Document 57805
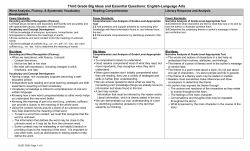
Strategies for Treating Elementary School-Age Children Who Stutter: An Integrative Approach E. Charles Healey Lisa A. Scott University of Nebraska-Lincoln, Lincoln clinician working in the public schools can play a significant role in helping children manage their fluency problems, particularly in the early stages of the disorder. Yet, research by Mallard, Gardner, and Downey (1988) showed that only 24% of the school-based speech-language pathologists with a master's degree have confidence in their ability to treat this disorder. Approximately 60% of school-based clinicians with a master's degree reported that they "need direction" in developing and implementing treatment programs for children who stutter. Even though this survey was conducted 5 years ago, we would speculate that many clinicians continue to lack confidence in treating this disorder and seek additional guidance in planning and implementing programs for children who stutter. This is in light of the new requirements by the American Speech-Language-Hearing Association, which do not dictate a specific number of clinical ABSTRACT: The speech-language pathologist plays a critical role in the treatment of the elementary schoolage child who stutters. The purpose of this article is to describe a model of service delivery for these children that emphasizes the integration of fluency-shaping and stuttering modification approaches. Procedures and techniques of previously published programs are supplemented with suggestions by the present authors. The treatment program is divided into three phases. Phase I is a description of procedures used to have the child understand and identify fluency and stuttering. Phase II involves a discussion of techniques for the instruction and integration of fluency-shaping and stuttering modification procedures. In Phase Ill, transfer and maintenance of speech improvement procedures are described briefly. KEY WORDS: stuttering, children, treatment, elementary LANGUAGE, SPEECH, AND HEARING SERVICES IN SCHOOLS * VOI. 26 clock hours in the area of fluency disorders. It is possible that a professional entering the field in the next few years will have minimal training in treating children who stutter. In addition to the limited training or lack of confidence clinicians have in treating stuttering in children, it is possible that they have limited access to a variety of clinical methods and materials. Thus, the seemingly best alternative is to resort to using one approach, strategy, or program for all children who stutter. Although one program or approach may be appropriate for some children who stutter, it is sure to fail with others. When these children fail to improve in treatment, clinicians begin to question their methods, the program, and/or the child's motivation for making improvements in the way he or she talks. The purpose of this article is to provide the school clinician with suggested strategies and procedures that could facilitate the treatment of elementary school-age children who stutter. For this article, we will focus on children who are between the ages of 6:0 and 12:0 (years:months) (i.e., grades K-6). An attempt has been made to show the similarities among treatment programs in terms of techniques that facilitate improvement in the child's speech behavior. It is recognized that each child's fluency disorder is unique and may require a different approach to the problem. The strategies and procedures discussed in this article represent an integration of ideas and approaches. Changes in a treatment approach may be necessary depending on the age and circumstances surrounding the disorder. For example, the nature, focus, and pace of therapy for a child in first grade will be distinctively different from that for a child in the fifth grade. A first grader usually will not display a great deal of fear, embarrassment, or avoidance behavior about stuttering. By contrast, the fifth- or sixth-grade child usually has developed fears and avoidance behaviors as well as a negative attitude toward therapy. Therefore, efforts directed toward 0161-1461/95/2602-0151 American Speech-Language-Hearing Association 151 improving or enhancing the fluency skills of upper elementary-grade children may prove unproductive unless time is spent in exploring and modifying the child's feelings, beliefs, and attitudes about stuttering. With the older elementary child, any treatment session can represent an opportunity for the child to feel accepted and understood. The school clinician may be the only person, or certainly one of a very few, in the child's life who takes the time to listen to his or her message rather than the quality of the fluency. In that sense, the school clinician represents the sympathetic ear the child may not find elsewhere. In no sense should a clinician view this form of therapy as a "waste of time." Providing a place where children can confront their stuttering and communicate freely is beneficial in the long term. Clinicians should be active and compassionate listeners when the need arises. * It is logical to assume that a plan for therapy }will evolve from data collected during the evaluation. However, if the evaluation is conducted to assess solely whether the child qualifies for services, then the data available for planning treatment may be incomplete. When this is the case, an assessment and in-depth analysis of certain aspects of the fluency problem may need to be explored in the initial stages of therapy. Ham (1990) lists a number of factors that need to be considered when developing a treatment plan that could evolve from a thorough assessment. Examples of these factors include an assessment of the form of stuttering, the quantitative and qualitative descriptions of the child's fluent and disfluent speech behavior, the child's response to stress, the parent's reaction to the stuttering, and the presence of articulation and/or language disorders that coexist with the stuttering. * Therapy is planned according to the constraints on a clinician's caseload size, scheduling of therapy, and the amount of parent involvement. It should be recognized PRINCIPLES UNDERLYING THERAPY FOR SCHOOL-AGE STUTTERERS that the best therapy plan may have limited effectiveness if too many constraints are placed on the delivery of services or there is a lack of support from the parents. In a companion article in this issue, Ramig and Bennett address these issues as they relate to treatment programs for school-age children. There are several principles that form the foundation of treatment with school-age children who stutter. Below is a description of eight principles that we believe are important for clinicians to consider when treating this age group: * Once scheduling and service delivery concerns have been minimized, changes in fluency cannot occur unless there is direct management of the problem. * Clinicians need to be flexible in the design and implementation of a treatment program. This suggests that the clinician needs to have a broad knowledge of the different approaches to treatment. Not all stutterers will "fit" into one approach or benefit from one program. The clinician needs to fit the program to the child rather than the child to the program. This principle necessitates that the clinician has the knowledge to make decisions about treatment based on data generated from an assessment of factors that contribute to the stuttering behavior. Those factors should be reevaluated periodically during the course of treatment so that changes in the program can be made in a timely manner. * A good working relationship needs to be established between the child and clinician. This implies that the clinician must take the time to know the child and his or her interests. Strong relationships are built on trust and respect that evolve over time. The sharing of feelings, attitudes, and experiences will assist in building a strong client-clinician relationship. * It is necessary and reasonable to expect that the elementary-age child can assume most of the responsibility of changing and managing the stuttering. Each child should learn and display self-corrective behaviors rather than relying on the clinician for all monitoring. In other words, each child in treatment should be an active participant in therapy. * The clinician also should take time to gain a better understanding about how the child cognitively perceives or represents events and experiences in his or her world. The cognitive component of stuttering therapy (i.e., conceptual knowledge and understanding of "slow talking" and "gentle onset of voicing") is critical to success. * Long-term change in speaking more fluently emerges once a feeling of control over the speech process has been developed, positive reactions to the stuttering have occurred, fear associated ith speech or stuttering has been reduced, and appropriate changes in the way one speaks have been chosen. Moreover, "successful therapy" does not mean that the child will exhibit 1% or less disfluency in all speaking situations. Rather, treatment has been effective if the child communicates easily whenever and to whomever he or she chooses (Conture & Guitar. 1993). 152 LANGUAGE, SPEECH, AND HEARING SERVICES IN SCHOOLS APPROACHES TO TREATMENT Treatment for school-age children who stutter has focused on "fluency-shaping," "stuttering modification," or an integration of the two treatment approaches. The application of either a fluency-shaping (i.e., establishment and operant shaping of fluency under controlled stimulus conditions) or stuttering modification (i.e., reduction in the severity of stuttered moments and negative emotions) treatment approach with children who stutter is discussed at length by Gregory (1979) and Peters and Guitar (1991). The reader will find an excellent discussion and explanation of each treatment philosophy in both texts. Vol. 26 April 1995 An integration of the fluency-shaping and stuttering modification therapies relates most specifically to the procedures suggested in this article. This is not to suggest that the exclusive use of either fluency-shaping or stuttering modification therapies is not effective with children. Our preference is to use whatever seems best for a child at any given time as it relates to factors that contribute to the fluency disorder. For example, it may be appropriate to apply specific fluency-shaping procedures to help the child manage the timing and coordination of respiratory, phonatory, and articulatory movements for a fluent response. The child may lack the physiological capacity to produce consistent fluency on command, as reflected in the presence of abrupt onsets of phonation and jaw tremors during a stuttering moment. The treatment program for this child would focus on helping him or her overcome the mistiming and temporal control of the speech mechanism (Kent, 1984; Van Riper. 1982). However, attending only to the physical changes necessary for fluency and ignoring the effects of negative attitudes and emotional responses does not seem wise. Fluency training cannot be done without considering the child's confidence as a speaker. The effects negative listener reactions or feelings of anxiety have on a child's ability to maintain learned fluency skills should be included in any treatment program. Likewise, physiological and emotional factors are influenced by how well the child believes he or she can manage fluency in a given speaking situation. The confidence and positive self-image he or she brings to a speaking situation usually will dictate how well a child's fluency is maintained. Some children we have treated can exhibit fluency that sounds normal in the therapy room when emotionally-neutral topics are discussed with the clinician. But, as soon as the emotionality or propositionality of the message increases, there is an immediate reduction in the child's ability to use the fluency skills that facilitate the proper coordination of the speech mechanism. It also should be recognized that no treatment program will be effective unless it takes into account the child's cognitive skills. This refers to how a child solves problems, conceptualizes, and assigns meaning to objects and events (Meyers & Woodford, 1992). Children between the ages of 7 to 11 are oriented toward events in the immediate past rather than events that happened long ago. Moreover, the event needs to be presented in concrete rather than abstract terms in order for comprehension to occur. Thus, children in this age group need considerable structure and multiple repetitions of events in order to comprehend their meaning (Gregory, 1991). A child's failure to comprehend concepts or techniques may be due to an insufficient number of repetitions of an event or the clinician's failure to explain concepts that match a child's cognitive understanding. Finally, it is important to note that the extent to which any treatment program is effective depends on a number of factors such as the length of treatment, responsiveness of the child to the program, support of the parents, and responsibility a child shows in changing and managing the stuttering. Most would agree that any stuttering management program involves a large investment of time because behavioral and attitudinal changes cannot occur quickly. Children in the school setting usually are enrolled in treatment for at least a year, maybe longer, considering the length of time they are treated each week. It is reasonable to expect that the child's acquisition of new behavioral strategies associated with talking as well as improvements in feelings and attitudes will take a considerable length of time. Therefore, the child, the child's parents, and the clinician should not expect or accept short-term improvements as a valid measure of treatment effectiveness. Due to the extended period of time children typically are enrolled in treatment, it is tempting to define "successful" therapy as that point in time when the child produces little, if any, overt stuttering and/or secondary behaviors. Indeed, a few published programs such as those by Runyan and Runyan (1993) and Goebel (1989) have reported that a high percentage of the children who had completed their treatment programs showed reductions in posttreatment stuttering and overall ratings of stuttering severity. These results support the effectiveness of these programs in reducing stuttering behavior and improving fluency, which is why the components of these programs are included in the integrative program described in this article. Many children treated in our program have achieved increased levels of fluency when pre- and posttreatment stuttering frequency data are used as the criterion for success. However. we are reluctant to base treatment effectiveness exclusively on pre- and posttreatment fluency data. This seems to us to be a rather narrow definition of "success." Some children in our program have demonstrated increased levels of fluency but were unable to achieve a positive attitude about themselves as fluent speakers. Approximately 20% of the children who had completed the second phase of our treatment program showed steady reductions in the frequency and duration of their stuttering as well as secondary behaviors. But, despite the increased levels of fluency, many of these children maintained fears and negative attitudes about speaking to particular people or in certain situations. As a result, we shifted the treatment program from fluency training to building self-esteem and improving attitudes and perceptions about themselves as effective communicators. Conversely, another small number (i.e., 20%) of children at the end of the second phase of treatment exhibited relatively high levels of frequency of stuttering ranging from 6 to 12%. But, they could modify their stuttering behavior and possessed positive attitudes about themselves and their stuttering. As a result, these children were not hesitant to talk with anyone at anytime. Attempts to instruct and encourage these children to achieve increased levels of fluency were met with strong resistance and a loss of motivation to attend treatment. As stated earlier in this article, we support Conture and Guitar's (1993) conclusion that treatment is successful when the child communicates easily whenever and to whomever he or she chooses. The small group of children who possessed high levels of fluency but negative attitudes about their speech might be viewed as "successfully treated" if we used stuttering frequency data as our criterion for success. Using Conture and Guitar's criterion for success, these children fall short of that goal. However, Healey & Scott 153 the small group of children who exhibited high levels of stuttering but were willing to speak to anyone at anytime without fear also might be considered "successful" because of their willingness to converse with anyone under any circumstance. We believe this positive attitude toward talking evolved from an understanding of how and why certain behavioral and emotional changes improved their communication ability. For these children, fluency was not the ultimate goal of treatment. Regardless of which criteria are used to determine treatment effectiveness, the assessment of therapy effects should be done several times during the course of treatment as well as several months following the child's termination from therapy. A treatment program would be considered ineffective if the child only used its procedures and methods within the clinical setting or showed no willingness to change his or her attitudes and perceptions about the stuttering. Thus, each child's fluency status should be evaluated periodically from speech samples from within and external to the clinic environment. Speech samples should be obtained from a variety of speaking conditions with a variety of listeners (Conture & Guitar, 1993). We should remember, too, that the child's attitudes and perceptions of his or her speech during and following treatment also should be measured because these aspects of speaking are as important as evaluating the level of fluency. AN INTEGRATIVE TREATMENT APPROACH From what has been said above, it should be clear that our approach to treatment emphasizes an integration of fluency-shaping and stuttering modification treatment philosophies. This integrative treatment approach incorporates data-based techniques and suggestions from previously published programs. We have supplemented the suggestions offered by others with those we have discovered helpful in implementing an integrative treatment approach. The service delivery model we use is divided into three phases. Phase I involves the identification and understanding of fluency and stuttering. Phase II focuses on the instruction and integration of fluency-shaping and stuttering modification procedures. Phase III is concerned with the transfer and maintenance of speech improvement to speaking situations outside of the clinic environment. TREATMENT PHASE I The goal of the first phase of the program is to have the clinician become familiar with the child who stutters and understand the nature of the stuttering problem. In order to do this successfully, we first focus on establishing a good working relationship and rapport with the child. Our intent is to understand all we can about the child as a person. Discussions about the stuttering will come in later sessions. One way to establish rapport is through a discussion of interests such as the child's favorite sports, games, movies, and television programs. Information derived from discus- 154 sions of these topics can serve as a basis for informal conversations with the child, fluency training activities, and transfer activities later in the therapy program. The next step is for the clinician to explore the degree of the child's awareness of the fluency disorder. We support Conture's (1990) suggestion of determining a child's emotional and intellectual "awareness." Emotional awareness is concerned with the extent to which the child copes with the stuttering problem on a daily basis. Intellectual awareness deals with the degree to which the child realizes when a stuttered moment occurs and what is experienced during that moment. It is unusual to find an elementaryschool-age child who is not aware that he or she talked differently from other children and who has some degree of emotional reaction that takes place when the stuttering occurs. The child's reactions and attitudes about stuttering can be evaluated using the Children's Attitudes About Talking-Revised (De Nil & Brutten, 1991). Exploring the child's awareness of the frequency of the stuttering is based on the notion that the child cannot address a problem area unless it is recognized or acknowledged openly. We also want to gain an understanding of the child's perspective on the fears and reactions that are associated with the stuttering, For those children who are unaware or fail to openly discuss their stuttering, it is beneficial to establish a level of awareness and some degree of openness regarding the stuttering before discussing the processes involved in fluent and stuttered speech. When discussing the child's awareness of stuttering, it may be helpful to determine how well the child perceives moments of stuttering as imitated by the clinician. Initially, we spend time having the children identify imitated stuttered moments from our speech. We also have the child recognize our imitations of secondary behaviors the child exhibits in order to avoid or conceal the stuttering. Van Riper (1982) advocates the use of this method as a way to reduce the negative emotions associated with the stuttering. Dell (1979) points out that increasing a child's awareness of stuttering is an important stage of cognitive understanding of the differences between stuttering and fluency. It also helps develop a common "language of stuttering" between the clinician and child. For some children who stutter, this activity will increase a child's awareness of stuttering in other speakers as well as in his or her own speech. However, during this awareness training, we have had the child say to us, "I hear you stutter, but I don't do that when I talk." For this child. we use audio- and videotaped segments of the child's stuttering within a spontaneous speech segment. After a brief segment has been recorded, we replay the segment of stuttering that the child may have missed several times. As the child begins to recognize the stuttered moments. we establish a signal, such as raising the hand, when we both agree on when a stuttered moment occurred. The next step involves a matter-of-fact discussion and analysis of speech behaviors associated with stuttering and fluency. Our intent is neither to increase the child's sensitivity to the stuttering nor engage in a detailed account of the stuttering. Rather, we are interested in knowing how the child feels about him or herself and the stuttering. Are LANGUAGE, SPEECH, AND HEARING SERVICES IN SCHOOLS * Vol. 26 April 1995 there feelings of shame, embarrassment, anger, or helplessness? We also want to help the child understand the relationship between speech fears and changes that occur in the speech mechanism during a moment of fear or negative self-perception. We like to emphasize that a common normal reaction to feared situations is an increase in muscle tension throughout the whole body. Much of that tension is felt in the throat, tongue, and jaw musculature. The tension felt during a feared speaking situation then is contrasted with the reduced tension levels and calm feelings that occur during a fluent moment. At this point, the clinician could develop a common language of fluency (Cooper & Cooper, 1991). The language of fluency refers to a variety of skills such as a slow rate, control of outward airflow during speech, easy onset of phonation, and proper loudness that are necessary to produce a fluent word. It is important to point out the coordinated movements of the speech mechanism that occur when these fluency skills are used. In order to increase the child's cognitive awareness of this concept, we need to take into account the age of the child. For children in the primary grades (i.e., K-3) we use pictures and line drawings of the speech mechanism and describe in very simple terms the respiratory, phonatory, and articulatory systems. For example, we have the child feel the chest rise during inhalation and the gradual fall that occurs as a steady flow of air is exhaled. We also have them feel the vibrations from their own larynx while counting or saying the days of the week with continuous phonation. For children in the intermediate grade levels (i.e., 4-6), we use similar drawings and pictures of the speech mechanism as with the younger children but supplement this discussion with videotaped segments of the clinician imitating stuttered moments. The child then could talk about the parts of the speech system that were disrupted in the clinician's speech. Clinicians should not underestimate a child's ability to analyze, observe, and understand stuttering behaviors. For older elementary children, we also include a description of Williams' (1979) normal talking model as a basis for helping the child understand the processes required for normal fluency. Children need to learn about the normal talking process and how stuttering fits into that model. Williams emphasized that normal talking involves the use of the airstream and levels of tension in the speech musculature, timing, and voicing, as well as movements and placements of the articulators. These speech parameters can be related to any disrupted speech process a stutterer might exhibit. These behaviors include the use of an abrupt onset of phonation and/or the presence of tense posturing of the articulators during a sound prolongation. It is important for the clinician to demonstrate and model behaviors rather than simply talk about the relationship between the disrupted process and changes that occur in the normal function of the speech mechanism. Conture (1990) described in detail some effective ways to convey meaning about disruptions in the speech mechanism and how the child interferes with the normal talking process. For example, his "garden hose" analogy is useful in explaining how the faucet resembles the function of the larynx whereas the hose and nozzle connected to the hose represent activity of the tongue and lips. The child learns how airflow, like water, can be turned off by the faucet (larynx), by kinking the hose (tongue), or by closing the nozzle (closing the lips). This and other similar analogies described in his book assist in helping the child focus on what happens in the vocal tract during talking. Through these analogies, the child can focus on "those things he is doing to interfere with talking and those things he is doing to facilitate it" (Williams, 1979, p. 254). Once the child can describe the basic concepts taught at this stage in a meaningful and reliable way, the clinician can elect to go to Phase II of the treatment program. It is important, however, to ensure that the child understands and adequately conceptualizes the changes that need to occur in the speech system. From this framework, the child will have an understanding of the rationale underlying a variety of techniques and methods designed to facilitate fluency and/or modify stuttering. TREATMENT PHASE II The goal of the second phase of our treatment approach involves instruction in the use of specific fluency-enhancing and stuttering modification procedures. We use a variety of techniques that seem appropriate for the type of fluency disorder each child exhibits. As mentioned above, when teaching fluency-enhancing and stuttering modification procedures, particular attention needs to be paid to the child's cognitive understanding of how and why certain techniques or methods help in managing his or her fluency disorder. However, even if the child understands how and why a particular method helps, there is no guarantee it will always work for the child in all speaking situations. It does, however, provide a reason why it can work for the child who chooses to try. Fluency-Enhancing Techniques The clinician has an array of methods from which to choose to assist the child in achieving increased fluency. There is general agreement among experts that considerable time should be spent in building fluency skills for children who stutter though the use of techniques that enhance fluency (Gregory, 1991). Some of the most common fluency-enhancing techniques include manipulation of linguistic length and complexity, speech rate reduction, airflow control, gentle onsets of phonation, and light articulatory contacts. These fluency procedures form the foundation from which other fluency management techniques are based, such as smooth transitions between sounds, proper phrasing, and pitch/loudness control. These procedures also allow for increased motor and linguistic planning time needed to coordinate respiratory, phonatory, and articulatory behaviors (Riley & Riley, 1983; Wall & Myers, 1984). The following is a description of each fluency-enhancing procedure along with a discussion of ways it can be integrated into therapy. Healey & Scott 155 Reduced linguistic length and complexity. Reductions in utterance length and syntactic complexity have a positive impact on the degree of fluent behavior that is exhibited (Gaines, Runyan, & Meyers, 1991; Ratner & Sih, 1987). It also has been shown that a short utterance can be made more linguistically complex by increasing syntactic complexity (Ratner & Sih, 1987). For these reasons, the control of utterance length and complexity reflects one of the fundamental procedures of almost any program for children who stutter. The gradual increase in the length and complexity of an utterance (e.g., Ryan's GILCU program, 1974) can be used exclusively to establish fluency or used in conjunction with the training of other fluency-enhancing techniques (Costello, 1983). Thus, linguistic length and complexity increase as the child becomes proficient in producing a fluent response or acquires skills needed for a new technique. Clinicians also can exercise control indirectly over the length and complexity of a response by modeling a slowerthan-normal speech rate. Ratner (1992) has shown that when mothers of young children were instructed to speak slowly, they automatically reduced the length and syntactic complexity of the spoken message. This effect is the same as speaking to a person from a foreign country who is not a proficient speaker of the English language. The message is short, simple, and to the point. Clinicians should adopt this type of speaking style throughout all interactions with school-age children who stutter. In order to facilitate fluent responses, clinicians could begin training at the single-word level or carrier-phrase level. For primary grade school-age children who stutter, the use of nursery rhymes could be used to elicit fluent responses as suggested in the Easy Does It-I (Heinze & Johnson, 1985) treatment program. For children who have been in treatment for an extended period of time or who are in the upper elementary grades, we would recommend that training begin at a linguistic level, where the child can experience fluency or mild stuttered moments. The clinician needs to manage the linguistic complexity of responses during a session so that the child can maintain the length and complexity of utterance that is expected. The child should know what level of response is expected during the training activity. Once reliable fluency is achieved at the word or carrier-phrase level, the clinician can gradually shift to short sentences, phrases, and structured conversation. When the structured conversation level is reached, the clinician can ask open-ended questions as in the Stocker Probe Technique (Stocker. 1980) about common objects (e.g., crayons, baseball, stamps). For example, the child can be asked to tell everything he or she knows about the object and to make up his or her own story about the object. At the sentence and phrase response level, have the child convey one central message about the sentence or phrase, then add another thought. The same procedure can be used when reading paragraph length or short-story material. Instead of asking the child to tell us the whole story, we break the story into small descriptive units, then have the child retell the story with all the units combined. Changes in the story units should be encouraged because they may reveal increased flexibility 156 LANGUAGE, SPEECH, AND HEARING SERVICES IN SCHOOLS of language skills. Compared to conversation, story retelling may enhance fluency because of the reduced length and complexity of the narrative utterances (Weiss & Zebrowski, 1992). Narratives appear to be a useful way to simulate the organization of thoughts and control of fluency skills that occur with conversations outside of therapy. Reductions in speech rate. Slowing speech rate is one of the most common techniques used in stuttering therapy. Because it is used so frequently as an aid to producing fluent responses, Runyan and Runyan (1993) consider rate control a universal (i.e., fundamental) treatment procedure in their Fluency Rules Program. The rationale for implementing a reduced speech rate is the powerful effect it has on facilitating the coordination of complex movements and timing associated with respiratory, phonatory, and articulatory activity (Perkins. 1973; Wall & Myers, 1984). An indirect benefit associated with reduced speech rate is a slow, relaxed conversational pace (Runyan & Runyan, 1993). We too have observed that a slower-than-normal conversational pace tends to have a physical and emotional calming effect. With elementary school-age children, we have found that this calming effect is facilitated through speech and nonspeech behaviors. Thus, the clinician needs to use a slower-than-normal interaction style as well as a slower-than-normal pace during the presentation of materials and activities within a treatment session. We believe it is essential for the clinician to control the pace of the conversation and session. Teaching someone who stutters to reduce his or her speech rate is not an easy task because most people, even children, are reluctant to speak slowly. Therefore, we like to emphasize that the use of a slowed rate of speech will provide the child with an increased "feeling of control" (Cooper & Cooper, 1991) over the stuttering. It is easier to have children engage in a deliberate change in speech rate initially, in order to understand the physical and emotional feelings associated with talking slower than they normally do. Once the child speaks more fluently or easily with the slower rate, the rate should be increased gradually to approximate normal levels. A speech rate that is slower than normal can be taught either by means of a programmed approach using the delayed auditory feedback (DAF) unit (Ryan, 1974) or by direct instruction and modeling. The DAF unit will force the speaker to prolong all syllabic units of a word spoken in the utterance. Other ways to reduce speech rate include increasing pause time between words or using a combination of increased pausing and prolonged speech (Healey & Adams, 1981). Research has shown that rate control through prolonged speech is an effective way to control stuttering if the resulting fluency is shaped to normal speech (Andrews, Guitar, & Howie, 1980; Ingham. 1984). Regardless of whether a pausing or prolonging rate control method is taught, it is important that school-age children have a clear understanding of how it feels to speak in this way and why it helps them manage their stuttering problem. When introducing, referring to, and/or modeling a rate control method to primary grade children who stutter, it is best to attach some meaningful term such as "turtle or stretched speech." With older children, one could use terms Vol. 26 April 1995 like "slow, easy speech," "slow-motion speech," or "stretched speech." One also could couple slow talking with slow walking (Meyers & Woodford, 1992; Runyan & Runyan, 1993) or say the names of objects slowly as the child slowly places objects or pictures in a container. In addition, we have found it beneficial to discuss the concepts underlying slow talking through the use of semantic mapping. The semantic map helps children organize and conceptualize how, when, where, and why rate control is effective in increasing fluency. Figure I is an example of a semantic map that would be used to teach the concept of rate control. The map guides a child through an understanding of how slow rates are produced, what speech changes occur when a slow rate is used, and why this manner of talking helps them gain control over the stuttering. The child is asked to describe in his or her own words the information under each main category. In this way, the perception of stuttering and fluency control emerges from the child's perspective, not the clinician's. Once the map is completed, it can be used as the basis for the instruction of a slower-than-normal speech rate. Using a single-subject design, we tested the notion that cues from a semantic map would be as effective in reducing speech rate as a sound-prolongation procedure. A 7-year-old male with moderate stuttering was taught two forms of rate reduction-sound-prolongation procedures and cues from semantic mapping. Baseline rate of speech before sound prolongation instruction was 4.4 syllables per second. The child's speech rate during the sound prolongation treatment phase was 2.5 syllables per second. Following the second baseline period, in which he spoke at a rate of 4.1 syllables per second, the child was instructed to use cues from a semantic map to slow his rate. The child's speech rate during this treatment phase was 2.8 syllables per second. During a third baseline period, after all rate control Figure 1. Semantic map for teaching concepts related to the use of a slow speech rate. __--A F--, When do you use your slow speech? * when I start to stutter * when I'm nervous * when I'm excited methods were withdrawn, the child spoke at 4.9 syllables per second (Ellis, Healey, Dombrovskis, & Antonius, 1992). These data show that cues from a semantic map are as effective in teaching a slower rate of speech as the traditional sound prolongation method. One of the biggest problems related to using any form of reduced speech rate is the artificial fluency that is created. Because of this, not many children who stutter choose to use a slow speech rate on a consistent basis. Perhaps that is why we discovered that children do not necessarily use or maintain the rate control method they are taught throughout an utterance unless reminded to do so (Healey & Scott, 1991). For example, a child who is instructed to use prolonged speech may not exhibit that method when attempting to reduce rate without prompting from the clinician. For this reason, some treatment programs such as Easy Does It-2 (Heinze & Johnson, 1987) and Shine's (1980) approach incorporate a continuous phonation pattern to reduce rate. Cooper and Cooper (1991) use a cartoon character called the "Slow FIG" (slow, fluency-initiating gesture) to represent this form of rate control. Likewise, the computer-aided fluency establishment trainer for children, Cafet-for-Kids (Goebel, 1989), teaches a continuous phonation pattern by creating a solid green bar in a box on the computer screen. When the child learns to consistently "paint" a continuous green bar on the screen, a game can be introduced to reinforce this concept. For example, an animated skier is shown skiing downhill in a slow continuous fashion as long as the child does not produce any breaks in phonation. Another method for teaching rate control is to prolong only the initial segments of an utterance because the initial segment is the location of most stuttered moments. The easy, relaxed approach with smooth movements (ERA-SM) method, advocated by Gregory and Campbell (1988), teaches a child to produce a slow, soft speech initiation by stretching the first sound of the first word in an utterance. After the first sound is stretched, the remaining words of the phrase are produced with continuous phonation while approximating normal rate and prosody. Pindzola's (1987) Stuttering Intervention Program (SIP) also emphasizes stretching the initial segment followed by a return to a normal rate on the remaining words in the phrase. One should note that this method of rate control incorporates a normalization of pitch and loudness variation after the initial segment of the utterance. Normalization of pitch and loudness allows the child to retain the melodic aspect of speech while controlling rate. Regulation of airflow. This technique is useful for those children who exhibit frequent breath holding behaviors, audible airflow release without accompanying phonation at the beginning of the phrase, speaking on inhalation, and/or shallow breathing (Ham, 1990). Goebel (1989) begins her Cafet-for-Kids fluency management program with this procedure. Emphasis is placed on taking a full inspiratory breath coupled with a slow exhalation of air. The program uses a color monitor and the children are reinforced visually for successful slow exhalation by "drawing" a green bar on the screen. Runyan and Runyan (1993) borrow heavily from the Cafet-for-Kids program in teaching "speech breathing." Healey & Scott 157 Both of these programs focus on having the child breathe in, let air out slowly, speak on the outward flow of air, and keep air moving throughout the phrase. Cooper and Cooper's (1991) Deep FIG character symbolizes a deep inhalation of air before the onset of phonation. If the child needs practice controlling the airstream, we have found that a simple line drawing of mountains or a playground slide provides a visual representation of a typical inhalation/exhalation curve for speech. We like to emphasize that children make a smooth inhalation as they go up the mountain or slide. This is followed by an immediate, slow, constant release of airflow as they go down the mountain or slide. Having the child trace the mountain or slide with his or her finger while inhaling and exhaling provides some tactile feedback for the motor pattern being taught. Runyan and Runyan (1993) also suggest that the child trace a breath curve with one hand and place the other hand on the abdominal area. At the top of the inhalation and just before exhalation begins, the clinician provides a gentle squeeze on the child's arm as a signal to begin speaking. Tactile feedback of this type can assist the child in achieving the proper timing associated with the release of the airflow and the onset of phonation. Repeated practice with this technique will prepare the child for the use of a gentle onset of phonation. Gentle onset of phonation. Many children who stutter have difficulty initiating phonation on command. Difficulty in initiating voicing is reflected in the presence of abrupt onsets of phonation, glottal fry, tense pauses, and/or the perception of audible vocal tension during fluent and stuttered moments (Costello, 1983; Ham, 1990). Children who exhibit any of these difficulties in phonation can create substantial control over their fluency from this technique alone. There are two ways of teaching an easy onset of phonation. The first and most common way involves a deliberate use of the exhaled air throughout the initial onset of phonation. We have used this method successfully with kindergarten-age children by focusing on audible exhalation of air like "putting an /h/ sound in front of your words." Instructing the child to contrast between words like "hat/at" helps the child feel and hear the difference between an easy and normal onset of phonation. Older school-age children have little difficulty producing easy onsets if there is appropriate modeling of the behavior. Once the child exhibits reliable use of this technique, the clinician should work on normalizing phonation onsets. Elimination of the audible use of airflow associated with the easy onset should be done gradually so the child can learn how to use the technique without any abnormal-sounding fluency. The second way to teach easy onsets is to use a gradual rise in vocal intensity at the beginning segment of a word. This method is used in Runyan and Runyan's (1993) program under the rule of "Start Mr. Voice Box Running Smoothly." The Runyans point out that they shifted to this form of easy onset instruction from the teaching of a breathy onset because of the difficulty in eliminating the breathy onset from the child's vocalizations. They have not observed this difficulty with the use of the increased rise in vocal intensity. However, in the Cafet-for-Kids program, 158 Goebel (1989) did not include the easy onset target because of the difficulty young children had learning the technique. Instead, Goebel focused on stretching the first syllable of the word at normal vocal intensity. Note how similar this method is to the ERA-SM and SIP programs described in the reductions in speech rate section above. Regardless of which method is used to teach an easy onset, the clinician also should be aware that children also will tend to reduce loudness in place of an easy onset. Others have observed this phenomenon and have included it as part of teaching the easy onset "rule" (Runyan & Runyan, 1993) or developed a specific fluency gesture for training such as Cooper and Cooper's (1991) Loud FIG. This FIG highlights the importance of how loudness control and variation in spontaneous speech facilitate a "feeling of control." Light articulatory contacts. This technique is used frequently as a means of reducing articulatory tension that occurs during a stuttered moment (Van Riper, 1982). It allows the child to minimize the muscle tension needed for articulatory contacts during an utterance. Maintaining loose contacts reduces blockage of the airstream, which renders proper control over phonation, lowers intra-oral pressure during stop consonant production, and allows for smooth transitions between sounds. It is important to teach this concept by having the child think of things that touch "lightly" and "softly," such as leaves falling to the ground, a butterfly landing on a flower, or clapping the hands lightly. Again, a semantic map might help a child grasp this concept. Things that touch lightly are contrasted with things that make hard contacts such as hail, hard rain, or making a loud sound by clapping the hands forcefully. Once this concept is understood, we shift to making light and hard contacts associated with speech sounds. We start training with bilabial sounds, then move to alveolar sound placements within single words. We have the child focus on the feeling of a soft bilabial contact for a sound like the /p/ in "paper." After several repetitions and modeling of light contacts, a forceful closure of the lips is demonstrated on the same sound. We want the child to discover the difference in feeling between a light contact and forceful tongue or lip contact. During the forceful contact, the child is encouraged to relax the tension of the articulatory contact gradually and continue with the word. The use of negative practice, which requires the child to alternate between light and hard contacts, increases the child's awareness of the physical difference between light and soft contacts. Stuttering Modification Techniques With many older elementary school-age children, it may be necessary to couple fluency-enhancing techniques with methods that teach the child how to modify a moment of stuttering. Peters and Guitar (1991) suggest that school-age children who stutter need to learn to modify residual, tense stutterings. We too, have found that some children who have stuttered for several years and exhibit excessive avoidance behaviors fail to achieve success in managing fluency exclusively through the use of fluency-enhancing LANGUAGE, SPEECH, AND HEARING SERVICES IN SCHOOLS * Vol. 26 April 1995 procedures. Therefore, in addition to the use of fluencyenhancing skills, some children should learn how to turn a tense stuttering moment into "easy" stuttering and cancel the stuttering as it occurs. Learning to stutter easily. This stuttering modification method could be taught by following Dell's (1979) suggestion that the child learn three ways to say a word. A word can be produced fluently, in an easy stuttered way, and with tension and struggle. The clinician could select a simple word like "ball" and then model a fluent production of the word. Next, the child would be asked to listen to the clinician's production of an easy, effortless prolongation or repetition of the /b/sound or syllable. Finally, the clinician says "ball" with tense blocking on the /b/ sound or blockage of airflow and voicing during multiple-unit, part word repetition of the /ba/ syllable. Following these examples, the clinician and child can play a game in which the child identifies the way the clinician produced the word. Van Riper (1982) refers to this as the "catch me" game in which the child points out disfluent moments from the clinician's speech. Once the child is comfortable with this level of monitoring, the clinician can ask the child to practice the three ways of saying a word. We focus on helping the child learn how to change from a tense stuttering to an easy stuttering by producing a slow, slightly stretched articulatory movement on the remaining segments of the word. After the child is skilled in stuttering more easily with words and phrases, the clinician can spend time rewarding modified stuttering during reading and spontaneous speech. Cancellations. This is one of the key techniques of the stuttering modification treatment approach and is an extension of the easy stuttering technique (Peters & Guitar, 1991). It involves a cancellation or interruption of a disfluent word followed by a second attempt at the word using an easy stuttering. The cancellation requires the use of a slight pause, during which time the child releases the tension in the speech mechanism and then attempts the word a second time. We also have suggested to some children that after the cancellation and before the second production of the word, they use a gentle onset of phonation or a slow stretched movement into the remaining syllables of the word. Clinicians should make sure the child understands that the second attempt at the word involves changing some aspect of talking (i.e., from a tense articulatory posture to a more relaxed posture) rather than simply saying the word again. Returning to a discussion of Williams' (1979) normal talking model might be appropriate when teaching this technique. Voluntary stuttering. Another technique that is used often as a way to reduce the embarrassment or fear of stuttering is to have the child engage in a voluntary stutter that involves a relaxed, easy repetition or prolongation of the sound or syllable. This technique is used purposely during the child's conversational speech. Peters and Guitar (1991) suggest that this technique be used during some type of enjoyable speaking activity such as playing a game. Dell (1979) recommends underlining some words in a reading passage and having the child voluntarily stutter on those words. The child also could take the turn as teacher and instruct the clinician how to stutter voluntarily on certain words in a passage or while telling a story. Each time the child shows evidence he or she has attempted to produce an easy, relaxed repetition or prolongation, the clinician should provide verbal praise and encouragement. This will help develop the child's confidence in using voluntary stuttering. Remind the child that the emphasis is on feeling comfortable with using a purposely stuttered word rather than on struggling through a stuttered moment. TREATMENT PHASE III This phase of treatment involves the transfer and maintenance of skills learned in the first two phases of the program. Ingham and Onslow (1987) indicate that "generalization and maintenance strategies should be mandatory features of therapy" (p. 320). They also point out that most treatment programs for children require maintenance of performance as long as 2 years after termination from treatment. In order for this long-term transfer and maintenance phase to be successful, the child should have made substantial improvements in controlling stuttering and/or effectively using certain fluency-enhancing procedures. This phase of treatment focuses on helping the child maintain the skills that have been learned, encouraging generalization of speech changes from the treatment setting to realistic speaking situations, and increasing the self-monitoring and self-recording of performance. The clinician also should consider training the parents to recognize changes in the child's speech behavior that signal a return of the stuttering (e.g., avoidance of speaking situations, developing negative attitudes, and subtle signs of struggle behavior). In terms of transfer, it is the clinician's responsibility to provide opportunities for the extension of fluency skills to settings outside of the clinic room during the establishment of those skills. Training should involve the use of fluency skills in settings that represent routine speaking situations within the school (i.e., the classroom, lunch room, gym, or playground) and home environment. We want the child to use fluency-shaping and stuttering modification techniques outside of the therapy room with the clinician as well as with other communication partners. This also is a good time to request that the child bring a friend to therapy. Interacting with a friend in the treatment setting may help the child feel at ease using newly acquired fluency skills and modified stuttering strategies. The peer also can serve as a "clinical assistant" by helping the child who stutters monitor the use of skills necessary for effective communication outside of the therapy room. The transfer phase also provides an opportunity for the clinician to include speaking situations that disrupt fluency. These situations might involve speaking with a teacher or parent, answering questions, speaking under time pressure, or making a telephone call. The clinician should strive to make these situations as realistic as possible. We agree with Conture's (1990) recommendation that there should be considerable advance planning before the child's exposure Healey & Scott 159 Figure 2. Semantic map related to speaking behavior in the classroom. to a real speaking situation. For example, the clinician could work with the child and his or her teacher on a subject area assignment (i.e.. social studies) for class. The child could bring the assignment to therapy and use it as a basis for discussion with the clinician during therapy. Before leaving the therapy room, the child and clinician could summarize the material and agree on the type and amount of information that will be shared with the classroom teacher. In this way, the child has a structured context from which to draw information but is free to choose how the information will be conveyed. The teacher's role is to confirm that the information is accurate and to be an attentive listener. Having children think through all aspects of this and other similar speaking situations should assist them in reducing the fear and uncertainty associated with those situations. Using visual imagery (i.e., mentally visualizing all portions of a speaking situation) and role-playing social interactions also are effective at this stage of therapy. Additionally, it is effective to use behavioral contracts that specify a fluency/ stuttering modification goal for a new speaking situation that can be practiced outside of therapy. The contract should be written with the child's input and contain specific tasks that will be performed. The child is responsible for returning these contracts and discussing the success or failure that occurred in a particular speaking situation. As shown previously in the second phase of the program, semantic maps can be used at this stage to help the child conceptualize a situation and develop strategies for dealing with fluency disrupters. Figure 2 shows a semantic map developed with two fifth-grade children who stutter about a classroom speaking situation. The map was completed by the children with direction from the clinician. Questions to the children focused on the connections between the internal feelings they have about the speaking situation and how their stuttering might be managed in that situation. Having children think through speaking situations should assist them in being mentally prepared for that situation. As the child maintains improved speaking skills in a variety of situations, we also are concerned about the maintenance of positive attitudes about talking. We have found that some children have a good attitude about themselves and their stuttering but continue to exhibit a high frequency of stuttering behavior. We continue to see the child in treatment but gradually decrease the amount of therapy time to once per week for a month to once every 2 weeks for 2 to 3 months. These children may not be motivated to continue with treatment because they do not express concern about their stuttering. Yet, the less intensive schedule allows the clinician to maintain contact with the child in order to monitor progress. A child's relapse of fluency skills or the ability to modify stuttered moments will usually require re-enrollment in therapy. When this happens, we like to get input from the parents and classroom teacher on the child's speech performance at home and in the classroom. We explore avoidance behaviors, factors related to the mismanagement of the speech system, and changes in the child's life such as death of a family member, separation or divorce of the parents, or other social and emotional factors. Analysis of 160 LANGUAGE, SPEECH, AND HEARING SERVICES IN SCHOOLS these circumstances might reveal the source of the relapse and provide direction for subsequent treatment sessions. CONCLUDING REMARKS We have attempted to illustrate an integrative approach to the treatment of stuttering in elementary school-age children. This approach emphasizes that before a child can learn to mentally and physically change the manner of the stuttering, there must be an increased understanding and knowledge of both stuttering and fluency. From this understanding evolves an increased awareness and recognition that emotional reactions and perceptions play a major role in how well the speech system can be controlled. Once the child is aware of the physical and emotional factors that perpetuate the stuttering, he or she is ready to learn a variety of fluency-enhancing and stuttering modification techniques. We believe that an integration of these procedures will help the child develop an improved self-concept and acquire the ability to use an improved manner of talking outside of the clinic environment. Finally, the clinician needs to foster a strong working relationship with the child so that feelings and emotions can be shared in an atmosphere of trust and understanding. All children should be given the opportunity to feel accepted by the adults important to their lives, and the school clinician has the unique opportunity to provide such acceptance to the child who stutters. Vol 26 April 1995 Seminars in Speech and Language, 8. 303-325. REFERENCES Andrews, G., Guitar, B., & Howie, P. (1980). Meta-analysis of the effects of stuttering treatment. Journal of Speech and Hearing Disorders. 45, 287-307. Kent, R. D. (1984). Stuttering as a temporal programming disorder. In R. F. Curlee & W. H. Perkins (Eds.), Nature and treatment of stuttering: New directions (pp. 283-301). San Diego: College-Hill Press. Conture, E. (1990). Stuttering (2nd ed.). Englewood Cliffs, NJ: Prentice-Hall. Mallard, A. R., Gardner, L. S., & Downey, C. S. (1988). Clinical training in stuttering for school clinicians. Journal of Fluency Disorders, 13, 253-259. Conture, E., & Guitar, B. E. (1993). Evaluating efficacy of treatment of stuttering: School-age children. Journal of Fluency Disorders, 18, 253-287. Meyers, S., & Woodford, L. (1992). The Fluency Development System for Young Children. Buffalo, NY: United Educational Services. Cooper, E. B., & Cooper, C. S. (1991). A fluency disorders prevention program for preschoolers and children In the primary grades. American Journal of Speech-Language Pathology. 1, 28-31. Perkins, W. H. (1973). Replacement of stuttering with normal speech: I. Rationale. Journal of Speech and Hearing Disorders, 38, 283-294. Costello, J. M. (1983). Current behavioral treatments for children. In D. Prins & R. Ingham (Eds.), Treatment of stuttering in early childhood: Methods and issues (pp. 69-112). San Diego: College-Hill Press. Dell, C. W. (1979). Treating the school age stutterer: A guide for clinicians. Memphis, TN: Speech Foundation of America. De Nil, L. F., & Brutten, G. J. (1991). Speech-associated attitudes of stuttering and nonstuttering children. Journal of Speech and Hearing Research. 34. 60-66. Ellis, G., Healey, E. C., Dombrovskis, M., & Antonius, K. (1992, November). Comparison of two rate control methods for a young stutterer. Paper presented at the meeting of the American SpeechLanguage-Hearing Association, San Antonio, TX. Gaines, N., Runyan, C., & Meyers, S. (1991). A comparison of young stutterers' fluent vs. stuttered utterances on measures of length and complexity. Journal of Speech and Hearing Research. 34, 37-42. Goebel, M. (1989) Cafet-for-Kids. Annandale, VA: Annandale Fluency Clinic. Gregory, H. (1979). Controversies about stuttering therapy. Baltimore University Park Press. Gregory, H. (1991). Therapy for elementary school-age children. Seminars In Speech and Language, 12, 323-335. Gregory, H., & Campbell, J. (1988). Stuttering in the school-age child. In D. Yoder & R. Kent (Eds.), Decision making in speech-language pathology (pp. 162-163). Toronto: B.C. Decker. Ham, R. E. (1990). Therapy of stuttering: Preschool through adolescence. Englewood Cliffs, NJ: Prentice-Hall. Healey, E. C., & Adams, M. R. (1981). Rate reduction strategies used by normally fluent and stuttering children and adults. Journal of Fluency Disorders. 6, 1-14. Healey, E. C., & Scott, L. A. (1991, November). Young stutterers' and nonstutterers' understanding of rate control strategies. Paper presented at the meeting of the American SpeechLanguage-Hearing Association. Atlanta. GA. Heinze, B., & Johnson, K. (1985). Easy Does It-1. Mohne, IL LinguiSystems. Heinze, B., & Johnson, K. (1987). Easy Does It-2. Moline, IL: LinguiSystems Ingham, R. J. (1984) Stuttering and behavior therapy: Current status and experimental foundations. San Diego: College-Hill Press. Ingham, R. J., & Onslow, M. (1987) Generalization and maintenance of treatment benefits for children who stutter Peters, T. J., & Guitar, B. (1991). Stuttering: An integrated approach to its nature and treatment. Baltimore: Willlams and Wilkins. Pindzola, R. (1987). The Stuttering Intervention Program (SIP). Tulsa, OK: Modern Education Corp. Ratner, N. B. (1992). Measurable outcomes of instructions to modify normal parent-child verbal interactions: Imphcations for indirect stuttering therapy. Journal of Speech and Hearing Research. 35. 14-20. Ratner, N. B., & Sih, C. (1987). Effects of gradual increases in sentence length and complexity on children's dysfluency. Journal of Speech and Hearing Disorders, 52, 278-287. Riley, G., & Riley, J. (1983). Evaluation as a basis for intervention. In D. Prins & R. Ingham (Eds.), Treatment of stuttering in early childhood: Methods and issues (pp. 43-67). San Diego: College-Hill Press. Runyan, C. M., & Runyan, S. E. (1993). Therapy for school-age stutterers: An update on the fluency rules program. In R. Curlee (Ed.), Stuttering and related disorders of fluency (pp. 101-114). New York: Thieme Medical Publishers. Ryan, B. (1974). Programmed therapy of stuttering In children and adults. Springfield, IL: Charles C. Thomas. Shine, R. (1980). Direct management of the beginning stutterer. Seminars in Speech, Language and Hearing, 1, 339-350. Stocker, B. (1980). The Stocker Probe Technique (Rev. ed.). Tulsa, OK: Modern Education. Van Riper, C. (1982). The nature of stuttering (2nd ed.). Englewood Cliffs, NJ: Prentice-Hall. Wall, M., & Myers, F. (1984). Clinical management of childhood stuttering. Baltimore: University Park Press. Weiss, A., & Zebrowski, P. (1992, November). Discourse competencies of children who stutter: Implications for treatment. Paper presented at the meeting of the American SpeechLanguage-Hearing Association, San Antonio, TX. Williams, D. E. (1979). A perspective on approaches to stuttering therapy. In H. Gregory (Ed.), Controversies about stuttering therapy (pp. 241-268). Baltimore: University Park Press. Received June 2, 1993 Accepted October 28, 1993 Contact author: E. Charles Healey, Department of Special Education and Communication Disorders, University of NebraskaLincoln, 253 Barkley Memorial Center, Lincoln, NE 68583-0731. Healey & Scott 161 Strategies for Treating Elementary School-Age Children Who Stutter: An Integrative Approach E. Charles Healey, and Lisa A. Scott Lang Speech Hear Serv Sch 1995;26;151-161 This article has been cited by 4 HighWire-hosted article(s) which you can access for free at: http://lshss.asha.org/cgi/content/abstract/26/2/151#otherarticles This information is current as of April 10, 2013 This article, along with updated information and services, is located on the World Wide Web at: http://lshss.asha.org/cgi/content/abstract/26/2/151
© Copyright 2026