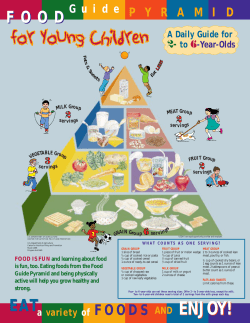
Nutritional Guidelines for Food Served in Public Institutions
Nutritional Guidelines for Food Served in Public Institutions Report prepared for The Food Standards Agency by The Caroline Walker Trust FINAL REPORT Acknowledgements This report was written by Dr Helen Crawley on behalf of the Caroline Walker Trust. Thanks are due to Lesley Stark and Gemma Hoffman, research associates at Caroline Walker Trust, Joe Harvey, Professor Martin Wiseman and other CWT trustees for useful conversations, Sheila Walker for providing some recipes suitable for ethnic minority groups and Rosie Leyden of Wordworks for her editing of the text and tables. Disclaimer This report was put together by The Caroline Walker Trust in good faith and we have done our best to check that this information is clear and correct. If any changes are subsequently made to the data in this report by anyone other than ourselves, however, then we cannot take responsibility for this. This report does not reflect the views of the Food Standards Agency. The Caroline Walker Trust PO Box 61 St Austell PL7 6YL ii www.cwt.org.uk Contents Background 1.0 Nutritional guidelines for food served in child care and schools 2.0 Nutritional guidelines for food served in residential premises for children and young people 3.0 Nutritional guidelines for food served on NHS premises 4.0 Nutritional guidelines for food served in residential premises for adults 5.0 Nutritional guidelines for food served in the prison service 6.0 Nutritional guidelines for food served in residential care for older Adults 7.0 Nutritional guidelines for food served as community meals Appendix 1: Rationale for the calculation of derived reference nutrient values used in this report Appendix 2: Good sources of nutrients Appendix 3: Food customs of ethnic and minority groups Appendix 4: Resources iii Background The Food Standards Agency commissioned the Caroline Walker Trust to develop nutrient-based and food-based guidelines for food served to population groups in public institutions in the UK, and to design example menus that show how these nutritional guidelines could be met. The aim of the guidelines is to help caterers with menu planning and to ensure that those who work for, visit or who are cared for in public institutions have access to a healthy, balanced diet. The public sector in England spends around £2 billion a year on providing food and drink to service users, staff, the general public, clients and visitors. 1 The four biggest public sector food service areas are schools, the NHS, the Armed Forces and the Prison Service, with an approximate joint annual spend of around £1.7 billion. In public sector settings where all food (i.e. three meals a day) is served within that setting, the average amount spent per day on providing food varies from £1.87 for prisoners to £2.60 for hospital patients. The average cost of food ingredients in a school lunch varies from 37p to 85p. There is considerable scope to increase the nutritional quality of food in the public sector. In addition to providing menus that meet the nutritional guidelines in this report, caterers should consider other measures to encourage healthy choices – such as promoting specific menu choices and providing sufficient information for people to make informed decisions. Some of the other suggestions to encourage healthy eating, made in a recent report by the National Audit Office,2 include: • increasing the price of less healthy food and reducing the price of healthier options • reducing the number of fried options used • working with catering contractors to introduce healthier options • offering promotions such as free gifts in return for purchases of fruit and vegetables • introducing a traffic light system to highlight the nutritional value of each option on the menu • providing a nutritional breakdown of all menu items, to help people make informed decisions. 1 National Audit Office 2006. Smarter food procurement in the public sector. The Stationery Office. London iv Additional information on ways that caterers can promote healthy eating can be found in The Food Standards Agency publication Catering for Health. 2 Setting nutrient-based guidelines In the UK, dietary reference values 3 provide population-wide guidance on intakes of energy (calories) and various nutrients (vitamins and minerals). If a population group achieves these dietary reference values, it is likely that all members of the group receive adequate nutrients for their needs. These dietary reference values, as well as new guidance on salt intakes, 4 have been used as the basis for the nutrient-based guidelines in this report. In setting guidelines for different institutions (publicly funded premises) it is also appropriate to consider and report on whether individual population groups served by that institution are getting too little, or too much, of particular nutrients, and whether these problems can be addressed through food provision in these settings. For example, if a population group is not getting enough of a particular nutrient, the guidelines could recommend that the food served by the institution should provide an increased amount of that nutrient relative to the energy content of meals to protect individuals at risk of insufficiency. In order for menu planners to assess whether their menus meet the nutritional guidelines, they will need specialist help from a Registered Public Health Nutritionist or Registered Dietitian, or they will need to use a computer program which contains a breakdown of the nutrients of individual foods and cooked dishes. In Scotland nutrient-based guidelines for school meals have been in use since 2004 and all those involved in catering provision for schools in Scotland have been provided with a computer program to help them plan and monitor the food served against the nutrient-based standards. A similar program is now being planned for school meal providers in Wales. Nutrient-based guidelines provide a framework around which caterers can design a range of menus to meet a variety of needs – including variations in appetite, cultural 2 Food Standards Agency 2001. Catering for Health. London. FSA. Department of Health 1991. Food Energy and Nutrients for the United Kingdom. Report on Health and Social Subjects No. 43. London. HMSO 4 Scientific Advisory Committee on Nutrition 2003. Salt and Health. London. The Stationery Office. 3 v or religious choices, requirements to avoid certain food products (e.g. meat or fish), local customs and traditions and the cost of food. Nutrient based guidelines ensure that food is served that can provide the amounts of nutrients that are needed by different population groups, and these type of standards are therefore considered to be the most robust method of ensuring nutritional needs are met. Setting food-based guidelines In addition to nutrient-based guidelines, it is useful to provide caterers with practical advice on how to choose foods which will contribute to healthy meal provision. The Balance of Good Health provides guidance on the proportion of food and drinks from the different food groups that should make up daily eating patterns to ensure a range of nutrients are consumed. Food-based approaches, which reflect the nutritional guidelines, assist caterers in achieving them. The Balance of Good Health is based on five food groups: • fruit and vegetables • bread, other cereals and potatoes • meat, fish and meat alternatives • milk and dairy foods, and • foods containing fat and foods and drinks containing sugar. The Balance of Good Health . vi Choosing a variety of foods from the first four groups every day will provide the body with the wide range of nutrients which it needs. Foods in the fifth group – foods containing fat and foods and drinks containing sugar – are not essential to a healthy diet but add variety, choice and palatability to meals. This group of foods should form the smallest part of the diet. This report therefore includes, for each public institution, food-based guidelines in terms of the food groups that should be offered at meals and the types of foods within those groups that are most likely to help caterers meet the nutrient-based guidelines. vii Public sector settings and population groups The nutritional guidance provided here provides guidance for public sector settings and population groups where individuals receive all their food and drinks over a 24 hour period as well as guidance for under 5s in child care at meals and snacks. 1.0 : Schools and nurseries • Children aged 1-4 years in child care settings • Children aged 5-18 years at school (caterers should seek appropriate guidance for their area of the UK and links are given here) 2.0 : Children and young people aged 5-18 years in residential accommodation • Children and young people aged 5-18 years in residential accommodation 3.0: The NHS • Children and young people aged 1-18 years (without special dietary needs) who are looked after 24 hours a day • Adults aged 19-74 years (without special dietary needs) who are looked after 24 hours a day • Older people aged 75 years or more (without special dietary needs) who are looked after 24 hours a day 4.0 : Residential care for adults • Adults aged 19-74 years in residential accommodation 5.0: The Prison Service • Male prisoners aged 18-74 years viii • Female prisoners aged 18-74 years 6.0 : Residential care for older people • Adults 75 years and over in residential accommodation 7.0 : Community meals • Adults aged 75 years and over having individual meals The nutritional guidelines for all these groups are based on normal nutritional requirements and do not include information on diets for medical conditions. This report outlines, for each group: • the rationale for the guidelines given • some of the evidence for current nutritional status in these population groups • nutrient-based and food-based guidelines. • an example menu which shows how caterers can meet the nutrient based guidelines ix Acknowledgements This report was written by Dr Helen Crawley on behalf of the Caroline Walker Trust. Thanks are due to Lesley Stark and Gemma Hoffman, research associates at Caroline Walker Trust; Professor Martin Wiseman and other CWT trustees for useful conversations; Sheila Walker for providing some recipes suitable for ethnic minority groups. Particular thanks are due to Rosie Leyden of Wordworks for her careful editing of the text and tables The Caroline Walker Trust PO Box 61 St Austell PL7 6YL www.cwt.org.uk T 020 8542 3469 Contents 1.0 Introduction 2.0 Nutritional guidelines for food served in child care and schools 3.0 Nutritional guidelines for food served in residential premises for children and young people 4.0 Nutritional guidelines for food served on NHS premises 5.0 Nutritional guidelines for food served in residential premises for adults 6.0 Nutritional guidelines for food served in the prison service 7.0 Nutritional guidelines for food served in residential premises for adults 8.0 Nutritional guidelines for food served in residential care for older Adults 9.0 Nutritional guidelines for food served as community meals Appendix 1: Rationale for the calculation of derived reference nutrient values used in this report Appendix 2: Good sources of nutrients Appendix 3: Food customs of ethnic and minority groups Appendix 4: 1.0 Nutritional guidelines for food served in child care and schools 1.1 Children aged 1-4 years in child care The number of children under the age of 5 spending some time being cared for outside the family home has risen substantially as an increasing number of mothers of young children return to the workforce. There are about 3 million children in the UK below compulsory school age and many of these children are cared for in a number of childcare settings including day nurseries, nursery schools, playgroups, with childminders, and in crèches, with au pairs, private nannies, relatives and friends. In addition some under-5s are in early education in both nursery classes and reception classes. The mix of provision of child care has changed substantially in recent years with providers in the public, private and voluntary sectors responding to government initiatives to increase the number of childcare places available through the National Childcare Strategy. Data from Ofsted on registered childcare providers and places showed that over 1.5 million places were available in England in 2005 1 . The largest childcare providers are those offering full-day care and sessional day care (periods of less than 4 hours of continuous care). In Scotland in 2005 there were 263,000 pre-school age children served by 6,100 childminders and 4,717 childcare and pre-school education centres of which 711 were private nurseries. 2 In Wales in 2005 it was reported that there were 72,856 registered childcare places for under-8s 3 and in Northern Ireland, 9,197 places for under-5s were registered with day nurseries and 18,065 places with childminders in 2005. 4 1.2 Food provision in child care Although parents or guardians have the main responsibility for providing adequate and appropriate food for their children, day care providers supply an increasing proportion of the total food eaten by children in their care. In 2006 Ofsted carried out a survey into food served in 110 childcare settings: 64 childminders and 46 day-care providers. 5 The inspectors judged that the majority of providers offered a healthy and 1 Ofsted 2005. Quarterly Childcare Statistics 30 December 2005. www.ofsted.gov.uk 2 Scottish Executive. 2005. Pre-school and Childcare Statistics 2005. Accessed from www.scotland.gov.uk 3 Care Standards Inspectorate for Wales. 2005. CSIW Annual Report 2004-2005. Accessed from www.csiw.wales.gov.uk 4 Information on childcare places in Northern Ireland for the year ending 31st March 2005, accessed from www.publications.parliament.uk/pa/cm200506/cmhansrd/cm060306/text/60306w14.htm 5 Oftsted. 2006. Food for Thought: A Survey of Healthy Eating in Registered Childcare. 1 balanced diet for children but some weaker providers were also identified. Particular concerns in some settings were infrequent serving of fruit and vegetables, lack of variety in snacks served, offering sweets as rewards, and the lack of integration of food served with discussions about healthy eating. A survey published in 2005 carried out among 168 childcare providers in West Yorkshire 6 found that only half of nurseries and a quarter of childminders offered fruit and vegetables at main meals every day. In this study only 14% of nurseries and 21% of childminders offered calcium-rich foods at main meals, and about half provided meat every day. New national standards have been introduced for children in full-day child care, sessional child care, crèches, out-of-school care, and with childminders. These standards are used by those inspecting childcare facilities through the appropriate regional agencies of the UK. The standards for England 7 , Scotland 8 and for Wales 9 provide some guidance for inspectors on food and drink in child care standards but further guidance is required to help them interpret what ‘healthy and nutritious’ meals and snacks means in practice. Nutritional guidance for the early years in Scotland 10 was published in 2006 and this provides practical support to all those working in the sector to meet the Scottish National Care Standards. The Caroline Walker Trust published Eating Well for Under 5s in Child Care in July 2006 11 which provides detailed practical and nutritional guidance for all those in the early years sector. 1.3 Nutrient based guidelines for food served to 1-4 year olds in child care Children have different needs depending on their age and gender, and the requirements of every child will be different. The recommendations therefore represent average intakes. If the food offered to a group of children provides the amount of nutrients recommended, and the children receive the balance of their Accessed from www.ofsted.gov.uk 6 Moore H, Nelson P, Marshall J, Cooper M, Zambas H, et al. 2005. Laying foundations for health: food provision for under 5’s in day care. Appetite; 44: 207-213. 7 www.ofsted.gov.uk 8 www.scotland.gov.uk/library5/education/ncsee.pdf. 9 www.csiw.wales.gov.uk 10 Scottish Executive. 2006. Nutritional Guidance for Early Years. Edinburgh: Scottish Executive. 11 Crawley 2006. Eating Well for Under 5s in Child Care. The Caroline Walker Trust. www.cwt.org.uk 2 requirements at home, then the nutritional needs of most members of that group are likely to be met. The recommendations are based on percentages of the total daily intake of nutrients that fulfil the needs of a group of children, on average, aged 1-4 years. It is assumed that older children in the group will eat larger portions of the food offered, and younger children smaller portions so that the needs of children of different appetites will be met. The nutrient based guidelines have been calculated for different periods of child care as shown below. - 1-4 year olds in child care for a full day (8 hours or more) - 1-4 year olds in half-day care which includes lunch - 1-4 year olds in half-day care which includes tea - 1-4 year olds those who attend for lunch only and - 1-4 year olds that receive a snack during a morning or afternoon session These recommendations apply to children who attend all forms of child care including playgroups, nursery units and reception classes and are based on average dietary reference values for boys and girls. 1.4 Rationale for nutrient based guidelines for specific periods of child care Full day care Children in child care for a full day will receive the majority of their food whilst in child care and therefore it is recommended that the food provided gives the children at least 70% of their daily requirement for energy and nutrients. The remaining 30% will come from breakfast and from any drinks, snacks or light meals the child receives at home. It is recommended that for these children there is provision for two meals (called here 'lunch' and 'tea') and two snacks (mid-morning snack and mid-afternoon snack). 3 Children in half-day care with lunch and snack Half-day care which includes one meal and a snack should provide 40% of a child’s daily energy needs. Children in half-day care with tea and snack or in half-day care having lunch only Children may be in child care for lunch only or for tea and a snack and these meals should provide 30% of the days energy Children having a snack only Children in child care for a morning or afternoon period which does not include a meal should receive a snack during this period if the period of care exceeds two hours, and two snacks if this period is five hours or more but does not include a meal (for example 12.30pm - 5.30pm care, missing lunch and leaving before tea). Snacks should provide about 10% of the day’s energy and nutrient requirements. The amount of non-milk extrinsic sugars is a maximum. It should be noted that there is no necessity to have sugars of this type in snacks or meals. 1.5 Rationale for distribution of nutrients between meals and snacks When setting nutritional guidance for population groups it is normal practice to ensure that the needs of individuals in the group with the highest needs are met – so that where there are discrepancies by age and gender for a specific nutrient for which there is a minimum, the higher value is selected. For children aged 1-4 years however, there is already an expectation that the diet will be nutrient dense and in practice it becomes difficult to enhance the micronutrient intakes relatively higher than the energy value when energy intakes are small. In this group therefore, micronutrient recommendations remain proportional to energy intake: the assumption is that the bigger and hungrier children will eat more and if they eat the types of food as suggested in the sample menus, they will obtain proportionally higher amounts of micronutrients to meet their needs. The exceptions to this are the minerals iron and zinc which are enhanced in main meals for the reasons outlined here. 4 Iron The iron intake of children under 5 is lower than currently recommended and there is evidence to suggest that low iron status is common in this age group. Iron is found in foods that are typically served as part of meals rather than snacks and it is therefore sensible to provide greater amounts of iron at meal times. In addition having vitamin C at the same meal as iron may enhance iron absorption and therefore meals containing food sources of iron with fruits and vegetables present are likely to be beneficial. Drinks (including milk) and many snacks are also likely to be low in iron, so this also suggests that it is important that children receive the bulk of their iron from their meals For this reason it is recommended that the intakes of iron in the diet of 1-4 year olds in child care should be enhanced to provide 80% of the derived reference nutrient intake in full day care, and proportionately more for half-day care as described in the tables that follow. Iron will be particularly provided by main meals. Care needs to be taken when menu planning for children receiving a vegetarian diet to ensure they obtain sufficient iron. Zinc Low intakes of zinc have been reported among a large proportion of Under 5’s particularly when milk intakes start to decline and it is important that good sources of zinc such as meat and meat dishes, cereals, milk and milk products and eggs are included in the diet regularly). Since the majority of zinc is likely to come from foods served at meals it is recommended that the intakes of zinc for children in all day care be enhanced to provide 80% of the reference nutrient intake as for iron above. Vitamin D There is a UK reference value for vitamin D for children aged 6 months -3 years of 7.0ug/day. For children 4 years and above there is an assumption that they will make enough vitamin D through the action of sunlight on their skin. There is increasing concern that many pre-school children have low vitamin D status and parents are recommended to continue giving vitamin D supplementation (though vitamin drops) until their child’s 5th birthday. It is difficult for children to obtain sufficient vitamin D from the diet alone since there are few good sources (see Appendix 1) so to achieve the recommended amounts from food alone is unlikely. The amount of vitamin D that a child should obtain has been included in the guidelines however to both encourage the use of good sources of vitamin D in menu planning and to raise awareness of this as a nutritional issue among under 5’s. 5 1.6 Nutrient based guidelines for children aged 1-4 years Table 1.1 and 1.2 outline the derived nutrient based guidelines for 1-4 years olds in child care for meals and snacks throughout the day. The tables summarise the proportion of nutrients that each eating occasion should achieve for children in child care. The figures are for the recommended average nutrient content of meals and snacks provided for children over a one-week period. The calculation of the derived dietary reference values on which these figures are based can be found in Appendix 1. 6 Table 1.1 Nutrient-based guidelines for food prepared for 1-4 year olds in child care Nutrient Energy Fat Total carbohydrate Non-milk extrinsic sugars Protein FULL-DAY CARE * Morning session: SNACK and LUNCH Afternoon session: SNACK and TEA SNACK only LUNCH only TEA Only % of the Estimated Average Requirement (EAR) % of energy 70% 40% 30% 10% 30% 20% About 35% About 35% About 35% About 35% About 35% About 35% % of energy About 50% About 50% About 50% About 50% About 50% About 50% % of energy MAX 11% 11% 11% 11% 11% 11% MIN 70% 40% 30% 10% 30% 20% Vitamin A % of the Reference Nutrient Intake (RNI) % of the RNI MIN 70% 40% 30% 10% 30% 20% Vitamin D1 % of the RNI MIN 70% 40% 30% 10% 30% 20% Vitamin C % of the RNI MIN 70% 40% 30% 10% 30% 20% Folate % of the RNI MIN 70% 40% 30% 10% 30% 10% Calcium % of the RNI MIN 70% 40% 30% 10% 30% 20% Iron % of the RNI MIN 80% 45% 35% 10% 35% 25% Zinc % of the RNI MIN 80% 45% 35% 10% 35% 25% Sodium % of the SACN target average % of the SACN target average MAX 70% 40% 30% 10% 30% 20% MAX 70% 40% 30% 10% 30% 20% Salt * Full-day care includes a morning snack, lunch, afternoon snack and tea. It does not include breakfast 1 For information on Vitamin D please see page 5 % of energy = Percentage of calories consumed RNI = Reference Nutrient Intake For an explanation of these terms see Appendix 1. EAR = Estimated Average Requirement SACN = Scientific Advisory Committee on Nutrition Table 1.2 Nutrient-based guidelines for food prepared for 1-4 year olds in child care FULL-DAY CARE* Nutrient Energy kcals 903 Morning session: SNACK and LUNCH 516 Afternoon session: SNACK and TEA 387 SNACK only 129 LUNCH only 387 TEA only 258 Fat About g 35.0 20.0 15.0 5.0 15.0 10.0 Total carbohydrate Non-milk extrinsic sugars Protein About g 120.4 68.8 51.6 17.2 51.6 34.4 MAX g 26.6 15.2 11.4 3.8 11.4 7.6 MIN g 11.0 6.3 4.7 1.6 4.7 3.1 Vitamin A MIN µg 300 170 130 40 130 90 Vitamin D1 MIN µg 5 2.9 2.1 0.7 2.1 1.4 Vitamin C MIN mg 21 12 9 3 9 6 Folate MIN µg 60 35 25 8 25 17 Calcium MIN mg 260 150 110 40 110 70 Iron MIN mg 5.5 3.1 2.4 0.7 2.4 1.7 Zinc MIN mg 4.3 2.4 1.9 0.5 1.9 1.4 Sodium MAX mg 630 360 270 90 270 180 MAX g 1.6 0.9 0.7 0.2 0.7 0.5 Salt Numbers have been rounded up or down where necessary, to ensure that figures for different periods of child care add up appropriately. * Full-day care includes a morning snack, lunch, afternoon snack and tea. It does not include breakfast. 1 For information about Vitamin D see page 5 For an explanation of other terms see Appendix 1. 8 1.6 Food based guidance for menu planners The following pages contain some information for caterers about food groups and how to choose foods which will contribute to a healthy balanced diet. It is also useful for caterers to look at food labels on foods and ingredients they buy or use and to choose those that are lower in salt, sugar and fat. The Food Standard’s Agency provides information on what is ‘a lot’ of salt, sugar and fat in foods and these are outlined below. Foods high in salt have 1.25 grams or more salt per 100grams or 500 milligrams of sodium per 100 grams of food Foods high in sugar have 10 grams or more of sugars per 100 grams of food Foods high in fat have 20 grams or more of fat per 100 grams of food Foods high in saturated fat have 5 grams of saturated fat or more per 100 grams of food For more information about nutritional information on food labels see www.eatwell.gov.uk Additional information about foods which are good sources of some of the nutrients which appear to be insufficient in the diets of some people in the UK can be found in Appendix 2. Liver Liver, including liver pate is very rich in vitamin A and it is recommended that these foods are given to children no more than once a week. For more information see SACN (2005) Review of Dietary Advice on Vitamin A. London: TSO 1.7 Food based guidelines for catering for children aged 1-4 years. Food group Guidance Rationale What’s included Bread, other cereals and potatoes Foods from this group should be offered at every meal, and can be useful foods to offer as part of snacks. Starchy foods provide energy, protein, fibre and vitamins and minerals such as the B vitamins, and some calcium, iron and zinc All types of bread – wholemeal, granary, brown, wheatgerm, white, multigrain, soda bread, potato bread, chapattis, naan bread, rotis, rolls, bagels, pitta bread, wraps, tortilla These foods should make up about a third of the food served each day. Starchy foods are filling And provide bulk to the diet Potatoes or sweet potatoes – boiled, mashed, baked or wedges. Potato chips should only be served once a week. Starchy foods are a good choice for snacks as they Yam, plaintain, cocoyam, cassava and other starchy root vegetables Pasta and noodles – wholemeal and white Rice – brown and white rice Other grains such as couscous or bulgur wheat, maize (polenta) and cornmeal Breakfast cereals Tips • • • • • • • Children aged 1-4 may have small appetites and very bulky foods may prevent them getting all the nutrients they need. High fibre foods should be served in moderation. Look for lower-salt breads. Processed potato products like waffles or smiley faces should be avoided. Avoid dried or canned ready-prepared pasta in sauce as these are very salty. Avoid fried rice or flavoured dried rice in packets. Avoid sugary breakfast cereals. (If a food contains more than 10g of sugar per 100g, it is considered a high-sugar food.) Choose low-sugar, low-salt cereals such as porridge, puffed wheat, weet bisks, crisped rice or flaked wheat. Fortified cereals can be a good source of iron. 10 Food group Guidance Rationale What’s included Fruit and vegetables Offer different fruits and vegetables at meals and snacks. Fruits and vegetables offer a range of important nutrients including fibre, vitamins A and C and folic acid Aim for each day’s menu for childcare settings to offer: 1-2 types of fruit and 2-3 types of vegetables. Evidence suggests that people who eat more fruits and vegetables are protected from a number of diseases in later life All types of fresh, frozen and canned vegetables – for example, broccoli, Brussels sprouts, cabbage, carrots, cauliflower, mushrooms, parsnips, peas, peppers, spinach, swede, sweet potato, turnip Children in fullday care should have the opportunity to try 4-5 different fruits and vegetables each day. Encouraging children to try fruits and vegetables when they are young will help to encourage a lifetime enjoyment of these foods Fruits and vegetables also provide colour and texture to the diet All types of salad vegetables – for example, lettuce, watercress, cucumber, tomato, raw carrot, raw pepper, radish or beetroot All types of fresh fruit – such as apples, bananas, pears, grapes, kiwi fruit, oranges, plums, berries, melon or mango All types of canned fruit in juice – for example, peaches, pears, pineapple, mandarin oranges, prunes, guava or lychees Stewed fruit such as stewed apple, stewed dried fruit, stewed plums, stewed currants or stewed rhubarb Dried fruit such as raisins, dried apricots, dates, dried figs, prunes Tips • • • • • • • • • Avoid vegetables canned with added salt and sugar Choose fruit canned in fruit juice rather in syrup Do not overcook fresh vegetables, or cut them up a long time before cooking and leave them in water, or cook them early and re-heat before serving – these practices all reduce the vitamin content. Sugar can be added to sweeten very sour fruit. Avoid dried fruit with added sugar and vegetable oil. Serve dried fruit with meals and not as snacks as the sugars in dried fruit can damage teeth Add vegetables to dishes such as stews, soups and casseroles Use fruit in desserts and when making cakes and biscuits Add dried fruit to milk puddings and yoghurts 11 Food group Guidance Rationale What’s included Meat, fish and meat alternatives Main meals should always contain an item from this group. Foods in this group are a good source of protein and are often high in iron and zinc. Meat. All types including beef, lamb, pork, chicken, turkey and offal such as liver1 and kidney. Offer a variety of meat, fish and alternatives each week Lean meat will have greater proportions of nutrients than meat products Meat products such as ham, bacon, corned beef, sausages, meat pies, coated meat products Include fish in the menu at least once a week Fish is a good source of protein and is low in fat. Oil rich fish are a good source of n-3 (omega 3) polyunsaturated fats which are thought to be beneficial for heart health Fish includes: • white fish such as cod, haddock, coley and white fish varieties from sustainable fish stocks such as pollack, saithe and blue whiting • oil-rich fish such as herring and mackerel, salmon, trout, sardines, sprats or pilchards. Canned tuna does not count as an oil-rich fish but is a good source of nutrients. Oil rich fish should be served regularly Make sure meat alternatives are varied for vegetarians Eggs including boiled, scrambled or poached, or in an omelette Pulses including all sorts of beans and peas such as butter beans, kidney beans, chick peas, lentils, processed peas or baked beans Meat alternatives – such as soya mince, textured vegetable protein, quorn or tofu Tips • Reduce intakes of meat products which are high in fat and salt such as crumb-coated chicken products, burgers, pies and canned meats. Some meat products such as sausages are popular with under-5s. Choose good quality versions if you serve these foods. • Reduce intakes of processed fish products such as fish fingers or fish cakes • Make sure all fish dishes are free of bones. • All eggs should be well cooked. • Look for canned pulses with no added salt and sugar. • Dahl and other dishes made from pulses should be made without adding a lot of oil and salt. • Choose lower-salt and lower-sugar baked beans. • Reduce intakes of processed products made from meat alternatives (e.g. vegetarian sausages, burgers and pies) as these can be high in fat or salt 1 Liver and liver pate are high in vitamin A and should be served to children no more than once a week 12 Food Group Guidance Rationale What’s included Milk and milk priducts Foods from this group should be offered at 2-3 meals and snacks each day. Milk and dairy products are excellent sources of calcium which is needed for optimal bone strength protein, vitamin A, riboflavin and vitamin D. Milk – Whole milk should be served for under-2s. Over-2s can have semi-skimmed milk if they are good eaters. Cheese e.g. Cheddar, cottage cheese, cheese spreads, feta, Edam, parmesan, pasteurised soft cheeses Yoghurt and fromage frais Tips • • • • • • • • • Offer plain milk drinks between meals Avoid unpasteurised milk and milk drinks with added sugar. Avoid unpasteurised cheese and mould-ripened (blue-vein) cheeses. Vegetarian cheese should be used where appropriate. Avoid yoghurts and fromage frais that have a high sugar content. It is preferable to add fresh fruit to natural yoghurt or natural fromage frais. Frozen yoghurts can be offered as an alternative to ice cream. Milk can be used in sweet and savoury sauces, custards and milk puddings. It is worth highlighting that some dairy products can contain high salt levels. Strong cheese can impart flavour in smaller amounts and cheese dishes may not need the addition of extra salt For dairy-free diets: serve soya drinks fortified with calcium as an alternative. 13 Food group Guidance Rationale What’s included Foods containing fat and foods and drinks containing sugar These foods add palatability to the diet and can increase the energy density of the diet for those with a small appetite The main nutrients provided by such foods are fat, including some essential fatty acids, and also some fatsoluble vitamins. These foods can be high in calories and offer few other nutrients. If appetites are poor it is important that these foods do not displace more nutrientrich foods. Carbohydrate (in the form of sugars) is also provided. Foods containing fat include butter, margarine, other spreading fats and low-fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, and gravies. Sweet foods eaten between meals can damage teeth. Keep sugary foods and drink to mealtimes only Some foods in this groups can also be high in salt. Foods containing sugar include soft drinks, sweets, jams and sugar, as well as foods such as cakes, puddings, biscuits, pastries and ice cream. Tips • • • • • Use mono- and polyunsaturated fat (such as sunflower, soya, olive, safflower, rapeseed, corn oil) based spreading fats and in salad dressings For cooking use fats high in monounsaturates such as soya, rapeseed and olive oils When making cakes and puddings include dried fruit or fresh fruit, Avoid sugary drinks between meals and always serve any drink other than milk or water in a cup Dilute 100% fruit juice with water for 1-4 year olds To increase the amount of dietary VITAMIN D in menus served in child care • • • • • Use margarine fortified with vitamin D for baking and as a fat spread. Include an oil rich fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 5-14µg of vitamin D per 100g. Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. Meat and poultry contribute small but significant amounts of vitamin D. 14 1.8 Example menus for food served to 1-4 year olds in child care The example menus given here show the sorts, and amounts of foods and drinks that could be offered to a group of 1-4 year olds which meet the nutritional and foodbased guidance. A nutritional analysis is provided to show how these menus compare with the nutritional guidelines suggested for this group across the whole day. For further practical advice on helping children aged 1-4 years eat well see The Caroline Walker Trust report Eating Well for Under 5s in Child Care 12 12 Crawley 2006. Eating Well for under 5s in Child Care. The Caroline Walker Trust. www.cwt.org.uk 15 1.9 An example menu for 1-4 year olds in child care (menu 1) Mid morning snack Water available Lunch Water and diluted fruit juice available Monday Tuesday Wednesday Thursday Friday Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Canned peaches in juice (100g) with whole milk yoghurt (60g) Tabbouleh (65g) with breadsticks (14g) and cherry tomatoes (40g) Vanilla yoghurt (60g) with banana (40g) Sliced grapes (40g), celery(20g) and red pepper slices (20g) Wholemeal savoury pancakes (40g) with butter (4g) and apple chunks (40g) Chicken korma (180g) Brown rice (80g) Naan bread (20g) Lamb burgers (45g) Bubble and squeak (100g) Sardines (40g) on toast (27g) Sliced tomato (40g) Vegetable and lentil lasagne (180g) Mixed salad (45g) Cottage pie (180g) Peas (40g) Broccoli (40g) Stewed apples (70g) with custard (60g) Rhubarb crumble (60g) Fresh fruit salad (80g) Rice pudding with sultanas (180g) Midafternoon snack Water available Tea Water and diluted fruit juice available Milk jelly (120g) with mandarins (80g) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Cucumber and carrot sticks (40g), pitta fingers (50g), mint and cucumber dip (25g) Plain popcorn (20g) Sliced pear (40g) Wholemeal toast fingers (20g) with margarine (4g) and apple slices (40g) Paprika potato wedges (65g), cheese chunks (15g) Orange segments (40g) Fromage frais (60g) with pineapple (100g) Egg and cress sandwiches (90g) Lettuce (40g) Cherry tomatoes (40g) Tuna and sweetcorn pasta (140g) Cucumber (20g) Red pepper (20g) Spanish omelette (80g) Baby jacket potatoes (90g) Baked beans (60g) with toast squares (30g) Chicken and vegetable couscous (145g) Salad (25g) Banana custard (100g) Fromage frais (60g) and Satsuma (40g) Semolina (100g) with pears (40g) Yoghurt with dates (145g) Fresh fruit jelly (60g) 16 1.10 An example vegetarian menu for 1-4 year olds in child care (menu 2) Mid morning snack Water available Lunch Water and diluted fruit juice available Midafternoon snack Water available Tea Water and diluted fruit juice available Monday Tuesday Wednesday Thursday Friday Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Breadsticks (14g) with houmous (20g), cherry tomatoes (40g) Wholemeal savoury pancakes (40g) with butter (4g), celery sticks (40g) Apple chunks (40g) and sliced grapes (40g) Yoghurt (60g) with sliced banana (40g) Wholemeal toast fingers (20g) with margarine (4g) and carrot sticks (40g) Vegetarian Bolognese (120g) with wholemeal spaghetti (80g) Stuffed peppers (110g) Potato salad (45g), Beansprout and tomato salad (40g) Broccoli quiche (100g) Mashed potato (80g) Baked beans (55g) Chickpea fritters (90g) Sweet potato (80g) Sweetcorn (40g) Green beans (40g) Mixed bean casserole (160g) Mashed potato (80g) Petits pois (40g) Swede (40g) Semolina pudding with dates (140g) Banana custard (100g) Stewed fruit (70g) with Greek yoghurt (30g) Milk jelly (120g) with mandarins (80g) Fresh fruit salad (80g) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Cucumber and carrot sticks (40g), cream crackers (12g), soft cheese (20g) Fromage frais (60g) with canned peaches (100g) Breadsticks (14g) with mint and cucumber dip (30g) and kiwi slices (40g) Plain popcorn (20g) Apple chunks (40g) Curried rice salad (45g), yellow and orange pepper slices (40g) Egg and cress sandwiches (90g) Lettuce (40g) Wholemeal pasta twirls (80g) Chickpea salad (50g) Cucumber and carrot sticks (40g) Vegetable couscous (100g) Mixed salad with butter beans (80g) Coleslaw (35g) Baby jacket potatoes (90g) with ratatouille and tofu sauce (140g) Quorn burger (45g) and bun (50g) Salad (40g) Fruit flan (100g) Greek yoghurt with orange (70g) Rice pudding with sultana (180g) Oaty fruit crumble (80g) with custard (60g) Orange and lemon rice (120g) 17 1.11 An example menu for 1-4 year olds in child care including multicultural choices (menu 3) Mid morning snack Water available Lunch Water and diluted fruit juice available Midafternoon snack Water available Tea Water and diluted fruit juice available Monday Tuesday Wednesday Thursday Friday Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Wholemeal toast (23g) with soft cheese (20g) and grape slices (40g) Natural yoghurt (60g) with sliced banana (40g) Wholemeal savoury pancakes (40g) with butter (4g) and canned peaches in juice (100g) White bread fingers (23g) with tuna pate (15g) and apple chunks (40g) Fromage frais (60g) with canned pineapple chunks in juice (100g) Coconut fish curry (100g) Basmati rice (80g) Sliced tomato (40g) Chicken fajitas (120g) Sweetcorn salsa (30g) Mixed salad (40g) Sweet and sour pork (120g) Egg noodles (70g) Stir-fried vegetables (100g) Channa aloo (80g) Masur dahl (40g) Mixed vegetable pilau (80g) Chilli con carne (100g) Jacket potato (90g) and crème fraiche (20g) Watercress salad (40g) Stewed fruit (70g) and whole milk yoghurt (50g) Lemon sorbet (40g) with wafers. Chinese fruit salad (115g) Neapolitan ice cream (50g) Banana custard (100g) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Milk (100ml) Pitta bread fingers (55g) with houmous (20g), carrot and cumber sticks (40g) Sliced celery (20g), grapes (40g) and red pepper (20g) Plain popcorn (20g) Lychees (40g) Breadsticks (14g) with raita (30g) Clementine (40g) Paprika potato wedges (60g) Tomato and sweetcorn salsa (32g) Spicy ratatouille with tofu (100g) Flat bread (50g) Spanish omelette (90g) Potato dice (60g) Cucumber, red pepper and spring onion (50g) Fruity couscous with kidney beans(105g) Mixed salad (45g) Chapati (45g) Chickpea salad (55g) Cucumber and carrot sticks (40g) Chicken tikka filling (60g) Wrap (20g) Mexican salad (45g) Watermelon (40g) Fruit smoothies (100ml) Chewy cereal bar (20g) Rice pudding with mandarins (100g) Spiced banana crumble (75g) Fromage frais with dates (100g) 18 1.12 Nutritional analysis of example menus for 1-4 year olds Average nutrient values from sample menus Nutrient based Guideline (full-day) Menu 1 Menu 2 Menu 3 941 4.0 27 970 4.1 22 956 4.0 30 Kcals MJ g Max 903 3.8 35.0 Total carbohydrate g Min 120 137 155 140 Non milk extrinsic sugars g Max 27 17 21 19 Protein g Min 11 46 39 41 Vitamin A µg Min 300 553 1084 721 Vitamin C mg Min 21 76 90 87 Folate µg Min 60 160 180 140 Calcium mg Min 260 770 684 650 Iron mg Min 5.5 5.8 7.5 6.2 Zinc mg Min 4.3 5.1 4.9 4.5 Sodium mg Max 630 704 785 630 g Max 1.6 1.7 1.9 1.6 Energy Fat Salt 19 1.13 Nutritional guidelines for school children aged 5-18 years Nutritional guidance for school meals was published as part of the Hungry for Success initiative in Scotland in 2002 13 and has recently been published for England 14 . Nutritional standards for school meals in Wales 15 are currently under consideration through their document Appetite for Life and in Northern Ireland standards produced for use in England are likely to be adopted. These standards involve both food based and nutrient based guidance. Some foods will no longer be made available to children in schools. In addition The Food Standards Agency’s voluntary target nutrient specifications set maximum levels for total fat, saturated fat, sodium/salt and sugar in a range of manufactured foods used in school meals, including bread, poultry products, soups, sausages and burgers. In addition, target minimum values for protein have been set for certain products to help ensure an adequate protein intake when pupils select vegetarian options. These can be found at www.food.gov.uk Caterers should ensure that they have copies of the nutritional guidance for schools for the area in which they live and that they are aware of the regulatory aspects relating to school food in their area. The Caroline Walker Trust report Eating Well at School 16 provides details of the rationale for standards for school food and nutrient based guidelines for schools by age and gender type, and this data formed the basis of the standards for England. Similar information is contained within the Hungry for Success and Appetite for Life documentation. Example menus and practical advice on how to achieve these guidelines are included in these documents. Additional practical advice and guidance can be obtained from The School Food Trust (www.schoolfoodtrust.org.uk) the Food in Schools Toolkit (www.foodinschools.org) and from the Food Standards Agency (www.eatwell.gov.uk). 13 Scottish Executive 2002. Hungry for Success; A whole school approach to school meals in Scotland. Scottish Executive. Edinburgh 14 DfES 2006. Turning the Tables: Transforming School Food - Recommendations for the Development and Implementation of Revised School Lunch Standards. http://www.teachernet.gov.uk/wholeschool/healthyliving/ 15 Welsh Assembly 2006. Appetite for Life. http://new.wales.gov.uk/consultations/ currentconsultation/2656718/486602/;jsessionid=37D364111E8032F26883F058FFE4F3C9.www2?lan g=en 16 Crawley 2005. Eating Well at School. The Caroline Walker Trust. www.cwt.org.uk 20 2.0 Nutritional guidelines for food served in residential accommodation for children and young people aged 5 -18 years 0 2.1 Background Children and young people may spend periods of time in residential care for a number of reasons. This may be because they have a health or social need specific need, it may be that their parents, extended family or other carers are unable to look after them and they are in the care of the state or it may be that they are required to spend time in secure accommodation. Whilst it is possible for children younger than 5 years to be in residential accommodation, in practice it is unlikely that younger children will live in residential units and therefore the nutritional guidelines in this chapter are aimed at children aged 5-18 years. In 2005 there were 60,900 children looked after in England, 3,300 of whom were in residential settings. There were also 12,185 looked after children in Scotland, 1,539 of whom were in residential care. In Wales in 2005 there were 4,668 looked after children, 234 of whom were in residential accommodation and in Northern Ireland there were 2,531 looked after children, 317 of whom were living in residential accommodation 1 . Whilst the numbers of children and young people living in residential accommodation is therefore relatively small, these children and young people may be particularly vulnerable and many of them are likely to have had poor nutrition in their early years and poor experiences of food in their early lives. The Caroline Walker Trust reviewed the need for guidance on eating well in their 2001 report Eating well for looked after children 2 and this book summarised the limited evidence available that suggests that there is a particular need for good nutrition in this population group. Healthy eating and physical activity are fundamental for proper growth and development in childhood and essential for good health and well-being in later life. To help children and young people develop patterns of healthy eating from an early age, it is important that the food and eating patterns to which they are exposed are those which promote positive attitudes to good nutrition. 1 2 https://www.baaf.org.uk/info/stats/ The Caroline Walker Trust 2001. Eating Well for Looked After Children. www.cwt.org.uk 1 There is evidence that the diets of children and young people in Britain are too low in vitamins A and C, iron, zinc and calcium and are too high in salt and the types of sugars that can damage teeth. The diets of many children and young people are also very low in fruits and vegetables. 3 It is therefore important that the food served to children and young people in residential accommodation provides enough of those vitamins and minerals that may typically be in short supply and that they have the opportunity to try, and hopefully eat, at least five different fruits and vegetables every day 2.2 Rationale for nutrient-based guidelines for children and young people in residential care The derived dietary reference values calculated for the age groups 5-10 year and 1118 years are explained in Appendix 1. Using these derived reference values it is assumed that menus offered in residential care for children and young people will provide all of the nutrients needed in the meals served. The values for 11-18 year olds for energy, fat, carbohydrate and protein are given as ranges. These reflect the fact that young people will be growing at very different rates and that some will have much greater needs for energy and nutrients since they may be growing rapidly, be physically bigger, be more active or all three. If the menus offered provide nutrients in the right balance then hungrier young people will eat bigger portions to satisfy their appetites. The current standards for school meals across the UK suggest that whilst a main meal should provide about 30% of energy it is prudent that it provides a greater proportion of vitamins and minerals to ensure adequacy, since these nutrients are more commonly found in meals compared to snack foods. The nutrient-based guidelines here assume that the total nutrients are met from an average intake of all the food served over a period of one week, but the proportions of energy and nutrients at meals and snacks should mirror the current recommendations made for school meals. Whilst there are differences between the school meal guidance in England, Scotland and Wales these differences are relatively small, and in practical terms menus which achieve the guidance for England and Wales will also meet the guidance for Scotland. For this reason the values adopted here for the distribution of 3 Gregory J, Lowe S, Bates C,J, Prentice A, Jackson L, Smithers G, Wenlock R, Farron M. 2000. The National Diet and Nutrition Survey: Young people aged 4-18 years, The Stationery Office. London 2 macro and micronutrients at meals for children and young people in residential accommodation are based on those for school aged children in England and Wales. The distribution of energy and other nutrients at meals and snacks will be as described in table 2.1. These figures will ensure that intakes of fat, saturated fat, salt and sugars are not too high and that sufficient amounts of all nutrients are provided. 2.3 Rationale for increasing intakes of some micronutrients at main meals for children and young people in residential accommodation The rationale for the setting of the guidance for children in residential accommodation across the UK is based on evidence that the diets of many school aged children contain insufficient amounts of some important micronutrients, as well as some foods such as fruit and vegetables and oil rich fish. Data from the National Diet and Nutrition Survey of young people aged 4-18 years published in 2000 4 showed that many children and young people do not get enough of certain important nutrients – for example iron, calcium, zinc, vitamin A, vitamin C and folate. For this reason the proportion of these micronutrients has been enhanced in main meals for school aged children in relation to their energy intake, to protect children and young people from insufficiencies. So, for example, although the amount of energy provided by a main meal is 30%, the amount of iron it provides should be 40%. The reason for this is that the majority of some nutrients are likely to be consumed at mealtimes rather than between meals as snacks, and therefore meals should provide a greater proportion of some important nutrients. It is also recommended that in a group of children or young people, the nutrient based guidance should meet the requirements of those children with the greatest needs. So, among mixed gender groups of children, the guidance for iron will meet the needs of the girls in the group who have higher requirements, and the standards for calcium, zinc and vitamin A will meet the greater needs of the boys in the group. Guidance given here assumes that groups will be of mixed gender. For children and young people in residential accommodation, the guidance presented here allows for two main meals of the same nutritional quality as is currently 4 Gregory J, Lowe S, Bates CJ, Prentice A et al 2000. National Diet and Nutrition Survey: Young People aged 4-18 years. London. The Stationery Office. 3 proposed for school meals since some children and young people in residential accommodation may not have their main meal as a school meal each day. Table 2.1 The proportion (%) of daily energy and nutrients to be supplied by meals and snacks Energy Protein, carbohydrate, non-milk extrinsic sugars, fat, saturated fat, fibre and salt Vitamin A, Vitamin C, Folate, Calcium, Iron and Zinc Breakfast 20% 20% 20% Lunch 30% 30% 40% Evening meal 30% 30% 40% Snacks 20% 20% + Total 100% 100% 100%+ For this population group it is recommended that 100% of micronutrient intakes are met at the three main meals each day. Additional micronutrients are likely to be provided by nutritious snacks, but since there is some evidence that children and young people in residential accommodation may be a particularly vulnerable group with some children having early experience of poor diet and poor health care 5 , this would appear prudent. Children and young people will not be exposed to excessive micronutrient intakes if they eat and drink the sorts of foods and drinks at meals and snacks recommended here. Vitamin D Young people who spend little time outside (e.g. less than half an hour a day during the summer months April to September) may not make enough vitamin D in their skin. It is difficult to get enough vitamin D from the diet alone, since there are few good food sources of vitamin D. If young people spend most of their time indoors for whatever reason, they may need vitamin D supplements. If young people rarely go outside and when they do wear clothing which covers most of their skin they may also be at risk of low vitamin D status. Young women who may become pregnant should consult their GP about their need for vitamin D during pregnancy. 5 The Caroline Walker Trust 2001. Eating Well for Looked After Children. www.cwt.org.uk 4 Folic acid Folic acid is another name for folate. It is important that all women who may become pregnant have sufficient folic acid. Young women who live in residential accommodation and who may become pregnant should consult their GP about the need for folic acid before and during pregnancy. Fluid intakes It is important that everyone has access to adequate fluid intakes throughout the day. In climates such as the UK, we should drink approximately 1.2 litres (6 to 8 glasses) of fluid every day to stop us getting dehydrated. In hotter climates the body needs more than this. We get some fluid from the food we eat but it is important that fluids are not restricted since dehydration can lead to headaches, confusion and irritability and lack of concentration as well as constipation and potentially urinary tract infections. Clean, chilled water should always be available with meals and between meals. 5 Table 2.2 Nutrient based guidelines for food served to children and young people in residential accommodation kcals MJ Energy Dietary reference value (DRV) Children 5-10 years Young people 11-18 years EAR 1780 7.5 1845 – 2755 7.7 – 11.6 Fat g No more than 35% of energy MAX 70 72 -107 Saturated fat g No more than 11% of energy MAX 22 23 -34 Total carbohydrate g At least 50% of energy MIN 237 246 - 367 Non-milk extrinsic sugars g No more than 11% of energy MAX 52 54 - 81 Fibre g DRV MIN 14 18 Protein g RNI MIN 25 41-55 Vitamin A µg RNI MIN 500 700 µg RNI MIN - - Vitamin C mg RNI MIN 30 40 Folate μg RNI MIN 150 200 Calcium mg RNI MIN 550 1000 Iron mg RNI MIN 9 15 Zinc mg RNI MIN 7 9.5 Sodium mg 1800 2400 4.5 6 Vitamin D1 Salt g SACN recommendation SACN recommendation MAX MAX EAR = Estimated Average Requirement DRV = Dietary Reference Value RNI = Reference Nutrient Intake For explanation of terms see glossary 1 Although there is not an RNI for Vitamin D for this age group it is assumed that all young people will spend at least half an hour outside each day during the summer months to ensure they make enough vitamin D. Young people who are housebound or do not regularly go outside or who go outside infrequently and wear clothing which means their skin is not exposed to the sun are likely to require vitamin D supplements. 6 2.4 Food based guidance for menu planners The following pages contain some information for caterers about food groups and how to choose foods which will contribute to a healthy balanced diet. It is also useful for caterers to look at food labels on foods and ingredients they buy or use and to choose those that are lower in salt, sugar and fat. The Food Standard’s Agency provides information on what is ‘a lot’ of salt, sugar and fat in foods and these are outlined below. Foods high in salt have 1.25 grams or more salt per 100grams or 500 milligrams of sodium per 100 grams of food Foods high in sugar have 10 grams or more of sugars per 100 grams of food Foods high in fat have 20 grams or more of fat per 100 grams of food Foods high in saturated fat have 5 grams of saturated fat or more per 100 grams of food For more information about nutritional information on food labels see www.eatwell.gov.uk Additional information about foods which are good sources of some of the nutrients which appear to be insufficient in the diets of some people in the UK can be found in Appendix 2. Liver Liver, including liver pate is very rich in vitamin A and it is recommended that these foods are given to children no more than once a week. For more information see SACN (2005) Review of Dietary Advice on Vitamin A. London: TSO 7 2.5 Food-based guidelines for food served to children and young people in residential accommodation Food Group Guidance Rationale What’s Included Bread, other cereals and potatoes Starchy foods should make up a third of the daily diet. Starchy foods are a good source of energy and the main source of a range of nutrients in the diet. As well as starch, these foods supply fibre, calcium iron and B vitamins. All varieties of bread including wholemeal, granary, seeded, chapattis, bagels, roti, tortillas, pitta bread A variety of breads should be available daily at every meal Different starchy foods should be offered in main meals throughout the week so that a variety of starchy foods are included. Aim to include pasta and rice on the menu once a week Potatoes, yam, sweet potato, plantain, cocoyam, dasheen, breadfruit, cassava Breakfast cereals Rice, couscous, bulgar wheat, maize (polenta), cornmeal Noodles, spaghetti and other pastas Wholegrain and wholemeal cereal foods are a good source of fibre and other nutrients Tips • • • • • • • • • Serve more pasta and rice and use less sauce. Opt for tomato based sauces instead of cheese-based to reduce fat content When serving rice and pasta, try to use wholemeal, wholegrain, brown or high fibre versions. Some breakfast cereals are nutrient fortified (have added iron, folic acid and other vitamins and minerals). Choose wholegrain cereals or mix some in with other cereals. Offer a variety of breads, such as seeded, wholegrain and granary and use thicker slices with low-fat options for fillings Large pieces of potato and thick or straight cut chips absorb less fat Boil potatoes in the minimum amount of water and for the shortest amount of time to retain vitamins. Use herbs or other shredded vegetables to add colour and flavour to baked potatoes, rather than butter or margarine. If you look after young people who have allergies to wheat, oats, barley and rye: good alternatives to offer are foods made from maize (e.g. polenta), rice, rice flour, potatoes, potato flour, buckwheat, sago, tapioca, soya and soya flour. Cereal foods which are good sources of iron and zinc include fortified cereals, whole grain cereals, wholemeal bread and flour, couscous and wholemeal pasta. 8 Food Group Guidance Rationale What’s Included Fruit and Vegetables Fruit and vegetables should make up about a third of the daily diet. Fruit and vegetables are good sources of many vitamins and minerals. All types of fresh, frozen and tinned vegetables i.e. broccoli, Brussels sprouts, cabbage, carrots, frozen peas, peppers, swede, sweetcorn It’s important to offer a variety. Five-a-day is an achievable target. Aim for one or two portions with each meal and offer fruit and vegetables as snacks. One portion s about 80g fresh fruit and vegetables and 40g of dried fruit Beans and pulses are included but only count as a maximum of 1 portion per day A glass of 100% fruit juice can count as one portion of fruit each day There is evidence that consuming 400g a day or more of fruit and vegetables reduces the risk of developing chronic diseases such as coronary heart disease and some cancers. Including fruits and vegetables in the diet will help to increase the intake of fibre and can help to reduce the total amount of calories consumed among those who may wish to lose weight All types of salad vegetables including lettuce, cucumber, tomato, raw carrots, peppers, beetroot All types of fresh fruit e.g apples, bananas, kiwi fruit, oranges, pears, mango, plums All types of tinned fruit in fruit juice e.g. pineapple, peaches, mandarin oranges Stewed fruit Dried Fruit Fruit juice (100% juice) Tips • • • • • • • • • • • • • • • • Avoid adding fat or rich sauces to vegetables or sugar or syrupy dressings to fruit Steaming or cooking vegetables with minimum amounts of water and serving as soon as possible will help retain vitamins. Use fresh fruit and vegetables as soon as possible, rather than storing, to avoid vitamin loss Incorporate fruit and vegetables in snack options. Offer a variety of healthy snack alternatives Add vegetable and pulses to curry, casserole or stir-fry and serve at least two types of vegetables with fish, chicken or meat. Baked beans (as a vegetable) should be served a maximum of twice a week Encourage a daily glass of fruit juice (100% juice, unsweetened) with meals Choose tinned fruit in fruit juice not in syrup Add a handful of dried fruit to cereal options and porridge Supply a good combination of traditional salads and raw vegetables, fruits and nuts to increase colour, taste and texture at meal times Add additional vegetables to savoury dishes Vegetable soups are a useful way of increasing vegetable intake Avoid dried fruit with added sugar or vegetable oil Fruit and vegetables which are useful sources of iron include spinach, broccoli, spring greens, dried apricots, raisins, baked beans, broad beans and blackcurrants Fruit and vegetables which are useful sources of folate include spinach, broccoli, peas, oranges, melon, green leafy salads and tomatoes. Fruit and vegetables which are useful non-dairy sources of calcium include green leafy vegetables, dried fruit and oranges. 9 Food Group Guidance Rationale Milk and Dairy Products Offer dairy foods such as milk, yoghurt and cheese as part of meals and snacks Milk and dairy products are excellent sources of calcium, protein, vitamin A and vitamin D. Calcium helps to contribute to good bone health Offer low fat options such as semiskimmed milk, low fat yoghurt and skimmed milk cheeses The fat content of different dairy products varies and much of this is saturated fat. Skimmed, semi-skimmed, whole milk Dried milk, goats and sheep’s milk All types of cheeses e.g. Cheddar cheese, cottage cheese, cheese spreads, brie, feta, Edam, goats cheese, stilton, parmesan Yoghurt Fromage frais Do not rely on cheese as the main protein item for vegetarians. Where no other option is available, cheese served as a sandwich filler should be offered no more than twice per week. Tips • • • • • • • • • • Try using very strong-tasting cheese (mature cheddar, blue cheese) if using to flavour dishes or sauces, because less will be required. Choose reduced-fat hard cheeses, cottage cheese and skimmed milk soft cheese Offer semi-skimmed or skimmed milk and low-fat yoghurts and fromage frais. Use plain yoghurt and fromage frais instead of cream, soured cream or crème fraiche in recipes Try serving frozen yoghurts as an alternative to ice cream. It is worth highlighting that some dairy product can contain high salt levels. Look for lower salt cheeses and use smaller amounts of stronger cheese Dairy foods are very important during pregnancy, but unpasteurised dairy produce and softmould-ripened cheese (e.g. camembert, Brie and all blue-veined cheese) should be avoided For those on dairy free diets serve soya drinks fortified with calcium as an alternative. Fresh fruit milkshakes and chilled milk drinks can be offered as snacks Restrict sweetened milk drinks to mealtimes as the sugars in these drinks can damage teeth 10 Food Group Guidance Rationale What’s Included Meat, fish and meat alternatives Offer a meat or alternative at all main meals Meat and meat alternatives are a good source of protein, vitamins and minerals such as iron and zinc Use lean meat (which has a fat content of about 10%) Some meat and meat products can have a high fat and saturated fat content Meat includes all cuts of beef, pork, lamb, poultry, offal1 and meat products such as bacon, sausages, beef burgers, pies and cold meats Fish should be offered at least twice per week. White fish is low in fat It is strongly recommended that oily fish such as salmon, trout, mackerel, herring, pilchards, sardines should be served once a week Oil-rich fish provides a good source of omega-3 fatty acids, which may help to protect against heart disease. Oil-rich fish are also a source of vitamins A and D. Eggs can be served at breakfast and as part of main meals Eggs are a good source of protein, vitamin A,vitamin D and some minerals Beans, pulses, eggs, meat alternatives and nuts all provide good sources of nutrients. Ensure meat alternatives for vegetarians are varied Fish includes fresh, frozen and tinned fish, such as tuna and sardines, Fish products such as fish cakes and fish fingers may have a low fish content Boiled, poached, scrambled eggs, omelettes Beans and pulses such as chick peas, lentils, kidney beans, butter beans, textured vegetable protein, nuts, soya products such as tofu, quorn Tips • • • • • • • • 1 Always select the leanest cuts of meat and remove visible fat and poultry skin Roast meat on a rack in order to let the fat run off. Grill, poach or bake meat rather than frying. If you do fry, use clean oil and at the correct temperature to minimise absorption. Note that larger pieces of fish and meat absorb less fat. Do not add extra fat or oil when cooking meat Use more vegetables, pulses and starchy food to extend dishes further, as well as add more texture and flavour. Less meat is also required, reducing the fat content and the cost of the meal. Offer unsalted nuts and seeds as snacks Reduce the amount of processed meat products served such as meat pies and pasties, coated, canned and composite meat products such as sausages, burgers, coated chicken products Reduce the amount of processed fish products on offer, particularly those that are fried or coated such as fish fingers or fish cakes Liver and liver pate are very high in vitamin A and should not be erved more than once a week 11 Food Group Guidance Rationale What’s Included Foods containing fat and foods and drinks containing sugar These foods can add palatability to the diet but should be eaten in small amounts each day Foods containing fat and foods containing sugar often provide a lot of calories and a lower proportion of other nutrients. Foods containing fat include: Reduce the amount of foods containing visible fat for example, margarine and butter, cooking oils and mayonnaise. Other foods containing fat such as cakes and biscuits should be eaten occasionally Foods and drinks containing sugar often contain few other nutrients and frequent consumption between meals can contribute to tooth decay Some foods in this group are also high in sodium/salt Butter, margarine, other spreading fats and low fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, gravies. Foods and drinks containing sugar include: Soft drinks, sweets, chocolate, jams, sugar, cakes, puddings, biscuits, pastries and ice cream Tips • • • • • • • • • • • Use mono- or poly-unsaturated fat spreads Use cooking oils high in monounsaturates such as soya, rapeseed or olive oils Avoid serving pastry dishes frequently Measure oil for cooking carefully and reduce oil used in the preparation of soups, stews and casseroles. Vegetables can often be dry fried, steamed or stewed to form the basis of sauces and other dishes Use low-fat yoghurt or non-dairy ice cream to compliment puddings or pies. Produce puddings lower in fat and sugar and incorporate fresh, tinned fruit in juice or dried fruit. Offer water, unsweetened fruit juices and chilled milk drinks Serve wholegrain or plain cereals rather than sugar coated cereals Provide currant buns, fruit bread, melon slices, malt loaf and other lower fat bread based foods as alternatives to cakes and biscuits. When preparing sandwiches, try and avoid using butter or spreads if the filling is already moist. Consider using reduced-fat spreads and opt for types that are soft straight from the fridge, so it is easier to spread thinly. To increase the amount of dietary VITAMIN D in menus • • • • • Use margarine fortified with vitamin D for baking and as a fat spread. Include an oily fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 5-14µg of vitamin D per 100g. Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. Meat and poultry contribute small but significant amounts of vitamin D. 12 2.6 Example menu for children and young people in residential accommodation An example menu is given here which show the sorts of foods that could be served to meet the nutritional and food-based guidance for children and young people. The menu is shown twice: firstly with portion sizes suitable for children aged 5-10 years (2.7) and secondly with portion sizes suitable for those aged 11-18 years (2.87. The analysis of both menus is included on pages 18 and 19. The example menus shown here include a sandwich style meal, however this is just an example. Caterers may wish to offer a variety of hot and cold meals at lunch and tea and may choose to offer one, two or more choices depending on the client groups that they serve. 13 2.7 Menu for children and young people in residential accommodation aged 5-10 years Monday Breakfast Midmorning Lunch Water or 100% fruit juice Tuesday Wednesday Thursday Friday Saturday Sunday Raw carrots/cucumber/pepper slices (40g) Pizza with choice of toppings (120g) Coleslaw (80g) Jacket potatoes (180g) Roast turkey (80g) Stuffing (30g) Roast potato (150g) Carrots (80g) Broccoli (80g) Fromage frais or yoghurt (60-125g) or Breakfast cereal (37g) (average of bran flakes/puffed wheat/wheat bisks) Semi-skimmed milk (100ml) Orange juice (150ml) Wholemeal toast (63g) with polyunsaturated margarine (7g) and marmalade/jam/honey (8g) Apple/banana/Satsuma/pear or other fresh fruit snack (80g) Water (200ml) or milk (200ml) Choice of sandwiches (75-110g) made with brown or white bread or wraps filled with cheese/tuna fish/corned beef/ham/egg mayonnaise/chicken tikka/sweetcorn/tomato/cress or Dried fruit snack (40g) Vegetable lasagne (v) (200g) Peas (80g) Lentil roast (v) (150g) New potatoes (160g) Green beans (80g) Banana custard (100g) Fresh fruit salad and ice cream (150g) or or Ice cream and topping sauce (60g) Lemon meringue pie (100g) Midafternoon / after school Tea Water or 100% fruit juice Banana bread (50g) Water or milk (200ml) Jacket potato (180g) with savoury mince filling (150g) Green beans (80g) Date bars (75g) Water or milk (200ml) or Lentil and mushroom crumble (240g) Tomato salad (80g) Crusty brown roll (48g) or Vegetarian burgers (v) (50g) Pasta Roma (160g) Carrot cake (80g) or Rhubarb fool (200g) or Fruit yoghurt with crunchy topping (130g) Summer pudding (150g) Chicken and vegetable stir-fry (230g) Egg noodles (200g) Swiss roll (25g) Water or milk (200ml) Lamb and potato hotpot (250g) Peas (80g) or Broccoli quiche (v) (120g) Crunchy coleslaw (80g) Rice salad (150g) Flapjack (50g) Water or milk (200ml) Banana and raisin bake (50g) Water or milk (200ml) Oat bars (40g) Water or milk (200ml) Chocolate yoghurt cake (60g) Water or milk (200ml) Sardine pasta (200g) Crunchy salad (90g) Baked cod (90g) Oven chips (100110g) Baked beans (90g) Chicken risotto (225g) Sweetcorn (80g) Cherry tomatoes (80g) Crusty bread (60/40g) Hot dogs with pork, beef or vegetarian sausages (115g) Carrot and apple salad (100g) Mixed bean salad (100g) or Chickpea rissoles (v) (100g) Spinach (80g) New potatoes (130g) or Sweetcorn and pasta bake (v) (200g) Carrots (80g) Oven chips (110g) Or Couscous with sweet and sour vegetables (v) (250g) Baked apples with yoghurt (210g) or Meringue baskets with fruit (100g) or Pineapple crunch (150g) or Fruit mousse (80g) or Apple crumble with custard (200g) or Rice and sultana pudding (150g) Mandarin oranges and ice cream (200g) Lemon sorbet (100g) Poached pear and custard (200g) Fresh fruit (80g) 1 2.8 Menu for children and young people in residential accommodation aged 11-18 years Monday Breakfast Midmorning Lunch Water or 100% fruit juice Tuesday Wednesday Thursday Friday Saturday Sunday Raw carrots/cucumber/pepper slices (40g) Pizza with choice of toppings (240g) Coleslaw (80g) Jacket potatoes (220g) Roast turkey (80g) Stuffing (30g) Roast potato (200g) Carrots (80g) Broccoli (80g) Currant bun/fruit bread/malt loaf/fortified cereal bar/crunchy muesli bar (20-75g) or Fromage frais or yoghurt (60-125g) Vegetable lasagne (v) (300g) Peas (80g) Breakfast cereal (37g) (average of bran flakes/puffed wheat/wheat bisks) Semi-skimmed milk (100ml) Orange juice (150ml) Wholemeal toast (63g) with polyunsaturated margarine (7g) and marmalade/jam/honey (8g) Apple/banana/Satsuma/pear or other fresh fruit snack (100g) Water (200ml) or milk (200ml) Choice of sandwiches (75-110g) made with brown or white bread or wraps filled with cheese/tuna fish/corned beef/ham/egg mayonnaise/chicken tikka/sweetcorn/tomato/cress or Dried fruit snack (40g) Banana custard (150g) Lentil roast (v) (170g) New potatoes (200g) Green beans (80g) Fresh fruit salad and ice cream (150g) or or Ice cream and topping sauce (60g) 2 Lemon meringue pie (100g) Midafternoon / after school Tea Water or 100% fruit juice Supper Banana bread (70g) Water or milk (200ml) Jacket potato (220g) with savoury mince filling (200g) Green beans (80g) Date bars (75g) Water or milk (200ml) or Lentil and mushroom crumble (250g) Tomato salad (80g) Crusty brown roll (48g) Polyunsaturated margarine (7g) or Vegetarian burgers (v) (50g) Pasta Roma (250g) Carrot cake (80g) or Rhubarb fool (200g) or Fruit yoghurt with crunchy topping (150g) Summer pudding (150g) Chicken and vegetable stir-fry (270g) Egg noodles (200g) Swiss roll (40g) Water or milk (200ml) Lamb and potato hotpot (300g) Peas (80g) Flapjack (50g) Water or milk (200ml) Banana and raisin bake (70g) Water or milk (200ml) Oat bars (40g) Water or milk (200ml) Chocolate yoghurt cake (60g) Water or milk (200ml) Sardine pasta (300g) Crunchy salad (90g) Baked cod (90g) Oven chips (150g) Baked beans (90g) Chicken risotto (250g) Sweetcorn (80g) Cherry tomatoes (80g) Crusty bread (50g) Polyunsaturated margarine (7g) Hot dogs with pork, beef or vegetarian sausages (115g) Carrot and apple salad (100g) Mixed bean salad (100g) or Sweetcorn and pasta bake (v) (300g) Carrots (80g) Oven chips (150g) Or Couscous with sweet and sour vegetables (v) (250280g) Baked apples with yoghurt (210g) or Meringue baskets with fruit (150g) or Pineapple crunch (170g) or Fruit mousse (80g) or Apple crumble with custard (250g) or Rice and sultana pudding (220g) Mandarin oranges and ice cream (200g) Lemon sorbet (100g) Poached pear and custard (270g) Fresh fruit (80g) or Broccoli quiche (v) (120g) Crunchy coleslaw (80g) Rice salad (200g) Milky drink (made with semi-skimmed milk) (200ml) Wholemeal biscuits (26g) or fresh fruit (100g) 3 or Chickpea rissoles (v) (100g) Spinach (80g) New potatoes (130200g) 2.9 Nutritional analysis of example menu for 5-10 year olds in residential accommodation Energy Kcals MJ g Max Saturated fat g Max Total carbohydrate Non milk extrinsic sugars Fibre g Min Fat g Max g Min Protein g Min Vitamin A µg Min Vitamin C mg Min Folate µg Min Calcium mg Min Iron mg Min Zinc mg Min Sodium mg Max Salt g Nutrient based Guideline (5-10 year olds) 1780 7.5 Average nutrient values from sample menu 70 52 22 18 237 280 52 47 14 22 25 68 500 1273 30 148 150 451 550 1032 9 16 7 9 1800 1796 4.5 4.5 1780 7.5 Max 2.10 Nutritional analysis of example menu for 11-18 year olds in residential accommodation Energy Kcals MJ Nutrient based Guideline (11-18 year olds) Average nutrient values from sample menus 2301 9.7 71.4 Fat g Max 1845 – 2755 7.7 – 11.6 72 -107 Saturated fat g Max 23 -34 26 Total carbohydrate Non milk extrinsic sugars Fibre g Min 246 - 367 351 g Max 54 - 81 55 g Min 18 26 Protein g Min 41-55 87 Vitamin A µg Min 700 1444 Vitamin C mg Min 40 167 Folate µg Min 200 507 Calcium mg Min 1000 1521 Iron mg Min 15 18 Zinc mg Min 9.5 11 Sodium mg Max 2400 2247 g Max 6 5.7 Salt 1 The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced 1 3.0 Nutritional Guidelines for food served on NHS premises 40 3.1 Background There have a been a number of initiatives around hospital food in recent years across all four countries of the UK and local NHS food and beverage systems are influenced by an increasingly broad range of legislation and guidance, both national and international. In 2003 the Council of Europe produced a report Food and Nutritional Care in Hospital: How to prevent under nutrition 1 with over 100 recommendations aiming to improve food service in hospital settings. New nutritional screening guidance from NICE 2 in 2006 has also contributed to increased awareness of the need for better nutritional support of older adults in hospital and this can be added to earlier initiatives such as the Department of Health’s 2001 initiative Essence of Care. 3 In England the NHS plan (2000) had a goal of enhanced food and beverage services in hospitals and England’s Better Hospital Food Programme was launched in 2001 4 . The Department of Health core standards which are assessed by the Healthcare Commission include a commitment to ‘provide choice and a safely prepared and balanced diet’. In Scotland Food, Fluid and Nutritional Care 5 was published in 2003 by Quality Improvement Scotland as part of their commitment to improving food in hospitals and in Wales there is an integrated framework for nutrition and catering as part of client care across all NHS organisations in Wales. There are currently no formal standards for hospital food in Northern Ireland. The Better Hospital Food programme recommended a standard menu plan containing 3 meals and 2 snacks, but with 24 hour access to food for those patients who have missed a meal. The guidance in this report makes recommendations for standards for meals and snacks only but it would seem prudent that snack boxes and light meals provided to patients who have missed meals should also provide the nutrients outlined here. 1 Council of Europe 2003. Food and Nutritional Care in Hospital: How to prevent under nutrition. Council of Europe. Strasbourg. 2 See www.nice.org.uk/page.aspx?o=cg032niceguideline 3 See www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsP olicyAndGuidanceArticle/fs/en?CONTENT_ID=4005475&chk=A0A4iz 4 Better Hospital Food 2001. www.betterhospitalfood.com 5 See www.nhshealthquality.org/nhsqis/files/Food,%20Fluid%20Nutrition.pdf 1 Previous nutritional targets for hospital catering produced by The Department of Health in 1995 6 stated that meals for adults should provide between 300-500kcals and 18g protein for omnivores, 12g protein for vegetarians. Sandwich meals were expected to offer 300kcals/12g protein and breakfast, snacks and milk in drinks a further 900kcals and 30g protein a day. It is suggested that menus should provide between 1200-2500kcals a day and 60-66g of protein but a broader range of nutrients are not included in these standards. 3.2 Who are these nutritional guidelines designed for? This report provides nutrient based guidelines for those eating in NHS settings who do not have special dietary requirements. It is acknowledged that many people in NHS settings will have special dietary requirements: this may be a particular special diet caused by ill health such as a low protein diet, it may be due to the need for additional energy and nutrients following illness, accident or surgery or it may be due to an underlying condition such as coeliac disease. In addition, many older people on NHS premises are known to have specific nutritional needs since undernutrition has been frequently documented 7 and the information in this report does not apply to inpatients for whom particularly energy and nutrient rich diets are required. This guidance is designed for those who eat all their meals and snacks on NHS premises but who require a diet in line with current healthy eating guidelines. For example, this may apply to those who are receiving treatment for mental health disorders, to those who have a physical condition which does not require special dietary consideration or to those who have recently given birth and do not require a therapeutic diet. It also applies to staff who, for whatever reason, may eat all their meals and snacks on NHS premises. Those groups for whom nutrient based standards are included here are: • Children aged 1-4 years 6 Nutrition Task Force (1995), Nutritional Guidelines for Hospital Catering, Department of Health, London 7 BAPEN 1999. Hospital Food as Treatment: A report by the British Association of Parenteral and Enteral Nutrition. (Allison SP. Ed). Maidenhead. BAPEN. 2 • Children aged 5-18 years • Adults aged 19-74 years • Adults aged over 75 years 3.3 Rationale for nutrient based guidance for food served to children aged 1-4 years catered in NHS settings Children under the age of 5 years have specific nutrient needs since they are in a period of rapid growth and development. There is evidence from the National Diet and Nutrition Survey for children aged 1½ to 4½ years 8 that the diets of children under 5 in the UK are too low in some essential nutrients such as vitamin A, vitamin C, iron and zinc and too high in the types of sugars that can damage teeth and salt. In addition some children have low vitamin D status. Intakes of meat, fish, fruits and vegetables are generally low. The food and nutrient intake of children under 5 has been recently reviewed by The Caroline Walker Trust. 9 This report provides guidance on the general principles of eating well for this population group. The average daily nutrient requirements for menu planners for a group of children of mixed gender aged 1-4 years (i.e. from 12 months of age up to their fifth birthday) has been derived for this report and this is outlined in Appendix 1. These values are also shown in table 3.1. In order that children under 5 receive sufficient nutrients for their needs, particularly when their appetites are small, they will require both nutritious meals and snacks. The example menu outlines the sorts of meals and snacks that could be served over a period of one week to ensure that these average values are met. It is also important that children under 5 are offered at least 5 different types of fruit and vegetables every day. Food based guidance for caterers providing food for those aged under 5 years are outlined in sections 3.4 and 3.5. 8 Gregory JR, Collins DL, Davies PSW, Hughes JM, Clarke PC. 1995. National Diet and Nutrition Survey: Children aged 1½ to 4½ years. Volume 1: Report of the Diet and Nutrition Survey. London. HMSO 9 Crawley 2006. Eating well for under 5s in child care. The Caroline Walker Trust. www.cwt.org.uk 3 Table 3.1 Nutrient based guidelines for food served to children aged 1-4 years on NHS premises Energy Dietary reference value (DRV) Children 1-4 years EAR 1290 5.4 kcals MJ Fat g No more than 35% of energy MAX 501 Saturated fat g No more than 11% of energy MAX * Total carbohydrate g MIN 1721 Non-milk extrinsic sugars Fibre g g DRV MIN Protein g RNI MIN Vitamin A µg RNI MIN µg RNI MIN Vitamin C mg RNI MIN Folate μg RNI MIN Calcium mg RNI MIN Iron mg RNI MIN Zinc mg RNI MIN Sodium mg Vitamin D2 Salt g At least 50% of energy No more than 11% of energy SACN recommendation SACN recommendation EAR = Estimated Average Requirement RNI = Reference Nutrient Intake For explanation of terms see glossary MAX MAX MAX 38 * 16 425 7 30 85 375 7 5.5 900 2.3 DRV = Dietary Reference Value SACN = Scientific Advisory Committee on Nutrition * There is currently no dietary reference value for fibre for children under the age of 5 years 1 For children aged 1-4 years the amounts of fat and carbohydrate should be about the figures shown but some flexibility is essential to ensure that young children have diets which are nutrient dense 2 It is difficult to obtain the vitamin D required from the diet. Children will make vitamin D from exposure of their skin to the sunlight in summer, but in the UK it is recommended that all children aged 1-4 years receive vitamin drops containing vitamins A, C and D daily. For older children who rarely go outside it is particularly important that they receive vitamin D supplements. 4 3.4 Food based guidance for menu planners The following pages contain some information for caterers about food groups and how to choose foods which will contribute to a healthy balanced diet. It is also useful for caterers to look at food labels on foods and ingredients they buy or use and to choose those that are lower in salt, sugar and fat. The Food Standard’s Agency provides information on what is ‘a lot’ of salt, sugar and fat in foods and these are outlined below. Foods high in salt have 1.25 grams or more salt per 100grams or 500 milligrams of sodium per 100 grams of food Foods high in sugar have 10 grams or more of sugars per 100 grams of food Foods high in fat have 20 grams or more of fat per 100 grams of food Foods high in saturated fat have 5 grams of saturated fat or more per 100 grams of food For more information about nutritional information on food labels see www.eatwell.gov.uk Additional information about foods which are good sources of some of the nutrients which appear to be insufficient in the diets of some people in the UK can be found in Appendix 2. Liver Liver, including liver pâté is very rich in vitamin A and it is recommended that these foods are given to children no more than once a week. For more information see SACN (2005) Review of Dietary Advice on Vitamin A. London: TSO 5 3.5 Food based guidelines for catering for children aged 1-4 years Food group Guidance Rationale What’s included Bread, other cereals and potatoes Foods from this group should be offered at every meal, and can be useful foods to offer as part of snacks. Starchy foods provide energy, protein, fibre and vitamins and minerals such as the B vitamins, and some calcium, iron and zinc All types of bread – wholemeal, granary, brown, wheatgerm, white, multigrain, soda bread, potato bread, chapattis, naan bread, roti, rolls, bagels, pitta bread, wraps, tortilla These foods should make up about a third of the food served each day. Starchy foods are filling And provide bulk to the diet Potatoes or sweet potatoes – boiled, mashed, baked or wedges. Potato chips should only be served once a week. Starchy foods are a good choice for snacks as they Yam, plaintain, cocoyam, cassava and other starchy root vegetables Pasta and noodles – wholemeal and white Rice – brown and white rice Other grains such as couscous or bulgur wheat, maize (polenta) and cornmeal Breakfast cereals Tips • • • • • • • Children aged 1-4 may have small appetites and very bulky foods may prevent them getting all the nutrients they need. High fibre foods should be served in moderation. Look for lower-salt breads. Processed potato products like waffles or smiley faces should be avoided. Avoid dried or canned ready-prepared pasta in sauce as these are very salty. Avoid fried rice or flavoured dried rice in packets. Avoid sugary breakfast cereals. (If a food contains more than 10g of sugar per 100g, it is considered a high-sugar food.) Choose low-sugar, low-salt cereals such as porridge, puffed wheat, weet bisks, crisped rice or flaked wheat. Fortified cereals can be a good source of iron. 6 Food group Guidance Rationale What’s included Fruit and vegetables Offer different fruits and vegetables at meals and snacks. Fruits and vegetables offer a range of important nutrients including fibre, vitamins A and C and folic acid Aim for each day’s menu for childcare settings to offer: 1-2 types of fruit and 2-3 types of vegetables. Evidence suggests that people who eat more fruits and vegetables are protected from a number of diseases in later life All types of fresh, frozen and canned vegetables – for example, broccoli, Brussels sprouts, cabbage, carrots, cauliflower, mushrooms, parsnips, peas, peppers, spinach, swede, sweet potato, turnip Children in fullday care should have the opportunity to try 4-5 different fruits and vegetables each day. Encouraging children to try fruits and vegetables when they are young will help to encourage a lifetime enjoyment of these foods Fruits and vegetables also provide colour and texture to the diet All types of salad vegetables – for example, lettuce, watercress, cucumber, tomato, raw carrot, raw pepper, radish or beetroot All types of fresh fruit – such as apples, bananas, pears, grapes, kiwi fruit, oranges, plums, berries, melon or mango All types of canned fruit in juice – for example, peaches, pears, pineapple, mandarin oranges, prunes, guava or lychees Stewed fruit such as stewed apple, stewed dried fruit, stewed plums, stewed currants or stewed rhubarb Dried fruit such as raisins, dried apricots, dates, dried figs, prunes Tips • • • • • • • • • Avoid vegetables canned with added salt and sugar Choose fruit canned in fruit juice rather in syrup Do not overcook fresh vegetables, or cut them up a long time before cooking and leave them in water, or cook them early and re-heat before serving – these practices all reduce the vitamin content. Sugar can be added to sweeten very sour fruit. Avoid dried fruit with added sugar and vegetable oil. Serve dried fruit with meals and not as snacks as the sugars in dried fruit can damage teeth Add vegetables to dishes such as stews, soups and casseroles Use fruit in desserts and when making cakes and biscuits Add dried fruit to milk puddings and yoghurts 7 Food group Guidance Rationale What’s included Meat, fish and meat alternatives Main meals should always contain an item from this group. Foods in this group are a good source of protein and are often high in iron and zinc. Meat. All types including beef, lamb, pork, chicken, turkey and offal such as liver1 and kidney. Offer a variety of meat, fish and alternatives each week Lean meat will have greater proportions of nutrients than meat products Meat products such as ham, bacon, corned beef, sausages, meat pies, coated meat products Include fish in the menu at least once a week Fish is a good source of protein and is low in fat. Oil rich fish are a good source of n-3 (omega 3) polyunsaturated fats which are thought to be beneficial for heart health Fish includes: • white fish such as cod, haddock, coley and white fish varieties from sustainable fish stocks such as pollack, saithe and blue whiting • oil-rich fish such as herring and mackerel, salmon, trout, sardines, sprats or pilchards. Canned tuna does not count as an oil-rich fish but is a good source of nutrients. Oil rich fish should be served regularly Make sure meat alternatives are varied for vegetarians Eggs including boiled, scrambled or poached, or in an omelette Pulses including all sorts of beans and peas such as butter beans, kidney beans, chick peas, lentils, processed peas or baked beans Meat alternatives – such as soya mince, textured vegetable protein, quorn or tofu Tips • Reduce intakes of meat products which are high in fat and salt such as crumb-coated chicken products, burgers, pies and canned meats. Some meat products such as sausages are popular with under-5s. Choose good quality versions if you serve these foods, and serve them no more than once a week. • Reduce intakes of processed fish products such as fish fingers or fish cakes • Make sure all fish dishes are free of bones. • All eggs should be well cooked. • Look for canned pulses with no added salt and sugar. • Dahl and other dishes made from pulses should be made without adding a lot of oil and salt. • Choose lower-salt and lower-sugar baked beans. • Reduce intakes of processed products made from meat alternatives (e.g. vegetarian sausages, burgers and pies) as these can be high in fat or salt 1 Liver and liver pâté are very high in vitamin A and children should consume these foods no more than once per week. 8 Food Group Guidance Rationale What’s included Milk and milk priducts Foods from this group should be offered at 2-3 meals and snacks each day. Milk and dairy products are excellent sources of calcium which is needed for optimal bone strength protein, vitamin A, riboflavin and vitamin D. Milk – Whole milk should be served for under-2s. Over-2s can have semi-skimmed milk if they are good eaters. Cheese e.g. Cheddar, cottage cheese, cheese spreads, feta, Edam, parmesan, pasteurised soft cheeses Yoghurt and fromage frais Tips • • • • • • • • • Offer plain milk drinks between meals Avoid unpasteurised milk and milk drinks with added sugar. Avoid unpasteurised cheese and mould-ripened (blue-vein) cheeses. Vegetarian cheese should be used where appropriate. Avoid yoghurts and fromage frais that have a high sugar content. It is preferable to add fresh fruit to natural yoghurt or natural fromage frais. Frozen yoghurts can be offered as an alternative to ice cream. Milk can be used in sweet and savoury sauces, custards and milk puddings. It is worth highlighting that some dairy products can contain high salt levels. Strong cheese can impart flavour in smaller amounts and cheese dishes may not need the addition of extra salt For dairy-free diets: serve soya drinks fortified with calcium as an alternative. 9 Food group Guidance Rationale What’s included Foods containing fat and foods and drinks containing sugar These foods add palatability to the diet and can increase the energy density of the diet for those with a small appetite The main nutrients provided by such foods are fat, including some essential fatty acids, and also some fatsoluble vitamins. These foods can be high in calories and offer few other nutrients. If appetites are poor it is important that these foods do not displace more nutrientrich foods. Carbohydrate (in the form of sugars) is also provided. Foods containing fat include butter, margarine, other spreading fats and low-fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, and gravies. Sweet foods eaten between meals can damage teeth. Keep sugary foods and drink to mealtimes only Some foods in this groups can also be high in salt. Foods containing sugar include soft drinks, sweets, jams and sugar, as well as foods such as cakes, puddings, biscuits, pastries and ice cream. Tips • • • • • Use mono- and polyunsaturated fat (such as sunflower, soya, olive, safflower, rapeseed, corn oil) based spreading fats and in salad dressings For cooking use fats high in monounsaturates such as soya, rapeseed and olive oils When making cakes and puddings include dried fruit or fresh fruit, Avoid sugary drinks between meals and always serve any drink other than milk or water in a cup Dilute 100% fruit juice with water for 1-4 year olds To increase the amount of dietary VITAMIN D in menus served in child care • • • • • Use margarine fortified with vitamin D for baking and as a fat spread. Include an oil rich fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 5-14µg of vitamin D per 100g. Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. Meat and poultry contribute small but significant amounts of vitamin D. 10 3.6 Example menu for children aged 1-4 years catered for on NHS premises The menu shown in 3.7 is an example of the types of foods, and the amounts that would meet nutrient based guidance for those aged 1-4 years who eat all their meals and snacks on NHS premises over one week. The menu offers some main meal and dessert choices, but this is an example, and many caterers would offer more choices as well as special dietary options not covered in this report. 11 3.7 Example menu for children aged 1-4 years catered for on NHS premises Monday Tuesday Wednesday Thursday Friday Saturday Sunday BREAKFAST Weet bisks or puffed wheat (24g) with 100ml whole milk Diluted 100% fruit juice (50ml) Soft brown or white toast (20g) with polyunsaturated margarine (5g) and jam, honey or marmalade (5g) MID MORNING SNACK Choice of fresh fruit slices : (40g): pear, banana, pineapple, grapes Choice of vegetable slices: (40g): Cucumber, cherry tomatoes, celery sticks Choice of dips: Whole milk yoghurt (60g), natural yoghurt (60g), fromage frais (60g) or tabbouleh (65g), mint and cucumber (35g), houmous (30g) LUNCH Main choice 1 Chicken korma (120g) brown rice (80g) naan bread (20g) Lamb burgers (45g) bubble and squeak (100g) Sardines (40g) on toast (27g) sliced tomato (40g) Vegetable and lentil lasagne (150g) mixed salad (35g) Cottage pie (150g) peas (40g) broccoli (40g) Lamb pilaf (130g) Mixed bean salad (40g) Main choice 2 (v) Vegetarian bolognese (100g) with wholemeal spaghetti (90g) Stuffed peppers (100g) potato salad (40g) Broccoli quiche (100g) mashed potato (80g) baked beans (55g) Chickpea burgers (90g) Mixed bean casserole (160g) Jacket potato (115g) sweet potato (80g) sweetcorn (40g) green beans (40g) mashed potato (75g) baked beans (55g) mixed salad (35g) Main choice 3 Coconut fish curry (100g) basmati rice (80g) beansprouts (40g) and cherry tomato (40g) salad Chicken fajitas (120g) sweetcorn salsa (35g) mixed salad (35g) Kedgeree (150g) Peas (40g) carrots (40g) Channa aloo (80g) masoor dahl (60g) mixed vegetable pilau (80g) Dessert choice 1 Tropical fruit salad (80g) Apricot conde (110g) Milk jelly (90g) with mandarins (70g) Dessert choice 2 Chocolate semolina (110g) Trifle (110g) Melon and grape salad (85g) with Stewed apples (75g) with custard (60g) Banana yogurt flan (90g) Dessert Fruit Lemon Cinnamon fruit Neapolitan 12 petits pois (40g) swede (40g) Chilli con carne (100g) Roast chicken and gravy (110g) roast potatoes (80g) mixed vegetables (40g) Lentil pasta (180g) grated cheese (10g) Caribbean chicken (100g) sweet potato (80g) rice and peas (50g) Sweet and sour pork (120g) egg noodles (70g) stir-fried vegetables (70g) Crème caramel (100g) Apple pie (70g) custard (60g) Banana custard (100g) Fresh fruit salad (85g) Rhubarb fool (90g) Lemon meringue pie (60g) Pineapple Fruit jelly Milk jelly jacket potato (90g) tomato salad (40g) choice 3 compote (50g) Whole milk yoghurt (50g) sorbet (40g) with wafers (2g) fool (90g) ice cream (50g) crush (85g) (90g) (90g) pears (60g) 100% orange juice (50ml) diluted with water MID-AFTERNOON SNACK Choice of fruit and vegetable slices : kiwi, peaches, clementine, apple, grapes, pepper, carrot, celery, cucumber (40g) Natural yoghurt (60g), fromage frais (60g), whole milk yoghurt (60g) Wholemeal pancake with butter (40g), rice cakes (20g), plain popcorn (20g), crackers with soft cheese (19g) 100% orange juice (50ml) diluted with water TEA Main choice 1 Main choice 2 (v) Main choice 3 Egg and cress sandwiches (90g) lettuce (20g) cherry tomatoes (40g) Vegetable couscous (100g) mixed salad(30g) with butter beans (20g) homemade coleslaw (35g) Spicy ratatouille (130g) with tofu (30g) flat bread (30g) Tuna (30g) and sweetcorn (30g) pasta (80g) cucumber (20g) red pepper (20g) Egg sandwiches (90g) green salad (40g) Spanish omelette (70g) baby jacket potatoes (90g) Cherry tomatoes (40g) Baked beans (60g) with white toast squares (30g) Chicken and vegetable couscous (145g) salad (35g) Curried bean and rice salad (100g) yellow and orange peppers (40g) Sardines (50g) white toast (20g) tomato (40g) Wholemeal pasta twirls (80g) Chickpea salad (50g) cucumber (20g) and carrot (20g) sticks Baby jacket potatoes (90g) with ratatouille sauce (130g) Quorn burger (45g) and bun (50g) Cheese and Onion sandwich (60g) salad (35g) Vegetable rice (110g) kidney beans (40g) Egg tortilla (70g) potato dice (60g) Vegetable sticks (40g) Fruity couscous (80g) Chicken tikka wrap (75g) mixed Salad (40g) Chapati (45g) Tuna and sweetcorn pasta (160g) Houmous (35g) and roasted red onion (35g) wrap (40g) Fromage frais (60g) satsuma (40g) Cool rice sundae (100g) mixed salad (35g) and kidney beans (40g) chickpea salad (55g) cucumber (20g) and carrot (20g) Fresh fruit jelly (60g) Dessert choice 1 Banana custard (100g) Canned peaches (in juice) (100g) Semolina (90g) with pears (40g) Yoghurt with raisins (145g) Dessert choice 2 Fruit mousse (80g) Greek yoghurt (30g) with orange (40g) Fruit flan (100g) Tropical granola (75g) Oaty fruit crumble (75g) with custard (60g) Orange and lemon rice (100g) Fruit trifle (120g) Clementine (40g) with natural yoghurt (60g) Dessert choice 3 Watermelon (40g) Fruit smoothies (100g) chewy cereal bar (20g) Rice pudding with mandarins (100g) Peach melba (100g) Fromage frais (60g) with dates (40g) Apple crumble (80g) Lemon jelly fluff (90g) EVENING Whole milk (200ml) 13 3.8 Analysis of NHS menu for children aged 1-4 years Nutrient based Guideline Average analysis about 1290 5.4 50 1290 5.4 44 g about 172 177 Non milk extrinsic sugars g MAX 38 29 Protein g Min 16 50 Vitamin A µg Min 425 928 Vitamin C mg Min 30 128 Folate µg Min 85 210 Calcium mg Min 375 928 Iron mg Min 7 8 Zinc mg Min 5.5 6 Sodium mg Max 900 925 g Max 2.3 2.3 Energy Kcals MJ g Total carbohydrate Fat Salt1 1 The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced 14 3.9 Rationale for nutrient based standards for food served to those over 5 years of age on NHS premises 3.9.1 Children and young people 5-18 years The rationale for the setting of the guidance for children and young people in NHS settings for all their meals, snacks and drinks is based on evidence that the diets of many school aged children contain insufficient amounts of some important micronutrients, as well as some foods such as fruit and vegetables and oil rich fish. Data from the National Diet and Nutrition Survey of young people aged 4-18 years published in 2000 10 showed that many children and young people do not get enough of certain important nutrients – for example iron, calcium, zinc, vitamin A, vitamin C and folate. For this reason it is important that the food served throughout the day provides enough of these essential nutrients to protect children and young people from insufficiencies. Since many of the important nutrients which may be insufficient in the diets of children and young people are more likely to be found at meals than in snacks, it is likely that meals will provide a greater proportion of these nutrients. It is also recommended that in a group of children or young people, the nutrient based guidance should meet the requirements of those children with the greatest needs. So, among mixed gender groups of children, the guidance for iron will meet the needs of the girls in the group who have higher requirements, and the standards for calcium, zinc and vitamin A will meet the greater needs of the boys in the group. Guidance given here assumes that groups will be of mixed gender. The derived dietary reference values calculated for the age groups 5-10 year and 1118 years are explained in Appendix 1 and are also shown in table 3.2. Using these derived reference values it is assumed that menus offered to children and young people on NHS premises will provide all of the nutrients needed in the meals, snacks and drinks served. The values for 11-18 year olds for energy, fat, carbohydrate and protein are given as ranges. This reflects the fact that young people will be growing at very different rates and that some will have much greater needs for energy and nutrients since they may be growing rapidly, be physically bigger, be more active or 10 Gregory J, Lowe S, Bates CJ, Prentice A et al 2000. National Diet and Nutrition Survey: Young People aged 4-18 years. London. The Stationery Office. 15 all three. If the menus offered provide nutrients in the right balance then hungrier young people will eat bigger portions to satisfy their appetites. 16 Table 3.2 Nutrient based guidelines for food served to children aged 5-18 years on NHS premises Energy kcals MJ Dietary reference value (DRV) Children 5-10 years Young people 11-18 years EAR 1780 7.5 1845 – 2755 7.7 – 11.6 Fat g No more than 35% of energy MAX 70 72 -107 Saturated fat g No more than 11% of energy MAX 22 23 -34 Total carbohydrate Non-milk extrinsic sugars Fibre g 237 246 - 367 g DRV MIN 52 14 54 - 81 18 Protein g RNI MIN 25 41-55 Vitamin A µg RNI MIN 500 700 µg RNI MIN - - Vitamin C mg RNI MIN 30 40 Folate μg RNI MIN 150 200 Calcium mg RNI MIN 550 1000 Iron mg RNI MIN 9 15 Zinc mg RNI MIN 7 9.5 Sodium mg 1800 2400 4.5 6 Vitamin D2 Salt g g At least 50% of energy No more than 11% of energy MIN MAX SACN recommendation SACN recommendation EAR = Estimated Average Requirement RNI = Reference Nutrient Intake For explanation of terms see glossary MAX MAX DRV = Dietary Reference Value SACN = Scientific Advisory Committee on Nutrition 1 For children aged 1-4 years the amounts of fat and carbohydrate should be about the figures shown but some flexibility is essential to ensure that young children have diets which are nutrient dense 2 It is very difficult to obtain enough vitamin D from the diet alone. Children will make vitamin D from exposure of their skin to the sunlight in summer. Older children who rarely go outside or who wear very restrictive clothing are likely to require vitamin D supplements. 17 3.9.2 Rationale for nutrient based guidance for food served to adults aged 19-74 years on NHS premises The National Diet and Nutrition Survey 11 (NDNS) of adults aged 19-64, carried out in 2002, has raised several key concerns with regards to nutrient intake and the nutritional status of this population group. Energy (calories) and fat intake Adults’ total carbohydrate intake is close to the dietary reference value (DRV) 12 of 50% of food energy for both men and women and since the last adult survey carried out in 1986/87 13 total fat intake has decreased. However, the proportion of energy derived from saturated fat still exceeds the dietary reference value of 11% of food energy. Also, in the 2002 survey the percentage of food energy derived from nonmilk extrinsic sugars was 13.6% for men and 11.9% for women – exceeding the DRV of 11% of food energy. Intakes were higher in the younger age groups (19-24 years). Non-starch polysaccharides (NSP, or fibre) In the survey of 19-64 year olds, the mean daily intake of non-starch polysaccharides (NSP) was below the recommended average intake of 18g per day for all sex and age groups, and a third of adults had intakes of less than 12g a day. Intakes were particularly low among those in the younger age group (19-24 years) where average intakes were 12.3g for men and 10.6 for women. Vitamins In the 2002 survey, adults’ average intakes of all vitamins were close to the Reference Nutrient Intake (RNI) for all sex and age groups, except for vitamin A in the youngest groups, where results were below the RNI. Assessments of nutritional status indicated issues regarding low vitamin D status as well as inadequate vitamin C and folate concentrations among some individuals. Adults who rarely go outside, or who wear very restrictive clothing will not get sufficient Vitamin D from their diet alone and are likely to need vitamin D supplements. 11 Henderson L et al 2002 and 2003. The National Diet and Nutrition Survey: Adults Aged 19-64 Years, Volumes 1-4. TSO. London 12 Department of Health 1991. Dietary Reference Values for Food Energy and Nutrients for the United Kingdom. Report on Health and Social Subjects No. 43. HMSO. London 13 Gregory J et al 1990. The National Dietary and Nutritional Survey of British Adults. HMSO. London. 18 Minerals Iron intakes in women were well below the RNI in all but the oldest age group. Over 40% of those women in the two youngest age groups had iron intakes below the LRNI (Lower Reference Nutrient Intake). Assessments of nutritional status indicated issues regarding low iron status, with 8% of women and 3% of men having signs of anaemia and 11% of women and 4% men having low serum ferritin levels (another measure of low iron status). The average intakes of some other minerals were below the RNI for a number of sex and age groups. Results indicated low intakes of potassium and magnesium, which were well below the RNI for the youngest male group and below the RNI for all female age groups. Issues regarding low intakes of iodine and zinc were also apparent in the younger female groups, and concerns with intakes of calcium and copper were also highlighted. Sodium/salt In the 2002 survey, the average salt intake for adults was estimated at 9.5g per day overall (based on mean urinary sodium excretion levels per 24 hours of 187.4mmol per day for men and 138.5mmol per day for women.) This result represents a slight increase from the 1986/87 adult survey and average intakes in all sex and age groups were well above the recommended maximum daily intake of 6g per day 14 . Fruit and vegetables The National Diet and Nutrition Survey reported that few adults achieved the 5 portions of fruit and vegetables recommended each day – with men and women having on average less than 3 portions a day. Overweight and obesity Data on overweight and obesity levels among adults in the UK from the 2004 Health Survey for England 15 and The Scottish Health Survey 2003 16 suggest that a significant proportion of adult men and women are now obese (with a body mass index of more than 30kg/m2). Nearly a quarter (23.6%) of men and 16% of women in England and 22.4% men and 26% of women in Scotland are reported to be obese 14 Scientific Advisory Committee on Nutrition 2003. Salt and Health. TSO. London Data from Healthy Survey for England 2004 accessed from: http://www.ic.nhs.uk/pubs/hlthsvyeng2004upd 16 Scottish Executive 2005. The Scottish Health Survey. Scottish Executive. Edinburgh. 15 19 and approximately two-thirds of all adults are overweight (with a body mass index greater than 25 kg/m2). Similar levels of overweight and obesity are found in Wales 17 and Northern Ireland 18 . Given the rising levels of obesity in the UK, it is important not to exceed average energy (calorie) requirements. It is therefore suggested that main meals should provide nutrient-dense food – that is, food which contains high levels of nutrients – but that these foods should not be correspondingly higher in calories. Those individuals who are in the normal range for bodyweight (BMI 20-25 kg/m2) but who have higher energy needs because they use up more calories (because they either have a larger body size, or do more activity, or both) should have the opportunity to eat more carbohydrate-based foods at meals to meet their higher energy requirements without disproportionately increasing their intake of fat, saturated fat, sugar or salt. Based on the most recent assessments of nutritional status for the UK population, it appears that it may also be prudent to ensure that food served in public institutions at breakfast and at main meals provides enhanced amounts of fibre, iron, folate, vitamin C and zinc. In order to ensure that population maximum intakes of fat, saturated fat, sugars and salt are within current recommendations, it is important that these nutrients are not exceeded in the guidance suggested. Another priority is to ensure that meals offer the opportunity to increase fruit and vegetable intakes. Table 3.3 outlines the nutrient based guidance for adults aged 19-74 years and the derivation of this is explained in Appendix 1. 17 Welsh Health Survey October 2003 - March 2004. Accessed from: wales.gov.uk/keypubstatisticsforwales/content/publication/health/2004/sdr82-2004/sdr82-2004.pdf 18 Northern Ireland Health and Social Wellbeing Survey 2001. Accessed from: www.csu.nisra.gov.uk/archive/Surveys/HWB/publications/1997/Health%20&%20lifestyle%20report% 201997.pdf 20 Table 3.3 Nutrient based guidelines for food served to adults aged 19-74 years on NHS premises Energy Dietary reference value (DRV) Adults 19-74 years EAR 2225 9.4 kcals MJ Fat g No more than 35% of energy MAX 87 Saturated fat g No more than 11% of energy MAX 27 Total carbohydrate g At least 50% of energy MIN 297 Non-milk extrinsic sugars g No more than 11% of energy MAX 65 Fibre g DRV MIN Protein g RNI MIN Vitamin A µg RNI MIN Vitamin D µg RNI MIN Vitamin C mg RNI MIN Folate μg RNI MIN Calcium mg RNI MIN Iron mg RNI MIN Zinc mg RNI MIN Sodium mg Salt g SACN recommendation SACN recommendation EAR = Estimated Average Requirement RNI = Reference Nutrient Intake For explanation of terms see glossary MAX MAX 18 50 700 -* 40 200 700 15 9.5 2400 6 DRV = Dietary Reference Value * Vitamin D It is difficult for adults to get all the vitamin D they require through the diet and most adults will also make Vitamin D on exposure of the skin to sunlight during the summer months. Adults who rarely go outside or who go outside infrequently and who wear clothing which means their skin is not exposed to the sun are likely to require vitamin D supplements. 21 3.9.3 Rationale for nutrient based guidance for food served to adults aged over 75 years on NHS premises The food provided for older people on NHS premises should as a minimum provide the average dietary reference values for energy and nutrients specified for people aged 75 years and over 19 . It should be stressed however that many older people may have higher requirements for energy and nutrients as well as specific requirements for help with eating and drinking. The nutrient-based guidelines in this report provide guidance for menu planners on the amounts of energy and nutrients that they should aim to provide for a group of older people in their care, while remembering that this is a vulnerable population group who are frequently found to eat and drink too little. The needs of each older person should be assessed as part of his or her care plan and meals and snacks organised to ensure that each individual is able to access sufficient nutrients each day. Monitoring nutritional status (e.g. whether a person loses weight) is an important part of the care of older people and this will indicate when specialist help may be needed to help someone eat and drink appropriately. Registered Dietitians are able to provide advice on how nutritional status should be measured in NHS settings. The foods and drinks offered each day should meet the total nutritional guidance outlined. The sample menus in section 6.0 show the sorts of foods and drinks that would be required across the day to do this. Where there are eating difficulties or the texture of food needs to be altered, it is important that appropriate advice is taken from a Registered Dietitian or a Speech and Language Therapist to ensure that residents receive adequate nutrition at both meals and snacks. Vitamin D It is impossible for most older adults to obtain the full daily requirement of 10 micrograms of vitamin D from the diet alone. It is likely that older adults in NHS accommodation who rarely go outside will need vitamin D supplements.4 They should seek medical advice about this. Good dietary sources of vitamin D are outlined in the food-based guidelines for older people in section 3.10. 19 Department of Health 1991. Dietary Reference Values for Food Energy and Nutrients for the United Kingdom. Report on Health and Social Subjects 41. HMSO. London 22 Folate and vitamin C The low intakes of folate and vitamin C among older people 20 may be due in part to reduced intakes of fruit and vegetables, since some older people may find it difficult to peel, cut up or chew these foods. Caterers should be aware of the importance of increasing fruits and vegetables in menus for older people and offer a variety of raw and cooked fruits and vegetables in accessible forms. Iron and zinc Low iron intakes and low iron status have been reported among older people 21 and this may be due both to poorer iron absorption, greater iron losses and lower iron intakes 22 . Meat is a good source of iron but as people get older they may find it more difficult to chew and therefore it is important that foods high in iron are included in the menu in forms that are easy for older people to access. Zinc intakes are also often low in the diets of older people and many good sources of iron are also good sources of zinc. Salt/sodium The current recommendation for salt intakes for all adults is 6g a day3 and the current daily intake by adults is approximately 9g. Older people may be used to adding salt to food out of habit, or they may have a reduced sense of taste and smell and therefore add salt to food to give it taste, or they may prefer highly salted foods and condiments that they typically ate when younger. NHS caterers should respect the food choices of those they cater for but attempt to reduce the use of highly salted foods and salt in cooking, while ensuring that food remains tasty. Advice on reducing salt in cooking can be found on the website www.salt.gov.uk Fluid Intakes A regular and adequate intake of fluids is extremely important for older people. It helps to prevent dehydration which can lead to confused states; helps to prevent and alleviate the symptoms of constipation and fluids can also provide important nutrients when appetites are small. It is recommended that older people drink at least 1.5 litres or 8 cups of non-alcoholic fluid a day11. Many older people may find they are less 20 Finch S, Doyle W, Lowe C, Bates CJ et al. 1998. National Diet and Nutrition Survey: People Aged 65 Years and Over. Volume 1: Report of the Diet and Nutrition Survey. TSO. London. 21 Finch S, Doyle W, Lowe C, Bates CJ et al. 1998. National Diet and Nutrition Survey: People Aged 65 Years and Over. Volume 1: Report of the Diet and Nutrition Survey. TSO. London. 22 Caroline Walker Trust 2003. Eating Well for Older People. CWT. www.cwt.org.uk 23 likely to recognise that they are thirsty or may be afraid of drinking because of fears of incontinence. It is important to explain to older people the importance of drinking and that more fluid, rather than less, can help with incontinence. The fluid older people require can be consumed in a number of ways, and some fluids may offer additional nutritional or psychological benefits to older people. Tea and coffee are sociable drinks which many older people habitually drink and enjoy. These should be offered regularly, and served in the style that the older person prefers. Some older people may enjoy milky coffee or tea or another hot beverage such as a malted or chocolate milk drink particularly at bedtime. Fruit juice should be offered at meals as the vitamin C it contains may help the absorption of iron from some foods. Fresh, chilled water should be freely available and offered regularly as an additional option. Some foods can also provide fluid: older people may enjoy frozen drinks if the weather is warm and nutritious soup can be offered. It is important that all those who care for older people work with the older person to ensure that they have access to 1.5 litres or 8 cups of fluid during the day, of the type that the older person enjoys. As older people may not recognise that they are thirsty it is important that drinks are offered, served and encouraged: provision of fluid alone e.g. water coolers in community areas or jugs of water by the side of the bed will not necessarily ensure adequate fluid intake. Table 3.3 outlines the nutrient based guidance for people over the age of 75 years and the derivation of this is explained in Appendix 1. Specific food based guidance for those aged over 75 years is shown in section 3.12 24 Table 3.3 Nutrient based guidelines for food served to adults aged over 75 years on NHS premises Energy Dietary reference value (DRV) Adults 75 years + EAR 1955 8.2 kcals MJ Fat g No more than 35% of energy MAX 76 Saturated fat g No more than 11% of energy MAX 24 Total carbohydrate g At least 50% of energy MIN 260 Non-milk extrinsic sugars g No more than 11% of energy MAX 57 Fibre g DRV MIN Protein g RNI MIN Vitamin A µg RNI MIN µg RNI MIN Vitamin C mg RNI MIN Folate μg RNI MIN Calcium mg RNI MIN Iron mg RNI MIN Zinc mg RNI MIN Sodium mg SACN recommendation MAX g SACN recommendation MAX Vitamin D1 Salt EAR = Estimated Average Requirement RNI = Reference Nutrient Intake For explanation of terms see glossary 18 50 700 10 40 200 700 9 9.5 2400 6 DRV = Dietary Reference Value 1 Vitamin D The RNI for Vitamin D for adults over 65 years is 10µg a day. It is very unlikely that older adults can get all the vitamin D they require through the diet and most adults will also make Vitamin D on exposure of the skin to sunlight during the summer months. Older adults who rarely go outside or who go outside infrequently and who wear clothing which means their skin is not exposed to the sun are likely to require vitamin D supplements. 25 3.10 Food based guidance for menu planners The following pages contain some information for caterers about food groups and how to choose foods which will contribute to a healthy balanced diet. It is also useful for caterers to look at food labels on foods and ingredients they buy or use and to choose those that are lower in salt, sugar and fat. The Food Standard’s Agency provides information on what is ‘a lot’ of salt, sugar and fat in foods and these are outlined below. Foods high in salt have 1.25 grams or more salt per 100grams or 500 milligrams of sodium per 100 grams of food Foods high in sugar have 10 grams or more of sugars per 100 grams of food Foods high in fat have 20 grams or more of fat per 100 grams of food Foods high in saturated fat have 5 grams of saturated fat or more per 100 grams of food For more information about nutritional information on food labels see www.eatwell.gov.uk Additional information about foods which are good sources of some of the nutrients which appear to be insufficient in the diets of some people in the UK can be found in Appendix 2. Fluid intakes It is important that everyone has access to adequate fluid intakes throughout the day. In climates such as the UK, we should drink approximately 1.2 litres (6 to 8 glasses) of fluid every day to stop us getting dehydrated. In hotter climates the body needs more than this. We get some fluid from the food we eat but it is important that fluids are not restricted since dehydration can lead to headaches, confusion and irritability and lack of concentration as well as constipation and potentially urinary tract infections. Clean, chilled water should always be available with meals and between meals. 26 3.11 Food-based guidelines for food served to all those over the age of five years on NHS premises Food Group Guidance Rationale What’s Included Bread, other cereals and potatoes Starchy foods should make up a third of the daily diet. Starchy foods are a good source of energy and the main source of a range of nutrients in the diet. As well as starch, these foods supply fibre, calcium iron and B vitamins. All varieties of bread including wholemeal, granary, seeded, chapattis, bagels, roti, tortillas, pitta bread A variety of breads should be available daily at every meal Different starchy foods should be offered in main meals throughout the week so that a variety of starchy foods are included. Aim to include pasta and rice on the menu once a week Potatoes, yam, sweet potato, plantain, cocoyam, dasheen, breadfruit, cassava Breakfast cereals Rice, couscous, bulgar wheat, maize (polenta), cornmeal Noodles, spaghetti and other pastas Wholegrain and wholemeal cereal foods are a good source of fibre and other nutrients Tips • • • • • • • • • Serve more pasta and rice and use less sauce. Opt for tomato based sauces instead of cheese-based to reduce fat content When serving rice and pasta, try to use wholemeal, wholegrain, brown or high fibre versions. Some breakfast cereals are nutrient fortified (have added iron, folic acid and other vitamins and minerals). Choose wholegrain cereals or mix some in with other cereals. Offer a variety of breads, such as seeded, wholegrain and granary and use thicker slices with low-fat options for fillings Large pieces of potato and thick or straight cut chips absorb less fat Boil potatoes in the minimum amount of water and for the shortest amount of time to retain vitamins. Use herbs or other shredded vegetables to add colour and flavour to baked potatoes, rather than butter or margarine. If you look after young people who have allergies to wheat, oats, barley and rye: good alternatives to offer are foods made from maize (e.g. polenta), rice, rice flour, potatoes, potato flour, buckwheat, sago, tapioca, soya and soya flour. Cereal foods which are good sources of iron and zinc include fortified cereals, whole grain cereals, wholemeal bread and flour, couscous and wholemeal pasta. 27 Food Group Guidance Rationale What’s Included Fruit and Vegetables Fruit and vegetables should make up about a third of the daily diet. Fruit and vegetables are good sources of many vitamins and minerals. All types of fresh, frozen and tinned vegetables i.e. broccoli, Brussels sprouts, cabbage, carrots, frozen peas, peppers, swede, sweetcorn It’s important to offer a variety. Five-a-day is an achievable target. Aim for one or two portions with each meal and offer fruit and vegetables as snacks. One portion is about 80g fresh fruit and vegetables and 40g of dried fruit Beans and pulses are included but only count as a maximum of 1 portion per day A glass of 100% fruit juice can count as one portion of fruit each day There is evidence that consuming 400g a day or more of fruit and vegetables reduces the risk of developing chronic diseases such as coronary heart disease and some cancers. Including fruits and vegetables in the diet will help to increase the intake of fibre and can help to reduce the total amount of calories consumed among those who may wish to lose weight All types of salad vegetables including lettuce, cucumber, tomato, raw carrots, peppers, beetroot All types of fresh fruit e.g apples, bananas, kiwi fruit, oranges, pears, mango, plums All types of tinned fruit in fruit juice e.g. pineapple, peaches, mandarin oranges Stewed fruit Dried Fruit Fruit juice (100% juice) Tips • • • • • • • • • • • • • • • • Avoid adding fat or rich sauces to vegetables or sugar or syrupy dressings to fruit Steaming or cooking vegetables with minimum amounts of water and serving as soon as possible will help retain vitamins. Use fresh fruit and vegetables as soon as possible, rather than storing, to avoid vitamin loss Incorporate fruit and vegetables in snack options. Offer a variety of healthy snack alternatives Add vegetable and pulses to curry, casserole or stir-fry and serve at least two types of vegetables with fish, chicken or meat. Baked beans (as a vegetable) should be served a maximum of twice a week Encourage a daily glass of fruit juice (100% juice, unsweetened) with meals Choose tinned fruit in fruit juice not in syrup Add a handful of dried fruit to cereal options and porridge Supply a good combination of traditional salads and raw vegetables, fruits and nuts to increase colour, taste and texture at meal times Add additional vegetables to savoury dishes Vegetable soups are a useful way of increasing vegetable intake Avoid dried fruit with added sugar or vegetable oil Fruit and vegetables which are useful sources of iron include spinach, broccoli, spring greens, dried apricots, raisins, baked beans, broad beans and blackcurrants Fruit and vegetables which are useful sources of folate include spinach, broccoli, peas, oranges, melon, green leafy salads and tomatoes. Fruit and vegetables which are useful non-dairy sources of calcium include green leafy vegetables, dried fruit and oranges. 28 Food Group Guidance Rationale What’s Included Milk and Dairy Products Offer dairy foods such as milk, yoghurt and cheese as part of meals and snacks Milk and dairy products are excellent sources of calcium, protein, vitamin A and vitamin D. Calcium helps to contribute to good bone health Skimmed, semi-skimmed, whole milk Offer low fat options such as semiskimmed milk, low fat yoghurt and skimmed milk cheeses The fat content of different dairy products varies and much of this is saturated fat. Dried milk, goats and sheep’s milk All types of cheeses e.g. Cheddar cheese, cottage cheese, cheese spreads, brie, feta, Edam, goats cheese, stilton, Parmesan Yoghurt Fromage frais Do not rely on cheese as the main protein item for vegetarians. Where no other option is available, cheese served as a sandwich filler should be offered no more than twice per week. Tips • • • • • • • • • • Try using very strong-tasting cheese (mature Cheddar, blue cheese) if using to flavour dishes or sauces, because less will be required. Choose reduced-fat hard cheeses, cottage cheese and skimmed milk soft cheese Offer semi-skimmed or skimmed milk and low-fat yoghurts and fromage frais. Use plain yoghurt and fromage frais instead of cream, soured cream or crème fraiche in recipes Try serving frozen yoghurts as an alternative to ice cream. It is worth highlighting that some dairy products can contain high salt levels. Look for lower salt cheeses and use smaller amounts of stronger cheese Dairy foods are very important during pregnancy, but unpasteurised dairy produce and softmould-ripened cheese (e.g. Camembert, Brie and all blue-veined cheese) should be avoided For those on dairy free diets serve soya drinks fortified with calcium as an alternative. Fresh fruit milkshakes and chilled milk drinks can be offered as snacks Restrict sweetened milk drinks to mealtimes as the sugars in these drinks can damage teeth 29 Food Group Guidance Rationale What’s Included Meat, fish and meat alternatives Offer a meat or alternative at all main meals Meat and meat alternatives are a good source of protein, vitamins and minerals such as iron and zinc Use lean meat (which has a fat content of about 10%) Some meat and meat products can have a high fat and saturated fat content Meat includes all cuts of beef, pork, lamb, poultry, offal1 and meat products such as bacon, sausages, beef burgers, pies and cold meats Fish should be offered at least twice per week. White fish is low in fat It is strongly recommended that oily fish such as salmon, trout, mackerel, herring, pilchards, sardines should be served once a week Oil-rich fish provides a good source of omega-3 fatty acids, which may help to protect against heart disease. Oil-rich fish are also a source of vitamins A and D. Eggs can be served at breakfast and as part of main meals Eggs are a good source of protein, vitamin A, vitamin D and some minerals Beans, pulses, eggs, meat alternatives and nuts all provide good sources of nutrients. Ensure meat alternatives for vegetarians are varied Fish includes fresh, frozen and tinned fish, such as tuna and sardines, Fish products such as fish cakes and fish fingers may have a low fish content Boiled, poached, scrambled eggs, omelettes Beans and pulses such as chick peas, lentils, kidney beans, butter beans, textured vegetable protein, nuts, soya products such as tofu, quorn Tips • • • • • • • • • • • Always select the leanest cuts of meat and remove visible fat and poultry skin Roast meat on a rack in order to let the fat run off. Grill, poach or bake meat rather than frying. If you do fry, use clean oil and at the correct temperature to minimise absorption. Note that larger pieces of fish and meat absorb less fat. Do not add extra fat or oil when cooking meat. Use more vegetables, pulses and starchy food to extend dishes further, as well as add more texture and flavour. Less meat is also required, reducing the fat content and the cost of the meal. Buy good quality meat and use smaller amounts. Use fish from sustainable fish stocks. Offer unsalted nuts and seeds as snacks. Reduce the amount of processed meat products served such as meat pies and pasties, coated, canned and composite meat products such as sausages, burgers, coated chicken products Reduce the amount of processed fish products on offer, particularly those that are fried or coated such as fish fingers or fish cakes. 1 Liver and liver pate is very rich in vitamin A and it is recommended that these foods are given to children no more than once a week. 30 Food Group Guidance Rationale What’s Included Foods containing fat and foods and drinks containing sugar These foods can add palatability to the diet but should be eaten in small amounts each day Foods containing fat and foods containing sugar often provide a lot of calories and a lower proportion of other nutrients. Foods containing fat include: Reduce the amount of foods containing visible fat for example, margarine and butter, cooking oils and mayonnaise. Other foods containing fat such as cakes and biscuits should be eaten occasionally Foods and drinks containing sugar often contain few other nutrients and frequent consumption between meals can contribute to tooth decay Some foods in this group are also high in sodium/salt Butter, margarine, other spreading fats and low fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, gravies. Foods and drinks containing sugar include: Soft drinks, sweets, chocolate, jams, sugar, cakes, puddings, biscuits, pastries and ice cream Tips • • • • • • • • • • • Use mono- or poly-unsaturated fat spreads. Use cooking oils high in monounsaturates such as soya, rapeseed or olive oils Avoid serving pastry dishes frequently. Measure oil for cooking carefully and reduce oil used in the preparation of soups, stews and casseroles. Vegetables can often be dry fried, steamed or stewed to form the basis of sauces and other dishes. Use low-fat yoghurt or non-dairy ice cream to complement puddings or pies. Produce puddings lower in fat and sugar and incorporate fresh, tinned fruit in juice or dried fruit. Offer water, unsweetened fruit juices and chilled milk drinks. Serve wholegrain or plain cereals rather than sugar coated cereals. Provide currant buns, fruit bread, melon slices, malt loaf and other lower fat bread based foods as alternatives to cakes and biscuits. When preparing sandwiches, try and avoid using butter or spreads if the filling is already moist. Consider using reduced-fat spreads and opt for types that are soft straight from the fridge, so it is easier to spread thinly. To increase the amount of dietary VITAMIN D in menus • • • • • Use margarine fortified with vitamin D for baking and as a fat spread. Include an oily fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 5-14µg of vitamin D per 100g. Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. Meat and poultry contribute small but significant amounts of vitamin D. 31 3.12 Food-based guidance for food served to adults aged 75 years + on NHS premises Food group Guidance Rationale What’s included Bread, other cereals and potatoes Starchy foods should make up a third of the daily diet. Foods from this group are a good source of energy and the main source of a range of nutrients in the diet. As well as starch, these foods supply fibre, calcium iron and B vitamins. All varieties of bread including wholemeal and granary bread, chappati and bagels. Older people may prefer white bread, and higher fibre white bread may also be acceptable, A variety of breads should be available daily as starters or meal accompaniments. Offer a variety of starchy foods with main meals including potatoes, rice, pasta, noodles and other grains. Potatoes, plantain, yam and sweet potato Breakfast cereals Rice, couscous, bulgar wheat, maize, cornmeal Wholegrain cereals provide fibre Noodles, pasta Tips • • • • • • Older people with small appetites need nutrient-dense meals and, if there is concern about how much someone is eating, starchy foods should be offered in moderate amounts. Avoid very high-fibre cereals unless an older person has a very good appetite. Some white bread has added nutrients and fibre and can be useful for older people who do not like brown or wholemeal bread. Some older people find it easier to chew brown or wholemeal bread if it is lightly toasted. Some breakfast cereals are nutrient-fortified (e.g. they may have added iron, folic acid, vitamin D and other nutrients). These can be good choices for breakfast but look for those with a lower salt content. Boil potatoes in the minimum amount of water and for the shortest amount of time to retain vitamins, but ensure they are cooked until soft. Roast potatoes in small amounts of vegetable oil and use milk to mash potatoes to smoothness. If you have customers who are allergic to wheat, oats, barley or rye, good alternatives are foods made from maize (i.e. polenta), rice, rice flour, potatoes, potato flour, buckwheat, sago, tapioca, soya and soya flour. Seek expert advice from a dietitian where necessary. 32 Food group Guidance Rationale What’s included Fruit and vegetables Fruit and vegetables should make up about a third of the daily diet. Fruit and vegetables are good sources of many vitamins and minerals. All types of fresh, frozen and tinned vegetables – e.g. broccoli, Brussels sprouts, cabbage, carrots, frozen peas, swede, green beans. It’s important to offer at least 5 different fruits and vegetables every day. Aim for 1 or 2 portions with each meal and offer fruit as a snack. A portion of fresh or cooked fruit or vegetables should be about 80g. 1 portion of dried fruit can be about 40g. (Dried fruit only counts once per day.) 1 glass of fruit juice = 1 portion (however much is consumed in a day) There is increasing evidence that consuming more than 400g of fruit and vegetables every day reduces the risk of developing chronic diseases such as coronary heart disease and some cancers. All types of salad vegetables including lettuce, cucumber, tomato, raw carrots, peppers and beetroot. All types of fresh fruit – e.g. apples, bananas, kiwi fruit, oranges, pears, mango and plums. All types of tinned fruit in juice – e.g. pineapple or peaches Stewed fruit Dried fruit Beans and pulses only count as a maximum of 1 portion per day. Fruit juice (100% juice) Tips • • • • • • • • • Steaming or cooking vegetables with minimum amounts of water and serving as soon as possible will help retain vitamins. Use fresh fruit and vegetables as soon as possible, rather than storing them, to avoid vitamin loss. Offer fruit as a snack. Older people may find it difficult to peel or cut whole fruit, so a plate of sliced ready prepared fruits may be more acceptable. Add vegetables and pulses to stews, casseroles or other dishes and offer a variety of vegetables at main meals. Baked beans (as a vegetable) should be served a maximum of twice a week. Encourage a daily glass of 100% fruit juice with breakfast or with a main meal. Buy tinned fruit in natural juice rather than in syrup. Offer a variety of dried fruits to add to cereal options and porridge and include dried fruit in cakes and desserts. Pureed stewed fruit can be offered with custard or yoghurt or ice cream as dessert 33 Food group Guidance Rationale What’s included Milk and dairy products Milk and dairy foods should be served every day. Milk and dairy products are excellent sources of calcium which is needed for optimal bone strength protein, vitamin A, riboflavin and vitamin D. All types of milk. Moderate amounts should be offered 2-3 times a day as milk in drinks, cheese, yoghurt or milkbased puddings and sauces. Dried milk, goat’s and sheep’s milk. Cheeses – e.g. Cheddar, cottage cheese, cheese spreads, brie, feta, Edam, goat’s cheese, Stilton, Parmesan. Yoghurt (fruit or plain, whole milk or low-fat), or fromage frais. Older people with small appetites who may need to gain weight or who are of low weight should be encouraged to have full-fat milk and yoghurt. Milk-based sauces, custard and milk puddings. Semi-skimmed milk is suitable for older people with good appetites. Tips • • • • • • • • To add extra calories, protein and nutrients to dishes, extra milk, cheese or dried milk powder can be added in cooking. Whole milk can be fortified further by the addition of extra dried skimmed milk powder for those older people who are of low weight or who have small appetites. Offer milky drinks at snacks and before bed. Milkshakes may be an acceptable alternative, particularly in hot weather. Frozen yoghurts can be offered as an alternative to ice cream. Milk can be used in sweet and savoury sauces, custards and puddings. Smooth yoghurt and fromage frais can be offered as a snack and is useful if older people have eating difficulties. It is worth highlighting that some dairy products can contain high salt levels. Strong cheese can impart flavour in smaller amounts. For dairy-free diets, serve soya drinks (fortified with calcium) as an alternative. 34 Food group Guidance Rationale What’s included Meat, fish and meat alternatives A meat or alternative should be offered at all main meals. Meat is a good source of protein and of vitamins and minerals such as iron and zinc Meat, poultry, offal1, fish, eggs, nuts, beans, pulses and meat alternatives. Red meat should be offered a minimum of twice a week. Fish is an excellent protein source and contains selenium and iodine. Meat includes all cuts of beef, lamb and pork and meat and meat products such as ham, corned beef and sausages. Look for meat products with a high meat content. Use lean meat (with a fat content of about 10%). Fish should be offered at least twice a week. It is strongly recommended that oily fish should be served once a week. Meat alternatives for vegetarians should be varied and use a variety of foods from this group (e.g. eggs, peas, beans and pulses, soy-based meat alternatives, nuts, quorn or tofu). Oil-rich fish provides omega-3 fatty acids which may help to prevent heart disease. Such foods are also a source of vitamins A and D, and iron. Beans and pulses are sources of protein, iron and zinc. Eggs are a good source of protein, vitamins A and D Nuts provide a source of protein, iron, fibre, zinc and calcium. Fish includes fresh, frozen and tinned fish, such as tuna, sardines, pilchards and mackerel, and fish products such as fish cakes and fish fingers. Oily fish, such as salmon and sardines. Beans – e.g baked beans, butter beans, kidney beans and lentils are in this group and provide a good source of protein for vegetarians. Tips • • • • • • • • Always select the leanest cuts of meat and remove visible fat and poultry skin. Reduce the amount of processed meat and fish products which are high in fat and salt, such as crumb-coated chicken products, burgers, pies and canned meats. These are often high in salt and low in meat content. Customers need to be made aware of nuts and nut products incorporated into dishes. Eggs are a useful source of nutrients but they should always be well cooked for older people. Oil-rich fish can be used in pâtés and spreads on bread and toast. Liver pâté is a useful source of nutrients for older people but liver and liver products should not be served more than once a week. For older people who have difficulty chewing, offer soft lean meat and fish or meat and fish dishes where the meat has been minced or served in a sauce. 1 Liver and liver pâté are very rich in vitamin A and it is recommended that these foods are consumed no more than once a week 35 Food group Guidance Rationale What’s included Foods containing fat and foods and drinks containing sugar These foods add palatability to the diet and can be useful in the diets of older people for encouraging eating and stimulating the appetite. The main nutrients provided by such foods are fat, including some essential fatty acids, and also some fatsoluble vitamins. Foods containing fat include: butter, margarine, other spreading fats and low-fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, and gravies. These foods can be high in calories and offer few other nutrients. If appetites are poor, it is important that these foods do not displace more nutrientrich foods. As for the rest of the population, foods from this group can contribute to excess energy intakes if they are eaten in large amounts. Snacking on sugary foods and drinks throughout the day is discouraged as this can cause tooth decay. Older people may enjoy some sweet foods as snacks, and moderate amounts of these foods are acceptable. Carbohydrate (in the form of sugars) is also provided. Some foods in this group also contain salt. Foods containing sugar include: soft drinks, sweets, jams and sugar, as well as foods such as cakes, puddings, biscuits, pastries and ice cream. Tips Use mono- and poly- unsaturated fats wherever possible for cooking, spreading and in dressings. Good choices of cooking and salad dressing fats include soya, rapeseed and olive oils and good choices of fat spread are those made from sunflower oil, soya oil or olive oil. Vitamin D To increase the amount of dietary vitamin D in menus served to older people: • Use margarine fortified with vitamin D for baking and as a fat spread. • Include an oily fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 514µg of vitamin D per 100g. • Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. • Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. • Meat and poultry contribute small but significant amounts of vitamin D. 36 3.13 Example menu for those eating all their meals and snacks on NHS premises An example menu which shows the types and amounts of foods and drinks that would meet the nutrient based guidance for adults aged 19-74 years is shown in section 3.12. This is an example only: many NHS setting may offer more choices at meals and snacks and may also offer a range of special diet options which are not covered by this report. This menu is based on the portion sizes that would be needed by those aged 19-74 years to meet the nutrient guidance. For those aged 5-18 years and those aged 75 years +, smaller, or larger, portion sizes of these foods are likely to provide appropriate amounts of nutrients. Further information about how to encourage eating well for young people and older people can be found in the sections: 4.0 Nutritional guidelines for children and young people aged 5-18 years in residential accommodation and 6.0 Nutritional guidelines for older people in residential care. 40 3.14 Example menu for those eating all their meals and snacks on NHS premises Monday Tuesday Wednesday Thursday Friday Saturday Sunday BREAKFAST Fruit choice Cereal choice Cooked choice 1 Cooked choice 2 Cooked choice 3 Bread choice Drinks Orange juice (200ml), grapefruit juice (200ml), grapefruit segments (105g), prunes (50g), or fruit compote (105g) Weet bisks (20g), Shredded wheat (22g), or Bran flakes (21g) with semi-skimmed milk (100g), or porridge (110g) Bacon – reduced salt (25g) or sausage – lean (35g) with baked beans – lower salt and sugar (80g) or grilled tomato (80g) Scrambled egg (60g) or poached egg (50g) Kedgeree – reduced salt (200g) Slice white toast (27g), wholemeal toast (31g), white bread (31g) or wholemeal bread (35g), with low fat spread (7g) and jam (15g) or marmalade (15g) Water, tea or coffee with semi-skimmed milk (30ml) MID MORNING SNACK Tea or coffee with Semi-skimmed milk (30ml), with Digestive biscuit (13g) or Oat based biscuit (15g) LUNCH Tomato and lentil soup (180g) Beef Olives (150g) Gravy (50g) Courgette and watercress soup (180g) Irish Stew (190g) Tomato soup (180g) Scotch broth (180g) Mushroom soup (180g) Onion soup (180g) Spicy lentil soup (180g) Chicken and mushroom pasta (340g) Pork and potato bake (260g) Braised Steak (120g) Gravy (50g) Lamb Curry (200g) Main choice 2 Vegetable shepherd s pie 200g Vegetable bake (90g) (110g) Mixed bean casserole (250g) Mixed vegetable crumble (160g) Mushroom stroganoff (150g) Vegetable chilli (150g) Roast Beef (70g) and Yorkshire Pudding (35g) Gravy 50g) Vegetable lasagne (240g) Main choice 3 Goujons of fish (80g) with tartare sauce (10g) Chips (100g) Chicken chasseur (200g) Prawn curry (140g) Tuna (45g) Salad (50g) Option of Coleslaw (40g) and/or Potato salad (85g) Chicken and vegetable casserole (225g) Salmon in spicy tomato sauce (230g) Seafood pasta (230g) Tuna and tomato pasta (260g) Beef stew (150g) Beef curry (180g) Oriental beef stir fry (135g) Egg fried rice (140g) Roast chicken (60g) Calypso turkey (165g) Pork with apricots (140g) Soup Main choice 1 Main choice 4 40 Starchy choice 1 Boiled new potatoes (120g), Jacket potato (120g) or Mashed potato (120g) Starchy choice 2 Rice (150g) or Pasta (200g) Vegetable choice 1 Leeks (80g) Cauliflower Gratin (90g) Aubergine in Tomato Sauce (90g) Carrots (80g) Spinach (80g) Vegetable choice 2 Broccoli (80g) Peas (80g) Brussels sprouts (80g) Parsnips (80g) Mixed diced vegetables (80g). Vegetable choice 3 Side salad (80g) Dessert choice 1 Fresh fruit slices (100g) or Low fat fruit yoghurt (125g) Dessert choice 2 Rhubarb crumble (100g) with Custard (150g) Chocolate fudge pudding (100g) Dessert choice 3 Drinks Apple Pie (100g) with Cream (40g) Fruit compote (160g) with Custard (150g) Bread & Butter Pudding (115g) with Custard (150g) Sweet oat cake (45g) Apple crumble (100g) with Custard (150g) French beans (80g) with tomato sauce (10g) Ratatouille (90g) Cabbage (80g) Apricot and pear layer (100g) with Custard (150g) Dutch apple tart (100g) with Custard (150g) Apricots Trifle (150g) Bakewell Lemon canned in tart (100g) Meringue juice (125g) pie (100g) with Custard (150g) Water, tea, coffee (with semi-skimmed milk 30ml), 100% fruit juice (150ml) Curly kale (80g) Chocolate mousse (100g) MID AFTERNOON SNACK Tea or coffee with semi-skimmed milk (30ml) Fruit loaf (45g), Madeira cake (45g), banana bread (45g) EVENING MEAL Bread Bread roll selection – granary, wholemeal, crusty white and soft white rolls with soft margarine (60g) Main choice 1 Fish Pie (220g) Baked cod (70g) Main choice 2 Chicken and broccoli lasagne (300g) Macaroni cheese (250g) Main choice 3 Cheese salad (90g) Oriental chicken curried rice Steamed fish with Ginger and Spring Onion (70g) Vegetable curry (225g) Breaded cod (95g) Chicken dansak (230g) Kedgeree – reduced salt (200g) Plaice Veronique (100g) Vegetable pie (250g) Vegetable crumble (160g) Cheese and onion turnovers (120g) Mushroom and pepper bake (120g) Chicken salad (100g) Option of Cottage cheese & pineapple Salmon (salad (95g) Corned beef salad (100g) Turkey salad (100g) 1 Coleslaw (40g) and/or Potato salad (85g) Starchy choice 1 (300g) Mixed salad (50g) Coleslaw (40g) and/or Potato salad (85g) salad Option of Option of (100g) Coleslaw Coleslaw Option of (40g) (40g) and/or Coleslaw and/or Potato salad (40g) Potato (85g) and/or salad (85g) Potato salad (85g) Boiled new potatoes (120g), Jacket potato (120g) or Mashed potato (120g) Starchy choice 2 Rice (150g) or Pasta (200g) Vegetable choice 1 Spinach (80g) Vegetable choice 2 Ratatouill e (90g) Vegetable choice 3 Coleslaw (40g) and/or Potato salad (85g) Leeks (80g) Cabbage (80g) French beans (80g) with tomato sauce (10g) Side salad (80g) Parsnips (80g) Aubergine in Tomato Sauce (90g) Peas (80g) Curly kale (80g) Brussels sprouts (80g) Cauliflower gratin (90g) Carrots (80g) Mixed diced vegetables (80g). Broccoli (80g) Dessert choice 1 Fresh fruit (100g) or low fat fruit yoghurt (125g) Dessert choice 2 Muesli Chocolate Flapjack (55g) Spiced Fruit tea Sultana slice brownie apple slice bake (50g) sponge (50g) (60g) (50g) (50g) Melon Fruit jelly Fresh fruit Poached Fruit flan Rhubarb and grape (160g) salad (120g) pear (140g) (150g) fool (120g) salad (120g) Water, tea or coffee with semi-skimmed milk (30ml), 100% fruit juice (150ml) Dessert choice 3 Drinks Option of Coleslaw (40g) and/or Potato salad (85g) Flapjack (60g) Tropical fruit salad (120g) EVENING DRINK Tea or coffee with semi-skimmed milk (30ml), hot chocolate (218g), Horlicks (218g) or Ovaltine (218g) Water and 100% fruit juice should be available with main meals Water should be freely available throughout the day Please Note 1 The portion sizes outlined here are for adults aged 19-74 years. The analysis of this menu is compared with the guidance for an adult of this age below. For those aged 5-18 years and those aged 75 years +, smaller, or larger, portion sizes of these foods are likely to provide appropriate amounts of nutrients for those who do not have specific nutritional needs. . 2 3.15 Analysis of NHS menu compared with the guidance for adults aged 19-74 years Energy kcals MJ Dietary reference value (DRV) Adults 19-74 years Menu analysis EAR 2225 9.4 2225 9.4 Fat g No more than 35% of energy MAX 87 64 Saturated fat g No more than 11% of energy MAX 27 23 Total carbohydrate g At least 50% of energy MIN 297 343 Non-milk extrinsic sugars g No more than 11% of energy MAX 65 65 Fibre g DRV MIN 18 22.5 Protein g RNI MIN 50 92.9 Vitamin A µg RNI MIN 700 1497 Vitamin C mg RNI MIN 40 197 Folate μg RNI MIN 200 427 Calcium mg RNI MIN 700 1333 Iron mg RNI MIN 15 17 Zinc mg RNI MIN 9.5 11.3 Sodium mg MAX 2400 2393 MAX 6 6 Salt 1 g SACN recommendation SACN recommendation The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced 40 4.0 Nutritional guidelines for food served to adults in residential accommodation 4.1 Background There are a number of reasons why adults might be in residential accommodation. The majority of adults living in residential accommodation however are likely to have some form of physical or learning disability. It is estimated that there are about 1.5 million people with learning disabilities in the UK, and approximately 40% of this population group live in some form of residential accommodation. 1 There is considerable evidence that the nutritional status of people with learning disabilities is frequently poor. Studies have shown that people with learning disabilities are frequently both underweight and overweight 2 and that their diets are frequently inadequate 3 . Poor intakes of fruits and vegetables, low fibre, high fat diets have been reported. There is currently a lack of good data reviewing the diets of people with learning disabilities in the UK. 4.2 Who are these nutritional guidelines for? These guidelines apply to all adults aged 19-74 years in residential accommodation who do not have special dietary requirements. Nutrient guidelines for adults aged over 75 years can be found in section 6.0. This guidance is therefore not appropriate for those catering for adults with any medical condition which requires a therapeutic diet or any disability which requires dietary manipulation. Advice on special diets should be sought from a Registered Dietitian. 4.3 Rationale for nutrient based guidance for food served to adults aged 19-74 years in residential accommodation The majority of adults in residential care have the same needs for a healthy balanced diet as all other adults in the population. The rationale here is based on the current evidence available for all adults in the population. 1 http://www.mencap.org.uk/html/press_office/fact_figures.asp Emerson E 2005. Underweight, obesity and exercise among adults with intellectual disabilities in supported accommodation in Northern England. Journal of Intellectual Disability Research, 49, 134143 3 Robertson J, Emerson E, Gregory N, Hatton C et al. Lifestyle related risk factors for poor health in residential settings for people with intellectual disabilities. Research in Developmental Disabilities, 21, 469-486 2 The National Diet and Nutrition Survey 4 (NDNS) of adults aged 19-64, carried out in 2002, has raised several key concerns with regards to nutrient intake and the nutritional status of this population group. Energy (calories) and fat intake Adults’ total carbohydrate intake is close to the dietary reference value (DRV) 5 of 50% of food energy for both men and women and since the last adult survey carried out in 1986/87 6 total fat intake has decreased. However, the proportion of energy derived from saturated fat still exceeds the dietary reference value of 11% of food energy. Also, in the 2002 survey the percentage of food energy derived from nonmilk extrinsic sugars was 13.6% for men and 11.9% for women – exceeding the DRV of 11% of food energy. Intakes were higher in the younger age groups (19-24 years). Non-starch polysaccharides (NSP, or fibre) In the survey of 19-64 year olds, the mean daily intake of non-starch polysaccharides (NSP) was below the recommended average intake of 18g per day for all sex and age groups, and a third of adults had intakes of less than 12g a day. Intakes were particularly low among those in the younger age group (19-24 years) where average intakes were 12.3g for men and 10.6 for women. Vitamins In the 2002 survey, adults’ average intakes of all vitamins were close to the Reference Nutrient Intake (RNI) for all sex and age groups, except for vitamin A in the youngest groups, where results were below the RNI. Assessments of nutritional status indicated issues regarding low vitamin D status as well as inadequate vitamin C and folate concentrations among some individuals. Adults who rarely go outside, or who wear very restrictive clothing will not get sufficient Vitamin D from their diet alone and are likely to need vitamin D supplements. Minerals Iron intakes in women were well below the RNI in all but the oldest age group. Over 40% of those women in the two youngest age groups had iron intakes below the LRNI (Lower Reference Nutrient Intake). Assessments of nutritional status indicated issues regarding low iron status, with 8% of women and 3% of men having signs of 4 Henderson L et al 2002 and 2003. The National Diet and Nutrition Survey: Adults Aged 19-64 Years, Volumes 1-4. TSO. London 5 Department of Health 1991. Dietary Reference Values for Food Energy and Nutrients for the United Kingdom. Report on Health and Social Subjects No. 43. HMSO. London 6 Gregory J et al 1990. The National Dietary and Nutritional Survey of British Adults. HMSO. London. anaemia and 11% of women and 4% men having low serum ferritin levels (another measure of low iron status). The average intakes of some other minerals were below the RNI for a number of sex and age groups. Results indicated low intakes of potassium and magnesium, which were well below the RNI for the youngest male group and below the RNI for all female age groups. Issues regarding low intakes of iodine and zinc were also apparent in the younger female groups, and concerns with intakes of calcium and copper were also highlighted. Sodium/salt In the 2002 survey, the average salt intake for adults was estimated at 9.5g per day overall (based on mean urinary sodium excretion levels per 24 hours of 187.4mmol per day for men and 138.5mmol per day for women.) This result represents a slight increase from the 1986/87 adult survey and average intakes in all sex and age groups were well above the recommended maximum daily intake of 6g per day 7 . Fruit and vegetables The National Diet and Nutrition Survey reported that few adults achieved the 5 portions of fruit and vegetables recommended each day – with men and women having on average less than 3 portions a day. Overweight and obesity Data on overweight and obesity levels among adults in the UK from the 2004 Health Survey for England 8 and The Scottish Health Survey 2003 9 suggest that a significant proportion of adult men and women are now obese (with a body mass index of more than 30kg/m2). Nearly a quarter (23.6%) of men and 16% of women in England and 22.4% men and 26% of women in Scotland are reported to be obese and approximately two-thirds of all adults are overweight (with a body mass index 7 Scientific Advisory Committee on Nutrition 2003. Salt and Health. TSO. London Data from Healthy Survey for England 2004 accessed from: http://www.ic.nhs.uk/pubs/hlthsvyeng2004upd 9 Scottish Executive 2005. The Scottish Health Survey. Scottish Executive. Edinburgh. 8 greater than 25 kg/m2). Similar levels of overweight and obesity are found in Wales 10 and Northern Ireland 11 . Given the rising levels of obesity in the UK, it is important not to exceed average energy (calorie) requirements. It is therefore suggested that main meals should provide nutrient-dense food – that is, food which contains high levels of nutrients – but that these foods should not be correspondingly higher in calories. Those individuals who are in the normal range for bodyweight (BMI 20-25 kg/m2) but who have higher energy needs because they use up more calories (because they either have a larger body size, or do more activity, or both) should have the opportunity to eat more carbohydrate-based foods at meals to meet their higher energy requirements without disproportionately increasing their intake of fat, saturated fat, sugar or salt. Based on the most recent assessments of nutritional status for the UK population, it appears that it may also be prudent to ensure that food served in public institutions at breakfast and at main meals provides enhanced amounts of fibre, iron, folate, vitamin C and zinc. In order to ensure that population maximum intakes of fat, saturated fat, sugars and salt are within current recommendations, it is important that these nutrients are not exceeded in the guidance suggested. Another priority is to ensure that meals offer the opportunity to increase fruit and vegetable intakes. The example menu provided here for adults aged 19-74 years outlines the sorts of foods and drinks that could be offered to ensure that adults have the opportunity to consume a healthy, balanced diet that corrects current insufficiencies and provides amounts of fat, saturated fat, salt and sugar in line with current recommendations. The food based guidance on pages 7-12 provides caterers with practical guidance on how to prepare menus for adults who receive all their meals and snacks on NHS premises. 10 Welsh Health Survey October 2003 - March 2004. Accessed from: wales.gov.uk/keypubstatisticsforwales/content/publication/health/2004/sdr82-2004/sdr82-2004.pdf 11 Northern Ireland Health and Social Wellbeing Survey 2001. Accessed from: www.csu.nisra.gov.uk/archive/Surveys/HWB/publications/1997/Health%20&%20lifestyle%20report% 201997.pdf Table 4.1 Nutrient based guidelines for food served to adults aged 19-74 years in residential accommodation Energy Dietary reference value (DRV) Adults 19-74 years EAR 2225 9.4 kcals MJ Fat g No more than 35% of energy MAX 87 Saturated fat g No more than 11% of energy MAX 27 Total carbohydrate g At least 50% of energy MIN 297 Non-milk extrinsic sugars g No more than 11% of energy MAX 65 Fibre g DRV MIN Protein g RNI MIN Vitamin A µg RNI MIN Vitamin D µg RNI MIN Vitamin C mg RNI MIN Folate μg RNI MIN Calcium mg RNI MIN Iron mg RNI MIN Zinc mg RNI MIN Sodium mg Salt g SACN recommendation SACN recommendation EAR = Estimated Average Requirement RNI = Reference Nutrient Intake For explanation of terms see glossary MAX MAX 18 50 700 -* 40 200 700 15 9.5 2400 6 DRV = Dietary Reference Value * Vitamin D It is difficult for adults to get all the vitamin D they require through the diet and most adults will also make Vitamin D on exposure of the skin to sunlight during the summer months. Adults who rarely go outside or who go outside infrequently and who wear clothing which means their skin is not exposed to the sun are likely to require vitamin D supplements. 4.3 Food based guidance for menu planners The following pages contain some information for caterers about food groups and how to choose foods which will contribute to a healthy balanced diet. It is also useful for caterers to look at food labels on foods and ingredients they buy or use and to choose those that are lower in salt, sugar and fat. The Food Standard’s Agency provides information on what is ‘a lot’ of salt, sugar and fat in foods and these are outlined below. Foods high in salt have 1.25 grams or more salt per 100grams or 500 milligrams of sodium per 100 grams of food Foods high in sugar have 10 grams or more of sugars per 100 grams of food Foods high in fat have 20 grams or more of fat per 100 grams of food Foods high in saturated fat have 5 grams of saturated fat or more per 100 grams of food For more information about nutritional information on food labels see www.eatwell.gov.uk Additional information about foods which are good sources of some of the nutrients which appear to be insufficient in the diets of some people in the UK can be found in Appendix 2. Fluid intakes It is important that everyone has access to adequate fluid intakes throughout the day. In climates such as the UK, we should drink approximately 1.2 litres (6 to 8 glasses) of fluid every day to stop us getting dehydrated. In hotter climates the body needs more than this. We get some fluid from the food we eat but it is important that fluids are not restricted since dehydration can lead to headaches, confusion and irritability and lack of concentration as well as constipation and potentially urinary tract infections. Clean, chilled water should always be available with meals and between meals. 4.4 Food-based guidelines for food served to adults aged 19-74 years in residential accommodation Food Group Guidance Rationale What’s Included Bread, other cereals and potatoes Starchy foods should make up a third of the daily diet. Starchy foods are a good source of energy and the main source of a range of nutrients in the diet. As well as starch, these foods supply fibre, calcium iron and B vitamins. All varieties of bread including wholemeal, granary, seeded, chapattis, bagels, roti, tortillas, pitta bread A variety of breads should be available daily at every meal Different starchy foods should be offered in main meals throughout the week so that a variety of starchy foods are included. Aim to include pasta and rice on the menu once a week Potatoes, yam, sweet potato, plantain, cocoyam, dasheen, breadfruit, cassava Breakfast cereals Rice, couscous, bulgar wheat, maize (polenta), cornmeal Noodles, spaghetti and other pastas Wholegrain and wholemeal cereal foods are a good source of fibre and other nutrients Tips • • • • • • • • • Serve more pasta and rice and use less sauce. Opt for tomato based sauces instead of cheese-based to reduce fat content When serving rice and pasta, try to use wholemeal, wholegrain, brown or high fibre versions. Some breakfast cereals are nutrient fortified (have added iron, folic acid and other vitamins and minerals). Choose wholegrain cereals or mix some in with other cereals. Offer a variety of breads, such as seeded, wholegrain and granary and use thicker slices with low-fat options for fillings Large pieces of potato and thick or straight cut chips absorb less fat Boil potatoes in the minimum amount of water and for the shortest amount of time to retain vitamins. Use herbs or other shredded vegetables to add colour and flavour to baked potatoes, rather than butter or margarine. If you look after young people who have allergies to wheat, oats, barley and rye: good alternatives to offer are foods made from maize (e.g. polenta), rice, rice flour, potatoes, potato flour, buckwheat, sago, tapioca, soya and soya flour. Cereal foods which are good sources of iron and zinc include fortified cereals, whole grain cereals, wholemeal bread and flour, couscous and wholemeal pasta. Food Group Guidance Rationale What’s Included Fruit and Vegetables Fruit and vegetables should make up about a third of the daily diet. Fruit and vegetables are good sources of many vitamins and minerals. All types of fresh, frozen and tinned vegetables i.e. broccoli, Brussels sprouts, cabbage, carrots, frozen peas, peppers, swede, sweetcorn It’s important to offer a variety. Five-a-day is an achievable target. Aim for one or two portions with each meal and offer fruit and vegetables as snacks. One portion s about 80g fresh fruit and vegetables and 40g of dried fruit Beans and pulses are included but only count as a maximum of 1 portion per day A glass of 100% fruit juice can count as one portion of fruit each day There is evidence that consuming 400g a day or more of fruit and vegetables reduces the risk of developing chronic diseases such as coronary heart disease and some cancers. Including fruits and vegetables in the diet will help to increase the intake of fibre and can help to reduce the total amount of calories consumed among those who may wish to lose weight All types of salad vegetables including lettuce, cucumber, tomato, raw carrots, peppers, beetroot All types of fresh fruit e.g. apples, bananas, kiwi fruit, oranges, pears, mango, plums All types of tinned fruit in fruit juice e.g. pineapple, peaches, mandarin oranges Stewed fruit Dried Fruit Fruit juice (100% juice) Tips • • • • • • • • • • • • • • • • Avoid adding fat or rich sauces to vegetables or sugar or syrupy dressings to fruit Steaming or cooking vegetables with minimum amounts of water and serving as soon as possible will help retain vitamins. Use fresh fruit and vegetables as soon as possible, rather than storing, to avoid vitamin loss Incorporate fruit and vegetables in snack options. Offer a variety of healthy snack alternatives Add vegetable and pulses to curry, casserole or stir-fry and serve at least two types of vegetables with fish, chicken or meat. Baked beans (as a vegetable) should be served a maximum of twice a week. Encourage a daily glass of fruit juice (100% juice, unsweetened) with meals. Choose tinned fruit in fruit juice not in syrup. Add a handful of dried fruit to cereal options and porridge. Supply a good combination of traditional salads and raw vegetables, fruits and nuts to increase colour, taste and texture at meal times. Add additional vegetables to savoury dishes. Vegetable soups are a useful way of increasing vegetable intake. Avoid dried fruit with added sugar or vegetable oil. Fruit and vegetables which are useful sources of iron include spinach, broccoli, spring greens, dried apricots, raisins, baked beans, broad beans and blackcurrants. Fruit and vegetables which are useful sources of folate include spinach, broccoli, peas, oranges, melon, green leafy salads and tomatoes. Fruit and vegetables which are useful non-dairy sources of calcium include green leafy vegetables, dried fruit and oranges. Food Group Guidance Rationale What’s Included Milk and Dairy Products Offer dairy foods such as milk, yoghurt and cheese as part of meals and snacks Milk and dairy products are excellent sources of calcium, protein, vitamin A and vitamin D. Calcium helps to contribute to good bone health Skimmed, semi-skimmed, whole milk Offer low fat options such as semiskimmed milk, low fat yoghurt and skimmed milk cheeses The fat content of different dairy products varies and much of this is saturated fat. Dried milk, goats and sheep’s milk All types of cheeses e.g. Cheddar cheese, cottage cheese, cheese spreads, Brie, Feta, Edam, goats cheese, Stilton, Parmesan Yoghurt Fromage frais Do not rely on cheese as the main protein item for vegetarians. Where no other option is available, cheese served as a sandwich filler should be offered no more than twice per week. Tips • • • • • • • • • • Try using very strong-tasting cheese (mature cheddar, blue cheese) if using to flavour dishes or sauces, because less will be required. Choose reduced-fat hard cheeses, cottage cheese and skimmed milk soft cheese. Offer semi-skimmed or skimmed milk and low-fat yoghurts and fromage frais. Use plain yoghurt and fromage frais instead of cream, soured cream or crème fraiche in recipes Try serving frozen yoghurts as an alternative to ice cream. It is worth highlighting that some dairy product can contain high salt levels. Look for lower salt cheeses and use smaller amounts of stronger cheese. Dairy foods are very important during pregnancy, but unpasteurised dairy produce and softmould-ripened cheese (e.g. Camembert, Brie and all blue-veined cheese) should be avoided. For those on dairy free diets serve soya drinks fortified with calcium as an alternative. Fresh fruit milkshakes and chilled milk drinks can be offered as snacks. Restrict sweetened milk drinks to mealtimes as the sugars in these drinks can damage teeth. Food Group Guidance Rationale What’s Included Meat, fish and meat alternatives Offer a meat or alternative at all main meals Meat and meat alternatives are a good source of protein, vitamins and minerals such as iron and zinc Use lean meat (which has a fat content of about 10%) Some meat and meat products can have a high fat and saturated fat content Meat includes all cuts of beef, pork, lamb, poultry, offal1 and meat products such as bacon, sausages, beef burgers, pies and cold meats Fish should be offered at least twice per week. White fish is low in fat It is strongly recommended that oily fish such as salmon, trout, mackerel, herring, pilchards, sardines should be served once a week Oil-rich fish provides a good source of omega-3 fatty acids, which may help to protect against heart disease. Oil-rich fish are also a source of vitamins A and D. Eggs can be served at breakfast and as part of main meals Eggs are a good source of protein, vitamin A, vitamin D and some minerals Ensure meat alternatives for vegetarians are varied Beans, pulses, eggs, meat alternatives and nuts all provide good sources of nutrients. Fish includes fresh, frozen and tinned fish, such as tuna and sardines, Fish products such as fish cakes and fish fingers may have a low fish content Boiled, poached, scrambled eggs, omelettes Beans and pulses such as chick peas, lentils, kidney beans, butter beans, textured vegetable protein, nuts, soya products such as tofu, quorn Tips • • • • • • • • • • 1 Always select the leanest cuts of meat and remove visible fat and poultry skin. Roast meat on a rack in order to let the fat run off. Grill, poach or bake meat rather than frying. If you do fry, use clean oil and at the correct. temperature to minimise absorption. Note that larger pieces of fish and meat absorb less fat. Do not add extra fat or oil when cooking meat. Use more vegetables, pulses and starchy food to extend dishes further, as well as add more texture and flavour. Less meat is also required, reducing the fat content and the cost of the meal. Buy good quality meat and use smaller amounts. Use fish from sustainable fish stocks. Offer unsalted nuts and seeds as snacks. Reduce the amount of processed meat products served such as meat pies and pasties, coated, canned and composite meat products such as sausages, burgers, coated chicken products. Reduce the amount of processed fish products on offer, particularly those that are fried or coated such as fish fingers or fish cakes. Liver and liver pâté are very rich in vitamin A and it is recommended that these foods are consumed no more than once a week. Food Group Guidance Rationale What’s Included Foods containing fat and foods and drinks containing sugar These foods can add palatability to the diet but should be eaten in small amounts each day Foods containing fat and foods containing sugar often provide a lot of calories and a lower proportion of other nutrients. Foods containing fat include: Reduce the amount of foods containing visible fat for example, margarine and butter, cooking oils and mayonnaise. Other foods containing fat such as cakes and biscuits should be eaten occasionally Foods and drinks containing sugar often contain few other nutrients and frequent consumption between meals can contribute to tooth decay Some foods in this group are also high in sodium/salt Butter, margarine, other spreading fats and low fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, gravies. Foods and drinks containing sugar include: Soft drinks, sweets, chocolate, jams, sugar, cakes, puddings, biscuits, pastries and ice cream Tips • • • • • • • • • • • Use mono- or poly-unsaturated fat spreads Use cooking oils high in monounsaturates such as soya, rapeseed or olive oils Avoid serving pastry dishes frequently Measure oil for cooking carefully and reduce oil used in the preparation of soups, stews and casseroles. Vegetables can often be dry fried, steamed or stewed to form the basis of sauces and other dishes Use low-fat yoghurt or non-dairy ice cream to complement puddings or pies. Produce puddings lower in fat and sugar and incorporate fresh, tinned fruit in juice or dried fruit. Offer water, unsweetened fruit juices and chilled milk drinks Serve wholegrain or plain cereals rather than sugar coated cereals Provide currant buns, fruit bread, melon slices, malt loaf and other lower fat bread based foods as alternatives to cakes and biscuits. When preparing sandwiches, try and avoid using butter or spreads if the filling is already moist. Consider using reduced-fat spreads and opt for types that are soft straight from the fridge, so it is easier to spread thinly. To increase the amount of dietary VITAMIN D in menus • • • • • Use margarine fortified with vitamin D for baking and as a fat spread. Include an oily fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 5-14µg of vitamin D per 100g. Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. Meat and poultry contribute small but significant amounts of vitamin D. 4.5 Example menu for adults aged 19-74 years in residential accommodation An example menu is given here which show the sorts of foods, and the amounts of these foods, that could be served to meet the nutritional and food-based guidance for adults in residential accommodation. The analysis of the menu is included on page 16. The example menu shown here includes a sandwich style lunch, however this is just an example. Caterers may wish to offer a variety of hot and cold meals at lunch and tea and may choose to offer one, two or more choices depending on the client groups that they serve. 4.6 Example menu for adults in residential accommodation Monday Breakfast Midmorning Tuesday Wednesday Thursday Friday Saturday Sunday Raw carrots/cucumber/pepper slices (40g) Pizza with choice of toppings (240g) Coleslaw (80g) Jacket potatoes (220g) Roast turkey (80g) Stuffing (30g) Roast potato (200g) Carrots (80g) Broccoli (80g) Currant bun/fruit bread/malt loaf/fortified cereal bar/crunchy muesli bar (20-75g) or Fromage frais or yoghurt (60-125g) Vegetable lasagne (v) (300g) Peas (80g) Breakfast cereal (37g) (average of bran flakes/puffed wheat/wheat bisks) Semi-skimmed milk (100ml) Orange juice (150ml) Wholemeal toast (63g) with polyunsaturated margarine (7g) and marmalade/jam/honey (8g) Tea, coffee with semi-skimmed milk (30ml) Apple/banana/Satsuma/pear or other fresh fruit snack (100g) Tea, coffee, water Lunch Water or 100% fruit juice Choice of sandwiches (75-110g) made with brown or white bread or wraps filled with cheese/tuna fish/corned beef/ham/egg mayonnaise/chicken tikka/sweetcorn/tomato/cress or Dried fruit snack (40g) Banana custard (150g) or Ice cream and topping sauce (60g) Lentil roast (v) (170g) New potatoes (200g) Green beans (80g) Fresh fruit salad and ice cream (150g) or Lemon meringue pie (100g) Midafternoon Tea, coffee, water Water or 100% fruit juice available Banana bread (70g) Date bars (75g) Swiss roll (40g) Flapjack (50g) Banana and raisin bake (70g) Oat bars (40g) Chocolate yoghurt cake (60g) Jacket potato (220g) with savoury mince filling (200g) Green beans (80g) Chicken and vegetable stir-fry (270g) Egg noodles (200g) Lamb and potato hotpot (300g) Peas (80g) Sardine pasta (300g) Crunchy salad (90g) Baked cod (90g) Oven chips (150g) Baked beans (90g) Chicken risotto (250g) Sweetcorn (80g) Cherry tomatoes (80g) Crusty bread (50g) Polyunsaturated margarine (7g) Hot dogs with pork, beef or vegetarian sausages (115g) Carrot and apple salad (100g) Mixed bean salad (100g) or Lentil and mushroom crumble (250g) Tomato salad (80g) Crusty brown roll (48g) Polyunsaturated margarine (7g) or Vegetarian burgers (v) (50g) Pasta Roma (250g) or Broccoli quiche (v) (120g) Crunchy coleslaw (80g) Rice salad (200g) or Sweetcorn and pasta bake (v) (300g) Carrots (80g) Oven chips (150g) Or Couscous with sweet and sour vegetables (v) (280g) or Chickpea rissoles (v) (100g) Spinach (80g) New potatoes (200g) Carrot cake (80g) or Rhubarb fool (200g) or Meringue baskets with fruit (150g) or Mandarin oranges and ice cream (200g) Pineapple crunch (170g) or Lemon sorbet (100g) Fruit mousse (80g) or Poached pear and custard (270g) Rice and sultana pudding (220g) Warm milky drink (option of Milk, Hot chocolate, Ovaltine or Horlicks -made with semi-skimmed milk) (218ml) Wholemeal biscuits (26g) or fresh fruit (100g) Fruit yoghurt with crunchy topping (150g) Supper Baked apples with yoghurt (210g) or Summer pudding (150g) Apple crumble with custard (250g) or Fresh fruit (100g) 4.7 Nutritional analysis of example menu for adults in residential accommodation Energy Kcals MJ Nutrient based Guideline Average nutrient values from sample menu 2225 9.4 2227 9.2 Fat g Max 87 68 Saturated fat g Max 27 24 Total carbohydrate Non milk extrinsic sugars Fibre g Min 297 346 g Max 65 59 g Min 18 26 Protein g Min 50 80 Vitamin A µg Min 700 1417 Vitamin C mg Min 40 1 73 Folate µg Min 200 5 11 Calcium mg Min 700 1300 Iron mg Min 15 19 Zinc mg Min 9.5 10 Sodium mg Max 2400 2212 g Max 6 5.5 Salt1 1 The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced 5.0 Nutritional guidelines for food served in prisons 5.1 Background In England and Wales there are 128 prisons: 91 for male prisoners and 17 for females, 16 are Young Offender Institutions and 4 are juvenile establishments. The prison population, at 31st March 2005 was 68,306 and consisted of 54,982 adult male prisoners and 3,517 adult female prisoners 1 . There were 9,386 male and 421 female prisoners under the age of 21. The Home Office Prison Population Projections anticipates the number of prisoners to increase over the next four years from between 76,060 – 79,490 in 2006, to between 77,380 and 91,500 in 2010. At the end of September 2002 there were 2633 children between the ages of 15 to 17 in prison in England and Wales, just 4% of those were girls. In England and Wales, young black people represent just 2% of the population, but inside prison, they represent 20% of the population. Young people held in prison are particularly vulnerable as about half of them have been looked after children and may have had poor nutritional intakes in childhood. The fastest growing population of prisoners is the ‘older’ prisoner: between 1992 and 2002 the population of male prisoners over 60 had more than trebled from 442 to 1359, comprising 2.6% of the male adult prison population over the age of 18. Only 5.2% of the female prison population was over the age of 50 in 2002. A recent report by the National Audit Office has found that the overall quality of prison catering has improved since 1998 but suggests that further improvements are needed 2 . Prison Service catering in 2004-2005 cost £94 million, £43million of which was spent on food and £32 million on catering staff. In each prison the governor sets the daily food budget and this averages at £1.87 per prisoner per day, but ranges from £1.20 to £3.41. The Scottish Prison Service spends an average of £1.57 daily. This can be compared with the amount typically spent on a hospital in-patient of about £2.50 per person per day The National Audit Office highlighted a number of issues around prison food summarised on page 2. 1 2 HM Prisons Service: Sustainable Development Report 2004-2005 National Audit Office 2006 Serving Time: Prisoner diet and exercise. The Stationery Office London 1 • In some Scottish prisons that there has been insufficient food provided for young men, in addition to an insufficient supply of fresh fruit and vegetables. • The nutritional content of food may be reduced due to long standing time after preparation. • Food is often served cool or cold and is therefore less palatable. • The main lunch meal (often the only hot meal in the day) has been served as early as 11.15 am and an evening meal at 4pm, leaving an interval of well over the recommended 14 hours between meals overnight. Because of this sometimes a snack such as biscuits or fruit may have been provided for consumption in the evenings. • Whilst prisons met the standard requirements for a choice of religious and ethnic food prisoners were not always convinced that this was the case. Equipment for Muslim food production, such as knives and cutting boards, pots and pans had been found with other equipment, unlabelled. • Prisoners are unlikely to be offered a hot meal for breakfast. It is apparent that the majority of prisoners are provided with ‘breakfast packs’ during the evening service. These are cold meals costing around 27p and although are intended to be eaten for breakfast, are often consumed during the preceding evening. • Salt content of meals was high with some meals containing up to 93% more than salt than is currently recommended. • Fibre was found to be low in many meals owing to the low level of fresh fruit and vegetables and wholegrain products such as bread and cereals. Most prison meals did not appear to contain sufficient dietary fibre. Instead of the recommended 18g dietary fibre daily, the levels ranged from 5.7g for women prisoners’ meals to 12.7g in vegan meals for male prisoners. • A major concern for prisoners is that they are likely to have limited exposure to sunlight and consequently have a greater dietary requirement for vitamin D than the population at large. Vitamin D was not sufficiently provided by any meals investigated by the National Audit Office. • Many of the meals examined were high in calories, and these exceeded government recommendations, and were also high in saturated fatty acids. Many of these meals relied heavily on convenience foods such as pies and burgers and tinned food, with little use of seasonal produce. • Most meals offered to women prisoners provided similar energy levels as those offered to the male prisoners. 2 One of the main findings of the report was that even though some prisons offered as many as six options for an evening meal, meeting the recommendations for fruit and vegetables was difficult as many meals relied on convenience foods, such as pies, burgers, soups and noodles. These foods are often poor sources of some important nutrients and most contain high levels of salt. Many prisons do not offer oil rich fish every week. 5.2 Rationale for nutrient based guidelines for food served to male and female prisoners The amounts of energy and nutrients that are recommended for populations of males and females aged 19-74 years have been calculated for this report and these are given in Appendix 1 and are outlined in table 5.1. The nutrient based guidelines are outlined for the whole day. Since not all prisoners may have access to snacks and are therefore reliant on the food provided at breakfast, lunch and tea for all their nutrient requirements, it is recommended here that 100% of requirements are spread across the day. The proportions of energy and other nutrients offered at these meals are recommended as follows: Breakfast 20% Lunch 40% Evening meal 40% Many prisoners may have access to a prison shop and will therefore be able to buy foods to supplement their daily rations. This could mean that some prisoners routinely eat more calories each day than they burn up and this could lead to weight gain. It is difficult to ensure that the needs of both those individuals who have higher energy and nutrient requirements are met whilst others do not receive more food energy than they need. Prisoners are more likely to have excessive calories if they frequently snack on high fat, high sugar foods between meals. It is important however that the three meals provided to prisoners contain all the vitamins and minerals that are needed for good health as snack foods cannot be relied on to be good sources of these nutrients. 3 The menus suggested here are nutritionally balanced and prisoners who eat from menus similar to these, to appetite, are likely to eat appropriate quantities of energy and nutrients. It is strongly suggested that there needs to be further debate about the energy needs of prisoners who may be less active than the general population. In addition some prisoners may have increased needs for some micronutrients. There currently remains insufficient evidence on the requirements of prison populations to recommend intakes that differ from current reference nutrient intakes. 5.3 Breakfast It is recommended here that prisoners should receive 20% of their energy and nutrient needs at breakfast. This may be difficult to achieve if the current system of breakfast packs used in some establishments continues since this means that the choice of food and drink items available is severely limited. Example breakfasts which provide 20% of daily energy and nutrient needs are included on page 13 and prison caterers, prison staff, Governors and prisoners themselves may wish to discuss the practical implications of supplying prisoners with more energy and nutrients at breakfast. 5.4 Ethnic and cultural food choices It is likely that the prison catering service will be required to offer food suitable for a number of different ethnic and minority groups. The food customs typically observed by different groups are shown in Appendix 3, but caterers should be aware that individuals may have requirements different to these. It is important that prison caterers respect the food habits and choices of different groups and understand the importance of keeping cooking pans and utensils separate and using appropriate ingredients in mixed meals. For example, care should be taken when using stock products that they do not contain animal ingredients that cannot be eaten by some groups or that animal fats or gelatine are not present in purchased foods when these are unacceptable. 5.5 Fluid intakes It is important that everyone has access to adequate fluid intakes throughout the day. In climates such as the UK, we should drink approximately 1.2 litres (6 to 8 glasses) 4 of fluid every day to stop us getting dehydrated. In hotter climates the body needs more than this. We get some fluid from the food we eat but it is important that fluids are not restricted since dehydration can lead to headaches, confusion and irritability and lack of concentration as well as constipation and potentially urinary tract infections. Clean, chilled water should always be available with meals and between meals. 5 Table 5.1 Nutrient based guidelines for food served to male and female prisoners Dietary reference value (DRV) Men 19-74 years Women 19-74 years kcals MJ EAR 2515 10.6 1930 8.1 Fat g No more than 35% of energy MAX 98 75 Saturated fat g No more than 11% of energy MAX 31 24 Total carbohydrate g At least 50% of energy MIN 335 257 g No more than 11% of energy MAX 74 57 g DRV MIN 18 18 Protein g RNI MIN 55 45 Vitamin A µg RNI MIN 700 600 Vitamin D µg RNI MIN -1 -1 Vitamin C mg RNI MIN 40 40 Folate μg RNI MIN 200 200 Calcium mg RNI MIN 700 700 Iron mg RNI MIN 9 15 Zinc mg RNI MIN 9.5 7 Sodium mg 2400 2400 6 6 Energy Non-milk extrinsic sugars Fibre Salt g SACN recommendation SACN recommendation MAX MAX EAR = Estimated Average Requirement For explanation of terms see Appendix 1 RNI = Reference Nutrient Intake 1 Vitamin D It is difficult for adults to get the vitamin D they require through the diet and most adults will also make Vitamin D on exposure of the skin to sunlight during the summer months. Adults who rarely go outside or who go outside infrequently and who wear clothing which means their skin is not exposed to the sun are likely to require vitamin D supplements. 6 5.6 Food based guidance for menu planners The following pages contain some information for caterers about food groups and how to choose foods which will contribute to a healthy balanced diet. It is also useful for caterers to look at food labels on foods and ingredients they buy or use and to choose those that are lower in salt, sugar and fat. The Food Standard’s Agency provides information on what is ‘a lot’ of salt, sugar and fat in foods and these are outlined below. Foods high in salt have 1.25 grams or more salt per 100grams or 500 milligrams of sodium per 100 grams of food Foods high in sugar have 10 grams or more of sugars per 100 grams of food Foods high in fat have 20 grams or more of fat per 100 grams of food Foods high in saturated fat have 5 grams of saturated fat or more per 100 grams of food For more information about nutritional information on food labels see www.eatwell.gov.uk Additional information about foods which are good sources of some of the nutrients which appear to be insufficient in the diets of some people in the UK can be found in Appendix 2. 7 5.7 Food-based guidelines for caterers preparing food for prisons Food Group Guidance Rationale What’s Included Bread, other cereals and potatoes Starchy foods should make up a third of the daily diet. Starchy foods are a good source of energy and the main source of a range of nutrients in the diet. As well as starch, these foods supply fibre, calcium iron and B vitamins. All varieties of bread including wholemeal, granary, seeded, chapattis, bagels, roti, tortillas, pitta bread A variety of breads should be available daily at every meal Different starchy foods should be offered in main meals throughout the week so that a variety of starchy foods are included. Aim to include pasta and rice on the menu once a week Potatoes, yam, sweet potato, plantain, cocoyam, dasheen, breadfruit, cassava Breakfast cereals Rice, couscous, bulgar wheat, maize (polenta), cornmeal Noodles, spaghetti and other pastas Wholegrain and wholemeal cereal foods are a good source of fibre and other nutrients Tips • • • • • • • • • Serve more pasta and rice and use less sauce. Opt for tomato based sauces instead of cheese-based to reduce fat content. When serving rice and pasta, try to use wholemeal, wholegrain, brown or high fibre versions. Some breakfast cereals are nutrient fortified (have added iron, folic acid and other vitamins and minerals). Choose wholegrain cereals or mix some in with other cereals. Offer a variety of breads, such as seeded, wholegrain and granary and use thicker slices with low-fat options for fillings. Large pieces of potato and thick or straight cut chips absorb less fat. Boil potatoes in the minimum amount of water and for the shortest amount of time to retain vitamins. Use herbs or other shredded vegetables to add colour and flavour to baked potatoes, rather than butter or margarine. If you look after young people who have allergies to wheat, oats, barley and rye: good alternatives to offer are foods made from maize (e.g. polenta), rice, rice flour, potatoes, potato flour, buckwheat, sago, tapioca, soya and soya flour. Cereal foods which are good sources of iron and zinc include fortified cereals, whole grain cereals, wholemeal bread and flour, couscous and wholemeal pasta. 8 Food Group Guidance Rationale What’s Included Fruit and Vegetables Fruit and vegetables should make up about a third of the daily diet. Fruit and vegetables are good sources of many vitamins and minerals. All types of fresh, frozen and tinned vegetables i.e. broccoli, Brussels sprouts, cabbage, carrots, frozen peas, peppers, swede, sweetcorn It’s important to offer a variety. Five-a-day is an achievable target. Aim for one or two portions with each meal and offer fruit and vegetables as snacks. One portion s about 80g fresh fruit and vegetables and 40g of dried fruit Beans and pulses are included but only count as a maximum of 1 portion per day A glass of 100% fruit juice can count as one portion of fruit each day There is evidence that consuming 400g a day or more of fruit and vegetables reduces the risk of developing chronic diseases such as coronary heart disease and some cancers. Including fruits and vegetables in the diet will help to increase the intake of fibre and can help to reduce the total amount of calories consumed among those who may wish to lose weight All types of salad vegetables including lettuce, cucumber, tomato, raw carrots, peppers, beetroot All types of fresh fruit e.g. apples, bananas, kiwi fruit, oranges, pears, mango, plums All types of tinned fruit in fruit juice e.g. pineapple, peaches, mandarin oranges Stewed fruit Dried Fruit Fruit juice (100% juice) Tips • • • • • • • • • • • • • • • • Avoid adding fat or rich sauces to vegetables or sugar or syrupy dressings to fruit. Steaming or cooking vegetables with minimum amounts of water and serving as soon as possible will help retain vitamins. Use fresh fruit and vegetables as soon as possible, rather than storing, to avoid vitamin loss. Incorporate fruit and vegetables in snack options. Offer a variety of healthy snack alternatives. Add vegetable and pulses to curry, casserole or stir-fry and serve at least two types of vegetables with fish, chicken or meat. Baked beans (as a vegetable) should be served a maximum of twice a week. Encourage a daily glass of fruit juice (100% juice, unsweetened) with meals. Choose tinned fruit in fruit juice not in syrup. Add a handful of dried fruit to cereal options and porridge. Supply a good combination of traditional salads and raw vegetables, fruits and nuts to increase colour, taste and texture at meal times. Add additional vegetables to savoury dishes. Vegetable soups are a useful way of increasing vegetable intake. Avoid dried fruit with added sugar or vegetable oil. Fruit and vegetables which are useful sources of iron include spinach, broccoli, spring greens, dried apricots, raisins, baked beans, broad beans and blackcurrants. Fruit and vegetables which are useful sources of folate include spinach, broccoli, peas, oranges, melon, green leafy salads and tomatoes. Fruit and vegetables which are useful non-dairy sources of calcium include green leafy vegetables, dried fruit and oranges. 9 Food Group Guidance Rationale What’s Included Milk and Dairy Products Offer dairy foods such as milk, yoghurt and cheese as part of meals and snacks Milk and dairy products are excellent sources of calcium, protein, vitamin A and vitamin D. Calcium helps to contribute to good bone health Skimmed, semi-skimmed, whole milk Offer low fat options such as semiskimmed milk, low fat yoghurt and skimmed milk cheeses The fat content of different dairy products varies and much of this is saturated fat. Dried milk, goats and sheep’s milk All types of cheeses e.g. Cheddar cheese, cottage cheese, cheese spreads, Brie, feta, Edam, goats cheese, stilton, parmesan Yoghurt Fromage frais Do not rely on cheese as the main protein item for vegetarians. Where no other option is available, cheese served as a sandwich filler should be offered no more than twice per week. Tips • • • • • • • • • • Try using very strong-tasting cheese (mature cheddar, blue cheese) if using to flavour dishes or sauces, because less will be required. Choose reduced-fat hard cheeses, cottage cheese and skimmed milk soft cheese. Offer semi-skimmed or skimmed milk and low-fat yoghurts and fromage frais. Use plain yoghurt and fromage frais instead of cream, soured cream or crème fraiche in recipes Try serving frozen yoghurts as an alternative to ice cream. It is worth highlighting that some dairy product can contain high salt levels. Look for lower salt cheeses and use smaller amounts of stronger cheese. Dairy foods are very important during pregnancy, but unpasteurised dairy produce and softmould-ripened cheese (e.g. Camembert, Brie and all blue-veined cheese) should be avoided For those on dairy free diets serve soya drinks fortified with calcium as an alternative. Fresh fruit milkshakes and chilled milk drinks can be offered as snacks Restrict sweetened milk drinks to mealtimes as the sugars in these drinks can damage teeth 10 Food Group Guidance Rationale What’s Included Meat, fish and meat alternatives Offer a meat or alternative at all main meals Meat and meat alternatives are a good source of protein, vitamins and minerals such as iron and zinc Use lean meat (which has a fat content of about 10%) Some meat and meat products can have a high fat and saturated fat content Meat includes all cuts of beef, pork, lamb, poultry, offal1 and meat products such as bacon, sausages, beef burgers, pies and cold meats Fish should be offered at least twice per week. White fish is low in fat It is strongly recommended that oily fish such as salmon, trout, mackerel, herring, pilchards, sardines should be served once a week Oil-rich fish provides a good source of omega-3 fatty acids, which may help to protect against heart disease. Oil-rich fish are also a source of vitamins A and D. Eggs can be served at breakfast and as part of main meals Eggs are a good source of protein, vitamin A, vitamin D and some minerals Beans, pulses, eggs, meat alternatives and nuts all provide good sources of nutrients. Ensure meat alternatives for vegetarians are varied Fish includes fresh, frozen and tinned fish, such as tuna and sardines, Fish products such as fish cakes and fish fingers may have a low fish content Boiled, poached, scrambled eggs, omelettes Beans and pulses such as chick peas, lentils, kidney beans, butter beans, textured vegetable protein, nuts, soya products such as tofu, quorn Tips Always select the leanest cuts of meat and remove visible fat and poultry skin. Roast meat on a rack in order to let the fat run off. Grill, poach or bake meat rather than frying. If you do fry, use clean oil and at the correct temperature to minimise absorption. Note that larger pieces of fish and meat absorb less fat. • Do not add extra fat or oil when cooking meat. • Use more vegetables, pulses and starchy food to extend dishes further, as well as add more texture and flavour. Less meat is also required, reducing the fat content and the cost of the meal. • Buy good quality meat and use smaller amounts. • Use fish from sustainable fish stocks. • Offer unsalted nuts and seeds as snacks. • Reduce the amount of processed meat products served such as meat pies and pasties, coated, canned and composite meat products such as sausages, burgers, coated chicken products. • Reduce the amount of processed fish products on offer, particularly those that are fried or coated such as fish fingers or fish cakes. 1 Liver and liver pâté are very rich in vitamin A and it is recommended that these foods are consumed no more than once a week. • • • 11 Food Group Guidance Rationale What’s Included Foods containing fat and foods and drinks containing sugar These foods can add palatability to the diet but should be eaten in small amounts each day Foods containing fat and foods containing sugar often provide a lot of calories and a lower proportion of other nutrients. Foods containing fat include: Reduce the amount of foods containing visible fat for example, margarine and butter, cooking oils and mayonnaise. Other foods containing fat such as cakes and biscuits should be eaten occasionally Foods and drinks containing sugar often contain few other nutrients and frequent consumption between meals can contribute to tooth decay Some foods in this group are also high in sodium/salt Butter, margarine, other spreading fats and low fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, gravies. Foods and drinks containing sugar include: Soft drinks, sweets, chocolate, jams, sugar, cakes, puddings, biscuits, pastries and ice cream Tips • • • • • • • • • • • Use mono- or poly-unsaturated fat spreads. Use cooking oils high in monounsaturates such as soya, rapeseed or olive oils. Avoid serving pastry dishes frequently. Measure oil for cooking carefully and reduce oil used in the preparation of soups, stews and casseroles. Vegetables can often be dry fried, steamed or stewed to form the basis of sauces and other dishes. Use low-fat yoghurt or non-dairy ice cream to compliment puddings or pies. Produce puddings lower in fat and sugar and incorporate fresh, tinned fruit in juice or dried fruit. Offer water, unsweetened fruit juices and chilled milk drinks. Serve wholegrain or plain cereals rather than sugar coated cereals. Provide currant buns, fruit bread, melon slices, malt loaf and other lower fat bread based foods as alternatives to cakes and biscuits. When preparing sandwiches, try and avoid using butter or spreads if the filling is already moist. Consider using reduced-fat spreads and opt for types that are soft straight from the fridge, so it is easier to spread thinly. To increase the amount of dietary VITAMIN D in menus • • • • • Use margarine fortified with vitamin D for baking and as a fat spread. Include an oily fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 5-14µg of vitamin D per 100g. Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. Meat and poultry contribute small but significant amounts of vitamin D. 12 5.8 Example breakfast menus for male and female prisoners Example male breakfast Example female breakfast Carton of semi-skimmed milk (200ml) 1 piece fresh fruit (banana, apple or orange) (108g) 1 low fat fruit yoghurt (125g) 1 brown bread roll (65g) with polyunsaturated spread (7g) 43g dried fruit mix (apricots, dates, raisins) Drinking water Semi-skimmed milk (100ml) 1 piece fresh fruit (banana, apple or orange) (40g) 1 low fat fruit yoghurt (125g) 1 brown bread roll (48g) with low fat spread (7g) 40g dried fruit mix (apricots, raisins, prunes) Drinking water Nutrient Males Females Guidance (20% energy and nutrients) Menu analysis Guidance (20% energy and nutrients) Menu analysis 503 2.1 8 386 1.6 15 386 1.6 8 Energy kcals MJ Fat g MAX 503 2.1 20 Saturated fat g MAX 6 3 5 3 Carbohydrate g MIN 67 91 51 68 Non milk extrinsic sugars g MAX 15 8 11 8 Fibre g MIN 4 8 4 5 Protein g MIN 11 21 9 15 Vitamin A μg MIN 140 92 120 88 Vitamin C mg MIN 8 31 8 12 Folate ug MIN 40 98 40 66 Calcium mg MIN 140 597 140 423 Iron mg MIN 2 3 3 3 Zinc mg MIN 2 2.9 1 2 Sodium mg MAX 480 427 480 430 Salt g MAX 1.2 1.1 1.2 1.1 13 5.9 Example weekly menu for male prisoners (v) Suitable for Vegetarians Lunch 1 v) Chickpea curry (100g) with spiced vegetable pilau (320g), Punjabi M . courgette (80g), naan bread (80g) O N D 2 Shepherd’s pie (300g) with gravy (70g)* A . Y 3 Cottage pie (300g) with gravy (70g)* . 4 (v) Butter bean and vegetable pie . (250g)* Tea 1 Oriental chicken curried rice (280g) with . egg noodles (150g) 2 (v) Cauliflower gratin* (250g) . 3 (v) Macaroni cheese* (250g) . 4 Corned beef hash* (245g) . *options served with potato dice (200g) - all options served with broccoli florets (80g), and wholemeal roll (48g) or French bread ( 60g) with low fat margarine (7g) * options served with extra mashed potatoes (80g) , broccoli florets (80g) and choice of bread roll with soft vegetable margarine (60g) Oat biscuits (60g) or, banana and chocolate brownie (60g) Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) Spotted dick (170g) with custard (150g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) T U E S D A Y 1 . Tanzanian coconut fish curry (250g), with rice (180g), plantain (100g) and flat bread (50g) 2 . Fish Pie (250g) with extra mashed potatoes (80g)* French beans (80g) 3 . (v) Courgette and cheese bake (250g), couscous (150g) and tomatoes stuffed with rice(120g)* 4 . (v) Potato & broccoli bake (280g)* French beans (80g) *options with choice of bread roll with soft vegetable margarine (60g) Chocolate fudge pudding (170g) custard (150g), or choice of fresh fruit apple (100g), banana (100g) or orange(120g) 14 1 . 2 . 3 . 4 . (v) Chickpea rissoles (250g) (v) Pasta Provencal (300g) Chicken and broccoli lasagne (280g) Salmon quiche (130g) -all options served with green salad (50g) or ratatouille (100g), and baby jacket potatoes (200g) or mashed potatoes (200g) Wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) Banana tea bread (60g) or Bakewell tart (55g) low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) W E D N E S D A Y 1 . Chicken biryani (350g) lentil dahl (175g), mixed vegetable curry (100g), and chapatti (55g) 2 . 3 . 4 . Chicken curry with pineapple (320g)* (v) Caribbean casserole (250g)*, Pork with apricot sauce (300g)* *options served with rice (180g), diced mixed vegetables (80g) and choice of bread roll with soft vegetable margarine (60g) Crème caramel (100g) or choice of fresh fruit - apple (100g), banana (100g) or orange (120g) T H U R S D A Y F R I D A Y 1 . African beef and bean stew (250g), African dumplings (80g), rice (180g) & sweet potato (100g) 2 . Steak Hotpot (300g) Boiled potatoes (150g) * 3 . (v) Crunchy vegetable crumble (300g), Jacket wedges (180g)* 4 . Savoury pork and vegetable pie (250g) and Gravy (70g) Boiled potatoes (150g) * 1 Beef curry (280g) with spiced vegetable . pilau (300g) 2 (v) Sweetcorn & pasta bake (280g)* . 3 Kedgeree (250g)* . 4 Scotch egg (120g)* . *options served with jacket potato (200g), green salad (50g), and mixed bean salad (100g) Wholemeal roll (48g) or French bread (60g), with low fat margarine (7g) Sultana sponge cake (55g) or gingerbread (60g) Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1 Caribbean chicken (250g) with egg . noodles (150g) 2 (v) Lentil & tomato quiche (140g)* . 3 (v) Cheese and tomato quiche (130g)* . 4 Pilchards in tomato sauce (165g)* . *options served with Peas (80g) and Choice of bread roll with soft vegetable margarine (60g) *options served with vegetable rice salad (170g), mixed salad (50g) and coleslaw (80g) Wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) Rice pudding with jam (200g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) Apple cake (60g), or fruit flapjack (50g) low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1 . Sardine Curry (250g), rice (180g) & naan bread (80g) 2 . Mackerel Fishcakes (150g), tartare Sauce (10g) oven chips (180g)* 3 . (v) Chickpea burgers (150g) with oven chips (180g) or rice (180g)* 15 1 . 2 . 3 . 4 . South African Bobotie (280g) (v) Broccoli bake (240g) (v) Cauliflower crunch (250g) (v) Sweetcorn & pepper quiche (130g) 4 . (v) Mixed Bean casserole (300g) with oven chips (180g) or rice (180g)* *options served with choice of bread roll with soft vegetable margarine (60g) all options served with spinach bhaji (100g) or green beans (80g) S A T U R D A Y 1 . 2 . Bread & butter pudding (170g) and Custard (150g) or Choice of fresh fruit - Apple (100g), Banana (100g) or Orange(120g) Lamb keema (320g), spinach curry (80g), brown rice (180g) & chapatti (55g) Pasta (300g) with bolognese sauce* (200g) 3 . (v) Pasta (300g) with creamy mushroom Sauce* (150g) 4 . Pasta shells with tuna and tomato sauce* (380g) 1 . Apricot cereal bars (40g) or carrot cake (60g) or low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1 (v) Vegetable and bean curry (300g . raita (35g) and basmati rice (200g) 2 (v) Mushroom omelette (140g) with . oven chips (200g) 3 Salmon fishcakes(150g) with oven . chips (200g) Served with mixed salad (50g) & garlic bread (55g) S U N D A Y -all options served with mixed salad (50g) and boiled new potatoes (200 g) or curried rice salad (180g) Wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) Queen of puddings (140g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) Chicken bhuna (320g), okra (80g) & basmati rice (180g), naan bread (80g) 2 . Roast chicken and chipolatas with gravy (190g), stuffing (40g), roast potatoes (180g) and cabbage (80g) 3 . 4 . (v) Crispy vegetable bake (300g),* (v) Sweetcorn and mushroom bake* (300g) *options served with jacket wedges (180g), cabbage (80g) and choice of bread roll with soft vegetable margarine (60g) Apple crumble (170g) with custard (150g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 4 Chicken and prawn paella (240g) . - all options served with peas (80g) wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) Fruit loaf (50g) or chocolate cake (50g) low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1 Oriental beef stir fry (250g) . 2 (v) Mushroom stroganoff (200g) . 3 (v) Spanish omelette (140g) . 4 (v) Vegetable lasagne (300g) . - all options served with rice (200g) or boiled new potatoes (200g) and green beans (80g), or carrot apple and sultana salad (110g) Wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) Date square (40g) or iced sponge (60g) Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) Choice of bread rolls from wholemeal, soft white, crusty white & granary rolls 16 5.10 Analysis of example menu for male prisoners compared with nutrient based guidance Nutrient based guideline 40% energy and other nutrients Energy Kcals MJ g Max Saturated fat g Max Total carbohydrate g Min Non milk extrinsic sugars g Fibre g Min Protein g Min Vitamin A µg Min Vitamin C mg Min Folate µg Min Calcium mg Min Iron mg Min Zinc mg Min Sodium mg Max g Max Fat Salt1 Lunch Tea 1006 4.2 1006 4.2 1006 4.2 39 30 31 12 9 10 134 145 155 30 12 18 7 11 11 22 40 37 280 684 425 16 51 69 80 163 245 280 418 444 4 7 6.5 4 5.2 4.8 960 922 960 2.4 2.4 2.4 Max 1 The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced 17 5.11 Example weekly menu for female prisoners (v) Suitable for Vegetarians Females lunch 1. v) Chickpea curry (100g) with Vegetable pilau (300g), & Punjabi M courgette (80g), naan bread (80g) O N D 2. Shepherd’s pie (300g) with Gravy (65g)* A Y 3. Cottage pie (300g) with Gravy (70g)* Females Tea 1. Oriental chicken curried rice (200g) with egg noodles (120g) 2. (v) Cauliflower gratin* (180g) 3. (v) Macaroni cheese* (180g) 4. Corned beef hash* (220g) 4. (v) Butter bean & vegetable pie (250g)* options served with broccoli florets (80g) and choice of bread roll with soft vegetable margarine (60g) Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) T U E S D A Y 1. Tanzanian coconut fish curry (250g), with rice (100g), plantain (100g) and flat bread (50g) *options served with potato dice (100g) - all options served with broccoli florets (80g), and wholemeal roll (48g) or French bread ( 60g) with low fat margarine (7g) Rock bun (40g) Mixed dried fruit selection of apricots, raisins & dates (40g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1. (v) Chickpea fritters (150g) 2. (v) Lentil & mushroom crumble (200g) 2. Fish Pie (250g) French beans (80g)* 3. (v) Courgette & cheese bake (250g), couscous (150g) & tomatoes stuffed with rice(120g)* 4. (v) Potato & broccoli bake (250g) French beans (80g)* *Options served with choice of bread roll with soft vegetable margarine (60g) Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 18 3. Chicken and broccoli lasagne (180g) 4. Salmon quiche (120g) -all options served with green salad (50g) or ratatouille (100g), and baby jacket potatoes (100g) or mashed potatoes (100g) Wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) Sponge cake (40g) Mixed dried fruit selection of apricots, raisins & dates (40g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1. Ismaili chicken biryani (280g), lentil dahl (160g), mixed vegetable curry W (100g), and chapatti (55g) E D N 2. Chicken curry with pineapple (280g)* E S D 3. (v) Caribbean casserole (250g)* A Y 4. Pork with apricot sauce (280g)* 1. Beef and banana curry (250g) with spiced vegetable pilau (150g) 2. 3. Kedgeree (200g)* 4. Scotch egg (120g)* *options served with jacket potato (100g), green salad (50g), and mixed bean salad (100g) Wholemeal roll (48g) or French bread (60g), with low fat margarine (7g) *options served with rice (100g), diced mixed vegetables (80g) and choice of bread roll with soft vegetable margarine (60g) Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) T H U R S D A Y 1. African beef and bean stew (250g), African dumplings (80g), rice (105g) & sweet potato (100g) Apricot oat bars (40g) Mixed dried fruit selection of apricots, raisins & dates (40g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1. Caribbean chicken (200g) with egg noodles (120g) 2. (v) Lentil & tomato quiche (120g)* 2. Steak Hotpot (280g)* 3. (v) Broccoli quiche (120g)* 3. (v) Crunchy vegetable crumble (250g), jacket wedges (150g)* 4. Pilchards in tomato sauce (110g)* 4. Savoury pork and vegetable pie (250g) and gravy (65g)* *options served with vegetable rice salad (100g), mixed salad (50g) and coleslaw (80g) Wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) *options served with boiled potatoes (100g) & peas (80g) and choice of bread roll with soft vegetable margarine (60g) Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) F R I D A Y (v) Sweetcorn & pasta bake(250g)* 1. Sardine Curry (250g), rice (105g) & naan bread (80g) Gingerbread (45g) Mixed dried fruit selection of apricots, raisins & dates (40g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1. South African Bobotie (230g) 2. 2. Mackerel fishcakes (150g), tartare Sauce (10g) oven chips (120g)* 3. (v) Cauliflower crunch (200g) 4. 3. (v) Chickpea fritters (150g) with oven chips (120g) or rice (100g)* (v) Broccoli bake (200g) (v) Sweetcorn & pepper quiche (120g) -all options served with mixed salad (50g) and boiled new potatoes (100 g) or curried rice salad (100g) 4. (v) Mixed Bean casserole (280g) with oven chips (120g) or rice 19 Wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) (100g)* *options served with choice of bread roll with soft vegetable margarine (60g) - all options served with spinach bhaji (100g) or green beans (80g) S A T U R D A Y Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1. Lamb keema (250g), spinach curry (80g), brown rice (105g) & chapatti (55g) Fruit loaf (50g) Mixed dried fruit selection of apricots, raisins & dates (40g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1. (v) Vegetable and bean curry (200g) raita (35g) and basmati rice (100g) 2. 2. Pasta (150g) with bolognese Sauce* (180g) (v) Mushroom rice omelette (140g) with oven chips (100g) 3. Salmon fishcakes(120g) with oven chips (100g) 3. (v) Pasta (150g) with creamy mushroom Sauce* (150g) 4. Chicken and prawn paella (200g) 4. Pasta shells with tuna and tomato sauce* (350g) -all options served with spinach (80g) wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) options served with mixed salad (50g) & garlic bread (55g) Low fat fruit yoghurt (125g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) S U N D A Y 1. Chicken bhuna (250g), okra (80g) & basmati rice (100g), naan bread (80g) 2. Roast Chicken and chipolatas with gravy (190g), stuffing (40g), roast potatoes (100g) and cabbage (80g) Fairy cake (30g) Mixed dried fruit selection of apricots, raisins & dates (40g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 1. Oriental beef stir fry (200g) 2. (v) Moroccan spicy lamb (180g) 3. (v) Spanish omelette (130g) 4. (v) Vegetable lasagne (180g) 3. (v) Crispy vegetable bake (250g)* 4. (v) Sweetcorn and mushroom bake (280g)* *options served with jacket wedges (100g), cabbage (80g) and choice of bread roll with soft vegetable margarine (60g) Apple crumble (170g) with custard (145g) or choice of fresh fruit apple (100g), banana (100g) or orange(120g) 20 - all options served with rice (100g) or boiled new potatoes (100g) and green beans (80g), or carrot apple and sultana salad (100g) Wholemeal roll (48g) or French bread (60g) with low fat margarine (7g) Fruit scone (40g) Mixed dried fruit selection of apricots, raisins & dates (40g) or choice of fresh fruit - apple (100g), banana (100g) or orange(120g) 5.12 Analysis of example menu for female prisoners compared with nutrient based guidance Nutritional Guideline 40% energy and other nutrients Energy Lunch Tea 772 772 772 Kcals MJ g Max 30 23 23. Saturated fat g Max 10 7 7 Total carbohydrate g Min 103 105 120 Non milk extrinsic sugars g Max 23 5 8 Fibre g Min 7 9 10 Protein g Min 18 34 28 Vitamin A µg Min 240 612 483 Vitamin C mg Min 16 46 54 Folate µg Min 80 142 198 Calcium mg Min 280 361 324 Iron mg Min 6 6 6 Zinc mg Min 3 4.3 3.6 Sodium mg Max 960 763 876 g Max 2.4 2.0 2.2 Fat Salt1 1 The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced 21 6.0 Nutritional guidelines for food served to older people in residential care 6.1 Background There are approximately 410,000 people living in residential and nursing homes across the UK 1 . A quarter of people aged over 85 years live in a residential or nursing home or long-stay hospital environment and the population in these settings are increasingly old and frail 2 . While this population is increasingly dependent on care of both a personal and practical nature, there remains evidence that many older people living in residential accommodation are undernourished2. It has been estimated that about a half of all older people in residential care may have some form of dementia2 and it is known that dementia will often impact on a person’s ability to eat and drink well. In England, Wales and Northern Ireland, the 2002 National Minimum Standards for Care Homes for Older People 3 provided new standards for all aspects of care, including issues around food and drink, and the standards demand that residents ‘should receive a wholesome, appealing, balanced diet in pleasing surroundings at times convenient to them’. Guidance on how this can be achieved is outlined in nine individual standards that cover aspects such as nutritional screening, timing of meals and snacks, having sufficient staff are available to help ensure food standards are met, and some meal-specific standards. Older people in residential care should be offered three full meals each day, at least one of which must be cooked, as well as snack meals as appropriate. Similar care standards 4 are also available for Scotland as part of the Regulation of Care Scotland Act (2001). A recent report by the Care Standards Commission, Highlight of the Day?, 5 outlined some of the issues about food that older people in care homes still face. This research, collected in 2005, reported that while 83% of care homes met the requirements of meals and mealtime standards, a significant proportion did not, with one in six homes requiring improvement in how food is cooked and served to residents. The most common themes for complaint about food in care homes were 1 Office of Fair Trading 2005. Care Homes for Older People in the UK. Accessed from: www.oft.gov.uk 2 Caroline Walker Trust 2003. Eating Well for Older People. CWT. www.cwt.org.uk 3 Department of Health 2002. Care Homes for Older People: National Minimum Standards. London. TSO. 4 National Care Standards for Scotland. Accessed from: www.scotland.gov.uk/library3/social/chop.pdf 5 Commission for Social Care Inspection 2006. Highlight of the Day? Improving Meals for Older People in Care Homes. Accessed from: http://www.csci.org.uk/PDF/highlight_of_day.pdf 1 the quality of food, the choice and the availability. It was reported, both in the Care Standards Commission report and elsewhere, that for older people food remains a priority among the factors they associate with good personal care and, for people over 85 years of age food has been ranked as the most important part of the personal care they receive 6 . The importance of good food and good nutrition for older people has been well established and it has been reported that the diets of older people in residential care are often low in folate, riboflavin, vitamin C, vitamin D, iron, zinc and potassium.2 In addition the diets of older people are often high in salt, and intakes of fruits and vegetables are frequently poor. It is therefore essential that the food provided in residential care accommodation for older people provides adequate nutrition in food that is accessible and well liked. Smaller appetites are likely to require nutrient-dense meals which ensure that all the essential nutrients are included without unnecessary bulk. 6.2 Rationale for nutrient-based guidelines for food prepared for older people in residential care The food provided for older people in residential care should as a minimum provide the average dietary reference values for energy and nutrients specified for people aged 75 years and over 7 . It should be stressed however that some older people may have higher requirements for energy and nutrients. The nutrient-based guidelines in this report provide guidance for menu planners on the amounts of energy and nutrients that they should aim to provide for a group of older people in their care, while remembering that this is a vulnerable population group who are frequently found to eat and drink too little. The needs of each resident should be assessed as part of his or her care plan and meals and snacks organised to ensure that each individual is able to access sufficient nutrients each day. Monitoring nutritional status (e.g. whether a person loses weight) is an important part of the care of older people and this will indicate when specialist help may be needed to help someone eat and drink appropriately. Details of a tool for monitoring nutritional status of older people in 6 Personal Services Research Unit 2002. OPUS: A Measure of Social Care Outcome for Older People. Accessed from: www.ukc.ac.uk/PSSRU 7 Department of Health 1991. Dietary Reference Values for Food Energy and Nutrients for the United Kingdom. Report on Health and Social Subjects 41. HMSO. London 2 residential care (The Malnutrition Universal Screening Tool – MUST) can be found on the BAPEN website. 8 The nutrient-based guidelines in section 6.3 assume that older people will receive three meals and two snacks each day as well as a milky drink in the evening. The guidelines do not specify the proportion of energy and other nutrients to be provided by individual meals and snacks, since the eating patterns of older people may vary considerably depending on appetite and eating ability. The foods and drinks offered each day should meet the total nutritional guidance outlined. The sample menus on pages 13-14 show the sorts of foods that would be required across the day to do this. Where there are eating difficulties or the texture of food needs to be altered, it is important that appropriate advice is taken to ensure that residents receive adequate nutrition at both meals and snacks. Vitamin D It is impossible for most older adults to obtain the full daily requirement of 10 micrograms of vitamin D from the diet alone. It is likely that older adults in residential accommodation who rarely go outside will need vitamin D supplements.4 They should seek medical advice about this. Good dietary sources of vitamin D are outlined in the food-based guidelines for older people in residential care in section 6.3 Folate and vitamin C The low intakes of folate and vitamin C among older people 9 may be due in part to reduced intakes of fruit and vegetables, since some older people may find it difficult to peel, cut up or chew these foods. Caterers should be aware of the importance of increasing fruits and vegetables in menus and offer a variety of raw and cooked fruits and vegetables in accessible forms. Iron and zinc Low iron intakes and low iron status have been reported among older people in residential care 10 and this may be due both to poorer iron absorption, greater iron 8 http://www.bapen.org.uk/the-must.htm 9 Finch S, Doyle W, Lowe C, Bates CJ et al. 1998. National Diet and Nutrition Survey: People Aged 65 Years and Over. Volume 1: Report of the Diet and Nutrition Survey. TSO. London. 10 Finch S, Doyle W, Lowe C, Bates CJ et al. 1998. National Diet and Nutrition Survey: People Aged 65 Years and Over. Volume 1: Report of the Diet and Nutrition Survey. TSO. London. 3 losses and lower iron intakes 11 . Meat is a good source of iron but as people get older they may find it more difficult to chew and therefore it is important that foods high in iron are included in the menu in forms that are easy for older people to access. Zinc intakes are also often low in the diets of older people and many good sources of iron are also good sources of zinc. Good sources of nutrients are outlined in Appendix 2. Salt/sodium The current recommendation for salt intakes for all adults is 6g a day3 and the current daily intake by adults is approximately 9g. Older people may be used to adding salt to food out of habit, or they may have a reduced sense of taste and smell and therefore add salt to food to give it taste, or they may prefer highly salted foods and condiments that they typically ate when younger. Caterers in residential care accommodation should respect the food choices of those they cater for but attempt to reduce the use of highly salted foods and salt in cooking, while ensuring that food remains tasty. Fluid Intakes A regular and adequate intake of fluids is extremely important for older people. It helps to prevent dehydration which can lead to confused states; helps to prevent and alleviate the symptoms of constipation and fluids can also provide important nutrients when appetites are small. It is recommended that older people drink at least 1.5 litres or 8 cups of non-alcoholic fluid a day11. Many older people may find they are less likely to recognise that they are thirsty or may be afraid of drinking because of fears of incontinence. It is important to explain to older people the importance of drinking and that more fluid, rather than less, can help with incontinence. The fluid older people require can be consumed in a number of ways, and some fluids may offer additional nutritional or psychological benefits to older people. Tea and coffee are sociable drinks which many older people habitually drink and enjoy. These should be offered regularly, and served in the style that the older person prefers. Some older people may enjoy milky coffee or tea or another hot beverage such as a malted or chocolate milk drink particularly at bedtime. Fruit juice should be offered at meals as the vitamin C it contains may help the absorption of iron from some foods. Clean, 11 Caroline Walker Trust 2003. Eating Well for Older People. CWT. www.cwt.org.uk 4 chilled water should be freely available and offered regularly as an additional option. Some foods can also provide fluid: older people may enjoy frozen drinks if the weather is warm and nutritious soup can be offered at meals and snacks. It is important that all those who care for older people in residential care works with the older person to ensure that they have access to at least 1.5 litres or 8 cups of fluid during the day, of the type that the older person enjoys. As older people may not recognise that they are thirsty it is important that drinks are offered, served and encouraged: provision of fluid alone e.g. water coolers in community areas, will not necessarily encourage fluid intake. 5 Table 6.1 Nutrient based guidelines for food served to older people in residential care Dietary reference value (DRV) Men and women aged 75 years and over kcals MJ EAR Fat g About 35% energy MAX 76 Saturated fat g About 11% of energy MAX 24 Total carbohydrate g About 50% of energy MIN 260 Non-milk extrinsic sugars g About 11% of energy MAX 57 Fibre g RNI MIN 18 Protein g RNI MIN 50 Vitamin A μg RNI MIN 700 μg RNI MIN 10 Vitamin C mg RNI MIN 40 Folate μg RNI MIN 200 Calcium mg RNI MIN 700 Iron mg RNI MIN 9 Zinc mg RNI MIN 9.5 Sodium mg SACN recommendation MAX 2,400 g SACN recommendation MAX 6 Energy Vitamin D1 Salt 1955 8.2 EAR = Estimated Average Requirement DRV = Dietary Reference Value RNI = Reference Nutrient Intake For an explanation of these terms see Appendix 1. 1 Vitamin D It is impossible for most older adults to obtain the full daily requirement of 10 micrograms of vitamin D from the diet alone. It is very likely that older adults who live in residential accommodation will need vitamin D supplements. 6 6.3 Food-based guidelines for older people in residential care Below are some food-based guidelines that caterers may find useful in planning menus for older people in their care. Food group Guidance Rationale What’s included Bread, other cereals and potatoes Starchy foods should make up a third of the daily diet. Foods from this group are a good source of energy and the main source of a range of nutrients in the diet. As well as starch, these foods supply fibre, calcium iron and B vitamins. All varieties of bread including wholemeal and granary bread, chapattis and bagels. Older people may prefer white bread, and higher fibre white bread may also be acceptable, A variety of breads should be available daily as starters or meal accompaniments. Offer a variety of starchy foods with main meals including potatoes, rice, pasta, noodles and other grains. Wholegrain cereals are higher in fibre Potatoes, plantain, yam and sweet potato Breakfast cereals Rice, couscous, bulgar wheat, maize, cornmeal Noodles, pasta Tips • • • • • • Older people with small appetites need nutrient-dense meals and, if there is concern about how much someone is eating, starchy foods should be offered in moderate amounts. Avoid very high-fibre cereals unless an older person has a very good appetite. Some white bread has added nutrients and fibre and can be useful for older people who do not like brown or wholemeal bread. Some older people find it easier to chew brown or wholemeal bread if it is lightly toasted. Some breakfast cereals are nutrient-fortified (e.g. they may have added iron, folic acid, vitamin D and other nutrients). These can be good choices for breakfast but look for those with a lower salt content. Boil potatoes in the minimum amount of water and for the shortest amount of time to retain vitamins, but ensure they are cooked until soft. Roast potatoes in small amounts of vegetable oil and use milk to mash potatoes to smoothness. If you have customers who are allergic to wheat, oats, barley or rye, good alternatives are foods made from maize (i.e. polenta), rice, rice flour, potatoes, potato flour, buckwheat, sago, tapioca, soya and soya flour. Seek expert advice from a dietitian where necessary. 7 Food group Guidance Rationale What’s included Fruit and vegetables Fruit and vegetables should make up about a third of the daily diet. Fruit and vegetables are good sources of many vitamins and minerals. All types of fresh, frozen and tinned vegetables – e.g. broccoli, Brussels sprouts, cabbage, carrots, frozen peas, swede, green beans. It’s important to offer at least 5 different fruits and vegetables every day. Aim for 1 or 2 portions with each meal and offer fruit as a snack. A portion of fresh or cooked fruit or vegetables should be about 80g. 1 portion of dried fruit can be about 40g. (Dried fruit only counts once per day.) 1 glass of fruit juice = 1 portion (however much is consumed in a day) There is increasing evidence that consuming more than 400g of fruit and vegetables every day reduces the risk of developing chronic diseases such as coronary heart disease and some cancers. All types of salad vegetables including lettuce, cucumber, tomato, raw carrots, peppers and beetroot. All types of fresh fruit – e.g. apples, bananas, kiwi fruit, oranges, pears, mango and plums. All types of tinned fruit in juice – e.g. pineapple or peaches Stewed fruit Dried fruit Beans and pulses only count as a maximum of 1 portion per day. Fruit juice (100% juice) Tips • • • • • • • • • • • Steaming or cooking vegetables with minimum amounts of water and serving as soon as possible will help retain vitamins. Use fresh fruit and vegetables as soon as possible, rather than storing them, to avoid vitamin loss. Offer fruit as a snack. Older people may find it difficult to peel or cut whole fruit, so a plate of sliced ready prepared fruits may be more acceptable. Add vegetables and pulses to stews, casseroles or other dishes and offer a variety of vegetables at main meals. Baked beans (as a vegetable) should be served a maximum of twice a week. Encourage a daily glass of 100% fruit juice with breakfast or with a main meal. Buy tinned fruit in natural juice rather than in syrup. Offer a variety of dried fruits to add to cereal options and porridge and include dried fruit in cakes and desserts. Pureed stewed fruit can be offered with custard or yoghurt or ice cream as dessert. Fruit and vegetables which are useful sources of folate include spinach, broccoli, peas, oranges, melons, green leafy salads and tomatoes. Fruit and vegetables which are useful sources of iron include green leafy vegetables, peas, broccoli, baked beans, dried apricots and raisins, blackcurrants and broad beans. 8 Food group Guidance Rationale What’s included Milk and dairy products Milk and dairy foods should be served every day. Milk and dairy products are excellent sources of calcium which is needed for optimal bone strength protein, vitamin A, riboflavin and vitamin D. All types of milk. Moderate amounts should be offered 2-3 times a day as milk in drinks, cheese, yoghurt or milkbased puddings and sauces. Dried milk, goat’s and sheep’s milk. Cheeses – e.g. Cheddar, cottage cheese, cheese spreads, brie, feta, Edam, goat’s cheese, stilton, parmesan. Yoghurt (fruit or plain, whole milk or low-fat), or fromage frais. Older people with small appetites who may need to gain weight or who are of low weight should be encouraged to have full-fat milk and yoghurt. Milk-based sauces, custard and milk puddings. Semi-skimmed milk is suitable for older people with good appetites. Tips • • • • • • • • To add extra calories, protein and nutrients to dishes, extra milk, cheese or dried milk powder can be added in cooking. Whole milk can be fortified further by the addition of extra dried skimmed milk powder for those older people who are of low weight or who have small appetites. Offer milky drinks at snacks and before bed. Milkshakes may be an acceptable alternative, particularly in hot weather. Frozen yoghurts can be offered as an alternative to ice cream. Milk can be used in sweet and savoury sauces, custards and puddings. Smooth yoghurt and fromage frais can be offered as a snack and is useful if older people have eating difficulties. It is worth highlighting that some dairy products can contain high salt levels. Strong cheese can impart flavour in smaller amounts. For dairy-free diets, serve soya drinks fortified with calcium as an alternative. 9 Food group Guidance Rationale What’s included Meat, fish and meat alternatives A meat or alternative should be offered at all main meals. Meat is a good source of protein and of vitamins and minerals such as iron and zinc Meat, poultry, offal1, fish, eggs, nuts, beans, pulses and meat alternatives. Fish is an excellent protein source and contains selenium and iodine. Meat includes all cuts of beef, lamb and pork and meat and meat products such as ham, corned beef and sausages. Look for meat products with a high meat content. Red meat should be offered a minimum of twice a week. Use lean meat (with a fat content of about 10%). Fish should be offered at least twice a week. It is strongly recommended that oily fish should be served once a week. Meat alternatives for vegetarians should be varied and use a variety of foods from this group (e.g. eggs, peas, beans and pulses, soy-based meat alternatives, nuts, quorn or tofu). Oil-rich fish provides omega-3 fatty acids which may help to prevent heart disease. Such foods are also a source of vitamins A and D and iron. Beans and pulses are sources of protein, iron and zinc. Eggs are a good source of protein, vitamins A and D Nuts provide a source of protein, iron, fibre, zinc and calcium. Fish includes fresh, frozen and tinned fish, such as tuna, sardines, pilchards and mackerel, and fish products such as fish cakes and fish fingers. Oily fish, such as salmon and sardines. Beans – e.g. baked beans, butter beans, kidney beans and lentils are in this group and provide a good source of protein for vegetarians. Notes • • • • • • • Always select the leanest cuts of meat and remove visible fat and poultry skin. Avoid processed meat and fish products which are high in fat and salt, such as crumb-coated chicken products, burgers, pies, fish cakes and canned meats. These are often high in salt and low in meat content. Customers need to be made aware of nuts and nut products incorporated into dishes. Eggs are a useful source of nutrients but they should always be well cooked for older people. Oil-rich fish can be used in pâtés and spreads on bread and toast. For older people who have difficulty chewing, offer soft lean meat and fish or meat and fish dishes where the meat has been minced or served in a sauce. 1 Liver pâté is a useful source of nutrients for older people but liver and liver products should not be served more than once a week. 10 Food group Guidance Rationale What’s included Foods containing fat and foods and drinks containing sugar These foods add palatability to the diet and can be useful in the diets of older people for encouraging eating and stimulating the appetite. The main nutrients provided by such foods are fat, including some essential fatty acids, and also some fatsoluble vitamins. Foods containing fat include: butter, margarine, other spreading fats and low-fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, and gravies. These foods can be high in calories and offer few other nutrients. If appetites are poor, it is important that these foods do not displace more nutrientrich foods. As for the rest of the population, foods from this group can contribute to excess energy intakes if they are eaten in large amounts. Snacking on sugary foods and drinks throughout the day is discouraged as this can cause tooth decay. Older people may enjoy some sweet foods as snacks, and moderate amounts of these foods are acceptable. Carbohydrate (in the form of sugars) is also provided. Some products also contain salt. Foods containing sugar include: soft drinks, sweets, jams and sugar, as well as foods such as cakes, puddings, biscuits, pastries and ice cream. Tips Use mono- and poly- unsaturated fats wherever possible for cooking, spreading and in dressings. Good choices of cooking and salad dressing fats include soya, rapeseed and olive oils and good choices of fat spread are those made from sunflower oil, soya oil or olive oil. Vitamin D To increase the amount of dietary vitamin D in menus served for older people: • Use margarine fortified with vitamin D for baking and as a fat spread. • Include an oily fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 514µg of vitamin D per 100g. • Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. • Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. • Meat and poultry contribute small but significant amounts of vitamin D. 11 6.4 Example menus for older people in residential care Two example menus are given here which show the sorts, and amounts, of foods and drinks that could be served to meet the nutrient-based and food-based guidelines. A nutritional analysis is provided for each of the menus, showing how the menu compares with the nutritional guidelines. Additional resources for caterers are given in Appendix 4. Further practical guidance on preparing and serving food to older people in residential care are can be found in The Caroline Walker Trust publications Eating Well for Older People and Eating Well for Older People with Dementia, both available from www.cwt.org.uk. 12 6.5 Example weekly menu for older people in residential care (menu 1) Monday Breakfast Midmorning Lunch Tuesday Wednesday Thursday Friday Saturday Sunday Choice of porridge or cereal (i.e. weet bisks, bran flakes, muesli, shredded wheat, puffed wheat) Fresh fruit juice or cranberry juice drink (150g) Scrambled eggs or baked beans or grilled bacon or grilled tomatoes with toast with Polyunsaturated margarine (7g) Tea, coffee Choice of fresh fruit slices (apple, orange and banana (80g)) Tea, coffee or milky drink Pasta Salmon Lamb and Cottage pie Savoury pie Provencale fish potato (180g) (300g) (180g) Peas (80g) Braised rice cakes hotpot Broad Cauliflower (150g) (120g) (210g) Oven Carrot and beans with Celery (80g) (80g) Green beans swede chips baby (80g) (110g) mash carrots Baked (100g) (80g) Spinach beans (80g) (90g) Roast pork apple sauce and gravy(145g Roast potatoes (100g) Courgette (80g) Spring greens (80g) Water and fruit juice available Chicken Fricassee (150g) New potatoes (140g) Broccoli (80g) Midafternoon Chocolate Lemon Apricot Queen of Stewed Raspberry Fruit meringue pudding Conde puddings Plums and apple Compote (90g) with pie (150g) (140g) (90g) and pie (100g) (160g) Custard Cream ice cream (115g) fromage (100g) (40g) (30g) frais (40g) Choice of: apple and sultana cake, banana tea bread, Sultana sponge, fruit scones with butter, sticky prune cake, Madeira cake, lemon cake (average slice (52g)) Tea or coffee or milky drink Tomato Vegetable Lentil soup Chicken Leek and Mushroom Carrot and soup (150g) Potato soup (150g) soup noodle coriander (150g) (150g) soup soup soup (150g) (150g) (150g) Evening meal Water and fruit juice available Bedtime Soft roll white (45g) or brown (50g) Soft roll white (45g) or brown (50g) Soft roll white (45g) or brown (50g) Soft roll white (45g) or brown (50g) Tuna and tomato pasta (200g) Green salad (45g) Cheese and pineapple salad (95g) Green salad (45g) Smoked mackerel (70g) Mixed salad (45g) Roast chicken salad (180g) Potato salad (90g) Fresh orange (100g) Banana (100g) Fruit yoghurt (125g) Tinned mandarins (100g) with Milk jelly (150g) Soft roll white (45g) or brown (50g) Soft roll white (45g) or brown (50g) Omelette (55g) Tomato, and basil salad (50g) Chicken and pasta swirl salad (210g) Grated carrot salad (60g) Broccoli quiche (70g) Mixed bean salad (145g) Rhubarb fool (120g) Poached pears (100g) Fruit mousse (80g) Soft roll white (45g) or brown (50g) Milky drink: Horlicks, Ovaltine, hot chocolate, milky tea, milk shake 13 6.6 Example weekly menu for older people in residential care (menu 2) Monday Breakfast Water and fruit juice available MidAfternoon Evening Meal Water and fruit juice available Wednesday Thursday Friday Saturday Sunday Stewed prunes or grapefruit (110g) Porridge or cereals with milk (e.g. weet bisks, bran flakes, muesli, shredded wheat, puffed wheat) Wholemeal (31g) or white toast (27g) with polyunsaturated margarine (7g) and jam (8g) Fruit juice choice including Cranberry fruit drink (150g) Tea or coffee with milk MidMorning Lunch Tuesday Tea coffee or milky drink with milk and digestive biscuit (26g) Roast beef (90g) and Yorkshire pudding (35g) Roast potatoes (120g) Gravy (50g) Carrots (80g) Cabbage (80g) Vegetable lasagne (250g) Mixed salad (60g) Chicken casserole (250g) Carrots (80g) Broccoli (80g) Mashed potato (130g) Sweet and sour pork (200g) Rice (150g) Sweetcorn (80g) Beef olives (250g) Cauliflower (80g) Spring greens (80g) Jacket wedges (120g) Steamed haddock (75g) Courgettes (80g) Peas (80g) Boiled new potatoes (140g) Irish stew (200g) Green beans (80g) Swede (80g) Baked sliced potatoes (130g) Plum crunchies (120g) Rice pudding (180g) Stewed apple (80g) Rhubarb crumble (100g) Custard (100g) Fruit trifle (150g) Bread and butter pudding (150g) Crème caramel (100g) Tea/coffee with milk Chocolate yoghurt cake (70g) Tea/coffee with milk Apricot oat bars (45g) Tea/coffee with milk Lemon sponge cake (50g) Tea/coffee with milk Madeira cake (50g) Tea/coffee with milk Shortbread (30g) Tea/coffee with milk Bran tea loaf (65g) Tea/coffee with milk Fruit scone (40g) with margarine (7g) Kedgeree (200g) Peas (80g) Soft white (45g) or brown (50g) roll with polyunsatur ated margarine (7g) Cream of vegetable soup (200g) Boiled egg (50g) White (30g) or Wholemeal bread (35g) Margarine (7g) Salmon Fish cakes (120g) Tomato onion and basil salad (50g) Green salad (45g) French stick (60g) Courgette and watercress soup (200g) Smoked mackerel pate (75g) White o wholemeal (60g) toast Mixed salad (45g) Tomato soup (150g) Bread roll Roast beef and salad sandwich (145g) Macaroni cheese (200g)and Sweetcorn (80g) Chicken soup (150g) Bread roll Egg and cress sandwich (130g) Tropical fruit salad (160g) Apricot and pear crunch layer (120g) Fruit compote (120g) Fromage frais (40g) Fresh fruit salad (120g) Banana and yogurt dessert (120g) Melon and grape salad (100g) Canned peaches (120g) and ice cream (30g) Milky drink at bedtime Horlicks, Ovaltine, hot chocolate, milky tea, milk shake 14 Apple pie (100g) Custard (100g) 6.7 Nutritional analyses of example menus for older people in residential care compared to the nutritional guidelines for food served for this group. Nutritional Guideline Energy Kcals MJ g Max Saturated fat g Max Total carbohydrate g Min Non milk extrinsic sugars g Fibre g Min Protein g Min Vitamin A µg Min Vitamin C mg Min Folate µg Min Calcium mg Min Iron mg Min Zinc mg Min Sodium mg Max g Max Fat Salt 1 Average nutrient values from sample menus Menu 1 Menu 2 1955 8.2 1956 8.2 1955 8.2 76 63 65 24 24 24 260 283 313 57 53 55 18 21 20 50 82 77 700 2149 1657 40 154 143 200 460 311 700 1282 1237 9 14 16 9.5 9.7 10.1 2400 2392 2085 6 6 5.2 Max 1 The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced 15 7.0 Nutritional guidelines for food served as community meals 7.1 Background Community meals in this report refers to • meals delivered to older people’s homes • meals provided for those living in sheltered accommodation, and • meals served in lunch clubs. It is estimated that about 1 in 4 older people receives some form of home help and 1 in 12 older people receives a community meal at home 1 . Others may be referred to lunch clubs or receive help from family and friends. There are little data on the quality and nutritional content of community meals and how these meet the needs of the clients for which they are designed, but it is likely that most service users are very vulnerable and the provision of nutrient-dense food to this population group is particularly important. The number of community meals served to an individual each week varies from one meal to fourteen meals a week, although frequently only five meals a week are available to an older person through ‘meals-on-wheels’ services and many older people may only receive these on several days each week. Most meals provided at lunch clubs or delivered to people’s homes are the ‘main meal of the day’. In many local authorities the nutritional content of community meals is based either on the guidelines of the National Association for Care Catering (NACC) 2 or those produced by The Caroline Walker Trust 3 . The NACC provide detailed guidance on the practical aspects of providing community meals. 7.2 Rationale for the nutrient based guidelines Conventionally a main meal would be expected to provide 33% of the Estimated Average Requirement for energy and 33% of the Reference Nutrient Intakes for other nutrients. Among vulnerable housebound older people, however, it is likely that a community meal needs to provide a greater proportion of the day’s nutrients than this, especially if community meals are not provided every day of the week. In order 1 Office for National Statistics 2004. General Household Survey: People Aged 65 Years and Over. 2002/2003. Available from: www.ons.gov.uk 2 National Association of Care Catering 2003. A Recommended Standard for Community Meals. See www.carecatering.org.uk 3 Caroline Walker Trust 2003. Eating Well for Older People: Practical and Nutritional Guidelines. CWT. See www.cwt.org.uk 1 to ensure that community meals make a significant contribution to the nutritional needs of those vulnerable older people who are likely to be the recipients of these meals, it is recommended that the proportion of requirements be increased from 33% to 40% for energy, iron, zinc, calcium and vitamin A. This should enable community meals to deliver as much nutritional benefit as possible, while keeping meals attractive. This may be best achieved among those with smaller appetites by providing a meal and a snack. A summary of these guidelines is given in Table 7.1 Alternative methods of providing food – such as providing smaller meals and snacks which together comprise the nutrients more usually associated with a main meal – also need to be evaluated. For those residents living in very sheltered housing accommodation who are provided with two meals a day, which may form the majority of their nutrient intake, it would be prudent for each meal to fulfil the recommendations given here for a community meal. This would ensure that these residents receive at least 80% of average energy needs and 100% of the current reference nutrient intake for folate and vitamin C from the food provided. Fibre, protein and vitamin D The nutritional guidelines for the amounts of fibre, protein and vitamin D in community meals have not been enhanced beyond a third of daily requirement for the following reasons: Fibre While adequate fibre is important for good gut health, foods which are higher in fibre may make meals bulky and reduce nutrient density. Older people with smaller appetites may find that higher fibre dishes fulfil their appetite quickly and they may therefore find it difficult to finish their meals. For this reason the amount of fibre is set at 33% of the daily recommended intake. Protein It is likely that most menus will provide significantly more protein than the minimum recommended figure. There is however debate about how much protein older people can absorb and use efficiently and a balance is required between providing enough protein and not overburdening the kidneys. The 33% guideline figure for protein reflects this consideration. 2 Vitamin D A daily total intake of 10µg of vitamin D a day is recommended and the nutrientbased guideline suggests that about a third of this should be provided by a community meal. It is acknowledged however that it is generally impossible for older people – particularly those on a vegetarian diet – to receive enough vitamin D through diet alone and therefore the need for supplementation with vitamin D among those receiving community meals should be highlighted. Older people who are receiving community meals are likely to be housebound or have limited exposure to summer sun and are therefore particularly likely to require additional vitamin D through foods rich in vitamin D or through dietary supplements. Those on a vegetarian diet are also unlikely to get enough vitamin D from diet alone. Good food sources of vitamin D for inclusion in community meals are suggested in the foodbased guidelines on page 11. It is very likely however that older people in receipt of community meals will require vitamin D supplementation. Energy, iron, zinc and calcium The following nutrients are recommended in amounts equivalent to at least 40% of the daily recommendations. Energy The importance of maintaining an adequate energy intake has been stressed by the COMA Working Group on the Nutrition of the Elderly 4 . The ‘thin, frail, old lady’ is usually an undernourished person whose smallness represents several years of progressive weight loss. Such a person has no reserves for future episodes of ill health. People who are ill need more calories, and extra care needs to be taken both before and after illness to ensure that increased nutritional needs are met 5 . Since being ill is often one of the criteria for receiving community meals at home, this group may require more calories than their sedentary lifestyles may at first indicate. Increasing the calorie intake of a community meal would also enable more nutrients to be provided and help to compensate for the days when no community meal is provided and lower energy intakes are likely. 4 Department of Health 1992. The Nutrition of Elderly People. Report on Health and Social Subjects No 42. HMSO. London 5 McLaren S, Crawley H 2000. Managing Nutritional Risks in Older Adults. Nursing Times Clinical Monographs. No. 44. NT Books. London. 3 Iron Low iron status has been reported both among people in residential care and among those living in their own homes, and low iron status increases with increasing age.6 Since the majority of people receiving community meals will be both very old and frail and at increased risk of low iron status, community meals should aim to offer at least 40% of the daily Reference Nutrient Intake for iron. Ensuring sufficient vitamin C with meals is also important as this may help the body to absorb the iron Older people are vulnerable to iron deficiencies for three main reasons. Firstly, they tend to have a reduced intake of iron-rich foods. Secondly, in some older people the gut may absorb nutrients less efficiently, and thirdly some older people may consume smaller amounts of vitamin C rich foods which can help iron to be absorbed. Zinc Average intakes of zinc among older people have been shown to be lower than the Reference Nutrient Intake. Zinc plays an important role in maintaining the immune system and in wound healing and low intakes may contribute to other chronic diseases and undernutrition in older people. Calcium Low intakes of calcium among some older people living in their own homes have been reported1 and therefore it seems prudent to ensure that the community meal provides sufficient calcium to offer some protection against low intakes. Vitamin C and folate The following nutrients are frequently found to be lacking in the diets of older people and they are nutrients that are sensitive to heating of food. They are therefore recommended in amounts of at least 50% of current recommendations. Vitamin C Low vitamin C intakes have been reported both among older people in residential care and among those living in their own homes.6 Sufficient vitamin C with meals is also important as this may aid iron absorption. Vitamin C is sensitive to heat, light and exposure to air and therefore caterers should follow good cooking guidance to minimise the loss of vitamin C in meal preparation. 4 Folate Folate deficiency is associated with a particular form of anaemia and both the intakes of folate and folate status have been found to be low in some older people both in residential care and living in their own homes. 6 Low folate status is also more common among older people with dementia, many of whom live in their own homes and receive community meals. Folates are extremely sensitive to heat and may be lost in cooking and when heated food is left for long periods. Caterers should attempt to minimise folate losses in cooking and food presentation. Fluid Intakes A regular and adequate intake of fluids is extremely important for older people. It helps to prevent dehydration which can lead to confused states; helps to prevent and alleviate the symptoms of constipation and fluids can also provide important nutrients when appetites are small. It is recommended that older people drink at least 1.5 litres or about 8 cups of non-alcoholic fluid a day 7 . As part of the community meal it is recommended that older people receive a drink of fruit juice or water with their meal and that wherever possible (for example where a hot meal is still delivered and served), drinks of tea or coffee or additional water or another beverage are offered to the older person after their meal. If the meal does not provide an additional snack, or it may be difficult for the older person to make a drink for themselves to have with their snack, it is recommended that both water and fruit juice are given with the main meal. Those responsible for the provision of community meals should make it a priority that all older people for whom they provide a meal have access to 2 drinks or more as part of this meal provision. In some cases there may be an opportunity as part of community meal provision to organise drinks for other periods of the day and community meals providers should work with other carers and service providers, and the older person themselves, to ensure that they have access to 1.5 litres or about 8 cups of fluid every day. 6 Finch S, Doyle W, Lowe C, Bates CJ et al. 1998. National Diet and Nutrition Survey: People Aged 65 Years and Over. Volume 1: Report of the Diet and Nutrition Survey. London. TSO. 7 CWT 2003. Eating Well for Older People. London. Caroline Walker Trust. 5 Table 7.1 Nutrient-based guidelines for community meals for older people Dietary reference value (DRV) Energy Men and women aged 75 years and over kcals Not less than 40% EAR MJ 782 3.3 Fat g About 35% of energy MAX 30 Saturated fat g About 11% of energy MAX 10 Total carbohydrate g About 50% of energy MIN 104 Non-milk extrinsic sugars g About 11% of energy MAX 23 Fibre g At least 33% of RNI MIN 6 Protein g At least 40% of RNI MIN 17 Vitamin A μg At least 40% of RNI MIN 260 μg About 33% of RNI MIN 3 Vitamin C mg At least 50% of RNI MIN 20 Folate μg At least 50% of RNI MIN 100 Calcium mg At least 40% of RNI MIN 280 Iron mg At least 40% of RNI MIN 3.6 Zinc mg At least 40% of RNI MIN 3.8 Sodium mg MAX 960 MAX 2.4 Vitamin D1 Salt g 40% SACN recommendation 40% SACN recommendation EAR = Estimated Average Requirement DRV = Dietary Reference Value RNI = Reference Nutrient Intake For an explanation of these terms see Appendix 1. 1 Vitamin D It is impossible for most older adults to obtain the full daily requirement of 10 micrograms of vitamin D from the diet alone. It is very likely that older adults who receive community meals will need vitamin D supplements 6 7.3 Food-based guidelines for community meals for older people Below are some food-based guidelines that caterers may find useful in planning menus for community meals. Food group Guidance Rationale What’s included Bread, other cereals and potatoes Starchy foods should make up a third of the daily diet. Foods from this group are a good source of energy and the main source of a range of nutrients in the diet. As well as starch, these foods supply fibre, calcium iron and B vitamins. All varieties of bread including wholemeal and granary bread, chapattis and bagels. Older people may prefer white bread and higher-fibre white bread may also be acceptable. A variety of breads should be used with sandwiches and offered with soup or light meals. Offer a variety of starchy foods with main meals including potatoes, rice, pasta, noodles and other grains. Potatoes, plantain, yam and sweet potato Rice, couscous, bulgar wheat, maize, cornmeal Noodles, pasta Tips • • • • • Older people with small appetites need nutrient-dense meals, and starchy foods should be offered in moderate amounts if there is concern about how much someone is eating. Some white bread has added nutrients and fibre, and can be useful for older people who not like brown or wholemeal bread. Some older people find it easier to eat brown or wholemeal bread if it has been lightly toasted. Offer a variety of starchy foods with meals but ensure that potatoes are offered as a choice each day, as older people may be less familiar with other starchy staple foods. Boil potatoes in the minimum amount of water and for the shortest amount of time to retain vitamins, but ensure they are cooked until soft. Roast potatoes in small amounts of vegetable oil and use milk to mash potatoes to smoothness. If you have customers who are allergic to wheat, oats, barley and rye, good alternatives are foods made from maize (i.e. polenta), rice, rice flour, potatoes, potato flour, buckwheat, sago, tapioca, soya and soya flour. Seek expert advice from a dietitian where necessary. 7 Food group Guidance Rationale What’s included Fruit and vegetables Fruit and vegetables should make up about a third of the daily diet. Fruit and vegetables are good sources of many vitamins and minerals. All types of fresh, frozen and tinned vegetables – e.g. broccoli, Brussels sprouts, cabbage, carrots, frozen peas, swede and green beans Aim for 1 or 2 portions with each meal. 1 portion of fresh or cooked fruit of vegetables should be about 80g. Beans and pulses only count as a maximum of 1 portion per day and cannot count as both a meat alternative and a vegetable in meals. For more information on fruit and vegetable portions see Appendix 0. There is increasing evidence that consuming more than 400g of fruit and vegetables every day reduces the risk of developing chronic diseases such as coronary heart disease and some cancers. All types of salad vegetables, including lettuce, cucumber, tomato, raw carrots, peppers and beetroot All types of fresh fruit – e.g. apples, bananas, kiwi fruit, oranges, pears, mango, plums All types of tinned fruit in juice – e.g. pineapple, peaches Stewed fruit Dried fruit Fruit juice (100% juice) Notes • • • • • • • Steaming or cooking vegetables with minimum amounts of water and serving as soon as possible will help retain vitamins. Use fresh fruit and vegetables as soon as possible, rather than storing them, to avoid vitamin loss. Add vegetables and pulses to stews, casseroles or other dishes and offer a variety of vegetables at main meals. Baked beans (as a vegetable) should be served a maximum of twice a week. Use tinned fruit in natural juice rather than in syrup. Include cooked fruit in puddings and desserts. Include dried fruit in cakes, puddings and desserts. 8 Food group Guidance Rationale What’s included Milk and dairy products Milk and dairy foods should be served every day. Milk and dairy products are excellent sources of calcium which is needed for optimal bone strength protein, vitamin A, riboflavin and vitamin D. All types of milk Community meals should include a source of calcium in the main meal or snack which accompanies it. This could be a milky drink. Dried milk, goat’s and sheep’s milk Cheeses e.g. Cheddar, cottage cheese, cheese spreads, brie, feta, Edam, goat’s cheese, stilton, parmesan Yoghurt (fruit or plain, whole-milk or low-fat), fromage frais Older people with small appetites who may need to gain weight or who are of low weight should be encouraged to have full-fat milk and yoghurt. Milk-based sauces, custard and milk puddings Semi-skimmed milk is suitable for older people with good appetites. Tips • • • • • • • To add extra calories, protein and nutrients to dishes, extra milk, cheese or dried milk powder can be added in cooking. Whole milk can be fortified further by the addition of extra dried skimmed milk powder for those older people who are of low weight or who have small appetites. Frozen yoghurts can be offered as an alternative to ice cream. Milk can be used in sweet and savoury sauces, custards and puddings. It is worth highlighting that some dairy products can contain high salt levels. Strong cheese can impart flavour in smaller amounts. Vegetarian cheese should be used where appropriate For dairy-free diets: serve soya drinks (fortified with calcium) as an alternative. 9 Food group Guidance Rationale What’s included Meat, fish and alternatives (e.g. beans, pulses, nuts, eggs, textured vegetable protein, quorn, tofu) A meat or alternative should be offered at all main meals. Meat is a good source of protein and of vitamins and minerals such as iron and zinc Meat, poultry, offal1, fish, eggs, nuts, beans, pulses and meat alternatives Fish is an excellent protein source and contains selenium and iodine. Meat includes all cuts of beef, lamb and pork and meat and meat products such as ham, corned beef and sausages. Look for meat products with a high meat content. Red meat should be offered at least twice a week. Use lean meat (with a fat content of about 10%). Fish should be offered at least twice a week. It is strongly recommended that oily fish should be served once a week Meat alternatives for vegetarians should be varied and use a variety of foods from this group (e.g. eggs, peas, beans and pulses, soy-based meat alternatives, nuts, quorn or tofu). Oil-rich fish provides omega-3 fatty acids which may help to prevent heart disease. Such foods are also a source of vitamins A and D and iron. Beans and pulses are sources of protein, iron and zinc. Eggs are a good source of protein and vitamins A and D Nuts provide a source of protein, iron, fibre, zinc and calcium. Fish includes fresh, frozen and tinned fish such as tuna. Oil rich fish include, sardines, pilchards mackerel, salmon, trout and herring. Fish products include foods such as fish cakes and fish fingers. Beans – e.g. baked beans, butter beans, kidney beans, lentils are in this group and provide a good source of protein for vegetarians. Tips • • • • • • • • Always choose the leanest cuts of meat and remove visible fat and poultry skin. Reduce intakes of processed meat and fish products which are high in fat and salt such as crumb-coated chicken products, burgers, pies, fish cakes and canned meats. These are often high in salt and low in meat content. Customers need to be made aware of nuts and nut products incorporated into dishes. Eggs are a useful source of nutrients but these should always be well cooked for older people. Oil-rich fish can be used in pâtés and spreads on bread and toast. For older people who have difficulty chewing, offer soft lean meat and fish or meat dishes where the meat has been minced or served in a sauce. Reduce intakes of processed foods made as alternatives to meat such as vegetarian pasties, pies and sausages as these can be high in salt Lean red meat, oil rich fish and offal1 are good sources of iron and zinc 1 Liver pâté is a useful source of nutrients for older people but liver and liver products should not be served more than once a week 10 Food group Guidance Rationale What’s included Foods containing fat and foods containing sugar These foods add palatability to the diet and can be useful in the diets of older people for encouraging eating and stimulating the appetite. The main nutrients provided by such foods are fat, including some essential fatty acids, and also some fatsoluble vitamins. Foods containing fat include butter, margarine, other spreading fats and low-fat spreads, cooking oils, oil-based salad dressings, mayonnaise, cream, chocolate, crisps, biscuits, pastries, cakes, puddings, ice cream, rich sauces, and gravies. These foods can be high in calories and offer few other nutrients. If appetites are poor it is important that these foods do not displace more nutrientrich foods. As for the rest of the population, foods from this group can contribute to excess energy intakes if they are eaten in large amounts. Carbohydrate (in the form of sugars) is also provided. Some products also contain salt. Foods containing sugar include soft drinks, sweets, jams and sugar, as well as foods such as cakes, puddings, biscuits, pastries and ice cream. Tips • • • • Use mono- and polyunsaturated fat (such as sunflower, soya, olive, safflower, rapeseed, corn oil) based spreading fats and in salad dressings For cooking use fats high in monounsaturates such as soya, rapeseed and olive oils When making cakes and puddings include dried fruit or fresh fruit, wholemeal flours and ground nuts if acceptable If older people have a sweet tooth and a poor appetite make sure that the sweet foods on offer are as nutrient dense as possible by including dairy products, cereal foods and fresh and dried fruits. Vitamin D To increase the amount of dietary vitamin D in menus served for older people: • Use margarine fortified with vitamin D for baking and as a fat spread. • Include an oily fish that is rich in vitamin D in the menu at least once a week – for example, herring, mackerel, pilchards, salmon, sardines, trout or roe. These fish contain between 514µg of vitamin D per 100g. • Canned tuna fish can also make a significant contribution to vitamin D intake as it contains about 3.6µg of vitamin D per 100g. • Egg yolks are rich in vitamin D and eggs contain about 2.0µg of vitamin D per 100g. • Meat and poultry contribute small but significant amounts of vitamin D. 11 7.4 Example menus Some example menus are given here which show the sorts, and amounts of foods and drinks that could be served to meet the nutritional and food-based guidance. A nutritional analysis is provided for each of the three menus, showing how the menu compares with the nutritional guidelines. For further advice on practical aspects of catering for community meals see the National Association of Care Catering publication Recommended Standard for Community Meals 8 and Eating Well for Older People: Practical and Nutritional Guidelines 9 produced by the Caroline Walker Trust. 8 National Association of Care Catering 2003. A Recommended Standard for Community Meals. See www.carecatering.org.uk 9 Caroline Walker Trust 2003. Eating Well for Older People: Practical and Nutritional Guidelines. CWT. See www.cwt.org.uk 12 7.5 Example of a community meal with an afternoon snack (menu 1) Monday Tuesday Wednesday Thursday Friday Saturday Sunday Steak and kidney pie (160g) Chicken fricassee (190g) Roast pork (80g)and apple sauce (35g) Savoury pie (150g) Steamed haddock (75g) Lamb and potato hot pot (175g) Mixed vegetables (80g) Cauliflower (80g) Carrots (80g) Broccoli (80g) Roast beef Yorkshire pudding Gravy (150g) Mashed potato (100g) Mashed potato (100g) Roast potatoes (120g) Mashed potato (100g) Chipped potatoes (100g) Mashed potato (100g) Roast potatoes (120g) Trifle (130g) Apple pie (100g) and custard (100g) Rhubarb crumble (125g) and custard (100g) Lemon meringue pie (80g) Bread and butter pudding (145g) Apple tart (100g) and custard (100g) Rice pudding and jam (200g) Tea or coffee with milk Tea or coffee with milk Tea or coffee with milk Tea or coffee with milk Tea or coffee with milk Tea or coffee with milk Tea or coffee with milk Toasted teacake (55g) Fruit scone (50g) Jam sponge (53g) Plain scone with jam (65g) Shortbread (50g) Fairy Cake (30g) Madeira cake (40g) Lunch Fruit juice or water should be provided MidAfternoon A drink should be provided Swede (80g) Peas (80g) Cabbage (80g) Sweetcorn (80g) . 13 Green beans (80g) Cauliflower (80g) Cabbage (80g) Carrots (80g) 7.6 Example of a multicultural community meal with an afternoon snack (menu 2) South Asian vegetarian meal South Asian nonvegetarian meal AfroCaribbean meal AfroCaribbean vegetarian meal Middle Eastern meal Asian meal Asian vegetarian meal Red lentil dahl (45g) Chicken curry (150g) African beef and bean stew (250g) Sweetcorn Chowder (180g) Shammi (lamb) kebabs (151g) Fish Curry (100g) Sweet and sour vegetables (200g) Rice (120g) Dumplings (60g) Fried yam cakes (50g) Spicy pilau rice (190g) Rice (120g) Spinach (80g) Rice and peas (150g) Stir-fried vegetables (200g) Spiced banana crumble (75g) Rice pudding (180g) Lunch Fruit juice or water should be provided Spinach and chick pea curry (165g) Yoghurt raita (30g) Yoghurt raita (30g) Side salad (45g) Side salad (45g) Sweet potato (130g) Chapatti (55g) Banana (80g) Afternoon Snack Grapes (80g) Semolina pudding (180g) Tinned pineapple (100g) Rice (120g) Tofu (60g) Tabbouleh (65g) Green salad (45g) Greek yoghurt (100g) Tea or coffee with: sticky prune cake (50g), carrot cake (60g), coconut short cake (60g), honey cake (45g), fruit loaf (45g), orange and cinnamon cake (60g) or gingerbread (55g) A drink should be provided 14 7.7 Example of a community meal without an afternoon snack (menu 3) Lunch Fruit juice and water should be provided Monday Tuesday Wednesday Thursday Friday Saturday Sunday Lamb Moussaka (330g) Pork and apple casserole (250g) Pork sausages (105g) Savoury minced beef (150g) Salmon fish cakes (120g) Cheese and vegetable bake (250g) Garlic bread (55g) Wholemeal roll (50g) margarine (7g) Baked sliced potatoes (140g) Oven chips (150/120g) Roast chicken and gravy (150g) Sage and onion stuffing (50g) Broccoli (80g) Sweetcorn and peas (80g) Sliced tomato (80g) Green salad (45g) Red pepper (40g) and tomato (40g) garnish Apple and blackberry crumble (170g) Custard (100g) Mashed potato (120g) Potato croquettes (120g) Baked beans (70g) Cauliflower (80g) Rice pudding with jam (200g) Carrots (80g) Mixed Salad (60g) Roast potatoes (120g) Soft white roll with margarine (55g) Brussels sprouts (80g) Swede (80g) Sticky Prune cake (55g) Custard (100g) Queen of puddings (160g) Runner beans (80g) Fruit trifle (170g) Apple meringue pie (120g) Custard (100g) Fresh banana (80g) 15 Stewed fruit compote (120g) Vanilla ice cream (40g) 7.8 Nutritional contribution from community meal menus Average nutrient values from sample menus Energy Nutrient based guideline 782 3.3 Menu 1 Menu 2 Menu 3 832 4.1 805 3.3 782 3.2 Kcals MJ MIN Fat g About 30 30 29 28 Saturated fat Total carbohydrate Non milk extrinsic sugars g About 10 10 9 10 g About 104 114 116 139 g About 23 23 19 18 Fibre g Min 6 8 6.8 8 Protein g Min 17 33.7 28.7 32.6 Vitamin A µg Min 260 1140 804 794 Vitamin C mg Min 20 37 36 60 Folate µg Min 100 140 95 143 Calcium mg Min 280 335 379 367 Iron mg Min 3.6 4.2 5.8 4.1 Zinc mg Min 3.8 3.9 4.5 3.8 Sodium mg Max 960 669 767 963 g Max 2.4 1.7 1.9 2.4 Salt1 1 The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced 16 8.0 Example lunch and evening meal menus for adults EXAMPLE LUNCH MENU Soup Tomato and lentil soup (180g) Courgette and watercres s soup (180g) Irish Stew (190g) Tomato soup (180g) Scotch broth (180g) Mushroom soup (180g) Onion soup (180g) Spicy lentil soup (180g) Main choice 1 Beef Olives (150g) Gravy (50g) Chicken and mushroom pasta (340g) Pork and potato bake (260g) Braised Steak (120g) Gravy (50g) Lamb Curry (200g) Vegetable shepherds pie 200g Vegetable bake (90g) (110g) Mixed bean casserole (250g) Mixed vegetable crumble (160g) Mushroom stroganoff (150g) Vegetable chilli (150g) Roast Beef (70g) and Yorkshire Pudding (35g) Gravy 50g) Vegetable lasagne (240g) Main choice 2 Main choice 3 Goujons of fish (80g) with tartare sauce (10g) Chips (100g) Chicken chasseur (200g) Prawn curry (140g) Tuna (45g) Salad (50g) Option of Coleslaw (40g) and/or Potato salad (85g) Chicken and vegetable casserole (225g) Salmon in spicy tomato sauce (230g) Seafood pasta (230g) Tuna and tomato pasta (260g) Beef stew (150g) Beef curry (180g) Oriental Roast Calypso beef stir chicken turkey fry (135g) (60g) (165g) Egg fried rice (140g) Boiled new potatoes (120g), Jacket potato (120g), Mashed potato (120g) Rice (150g), Pasta (205g) Pork with apricots (140g) Vegetable choices Leeks (80g) Broccoli (80g) Side salad (80g) Dessert choice 1 Fresh fruit slices (100g) or Low fat fruit yoghurt (125g) Dessert choice 2 Rhubarb crumble (100g) with Custard (150g) Chocolat e fudge pudding (100g) Main choice 4 Starchy choices Dessert choice 3 Drinks Cauliflower Gratin (90g) Peas (80g) Side salad (80g) Apple Pie (100g) with Cream (40g) Aubergine (90g) Brussels sprouts (80g) Side salad (80g) Fruit compote (160g) with Custard (150g) Carrots (80g) Parsnips (80g) Side salad (80g) Bread & Butter Pudding (115g) Custard (150g) Sweet oat cake (45g) Spinach (80g) Mixed diced vegetables (80g) Side salad (80g) French beans (80g) Ratatouille (90g) Side salad (80g) Cabbage (80g) Curly Kale (80g) Side salad (80g) Apple crumble (100g) with Custard (150g) Bakewell tart (100g) Apricot and pear layer (100g) with Custard (150g) Lemon Meringue pie (100g) Dutch apple tart (100g) with Custard (150g) Apricots Trifle (150g) canned in juice (125g) with Custard (150g) Water, tea or coffee (with semi-skimmed milk 30ml), 100% fruit juice Chocolate mousse (80g) EXAMPLE EVENING MEALS Bread Main choice 1 Main choice 2 Main choice 3 Starchy choices Vegetable choices Dessert choice 1 Dessert choice 2 Dessert choice 3 Drinks Bread roll selection – granary, wholemeal, crusty white and soft white rolls with soft margarine (60g) Fish Pie Baked cod Steamed fish Breaded Chicken Kedgeree - Plaice (220g) (70g) with Ginger cod (95g) dansak (200g) Veronique and Spring (230g) (100g) Onion (70g) Chicken Macaroni Vegetable Vegetable Vegetable Cheese Mushroom and cheese curry (225g) pie (250g) crumble and onion and pepper broccoli (250g) (160g) turnovers bake lasagne (120g) (110g) (300g) Corned Salmon Cottage beef salad (salad cheese & (100g) (95g) pineapple Option of salad Option of Coleslaw (100g) Option of Coleslaw (40g) Coleslaw (40g) and/or (40g) and/or Potato and/or Potato salad Potato salad (85g) (85g) salad (85g) Boiled new potatoes (120g), Jacket potato (120g) or Mashed potato (120g) Rice (150g), Pasta (200g) Turkey salad (100g) Spinach (80g) Ratatouill e (90g) Side salad (80g) Cauliflower gratin (90g) Broccoli (80g) Side salad (80g) Cheese salad (90g) Coleslaw (40g) and/or Potato salad (85g) Oriental chicken curried rice (300g) Mixed salad (50g) Coleslaw (40g) and/or Potato salad (85g) Chicken salad (100g) Option of Coleslaw (40g) and/or Potato salad (85g) Leeks Cabbage Aubergine (80g) (80g) (90g) French Parsnips Peas beans with (80g) (80g) Side salad Side salad tomato (80g) (80g) sauce (90g) Side salad (80g) Fresh fruit (100g) or low fat fruit yoghurt (125g) Curly kale (80g) Carrots (80g) Side salad (80g) Brussels sprouts (80g) Mixed diced vegetables (80g) Side salad (80g) Muesli Chocolate Flapjack Spiced Fruit tea Sultana slice brownie (55g) apple slice bake (60g) sponge (50g) (60g) (50g) (50g) Melon Fruit jelly Fresh fruit Poached Fruit flan Rhubarb and (160g) salad (120g) pear (150g) fool (120g) grape (140g) salad (120g) Water, tea or coffee with semi-skimmed milk (30ml), 100% fruit juice Option of Coleslaw (40g) and/or Potato salad (85g) Flapjack (60g) Tropical fruit salad (120g) Analysis of average lunch and evening meal menus Energy kcals MJ Dietary reference value (DRV) Average Lunch Average Evening Meal EAR 710 662 Fat g No more than 35% of energy MAX 19.1 15.7 Saturated fat g No more than 11% of energy MAX 6.5 4.8 Total carbohydrate g At least 50% of energy MIN 109 109 Non-milk extrinsic sugars g No more than 11% of energy MAX 16.4 13.9 Fibre g DRV MIN 8.2 7.4 Protein g RNI MIN 32 29 Vitamin A µg RNI MIN 671 436 Vitamin C mg RNI MIN 86 54.5 Folate μg RNI MIN 158 141 Calcium mg RNI MIN 350 352 Iron mg RNI MIN 5.0 4.1 Zinc mg RNI MIN 4.1 3.3 Sodium mg MAX 711 645 MAX 1.8 1.6 1 Salt 1 g SACN recommendation SACN recommendation The salt content of menus will go down as the amount of salt in common commodities such as bread is reduced Appendix 1 Rationale for derived dietary reference values for use in preparation of the nutrient based guidelines for food served in public institutions Derived dietary reference values have been used to calculate the recommended average nutrient content of meals and snacks provided for population groups over periods of one week or more in this report. This Appendix explains how these were calculated and Table A1 on page 9 provides a summary of these values. These values are based on those prepared for the United Kingdom by the Department of Health 1 and additional information on sodium/salt published in 2003. 2 When prescribing diets for groups of people the intention is to ensure adequacy of the diet. The Dietary Reference Values are designed to provide guidance for groups of individuals by age and gender. It is recommended that where appropriate the Reference Nutrient Intakes (RNI) are used for groups to ensure that the risk of deficiency to any individual is small. (For an explanation of the terms dietary reference values and reference nutrient intake please see page 2). The aim of the derived reference values described in this appendix is to ensure that all individuals in a group are likely to have their needs met for those nutrients where there is a minimum requirement without providing too much of those nutrients for which there is a maximum recommendation. In many public institutions food will be served to groups of people mixed by age and gender. A pragmatic approach has therefore been taken to develop simple reference values which can be used to develop the nutrient based guidelines. The rationale for the calculation of the derived dietary reference values for each age group is explained on the following pages. For simplicity the values have been rounded to whole numbers (or where it is the convention to the nearest 5 or 10). These values are intended to act as guidance only to encourage menu planners to produce menus which contain the types of food which provide nutrients in the proportions recommended for good health. 1 Department of Health 1991. Dietary Reference Values for Food and Energy and Nutrients for the United Kingdom. Report on Health and Social Subjects No.41. HMSO London. 2 SACN 2003. Salt and Health. TSO. London 1 Definition of Dietary Reference Value 3 terms Dietary Reference Values (DRVs) Dietary Reference Values (DRVs) are benchmark intakes of energy and nutrients. They indicate the amount of energy or individual nutrients needed by a group of people of a certain age range (and sometimes gender) for good health. They are not designed for working out a diet for an individual; eating less of a nutrient than is recommended cannot tell us that an individual is deficient. However, if more than quite a few people in a group fall below the recommendations, this suggests that some individuals in that population may be at risk of deficiency. The DRVs for energy are described as the Estimated Average Requirement (EAR). Most other nutrients have an EAR and also a Reference Nutrient Intake (RNI) Estimated Average Requirement (EAR) The average amount of energy or nutrients needed by a group of people. Half the population will have needs greater than this, and half will have needs below this amount. Reference Nutrient Intake (RNI) This is the amount of a nutrient which is enough to meet the dietary requirements of about 97% of a group of people. If people get more than this amount they will almost certainly be getting enough. Percentage (%) of Energy This describes what proportion of the energy consumed should come from fat, carbohydrates or protein. It is calculated from the known contribution that each of these macronutrients makes to energy intake: fat provides 9 kcals/g, carbohydrates 3.75 kcals/g and protein 4 kcals/g. Recommendations for sodium/salt intakes The Scientific Advisory Committee on Nutrition (SACN) 4 made the following recommendations on maximum recommended salt intakes for the population. Age 1-3 years 4-6 years 7-10 years 11 years + SACN recommendation for maximum daily salt and sodium intakes Salt g/day 2 3 5 6 3 Sodium mg/day 800 1200 2000 2400 Department of Health 1991. Dietary Reference Values for Food and Energy and Nutrients for the United Kingdom. Report on Health and Social Subjects No.41. HMSO London 4 SACN 2003. Salt and Health. TSO. London 2 Derivation of nutrient values by age group 1. Children aged 1-4 years Energy The Estimated Average Requirements (EAR) for energy for children aged 1 year to 4 years are shown below. Estimated Average Requirements for energy for children under 5 years Age of child 1 year 1½years 2 years 2½years 3 years 4 years Estimated Average Requirement in kcal (MJ) per day* Boys Girls 960kcal (4.0 MJ) 910kcal (3.8MJ) 1,080kcal (4.5MJ) 1,020kcal (4.3MJ) 1,190kcal (5.0MJ) 1,130kcal (4.7MJ) 1,280kcal (5.4MJ) 1,230kcal (5.1MJ) 1,490kcal (6.2MJ) 1,370kcal (5.7MJ) 1,600kcal (6.7MJ) 1,460kcal (6.1MJ) * In practice the intakes of energy and of nutrients needs to be averaged over several days to take account of variations in appetite and in the diverse foods in a diet from day to day. Derived energy values for 1-4 year old are based on the average dietary reference values for boys and girls based on the figures in the table above. Fat and carbohydrate There are no recommendations for the 1-4 year olds in terms of the proportion of energy in the diet which should come from fat and total carbohydrate. If 1-4 year olds have too little fat, this may affect their growth and development and their diet may be too low in other essential nutrients. Between the ages of 2 and 5 years children's diets should move towards the recommendations currently made for those over 5 years of age. However, in this report it is argued that diets which provide about 35% of energy from fat are likely to be suitable for children aged 1-4 years (see page 00). There is however no recommendation for the amount of saturated fat in the diets of 1-4 year olds since restriction on milk and dairy products is not desirable. Similarly no recommendation is made for fibre since it is important that the diets of 1-4 year olds are not too bulky but remain nutrient dense. The recommendation currently made for the whole population to restrict the amount of NME sugars in the diet to no more than 11% of energy intake is however appropriate to children under the age of 5. Protein Protein values are based on ¾ of the RNI for 1-3 year olds plus ¼ of the RNI for 4-6 year olds Other nutrients 1-2 year olds: Values are taken from those for the age group 1-3 year olds 3-4 year olds: Values are taken as 50% of the DRV for 1-3 year olds and 50% of the DRV for 4-6 year olds. 3 The values for children aged 1-4 years are therefore the average of those aged 1-2 and 3-4 years. When setting nutritional guidance for population groups it is normal practice to ensure that the needs of the group with the highest needs are met – so that where there are discrepancies by age and gender for a specific nutrient for which there is a minimum, the higher value is selected. For children aged 1-4 years however, there is already an expectation that the diet will be nutrient dense and in practice it becomes difficult to enhance the micronutrient intakes relatively higher than the energy value when energy intakes are small. In this group therefore, micronutrient recommendations remain proportional to energy intake: the assumption is that the bigger and hungrier children will eat more and if they eat the types of food as suggested in the sample menus, they will obtain proportionally higher amounts of micronutrients to meet their needs. Sodium/salt values are taken as 75% of the value for 1-3 year olds and 25% of the value for 4-6 year olds. 2. Children aged 5-10 years Estimated Average Requirements for energy for children Age of child 4-6 years 7-10 years Estimated Average Requirement in kcal (MJ) per day* Boys Girls 1,715kcal (7.2MJ) 1,545kcal (6.5MJ) 1,970kcal (8.2MJ) 1,740kcal (7.3MJ) * In practice the intakes of energy and of nutrients needs to be averaged over several days to take account of variations in appetite and in the diverse foods in a diet from day to day. The derived energy values for children aged 5-10 years for this report are taken proportionally from these figures: 1/3 x mean EAR at 4-6 years (for those aged 5 and 6 years) + 2/3 mean EAR at 7-10 years (for those aged 7, 8, 9,10 years) The values for fat and carbohydrate are derived as a proportion of these based on their energy contribution as described in table 1. Protein is estimated as 1/3 x the RNI 4-6 year olds (for those aged 5 and 6 years) and 2/3 of the RNI of 7-10 year olds (for those aged 7, 8, 9,10 years) Fibre (non-starch polysaccharides) estimates are made for this group based on their energy requirement relative to an adult, where the DRV for fibre is 18g per day. The values for vitamins and minerals (except sodium/salt) for this group are however taken as the highest requirement in the group: i.e. the values for 7-10 year olds. 4 Sodium/salt values are taken as 1/3 of the value for 4-6 year olds and 2/3 of the value for 7-10 year olds in line with energy requirements, however to aid menu planners this figure has been rounded up to the nearest 0.5g salt. 5 3. Young people aged 11-18 years Estimated average requirements of energy for young people Age of child 11-14 years 15-18years Estimated Average Requirement in kcal (MJ) per day* Boys Girls 2,220kcal (9.3MJ) 1,845kcal (7.7MJ) 2,755kcal (11.5MJ) 2,110kcal (8.8MJ) * In practice the intakes of energy and of nutrients needs to be averaged over several days to take account of variations in appetite and in the diverse foods in a diet from day to day. For this age group there will be wide variations in energy need depending on growth rate, stage of development, activity levels and gender and it is difficult to provide an average figure for young people of this age. Table 1 therefore provides a range of figures for energy and macronutrients. Menu planners should aim to provide food which allows the range of energy intakes to be accessed by those with smaller and bigger appetites (i.e. by offering a range of portion sizes) while maintaining the micronutrient intakes recommended. Protein is given as a range of figures representing the RNI for males and females aged from 11--18 years. Values for vitamins and minerals for the whole group are taken using the principle of meeting the needs of the members of the group with the highest requirement. For example for calcium the value for boys aged 15-18 years has been taken and for iron the value for girls 15-18 years has been taken. 6 4. Adults aged 19-74 years The energy needs of adults are likely to be highly variable but it is generally accepted that energy requirements fall among older adults as energy expenditure declines and there are changes to body composition which affect the basal metabolic rate. These differences are however relatively small and for practical purposes an average energy value for adults has been determined which is likely to apply to the majority of adults in this group. Those with higher energy needs will be able to meet these needs by having larger portion sizes and more carbohydrate foods such as bread with meals. Average requirements of energy for adults aged 19-74 years Age 19-50 years 51-59 years 60-64 years 65-74 years Estimated Average Requirement in kcal (MJ) per day* Men Women 2,550kcal (10.6MJ) 1,940kcal (8.1MJ) 2,550kcal (10.6MJ) 1,900kcal (8.0MJ) 2,380kcal (9.9MJ) 1,900kcal (8.0MJ) 2,330kcal (9.7MJ) 1,900kcal (8.0MJ) * In practice the intakes of energy and of nutrients needs to be averaged over several days to take account of variations in appetite and in the diverse foods in a diet from day to day. Since the differences between age groups are relatively small, for practical purposes in this report the average energy intakes for this group have been estimated as: the average of 80% of the EAR for 19-50 year olds plus 20%of the EAR for 60-64 year olds The values for fat and carbohydrate for this group have been calculated proportionally to the derived energy value For protein the value is taken as the mean RNI for men and women aged 19-50 years and for those aged 50+ years For vitamins and minerals the principle applies that the values should meet the needs of those with the highest needs in the group. Vitamin D There is an RNI for vitamin D for all adults over 65 years of 10µgday. It is however difficult to obtain vitamin D from the diet alone and therefore it is unlikely that menus will be able to provide this level of vitamin D. Adults who live normal lives (i.e. are active and spend time out of doors in summer) are likely to make enough vitamin D in their skin to provide for their needs. Any older adult who is housebound or spends limited time outdoors or wears very restrictive clothing so that their skin is not exposed to the sun is likely to need vitamin D supplements. Single gender groups Where caterers are providing for single gender groups, the values for men only and women only in the age group 19-74 years is also provided here calculated using the same principles. 7 5. Adults aged 75 years and over The needs of older adults aged 75 years and over will vary from those for the younger adult age group since they are likely to have lower energy requirements. The need for nutrient dense foods for this age group is fully explained in chapter 8. Age 75 years + Estimated Average Requirement in kcal (MJ) per day* Men Women 2,100kcal (8.8MJ)) 1,810kcal (7.6MJ) * In practice the intakes of energy and of nutrients needs to be averaged over several days to take account of variations in appetite and in the diverse foods in a diet from day to day. For this group energy values are taken as the average for men and women The values for fat and carbohydrate are taken proportionally to the energy value as shown in Table 1 The protein value is taken as the mean of the RNI for men and women aged 75 years and over Recommendations for vitamins and minerals are calculated using the principle that the highest needs of any member of the group should be met Vitamin D There is an RNI for vitamin D for all adults over 65 years of 10µgday. It is however difficult to obtain vitamin D from the diet alone and therefore it is unlikely that menus will be able to provide this level of vitamin D. Adults who live normal lives (i.e. are active and spend time out of doors in summer) are likely to make enough vitamin D in their skin to provide for their needs. Any older adult who is housebound or spends limited time outdoors or wears clothing which covers their body so that their skin is not exposed to the sun is likely to need vitamin D supplements. All older people in residential care or having community meals are likely to need vitamin D supplements. 8 Table A1 Derived nutrient values for nutrient-based standards Nutrient requirement based on Nutrient Energy kcals MJ EAR Fat g MAX Saturated fat g MAX Carbohydrate g MIN Non milk extrinsic MAX sugars g Fibre g MIN Derived dietary reference values for population groups by age Children 1-4 years Children 5-10 years Young people 11-18 years 1845 – 2755 7.7 – 11.6 Adults 19-74 years 2225 9.4 Men 19-74 years 2515 10.6 Women 19-74 years 1930 8.1 Adults 75 years and over 1955 8.2 1290 5.4 1780 7.5 501 70 72 -107 87 98 75 76 No more than 35% energy No more than 11% energy At least 50% energy No more than 11% energy DRV * 22 23 -34 27 31 24 24 1721 237 246 - 367 297 335 257 260 38 52 54 - 81 65 74 57 57 * 15 18 18 18 18 18 Protein g MIN RNI 16 25 41-55 50 55 45 50 Vitamin A µg MIN RNI 425 500 700 700 700 600 700 Vitamin D µg MIN RNI 7 - - - - ** - ** 10 Vitamin C mg MIN RNI 30 30 40 40 40 40 40 Folate µg MIN RNI 85 150 200 200 200 200 200 Calcium mg MIN RNI 375 550 1000 700 700 700 700 Iron mg MIN RNI 7 9 15 15 9 15 9 Zinc mg MIN RNI 5.5 7 9.5 9.5 9.5 7 9.5 Sodium mg MAX 900 1800 2400 2400 2400 2400 2400 Salt g MAX SACN maximum SACN maximum 2.3 4.5 6 6 6 6 6 1 For children aged 1-4 years it is recommended that about 35% energy comes from fat and about 50% of energy from carbohydrate * No value is given for these nutrients for this age group. ** For adults aged over 65 years the reference nutrient intake is 10µg per day 9 . 10 Appendix 2 Good sources of nutrients This Appendix shows a number of foods and drinks which are useful sources of certain vitamins and minerals. These are based on average servings. This data has been adapted from tables prepared for the Caroline Walker Trust report Eating Well at School 1 1 Crawley 2005. Eating well at school. The Caroline Walker Trust. www.cwt.org.uk EXCELLENT GOOD USEFUL VITAMIN A Liver* liver sausage/pâté* carrots spinach sweet potatoes red peppers mango canteloupe melon dried apricots canned salmon herrings egg honeydew melon prunes orange sweetcorn peas whole milk VITAMIN D fortified breakfast cereals herrings pilchards sardines tuna canned salmon egg liver and liver pâté* pork, bacon and ham fortified breakfast cereals malted drinks nectarine peach blackcurrants fresh or canned apricots watercress tomatoes cabbage (dark) broccoli Brussels sprouts runner beans broad beans margarine butter cheese kidney lLiver* (other than chicken liver) liver sausage/pâté* margarine wholemeal bread yeast extract oatcakes currant buns nuts potatoes milk malted drinks fortified breakfast cereals almonds lean meat chicken and other poultry eggs white or brown bread semi-sweet biscuits lean meat or poultry bacon mackerel, tuna, salmon sardines, pilchards cheese yoghurt eggs wholemeal bread peanut butter yeast extract bacon liver sausage* baked beans lentils and other pulses green vegetables tomatoes wholemeal bread cheese THIAMIN RIBOFLAVIN liver* kidney NIACIN fortified breakfast cereals canned salmon, tuna pilchards chicken VITAMIN B6 bran flakes red meat poultry liver* oily fish VITAMIN B12 liver* kidney oily fish beef lamb pork turkey white fish eggs FOLATE most fortified breakfast cereals, e.g. cornflakes, branflakes, crisped rice liver* spinach yeast extract cabbage Brussels sprouts broccoli peas orange melon lean meat sausages kidneys herrings sardines potatoes bananas nuts peanut butter dried fruit white fish chicken liver malted-style drinks chicken milk cheese yoghurt marmite ribena bran flakes wholemeal bread/flour wheat bisks cauliflower beef runner beans tomatoes parsnip kidney VITAMIN C blackcurrants orange (and orange juice) strawberries canned guava spring greens green and red peppers (raw) broccoli, cabbage cauliflower, spinach tomato Brussels sprouts watercress kiwi fruit mango grapefruit IRON fortified breakfast cereals liver* kidney liver sausage/pâté* CALCIUM green leafy vegetables sardines cheese tofu wholemeal bread/flour wheat bisks beef, beefburger corned beef lamb sardines, pilchards soya beans chick peas, lentils spinach, broccoli spring greens dried apricots raisins pilchards yoghurt milk (all types) soya drink fortified with calcium cheese spread sesame seeds bacon ham poultry canned sardines shrimps and prawns tofu wholegrain breakfast cereals, e.g. puffed wheat, bran flakes, wheat bisks nuts muesli wholemeal pasta brown breads white bread with added fibre baked potato with skin sweet potato broad beans fresh or frozen peas sweetcorn broccoli, Brussels sprouts quorn blackberries dried dates almonds, hazelnuts ZINC FIBRE (non-starch polysaccharides – NSP) liver* kidney lean meat corned beef wholegrain or wholewheat breakfast cereals such as bran flakes, wheat bisks, shreddies, shredded wheat, sultana bran wholemeal breads baked beans, chick peas, kidney beans (and most beans) lentils dried apricots, figs, prunes potatoes green leafy salads ackee peanuts potatoes green beans peas satsumas eating apples nectarines peaches raspberries blackberries white bread baked beans broad beans black-eyed peas blackcurrants salmon, tuna herrings sausage chicken and other poultry egg tofu canned salmon muesli white bread/flour peas, beans, lentils dried fruit orange egg yolk sausages cold cooked meats canned tuna or pilchards eggs milk cheese beans and lentils brown or wholemeal bread plain popcorn sesame seeds puffed wheat cereal brown rice white pitta bread pizza potatoes yam houmous canned peas cabbage carrots plantain banana mango raisins sunflower seeds potato crisps * Liver and liver pate are very rich in vitamin A and these foods should be consumed no more than once a week. For more information see SACN (2005) Review of Dietary Advice on Vitamin A. London. TSO. Food-related customs This is a guide to some of the differences in food choice commonly observed by those from different religious and cultural groups. It is important to emphasise that there may be individual differences in food choices between families and individuals Jewish Hindu1 Sikh1 Muslim Buddhist Rastafarian2 It may vary Yes Yes It may vary It may vary Yes Yes Yes Yes It may vary Yes Yes It may vary It may vary Kosher Halal No It may vary Beef and beef products Pork and pork products Fish Kosher It may vary It may vary No No Mutton/lamb It may vary It may vary No It may vary Halal Yes Chicken No blood spots Not with meat Not with meat Kosher Halal No It may vary No Rarely Rarely No No No It may vary It may vary Yes It may vary Yes No Kosher It may vary Yes No Butter/ghee With fins and scaes It may vary Yes It may vary Shellfish With fins and scales No No It may vary Lard No No No No No No Cereal foods Yes Yes Yes Yes Yes Yes Nuts/pulses Yes Yes Yes Yes Yes Yes Fruits/vegetables Yes Yes3 Yes Yes Yes Yes Fasting4 Yes Yes Yes Yes Yes Yes Eggs Milk/yoghurt Cheese 1 Strict Hindus and Sikhs will not eat eggs, meat, fish, and some fats. 2 Some Rastafarians are vegan. 3 Jains have restrictions on some vegetable foods. Check with the individuals. 4 Fasting is unlikely to apply to young children. Reproduced from Crawley 2006. Eating Well for Under 5s in Child Care. The Caroline Walker Trust. www.cwt.org.uk Resources and Useful Addresses This list is not intended to be comprehensive but provides details of some of the organisations and publications which may be useful to caterers in the public sector. Better Hospital Food www.betterhospitalfood.com This site provides information on all aspects of food service and delivery within the NHS. Chartered Institute of Environmental Health Chadwick Court 15 Hatfields London SE1 8DJ T: 020 7928 6006 E: [email protected] www.cieh.org.uk LACORS Local Authorities Coordinators of Regulatory Services 10 Albert Embankment London SE1 7SP TL 020 7840 7200 www.lacors.com Local Authorities Catering Association (LACA) Bourne House Horsell Park Woking GU21 4LY T: 01483 766777 www.laca.co.uk National Association Care Catering 45, Palace View Bromley BR1 3EJ T 020 8460 4477 www.carecatering.org.uk The Royal Institute of Public Health and Hygiene 28 Portland Place London W1B 1DE T: 020 7580 2731 www.riph.org.uk Vegan Society Donald Watson House 7 Battle Road St Leonard's on Sea East Sussex TN37 7AA T: 01424 427393 www.vegansociety.com Vegetarian Society Parkdale Dunham Road Altrincham Cheshire WA14 4QG T: 0161 928 0793 www.vegsoc.org Food Standards Agency publications Available from: PO Box 369 Hayes Middlesex UB3 1UT T: 0845 606 0667 F: 020 8867 3225 Minicom (for people with hearing disabilities): 0845 606 0678 E: [email protected] Be Allergy Aware FSA0002 Catering for Health ISBN 0 907667 27 9 (also available in Welsh) Ten Tips for Food Safety FSA0006 The Food Safety Act 1990 and You FSA0238. Booklet summarising the Food Safety Act. The Balance of Good Health FSA/0008/0604 The following resources can be downloaded from the FSA website: www.food.gov.uk A guide for healthier eating for the over 60s FSA Northern Ireland 2006 Calendar A guide to healthier eating for the over 60s FSA Wales publication BSE and Beef: A Brief Guide to New Controls Leaflet published by the FSA BSE and Beef: New Controls Explained Booklet published by the FSA Germs Love To Travel Labelling claims Labels Preventing food poisoning When you need to avoid a food A guide for people with food allergy or intolerance Further information on healthy eating can be obtained from: www.eatwell.gov.uk www.salt.gov.uk www.food.gov.uk Publications from the National Audit Office 157-159 Buckingham Palace Road London SW1W 9SP T: 020 7798 7400 E: [email protected] www.nao.gsi.gov.uk Smarter food procurement in the public sector (2006) London. TSO Smarter food procurement in the public sector: A good practice guide (2006) Smarter food procurement in the public sector: Case Studies (2006) Serving Time: Prisoner Diet and Exercise (2006) SUSTAIN Publication The Manual for Sustainability in Public Sector Food and Catering (2003) Available from Sustain, 94, White Lion Street, London N1 9PF T: 020 7837 7200 www.sustainweb.org Additional resources on catering across the public sector in Scotland and Wales are available via The Scottish Executive Website and the website of the Welsh Assembly www.scotland.gov.uk www.wales.gov.uk Menu analysis The menu plans in this report were put together by nutritionists using a combination of food and recipe composition data from a number of sources: Data from a number of volumes of McCance and Widdowson’s The Composition of Food 1 and other food composition information in tables and scientific papers Data from manufacturers and food labels Data provided by other menu planners and caterers Data included in the Nutmeg Menu Planner software package The Caroline Walker Trust recommends that caterers use appropriate software to analyse their menus. This should include information about cooked foods and dishes and should be designed to ensure that all the nutrients of interest, including non-milk extrinsic sugars, are included for all the foods and recipes that are included in the database. The Nutmeg Menu Planner fulfils all these functions and further details can be found on www.nutmeg-uk.com 1 For details of these publications see www.food.gov.uk
© Copyright 2026