Speech Therapy post Concussion - the Brain Injury Alliance of New
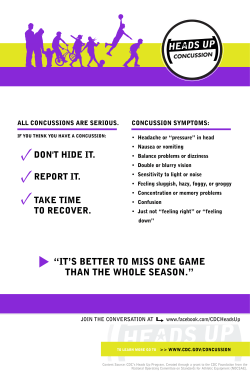
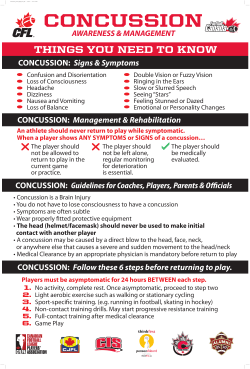
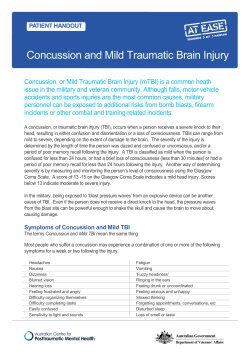
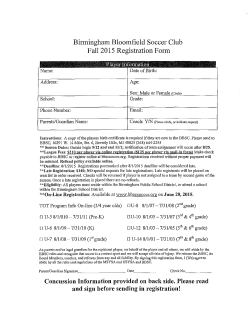
Suzanne W. Kutsmeda, MS, CCC-SLP Concussion Overview Concussion is a brain injury and is defined as a complex pathophysiological process affecting the brain, induced by biomechanical forces. Several common features that incorporate clinical, pathologic and biomechanical injury constructs that may be utilized in defining the nature of a concussive head injury include: Consensus Statement on Concussion in Sport, Zurich International Conference 2012 Concussion continued: Concussion may be caused either by a direct blow to the head, face, neck or elsewhere on the body with an ‘‘impulsive’ force transmitted to the head. Concussion typically results in the rapid onset of short-lived impairment of neurological function that resolves spontaneously. However, in some cases, symptoms and signs may evolve over a number of minutes to hours. Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury and, as such, no abnormality is seen on standard structural neuroimaging studies. Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course. However, it is important to note that in some cases symptoms may be prolonged. Consensus Statement on Concussion in Sport, Zurich International Conference 2012 Common Symptoms: Headache or a feeling of pressure in the head Temporary loss of consciousness Confusion or feeling as if in a fog Amnesia surrounding the traumatic event Dizziness or "seeing stars" Ringing in the ears Nausea Vomiting Slurred speech Delayed response to questions Appearing dazed Fatigue Concentration and memory complaints Irritability and other personality changes Sensitivity to light and noise Sleep disturbances Psychological adjustment problems and depression Disorders of taste and smell Symptoms common to young children: Appearing dazed Listlessness and tiring easily Irritability and crankiness Loss of balance and unsteady walking Crying excessively Change in eating or sleeping patterns Lack of interest in favorite toys Who is part of the Post concussion team? The most effective way to help a child who has sustained a concussion is with a team approach The Student/Child/Athlete The Parents/ Caregivers The Primary Care provider The concussion specialist (neurologist, physiatrist, orthopedist) The Neuro-psychologist The Opthamologist/Optometrist The PT The OT The School Nurse The Special Ed. Director The Teachers The Guidance Counselor The Athletic Director/Trainer THE SPEECH PATHOLOGIST Referrals to speech therapy Most common referral sources are: NeuroPsychologist Concussion specialists Why do I need Speech Therapy? “ Why do I need this (speech therapy)? I talk just fine!” -Casey 17 year old patient “SLP’s can help bride the gap between the medical and educational models for children with TBI. Although “cognitive rehabilitation” may not be a term used in IEP or 504 plans, cognitive communication rehabilitation treatment strategies can be incorporated into students’ education plans. Speech Pathologists can contribute to an educational program in several ways: SLPs often devise compensatory strategies for executive functions and memory, such as notebooks and organizers. Training in Language development and assessment and treatment of language disorders is a specialty in our field. Children and teens with TBI need a comprehensive assessment of their language and literacy skills following an injury. They are most likely to benefit this type of assessment when they return to school”. Assessment Pediatric assessment Tools: Health and Behavior Inventory Post Concussion Symptom Inventory Pediatric test of Brain Injury Continuous Performance Test Behavior Rating Inventory of Executive Functions (BRIEF) Test of Everyday Attention for Children (TEACh) California Verbal Learning Test Rivermead Post Conussive Symptom Questionnaire Neurobehavioral Symptom Inventory Test of Everyday Attention Dysexecutive Questionaire Motivated Strategies for Learning Questionaire Supplemental Assessment: Functional Age Appropriate Reading Task Confrontational Naming Task Timed/Untimed Verbal Description Task Navigation with a smart phone/ computer Visual Memory Task Auditory Memory Task Serial subtraction tasks Familiar series backwards task Treatment Speech therapy that focuses on cognitive communication skills is typically covered by insurance companies Lasts between 8-16 weeks The Evidence There is a strong evidence base with empirical evidence to support assessment and treatment strategies for: Executive function impairments Memory Attention Social communication Interventions meet criteria for high quality evidenced based systematic review: cognitive – communication language skills motor speech skills swallowing ASHA National Center for Evidence Based Practice Target Areas for Treatment Common Deficit areas Receptive Language Auditory and Reading Comprehension Following multi-step directions Understanding abstract language Expressive Language Verbal Fluency Flexible word use Topic Maintenance Word Finding Memory: Working Short term Organization Receptive Language Skills Auditory and Reading Comprehension Following Multi-step Directions Understanding Abstract Langauge Expressive Language Skills Word Finding Verbal Fluency Flexible Word Use Topic Maintainance Memory, Organization , and Attention Memory Strategy training for the treatment of mild memory impairments from TBI: Internal strategies external memory compensations Cognitive Rehabilitation Manual, Translating Evidence Based Recommendations into Practice, 2012 PQRST PREVIEW: Preview the Information to be recalled QUESTION: Ask Key questions about the text (“what is the main idea?”) READ: Read the material carefully STATE: State the answers and if necessary read again until you are able to answer the questions. Encourage students to summarize in their own words TEST: Test regularly for retention of the information Attention Recommend remediation off attentions during Post-Acute rehab. Direct Attention Training Strategy Training Cognitive Rehabilitation Manual, Translating Evidence Based Recommendations into Practice, 2012 Team Approach Throughout speech therapy it is important to maintain a team approach and be in contact with: Referring Doctors Pediatrician Concussion Specialist Neuro-psychologist School Professionals Recommendations to parents Guidance Counselor Help!! They aren’t following my 504 Reiterating recommendations that have been made by the students doctors Problem solving Encouraging parent involvement Encouraging student to take ownership of accommodations Discharge Learning and demonstrating use and understanding of strategies Increased function in an academic and social environment Recommend follow up re-evaluation in 3-6 months if difficulties continue other strategies are needed New symptoms arise Bibliography www.asha.org Babcock, Lynn; Byczkowski Terri Wade Shari L.; Ho Mona; Mookerjee Sohug; Bazarian Jeffrey J. (2013). “Predicting Postconcussion Syndrome After Mild Traumatic Brain Injury in Children and Adolescents Who Present to the Emergency Department” JAMA Pediatrics 167(2):156-161. Brown NJ, Mannix RC, O’Brien MJ, Gostine D, Collings MW, Meehean WP 3rd. (2014). “Effect of cognitive activity level on duration of post-concussion symptoms.” Pediatrics. 2014 Feb;133(2):e299-304. Ciccia, Angela Hein, Meulenbroek, Peter, Turkstra, Lyn S. (2009). “Adolescent Brain and Cognitive Developments. Implications for Clinical Assessment in Traumatic Brain Injury.” Topics in Language Disorders Vol. 29, No. 3: 249-265 Cicerone, K (2002) Remediation of working attention in mild traumatic brain injrry. Brain INjury Cicerone, KD. et al. “Evidence Based Cognitive Rehabilitation: Updated review of the literature from 2003-2008". Archives of physical medicine and Rehabilitation Journal, Vol 92 No. 519, 2011Z Eisenberg, M. et al. (2013). “Time Interval Between Concussions and Symptom Duration”. Pediatrics (10) 1542 Haskins, Edmund C. “Cognitive Re, 16, 185-195habilitation Manual: Translating Evidence- Based Recommendations into Practice.” ACRM Publishing, Virginia (2012). LinguiSystems Testing Guide, 2011 Edition. LinguiSystems Inc. East Moline, Illinois McCrory, P., Meeuwisse, W., Aubry, M., Cantu, R., et al. (2013). “Consensus Statement on Concussion in Sport, Zurich International Conference 2012". British Journal of Sports Medicine 47:250-258 Roberts, Greg et al. (2008) Evidence-Based Strategies for Reading Instruction of Older Students with Learning Disabilities. Learning Disabilities Research & Practice, 23(2), 63–69 Vermont Brain Injury Association: School Sports and Concussion Toolkit; revised 2013 www.cdc.gov/concussion
© Copyright 2026