Eradication of minimal disease in severe combined immunodeficient an
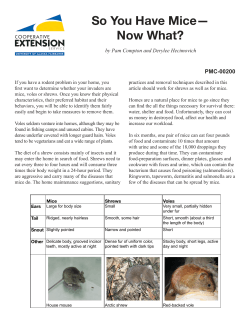
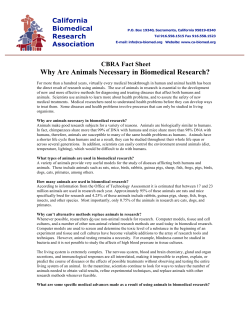
From www.bloodjournal.org by guest on November 17, 2014. For personal use only. 1994 84: 702-707 Eradication of minimal disease in severe combined immunodeficient mice with disseminated Daudi lymphoma using chemotherapy and an immunotoxin cocktail MA Ghetie, K Tucker, J Richardson, JW Uhr and ES Vitetta Updated information and services can be found at: http://www.bloodjournal.org/content/84/3/702.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved. From www.bloodjournal.org by guest on November 17, 2014. For personal use only. RAPID COMMUNICATION Eradication of Minimal Disease in Severe Combined Immunodeficient Mice With Disseminated Daudi Lymphoma Using Chemotherapy and an Immunotoxin Cocktail By M.-A. Ghetie, K. Tucker, J. Richardson, J.W. Uhr, and E.S. Vitetta Severe combined immunodeficient (SCID) mice injected intravenously with ahumanBurkitt’slymphoma cell line (Daudi) develop disseminated lymphoma (SCID/Daudi), which is fatal in 100% of the mice. Earlytreatment of these mice with either an immunotoxin (IT) cocktail (consisting of anti-CD19-ricin A chain plus anti-CD=-ricin A chain) or chemotherapy significantly prolonged survival but was not curative. Combination therapywith the IT cocktail and any one of three chemotherapeutic drugs (doxorubicin, cytoxan, or camptothecin) cured the mice. Cure was demonstrated by both histopathologic examination of treated mice and, more importantly, by adoptive transferof cells from organs of the cured miceto naive SCID micewhere 100 tumor cells would have caused disease in the recipients. These results provide a strong rationale for combining IT therapy with conventional chemotherapyin the treatment of B-cell neoplasia. 0 1994 by The American Societyof Hematology. C phosphamide), doxorubicin, and methotrexate, as well as a less commonly used drug, camptothecin, which has recently been re-evaluated for the therapy of human carcinoma^.^"^ Neither doxorubicin nor methotrexate has beenusedin combination with ITS.The most significant therapeutic effect of either drug alone was achieved using an immunoconjugate containing doxorubicin and the BR96 antibody. This conjugate cured xenografted human lung, breast, and colon carcinomas grown subcutaneously in athymic mice. This conjugate also cured 70%of mice with metastatic human lung carcinoma.I’ Liposome-encapsulated doxorubicin has also been used to eradicate lung cancer in The toxicity of doxorubicin to the gastrointestinal tract and myocardium is reduced whenthe drug is administered in encapsulated form. In a phase I clinical trial, TLCD-99 (doxorubicin encapsulated in liposomes) was well-tolerated andproduced fewer side effects than would be expected with nonencapsulated drug at equal doses.“ Clinical trials with camptothecin in its water-soluble form were discontinued because of severe However, new derivatives of camptothecin have been used with some success in phase I1 clinical studies in patients with refractory leukemia and lymphomaI7 and in phase I and I1 studies in patients with advanced non-small cell lung carcinoma” or with gynecologic cancers.” Complete inhibition of the growth of human malignant melanoma cells in vitro and regression of human melanoma xenografts,’ breast xenografts,” and ovarian carcinomas” in nude mice have also been induced with camptothecin. These studies suggested that a combination of ITS and different chemotherapeutic regimens might improve the efficacy of ITS reactive with human B lymphoma. This study shows that therapy with a cocktail of two ITS (anti-CD22-dgA and anti-CD19-dgA) plus a single chemotherapeutic agent cures human Burkitt’s lymphoma (Daudi cells) in SCID mice with no evidence of minimal residual disease or dormant tumor cells. ONVENTIONAL APPROACHES to the treatment of B-cell lymphoma have emphasized the use of cytotoxic agents that cancure 30%to 50% of high-grade lymphomas, but not low-grade lymphomas.’,2We have used our severe combined immunodeficient (SCID)/Daudi model of disseminated human Burkitt’s B lymphoma3 for preclinical evaluation of different immunotoxin (IT) constructs containing either anti-CD22 or anti-CD19 antibodies and deglycosylated ricin A chain (dgA).4,5These ITS have also been used in over 100 patients in phase VI1 clinical trials in patients with refractory non-Hodgkin’s lymphoma (NHL)6,7 and (Stone et al, unpublished data; Sausville et al, unpublished data, Kaplan et al, unpublished data, 1994). Our previous studies have shown that neither Fab’ nor IgG anti-CD22 (RFB4)-dgA4 or IgG anti-CD19 (HD37)dgA5 cured SCIDDaudi mice with early disease, although survival was significantly prolonged. A combination of the two ITS or a combination of anti-CD22-dgA and anti-CD19 antibody (without dgA) extended survival of SCID/Daudi mice significantly longer than either treatment alone. Thus far, the only combination treatment that has been curative in SCID mice was a large amount of anti-CD19 antibody and the anti-CD22-immunotoxin, RFB4-dgA. The mice treated with this combination survived more than 1 year, at which timethey appeared tumor free.8Inthe present study we compare the therapeutic effect of combination treatment with chemotherapy and ITS. We selected three chemotherapeutic drugs that are commonly used in humans: cytoxan (cyclo- From the Cancer Immunobiology Center, the Department of Pathology, and the Department of Microbiology, University of Texas Southwestern Medical Center at Dallas. Submitted April 4, 1994; accepted May 17, 1994. Supported by National Institutes of Health Grants No. CA-28149 and CA-41087. Address reprint requests to E.S. Vitetta, PhD, Cancer Immunobiology Center and Department of Microbiology, 6000 Harry Hines Blvd, Dallas, lX 75235-8576. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “adveaisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 I994 by The American Society of Hematology. 0006-497//94/8403-0038$3.00/0 702 MATERIALS AND METHODS Cells. The Burkitt’s lymphoma cell line Daudi was maintained in culture by serial passage in RMPI 1640 medium containing 25 mmol/L HEPES, 10% heat-inactivated fetal bovine serum, 100 U/ mL penicillin, 100 pg/mL streptomycin, and 100 mmoVL L-glutamine (complete medium). The cells were grown in a humidified Blood, VOI 84, NO 3 (August l), 1994: PP 702-707 From www.bloodjournal.org by guest on November 17, 2014. For personal use only. IMMUNOTOXINS IN SCID/LYMPHOMA 703 atmosphere of 5% CO2and air. Cells were used for intravenous (IV) inoculation of SCID mice. Cell viability was determined by trypan blue exclusion. Animals. Female SCID mice (CB-l7 SCIDISCID) were purchased from the Harlan Sprague Dawley Laboratory (Madison, WI). They were housed and maintained in a specific pathogen-free (SPF) facility. Animals were fed autoclaved food and sterile water ad libitum, and all manipulations were performed in a laminar flow hood. Induction ofhumantumor in SCID mice. Six- to10-week old SCIDs were inoculated IVwith 5 X lo6 Daudi cells in 0.1 mL phosphate-buffered saline (PBS). Mice were monitored daily and killed at the onset of paralysis of both hind legs, a clinical symptom that preceeds death.3 (The mean paralysis time [MPT] has been established as the end point in this animal model.*) Complete necropsy and histopathologic examination were performed on several animals in each experimental group. Tissue from lung, heart, liver, spleen, kidney, ovary, and vertebrae were fixed in 10% buffered formalin, embedded in paraffin, sectioned, and stained with hematoxylin and eosin. Therapy of SCIDDaudi mice. SCID mice were inoculated with 5 x lo6 Daudi cells 24 hours before treatment. In each experiment, four groups of 5 to 10 mice with an average weight of 20 g were used and treatment was administered on days 1 through 4 after tumor injection as follows: (1) control mice were injected retroorbitally (RO) with PBS or saline; (2) mice were injected R 0 with an IT cocktail (WB4-dgA [60 pg] + HD37-dgA [60 pg]); (3) mice received either one of the following chemotherapeutic drugs: methotrexate (1 12 pg), doxorubicin (80 pg), cytoxan (1.6 mg), or camptothecin (640 pg) (all chemotherapeutics but camptothecin were administered IV on days 1 through 4 divided into four equal amounts; camptothecin was injected intramuscular (IM) in an emulsion in intralipid two times per week for 4 weeks); (4) mice were administered a combination of treatments (2) and (3) as described above. When therapy was initiated, the SCID mice had 1 X lo7disseminated Daudi cells as described el~ewhere.~ Adoptive transfer. Mice surviving for 150 to 200 days were killed and cells from ovaries and spinal cords' were injected IV into healthy SCID mice. Adoptive recipients were followed-up for 200 days. At this time, the transfer of 100 tumor cells should have caused death in the recipients.' Cytotoxic effect of different chemotherapeutic drugs alone or in combination with ITS. A Daudi killing assay for each drug (methotrexate, doxorubicin, cytoxan, and camptothecin) was performed as described else~here.*~ The inhibition of 'H-thymidine incorporation was used to determine individual ICs0s (M). The cytotoxic effect of a cocktail containing different amounts of anti-CD22-dgA and a constant amount of anti-CD19-dgA (eg, the ICso dose) andvice versa was also determined and compared with combination treatment using each IT plus either one of the chemotherapeutic drugs at a Table 1. Cytotoxic Effect of Dierent Chemotherapeutics on Daudi Cells In Vitro and on SCID Mice Chemotherapeutic Methotrexate Category Antimetabolite ICw (mollL) LDm Dose (mg/kg)* Not toxic u p to 14 2.2 x mol/L Doxorubicin Antibiotic 4.2 ? 1.3 X lo-' (3)t 10 200 Alkylating agent 8.8 t 1.6 x 10" (3)t Cytoxan 1.1 ? 0.2 X 10-9 (3)t ND Camptothecin Alkaloid Abbreviation: ND, not determined. Two mice were used to determine the LDm. t The number in parentheses is the number of experiments performed. Table 2. Antitumor Effect of DHerent Chemotherapeutic Drugs in SCID/Daudi Mice Drug Treatment (dose)* MW 2 SD (d) Control Methotrexate Cytoxan No treatment 40% LDW ( 1 12 pg) 20% LD5o (0.8mg) 40% LD50 (1.6 mg) 20% LDso (40 pg) 40% LDso (80/le) 40 pg X 8 = 320 pg 80 pg X 8 = 640 pg 31.7 t 2.6(10)t 31.6 ? 2.4 (5) 51.8 2 4.1 (5) 63.4 t 12.7 (11) 31.2 C 1.2 ( 1 1 ) 62.2 ? 13.6 (27) 44.4 t 9.7 (7) 74.7 ? 17.5 (12) ~ Doxorubicin Camptothecin ~~~ *All drugs but camptothecin were injected IV in four equal doses on days 1-4 after injection with tumor cells; camptothecin (sonicated in intralipid)was administered IM 2 times per week for 4 weeks. t The number in parentheses is the number of mice in each group. certain concentration (eg, the ICs0 dose). To determine whether the cytotoxic effect of combination treatment was additive or synergistic, an analysis using an algebraic method was performed and the combination index (CI) was calculated using the equation: C1 = A/Ae + BlBe < 1 (synergistic); = 1 (additive), where A and B are the concentrations of the two drugs that, in combination, kill 90% of the Daudi cells, and Ae and Be are the concentrations of the two drugs extrapolated from their individual killing curves and corresponding to 90% killing." Immunojuorescence assay. The phenotype of Daudi tumor grown in SCID mice has been previously de~cribed.~ To determine whether treatment with drugs generated CD22- or CD19- Daudi cells, we harvested tumors from doxorubicin-treated mice (ovary and spine) and as well as from untreated SCIDDaudi mice (ovary). Single-cell suspensions were prepared and cells were analyzed by indirect immunofluorescence, using the parental Daudi cells as a control." Cells were stained with the primary antibodies anti-CD22 and anti-CD19 followed by a fluorescein isothiocyanate (FITC)labeled goat-antimouse Ig (GAMIg). The cells were analyzed on a fluorescence-activated cell sorter (Becton-Dickinson, Oxnard, CA). RESULTS Cytotoxic effect of different Chemotherapeutic agents on Daudi cells. The chemotherapeutic drugs used in the SCJDDaudi model are described in Table 1. These drugs (methotrexate, cytoxan, doxorubicin, and camptothecin) induce antitumor effects by interacting with cellular DNA. As shown in the table, methotrexate didnot kill Daudi cells whereas doxorubicin and camptothecin had comparable IC50s m o m ) and cytoxan was less potent (ICso = mom). Antitumor effect of difSerent drugs in SCID/Daudi mice. Two different doses (20% and 40% of the LD50 dose) were administered to separate groups of SCIDDaudi mice.As shown in Table 2, methotrexate did not prolong survival of SCIDDaudi mice at the 40% LDS0 dose whereas the other three drugs gave dose-dependent prolongation of survival. Therefore, 40% of the LD50 dose of cytoxan or doxorubicin or 640 pg campothecin was used insubsequent experiments, because this dose induced a significant prolongation of MPT in SCIDDaudi mice. Furthermore, at this dose mice did not show toxic effects as determined by histopathologic examination. Phenotype of Daudi tumor inSCID mice treatedwith From www.bloodjournal.org by guest on November 17, 2014. For personal use only. 704 GHETIE ET AL Table 3. Effect of Treatment With Doxorubicin on the Phenotype of Residual Daudi Tumor in Treated SCID Mice % Positive Cells Untreated Daudi Staining Mice Mice Treated With Doxorubicin Antibody Parental Used for Anti-CD22 Anti-CD19 4.1 MOPC-21 83.8 87.6 4.3 64.2 91.7 2.1 79.9 97.1 2.8 86.4 93.8 doxorubicin. Daudi cells from SCID mice treatedwith 40% of the LDSodose of doxorubicin were analyzed for their CD19/CD22 phenotype. As shown in Table 3, residual tumor cells from treated mice had the same phenotype as parental Daudi cells andtumor cells from untreated mice. Hence, chemotherapy did not change the expression of the target antigens for the two ITS. Effect of combination therapy of SCID/Daudi mice. Chemotherapeutic drugs (doxorubicin, cytoxan, or camptothecin) significantly extended the MPT of treated mice as did treatment with a cocktail of the two ITS (anti-CD22-dgA + anti-CD19-dgA).' However, at the time of killing these mice showed the same pattern of tumor growth as control mice. The mice treated with any one of the chemotherapeutic drugs in combination with the cocktail of the two ITS survived over 150 days with no sign of paralysis (Fig 1). When gross and histopathologic examination was performed, none of these mice showed any sign of tumor. At least lo7 cells from ovary and spine were adoptively transferred into naive SCID mice. There was no evidence of tumor growth in recipients after 7 months, at whichtime the experiments were terminated. Because 100 Daudi cells are sufficient to cause progressive tumor in all the adoptive recipients at 5 months,' we considered the original donor mice to be cured. Synergistic effect of treatment with a cocktail of ITS plus chemotherapeutic drugs in Daudi cells. Both ITS have a significant cytotoxic effect on Daudi cells with ICsos of 5.0 X lo"* mol/L (RFBCdgA) and 4.5 X lo-" moVL (HD37dgA).' The combination of the two ITS (Fig 2A) or each of the two ITS together with a single chemotherapeutic drug had an enhanced cytotoxic effect, which is shown inFig 2, B and C. Figure 2D shows the cytotoxic effect of each chemotherapeutic drug. The analysis (algebraic method)" of the cytotoxic effect of combination treatment shows that the addition of chemotherapeutic drugs to the two ITS induced a synergistic cytotoxic effect on Daudi cells because the C1 was < 1 for 90% killing. The data in Table 4 show that the combination of the two ITS or one IT plus one chemotherapeutic drug increases the cytotoxic effect on Daudi cells and that the cytotoxic effect is synergistic. DISCUSSION The objective of the present study was to compare the antitumor activity of different chemotherapeutic drugs alone or in combination with the two ITS used in other studies in SCID/Daudi mice4,5,8 as well as in clinical trials6.' (and Stone so 2 100 150 PARALYSIS T I M t ( d a y s ) " . 50 . . 1 00 l50 PARALYSIS TIME (days) C 100 - 80 > W 2 60 k z 40 W W a 20 0 100 PARALYSIS TIME ( d a y s ) 50 0 150 Fig 1. A combination of a cocktail of two ITS (anti-CD22-dgA + anti-CD19-dgA) and chemotherapeutic drugs in SCID/Daudi mice induces complete inhibition of tumor growth: (A) cocktail of ITS + doxorubicin (40% of theLDw administered in 4 equal doses); (B) cocktail of ITS cytoxan (40% of LDw administered in 4 equal doses); (C) cocktail of ITS camptothecin (totaldose = 640 p g administered in 8 equal doses [2 times per week for 4 weeks]). SClDmice wereinoculated IV with Daudi cells (5 x lo6 per mouse) and were treated as follows: (0) saline (control) (10 mice); (A)chemotherapeutic drugs only: doxorubicin, cytoxan, or camptothecin (10 mice); (0)cocktail of two I T S (RFB4-dgA + HD37-dgA) (20% of LDS each, totaling 120 p g administered in 4 equal doses) (10 mice); ( ) chemotherapeutic drug (any one above) plus cocktail oftwo ITS (10 mice). The percent of survivors is plotted against the paralysis time. Each panel shows a representative experiment of two t o four performed. + + From www.bloodjournal.org by guest on November 17, 2014. For personal use only. L 0 U I 0-1' 1 o+ 10"' IT concentrotion (M) 1 o-'L 1 o"6 IO"' 1 0-12 IT concentration (M) 10"' \ 10 - I S 1 0-11 IT concentration (M) 1 0-g 10"O 1 0-B 10" 1 0" Chernotheropeuticconcentrotion (M) 1 o-2 Fig 2. Cytotoxic effect of combination treatment was analyzed on Daudi cells(1 x 105/we11/200pLl as follows: (A) anti-CD22-dgA (0);antiCDl9-dgA (0);anti-CDP2-dgA (2.8 x lo-' to 2.8 x 10"' mol/L) plus anti-CD19-dgA at 2.8 x 10"' mollL (A); anti-CD19-dgA (2.8 x lo-' to 2.8 x 10"' mollLI plus anti-CD22-dgA at 2.8 x 10"' mol/L (AI; (B) anti-CD22-dgA alone (0)or anti-CD22-dgA (2.8 x 10"' t o 2.8 x lo-" mollLI plus doxorubicin at 9.2 x 10" mol/L (A);or plus cytoxan at 9.0 x 10" mollL (M); or plus camptothecin at 1.4 x 10"' mollL (0);(Cl anti-CD19dgA alone (0)or anti-CD19-dgA (2.8 x lo-' t o 2.8 x 10"' mol/L) plus doxorubicin at 9.2 x lo-' mol/L (AI; or plus cytoxan at 9.0 x 10" moll L (M); or plus camptothecin at 1.4 x 10"' mol/L (0);(D) doxorubicin (01;camptothecin (Dl; cytoxan (A).The plates with cells were incubated for 24 hours, pulsed with IaHl-thymidinefor 18 hours, harvested, and counted. The reduction of incorporation of cells treated with ITS (percent of control) was plotted against the concentration. et al, unpublished data; Sausville et al, unpublished data, Kaplan et al, unpublished data, 1994). In a previous study,' we showed that SCIDDaudi mice treated with a combination of anti-CD22-dgA (20% of LD50dose) and large amounts of F(ab'), fragments of anti-CD19 antibodies were tumorfree 1 year after treatment. The present study was undertaken inan attempt tofind less expensive but equally effective curative therapies for minimal disease in SCIDDaudi mice. Our major finding is that chemotherapy and immunotoxins have synergistic antitumor activity in vitro and cure SCID mice with disseminated B lymphoma. The in vitro studies of Daudi cells treated with methotrexate, doxorubicin, cytoxan, or camptothecin showed that: (1) methotrexate was not effective at killing Daudi cells either because it must be metabolized by the liver to be active or the Daudi cells are naturally resistant to this drug; (2) Daudi cells were very sensitive to both doxorubicin and carnptothecin, with an IC5o of m o m ; (3) cytoxan was less cytotoxic for Daudi cells and its lower toxic effect (IC50 = m o m ) was consistent with its higher LDso in mice. The doses chosen for in vivo studies (20% and 40% of the LD50doses) for methotrexate, doxorubicin, and cytoxan, and 640 pg for camptothecingwere administered safely with no signs of toxicity. Because methotrexate did not extend the MPT at 40% of the LD5,,, it was not used in combination with the ITS in vivo. In a previous studywe have shown that a cocktail of two ITS (anti-CD22-dgA and anti-CD19-dgA) extended survival of SCIDDaudi mice in a manner consistent with the killing of 6 logs of tumor cells (50% of mice survived over 100 days).' In this study, we combined the two therapies known to be effective individually and show that the combination of the two ITS and one of the above chemotherapeutic agents had a synergistic effect in vitro and eradicated disseminated minimal disease in vivo.Our studies confirmand extend earlier reports that ITS and mafosfamid eliminated From www.bloodjournal.org by guest on November 17, 2014. For personal use only. 706 GHETIE ET AL Table 4. Increase of IT'SCytotoxic Effect When Used in Combination With Each Other or With Chemotherapeutics Drug None Doxorubicin§ Cytoxanll Camptothecinf Anti-CDZZ-dgA Anti-CD19dgA +* - - +* +* +t 0.08 +S +* 0.03 +* - 0.005 - +* +* ICso rnol/L X 10." 1.2 22 - 0.08 0.00004 - +* 0.0007 +* - 0.004 - +* 0.32 ~~~~ ~ For each combination above, a Cl was calculated using the formula Cl = NAe + B/Be (see Materials and Methods)21;for 90%killing of Daudi cells, the Cl was < l for all the combinations in the abovetable meaning that the effect was synergistic. * Each IT was titrated from2.8 x IO-' to 2.8 x mol/L. t Anti-CD19-dgAwas added at 2.8 x IO"' mol/L. Anti-CD22-dgAwas added at 2.8 x IO'" mol/L. § Doxorubicin was added at 9.2 x IO-' mol/L. 11 Cytoxan was added at 9.0 x mol/L. f Camptothecin was added at 1.4 x IO"' mol/L. * neoplastic T cells from autologous marrow grafts before bone marrow transplantation" and induced a greater antitumor effect than either therapy alone in human solid tumors (T-ALL) grown in nude mice.23In addition, an anti-CD19pokeweed antiviral protein (PAP) IT in combination with cyclophosphamide was highly effective against human t(4; 1I ) leukemia and CALLA' Cp' human pre-B ALL in SCID mi~e.'~.'~ The antitumor activity of two ITS (SNI-RA and SNZRA) directed against human T leukemia in nude mice was potentiated by recombinant a-interferon and daunorubicin." Doxorubicin has not been used previously in combination therapy with ITS, but it has been shown that immunoconjugates containing doxorubicin and a tumor-reactive antibody cured several xenografted human tumors in athymic mice.13 The toxicity of doxorubicin in SCID miceI5 and humans" has been circumvented by multiple injections at lower doses. The fact that mice treated with combination therapy (cocktail of ITS and doxorubicin) were tumor free at 200 days was supported by the adoptive transfer experiment which gave no evidence for the presence of residual tumor cells. In summary, our results support the rationale of using chemotherapy together with an immunotoxin cocktail to treat early and/or minimal disease. ACKNOWLEDGMENT We thank Cindy Patterson for expert secretarial assistance. We are indebted to Dr P. Pantazis for providing campothecin and Dr V. Ghetie for preparing the immunotoxins. REFERENCES 1. DeVita VT, Jaffe ES, Mauch P, Longo DL: Lymphocytic lymphomas, in DeVita VT, Hellman S, Rosenberg SA (eds): Cancer: Principles and Practice of Oncology. Philadelphia, PA, Lippincott, I989 2. Armitage JO, Fyfe MA, Lewis J: Long-term remission durability and functional status of patients treated for diffuse histiocytic lymphoma with the CHOP regimen. J Clin Oncol 22398, 1984 3. Ghetie MA, Richardson J, Tucker T, Jones D, Uhr JW, Vitetta ES: Disseminated or localized growth of a human B cell tumor (Daudi) in SCID mice. Int J Cancer 45:481, 1990 4. Ghetie MA, Richardson J, Tucker T, Jones D, Uhr JW, Vitetta ES: Antitumor activity of Fah' and IgG-anti-CD22 immunotoxins in disseminated human B-lymphomas grown in mice with severe combined immunodeficiency disease: Effect on tumor cells in extranodal sites. Cancer Res SI 5876, 1991 5. Ghetie MA, Tucker K, Richardson J, Uhr JW, Vitetta ES: The anti-tumor activity of an anti-CD22-immunotoxin in SCIDmice with disseminated Daudi lymphoma is enhanced by either an anti-CD 19 antibody or an anti-CD19 immunotoxin. Blood 80:231S, 1992 6. Vitetta ES, Stone M, Amlot P, Fay J, May R, Till M, Newman J, Clark P, Collins R, Cunningham D, Ghetie V, Uhr JW, Thorpe PE: A phase I immunotoxin trial in patients with B cell lymphoma. Cancer Res 15:4052, 1991 7. Amlot PL, Stone MJ, Cunningham D, Fay J, Newman J, Collins R, May R, McCarthy M, Richardson J, Ghetie V, Ramilo 0, Thorpe PE, Uhr JW, Vitetta ES: A phase-I study of an anti-CD22deglycosylated ricin-A chain immunotoxin in the treatment of Bcell lymphomas resistant to conventional therapy. Blood 82:2624, 1993 8. Ghetie MA, Picker LJ, Richardson JA, Tucker K, Uhr JW, Vitetta ES: Anti-CD19 inhibits the growth of human B cell tumor lines in vitro and of Daudi cells in SCIDmice by inducing reversible cell cycle arrest. Blood 83:1329, 1994 9. Pantazis P, Heinz HR, Mendoza JT, Kozielski AI, Williams LJ, Stehlin JS, Giovanella BC: Complete inhibition of growth followed by death of human malignant melanoma cells in vitro and regression of human melanoma xenografts in immunodeficient mice by camptothecins. Cancer Res 52:3980, 1992 IO. Pantazis P, Kozielski AJ, Mendoza JT, Early JA, Hinz HR, Giovanella BC: Camptothecin derivatives induce regression of human ovarian carcinomas grown in nude mice and distinguish between non-tumorigenic and tumorigenic cells in vitro. Int J Cancer 53:863, 1993 11. Pantazis P, Early JA, Kozielski A J , Mendoza JT, Hinz HR. Giovanella BC: Regression of human breast carcinoma tumors in immunodeficient mice treated with 9-nitrocamptothecin: Differential response of nontumorigenic and tumorigenic human breast cells in vitro. Cancer Res 53:1577, 1993 12. Potmesil M: Camptothecins: From bench research to hospital wards. Cancer Res 54:1431, 1994 13. Trail PA, Willner D, Lasch SJ, Henderson AJ, Hofstead S, Casazza AM, Firestone RA, Hellstrom I, Hellstrom KE: Cure of xenografted human carcinomas by BR96-doxorubicin immunoconjugates. Science 261:212, 1993 14. Ahmad I, Longenecker M, Samuel J, Allen TM: Antibodytargeted delivery of doxorubicin entrapped in sterically stabilized liposomes can eradicate lung cancer in mice. Cancer Res S3:1484, I993 15. Williams SS, Alosco TR, Mayhew E, Lasic DD, Martin FJ, Bankert RB: Arrest of human lung tumor xenograft growth in severe combined immunodeficient mice using doxorubicin encapsulated in sterically stabilized liposomes. Cancer Res 53:3964, 1993 16. Cowens JW, Creaven PJ, Greco WR, Brenner DE, Tung Y, Ostro M, Pikiewicz F, Ginsberg R, Petrelli N: Initial clinical (Phase I) trial of TLC D-99 (doxorubicin encapsulated in liposomes). Cancer Res 53:2796, 1993 17. Ohno R, Okada K, Masaoka T, Kuramoto A, Arima T, Yoshida Y, Ariyoshi H, Ichimani M, Sakei Y, Oguro M, Ito Y, Morishina Y, Yokomaku S, Ota K: An early phase I1 study of C m - I 1: From www.bloodjournal.org by guest on November 17, 2014. For personal use only. IMMUNOTOXINS IN SCID/LYMPHOMA A new derivative of camptothecin for the treatment of leukemia and lymphomas. J Clin Oncol 8:1907, 1990 18. Negoro S, Fukuoka M, Masuda N, Takada M, Kusunoki Y, Matsui K, Takifugi N, Kudoh S, Niitani H, Taguchi T: Phase I study of weekly intravenous infusions of CPT-11, a new derivative of camptothecin, in the treatment of advanced non-small-cell lung cancer. J Natl Cancer Inst 83:1164, 1991 19. Takeuchi S, Dobashi K, Fujimoto S, Tanaka K, Suzuki M, Terashima Y, Hasumi K, Akiya K, Negishi Y, Tamaya T, Tanizawa 0, Sugawa T, Umesaki N, Sekiba K, Aono T, Nakano H, Noda K, Shiota M, Yakushiji M, Sugiyama T, Hashimoto M, Yajima A, Takamizawa H, Sonoda T, Takeda Y, Tomoda Y,Ohta M, Ozaki M, Hirabayashi K, Hiura M, Hatae M, Nishigaki K, Taguchi T: A late phase I1 study of CPT-1 1 on uterine cervical cancer and ovarian cancer. Jpn J Cancer Chemother 18:1681, 1991 20. Ghetie MA, May RD, Till M, Uhr J W , Ghetie V, Knowles PP, Relf M, Brown A, Wallace PM, Janossy G , Amlot P, Vitetta ES, Thorpe PE: Evaluation of ricin A chain-containing immunotoxins directed against CD19 and CD22 antigens on normal and malignant human B-cells as potential reagents for in vivo therapy. Cancer Res 48:2610, 1988 21. Berenbaum MC: Synergy, additivism and antagonism in immunosuppression. A critical review. Clin Exp Immunol 28:1, 1977 22. Uckun FM, Ramakrishnan S, Haag D, Houston LL: Ex vivo 707 elimination of lymphoblastic leukemia cells from human marrow by mafosfamid. Leuk Res 9:83, 1985 23. Weil-Hillman G , Uckun F M , Manske JM, Vallera DA: Combined immunochemotherapy of human solid tumors in nude mice. Cancer Res 47579, 1987 24. Jansen B, Kersey JH, Jaszcz WB, Gunther R, Nguyen DP, Chelstrom LM, Tuelahlgren L, Uckun FM: Effective immunochemotherapy of human t(4; 11) leukemia in mice with severe combined immunodeficiency (SCID) using B43 (anti-CD19)-pkeweed antiviral protein immunotoxin plus cyclophosphamide. Leukemia 7:290, 1993 25. Uckun FM, Chelstrom LM, Finnegan D, Tuel-Ahlgren L, Manivel C, Irvin JD, Myers DE, Gunther R: Effective immunochemotherapy of CALLA+ Cp+ human pre-B acute lymphoblastic leukemia in mice with severe combined immunodeficiency using B43 (anti-CD19) pokeweed antiviral protein immunotoxin plus cyclophosphamide. Blood 79:3116, 1992 26. Yokota S , Hara H, Luo Y, Seon BK: Synergistic potentiation of in vivo antitumor activity of anti-human T leukemia immunotoxins by recombinant a-interferon and daunorubicin. Cancer Res 50:32, 1990 27. Valdivieso M, Burgess MA, Ewer MS, Mackay B, Wallace S, Benjamin RS, Ali MA, Bodey GP, Freireich ET: Increased therapeutic index of doxorubicin in the therapy of non-small cell lung cancer: A prospective, randomized study. J Clin Oncol 2:207, 1984
© Copyright 2026