disease-free state?” and “How do we convert patients with diffuse metastases to the potentially curable oligometastatic state?” will provide important clues that may make it possible to conquer cancer in our lifetime. Photography Donna Santos, Donna Santos Studio Princess Margaret Cancer Foundation layout Meta Antolin, Metagrafix Design In the next issue… PERSONALIZED MEDICINE AND GENOMIC TESTING 2 radiationatpmh.com Hardy Sonnenberg, Jeffrey Link, Doris Sonnenberg, REBECCA WONG Clinical TrIAl Highlight Rebecca Wong MBChB, MSc, FRCPC Radiation Oncologist Professor, UTDRO The Radiation Medicine Program is committed to improving therapies and outcomes for cancer patients through innovative clinical studies. A prospective Phase II oligometastases SBRT trial is currently being conducted at the Princess Margaret Cancer Centre and is actively accruing patients. Wilfred Levin MBChB, FRCPC Adult Radiation Late Effects Clinic (ARLEC): Improving Care Beyond Cure Wilfred Levin MBChB, FRCPC Radiation Oncologist Assistant Professor, UTDRO For over a decade, ARLEC at the Princess Margaret Cancer Centre — the only one of its kind in Canada — has helped approximately 800 patients nationwide with radiation late effects. Radiation late effects are due to normal tissue injuries that manifest months to years after completion of radiotherapy and occur in the irradiated volume. The pathogenesis involves a metabolically active and ongoing inflammatory response, which results in the excessive production of fibrous tissue (scarring) and microvascular damage (endarteritis). By impeding the progression of these damaging effects, particularly when caught early, tissue toxicity can be limited and treated. Phase II Study on the Toxicity and Efficacy of a Normal Tissue Tolerance Adapted, 5-Fraction Stereotactic Body Radiation Therapy (SBRT) Regimen for Extra-Cranial Oligometastases PI – Rebecca Wong This ongoing clinical trial evaluates the efficacy and toxicity of treating patients with oligometastatic spread (up to five metastatic lesions) with an aggressive SBRT regimen (25-50 Gy/5 fractions) adapted to normal tissue tolerances. Eligible Patients: Patients with any controlled solid primary tumour type with a maximum of five metastatic lesions, including at least one lesion that is suitable for SBRT. Patients should not have had prior radiotherapy to any of the sites of metastatic disease and no chemotherapy planned within two weeks of intended radiotherapy. For more information, see ClinicalTrials.gov Identifier: NCT01761929 Patients can present with late effects affecting all body systems and with varying grades of severity. Symptoms may include hemorrhagic proctitis, cystitis, enteritis, vaginitis, osteoradionecrosis, non-healing ulcers, breast swelling and fibrosis, muscle fibrosis, neuropathies and soft tissue necrosis. Anti-inflammatory, anti-fibrosis and anti-oxidant agents, as well as vasoactive drugs, physiotherapy and hyperbaric oxygen therapy have been shown to be effective in the management of late effects. ARLEC is currently open to patients one afternoon per week. Patients will have their specific symptoms assessed and treated by radiation oncologists with specialized expertise in late radiation toxicities, who are committed to advancing research in late effects. ARLEC is currently leading studies addressing the reversal of tissue fibrosis and radiation repair, and anticipates examining the role of stem cells in tissue regeneration. To refer your patients to ARLEC, please fax: 416-946-4442 to the attention of Drs. Wilfred Levin and Robert Dinniwell. radiationatpmh.com Rotational delivery techniques (blue lines) produce a highly conformal dose distribution (yellow) around the oligometastasis (red), sparing adjacent normal tissue. Radiation Medicine Program at the Princess Margaret 3 For your referrals We offer three ways to facilitate your requests for consultation: 2. Princess Margaret New Patient Referral Centre 1. Site Group Coordinators Site group coordinators serve as a liaison for referring physicians, radiation oncologists and the Princess Margaret Patient Referral Centre. 3. Direct to Specific Radiation Oncologists Tel: 416.946.4575 Fax: 416.946.2900 Referrals to specific radiation oncologists should be directed to site group coordinators. Palliative Radiation Oncology Program (PROP) Emergencies For patients requiring same day Direct palliative referral patients to our PROP coordinator. Within 24 hours, she will contact you with an appointment. Patients will be seen within a few days. [email protected] consultations (e.g. spinal cord compression), please contact our Palliative Radiation Oncology referral coordinator (416.946.2902) who will identify the radiation oncologist that is best able to respond to your requests. Coordinator Novlette Douglas Tel: 416.946.2902 Fax: 416.946.4657 [email protected] Leader Dr. Jolie Ringash Tel: 416.946.2919 [email protected] For After-Hour Requests Please page the radiation oncologist on call through the switchboard at 416.946.2000. updated November 2014 Breast CNS Endocrine EYE Coordinator Anila Samji Coordinator Alannah Pyke Coordinator Novlette Douglas Coordinator Alannah Pyke [email protected] [email protected] [email protected] [email protected] Leader Dr. Anne Koch Tel: 416.946.2122 Leader Dr. Normand Laperriere Tel: 416.946.2127 Leader Dr. James Brierley Tel: 416.946.2124 Leader Dr. Normand Laperriere Tel: 416.946.2127 [email protected] [email protected] [email protected] [email protected] Gastrointestinal Genitourinary Gynaecological Head and Neck Coordinator Anila Samji Coordinator Anila Samji Coordinator Anila Samji Coordinator Ellen Hoffman [email protected] [email protected] [email protected] [email protected] Leader Dr. John Kim Tel: 416.946.2126 [email protected] Leader Dr. Charles Catton Tel: 416.946.2121 [email protected] Leader Dr. Michael Milosevic Tel: 416.946.2932 [email protected] Leader Dr. John Waldron Tel: 416.946.6522 Lung Lymphoma Pediatrics Coordinator Alannah Pyke Coordinator Novlette Douglas Multi-Disciplinary Brain Mets clinic Coordinator Alannah Pyke Tel: 416.946.2902 Fax: 416.946.4657 [email protected] Tel: 416.946.2130 Fax: 416.946.4657 Tel: 416.946.4501 x3639 Fax: 416.946.4657 Tel: 416.946.4501 x3639 Fax: 416.946.4657 Tel: 416.946.2130 Fax: 416.946.4657 [email protected] Tel: 416.946.2130 Fax: 416.946.4657 Tel: 416.946.4501 x3639 Fax: 416.946.4657 Tel: 416.946.2902 Fax: 416.946.4657 Leader Dr. Alex Sun Tel: 416.946.2126 Leader Dr. Richard Tsang Tel: 416.946.6513 [email protected] [email protected] Tel: 416.946.2902 Fax: 416.946.4657 Tel: 416.946.4501 x3639 Fax: 416.946.4657 [email protected] Leader Dr. Caroline Chung Tel: 416.946.6513 Tel: 416.946.2130 Fax: 416.946.4657 Tel: 416.946.6522 Fax: 416.946.2111 [email protected] Coordinator Novlette Douglas [email protected] Leader Dr. David Hodgson Tel: 416.946.2121 [email protected] [email protected] Sarcoma skin Unknown Primary Coordinator Maria Prentice Coordinator Maria Prentice Coordinator Novlette Douglas [email protected] [email protected] [email protected] Leader Dr. Brian O’Sullivan Tel: 416.946.2125 Leader Dr. Alex Sun Tel: 416.946.2126 [email protected] Leader Dr. Jolie Ringash Tel: 416.946.2919 [email protected] Tel: 416.946.4575 Fax: 416.946.2900 [email protected] Tel: 416.946.4575 Fax: 416.946.2900 Tel: 416.946.2902 Fax: 416.946.4657 © 2 014 Radiation Medicine Program Princess Margaret Cancer Centre radiationatpmh.com Radiation Medicine Program at the Princess Margaret
© Copyright 2026