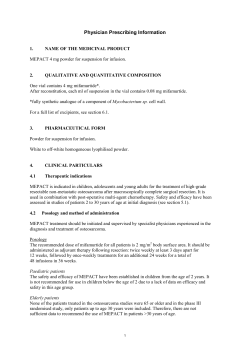
General Test Listing 1
General Test Listing 1 2 A1c A B See “Hemoglobin A1c” A2 Quantitation, Hemoglobin Variant, Thalassemia See “Hemoglobinopathy Evaluation” ABL Kinase Domain Mutation in CML, Plasma-Based, LeumetaTM Preferred Specimen(s) Instructions Transport Container Transport Temperature Methodology Clinical Significance 3 mL whole blood collected in EDTA (lavender-top) tube Information regarding draw time and date is required to ensure stability of the sample is maintained. Submission of whole blood is preferred. To avoid contamination, the laboratory will separate the plasma upon arrival. Follow standard whole blood collection procedure. Collect 3-5 mL whole blood samples in an EDTA tube. Blood samples are shipped at room temperature or 4°C. Do not freeze whole blood. Record the draw time and date on the tube. Ship immediately to maintain sample stability. Submission of plasma is acceptable. Collect blood in sterile tubes containing EDTA (lavender-top). Separate plasma from the cells by centrifugation, transfer the plasma to a separate plastic screw-cap vial, and ship frozen. EDTA (Lavender top) tube Whole blood: Refrigerated (cold packs), stable 72 hours Plasma: Frozen Reverse Transcriptase Polymerase Chain Reaction (RTPCR) • Nested PCR • Sequencing Chronic myelogeneous leukemia (CML) is a hematopoietic stem cell disorder, the result of a (9:22) translocation that produces the constitutively active, BCR-ABL tyrosine kinase. Mutations within the BCR-ABL kinase domain are the most commonly identified mechanism associated with relapse. Specific amino acid substitutions lead to drug resistance. ABO Group and Rh Type (Blood Grouping) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 4503 Sputum( Three consecutive morning samples are preferered; Random samples are also acceptable), Gastric lavage ( Patient should be fasting for previous 12 hours), BAL, Tracheal secretion, urine, Pus, Body fluids,tissue, Bone marrow in heparinised tubes, stool Slide carrier or sterile plastic screw-cap container with sample type labeled Slide at Room Temperature & other specimens refrigerated Raw specimens greater than 5 days old • Pooled specimens • Blood in EDTA (lavender-top) tube • Specimens in formalin Decontamination and concentration as needed and microscopic examination by fluorochrome stain (auramine rhodamine) Positive smears indicate the presence of acid fast organisms Acid Fast Stain - Kinyoun Method Preferred Specimen(s) Transport Container Transport Temperature 7788 3mL whole blood collected in a EDTA (lavender-top) tube or ACD-A or ACD-B (yellow-top) tube. If submitted with a CBC, HbA1c or any other test requiring a EDTA (lavendertop) tube, submit a separate tube for this test. EDTA (lavender-top) tube or ACD-A or ACD-B (yellow-top) tube Room temperature, Stable 6 Days Hemolysis • Received frozen • Serum Separator Tube (SST®) Immune Agglutination ABO type and Rh are needed to identify candidates for Rh immune globulin and to assess the risk of hemolytic disease of the newborn Acid Fast Stain - Flurochrome Method Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 16031 14511 Sputum (Three consecutive morning samples are preferered;Random samples are also acceptable), Gastric lavage ( Patient should be fasting for previous 12 hours), BAL, Tracheal secretion,urine, Pus , Body fluids,tissue,Bone marrow in heparinised tubes, stool Slide carrier or sterile plastic screw-cap container with sample type labeled Slide at Room Temperature & other specimens refrigerated 3 A B Reject Criteria Methodology Clinical Significance Raw specimens greater than 5 days old • Pooled specimens • Blood in EDTA (lavender-top) tube • Specimens in formalin Microscopic Examination Positive smears indicate the presence of acid fast organisms Acid Fast Stain, modified Stool Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 14512 5 grams (5 mL) stool. Transfer stool within 30 minutes of collection into formalin vial. Fill to the line on the transport vial. 10% formalin transport vial Room temperature, stable 48 hours Unpreserved stool • Frozen Microscopic exam of modified acid fast stain Cyclospora cayetanensis and Isospora belli are coccidian parasites which cause malaise, low grade fever, and diarrhea. Fatigue, anorexia, vomiting, myalgia and weight loss occur. The clinical presentation for those patients infected with either disease is similar. ACTH See “ACTH, Plasma” Actin See “Smooth Muscle Antibody (IgG)” Activated Protein C-Resistance 22 Preferred Specimen(s) 2 mL plasma collected in a tube with 3.2% sodium citrate (light blue-top) Freeze immediately Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Hemolysis • Received room temperature • Received refrigerated Methodology RVVT Based Clot Assay Clinical Significance To screen for APC-R associated with venous thromboembolic disorders. Acute Hepatitis Panel with Reflex See “Hepatitis Panel, Acute with Reflex Confirmation” Acid Fast Stain-Ziehl Neelsen Method Preferred Specimen(s) Instructions Transport Container Transport Temperature Methodology Clinical Significance 78649 Sputum (Three consecutive morning samples are preferered;Random samples are also acceptable), Gastric lavage ( Patient should be fasting for previous 12 hours), BAL, Tracheal secretion, urine, Pus, Body fluids, tissue, Bone marrow in heparinised tubes, stool Specimens of gastric aspirates should be neutralized with 1 gm of sodium carbonate per 15 mL of specimen before transport to the laboratory. Specimens should be delivered to the laboratory within one day of collection. See Specimen Collection section for general sitespecific instructions. Slide carrier or sterile plastic screw-cap container with sample type labeled Slide at Room Temperature & other specimens refrigerated Microscopic Examination The Ziehl Neelsen method serves to confirm the acidfast nature of recovered organisms from solid media and from positive broth cultures detected by the MGIT 960. ADA (Adenosine Deaminase) 79114 Preferred Specimen(s) 1.0 mL Serum, Heparinized plasma, Body fluids (Pleural fluid, Peritoneal fluid, CSF) Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, Stable for 7 days MethodologySpectrophotometry Clinical Significance ADA is an enzyme catalyzing the deamination reaction from adenosine to inosine. The enzyme is widely distributed in human tissues, especially high in T Iymphocytes. 4 Elevated serum ADA activity has been observed in patients with acute hepatitis, alcoholic hepatic fibrosis, chronic active hepatitis, liver cirrhosis, viral hepatitis and hepatoma. Increased ADA activity was also observed in patients with tuberculous effusions. Deamination of ADA activity in patient serum may add unique values to the diagnosis of liver diseases in combination with ALT or gamma-GT (GGT) tests. ADA assay may also be useful in the diagnosis of tuberculosis. AFP See “Alpha-Fetoprotein, Tumor Marker” AFP Quad Screen See “Maternal Serum Screen 4” Alanine Amino Transferase (ALT) / (SGPT) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Gross hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Alanine Aminotransferase (ALT) measurements are useful in the diagnosis and treatment of heart disease and certain liver diseases, e.g., viral hepatitis and cirrhosis. ALT activity in tissue is generally much lower than aspartate aminotransferase (AST) activity and is found in highest concentrations in the liver. Significant elevations of ALT occur only in diseases of the liver. ALT is often measured in conjunction with AST to determine whether the source of the AST is the liver or the heart. ALT is normally not elevated in cases of myocardial infarction, i.e., a normal ALT, in conjunction with an elevated AST, tends to suggest cardiac disease. However, slight elevations of ALT may occur if an infarct destroys a very large volume of heart muscle. Albumin Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 823 223 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Anticoagulants other than heparin • Hemolysis Spectrophotometry (SP) Serum albumin measurements are used in the monitoring and treatment of numerous diseases involving primarily the liver and kidney. Its main value lies in the follow-up therapy where improvement in the serum albumin level is the best sign of successful medical treatment. There may also be a loss of albumin in the gastrointestinal tract, in the urine by the damaged kidney or direct loss of albumin through the skin. More than 50% of patients with gluten enteropathy have depressed albumin. The only cause of increased albumin is dehydration; there is no naturally occurring hyperalbuminemia. Alcohol, Ethyl Qualitative, Urine (Ethanol) 78094 Preferred Specimen(s) 10 mL random urine Transport Container Plastic urine container Transport Temperature Ambient 7 days, Refrigerated 14 days Reject Criteria Urine with preservative MethodologyImmunoassay Clinical Significance Ethanol is the most often abused chemical substance. Other CNS depressant drugs have an additive effect when taken in combination with ethanol. Ethyl alcohol is present in many medicinal liquids and mouthwashes. 5 A B A B Alkaline Phosphatase Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Serum alkaline phosphatase levels are of interest in the diagnosis of hepatobiliary disorders and bone disease associated with increased osteoblastic activity. Moderate elevations of alkaline phosphatase may be seen in several conditions that do not involve the liver or bone. Among these are Hodgkin’s disease, congestive heart failure, ulcerative colitis, regional enteritis, and intra-abdominal bacterial infections. Elevations are also bserved during the third trimester of pregnancy. Alpha-1- Antitrypsin Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 235 1.0 mL Serum Plastic Screw cap vial Refrigerated, stable 7 days Gross Hemolysis Nephelometry Alpha-1-Antitrypsin level may be increased in normal pregnancy and in several diseases including chronic pulmonary disease; hereditary angieoedma; renal, gastric, liver and pancreatic disease; diabetes, carcinomas and rheumatoid diseases. Alpha-1-Antitrypsin may be decreased in emphysema, hepatic cirrhosis, respiratory distress syndrome of newborn, nephrosis, malnutrition and cachexia. Alpha-1 Antitrypsin (AAT) Mutation Analysis, Genotype Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 234 15340 5 mL whole blood collected in EDTA (lavender-top) tube Whole blood: Normal phlebotomy procedure. Specimen stability is crucial. Store and ship room temperature immediately. Do not freeze. EDTA (lavender-top) tube Whole blood: Room temperature, stable 8 days Serum: Refrigerated stable 7 days Moderate or gross hemolysis • Received refrigerated • Whole blood received frozen • Serum received room temperature Fluorescent Restriction Fragment Length Polymorphism Individuals who carry two copies (homozygous) for the Z allele are at a higher risk to develop liver disease and emphysema. Alpha-Fetoprotein, Maternal Serum See “Maternal Serum Screen 3” See “Maternal Serum Screen 4” See “Maternal Serum Screen 5” Alpha-Fetoprotein, Tumor Marker 237 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Stable 1 week, Refrigerated 7 days Reject Criteria Gross hemolysis • Hyperlipemic • EDTA or heparinized plasma MethodologyChemiluminescence Clinical Significance Elevation of serum AFP above values found in healthy individuals occurs in several malignant diseases, most notably nonseminomatous testicular cancer and primary hepatocellular carcinoma. AFP is not recommended as a screening procedure to detect cancer in the general population. ALT See “Alanine Aminotransferase (ALT)” 6 AML1-ETO t(8;21) RT PCR Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79560 3 mL Whole blood (EDTA) Do not freeze. Record the draw time and date on the tube. Information regarding draw time and date is required to ensure stability of the sample is maintained. Ship immediately to maintain sample stability. EDTA (lavender-top) Refrigerated acceptable 72 hrs Received Frozen Real-Time Reverse Transcriptase Polymerase Chain Reaction This assay is a real-time quantitative RT-PCR assay. Extracted sample RNA is subjected to two tubes realtime RT-PCR reaction to measure the quantity of the fused mRNA and the mRNA of an internal control. The results are reported as a ratio between the quantity of the fused mRNA to the internal control mRNA. In general, a normal person does not have any fused mRNA and the report will show ‘ ‘negative’ ‘ without any number. The positive sample will report the ratio. The analytical sensitivity of this test is 1 tumor cell in 100,000 normal cells. The mRNA transcripts of samples produced by the tumor cells vary widely from patient to patient, making it difficult to compare the quantitative results between patients. The quantitative results should only be used to monitor the patient’s own tumor load sequentially. Amoeba See “Entamoeba histolytica Antibody, IgG, EIA” Amphetamine Urine Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78080 5.0 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay, Spectrophotometry The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. Amylase serum 243 Preferred Specimen(s) 1 mL serum Transport Container Red-top tube, serum separator tube (SST®), plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 3 weeks Reject Criteria Hemolysis • Lipemia MethodologySpectrophotometry Clinical Significance The major sources of amylase are the pancreas and the salivary glands. The most common cause of elevation of serum amylase is inflammation of the pancreas (pancreatitis). In acute pancreatitis, serum amylase begins to rise within 6-24 hours, remains elevated for a few days and returns to normal in 3-7 days. Other causes of elevated serum amylase are inflammation of salivary glands (mumps), biliary tract disease and bowel obstruction. Elevated serum amylase can also be seen with drugs (e.g., morphine) that constrict the pancreatic duct sphincter preventing excretion of amylase into the intestine. Anemia Extended Profile (CBC, Reticulocyte Count, Folate Serum, Vitamin B12, Iron Total and Total Iron Binding Capacity) 78664 Preferred Specimen(s) 1.0 mL Serum, 2.0 mL Whole Blood collected in (lavender top) EDTA tube Transport Container Plastic screw cap vial Transport TemperatureRefrigerated Reject Criteria Grossly hemolysed specimens are rejected 7 A B A B Mathodology Clinical Significance See individual analyte See individual test for Clinical significance Antifungal Susceptibility Panel Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance A Pure Culture yeast Isolate Medium in tube or plate (e.g. SDA) Isolates greater than 24 hours old should be subcultured prior to testing. Isolates may be stored at room temperature or refrigerated prior to subculture (1 week). Contaminated specimen Colorimetric Method Fungi cause many types of infections, some of which may become serious, especially in immunocompromised and hospitalized patients. The appropriate collection, transport and processing of specimens are very important considerations in determining the etiology of fungal disease. The appropriate handling of specimens allows the recovery of fungal organisms and the association of a specific fungus with a disease process. Antinuclear Antibody Screen (ANA), IFA Perferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79030 79005 1 mL serum Plastic screw-cap vial Ambient : Not defined, Refrigerated 7 days, -20oC Longterm Gross hemolysis Hyperlipemic Titer: Indirect Immunofluorescence (IFA) This screening test with reflexive testing to the traditional IFA procedure is useful for the diagnosis of SLE and other autoimmune disorders. The descriptive IFA pattern may suggest a specific disease entity or autoantibodies. Anti Thyriod proxidase (Anti-TPO) 5081 Preferred Specimen(s) 1.0 mL Serum Transport Container Plsatic screw cap vial Transport Temperature Refrigerated 2 days Reject Criteria Grossly hemolyzed specimen MethodologyChemiluminescence Clinical Significance Thyroid peroxidase (TPO) is an enzyme that catalyzes the iodination and coupling steps in thyroid hormone biosynthesis. It is now known to be the principal microsomal antigen against which antibodies are directed in autoimmune thyroid diseases. The main use of this test is to confim that a patient’s diffuse goiter and/or hypothyroidism is due to autoimmune thyroiditis. The test may also help distinguish Graves disease from toxic nodular goiter. The TPO antibody measurement has replaced the thyroid antimicrosomal antibody (AMA) measurement. TPO antibodies may be detected in individuals without clinically significant thyroid disease. They do not define the patient’s thyroid functional status. Anti Thyroglobulin Panel 7260 Includes Anti-TPO, Anti-TG Preferred Specimen(s) 1.0 mL Serum Transport Container Plsatic screw cap vial Transport Temperature Refrigerated 2 days Reject Criteria Grossly hemolyzed specimen MethodologyCLIA Clinical Significance Measurement of thyroglobulin antibodies is useful inthe diagnosis and management of a variety of thyroid disorders including Hashimoto’s thyroiditis, Grave’s disease and certain types of goiter. ANCA See “ANCA Vasculidites” 8 Androstenedione 78110 Preferred Specimen(s) 1.0 mL Serum Transport Container Plastic screw cap vial Transport Temperature Refrigerated 24 hrs Reject Criteria Grossly hemolyzed specimens are rejected MethodologyChemiluminescence Clinical Significance Androstenedione may be useful in evaluating patients with androgen excess and managing patients with congenital adrenal hyperplasia (CAH). Anemia Panel 1 78531 Includes Complete Blood Count (CBC), Reticulocyte count. Preferred Specimen(s) Two 3 mL whole blood in EDTA (lavender-top) tubes Transport Container 2 EDTA tubes Transport TemperatureRefrigerated Reject Criteria EDTA with hemolysis or received frozen or clotted Methodology Electronic Cell Sizing, Sorting/Microscopy Clinical Significance See Individual test Anemia Panel 2 78532 Includes Complete Blood Count (CBC), Iron, TIBC, % Saturation (calculated), Reticulocyte count, Ferritin, Peripheral blood smear, Hemoglobin Electrophoresis Preferred Specimen(s) Two 3 mL whole blood in EDTA (lavender-top) tubes, 1.5 mL serum from a red-top tube Transport Container 2 EDTA tubes, 1 red-top tube Instruction Transfer whole blood to a plastic shipping vial to prevent breakage. Repeated freezing and thawing (up to 10 times) does not affect the test result. Mix specimen thoroughly after thawing. Transport Temperature Room temperatureor Refrigerated Reject Criteria EDTA with hemolysis or received frozen or clotted • Serum: gross hemolysis or Hyperlipemic Methodology Electronic Cell Sizing, Sorting/Microscopy, Spectrophotometry, Electrophoresis, Sepctrophotometry Clinical Significance See Individual test Anemia Panel 3 Includes Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78534 Complete Blood Count (CBC), Vitamin B12, Folate, Intrinsic Factor Blocking Antibody, Reticulocyte count Two 3 mL whole blood in EDTA (lavender-top) tubes, 1.5 mL serum from a red-top tube and 2 ml serum in no additive (red-top) tube (for B12) Do not expose the serum specimen to light for more than 24 hours. Avoid freezing and thawing. (for Folate and B12 test). For Anti Intrinsic Factor Antibody test, Centrifuge cells, pour off, and transport serum on ice. 2 EDTA tubes; plastic screw-cap vial (frozen serum), No additive (red-top) tube Room temperature No additive (red-top) vial with 2 ml serum should be refrigerated, on cold pack Frozen serum for Anti Intrinsic Factor Antibody test EDTA with hemolysis or received frozen or clotted • Serum: gross hemolysis or Hyperlipemic Chemiluminescence, Electronic Cell Sizing, Sorting/Microscopy, Immunoassay See Individual test Angiotensin-1-Converting Enzyme 683 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 1 week Reject Criteria Gross hemolysis MethodologySpectrophotometry Clinical Significance Increased in sarcoidosis, Gaucher’s disease and lymphoangiomyomatosis 9 A B A B Ankylosing Spondylitis See “HLA-B27 Antigen” Antenatal Panel - I Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 19909 ABO group & Rh; CBC with Differential; Urinalysis, Complete; ALT, Albumin, Direct Bilirubin, Total Bilirubin, Total Cholesterol, Ferritin (if Iron:TIBC is < 0.15 or > 0.50), Calculated Globulin, Glucose, Hemoglobin A1c (if glucose > 7.75 mmol/L), Iron, LD, TIBC, Total Protein Two 5 mL whole blood in EDTA (lavender-top) tubes, 10 mL urine in a yellow-top with blue fill line urinalysis preservative transport tube and 4 mL serum from a red-top tube and one gray-top tube Urinalysis: Encourage clean-catch mid-stream samples to minimize contamination and improve accuracy. Label the sample; store and transport at room temperature. 2 EDTA tubes; one yellow-top, blue fill line urinalysis preservative transport tube; one gray-top tube and plastic screw-cap vial Room temperature EDTA with hemolysis or received frozen or clotted • Serum: gross hemolysis or Hyperlipemic • Urine: unpreserved See Individual Analytes Antenatal Panel - II Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78530 ABO group and Rh; Complete Blood Count Urinalysis,; HIV 1/2 Antibody, HbsAg, RPR, Thyroid profile (T3, T4, TSH) Two 5 mL whole blood in EDTA (lavender-top) tubes, 10 mL urine in a yellow-top with blue fill line urinalysis preservative transport tube 4 mL serum from a red-top tube Urinalysis: Encourage clean-catch mid-stream samples to minimize contamination and improve accuracy. Label the sample; store and transport at room temperature. 2 EDTA tubes; one yellow-top, blue fill line urinalysis preservative transport tube; and plastic screw-cap vial Room temperature EDTA with hemolysis or received frozen or clotted • Serum: gross hemolysis or Hyperlipemic • Urine: unpreserved EIA, Chemiluminescence, Immuno Agglutination, Microscopy Examination, Reagent Impregnated Strips or dipstick indicates See Individual test Antibody to PM-Scl 37103 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature : Not defined, Refrigerated 3 days, -20oC Long term MethodologyELISA Clinical Significance Scleroderma may be localized or diffuse (Progressive Systemic Sclerosis [PSS]) and may involve skin, gastrointestinal tracts, lungs, vascular and cardiac systems, and kidneys. PM-1 (PM-Scl) Antibody is present in approximately one-fourth of patients with the polymyositis/ scleroderma overlap syndrome, 8% of patients with polymyositis alone and 2-5% of patients with scleroderma alone. Anti-DNA, (dsDNA) See “DNA (ds) Antibodies” Anti-ENA Antibody See “Sm and Sm/RNP Antibodies” Anti-HBc, IgM See “Hepatitis B Core IgM Antibody” 10 Anti-Phospholipid Syndrome Panel 3 Includes Preferred Specimen(s) Transport Container Instructions Transport Temperature Reject Criteria Methodology Clinical Significance 78525 Antiphospholipid Antibody (IgG, IgM, IgA), Cardiolipin Antibody (IgG, IgM, IgA) aPTT, dRVVT 3 mL serum, 3 mL platelet-poor citrate plasma in a plastic vial 2 vials of sterile plastic screw-cap vial - Serum Frozen platelet-poor citrate plasma in a plastic vial Draw blood in (light blue-top) tube containing 3.2% sodium citrate, mix gently by inverting 3-4 times. Centrifuge 15 minutes at 2500-3500 RPM. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet buffy layer and place into a plastic vial. Centrifuge a second time and, using a plastic pipette, transfer platelet-poor plasma into a new plastic vial. Plasma must be free of platelets (<10,000/uL). Freeze immediately and ship on dry ice. Serum : Refrigerated : 2 - 8oC Frozen Citrate plasma Gross hemolysis • Hyperlipemia ELISA, Coagulation See individual test A B Anti-Ribonucleic Protein Antigen See “Sm and Sm/RNP Antibodies” Anti-Smith Antibody See “Sm and Sm/RNP Antibodies” Anti-Streptolysin O Antibody (ASO) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 265 1 mL serum Plastic screw-cap vial Refrigerated 1 week Gross hemolysis • Lipemia Nephelometry This test is a sensitive test for recent streptococcal infection. A rise in ASO begins about one week after infection and peaks two to four weeks later. ASO levels do not rise with cutaneous infections. In the absence of complications or reinfection, the ASO level will fall to preinfection levels within 6 to 12 months. Over 80% of patients with acute rheumatic fever and 95% of patients with acute glomerulonephritis have elevated levels of ASO. Antithrombin III Activity 216 Preferred Specimen(s) 2 mL platelet poor 3.2% sodium citrate-anticoagulated plasma collected in a light blue-top tube; separate and freeze immediately Instructions Draw blood in light blue-top tube containing 3.2% sodium citrate, mix gently by inverting 3-4 times. Centrifuge 15 minutes at 1500 RCF (relative centrifugal force). Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet (buffy) layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and transport on dry ice. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Hemolysis • Received thawed Methodology Chromogenic Substrate Clinical Significance Aids in the detection of hypercoagulable states associated with venous thrombotic episodes. May be useful in patients who appear to be hyporesponsive to heparin. Antithrombin III, Antigen Patient Preparation Preferred Specimen(s) 5158 Patient should abstain from anabolic steroids, Gemfibrozil, Warfarin (Coumadin®), heparin therapy, asparaginase, estrogens, gestodene and oral contraceptives optimally for 3 days prior to specimen collection. Overnight fasting is preferred. 1 mL plasma collected in a 3.2% sodium citrate (light blue-top) tube 11 A B Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received thawed • Freeze/thaw Methodology Fixed Rate/Time Nephelometry Clinical Significance Previously referred to as “Antithrombin,” antithrombin antigen is an inhibitor of several coagulation factors. Patients with low concentrations of Antithrombin Antigen may have a hereditary or acquired prothrombotic state. The Antigenic test differentiates a Type I from Type II deficiency. Antinuclear Antibody Screen (ANA), ELISA 79004 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 24 hrs, -20oC Long term Reject Criteria Gross hemolysis, hyperlipemic, icteric samples; MethodologyELISA Clinical Significance This ANA screening test is useful when SLE and other autoimmune disorers are suspected. Anti-Neutrophil Cytoplasmic Antibody By IFA Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79006 C-ANCA and P- ANCA 1 mL serum Plastic screw-cap vial Room temperature : Not defined, Refrigerated 7 days, -20oC Long term Gross hemolysis; Gross lipemic Immunofluorescent Assay (IFA) Testing for anti-neutrophil cytoplasmic antibodies (PANCA and/or ANCA-IBD) has been found to be useful in establishing the diagnosis of suspected vascular diseases (e.g., crescentric glomerulonephritis, microscopic polyarteritis and Churg-Strauss syndrome), bowel disease (e.g., Crohn’s Disease, ulcerative colitis, primary sclerosing cholangitis, and autoimmune hepatitis) as well as with other autoimmune diseases (e.g., drug-induced lupus, SLE, and Felty’s syndrome). Apolipoprotein A1 78092 Preferred Specimen(s) 1.0 mL Serum Instruction 12 hours fasting is required Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 8 days Reject Criteria Gross hemolysis, Hyperlipemia Methodology Nephelometry Clinical Significance Apolipoprotein A1 is the primary protein associated with HDL cholesterol. Like HDL cholesterol, increased concentrations are associated with reduced risk of cardiovascular disease. Apolipoprotein B Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78093 1.0 mL Serum 12 hours fasting is required Plastic screw-cap vial Refrigerated 8 days Gross hemolysis, Hyperlipemia Nephelometry There are two major forms of Apolipoprotein B, B-100 and B-48. B-100, synthesized in the liver, is the major protein in VLDL, IDL, and LDL cholesterol. B-48, synthesized in the intestines, is essential for the assembly and secretion of chlyomicrons. Patients with increased concentrations of Apolipoprotein B are at increased risk of atherosclerosis. APTT See “Partial Thromboplastin Time, Activated (aPTT)” 12 Arthritis Panel 1 78515 Includes Complete Blood Count (CBC), C Reative Protein (CRP), Uric Acid, Antinuclear Antibody Screen, ELISA, with Reflex to Titer, IFA, and Rheumatoid Factor (RF), Complement 4 (C4) and Urinalysis Preferred Specimen(s) 3 mL Serum (2 vials each) 5 mL whole Blood – EDTA 10 mL urine - Urinalysis transport tube (yellow-top, blue fill line, preservative tube) Transport Container Sterile plastic screw-cap vial - Serum Yellow-top, blue fill line urinalysis transport tube - Urine EDTA (lavender-top) tube – Whole Blood Instructions Maintain specimen at room temperature. If multiple draw, collect EDTA (lavender-top) tube last. Traumatic tap can introduce thromboplastin and trap WBC and platelets. Transport Temperature Whole blood: Refrigerated Serum : Refrigerated 24 hrs, -20oC Long term Reject Criteria Gross hemolysis • Hyperlipemia • Hemolysis • Clotted • Received frozen Methodology IFA, Spectrophotometery, Microscopy Examination, Reagent Impregnated Strips or dipstick Clinical Significance See individual test ASO See “Anti-Streptolysin O Antibody (ASO)” Aspartate Amino Transferase (AST) / (SGOT) 822 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 2 weeks Reject Criteria Gross hemolysis • Anticoagulants other than heparin Methodology Spectrophotometry (SP) Clinical Significance AST is widely distributed throughout the tissues with significant amounts being in the heart and liver. Lesser amounts are also found in skeletal muscles, kidneys, pancreas, spleen, lungs, and brain. Injury to these tissues results in the release of the AST enzyme to the general circulation. In myocardial infarction, serum AST may begin to rise within 6-8 hours after onset, peak within two days and return to normal by the fourth orfifth day post infarction. An increase in serum AST is also found with hepatitis, liver necrosis, cirrhosis, and liver metastasis. AST See “Aspartate Aminotransferase (AST)” Barbiturates, Urine 78081 Preferred Specimen(s)Urine Instruction Collect urine sample without preservative Transport Container Plastic, leakproof container Transport Temperature Ambient 7 days, Refrigerated 14 days Reject Criteria Sample coating preservative Methodology Enzyme Immunoassay Clinical Significance The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. Basic Fever Panel Includes Test Components 78584 CBC, ESR, Malarial Parasite, Urinalysis & Dengue NS1 831 - Malaria/Blood Parasites 5463 - Urinalysis, complete 13 A B A B 6399 - CBC (Includes Diff/Plt) 79930 - ESR, Modified Westergren 79555 - Dengue NS1 Antigen See individual test for details. BCR/ABL FISH Assay 14641 Preferred Specimen(s) 3 mL Bone Marrow (Min1 mL) in transport media or Green Top Sodium Heparin Tube (Random); Room Temperature; -OR 3-5 ml Whole Blood (Min2-3 ml) Green Top Sodium Heparin Tube (Random); Room Temperature; Instructions Clinical history and reason for referral are required with test order. Prior therapy and bone marrow transplant history should be provided with test order. This test is performed to detect the molecular rearrangement of the bcr and abl genes involved in translocation (9;22), associated with chronic myelogenous leukemia (CML) and acute lymphocytic leukemi a (ALL), using FISH (fluorescence in situ hybridization). This test may be used in the evaluation of Ph negative CML, complex rearrangements or for follow-up to therapy for previously diagnosed Ph+ patients. Bone marrow transport medium is available upon request. Instructions, Specimen stability/rejection requirements: Specimen viability decreases during transit. Send specimen to testing laboratory for viability determination. Do not reject. Transport Container Culture Transport Media-Green Top Sodium Heparin Tube Transport Temperature Room Temperature Reject Criteria Received Frozen; Hemolysed; Clotted Methodology Fluorescence In Situ Hybridization Clinical Significance To rule out the presence of a bcr/abl rearrangement in chronic myelogenous leukemia or Ph-positive acute leukemia. Beta-2-Microglobulin, Serum Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 7 days Hemolysis • Lipemia Nephelometry Beta-2-microglobulin normally passes through the glomerulus into the proximal tubule where much of it is reabsorbed. Serum levels are therefore an index of glomerular function. When impaired, serum levels rise in inverse ratio to glomerular filtration rate. Increased amounts of beta-2-microglobulin are excreted in several renal disorders, e.g., Balkan nephropathy, heavy metal poisoning and renal tubular disease due to therapeutic agents. Serial levels of beta-2microglobulin in serum and urine are used to evaluate transplant viability and anticipate rejection. Following a successful graft, serum levels decline toward normal. Increasing serum levels provide an early sign of rejection. Elevated levels are also noted in lymphproliferative disorders, neoplasms (malignant and benign), inflammatory disease, and autoimmune diseases such as systemic lupus erythematosus (SLE) and Sjögren’s disease. Benzodiazepine, Urine Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 14 852 78082 10.0 mL Urine without preservative Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. Bicarbonate A B See “Carbon Dioxide” Bilirubin, Direct 285 Preferred Specimen(s) 1 mL serum Transport Container Amber plastic screw-cap vial or foil-wrapped plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 2 weeks Reject Criteria Gross hemolysis • Anticoagulants other than heparin MethodologySpectrophotometry Clinical Significance Measurement of the levels of bilirubin is used in the diagnosis and treatment of liver, hemolytic, hematologic, and metabolic disorders, including hepatitis and gall bladder obstruction. The assessment of direct bilirubin is helpful in the differentiation of hepatic disorders. The increase in total bilirubin associated with obstructive jaundice is primarily due to the direct (conjugated) fraction. Both direct and indirect bilirubin are increased in the serum with hepatitis. Bilirubin, Fractionated Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Direct Bilirubin, Indirect Bilirubin (calculated), Total Bilirubin 1 mL serum Amber plastic screw-cap vial or foil-wrapped plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Gross hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Measurement of the levels of bilirubin is used in thediagnosis and treatment of liver, hemolytic, hematologic, and metabolic disorders, including hepatitis and gall bladder obstructive disease. The assessment of direct bilirubin is helpful in the differentiation of hepatic disorders. The increase in total bilirubin associated with obstructive jaundice is primarily due to the direct (conjugated) fraction. Both direct and indirect bilirubin are increased in the serum with hepatitis. In the newborn patient with hemolytic jaundice and neonatal jaundice, the increase in the total bilirubin is primarily due to the indirect (unconjugated) bilirubin fraction. This jaundice may be caused by Rh, ABO, or other blood group incompatibilities, by hepatic immaturity, or by hereditary defects in bilirubin conjugation. Bilirubin, Total Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 7286 287 1 mL serum Amber plastic screw-cap vial or foil-wrapped plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Gross hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Measurement of the levels of bilirubin is used in the diagnosis and treatment of liver, hemolytic, hematologic, and metabolic disorders, including hepatitis and gallbladder obstructive disease Bladder Cancer (UroVysion™) See “FISH, Vysis® UroVysion™, Bladder Cancer” Blood Culture See “Culture, Blood” Blood Type and Rh See “ABO Group and Rh Type” Blood Urea Nitrogen See “Urea Nitrogen (BUN)” 15 A B BOH (Bad Obstetrics History) Panel Includes Test Components 78910 ToRCH 10, TSH, Cardiolipin IgA, Cardiolipin IgG, Cardiolipin IgM, Antiphospholipid Ab IgA, IgG, IgM, aPTT, dRVVT) 763 - Partial Thromboplastin time, activates (aPTT) 899 - TSH 4661 - Cardiolipin IgA 4662 - Cardiolipin IgG 4663 - Cardiolipin IgM 79531 - Torch 10 79047 - Antiphospholipid Ab IgG 79048 - Antiphospholipid Ab IgM 79049 - Antiphospholipid Ab IgA See individual test for details Bone Marrow Biopsy with Reticulin Stain 79199 Preferred Specimen(s) Bone marrow biopsy in 10% buffered formalin or formalin fixed paraffin embedded tissue block Transport Container Paraffin block bag Transport Temperature Room temperature Reject Criteria Improper fixation; Receive Frozen Methodology Manual staining Clinical Significance Reticular fibers are present in normal human tissues and have a support function. They are normally found throughout the body but are most abundant in liver, spleen, kidney and lymph nodes. In certain tumors, reticulin is located in a characteristic position in relation to the actual tumor cells. Reticulin stains can therefore be an important diagnostic tool for the differential diagnosis of certain types of tumor. Bone Marrow Examination Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78685 2 ml Bone marrow aspirate, 2 ml Whole blood, 4 Bone marrow aspirate smear and 2 Peripheral blood smears. Bone marrow aspirate: Lavender top Whole blood: Lavender top (EDTA) Bone marrow aspirate smear: slide holder Peripheral blood smears: slide holder Refrigerated 48 hrs Receive Frozen Morphology Review Examination of bone marrow is required for further workup of hematological abnormalities observed in peripheral blood smear, staging for bone marrow involvement by metastatic tumor, assessment of infectious disease processes includes fever of unknown origin and in the evaluation of metabolic storage diseases. B-Type Natriuretic Peptide (BNP) 37386 Preferred Specimen(s) 1 mL plasma from an EDTA (Lavender Top) tube. Collect specimen in a plastic Lavender Top tube. Instruction Mix thoroughly by inversion. Centrifuge and separate the plasma from the cells within one hour of collection. Transfer the plasma to a plastic vial using a plastic transfer pipette. Freeze specimen immediately for storage and transport. Transport Container Plastic, leakproof container Transport TemperatureFrozen Reject Criteria Specimens received in glass vacutainers, Specimens not received frozen MethodologyChemiluminescene Clinical Significance Rule out congestive heart failure (CHF) in symptomatic individuals, Determine prognosis in individuals with CHF or other cardiac disease, Maximize therapy in individuals with heart failure 16 BUN See “Urea Nitrogen (BUN)” CA 15-3, serum 5819 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient, Stable 1 week, Refrigerated 1 weeks Reject Criteria Gross hemolysis • Gross lipemia MethodologyChemiluminescence Clinical Significance CA 15-3 may be useful for monitoring patients with metastatic breast cancer and certain ovarian cancers. The CA 15-3 values from sequential samples have a high correlation with the clinical course in most patients with metastatic breast cancer. See CA 15-3 in the Hematology/Oncology section of Test Application and Interpretation. CA 19-9, serum 4698 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 1 week Reject Criteria Gross hemolysis MethodologyChemiluminescence Clinical Significance A large percentage of patients with gastrointestinal tumors (such as pancreatic, liver, gastric, colorectal tumors) and some other malignancies have been shown to have elevated serum or plasma CA 19-9 levels. The serum or plasma CA 19-9 levels may be useful for monitoring disease activity predicting relapse following treatment. CA 19-9 should not be used as a screening test. See CA 19-9 in the Hematology/Oncology section of Test Application and Interpretation. CA 125, Serum 29256 Preferred Specimen(s) 1 mL serum Instructions Specimen must be refrigerated or frozen if received by the laboratory more than 24 hours after collection Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) 7 days Reject Criteria Gross hemolysis MethodologyChemiluminescence Clinical Significance The CA 125 level can provide prognostic information in the follow-up management of patients with ovarian carcinoma. The assay should be used as an adjunctive test in the management of ovarian cancer patients. CA 125 is not recommended as a cancer screening procedure to detect cancer in the general population. See Ovarian Cancer in the Hematology/ Oncology section of Test Application and Interpretation. Calcium Random Urine 79838 Preferred Specimen(s) 10 mL random Urine. Collect urine with 25 mL 6N HCL Transport Container Sterile urine container or Plastic screw urine vial Transport Temperature Refrigerated preferred; Room temperature acceptable;Frozen acceptable Reject Criteria None MethodologySpectrophotometry Clinical Significance Urinary calcium reflects dietary intake, rate of calcium absorption by the intestine and bone resorption. Urinary calcium is used primarily to evaluate parathyroid function and the effects of Vitamin D. A significant number of patients withy primary hyperparathyroidism will have elevated urinary calcium. However, there are other clinical entities that may be associated with increased urine calcium: Sarcoidosis, Paget’s disease of bone, Vitamin D intoxication, hyper thyroidism and glucocorticoid excess. Decreased urine calcium is seen with thiazide diuretics, vitamin D deficiency and familial hypocalciuric hypercalcemia. 17 C D Calcium, Serum C D Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 303 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Serum calcium is involved in the regulation of neuromuscular and enzyme activity, bone metabolism and blood coagulation. Calcium blood levels are controlled by a complex interaction of parathyroid hormone, vitamin D, calcitonin and adrenal cortical steroids. Calcium measurements are useful in the diagnosis of parathyroid disease, some bone disorders and chronic renal disease. A low level of calcium may result in tetany. Calcium, 24-Hour Urine 1635 Includes Creatinine, 24 Hour Urine Preferred Specimen(s) 10 ml aliquot of a 24-hour collection. Collect urine with 25 mL 6N HCl. Instructions Refrigerate during and after collection. Do not include first morning specimen; collect all subsequent voidings. The last sample collected should be the first morning specimen voided the following morning at the same time as the previous morning’s first voiding. Record 24 hour urine volume on test request form and urine vial. Transport Container 24-hour urine container Transport Temperature Refrigerated preferred; Room temperature acceptable; Frozen acceptable Reject Criteria None MethodologySpectrophotometry Clinical Significance Urinary calcium reflects dietary intake, rate of calcium absorption by the intestine and bone resorption. Urinary calcium is used primarily to evaluate parathyroid function and the effects of Vitamin D. A significant number of patients withy primary hyperparathyroidism will have elevated urinary calcium. However, there are other clinical entities that may be associated with increased urine calcium: sarcoidosis, Paget’s disease of bone, vitamin D intoxication, hyperthyroidism and glucocorticoid excess. Decreased urine calcium is seen with thiazide diuretics, vitamin D deficiency, and familial hypocalciuric hypercalcemia. Culture, Fungus, Blood ,Rapid Includes Preferred Specimen(s) inoculation Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Fungal culture. If culture is positive,identification will be performed. Antifungal susceptibilities are only performed when requested. Submit blood for fungal culture, in BD BACTECR Mycosis or BD BACTECR Myco® F/Lytic blood bottle(s). Gently mix the bottle(s) following See Blood Cultures in the Bacteria section of Specimen Collection and Handling Do not submit specimens in SPS, heparin, EDTA, and sodium citrate tubes Do not refrigerate In BD BACTECR Mycosis or BD BACTEC MycoF/Lytic blood bottle Room temperature 48 hrs, Refrigerated 72 hrs, Frozen : Unacceptable Blood specimens collected in EDTA, sodium citrate or anticoagulants other than SPS or heparin • Frozen specimens or specimens broken in transit Rapid Automated Fluroscent Technique Fungal sepsis constitutes one of the most serious infectious diseases. The detection of microorganisms in a patient’s blood has importance in the diagnosis of sepsis. Campath®-1H Sensitivity (CD52) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 18 79886 10980 5 mL whole blood or bone marrow collected in a sodium heparin (green-top) tube Sodium heparin (green-top) tube Room temperature Received refrigerated • Received frozen Flow Cytometry Campath® (alemtuzumab) is indicated for the treatment of patients with CD52 positive chronic lymphocytic leukemia. See Campath Sensitivity (CD52) in the Hematology/Oncology section of Test Application and Interpretation. Carbon Dioxide, Serum Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 310 1 full unopened spun gel barrier tube Do not open tube 1 full, unopened spun gel barrier tube Ambient 5 days, Refrigerated 2 weeks Hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Measurements are used in the diagnosis and treatment of numerous potentially serious disorders associated with changes in body acid-base balance Carcinoembryonic Antigen See “CEA” Cardio CRP (hsCRP) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10124 1 mL serum Plastic screw-cap vial Refrigerated 1 week Gross hemolysis • Lipemia End Point Nephelometry Useful in predicting risk for cardiovascular disease. See Cardio CRP™ in the Cardiovascular Tests section of Test Application and Interpretation. Cardiolipin IgA Ab 4661 Preferred Specimen(s) 1 ml serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature : Not defined, Refrigerated : Not defined, -20oC Long term MethodologyELISA Clinical Significance Cardiolipin antibodies (CA) are seen in a subgroup of patients with autoimmune disorders, particularly Systemic Lupus Erythematosus (SLE), who are at risk for vascular thrombosis, thrombocytopenia, cerebral infarct and/or recurrent spontaneous abortion. Elevations of CA associated with increased risk have also been seen in idiopathic thrombocytopenic purpura, rheumatoid and psoriatic arthritis, and primary Sjögren’s syndrome. See Non-Lipid Markers in the Cardiovascular chapter, Venous Thrombosis: Laboratory Support of Risk Assessment and Diagnosis in the Coagulation chapter and Cardiolipin Antibodies in the Immunology section of Test Application and Interpretation. Cardiolipin IgG Ab 4662 Preferred Specimen(s) 1 ml serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature : Not defined, Refrigerated : Not defined, -20oC Long term MethodologyELISA Clinical Significance Cardiolipin antibodies (CA) are seen in a subgroup of patients with autoimmune disorders, particularly Systemic Lupus Erythematosus (SLE), who are at risk for vascular thrombosis, thrombocytopenia, cerebral infarct and/or recurrent spontaneous abortion. Elevations of CA associated with increased risk have also been seen in idiopathic thrombocytopenic purpura, rheumatoid and psoriatic arthritis, and primary Sjögren’s syndrome. See Non-Lipid Markers in the Cardiovascular chapter, Venous Thrombosis: Laboratory Support of Risk Assessment and Diagnosis in the Coagulation chapter and Cardiolipin Antibodies in the Immunology section of Test Application and Interpretation. Cardiolipin IgM Ab Preferred Specimen(s) Transport Container Transport Temperature 4663 1 ml serum Plastic screw-cap vial Room temperature : Not defined, Refrigerated : Not defined, -20oC Long term 19 C D C D MethodologyELISA Clinical Significance Cardiolipin antibodies (CA) are seen in a subgroup of patients with autoimmune disorders, particularly Systemic Lupus Erythematosus (SLE), who are at risk for vascular thrombosis, thrombocytopenia, cerebral infarct and/or recurrent spontaneous abortion. Elevations of CA associated with increased risk have also been seen in idiopathic thrombocytopenic purpura, rheumatoid and psoriatic arthritis and primary Sjögren’s syndrome. See Non-Lipid Markers in the Cardiovascular chapter, Venous Thrombosis: Laboratory Support of Risk Assessment and Diagnosis in the Coagulation chapter and Cardiolipin Antibodies in the Immunology section of Test Application and Interpretation. Cardiolipin Antibody Panel (IgA, IgG, IgM) 36189 Order Code 7352 (screen only) Preferred Specimen(s) 3mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature/ Refrigerated : Not defined, -20oC Long term MethodologyELISA Clinical Significance Cardiolipin Antibodies (CA) may be seen during the convalescent phase of acute bacterial and viral infections (including syphilis). All patients that test positive for CA should be retested after six to eight weeks to rule out transient antibodies Individuals with the antiphospholipid antibody syndrome (APS) have an increased risk for stroke, myocardial infarction, venous thrombosis, thromboembolism, thrombocytopenia, and/or recurrent miscarriages (women). CBFB beta/MYH11 inv(16) RT PCR, CELLS Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 14992 5 mL Whole blood EDTA (lavender-top) Refrigerated, stable 72 hrs Received Frozen Real-Time Reverse Transcriptase Polymerase Chain Reaction This assay is a real-time quantitative RT-PCR assay. Extracted sample RNA is subjected to two separated tubes of real-time RT-PCR reaction to measure the quantity of the fused mRNA and the mRNA of an internal control. The results are reported as a ratio between the quantity of the fused mRNA to the internal control mRNA. In general, normal person does not have any fused mRNA and the report will show ‘ ‘negative’ ‘ without any number. The positive sample will report the ratio. The analytical sensitivity of this test is 1 tumor cell in 100,000 normal cells. The mRNA transcripts of samples produced by the tumor cells vary widely from patient to patient, making it difficult to compare the quantitative results between patients. The quantitative results should only be used to monitor the patient’s own tumor load sequentially. CBFB/MYH11, Inversion 16 FISH Assay 14642 Preferred Specimen(s) 3 mL Bone Marrow (Min1 mL) Green Top Sodium Heparin Tube (Random); Room Temperature; -OR 3 mL Whole Blood (Min1 mL) Green Top Sodium Heparin Tube (Random); Room Temperature; Instructions Clinical history and reason for referral are required with test order. Prior therapy/transplant information should be submitted with test order. Interphase nuclei are examined microscopi cally for the presence of break apart signals that indicate rearrangement of the CBFB gene, located in chromosome band 16q22, such as inv(16)(p13;q22) and t(16;16)(p13;q22), using FISH (fluorescence in situ hybridization). Rearrangements of CBFB are found predominantly in myeloid leukemia (M4eo).This test is useful for detecting cell populations that may not be mitotically active, that have suboptimal chromosome morphology, or that have variant or cryptic rearrangements. Bone marrow transport medium is available upon request. Instructions, Specimen stability/rejection requirements: Specimen viability decreases during transit. Send specimen to testing laboratory for viability determination. Do not reject. 20 Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Culture Transport Media Room Temperature Frozen: Unacceptable Fluorescence In Situ Hybridization To rule out the presence of a CBFB rearrangement, associated with the majority of acute myelomonocytic leukemia with eosinophilia ( M4eo ). Carcinoembryonic Antigen (CEA) C D 978 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Note: Ambient 5 days (Frozen acceptable), Refrigerated 14 days MethodologyChemiluminescence Clinical Significance Increased serum CEA levels have been detected in persons with primary colorectal cancer and in patients with other malignancies involving the gastrointestinal tract, breast, lung, ovarian, prostatic, liver and pancreatic cancers. Elevated serum CEA levels have also been detected in patients with nonmalignant disease, especially patients who are older or who are smokers. CEA levels are notuseful in screening the general population for undetected cancers. However, CEA levels provide important information about patient prognosis, recurrence of tumors after surgical removal, and effectiveness of therapy. See Carcinoembryonic Antigen (CEA) in the Hematology/Oncology section of Test Application and Interpretation. Ceruloplasmin Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 326 1.0 mL Serum, EDTA/Heparin Plasma Plastic screw cap vial Refrigerated 1 week Hemolysis, Hyperlipemia Nephelometery Approximately 80% of the body’s copper is bound to Ceruloplasmin. Ceruloplasmin is an acute phase reactant. Concentrations are decreased in approximately 75% of patients with Wilson disease, an autosomal recessive disorder of copper metabolism. Celiac Disease Panel Includes Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance 15980 Tissue Transglutaminase IgA, Total IgA, Gliadin Antibody IgA 2 mL serum Plastic screw-cap vial Refrigerated (cold packs) ELISA, Nephlometry Patients with celiac disease display a hypersensitivity to gluten (wheat) in their diet. This panel helps differentiate patients with celiac disease from patients with other inflammatory bowel diseases. Chikungunya Fever, Igm 19915 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature : Not defined, Refrigerated 4 days, -20oC Long term Reject Criteria Gross hemolysis • Hyperlipemia MethodologyELISA Clinical Significance See Chikungunya Fever in the Infectious Disease section of Test Application and Interpretation. Chikungunya Fever, IgG Preferred Specimen(s) Transport Container 79093 1.0 mL serum Plastic screw-cap vial 21 C D Transport Temperature Room temperature : Not defined, Refrigerated 4 days, -20oC Long term Reject Criteria Gross hemolysis • Hyperlipemia MethodologyELISA Clinical Significance Chikungunya virus is a mosquite-borne alpha-virus associated with large outbreaks of a febrile illness in Africa, Ocean Islands, India, and Southeast Asia. These infections are associated with severe arthralgia, rash, and headache. Cases acquired by US residents during international travel have been described. See Chikungunya Fever in the Infectious Disease section of Test Application and Interpretation. Chloride 330 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Stable 5 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Anticoagulants other than heparin Methodology Ion Selective Electrode (ISE) Clinical Significance Serum chloride is the major extracellular anion and counter-balances the major cation, sodium, maintaining electrical neutrality of the body fluids. Two thirds of the total anion concentration in extracellular fluids is chloride and it is significantly involved in maintaining proper hydration and osmotic pressure. Movement of chloride ions across the red blood cell membrane is essential for the transport of biocarbonate ions in response to changing concentrations of carbon dioxide. Chloride measurements are used in the diagnosis and treatment of electrolyte and metabolic disorders such as cystic fibrosis and diabetic acidosis. Chloride, 24-Hour Urine Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 368 Creatinine, 24 Hour Urine 10 mL 24-hour urine Collect without preservatives. Refrigerate during and after collection. Aliquot unpreserved specimen before adding acid. Do not include first morning specimen; collect all subsequent voidings. The last sample collected should be the first morning specimen voided the following morning at the same time as the previous morning’s first voiding. Record 24-hour urine volume on test request form and urine vial. Plastic, screw-cap container Refrigerated & ambient 7 days, Stable 1 week None Ion Specific Electrode (ISE) Urine chloride excretion approximates the dietary intake. The chloride content of most foods parallels that of sodium. An increase in urine chloride may result from water deficient dehydration, diabetic acidosis, Addison’s disease and salt-losing renal disease. Decreased urine levels are seen in congestive heart failure, severe diaphoresis and in hypochloremic metabolic alkalosis due to prolonged vomiting. Cholesterol, LDL See “Direct LDL” Cholesterol, HDL See “HDL Cholesterol” Cholesterol, Total Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology 22 334 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Gross hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Clinical Significance Total LDL and HDL cholesterol, in conjunction with a triglyceride determination, provide valuable information for the risk of coronary artery disease. Total serum cholesterol analysis is useful in the diagnosis of hyperlipoproteinemia, atherosclerosis, hepatic and thyroid diseases. See Markers of Lipidemia in the Cardiovascular section of Test Application and Interpretation. Chorionic Gonadotropin C D See “hCG, Qualitative, Urine” Chromosome Analysis / Peripheral Blood Leukocyte Culture for Genetic Analysis (Karyotyping) 14627 Preferred Specimen(s) 4.0 mL Sodium Heparin Peripheral Blood, Cord blood Instruction A test requisition with preliminary diagnosis and clinical history should accompany the specimen Transport Container Collection in Sodium Heparin Green top tube Transport Temperature Room Temperature Reject Criteria Specimens received frozen, hemolyzed, or those received in a non-sodium heparin vacutainer tubes; Clotted MethodologyCulture Clinical Significance Peripheral blood is the most commonly utilized tissue for determination of constitutional karyotypes and this test looks at numerical and structural chromosomal rearrangement. Most common indication for study include repeated spontaneous abortion, infertility, developmental delays, dysmorphology, mental retardation, suspected sex chromosome abnormalities and for parents requiring genetic counseling. Chromosome Analysis, Hematologic, Malignancy 14636 Preferred Specimen(s) 4.0 mL Sodium Heparin, Bone Marrow / Astirate Instruction A test requisition with a current CBC and preliminary diagnosis should accompany the specimen Transport Container Collection in Sodium Heparin tube / Bone Marrow kit supplied by Lab Transport Temperature Room Temperature Reject Criteria Specimens received frozen, hemolyzed, or those received in a non-sodium heparin vacutainer tubes; Clotted; Dry taps MethodologyCulture Clinical Significance Cytogenetics of hematologic disorders attempts to define and interpret chromosomal aberrations that occur in neoplastic cells associated with leukemia and other hematologic malignancies. Chromosome abnormalities in cancer cells of patients with malignant hematologic disorders including acute myeloid and lymphoblastic leukemias, chronic myelogenous leukemia (CML, CGL), myelodysplastic and myeloproliferative disorders; may aid in the diagnosis, prognosis, treatment, and etiology of disease. Chromosome Analysis, Mosaicism 14632 Preferred Specimen(s) 4.0 mL Sodium Heparin Blood Instruction A test requisition with preliminary diagnosis and clinical history should accompany the specimen Transport Container Collection Sodium Heparin tube Transport Temperature Room Temperature Reject Criteria Specimens received frozen, hemolyzed, or those received in a non-sodium heparin vacutainer tubes, Clotted. MethodologyCulture Clinical Significance The chromosome analysis, Mosaicism test rules out the following: • Trisomies such as trisomy 21 (Down syndrome), Trisomy 18, Trisomy 13. • Sex chromosome abnormalities such as Turner syndrome (45, X) and Klinefelter syndrome (47, XXY). • Most rearrangement including Robertsonian translocation, reciprocal translocation and inversions. • Most marker chromosomes. Mosaicism above 6% (at 95% confidence level). 23 Cobalamine See “Vitamin B12” Cocaine Metabolites By GC/MS (Urine) C D Preferred Specimen(s) Transport Container Transport Temperature Methodology 20 mL urine, random collection Plastic urine container Room temperature 7 days, Refrigerated 14 days Gas Chromatography/Mass Spectrophotometry (GC/MS) Cocaine Urine Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78083 10 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. Complement 3 (C3) Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78050 0.5 mL Serum Overnight fasting is preferred. Serum should be separated immediately from clot. Plastic screw cap vial Refrigerated 1 week Grossly hemolysed specimen Nephelometry C3 is the most abundant complement protein and is critical to activation of both the classical and alternative pathways. C3 is an acute phase reactant. Decreased concentrations are observed in patients with systemic lupus erythematosus (SLE), endocarditis, and disseminated intravascular coagulation (DIC). Congenital deficiency of C3 places such patients at high risk for recurrent bacteremia. Complement 4 (C4) Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78051 0.5 mL Serum Overnight fasting is preferred. Serum should be separated immediately from clot. Plastic screw cap vial Refrigerated 1 week Grossly hemolysed specimen Nephelometry C4 is critical to activation of the classical pathway.Concentrations of C4 are decreased in patients with systemic lupus erythematosus (SLE), immune complex disease, and hereditary angioedema. Congenital absence of C4 places such patients at increased risk of bacteremia, especially infections by S. pneumoniae. Codeine See “Opiates, Clinical Screen with Confirmation” Collagen Cross-Linked N-Telopeptide See “Collagen Cross-Linked N-Telopeptide (NTx), Urine” 24 5530 Complete Blood Count See “CBC (includes Differential and Platelets)” Complete Blood Count (CBC) with Peripheral blood smear and ESR Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Two 3 mL whole blood in EDTA vacutainer, fresh slide smear Slide smear should be dry and thin EDTA Vial (lavender top tube), Sodium citrate vial (black-top tube) Room temperature or Refrigerated; Stability 48 hrs Heparinized sample; frozen; hemolyzed specimen Cell Counter/Microscopic examination/ Westergren Method See individual tests. ESR testing should be performed within 24 hours of specimen collection. An alternative acute inflammatory marker is C reactive Protein (CRP). Complete Blood Count (CBC) with Peripheral blood smear Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78512 3 mL whole blood in EDTA vacutainer, fresh slide smear Slide smear should be dry and thin EDTA Vial (lavender-top) tube Room temperature or Refrigerated; Stability 48 hrs Heparinized sample; Received frozen Cell counter/Microscopic examination An automated blood analysis provides insights into medical conditions associated with changes in red blood cells, white blood cells, and platelets. The peripheral blood smear may be useful to describe morphologic abnormalities and leukemias. Complete Blood Count (CBC) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78511 6399 3ml Whole blood in EDTA vial, fresh slide smear Slide smear should be dry and thin EDTA vial (lavender-top) tube Room temperature or Refrigerated; Stability 48 hrs Frozen; heparinized sample Cell counter, Methemoglobin An automated blood analysis provides insights into medical conditions associated with changes in red blood cells, white blood cells, and platelets. The peripheral blood smear may be useful to describe morphologic abnormalities and leukemias. Compound S See “11-Deoxycortisol, LC/MS/MS” Conjugated Bilirubin See “Bilirubin, Direct” Cortisol – Total 367 Preferred Specimen(s) 1 mL serum Note: Assay not recommended when patient is receiving prednisone/prednisolone therapy due to cross reactivity with the antibody used in this assay. Instruction Assay not recommended when patient is on prednisone/prednisolone therapy due to cross reactivity with the antibody used in this assay Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 7 days MethodologyChemiluminescence Clinical Significance Cortisol is increased in Cushing’s Disease and decreased in Addison’s Disease (adrenal insufficiency) 25 C D Cortisol, A.M. C D 4212 Patient Preparation Assay is not recommended when patient is receiving prednisone/prednisolone therapy due to cross reactivity with the antibody used in this assay Preferred Specimen(s) 1 mL serum Instructions Collect specimen between 7-9 A.M. Indicate thecollection time on the specimen container and test requisition. Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 7 days MethodologyChemiluminescence Clinical Significance Cortisol is increased in Cushing’s Disease and decreased in Addison’s Disease (adrenal insufficiency) Cortisol, P.M. 4213 Patient Preparation Assay not recommended when patient is receiving prednisone/prednisolone therapy due to cross reactivity with the antibody used in this assay Preferred Specimen(s) 1 mL serum Instructions Collect specimen between 3-5 P.M. Indicate collection time on specimen container and test requisition. Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 7 days MethodologyChemiluminescence Clinical Significance Cortisol is increased in Cushing’s Disease and decreased in Addison’s Disease (adrenal insufficiency) Coombs Test - Indirect Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 795 3 ml Whole blood EDTA (lavender top tube), Red top tube Refrigerated, Stable 48 hrs Received frozen Agglutination Method The indirect Coombs test is used in prenatal testing of pregnant women, and in testing blood prior to a blood transfusion. It detects antibodies against RBCs that are present unbound in the patient’s serum. In this case, serum is extracted from the blood, and the serum is incubated with RBCs of known antigenicity. If agglutination occurs, the indirect Coombs test is positive. A negative test in a woman who is pregnant means that she has not developed detectable antibodies against the blood of her fetus; e.g., no Rh sensitization. Coombs Test - Direct See “Direct Anti Globulin test (DAT)” C-Peptide 531 Preferred Specimen(s) 1.0 mL Serum Instruction Overnight fasting is required Transport Container Plastic screw cap vial Transport TemperatureFrozen Reject Criteria Grossly hemolysed, Cord blood Methodology Chemiluminescent Enzyme Immunoassay Clinical Significance C-Peptide is useful in distinguishing insulin-secreting tumors, i.e., insulinomas, from exogenous insulin administration. C-Peptide concentrations are severely depressed or absent in Type I diabetes mellitus. CPeptide is also useful in monitoring patients who have received islet cell or pancreatic transplants. C-Reactive Protein (CRP) Preferred Specimen(s) Transport Container 26 1 mL serum Plastic screw-cap vial 4420 Transport Temperature Reject Criteria Methodology Clinical Significance Refrigerated 1 week Gross hemolysis • Lipemia Nephelometry Increased CRP levels are found in inflammatory conditions including: bacterial infection, rheumatic fever, active arthritis, myocardial infarction, malignancies and in the post-operative state. This test cannot detect the relatively small elevations of CRP that are associated with increased cardiovascular risk. See Non-Lipid Markers of Cardiovascular Disease in the Cardiovascular section of Test Application and Interpretation Creatine Kinase (CK), Total Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 374 1 mL serum If CK and CK Isoenzymes are ordered together, specimen must be submitted frozen Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Test for myocardial infarction and skeletal muscle damage. Elevated results may be due to: myocarditis, myocardial infarction (heart attack), muscular dystrophy, muscle trauma or excessive exercise. Creatinine, Random Urine 8459 Preferred Specimen(s) 10 mL random urine - no preservative Transport Container Plastic screw-cap container Transport Temperature Ambient 7 days, Refrigerated 62 days MethodologySpectrophotometry Clinical Significance Creatinine is the endproduct of creatine metabolism. Creatine is present primarily in muscle and the amount of creatinine produced is related to total skeletal muscle mass. Daily creatinine production is fairly constant except when there is massive injury to muscle. The kidneys excrete creatinine very efficiently and blood levels and daily urinary excretion of creatinine fluctuates very little in healthy normal people. Since blood and daily urine excretion of creatinine shows minimal fluctuation, creatinine excretion is useful in determining whether 24-hour urine specimens for other analytes (e.g., protein) have been completely and accurately collected. Creatinine with Glomerular Filtration Rate, Estimated (eGFR) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 375 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Serum creatinine is useful in the evaluation of kidney function and in monitoring renal dialysis. A serum creatinine result within the reference range does not rule out renal function impairment: serum creatinine is not sensitive to early renal damage since it varies with age, gender and ethnic background. The impact of these variables can be reduced by an estimation of the glomerular filtration rate using an equation that includes serum creatinine, age and gender. See Creatinine with Glomerular Filtration Rate, Estimated (eGFR) see also Estimated Glomerular Filtration Rate in the Chronic Kidney Disease section of Test Application and Interpretation. Crescentic Glomeruloephritis See “Myeloperoxidase Antibody (MPO)” Creatinine, 24-Hour Urine Preferred Specimen(s) 381 2 mL urine 27 C D C D Instructions Record 24-hour urine volume on test request form and urine vial. Transport Container 24-hour urine container Transport Temperature Ambient 7 days, Refrigerated 62 days Reject Criteria Received at room temperature MethodologySpectrophotometry Clinical Significance Creatinine is the end product of creatine metabolism. Creatine is present primarily in muscle and the amount of creatinine produced is related to total skeletal muscle mass. Daily creatinine production is fairly constant except when there is massive injury to muscle. The kidneys excrete creatinine very efficiently and blood levels and daily urinary excretion of creatinine fluctuates very little in healthy normal people. Since blood and daily urine excretion of creatinine shows minimal fluctuation, creatinine excretion is useful in determining whether 24-hour urine specimens for other analytes (e.g., protein) have been completely and accurately collected. CRP See “C-Reactive Protein (CRP)” Culture, Genital Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 4558 Vaginal, endocervical, urethral, prostatic secretions Sterile Leak-proof Container Room Temperature 48 hrs for Swab Frozen Swabs, Specimens submitted in formalin or other preservative Conventional Culture,Microscopic & Automation Used for diagnosis and treatment of infection. Proper interpretation of culture results depends on specimen source and known pathogenicity of the organism isolated Culture, Genital (Charcoal Media) Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Vaginal, endocervical, urethral, prostatic secretions. Collect specimen using culture swab transport device. Indicate source of specimen on both the test requisition and specimen transport device. Blue cap culture swab device with amies gel transport medium Room temperature 48 hrs for Swab Expired transport swabs • Frozen specimens or requests for anaerobic culture Bacterial culture, aerobic includes routine isolation and identification procedures antibiotic susceptibility testing when appropriate The significance of any isolate(s), in pure or mixed culture, must be assessed with respect to the source cultured, the organism’s pathogenic potential, the possibility of colonization versus infection, and the number of other organisms recovered from the same culture. Culture Fungus other than Blood Includes Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance 45559 4553 Fungal smear, Fungal culture. If culture is positive identification will be performed Raw specimen from any source except blood Sterile container • Swabs in Amies liquid transport medium, or equivalent Room temperature 72 hrs for transport swabs; 2 weeks for hair, skin and nail Refrigerated : 72 hrs for unpreserved specimens other than hair, skin and nail Conventional Culture, Microscopic & Automation This examination can provide the physician with early information regarding the possible need for antifungal treatment. Culture, Aerobic Bacteria with Susceptibility 4550 Includes If culture is positive, identification will be performed. In addition, antibiotic susceptibilities are only performed when appropriate. Preferred Specimen(s)Fluids Instructions Aseptic collection Transport Container Sterile, screw-cap vial Transport Temperature Room temperature 28 Reject Criteria Methodology Clinical Significance Received frozen; non-viable isolates Conventional Culture, Microscopic & Automation Antibiotic susceptibility testing is important in the selection of effective therapy to eradicate infection that if untreated can cause or lead to the development of abscess, tissue damage, and sepsis Culture, Aerobic Blood Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Culture, Throat Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance C D Aerobic culture. If culture is positive,identification will be performed. Antibiotic susceptibilitiesare only performed when appropriate. Adults: 8-10 mL of blood in each of BD BACTEC® Plus Aerobic/F (silver label/gray cap) and Lytic/10 Anaerobic/F bottles (purple label and cap) Neonates and Children 1 to 6 years: 1-3 mL of blood in a BACTEC Peds Plus®/F bottle Children weighing 30-80 lbs: 3 mL of blood in BD BACTEC Peds Plus®/F bottle or 8-10 mL of blood in BD BACTEC® Plus Aerobic/F and Lytic/10 Anaerobic/F bottles Note: Please label requisition “Rule out Anthrax” if suspected. See Blood Cultures in the Bacteria section of Specimen Collection and Handling Do not submit specimens in SPS, heparin, EDTA, and sodium citrate tubes. Do not refrigerate Note: Please label requisition as “Rule Out Anthrax” if suspected. BD BACTEC® Plus Aerobic/F (silver label/gray cap) and Lytic/10 Anaerobic/F bottles (purple label and cap), or BD BACTEC Peds Plus®/F Room temperature 48 hrs Blood specimens collected in EDTA, sodium citrate or anticoagulants other than SPS or heparin • Frozen specimens or specimens broken in transit Rapid Automated Fluroscent Technique Bacterial sepsis constitutes one of the most serious infectious diseases. The detection of microorganisms in a patient’s blood has importance in the diagnosis and prognosis of endocarditis, septicemia, or chronic bacteremia. Culture, Stool (Salmonella/Shigella/Campylobacter) Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology 389 10045 If culture is positive,identification will be performed. Antibiotic susceptibilitiesare only performed when appropriate. Stool submitted in Cary-Blair stool culture transport medium See Stool Specimens in the Bacteria section of Specimen Collection and Handling Cary-Blair transport (or appropriate stool transport medium) Room temperature. Do not refrigerate Unpreserved, at any temperature • Frozen specimens in Cary-Blair transport medium • Expired transport medium • Specimen in diaper or parisitology transport vials Conventional Culture,Microscopic & Automation 394 If culture is positive,identification will be performed. Antibiotic susceptibilitiesare only performed when appropriate. Collect throat specimen using either a BD™ red-cap Amies liquid transport medium swab or BD™ blue-cap, Amies gel medium swab. See Nasopharyngeal Specimens in the Bacteria section of Specimen Collection and Handling. Transport swab Room temperature 48 hrs in Hi culture transport swab & Amies medium Expired transport device • Frozen • Request for anaerobic culture Conventional Culture,Microscopic & Automation The significance of any isolate in pure or mixed culture must be assessed with respect to the source cultured, the organism’s pathogenic potential, the possibility of colonization versus infection, and the number of other organisms recovered in the same culture. This test may be useful in the detection of agents of epiglottis and thrush and A. haemolyticum. 29 Culture, Urine, Routine C D Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 395 If culture is positive,identification will be performed. Antibiotic susceptibilitiesare only performed when appropriate. Clean, sterile plastic or waxed paper cups are used to collect urine before transfer to a 5 ml Vacutainer gray top urine tranport tube. Urine collection kits (gray-top tube); sterile container for specimens <5 mL (for pediatric patients only) Room temperature for preserved urine : 48 hrs; Refrigerated 48 hrs in Vaccutainer brand urine C & S transport kit; Refrigerated : 24 hrs in sterile urine container. If urinalysis transport tube is received • Unpreserved urine >5 mL • Preserved urine >2 days old • Urine tube not filled to minimum fill line • Foley tips • Frozen specimens • Specimens from catheter bag • Urine in urinalysis transport tube Conventional Culture,Microscopic & Automation This culture is designed to quantitate the growth of significant bacteria when collected by the Clean Catch Guidelines or from indwelling catheters. Quantitative culturing of urine is an established tool to differentiate significant bacteruria from contamination introduced during voiding. This test has a reference range of less than 1,000 bacteria per mL. More than 95% of Urinary Tract Infections (UTI) are attributed to a single organism. Infecting organisms are usually present at greater that 100,000 per mL, but a lower density may be clinically important. In cases of UTI where more than one organism is present, the predominant organism is usually significant and others are probably urethral or collection contaminants. When multiple organisms are isolated from patients with indwelling catheters, UTI is doubtful and colonization likely. Culture, Body Fluid 4473 Includes If culture is positive,identification will be performed. Antibiotic susceptibilitiesare only performed when appropriate. Preferred Specimen(s) All body fluids from sterile sites (CSF, Ascitic fluid, Pleural fluid, Synovial fluid) Instructions Collect aseptically and label it appropriately. Transport Container Designated bottles supplied by manufacturer. Transport Temperature Room temperature 24 hrs; Refrigerated : Do not refrigerate cerebrospiral fluid Reject Criteria No swabs are acceptable. Samples like urine, sputum, swabs, stool are unacceptable; received frozen. Methodology Conventional Culture,Microscopic & Automation Clinical Significance Bacterial infections may cause development of abscess, tissue damage, or sepsis, if untreated. Culture, Sputum Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 4556 If culture is positive,identification will be performed. Antibiotic susceptibilitiesare only performed when appropriate. 3 mL sputum Instruct patient to gargle with water and to cough deeply to collect 3 mL deep respiratory specimen in a sterile, leak proof container Sterile screw-cap container Refrigerated, stable 1 week Received at room temperature, frozen; Contaminated; Non-viable isolate Conventional Culture,Microscopic & Automation Respiratory infections may cause bronchitis and pneumonia. Antibiotic susceptibility testing is important in the selection of effective therapy. Cyanocobalamin See “Vitamin B12” Cyclic Citrullinated Peptide (CCP) Antibody IgG Preferred Specimen(s) Transport Container 30 1 mL serum Plastic screw-cap vial 11173 Transport Temperature Room temperature 8 hrs, Refrigerated 48 hrs, -20oC Long term Reject Criteria Gross hemolysis • Gross lipemia • Plasma MethodologyELISA Clinical Significance A synthetic circular peptide containing citrulline called CCP IgG (cyclic citrullinated peptide) has been found to be better at discriminating Rheumatoid Arthritis patients from other patients than either the perinuclear autoantibody test or the test for rheumatoid factor. Approximately 70% of patients with Rheumatoid Arthritis are positive for Anti-CCP IgG, while only about 2% of random blood donors and disease controls subjects are positive. Cysticercus Antibody IgG (Serum) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79494 1 mL Serum Instructions: Centrifuge and immediately separate serum specimens from the cells into clean, plastic, screw-capped vial(s). Transport refrigerated (cold packs). Red-top tube (no gel) Room Temperature: Not defined, Refrigerated : Not applicable, -20oC Long term Gross hemolysis • Hyperlipemia Enzyme-Linked Immunosorbent Assay Cysticercosis is caused by infection with the larval form (cysticercus) of the pork tapeworm Taenia solium. Clinical manifestations of cysticercosis most commonly result from the lodging of cysticerci in brain and neural tissue. Common symptoms of eurocysticercosis include seizures and convulsions. Antibodies from other parasitic infections, especially echinococcosis, may cross-react in the Cysticercus IgG ELISA. Confirmation of positive ELISA results by the Cysticercus IgG Antibody Western Blot is recommended. Cytomegalovirus Antibodies (IgG, IgM) 79533 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient : Not defined, Refrigerated 3 days Reject Criteria Gross Hemolysis MethodologyCLIA Clinical Significance Intrauterine or congenital CMV infections occur in 0.5 to 2.2% of all live births. Symptomatic congenital infections usually occur in infants born to nonimmune mothers who have primary infections during pregnancy. Latency and reactivation of CMV influence the interpretation of serological results. A single positive CMV IgG result is and indication of present or past infection. The presence of CMV IgM suggests a recent CMV exposure but does not differentiate between primary infection and reactivation. Cytomegalovirus Antibodies (IgG) 79910 Preferred Specimen(s) 1 mL serum Transport Container No additive (red-top) or Plastic screw-cap vial Transport Temperature Refrigerated 3 days Reject Criteria Received frozen; Gross hemolysis MethodologyCLIA Clinical Significance The presence of IgG antibodies demonstrate prior infection with Cytomegalovirus (CMV). Seroconversion of CMV IgG from negative to positive or a significant rise in antibody level between paired sera is indicative of active or recent infection. Testing for IgM antibodies (also indicative of active or recent infection) is recommended to support a diagnosis of active disease. Cytomegalovirus Antibodies (IgM) 79912 Preferred Specimen(s) 1 mL serum Transport Container No additive (red-top) or Plastic screw-cap vial. Transport Temperature Refrigerated 3 days Reject Criteria Received frozen; Gross hemolysis. MethodologyCLIA Clinical Significance Exposure to cytomegalovirus (CMV) occurs throughout life and by adulthood, 50 to 90% of 31 C D C D the population is seropositive for CMV antibodies. CMV is spread by close contact, sexual transmission, perinatal or congenital transmission, and through blood transfusions and tissue transplants. Intrauterine or congenital infections occur in 0.5 to 2.2% of all live births. Symptomatic congenital infections usually occur in infants born to nonimmune mothers who have primary infections during pregnancy. Latency and reactivation of CMV influence the interpretation of serological results. A single positive CMV IgG result is an indication of present or past infection. The presence of CMV IgM suggests a recent CMV exposure but does not differentiate between primary infection and reactivation. D-Dimer, Semi-Quantitative Order Code Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79007 1 mL Plasma Do not thaw 3.2% Sodium Citrate (light blue top tube) or Plastic screw vial (Plasma) Frozen, stable 1 month Received Room temperature; Hemolysis Latex agglutination D-Dimer is one of the measurable activation by-products fibrin degradation within the fibrinolytic system. Quantitation of D-Dimer assesses fibrinolytic activation and intravascular thrombosis. D-Dimer is of particular value in excluding the diagnosis of venous thromboembolism among patients at high risk. Dengue Fever Antibody (IgG) 37579 Preferred Specimen(s) 1.0 mL serum Instructions Separate serum from cells as soon as possible Transport Temperature Refrigerated (cold packs) Reject Criteria Received room temperature MethodologyELISA Clinical Significance Dengue hemorrhagic fever and Dengue shock syndrome are caused by infection of a RNA flavivirus transmitted by a mosquito vector. Paired acute and convalescent specimens that exhibit a significant change in titer are useful to confirm clinical diagnosis of infection. See Dengue Fever in the Infectious Disease section of Test Application and Interpretation. Dengue Fever Antibody (IgM) 37580 Preferred Specimen(s) 1.0 mL serum Instructions Separate serum from cells as soon as possible Transport Temperature Refrigerated (cold packs) Reject Criteria Received room temperature MethodologyELISA Clinical Significance Dengue hemorrhagic fever and Dengue shock syndrome are caused by infection of a RNA flavivirus transmitted by a mosquito vector. Paired acute and convalescent specimens that exhibit a significant change in titer are useful to confirm clinical diagnosis of infection. See Dengue Fever in the Infectious Disease section of Test Application and Interpretation. Dengue NS1 Antigen 79555 Preferred Specimen(s) 0.5 mL Serum Transport Container Plastic screw cap vial Transport TemperatureRefrigerated Reject Criteria Grossly hemolyzed, lipemic specimens Methodology Enzyme Immunoassay Clinical Significance Dengue hemorrhagic fever and Dengue shock syndrome are caused by infection of a RNA flavi virus transmitted by a mosquito vector. Paired acute and convalescent specimens that exhibit a significant change in titer are useful to confirm clinical diagnosis of infection. 32 Dengue NS1 Antigen and Dengue Antibodies Panel (IgG & IgM) 78612 Includes NS1 antigen; IgG, IgM antibodies Preferred Specimen(s) 0.5 mL Serum Transport Container Plastic screw cap vial Transport TemperatureRefrigerated Reject Criteria Grossly hemolyzed, lipemic specimens MethodologyELISA Clinical Significance dengue hemorrhagic fever and dengue shock syndrome are caused by infection of therna flavivirus transmitted by a mosquito vector. paired acute and convalescent specimens that exhibit a significant change in titer are useful to confirm clinical diagnosis of infection. Dengue NS1 Antigen And Dengue IgM Panel 78611 Includes NS1 antigen; IgM antibody Preferred Specimen(s) 0.5 mL Serum Transport Container Plastic screw cap vial Transport TemperatureRefrigerated Reject Criteria Grossly hemolyzed, lipemic specimens MethodologyELISA Clinical Significance Dengue hemorrhagic fever and dengue shock syndrome are caused by infection of therna flavivirus transmitted by a mosquito vector. Paired acute and convalescent specimens that exhibit a significant change in titer are useful to confirm clinical diagnosis of infection. Dengue Fever Antibody (IgG, IgM) 34301 Preferred Specimen(s) 1 mL serum Instructions Separate serum from cells as soon as possible Transport Temperature Refrigerated (cold packs) Reject Criteria Received room temperature MethodologyELISA Clinical Significance Dengue hemorrhagic fever and Dengue shock syndrome are caused by infection of a RNA flavivirus transmitted by a mosquito vector. Paired acute and convalescent specimens that exhibit a significant change in titer are useful to confirm clinical diagnosis of infection. See Dengue Fever in the Infectious Disease section of Test Application and Interpretation. Dengue, Antibodies Rapid Detection 79019 Preferred Specimen(s) 1 mL serum Instructions Separate serum from cells as soon as possible Transport Container Plastic screw-cap vial Transport Temperature Refrigerated or room temperature Reject Criteria Received frozen MethodologyImmunochromatography Clinical Significance Dengue hemorrhagic fever and Dengue shock syndrome are caused by infection of a RNA flavivirus transmitted by a mosquito vector. Paired acute and convalescent specimens that exhibit a significant change in titer are useful to confirm diagnosis of infection. DHEA Sulfate 402 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) : 7 days, - 20oc, -2 months Reject Criteria Gross hemolysis MethodologyChemiluminescence Clinical Significance DHEA-S is the sulfated form of DHEA and is the major androgen produced by the adrenal glands. This test is used in the differential diagnosis of hirsute or virilized female patients and for the diagnosis of isolated premature adrenarche and adrenal tumors. About 10% of hirsute women with Polycystic Ovarian Syndrome (PCOS) have elevated DHEA-S but normal levels of other androgens. See Polycystic Ovary Syndrome (PCOS) in the Endocrinology section of Test Application and Interpretation. 33 C D DHT See “Dihydrotestosterone” Diabetic Management Cardiac Panel C D 78535 Includes Glucose Fasting, Glucose Postprandial, Hemoglobin A1c, Cholesterol, Total, Cholesterol, HDL, Cholesterol, LDL (calculated if triglycerides <400 mg/dL), Triglyceride, hs CRP (High sensitivity C Reactive Protein) Preferred Specimen(s) 5 mL whole blood in EDTA (lavender-top) tubes, 4 mL serum from a red-top tube Transport Container 2 EDTA tubes; plastic screw-cap vial Instructions Fasting for at least 12 hours is required for triglycerides. Transport TemperatureRefrigerated Reject Criteria EDTA with hemolysis or received frozen or clotted • Serum: gross hemolysis or Hyperlipemic • Frozen or stored Urine Methodology Spectrophotometry, Neplhometry, HPLC. Clinical Significance See Individual test Diabetes Management Panel Basic (Glucose F & HbA1c) 78559 Preferred Specimen(s) 5 mL whole blood in EDTA (lavender-top) tubes, 4 mL serum from a red-top tube Transport Container 2 EDTA tubes; plastic screw-cap vial Instructions Fasting for at least 12 hours is required for triglycerides. Transport TemperatureRefrigerated Reject Criteria EDTA with hemolysis or received frozen or clotted • Serum: gross hemolysis or Hyperlipemic • Frozen or stored Urine Methodology Spectrophotometry, HPLC Clinical Significance See Individual test Diabetic Profile Includes Instruction Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78665 Lipid Panel, includes Triglycerides, Total Cholesterol, HDL-Cholesterol, LDL- Cholesterol (calculated), Reflex to direct LDL-Cholesterol if Triglycerides 250 mg/dL; Glucose (fasting); Hemoglobin A1c; Creatnine Random Urine, Urea Nitrogen Random Urine 12 hour fasting required 2.0 mL Serum, 0.5 mL fasting plasma in Fluoride tube, 1.0 mL EDTA whole blood, 10.0 mL Random Urine Plastic screw cap vial, Fluoride tube, EDTA tube, Urine Container Serum, Fluoride tube and EDTA tube – Refrigerated, Urine – room Temperature Grossly hemolyzed, lipemic specimens Spectrophotometry, HPLC See individual test for clinical Significance. Dihydropyrimidine Dehydrogenase (DPD) Gene Mutation Analysis 15538 Preferred Specimen(s) 5 mL whole blood collected in an EDTA (lavender-top) or ACD solution B (yellow-top) tube Instructions Whole blood: Normal phlebotomy procedure. Specimen stability is crucial. Store and ship ambient immediately. Do not freeze. Transport Container EDTA (lavender-top) tube Transport Temperature Room temperature Reject Criteria Received frozen Methodology Polymerase Chain Reaction (PCR) • Oligonucleotide hybridizations • Chemiluminescent detection Clinical Significance Partial or complete deficiency of DPD activity has been associated with an increased risk for severe adverse reactions when treated with pyrimidine-based chemotherapeutic agents, such as 5-fluorouracil (5-FU). This test can also be used to confirm the clinical diagnosis of dihydropyrimidine dehydrogenase (DPD) deficiency in affected patients and for the detection of the IVS14 + 1G A mutation in asymptomatic carriers. 34 Dilantin® See “Phenytoin” See “Phenytoin, Free” Direct Antiglobulin Test (DAT) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 5 mL EDTA (lavender-top) whole blood or ACD-A or ACD-B (yellow-top) tube If submitted with a CBC, HBA1c or any other test requiring a lavender-top tube, please submit a separate tube for this test EDTA (lavender-top) tube or ACD-A or ACD-B (yellowtop) tube Room temperature Gross hemolysis • Serum separator tube (SST®) • Received frozen • Red-top tube Immune Agglutination The DAT (Direct Coomb’s test) is positive if red cells have been coated, in vivo, with immunoglobulin, complement, or both. A positive result can occur in immunemediated red cell destruction, autoimmune hemolytic anemia, a transfusion reaction or in patients receiving certain drugs. Direct LDL Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 361 8293 1 mL serum or plasma from EDTA (lavender-top) tube Plastic screw-cap vial Ambient 5 days, Refrigerated 5 days Gross hemolysis • Citrate containing anticoagulants Immunoseparation, Spectrophotometry LDL cholesterol is a key factor in the pathogenesis of atherosclerosis and Coronary Artery Disease (CAD), while HDL cholesterol has often been observed to have a protective effect. Even within the normal range of total cholesterol concentrations, an increase in LDL cholesterol can produce an associated increased risk for CAD. LDL cholesterol binds to receptor sites on macrophages in blood vessel walls inciting several changes to the blood wall which enhance atherosclerotic plaque development. See Markers of Lipidemia in the Cardiovascular section of Test Application and Interpretation. DNA (ds) Antibodies 255 Patient Preparation Overnight fasting is preferred Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 24 hrs, -20oC Long term Reject Criteria Gross hemolysis • Hyperlipemia MethodologyELISA Clinical Significance High levels of antibody to double stranded DNA are found in active systemic lupus erythematosus, but are uncommon in other autoimmune diseases DOC See “Deoxycorticosterone” Drug Panel 11 Includes Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78623 Amphetamine, Cocaine, Methadone, Methaqualone, Cannabinoids (THC), Phencyclidine (PCP), Propoxyphen, Opiates, Barbiturates, Benzodiazepine, Ethanol 10.0 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay See individual test for clinical significance 35 C D Drug Panel 9 Includes Preferred Specimen(s) Instruction Transport Temperature Reject Criteria Methodology Clinical Significance E F 78617 Amphetamine, Cocaine, Cannabinoids (THC), Phencyclidine (PCP), Propoxyphen, Opiates, Barbiturates, Benzodiazepine, Methadone 10.0 mL Urine Collect urine sample without preservative Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay See individual test for clinical significance EBV See “Epstein-Barr Virus testing” Electrolyte Panel Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 34392 Carbon Dioxide, Chloride, Potassium, Sodium 2 mL serum Plastic screw-cap vial Room temperature Gross hemolysis • Plasma See individual tests See individual tests Electrophoresis, Urine See “Protein Electrophoresis, 24-Hour Urine (UPEP)” ENA Antibodies See “Sm and Sm/RNP Antibodies” Entamoeba Antibodies See “Entamoeba histolytica Antibody, IgG, EIA” Entamoeba histolytica Antibody, IgG, EIA 30262 Preferred Specimen(s) 1 mL serum Instructions Separate serum from cells as soon as possible Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Plasma MethodologyELISA Clinical Significance Entamoeba histolytica is a parasitic protozoan that can infect the digestive tract and occasionally other tissues. Antibody IgG is useful in differentiating amebiasis from other causes of liver cysts and parasitic infection. Entamoeba histolytica Antigen, EIA 34964 Preferred Specimen(s) Fresh stool Transport Temperature Refrigerated: 24 hrs, -20oC Long term Frozen: 1 year MethodologyEIA ERA/PRA See “ER/PR Receptor, Paraffin Block, Immunohistochemical” Estrogen and progesterone receptor assays are routinely performed on breast carcinomas to assess responsiveness to endocrine therapy and prognosis. 36 Erythrocyte Sedimentation Rate (ESR) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79930 3 mL of EDTA whole blood or 3 ml whole blood 3.2% sodium citrate Ship samples to laboratory immediately upon collection EDTA vial (Lavender top) or Sodium citrate vial (black top tube) Room temperature or Refrigerated Received frozen Westergren Method The erythrocyte sedimentation rate (ESR), also called a “sedimentation rate,” “sed rate” or ”Biernacki Reaction,” is a non-specific measure of inflammation that is commonly used as a medical screening test. The ESR is increased by any cause or focus of inflammation. The ESR is decreased in sickle cell anemia, polycythemia, and congestive heart failure. The basal ESR is slightly higher in females. ESR testing should be performed within 12 hours of specimen collection. A better alternative acute inflammatory marker is C reactive Protein (CRP). Enhanced Estradiol (eE2) 15577 Preferred Specimen(s) 1.0 mL Serum Transport Container Plastic screw cap vial Transport Temperature Ambient 7 days, Refrigerated 7 days Reject Criteria Grossly hemolyzed, lipemic specimens MethodologyChemiluminescence Clinical Significance Estradiol is the major estrogenic hormone secreted by the ovaries. Measurement of estradiol may be useful in women to assess ovarian function in patients with menstrual disorders, precocious or delayed puberty, and menopause and useful in men to assess gynecomastia. Eosinophil Count, Absolute Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 425 Whole blood full EDTA (lavender-top) tube Maintain specimen at room temperature. If multiple draw, collect EDTA (lavender-top) tube last. Traumatic tap can introduce thromboplastin and trap WBC and platelets. Refrigeration can precipitate fibrin and trap WBC and platelets. Do not refrigerate. EDTA (lavender-top) tube Room temperature Hemolysis • Clotted • Received frozen Electronic Cell Sizing, Sorting/Cytometry/Microscopy Estriol, Unconjugated (uE3) 434 Preferred Specimen(s) 1.0 mL Serum Transport Container Plastic screw cap vial Transport Temperature Ambient 7 days, Refrigerated 7 days Reject Criteria Grossly hemolyzed, lipemic specimens MethodologyChemiluminescence Clinical Significance Much of Estradiol is bound to proteins. The unbound portion and Estradiol bound to proteins with low affinity reflect the Free concentration. The Free Estradiol may better correlate with medical conditions than the Total Estradiol concentrations. Factor V Activity 79347 Preferred Specimen(s) 1.0 mL Citrate Plasma Instruction Give detail of Oral Anticoagulant Therapy Transport Container Plastic screw cap vial Transport TemperatureFrozen Reject Criteria Grossly hemolyzed, lipemic specimens MethodologyCoagulation Clinical Significance This test is useful to evaluate a prolonged PT. Deficiency is associated with bleeding risk. 37 E F Factor V (Leiden) Mutation Analysis E F 17900 Preferred Specimen(s) 5 mL whole blood, EDTA (lavender-top) tube Instructions Whole blood: Normal phlebotomy procedure. Specimen stability is crucial. Store and ship room temperature immediately. Do not freeze. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received frozen Methodology Polymerase Chain Reaction (PCR), Oligonucleotide Ligation Assay, Fluorescent Microspheres Clinical Significance Factor V (Leiden) Mutation is a point mutation that causes resistance of Factor V protein degradation by activated protein C (APC). This mutation is associated with increased risk of venous thrombosis. Factor V HR2 Allele DNA Mutation Analysis 17902 Preferred Specimen(s) 5 mL whole blood EDTA (lavender-top) preferred Instructions Forward tissue specimens immediately to the Molecular Genetics Laboratory; do not hold. Whole Blood: Normal phlebotomy procedure. Specimen stability is crucial. Store and ship room temperature immediately. Do not freeze. For prenatal diagnosis with a fetal specimen: 1) parents must be documented carriers of one of the mutations tested; 2) maternal blood or DNA must be available; 3) contact the laboratory genetic counselor before submission. Amniotic fluid: Normal collection procedure. Specimen stability is crucial. Store and ship room temperature immediately. Do not refrigerate or freeze. Amniotic culture: Sterile T25 flask, filled with culture medium. Specimen stability is crucial. Store and ship room temperature immediately. Do not refrigerate or freeze. Dissected chorionic villus (CVS) biopsy: 10-20 mg dissected chorionic villi collected in sterile tube filled with sterile culture media. Specimen stability is crucial. Store and ship room temperature immediately. Do not refrigerate or freeze. Please indicate the ethnicity of the patient. Do not hold cells; forward to laboratory when cells arrive. Transport TemperatureFrozen Reject Criteria Frozen samples • Exceeds specimen stability • Wrong specimen type Methodology Polymerase Chain Reaction (PCR), Oligonucleotide Ligation Assay, Fluorescent Microspheres Clinical Significance Factor V HR2 Allele, DNA Mutation Analysis is useful in patients who are carriers of Factor V Mutation (Leiden). Coinheritance ofFactor V Mutation (Leiden) is associated with a 3-4- fold increased risk of venous thrombosis compared to inheritance of Factor V Mutation (Leiden) alone. Factor VII 79113 Preferred Specimen(s) 1.0 mL Citrate Plasma Instruction Give detail of Oral Anticoagulant Therapy Transport Container Plastic screw cap vial Transport TemperatureFrozen Reject Criteria Grossly hemolyzed, lipemic specimens MethodologyCoagulation Clinical Significance This test is useful to evaluate a prolonged PT. Deficiency is associated with bleeding risk. Factor VIII Activity, Clotting 347 Preferred Specimen(s) 1.0 mL Citrate Plasma Instruction Give detail of Oral Anticoagulant Therapy Transport Container Plastic screw cap vial Transport TemperatureFrozen Reject Criteria Grossly hemolyzed, lipemic specimens MethodologyCoagulation Clinical Significance This test is useful to evaluate a prolonged aPTT. The most common form of hemophilia is caused by deficiency of factor VIII. Hemophilia A is an x-linked disorder affecting between 1 in 5,000 to 10,000 males. 38 Factor X, Activity 79112 Preferred Specimen(s) 1.0mL Citrate Plasma Instruction Give detail of Oral Anticoagulant Therapy Transport Container Plastic screw cap vial Transport TemperatureFrozen Reject Criteria Grossly hemolyzed, lipemic specimens MethodologyCoagulation Clinical Significance This test is useful to evaluate a prolonged PT. Factor XIII Activity 14461 Preferred Specimen(s) 1 mL citrated plasma Instructions Freeze immediately after separating from cells. Do not thaw. Transport Container Plastic screw vial Transport TemperatureFrozen Reject Criteria Received room temperature or refrigerated; hemolysis; lipemia MethodologyChromogenic Clinical Significance Low Factor XIII levels, i.e., <15%, may cause a bleeding disorder and levels <2% have been associated with spontaneous intracranial hemorrhage. Ferritin 457 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 7 days Reject Criteria Plasma • Gross hemolysis MethodologyChemiluminescence Clinical Significance Useful in the diagnosis of hypochromic, microcytic anemias. Decreased in iron deficiency anemia and increased in iron overload. Fibrinogen Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 461 3.2% sodium citrate (light blue-top) tube Correct ratio of blood to citrate is critical. Do not overfill or underfill collection tube. Mix by inversion 4 times. Do not pool plasma from multiple tubes. For nonheparinized patients, maintain specimen at room temperature. Do not uncap. Non-heparinized patients are stable up to 72 hours at room temperature. Heparinized patients stable for 24 hours at room temperature. If testing cannot be completed within stability limits, centrifuge specimen within 1 hour of collection at least 1500 RCF (relative centrifugal force) for 15 minutes. Transfer plasma to a plastic screw-cap vial and freeze at -200 C immediately. Whole blood: 3.2% sodium citrate (light blue-top) tube Plasma: Plastic screw-cap vial (frozen) Room temperature for light blue-top (sodium citrate) tube; frozen for plasma in plastic screw-cap vials Hemolysis • Clotted Cloth Detection Fibrinogen is essential for the formation of a blood clot. Deficiency can produce mild to severe bleeding disorders. See Non-Lipid Markers of Cardiovascular Disease in the Cardiovascular chapter of Test Application and Interpretation. Fibrinogen Degradation Product (FDP) Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance 458 1 mL citrated plasma Plastic screw cap vial Frozen, stable 1 month Latex Agglutination Bleeding disorders may be due to inherited or acquired deficiencies of a clotting factor. Filariasis, Blood See “Malaria Blood Parasites” 39 E F First Trimester Screening With NT Value E F 79223 Preferred Specimen(s) 2mL Serum Transport Container Red top tube or SST or Plastic screw cap tube Transport Temperature Refrigerated (2-8°C) - 24 hrs; Frozen - 20°C - 2 months Reject Criteria EDTA Plasma, Hemolyzed, Lipemic and icteric specimens not acceptable. MethodologyChemiluminescene Clinical Significance Maternal serum PAPP-A and free beta HCG assessment between 11 and 14 weeks of pregnancy is reported to have significant utility in screening & Down syndrome and other chromosomal abnormalities. A combination of maternal age related risk, Free beta - HCG & fetal nuchal translucency (NT) measurements might substantially increase the efficiency of prenatal screening. First Trimester Screening Without NT Value 79221 Preferred Specimen(s)Serum Transport Container Red top tube or SST or Plastic screw cap tube Transport Temperature Refrigerated (2-8°C) - 24 hrs; Frozen - 20°C - 2 months Reject Criteria EDTA Plasma, Hemolyzed, Lipemic and icteric specimens not acceptable. MethodologyChemiluminescene Clinical Significance Maternal serum PAPP-A and free beta HCG assessment between 11 and 14 weeks of pregnancy is reported to have significant utility in screening & Down syndrome and other chromosomal abnormalities. A combination of maternal age related risk, Free beta - HCG & fetal nuchal translucency (NT) measurements might substantially increase the efficiency of prenatal screening. FISH TEL/AML 1 assay 14644 Preferred Specimen(s) 3 - 4 ml Whole Blood (Min2 - 3 ml) Green Top Sodium Heparin Tube (Random); Room Temperature; -OR 3 mL Bone Marrow (Min1 mL) in Transport Media or Green Top Sodium Heparin Tube (Random); Room Temperature; Instructions Clinical history and reason for referral are required with test order. Prior therapy/transplant information should be submitted with test order. This FISH (fluorescence in situ hybridization) procedure is used to detect the TEL/AML1 gene fusion resulting from a cytogenetically undetectable t(12;21)(p13;q22) translocation, which is common in pediatric pre B-ALL. This test is useful for the evaluation of suboptimal specimens, cases with a normal karyotype, or when an abnormal karyotype lacking a specific/prognostically defined abnormality or demonstrating deletion 12p is found. Bone marrow transport medium is available upon request. Instructions, Specimen stability/rejection requirements: Specimen viability decreases during transit. Send specimen to testing laboratory for viability determination. Do not reject. Transport Container Culture Transport Media Transport Temperature Room Temperature Reject Criteria Frozen; Clotted; Hemolysed Methodology Fluorescence In Situ Hybridization Clinical Significance Cryptic translocation undetectable by routine cytogenetic analysis, present in approximately 30% of precursor B-cell acute lymphoblastic leukemia and associated with favorable prognosis. FISH PML/RARA Assay 14643 Preferred Specimen(s) 3 - 4 mL Whole Blood (Min3 mL) Green Top Sodium Heparin Tube (Random); Room Temperature; -OR 3 mL Bone Marrow (Min1 mL) in Transport Media or Green Top Sodium Heparin Tube (Random); Room Temperature; Instructions Clinical history and reason for referral are required with test order. Prior therapy/transplant history should be submitted with test order. This test is performed to detect the PML/RARA molecular rearrangement by FISH (fluorescence in situ hybridization). Bone marrow transport 40 Transport Container Transport Temperature Specimen Stability Reject Criteria Methodology Clinical Significance medium is available upon request. Instructions, Specimen stability/rejection Requirements: Specimen viability decreases during transit. Send specimen to testing laboratory for viability determination. Do not reject. Culture Transport Media Room Temperature Room Temperature: See instruction Refrigerated: See instruction Frozen; Clotted; Hemolysed Fluorescence In Situ Hybridization To rule out the presence of a PML/RARA rearrangement specific for acute promyelocytic leukemia (APML). FISH ETO/AML1 Assay 14640 Preferred Specimen(s) 3 mL Bone Marrow (Min 1 mL) in Transport Media or Green Top Sodium Heparin Tube (Random); Room Temperature; -OR 3 - 4 mL Whole Blood (Min 1 mL) Green Top Sodium Heparin Tube (Random); Room Temperature; Instructions Clinical history and reason for referral are required with test order. Prior therapy/transplant information should be submitted with test order. This test is useful for detecting cell populations that may not be mitotically active, that have suboptimal chromosome morphology, or that have variant or cryptic rearrangements. Bone marrow transport medium is available upon request. Instructions, Specimen stability/rejection Requirements: Specimen viability decreases during transit. Send specimen to testing laboratory for viability determination. Do not reject. Transport Container Culture Transport Media Transport Temperature Room Temperature Reject Criteria Frozen; Clotted; Hemolysed Methodology Fluorescence In Situ Hybridization Clinical Significance The (8:21) translocation is the most frequently observed karyotypic abnormality associated with acute myeloid leukemia (AML), subtype M2. Patients with this type of AML have a high remission rate with conventional chemotherapy. FISH, EGFR Preferred Specimen(s) Instructions Transport Container Transport Temperature Methodology Clinical Significance 19041 Formalin fixed paraffin embedded tissue Formalin fixed, paraffin embedded human tissue specimen. Formalin fixed paraffin embedded tissue block Room temperature Fluorescence In-Situ Hybridization (FISH) The epidermal growth factor receptor (EGFR) is a cellular transmembrane receptor with tyrosine kinase enzymatic activity that plays a key role in human cancer. EGFR-dependent signaling is involved in cancer cell proliferation, apoptosis, angiogenesis, invasion and metastasis. Targeting the EGFR is a valuable molecular approach in cancer therapy. FISH, HER-2/neu, Paraffin Block Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance 14620 Breast tissue biopsy, formalin fixed paraffin-embedded block Pathology report or pathologic diagnosis must be included with IHC score for ER, PR & HER-2/neu findings Sterile screw-cap vial or paraffin block bag Room temperature Fluorescence in situ Hybridization (FISH) HER-2 oncogene amplification in stage 2 lymph node positive breast cancer which aids in treatment selection and prognostication See FISH, HER-2/neu, Paraffin Block in the Hematology/Oncology section of Test Application and Interpretation 41 E F Flow Surface Light Chains, Flow Cytometry E F 11015 Includes Kappa and Lambda Light Chains Preferred Specimen(s) 5 mL whole blood, bone marrow or tissue/fluid collected into a sodium heparin (green-top) tube Instructions Submit Sodium Heparin (green-top) tube whole blood or 2 mL heparinized bone marrow. A freshly prepared smear (stained or unstained) is also recommended. A clinical summary or differential diagnosis is required along with specimen OR place a representative portion of fresh tissue (0.5 cm square) in sterile tissue culture medium such as RPM1-1640 in a sterile container. Alternatively, place the tissue on a saline-soaked gauze pad in a sealed specimen cup and ship refrigerated. Do not suspend the tissue in saline. Please submit stained H & E slide, a copy of the pathology report and a brief clinical summary. Transport Container Sodium heparin (green-top) tube Transport Temperature Blood/Bone Marrow: Room temperature Tissue/Fluid: Refrigerated (cold packs) Reject Criteria Received frozen • Fixed sample Methodology Flow Cytometry Clinical Significance The presence of immunoglobulin light chains (kappa or lambda) on the cell surface is characteristic of clonal proliferation most often seen in multiple myeloma and lymphoproliferative diseases Flow ONTAK® Sensitivity (CD25) 11237 Preferred Specimen(s) 5 mL whole blood or bone marrow collected in a (greentop) sodium heparin tube Transport Container Plastic screw-cap vial Transport Temperature Room temperature Reject CriteriaFrozen Methodology Flow Cytometry Clinical Significance ONTAK® is indicated for the treatment of patients with persistent or recurrent cutaneous T-cell lymphoma (CTCL) with malignant cells that express CD25. Pretreatment testing to establish CD25 sensitivity is available. See Hematopoietic/Lymphoid Disorders in the Hematology/Oncology section of Test Application and Interpretation. Flow NK Cells (CD3/CD45/CD16+CD 56/CD19) Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 1.0 mL Whole Blood in EDTA (lavender top) Vial Do not freeze. Submit the EDTA tubes at room temperature. Collection Tube Room Temperature Hemolyzed, Whole blood received frozen Flow Cytometry This test measures Natural Killer cells. Measurement of NK cells is useful in the diagnosis of retinoblastomas, medullblastomas, astrocytomas, and neuroblastomas. Flow Lymphocte Subset CD3% (Flow Cytometry) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 42 14798 19913 5 mL whole blood collected in an EDTA (lavender-top) tube Specimens are stable for 48 to 72 hours at room temperature. If a CBC is also required, a separate EDTA (lavender-top) tube must be submitted. 5 mL (or 3 mL pediatric) EDTA (lavender-top) tube Room temperature Hemolysis • Clotted • Frozen Flow Cytometry CD3 is a cell surface marker on lymphocyte T cell population that defines the total population of T cells. A common usage of lymphocyte characterization is to monitor patients with HIV infection. The CD4:CD8 (CD3) ratio is often inverted in patients infected with HIV. These patients are at increased risk of opportunistic infections. Flow Lymphocte Subset CD4% (Flow Cytometry) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 5 mL whole blood collected in an EDTA (lavender-top) tube Specimens are stable for 48 to 72 hours at room temperature. If a CBC is also required, a separate EDTA (lavender-top) tube must be submitted. 5 mL (or 3 mL pediatric) EDTA (lavender-top) tube Room temperature Hemolysis • Clotted • Frozen Flow Cytometry CD4 is a cell surface marker on lymphocyte T cell population that defines the subpopulation of T helper cells. A common usage is to monitor patients with HIV infection since CD4 cell population is down-regulated during disease progression. The CD4:CD8 (CD3) ratio is often inverted in patients infected with HIV. These patients are at increased risk of opportunistic infections. Flow Lymphocte Subset CD8% (Flow Cytometry) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 14804 19914 5 mL whole blood collected in an EDTA (lavender-top) tube Specimens are stable for 48 to 72 hours at room temperature. If a CBC is also required, a separate EDTA (lavender-top) tube must be submitted. 5 mL (or 3 mL pediatric) EDTA (lavender-top) tube Room temperature Hemolysis • Clotted • Frozen Flow Cytometry CD8 is a cell surface marker on lymphocyte T cell population that defines the subpopulation of T suppressor cells. A common usage is to monitor patients with HIV infection. The CD4: CD8 (CD3) ratio is often inverted in patients infected with HIV. These patients are at increased risk of opportunistic infections. Fluid Analysis, Ascitic Fluid 78549 Includes Biochemistry, Cell count Preferred Specimen(s) 2 ml ascitic fluid Transport Container Plastic screw-cap container/EDTA tube Transport TemperatureRefrigerated Reject Criteria Gel barrier tube; frozen Methodology PAP stain, Geimsa stain, Microscopic examination Clinical Significance Fluid analysis is useful to describe the cause of fluid accumulation, i.e., transudate, exudate, hemorrhage, or effusion. Ascites fluid may be secondary to malignancy even with negative cytological exam. Fluid Analysis, Pericardial Fluid 78551 Includes Biochemistry, Cell count Preferred Specimen(s) 3 ml pericardial fluid Instructions Grossly hemolyzed specimens are unacceptable. Freeze immediately after collection. Transport Container Sterile, screw-cap container/EDTA tube Transport TemperatureRefrigerated Reject Criteria Gel barrier tube, received at room temperature; frozen Methodology PAP stain, Geimsa stain, Microscopic examination Clinical Significance Fluid analysis is useful to describe the cause of fluid accumulation, i.e., transudate, exudate, hemorrhage, or effusion. Abnormal pericardial fluid analysis may suggest infection, inflammation, cardiac trauma, or tumor. Fluid Analysis, Pleural Fluid Includes Preferred Specimen(s) Instructions Transport Container 78552 Biochemistry, Cell count 2 ml pleural fluid Avoid hemolysis Sterile, screw cap container/EDTA tube 43 E F Transport TemperatureRefrigerated Reject Criteria Gel barrier tube, received at room temperature; Frozen Methodology PAP stain, Geimsa stain, Microscopic examination Clinical Significance Fluid analysis is useful to describe the cause of fluid accumulation, i.e., transudate, exudate, hemorrhage, or effusion. Abnormal pleural fluid analysis may suggest infection including tuberculosis, congestive heart failure, cirrhosis, nephritis, injury such as perforation, and tumor. Fluid Analysis, Synovial Fluid E F 78553 Includes Cytology, Biochemistry, Cell count Preferred Specimen(s) 2 ml synovial fluid Transport Container Sterile plastic transport tube Transport TemperatureRefrigerated Reject Criteria Gel barrier tube, frozen Methodology PAP stain, Geimsa stain, Microscopic examination Clinical Significance Fluid analysis is useful to describe the cause of the fluid accumulation. Abnormal synovial fluid analysis is associated with gout, rheumatoid arthritis, septic arthritis, traumatic arthritis, and infections. Free ß-hCG Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79620 1.0 mL Serum Plastic screw cap vial Refrigerated, stable 7 day’s Grossly hemolyzed, lipemic specimens Chemiluminescent Enzyme Immunoassay Maternal serum free Beta HCG assessment is reported to have significant utility in first & second trimester prenatal screening for Down syndrome & other chromosomal anomalies. A first trimester combination of maternal age, serum PAPP-A & fetal nuchal translucency (NT) measurements might substantially increase the efficiency of the prenatal screening compared to second trimester screening; using this approach, various investigator have reported detection rates for Down syndrome of 85 to 90 percent at a 5% false positive rate. FOBT See “Fecal Globin by Immunochemistry (InSure®)” Folate, Serum 466 Preferred Specimen(s) 1 mL serum Instructions Folate is light sensitive. Minimize exposure to light during sample handling and storage. Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, stable 5 day’s Reject CriteriaHemolysis MethodologyChemiluminescence Clinical Significance Folic acid deficiency is common in pregnant women, alcoholics, in patients whose diets do not include raw fruits and vegetables, and in people with structural damage to the small intestine. The most reliable and direct method of diagnosing folate deficiency is the determination of folate levels in both erythrocytes and serum. Low folic acid levels, however, can also be the result of a primary vitamin B12 deficiency that decreases the ability of cells to take up folic acid. Folic Acid See “Folate, Serum” 44 Follicular Lymphoma, bcl-2/JH t(14;18), Real-Time PCR, Plasma-Based Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 17690 3 mL EDTA (lavender-top tube) whole blood Submission of whole blood: Follow standard whole blood collection procedure. Collect 3-5mL whole blood samples in an EDTA tube. Blood samples are shipped at room temperature or 4°C. Do not freeze whole blood. Record the draw time and the date on the tube. Ship immediately to maintain sample stability. Submission of plasma: Collect blood in a sterile tube containing EDTA anticoagulant (lavender-top). Separate plasma from the cellsy centrifugation within 2 hours after collection at least 1250 RCF (relative centrifugal force) for 15 minutes, transfer the plasma to a separate plastic screw-cap vial, and ship frozen. Note: Information regarding draw time and date is required to ensure stability of the sample is maintained. EDTA (lavender-top) tube Refrigerated (cold packs) 5 days Gross hemolysis • Received frozen blood samples • Received clotted blood samples Real-Time Polymerase Chain Reaction, (RT-PCR) The plasma based molecular assay is based on the concept that in hematological diseases, tumor cells pour their DNA and RNA into the circulation. These components can be detected in plasma, and can replace the routine painful bone marrow aspiration or biopsy procedure. The presence of the bcl-2 translocation has been associated with poor prognosis in one group of diffuse large-cell and follicular lymphoma patients. Analysis of bcl-2 translocation also provides an important marker for detection and of monitoring of malignancy during patient treatment and follow-up. Fructosamine 8340 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial or spun barrier tube Transport Temperature Refrigerated 2 weeks Reject Criteria Hemolysis • Moderate or grossly icteric MethodologyColorimetry Clinical Significance The fructosamine assay is useful in monitoring the degree of glycemia over short-to- intermediate time frames (1-3 weeks). A fructosamine concentration greater than the established normal range is an indication of prolonged hyperglycemia of 1-3 weeks or longer. The higher the fructosamine value, the poorer the degree of glycemic control. FSH (Follicle Stimulating Hormone) 470 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Stable 7 days, Refrigerated 14 days MethodologyChemiluminescence Clinical Significance This test is useful in the differential diagnosis of pituitary and gonadal insufficiency and in children with precocious puberty FT4 See “T4 Free (FT4)” Fungus Culture, Blood See “Culture, Blood” Fungus, Direct Examination, Skin, Hair or Nails Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria 14824 Skin, hair, or nails Sterile screw-cap container Room temperature 2 weeks Received frozen 45 E F Methodology Fluroscent Microscopic Clinical Significance Tissues containing keratin (skin, hair, and nails) can become infected with dermatophytes. These superficial fungal infections range in severity. Proper diagnosis can guide selection of therapy. G-6-PD See “Glucose-6-Phosphate Dehydrogenase, Quantitative” Gamma Glutamyl Transferase (GGT) G H 482 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 2 weeks Reject Criteria Hemolysis • Plasma MethodologySpectrophotometry Clinical Significance Elevated GGT is found in all forms of liver disease. Measurement of GGT is used in the diagnosis and treatment of alcoholic cirrhosis, as well as primary and secondary liver tumors. It is moresensitive than alkaline phosphatase, the transaminases, and leucine aminopeptidase in detecting obstructive jaundice, cholangitis, and cholecystitis. Normal levels of GGT are seen in skeletal diseases; thus, GGT in serum can be used to ascertain whether a disease, suggested by elevated alkaline phosphatase, is skeletal or hepatobiliary. Genotype MTbDR Panel 79554 Includes MTb Rapid RIF/INH sens. assay and Genotype MTb second line (Aminoglycosides and Flouroquinolones) 79552 - MTb Rapid RIF/INH sens. assay 79553 - Genotype MTb second line See individual test for details GGT See “Gamma Glutamyl Transferase (GGT)” Gliadin Antibody (IgA) 11228 Preferred Specimen(s) 1 mL serum Instructions Avoid lipemia Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 48 hrs, Ambient 8 hrs, -20oC Long term Reject Criteria Gross hemolysis • Lipemia MethodologyELISA Clinical Significance See Gliadin Antibody Panel (IgA, IgG) in the Immunology section of Test Application and Interpretation. Gliadin Antibody (IgG) 11212 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 48 hrs, Ambient 8 hrs, -20oC Long term Reject Criteria Gross hemolysis • Gross Lipemia • Plasma MethodologyELISA Clinical Significance Celiac Disease is characterized by the presence of Gliadin Antibody. Such patients display a hypersensitivity to gluten (wheat) in their diet. The antibody is undetectable when patients with hypersensitivity are placed on gluten-free diets. Antibody IgA is more specific and IgG is a more sensitive assay to Celiac Disease. See Gliadin Antibody Panel (IgA, IgG) in the Immunology section of Test Application and Interpretation. 46 Glucose Patient Preparation Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 483 Patient should fast for 8 hours 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Unspun SST • Red-top or non-plasma separator (PST) green-top tubes • Anticoagulants other than litium heparin, sodium heparin or fluoride/oxalate Spectrophotometry (SP) Serum glucose levels may be abnormally high (hyperglycemia) or abnormally low (hypoglycemia). Glucose measurements are used in the diagnosis and treatment of carbohydrate metabolic disorders including diabetes mellitus, idiopathic hypoglycemia, and pancreatic islet cell neoplasm. See Diabetes in the Endocrinology section of Test Application and Interpretation. Glucose, Random (Plasma) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 8917 1 mL plasma collected in a Fluoride/EDTA Tube Plastic Screw cap vial Ambient 5 days, Refrigerated 2 weeks Unspun sst, red-top or non-plasma separator (pst) green-top tubes. Anticoagulants other than lithium heparin, sodium heparin or fluoride/oxalate. Spectrophotometry (SP) Plasma glucose levels may be abnormally high (hyperglycemia) or abnormally low (hypoglycemia). Glucose measurements are used in the diagnosis and treatment of carbohydrate metabolic disorders including diabetes mellitus, idiopathic hypoglycemia, and pancreatic islet cell neoplasm. Glucose Tolerance Test, 3 serum specimens (75g) 23475 Includes Fasting, 1-Hour, 2-Hour glucose Patient Preparation Fasting required. Fasting is defined as no consumption of food or beverage other than water for at least 8 hours before testing. Preferred Specimen(s) Three - 1 mL plasma specimens collected in fluoride/EDTA Tubes Instructions Immediately after a fasting specimen is obtained, have patient ingest a 75 g load of glucose. Draw subsequent specimens 1 and 2 hours later. Label each with the specific draw time. For children, the glucose load is 1.75 g glucose per kg ideal body weight, up to 75 g (pounds/2.2 = kilograms). See table below. Weight of Patient (kg) g of glucose 10.9-14.9 22.5 15.0-19.4 30.0 19.5-23.5 37.5 23.6-28.1 45.0 28.2-32.2 52.5 32.3-36.7 60.0 36.8-40.8 67.5 >40.8 75.0 Transport Container Plastic screw-cap vials Transport Temperature Ambient 5 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Serum • Anticoagulants other than fluoride/ oxalate MethodologyHexokinase Clinical Significance This test is used for the routine diagnosis of diabetes in children and the non-pregnant adult. For pregnant females see test “Glucose Tolerance Test, Gestational, 4 Specimens (100 g)”. For appropriate interpretation of this test, the patient must fast overnight and ingest a 75 g load of glucose. Immediately after, a fasting specimen is obtained. For children, the glucose load is 1.75 g/Kg of body weight, up to 75. The diagnosis of diabetes is made if the fasting glucose is .126 mg/dL or if the 2-hour specimen is .200 mg/dL. 47 G H Glucose, Fasting & Post Prandial Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 1.0 mL plasma after 12 hour fasting and 1.0 mL plasma post 2 hours of breakfast in Fluoride/ EDTA Tube Patient should fast for 8 hours Plastic screw-cap vial Ambient 5 days, Refrigerated 14 days Unspun SST • Red-top or non-plasma separator (PST) green-top tubes • Anticoagulants other than litium heparin, sodium heparin or fluoride/oxalate Spectrophotometry (SP) Diagnosis of diabetes mellitus and evaluation of carbohydrate metabolism. Glucose, Fasting (Plasma) G H Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 6881 484 1.0 mL plasma after 12 hrs Fasting in Fluoride/EDTA Tube Patient should fast for 8 hours Plastic screw-cap vial Ambient 5 days, Refrigerated 14 days Unspun SST • Red-top or non-plasma separator (PST) green-top tubes • Anticoagulants other than litium heparin, sodium heparin or fluoride/oxalate Spectrophotometry (SP) Diagnosis of diabetes mellitus and evaluation of carbohydrate metabolism. Glucose 6 Phosphate Dehydrogenase (G-6-PD) Activity Blood (Quantitative) 78024 Preferred Specimen(s) 1.0 mL whole blood collected in an EDTA (lavender-top) tube Transport Container EDTA (lavender-top) tube Transport Temperature Refrigerated (cold packs) 7 days Reject Criteria Received frozen, grossly hemolysed MethodologySpectrophotometry Clinical Significance G-6-PD is the most common enzyme deficiency in the world. Newborns with G-6-PD may have prolonged and more pronounced neonatal jaundice than other newborns. Older individuals are subject to hemolytic anemia that can be induced by some foods, drugs, and infections. Glucose Tolerance Test, Gestational, 4 Specimens (100mg) Includes Patient Preparation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Fasting, 1-Hour, 2-Hour, 3-Hour glucose Fasting required. Fasting is defined as no consumption of food or beverage other than water for at least 8 hours before testing. Four-1 mL plasma specimens collected in fluoride/EDTA Tubes Immediately after a fasting specimen is obtained, have patient ingest a 100 g load of glucose. Draw subsequent specimens 1, 2 and 3 hours later. Label each with the specific draw time. Plastic screw-cap vials Ambient 5 days, Refrigerated 14 days Gross hemolysis • Serum • Anticoagulants other than fluoride/ oxalate Spectrophotometry (SP) Plasma glucose levels may be abnormally high (hyperglycemia) or abnormally low (hypoglycemia). Glucose measurements are used in the diagnosis and treatment of carbohydrate metabolic disorders. Glucose, Gestational Screen (50g) Patient Preparation Preferred Specimen(s) Instructions 48 6745 8477 The patient is given a 50 gram dose of glucose and a single blood specimen is obtained one hour later. Fasting is not required. 1 mL plasma collected in a fluoride/EDTA Tube The patient is given a 50 gram dose of glucose and a single blood specimen is obtained one hour later. Fasting is not required. Note: The test should be performed between weeks 24 and 28 of gestation. Transport Container Fluoride/EDTA Tube or plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Anticoagulants other than fluoride/oxalate • Serum MethodologyHexokinase Clinical Significance A value of 130 mg/dL or greater indicates the need for a full diagnostic, gestational glucose tolerance performed in the fasting state to determine if the patient has gestational diabetes. Glucose, Postprandial 78005 Preferred Specimen(s) 1 ml plasma NaF Instructions Sample should be collected 2 hours after meal Transport Container Plastic screw cap vial Transport Temperature Ambient 5 days, Refrigerated 14 days Reject Criteria Received room temperature MethodologySpectrophotometry Clinical Significance Postprandial glucose may be useful in evaluating diabetes mellitus and carbohydrate metabolism. Gram Stain 497 Preferred Specimen(s) Swabs, sputum, bronchial washing, body fluids, urine, tissue Instructions Collect using sterile technique Transport Container Bacterial transport tube, sterile screw cap container, or transport tube with preservative (for urine) Transport Temperature Room termperature : 10 days for dried smear and 2 days for specimen swab Refrigerated : Respiratory specimen and body fluids are stable upto 24 hrs & 48 hrs, respectively Reject Criteria Received at room temperature; Frozen Methodology Microscopic Examination Clinical Significance The Gram Stain is a rapid, preliminary test to identify bacterial infections and to guide initial antibacterial therapy. Growth Hormone Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 521 1.0 mL Serum Patient should be fasting and at complete rest 30 minutes before blood collection. Plastic screw cap vial Refrigerated (Stability 7 days) Grossly hemolyzed, lipemic specimens Chemiluminescent Enzyme Immunoassay Measurement of GH is primarily of interest in the diagnosis and treatment of various forms of inappropriate growth hormone secretion. Growth hormone measurements in children are used in the evaluation of short stature and help differentiate low GH production from other sources of growth failure. Stimulation and suppression tests are often more meaningful than random measurements. Haptoglobin Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 502 1 mL serum Plastic screw-cap vial Refrigerated 7 days Hemolysis • Hyperlipemia Nephelometry Decreased haptoglobin is found in hemolytic disease, hepatocellular disease and infectious mononucleosis. Increased level is found in inflammatory disease in the presence of tissue necrosis and in general acute inflammatory conditions. Haemoglobin and Hematocrit Panel Preferred Specimen(s) Transport Container 7998 3 ml whole blood in EDTA vial (lavender-top tube) EDTA vial (lavender-top) tube 49 G H Transport Temperature Room temperature Reject Criteria Received frozen MethodologyMethemoglobin Clinical Significance An automated blood analysis provides insights into medical conditions associated with changes in red blood cells, e.g., polycythemia vera and anemias. HBe Antigen See “Hepatitis Be Antigen” Hb Electrophoresis by Capillarys G H 78942 Preferred Specimen(s) 3 mL whole blood Instruction Overnight fasting is preferred Transport Container lavender top EDTA Transport TemperatureRefrigerated Reject Criteria Received clotted Methodology Capillarys Electrophoresis Clinical Significance Haptoglobin binds free hemoglobin and acts as an indicator of erythrocyte destruction or hemolysis. With binding of hemoglobin, the haptoglobin complex is destroyed and concentrations are low. Haptoglobin is an acute phase reactant and elevated concentrations are observed with inflammatory diseases. hCG, Qualitative, Urine Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance 396 10 mL urine from a first morning voided specimen Urine Collection Container Room temperature Immunoblot assay This test is specific for hCG beta subunit and offers sensitivity necessary to detect pregnancy as early as ten days post conception hCG, Total, Quantitative 8396 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 7 days MethodologyChemiluminescence Clinical Significance hCG may reach detectable limits within 7-10 days of conception. hCG is produced by the placenta and reaches a peak between the 7th and 10th week of gestation. hCG is a glycoprotein hormone produced by the syncytiotrophoblast of the placenta and secreted during normal pregnancy and with pathologic conditions such as hydatidiform mole, choriocarcinoma and testicular neoplasm. Order hCG, Total, QL, Urine, if hCG serum result is inconsistent with clinical presentation. HDL Cholesterol 608 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Anticoagulants other than heparin Methodology Spectrophotometry (SP) Clinical Significance HDL cholesterol is inversely related to the risk for cardiovascular disease. It increases following regular exercise, moderate alcohol consumption and with oral estrogen therapy. Decreased levels are associated with obesity, stress, cigarette smoking and diabetes mellitus. See Markers of Lipidemia in the Cardiovascular Tests section of Test Application and Interpretation. 50 Hemoglobin A1c 496 Preferred Specimen(s) 1 mL whole blood collected in a EDTA (lavender-top) tube Transport Container EDTA (lavender-top) tube Transport Temperature Ambient 3 days, Refrigerated 7 days MethodologyHPLC Clinical Significance Assesses long term diabetic control in diabetes mellitus See Diabetes in the Endocrinology section of Test Application and Interpretation. Hemoglobin Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 510 3 ml Whole blood full EDTA (lavender-top) tube Maintain specimen at room temperature. If multiple draw, collect EDTA (lavender-top) tube last. Traumatic tap can introduce thromboplastin and trap WBC and platelets. Refrigeration can precipitate fibrin and trap WBC and platelets. Do not refrigerate. EDTA (lavender-top) tube Room temperature Hemolysis • Clotted • Received frozen Electronic Cell Sizing, Sorting/Cytometry/Microscopy Usual method for determining anemia. Used to calculate indices. Hepatic Function Panel 10256 Includes Total Protein, Albumin, Globulin (calculated), Total Bilirubin, Direct Bilirubin, AST, ALT, LD Alkaline Phosphates, Prothrombin Time (PT-INR) Preferred Specimen(s) 4 mL serum from a red-top tube plus 1 whole blood sodium citrate (light blue-top) tube Transport Container Serum Separator Tube or plastic screw-cap vial; sodium citrate (light blue-top) tube Transport Temperature Ambient 5 days, Refrigerated 2 weeks Reject CriteriaHemolysis Methodology See individual analytes Clinical Significance See Hepatitis in the Infectious Disease section of Test Application and Interpretation. Hepatic Function Panel 2 78570 Includes Total Protein; Albumin, Globulin (calculated); Total Bilirubin; Direct Bilirubin; AST; ALT; Alkaline Phospatase; Gamma Glutamyl Transferase Preferred Specimen(s) 4.0 mL serum from a red-top tube Transport Container Serum Separator Tube or plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 14 days Reject CriteriaHemolysis Methodology See individual analytes Clinical Significance See individual test for clinical significance Hepatitis A Antibody, Total 508 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 5 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Gross lipemia MethodologyImmunoassay Clinical Significance HAV antibody indicates prior or acute infection with, or immunization to, Hepatitis A virus. See Hepatitis in the Infectious Disease section of Test Application and Interpretation Hepatitis A IgM Antibody 512 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 7 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Gross lipemia MethodologyChemiluminescence 51 G H Clinical Significance IgM antibodies to Hepatitis A suggest a current, acute or recent Hepatitis A infection. See Hepatitis in the Infectious Disease section of Test Application and Interpretation Hepatitis B Core Antibody Total 37676 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 7 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Gross lipemia MethodologyChemiluminescence Clinical Significance Hepatitis B core-specific IgM class antibody has been detected in most acute infections and is a reliable marker for acute disease. In some cases, Hepatitis B core IgM antibody may be the only specific marker for the diagnosis of acute infection with Hepatitis B virus. See Hepatitis in the Infectious Disease section of Test Application and Interpretation. Hepatitis B Virus Surface Antigen, CLIA G H Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 37567 2 mL serum Plastic screw cap vial Refrigerated 5 days, -20oC 4 weeks Gross hemolysis, Lipemic Chemiluminescent Competitive Immunoassay HBsAg, derived from the viral envelope, is the first antigen to appear following infection and can be detected serologically as an aid in the laboratory diagnosis of acute HBV infection. Hepatitis Be Antibody 556 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 5 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Lipemia • Plasma MethodologyChemiluminescence Clinical Significance The presence of anti-HBe serves to distinguish these two periods and confirms a seroconversion. The appearance of anti-HBe or the seroconversion from HBeAg positivity to anti-HBe positivity thus indicates a reduced level of infectious virus because virus replication has decreased. Though resolution of the disease generally follows, an HBsAg carrier state may persist. Anti-HBe positivity in this carrier is often associated with chronic asymptomatic infection. During the HBeAg positive stage, therefore, Hepatitis B patients are at increased risk of transmitting the virus to their contacts. Persistence of HBeAg in the Hepatitis B virus carrier is often associated with chronic active hepatitis. See Hepatitis in the Infectious Disease section of Test Application and Interpretation. Hepatitis Be Antigen and Antibodies serum 78558 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 5 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Lipemia • Plasma MethodologyChemiluminescence Clinical Significance Persistence of HBeAg for greater than 6 months is a prognostic indicator of a chronic hepatitis B virus carrier state. The presence of anti-HBe serves to distinguish these two periods and confirms a seroconversion. The appearance of anti-HBe or the seroconversion from HBeAg positivity to anti-HBe positivity thus indicates a reduced level of infectious virus because virus replication has decreased. Though resolution of the disease generally follows, an HBsAg carrier state may persist. Anti-HBe positivity in this carrier is often associated with chronic asymptomatic infection. During the HBeAg positive stage, therefore, Hepatitis B patients are at increased risk of transmitting the virus to their contacts. Persistence of HBeAg in the epatitis B virus carrier is often associated with chronic active hepatitis. See Hepatitis in the Infectious Disease section of Test Application and Interpretation. 52 Hepatitis B Core IgM Antibody 4848 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 5 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Gross lipemia MethodologyChemiluminescence Clinical Significance Hepatitis B core-specific IgM class antibody has been detected in most acute infections and is a reliable marker for acute disease. In some cases, hepatitis B core IgM antibody may be the only specific marker for the diagnosis of acute infection with hepatitis B virus. See Hepatitis in the Infectious Disease section of Test Application and Interpretation Hepatitis B Surface Antibody, Qualitative 499 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 5 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Hyperlipemia MethodologyChemiluminescence Clinical Significance The detection of anti-HBs is indicative of a prior immunologic exposure to the antigen or vaccine. To determine immune status as > 10 uIU/mL as per CDC guidelines, please order Hepatitis B Surface Antibody, Quantitative. See Hepatitis in the Infectious Disease section of Test Application and Interpretation Hepatitis B Surface Antibody, Quantitative 8475 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 5 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Sodium citrate (light blue-top) tubes • Hyperlipemia MethodologyChemiluminescence Clinical Significance This assay is used to determine immune status for Hepatitis B as > 10 uIU/mL as per CDC Guidelines. See Hepatitis in the Infectious Disease section of Test Application and Interpretation. Hepatitis B Viral DNA, Quantitative, PCR Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Hepatitis Be Antigen 8369 2 mL plasma collected in a PPT-Potassium EDTA (white-top) tube. EDTA plasma: Separate plasma within 6 hours of collection, transfer plasma to a sterile, screw-capped plastic aliquot tube. Freeze immediately at -20° C. Ship frozen. Plastic screw-cap vial Refrigerated 7 days, Frozen 35 days Received room temperature • SST® (red-top/glass) • Unspun PPT tube Real-Time Polymerase Chain Reaction (RT-PCR) Chronic carriers will persist in producing detectable HBV. Patients with chronic liver disease of unknown origin most commonly have HBV that is detected by viral DNA testing. Quantitative measurement of HBV viral DNA may be used to monitor progression of disease. See Hepatitis in the Infectious Disease section of Test Application and Interpretation. 555 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 5 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Lipemia • Plasma MethodologyChemiluminescene Clinical Significance Persistence of HBeAg for greater than 6 months is a prognostic indicator of a chronic hepatitis B virus carrier state. See Hepatitis in the Infectious Disease section of Test Application and Interpretation. 53 G H Hepatitis C Antibody 8472 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 7 days, -20oC 4 weeks Reject Criteria Gross hemolysis • Gross lipemia MethodologyChemiluminescence Clinical Significance Hepatitis C Virus (HCV) is the major cause of hepatitis. Approximately 1% of blood donors are seropositive for anti-HCV. The clinical symptoms of a HCV infection are variable. Exposure to HCV results in a chronic infection in 50 to 80% of cases. The “window” between infection and seroreactivity is highly variable, up to 12 months. See Hepatitis in the Infectious Disease section of Test Application and Interpretation. Hepatitis C Virus RNA, Quantitative, Real-Time PCR G H Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 35645 3 mL frozen plasma collected in a PPT EDTA (whitetop) tube or EDTA (lavender-top) tube Separate plasma from cells by centrifugation within 6 hours of sellection and transfer plasma to sepreate plastic screw cap vial. Plastic screw-cap vial Refrigerated 5 days, Frozen 35 days Received refrigerated later than 72 hours from collection • Received room temperature • Received thawed Real-Time Polymerase Chain Reaction (PCR) Useful in monitoring therapy and disease progression.Reportable range is 50 to 50,000,000 IU/mL. See Hepatitis in the Infectious Disease section of Test Application and Interpretation. Hepatitis E Antibody (IgG) 36583 Preferred Specimen(s) 1 mL serum collected in a (red-top) tube (no gel). Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 3 days, -20oC Long term MethodologyELISA Clinical Significance Hepatitis E virus (HEV) is the major etiologic agent of enterically transmiited non-A, non-B hepatitis worldwide and has a high case-fatality rate in pregnant women. Both IgM and IgG antibody to HEV (anti-HEV) are produced following infection. The titer of IgM anti-HEV declines rapidly during early convalescence; IgG anti-HEV persists and appears to provide at least short-term protection against disease. Hepatitis E Antibody (IgM) 36582 Preferred Specimen(s) 0.5 mL serum collected in a red-top tube (no gel). Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 3 days, -20oC Long term MethodologyELISA Clinical Significance Hepatitis E causes an acute, self-limiting infection. Antibody IgG is detected after Antibody IgM is detected, typically 1 month post-infection. Antibody IgM is detected 1-4 weeks post- infection. Hepatitis B Viral DNA, Qualitative, RT-PCR Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 54 78018 2 mL plasma collected in an EDTA (lavender-top) tube Separate plasma from cells by centrifugation within six hours of collection and transfer the plasma to a separate plastic screw-cap vial. Ship frozen. Plastic screw-cap vial Refrigerated 7 days, Frozen 35 days Received room temperature • Received thawed • Serum • Heparinized plasma • Received frozen PPT (white-top) tubes • Unspun PPT tube Real Time Polymerase Chain Reaction (RT-PCR) This test is useful in the monitoring of therapy and disease progression Hepatitis C Virus RNA, Qualitative PCR Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 34024 3 mL frozen plasma collected in a PPT (white-top EDTA) tube or EDTA (lavender-top) tube Separate plasma from cells by centrifugation within six hours of selection and transfer the seprated plasma into screw cap vail plastic screw-cap vial Refrigerated 5 days, Frozen 35 days Received refrigerated later than 72 hours from collection • Received room temperature Real-Time Polymerase Chain Reaction Useful in monitoring therapy and disease progression. Herpes Simplex Virus 1 IgG, Type Specific Antibody 79488 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature 8 hrs, Refrigerated 48 hrs, -20oC Long term Reject Criteria Gross hemolysis • Hyperlipemia MethodologyELISA Clinical Significance Herpes Simplex Virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from inapparent to fatal. Clinical manifestations include genital tract infections, neonatal herpes, meningo-encephalitis, keratoconjunctivitis, and gingivostomatitis. There are two HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, while HSV type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion using the type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. See STI/Genitourinary Infections in Infectious Diseases section of Test Application and Interpretation. Herpes Simplex Virus 2 IgG, Type Specific Antibody 79489 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature 8 hrs, Refrigerated 48 hrs, -20oC Long term Reject Criteria Gross hemolysis • Gross lipemia MethodologyELISA Clinical Significance Herpes simplex virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from inapparent to fatal. Clinical manifestations include genital tract infections, neonatal herpes, meningo-encephalitis, keratoconjunctivitis, and gingivostomatitis. There are two HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, while HSV type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion using the type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. See STI/Genitourinary Infections in Infectious Diseases section of Test Application and Interpretation. Herpes Simplex Virus 1 & 2, IgG 6447 Preferred Specimen(s) 1 mL serum Instructions Specimen may be collected in an SST red top glass tube and transferred to plastic for transport. Do not submit glass tubes. Transport Container No additive (red-top) tube Transport Temperature Room Temperature 8 hrs, Refrigerated 48 hrs, -20oC Long term Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Herpes Simplex Virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from self-limiting to fatal. Clinical manifestations include genital tract infections, neonatal herpes, meningo-encephalitis, keratoconjunctivitis, and 55 G H gingivostomatitis. There are two types of HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, while HSV Type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion using the type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. Herpes Simplex Virus 1 & 2, IgG and IgM G H 10014 Preferred Specimen(s) 1 mL serum Instructions Specimen may be collected in an SST red top glass tube and transferred to plastic for transport. Do not submit glass tubes. Transport Container No additive (red-top) tube Transport Temperature Refrigerated 48 hrs, -20oC Long term Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Herpes Simplex Virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from in apparent to fatal. Clinical manifestations include genital tract infections, neonatal herpes, meningo-encephalitis, keratoconjunctivitis, and gingivostomatitis. There are two types of HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, while HSV Type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion using the type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. Herpes Simplex Virus 1 & 2, IgM 17369 Preferred Specimen(s) 1 mL serum Instructions Separate serum from cells as soon as possible Transport Container No additive (red-top) tube Transport Temperature Refrigerated 4 days, -20oC Long term Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Herpes Simplex Virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from inapparent to fatal. Clinical manifestations include genital tract infections, neonatal herpes, meningo-encephalitis, keratoconjunctivitis, and gingivostomatitis. There are two types of HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, while HSV Type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion using the type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. Herpes Simplex Virus 1, IgG and IgM 78547 Preferred Specimen(s) 1 mL serum Instructions Specimen may be collected in an SST red top glass tube and transferred to plastic for transport. Do not submit glass tubes. Transport Container No additive (red-top) tube Transport Temperature Refrigerated 48 hrs, -20oC Long term Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Herpes Simplex Virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from in apparent to fatal. Clinical manifestations include genital tract infections, neonatal herpes, meningoencephalitis, keratoconjunctivitis, and gingivostomatitis. There are two types of HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, 56 while HSV Type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion sing the type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. Herpes Simplex Virus 1, IgM 79490 Preferred Specimen(s) 1 mL serum Instructions Separate serum from cells as soon as possible Transport Container No additive (red-top) tube Transport Temperature Refrigerated 4 days, -20oC Long term Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Herpes Simplex Virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from in apparent to fatal. Clinical manifestations include genital tract infections, neonatal herpes, meningo-encephalitis, keratoconjunctivitis, and gingivostomatitis. There are two types of HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, while HSV Type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion using the type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. Herpes Simplex Virus 2, IgG and IgM 78548 Preferred Specimen(s) 1 mL serum Instructions Specimen may be collected in an SST red top glass tube and transferred to plastic for transport. Do not submit glass tubes. Transport Container No additive (red-top) tube Transport Temperature Refrigerated 48 hrs, -20oC Long term Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Herpes Simplex Virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from in apparent to fatal. Clinical manifestations include genital tract infections, neonatal herpes, meningo-encephalitis, keratoconjunctivitis, and gingivostomatitis. There are two types of HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, while HSV Type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion using the type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. Herpes Simplex Virus 2, IgM 79491 Preferred Specimen(s) 1 mL serum Instructions Separate serum from cells as soon as possible Transport Container No additive (red-top) tube Transport Temperature Refrigerated 4 days, -20oC Long term Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Herpes Simplex Virus (HSV) is responsible for several clinically significant human viral diseases, with severity ranging from inapparent to fatal. Clinical manifestations include genital tract infections, neonatal herpes,meningo-encephalitis, keratoconjunctivitis, and gingivostomatitis. There are two types of HSV serotypes that are closely related antigenically. HSV type 2 is more commonly associated with genital tract and neonatal infections, while HSV Type 1 is more commonly associated with infections of non-genital sites. Specific typing is not usually required for diagnosis or treatment. The mean time to seroconversion using the 57 G H type specific assay is 25 days. The performance of this assay has not been established for use in a pediatric population, for neonatal screening, or for testing of immunocompromised patients. Highly Sensitive CRP See “Cardio CRP™” HIV Prognosticator Panel HIV Quantitative, CD3, CD4, and CD8 Absolute and Percentage counts 78540 G H Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 2 mL whole blood plasma collected in an EDTA (lavender-top) tube in two tubes For follow up patients of CD4/CD8 counts collect sample at the same time of the day Separate plasma from cells by centrifugation within two hours of collection and transfer the plasma to a separate plastic screw-cap vial. Ship frozen. For flow cytometry samples have to be sent at room temperature at 20- 25°C Plastic screw-cap vial EDTA tube for flow samples Frozen for Viral load Room temperature for flow Received room temperature • Received thawed • Serum • Heparinized plasma • Received frozen PPT (white-top) tubes • Unspun PPT tube Reverse Transcriptase Polymerase Chain Reaction (RTPCR) Flow cytometry This test is useful in the monitoring of therapy and disease progression HIV-1 and 2 Antibody 19923 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 5 days, -20oC 4 weeks MethodologyChemiluminescene Clinical Significance The combination of HIV -1/HIV -2 includes detecion of subtype HIV -1. HIV -2 is closely releted to HIV - 1 regarding nucleic acid sequence and clinical disease. HIV-1 Antibody Confirmation by Western Blot Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance This test should be ordered only as a confirmation for a previously positive HIV EIA screening test 1 mL serum Tube must be labeled with patient identifier Plastic screw-cap vial or original collection tube with the patient’s name or ID number Refrigerated 3 days, -20oC Long term Specimens that are not properly labeled with patient identifier • Gross hemolysis • Hyperlipemia Western Blot The etiological agent of acquired immunodeficiency syndrome (AIDS) has been recognized as a retrovirus, human immunodeficiency virus (HIV-1). The virus is believed to be transmitted by sexual contact, blood transfusion, feto-maternal transmission, breast feeding and intravenous drug abuse. The presence of circulating antibodies to the virus indicates prior exposure of the individual to viral antigen(s). The presence of antibody to HIV is not in itself diagnostic of AIDS. Likewise, a non-reactive test result does not exclude the possibility of exposure to or infection with HIV. Specimens that screen positive and are repeatedly reactive are confirmed by Western Blot. See the HIV section in the Infectious Disease section of Test Application and Interpretation. HIV-1 RNA, Quantitative, PCR, Expanded Range Preferred Specimen(s) Instructions Transport Container Transport Temperature 58 79003 14484 2 mL plasma collected in a (lavender-top) EDTA tube Separate plasma from the cells by centrifugation within six hours of collection, and transfer the plasma to a separate plastic screw-cap vial. Ship frozen. Plastic screw-cap vial Refrigerated 5 days, Frozen 35 days Reject Criteria Methodology Clinical Significance Received thawed • Serum • Heparinized plasma • Frozen PPT (white-top) tubes Polymerase Chain Reaction (PCR) Useful in the monitoring therapy and disease progression. The reportable range is 20 to 221*107 copies/mL. See HIV-1 RNA, Quantitative in the Infectious Disease section of Test Application and Interpretation. HIV-1 RNA, Qualitative, RT-PCR 37815 Preferred Specimen(s) 2 mL plasma collected in an EDTA (lavender-top) tube or PPT (white-top) tubes. Instructions Separate plasma from cells by centrifugation within six hours of collection and transfer the plasma to a separate plastic screw-cap vial. Ship frozen. Do not freeze PPT tubes. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Received thawed • Serum • Heparinized plasma • Received frozen PPT (white-top) tubes • Unspun PPT tube Methodology Real time Polymerase Chain Reaction (RT-PCR) Clinical Significance Useful in the monitoring therapy and disease progreffion. HLA B27 DNA Typing PCR Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 15584 3.0 mL Whole Blood in EDTA vial. Collection Vial Refrigerated 7 days, 20-26oC 7 days Received Frozen Polymerase Chain Reaction HLA-B-27 positive individuals have a higher possibility of developing ankylosing spondylitis as opposed to HLAB27 negative individuals. Homocysteine, Cardiovascular 31789 Patient Preparation Fasting for at least 8 hours is preferred Preferred Specimen(s) 1 mL serum or EDTA plasma Instructions EDTA plasma: Place the specimen in the refrigrator or ice bath until the specimen can be centrifuged. Centrifuge the specimen as soon as possible and seperate the plasma to plastic screw cap vial Red-top tube: Place the specimen in the refrigerator or ice bath for 30 minutes after collection. Centrifuge the specimen as soon as possible after complete clot formation. Transfer the serum to a plastic specimen transport tube. Mark the specimen type as serum on the transport tube. Barrier gel separator tube: Place the specimen in arefrigerator for 30 minutes after collection. Do not place barrier tubes in an ice bath as freezing may prevent the barrier gel from adequately separating from cells. Centrifuge specimen as soon as possible after complete clot formation, ensuring that the barrier gel completely separates serum from cells. Note: It is very important to centrifuge and separate serum or plasma from red blood cells as soon as possible to avoid falsely elevated results. Transport Container Plastic screw-cap vial Transport Temperature Frozen 3 months, Refrigerated 14 days Reject Criteria Gross hemolysis • Unseparated serum or plasma • Whole blood specimens MethodologyChemiluminescence Clinical Significance Elevated levels of homocysteine are observed in patients at risk for coronary heart disease and stroke. See Non-Lipid Markers in the Cardiovascular Disease section and Biochemical Markers in the Genetics section of Test Application and Interpretation. Homocysteine, Nutritional and Congenital Patient Preparation Preferred Specimen(s) Instructions 36362 Fasting for at least 8 hours is preferred 1 mL serum or EDTA plasma EDTA plasma: Place the specimen in the refrigrator or ice bath until the specimen can be centrifuged. Centrifuge the specimen as soon as possible and seperate the plasma to plastic screw cap vial 59 G H Red-top tube: Place the specimen in the refrigerator or ice bath for 30 minutes after collection. Centrifuge the specimen as soon as possible after complete clot formation. Transfer the serum to a plastic specimen transport tube. Mark the specimen type as serum on the transport tube. Barrier gel separator tube: Place the specimen in a refrigerator for 30 minutes after collection. Do not place barrier tubes in an ice bath as freezing may prevent the barrier gel from adequately separating serum from cells. Centrifuge specimen as soon as possible after complete clot formation, ensuring that the barrier gel completely separates serum from cells. Note: It is very important to centrifuge and separate serum or plasma from red blood cells as soon as possible to avoid falsely elevated results Transport Container Plastic screw-cap vial Transport Temperature Frozen 3 months, Refrigerated 14 days Reject Criteria Gross hemolysis • Unseparated serum or plasma • Whole blood specimens MethodologyChemiluminescence Clinical Significance Diagnose and monitor treatment of homocystinuria, folate deficiency, or vitamin B12 deficiency. See Homocysteine in the Genetics section of Test Application and Interpretation. G H HPV DNA, High Risk (cervista) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10ml servical specimen collected with appropriate collection device. Collect the sample as usual according to manufacturer instruction. Thin prep vial Room Temperature 3 months, Refrigerated 3 months Specimens other than ThinPrep. For example sample colleted in Qiagen Specimen Transport or SurePath cell pellet fraction specimens. Third Wave Technologies Invader(R) signal amplification HPV is the causative agent of cervical dysplasia and cervical carcinoma. See Cervical Cancer in the Hematology/Oncology section of Interpretive Information HPV Genotypes 16 & 18 (Cervista) Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance hs-CRP See “Cardio CRP™” 60 79557 79558 10 mL Cervical specimens collected with an appropriate collection device and placed in Cytyc PreservCyt Solution, (ThinPrep Vial). Collect the sample as usual according to the manufacturers instructions. ThinPrep Vial Room Temperature 3 months, Refrigerated 3 months Specimens other than ThinPrep. For example sample colleted in Qiagen Specimen Transport or SurePath cell pellet fraction specimens Third Wave Technologies Invader(R) signal amplification Persistent infection with any of the 14 high-risk HPV types increases a woman’s risk for progression to dysplasia or cervical cancer. The rate of progression or degree of risk depends on the HPV type. Of all 14 highrisk types, HPV Types 16 and 18 cause more than 60-65% od cervical cancers. This test will identify the presence or absence of HPV Type 16 DNA and /or Type 18 DNA in PreservCyt ThinPrep. Knowledge of the HPV genotype will help physicians diagnose the type of HPV infection and its risk of delevoping into dysplasia or cervical cancer. IBD Panel See “Inflammatory Bowel Disease Differential Panel” IF-Blocking Antibody See “Intrinsic Factor Blocking Antibody” IFE, Serum See “Immunofixation (IFE), Serum” IGF BINDING PROTEIN-1 36590 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport TemperatureRefrigerated Reject Criteria Gross hemolysis • Hyperlipemia • Serum received room temperature MethodologyRadioimmunoassay Clinical Significance IGF-I (somatomedin-C) measurements are useful in the evaluation of growth deficiencies and acromegaly IHC-AE1/AE3 With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Lines the normal and neoplastic epithelium of simple and complex epithelia. It is crucial in diagnostic IHC for identification of carcinomatous differentiation. IHC-AE1/AE3 Without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78701 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Lines the normal and neoplastic epithelium of simple and complex epithelia. It is crucial in diagnostic IHC for identification of carcinomatous differentiation. IHC-AFP With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78700 78821 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) 61 I J Clinical Significance Major plasma protein of early fetus; synthesized by the cells of the embryonic yolk sac, fetal gut and liver. AFP expression demonstrated in many hepatocellular carcinomas, and in extragonadal and gonadal germ cell tumors, including yolk sac tumors. IHC-AFP Without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Major plasma protein of early fetus; synthesized by the cells of the embryonic yolk sac, fetal gut and liver. AFP expression demonstrated in many hepatocellular carcinomas, and in extragonadal and gonadal germ cell tumors, including yolk sac tumors. IHC-ANNEXIN A1 with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 62 78774 10 % neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A member of the annexin family of calcium binding proteins, and has roles in many diverse cellular functions, such as membrane aggregation, inflammation, phagocytosis, proliferation, apoptosis, and tumorigenesis and cancer development.Strongly expressed in 97% of patients with hairy cell leukemia and can be used to differentiate this disease from other B-cell lymphomas; esophageal and esophagogastric junction adenocarcinomas IHC-BCL2 With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78773 10 % neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10 % neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A member of the annexin family of calcium binding proteins, and has roles in many diverse cellular functions, such as membrane aggregation, inflammation, phagocytosis, proliferation, apoptosis, and tumorigenesis and cancer development.Strongly expressed in 97% of patients with hairy cell leukemia and can be used to differentiate this disease from other B-cell lymphomas; esophageal and esophagogastric junction adenocarcinomas IHC-ANNEXIN A1 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78812 78759 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Clinical Significance Bcl2 is a proto-oncogene ; maintains memory B cells, plasma cells and neurons by prolonging life span without cell division. Used to distinguish follicular hyperplasia of lymph node (germinal centers are bcl2 negative) and follicular lymphoma (germinal centers are bcl2 positive), but also positive in other lymphomas. IHC-BCL2 Without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Bcl2 is a proto-oncogene ; maintains memory B cells, plasma cells and neurons by prolonging life span without cell division. Used to distinguish follicular hyperplasia of lymph node (germinal centers are bcl2 negative) and follicular lymphoma (germinal centers are bcl2 positive), but also positive in other lymphomas. IHC-BCL6 With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78762 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Transcription factor involved in cell proliferation and differentiation; selectively expressed by germinal center cells. Positive staining (disease): 30-80% of large cell lymphomas, 6-10% of follicular lymphomas. IHC-BER-EP4 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78761 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Transcription factor involved in cell proliferation and differentiation; selectively expressed by germinal center cells. Positive staining (disease): 30-80% of large cell lymphomas, 6-10% of follicular lymphomas. IHC-BCL6 Without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78760 78789 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Antibody to cell membrane glycoproteins; does not react with cytokeratin.100% sensitive, 91% specific marker for lung adenocarcinoma vs. mesothelioma differentiation; also useful in diagnosing mammary Paget’s disease. 63 I J IHC-BER-EP4 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Antibody to cell membrane glycoproteins; does not react with cytokeratin.100% sensitive, 91% specific marker for lung adenocarcinoma vs. mesothelioma differentiation; also useful in diagnosing mammary Paget’s disease. IHC-BRCA1 with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78842 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A tumor suppressor gene which confers susceptibility to breast and ovarian cancer. BRCA1 or BRCA2 mutation is associated with medullary carcinoma of breast (more favorable prognosis), adenocarcinomas of colon, ovary and prostate.BRCA1 or BRCA2 mutation is associated with medullary carcinoma of breast (more favorable prognosis),adenocarcinomas of colon, ovary and prostate. IHC-BRCA2 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 64 78841 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A tumor suppressor gene which confers susceptibility to breast and ovarian cancer. BRCA1 or BRCA2 mutation is associated with medullary carcinoma of breast (more favorable prognosis),adenocarcinomas of colon, ovary and prostate.BRCA1 or BRCA2 mutation is associated with medullary carcinoma of breast (more favorable prognosis),adenocarcinomas of colon, ovary and prostate. IHC-BRCA1 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78790 78798 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A tumor suppressor gene and is a sensitive marker for breast and ovarian cancers in women. BRCA1 or BRCA2 mutation is associated with medullary carcinoma of breast (more favorable rognosis), adenocarcinomas of colon, ovary and prostate; men with BRCA2 mutation also have higher risk of breast cancer. IHC-BRCA2 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78799 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A tumor suppressor gene and is a sensitive marker for breast and ovarian cancers in women. BRCA1 or BRCA2 mutation is associated with medullary carcinoma of breast (more favorable prognosis), adenocarcinomas of colon, ovary and prostate; men with BRCA2 mutation also have higher risk of breast cancer. IHC-34 Beta E12 With Interpretation 78736 Preferred Specimen(s) 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Instructions Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received frozen, broken slides, Insufficient tumor containing block Methodology Immunohistochemical Assay (IHC) Clinical Significance The antibody labels squamous, ductal and complex epithelia and virtually all of the normal basal cells of prostate.Helps to establish a benign or malignant diagnosis of prostatic adenocarcinoma. IHC-34 Beta E12 Without Interpretation 78737 Preferred Specimen(s) 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Instructions Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received frozen, broken slides, Insufficient tumor containing block Methodology Immunohistochemical Assay (IHC) Clinical Significance The antibody labels squamous, ductal and complex epithelia and virtually all of the normal basal cells of prostate.Helps to establish a benign or malignant diagnosis of prostatic adenocarcinoma. IHC-CA19.9 With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Majority of tumors of gastrointestinal tract and pancreas express CA19.9 IHC-CA19.9 Without Interpretation Preferred Specimen(s) Instructions Transport Container 78830 78831 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder 65 I J Transport Temperature Reject Criteria Methodology Clinical Significance Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Majority of tumors of gastrointestinal tract and pancreas express CA19.9 IHC-CA125 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance I J 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Recognizes a mucin like glycoprotein, expressesing the CA 125 epitope.This antibody labels a variety of tumors such as some adenocarcinomas of the colon, breast carcinomas, uterine adenomatoid tumor, bronchoalveolar carcinoma and ovarian endometroid and serous carcinomas. Antibodies to CA 125 may be useful for the differential diagnosis of adenocarcinomas, as positive reactivity in prostate, colorectal and renal carcinomas is rare. IHC-CA125 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 66 78708 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) convoluted tubules, eccrine glands and thymic keratinized cells. Typically used as a marker for neural, mesothelial, ovarian sex- cord stromal and adrenal cortical tumors; suggested in differentiation of epithelial malignant mesotheliomas from lung adenocarcinomas. IHC-Calretinin Without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature 78875 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Recognizes a mucin like glycoprotein, expressesing the CA 125 epitope.This antibody labels a variety of tumors such as some adenocarcinomas of the colon, breast carcinomas, uterine adenomatoid tumor, bronchoalveolar carcinoma and ovarian endometroid and serous carcinomas. Antibodies to CA 125 may be useful for the differential diagnosis of adenocarcinomas, as positive reactivity in prostate, colorectal and renal carcinomas is rare. IHC-Calretinin With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78874 78709 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Reject Criteria Methodology Clinical Significance Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Expressed in central and peripheral neural tissues particularly in retina and neurons of sensory pathways, normal and neoplastic mesothelial cells, steroid producing cells, renal convoluted tubules, eccrine glands and thymic keratinized cells. Typically used as a marker for neural, mesothelial, ovarian sex- cord stromal and adrenal cortical tumors; suggested in differentiation of epithelial malignant mesotheliomas from lung adenocarcinomas. IHC-CD2 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A transmembrane glycoprotein that is considered a pan T cell antigen expressed on a majority of thymocytes and virtually all peripheral T lymphocytes. Useful for identification of peripheral T- cell lymphoma, anaplastic large cell lymphoma and precursor T-cell lymphoma. IHC-CD2 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78702 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Binds with T cell antigen receptor in the cell membrane and is specific for T cells. Expressed by peripheral T cells, thymocytes and activated natural killer cells and is present in great majotity of T cell lymphomas IHC-CD3 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78846 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A transmembrane glycoprotein that is considered a pan T cell antigen expressed on a majority of thymocytes and virtually all peripheral T lymphocytes. Useful for identification of peripheral T- cell lymphoma, anaplastic large cell lymphoma and precursor T-cell lymphoma. IHC-CD3 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78845 78703 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines. IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) 67 I J Clinical Significance Binds with T cell antigen receptor in the cell membrane and is specific for T cells. Expressed by peripheral T cells, thymocytes and activated natural killer cells and is present in great majotity of T cell lymphomas IHC-CD4 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Nonpolymorphous transmembrane glycoproteins belonging to immunoglobulin superfamily expressed on majority of mature peripheral T cells. Useful for identification of anaplastic large cell lymphoma and unspecified peripheral T- cell lymphoma. IHC-CD4 without Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 68 78748 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) CD5+ B cells, which may arise from B-1 cells (subset of B cells) produce generalist antibodies; the first line of defense against antigens.Used as a marker for CLL, mantle cell lymphoma, T cells (normal and malignant) and thymic carcinoma. IHC-CD 5 Without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78840 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Nonpolymorphous transmembrane glycoproteins belonging to immunoglobulin superfamily expressed on majority of mature peripheral T cells. Useful for identification of anaplastic large cell lymphoma and unspecified peripheral T- cell lymphoma. IHC-CD 5 With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78839 78749 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) CD5+ B cells, which may arise from B-1 cells (subset of B cells) produce generalist antibodies; the first line of defense against antigens.Used as a marker for CLL, mantle cell lymphoma, T cells (normal and malignant) and thymic carcinoma. IHC-CD7 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Expressed by the majority of peripheral blood T cells, NK cells, and all thymocytes. It is one of the earliest surface antigens on T and NK-cell lineages, and the antibody is useful for the classification of T-cell malignancies. IHC-CD7 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78814 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A transmembrane glycoprotein expressed by majority of thymocytes, and by class I major histocompatibility complex restricted, mature, suppressor/cytotoxic T cells. Useful for identification of cytotoxic/suppressor T cells and their neoplastic counteparts. IHC-CD10 with interpretation Preferred Specimen(s) Instructions Transport Container 78813 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A transmembrane glycoprotein expressed by majority of thymocytes, and by class I major histocompatibility complex restricted, mature, suppressor/cytotoxic T cells. Useful for identification of cytotoxic/suppressor T cells and their neoplastic counteparts. IHC-CD8 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78766 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Expressed by the majority of peripheral blood T cells, NK cells, and all thymocytes. It is one of the earliest surface antigens on T and NK-cell lineages, and the antibody is useful for the classification of T-cell malignancies. IHC-CD8 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78765 78742 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder 69 I J Transport Temperature Reject Criteria Methodology Clinical Significance Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Characteristic marker of follicular center cells and follicular lymphoma.Marker for germinal center phenotype and used to identify Acute lymphoblastic leukemia (ALL), Angioimmunoblastic T cell lymphoma and Burkitt’s lymphoma. IHC-CD10 without interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance I J 78743 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Characteristic marker of follicular center cells and follicular lymphoma.Marker for germinal center phenotype and used to identify Acute lymphoblastic leukemia (ALL), Angioimmunoblastic T cell lymphoma and Burkitt’s lymphoma. IHC-CD15 With Interpretation 78847 Preferred Specimen(s) 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Instructions Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received frozen, broken slides, Insufficient tumor containing block Methodology Immunohistochemical Assay (IHC) Clinical Significance A carbohydrate adhesion molecule (not a protein) that mediates phagocytosis and chemotaxis. Used as a confirmatory marker for diagnosis of Hodgkin’s lymphoma, helps differentiate between Hodgkin’s lymphoma and anaplastic large cell lymphoma, adenocarcinoma and mesothelioma. IHC-CD15 without Interpretation 78848 Preferred Specimen(s) 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Instructions Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received frozen, broken slides, Insufficient tumor containing block Methodology Immunohistochemical Assay (IHC) Clinical Significance A carbohydrate adhesion molecule (not a protein) that mediates phagocytosis and chemotaxis. Used as a confirmatory marker for diagnosis of Hodgkin’s lymphoma, helps differentiate between Hodgkin’s lymphoma and anaplastic large cell lymphoma, adenocarcinoma and mesothelioma. IHC-CD20 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria 70 78726 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Methodology Clinical Significance Immunohistochemical Assay (IHC) Acquired late in the pre-B-cell stage of maturation, and remains on cells throughout most of their differentiation. Positive in B cell Lymphoblastic Leukemia/Lymphoma and all mature B cell Lymphomas (except plasma cell lesions) and Reed-Sternberg cells in 25% cases of classical Hodgkin’s disease IHC-CD20 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Acquired late in the pre-B-cell stage of maturation, and remains on cells throughout most of their differentiation. Positive in B cell Lymphoblastic Leukemia/Lymphoma and all mature B cell Lymphomas (except plasma cell lesions) and Reed-Sternberg cells in 25% cases of classical Hodgkin’s disease IHC-CD21 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78768 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) CD21 is expressed by follicular dendritic cells, mature B cells as well as several types of epithelial cells. Used to diagnose follicular dendritic cell sarcomas, distinguishes cutaneous or nodal mantle cell lymphoma from follicular lymphoma. IHC-CD23 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78767 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) CD21 is expressed by follicular dendritic cells, mature B cells as well as several types of epithelial cells. Used to diagnose follicular dendritic cell sarcomas, distinguishes cutaneous or nodal mantle cell lymphoma from follicular lymphoma. IHC-CD21 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78729 78817 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) 71 I J Clinical Significance A dendritic cell marker and acts as a B cell growth and activation factor.Strongly expressed on B cells and monocytes, including a strong expression on Epstein Barr virus transformed B lymphoblasts. A B cell marker particularly for SLL/CLL, mediastinal large B cell lymphoma and lymphoplasmacytic lymphoma and may be used to differentiate B-CLL (B - cell chronic lymphocytic Leukemia /Lymphoma) from mantle cell lymphoma or MALT lymphoma. IHC-CD23 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance I J 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry &Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A dendritic cell marker and acts as a B cell growth and activation factor.Strongly expressed on B cells and monocytes, including a strong expression on Epstein Barr virus transformed B lymphoblasts. A B cell marker particularly for SLL/CLL, mediastinal large B cell lymphoma and lymphoplasmacytic lymphoma and may be used to differentiate B-CLL (B - cell chronic lymphocytic Leukemia /Lymphoma) from mantle cell lymphoma or MALT lymphoma. IHC-CD 30 With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 72 78780 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Member of tumor necrosis factor family of cell surface receptors; also a lymphocyte activation antigen.Confirms diagnosis of Anaplastic large cell lymphoma, Classic Hodgkin’s lymphoma, Embryonal carcinoma; other lymphoma diagnosis. IHC-CD31 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78758 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Member of tumor necrosis factor family of cell surface receptors; also a lymphocyte activation antigen.Confirms diagnosis of Anaplastic large cell lymphoma, Classic Hodgkin’s lymphoma, Embryonal carcinoma; other lymphoma diagnosis. IHC-CD 30 Without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78818 78793 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Clinical Significance This marker strongly labels endothelial cells and confirms vascular origin of tumors and highlights vessels arising from endothelial cells. CD31 is the most sensitive and specific endothelial marker in paraffin sections; stains small and large vessels. IHC-CD31 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) This marker strongly labels endothelial cells and confirms vascular origin of tumors and highlights vessels arising from endothelial cells. CD31 is the most sensitive and specific endothelial marker in paraffin sections; stains small and large vessels. IHC-CD34 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78770 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Intercellular adhesion protein and cell surface glycoprotein; expressed in immature haemotopoeitic stem cells, capillary endothelial cells, embryonic fibroblasts and rare glial cells in nervous tissue. Useful marker for diagnosis of pre B ALL, alveolar soft part sarcoma, AML, angiosarcoma. IHC-CD43 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78769 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Intercellular adhesion protein and cell surface glycoprotein; expressed in immature haemotopoeitic stem cells, capillary endothelial cells, embryonic fibroblasts and rare glial cells in nervous tissue. Useful marker for diagnosis of pre B ALL , alveolar soft part sarcoma, AML, angiosarcoma. IHC-CD34 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78794 78785 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) An integeral membrane protein typically expressed at high levels on all leukocytes, except most resting B lymphocytes.Also useful in diagnosing AML, granulocytic sarcoma, hemangioma, Langerhans cell histiocytosis, mast cell disease, plasmacytoma and early colonic adenoma. 73 I J IHC-CD43 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) An integeral membrane protein typically expressed at high levels on all leukocytes , except most resting B lymphocytes.Also useful in diagnosing AML, granulocytic sarcoma, hemangioma, Langerhans cell histiocytosis, mast cell disease, plasmacytoma and early colonic adenoma. IHC-CD 45 With Interpretation I J 78786 78746 Preferred Specimen(s) 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Instructions Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received frozen, broken slides, Insufficient tumor containing block Methodology Immunohistochemical Assay (IHC) Clinical Significance CD 45 is membrane tyrosine protein phosphatase found on all leukocytes.An essential regulator of T and B cell antigen receptor-mediated activation; also required for thymic selection. IHC-CD 45 Without Interpretation 78747 Preferred Specimen(s) 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Instructions Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received frozen, broken slides, Insufficient tumor containing block Methodology Immunohistochemical Assay (IHC) Clinical Significance CD 45 is membrane tyrosine protein phosphatase found on all leukocytes.An essential regulator of T and B cell antigen receptor-mediated activation; also required for thymic selection. IHC-CD56 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Also called N-CAM (neural cell adhesion molecule), it contributes to cell-cell or cell-matrix adhesion during development.Used as a marker for NK cells and NK lymphomas, neuroblastomas and small lung cell carcinomas. Useful for labelling atypical plasma cells. IHC-CD56 without Interpretation Preferred Specimen(s) Instructions Transport Container 74 78783 78784 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Transport Temperature Reject Criteria Methodology Clinical Significance Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Also called N-CAM (neural cell adhesion molecule), it contributes to cell-cell or cell-matrix adhesion during development.Used as a marker for NK cells and NK lymphomas, neuroblastomas and small lung cell carcinomas. IHC-CD61 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Detects platelets in smears of blood and bone marrow and megakaryocytes in cell smears. Valuable in diagnosis of megakaryoblastic leukemia and can also reveal absence of GpIIb/ IIIa in Glanzmann thrombasthenia. IHC-CD61 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78797 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Lines human monocytes, macrophages and myeloid cells.Useful marker of histiocytes and histiocytic tumors and also useful in diagnosis of AML-M4/M5, angiosarcoma, atypical fibroxanthoma, B cell lymphoma (some), blastic NK lymphoma, calcifying aponeurotic fibroma, and cellular fibrous histiocytoma. IHC-CD 68 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78858 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Detects platelets in smears of blood and bone marrow and megakaryocytes in cell smears. Valuable in diagnosis of megakaryoblastic leukemia and can also reveal absence of GpIIb/IIIa in Glanzmann thrombasthenia. IHC-CD68 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78857 78832 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) 75 I J Clinical Significance Lines human monocytes, macrophages and myeloid cells.Useful marker of histiocytes and histiocytic tumors and also useful in diagnosis of AML-M4/M5, angiosarcoma, atypical fibroxanthoma, B cell lymphoma (some), blastic NK lymphoma, calcifying aponeurotic fibroma, and cellular fibrous histiocytoma. IHC-CD79a with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) CD79a markers are expressed on specific B-cell type lymphoid cells. Individual and a series of IHC markers can be run on unknown cells and presence or absence of the antigen can help to characterize the cell of interest. IHC-CD79a without Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78836 78833 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Expressed early in B-cell differentiation ; also expressed in plasma cells.Useful marker for general detection of B cells; also used in ALL or small B cell lymphoproliferative disorders when CD20 may be negative or after rituximab (anti CD-20) therapy , in infarcted lymphomas and to differentiate pre B lymphoblastic lymphoma from Ewing’s sarcoma. IHC-CD99 with Interpretation 78781 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen Methodology Immunohistochemical Assay (IHC) Clinical Significance Expressed on cell membrane of some lymphocytes, cortical thymocytes, granulosa cells of ovary, CNS ependymal cells and and Sertoli’s cells of testis.Relatively non-specific marker for Ewing’s sarcoma and T cell lymphoma, but does distinguish Ewing’s sarcoma from neuroblastoma; also distinguishes meningeal hemangiopericytoma from anaplastic meningiomas. IHC-CD99 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 76 78782 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Clinical Significance Expressed on cell membrane of some lymphocytes, cortical thymocytes, granulosa cells of ovary, CNS ependymal cells and and Sertoli’s cells of testis.Relatively non-specific marker for Ewing’s sarcoma and T cell lymphoma, but does distinguish Ewing’s sarcoma from neuroblastoma; also distinguishes meningeal hemangiopericytoma from anaplastic meningiomas. IHC-CDX 2 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Widely expressed in intestinal epithelium from the duodenum to the rectum. Positive in colorectal adenocarcinomas, primary and metastatic gastric adenocarcinomas and carcinoids as well as adenocarcinomas of the ovary, urinary bladder and pancreas. IHC-CDX 2 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78750 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Useful for identification of malignancies involving terminally differentiated plasma cells, and is associated with multiple myeloma. It might also be useful for the subclassification of difuse large B-cell lymphomas. IHC-CD138 without interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78728 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Widely expressed in intestinal epithelium from the duodenum to the rectum. Positive in colorectal adenocarcinomas, primary and metastatic gastric adenocarcinomas and carcinoids as well as adenocarcinomas of the ovary, urinary bladder and pancreas. IHC-CD 138 With Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78727 78751 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Useful for identification of malignancies involving terminally differentiated plasma cells, and is associated with multiple myeloma. It might also be useful for the subclassification of difuse large B-cell lymphomas. 77 I J IHC-Chromogranin A with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A momomeric protein that composes the major portion of the neurosecretory granules of neuroendocrine cells (normal as well as neoplastic). Positive in tumors of neuroendocrine origin (Pheochromocytoma, carotid body tumor, medullary thyroid carcinoma, carcinoid). IHC-Chromogranin A without Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78 78803 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) It labels mesothelioma and epithelial based cells in prostate and tonsil.Expressed at low levels in adenocarcinoma whereas present at high levels in epithelioid mesotheliomas and therefore used in differentiation between these types of cancers. IHC-CK7 with Interpretation Preferred Specimen(s) Instructions Transport Container 78802 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) It labels mesothelioma and epithelial based cells in prostate and tonsil.Expressed at low levels in adenocarcinoma whereas present at high levels in epithelioid mesotheliomas and therefore used in differentiation between these types of cancers. IHC-CK5/6 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78731 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A momomeric protein that composes the major portion of the neurosecretory granules of neuroendocrine cells (normal as well as neoplastic). Positive in tumors of neuroendocrine origin (Pheochromocytoma, carotid body tumor, medullary thyroid carcinoma, carcinoid). IHC-CK5/6 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78730 78706 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen Methodology Immunohistochemical Assay (IHC) Clinical Significance Lines the normal and neoplastic epithelia including many ductal and glandular epithelia. Diagnostic utility in carcinomas of ovary, salivary gland, lung, breast, endometrium and bladder IHC-CK7 without Interpretation 78707 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen Methodology Immunohistochemical Assay (IHC) Clinical Significance Lines the normal and neoplastic epithelia including many ductal and glandular epithelia. Diagnostic utility in carcinomas of ovary, salivary gland, lung, breast, endometrium and bladder IHC-CK8 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78808 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A low molecular weight keratin ; a component of nuclear inclusions of rhabdoid tumors and Mallory bodies; labels almost all non squamous epithelia. Useful marker to confirm epithelial nature of tissue/tumors, assess sentinel lymph nodes in colon carcinoma, and diagnose adenocarcinomas of ovary, gastrointestinal tract and thyroid and majority of ductal carcinoma. IHC-CK8 without Interpretation 78809 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen Methodology Immunohistochemical Assay (IHC) Clinical Significance A low molecular weight keratin ; a component of nuclear inclusions of rhabdoid tumors and Mallory bodies; labels almost all non squamous epithelia. Useful marker to confirm epithelial nature of tissue/tumors, assess sentinel lymph nodes in colon carcinoma, and diagnose adenocarcinomas of ovary, gastrointestinal tract and thyroid and majority of ductal carcinoma. IHC-CK18(LMW) with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78868 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) The antibody labels tumor cells of epithelial origin including many ductal and glandular epithelia. A useful tumor marker for breast cancer and bladder carcinoma. 79 I J IHC-CK18(LMW) without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) The antibody labels tumor cells of epithelial origin including many ductal and glandular epithelia. A useful tumor marker for breast cancer and bladder carcinoma. IHC-CK20 with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 80 78815 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A proto-oncogene; acts as a receptor for kit protein, important for development and survival of mast cells, hematopoietic stem cells, melanocytes, germ cells, interstitial cells of Cajal. Useful marker for confirming diagnosis of GIST (gastrointestinal stromal tumors), AML, angiomyolipoma , angiosarcomas (50%), clear cell sarcoma, CML, epithelioid sarcoma, Ewing sarcoma, granulocytic sarcoma, Hodgkin’s lymphoma (some Reed-Sternberg cells). IHC-CKIT (CD117) without Interpretation Preferred Specimen(s) Instructions 78705 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Lines gastrointestinal epithelium and is useful in identification of GIT adenocarcinomas (colorectal, pancreatic, gall bladder). Also lines mucinous ovarian tumors, transitional cell and Merkel-cell carcinomas hence used in their diagnosis IHC-CKIT (CD117) with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78704 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Lines gastrointestinal epithelium and is useful in identification of GIT adenocarcinomas (colorectal, pancreatic, gall bladder). Also lines mucinous ovarian tumors, transitional cell and Merkel-cell carcinomas hence used in their diagnosis IHC-CK20 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78869 78816 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A proto-oncogene; acts as a receptor for kit protein, important for development and survival of mast cells, hematopoietic stem cells, melanocytes, germ cells, interstitial cells of Cajal. Useful marker for confirming diagnosis of GIST (gastrointestinal stromal tumors), AML, angiomyolipoma , angiosarcomas (50%), clear cell sarcoma, CML, epithelioid sarcoma, Ewing sarcoma, granulocytic sarcoma, Hodgkin’s lymphoma (some Reed-Sternberg cells). IHC-Collagen IV with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) The antibody is directed against collagen IV, a major constituent of the basement membrane. The antibody is important in demonstrating the loss of basement membrane components by invasive carcinomas. IHC-Collagen IV without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78837 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Cyclin D1 gene is amplified in a number of cancers and is therefore of interst in tumorigenesis investigations.Overexpression promotes transformation to a malignant phenotype; overexpressed in many tumors particularly Mantle cell lymphomas and also parathyroid adenomas, multiple myeloma and hairy cell leukemia. IHC- Cyclin D1 Without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature 78882 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) The antibody is directed against collagen IV, a major constituent of the basement membrane. The antibody is important in demonstrating the loss of basement membrane components by invasive carcinomas. IHC-Cyclin D1 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78881 78838 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature 81 I J Reject Criteria Methodology Clinical Significance Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Cyclin D1 gene is amplified in a number of cancers and is therefore of interst in tumorigenesis investigations. Overexpression promotes transformation to a malignant phenotype; overexpressed in many tumors particularly Mantle cell lymphomas and also parathyroid adenomas, multiple myeloma and hairy cell leukemia. IHC-Cytoplasmic IgA with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Cytoplasmic IgA (Immunoglobulin A) is expressed on specific hematologic cells. Useful in identifying leukemias, plasmacytomas, and B-cell lineage-derived lymphomas. IHC-Cytoplasmic IgA without Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 82 78825 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Cytoplasmic IgG (Immunoglobulin G) is expressed on specific hematologic cells. Useful in identifying leukemias, plasmacytomas, and B-cell lineage-derived lymphomas. IHC-Cytoplasmic IgM with Interpretation Preferred Specimen(s) Instructions Transport Container 78824 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Cytoplasmic IgG (Immunoglobulin G) is expressed on specific hematologic cells. Useful in identifying leukemias, plasmacytomas, and B-cell lineage-derived lymphomas. IHC-Cytoplasmic IgG without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78854 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Cytoplasmic IgA (Immunoglobulin A) is expressed on specific hematologic cells. Useful in identifying leukemias, plasmacytomas, and B-cell lineage-derived lymphomas. IHC-Cytoplasmic IgG with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78853 78879 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Transport Temperature Reject Criteria Methodology Clinical Significance Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Cytoplasmic IgM (Immunoglobulin M) is expressed on specific hematologic cells. Useful in identifying leukemias, plasmacytomas, and B-cell lineage-derived lymphomas. IHC-Cytoplasmic IgM without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Cytoplasmic IgM (Immunoglobulin M) is expressed on specific hematologic cells. Useful in identifying leukemias, plasmacytomas, and B-cell lineage-derived lymphomas. IHC-DBA44 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78883 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Antibody raised against B cell centroblastic cell line; sensitive and relatively specific marker for hairy cell leukemia. Stains positive in Hairy cell leukemia (particularly “hairy” cytoplasmic processes), splenic margin zone lymphoma (71%), follicular center cell lymphomas (46%) and high grade B cell lymphomas. IHC-DBA44 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78880 78884 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Antibody raised against B cell centroblastic cell line; sensitive and relatively specific marker for hairy cell leukemia. Stains positive in Hairy cell leukemia (particularly “hairy” cytoplasmic processes), splenic margin zone lymphoma (71%), follicular center cell lymphomas (46%) and high grade B cell lymphomas. IHC-Desmin with Interpretation 78740 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen Methodology Immunohistochemical Assay (IHC) Clinical Significance Characteristically found in smooth and striated muscle cells and in neoplasms associated with them. A specific marker for myogenic differentiation among soft tissue tumors and is seen in rhabdomyomas, leiomyomas, rhabdomyosarcomas ,desmoid tumors and myofibromas. 83 I J IHC-Desmin without Interpretation 78741 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen Methodology Immunohistochemical Assay (IHC) Clinical Significance Characteristically found in smooth and striated muscle cells and in neoplasms associated with them. A specific marker for myogenic differentiation among soft tissue tumors and is seen in rhabdomyomas, leiomyomas, rhabdomyosarcomas ,desmoid tumors and myofibromas. IHC-EBV with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Labels the Epstein-Barr virus-encoded latent gene product, latent membrane protein (LMP). The antibody can be used for the demonstration of latent EBV infection in cells and tissues. EBV is associated with Hodgkin’s disease, nasopharyngeal carcinoma and nonlymphoblastic T-cell lymphoma IHC-EBV without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 84 78835 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Labels the Epstein-Barr virus-encoded latent gene product, latent membrane protein (LMP). The antibody can be used for the demonstration of latent EBV infection in cells and tissues. EBV is associated with Hodgkin’s disease, nasopharyngeal carcinoma and nonlymphoblastic T-cell lymphoma IHC-E Cadherin with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78834 78826 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Calcium-dependent transmembrane epithelial protein that promotes intercellular adhesion; its loss is associated with invasive carcinoma.The antibody is useful for the identification of E-cadherin-positive cells in normal and neoplastic tissues. Strong marker for majority of ductal breast carcinomas whereas the majority of lobular carcinoma of the breast showed weak or no labelling. IHC-E Cadherin without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Calcium-dependent transmembrane epithelial protein that promotes intercellular adhesion; its loss is associated with invasive carcinoma.The antibody is useful for the identification of E-cadherin-positive cells in normal and neoplastic tissues. Strong marker for majority of ductal breast carcinomas whereas the majority of lobular carcinoma of the breast showed weak or no labelling. IHC-EGFR with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78720 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) An important biomarker for several different tumor types as there are several FDA approved compounds that use this receptor for targeted drug therapy ; main tumor types being lung cancer, head and neck cancer and metastatic colon cancer. Overexpressed by many epithelial tumors including bladder cancers and also in a more virulent form of breast carcinoma. IHC-EMA with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78719 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) An important biomarker for several different tumor types as there are several FDA approved compounds that use this receptor for targeted drug therapy ; main tumor types being lung cancer, head and neck cancer and metastatic colon cancer. Overexpressed by many epithelial tumors including bladder cancers and also in a more virulent form of breast carcinoma. IHC-EGFR without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78827 78763 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A large cell surface mucin glycoprotein expressed by most glandular and ductal epithelial cells and some hematopoietic cells.Highly expressed by most adenocarcinomas and associated with poor prognosis; expressed by nearly all cases of Paget’s disease, and associated with invasion in pancreatic tumors 85 I J IHC-EMA without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A large cell surface mucin glycoprotein expressed by most glandular and ductal epithelial cells and some hematopoietic cells.Highly expressed by most adenocarcinomas and associated with poor prognosis; expressed by nearly all cases of Paget’s disease, and associated with invasion in pancreatic tumors IHC-ER/PgR/DNA, Paraffin Block I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78764 39479 Formalin-fixed, paraffin embedded tissue block or ten 4-micron unstained sections and six 50-micron shavings See Paraffin Blocks in the Tissue Pathology section of Specimen Collection and Handling. Tumor paraffin block (formalin-fixed only). Please submit stained H & E slide and a copy of the pathology report. Do not place paper labels with adhesive backing on slides. Use pencil or xylene resistant pen to write on the frosted end of the slide only. Mention time to fixation and duration of fixation of breast biopsy or specimen. Paraffin block bag Room temperature Received refrigerated • Received frozen Immunohistochemical Assay (IHC) Estrogen and progesterone receptor assays are routinely performed on breast carcinomas to assess responsiveness to endocrine therapy and prognosis. IHC-ER/PgR with Interpretation 10736 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides (minimum 5 in number) Tissue biopsy fixed in 10% Neutral Buffered Formalin. Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Appropriate clinical history and surgical pathology report required. Mention cold Ischemia time, Time to fixation, Duration of fixation, Fixative used and Type of processing. Note: For ER/PgR: Time to fixation should be less than one hour and duration of fixation should be more than 6 hrs and less than 72 hrs for optimum results. Fixative: 10% Neutral buffered formalin. Transport Container IHC specimen transport kit or slide folder. Biopsy in 10% NBF container with formalin as health hazard label sign. Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen : Tissue biopsy received in fixative other than 10% Neutral Buffered Formalin. Samples with prior decalcification using strong slides. Methodology Immunohistochemical Assay (IHC) Clinical Significance As a prognostic and predictive marker in a case of diagnosed Ca Breast. IHC-ER/PgR without Interpretation 79495 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides (minimum 5 in number) Tissue biopsy fixed in 10% Neutral Buffered Formalin. Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Appropriate clinical history and surgical pathology report required. Mention cold Ischemia time, Time to fixation, Duration of fixation, Fixative used and Type of processing. Note: For ER/PgR: Time to fixation should be less than one hour and duration of fixation should be more than 6 hrs and less than 72 hrs for optimum results. Fixative: 10% Neutral buffered formalin. 86 Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance IHC specimen transport kit or slide folder. Biopsy in 10% NBF container with formalin as health hazard label sign. Room temperature Received refrigerated, Received frozen : Tissue biopsy received in fixative other than 10% Neutral Buffered Formalin. Samples with prior decalcification using strong slides. Immunohistochemical Assay (IHC) As a prognostic and predictive marker in a case of diagnosed Ca Breast. IHC-ER/PgR/HER-2/neu with Interpretation 78927 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides (minimum 8 slides in number) Tissue biopsy fixed in 10% Neutral Buffered Formalin. Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Appropriate clinical history and surgical pathology report required. Mention cold Ischemia time, Time to fixation, Duration of fixation, Fixative used and Type of processing. Note: For ER/PgR: Time to fixation should be less than one hour and duration of fixation should be more than 6 hrs and less than 72 hrs for optimum results. Fixative: 10% Neutral buffered formalin. Transport Container IHC specimen transport kit or slide folder. Biopsy in 10% NBF container with formalin as health hazard label sign. Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen : Tissue biopsy received in fixative other than 10% Neutral Buffered Formalin. Samples with prior decalcification using strong slides. Methodology Immunohistochemical Assay (IHC) Clinical Significance As a prognostic and predictive marker in a case of diagnosed Ca Breast. Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides (minimum 8 slides in number) Tissue biopsy fixed in 10% Neutral Buffered Formalin. Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Appropriate clinical history and surgical pathology report required. Mention cold Ischemia time, Time to fixation, Duration of fixation, Fixative used and Type of processing. Note: For HER-2/neu: Time to fixation should be less than one hour (shorter the better). Duration of fixation should be more than 6 hrs and less than 48 hrs for optimum results. Fixative: 10% Neutral buffered formalin. Transport Container IHC specimen transport kit or slide folder. Biopsy in 10% NBF container with formalin as health hazard label sign. Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen : Tissue biopsy received in fixative other than 10% Neutral Buffered Formalin. Samples with prior decalcification using strong slides. Methodology Immunohistochemical Assay (IHC) Clinical Significance As a prognostic and predictive marker in a case of diagnosed Ca Breast. IHC-ER/PgR/HER-2/neu without Interpretation 79496 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides (minimum 8 slides in number) Tissue biopsy fixed in 10% Neutral Buffered Formalin. Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Appropriate clinical history and surgical pathology report required. Mention cold Ischemia time, Time to fixation, Duration of fixation, Fixative used and Type of processing. Note: For ER/PgR: Time to fixation should be less than one hour and duration of fixation should be more than 6 hrs and less than 72 hrs for optimum results. Fixative: 10% Neutral buffered formalin. Transport Container IHC specimen transport kit or slide folder. Biopsy in 10% NBF container with formalin as health hazard label sign. Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen : Tissue biopsy received in fixative other than 10% Neutral Buffered Formalin. Samples with prior decalcification using strong slides. 87 I J Methodology Clinical Significance Immunohistochemical Assay (IHC) As a prognostic and predictive marker in a case of diagnosed Ca Breast. Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides (minimum 8 slides in number) Tissue biopsy fixed in 10% Neutral Buffered Formalin. Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Appropriate clinical history and surgical pathology report required. Mention cold Ischemia time, Time to fixation, Duration of fixation, Fixative used and Type of processing. Note: For HER-2/neu: Time to fixation should be less than one hour (shorter the better). Duration of fixation should be more than 6 hrs and less than 48 hrs for optimum results. Fixative: 10% Neutral buffered formalin. Transport Container IHC specimen transport kit or slide folder. Biopsy in 10% NBF container with formalin as health hazard label sign. Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen : Tissue biopsy received in fixative other than 10% Neutral Buffered Formalin. Samples with prior decalcification using strong slides. Methodology Immunohistochemical Assay (IHC) Clinical Significance As a prognostic and predictive marker in a case of diagnosed Ca Breast. I J IHC-GFAP with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Intracytoplasmic filamentous protein that constitutes a portion of cytoskeleton in astrocytes (normal, reactive, neoplastic); a useful marker for CNS tumors and colonic schwannoma. With increasing astrocyte malignancy, there is progressive loss of GFAP production; used for identification of astrocytes in CNS in normal and pathological conditions. IHC-GFAP without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 88 78877 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Intracytoplasmic filamentous protein that constitutes a portion of cytoskeleton in astrocytes (normal, reactive, neoplastic); a useful marker for CNS tumors and colonic schwannoma. With increasing astrocyte malignancy, there is progressive loss of GFAP production; used for identification of astrocytes in CNS in normal and pathological conditions. IHC-HEP PAR-1 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78876 78778 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Clinical Significance Hepatocyte Paraffin 1 marker determines hepatocellular origin, particularly in panel with alpha-fetoprotein and CEA or CD10.Useful marker for most hepatocellular carcinomas, and some non hepatocellular carcinomas metastatic to liver. IHC-HEP PAR-1 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Hepatocyte Paraffin 1 marker determines hepatocellular origin, particularly in panel with alpha-fetoprotein and CEA or CD10. Useful marker for most hepatocellular carcinomas, and some non hepatocellular carcinomas metastatic to liver. IHC-Her2 neu Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78811 79021 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines. Mention time to fixation and duration of fixation of breast biopsy or specimen. Paraffin block bag Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunocytochemical Assay See Breast Cancer in the Hematology/Oncology section of Test Application and Interpretation. IHC-HER-2/neu with Interpretation 79021 Preferred Specimen(s) Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides (minimum 3 in number) Tissue biopsy fixed in 10% Neutral Buffered Formalin. Instructions Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Appropriate clinical history and surgical pathology report required. Mention cold Ischemia time, Time to fixation, Duration of fixation, Fixative used and Type of processing. Note: For HER2/neu: Time to fixation should be less than one hour (shorter the better). Duration of fixation should be more than 6 hrs and less than 48 hrs for optimum results. Fixative: 10% Neutral buffered formalin. Transport Container IHC specimen transport kit or slide folder. Biopsy in 10% NBF container with formalin as health hazard label sign. Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen : Tissue biopsy received in fixative other than 10% Neutral Buffered Formalin. Samples with prior decalcification using strong slides. Methodology Immunohistochemical Assay (IHC) Clinical Significance As a prognostic and predictive marker in a case of diagnosed Ca Breast. IHC-HER-2/neu without Interpretation Preferred Specimen(s) Instructions 79497 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides (minimum 3 in number) Tissue biopsy fixed in 10% Neutral Buffered Formalin. Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Appropriate clinical history and surgical pathology report required. Mention cold Ischemia time, Time to fixation, Duration of fixation, Fixative used and Type of processing. 89 I J Note: For HER-2/neu: Time to fixation should be less than one hour (shorter the better). Duration of fixation should be more than 6 hrs and less than 48 hrs for optimum results. Fixative: 10% Neutral buffered formalin. Transport Container IHC specimen transport kit or slide folder. Biopsy in 10% NBF container with formalin as health hazard label sign. Transport Temperature Room temperature Reject Criteria Received refrigerated, Received frozen : Tissue biopsy received in fixative other than 10% Neutral Buffered Formalin. Samples with prior decalcification using strong slides. Methodology Immunohistochemical Assay (IHC) Clinical Significance As a prognostic and predictive marker in a case of diagnosed Ca Breast. IHC-HLA DR with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Reacts with the alpha chain of monomeric HLA class II DR antigen and is valuable for analysing variations in class II expression, e.g. in B cell Non Hodgkin Lymphomas. The antibody also stains positive in AML-M3, AML-M6 IHC-HLA DR without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 90 78754 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Monoclonal antibody originally identified from melanoma extract, recognizes melanosomal glycoprotein gp100. Used in confirmation of angiomyolipoma of kidney, melanomas (85-90%), soft part sarcomas. IHC-HMB 45 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78878 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Reacts with the alpha chain of monomeric HLA class II DR antigen and is valuable for analysing variations in class II expression, e.g. in B cell Non Hodgkin Lymphomas. The antibody also stains positive in AML-M3, AML-M6 IHC-HMB 45 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78885 78755 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Clinical Significance Monoclonal antibody originally identified from melanoma extract, recognizes melanosomal glycoprotein gp100. Used in confirmation of angiomyolipoma of kidney, melanomas (85-90%), soft part sarcomas. IHC-IgD with Interpretation 78843 Preferred Specimen(s) 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Instructions Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines Transport Container IHC specimen transport kit or slide folder Transport Temperature Room temperature Reject Criteria Received frozen, broken slides, Insufficient tumor containing block Methodology Immunohistochemical Assay (IHC) Clinical Significance Human Immunoglobulin D (IgD) is present in the serum of normal individuals or of patients with Hodgkin’s disease (having high IgD concentrations). Useful in identifying leukemias, plasmacytomas and B-cell lineage-derived lymphomas (in particular marginal zone lymphoma). IHC-IgD without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Human Immunoglobulin D (IgD) is present in the serum of normal individuals or of patients with Hodgkin’s disease (having high IgD concentrations). Useful in identifying leukemias, plasmacytomas and B-cell lineage-derived lymphomas (in particular marginal zone lymphoma). IHC-INHIBIN with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78864 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Inhibin is a heterodimeric protein (with alpha and beta subunits) that inhibits or activates pituitary gonadotrophins secretion particularly follicle stimulating hormone. A sensitive marker for majority of sex cord stromal tumors, including Sertoli cell tumors, adrenocortical tumors, placental and gestational trophoblastic lesions, granular cell tumors of gallbladder and extrahepatic bile ducts. IHC-INHIBIN without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78844 78865 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Inhibin is a heterodimeric protein (with alpha and beta subunits) that inhibits or activates pituitary gonadotrophins secretion particularly follicle stimulating hormone. A sensitive marker for majority of sex cord stromal tumors, including Sertoli cell tumors, adrenocortical 91 I J tumors, placental and gestational trophoblastic lesions, granular cell tumors of gallbladder and extrahepatic bile ducts. IHC-KAPPA Light Chains with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) The presence of immunoglobulin light chains (kappa and lambda) on the cell surface is characteristic of clonal proliferation most often seen in multiple myeloma and lymphoproliferative diseases. IHC-KAPPA Light Chains without Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 92 78722 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Ki-67 is a proliferation marker. It helps to guide patient prognosis & treatment response. IHC-LAMBDA Light Chain with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78721 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Ki-67 is a proliferation marker. It helps to guide patient prognosis & treatment response. IHC-Ki 67 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78807 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) The presence of immunoglobulin light chains (kappa and lambda) on the cell surface is characteristic of clonal proliferation most often seen in multiple myeloma and lymphoproliferative diseases. IHC-Ki 67 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78806 78775 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Clinical Significance The presence of immunoglobulin light chains (kappa and lambda) on the cell surface is characteristic of clonal proliferation most often seen in multiple myeloma and lymphoproliferative diseases. IHC-LAMBDA Light Chain without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) The presence of immunoglobulin light chains (kappa and lambda) on the cell surface is characteristic of clonal proliferation most often seen in multiple myeloma and lymphoproliferative diseases. IHC-MELAN A with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78745 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Expressed in skin, retina, majority of cultured melanocytes as well as in melanomas and angiomyolipoma. Useful marker for identification of melanomas, and if melanomas are ruled out, for adrenocortical carcinomas and also angiomyolipomas. IHC-MLH-1 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78744 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Expressed in skin, retina, majority of cultured melanocytes as well as in melanomas and angiomyolipoma. Useful marker for identification of melanomas, and if melanomas are ruled out, for adrenocortical carcinomas and also angiomyolipomas. IHC-MELAN A without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78776 78859 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A protein which functions as one of the four major DNA mismatch repair genes and recombination pathway genes along with MSH2, PMS1 and PMS2. Mutations in the hMLH1 and hMLH2 genes contribute to the development of sporadic colorectal carcinoma and other hereditary and sporadic forms of human cancer. 93 I J IHC-MLH-1 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A protein which functions as one of the four major DNA mismatch repair genes and recombination pathway genes along with MSH2, PMS1 and PMS2. Mutations in the hMLH1 and hMLH2 genes contribute to the development of sporadic colorectal carcinoma and other hereditary and sporadic forms of human cancer. IHC-MPO with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 94 78856 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) This marker can be used to aid in the diagnosis and/or prognosis of cancer. The clinical interpretation of any staining or its absence should be complemented by morphological studies using proper controls and should be evaluated within the context of the patient’s clinical history and other diagnostic tests by a qualified pathologist. IHC-MSH-2 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78855 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) This marker can be used to aid in the diagnosis and/or prognosis of cancer. The clinical interpretation of any staining or its absence should be complemented by morphological studies using proper controls and should be evaluated within the context of the patient’s clinical history and other diagnostic tests by a qualified pathologist. IHC-MPO without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78860 78872 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) MSH2 is reported to be expressed in the nuclei of cells from a variety of tissues including ileum and colon, thyroid, heart, smooth muscle and the germinal centers of lymphoid follicles. Loss of MSH2 function leads to the accumulation of multiple mutations required for multistage carcinogenesis and have been linked to hereditary non polyposis colon cancer and to sporadic cancers which exhibit microsatellite instability. IHC-MSH-2 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) MSH2 is reported to be expressed in the nuclei of cells from a variety of tissues including ileum and colon, thyroid, heart, smooth muscle and the germinal centers of lymphoid follicles. Loss of MSH2 function leads to the accumulation of multiple mutations required for multistage carcinogenesis and have been linked to hereditary non polyposis colon cancer and to sporadic cancers which exhibit microsatellite instability. IHC-MUM1 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78788 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Multiple myeloma oncogene-1 (MUM1) is a 50 kDa protein encoded by the MUM1 gene. IRF4/MUM-1 is expressed in the nuclei and cytoplasm of plasma cells and a small percentage of germinal center (GC) B cells located in the light zone. This assay identifies MUM1 protein in centrocytes and their progeny, plasma cells, activated T cells, and a wide spectrum of hematolymphoid neoplasms derived from these cells. Therefore, this assay can be used as a powerful tool for the identification and the sub classification of lymphoid malignancies. IHC-MYO D1 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 78787 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Multiple myeloma oncogene-1 (MUM1) is a 50 kDa protein encoded by the MUM1 gene. IRF4/MUM-1 is expressed in the nuclei and cytoplasm of plasma cells and a small percentage of germinal center (GC) B cells located in the light zone. This assay identifies MUM1 protein in centrocytes and their progeny, plasma cells, activated T cells, and a wide spectrum of hematolymphoid neoplasms derived from these cells. Therefore, this assay can be used as a powerful tool for the identification and the sub classification of lymphoid malignancies. IHC-MUM1 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78873 78752 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) 95 I J Clinical Significance A nuclear phosphoprotein which induces myogenesis through transcriptional activation of muscle specific genes; is a sensitive marker of myogenic differentiation.Strongly labels the nuclei of myoblasts in developing skeletal muscle tissue whereas the majority of adult skeletal tissue is negative. IHC-MYO D1 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A nuclear phosphoprotein which induces myogenesis through transcriptional activation of muscle specific genes; is a sensitive marker of myogenic differentiation.Strongly labels the nuclei of myoblasts in developing skeletal muscle tissue whereas the majority of adult skeletal tissue is negative. IHC-MYOGENIN with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 96 78772 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A myogenic transcriptional regulatory protein expressed early in skeletal muscle differentiation and essential for muscle development.Sensitive and specific for rhabdomyosarcoma and Wilm’s tumors. IHC-NSE with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78771 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A myogenic transcriptional regulatory protein expressed early in skeletal muscle differentiation and essential for muscle development.Sensitive and specific for rhabdomyosarcoma and Wilm’s tumors. IHC-MYOGENIN without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78753 78819 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) This marker can be used to aid in the diagnosis and/or prognosis of cancer. The clinical interpretation of any staining or its absence should be complemented by morphological studies using proper controls and should be evaluated within the context of the patient’s clinical history and other diagnostic tests by a qualified pathologist. IHC-NSE without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) This marker can be used to aid in the diagnosis and/or prognosis of cancer. The clinical interpretation of any staining or its absence should be complemented by morphological studies using proper controls and should be evaluated within the context of the patient’s clinical history and other diagnostic tests by a qualified pathologist. IHC-P504S (AMACR) with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78710 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) p53 is a tumor suppressor gene. Mutations of the p53 gene are detectable in approximately half of all carcinomas. Detection of p53 by Immunohistochemistry serves as a surrogate marker of the mutant p53 gene. Generally, the presence of mutant p53 gene expression is associated with a poorer prognosis. IHC-P53 without Interpretation Preferred Specimen(s) Instructions 78739 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) p504s is expressed in various normal tissues and carcinomas, while it is overexpressed over 30-fold in prostate carcinoma compared to benign glandular tissue; hence used in its diagnosis. Colorectal adenocarcinoma, high-grade prostatic intraepithelial neoplasia, atypical adenomatous hyperplasia and urothelial carcinoma may also express p504s. IHC-P53 with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78738 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) p504s is expressed in various normal tissues and carcinomas, while it is overexpressed over 30-fold in prostate carcinoma compared to benign glandular tissue; hence used in its diagnosis. Colorectal adenocarcinoma, high-grade prostatic intraepithelial neoplasia, atypical adenomatous hyperplasia and urothelial carcinoma may also express p504s IHC-P504S (AMACR) without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78820 78711 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. 97 I J Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) p53 is a tumor suppressor gene. Mutations of the p53 gene are detectable in approximately half of all carcinomas. Detection of p53 by Immunohistochemistry serves as a surrogate marker of the mutant p53 gene. Generally, the presence of mutant p53 gene expression is associated with a poorer prognosis. IHC-PAX 5 (BSAP) with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Pax genes are a family of developmental control genes that encode nuclear transcription factors and have been implicated in the control of mammalian development. PAX-5 is a B cell speciric transcription factor that is expressed in pro B-cells, pre-B and mature B cells, and subsequently in all stages of B cell development until that plasma cell stage in which it is down regulated. IHC-PAX 5 (BSAP) without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 98 78712 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Normally detected in glycocalyx of fetal epithelial cells; Useful marker in diagnosing colorectal carcinoma, adenocarcinoma (lung) vs. epithelioid mesothelioma, Breast cancer vs. benign breast disease and Pancreatic adenocarcinoma. Differentiation between Cholangiocarcinoma and Hepatocellular carcinoma. IHC-P-CEA without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature 78757 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Pax genes are a family of developmental control genes that encode nuclear transcription factors and have been implicated in the control of mammalian development. PAX-5 is a B cell speciric transcription factor that is expressed in pro B-cells, pre-B and mature B cells, and subsequently in all stages of B cell development until that plasma cell stage in which it is down regulated. IHC-P-CEA with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78756 78713 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report isrequired. IHC specimen transport kit or slide folder Room temperature Reject Criteria Methodology Clinical Significance Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Normally detected in glycocalyx of fetal epithelial cells; Useful marker in diagnosing colorectal carcinoma, adenocarcinoma (lung) vs. epithelioid mesothelioma, Breast cancer vs. benign breast disease and Pancreatic adenocarcinoma. Differentiation between Cholangiocarcinoma and Hepatocellular carcinoma. IHC-PLAP with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Detection of PLAP ( Placental Alkaline Phosphatase) is of great value in the evaluation of many different types of germ cell neoplasia, particularly seminomas and carcinomas of lung, stomach, pancreas, breast and ovary. IHC-PLAP without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78732 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A glycoprotein produced almost exclusively by prostatic epithelial and the epithlieal lining of periurethral glands. PSA is strongly expressed in both normal and neoplastic prostatic tissue hence the antibody is used to label prostatic carcinoma. IHC-PSA without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78810 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Detection of PLAP ( Placental Alkaline Phosphatase) is of great value in the evaluation of many different types of germ cell neoplasia, particularly seminomas and carcinomas of lung, stomach, pancreas, breast and ovary. IHC-PSA with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78777 78733 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A glycoprotein produced almost exclusively by prostatic epithelial and the epithlieal lining of periurethral glands.PSA is strongly expressed in both normal and neoplastic prostatic tissue hence the antibody is used to label prostatic carcinoma. 99 I J IHC-PTEN with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A lipid phosphatase with tumor suppressor properties; has important role in cell cycle regulation and apoptosis.Reduced expression in seen in various malignancies including breast, prostate and endometrial cancers. IHC-PTEN without Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 100 78717 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Has wide distribution in human tissues including glia, neurons, chondrocytes, Schwann cells, melanocytes, mononuclear cells, Langerhan’s histiocytes, myoepithelial cells, notochord and various epithelia esp. in breast, salivary glands, sweat glands and female genital system. Crucial marker for malignanat melanoma; also important in Schwannonian, melanocytic and chondrocytic tumors of soft tissue and bone and ovarian melanomas IHC-S100 without Interpretatation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78852 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A lipid phosphatase with tumor suppressor properties; has important role in cell cycle regulation and apoptosis.Reduced expression in seen in various malignancies including breast, prostate and endometrial cancers. IHC-S100 with Interpretatation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78851 78718 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Has wide distribution in human tissues including glia, neurons, chondrocytes, Schwann cells, melanocytes, mononuclear cells, Langerhan’s histiocytes, myoepithelial cells, notochord and various epithelia esp. in breast, salivary glands, sweat glands and female genital system. Crucial marker for malignanat melanoma; also important in Schwannonian, melanocytic and chondrocytic tumors of soft tissue and bone and ovarian melanomas IHC-SMA with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Antibody to smooth muscle actin can be used to identify smooth muscle origin of sarcomas, and to identify myoepithelial cells of the breast. IHC-SMA without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78716 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A calcium binding glycoprotein present in the membrane component of synaptic vessels. A broad spectrum neuroendocrine marker and expressed in majority of neoplastic neuroendocrine cells and their equivalents in adrenal medulla, carotid body, skin, pituitary, thyroid, lungs, pancreas and gastrointestinal mucosa. IHC-TDT with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria 78723 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) A calcium binding glycoprotein present in the membrane component of synaptic vessels. A broad spectrum neuroendocrine marker and expressed in majority of neoplastic neuroendocrine cells and their equivalents in adrenal medulla, carotid body, skin, pituitary, thyroid, lungs, pancreas and gastrointestinal mucosa. IHC-SYNAPTOPHYSIN without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78871 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Antibody to smooth muscle actin can be used to identify smooth muscle origin of sarcomas, and to identify myoepithelial cells of the breast. IHC-SYNAPTOPHYSIN with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78870 78791 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen 101 I J Methodology Clinical Significance Immunohistochemical Assay (IHC) Terminal deoxynucleotidyl transferase is a nuclear DNA polymerase in thymic and small number of bone marrow cortical lymphocytes.Useful in diagnosis of acute lymphoblastic lymphoma (95%, diffuse strong), AML (5-10%, weak, focal). IHC-TDT without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Terminal deoxynucleotidyl transferase is a nuclear DNA polymerase in thymic and small number of bone marrow cortical lymphocytes.Useful in diagnosis of acute lymphoblastic lymphoma (95%, diffuse strong), AML (5-10%, weak, focal). IHC-THYROGLOBIN with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 102 78861 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Large glycoprotein produced by thyroid follicular cells; later iodinated to form T3 and T4. Reacts with cells in normal, hyperplastic and neoplastic thyroid tissue; specific marker of thyroid differentiation. IHC-Thrombomodulin with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78795 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Large glycoprotein produced by thyroid follicular cells; later iodinated to form T3 and T4. Reacts with cells in normal, hyperplastic and neoplastic thyroid tissue; specific marker of thyroid differentiation. IHC-THYROGLOBIN without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78792 78796 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Also called CD141, thrombomodulin is an endothelial cell transmembrane glycoprotein. It has been used for the study of vascular tumors, and for the differentiation of mesothelioma from pulmonary adenocarcinoma IHC-Thrombomodulin without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) Also called CD141, thrombomodulin is an endothelial cell transmembrane glycoprotein. It has been used for the study of vascular tumors, and for the differentiation of mesothelioma from pulmonary adenocarcinoma IHC-TTF-I with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78714 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) An intermediate filament protein which forms part of cytoskeleton of vertebrate cells; characteristically found in cells of mesenchymal origin.Expressed in a variety of normal cells/tissues and neoplastic lesions and is useful in identification of cells of mesenchymal origin in normal and neoplastic tissues. IHC-VIMENTIN without Interpretation Preferred Specimen(s) Instructions Transport Container 78725 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Selectively expressed during embryogenesis in the thyroid, the diencephalon of the brain and respiratory epithelium. Positive in thyroid and thyroid cancers regardless of histologic type and Lung cancers(adenocarcinomas-66%, large cell and small cell-95%) IHC-VIMENTIN with Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78724 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) Selectively expressed during embryogenesis in the thyroid, the diencephalon of the brain and respiratory epithelium. Positive in thyroid and thyroid cancers regardless of histologic type and Lung cancers (adenocarcinomas-66%, large cell and small cell-95%) IHC-TTF-I without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78862 78715 Formalin-fixed, paraffin-embedded tissue block, 4-micron unstained slides Please indicate on the histology request form the name of the marker(s) requested. Do not refrigerate or freeze. Pathology report is required. IHC specimen transport kit or slide folder 103 I J Transport Temperature Reject Criteria Methodology Clinical Significance Room temperature Received refrigerated, Received frozen Immunohistochemical Assay (IHC) An intermediate filament protein which forms part of cytoskeleton of vertebrate cells; characteristically found in cells of mesenchymal origin.Expressed in a variety of normal cells/tissues and neoplastic lesions and is useful in identification of cells of mesenchymal origin in normal and neoplastic tissues. IHC-WT1 with Interpretation I J Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A gene involved in the induction of Wilm’s tumor, a pediatric renal malignancy. WT1 overex pression demonstrated in Wilm’s tumor, and in majority of mesotheliomas and acute leukemias; useful marker to differentiate ovarian carcinoma (WT1+) from breast/pancreatic carcinoma (WT1-). IHC-WT1 without Interpretation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78823 10% neutral buffered Formalin-fixed, paraffin-embedded tissue block, 4-micron cut, 2 unstained section on positively charged Poly-L-Lysine/APES coated slides. Ideal Fixation time for all Immunohistochemistry & Biopsy specimens is 6-72 Hrs in 10% neutral bufferred formalin as per CAP guidelines IHC specimen transport kit or slide folder Room temperature Received frozen, broken slides, Insufficient tumor containing block Immunohistochemical Assay (IHC) A gene involved in the induction of Wilm’s tumor, a pediatric renal malignancy. WT1 overex pression demonstrated in Wilm’s tumor, and in majority of mesotheliomas and acute leukemias; useful marker to differentiate ovarian carcinoma (WT1+) from breast/pancreatic carcinoma (WT1-) Immunoglobulin A (IgA), Serum Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78822 539 1.0 mL Serum Overnight fasting is preferred. Plastic Screw cap vial Ambient 7 days, Refrigerated 14 days Gross hemolysis, lipemic Nephelometry Approximately 1 in 1000 people have IgA deficiency. Individuals with low concentrations of IgA may be asymptomatic or have sinopulmonary, gastrointestinal (including sprue-like ill ness), rheumatic, or autoimmune diseases. Immunoglobulin E (IgE), Total, Serum - Serology 542 Preferred Specimen(s) 1.0 mL Serum Transport Container Plastic Screw cap vial Transport Temperature Refrigerated 1 week, -20oC Long term Reject Criteria Gross hemolysis, lipemic MethodologyFEIA Clinical Significance IgE concentrations are increased with allergies (atopic disease), asthma, parasitic infections, unusual monoclonal gammopathies, and severe atopic dermatitis. IgE concentrations can be within the reference range with atopic disease. Individuals with low or low-normal concentra- tions typically do not have atopic disease. 104 Immunoglobulin G (IgG), Serum 543 Preferred Specimen(s) 1.0 mL Serum Instruction Overnight fasting is preferred Transport Container Plastic Screw cap vial Transport Temperature Ambient 7 days, Refrigerated 14 days Reject Criteria Gross hemolysis, lipemic Methodology Nephelometry Clinical Significance Patients with low concentrations of IgG may have a wide variety of respiratory illnesses including recurrent otitis media, sinusitis, pneumonia, chronic obstructive airway disease, bronchiectasis, and asthma. Measurement of IgG may be useful in monitoring patients being treated for IgG monoclonal gammopathies and during replacement with intravenous immunoglobulins. Immunoglobulin M (IgM), Serum Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 545 1.0 mL Serum Overnight fasting is preferred. Plastic Screw cap vial Ambient 7 days, Refrigerated 14 days Gross hemolysis, lipemic Nephelometry IgM is useful in diagnosing and monitoring patients with Waldenstrom’s macroglobinemia and other gammopathies. Infertility Panel 1, Male 78528 Includes TSH, FSH, Prolactin, Testosterone, Free and Total Preferred Specimen(s) 3 mL serum Transport Container Sterile plastic screw-cap vial - Serum Transport Temperature Room Temperature Reject Criteria Gross hemolysis • Hyperlipemia MethodologyChemiluminescence Clinical Significance See individual test Influenza A H1N1 Real Time RT PCR Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79702 3.0 mL Nasal swab or Nasopharyngeal swab or Throat swab or Nasal aspirate in viral transport media. Use only sterile swabs: Dacron®, nylon, or rayon with plastic shafts. DO NOT USE calcium alginate swabs. Viral transport media vial Refrigerated 15 days, Frozen 1 month Sputum, Bronchial lavage, specimen containing alginate swab Real-Time Reverse Transcriptase Polymerase Chain Reaction Aid in the detection and differentiation of seasonal Influenza A virus infection and infection by the 2009 H1N1 influenza virus. Inflammatory Bowel Disease See “Inflammatory Bowel Disease Differential Panel” Inhibin A 34472 Preferred Specimen(s) 1.0 mL Serum Instruction Specimens should be collected between the 14th and 22nd week of gestation. 15-16 weeks is the optimum time for testing. Transport Container Plastic Screw cap vial Transport Temperature Refrigerated 7 days Reject Criteria Gross hemolysis, lipemic MethodologyEIA 105 I J Clinical Significance Inhibin A is useful as an indicator of gonadal function, and ovarian response to hMg or to FSH stimulation. Inhibin A, produced by the placenta, is used along with other maternal serum biochemical markers to improve sensitivity of the screen for Down syndrome risk. Insulin 561 Patient PreparationFasting Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Gross hemolysis • EDTA plasma • Grossly icteric MethodologyChemiluminescence Clinical Significance For diagnosis and monitoring of diabetes and insulinsecreting tumors Insulin-Like Growth Factor See “IGF-I” Insulin Response to Glucose, 120 min I J Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 1.0 mL Serum or Heparinized plasma Plastic Screw cap vial Transport frozen Unfrozen sample,Gross hemolysis, lipemic Sandwich Chemiluminescent Immunoassay The insulin response to glucose infusion is useful in evaluating patients with hypoglycemia and suspected insulin-resistance. Integrated Panel 1 Includes Test Components 79801 CBC with Peripheral smear ESR and Bone marrow examination 14645 - CBC with Peripheral smear 78685 - Bone marrow examination See individual test for details Integrated Panel 2 Includes Test Components 78043 79802 CBC with Peripheral smear ESR, Bone marrow examination and Bone marrow biopsy with reticulin stain 14645 - CBC with Peripheral smear 78685 - Bone marrow examination 79199 - Bone marrow biopsy with reticulin stain See individual test for details Intrinsic Factor Blocking Antibody 568 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Grossly hemolysed MethodologyImmunoassay Clinical Significance Intrinsic Factor, produced by cells lining the stomach, binds vitamin B12 (cyanocobalamin) to facilitate absorption of the vitamin. Blocking antibody impedes the action of Intrinsic Factor as observed in approximately half of the patients who develop pernicious anemia. Iron, Total Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria 106 571 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 14 days Gross hemolysis Methodology Clinical Significance Spectrophotometry (SP) Serum measurements are useful in the diagnosis of iron deficiency and hemochromatosis Iron, Total and Total Iron Binding Capacity Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 7573 Total Iron, Iron Binding Capacity, and % Saturation (calculated) 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 14 days Gross hemolysis Spectrophotometry (SP) Serum iron quantification is useful in confirming the diagnosis of iron-deficiency anemia or hemochromatosis. The measurement of total iron binding in the same specimen may facilitate the clinician’s ability to distinguish between low serum iron levels caused by iron deficiency from those related to inflammatory neoplastic disorders. The assay for iron measures the amount of iron which is bound to transferrin. The total iron binding capacity (TIBC) measures the amount of iron that would appear in blood if all the transferrin were saturated with iron. It is an indirect measurement of transferrin concentrations but expressed as an iron measurement. To obtain the percent saturation, the serum iron is divided by the TIBC which gives the actual amount of saturated transferrin. The percent saturation is low in iron deficiency and high in iron storage diseases. Lactate Dehydrogenase (LD) 593 Preferred Specimen(s) 1 mL serum Instructions Do not allow multiple freeze and thaw Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 7 days Reject Criteria Gross hemolysis • Received frozen • Anticoagulants other than heparin • Received refrigerated MethodologySpectrophotometry Clinical Significance Elevations in serum lactate dehydrogenase occur from myocardial infarction, liver disease, pernicious and megaloblastic anemia, pulmonary emboli, malignancies, and muscular dystrophy LD See “Lactate Dehydrogenase (LD)” LDH See “Lactate Dehydrogenase (LD)” LDL Cholesterol, Direct See “Direct LDL” LDL Sub Fraction See “VAP® Cholesterol Test” LH (Leuteinizing Hormone) Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance 615 1 mL serum (red top tube) no additive Plastic screw-cap vial Ambient 7 days, Refrigerated 14 days Chemiluminescence This test is useful in the differential diagnosis of pituitary and gonadal insufficiency and in children with precocious puberty 107 K L LH, FSH, and PRL 78529 Includes Leuteinizing Hormone (LH), Follicle Stimulating Hormone (FSH), and Prolactin (PRL) Preferred Specimen(s) 4 mL serum from a red-top tube Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 14 days Reject Criteria • Serum: gross hemolysis or Hyperlipemic MethodologyChemiluminescence Clinical Significance See Individual test Lipase 606 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 14 days Reject Criteria Hemolysis • Lipemia MethodologySpectrophotometry Clinical Significance Confirmatory evidence for diagnosis of pancreatitis Lipid Fractionation See “VAP® Cholesterol Test” Lipid Panel with calculated LDL K L 7600 Includes Triglycerides, Total Cholesterol, HDL-Cholesterol, LDL Cholesterol (calculated) Patient Preparation Patient should fast 8 hours prior to collection Preferred Specimen(s) 3 mL serum Instructions Centrifuge within 30-60 minutes following collection Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 7 days Reject CriteriaHemolysis Methodology See individual tests for methodologies Clinical Significance See Markers of Lipidemia in the Cardiovascular section of Test Application and Interpretation. Lipid-Associated Sialic Acid (LSA,LASA) 8343 Preferred Specimen(s) 1 mL serum (red top tube ) no additive Transport Container Plastic screw-cap vial Transport TemperatureRefrigerated MethodologyImmunoprecipitin Clinical Significance This test is used to monitor tumor burden in patients with various malignant conditions, including Hodgkin’s Disease, leukemia, and melanoma. Increased levels are associated with breast cancer, colorectal cancer, gynecologic cancer, lung cancer, hematologic malignancies, melanoma, and benign, inflammatory and chronic diseases. Decreased levels are associated with therapeutic response. See Lipid Associated Sialic Acid (LASA, LSA) in the Hematology/Oncology section of Test Application and Interpretation. Lipoprotein (a) 34604 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 14 days Reject Criteria Hyperlipemia, hemolysis MethodologyImmunoturbidometric Clinical Significance Elevated concentrations of Lp(a) are associated with increased risk of coronary artery disease. See Markers of Lipidemia in the Cardiovascular Tests section of Test Application and Interpretation. 108 Liver Kidney Microsomal (LKM-1) Antibody (IgG) 15038 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Gross hemolysis • Lipemic MethodologyELISA Clinical Significance The presence of LKM-1 antibodies can be used in conjunction with clinical findings and other laboratory tests to aid in the diagnosis of autoimmune liver diseases such as autoimmune hepatitis (AIH-2) Liver Panel See “Hepatic Function Panel” Lp (a) See “Lipoprotein (a)” MAG See “Magnesium” Magnesium 622 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Anticoagulants other than heparin MethodologySpectrophotometry Clinical Significance Magnesium measurements are used in the diagnosis and treatment of hypomagnesemia (abnormally low plasma levels of magnesium) and hypermagnesemia (abnormally high plasma levels of magnesium). Magnesium is decreased in chronic nephritis, acute pancreatitis, and alcoholic cirrhosis. It is increased in acute or chronic renal failure and Addison’s Disease. Malaria and Blood Parasites 831 Patient Preparation Blood drawn 1 to 2 hours prior to expected chill will enhance recovery of malarial parasites by the laboratory Preferred Specimen(s) 2-3 air-dried blood smears (1 thick and 1-2 thin) and a whole blood EDTA (lavender-top) tube See Blood Parasites in the Parasites section of Specimen Collection and Handling for instructions Transport Container Slides in slide holders and an EDTA (lavender-top) tube Transport Temperature Room temperature Reject Criteria Hemolysis • Clotted Methodology Microscopic Examination Clinical Significance The identification of malarial parasites and other blood parasites is used to determine treatment and prognosis. One negative observation cannot rule out blood parasites. Babesia and other blood parasites are noted and reported. See the Vector-Borne Diseases section in the Infectious Disease section of Test Application and Interpretation. Malarial antigen detection 79022 Patient Preparation Blood drawn 1 to 2 hours prior to expected chill will enhance recovery of malarial parasites by the laboratory Preferred Specimen(s) 3 ml whole blood EDTA (lavender-top) tube See Blood Parasites in the Parasites section of Specimen Collection and Handling for instructions Transport Container EDTA (lavender-top) tube 109 M N Transport Temperature Reject Criteria Methodology Clinical Significance Refrigerated 3 days Hemolysis • Clotted Rapid card The identification of malarial parasites and other blood parasites is used to determine treatment and prognosis. See the Vector-Borne Diseases section in the Infectious Disease section of Test Application and Interpretation. Marijuana Metabolites, GC/MS, Urine Preferred Specimen(s) Transport Container Transport Temperature Methodology 30 mL random urine Plastic screw-cap vial Room temperature or Refrigerated Gas Chromatography/Mass Spectrometry (GC/MS) Marijuana Metabolite (50) (Cannabinoids / THC) Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance M N 78084 10 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. Methaqualone, Urine Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 4846 78086 10 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. Maternal Serum Screen 1 (AFP), Second Trimester 78321 Includes AFP and Maternal Risk Interpretation Preferred Specimen(s) 1.0 mL serum Instructions Order using special requisition. A special requisition form designed to obtain patient data and the patient’s informed consent must be utilized when ordering the MSS1 test. Because MSS1 test results are influenced by certain patient characteristics, thefollowing data must be provided with the specimen in order to permit accurate interpretation of results: date of collection, patient’s (maternal) date of birth, patient’s estimated date ofdelivery, patient’s weight, patient’s race, patient’s diabetic status (is patient insulin dependent prior to pregnancy), number of fetuses, and whether this is a repeat sample. Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 7 days Reject Criteria Gross hemolysis • Grossly icteric MethodologyChemiluminescence Clinical Significance Maternal serum Alpha-Fetoprotein (AFP) elevation is associated with an increased risk for open neural tube defects, multiple gestation, placental anomalies, ventral abdominal wall defects, congenital nephrosis and oligohydramnios. Follow-up for abnormal AFP results include genetic counseling, level II or level III ultrasound examination and consideration of Amniocentesis for chromosome and AFP analysis. Normal level do not ensure birth of a normal 110 infant; in addition, 2-3% of newborns have some type of physical or mental defects, many of which may be undetectable with current prenatal diagnostics procedure. Maternal Serum Screen 3 by using Prisca Software 7292 Includes AFP, unconjugated Estriol, hCG and Maternal Risk Interpretation Preferred Specimen(s) 3 mL serum Instructions Order using special requisition. The Maternal Serum Screen 3 (MSS3) test in pregnant women should be performed between 14.0 and 22.9 weeks gestational age, although the optimal period is 15-16 weeks. This time frame allows sufficient opportunity for further diagnostic studies if the initial MSS3 test results are abnormal. Specimens submitted before 14.0 weeks or after 22.9 weeks gestation cannot be properly evaluated for open neural tube defects, Down syndrome or Trisomy 18. A special requisition form designed to obtain patient data and the patient’s informed consent must be utilized when ordering the MSS3 test. Because MSS3 test results are influenced by certain patient characteristics, the following data must be provided with the specimen in order to permit accurate interpretation of results: date of collection, patient’s (maternal) date of birth, patient’s estimated date of delivery, patient’s weight, patient’s race, patient’s diabetic status (is patient insulin dependent prior to pregnancy), number of fetuses, and whether this is a repeat sample. Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 7 days Reject Criteria Gross hemolysis • Grossly icteric MethodologyChemiluminescence Clinical Significance Maternal serum triple screen is used for prenatal screening for Down syndrome (Trisomy 21), Trisomy 18 (Edwards syndrome), and Open Neural Tube Defects (ONTD). This profile includes Alpha-Fetoprotein (AFP), unconjugated Estriol (uE3), and human Chorionic Gonadotropin (hCG). Establishing risk for fetal Down syndrome, using the triple creen achieves a 55-65% detection rate with a 5% false positive rate. Screening for Trisomy 18 detects 60% of affected fetuses with a 0.2% false positive rate. MSAFP screening detects 88% of anencephaly and 79% of open spina bifida with a 3% false positive rate. Normal results do not ensure birth of a normal infant. In addition, 2-3% of newborns have some type of physical or mental defect, many of which may be undetectable with current prenatal diagnostic procedures. Maternal Serum Screen 3 by using Maciel Software 78322 Includes AFP, unconjugated Estriol, hCG and Maternal Risk Interpretation Preferred Specimen(s) 3.0 mL serum Instructions Order using special requisition. The Maternal Serum Screen 3 (MSS3) test in pregnant women should be performed between 14.0 and 22.9 weeks gestational age, although the optimal period is 15-16 weeks. This time frame allows sufficient opportunity for further diagnostic studies if the initial MSS3 test results are abnormal. Specimens submitted before 14.0 weeks or after 22.9 weeks gestation cannot be properly evaluated for open neural tube defects, Down syndrome or Trisomy 18. A special requisition form designed to obtain patient data and the patient’s informed consent must be utilized when ordering the MSS3 test. Because MSS3 test results are influenced by certain patient characteristics, the following data must be provided with the specimen in order to permit accurate interpretation of results: date of collection, patient’s (maternal) date of birth, patient’s estimated date of delivery, patient’s weight, patient’s race, patient’s diabetic status (is patient insulin dependent prior to pregnancy), number of fetuses, and whether this is a repeat sample. Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 7 days Reject Criteria Gross hemolysis • Grossly icteric MethodologyChemiluminescence Clinical Significance Maternal serum triple screen is used for prenatal screening for Down syndrome (Trisomy 21), Trisomy 18 (Edwards syndrome), and Open Neural Tube Defects (ONTD). This profile includes Alpha-Fetoprotein (AFP), unconjugated Estriol (uE3), and human Chorionic Gonadotropin (hCG). Establishing risk for fetal Down syndrome, using the triple screen achieves a 55-65% detection rate with a 5% false positive rate. Screening for Trisomy 18 detects 60% of affected fetuses with a 0.2% false positive rate. MSAFP screening detects 111 M N 88% of anencephaly and 79% of open spina bifida with a 3% false positive rate. Normal results do not ensure birth of a normal infant. In addition, 2-3% of newborns have some type of physical or mental defect, many of which may be undetectable with current prenatal diagnostic procedures. Maternal Serum Screen 4 (Quad Screen by using Maciel Software) M N 78324 Includes AFP, unconjugated Estriol, hCG, Dimeric Inhibin A, and Maternal Risk Interpretation Preferred Specimen(s) 3 mL serum Instructions Order using special requisition. Room temperature specimens must be received within 48 hours of collection. The Maternal Serum Screen 4 (MSS4) test in pregnant women should be performed between 14.0 and 22.9 weeks gestational age, although the optimal period is 15-16 weeks. This time frame allows sufficient opportunity for further diagnostic studies if the initial MSS4 test results are abnormal. Specimens submitted before 14.0 weeks or after 22.9 weeks gestation cannot be properly evaluated for open neural tube defects, Down syndrome or Trisomy 18. A special requisition form designed to obtain patient data and the patient’s informed consent must be utilized when ordering the MSS4 test. Because MSS4 test results are influenced by certain patient characteristics, the following data must be provided with the specimen in order to permit accurate interpretation of results: date of collection, patient’s (maternal) date of birth, patient’s estimated date of delivery, patient’s weight, patient’s race, patient’s diabetic status (is patient insulin dependent prior to pregnancy), number of fetuses, and whether this is a repeat sample. Transport Container Plastic screw-cap vial Transport Temperature Ambient 3 days, Refrigerated (cold packs) 7 days Reject Criteria Gross hemolysis • Gross lipemia • Grossly icteric MethodologyChemiluminescence Clinical Significance Maternal Serum Screen 4 is used for prenatal screening of Down syndrome (Trisomy 21), Trisomy 18 (Edwards syndrome), and open neural tube defects (ONTD). This profile includes alpha-fetaprotein (AFP), unconjugated estriol (uE3), human chorionic gonadotropin (hCG), and inhibin A. Establishing risk for fetal Down syndrome, using the quad screen achieves a 70-75% detection rate with a 5% false positive rate. Screening for Trisomy 18 detects 60% of affected fetuses with a 0.2% false positive rate. MSAFP screening detects 88% of anencephaly and 79% of open spina bifida with a 3% false positive rate. Normal results do not ensure birth of a normal infant. In addition, 2-3% of newborns have some type of physical or mental defect, many of which may be undetectable with current prenatal diagnostic procedures. Methadone, Urine Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78085 10 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. Metanephrines, Fractionated, Plasma Includes Patient Preparation Preferred Specimen(s) Instructions 112 15920 Metanephrine, Normetanephrine, and Total Metanephrine Patient should avoid alcohol, coffee, tea, tobacco and strenuous exercise before collection. Overnight fasting is preferred. Patient should be relaxed in either a supine or upright position before blood is drawn. 2 mL plasma collected in a pre-chilled EDTA (lavendertop) tube The whole blood sample should be kept on wet ice until centrifuged (preferably at 4° C) to separate the plasma within 2 hours of venipuncture. After centrifugation, the plasma should be transferred to a plastic, leakproof vial and immediately frozen. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Heparinized plasma • Serum • CSF • Room temperature urine Methodology High Performance Liquid Chromatography (HPLC) • Electrochemical Detection Clinical Significance Normetanephrine (NM) and metanephrine (MN) are the extra-neuronal catechol-o-methyl transferase (COMT) metabolites of the catecholamines norepinephrine and epinephrine, respectively. Measurement of plasma metanephrines is more sensitive (but may be less specific) than measurement of catecholamines for the detection of pheochromocytoma. Proper interpretation of results requires awareness of recent medication/drug history (e.g., antihypertensive agents, alcohol, cocaine) and other pre-analytical factors (e.g., stress, severe congestive heart failure, myocardial infarction) that influence release of catecholamines and metanephrines. Microalbuminuria, 24Hrs urine 78576 Preferred Specimen(s) 5.0 mL 24 hour urine - no preservative Instruction Submit 5.0 mL aliquot from a well-mixed 24-hour, submitted in a plastic, leak-proof container. Do not use preservatives. Record 24-hour urine volume on test request form and urine vial. Transport Container Plastic leak proof container Transport TemperatureRefrigerated Reject CriteriaFrozen MethodologySpectrophotometry Clinical Significance Microalbumin is albumin excreted in the urine and is a sensitive marker of nephropathy. It is used to screen for early renal disease in diabetic patients. Microalbumin, Random Urine with Creatinine 6517 Preferred Specimen(s) 10 mL random urine - no preservative Transport Container Plastic screw-cap vial Transport TemperatureRefrigerated MethodologySpectrophotometry Clinical Significance See Microalbumin, Urine in the Chronic Kidney Disease section of Test Application and Interpretation. Microfilaria Detection 10060 This test is appropriate if the suspected microfilaria is wucheria bancrofti, loa loa, Brugia malayi, Brugia timori, Mansonella perstaris, or Mansonella ozzardi. Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 3 mL whole blood, Slide smear Store the slide in the slide box only after the smear has dried up. EDTA vial (lavender-top) tube, Slide box Room temperature Received frozen Geimsa Stain, Microscopic Examination Detection of microfilariae in blood was the standard approach to diagnosing lymphatic filarial infection (or loiasis), and it is the one still required today for both brugian filariasis and those situations where the antigen detection test is not available for bancroftian filariasis. Micrometastasis Detection in Lymph Nodes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 12740 Formalin-fixed, paraffin embedded tissue block Pathology report is required Paraffin block bag Room temperature Received frozen Immunohistochemical Assay (IHC) This test is used to detect micrometastases of epithelial cell origin (e.g., breast cancer), determine the stage of epithelial cancers, and to predict cancer recurrence/relapse and diminished overall survival. A positive result indicates the presence cytokeratin-positive cells suggestive of micrometastasis. 113 M N See Micrometastasis Detection, IHC, Lymph Node or Bone Marrow in the Hematology/ Oncology section of Test Application and Interpretation. MPO See “Myeloperoxidase Antibody (MPO)” Mumps Antibody Panel (IgG, IgM) 36564 Preferred Specimen(s) 1 mL serum Instructions Allow specimen to clot at room temperature and then centrifuge. Separate serum from cells as soon as possible. Refrigerate at 2-8° C. Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) MethodologyImmunoassay Mycobacterium Tuberculosis 1st line drug (RIF/INH) Sensitivity assay by Hains (Rapid) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance M N 79552 Pulmonary samples, Growth from appropriate solid media, such as Lowenstein-Jensen slants, Growth in Middlebrook 7H9 broth such as the MB (Blood) culture bottle. Sterile Plastic Container, Culture Vial Room Temperature 48 hrs, Refrigerated 7 days Sample submitted in non-sterile container, uncapped or broken containers; quantity not sufficient specimens; Specimens exceeding stability. PCR, Line Probe Assay The test is based on line probe technology and permits the molecular genetic identification of the M.tuberculosis complex (M.tuberculosis, M.bovis.bovis, M.bovis BCG, M.bovis.caprae, M.africanum and M.microtii) and its resistance to rifampicin and/or isoniazid. Mycobacterium Tuberculosis 2nd line drug (Ofloxacin, 79553 Levoflxacin, Moxifloxacin, ciprofloxacin, Amikacin, Kanamycin & Capreomycin) sensitivity by Hains (Rapid) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Smear positive pulmonary samples, Growth from appropriate solid media, such as Lowenstein-Jensen slants, Growth in Middlebrook 7H9 broth such as the MB (Blood) culture bottle. Sterile Plastic Container, Culture Vial Room Temperature 48 hrs, Refrigerated 7 days Sample submitted in non-sterile container, uncapped or broken containers; quantity not sufficient specimens; Specimens exceeding stability. Line Probe Assay This is used for the detection of fluoroquinolone and amikacin/capreomycin resistance and to a lesser extent also ethambutol resistance. In combination with a molecular test for detection of rifampin and isoniazid resistance, the potential for the detection of extensively resistant tuberculosis within 1 to 2 days can be postulated. Mycobacterium tuberculosis Complex, PCR, Non-Respiratory Preferred Specimen(s) Instructions Transport Container Transport Temperature 114 30277 3 mL CSF or 6 mL body fluid or urine or 2 g tissue Tissue: Collect aseptically as much as possible, up to 2 grams. Specimen must be kept moist with transport media, saline, broth or buffer. Tissues fixed in formalin or paraffin blocks are not acceptable. Fluids: Collect aseptically as much as possible, up to 150 mL. Gastric lavage fluids: Collect 5-10 mL of an early morning specimen, before food or water intake, in a sterile container without preservative. Adjust to normal pH with 100 mg of sodium carbonate within 4 hours of collection. Unneutralized specimens are not acceptable. Separate specimens collected on 3 consecutive days are recommended. Plastic screw-cap leak proof container, for blood use lavender top EDTA tube Refrigerated (cold packs) 5 days Reject Criteria Methodology Clinical Significance Received room temperature Polymerase Chain Reaction (PCR) This is an amplified method used to detect Mycobacterium tuberculosis complex nucleic acid in the raw specimen. It is used to aid the physician in the rapid diagnosis and treatment of a possible tuberculosis infection. A negative result does not rule out disease. Results should be supported by additional alternate testing. Mycobacterium tuberculosis Complex, PCR, Respiratory Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 7 mL sputum or bronchial lavage/wash or tracheal lavage/wash Collect first morning specimen for three consecutive days. Use standard tube-in-cylinder collection kit or submit in sterile, plastic container with leak-proof cap. Keep refrigerated. Plastic screw-cap vial Refrigerated (cold packs) 5 days Received room temperature Polymerase Chain Reaction (PCR) Mycobacterium tuberculosis Drug Sensitivity (5 Drugs) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79524 Pure culture on a suitable mycobacterial medium suchas Lowenstein-Jensen agar slant, MGIT 7ml, MB BactT bottles Along with the growth, the antibiotics required to betested for are to be mentioned. The antibiotics available are: amikacin, capreomycin, kanamycin, ofloxacin, ciprofloxacin, levofloxacin, PAS, Ethionamide. See Transport of Bacterial Isolates in the Bacteriology section Room temperature Non-viable isolates Rapid Automated Fluroscent Technique Susceptibility reports can be used as a guide in the choice of first course therapy or in confirming antimicrobial resistance that leads to a further course of treatment. Aggregate data may be used to estimate the prevalence of primary and acquired antimicrobial resistance in a community. Mycobacterium, Blood Culture Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78545 Pure culture on a suitable mycobacterial medium suchas Lowenstein-Jensen agar slant, MGIT 7ml, MB BactT bottles Along with the growth, the antibiotics required to be tested for are to be mentioned. The antibiotics available are: INH, Rifampicin, Streptomicin, pyrazinamide, and ethambutol. Test may require up to eight weeks to report. See Transport of Bacterial Isolates in the Bacteriology section Room temperature Non-viable isolates Rapid Automated Fluroscent Technique Susceptibility reports can be used as a guide in the choice of first course therapy or in confirming antimicrobial resistance that leads to a further course of treatment. Aggregate data may be used to estimate the prevalence of primary and acquired antimicrobial resistance in a community. Mycobacterium tuberculosis Drug Sensitivity (8 Drugs) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 30298 10526 If culture is positive,identification will be performed. Antibiotic susceptibilitiesare only performed when appropriate. BD Myco F- lytic bottles( Preferred) SPS (yellow-top) tube, Sodium heparin (green-top) tube. Specimens should be delivered to the laboratory within one day of collection • Sodium heparin (green-top) tube • Isostat® isolator tube (not provided by laboratory) Room temperature 48 hrs Blood or bone marrow in EDTA tube MGIT 960 Isolation and identification of mycobacteria is important for the management and treatment of tuberculosis and other mycobacterial diseases. 115 M N Mycobacterium, Culture Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Acid fast stain, Mycobacterium culture, Concentration If culture is positive, identification will be performed at an additional charge. Sputum: Collect three separate first morning deepcough sputum specimens for three consecutive days. Submit each specimen immediately following collection. Specimens of gastric aspirates should be neutralized with 1 gm of sodium carbonate per 15 mL of specimen before transport to the laboratory. Specimens should be delivered to the laboratory within one day of collection. See Specimen Collection section for general site specific instructions. Sterile plastic screw-capped tube Note: Blood should be transported in sodium heparinized (green-top) tubes or tubes with SPS anticoagulant (yellow-top) tubes. Room temperature 48 hrs, Refrigerated 5 days Swab transport medium >5 days old • Dry swabs • Expired swab transport medium or port-a-cul medium • Specimen received in formalin and/or alcohol • Raw specimens >5 days old • A bagged specimen that has leaked out and contaminated the exterior of the container • 24-hour pooled sputum or urine specimens • Urine received in Boricon tube • Frozen samples • Broken slides MGIT 960 Mycobacterium Tuberculosis RT-PCR M N Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Native DNA See “DNA (ds) Antibodies” 116 4554 79277 2.0 mL sputum, BAL , Bronchi Wash, urine, pleural fluid;1.0 mL CSF Sputum: collect in a sputum collection kit or a sterile, plastic container with a leak-proof cap. BAL, Bronchi Wash, pleural fluid, CSF and Urine: Collect in a sterile, plastic container with a leak-proof cap. Whole Blood or bone marrow: Collect in sterile tubes with EDTA as an anticoagulant. Refrigerated 5 days, -20oC for extracted DNA 30 days Specimens containing heparin;?specimens with calcium alginate swabs; Samples from leaking, uncapped or broken containers; quantity not sufficient specimens; Specimens exceeding stability. Real Time PCR ABI 7500 Fast Tuberculosis is a widespread disease, with over 20,000 new cases being reported annually in the United States, in addition to the over 10 million people already infected. Although presumptive diagnosis of tuberculosis can be made on the basis of patient histories, clinical and radiological findings, and the presence of acid-fast bacilli in patient specimens, the isolation of the etiologic agent is required for the definitive diagnosis of tuberculosis. Disease in humans is caused by both M. tuberculosis and M. bovis, which are members of the M. tuberculosis complex (which also includes M. africanum, M.microti, and M. canettii). The most significant route of infection is via a respiratory route, generally resulting in pulmonary tuberculosis. Extrapulmonary disease can occur following dissemination of the organism, and it may manifest itself as abdominal, CNS, joint, or bone disease (among others). Because of the morbidity associated with disease and the possibility for the spread of this disease, a rapid clinical diagnosis is required. Although presumptive diagnosis of tuberculosis can be made on the basis of patient histories, clinical and radiological findings, and the presence of acid-fast bacilli in patient specimens, the isolation of Mycobacterium tuberculosis is required for the definitive diagnosis of tuberculosis. Routine cultures are cumbersome and time-consuming. For that reason, the development of a more rapid method for diagnosis is highly desirable. PCR amplification and detection of Mycobacterial DNA has proved to be such a method. It is highly specific, and sensitivity can be greater than that of culture, which is considered to be the gold standard. A negative PCR indicates the absence of M. tuberculosis DNA in the sample tested, and it does not exclude the diagnosis of M. tuberculosis related diseases. If culture is positive, identification will be performed Neisseria gonorrhoeae (GC), Culture 480 Includes If culture is positive, identification will be performed at an additional charge. Antibiotic susceptibilities are only performed when appropriate. Preferred Specimen(s) Urethral, cervical, anorectal or throat. Collect specimen using a blue-cap, Amies gel transport medium swab delivered within 24 hours of collection. See Neisseria gonorrhoeae Culture in the Bacteria section of Specimen Collection and Handling for instructions. Instructions Deliver to the Microbiology lab ASAP transport swab Do not refrigerate. Indicate source of specimen on both the requisition and specimen collection device. For blood specimens, use test “Culture, Blood”. For sterile body fluids, use test “Culture, Aerobic and Anaerobic”. Transport Container Copan transport swab containing Amies gel medium Transport Temperature Room temperature 48 hrs Reject Criteria Expired transport swabs • Specimens >24 hours old • Received frozen Methodology Conventional Culture,Microscopic & Automation Clinical Significance Neisseria gonorrhoeae is considered a pathogen whenever isolated and its identification is important in initiating appropriate therapy to prevent the spread of the infection as well as the serious sequelae. See Prevention of Pelvic Inflammatory Disease (PID): Screening for Chlamydia trachomatis and Neisseria gonorrhoeae in the Infectious Disease section of Test Application and Interpretation. Neisseria gonorrhoeae Smear Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79025 Urethral swab/ Vaginal discharge/ Throat swab Collect with sterile swab Stuart Medium tube with swab Room temperature 10 days for dried smear, 2 days for specimen swab Incorrect labelling, insufficient and spoiled sample; frozen Microscopic Examination A GC smear (gonococcus smear) is a gram stain of urethral exudates in men and endocervical secretions in women and can be part of a presumptive diagnosis of gonorrhea. One looks for gram-negative diplococci with flattened adjacent walls that are seen both inside and outside of polymorphonuclear leukocytes. This test is quite sensitive in symptomatic males but only 40-60% sensitive in symptomatic females.In asymptomatic males and females the gram stain has a lower predictive value. Neuron Specific Enolase (NSE) 34476 Preferred Specimen(s) 1 mL serum Instructions NSE is high in platelets and RBC; therefore, plasma and hemolyzed specimens are not acceptable Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Plasma • Hemolysis Methodology Enzyme Immunoassay Clinical Significance This test is used to monitor disease progression and therapy in individuals with small cell lung cancer (SCLC) and in other cancers (e.g., prostate). See Tumor Markers in the Hematology/Oncology section of Test Application and Interpretation. NMP-22™ See “Nuclear Matrix Proteins (NMP-22®)” Non-Gynaecologic Cytology Preferred Specimen(s) Instruction 10676 Body fluids FNAC specimen, smeared on to four glass slides and air dried. Collection requirements differ greatly depending on the type and source of the submitted sample. Provide all patient information using the Cytology test requisition. Prefer Non gynecologic specimens in section Cytology of specimen collection and handling. 117 M N Transport Container Fluid: Fluid is collected in sterile vacuum bottle or other collection container and then aliquoted as needed into lavender top (EDTA), green top (Heparin), or red top (unpreserved) tube. Transport Temperature Fluid- Refrigerated; Reject Criteria Slide broken in transit beyond our ability to repair • Unlabeled container or slide • Leakage of fluid during transport • Mismatch between name of patient on slide and name on test requisition MethodologyMicroscopy Clinical Significance The nature of possible underlying disease states including cancer or infections can often be detected by microscopically visualizing cytological changes in cells which are exfoliated and captured by fluid extraction from body cavity, brushings, washings, or fine needle aspirations. Nuclear Matrix Proteins (NMP-22®) 34099 Preferred Specimen(s) 10 mL urine collected in a Matritech NMP-22® collection kit Instructions One random urine sample should be collected and stabilized immediately, by the patient or medical personnel, using the Matritech (NMP-22®) urine collection kit. Contact your local client services department to obtain this kit. All other collection methods are unacceptable. Stabilized samples should be stored at 2-8° C for up to one week or frozen at -80° C. Transport Container Matritech NMP-22® collection kit Transport Temperature Refrigerated (cold packs) Reject Criteria Received room temperature • Collected in any device other than Matritech NMP-22® MethodologyImmunoassay Clinical Significance NMP-22® is involved in DNA replication. NMP-22® is increased in patients with bladder carcinomas. NMP-22® appears to be more sensitive and specific for lowgrade bladder cancers than urine cytology alone. See Bladder Cancer in the Hematology/Oncology section of Test Application and Interpretation. O and P with Permanent Stain See “Ova and Parasites” Occult Blood See “Fecal Globin by Immunochemistry (InSure®)” O P Occult Blood Stool Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 118 79033 2.0 gm Stool Fasting not applicable. For at least two days before and during the test period all raw meat and red meat should be avoided. Raw broccoli, cauliflower, radishes and turnips may cause false positive results, hence should be avoided. For occult blood tests certain medications such as aspirin, indomethcin, phenylbutazone, reserpine, corticosteroids and non-steroidal anti-inflammatory drugs can induce gastrointestinal bleeding. Vitamin-C and iron containing medication should be discontinued for two days before and during the test period with the consent of the physician. The stool samples should be collected from different areas of the formed stool. Sterile Plastic Screw cap vial Room Temperature 48 hrs Stool submitted in non-sterile container SG Method Fecal occult blood test that qualitatively detects human hemoglobin from blood in fecal samples. This is a useful screening aid for detecting primarily lower gastrointestinal(G.I.) disorders that may be related to iron deficiency anemia, diverticulitis, ulcerative colitis, polyps, adenomas, colorectal cancers or other G.I. lesions that can bleed. It is recommended for use by health professionals as part of routine physical examinations and in screening for colorectal cancer or other sources of lower G.I. bleeding. Opiates, Clinical Screen with Confirmation Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Codeine, Hydrocodone, Hydromorphone, Morphine, Opiates 10 mL random urine Plastic urine container Ambient 7 days, Refrigerated 14 days Urine with preservative Spectroscopy Opiates are detected by EMIT® and individual drugs are confirmed (codeine, morphine). Codeine metabolizes to morphine. Hydrocodone metabolizes to hydromorphone. All four drugs are controlled drugs. Morphine may also be present from heroin and poppy seed ingestion. Presence of drug in the urine indicates prior exposure to the drug. Opiates, Urine Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 30470 78087 10 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine Ovarian Dysfunction Assessment Panel 78539 Includes (LH FSH, PRL, TSH, E2) Day 3 to Day 5 Preferred Specimen(s) 4 mL serum from a no additive (red-top tube) Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 7 days Reject Criteria EDTA with hemolysis or received frozen or clotted • Serum: gross hemolysis or Hyperlipemic • Frozen or stored Urine MethodologyChemiluminescence Clinical Significance See Individual test OVA-179841 Includes Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance Additional Information Beta-2 Microglobulin, Apolipoprotein-A1, Transferrin, Prealbumin, CA-125 2.0 mL Serum Plastic screw-cap vial Refrigerated, Stable for 7 days Nephelometry, Electrochemiluminescence The OVA1 test is based on a proprietary FDA-cleared software device that combines the results of five biomarker assays in to a single numerical result (The results of Beta-2 microglobulin, Transferrin, Prealbumin, Apolipoprotein A1 and CA 125. These tests should be ordered independently if clinically indicated. Intended use of OVA1: The OVA1 test is qualitative serum test that combines the results of 5 immunoassays in to a single numerical result. It is indicated for women who meet the following criteria; Over age 18 years, ovarian adenexal mass present for which surgery is planned, and not yet referred to an oncologist. The OVA1 test is an aid to further assess the likelihood that malignancy is present when the physician’s independent clinical and radiological evaluation does not indicate malignancy. PAI-1 See “Plasminogen Activator Inhibitor (PAI-1)” 119 O P PAI-1 (Plasminogen Activator Inhibitor-1) See “Plasminogen Activator Inhibitor (PAI-1)” Pap 1 Slide (Pap conventional) 3526 Includes Pap results requiring physician interpretation will be performed. If concurrent testing for HPV is desired then, a separately obtained swab must be obtained and separately ordered. HPV Reflex testing is not available with Conventional Pap Smear orders. Preferred Specimen(s) One smear fixed immediately with spray fixative or 95% ethyl alcohol See Gynecologic Specimens: The “Pap” Test in the Cytology section of Specimen Collection and Handling Instructions Includes Pap results requiring physician interpretation will be performed. If concurrent testing for HPV is desired then, a separately obtained thinprep vial must be obtained and separately ordered. HPV Reflex testing is not available with Conventional Pap Smear orders. Reject Criteria Slide broken in transit beyond our ability to repair • Unlabeled slide (labels on the slide carrier are not acceptable) • Mismatch between name of patient on slide and name on test requisition MethodologyMicroscopy Clinical Significance The Conventional Pap Smear is intended for use in screening for the presence of atypical cells, cervical cancer, or its precursor lesions, as well as all other cytologic categories as defined by The Bethesda System 2001 for Reporting Cervical/Vaginal Cytologic Diagnoses. Not reliable for endometrial screening. Pap, Liquid-Based See “ThinPap® Pap” Pap Test By Liquid Based Cytology (LBC) O P 35455 Preferred Specimen(s) Provide all patient information using the Cytology test requisition. See Gynecologic Specimens: The “Pap” Test in the Cytology section of Specimen Collection and Handling. Specimen to be collected in thin prep vial using brush Transport Container Thin Prep Vial Transport Temperature Room temperature Reject Criteria See Unacceptable Specimens with General Submission Requirements in the Cytology section of Specimen Collection and Handling. MethodologyMicroscopy Clinical Significance Liquid-based Pap Testing is intended for use in the screening and detection of cervical cancer, pre-cancerous lesions, atypical cells and all other cytologic categories as defined by The Bethesda System for Reporting Results of Cervical Cytology. Pap screening is not reliable for the detection of endometrial cancer. Gynecologic cytology is a screening test which is subject to both false positive and false negative results. For that reason, the test is most reliable when a satisfactory sample is obtained on a regular repetitive basis. Hence, these results must be interpreted in the context of historic and current clinical information. See Cervical Cancer in the Hematology/Oncology section of Interpretive Information. Pap Test By LBC Without Interpretation 35456 Preferred Specimen(s) Provide all patient information using the Cytology test requisition. See Gynecologic Specimens: The “Pap” Test in the Cytology section of Specimen Collection and Handling. Transport Container Thin Prep Vial Transport Temperature Room temperature Reject Criteria See Unacceptable Specimens with General Submission Requirements in the Cytology section of Specimen Collection and Handling. MethodologyMicroscopy Clinical Significance Liquid-based Pap Testing is intended for use in the screening and detection of cervical cancer, pre-cancerous lesions, atypical cells and all other cytologic categories as defined by The Bethesda System 2001 for Reporting Results of Cervical Cytology. Pap screening is not reliable for the detection of endometrial cancer. Gynecologic cytology is a screening test which is subject to both false positive and false negative results. For that reason, the test is most 120 reliable when a satisfactory sample is obtained on a regular repetitive basis. Pap Test By Liquid Based Cytology & High Risk HPV DNA 78990 Includes Thin Prep Pap with HPV Preferred Specimen(s) Provide all patient information using the Cytology test requisition. See Gynecologic Specimens: The “Pap” Test in the Cytology section of Specimen Collection and Handling. Specimen to be collected in thin prep vial using brush Transport Container Thin Prep Vial Transport Temperature Room temperature Reject Criteria See Unacceptable Specimens with General Submission Requirements in the Cytology section of Specimen Collection and Handling. Methodology Microscopy • Third wave technology invader signal amplification detection Clinical Significance Liquid-based Pap Testing is intended for use in the screening and detection of cervical cancer, pre-cancerous lesions, atypical cells and all other cytologic categories as define by The Bethesda System for Reporting Results of Cervical Cytology. Pap screening is not reliable for the detection of endometrial cancer. Gynecologic cytology is a screening test which is subject to both false positive and false negative results. For that reason, the test is most reliable when a satisfactory sample is obtained on a regular repetitive basis. Hence, these results must be interpreted in the context of historic and current clinical information. HPV is the causative agent for cervical dysplasia and cervical cancer. HPV DNA testing in conjunction with a Pap test in women 30 years and older can be used adjunctively to assess the presence or absence of high-risk HPV types. This information, together with the physician’s assessment of cytology history, other risk factors, and professional guidelines, may be used to guide patient management. The use of this test has not been evaluated for the management of women with prior cytologic or histologic abnormalities, hysterectomy, who are postmenopausal, or who have other risk factors (e.g., HIV+, immune-compromised, DES exposure, history of STD). Partial Thromboplastin Time, Activated (aPTT) 763 Preferred Specimen(s) 3.2% sodium citrate (light blue-top) tube Instructions Correct ratio of blood to citrate is critical (9:1). Do not overfill or underfill collection tube. Mix by inversion 4 times. For non-heparinized patients, maintain specimen at room temperature. Do not uncap. Stable 24 hours at room temperature. For heparinized patients or if testing will be delayed longer than 24 hours, centrifuge specimen within 1 hour of collection at 1500 RCF (relative centrifugal force) for 15 minutes. Transfer plasma to a plastic screw-cap vial and freeze at -20° C immediately. Transport Container Whole blood: 3.2% sodium citrate (light blue-top) tube Plasma: Plastic screw-cap vial (frozen) Transport Temperature Room temperature: (Light blue-top) tube - whole blood (if specimen sent to laboratory within 4 hours of collection) Frozen: Plasma Reject Criteria Gross hemolysis • Improper blood to citrate ratio • Clotted • Age of specimen • High hematocrits Methodology Clotting method Clinical Significance Screening test for deficiencies of plasma coagulation factors other than Factors VII and XIII. The test is also used to monitor patients on heparin therapy. Penta Screen See “Maternal Serum Screen 5” Periodic Acid Schiff (PAS) Stain Preferred Specimen(s) Transport Container 70012 Tissue section/paraffin embedded block Fluid: Plastic screw-cap vial Tissue section: Slide mailer Tissue: 10% Formalin Paraffin embedded block 121 O P Transport Temperature Reject Criteria Methodology Clinical Significance Tissue 10% bufferred formalin : Ambient Paraffin Embedded block : Ambient Poorly preserved tissue/Poorly processed paraffin block Microscopic Examination This method is primarily used to identify glycogen in tissues. The reaction of periodic acid selectively oxidizes the glucose residues, creates aldehydes that react with the Schiff reagent and creates a purple magenta color. A suitable basic stain is often used as a counter-stain. PAS staining is mainly used for staining structures containing a high proportion of carbohydrate macromolecules (glycogen, glycoprotein, proteoglycans), typically found in, e.g., connective tissues, mucus, and basal laminae. PAS staining can be used to distinguish between different types of glycogen storage disease. Peripheral Blood Smear 833 Preferred Specimen(s) 2ml whole blood in EDTA vial, slide (1 fresh smear) Instructions Place the slide carefully in the slide box after the smear is dry. Transport Container EDTA vial (lavender-top) tube, slide box Transport Temperature Room temperature, stable 48 hours Reject Criteria Received frozen; broken slide Methodology Microscopic Examination Clinical Significance The peripheral blood smear may be useful to describe morphologic abnormalities and leukemias. Phenytoin O P 79072 Patient Preparation Collect as a trough just prior to next dose. For patients receiving phenytoin therapy, collect as a trough at least 2 hours after IV infusion or at least 4 hours after IM injection. Preferred Specimen(s) 1 mL serum collected in a (red-top) tube (no gel) Transport Container Plastic screw-cap vial Transport Temperature Ambient 8 hrs, Refrigerated 2 days Reject Criteria Serum separator tube (SST®) MethodologyImmunoassay Clinical Significance Phenytoin is an anticonvulsant hydantoin used for the treatment of generalized tonic-clonic (grand mal) and complex partial seizures. Phenytoin is also used for prophylaxis in neurosurgical procedures. Phenytoin levels are monitored to assure adequate therapeutic levels are achieved and to avoid toxicity. See Drug Half-life, Steady State, and Recommended Sample Collection Time in the Toxicology section of Test Application and Interpretation. Phosphate 718 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Plasma MethodologySpectrophotometry Clinical Significance Serum phosphorus (phosphate) levels alone are of limited diagnostic value and should be correlated with serum calcium levels. An increased phosphorus with decreased calcium suggests either hypoparathyroidism or renal disease. A decreased phosphorus and an increased calcium suggests hyperparathyroidism or sarcoidosis. When both calcium and phosphorus are decreased diagnostic considerations include malabsorption, vitamin D deficiency and renal tubular acidosis. Increased phosphorus and normal or increased calcium suggests Milk-alkali syndrome or hypervitaminosis D. 122 Phosphate, 24-Hour Urine 719 Preferred Specimen(s) 10 mL of well mixed 24-hour urine Transport Container Plastic leak proof container Instruction Please submit a 10 mL aliquot of a 24-hour collection. Refrigerate during and after collection. Collect urine with 25 mL of 6N HCl to maintain a pH below 3. Do not include first morning specimen; collect all subsequent voidings. The last sample collected should be the first morning specimen voided the following morning at the same time as the previous morning’s first voiding. Record 24-hour urine volume on test request form and urine vial. Transport Temperature Refrigerated 7 days Reject Criteria Received at room temperature MethodologySpectrophotometry Clinical Significance Phosphorus is present in many foods with a mean intake of approximately 1.5 gm/day in adult men and 1.0 gm/day in adult women. Absorbed phosphate, under the influence of parathyroid hormone, is readily excreted by the kidney. Urinary phosphate measurement generally reflects dietary intake hence day-to-day excretion varies considerably. Phospholipid Antibodies Panel Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79050 IgG, IgM, IgA 1 mL serum Plastic screw-cap vial Refrigerated 3 days, -20oC Long term Gross hemolysis • Plasma ELISA See in individual tests for Clinical Significance Phospholipid Antibody IgA 79049 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, stable 3 days, -20oC Long term Reject Criteria Gross hemolysis • Plasma MethodologyELISA Clinical Significance Phospholipid autoantibodies specific to phosphatidylinositol(PI), phosphatidylglycerol(PG), phosphatidylserine(PS), phosphatidylethanolamine(PE), phosphatidylcholine(PC), phosphatidic acid(PA), cardiolipin(CL) and sphingomyelin are found in hematolgic autoimmune diseases, especially antiphospholipid syndrome(APS) and systemic lupus erythematosus(SLE). APS is characterized by arterial and venous thrombosis, thrombocytopenia, and recurrent fetal loss; thrombosis, thrombocytopenia and hemolytic anemia also occur in SLE and are associated with the presence of phospholipid autoantibodies. Women with infertility showing spontaneous abortion or in vitro fertilization failure demonstrate PI autoantibodies in 25% of cases. Phospholipid Antibody IgG 79047 Preferred Specimen(s) 1.0 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 3 days, -20oC Long term Reject Criteria Gross hemolysis • Plasma MethodologyELISA Clinical Significance Phospholipid autoantibodies specific to phosphatidylinositol(PI), phosphatidylglycerol(PG), phosphatidylserine(PS), phosphatidylethanolamine(PE), phosphatidylcholine(PC), phosphatidic acid(PA), cardiolipin(CL) and sphingomyelin are found in hematolgic autoimmune diseases, especially antiphospholipid syndrome(APS) and systemic lupus erythematosus(SLE). APS is characterized by arterial and venous thrombosis, thrombocytopenia, and recurrent fetal loss; thrombosis, thrombocytopenia and hemolytic anemia also occur in SLE and are associated with the presence of phospholipid autoantibodies. Women with infertility showing spontaneous abortion or in vitro fertilization failure demonstrate PI autoantibodies in 25% of cases. 123 O P Phospholipid Antibody IgM 79048 Preferred Specimen(s) 1.0 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 3 days, -20oC Long term Reject Criteria Gross hemolysis • Plasma MethodologyELISA Clinical Significance Phospholipid autoantibodies specific to phosphatidylinositol(PI), phosphatidylglycerol(PG), phosphatidylserine(PS), phosphatidylethanolamine(PE), phosphatidylcholine(PC), phosphatidic acid(PA), cardiolipin(CL) and sphingomyelin are found in hematolgic autoimmune diseases, especially antiphospholipid syndrome(APS) and systemic lupus erythematosus(SLE). APS is characterized by arterial and venous thrombosis, thrombocytopenia, and recurrent fetal loss; thrombosis, thrombocytopenia and hemolytic anemia also occur in SLE and are associated with the presence of phospholipid autoantibodies. Women with infertility showing spontaneous abortion or in vitro fertilization failure demonstrate PI autoantibodies in 25% of cases. Phosphorus See “Phosphate” Phosphorus, Random Urine 14579 Preferred Specimen(s) 2.0 mL hour urine Transport Container Plastic leak proof container Transport Temperature Refrigerated, stable 1 week Reject Criteria Received at room temperature MethodologySpectrophotometry Clinical Significance Phosphorus is present in many foods witha mean intake of approximately 1500 mg per day for adult males and about 1000 mg per day for adult females. Absorbed phosphate, under the influence of parathyroid hormone is readily excreted in the kidney. Measurement of urinary phosphorus generally reflects dietary intake hence day to day excretion may show considerable variation. Plasminogen Activator Inhibitor (PAI-1) O P 36555 Preferred Specimen(s) 1 mL plasma collected in a 3.2% sodium citrate (light blue-top) tube Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received thawed MethodologyImmunoassay Clinical Significance Increased activity is associated with increased risk of arterial thrombosis, such as with unexplained premature myocardial infarction. As an acute phase reactant, the activity is increased after an acute event. Studies suggest PAI-1 may be a prognostic marker in early stage breast cancer. See Breast Cancer in the Hematology/Oncology section of Test Application and Interpretation. Platelet Count EDTA Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance PM-Scl See “Antibody to PM-Scl” 124 723 3 ml whole blood collected lavender top EDTA tube Do not refrigerate Sodium citrate (light blue-top) tube Room temperature, stable 48 hours Gross hemolysis • Clotted Cell counting and Microscopy Used to evaluate patient’s suspected of EDTA mediated platelet clumping. Platelets must be present in adequate numbers and have proper function to aid in hemostasis. Polycystic Ovarian Syndrome Panel Includes Preferred Specimen(s) Transport Container Instruction Transport Temperature Reject Criteria Methodology Clinical Significance FSH, LH, Androstenedione, Testosterone, Fasting Insulin, Glucose, Fasting, , Insulin/Glucose Ratio– day 2 to day 5 of cycle 4 mL serum in no additive (red-top) tubes Insulin: 1 ml serum per specimen Plastic screw-cap vial Insulin tests: Overnight fasting is required. Draw fasting specimen. Administer oral glucose solution (1.75 g/kg body weight or 75 g maximum). Collect 1 mL serum for each timed specimen post glucose dose. All tubes must be clearly marked with time drawn. Submit all tubes with one test requisition. Room temperature Gross hemolysis • Hyperlipemia Chemiluminescence, Immunoassay See Individual test Potassium, Serum Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78544 733 1 mL serum See Phlebotomy (for serum) in the Blood, Urine and Stool section in Specimen Collection and Handling Separate from cells as soon as possible after clotting Plastic screw-cap vial Ambient 5 days, Refrigerated 14 days Gross hemolysis • Plasma Ion Selective Electrode (ISE) Potassium measurements are useful in monitoring electrolyte balance in the diagnosis and treatment of disease conditions characterized by low or high blood potassium levels. Potassium is elevated in adrenal cortical insufficiency, acute renal failure and in some cases of diabetic acidosis. Potassium is decreased in diuretic administration and renal tubular acidosis. Potassium, Random Urine 14521 Preferred Specimen(s) 2.0 mL Urine Transport Container Plastic Screw cap vial Transport Temperature Ambient 7 days, Refrigerated, stable 7 day’s MethodologySpectrophotometry Clinical Significance Urinary excretion of potassium is increased in primary aldosteronism. It is often increased in dehydration and in salicylate toxicity. Decreased levels are seen in malabsorption. PRA See “Renin Activity, Plasma” Prealbumin 4847 Preferred Specimen(s) 1 mL serum Transport Container 1 (red-top) tube Transport Temperature Refrigerated, stable 7 day’s Reject Criteria Gross hemolysis • Hyperlipemic Methodology Nephelometry Clinical Significance Prealbumin is decreased in protein-calorie malnutrition, liver disease, and acute inflammation. It may be used as an indicator of nutritional requirements and response to therapy during total parenteral nutrition and as a biochemical marker of nutritional adequacy in premature infants. Prenatal Panel See “Obstetric Panel” 125 O P Pregnancy Associated Plasma Protein - A (PAPP-A) 79971 Preferred Specimen(s) 1 mL Serum Transport Container Plastic screw cap vial Transport TemperatureFrozen Reject CriteriaHemolyzed Methodology Chemiluminescence Assay Clinical Significance Maternal serum PAPP-A assessment between 11 and 14 weeks of pregnancy is reported to have significant utility in screening & Down syndrome and other chromosomal abnormalities. A combination of maternal age related risk, Free â-HCG & fetal nuchal translucency (NT) measurements might substantially increase the efficiency of prenatal screening compared to second trimester screening; using this approach, various investigators have reported detection rate for Down syndrome of 85 to 90 percent at a five percent false positive rate. proBNP, N-terminal 11188 Preferred Specimen(s) 1 mL plasma Instructions Collect in EDTA (lavender-top) tube. Separate plasma as soon after collection as possible. Keep refrigerated or frozen after separation. Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, stable 3 day’s, Frozen 6 months Reject Criteria Received room temperature MethodologyElectrochemiluminescence Clinical Significance BNP is used to aid in the diagnosis of left ventricular dysfunction in heart failure. In contrast with BNP, Nterminal pro-BNP does not have interference with the drug Natrecor® used to treat left ventricular dysfunction. See Non-Lipid Markers in Cardiovascular Disease (CVD) in the Cardiovascular section of Test Application and Interpretation. Progesterone, LC/MS/MS O P 17183 Preferred Specimen(s) 1 mL serum collected in a (red-top) tube (no gel) Instructions Separate serum after clotting. Ship serum refrigerated or frozen. Do not submit glass tubes. An early morning specimen is preferred. Specify age, sex and menopausal status on the test requisition. Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Serum separator tubes (SST®s) • Glass tubes Methodology Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS) Clinical Significance This test (1) establishes the presence of a functioning corpus lutem or luteal cell function, (2) confirms basal body temperature measurements of the occurrence of ovulation, (3) affords an indication of the day of ovulation, (4) assesses placental function during pregnancy. Progesterone Serum 745 Preferred Specimen(s) 3 mL serum Instructions It is recommended that the serum is removed from the red cells or barrier gel and the serum submitted in a plastic serum transport container. Prolonged contact of the serum with the barrier gel can cause decreased progesterone results. Transport Container Plastic screw-cap vial or barrier. Barrier gel is acceptable if tested within 24 hours Transport Temperature Refrigerated, stable 48 hours MethodologyChemiluminescence Rejection Criteria Plasma; Hemolyzed specimens Prolactin Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria 126 746 1 mL serum Plastic screw-cap vial Ambient, stable 7 day’s, Refrigerated 14 days Gross hemolysis • Grossly icteric • Grossly lipemic MethodologyChemiluminescence Clinical Significance Prolactin is a single-chain polypeptide hormone secreted by the anterior pituitary under the control of prolactinreleasing factors. These inhibiting and releasing factors are secreted by the hypothalamus. Prolactin is also synthesized by the placenta and is present in amniotic fluid. Prolactin initiates and maintains lactation in females. It also plays a role in regulating gonadal function in both males and females. In adults, basal circulating prolactin is present in concentrations up to 30 ng/mL. During pregnancy and postpartum lactation, serum prolactin can increase 10- to 20-fold. Exercise, stress, and sleep also cause transient increases in prolactin levels. Consistently elevated serum prolactin levels greater than 30 ng/mL, in the absence of pregnancy and postpartum lactation, are indicative of hyperprolactinemia, which is the most common hypothalamic-pituitary dysfunction encountered in clinical endocrinology. Hyperprolactinemia often results in galactorrhea, amenorrhea, and infertility in females, and in impotence and hypogonadism in males. Renal failure, hypothyroidism, and prolactin-secreting pituitary adenomas are also common causes of abnormally elevated prolactin levels. See Polycystic Ovary Syndrome (PCOS) in the Endocrinology section of Test Application and Interpretation. Propoxyphene, Urine Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78089 5.0 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. Phencyclidine (PCP), Urine Preferred Specimen(s) Instruction Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Protein C Activity 78088 10 mL Urine Collect urine sample without preservative Plastic, leakproof container Ambient 7 days, Refrigerated 14 days Sample coating preservative Enzyme Immunoassay The presence of drug may be indicative of therapeutic use or of substance abuse, depending on the drug. The time period for which drug can be detected is variable and dependent on a large variety of factors. Some of these factors include: (1) Amount of drug ingested; (2) individual metabolism; (3) dilution of the urine by water. 1777 Preferred Specimen(s) 1 mL platelet-poor plasma collected in a sodium citrate (light blue-top) tube Instructions Draw blood in (light blue-top) tube containing 3.2% sodium citrate, mix gently by inverting 3-4 times. Centrifuge 15 minutes at 1500 RCF (relative centrifugal force). Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet buffy layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and transport on dry ice. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received thawed Methodology Clotting Assay Clinical Significance Aids in diagnosis of decreased activity of Protein C characterized by recurrent venous thrombosis. Acquired deficiencies associated with Protein C include: oral anticoagulant therapy, liver disease, vitamin K deficiency, malignancy, consumptive DIC, surgery, trauma, antibodies to Protein C and hepatic immaturity of the newborn. 127 O P Protein C Activity and Antigen 8757 Preferred Specimen(s) 1 mL plasma in two separate tubes collected in a 3.2% Sodium Citrate (light blue-top) tube Instructions Draw blood in (light blue-top) tube containing 3.2% sodium citrate, mix gently by inverting 3-4 times. Centrifuge 15 minutes at 1500 RCF (relative centrifugal force). Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet buffy layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and transport on dry ice. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received thawed • Hemolyzed samples • Received room temperature • Received refrigerated Methodology Chromogenic Substrate • Enzyme immunoassay Clinical Significance Comprehensive test assesses the total level of protein and its functional activity in determining Protein C deficiency, which is strongly prothrombotic, and may require long-term anticoagulation therapy. In the presence of low Protein C Activity, Protein C Antigen helps to confirm and to classify Protein C Deficiency as Type I or Type II. Protein C is a highly thrombophilic protein. Protein C Antigen 4948 Preferred Specimen(s) Platelet-poor 3.2% citrate anticoagulated plasma collected in (light blue-top) tube Instructions Draw blood in (light blue-top) tube containing 3.2% sodium citrate, mix gently by inverting 3-4 times. Centrifuge 15 minutes at 1500 RCF (relative centrifugal force). Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet (buffy) layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and transport on dry ice. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Received refrigerated • Received thawed Methodology Enzyme immunoassay Clinical Significance Aids in diagnosis of congenital deficiencies characterized by recurrent venous thrombosis. Acquired deficiencies associated with Protein C include: oral anticoagulant therapy, liver disease, vitamin K deficiency, malignancy, consumptive DIC, surgery, trauma, antibodies to Protein C and hepatic immaturity of the newborn. O P Protein Electrophoresis, Serum (SPEP) 747 Includes Total Protein, Protein Electrophoresis Preferred Specimen(s) 5 mL serum Transport Container Plastic screw-cap vial Transport TemperatureRefrigerated Methodology Capillary Electrophoresis Clinical Significance Protein Electrophoresis evaluates the major protein fractions (i.e., albumin, alpha 1, alpha 2, beta and gamma proteins) to determine if there are deficiencies or excesses, as seen with macroglobulinemia, monoclonal gammopathy of undetermined significance (MGUS), and multiple myeloma. Protein S Activity 1779 Preferred Specimen(s) 1 mL platelet poor plasma 3.2% sodium citrate in (light blue-top) tube Instructions Draw blood in (light blue-top) tube containing 3.2% sodium citrate, mix gently by inverting 3-4 times. Centrifuge 15 minutes at 1500 RCF (relative centrifugal force). Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet (buffy) layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and transport on dry ice. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Hemolysis • Received thawed Methodology Clot Detection 128 Clinical Significance The congenital or acquired deficiency of Protein S increases the risk for thromboembolism, owing to a decrease of blood anticoagulant potential. It results in recurring thrombotic episodes. A decrease of Protein S leads to a greater risk of thromboembolism. Protein S Antigen 5165 Preferred Specimen(s) Platelet poor 3.2% sodium citrate-anticoagulated plasma collected in (light blue-top) tube Instructions Draw blood in (light blue-top) tube containing 3.2% sodium citrate, mix gently by inverting 3-4 times. Centrifuge 15 minutes at 1500 RCF (relative centrifugal force). Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet (buffy) layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and transport on dry ice. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Hemolysis • Received thawed Methodology Latex Agglutination Clinical Significance The congenital or acquired deficiency of protein S increases the risk for thromboembolism, owing to a decrease of blood anticoagulant potential. It results in recurring thrombotic episodes. A decrease of protein S leads to a greater risk of thromboembolism. Protein, Total Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 754 1 mL serum Plastic screw-cap vial Refrigerated 14 days Gross hemolysis • Plasma Spectrophotometry (SP) The total serum protein level is the sum of all circulating proteins that are major components of blood. Serum total protein measurements are useful in the diagnosis and treatment of a variety of diseases involving the liver, kidney, or bone marrow as well as other metabolic or nutritional disorders. Protein, Total, CSF Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 755 1.0 mL CSF Plastic screw-cap container Refrigerated 72 hrs Hemolysed specimen Spectrophotometry, Colorimetric CSF Total Protein is derived from ultrafiltration of plasma through the meninges and choroid plexus and intrathecal production. CSF Total Protein is useful in identifying increased permeability of the blood-brain barrier or increased intrathecal production. Elevated CSF Total Protein is often consistent with central nervous system disease or trauma. Protein, Total, 24-Hour Urine with Creatinine 757 Preferred Specimen(s) 10 ml aliquot from a well-mixed, 24-hour collection Instructions No preservatives. Record volume on test request form and aliquot bottle. Note: The urinalysis transport tube (yellow-top, blue fill line, preservative tube) cannot be used for protein electrophoresis on urine. Please submit 25 mL aliquot of 24 hour urine (no preservatives). Transport Container Plastic screw-cap container Transport Temperature Refrigerated 7 days Reject Criteria Acidified urine Methodology Spectrophotometry, Colorimetric 129 O P Clinical Significance Proteinuria, mainly glomerular, is often a manifestation of primary renal disease although transient proteinuria may occur with fevers, thyroid disorders, and in heart disease. In the absence of renal disease, the degree of proteinuria is slight, usually amounting to less than 2 grams per day. In chronic glomerulonephritis and in the nephrotic syndrome including lipoid nephrosis and in some forms of hypertensive vascular disease, protein loss may vary from a few grams to as much as 30 g/day. See “Chronic Kidney Disease” in the Test Application and Interpretation. Protein, Total, Random Urine with Creatinine 1715 Preferred Specimen(s) 10 ml urine from a well mixed random collection. No preservative. Note: The urinalysis transport tube (yellow-top, blue fill line, preservative tube) cannot be used for protein electrophoresis on urine. Please submit random urine with no preservative. Transport Container Plastic screw-cap urine container Transport Temperature Refrigerated 48 hrs Reject Criteria Acid-preserved urine MethodologySpectrophotometry Clinical Significance Proteinuria is characteristic of renal disease and concentrations may be increased with diabetes, hypertension, nephritic syndrome, and drug nephrotoxicity Prothrombin (Factor II) 20210G. A Mutation Analysis Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 5 mL whole blood EDTA (lavender-top) Room temperature Received frozen Polymerase Chain Reaction, Oligonucleotide Ligation Assay, Fluorescent Microspheres Factor II Mutation (G20210A) is one of the most common causes of venous thrombosis. 2.3% of the general population is heterozygous in contrast with 6.2% of patients with venous thrombosis and 18% with familial venous thrombosis. Other risk factors compound the risk for venous thrombosis. Prothrombin Time with INR O P 17909 8847 Preferred Specimen(s) One full 3.2% sodium citrate (light blue-top) tube Instructions A completely filled tube is necessary because the correct ratio of blood to citrate is critical (9:1). Mix by gentle inversion 3-4 times. Do not uncap. Stable 2 days at room temperature. If the specimen will be delayed longer than 2 days, centrifuge specimen for 15 minutes at 1500 RCF (relative centrifugal force). Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet (buffy) layer and place into a plastic screw-cap vial and freeze at - 20o C. Ship on dry ice. Transport Container Whole blood: 3.2% sodium citrate (light blue-top) tube Plasma: Plastic screw-cap vial (frozen) Transport Temperature Room temperature: (Light blue-top) tube (whole blood) Frozen: Plasma Reject Criteria Gross hemolysis • Improper blood to citrate ratio • High hematocrit • Improper blood collection Methodology Clotting Method Clinical Significance Screening test for abnormalities of coagulation factors that are involved in the extrinsic pathway. Also used to monitor effects of Coumadin® anticoagulants and to study patients with hereditary and acquired clotting disorders. PSA Total Preferred Specimen(s) 1 mL serum Instructions Non-frozen specimens must be received in the laboratory within 24 hours Transport Container Plastic screw-cap vial Transport Temperature Ambient 24 hrs, Refrigerated 24 hrs MethodologyChemiluminescence 130 5363 Clinical Significance Elevated serum PSA concentrations have been reported in men with prostate cancer, benign prostatic hypertrophy, and inflammatory conditions of the prostate. See Prostate Cancer in the Hematology/Oncology section of Test Application and Interpretation. PSA, Free and Total 31348 Includes Total PSA, Free PSA, % Free PSA (calculated) Preferred Specimen(s) 2 mL serum Instructions Non-frozen specimens must be received in the laboratory within 24 hours Transport Container Plastic screw-cap vial Transport Temperature Ambient 24 hrs, Refrigerated 24 hrs Reject Criteria Gross hemolysis • Gross lipemia MethodologyChemiluminescence Clinical Significance In men over age 50 years with total PSA between 4.0 and 10.0 ng/mL, those with prostate cancer tend to have lower % free PSA than those with benign prostatic hypertrophy (BPH), although there is considerable overlap in results for the two populations. % free PSA may aid in avoiding unnecessary biopsies in these circumstances. See Prostate Cancer in the Hematology/Oncology section of Test Application and Interpretation. PT See “Prothrombin Time with INR” PTT See “Partial Thromboplastin Time, Activated (aPTT)” PTH, Intact and Calcium 8837 Preferred Specimen(s) 2 mL frozen serum collected in a (red-top) tube (no gel) Instructions Spin and transfer to a plastic transport vial. Mark the specimen type as serum on the vial. Freeze and submit to the laboratory. Do not submit glass tubes. Note: Sodium or lithium heparin are no longer acceptable specimen types. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Plasma • Received room temperature • Received refrigerated • Gross Hemolysis • Lipemia Methodology Immunochemiluminometric Assay (ICMA) Clinical Significance The major function of PTH is to maintain the serum total calcium concentration within a narrow range. The net effects of PTH are to increase the serum concentration of calcium and to decrease that of phosphate. The assay is useful in making the diagnosis of primary hyperparathyroidism, secondary hyperparathyroidism, and a differential diagnosis of hypercalcemia. The assay helps in distinguishing hypercalcemia caused by either primary hyperparathyroidism or malignant disease. See Calcium and Bone Metabolism (Including Osteoporosis) in the Endocrinology section of Test Application and Interpretation. PTH-Related Protein (PTH-rP) Preferred Specimen(s) Instructions 34478 1.5 mL plasma collected in a PTH-related protein (special collection) tube Store cocktail tube in the freezer at -20°C (tubes can be stored for up to one year). The cocktail tube is a heparin tube with protease inhibitor (aprotinin, leupeptin & blue dye) added (glass or plastics collection tubes are acceptable). Prior to drawing samples, place PTHrP cocktail tubes on ice. Collect the whole blood into a syringe and transfer the sample into the cocktail tube. Alternatively, if a syringe is not available, collect the blood in a plain red-top tube and immediately transfer the sample into the cold cocktail tube. Mix thoroughly by inversion. Immediately separate the plasma from the cells in a refrigerated centrifuge and transfer to a plastic test tube. Freeze immediately at -20°C or colder. If a refrigerated centrifuge is not available, chill the tubes and the centrifuge tube holders for 5 minutes in an ice lurry. Ship frozen. 131 O P Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Received refrigerated MethodologyImmunoassay Clinical Significance Parathyroid hormone-related peptide (PTH-rP) is structurally and functionally similar to human parathyroid hormone (HPTH). Hypercalcemia of malignancy is due either to local osteolysis at the site of bone metastases or to PTH-rP production by the malignant cells. Pyrexia of Unknown Origin (PUO) Panel Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance CBC with peripheral blood smear; ESR; Urinalysis Complete; Malaria Blood Parasite; Widal Test; Culture Blood; Alanine Amino Transferase (ALT/SGPT) 6.0 mL whole blood collected in EDTA tube (leavender top), 2.0 mL serum, 5.0 mL urine collected with preservative Serum - Plastic screw-cap vial, Whole blood – Collection tube, Urine – Leak proof container Room Temperature Plasma • Gross Hemolysis • Lipemia See individual analytes See individual tests for clinical significance. Quantiferon GoldTB Q R 78657 19453 Preferred Specimen(s) 1 ml whole blood in each grey, red top and purple top TB Gold tubes. ( Use the tube sent by Quest Diagnostics only) Transport Container 3 TB Gold tubes (grey, red top & purple top) Instructions -> Store & ship the tubes at room temperature if the tubes can reach the Quest Diagnostics (QDI) Lab at Gurgaon maximum within 16 hrs of collection of sample -> If the sample can not reach the QDI lab at Gurgaon within 16 hrs of collection then incubate the red top, grey top & the purple top tubes in calibrated incubator at 37°C ± 1°C for 16-24 hrs. This incubation is mandatory within 16 hrs of collection of the sample. After incubation for 16-24 hrs at 37°C ± 1°C in a calibrated incubator, the sample can be sent in the following ways: (i) If the incubated sample can reach the QDI lab at Gurgaon within 72 hrs after incubation then the red top, grey top & purple top should be ship at 2-8 °C (ii) If the incubated sample is likely to reach QDI lab after 72 hrs of incubation the primary tubes (red top, grey top & purple top) has to be centrifuged at 2000-3000 RCF(g). Separate the plasma in a screw capped plastic vial after centrifugation & ship frozen. Separate the plasma (from grey top, Red to & purple top vial) in three different screw capped transportation plastic vials after centrifugation & ship frozen. (iii) Label the vials with source of plasma for e.g. as grey top, red top & purple top. Transport Temperature If transported within 16 hours of collections: 22°C + 5°C If tubes incubated : 2 - 27°C for 3 days Separated Plasma : 2 - 8°C for 4 weeks & -20°C for extended period MethodologyELISA Clinical Significance The Quantiferon TB Gold test is helpful but insufficient in diagnosing M. tuberculosis complex infection in sick patients: a positive result can support the diagnosis of tuberculosis disease. However, infections by other mycobacteria (e.g., M. kansasii) could also cause a positive results. Other medical and diagnostic evaluations are necessary to confirm or exclude tuberculosis disease. Renal Function Panel 1 Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 132 Creatinine with eGFR; BUN; BUN/Creatinine Ratio; Uric Acid 2.0 mL serum and 5.0 mL urine collected with preservative Serum - Plastic screw-cap vial, Urine – Leak proof container Ambient 5 days, Refrigerated 14 days Plasma • Gross Hemolysis • Lipemia See individual analytes See individual tests for clinical significance. 78591 Renal Function Panel 2 Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Creatinine with eGFR; BUN; BUN/Creatinine Ratio; Uric Acid; Na; K; Cl; Anion Gap 2.0 mL serum and 5.0 mL urine collected with preservative Serum - Plastic screw-cap vial, Urine – Leak proof container Ambient 5 days, Refrigerated 14 days Plasma • Gross Hemolysis • Lipemia See individual analytes See individual tests for clinical significance Reticulin Stain With Interpretation Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78122 Tissue biopsy in 10% buffered formalin or formalin fixed paraffin embedded tissue block. Paraffin block bag; slide holder (as applicable) Room temperature Improper fixation; Receive Frozen Manual staining Reticular fibers are present in normal human tissues and have a support function.They are normally found throughout the body but are most abundant in liver, spleen, kidney and lymph nodes.In certain tumors, reticulin is located in a characteristic position in relation to the actual tumor cells. Reticulin stains can therefore be an important diagnostic tool for the differential diagnosis of certain types of tumor. Reticulin Stain Without Interpretation Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78592 78889 Tissue biopsy in 10% buffered formalin or formalin fixed paraffin embedded tissue block. Paraffin block bag; slide holder (as applicable) Room temperature Improper fixation; Received Frozen Manual staining Reticular fibers are present in normal human tissues and have a support function.They are normally found throughout the body but are most abundant in liver, spleen, kidney and lymph nodes.In certain tumors, reticulin is located in a characteristic position in relation to the actual tumor cells. Reticulin stains can therefore be an important diagnostic tool for the differential diagnosis of certain types of tumor. Reticulocyte Count, Automated 793 Preferred Specimen(s) Whole blood full EDTA (lavender-top) tube - mix well by gentle inversion Instructions Maintain specimen at room temperature. If multiple draw, collect (lavender-top) tube last. Transport Container EDTA (lavender-top) tube Transport Temperature Room temperature Reject CriteriaClotted Methodology Electronic Cell Sizing and Counting/Cytometry/Microscopy Clinical Significance Use in evaluating erythropoietic activity RF See “Rheumatoid Factor” Rheumatoid Factor Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 4418 1 mL serum Plastic screw-cap vial Room temperature 1 week, Refrigerated 14 days Gross hemolysis • Lipemia Nephlometry Elevated RF is found in collagen vascular diseases such as SLE, rheumatoid arthritis, scleroderma, Sjögren’s Syndrome, and in other conditions such as leprosy, tuberculosis, syphilis, malignancy, thyroid disease and in a significant percentage of otherwise normal elderly patients 133 Q R Rotavirus Antigen 79051 Preferred Specimen(s) Stool specimen or rectal swab in a clean, dry container without preservatives or media See Stool in the Bacteria section of Specimen Collection and Handling for instructions. Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Transport systems containing media, serum, preservatives or detergent MethodologyELISA Clinical Significance Rotavirus infection is the major cause of gastroenteritis in children from six months to two years. Infection occurs in both sporadic and epidemic forms and is responsible for approximately half the cases of diarrhea in infants that require hospitalization worldwide. The peak of rotavirus disease in temperate climates occurs during the cooler months of the year. Rotavirus has also emerged as a cause of enteritis in adults, particularly in elderly immunosuppressed patients. RPR for Syphilis 799 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, Stability 7 days Reject Criteria Gross hemolysis • Hyperlipemia • CSF MethodologyFloculation Clinical Significance This is a non-treponemal screening test for syphilis. False positive results may occur due to systemic lupus erythematosus, malaria, mononucleosis, infectious hepatitis, leprosy, brucellosis, atypical pneumonia, typhus, yaws, pinta, or pregnancy. Positive results should be confirmed with a more specific treponema pallidum antibody test (FTA-ABS). Monitoring of RPR is helpful in assessing effectiveness of therapy. Rubella Antibodies (IgG, IgM) 79534 Includes Rubella IgG, Rubella IgM Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, stability 3 days Reject Criteria Gross hemolysis • Gross lipemia MethodologyCLIA Clinical Significance Rubella is an acute exanthematous viral infection of children and adults. Rash, fever and lymphadenopathy characterize the illness. While many infections are subclinical, this virus has the potential to cause fetal infection with resultant birth defects. Diagnosis of a Rubella infection is best made serologically. In the absence of a current or recent infection, a demonstration of specific IgG on a serum sample is evident of immunity to Rubella. Rubella Antibodies, IgG S T 79916 Preferred Specimen(s) 1 mL serum Instructions Allow specimen to clot at room temperature and then centrifuge. Immediately separate from cells and refrigerate at 2-8°C. Transport Container No additive (red-top) tube Transport Temperature Refrigerated, stability 3 days Reject Criteria Received frozen MethodologyCLIA Clinical Significance Rubella is an acute exanthematous viral infection of children and adults. Rash, fever and lymphadenopathy characterize the illness. While many infections are subclinical, this virus has the potential to cause fetal infection with resultant birth defects. Diagnosis of a rubella infection is best made serologically. In the absence of a current or recent infection, a demonstration of specific IgG on a serum sample is evidence of immunity to rubella. Rubella Antibodies (IgM) Preferred Specimen(s) 134 1 mL serum 79915 Instructions Allow specimen to clot at room temperature and then centrifuge. Immediately separate from cells and refrigerate at 2-8°C. Transport Container No additive (red-top) tube Transport Temperature Refrigerated, stability 3 days Reject Criteria Received frozen MethodologyCLIA Clinical Significance Testing immediately post-exposure is of no value without a later convalescent specimen. While the presence of IgM antibodies suggests current or recent infection, low levels of IgM antibodies may occasionally persist for more than 12 months post-infection or immunization. Saccharomyces (ASCA) IgA 79061 Preferred Specimen(s) 1.0 mL Serum Transport Container Plastic Screw cap vial Transport Temperature Refrigerated, stable 48 hours Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Antibodies to Saccharormyces cerevisiae are found in approximately 75% of patients with Crohn’s disease, 15% of patients with ulcerative colitis, and 5% of the healthy population. High titers of antibody increase the likelihood of disease, and specifically Crohn’s disease, and are associated with more aggressive disease. Saccharomyces (ASCA) IgG 79062 Preferred Specimen(s) 1.0 mL Serum Transport Container Plastic Screw cap vial Transport Temperature Refrigerated, stable 48 hours Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Antibodies to Saccharormyces cerevisiae are found in approximately 75% of patients with Crohn’s disease, 15% of patients with ulcerative colitis, and 5% of the healthy population. High titers of antibody increase the likelihood of disease, and specifically Crohn’s disease, and are associated with more aggressive disease. Salmonella, Shigella, Campylobacter Stool Culture See “Culture, Stool (Salmonella/Shigella/ Campylobacter)” Screening Fever Panel Includes Test Components Scl-70 78583 CBC, ESR, Malarial Parasite & Urinalysis 79930 - ESR 5463 - Urinalysis 6399 - CBC 831 - Malaria/Blood parasite See individual test for details 79085 Preferred Specimen(s) 1.0 mL Serum Transport Container Plastic Screw cap vial Transport Temperature Refrigerated 3 days, -20oC Long term Reject Criteria Grossly Hemolysed MethodologyELISA Clinical Significance Scleroderma may be localized or diffuse [Progressive Systemic Sclerosis (PSS)] that may involve skin, gastrointestinal tracts, lungs, vascular and cardiac systems, and kidneys. Scl-70 Antibody is present in approximately 40% of patients with PSS. 135 S T Serotonin, Serum 29851 Patient Preparation Patient should avoid food high in indoles: Avocado, banana, tomato, plum, walnut, pineapple, and eggplant. Patient should also avoid tobacco, tea and coffee three days prior to specimen collection. Preferred Specimen(s) 2 mL serum collected in a (red-top) tube (no gel) Instructions Spin and freeze serum below -20oC within 2 hours after collection Transport TemperatureFrozen Reject Criteria Received room temperature • Received refrigerated Methodology High Performance Liquid Chromatography (HPLC) • Fluorescence Detection Serum Immunofixation Electophoresis Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance 79101 1.0 mL serum Plastic screw-cap vial Refrigerated, stable 10 day’s, Frozen 1 month Capillary Electrophoresis Monoclonal increases in IgG or IgA are often associated with diseases such as multiple myeloma, lymphomas or leukemia. A monoclonal increase in IgM is commonly associated with Waldenström’s macroglobulinemia. Sex Hormone Binding Globulin (SHBG) 30740 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 7 days Reject Criteria Gross hemolysis • Plasma MethodologyChemiluminescene Clinical Significance Testosterone, dihydrotestosterone and estrogens circulate in serum bound to Sex Hormone Binding Globulin (SHBG). SHBG concentrations are increased in pregnancy, hyperthyroidism, cirrhosis, oral estrogen administration and by certain drugs. Concentrations are decreased by testosterone, hypothyroidism, Cushings syndrome, acromegaly and obesity. Sickle Cell Anemia Mutation Analysis S T Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 26382 Amniotic fluid: Collect 10-20 mL amniotic fluid in a sterile plastic container Chorionic villus sample (CVS): Collect 15-30 mg of chorionic villi in a sterile container. Add 2-3 mL of sterile saline or tissue culture medium. Cultured cells: Ship two 100% confluent T-25 flasks filled with growth media. Ship at room temperature. Do not refrigerate or freeze. Call lab for additional requirements for prenatal testing. Indicate source of cells: Amniotic Fluid (AF) or Chorionic Villus Sample (CVS). Test code 10262 (Maternal Cell Contamination Study, STR Analysis) may be ordered with this test to rule out maternal contamination of the fetal sample Sterile transport tube for amniotic fluid Room temperature Received frozen Polymerase Chain Reaction (PCR), Restriction Fragment Length Polymorphism This test is intended for the detection of hemoglobin S and C sickle cell trait prenatally. Parents should be tested for carrier status before or simultaneously with the prenatal testing. Sjogren’s Antibody (SS-A) / (Anti-Ro) 38568 Preferred Specimen(s) 1.0 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, stable 24 hours, -20oC Long term Reject Criteria Gross hemolysis • Hyperlipemic MethodologyELISA Clinical Significance Sjögren’s syndrome is an autoimmune disease of unknown etiology occurring predominantly (over 90%) in women in the fourth to sixth decades of life. SSB antibodies have a high specificity for the sicca complex, which results from a failure of secretion by lacrimal, salivary and other glands. SSA antibodies may also be detected in cases of congenital heart block, 136 neonatal lupus and in approximately 30% of SLE patients. Sjogren’s Antibody (SS-B) / (Anti-La) 38569 Preferred Specimen(s) 1.0 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, stable 24 hours, -20oC Long term Reject Criteria Gross hemolysis • Hyperlipemic MethodologyELISA Clinical Significance Sjögren’s syndrome is an autoimmune disease of unknown etiology occurring predominantly (over 90%) in women in the fourth to sixth decades of life. SSB antibodies have a high specificity for the sicca complex, which results from a failure of secretion by lacrimal, salivary and other glands. SSA antibodies may also be detected in cases of congenital heart block, neonatal lupus and in approximately 30% of SLE patients. Slide Review (upto 2 slides/blocks) 79120 Preferred Specimen(s) Block, H & E slides submitted in slide folder Instructions This code is for a consultation (2nd opinion) on previously diagnosed material. Required information: Patient history and any other relevant information; name, telephone number and fax number of referring physician. Transport Container Send blocks in plastics containers & slides in slide folder (preferably) Transport Temperature Room temperature Reject Criteria Broken slides, Improperly stained slides MethodologyMicroscopy Clinical Significance The nature of possible underlying disease states can often be detected by microscopically visualizing histologic changes in tissue biopsies Slide Review (more than 2 slides/blocks) 79121 Preferred Specimen(s) Block, H & E slides submitted in slide folder Instructions This code is for a consultation (2nd opinion) on previously diagnosed material. Required information: Patient history and any other relevant information; name, telephone number and fax number of referring physician. Transport Container Send blocks in plastics containers & slides in slide folder (preferably) Transport Temperature Room temperature Reject Criteria Broken slides, Improperly stained slides MethodologyMicroscopy Clinical Significance The nature of possible underlying disease states can often be detected by microscopically visualizing histologic changes in tissue biopsies Slide for Issue (1 slide only) Instructions 79520 Provide a copy of the surgical pathology report. Mention number of slides to be issued. If more than one slide issue required, charges will be that number of time. SM/RNP antibodies 79075 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 24 hrs, -20oC Long term MethodologyELISA Clinical Significance Smith (Sm)/U1-RNP Antibody is detected in patients with mixed connective tissue disease (having features of systemic lupus erythematosus (SLE), scleroderma, and polymyositis). Sodium Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology 836 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 14 days Gross hemolysis • Anticoagulants other than heparin Ion Selective Electrode (ISE) 137 S T Clinical Significance Sodium measurements are useful in the diagnosis and treatment of aldosteronism, diabetes insipidus, adrenal hypertension, Addison’s Disease, dehydration, inappropriate antidiuretic hormone secretion, or other diseases involving electrolyte imbalance Sodium, Random Urine Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 14522 2 mL urine Collect without preservatives. Refrigerate during and after collection. Aliquot unpreserved specimen before adding acid. Plastic, screw cap container Ambient 7 days, Refrigerated, stable 7 day’s Received at room temperature Ion Selective Electrode (ISE) A urine test to check sodium levels is done to: • Check the water and electrolyte balance of the body. • Find the cause of symptoms from low or high levels of sodium. • Check the progress of diseases of the kidneys or adrenal glands. Decreased levels are seen in congestive heart failure, excessive sweating, diarrhea, pyloric obstruction, malabsorption, and primary aldosteronism. Increased levels may be due to increased salt intake, failure of the adrenal glands, diabetic acidosis, salt losing renal disease, and water deficient dehydration. Somatomedin-C See “IGF-I” SPEP See “Protein Electrophoresis, Serum (SPEP)” Stool Ova and Parasites S T Includes Patient Preparation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Ova and Parasite Concentrate Result, Trichrome Result Interfering substances - bismuth, barium (wait 7-10 days), antimicrobial agents (wait 2 weeks), gallbladder dye (wait 3 weeks after procedure) Stool in 10% Formalin and Polyvinyl Alcohol (PVA) transport vials See Stool Samples for Ova and Parasties (O & P) in the Parasites section of Specimen Collection and Handling Urine collected between noon and 3 PM may be submitted unpre served to examine for schistosoma. Deliver urine specimens to the laboratory as soon as possible 10% formalin and polyvinyl alcohol (PVA) transport vials Urine may be submitted in a sterile screw-cap container Stool: Room temperature 48 hrs in formlin Urine: Refrigerated (cold packs) Unpreserved specimens • Specimens containing barium • Stool preserved in medium other than 10% formalin, PVA, Sodium Acetate-Acetic Acid Formalin (SAF) or Merthiolate Iodine Formalin (MIF) • Stool in 10% formalin received frozen • Stool submitted in expired transport vial Microscopic Examination,Trichrome Stain & Modified Acid Fast Stain Diseases caused by human parasites remain on a worldwide basis among the principle causes of morbidity and mortality. Correct diagnosis of intestinal parasitic infection depends on proper collection, transport, detection and identification of parasites in stool specimens. Symptoms range from malaise to death. Treatment is dependent upon examining multiple stool exams due to the erratic shed rates of some parasites. Stool (Salmonella, Shigella, Campylobacter) Culture See “Culture, Stool (Salmonella/Shigella/Campylobacter)” Stool Blood See “Fecal Globin by Immunochemistry (InSure®)” 138 681 Stool Routine/Microscopic Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 4497 10 gm fecal specimen in plastic, leak-proof container Do not freeze Plastic, leak-proof feces container Room Temperature, stable 48 hours Received frozen Microscopic Examination Stool examination is useful to detect some gastrointestinal parasites and fungal elements. Other tests may be more appropriate to identify and culture bacterial infections. Strep A See “Anti-Streptolysin O Antibody (ASO)” Streptococcus, Group A See “Streptococcus, Group A, Culture” See “Anti-Streptolysin O Antibody (ASO)” Streptococcus, Group A, Culture 4485 Preferred Specimen(s) Collect throat specimen using a red-cap, Amies liquid transport medium swab or swab in other liquid transport media See Throat Cultures: Streptococcus, Group A in the Bacteria section of Specimen Collection and Handling. Instructions Indicate source of specimen on both the test request form and specimen transport device Transport Container Transport swab Transport Temperature Room temperature Reject Criteria Swabs >48 hours old • Expired transport device • Received frozen • Viral transport device • DNA probe transport device Methodology Conventional Culture,Microscopic & Automation Clinical Significance Recovery of group A Streptococcus from a symptomatic patient is usually considered significant Syphilis See “RPR (Monitor) with Reflex to Titer” T3 Free (FT3) 34429 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient, stable 4 day’s, Refrigerated 14 days MethodologyChemiluminescence Clinical Significance See Thyroid Disease in the Endocrinology section of Test Application and Interpretation. T3 Total 859 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient, stable 4 day’s, Refrigerated 14 days MethodologyChemiluminescence Clinical Significance For diagnosis of T3 thyrotoxicosis T4, Free (FT4) 866 Preferred Specimen(s) 1.0 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 14 days MethodologyChemiluminescence 139 S T Clinical Significance For diagnosis of hypothyroidism and hyperthyroidism See Thyroid Disease in the Endocrinology section of Test Application and Interpretation T4 Total (Thyroxine) 17733 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 7 days, Refrigerated 7 days MethodologyChemiluminescence Clinical Significance Thyroxine (T4) is the major secretory hormone of the thyroid. Only 0.03% of T4 is unbound and free for exchange with tissues. Thyroid function may be assessed with thyroid stimulating hormone (TSH) and free T4 measured. TA90 (Melanoma-Associated Antigen) 15524 Preferred Specimen(s) 1 mL serum Instructions Draw 5 mL blood in a red-top tube (no gel), allow blood to clot at room temperature for one hour and separate by centrifugation (1500 x g for 10 minutes) Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Hemolysis • Lipemia • Animal or post mortem specimen • Received room temperature MethodologyELISA Clinical Significance This assay is indicated in the post-operative evaluation of all patients whose localized melanoma is curatively resected. Potentially 90% of 50,000 new cases each year. See Melanoma in the Hematology/Oncology section of Test Application and Interpretation. Testosterone, Free, Bioavailable and Total, LC/MS/MS 14966 Includes Total Testosterone, Free and Bioavailable Testosterone (calculated), Sex Hormone Binding Globulin, Albumin Preferred Specimen(s) 2.5 mL serum collected in a (red-top) tube (no gel) Instructions Specify age and sex on test requisition. Shipping frozen is acceptable. Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Samples received in serum separator tubes (SST®s) Methodology Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS) • Calculation • Spectrophotometry • Immunochemiluminescent Assay Clinical Significance Helpful in assessing testicular function in males and managing hirsutism, virilization in females See Polycystic Ovary Syndrome (PCOS) in the Endocrinology section of Test Application and Interpretation. Testosterone, Total S T Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 873 2 mL serum collected in a (red-top) tube (no gel). Specify age and sex on test requisition. Plastic screw-cap vial Ambient 3 days, Refrigerated 14 days Body fluids Automated ICMA • Extraction • Chromatography •Chemiluminescence Testosterone circulates almost entirely bound to transport proteins. Normally less than 1% is free. Testosterone measurements are used to assess erectile dysfunction, infertility, gynecomastia, osteoporosis, and hormone replacement therapy. Throat Culture and Susceptibility See “Culture, Throat” Thrombophila Panel Includes 140 78590 Protein-C Functional, Protein-S Functional, APC-R, Antithrombin III, ANA ELISA, Anti DsDNA, Factor V Leiden, Complement C3, Complement C4, Lupus Anti Coagulant (screening), Anti Cardiolipin – IgG & Anti Cardiolipin IgM Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance For Specimen requirements see individual Tests listed under Test Components. Plastic screw cap vial See individual tests for transport temperature Hemolyzed, lipemic, leaked & QNS specimens Chromogenic; Enzyme Immunoassay Invader Assay/Signal Amplification Clotting Assay Fluorescence polarizaton Immunoassay Clot Detection Decreased antithrombin III activity, protein C activity, free protein S, and the presence of a factor V (Leiden) and/or factor II 20210G>A mutation each contribute to an increased risk of hereditary thrombophilia. Approximately 10% of factor V (Leiden) heterozygotes also carry the prothrombin 20210G>A mutation. Likewise, protein C and/or S deficiency have been reported with factor V (Leiden) mutation. Since venous thrombosis is a multifactorial disorder, presence of a second risk factor further increases the thrombotic risk. Thyroglobulin Antibodies (Atg) 267 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 7 days Reject Criteria Gross hemolysis • Hyperlipemic MethodologyChemiluminescene Clinical Significance Measurement of thyroglobulin antibodies is useful in the diagnosis and management of a variety of thyroid disorders including Hashimoto’s thyroiditis, Graves Disease and certain types of goiter Thyroglobulin Panel 30278 Includes Thyroglobulin, Thyroglobulin Antibodies Preferred Specimen(s) 2 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated, stable 7 day’s Reject Criteria Gross hemolysis • Hyperlipemia MethodologyChemiluminescene Clinical Significance Thyroglobulin (TG) is a secretory product only of the thyroid gland. The major clinical use of serum TG measurement is to monitor, but not to diagnose, patients with well-differentiated thyroid cancers. The measurement of thyroglobulin, after thyroidectomy and ablation of the thyroid gland, is useful to determine metastasis. Deficient TG synthesis is observed in infants with goitrous hypo-thyroidism. Most patients with thyroid autoimmune disease have thyroglobulin antibody. The antiperoxidase antibody (anti-tpo) provides additional specificity. Approximately 95% of patients with diffuse goiter, hypothyroidism, or both have anti-tpo. Anti-tpo is especially useful with patients with subclinical hypothyroidism (elevated TSH and normal free T4 concentrations). Many of these patients will develop hypothyroidism. With immunometric assays (sandwich assays), TGAB interference typically produces inappropriately low TG results, most likely caused by endogenous TG immune complexes that block one or more of the reagent antibodies from binding endogenous TG. Thyroglobulin (Tg) 15561 Preferred Specimen(s) 1.0 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated 3 days Reject Criteria Gross hemolysis • Hyperlipemic MethodologyCLIA Clinical Significance Thyroglobulin (Tg) is a secretory product only of the thyroid gland. The major clinical use of serum Tg measurement is to monitor, but not to diagnose, patients with well-differentiated thyroid cancers. The measurement of thyroglobulin, after thyroidectomy and ablation of the thyroid gland, is useful to determine metastasis. Deficient Tg synthesis is observed in infants with goitrous hypothyroidism. 141 S T Thyroid Hormone Panel 2 4776 Includes T3 (Triiodothyronine), T4 (Thyroxine) and TSH (Thyroid Stimulating Hormone) Preferred Specimen(s) 1 mL serum Transport Container Sterile plastic screw-cap vial Transport Temperature Ambient 4 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Gross lipemia MethodologyChemiluminescence Clinical Significance • The degree of suppression of TSH does not always reflect the severity of the hyperthyroidism. Therefore a measurement of free thyroid hormone levels is usually required in patients with a suppressed TSH level. TSH level mild to modest decreases in patients with normal T4 and T3 levels indicates sub-clinical hyperthyroidism. • Free T4 assays generally are considered to provide the more reliable indication of true thyroid status because only the free hormone is physiologically active. In developing hypothyroidism, T4 (Free T4) is the more sensitive indicator of developing disease and is therefore preferred for confirming hypothyroidism that has already been suggested by an elevated TSH result. • The T3 is increased in almost all cases of hyperthyroidism and goes up before the T4 is elevated. Thus T3 levels are more sensitive indicator of hyperthyroidism than the total T4. T3 levels are therefore preferred for confirming hyperthyroidism that has already been suggested by a suppressed TSH Levels. • The Total T3 and T4 hormone concentration is dependent on the concentrations of thyroid binding proteins like Thyroid Binding Globulin (TBG), albumin and Thyroid Binding pre- albumin (transthyretin). Thus, any conditions that affects the levels of thyroid binding proteins will effect these hormone levels. Thyroid Hormone Panel 3 S T 35454 Includes FT3, FT4, and TSH (Thyroid Stimulating Hormone) Preferred Specimen(s) 1 mL serum Transport Container Sterile plastic screw-cap vial Transport Temperature Ambient 4 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Hyperlipemia MethodologyChemiluminescence Clinical Significance • The degree of suppression of TSH does not always reflect the severity of the hyperthyroidism. Therefore a measurement of free thyroid hormone levels is usually required in patients with a suppressed TSH level. TSH level mild to modest decreases in patients with normal T4 and T3 levels indicates sub-clinical hyperthyroidism. • Free T4 assays generally are considered to provide the more reliable indication of true thyroid status because only the free hormone is physiologically active. In developing hypothyroidism, T4 (Free T4) is the more sensitive indicator of developing disease and is therefore preferred for confirming hypothyroidism that has already been suggested by an elevated TSH result. • The T3 is increased in almost all cases of hyperthyroidism and goes up before the T4 is elevated. Thus T3 levels are more sensitive indicator of hyperthyroidism than the total T4. T3 levels are therefore preferred for confirming hyperthyroidism that has already been suggested by a suppressed TSH Levels. • The Total T3 and T4 hormone concentration is dependent on the concentrations of thyroid binding proteins like Thyroid Binding Globulin (TBG), albumin and Thyroid Binding prealbumin (transthyretin). Thus, any conditions that affects the levels of thyroid binding proteins will effect these hormone levels. Thyroid Receptor Antibody See “TSI (Thyroid Stimulating Immunoglobulin)” Thyroid Stimulating Immunoglobulin See “TSI (Thyroid Stimulating Immunoglobulin)” 142 Thyrotropin See “TSH, Ultrasensitive“ Tissue Biopsy, Small Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 79016 *Endometrium *Cervical biopsy *Endoscopic biopsies *Trucut biopsies *Appendix *Conjunctival biopsy *Small diagnostic / incision biopsies, Tubal ligation/vas deferens (Lumps less than one cm will be included in this category) Send specimens only in 10% Neutral Buffered Formaldehyde (NBF) with formalin as health hazard label sign on container. Screw cap and spill proof container Room temperature Autolysed tissue Gross and Microscopic examination Tissue Biopsy, Medium 79017 Preferred Specimen(s) *Breast lump *Pilonidal sinus *Fistula/Sinus *Lymph Node *Ovarian Cyst *Eyeball (Non tumorous) *Gall bladder *Prostate (TURP) / Enucleation * Superficial lumps (more than one cm, less than 05 cm) *Brain & Spinal cord tumors *Small excision biopsies (lass than 5 cm) *Uterus with cervix without tubes/ovaries/Fibroids *Fibroids only *Products of conception, Liver biopsy (core), Renal biopsy(core), Skin biopsy, Bone biopsy (small) (For bone biopsy, please send preoperative radiograph. For liver and kidney core biopsy, please provide necessary clinical and laboratory parameters. For skin biopsy, preliminary clinical diagnosis/differential diagnosis should be provided with relevant clinical details. Uterus without tubes/ovary/fibroids will be included in this category.) Instructions Send specimens only in 10% Neutral Buffered Formaldehyde (NBF) with formalin as health hazard label sign on container. Transport Container Screw cap and spill proof container Transport Temperature Room temperature Reject Criteria Autolysed tissue Methodology Gross and Microscopic examination Tissue Biopsy, Large Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 79038 *Uterus with cervix & tubes/ovaries/Fibroids *Ovarian tumors/Large cysts (more than 5 cm) *Eyeball (tumorous) *Non tumorous conditions of Thyroid gland/Testes/ Kidney - Nephrectomy for nontumor conditions. Intestinal resection(segmental) *Lymph Node (Block dissection) *Large bone biopsy(>5 cm) (Please send preoperative radiographs for bone biopsy. Uterus with tubes/ovaries/fibroids are included in this category) Send specimens only in 10% Neutral Buffered Formaldehyde (NBF) with formalin as health hazard label sign on container. Screw cap and spill proof container Room temperature Autolysed tissue Gross and Microscopic examination Tissue Biopsy (Complex/Resection) Preferred Specimen(s) Instructions Transport Container Transport Temperature 79040 *Esophagectomy *Gastrectomy *Mastectomy *Hemi/Total colectomy *Large Bone Resection *Ovarian Tumor Resection. *Radical Nephrectomy for Cancer *Radical Neck Dissection *Radical Hysterectomy *Radical Orchidectomy *Soft Tissue Tumor Resections *Head & Neck Resection (This category includes cancer resection specimens.) Send specimens only in 10% Neutral Buffered Formaldehyde (NBF) with formalin as health hazard label sign on container. Screw cap and spill proof container Room temperature 143 S T Reject Criteria Methodology Autolysed tissue Gross and Microscopic examination Tissue Transglutaminase (tTG) Antibody (IgG) 11070 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) MethodologyELISA Clinical Significance Tissue Transglutaminase Antibody, IgG, test is useful in patients who are IgA-deficient. The IgG test also provides support for gluten-sensitive enteropathies beyond IgA the test. Tissue Transglutaminase (tTG) Antibodies (IgG, IgA) 11073 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) MethodologyELISA Clinical Significance Tissue Transglutaminase Antibody, IgA, is useful in diagnosing gluten-sensitive enteropathies, such as Celiac Sprue Disease, and an associated skin condition, dermatitis herpetiformis. The IgG test is useful in patients who are IgA-deficient. The IgG test also provides support for gluten-sensitive enteropathies beyond IgA the test. Tissue Transglutaminase (tTG) Antibody (IgA) 8821 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) MethodologyELISA Clinical Significance Tissue Transglutaminase Antibody, IgA, is useful in diagnosing gluten-sensitive enteropathies, such as Celiac Sprue Disease, and an associated skin condition, dermatitis herpetiformis. ToRCH 10 IgG/IgM (Toxoplasma IgG & IgM, Rubella IgG & IgM, CMV IgG & IgM and HSV IgG & IgM) Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance HSV 1 IgG, IgM; CMV IgG, IgM; Rubella IgG, IgM; Toxoplasma IgG, IgM 2.0 mL serum Plastic screw-cap vial Refrigerated 3 days (48 hrs for HSV1 IgG/IgM, 4 days HSV2 IgG/IgM) Gross hemolysis • Hyperlipemic CLIA (ELISA for HSV1 IgG/IgM & HSV2 IgG/IgM) See individual tests for clinical significance ToRCH 5 IgG (Toxoplasma IgG, Rubella IgG, CMV IgG, HSV1 IgG and HSV2 IgG) S T Includes Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 79531 79530 HSV 1 & 2 IgG; CMV IgG; Rubella IgG; Toxoplasma IgG 2.0 mL serum Plastic screw-cap vial Refrigerated 3 days (48 hrs for HSV1 IgG/IgM, 4 days HSV2 IgG/IgM) Gross hemolysis • Hyperlipemic CLIA (ELISA for HSV1 IgG/IgM & HSV2 IgG/IgM) See individual tests for clinical significance ToRCH 5 IgM (Toxoplasma IgM, Rubella IgM, CMV IgM, HSV1 IgM and HSV2 IgM) 79529 Preferred Specimen(s) Transport Container 144 2.0 mL serum Plastic screw-cap vial Transport Temperature Reject Criteria Methodology Clinical Significance Refrigerated 3 days (48 hrs for HSV1 IgG/IgM, 4 days HSV2 IgG/IgM) Gross hemolysis • Hyperlipemic CLIA (ELISA for HSV1 IgG/IgM & HSV2 IgG/IgM) See individual tests for clinical significance Total Protein and Albumin Panel 7577 Includes Total Protein; Albumin; Globulin; A/G Ratio Preferred Specimen(s) 2.0 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated 14 days Reject Criteria Gross hemolysis • Hyperlipemic MethodologySpectrophotometry Clinical Significance See individual test for Clinical Significance Toxoplasma Antibody (IgG, IgM) 79532 Preferred Specimen(s) 1 mL serum Instructions Allow specimen to clot at room temperature and then centrifuge. Immediately separate from cells and refrigerate at 2-8°C. If not tested within 1 week, store frozen at -20°C. Avoid freezing and thawing. Transport Container No additive (red-top) tube Transport Temperature Refrigerated 14 days Reject Criteria Received at room temperature; Received frozen MethodologyELISA Clinical Significance Toxoplasmosis is caused by infection by the parasite Toxoplasma gondii. Approximately 23% of the population carry the parasite but remain healthy while not immunocompromised. Transmission from a pregnant woman to her fetus can cause serious disease. A high Antibody IgG and Antibody IgM together support infection within the previously three months. A high Antibody IgG with a low-to-medium Antibody IgM together support infection within three to six months. Toxoplasma Gondii Antibody (IgG) 79911 Preferred Specimen(s) 1 mL serum Transport Container Plastic leak proof container Transport Temperature Refrigerated 3 days Reject Criteria Gross hemolysis • Hyperlipemia MethodologyCLIA Clinical Significance Toxoplasmosis is a parasitic infection caused by the protozoan Toxoplasma gondii. Approximately 23% of the immunocompetent population are asymptomatic carriers of the parasite. High titers of IgG antibodies to Toxoplasma gondii can persist for years. Rising IgG titers after birth, in the absence of a placental leak, are consistent with neonatal infection. Toxoplasma Gondii Antibody (IgM) 79913 Preferred Specimen(s) 1 mL serum Transport Container Plastic leak proof container Transport Temperature Refrigerated 3 days Reject Criteria Gross hemolysis • Hyperlipemia MethodologyCLIA Clinical Significance Toxoplasmosis is a parasitic infection of humans caused by the protozoan toxoplasma gondii. In acute infections in immunocompetent hosts, only 10-20% of toxoplasma infections are symptomatic and usually present as asymptomatic cervical lymphadenopathy. The clinical picture may resemble infectious mononucleosis or CMV infection and the course is selflimited. Acute toxoplasmosis in immunodeficient hosts is the most common cause of intracerebral mass lesions. Serologic tests rarely confirm the diagnosis of toxoplasmic encephalitis in AIDS patients. Although a negative test result for specific IgG antibody diminishes the likelihood of toxoplasmic encephalitis, approximately 3% of patients with toxoplasmic encephalitis do not have toxoplasma antibody in their serum. 145 S T Transferrin Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 891 1 mL serum Plastic screw-cap vial Refrigerated 14 days Gross hemolysis • Hyperlipemic • Plasma Nephelometry Transferrin concentration reflects the total iron-binding capacity (TIBC) and is used as an indicator of iron metabolism Triglycerides Patient Preparation Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 896 Fasting specimen required 1 mL serum Plastic screw-cap vial Room temperature, stable for 5 day’s Gross hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Serum triglyceride analysis has proven useful in the diagnosis and treatment of patients with diabetes mellitus, nephrosis, liver obstruction, other diseases involving lipid metabolism, and various endocrine disorders. In conjunction with high density lipoprotein and total serum cholesterol, a triglyceride determination provides valuable information for the assessment of coronary heart disease risk. Typhoid IgG/IgM, Rapid Test Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance Trypsin S T 79882 Serum: Collect blood specimen into collection tube(containing no anticoagulants in vacutainer®) by veinpuncture. Plasma: Collect blood specimen into a blue or green top collection tube (EDTA, citrate or heparin, respectively in vacutainer®) by veinpuncture. Red Top for serum; Lavender, blue or green Top for Plasma. Refrigerated 5 days Heat inactivated samples; Specimens which are grossly hemolyzed, lipemic or icteric; Microbial contaminated serum Rapid Test OnSite Typhoid IgG/IgM Rapid test is a simple and rapid laboratory test. The test simultane ously detects and differentiates the IgG and IgM antibodies to S.typhi specific antigen thus to aid in the determination of current or previous exposure to the S.typhi. 30329 Preferred Specimen(s) 1 mL serum collected in a (red-top) tube (no gel) Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) MethodologyRadioimmunoassay Clinical Significance Trypsin (or trypsinogen) is considered a specific indicator of pancreatic damage. Increased values over the determined normal range may indicate inflammatory pancreatic condition. TSH, Ultrasensitive 899 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 4 days, Refrigerated 30 days MethodologyChemiluminescence Clinical Significance For differential diagnosis of primary, secondary, and tertiary hypothyroidism. This assay is a third generation product capable of detecting values as low as 0.01 mIU/L. Also useful in screening for hyperthyroidism. This assay allows adjustment of exogenous thyroxine dosage in hypothyroid patients and in patients on suppressive thyroxine therapy for thyroid neoplasia. 146 TSI (Thyroid Stimulating Immunoglobulin) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 1 mL serum (red-top) tube Plastic screw-cap vial Refrigerated (cold packs) Gross hemolysis • Hyperlipemia • Collected in a sodium heparin (green-top) tube In vitro Bioassay/Luminescence Graves Disease is a classic form of hyperthyroid disease, affecting approximately 0.4% of the population in the United States. It is caused by IgG immunoglobulins, collectively known as thyroid stimulating immunoglobulins (TSI). Patients who are candidates for antithyroid drug therapy may not respond to this treatment when TSI levels are markedly elevated. The determination of TSI can also assist in predicting hyperthyroidism in neonates due to placental transmission of the immunoglobulins from a mother with hyperthyroidism. UGT1A1 Gene Polymorphism (TA Repeat) Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 30551 17813 5 mL whole blood collected in an EDTA (lavender-top) tube Record the draw time and date on the tube. Ship immediately to maintain sample stability. EDTA (lavender-top) Room temperature Gross hemolysis • Lipemia • Clotted blood received frozen Fluorescent Polymerase Chain Reaction This assay is intended for selection of colorectal cancer patients who would benefit most and experience the least toxicity from 5-FU, oxalipatin and irinotecan chemotherapy by determining the individual patient genotypes to guide chemotherapy choices in advanced stage colorectal cancer UPEP See “Protein Electrophoresis, 24-Hour Urine (UPEP)” Urea Nitrogen (BUN) Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 294 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 2 weeks Frozen, stable 28 day’s Hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Urea is the principle waste product of protein catabolism. BUN is most commonly measured in the diagnosis and treatment of certain renal and metabolic diseases. Increased BUN concentration may result from increased production of urea due to (1) diet or excessive destruction of cellular proteins as occurs in massive infection and fevers, (2) reduced renal perfusion resulting from dehydration or heart failure, (3) nearly all types of kidney disease, and (4) mechanical obstruction to urine excretion such as is caused by stones, tumors, infection, or stricture. Decreased urea levels are less frequent and occur primarily in advanced liver disease and in overhydration. Urea Nitrogen, 24-Hour Urine 973 Preferred Specimen(s) 10 mL urine Transport Container 24-hour urine container Instructions Refrigerate during and after collection. Record the 24 hour-urine volume, on the test requisition form, as well as on the urine vial. Collect 24-hour urine in the presence of 10 grams boric acid. Transport Temperature Refrigerated, stable 1 week Reject Criteria Received at room temperature; Received frozen MethodologySpecterophotometry 147 U V Clinical Significance Urea is the principle waste product of protein catabolism. Urea nitrogen is most commonly measured in the diagnosis and treatment of certain renal and metabolic diseases. Increased urea nitrogen concentration may result from increased production of urea due to (1) diet or excessive destruction of cellular proteins as occurs in massive infection and fevers, (2) reduced renal perfusion resulting from dehydration or heart failure, (3) nearly all types of kidney disease, and (4) mechanical obstruction to urine excretion such as is caused by stones, tumors, infection, or stricture. Decreased urea levels are less frequent and occur primarily in advanced liver disease and in overhydration. Urea Nitrogen, Random Urine Preferred Specimen(s) Transport Container Transport Temperature Methodology Clinical Significance 10 mL Random urine with out preservative Plastic leak proof container Refrigerated, stable 1 week Spectrophotometry (SP) Urea is the principle waste product of protein catabolism. Urine Nitrogen is most commonly measured in the diagnosis and treatment of certain renal and metabolic diseases. Uric Acid Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 78007 905 1 mL serum Plastic screw-cap vial Ambient 5 days, Refrigerated 14 days Gross hemolysis • Anticoagulants other than heparin Spectrophotometry (SP) Serum uric acid measurements are useful in the diagnosis and treatment of numerous renal and metabolic disorders, including renal failure, gout, leukemia, psoriasis, starvation or other wasting conditions, and in patients receiving cytotoxic drugs. Uric Acid , 24-Hour Urine 907 Includes Creatinine, 24-Hour Urine Preferred Specimen(s) 10 mL urine Instructions Collect urine without preservative. Do not acidify the specimen. Do not include first morning specimen; collect all subsequent voidings. The last sample collected should be the first morning specimen voided the following morning at the same time as the previous morning’s first voiding. Record 24-hour urine volume on test request form and urine vial. Please submit a 10mL aliquot of a 24-hour condition and aliquot unpreserved specimen prior to addition of any acid. Transport Container Plastic screw-cap container Transport Temperature Refrigerated 7 days Refrigerated, stable 1 week Reject Criteria Received frozen • Urine Received with preservative MethodologySpectrophotometry Clinical Significance Urine uric acid may supplement serum uric acid testing when trying to identify conditions in which there is alteration of uric acid production or excretion, e.g., gout, leukemia, renal disease. The amount of uric acid excreted may be useful in treating asymptomatic hyperuricemia. Measurement of urine uric acid is important in the investigation of urolithiasis. Uric Acid, Random Urine U V Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology 148 10 mL Random urine with out preservative Plastic leak proof container Refrigerated 7 days Refrigerated, stable 1 week Received frozen • Urine Received with preservative Spectrophotometry (SP) 14580 Clinical Significance Urine uric acid may supplement serum uric acid testing when trying to identify conditions in which there is alteration of uric acid production or excretion, e.g., gout, leukemia, renal disease. The amount of uric acid excreted may be useful in treating asymptomatic hyperuricemia. Measurement of urine uric acid is important in the investigation of urolithiasis. Urinalysis, Complete Includes Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Clinical Significance 5463 Macroscopic and Microscopic Examinations 10 mL urine - Urinalysis transport tube (yellow-top, blue fill line, preservative tube) Encourage clean catch mid stream samples to minimize contamination and improve accuracy. Label the sample appropriately and store at room temperature until pickup. Note: The Yellow-top, blue line tube cannot be used for collection and transport of specimens for urine culture. ***This order code does not include a reflex to culture*** If culture is being ordered separately, submit separate specimen (10 mL urine gray-top tube). Yellow-top, blue fill line urinalysis transport tube untreserved - Room temperature, 24 hours preserved: Refrigerated, 72 hours Pediatric Unpreserved: Refrigerated (cold packs) Unpreserved specimen (adults) received after 72 hours Reagent Impregnated Strips/Tablets/Microscopic Examination Dipstick urinalysis is important in accessing the chemical constituents in the urine and the relationship to various disease states. Microscopic examination helps to detect the presence of abnormal urine cells and formed elements. Urine, Routine Culture See “Culture, Urine, Routine” UroVysion™ See “Vaginosis/Vaginitis Panel” See “FISH, Vysis® UroVysion™, Bladder Cancer” Valproic Acid, Total 79071 Preferred Specimen(s) 2.0 mL Serum Instruction Record total volume and collection time on specimen, container and requisition. Transport Container Plastic Screw cap vial Transport Temperature Ambient 8 hrs, Refrigerated 2 days MethodologyImmunoassay Clinical Significance Valproic acid is used as an anticonvulsant to treat certain types of seizures, to prevent migrane head aches, and to treat various psychiatric illnesses suchas bipolar disorder and aggression. Therapeutic drug monitoring is useful to optimize dose and avoid VIP See “Vasoactive Intestinal Polypeptide (VIP)” Vitamin B12 927 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Ambient 5 days, Refrigerated (cold packs) 8 days Reject CriteriaHemolysis MethodologyChemiluminescence Clinical Significance Vitamin B12 is decreased in pernicious anemia, total or partial gastrectomy, malabsorption and certain congenital and biochemical disorders. Its deficiency causes neurological disturbances and increases the serum level of homocysteine which is a cardiovascular risk factor. 149 U V Vitamin B12 and Folate Panel, Serum 7065 Preferred Specimen(s) 2 mL serum Instructions Folate is light sensitive. Minimize exposure to light during sample handling and storage. Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) 5 days Reject CriteriaHemolysis MethodologyChemiluminescence Clinical Significance Folic acid deficiency is common in pregnant women, alcoholics, patients with diets that do not include raw fruits and vegetables, and people with structural damage to the small intestine. The most reliable and direct method of diagnosing folate deficiency is the determination of folate levels in both erythrocytes and serum. Low folic acid levels, however, can also be the result of a primary vitamin B12 deficiency that decreases the ability of cells to take up folic acid. B12 is decreased in pernicious anemia, total or partial gastrectomy, malabsorption and certain congenital biochemical disorders. Vitamin D, 1,25-dihydoxy 79280 Preferred Specimen(s) 3 mL serum Instructions The preferred specimen transport temperature is frozen. Room temperature and refrigerated transportation Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature MethodologyELISA Clinical Significance Vitamin D originating from dietary and endogenous sources is converted to 25-hydroxy vitamin D in the liver, and subsequently to 1-, 25-dihydroxyvitamin D in the kidney. Deficiencies of 1-,25-dihydroxyvitamin D, the most active form, cause hypocalcemia, osteomalacia, and related disorders. Measurement is useful in: differentiating primary hyperparathyroidism from hypercalcemia of cancer; distinguishing between vitamin D dependent and vitamin D resistant rickets; monitoring vitamin D status of patients with chronic renal disease; and, assessing compliance to therapy. Vitamin D, 25-Hydroxy, CLIA 78917 Includes D2, D3 and Total Vitamin D, 25-Hydroxy Preferred Specimen(s) 1 mL serum Instructions Collect blood by venipuncture into plain tubes (without anticoagulant). Separate the serum from the cells immediately. Transport Container Plastic screw-cap vial Transport Temperature Frozen; 2-8oC Reject Criteria Gross hemolysis • Gross lipemia • Plasma MethodologyCLIA Clinical Significance This assay should be used to monitor patients taking vitamin D supplements as well as to diagnose Vitamin D deficiency. The measurement of 25-OH Vitamin D is the best indicator of Vitamin D status in the body. This assay employs chemiluminescence and measures the total of 25-OH D2 (the analog form used to treat 25-OH D3 deficiency ) and 25-OH D3( the endogenous form of the vitamin). Vysis® UroVysion™ U V See “FISH, Vysis® UroVysion™, Bladder Cancer” 150 Widal Test (Tube Method) 17323 Preferred Specimen(s) 3ml serum Instructions Separate serum from cells as soon as possible Transport Container No additive (red-top) tube Transport Temperature Refrigerated, 48 hours Reject Criteria Received frozen; Room temperature Methodology Tube Method Clinical Significance The Widal test is a presumptive serological test for Enteric fever or Undulant fever that may be caused by Salmonella infections (S. typhi, S. paratyphi A & B). The most important causative factor in India is S. typhi. The antibodies are tested against two types of antigens, the protein H (flagellar) and the polysaccharide O (somatic) antigen. The H antigen is a protein and more antigenic and hence gives higher antibody titers. The H antigen is however relatively nonspecific due to due to shared antigens amongst entero-bacteriaceae. The O polysaccharide antigen gives lower titers and is more specific. A two fold rise in titer is diagnostic of typhoid fever. A single reading of titer more than 240 is also considered as diagnostic. Widal Slide test (Rapid) 79323 Preferred Specimen(s) 3ml serum Instructions Separate serum from cells as soon as possible Transport Container No additive (red-top) tube Transport Temperature Refrigerated 48 hours Reject Criteria Received frozen; Room temperature Methodology Agglutination on slide Clinical Significance The Widal test is a presumptive serological test for Enteric fever or Undulant fever that may be caused by Salmonella infections (S. typhi, S. paratyphi A & B). The most important causative factor in India is S. typhi. The antibodies are tested against two types of antigens, the protein H (flagellar) and the polysaccharide O (somatic) antigen. The H antigen is a protein and more antigenic and hence gives higher antibody titers. The H antigen is however relatively nonspecific due to due to shared antigens amongst entero-bacteriaceae. The O polysaccharide antigen gives lower titers and is more specific. A two fold rise in titer is diagnostic of typhoid fever. A single reading of titer more than 240 is also considered as diagnostic. W Z 151 152 Tests Performed in US Lab 153 154 Acetylcholine Receptor Binding Antibody 206 Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Limitations 1mL serum Plastic screw-cap vial Room temperature Hemolysis • Lipemia • Contaminated specimens • Icteric specimens • Radioactive compounds from in vivo testing • Plasma Radioimmunoassay (RIA) Antibodies may not be found in congenital myasthenia. Reference Range(s) Negative <0.30 nmol/L Equivocal 0.31-0.49 nmol/L Positive >0.50 nmol/L Acetylcholine Receptor Blocking Antibody 34459 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature MethodologyImmunoassay Limitations Antibodies may not be found in congenital myasthenia ACTH, Plasma 211 Patient Preparation Collect specimen between 7 A.M. and 10 A.M. If drawn at any other time, the reference ranges do not apply. Preferred Specimen(s) 1.5 mL plasma collected in an EDTA (lavender-top) tube Instructions Centrifuge immediately after collection to separate plasma from cells. Transfer plasma to a plastic specimen transport container and mark the specimen type as plasma on the container. Freeze immediately. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received thawed • Gross hemolysis MethodologyImmunoassay Limitations With patients receiving more than 5mg/day of biotin, a sample should be taken no sooner than eight hours after previous dose. Patients treated with monoclonal mouse antibodies may have inaccurate results. High titer of antibodies such as streptavidin and ruthenium may cause interference. Due to its correlation with cortisol levels, ACTH concentration is affected by stress. Any single measure may be within the reference range for patients with increased production (Cushing’s disease) or minimal production of ACTH. Reference Range(s) <3 Years Not established 3-17 Years 9-57 pg/mL >18 Years male 7-50 pg/mL >18 Years female 5-27 pg/mL ACTIN (Smooth Muscle) Antibody (IgG) 15043 Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology 0.5mL serum Plastic screw-cap vial Refrigerated (cold packs) Gross hemolysis • Lipemia • Received room temperature • Microbially contaminated serum • Specimens containing heavy, visible particulate Enzyme Linked Immunosorbent Immunoassay (ELISA) Reference Range(s) <20 U Negative 20-30 U Weak positive >30 U High positive 155 A B A B This ELISA assay is based on purified F-Actin IgG antibodies. IgG antibodies to F-Actin are present in approximately 75% of patients with autoimmune hepatitis type 1, 65% with autoimmune cholangitis, 30% with p rimary biliary cirrhosis, and 2% of the healthy population. Activated Protein C-Resistance 22 Preferred Specimen(s) 2 mL plasma collected in a 3.2% sodium citrate (light blue-top) tube Transport Temperature Frozen Reject Criteria Hemolysis • Thawed Plasma • Received room temperature • Received refrigerated • Clotted specimen • Serum Methodology RVVT Based Clot Assay Clinical Significance To screen for APC-R associated with venous thromboembolic disorders Aldosterone, Serum LC/MS/MS 17181 Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Limitations 1mL serum collected in a red-top tube (no gel) Separate serum after clotting. Do not submit glass tubes. Draw “upright” samples at least 1/2 hour after patient sits up. Plastic screw-cap vial Room temperature Serum Separator Tube (SST‰) • Glass tubes Liquid Chromatography/Tandem Mass Spectrometry (LC/MS/MS) Aldosterone concentration varies based on body position and sodium intake. 24-hour urine specimens for aldosterone are an alternative. Reference Range(s) Adult Pediatric Infants Tanner Stages Anti-Mullerian Hormone AssessR™ Upright 8:00-10:00 A.M. <28 ng/dL Upright 4:00-6:00 P.M. <21 ng/dL Supine 8:00-10:00 A.M. 3-16 ng/dL 1-12 Months 2-70 ng/dL 1-4 Years 2-37 ng/dL 5-9 Years <9 ng/dL 10-13 Years <21 ng/dL 14-17 Years <35 ng/dL Premature (31-35 Weeks) <144 ng/dL Term <217 ng/dL II-III Males 1-13 ng/dL II-III Females 2-20 ng/dL IV-V Males 3-14 ng/dL IV-V Females 4-32 ng/dL 16842 Preferred Specimen(s) 1 mL serum collected in a red-top tube (no gel) Collection Instructions Separate serum from clot and ship frozen. Frozen SST® tubes are not acceptable Transport TemperatureFrozen Reject Criteria Unspun Serum Separator Tube (SST®) Methodology Immunoassay (IA) Clinical Significance AMH/MIS may be used in the investigation of ovarian reserve and the perimenopausal transition in women; the detection and onset of puberty in the young, the differential diagnosis of intersex disorders; the diagnosis of cryptorchidism and anorchidism, and the evaluation of male gonadal function in all ages. 156 Antithrombin III Antigen 5158 Patient Preparation Patient should abstain from anabolic steroids, Gemfibrozil, Warfarin (Coumadin‰), heparin therapy, asparaginase, estrogens, gestodene and oral contraceptives optimally for 3 days prior to specimen collection. Overnight fasting is preferred. Preferred Specimen(s) 1mL frozen plasma collected in a 3.2% sodium citrate (light blue-top) tube See Coagulation in Specimen Collection and Handling Instructions Platelet-poor plasma: Centrifuge light blue-top tube for 15 minutes at approximately 1500g within 60 minutes of collection. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet buffy layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Plasma must be free of platelets (<10,000/uL). Freeze immediately and ship on dry ice. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received thawed • Received room temperature • Received refrigerated • Plasma collected in a 3.8% sodium citrate (light blue-top) tube Methodology Fixed Rate Time Nephelometry Limitations Falsely elevated results may be caused by heparin cofactor II. Reference Range(s) See Laboratory Report Aspergillus IgG, IgA, IgM, EIA (9941) Preferred Specimen(s) Specimen Container Transport Temperature Methodology 10239 1mL Serum Serum: Red-top (no gel) Serum: Refrigerated preferred; Room temperature acceptable; _Frozen acceptable Enzyme Immunoassay Aspergillus fumigatus (M3) IgE 60251 Preferred Specimen(s) 0.3mL serum Transport Temperature Room temperature Methodology Immunoassay BRAF Mutation Analysis Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Reference Range(s) 16767 Formalin-fixed paraffin embedded tissue Whole blood (acceptable): Collect 5 mL (minimum 4 mL) whole blood in an EDTA (lavender-top) tube. Formalin-fixed, paraffin embedded tissue block Room temperature Received frozen Direct Sequencing Negative Brucella Antibodies (IgG, IgM) 10566 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature MethodologyImmunoassay Limitations Previous vaccination may affect results C1 Inhibitor, Functional 297 Preferred Specimen(s) 1 mL serum collected in a red-top tube (no gel) Instructions Freeze serum within one hour of time drawn. Do not use gel barrier tubes. Do not submit the sample in a glass tube. Do not thaw. Transport Container Plastic screw-cap vial Transport TemperatureFrozen 157 A B Reject Criteria Gross hemolysis • Lipemia • Received thawed • Received room temperature • Received refrigerated • Serum Separator Tube (SST‰) • Glass tubes • CSF MethodologyImmunoassay Limitations Fifteen percent of patient with the inherited form of the disease will test within range. Reference Range(s) C D >68 % Normal 41-67 % Equivocal <40 % Abnormal Less than 40% of the reference functional activity indicates a likely diagnosis of hereditary angioedema or acquired C1 inhibitor deficiency. C1 Inhibitor, Protein Patient Preparation Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Limitations Reference Range(s) 298 Overnight fasting is preferred 1mL serum Collect on ice. Chill in ice bath during clotting. Separate from clot with minimum centrifugation. Refrigerate serum immediately. Avoid hemolysis. Plastic screw-cap vial Refrigerated (cold packs) Received room temperature • Pleural fluid • Synovial fluid Fixed Rate Time Nephelometry Fifteen percent of patient with the inherited form of the disease will test within range. 11-26 mg/dL CA 27.29 29493 Preferred Specimen(s) 1 mL serum Transport Container Serum Separator Tube (SST‰) Transport Temperature Room temperature Reject Criteria Gross hemolysis MethodologyImmunoassay Limitations CA 27.29 is not intended as a screening test Calcitonin30742 Patient Preparation Overnight fasting is preferred Preferred Specimen(s) 1mL serum Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Received refrigerated • Gross hemolysis MethodologyImmunoassay Limitations Basal concentrations of >100 pg/mL have been found to have 100% positive predictive value for medullary thyroid cancer. Lower concentrations may be observed in some patients with clinically apparent medullary thyroid cancer. Catecholamines, Fractionated, 24-Hour Urine without Creatinine Patient Preparation Preferred Specimen(s) Instructions Transport Container Transport Temperature Methodology Limitations 158 318 It is preferable for the patient to be off medications for a minimum of 18-24 hours prior to collection however, common antihypertensives (diuretics, ACE inhibitors, calcium channel blockers, alpha and beta blockers) may cause minimal or no interference. Patient should avoid tobacco, tea, coffee, and strenuous exercise for 8-12 hours prior to collection. 10mL aliquot from a 24-hour collection preserved with 6N HCl at the start of collection. Unpreserved specimens must be frozen. See Urine in the Blood, Urine and Stool section of Specimen Collection and Handling Record total volume on both the transport container and the test requisition Plastic urine container Room temperature (if preserved) • Frozen acceptable (if unpreserved) High Performance Liquid Chromatography (HPLC) Recent surgery, traumatic injury, upright posture, cold, anxiety, pain, clonidine withdrawal, and concurrent acute or chronic illness may produce elevated results. Requires accurate 24-hour urine collection. Reference Range(s) Norepinephrine Epinephrine Dopamine Total Catecholamines 3-8 Years 5-41 ug/24 h 9-12 Years 5-50 ug/24 h 13-17 Years 12-88 ug/24 h >17 Years 15-100 ug/24 h 3-8 Years 1-7 ug/24 h 9-12 Years <8 ug/24 h 13-17 Years <11 ug/24 h >17 Years 2-24 ug/24 h 3-8 Years 80-378 ug/24 h 9-12 Years 51-474 ug/24 h 13-17 Years 51-645 ug/24 h >17 Years 52-480 ug/24 h 3-8 Years 9-51 ug/24 h 9-12 Years 9-71 ug/24 h 13-17 Years 13-90 ug/24 h >17 Years 26-121 ug/24 h Chromogranin A, Electrochemiluminescence Preferred Specimen(s) Specimen Container Transport Temperature Reject Criteria Methodology Clinical Significance C D 16379 0.8 mL serum Serum: SST (red-top) Room temperature Gross hemolysis • Gross lipemia • Gross icteria Electrochemiluminescence (ECLIA) Chromogranin A has been identified in a number of normal and neoplastic endocrine tissues. Collagen Type I C-Telopeptide (CTx) 17406 Patient Preparation Fasting is required. Fasting morning collection 8-10 A.M. (diurnal variations cause elevated levels at night). Preferred Specimen(s) 1 mL serum Instructions Allow blood to clot (10-15 minutes) at room temperature. Centrifuge and separate the serum from the cells. Freeze as soon as possible. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Moderate/gross hemolysis • Gross lipemia • Non-fasting specimens • Gross icteric Methodology Electrochemiluminescent Immunoassay Reference Range(s) Adult Male Adult Female Pediatric Male 18-29 Years 87-1200 pg/mL 30-39 Years 70-780 pg/mL 40-49 Years 60-700 pg/mL 50-68 Years 87-345 pg/mL 18-29 Years 60-640 pg/mL 30-39 Years 60-650 pg/mL 40-49 Years 40-465 pg/mL 5-9 Years 574-1849 pg/mL 10-13 Years 519-2415 pg/mL 14-17 Years 435-2924 pg/mL 159 Pediatric Female C D 5-9 Years 574-1849 pg/mL 10-13 Years 519-2415 pg/mL 14-17 Years 242-1291 pg/mL Cortisol, Free, LC/MS/MS, 24-Hour Urine 11280 Preferred Specimen(s) 2mL Urine Specimen ContainerUrine _24-hour urine container (preferred) _No preservative (preferred) _25 mL 6N HCl _10 mL conc. glacial acetic acid _10 g Boric acid Transport Temperature Urine: Refrigerated preferred; Room temperature _unacceptable; Frozen acceptable Methodology Liquid Chromatography, Tandem Mass Spectrometry (LC/MS/MS) Clinical Significance Urinary Free Cortisol is useful in the detection of patients with Cushing’s syndrome for whom Free Cortisol concentrations are elevated. Cryptococcus Antigen Screen with Reflex to Titer 11197 Preferred Specimen(s) 1 mL CSF or 2 mL serum Transport Container CSF: Sterile screw-cap vial Serum: Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Glass tubes MethodologyImmunoassay Limitations Patients with capnocytophagna canimorsus and tichosporon beigelli infections may test falsely-positive. Reference Range(s) Not detected Cytomegalovirus (CMV) DNA, Qualitative, Real Time - PCR 10601 Preferred Specimen(s) 1mL whole blood collected in an EDTA (lavender-top) tube or 1mL plasma collected in an EDTA (lavender-top) tube or serum, CSF, amniotic fluid, random urine or fresh (unfixed) tissue Instructions Whole blood: Collect whole blood in sterile tubes containing EDTA or ACD as anticoagulant. Store refrigerated. Do not freeze whole blood. Plasma: Collect blood in sterile tubes containing EDTA or ACD as anticoagulant or in Plasma Preparation Tubes (PPT). Store collected whole blood at room temperature and separate plasma from cells within 2 hours of collection. Transfer plasma to sterile, plastic, screw-capped tubes and store refrigerated or frozen. If blood is collected in a PPT tube, centrifuge within 2 hours of collection and store refrigerated or frozen. It is not necessary to transfer the plasma from a PPT tube to aliquot tubes. Serum, CSF, amniotic fluid, urine and tissue: Collect in a sterile container and store refrigerated or frozen. Transport Container See Instructions Transport Temperature Refrigerated (cold packs): Whole blood, plasma, amniotic fluid, CSF and serum Frozen: Tissue or random urine Reject Criteria Frozen whole blood • Heparin whole blood • Heparin plasma• Synovial fluid • Vitreous fluid • Eye swab • Lesion (vesicle) aspirate swab • Fluid • Bone marrow • Buffy coat • Sputum • Tissue biopsy • Nasopharyngeal lavage/wash • Tracheal lavage/wash • Nasal/nasopharyngeal swab • Pericardial fluid • Peritoneal fluid • Pleural fluid • 24 hour urine • Bronchial lavage/wash Methodology Real-Time Polymerase Chain Reaction (RT-PCR) Reference Range(s) Not detected 160 Dihydrotestosterone, LC/MS/MS Preferred Specimen(s) Alternative Specimen(s) Transport Temperature Reject Criteria Methodology Clinical Significance 90567 0.6 mL serum collected in a red-top (no gel) tube Plasma collected in an EDTA tube Room temperature Moderate hemolysis • Gross hemolysis • Lipemia • SST tubes Liquid Chromatography/Tandem Mass Spectrometry (LC/MS/MS) DHT is a potent androgen derived from testosterone via 5-alpha-reductase activity. 5-alpha-reductase deficiency results in incompletely virilized males (phenotypic females). This diagnosis is supported by an elevated ratio of testosterone to DHT. Epidermal Growth Factor Receptor (EGFR) Mutation Analysis Preferred Specimen(s) Transport Temperature Reject Criteria Methodology Clinical Significance Formalin fixed paraffin embedded tissue block Room temperature Thawed tissue • Fresh tissue • Non-fixed tissue Polymerase Chain Reaction (PCR) • Sequencing This test was developed and its performance characteristics have been determined by Quest Diagnostics. Performance characteristics refer to the analytical performance of the test. Quest Diagnostics will offer a DNA sequencing test to identify patients with those specific mutations in the TK domain of the EGFR gene (exons 18-21). With this information, physicians will be able to select those patients who are most likely to respond to targeted lung cancer therapy, including Iressa and Tarceva. Physicians can also use this information to predict drug resistance as identified by those patients who do not have those mutations. We may also be able to identify novel mutations, and may be able to provide this test for other EGFR targeted drugs emerging from pharmaceutical pipelines. EML4-ALK Gene Fusion, PCR Preferred Specimen(s) Specimen Container Transport Temperature Reject Criteria Methodology Clinical Significance 16344 Formalin fixed paraffin embedded tissue Formalin-fixed paraffin embedded tissue block Room temperature Frozen tissue blocks Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) Recently, inhibitors of anaplastic lymphoma kinase (ALK) have been used successfully in treating patients harboring gene fusions between echinoderm microtubule-associated protein-like 4 (EML4) and ALK. This is a reverse transcription PCR-based exon scanning approach to encompass fusion variants spanning nearly the entire EML4 gene. Endomysial Antibody Screen (IgA) with Reflex to Titer Preferred Specimen(s) Transport Container Transport Temperature Methodology Reference Range(s) 16460 15064 1mL serum Plastic screw-cap vial Refrigerated (cold packs) Immunofluorescence Assay (IFA) Negative Epstein-Barr Virus Viral Capsid Antigen (VCA) Antibody (IgG) 8474 Preferred Specimen(s) 1 mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature Reject Criteria Gross hemolysis • Gross lipemia • Icteric MethodologyImmunoassay Reference Range(s) Index Interpretation <0.90 Negative 0.91-1.09 Equivocal >1.10 Positive 161 E F Erythropoietin427 Preferred Specimen(s) 1 mL serum Transport Container Serum Separator Tube (SST‰) Transport Temperature Room temperature Reject Criteria Gross hemolysis MethodologyImmunoassay Reference Range(s) E F <3 Weeks Not established 3 Weeks-2 Months 5.0-13.0 mIU/mL 3 Months-16 Years 9.0-28.0 mIU/mL >16 Years 4.1-19.5 mIU/mL Estradiol, Ultrasensitive, LC/MS/MS 30289 Preferred Specimen(s) 0.5mL serum collected in a red-top tube (no gel) Instructions Specify age and sex on test requisition Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Serum Separator Tube (SST‰) Methodology Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS) Reference Range(s) Adult Male <29 pg/mL Female Follicular Stage 39-375 pg/mL Luteal Stage 48-440 pg/mL Postmenopausal <10 pg/mL Pediatric Male (pg/mL) Female (pg/mL) Pre-pubertal (1-9 Years) ≤4 ≤16 10-11 Years ≤12 ≤65 12-14 Years ≤24 ≤142 15-17 Years ≤31 ≤283 Estrogen, Total, Serum Preferred Specimen(s) Alternative Specimen(s) Transport Temperature Reject Criteria Methodology Clinical Significance 1mL serum Plasma collected in: Lithium heparin (green-top), sodium heparin (green-top), 3.2% sodium citrate (light blue-top), ACD solution B (yellow-top), potassium oxalate (gray-top), sodium fluoride (gray-top), PPT potassium EDTA (white-top), EDTA (lavender-top) or EDTA (royal blue-top) tube Refrigerated (cold packs) Received room temperature Extraction • Radioimmunoassay (RIA) Estrogens are secreted by the gonads, adrenal glands, and placenta. Total estrogens provide an overall picture of estrogen status for men and women. Factor IX Activity, Clotting Preferred Specimen(s) Instructions 162 439 352 3 mL platelet poor 3.2% sodium citrate-anticoagulated plasma (collected in light blue-top tube), separated and frozen immediately See Coagulation in Specimen Collection and Handling Draw blood in (light blue-top) tube containing 3.2% sodium citrate. Mix gently by inverting 3-4 times. Centrifuge 15 minutes at 2500-3500 rpm. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet buffy layer and transfer into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Plasma must be free of platelet (<10,000/uL). Freeze immediately and ship on dry ice. Transport Container Plastic screw - cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Received refrigerated • Received thawed • Hemolysis Methodology Photometric Clot Detection Limitations Factor IX inhibitors, including alloantibodies that develop post-replacement therapy and autoantibodies that develop spontaneously, can cause falsely low factor IX levels. Factor V (Leiden) Mutation Analysis Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Reference Range(s) 17900 5 mL whole blood collected in an EDTA (lavender-top) tube Plastic screw-cap vial Room temperature Received frozen Polymerase Chain Reaction (PCR) • Oligonucleotide Ligation Assay • Fluorescent Microspheres The Factor V Leiden (R506Q) mutation [NM 000130.2: c. 1601GA (p.R534Q)] in the Factor V gene is one of the most common causes of inherited thrombophilia. This mutation causes resistance to degradation of activated Factor V protein by Activated Protein C (APC). The Factor V Leiden (R506Q) mutation is detected by Polymerase Chain Reaction (PCR) amplification of the Factor V gene, followed by an Oligonucleotide Ligation Assay (OLA). The biotinylated reaction products are hybridized to microspheres and allelic discrimination is performed by identifying microspheres and measuring the associated reported fluorescence. Since genetic variation and other factors can affect the accuracy of direct mutation testing, these results should be interpreted in light of clinical and familial data. Fibrinogen Degradation Products (FDP), Semi Quantitative 458 Preferred Specimen(s) 1 mL platelet-poor anticoagulated plasma collected in a 3.2% sodium citrate (light blue-top) tube See Coagulation in Specimen Collection and Handling Instructions Draw blood in a 3.2% sodium citrate (light blue-top) tube, mix gently by inverting 3-4 times. Centrifuge 15 minutes at 2500-3500 RPM. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet (buffy) layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and transport on dry ice. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Hemolysis • Clotted Methodology Latex Agglutination Reference Range(s) <5 ug/mL FISH, ALK, 2p23 Rearrangement Preferred Specimen(s) Alternative Specimen(s) Transport Temperature Methodology Clinical Significance 3mL bone marrow collected in transport media or 5 mL whole blood collected in sodium heparin (green-top) tube Bone marrow collected in sodium heparin (green-top), royal blue-top), or lead-free (tan-top) tube • Whole blood collected in Sodium heparin (royal blue-top) or lead-free (tan-top) • 5 X 5 m Tumor tissue collected in transport media formalin fixed, paraffin embedded tissue block • 5 X 5 mm Lymph node collected in transport media formalin fixed, paraffin embedded tissue block Room temperature Fluorescence In-Situ Hybridization (FISH) The anaplastic large cell lymphoma specific chromosomal rearrangements of 2p23 can be proved by FISH. The patients carrying t (2; 5) or ALK fusion protein have been reported to have a good response to chemotherapy and favorable outcome. FISH, EGFR Preferred Specimen(s) Specimen Container Transport Temperature 16114 19041 Formalin fixed paraffin embedded tissue Formalin fixed paraffin embedded tissue block Room temperature 163 E F Methodology Clinical Significance Fluorescence In-Situ Hybridization (FISH) The epidermal growth factor receptor (EGFR) is a cellular transmembrane receptor with tyrosine kinase enzymatic activity that plays a key role in human cancer. EGFR-dependent signaling is involved in cancer cell proliferation, apoptosis, angiogenesis, invasion and metastasis. Targeting the EGFR is a valuable molecular approach in cancer therapy. Gastrin478 Patient Preparation Overnight fasting (12 hours) Preferred Specimen(s) 1mL frozen serum Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Gross hemolysis • Gross lipemia • Received thawed • Grossly icteric MethodologyImmunoassay Reference Range(s) G H <5 Years Not established 5-17 Years 13-64 pg/mL >17 Years <100 pg/mL Glomerular Basement Membrane Antibody (IgG) (GBM Antibody) 257 Preferred Specimen(s) 1mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature MethodologyImmunoassay Limitations Weakly positive results (5-30 EU/mL) may occur in patients who do not have antiglomerular basement membrane antibody-mediated disease. Reference Range(s) <1.0 AI Helicobacter pylori Antibody (IgM) Preferred Specimen(s) Transport Temperature Methodology Clinical Significance 51771 1 mL serum Room temperature Enzyme Immunoassay (EIA) Colonization with H. pylori is associated with increased risk of patients developing gastritis, peptic ulcer disease, and gastric adenocarcinoma. Serologic testing is recommended only for symptomatic patients. Antibody IgM may be not be elevated in many infected individuals. Hepatitis B Virus Drug Resistance, Genotype, and BCP/Precore Mutations 10529 Preferred Specimen(s) 1mL plasma collected in a PPT potassium EDTA (white-top) tube Instructions Plasma: Collect blood in sterile tubes containing EDTA anticoagulant; either 0.15% solution v/v final EDTA K3 (standard EDTA tube) or 9 mg spray-dried EDTA K2 (plasma preparation tube or PPT tube with plasma separator-gel, preferred). Store whole blood at room temperature and separate plasma from cells within 2 hours of collection. Transfer plasma to sterile, plastic, screw-cap vials and store at -18° C or colder. Serum: Collect blood in sterile tubes with no anticoagulants; plastic Serum Separator Tubes (SST‰s) are recommended. Allow blood to clot at room temperature and separate serum from cells within 2 hours of collection. Transfer serum to sterile, plastic screw-cap vials and store refrigerated or frozen. Ship frozen. If blood is collected in a PPT tube, centrifuge preferably within 2 hours of collection as before but it is not necessary to transfer plasma to aliquot tubes. Following centrifugation, a gel barrier maintains separation of plasma from cellular components during specimen transport and storage. The PPT is plastic and hence plasma can be stored and shipped frozen in the original tube. Avoid repeated freezing and thawing of specimen. Ship frozen. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Unspun PPT tube Methodology Polymerase Chain Reaction (PCR) • Sequencing 164 Limitations Reference Range(s) Results obtained from immunosuppressed patients should be interpreted with caution. See Laboratory Report Hepatitis C Viral RNA, Genotype, LiPA‰ 37811 Preferred Specimen(s) 2 mL plasma collected in a PPT potassium EDTA (white-top) tube Instructions Plasma (preferred): Collect blood in sterile tubes containing EDTA anticoagulant, either 0.15% solution v/v final EDTA K3 (standard EDTA tube) or 9 mg spray-dried EDTA K2 (Plasma Preparation Tube or PPT tube with plasma separator-gel, preferred). Blood collected in tubes containing ACD anticoagulant are acceptable but will yield results approximately 15% lower when compared to EDTA tubes due to the dilution effect of the 1.5 mL of anticoagulant used in the tube. Store whole blood at room temperature and separate plasma from cells within 6 hours of collection. Transfer plasma to sterile, plastic, screw-capped aliquot tubes and store at -18°C or colder. Do not clarify plasma by filtration or further centrifugation. Avoid repeated freezing and thawing of specimen. Note: If blood is collected in a PPT tube, centrifuge within 6 hours of collection as before, but it is not necessary to transfer the plasma to aliquot tubes. Following centrifugation, a gel barrier maintains separation of plasma from cellular components during specimen transport and storage, and unlike standard Vacutainer‰ Brand blood collection tubes, the PPT tube is plastic and hence the plasma can be shipped and stored frozen in the original tube. Serum (acceptable): Collect blood in sterile tubes with no anticoagulants; Serum Separator Tubes (SST‰s) are recommended. Allow blood to clot at room temperature and separate serum from cells within 6 hours of collection. Transfer serum to sterile, plastic screw-capped, aliquot tubes and store at -18°C or colder. Avoid repeated freezing and thawing of specimen. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Received room temperature • Unspun Serum Separator Tube (SST‰) • Unspun PPT tubes Methodology Multi-Probe Reverse Hybridization Reference Range(s) See Laboratory Report Hereditary Hemochromatosis, DNA, Mutation Analysis Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Limitations G H 35079 5 mL whole blood collected in an EDTA (lavender-top) tube EDTA (lavender-top) tube Room temperature Received frozen Polymerase Chain Reaction (PCR) • Fluorescent Restriction Fragment Length Polymorphism Expression of C282Y/C282Y homozygosity is variable. Some individuals who fail to meet the diagnostic criteria for hemochromatosis are homozygous for the gene. If these mutations are not found by the testing procedure, it does not mean that the risk of carrying or developing HH is not present. It simply means that these specific mutations have not been found, although other mutations may be present. It is also possible that such a patient may have secondary hemochromatosis, due to nongenetic causes, that would not be detected by this test. Herpes Simplex Virus, Type 1 and 2 DNA, Real-Time PCR 34257 Preferred Specimen(s) 1mL CSF in sterile leak-proof container only Instructions CSF: Collect in a sterile container and store refrigerated or frozen Swab: Submit in M4 or V-C-M transport medium Swab (dry or in transport media): Store refrigerated or frozen Serum: Collect blood in sterile tubes with no anticoagulants; Serum Separator Tubes (SST‰s) are recommended. Allow blood to clot at room temperature and separate serum from cells within 2 hours of collection. Transfer serum to sterile, plastic screw-capped aliquot tubes and store refrigerated or frozen. Plasma: EDTA (lavender-top) or ACD-B (yellow-top) tube Whole blood: EDTA (lavender-top) or ACD-B (yellow-top) tube Transport Container Sterile leak-proof container Transport Temperature Refrigerated (cold packs) Reject CriteriaSputum 165 Methodology Reference Range(s) Real-Time Polymerase Chain Reaction (RT-PCR) Not detected Hydroxyprogesterone, 17 Alpha, Serum 17180 Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 0.5 mL serum collected in a red-top tube (no gel) Separate serum after clotting. Ship serum refrigerated or frozen. Do not submit glass tubes. Plastic screw-cap vial Refrigerated (cold packs) Serum Separator Tube (SST‰) • Glass tubes • Received room temperature Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS) Reference Range(s) Adult Male G H Adult Female 18-30 Years 32-307 ng/dL 31-40 Years 42-196 ng/dL 41-50 Years 33-195 ng/dL 51-60 Years 37-129 ng/dL Follicular Phase <185 ng/d Luteal Phase <285 ng/dL Postmenopausal <45 ng/dL Pregnancy Pediatric Infant Tanner Stages First Trimester 78-457 ng/dL Second Trimester 90-357 ng/dL Third Trimester 144-578 ng/dL 1-12 Months 11-170 ng/dL 1-4 Years 4-115 ng/dL 5-9 Years <90 ng/dL 10-13 Years <169 ng/dL 14-17 Years 16-283 ng/dL Premature (31-35 Weeks) <360 ng/dL Term (3 Days) <420 ng/dL II-III Male 12-130 ng/dL II-III Female 18-220 ng/dL IV-V Male 51-190 ng/dL IV-V Female 36-200 ng/dL IgG Subclass 4 Preferred Specimen(s) Transport Temperature Methodology Clinical Significance 5428 1 mL serum Refrigerated (cold packs) Nephelometry Overnight fasting is preferred Inflammatory Bowel Disease Differentiation Panel 16503 Preferred Specimen(s) 2 mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature MethodologyImmunoassay Reference Range(s) 166 ANCA Screen Negative P-ANCA Titer <1:20 C-ANCA Titer <1:20 Atypical P-ANCA Titer <1:20 Myeloperoxidase Ab (MPO) <6 U/mL Negative 6-9 U/mL Equivocal >9 U/mL Positive <6 U/mL Negative 6-9 U/mL Equivocal >9 U/mL Positive <20 U Negative 20.1-29.9 U Equivocal >30 U Positive <20 U Negative 20.1-29.9 U Equivocal >25 U Positive Proteinase-3 Ab (PR3) Saccharomyces cerevisiae (IgG) Saccharomyces cerevisiae (IgA) IGF Binding Protein-3 (IGFBP-3) Preferred Specimen(s) Transport Temperature Reject Criteria Methodology Clinical Significance 34458 1 mL serum Room temperature Gross hemolysis • Gross lipemia • Plasma • Specimens out of stability Immunoassay (IA) Insulin-like growth factor binding proteins bind IGF-I and IGF-II with high affinity but do not bind insulin. Of the six distinct IGF binding proteins structurally characterized at this time, IGFBP-3 has been shown to be the major carrier of the IGFs, transporting approximately 95% of circulating IGF-I and IGF-II. IGFBP-3 is growth hormone (GH) responsive. Thus, levels are high in cromegaly and low in hypopituitarism, and levels increase in GH-deficient children after GH administration. Thus, both assays and the ratios of IGF-I/IGFBP-2 and IGFBP-2/IGFBP-3 are useful as markers of GH action and for discriminating between growth hormone deficiency and short stature due to other etiologies in children. Other causes of short stature that result in reduced IGFBP-3 levels include poorly controlled diabetes. The IGFBP-3 assay is useful in assessing nutritional status, since IGFBP-3 decreases during both caloric and protein restriction. Insulin like Growth Factor I (IGF-I) 16293 Preferred Specimen(s) 1mL serum Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Gross hemolysis • Gross Lipemia • Received room temperature • Frozen glass tubes • Slightly, moderate, and grossly icteric specimens MethodologyElectrochemiluminescence Reference Range(s) See Laboratory Report Ion Mobility Lipoprotein Fraction Patient Preparation Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology 16129 Fasting preferred 4.5 mL serum Note: Lab needs 3 tubes totaling 4.5 mL. Plastic screw-cap vial (x3) Refrigerated (cold packs) Gross hemolysis • Gross lipemia Colorimetric, Calculated, Ion Mobility, Immunoturbidimetry, Enzymatic 167 I J KRAS Mutation Analysis Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Reference Range(s) 16510 Formalin fixed, paraffin embedded tissue block For submission of paraffin block, tissue source, and block ID are required on the test requisition Formalin-fixed, paraffin embedded tissue block Room temperature Gross hemolysis • Clotted whole blood or bone marrow • Frozen whole blood or bone marrow Polymerase Chain Reaction (PCR) • Sequencing Negative Lactic Acid, Plasma 585 Patient Preparation Sample should be collected without the use of a tourniquet, avoid hand-clenching. If a tourniquet has been used, it should be released for one minute prior to drawing blood. Collected blood should be cooled on ice immediately and separated from the cells within 3 hours. Preferred Specimen(s) 2mL frozen plasma from a gray-top tube Instructions The collected blood should be well-mixed and separated from the cells within 3 hours Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Gross hemolysis • Specimens with visible icterus Methodology Spectrophotometry (SP) Reference Range(s) 4-16 mg/dL Lead, Blood K L 599 Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Whole blood in certified low-lead collection tube: • 3 mL venous whole blood in an EDTA (tan-top) tube or equivalent • 0.5 mL capillary whole blood in a capillary collection EDTA (lavender-top) tube or equivalent Note: 1. Not all EDTA collection tubes are certified as low lead content. 2. Submit separate collection tube if ordering another test, such as CBC. Blood collection tube Room temperature Serum • Plasma • Glass capillary, yellow-top, red-top, gray-top oxalate, and (light blue-top) citrate tubes • Clotted, viscous specimens Atomic Spectroscopy (AS) Reference Range(s) Birth-6 Years <5 ug/dL >6 Years <10 ug/dL Blood lead levels in the range of 5-9 ug/dL have been associated with adverse health effects in children aged 6 years and younger. For this age group, case management varies by CDC Blood Level range. Refer to current guidelines for recommended interventions. CDC ranges (ug/dL) <10 10-14 15-19 20-44 45-69 >69 Leptin Preferred Specimen(s) Transport Temperature Methodology Clinical Significance 168 90367 1 mL Serum Serum: Refrigerated preferred; Electrochemiluminescence (ECL) Leptin is an adipocyte-derived hormone that is essential for normal body weight regulation. Leptin production is under neuroendocrine control so that serum concentrations vary directly with the amount of triglycerides stored in adipose tissue depots. Levetiracetam (1514) Preferred Specimen(s) Alternative Specimen(s) Transport Temperature Methodology Clinical Significance 1mL serum collected in a red-top tube (no gel) Plasma collected in an EDTA (lavender-top), EDTA (royal blue-top) or sodium heparin (green-top) tube Room temperature Liquid Chromatography/Tandem Mass Spectrometry (LC/MS/MS) Levetiracetam is an anticonvulsant used as adjunct therapy to treat adult partial seizures. As multiple anticonvulsants are administered, it is important to monitor its level to (1) optimize therapy, (2) assure compliance, and (3) to avoid toxicity. Lithium, Serum Patient Preparation Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Reference Range(s) 15142 613 Collect just prior to next dose 2 mL serum Serum Separator Tube (SST‰) Room temperature Plasma from lithium-based anticoagulants • EDTA plasma Atomic Absorption Spectrometry (AAS) • Ion Selective Electrode (ISE) 0.5-1.3 mEq/L Maternal Serum Screen 5 (Penta Screen) 15934 Preferred Specimen(s) 4 mL serum Instructions For manual orders use ”Maternal Serum Screen Requisition”. The Penta Screen test in pregnant women should be performed between 14.0 and 22.9 weeks gestational age, although the optimal period is 15.0-16.9 weeks. This time frame allows sufficient opportunity for further diagnostic studies if the initial penta screen test results are abnormal. Specimens submitted before 14.0 weeks or after 22.9 weeks gestation cannot be properly evaluated for open Neural Tube Defects, Down Syndrome or Trisomy 18. The “Maternal Serum Screen Requisition”; designed to obtain patient data and the patient’s informed consent must be utilized when ordering the Penta Screen test. Because the Penta Screen test results are influenced by certain patient characteristics, the following data must be provided with the specimen in order to permit accurate interpretation of results: Date of collection, patient’s (maternal) date of birth, patient’s estimated date of delivery, patient’s weight, patient’s race, patient’s diabetic status (is patient insulin dependent prior to pregnancy), number of fetuses, and whether this is a repeat sample. Transport Container Plastic screw-cap vial Transport Temperature Refrigerated (cold packs) Reject Criteria Gross hemolysis • Lipemia • Received room temperature MethodologyImmunoassay Limitations Maternal age confirmation and number of fetuses may alter result interpretation. Maternal screening tests consistent with increased risk of trisomy should be confirmed with CVS or amniotic fluid specimen. Maternal serum screening yields a low percentage of false negatives. A wide range of other chromosomal abnormalities are not identified by maternal serum screening. Metanephrines, Fractionated, LC/MS/MS, 24-Hour Urine 14962 Patient Preparation It is preferable for the patient to be off medications for three days prior to collection. Patient should avoid tobacco, tea, coffee, for three days prior to specimen collection. Common antihypertensives (diuretics, ACE inhibitors, calcium channel blockers, alpha and beta blockers) cause minimal or no interference. Medications which are alpha agonists (Aldomet), alpha blockers (Dibenzyline) should be avoided 18-24 hours prior to specimen collection. Preferred Specimen(s) 5 mL 24-hour urine sollected with 25 mL 6N HCL to maintain a pH <3 Alternative Specimen(s) No preservative Transport Temperature Room temperature Methodology Liquid Chromatomagraphy Tandem Mass Spectrometry (LC/MS/MS) Clinical Significance Useful in the evaluation of Pheochromocytoma. 169 M N Metanephrines, Fractionated, Free, LCMSMS, Plasma 19548 Methodology Liquid Chromatography/Tandem Mass Spectrometry (LC/MS/MS) Limitations False-positive results have been observed in patients with either chronic kidney disease or hypertension. Clinical Significance Normetanephrine (NM) and metanephrine (MN) are the extra-neuronal catechol-o-methyl transferase (COMT) metabolites of the catecholamines norepinephrine and epinephrine, respectively. Measurement of plasma metanephrines is more sensitive (but may be less specific) than measurement of catecholamines for the detection of pheochromocytoma. Proper interpretation of results requires awareness of recent medication/drug history (e.g., antyhypertensive agents, alcohol, cocaine) and other pre-analytical factors (e.g., stress, severe congestive heart failure, myocardial infarction) that influence release of catecholamines and metanephrines. Mitochondrial Antibody with Reflex to Titer 259 Preferred Specimen(s) 0.5mL serum Transport Container Plastic screw-cap vial Transport Temperature Room temperature Reject Criteria Gross hemolysis • Gross lipemia MethodologyImmunoassay Reference Range(s) Negative Oligoclonal Bands, CSF Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology O P Protein C Antigen 674 1mL CSF submitted in a sterile, plastic, leak-proof container and 1mL serum It is preferred that the collection date and time be the same for both CSF and serum; however, it is acceptable for them to be drawn within 48 hours of each other. Client must be contacted when no serum is supplied to confirm the order. It is acceptable to send through CSF without serum when client has indicated to “run with serum control”. CSF must be crystalline and clear. (CSF collection tube #4 preferred). Plastic screw-cap vial Refrigerated (cold packs) Received room temperature Isoelectric Focusing 4948 Preferred Specimen(s) 1 mL frozen plasma collected in 3.2% sodium citrate (light blue-top) tube Instructions Draw blood in light blue-top tube containing 3.2% sodium citrate. Mix gently by inverting 3-4 times. Centrifuge 15 minutes at 1500 g within 1 hour of collection. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet (buffy) layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and ship on dry ice. *Note: 3.8% sodium citrate (light blue-top) tube is unacceptable. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Hemolysis • Received room temperature • Received refrigerated MethodologyImmunoassay Reference Range(s) 70-140% normal Protein S Antigen 5165 Preferred Specimen(s) 1 mL frozen plasma collected in a 3.2% sodium citrate (light blue-top) tube Instructions Draw blood in 3.2 % sodium citrate (light blue-top) tube. Mix gently by inverting 3-4 times. Centrifuge 15 minutes at 1500g within 1 hour of collection. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet (buffy) layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Freeze immediately and ship on dry ice. Note: 3.8% sodium citrate (light blue-top) tube is unacceptable 170 Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Hemolysis • Received room temperature • Received room temperature • Received thawed Methodology Micro Latex Particle Mediated Immunoassay Reference Range(s) 70-140 % normal Prothrombin (Factor II) 20210GA Mutation Analysis Preferred Specimen(s) Transport Container Transport Temperature Reject Criteria Methodology Limitations 5mL whole blood collected in an EDTA (lavender-top) tube EDTA (lavender-top) Room temperature Received frozen Polymerase Chain Reaction (PCR) • Oligonucleotide Ligation Assay • Fluorescent Microspheres If this mutation is not found by the testing procedure, it does not mean that the risk of carrying or developing deep vein thrombosis is not present. It simply means that this specific mutation has not been found, although other mutations may be present. It is also possible that such a patient may have secondary deep vein thrombosis due to non-genetic causes that would not be detected by this test. A person with one copy of the mutation has an approximate 3-fold increase in risk for venous thrombosis. The increase in risk for a person with two copies of the mutation is not known. Testosterone, Free and Total, LC/MS/MS Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology 36170 0.9 mL serum collected in a red-top tube (no gel) Specify age and sex on test requisition Plastic screw-cap vial Refrigerated (cold packs) Serum Separator Tube (SST‰) Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS) • Tracer Equilibrium Dialysis • Calculation Testosterone, Free, Bioavailable and Total, LC/MS/MS Preferred Specimen(s) Instructions Transport Container Transport Temperature Reject Criteria Methodology Reference Range(s) 17909 2.8 mL serum collected in a red-top tube (no gel) Serum Separator Tubes (SST‰s) are not acceptable Plastic screw-cap vial Room Temperature Serum Separator Tube (SST‰) Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS) • Calculation • Spectrophotometry (SP) • Immunochemiluminescent Assay See Laboratory Report Thiopurine S-Methyltransferase (TPMT) Genotype 14966 37742 Preferred Specimen(s) 5 mL whole blood collected in an EDTA (lavender-top) tube Instructions Whole blood: Normal phlebotomy procedure. Specimen stability is crucial. Store and ship room temperature immediately. Do not freeze. Transport Container EDTA (lavender-top) tube Transport Temperature Room temperature Reject Criteria Received frozen • Wrong specimen type • Exceeds stability • Less than minimum volume received Methodology Polymerase Chain Reaction (PCR) • Single Nucleotide Primer Extension Limitations This test detects 95% of the mutations in the TPMT gene and thus not all intermediate or slow metabolizers will be identified. Reference Range(s) See Laboratory Report Vanillymandelic Acid (VMA), 24-Hour Urine Patient Preparation 39517 It is preferable for the patient to be off medications for three days prior to collection. However, common antihypertensives (diuretics, ACE inhibitors, calcium channel blockers, alpha and beta blockers) cause minimal or no interference. Patient should avoid alcohol, coffee, tea, 171 S T Preferred Specimen(s) Transport Container Transport Temperature Methodology Limitations tobacco (including use of nicotine patch), bananas, citrus fruits and strenuous exercise prior to collection. 10 mL of a 24-hour urine collected with 25 mL 6N HCl to maintain a pH below 3 during collection. Urine without preservative is acceptable if pH is below 6 and the sample is shipped frozen. Plastic urine container Room temperature High Performance Liquid Chromatography (HPLC) • Electrochemical Detection Requires accurate 24-hour urine collection. Reference Range(s) VMA Creatinine, Urine 3-8 Years <2.3 mg/24 h 9-12 Years <3.4 mg/24 h 13-17 Years <3.9 mg/24 h Adults <6.0 mg/24 h 3-8 Years 0.11-0.68 g/24 h 9-12 Years 0.17-1.41 g/24 h 13-17 Years 0.29-1.87 g/24 h Adults 0.63-2.50 g/24 h Varicella-Zoster Virus Antibody (IgG) 4439 Preferred Specimen(s) 1 mL serum Instructions Avoid hemolysis by prompt separation of the serum from the clot Transport Container Plastic screw-cap vial Transport Temperature Room temperature Reject Criteria Gross hemolysis • Gross lipemia • Plasma • Grossly icteric MethodologyImmunoassay Limitations Other herpes viruses may cross react and produce high titers. Protection may be limited at low positive titers. Antibodies persist after infection has been treated or becomes dormant. Reference Range(s) <0.90 Negative - No VZV IgG Antibody detected 0.91-1.09 Equivocal >1.10 Positive - VZV IgG Antibody detected Vitamin B6 (Pyridoxine) U V 926 Patient Preparation Overnight fasting. Patient must be restricted from alcohol and vitamins for at least 24 hours before a sample collection. Preferred Specimen(s) 1 mL frozen plasma collected in an EDTA (lavender-top) tube - protected from light Instructions Draw blood into a protected from light lavender-top evacuated tube. If separation of cells can’t be performed immediately after collection, keep the whole blood refrigerated and protect from light. The separation of cells must be completed within 6 hours. Separate cells by centrifugation at 2-8° C (2200-2500 rpm, 800-1000 g) for 5-10 minutes. Transfer plasma to dark brown polypropylene or polyethylene transport tubes to protect from light. Alternately, neutral color polypropylene or polyethylene tubes can be used if wrapped in aluminum foil. Freeze the tubes at -10 to -30° C. Ship frozen. Transport Container Plastic screw-cap vial Transport TemperatureFrozen Reject Criteria Hemolysis • Lipemia • Received room temperature • Received refrigerated • Received thawed • Plasma collected in EDTA (royal blue-top), sodium heparin (green-top) or lithium heparin (green-top) tube • Specimens not protected from light Methodology Liquid Chromatography, Tandem Mass Spectrometry (LC/MS/MS) Reference Range(s) 172 2-17 years 3.0-35.0 ng/mL Adult 2.1-21.7 ng/mL Vitamin D, 1,25-Dihydroxy, LC/MS/MS 16558 Preferred Specimen(s) Instructions Transport Container Transport Temperature Methodology 2 mL serum Collect blood in a Vacutainer‰. Allow blood to clot (30 minutes) at room temperature, 18-25°C. Centrifuge and separate the serum from the cells. If sample is submitted with less than 1.1 mL and needs to be repeated the sample will be canceled with the comment “TNP-Initial testing necessitated a repeat, but there was insufficient sample to perform repeat”. Plastic screw-cap vial Room temperature Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS) Reference Range(s) Vitamin D, 1,25 (OH)2, Total Vitamin D3, 1,25 (OH)2 1-9 Years 31-87 pg/mL 10-13 Years 30-83 pg/mL 14-17 Years 19-83 pg/mL Adult 18-72 pg/mL Not available Vitamin D2, 1,25 (OH)2 Vitamin D, 25-Hydroxy, LC/MS/MS 17306 Patient Preparation Fasting preferred, but not required Preferred Specimen(s) 0.3 mL serum Instructions Collect blood in a standard red-top serum Vacutainer‰ tube. Allow blood to clot at room temperature. Centrifuge and separate the serum from the cells immediately. Alternatively, collect blood in an SST‰, allow to clot at room temperature, centrifuge and remove from the gel within 48 hours. Transport Container Plastic screw-cap vial Transport Temperature Room temperature Reject Criteria Gross hemolysis • Gross lipemia • Heparinized or EDTA plasma • Serum not separated from SST‰ gel or clot within 48 hours Methodology Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS) Reference Range(s) Vitamin D, 25-OH, Total 30-100 ng/mL 25-OHD3 indicates both endogenous production and supplementation. 25-OHD2 is an indicator of exogenous sources such as diet or supplementation. Therapy is based on measurement of Total 25-OHD, with levels <20 ng/mL indicative of Vitamin D deficiency, while levels between 20 ng/mL and 30 ng/mL suggest insufficiency. Optimal levels are ≥30 ng/mL. Vitamin D, 25-OH, D3 Reference range not established Vitamin D, 25-OH, D2 Reference range not established U V 173
© Copyright 2026