Weekly Media Report - Saint Francis Hospital
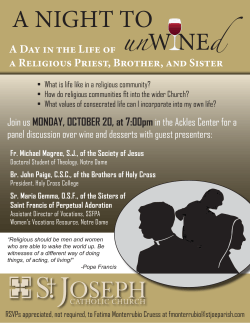
`+ Marketing Department Weekly Media Report January 16, 2015 Weekly Media Report – January 16, 2015 Print Hartford Courant - Johnson Memorial Files for Bankruptcy to Become Saint Francis Subsidiary (1/15/2015) West Hartford News - Saint Francis Care Names Spirit Award Recipients (1/14/2015) Journal Inquirer - JMMC Seeks Bankruptcy Again (1/15/2015) Becker’s Hospital CFO - Johnson Memorial Medical Center eyes bankruptcy in transaction with Saint Francis Care (1/15/2015) CHA Update - Johnson Memorial Medical Center Announces Approval of Asset Purchase Agreement with Saint Francis Care (1/15/2015) Catholic Transcript - Hospital looks ahead to merger, looks back on Archbishop Mansell's Leadership (1/12/2015) Catholic Health Association - Saint Francis Care in Connecticut plans to join Trinity Health (1/2015) Catholic Health World - Saint Francis Announces Executive Appointment (1/9/2015) - Saint Francis Receives W.K. Kellogg Foundation Grant for Breastfeeding Program (12/19/2014) MASS Live - Johnson Memorial Medical Center plans bankruptcy to become part of Saint Francis Care (1/14/2015) Healthcare Finance - Saint Francis creates affiliated post-acute care network (1/13/2015) Advisen FPN - Connecticut Hospital Heads Back Into Chapter 11 (1/15/2015) News On Line WTIC - CBS - Johnson Memorial Declaring Bankruptcy, Being Purchased by Saint Francis (1/14/2015) WNPR News - Chemotherapy Refusal is at Center of Connecticut Case – But What is Chemo? (1/12/2015) Television WTIC - Fox - Kara Moscato – Dash Diet (1/13/2015) WVIT-NBC - Johnson Memorial Hospital (1/15/2105) Radio WTIC-Fox - Hospital Observation Status (1/15/2015) - Dr. Adam Boruchov – Chemotherapy (1/9/2015) WNPR-FM - Dr. Alan Boruchov – Chemotherapy (1/12/2015) - Dr. Ulysses Wu – Flu (1/2/2015) January 15, 2015 By Matthew Sturdevant and Brian Dowling Johnson Memorial Files For Bankruptcy To Become Saint Francis Subsidiary Johnson Memorial files Chapter 11 bankruptcy to clear path for acquisition by Saint Francis Care. The parent company of Johnson Memorial Hospital in Stafford on Wednesday filed for Chapter 11 bankruptcy protection to clear the path for acquisition by Saint Francis Care in Hartford. Johnson Memorial Medical Center's executives decided to file for Chapter 11 bankruptcy after discussing the issue with its Board of Directors and with lenders, government agencies and "multiple advisors," the health systems said in a joint release. Financial terms were not disclosed. The deal means Johnson Memorial's assets would transfer to Saint Francis Care, the parent company of Saint Francis Hospital and Medical Center. This is just the latest development in a changing health-care landscape across Connecticut and the nation. For example, Tenet Healthcare Corp. of Dallas is in talks with state officials who hope to revive Tenet's plans to acquire five hospitals in Connecticut. Saint Francis itself is being acquired. Last month, Saint Francis Care said it plans to become a part of Trinity Health of Livonia, Mich., a large Catholic health care system that operates 86 hospitals in 21 states. The Johnson Memorial acquisition includes various affiliates: Evergreen Health Care Center, which is a short-term and long-term nursing care facility; Home & Community Health Services, which used to be Enfield Visiting Nurse Association and includes hospice; and Johnson Health Care. Johnson Memorial is one of the state's smallest hospitals with 95 beds and 460 full-timeequivalent staff positions. It is also among the state's weakest, financially. The hospital's parent company posted a total shortfall of $18.5 million from operations in the four years ending in 2013, state Department of Public Health records show. In fiscal 2013, Johnson reported an operating loss of $5.3 million during a year when the hospital had operating revenues of $87.68 million. That loss was partly offset by $2.6 million in revenues other than operations, such as investment gains. Johnson had an occupancy rate of 47 percent of its available beds, compared with 65 percent for all hospitals statewide, during fiscal 2013. In bankruptcy filings for each of its major affiliates, Johnson Memorial Medical Center outlined about $29.3 million in unsecured debt. The largest chunk of that is owed to People's United Bank in Bridgeport; Saint Francis Hospital in Hartford; and McKesson Technologies Inc., a health care information technology company in Chicago. In 2012, Johnson Memorial and Saint Francis Care signed an affiliation agreement that provided the rural, financially troubled hospital with access to a larger organization. As a result of the affiliation, Johnson Memorial has improved operations by all financial measures, the hospitals said. "The terms of the transaction include a pre-negotiated debt restructuring with our lender, who supports this process," Johnson Memorial's director of business development, Amy DuBoisZwaan, said in an e-mail. Johnson Memorial is using the bankruptcy process to bring about the sale to Saint Francis "under the terms to which have already been agreed by all parties," DuBois-Zwaan said. Emerging from bankruptcy with less debt and a stronger relationship with Saint Francis will help the Stafford hospital achieve its goal of becoming stronger and more financially sound, she said. Wednesday's bankruptcy filings report that financial difficulties at Johnson Memorial Medical Center continued even after the system emerged from an earlier bankruptcy in 2010. The earlier bankruptcy shaved away millions of dollars in debt from the company's balance sheet. Nevertheless, Johnson Memorial Medical Center had net losses of $2.8 million in 2012 and $7.5 million in 2013, which the health system said in its filing had "accumulated and threatened [its] viability." In financial terms, net losses are different from operating losses. The Johnson Memorial Medical Center's board of directors approved the bankruptcy in a special meeting Dec. 30. The board placed Johnson Memorial Medical Center CEO Stuart E. Rosenberg in charge of the bankruptcy process. It is uncommon for a hospital to file for bankruptcy immediately before becoming acquired by another hospital system, said Gautam Gowrisankaran, an economics professor at the University of Arizona's Eller College of Management, who researches hospital acquisitions. Struggling rural hospitals do not normally file for bankruptcy in part because of a federal program that allows them to become a "critical access hospital," allowing it to be reimbursed by Medicare on a cost-plus basis, Gowrisankaran said "It's not extremely generous, but it's certainly enough that you're going to be avoiding bankruptcy," Gowrisankaran said. "The number of rural hospital bankruptcies has gone way down since this program was implemented [in 1997]." The program does have criteria, such as a certain distance from other hospitals, and it's possible Johnson Memorial would not qualify, Gowrisankaran said. There is a lot of hospital merger activity, generally, in the U.S., he said. "I haven't heard of a hospital strategically filing for Chapter 11 before they merge. That's certainly common in other sectors," Gowrisankaran said. "Our current affiliation agreement provides the framework necessary to ensure the continued delivery of quality care to the local community and sustain a major economic resource for the region," Saint Francis Care CEO and President Christopher Dadlez said in a statement. "Recently we have watched JMMC stabilize and strengthen its operations. Both parties are enthusiastic about the next steps ahead." The Johnson Memorial CEO, Rosenberg, said in a statement: ""Throughout our working affiliation, JMMC and Saint Francis Care have been on the path of creating a long-term partnership. One of the achieved goals from our partnership with Saint Francis has been the ability to continue our mission as we have for the last 102 years, providing quality healthcare in the community. Johnson Memorial Medical Center will be a key member of an integrated system of care." Courant Staff Writer Dan Haar contributed to this story. Wednesday, January 14, 2015 Saint Francis Care names Spirit Award recipients At its recent annual meeting, Saint Francis Care officials announced that the late David Lentini and current Archbishop Emeritus, The Most Reverend Henry Mansell are the 2015 recipients of the annual Saint Francis Spirit Awards. David Lentini’s wife, Barbara, and son, Mark, accepted the award on his behalf. Lentini, the former CEO of Connecticut Bank and Trust served the greater Hartford community as a Saint Francis board member and a Renbrook School board member. Mansell chaired the Saint Francis Above, from left, are Mark Lentini, Barbara Lentini, Saint board of directors for 10 years and Francis Board Chairman Daniel P. O’Connell, Saint has worked tirelessly in Hartford to Francis President and CEO Christopher Dadlez. end homelessness and provide tuition assistance to Catholic school students. He also helped to develop the Malta House of Care Mobile clinic, a free medical service, among many other charitable acts. Saint Francis Board Chairman Daniel P. O’Connell accepted the award for Archbishop Mansell, who was unable to attend. Thursday, January 15, 2015 Don Michak JMMC seeks bankruptcy again Hospital’s federal filing is part of buyout deal with Saint Francis Care Johnson Memorial Medical Center in Stafford will seek federal bankruptcy protection for the second time in seven years in a deal to sell itself to St. Francis Care, the corporate parent of St. Francis Hospital and Medical Center in Hartford, company officials say. The “asset purchase agreement” announced Wednesday comes less than a month after St. Francis Care itself agreed to merge with Trinity Health, a Catholic, 86-hospital chain based in Michigan, which would invest $275 million in St. Francis within five years after the expected closing of their deal this year. The agreement also comes nearly three years after St. Francis Care forged a “partnership” with JMMC, the owner of the 101-bed acute care Johnson Memorial Hospital and the 180-bed nursing facility Evergreen Health Center, both in Stafford, and the surgery center and visiting nurse operation Home & Community Health Services in Enfield. Under the affiliation agreement struck in July 2012, Saint Francis Care agreed to pay $2.35 million to help JMMC pay off debt related to its 2008 bankruptcy. Saint Francis Care also had the option to make additional payments of just over $2 million between 2013 and 2015. JMMC, which was created when the former Johnson Memorial Corp. emerged from bankruptcy protection in 2010, also would use the money to satisfy payment of claims under that reorganization plan. All such payments were to constitute a unsecured loan and with its initial payment Saint Francis Care was provided the right to appoint three members to JMMC’s board of directors. A Saint Francis Care spokeswoman, Fiona Phelan, declined to provide any details about the financial terms of the newly proposed transaction, which must be approved by the state’s hospital regulators and attorney general. She said officials at both nonprofit companies had agreed to keep the exact terms “proprietary and confidential.” The spokeswoman also said there are no plans to make any changes in management or to close any facilities in connection with the deal, that day-to-day operations at Johnson Memorial Hospital are expected to “continue uninterrupted,” and that in the interim JMMC will continue to provide services on a “business-as-usual basis.” After the deal is completed, she added, JMMC employees would become employees of a wholly owned subsidiary of Saint Francis Care and “eligible employees” would be offered a benefits package. Phelan offered no details about the pension obligations or other costs Saint Francis Care might assume in the buyout. Nevertheless, in a prepared statement issued Wednesday, the hospital officials said their deal would “clear the way for JMMC’s continued financial strength and stability.” “After discussions among JMMC’s board of directors, lenders, government agencies, and multiple advisers, a pre-planned and voluntary reorganization under a Chapter 11 bankruptcy filing was collectively determined as the most efficient and expedient process to proceed with the business transaction under the terms negotiated, which include a debt restructuring,” they said. “The terms of the transaction will allow JMMC to emerge from this process with less debt and the deepened relationship with Saint Francis Care will help to achieve the goal of becoming a stronger, more financially sound hospital, well-positioned for the future,” they added. Johnson Memorial Hospital was among only five Connecticut hospitals that ended the last fiscal year with a negative total margin, which state regulators put at a negative 4.94 percent. The JMMC system had a negative 3.11 percent total margin. The Saint Francis Care system, on the other hand, had a 4.05 percent positive margin, which means that it kept as “profit” just over 4 cents for each dollar of revenue. Saint Francis Care was one of the hospital systems that had bid to buy Eastern Connecticut Health Network and its Manchester Memorial and Rockville General hospitals. Peter Karl, the president and CEO at ECHN, said last year that it had dropped Saint Francis from consideration after a plan by Saint Francis to combine with a for-profit chain affiliated with the nation’s biggest Catholic health care system, Ascension Health Care Network in Missouri, “fell apart.” ECHN subsequently agreed to sell itself to Tenet Healthcare Corp., a for-profit hospital chain based in Texas, which last month withdrew its application for state approval of the deal after regulators said it could go forward only if a series of “conditions” were met. January 15, 2015 Kelly Gooch Financial Management Johnson Memorial Medical Center eyes bankruptcy in transaction with Saint Francis Care Stafford Springs, Conn.-based Johnson Memorial Medical Center announced approval of an asset purchase agreement with Hartford, Conn.-based Saint Francis Care. Johnson Memorial Medical Center is seeking Chapter 11 bankruptcy in the deal, under which Johnson Memorial Medical Center would become a wholly-owned subsidiary of Saint Francis Care. "After discussions among (Johnson Memorial Medical Center's) board of directors, lenders, governmental agencies and multiple advisors, a pre-planned and voluntary reorganization under a Chapter 11 bankruptcy filing was collectively determined as the most efficient and expedient process to proceed with the business transaction under the terms negotiated, which includes a debt restructuring," Johnson Memorial Medical Center said in a prepared statement. Specific terms of the deal were not addressed in a joint news release. However, the release does say the terms "will allow (Johnson Memorial Medical Center) to emerge from this process with less debt" and that "the deepened relationship with Saint Francis Carewill help to achieve the goal of becoming a stronger, more financially sound hospital, well-positioned for the future." The agreement still requires regulatory approval. Johnson Memorial Medical Center and Saint Francis Care already have an affiliation agreement, which both sides signed in July 2012. Johnson Memorial Medical Center serves as the parent organization of Stafford Springs-based Johnson Memorial Hospital, Evergreen Health Care Center in Stafford Springs; Home & Community Health Services in Enfield, Conn.; and Johnson Health Care in Enfield, while Saint Francis Care serves as the parent company of Saint Francis Hospital and Medical Center in Hartford, as well as Mount Sinai Rehabilitation Hospital in Hartford and its other providers, according to a news release. January 15, 2015 Johnson Memorial Medical Center Announces Approval of Asset Purchase Agreement with Saint Francis Care On January 14, 2015, Johnson Memorial Medical Center (“JMMC”) announced the approval of an Asset Purchase Agreement with Saint Francis Care. After discussions among JMMC’s Board of Directors, lenders, governmental agencies, and multiple advisors, a pre-planned and voluntary reorganization under a Chapter 11 bankruptcy filing was collectively determined as the most efficient and expedient process to proceed with the business transaction under the terms negotiated, which includes a debt restructuring. This will clear the path for JMMC’s continued financial strength and stability. The terms of the transaction will allow JMMC to emerge from this process with less debt, and the deepened relationship with Saint Francis Care will help to achieve the goal of becoming a stronger, more financially sound hospital, well-positioned for the future. Patient care will not be interrupted and JMMC will continue to deliver high quality care to the community. “Throughout our working affiliation, JMMC and Saint Francis Care have been on the path of creating a long-term partnership,” said Stuart E. Rosenberg, President and Chief Executive Officer at JMMC. “One of the achieved goals from our partnership with Saint Francis has been the ability to continue our mission as we have for the last 102 years, providing quality healthcare in the community. Johnson Memorial Medical Center will be a key member of an integrated system of care.” JMMC and Saint Francis Care signed an Affiliation Agreement in July 2012, resulting in a mutually beneficial relationship that has provided the community with a sustainable, high-quality healthcare resource. As a result, JMMC has recently experienced improved operations by all measures of financial performance. “Our current affiliation agreement provides the framework necessary to ensure the continued delivery of quality care to the local community and sustain a major economic resource for the region,” said Christopher Dadlez, President and Chief Executive Officer, Saint Francis Care. “Recently we have watched JMMC stabilize and strengthen its operations. Both parties are enthusiastic about the next steps ahead.” Under terms of the Asset Purchase Agreement, JMMC would become a wholly-owned subsidiary of Saint Francis Care as part of a clinically integrated healthcare delivery system. Any finalized agreement will be contingent upon regulatory approvals, including by the Office of Health Care Access, and Office of the Attorney General of the State of Connecticut. A Certificate of Need will be filed, as required, to initiate the review process. Monday, January 12, 2015 Jack Sheedy Hospital looks ahead to merger, looks back on Archbishop Mansell's Leadership January 2014 Saint Francis Care in Connecticut plans to join Trinity Health Hartford, Conn.-based Saint Francis Care will become part of Trinity Health as Trinity Health forms a regional, nonprofit Catholic health care system in New England that also will include another Trinity Health system, the Sisters of Providence Health System in Springfield, Mass. Saint Francis Care and Trinity Health announced their definitive agreement Dec. 17, after eight months of discussion. Financial terms were not disclosed. Dr. Richard Gilfillan, Trinity Health's president and chief executive, said the new collaboration will improve care coordination in the region, leading to improvements in patients' health. Springfield is about 25 miles north of Hartford. Trinity Health will invest at least $275 million in the new regional ministry over five years once the deal is complete. Trinity Health and Saint Francis Care leaders said part of those funds will be for bricks-and-mortar improvements to facilities, and much of it will be to improve care across the continuum including by funding information technology or ambulatory settings to advance population health in the region. Livonia, Mich.-based Trinity Health is one of the nation's largest Catholic health care systems, providing patient care in 21 states at 86 hospitals and 128 continuing care facilities. Saint Francis Hospital and Medical Center is a teaching hospital affiliated with the University of Connecticut School of Medicine and licensed for 617 beds. Saint Francis Care includes the Mount Sinai Rehabilitation Hospital, a 60-bed hospital; and Saint Francis/Mount Sinai Regional Cancer Center. Sisters of Providence Health System includes Mercy Medical Center, a 182-bed acute care hospital in Springfield; and the 126-bed Providence Behavioral Health Hospital in Holyoke, Mass. Leadership moving forward Christopher Dadlez, president and chief executive of Saint Francis Care, will lead the new regional health care system, which has not yet been named. Daniel P. Moen will continue as Sisters of Providence Health System president and chief executive and be involved in the formation of the new regional ministry, according to the systems. A new regional board will be created for the regional health care system, with existing local boards serving in an advisory capacity, system leaders said. Dadlez said Saint Francis Care realized a few years ago that it needed to become part of a larger organization due to changes under health reform and due to increased focus on caring for the health of populations. Despite growing income from operations by about 40 percent in the last fiscal year, profit margins have hovered at about 2 percent, he said. "It's been a beautiful thing (to) meet Trinity and find out our strategic plans are aligned almost 100 percent; our direction and vision are aligned, and we're about creating in health care a people-centered environment focusing on both our community and the people we serve in a Catholic tradition." Saint Francis Care will be Trinity Health's first hospital in Connecticut; Trinity Health owns The Mercy Community, which includes Saint Mary Home, a skilled nursing home, and The McAuley, a continuing care retirement community, colocated on a 65 acre campus in West Hartford. Saint Francis Care previously had been in talks to become part of Ascension Health Care Network, a for-profit arm of the St. Louis-based Catholic nonprofit Ascension. Dadlez called Ascension a "great organization," but said he thinks Trinity Health is a better fit for Saint Francis Care, which will remain a nonprofit. Saint Francis Care is currently sponsored by the Archdiocese of Hartford, which approved the agreement. The deal still needs approvals required by canon law, and regulatory approvals from state and federal agencies. Saint Francis Care will be transferred to sponsorship by Trinity Health's sponsor, Catholic Health Ministries. The systems said they hope to complete the deal late this year. SAINT FRANCIS ANNOUNCES EXECUTIVE APPOINTMENT Matthew R. Kenney, Ph.D., Named as Vice President, Mission & Ethics (Hartford, CT – January 9, 2015) – Saint Francis Care has named Matthew R. Kenney, Ph.D., to the position of Vice President, Mission & Ethics. In this role, Dr. Kenney is responsible for promoting and integrating Saint Francis’ Mission and Core Values to help create an ethical, spiritual and healing environment throughout the Hospital system. Dr. Kenney was appointed interim Vice President, Mission Integration in April, 2014. He joined Saint Francis as a Clinical Ethicist in 2012. Prior to joining the Saint Francis family he served as Executive Assistant to the President and Assistant Vice President for Mission and Catholic Identity at Sacred Heart University, Fairfield. Dr. Kenney holds a Ph.D. in systematic theology, along with a certification in bioethics from the Center for Health Care Ethics at Duquesne University. He teaches both graduate and undergraduate courses in bioethics at Sacred Heart University in Fairfield, as well as advance practice nursing ethics and theology courses at the University of Saint Joseph, West Hartford. Dr. Kenney also serves as a consultant at St. Vincent’s Medical Center in Bridgeport and St. Mary’s Hospital in Waterbury. He has presented ethics grand rounds and workshops on a wide range of bioethical issues ranging from ethical considerations at the origin of life to withholding and withdrawing medical treatment, and has provided expert testimony to various state legislatures on a range of ethical issues. Saint Francis Receives W.K. Kellogg Foundation Grant for Breastfeeding Program $498,980 to support a peer counseling program (Hartford, CT – December 29, 2014) - Saint Francis Hospital and Medical Center, in partnership with The Hispanic Health Council, has received a $498,980 grant from the W.K. Kellogg Foundation to expand a “Breastfeeding: Heritage and Pride” program to low-income AfricanAmerican and Hispanic mothers who are patients at the Saint Francis Center for Women’s Health. The breastfeeding program, developed and currently delivered in other Hartford neighborhoods by The Hispanic Health Council in partnership with Hartford Hospital, recruits, trains, and hires women from Hartford’s low-income neighborhoods who have successfully breast-fed their own infants for at least six months. The rigorous training prepares these women to become breastfeeding peer counselors. “Breast milk is the perfect food for babies,” said Walter Trymbulak, M.D., Ph.D, Director of the Center for Women’s Health. “Low-income women in Hartford have the lowest rates of breastfeeding in the state. This grant will help us change the culture of formula-feeding the babies of the women who use our Center.” The Center for Women’s Health located at 1075 Asylum Avenue and its satellite office in the Burgdorf Health Center provide full service obstetric and gynecologic care to the women of Hartford and the surrounding communities. The Center does over 12,000 patient visits each year and cares for over 600 pregnant women each year. In serving the Saint Francis mission the Center offers health and wellness programs to all women regardless of insurance status. Jose Ortiz, The Hispanic Health Council’s President and CEO, states, “We are delighted to have the opportunity to bring this important and evidence-based service to the patients at the Saint Francis Center for Women’s Health. This is another opportunity for the two organizations to partner in addressing health disparities.” Over a decade of studies has shown that “Breastfeeding: Heritage and Pride” raises the rates of 6month and 12-month breastfeeding in low-income African-American and Hispanic women in other sections of Hartford. Now, with the support of the Kellogg Foundation grant, mothers in Saint Francis’ neighborhoods will have the same high-quality peer counseling to help them overcome obstacles to breastfeeding. The peer counselors from “Breastfeeding: Heritage and Pride” will begin working with expectant mothers during their pregnancy, helping to educate them on the health and emotional benefits of breastfeeding for infants and mothers. After the babies are born, the peer counselors will visit the mother each day at Saint Francis and assist the Hospital’s certified lactation consultants in helping the mother initiate breastfeeding. When the mothers and their babies return home, the peer counselors make home visits to ensure that the breastfeeding is going well, to assist with any issues or problems that arise, and to offer continued encouragement to the new mother. The peer counselors are also available by cell phone at all times to answer mothers’ questions or to help solve any emergent problems. Studies have shown that intensive peer counseling increases the initiation and duration of breastfeeding, and is successful in populations that have historically low rates of 6-month and 12month breastfeeding. Peer counseling is even more effective when the counselors share the same racial/ethnic, economic and language background as the mothers they support. Counselors help mothers overcome pain, discomfort, and feelings that the infant is not receiving enough nutrition. Intensive peer counseling in guiding mothers during the first six months of exclusive breastfeeding also increases the probability that mothers will choose to fully breastfeed any additional infants they may have in the future. After six months of exclusive breastfeeding, the peer counselors help mothers introduce appropriate baby foods and remain as a resource for mothers who decide to continue supplementary breastfeeding to 12 months. Research has established that breast milk is the ideal “first food” for infants. In the first few days after birth, the antibody Secretory Immunoglobulin-A is present in large amounts in colostrum (the early milk). This and other antibodies in breast milk strengthen the baby’s immune system. Breast milk: is easier to digest; protects against diarrhea and constipation; reduces the risk of Sudden Infant Death Syndrome; decreases the risk of asthma, respiratory infections, allergies, and eczema; contains essential nutrients for the development of the brain, eyes, and nervous system; helps in the development of the mouth and jaw; increases the baby’s feeling of comfort and reinforces a strong emotional bond with the mother. Research also shows that breast-fed babies: are less likely to be overweight or obese in childhood; are less likely to develop childhood cancers and diabetes; may have fewer behavioral, psychological, and learning difficulties as children; may have increased intelligence levels compared to formula-fed children; and have lower LDL cholesterol and lower blood pressure in childhood. Pediatricians recommend exclusive breastfeeding up to six months and complementary breastfeeding up to 12 months. January 14, 2015 Anne-Gerard Flynn Johnson Memorial Medical Center plans bankruptcy to become part of Saint Francis Care 0 Sisters of Providence Health System, which includes Mercy Medical Center, is part of Trinity Health, which has entered into an agreement to purchase Hartford-based Saint Francis Care and form it into a regional health system with the Sisters of Providence. Today, Saint Francis Care announced that it reached an agreement to purchase the assets of Johnson Memorial Medical Center, which could also make JMMC part of the regional system. (REPUBLICAN FILE) The emerging pattern in the delivery of health care, in this age of accountable and affordable care, is for smaller hospitals systems to merge with bigger ones. In December, Michigan-based Trinity Health, the country's second largest non-profit health system, announced it had signed a definitive agreement for Hartford-basedSaint Francis Care to join its system. Today, another Connecticut-based system, Johnson Memorial Medical Center,announced plans to file for Chapter 11 bankruptcy protection to allow it to become a subsidiary of Saint Francis Care. Johnson Memorial has been in a two-year affiliated arrangement with Saint Francis Care. "Throughout our working affiliation, JMMC and Saint Francis Care have been on the path of creating a long-term partnership," said Stuart E. Rosenberg, Johnson Memorial Medical Center president and chief executive officer, in a center release. In the same release, the head of Saint Francis Care described both systems as being "enthusiastic" over the next steps, which include a review and state approval of the asset of purchase agreement between the two. This is the second time Johnson Memorial has sought bankruptcy protection to restructure debt. "Our current affiliation agreement provides the framework necessary to ensure the continued delivery of quality care to the local community and sustain a major economic resource for the region," said Christopher Dadlez, president and chief executive officer, of Saint Francis Care. "Recently we have watched JMMC stabilize and strengthen its operations. Both parties are enthusiastic about the next steps ahead." Johnson Memorial Medical Center is the parent organization of several Connecticutbased facilities including Johnson Memorial Hospital and Evergreen Health Care Center, both in Stafford Springs, and Home & Community Health Services, in Enfield. JANUARY 13, 2015 Saint Francis creates affiliated post-acute care network Saint Francis HealthCare Partners (SFHCP) has formed an affiliated Post-Acute Care Network to offer patients of Saint Francis Care a high-quality, highly efficient network of preferred providers to enhance the transition from hospital care to post-acute care. This affiliated provider network will include the full continuum of post-acute care services, including long-term acute care, inpatient rehabilitation, skilled nursing, and home health and hospice. The Saint Francis HealthCare Partners affiliation with these providers helps ensure that patients will receive post-acute care and rehabilitation services in collaboration with their medical team at Saint Francis Hospital and Medical Center, as well as their primary care providers. Selection criteria for participation in the network included Centers for Medicare and Medicaid Services (CMS) quality scores, readmission rates, availability of specialty clinical programs/capabilities, other quality criteria, and proximity. To facilitate ease of planning, the affiliated providers will have access to patient information through the Saint Francis electronic medical records (EMR) EpiCare software. The EMR at Saint Francis is a single point of data entry for patient medical services, providing medical history for each patient. “Our goal was to select a group of affiliated providers to help enhance the transition from hospital care to post-acute care for our patients,” said Jess Kupec, President and Chief Executive Officer, Saint Francis HealthCare Partners. “This network will match patient needs with the right level of care to improve transitions of care, help reduce readmissions, and improve overall patient outcomes.” “As hospitals and physicians look to manage patients across care settings, post-acute providers play a vital role in building an effective continuum of care,” said Adam Silverman, M.D., Vice President, Ambulatory Strategy and Development, Saint Francis Care. “Our goal is to provide our patients and their families with the peace of mind that everyone is working toward providing the best possible care plan with the goal of getting the patient better, faster.” Patients and families always have the right to select a post-acute provider of their choice. They will continue to be offered provider options based on their individual clinical needs. SFHCP will be working with providers in the post-acute network to develop protocols for admission, patient education, coordination with the patient’s primary care provider, and facility discharge. Members of the affiliated Post-Acute Care Network are: · Long-Term Acute Care Hospital: Hospital for Special Care in New Britain · Inpatient Rehabilitation Facility: Mount Sinai Rehabilitation Hospital in Hartford · Skilled Nursing Facilities: o Avon – Avon Health Center o Bloomfield – Touchpoints at Bloomfield o East Hartford – Riverside Health and Rehabilitation Center o Glastonbury – Glastonbury Health Care Center o Manchester – Touchpoints at Manchester o Simsbury – McLean o Stafford Springs – Evergreen Health Care Center o West Hartford – Hughes Health and Rehabilitation; The Reservoir; Saint Mary Home; West Hartford Health and Rehabilitation Center o Windsor – Kimberly Hall South · Home Health and Hospice: Masonicare Partners and Masonicare Home Health and Hospice 01/15/2015 Sara Randazzo Business & Economy Connecticut Hospital Heads Back into Chapter 11 A Connecticut hospital put itself under Chapter 11 protection on Wednesday with plans to sell itself to a nearby healthcare system, five years after an unsuccessful bankruptcy reorganization left it saddled with $40 million in debt. Johnson Memorial Medical Center Inc. and five affiliates filed for bankruptcy in U.S. Bankruptcy Court in Hartford, Conn. with a sale agreement in hand to turn over its entire operation, including a 92-bed hospital, 180-bed skilled nursing facility and hospice-care services arm, to Saint Francis Care Inc. "The path to the proposed sale has been a long and difficult one," the hospital said in court papers, citing years-long financial difficulties caused by a shrinking number of patients, lack of capital, regulatory changes in the health care industry and an unsustainable level of debt. David Neier, a bankruptcy partner at Winston & Strawn LLP who often works on healthcare reorganizations, said the proposed sale is the latest example in a wave of hospital consolidation that started around 2008. "The day of regional hospitals is becoming less and less," Mr. Neier said, citing technological and pharmaceutical advances that prevent patients from needing lengthy hospital stays. "Hospitals are becoming less necessary." Johnson Memorial has been trying to find a buyer since at least 2008, when it first filed for bankruptcy. A proposed suitor at that time, Eastern Connecticut Health Network, backed out, and the health system reorganized itself through Chapter 11 as an independent health care organization. Since then, it has continued to ask five of the largest health systems in Connecticut to bail it out, according to court documents. Saint Francis, one of the Connecticut healthcare systems, agreed in 2012 to enter into an agreement to provide clinical and management support to Johnson Memorial as well as pay off a few million dollars of its debt. Now, Saint Francis plans to assume more than $17 million of Johnson Memorial's debt, pay $800,000 in obligations, assume its union contract and pay $1.25 million in cash for administrative expenses, among other contingencies. The sale, which is expected to protect the jobs of most of Johnson Memorial's 970 employees, is subject to regulatory and bankruptcycourt approval. The agreement also requires Saint Francis to put down a $750,000 deposit it would get back as a break-up fee if another buyer comes forward and consummates a deal instead. As part of the agreement, Saint Francis said it plans to invest $13 million into capital improvements and new technology within the first three years of its ownership. Johnson Memorial owes $29 million in bank loans to the People's United Bank, $4.5 million to Healthcare Finance Group LLC and $6 million to the Pension Benefit Guaranty Corp. and other unsecured creditors from its first bankruptcy proceedings, filings show. The not-for-profit health system brought in more than $94 million in revenue last year but has been operating at a loss. The hospital is asking for bankruptcy-court approval to take on up to $7 million in financing from Healthcare Finance Group, which would roll up some of its pre-bankruptcy debt. Johnson Memorial also asked for the ability to maintain its cash management system, pay its employees and process refunds to patients who gave advanced payments for services. The case, numbered 15-20056, has been assigned to Judge Albert Dabrowski. January 14, 2015 Johnson Memorial Declaring Bankruptcy, Being Purchased By Saint Francis (CBS Connecticut) – Johnson Memorial Medical Center in Stafford Springs is declaring chapter eleven bankruptcy to reorganize. The Stafford Springs hosptial is being purchased by the parent company of Saint Francis Hospital. Johnson Memorial President Stuart Rosenberg says patient care will continue as normal. “There will be no impact to the quality of patient care at Johnson. It is business as usual during the process,” Rosenberg said. Rosenberg says layoffs have not been considered. The deal must still be approved by state regulators. Tough economic conditions have prompted small hospitals across Connecticut and the country to merge or affiliate with larger hospitals in recent years. Rosenberg says reductions in federal and state reimbursement for patient care has prompted reorganizations of services and expenses. JANUARY 12, 2015 LUCY NALPATHANCHIL Chemotherapy Refusal Is at Center of Connecticut Case -- But What Is Chemo? No matter what type of treatment a patient decides on, there are short- and long-term consequences. The story of a Connecticut girl fighting for the right to choose how to treat her cancer has filled the headlines. Cassandra C's case centers on her refusal of chemotherapy. Chemotherapy is one of the more common treatments for cancer. Dr. Adam Boruchov is an oncologist at Saint Francis Hospital in Hartford. He explained that chemotherapy is used when cancer is widespread in a person's body, because the chemicals can go into the blood system and travel throughout the entire body. These therapies kill actively dividing cells in the body, like cancer cells, Boruchov said. "It's kind of like when you put a pizza in a room with a bunch of hungry people," he said. "If the pizza has poison, the hungrier people who eat the most pizza are going to get the most poison." That's how chemotherapy works, Boruchov said. "If you put it in the body, the cells most actively dividing are going to take up the most chemotherapy, and be destroyed." But chemotherapy also produces side effects, Boruchov said, because there are other cells in our bodies that also rapidly divide. "Normal cells such as the immune system, or the skin, or the gastro-intestinal tract, can also take up some of the A rendering of blood cells in the body. toxin, and therefore the cells there Credit Purestock / Thinkstock can die," he said. "We can get side effects such as suppression of the immune system, or nausea, vomiting, diarrhea, or even the hair falling out." Boruchov specializes in treating leukemia and lymphoma, or blood cancers. He said treatment options for those are different from solid organ cancers like lung and breast. When talking about chance of survival with his patients, he said he discusses how and when to treat cancer. "What we always talk about is Risk Benefit Ratio, because sometimes we can treat and make cancer go away but we don’t necessarily have to and the side effects that would be brought on aren’t necessarily worth it. So why expose someone to needless side effects if you’re not going to cure them of the disease?" Boruchov said. "On the other hand, there are certain types of aggressive lymphomas and leukemias [which], if not treated, are lethal. In that setting, if we do nothing, we know that alternative is death, and that is clearly unacceptable, so we offer chemotherapy options." No matter what type of treatment a patient decides on, there are short- and long-term Chemotherapy has negative side effects, consequences, from nausea to organ damage, to like nausea. a chance for new cancer later in life. Boruchov Credit christine.gleason / Creative Commons stressed that in medicine, particularly in oncology, "nothing is for free; nothing is without its side effects." Below is more from our conversation with Boruchov: WNPR's Lucy Nalpathanchil: What are the short-term and long-term side effects for someone going through chemotherapy? Dr. Adam Boruchov: One of the most common side effects of most chemotherapies is lowering of the blood counts, and lowering of the red blood cells, which can make people tired and anemic. There are some therapies we can do for that. One of the simplest is a blood transfusion. Lowering of the platelets can make patients have easy bleeding or bruising, and we can give them platelet transfusions. Lowering of the white blood cells is the most dangerous, because that sets people up for lifethreatening infections. So one of the newer developments in recent years are some of the supportive therapies that we have to manage these side effects. For example, there's a white blood cell growth factor we deliver right after chemotherapy to help rescue the white blood cells, to minimize the time that patients have low white blood cell counts to minimize their chance of infections. And long-term side effects? The most bizarre side effect to talk about with a patient is not a very common side effect. Many chemotherapies can cause a secondary leukemia, or another blood cancer. So you are getting rid of one blood cancer, and can get another blood cancer, but that is rare. I'm always up front with patients [that] that can happen. Some other side effects of chemo and radiation, in combination, are long-term damage to the heart. Or a patient can get a side effect in the short term that is long-lasting, such as neuropathy, which is damage to the nerve tissue. There are other times that chemotherapy can cause damage in the short term that is long lasting. For example, some chemotherapies can cause damage to organs, such as the liver, or the kidney, or as I said before, the heart, or even the lung, and those can be life-long damage. How do you talk about chance of survival with a patient? Oncologists read about data in terms of percentages and overall survival, or median survival, at five years. These are ways to look at previous studies with patients. It’s an important way to frame it, but in the end, there’s no such thing as 20 percent survival. You're either surviving, or not. For any given patient, it’s either going to work or not work. Those numbers are really used when looking at thousands of patients. It's very misleading to use those averages or median survival. Because when you are sitting in a room one-on-one with a patient, it's just one patient. They were not 1,000 patients on those previous studies. What I do, is I say: is there a chance for a cure? Yes or no. If there is: how big of a chance; is it worth going through? How do you compare cancer treatments 30 years ago to today? There's been great developments not only in chemotherapies, but in the different types of surgeries we do. Even radiation therapies have changed. There's new chemotherapies; there's immune therapies; there's vaccine therapies; there's a whole host of therapies. Even supportive therapies -- the medicines to treat or prevent nausea -- are amazing; 2015 is a new time in oncology. There's a lot of reasons to look forward to the future Jan 13 201509:21AM ET WTIC-FOX Hartford-New Haven, CT St Francis Hosp-Kara Moscato-DASH Diet Play and Download File TRANSCRIPT CLIENT: ST. FRANCIS HOSPITAL STATION: WTIC-TV PROGRAM: FOX CONNECTICUT NEWS DATE/TIME: 1/13/14 SUBJECT: LENGTH: NIELSEN AUDIENCE: CALCULATED AD VALUE: PUBLICITY VALUE: 9:00 AM KARA MOSCATO – DASH DIET 4:39 12,849 $919.30 $2757.90 ANCHOR: Welcome back. It’s called the DASH Diet, and if you aren’t familiar yet, you’re about to learn all about it. The DASH Diet, rich in vegetables, whole grains and low-fat dairy has been named the best overall diet for the fifth consecutive year, outpacing Weight Watchers and the Mediterranean Diet, according to US News and World Report. Now, if your New Year’s resolution is to lose weight and get healthy, this could be for you. This could be your year. So to explain all about the DASH Diet is Registered Nurse Kara Moscato, with the Hoffman Heart and Vascular Institute of Connecticut at St. Francis Hospital. Thanks so much for being with us Kara. KARA MOSCATO, ST. FRANCIS HOSPITAL: Thanks for having me, yes. ANCHOR: All right, so talk about the DASH Diet for those who are not familiar at all, and what sets it apart from any other diet? MOSCATO: Sure. So the DASH Diet stands for Dietary Approaches to Stop Hypertension. It was actually established from a study that was conducted by the National Heart, Lung and Blood Institute. And basically, what they found was that a diet that’s low in saturated fat, low in dairy, low-fat dairy rather, low in sodium, actually helps decrease your blood pressure. ANCHOR: Now, how is this different from somebody who maybe already thinks they eat generally healthy, lower in fat, they do drink some dairy, you know, low-fat milk, things like that. MOSCATO: It’s actually very similar to the dietary guidelines for Americans. It’s a little teeny bit lower in saturated fat content. And what’s nice about it is that it gives you specifics for sodium. Usually what it does, once you determine your calorie level, you can do either a fifteen hundred milligram or a twenty three hundred milligram sodium diet. And as most people know, sodium is very high in pretty much our diet in America today, because sodium is in almost everything. ANCHOR: It is. MOSCATO: So it’s very hard to stick to a low sodium diet. ANCHOR: All right, so what would you say to somebody who wants to get on the diet. Do they have to make some major changes? I guess it depends on what they’re doing right. MOSCATO: Well, first of all, I would probably recommend they start gradually. I know for some people, the planning ahead piece might be a little difficult, so maybe just start gradually by maybe writing in what you’re eating, and then kind of make some small changes to your diet, like adding in a fruit or a vegetable, and then start to kind of increase the serving sizes and things like that. ANCHOR: Now, I have to imagine this might be a little bit easier to stick to. There are other diets that you completely cut out carbs, all high-protein. So since you are still able to eat whole grains, you’re able to eat some low-fat, some dairy, people might find ‘Hey, you know what, I can do this one.’ MOSCATO: Yes, yes. That’s what I like about it, actually. You know, it doesn’t restrict your food groups, which is nice. So the fact that it’s not restrictive, I know for me personally, if you told me not to eat a certain food group or eliminate a food, I might actually want it more. So this is actually telling me, you can eat all foods, it’s just really practicing moderation with a big emphasis on your fruits and vegetables and fiber. ANCHOR: I can imagine it’s really re-examining portion size as well. MOSCATO: Yes, absolutely. And that’s one thing I like about it as well, is that once it determines your calorie level, it gives you serving sizes from each food group. ANCHOR: So break down like a day’s worth of menu items for us, real quickly. Like, as far as what you would do for breakfast, lunch and then dinner, and snacks in between. MOSCATO: Sure, absolutely. So basically what you would do is, it really emphasizes your whole grains, so doing like a whole grain cereal, like a high fiber bran flake, or an oatmeal, adding in some fruits and maybe some blueberries, and maybe some low-fat dairy, so maybe like a low-fat yogurt or something for breakfast. Some healthy snacks might be just a small handful of almonds. Lunch would be something like a lean piece of meat. You know, lean protein meaning low in saturated fat, so removing the skin off the chicken, removing any visible fat you see on a piece of meat, a little bit of whole grain, and then big on the vegetables. Snacks should really be more fruits and vegetables, and dinner kind of the same principle, a little bit of lean meat, some whole grain and some fruit or vegetable. ANCHOR: And this sounds like a diet that kids can very easily sort of transition to, if they’re trying to sort of maybe shift to a healthier lifestyle in general, because they can still have cereal with milk, they can have fruits… MOSCATO: Absolutely. ANCHOR: Vegetables, sandwiches even maybe. Right? Would you say? MOSCATO: Sure. Really anyone can do the diet if they wanted to. ANCHOR: Yeah. So for some more information, folks can head to the website, right? MOSCATO: Absolutely, yes. ANCHOR: What is it? Your website at St. Francis, right? MOSCATO: Yeah, you go to stfranciscare.com, and you can actually go onto the Hoffman Heart website. Or you can just go on to any, you know, looking for the DASH Diet. DASH Diet itself actually has its own website as well. If you go onto the National Heart, Lung and Blood Institute, which is NHLBI as well, and you can find some information. ANCHOR: Any last final tips for our viewers before we leave? MOSCATO: Bottom line, moderation is key. You know, don’t eliminate food groups from your diet, big on the fiber, fruits and vegetables is really key. ANCHOR: I have to imagine, don’t give up, if you slip up once, it’s not that big of a deal. MOSCATO: Exactly. ANCHOR: You get back up there. MOSCATO: Keep moving forward, yes, absolutely. ANCHOR: You can do it. All right Kara, thanks so much for being with us, appreciate it. MOSCATO: Thank you so much. Jan 15 201505:48AM ET WVIT-NBC Hartford-New Haven, CT St Francis Hosp-Proposed purchase of Johnson Memorial Medical Ctr Play and Download File TRANSCRIPT CLIENT: ST. FRANCIS HOSPITAL STATION: WVIT-TV PROGRAM: NBC NEWS CONNECTICUT DATE/TIME: 1/15/15 SUBJECT: JOHNSON MEMORIAL HOSPITAL LENGTH: :24 NIELSEN AUDIENCE: 27,722 CALCULATED AD VALUE: $59.97 PUBLICITY VALUE: 5:00 AM $179.91 ANCHOR #1: Turning now to your Business News. ANCHOR #2: Here’s some of the Greater Hartford’s top business stories. Johnson Memorial Hospital in Stafford Springs has filed for Chapter Eleven bankruptcy. The move will allow them to become part of the St. Francis network. They’ll also be able to restructure their debt, which is reportedly between ten million and fifty million dollars. Johnson and St. Francis have been affiliated since 2012. Jan 15 201506:50AM ET WTIC-AM Hartford-New Haven, CT St Francis Hosp-Hosp Observation Status-Sharon Gothea Play and Download File TRANSCRIPT CLIENT: ST. FRANCIS HOSPITAL STATION: WTIC-AM PROGRAM: RAY DUNAWAY SHOW DATE/TIME: 1/15/15 SUBJECT: LENGTH: NIELSEN AUDIENCE: CALCULATED AD VALUE: PUBLICITY VALUE: 6:00 AM HOSPITAL OBSERVATION STATUS 5:39 24,100 $1231.36 $3694.08 RAY DUNAWAY, HOST: So here’s the problem. Sharon Gothea is with us. She’s a Registered Nurse and she is a Patient Advocate. How long have you been doing this? SHARON GOTHEA, RN, PATIENT ADVOCATE: About seven years. DUNAWAY: Wow. GOTHEA: Well actually my whole life, because I’ve been a nurse a long time. DUNAWAY: Well, you’re a nurse, yeah. GOTHEA: All nurses make great advocates. But I started a nursing practice about seven years ago. This wrapped around advocacy and coordination of care. DUNAWAY: You know, I think a lot of times, in a case that you and I were talking about off the air, or an example would be, let’s say for example, your family’s all out in California. GOTHEA: Right. DUNAWAY: Well, you need to be hospitalized, you need to be put in a nursing home, something of that sort, you know, you really, unless you’re going to do a lot of long distance, and then there’s the time difference and all that, it’s really nice to have somebody here that’s going to kind of work through this whole thing. GOTHEA: Right, I think it evolved into us being the voice for that person. So you’re correct, most of our population started off with a son or a daughter that lives out-of-state, and their mom or dad end up in the hospital. So they initially know that they’re there, may not know the reason, and two days later get a call from mom that says the doctor came in and just discharged them. And they’re kind of in a panic because they don’t know what that means. DUNAWAY: So will you help them with other things? In other words, if they do kick you out, okay, then, you know, you have to find someplace to put them. Do you work on that as well? GOTHEA: We work on the whole picture. So what we do, and nurses are again very good at that, is we have kind of a holistic approach. So, we’ve been credentialed in all the hospitals in Connecticut, which is the requirement and, for us to get involved. So we have great relationships with the staff, and we can go in and say ‘Okay, what’s going on?,’ find out what ‘home’ means, and it may be that it isn’t just a medical issue. And maybe what got them in there was they didn’t have the transportation to see the doctor, or they didn’t have the money to buy the medications, and kids are usually the last ones to find that out, so. DUNAWAY: Absolutely. GOTHEA: We look at the whole picture and then we put all that together for them. DUNAWAY: But I think one of the things we’re talking about this morning is, with the Affordable Care Act, aka ObamaCare, the ACA, aka ObamaCare, there’s been the creation of the Accountable Care Organizations. GOTHEA: Right. DUNAWAY: Now, what has that ended up doing to patients? GOTHEA: Well, I think the process on paper looked great, in that Medicare, it’s basically a Medicareguided program that’s said to physicians and hospitals, ‘We want you to coordinate care for those patients before they go to the hospital, to decrease readmissions. So typically, a few years ago, you would get someone who came in with an issue and maybe discharged a little early and go home, and then return with the same issue. Medicare now says they’re not going to pay you for that issue. Not all of them, but a percentage. So the Accountable Care Organizations were implemented basically as an umbrella, between the hospitals and the physician groups. And mostly the physician groups, if not all of them, that are now owned by the… DUNAWAY: …major hospitals. GOTHEA: Right, major hospitals. So let’s take St. Francis, for instance. They started Accountable Care Organization that created this umbrella between the hospital and the physicians. DUNAWAY: Right. GOTHEA: And that umbrella was supposed to, and is supposed to help coordinate care for those patients so that they’re connected back to the doctors. DUNAWAY: Once again, let’s go back to this whole thing, because we’ve talked about this on the air before. I don’t know if it was with you, but we have talked about this, and that’s that whole thirty day readmission penalty. GOTHEA: Correct. DUNAWAY: And so if you’re in the hospital being treated for something, and they then release you, and then you end up coming back, they get the amount of remuneration they get from, let’s say, Medicare. GOTHEA: Right. DUNAWAY: Is, fairly significant penalties? GOTHEA: Right. DUNAWAY: So, but there’s a little loophole they came up with. GOTHEA: Correct. So the loophole that I feel that they had come up with was that the number of observations increased. So people were showing up in the hospital, the hospitals were very well aware that if they got admitted and came back, there would be a penalty... DUNAWAY: Right. GOTHEA: …which is actually increased in January 2015. So I suddenly got calls from families frustrated because their loved one would end up on a unit, like they got admitted, and not know they weren’t. The problem with that is twofold: one is, it’s a benefit for the hospital. I believe, my personal opinion... DUNAWAY: Okay. GOTHEA: That if that person is under observation and not admitted, and they do show up within thirty days, then that isn’t counted as… DUNAWAY: No harm, no foul. GOTHEA: Right. The downside of that for the families is that if their loved one stayed for three days… DUNAWAY: This is good. GOTHEA: …and you know you need that three-day qualifier to go to rehab, they now come back to the families and say, ‘Mom’s ready to go. Oh, by the way, she was never admitted, she was under observation.’ DUNAWAY: So… GOTHEA: You now have to pay for the rehab. So Medicare did come on board and reevaluate that, and they have a two-night stay now, stating to the hospitals that if they stay two nights, they’re admitted. DUNAWAY: Okay. Well, I wish we had more time. You do have a website if guys would like to go. And Sharon if you want to share that with us. I have it up here somewhere, I don’t know where I put it though. GOTHEA: Yeah, it’s called patientadvocateforyou.com, and all our information is up there and it’s evolving. And thank you again for having me. DUNAWAY: Well, no, thank you. Let us know how this goes. GOTHEA: Absolutely. DUNAWAY: I love that little observation trick. And you can get stuck for the bill too. I mean, there are all kinds of things you can get stuck with. GOTHEA: Quite a bit. DUNAWAY: So guys, pay attention, it’s the way it’s going. Or call Sharon. Just do that. GOTHEA: It’s important. DUNAWAY: Yeah, it is. Jan 9 201510:00AM ET WTIC-AM Hartford-New Haven, CT St Francis Hosp-Dr Adam Boruchov-Chemotherapy Play and Download File TRANSCRIPT CLIENT: ST. FRANCIS HOSPITAL STATION: WTIC-AM PROGRAM: NEWS DATE/TIME: 1/9/15 SUBJECT: 10:00 AM DR. ADAM BORUCHOV - CHEMOTHERAPY LENGTH: NIELSEN AUDIENCE: CALCULATED AD VALUE: PUBLICITY VALUE: :39 10,500 $86.79 $260.37 HOST: This week’s State Supreme Court case on a seventeen year-old’s efforts to stop her cancer treatments dealt with the legal issues in the case, but it also brought up for discussion the medical aspects of the diagnosis. A doctor who is not associated with the treatment of Cassandra C, but who specialize in leukemias and lymphomas, says the type of cancer she has, Hodgkins lymphoma, is one of the most treatable. DR. ADAM BORUCHOV, ST. FRANCIS HOSPITAL: We often don’t use the ‘cure’ word in cancer, but Hodgkins lymphoma is one of those conditions where we have used that word for quite a while. HOST: That’s Dr. Adam Boruchov. He also points out that there have been great strides in the treatment of the side effects of the chemotherapy drugs. Jan 12 201504:32PM ET WNPR-FM St Francis Hosp-Dr Adam Boruchov-Chemotherapy Play and Download File TRANSCRIPT CLIENT: ST. FRANCIS HOSPITAL STATION: WNPR-FM PROGRAM: WNPR NEWS DATE/TIME: 1/12/14 SUBJECT: LENGTH: NIELSEN AUDIENCE: CALCULATED AD VALUE: PUBLICITY VALUE: 4:00 PM DR. ALAN BORUCHOV - CHEMOTHERAPY 2:09 11,300 $357.55 $1072.65 HOST: The story of a Connecticut girl fighting for the right to choose how to refuse chemotherapy has filled the headlines. As WNPR’s Lucy Nalpathanchil reports, chemotherapy is one of the more common treatments for cancer. LUCY NALPATHANCHIL, REPORTER: Doctor Adam Boruchov is a hemotologist at St. Francis Hospital in Hartford. He explains, chemotherapy is a chemical therapy that’s used when cancer is widespread, because the chemicals can go into the blood system and travel throughout the entire body. He says those therapies kill actively dividing cells in the body, like cancer cells. DR. ADAM BORUCHOV, ST. FRANCIS HOSPITAL: It’s kind of like if you put pizza in a room with a bunch of hungry people in there, and if the pizza has poison, the hungrier people who eat the most pizza are going to get the most poison. And that’s kind of how chemotherapy works. If you put it in the body, the cells that are most actively dividing are going to take up the most chemotherapy and be destroyed. NALPATHANCHIL: But chemotherapy also produces side effects, because Boruchov says there are other cells in our bodies that also rapidly divide. BORUCHOV: Normal cells, such as the immune system or the skin, or the GI tract can also take up some of this toxin. Therefore, the cells there can die and you can get side effects, such as suppression of the immune system or nausea or vomiting or even the hair falling out. NALPATHANCHIL: Boruchov specializes in leukemia and lymphoma for blood cancers, and says treatment options for those are different from solid organ cancers like lung and breast. He says when talking about chance of survival with patients, it’s important to discuss how and when to treat cancer. BORUCHOV: So why expose someone to needless side effects if you’re not going to cure them of the disease? On the other hand, there are certain type of leukemias or aggressive lymphomas that, if not treated, are lethal. In that setting, we say if we do nothing, we know the alternative is death. So we offer chemotherapy options. NALPATHANCHIL: Boruchov says no matter what type of treatment a patient decides on, there are short-term and long-term consequences, from nausea to organ damage to new cancers later in life. He stresses in medicine, particularly in oncology, nothing is free. Nothing is without its side effects. Lucy Nalpathanchil, WNPR News. Jan 2 201512:00PM ET WNPR-FM St Francis Hosp-Dr Ulysses Wu-Flu Play and Download File TRANSCRIPT CLIENT: ST. FRANCIS HOSPITAL STATION: WNPR-FM PROGRAM: WNPR NEWS DATE/TIME: 1/2/15 SUBJECT: LENGTH: NIELSEN AUDIENCE: CALCULATED AD VALUE: PUBLICITY VALUE: DR. ULYSSES WU - FLU 1:15 11,300 $207.87 $623.61 RAY HARDMAN, HOST: According to the State Department of Public Health, as of last week, four hundred and forty-four people had tested positive for the flu so far this season, with one hundred and eighty hospitalizations. No deaths have been reported so far. The DPH says the number of flu cases in Connecticut is higher than average for this time of year, but the rate of hospitalization is normal. Influenza A, or H3N2 has been the predominant strain so far this season, but there’s a hitch, according to Dr. Ulysses Wu, Chief of Infectious Diseases at St. Francis Hospital in Hartford. DR. ULYSSES WU, ST. FRANCIS HOSPITAL: What has happened with the H3N2 this year is that it has changed just a little bit, and that’s why the vaccine may not work as well this year. HARDMAN: Still, Dr. Wu says that’s not an excuse to skip the flu shot this season. WU: You should definitely get a flu shot. It still protects you from other types of influenza, and there’s the belief that it may attenuate your illness, so it’s maybe not going to be as severe. HARDMAN: The DPH says, last week Connecticut saw the highest levels of both outpatient and emergency room visits for people with flu-like symptoms so far this season. The Centers for Disease Control and Prevention report that flu cases are widespread in twenty-nine states. Ray Hardman, WNPR News. Developing Stories: Outcome: Patient Safety/Coverys Grant Contact: Fiona Phelan Saint Francis has received a $227,044 grant from Coverys Health Care Foundation to support patient safety training for perioperative teams in CT. WTIC Healthy Rounds interview to air Jan. 17. DASH Diet Contact: Fiona Phelan US News and World Report lists this as the top diet for 2014. Hoffman Heart Institute promotes this diet to lower blood pressure. Dr. Nissin Nahmias to be interviewed by NBC CT Jan. 18 @ 7:50 a.m. Bariatric Implant Contact: Fiona Phelan FDA has just approved an implantable device that curbs eating. Dr. Nissin Nahmias interviewed by WTNH about benefits, risks. Air date TBD. Drum Major for Justice Award Contact: Fiona Phelan Marcus McKinney to receive award from the Greater Hartford Interdenominational Ministerial Alliance, Inc. on Jan. 19 at Shiloh Baptist Church on Albany Ave. HealthGrades Contact: Fiona Phelan 2015 clinical excellence award announcement to be released. Press release to be issued Jan. 20. Topera FIRM-guided therapy Contact: Alix Boyle We are the only hospital in CT to combine the use of Topera with Stereotaxis, we provide the safest, most effective treatment for these disorders. NBC Lisa Carberg to interview Dr. Aneesh Tolat and patient Jan. 20 3D Tomosynthesis Contact: Fiona Phelan Dr. Niamey Wilson to be interviewed by C-HIT for online article on benefits of 3D tomosynthesis. Jan. 20. Coat Drive Contact: Alix Boyle Annual coat drive at Burgdorf Clinic. Media advisory to be issued. Jan. 21. Insurance Literacy Contact: Alix Boyle Rebecca Santiago will assist students at Capital Community College sign up for health insurance, Jan. 26. Hartford Courant, Hartford Business Journal interviews to be scheduled. Medical Ethics Contact: Fiona Phelan Pitch to WNPR interview with Matthew Kenney. Medical Ethics Advisor magazine to interview Dr. Kenney for upcoming article. Pet Therapy Contact: Fiona Phelan Patients at MSRH benefit from weekly visits from dogs trained to work with patients. Pitch to media. Flu Season Contact: Fiona Phelan Pitch stories as relevant. Winter Safety Contact: Fiona Phelan Snow shoveling, snow blower tips. Dr. Wolf. Thyroid Awareness Contact: Fiona Phelan January is Thyroid Awareness month. Pitch patient story to local TV outlets. Colonoscopy Screening Contact: Fiona Phelan Saint Francis GI Endoscopy LLC will be offering Saturday morning colonoscopy screenings at their Windsor location. Hospital Access Management Contact: Fiona Phelan Patient access success stories on new technology, retention, registration improvements, patient satisfaction. Blood Cancers Contact: Fiona Phelan Dr. Adam Boruchov to discuss blood cancers with Dr. Tony Alessi, WTIC 1080 AM Healthy Rounds, TBD. Transcatheter Aortic Valve Replacement Contact: Fiona Phelan New minimally invasive surgery to be offered in Hoffman Heart for patients with severe aortic stenosis. Waiting for patients. Bariatric Center of Distinction Contact: Alix Boyle Blue Cross Blue Shield has awarded the Bariatric surgery center as a center of distinction. Press release to be developed. Seasonal Affective Disorder Contact: Fiona Phelan Valley Press to interview Dr. Bruce Rothschild for article on Jan. 8. February publication. Pitch other media. Total Health Contact: Gina Munson/Fiona Phelan Clinically Integrated Network for population management. Press release to be issued TBD. Smilow Cancer Affiliation Contact: Fiona Phelan Definitive agreement with SFC and Smilow Cancer Hospital to be signed April. Press release to be developed. FastCare Contact: Fiona Phelan Opening of Manchester store slated for early April. Media materials to be developed. Women’s Infusion Center Contact: Fiona Phelan/Alix Boyle The Cancer Center has opened a six-chair infusion center in the CWHC for women. Ribbon cutting TBD. Ebola Contact: Fiona Phelan Pitch Saint Francis initiatives to media. Fragility Fracture Program Contact: Fiona Phelan Dr. Jeffrey Meter is introducing a program that coordinates care for elderly patients for develop fractures. 2nd program of its kind in New England. Press release to be developed. Contact Brad Davis, WDRC. ISO 9001:2008 Contact: Fiona Phelan Develop media opportunities to acknowledge CJRI ISO 9001:2008 certification. MS Study Improves Motor Function Contact: Fiona Phelan Dr. Lo study involving drug therapy to improve motor function among MS patients. Vitamin Water Contact: Fiona Phelan Sally Lerman interviewed by FoxCT about the nutritional value of drinks like Vitamin Water which is being sued over improper advertising of its healthy benefits. Air date TBD. IT Project Management Contact: Fiona Phelan Healthcare Business Insights interview with Linda Shanley on project management for IT projects. Publication TBD. Love Photo Shoot Contact: Fiona Phelan Hartford Magazine photo shoot for February issue on Love. Dr. Sam Buonocore photographed with his children. Discovery Fit and Healthy Contact: Fiona Phelan Discovery Channel interview with Dr. Bill Marshall about craniotomy he performed on woman rock climber who is back to climbing. Show will air Jan/Feb. Discovery Fit and Healthy Contact: Fiona Phelan Discovery Channel interview with Dr. Scott Ellner patient who amputated his arm. Airdate TBD. Seasons Magazine Contact: Alix Boyle Dr. Aneesh Tolat and Topera procedure, a-fib to be featured in spring issue. Interview conducted Dec. 24. Photo to follow. Connecticut Doctors Orchestra Contact: Alix Boyle Dr. Latha Dulipsingh plays cello in an orchestra comprised of Hartford-area physicians. Hartford magazine to publish article in March. Big Data Contact: Fiona Phelan Dr. Adam Silverman interviewed by Wall Street Journal on population health management, aging in place, risk assessment. Publication TBD Community Events Calendar – January 16, 2015 Event “Go Red” Celebration Date Time 2/6/2015 1:00 p.m. Location Rotunda - Hospital 3/19/2015 TBD 4/22/2015 2:30 p.m. PCT 1 – Rotunda 5/5/2015 6:00 p.m. Supplier Diversity Event 5/6/2015 9 a.m. – 3 p.m. Nightingale Event 5/7/2015 5:30 p.m. cocktails 6:00 p.m. dinner Annual Barbara Gordon Cocktail Party 6/10/2015 Travelers Championship 6/22 – 6/28/2015 Annual Living Our Mission and Sisters of Saint Joseph Awards Employee Service Awards 8 a.m. – 6 p.m. daily CT Convention Center Mahelys Banquet and Catering Facility, South Windsor CT Convention Center TPC River Highlands, Cromwell th 26 Annual SWING Golf and Tennis Outing This event celebrates Heart Month on both campuses. Lobby – Mt. Sinai Hartford Marriott Farmington, 15 Spring Farms Rd., Farmington Saint Francis HealthCare th Partners 13 Annual Conference Background 6/29/2015 Annual medical conference. Annual celebration and presentation of the Sisters of Saint Joseph and Living Our Mission Awards. Annual Celebration to acknowledge long term service of employees. Annual event to celebrate nursing. Annual backyard picnic hosted by Barbara Gordon – a cancer survivor and grateful patient. Staff from Saint Francis provide medical coverage, food tent coordination, and activities in the Fan Zone and Military Outpost during the tournament. To benefit Nursing Education and special programs at Mount Sinai. th 17 Annual Paul Karvoski memorial Golf Tournament th 6 Annual Curtis D. Robinson Celebrity Golf Classic th 6 Annual CHARLIE’s Ride MIRACLES Gala 8/1/2015 Funds raised during the Tournament go to the Men’s Health Institute Prostate Cancer fund 8/6/2015 8/2015 9/19/2015 rd 3 Annual Chip in for A Cure Golf Classic 9/28/2015 Tunxis Plantation To benefit the Curtis D. Robinson Center for Health Equity To benefit the Breast Center
© Copyright 2026