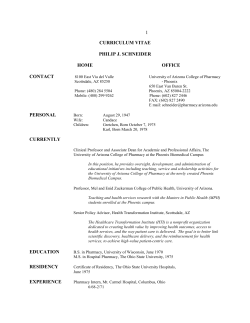
APhA–APPM
FEATURE APhA2004 Abstracts of Contributed Papers The following are abstracts of original research being presented at APhA2004, March 26–30, 2004, Seattle, Wash. Inquiries specific to the research should be directed to the principal author, indicated in the abstracts by underlined name. The abstracts are organized according to sections of the APhA–Academy of Pharmacy Practice and Management (APhA–APPM), APhA–Academy of Pharmaceutical Research and Science (APhA–APRS), and other organizations, as follows: • APhA–APPM Administrative & Management Practice: Abstracts 1–19 • APhA–APPM Clinical & Pharmacotherapeutic Practice: Abstracts 20–51 • APhA–APPM Community & Ambulatory Practice: Abstracts 52–105 • APhA–APPM Hospital & Institutional Practice: Abstracts 106–112 • APhA–APPM Nuclear Pharmacy Practice: Abstracts 113-119 • APhA–APPM Specialized Pharmaceutical Services: Abstracts 120–126 • APhA–APPM Miscellaneous: Abstracts 127–129 APhA–APPM Administrative & Management Practice 1—A BUSINESS MODEL FOR A SELFSUSTAINING PHARMACY PROGRAM IN A COMMUNITY HEALTH CENTER. Stubbings J, University of Illinois at Chicago, Talsania Patel S, Assam A, Mile Square Health Center. E-mail: [email protected] Objective: To create a self-sustaining pharmacy program that improves patient access to clinical pharmacy services and medications and reduces total health care costs. Methods: In 2002, the Bureau of Primary Health Care awarded a grant to an urban community health center for a comprehensive clinical pharmacy demonstration project. The focus of the clinical services was on diabetes and comorbidities. The business goal was to create a financially self-sufficient pharmacy program. A two-pronged business model was developed to generate revenue and save costs. The primary source of revenue came from third party reimbursement of clinical pharmacy services through incident-to-physician billing. Recognizing that payment for services would not generate enough revenue to make the program self-sufficient, we set out to reduce the drug budget for the community health center. This was accomplished by expanding the Medication Assistance Program that matched uninsured patients with medications donated by pharmaceutical companies. Data were collected on total number of patients served, revenue from clinical pharmacy services, and cost savings through donations of pharmaceuticals and other items. Results: After the first year of implementation, 92 patients were enrolled in the clinical pharmacy services program and 554 were enrolled in the Medication Assistance Program. Of the patients who received clinical pharmacy services, 36% were uninsured, 27% were Medicare recipients, and 21% had 226 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 • • • • APhA–APPM Pharmacy Residents: Abstracts 130–179 APhA–APRS Basic Sciences: Abstracts 180–181 APhA–APRS Clinical Sciences: Abstracts 182–203 APhA–APRS Economic, Social, & Administrative Sciences: Abstracts 204–283 • American Society for Pharmacy Law (ASPL): Abstracts 284–290 • American Institute of the History of Pharmacy (AIHP): Abstracts 291–306 APhA is especially proud to note that 18 of this year’s presented papers come from current pharmacy students. In recognition of their outstanding achievements, students’ abstracts are noted with a special symbol () next to the abstract number. In the abstracts, “NA” denotes that the information was not available when the abstract was prepared. Encore presentations—papers presented previously ). at other meetings—are marked with a special symbol ( Medicaid. Payment for clinical pharmacy services totaled $1,682. The major impact came from cost reduction through the Medication Assistance Program. Savings to the health center’s drug budget totaled $283,000. Bayer Diagnostics also donated 95 Ascensia Dex glucose monitoring systems at a total retail value of $6,650. Conclusions: The business model was successful in creating a self-sustaining clinical pharmacy program at an urban community health center, primarily by reducing the pharmacy budget through the Medication Assistance Program. This program had the added benefit of increasing access to pharmaceuticals in an uninsured population. 2—ANALYSIS OF THE PATENT LIFE OF NEW MOLECULAR ENTITIES APPROVED BY THE FDA BETWEEN 1980 AND 2001. Seoane E, Ohio State University, Schondelmeyer S, Ronald H, Rodriguez R, Weckwerth V, University of Minnesota. E-mail: [email protected] Objective: The purpose of this study was to describe and analyze the factors affecting the life of the first and last patent listed in the Orange Book (OB) for the first NDA of the NMEs approved in the U.S. between 1980 and 2001. Methods: Summary descriptive statistics were computed for dependent and independent covariates. A linear regression analysis model was used to determine the impact of the characteristics of the drug, the sponsor of a first NDA, the drug market size, drug policy, and the intellectual protection policy on NMEs’ patent life. A total of 330 drugs approved between 1980 and 1999 were included in the regression analysis. NMEs approved during the period 2000–2001 were excluded from the study. FDA and the U.S. Patent Office were the main sources of data for this study. Results: The results of the study demonstrate an increase in post-NDA patent and pediatric exclusivity time of the NMEs included in the study by almost 2 years from the period 1980–1989 to the period 1990–1999. The study also shows an increase in last patent post-NDA time and pediatric exclusivity by 1.5 years from the period 1980–1989 to the period 1990–1999. These results contradict the results found in the literature review showing a downward trend in post-NDA patent time in late 1980s and early 1990s. Conclusions: Several factors explain the increase in patent protection including: reduction of the NDA review time, pharmaceutical patent extensions, pediatric exclusivity, and changes in patent statutory term. The reduction in NDA review time is the main factor accounting for the increase in patent postNDA statutory term time. 3—CHARACTERISTICS OF NEW INDEPENDENTLY OWNED COMMUNITY PHARMACIES IN NC. Boyd J, Evans J, Robert C, Campbell University School of Pharmacy. E-mail: [email protected] Objective: To determine and evaluate the relative importance of specific services and products offered by newly owned independent pharmacies. A second objective is to distribute this information to pharmacists in North Carolina who are considering purchasing or opening an independent pharmacy. Methods: The North Carolina Board of Pharmacy provided a list of new pharmacy permits with the names and addresses of corresponding pharmacy managers. These permits were issued after January 1, 2000. The pharmacy managers were mailed a survey. Exclusions included existing pharmacies with changes in ownership, new pharmacies owned by corporations and multiple pharmacies owned by the same individual. The survey included questions about clinical services offered, including: blood pressure monitoring, bone density screening, diabetes education, health screenings, immunizations and other clinical services. Administrative questions included the availability of customer charge accounts, delivery services, and use of technologies including automated dispensing. Other information www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 obtained includes demographics, web site availability and types of nonprescription medication inventories. A small panel of new pharmacy owners was interviewed for comments prior to the development of the pretest. Based on comments from the panel, drive through windows, friendly service and the availability of after-hours emergency medicine pickup were rated highly as important factors for success of the pharmacy. The survey was developed and pretested in approximately 10% of the population. The results of the pretest were used to refine the survey. Results: The importance of specific programs and services in starting a new community pharmacy will be evaluated and described using Likert scale and frequency analysis. Conclusions: Will be reported upon completion of the project. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 6—EVALUATION OF MEDICATION NONCOMPLIANCE AT AN INDIAN HEALTH SERVICE HOSPITAL. Dupree M, Foster S, Dennewitz M, Cass Lake Indian Health Service Hospital. E-mail: [email protected] Objective: The purpose of our retrospective evaluation was to assess improvement in medication compliance at an Indian Health Service Hospital with regard to patients picking up prescriptions. Methods: In October 2003, the Department of Pharmacy installed an Interactive Voice Response (IVR) Application, Bin Management, Outbound Calling, and Status Inquiry Solution System to improve medication compliance and decrease the number of prescriptions that were being returned to stock. Through retrospective review, prescriptions unclaimed by patients for a 10-month period from 1 April 2003 to 31 Jan 2004 were analyzed. Pharmacy staff used the weekly return to stock medication labels and bin management return to stock reports before and after IVR installation. To determine which prescriptions were never dispensed, system reports were used for medication utilization review for data categorization and tracking purposes. Unclaimed prescriptions were tracked according to the following criteria: (1) Prevalence based on indi- vidual drug therapeutic classification; (2) total number of unclaimed prescriptions compared with the total number of patients with unclaimed prescriptions (some patients had multiple prescriptions); and (3) total number of unclaimed prescriptions compared with the total number of prescriptions filled during the tracking period. Results: Data collection ongoing, Conclusions: NA. 7—MEDMARX: A MEDICATION ANALYSIS TOOL FOR THE 21ST CENTURY, OR TEACHING AN OLD DOG NEW TRICKS. Shalita E, Guill J, United States Air Force, Rogers L, University of the Sciences in Philadelphia. E-mail: [email protected] Objective: Medication error analysis has become a mainstay of administrative pharmacy practice. Tying medication errors to breakdowns in process has been an emphasis since the early 1990s. Various methods have been used to determine the root causes of medication errors, leading to process improvement. Some of these methods include electronic spreadsheets, manual paper trail, AF form 765, CRAF documentation, and home-grown databases. A new tool, MedMarx was installed at McGuire Air Force Base (AFB), N.J., in December 2002. This program will examine the utility of this tool in root cause analysis of medication errors. Methods: McGuire AFB Pharmacy conducted two retrospective error analyses using 18 months of data. Results: Error analysis tied greatest risk to a single process step and identified new targets for opportunity. Conclusions: MEDMARX provides standardized tools for evaluating errors in an objective manner. Data can be analyzed using a concise reporting format and a standard definition of errors. Meaningful reports and charts present data in a way that clearly and easily identifies trends so that it can be acted upon to make valuable process improvements. 8—OVER-THE-COUNTER MEDICATION LABELS FOR BLIND CONSUMERS. Pawaskar M, Sansgiry S, University of Houston. E-mail: [email protected] Objective: To develop and evaluate the use of Braille and large print, over-the-counter (OTC) medication labels for blind and visually impaired consumers. Methods: The project is divided into three phases: development, implementation, and evaluation. In the first phase, OTC medication labels of analgesics will be developed in Braille for totally blind consumers. The study will also develop large print (18font size) labels especially for visually impaired consumers. In implementation phase, these labels will be tested in 50 blind and 50 visually impaired consumers. Participants will be chosen randomly from organizations and institutes that provide services and education for blind and visually impaired population. An experimental study design will be conducted to assess the effectiveness of such labels to help blind consumers comprehend OTC medication Journal of the American Pharmacists Association 227 2004 Abstracts of Contributed Papers 4—DRUG BENEFIT MANAGEMENT STRATEGIES: CONSUMERS’ ATTITUDE AND PERCEPTIONS REGARDING FORMULARIES. Sikri S, Kawatkar A, Sansgiry S, University of Houston. E-mail: [email protected] Objective: In recent years there has been a growing concern about the quality and cost of health care in America. Managed care has implemented drug benefits management strategies like formularies, which have evolved foremost amid cost containment strategies. However, most patients lack understanding of these drug management strategies, which may lead to dissatisfaction. The objective of this study was to evaluate consumer perceptions regarding formularies and to understand their knowledge regarding formularies. Methods: A cross-sectional study was conducted by administering a survey to consumers (N = 714) waiting to pick a prescription in community pharmacies (N = 72) in the Houston metropolitan area. A prevalidated questionnaire using an 11-item, 5-point Likert scale (strongly disagree, 1; strongly agree, 5) was used to measure consumer perceptions and knowledge regarding drug formularies. Data along with demographic information such as age, gender, marital status, race, education and income were collected, coded, and analyzed using SAS at an a priori significance level of .05. Descriptive and correlation analyses were performed on the data. Results: Among the surveyed population, only 25% of patients owned a copy of the formulary and 75% had no knowledge that their prescription plan used the formularies. Majority of the respondents were white (43%), female (52%), married (52%), and working full-time (64%) with a mean age of 39.58 (± 13.96) years. Overall, consumers had negative attitude towards formularies 2.77 (± 0.66). The respondents were neutral with respect to satisfaction with drugs included in their formulary 3.0 (±0.9). However analysis indicated that consumers were motivated to seek information regarding formularies 3.20 (± 0.98). Conclusions: Consumers had negative attitude toward formularies, which may be attributed to their lack of knowledge regarding formularies. Patient education efforts by health plan providers may help change consumer attitude and perception towards formularies. 5—EVALUATION OF INSULIN GLARGINE USE IN MEDICAID PATIENT. Mohamed O, Bultemeier N, Yeah C, Oregon State University, College of Pharmacy. E-mail: mohamedo @ohsu.edu Objective: The objective of this study is to evaluate the increase in use of insulin glargine in the Oregon Medicaid fee-for-service population. Methods: Design: This is a retrospective study utilizing a prescription claim database and manual chart review. Setting: Office of Medical Assistance Programs (OMAP) prescription claim database and Oregon Health & Science University (OHSU) medical records will be used to identify subjects. Participants: Subjects 18 years and older with an insulin glargine claim during the 18-month period of May 1, 2001 through October 31, 2002 and continuous eligibility 6 months prior to the claim will be eligible. Subjects receiving glargine from an OHSU prescriber and chronic diabetes care at OHSU will be identified to obtain clinical data. Subjects on chronic corticosteroid and/or immunosuppressant therapy and pregnant women will be excluded. Data collection: Diabetes medications before and after the sentinel glargine claim will be identified for all subjects. The following clinical data will be collected from chart review: weight, A1c, age, reasons for initiating and discontinuing glargine, type of diabetes, and prescriber’s specialty. All data will be de-identified. Analysis Plan: Descriptive statistics will be used to evaluate the characteristics of the sampled records. Furthermore, paired t-tests will be used to assess the change in A1c and weight at baseline versus 6months and 12-months postsentinel claim. Results: Study findings will be presented. Conclusions: A conclusion will be presented based on study findings. FEATURE FEATURE Annual Meeting Abstracts 2004 information. The OTC label evaluation process model will be used to test labels. Variables such as ease of product use, product knowledge, attitude toward product label, product evaluations, purchase intention, and overall satisfaction with the product performance will be measured using previously validated and reliable scales. The test instrument will be provided in English and in Braille, and participants will have a choice as to which they would prefer to use. Data will be coded and analyzed using SAS statistical package to estimate effectiveness of labels in providing appropriate product use information. Results: Currently data collection is in progress. After data analysis, results will highlight consumers’ proficiency and satisfaction with the use of Braille and large print labels. Conclusions: Braille and large print medication labels are expected to be beneficial for consumers in making informed decisions regarding product selection and use. These labels may promote safe and effective use of OTC medications and help these consumers to administer medications independently. 9—PATIENT ACCESS TO PHARMACIES IN HEALTH PROFESSIONAL SHORTAGE AREAS (HPSAS). Gadkari A, Mott D, University of Wisconsin–Madison. E-mail: [email protected] Objective: To identify the characteristics of Health Professional Shortage Areas (HPSAs) in terms of access to pharmacy sites. Methods: Two databases will be used for this study. First, the HPSA database created by the Health Resources and Service Administration (HRSA) will be used to identify all Primary Medical Care HPSA designations in the state of Wisconsin. From this, we will select HPSAs identified by boundaries of townships, towns, villages and districts. Second, a database of all licensed pharmacies in Wisconsin containing contact information will be obtained from the Department of Regulation and Licensing in Wisconsin. Using these two databases, all the selected HPSAs and the surrounding pharmacies will be identified. A database containing HPSA characteristics will be created, which will describe access in the form of presence/absence of a pharmacy within a HPSA, the estimated distance of a HPSA from the closest pharmacy, number of pharmacies within a 10/20/30 mile radius of a HPSA, and types (i.e., clinic, hospital, chain, independent) of pharmacies accessible to a HPSA. Results: This study will help describe access to pharmacies for patients living in HPSAs and inform policy makers about access to pharmacy goods and services in these areas. The other chief outcome of this study will be the generation of a database of Wisconsin pharmacies that serve HPSA populations. This database will serve as a sampling frame for a future survey of pharmacies, which will help us obtain insight into a number of diverse issues including workload for these pharmacists and pharmaceutical services provided to HPSA populations. Conclusions: Given the current shortage of pharmacists and concern for access to health care for vulnerable populations, the study is expected to improve understanding of patients’ access to pharmacies in HPSAs. 228 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 10—PERCEPTIONS OF HIGH SCHOOL STUDENTS TOWARD PHARMACISTS. Mattingly L, Stensland S, Jackson T, Lullo A, Midwestern University. E-mail: Lisa.Mattingly@ mwumail.midwestern.edu Objective: To evaluate students’ overall perception of pharmacists after participation in a pharmacy summer program. Methods: The Career Explorers Program provides an opportunity for high school students to gain pharmacy practice experience. A retrospective pre–post survey was given to students during the last week of the program. This 16-item survey was adapted from a survey used in 2002. Statements were restructured to assess student agreement with common pharmacist stereotypes. The survey was designed using three different Likert-type scales based on the nature of the question. Results: All participants completed this survey (N = 50). Each statement was evaluated using the Wilcoxon Signed Rank Test with a Bonferroni correction. Responses to 13 of the 16 statements were significantly changed upon posttest. Improvements in students’ attitude were seen toward: pharmacists’ knowledge of prescription (P < .001), over-thecounter (P < .001), and herbal (P < .001) medications. Upon posttest, students were more likely to agree that pharmacists are medication experts (P < .001), improve patients’ health (P < .001), have many responsibilities when filling a prescription (P < .001), are accessible to patients (P < .001), counsel patients (P < .001), prevent medication problems (P < .001), and make drug therapy recommendations (P < .001). Perceptions of pharmacists’ career options expanded beyond community and hospital upon posttest (P < .001). Pharmacists’ education to practice (P < .001) and specialize were better understood (P = .002). Two statements—“pharmacists act in an ethical manner” and “pharmacists are trustworthy”—were not statistically significant because 98% of students agreed with these characteristics on the presurvey. The third statement that was not statistically significant concerned compensation for services; 60% agreed pharmacists are compensated “just right” before the program and 63% agreed after. Conclusions: The results show that students did not have an understanding of the expectations and roles of a pharmacist before entering the program, and the program was successful at changing students’ perceptions. 11—PERSISTENCE AFTER CHOLINESTERASE THERAPY CHANGE IN A MEDICAID DATASET. Bunz T, Dore D, Kogut S, University of Rhode Island. E-mail: [email protected] Objective: The purpose of this project is to determine the frequency of change in cholinesterase inhibitor (ChEI) therapy and to determine if patients changing therapy are likely to persist with therapy. Methods: Thirty-two months of pharmacy dispensing records of Rhode Island Medicaid enrollees were examined using the SAS software package. The data included a unique patient identification, a medication description, including date dispensed and days supply, as well as variety of demographic information. We identified patients having at least 18 months of data describing medication use, and excluded patients who switched to a different ChEI drug within 180 days of the end of the dataset. Patients changing repeatedly between different ChEI drugs, or switching between more than two medications were also excluded. Patients were included in our study only if at least 80% adherent with therapy, according to their medication possession ratio. The number of patients who were adherent and persistent for 6 months before switching to a different ChEI drug, for 6 months after the switch, and those patients persistent before and after change were then recorded. Results: The dataset contained records for 2,336 patients, 1,547 of whom had 18 months of data for analysis. Of these patients, 217 had received a dispensing for more than one of the ChEIs. Sixty-seven patients were eligible for inclusion in the assessment. Of these patients, 45 (67.2%) were persistent for 6 months after the switch, 48 (71.6%) were persistent before the switch, and 33 (49.3%) were persistent before and after the switch. Conclusions: The number of patients persistent before or after change is similar to the number of patients persistent throughout the rest of the population. This appears to support the practice of changing between ChEIs. More studies should be done to determine the variables affecting patient therapy and to determine the clinical and economic impacts of therapy changes. 12—PHARMACY CAREER OPPORTUNITY AWARENESS AMONGST HIGH SCHOOL STUDENTS. Jain B, Stensland S, Jackson T, Midwestern University. E-mail: [email protected] Objective: To increase pharmacy career opportunity awareness of high school students enrolled in a pharmacy summer program. Methods: The Career Explorers Program engaged students in activities that consisted of both experiential and didactic components designed to introduce them to the world of pharmacy. Ten pharmacy career descriptions were selected and compiled in a handout. A paired pre–post survey was created with questions regarding these pharmacy career opportunities, factors influencing their decision in choosing a certain career opportunity, and other issues. The presurvey was completed in class, while the postsurvey and job description handouts were completed at home. The postsurvey additionally asked students to explain why responses changed from the presurvey. Results: All students completed the paired surveys (N = 50). Respondents indicated the most interesting option presented was Industry-Based Pharmacist (30% pretest, 24% posttest). On pretest, the number 1 pharmacy career respondents indicated a desire to learn more about was Nuclear Pharmacy (76%), while on postsurvey respondents most often wanted additional information on Pediatric Pharmacy (52%). Respondents chose Industry-Based Pharmacy as the option they were most likely to pursue on pretest (26%), but this preference changed to Pediatric www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 Pharmacy (28%) on postsurvey. The career choice students were least likely to pursue was Military Pharmacy (30% pretest, 20% posttest). The most influential factor in pursuing a career was genuine interest in the field (72% pretest, 68% posttest). The least influential factor was family pressure (70% pretest, 66% posttest). Overall, 74% (N = 37) of students changed their career option choices, while 88% (N = 44) did not change the factors influencing their decision in a pharmacy career choice. Conclusions: The Career Explorers Program raised awareness about pharmacy career opportunities. This research helped to establish where students interests lies and what may influence their decision to pursue certain pharmacy-based careers. 14—THE DEFENSE SUPPLY CENTER: PHILADELPHIA’S COLD CHAIN MANAGEMENT PROGRAM FOR THE INFLUENZA VIRUS VACCINE. Dallas D, Defense Supply Center Philadelphia. E-mail: [email protected] Objective: To identify and improve problem areas associated with the distribution and storage of Influenza Virus Vaccine for Department of Defense (DoD) personnel and beneficiaries. Methods: The Pharmaceutical Commodity Business Unit of the Medical Directorate at the Defense Supply Center Philadelphia (DSCP) is responsible for the distribution of the Influenza Virus Vaccine for the Department of Defense. DSCP’s Cold Chain Management program was established to ensure product integrity following losses of hard to replace vaccine due to freezing during shipment. The program benchmarked off the Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 15—THE EVOLVING ROLE OF PATIENT ADVOCACY GROUPS IN IMPROVING HEALTH AND HEALTH CARE. Lee S, Amgen, Ascione F, McKercher P, University of Michigan. Email: [email protected] Objective: The primary purpose of this study was to better understand the role of patient advocacy groups’ efforts to raise disease awareness and improve access to appropriate modern therapies. Methods: In-depth telephone interviews were commissioned by the University of Michigan’s Center for Medication Use, Policy & Economics and conducted by Market Strategies, Inc. Key representatives within selected patient advocacy organizations dedicated to serving patients in two different disease categories, kidney disease and breast cancer, were interviewed. In kidney disease advocacy groups, members at the National Kidney Foundation (NKF) and American Society of Nephrologists (ASN) were interviewed. In breast cancer, members at the American Cancer Society (ACS) and Susan G. Komen Foundation were interviewed. The targeted subjects for each organization were staff members at the national office as well as the state affiliates in California, Florida, Michigan, New Jersey, and Texas. Interviews lasted approximately 45–60 minutes and were conducted during April and May 2003. In total, 18 interviews (9 nephrology and 9 oncology) were conducted. Results: Differences were noted between the patient advocacy groups within each of two disease states. The NKF is focused on educating the general public and health care professionals, while ASN is heavily focused on nephrologists. Both organizations play a role in legislative issues. NKF tends to be more involved in areas of primary interest to patients, whereas ASN tends to be more involved in issues affecting the health care system as a whole. In terms of breast cancer, ACS is more involved in working with and educating health care professionals, whereas the Komen Foundation concentrates more of their efforts with the general public. Activities that appear to be the most effective are educational activities directed toward both consumers and health care professionals. Outreach activities are extremely successful in reaching the general public, especially the health fairs, and wellpublicized and -organized walks and runs. Conclusions: The role of patient advocacy groups has evolved from charitable public champions for disease victims to facilitating and enhancing early and progressive care. Our research suggests that patient advocacy groups play a growing and important role in dissemination of disease and treatment information and providing a forum for individuals seeking additional insight into their disease. 16—DRUG THERAPY FOR ALZHEIMER´S DISEASE: PERSISTENCE ON CHOLINESTERASE INHIBITORS MEASURED USING MEDICAID PHARMACY CLAIMS DATA. Dore D, Bunz T, Kogut S, University of Rhode Island. E-mail: dave@ daviddore.com Objective: To measure and compare persistence with the three commonly used cholinesterase inhibitors (ChEIs). Methods: A retrospective cohort analysis was completed using de-identified Rhode Island Medicaid pharmacy claims data between January 1, 2000 and August 31, 2003. Inclusion criteria were all Rhode Island Medicaid patients whom received newly initiated therapy on donepezil, rivastigmine, or galantamine between June 1, 2000 and August 31, 2002 and had at least 12 months of data for followup. Exclusion criteria were having received a dispensing for more than one ChEI product, having received any dispensing for a greater than 60-day supply, or having a greater than 90-day interval between any two dispensings. Persistence was defined as continuous therapy for at least 180 days. Patients were identified as not persistent if he or she did not receive a dispensing for a ChEI on days 180 through 365. The patient population included a total of 2,336 individuals; 1,802 supplied 12 months of follow-up data, and 1,612 did not switch between agents. Results: Persistence was measured in 888 individuals whom received any ChEI, 556 whom received donepezil, 193 whom received rivastigmine, and 139 whom received galantamine. Persistence at 6 months was estimated to be 75% overall and 76%, 74%, and 75% for donepezil, rivastigmine, and galantamine respectively. Conclusions: Approximately 1 in 4 patients did not persist to 6 months with ChEI therapy. In addition, persistence did not differ between ChEIs. Further research should be conducted to identify characteristics of individuals likely to fail therapy and to subsequently decrease prescribing in that population. Optimizing use of ChEIs may improve patient care and reduce expenditures on ineffective therapy. Journal of the American Pharmacists Association 229 2004 Abstracts of Contributed Papers 13—POTENTIAL COST SAVINGS AT AN INDIGENT CARE CLINIC BY MAXIMIZING PATIENT ASSISTANCE PROGRAMS. Lindsey C, Sutherland J, University of Missouri–Kansas City. E-mail: [email protected] Objective: To evaluate the cost of medications used in an indigent care clinic dispensary and determine the potential cost savings if patient assistance programs were optimized. Methods: This was a retrospective review of medication invoice purchases that took place at the Jackson County Free Health Clinic between August 2002 and August 2003. All purchases were recorded by medication, dose, drug class, date of purchase, and cost. Medication purchases were summated and evaluated based on the ability to access these products through assistance programs and therapeutic substitutions. Results: A total of $5,168.13 was spent to purchase 38 different medications for the dispensary over a 12-month time frame. Majority of medications were antihypertensives, antidepressants, and hypoglycemics. Of all of the maintenance medication purchases, 79.5% of our dispensary expenses could have been saved by ensuring the patient assistance program was optimized. Conclusions: Medication cost to the clinic could be potentially reduced by $4,107.93 annually by ensuring that each drug order is evaluated for its ability to be acquired through assistance programs. United States Army Medical Materiel Agency’s Anthrax Cold Chain Management Program. It includes three packaging protocols: warm, moderate, and cold. These packaging protocols, using endothermic containers and temperature monitors, have been third party tested, and permit DSCP to ship and track Influenza Virus Vaccine in any ambient temperature to DoD medical facilities and deployed units worldwide. The temperature monitors enable DSCP to monitor the temperature of the vaccine during shipment by recording temperature readings every 15 minutes for up to 20 days. Results: Over the past 3 years, DSCP’s Cold Chain Management Program has dramatically improved the reliability of shipping temperature sensitive vaccines through training end users, increasing in transit visibility, established set shipping schedules with commercial carriers, and allowed DSCP to monitor 100% of the shipments from manufacturer to customer receipt. Conclusions: The Defense Supply Center Philadelphia’s Cold Chain Management program has been highly successful in ensuring more timely deliveries and most importantly, product integrity. FEATURE FEATURE Annual Meeting Abstracts 2004 17—EVALUATION OF CARDIOPULMONARY RESUSCITATION CERTIFICATION AMONG PHARMACY STUDENTS. Patel S, Eap N, Blodgett B, Onamade A, University of Illinois at Chicago. E-mail: [email protected] Objective: The morbidity and mortality of cardiac arrest are costly in the United States. Research has demonstrated that immediate cardiopulmonary resuscitation (CPR) improves survivability in patients who experience cardiac arrest and respiratory failure. Even though they are future health professionals, pharmacy students are often minimally trained in CPR. Because patients at increased risk of cardiovascular and pulmonary events regularly visit health care settings, pharmacy students should have adequate CPR training before entering the workforce. The purpose of this study is to assess the knowledge and attitude regarding CPR certification among pharmacy students and to evaluate the effectiveness of their training. Developing confidence through repetition enhances students’ ability to perform these skills. Currently, CPR training is offered to students during the fourth (experiential) year. This study will investigate whether students perceive a benefit to CPR being offered earlier in the curriculum. Specifically, the investigators will assess student knowledge and confidence regarding their ability to perform CPR as a health care professional. Methods: Students in their fourth year at a college of pharmacy who have completed CPR training will be asked to complete a self-assessment instrument. The instrument will measure students’ perceived knowledge and attitudes about their ability to use CPR in immediate response situations. Additionally, first- through third-year students will be surveyed about their perceived need for obtaining CPR training earlier in the curriculum and their willingness to participate in these programs if offered. Results: Data will be analyzed using Rasch rating scale model to measure hierarchically responses provided by the two instruments. Conclusions: Students are expected to perceive value in having CPR offered earlier in the curriculum and in repeated participation in these training sessions that allow students to demonstrate their ability, willingness to initiate immediate response, and develop confidence in performing CPR. 18—PHARMACY STUDENTS’ ATTITUDES ABOUT MEDICALLY UNDERSERVED POPULATIONS. Langridge S, Jackson T, Lurvey P, Midwestern University. E-mail: [email protected] Objective: To determine the extent to which experience and knowledge gained regarding medically underserved populations affects pharmacy students’ attitudes about community health centers (CHCs), clinicians, and patients. BACKGROUND: Approximately 40 million Americans are medically uninsured or underinsured. Poor health outcomes occur more frequently in these patients when compared with insured populations. Clinicians in collaboration with pharmacists in CHCs have been successful in improving patient health outcomes. However, many are unaware of these resources. To 230 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 introduce these resources to fourth professional year pharmacy students, an elective class was developed, “Bringing Pharmaceutical Care to Underserved Populations.” Methods: A retrospective pre–post attitudinal survey, comprising three different sections, was developed and administered to students in the course. Section 1 used a four-point Likert-type scale to assess students’ perceived knowledge of CHCs, services they offer, patients who use these services, and characteristics of clinicians who provide them. Section 2 evaluated responses about the perceived frequencies of services provided, barriers encountered, and duties of CHC pharmacists. Section 3 assessed students’ intentions to provide pharmaceutical care services in a CHC environment and their confidence level regarding their ability to develop a pharmaceutical care services plan for a CHC. Results: Students who completed the class participated in the pilot study (N = 2). Students believed this elective class increased their awareness of the services CHCs provide and that these services are not exclusive to indigent populations. Students viewed pharmaceutical care in a CHC as a viable career option and indicated their confidence level in their ability to implement these services increased. The effectiveness of this elective will be evaluated with the same instrument in winter 2003, and the final poster will reflect these data. Conclusions: Overall, the perceptions about services provided in CHC environments and the patients who use these services improved after taking this elective. 19—RETURN ON INVESTMENT ANALYSIS FOR BONE MINERAL DENSITY (BMD) SCREENING. Patel H, Shenandoah University, Skelton J, US Wellness, Inc., Ahrens R, Stolte S, Shenandoah University. E-mail: [email protected] Objective: To estimate the number of new antiosteoporosis prescriptions generated for patients with low BMD upon screening, and to estimate the potential return on investment (ROI) in terms of new antiosteoporosis prescriptions for a pharmaceutical manufacturer–sponsor of BMD screenings. Methods: A total of 262 patients were screened for osteoporosis using the Hologic Sahara Clinical Bone Sonometer. Screenings were conducted at four physician offices and six employer groups. All patients were 40 years or older and were not currently taking any antiosteoporosis prescription medications. Patients were placed into either a low-, moderate-, or high-risk fracture group based on their T scores from the BMD screening. A follow-up survey was performed within 60 days after initial screening to determine whether the patient scheduled a followup appointment with their physician. Patients were also asked whether an antiosteoporosis medication was prescribed. Results: A total of 98 patients were identified as low risk were excluded from the follow-up and ROI analysis, and 2 other patients were lost to follow-up. Among the remaining 162 patients, the fracture risk at initial screening was 76% for physician office patients and 58% from employer group patients. A total of 78% of patients initiated a follow-up appointment with their physicians, and 69% of patients in the high-risk category received a prescription antiosteoporosis medication. The return on investment for the BMD screenings was 256%, assuming the patients’ average medication adherence was 6 months. Conclusions: The BMD screening program demonstrated that 9.8% of patients screened received an antiosteoporosis prescription. Screenings appear to be beneficial to both patients and a pharmaceutical manufacturer–sponsor. APhA–APPM Clinical & Pharmacotherapeutic Practice 20—A RANDOMIZED, DOUBLE-BLIND TRIAL OF LOW-DOSE OXYMORPHONE IMMEDIATE RELEASE (5 MG) FOR MILD TO MODERATE PAIN IN AMBULATORY PATIENTS. Walker D, Granger Medical Clinic, Inc. Gimbel J, Arizona Research Center, Ma T, Zagorski A, Ahdieh H, Endo Pharmaceuticals, Inc. E-mail: [email protected] Objective: To assess the safety and efficacy of low-dose (5 mg) oxymorphone immediate release (IR) in patients with mild to moderate pain following outpatient knee arthroscopy. Methods: A double-blind, randomized, placebocontrolled study will include patients 18 years of age and older following ambulatory arthroscopic knee surgery. To enter the study, patients must have initial postsurgical pain between 30 and 70 mm on a 100mm visual analog scale (VAS) and a pain rating of mild or moderate on a categorical scale. Patients will be instructed to take the study medication (5 mg oxymorphone IR or placebo) as needed for pain for up to 8 hours, and not more frequently than 1 dose per hour. Pain will be assessed at 30 minutes after the first dose and every hour thereafter. Patients requiring rescue medication will be discontinued from the study. Patients will record in diaries pain intensity, relief, and use of study medication and rescue medication. Efficacy measures are hourly pain intensity scores (VAS), pain intensity and relief scores (Brief Pain Inventory), frequency of remedication, time to rescue medication or discontinuation, and patient global assessment of pain relief. Records of adverse events will measure safety. Results: Data will be presented for approximately 100 patients (50 patients per group). Conclusions: Conclusions will be presented based on the trial results, and the implications for pharmacists will be discussed. 21—ANALGESIC EFFICACY OF OXYMORPHONE IMMEDIATE RELEASE IN POSTSURGICAL ORTHOPEDIC PAIN: RESULTS OF A RANDOMIZED, DOUBLEBLIND, PLACEBO-CONTROLLED, DOSERANGING COMPARISON WITH OXYCODONE. Gimbel J, Lee W, Arizona Research Center, Ma T, Zagorski A, Ahdieh H, Endo Pharmaceuticals, Inc. E-mail: [email protected] www.japha.org March/April 2004 Vol. 44, No. 2 FEATURE Annual Meeting Abstracts 2004 vices. Surveys were anonymous and were collected from January to March of 2001. Results: A total of 153 surveys were returned for a response rate of 49%. Nurses were the most common health care provider on staff at health departments, and the most frequently additional personnel requested. The most common service offered by health departments was immunizations. Most respondents desired to establish preventive services such as disease management, indigent care clinics, and health information libraries. Only 13% had a pharmacist on staff, and an additional 11% partnered with their local pharmacist. Approximately 60% had not considered partnering with their local pharmacists; most stated that cost was the barrier preventing an alliance. Officials identified indigent care clinics, dispensing medications, and drug-use review as the main services they would like to see provided by pharmacists. Conclusions: Pharmacists appear to be underused in public health plans for meeting goals of Healthy People 2010. 96—MOTIVATION AND JOB SATISFACTION OF COMMUNITY PHARMACISTS INVOLVED WITH PHARMACEUTICAL CARE. Swensgard L, Ohio State University. Email: [email protected] Objective: Community pharmacists are becoming increasingly involved with direct patient care services as a way to expand their role as health care professionals. The future success of these services depends in part on the ability of community pharmacies’ corporate management to keep the participating pharmacists motivated to continue their roles as pharmaceutical care providers and motivate other community pharmacists to become involved. The purpose of this study is to assist Kroger corporate management in identifying what motivational factors contribute to the decision of central Ohio Kroger pharmacists to become involved in or abstain from pharmaceutical care services. Also, the study will identify what barriers central Ohio Kroger pharmacists perceive to becoming involved in pharmaceutical care. Factors contributing to job dissatisfaction and job satisfaction will also be assessed. Methods: Mail surveys will be sent to two groups of central Ohio Kroger pharmacists, those actively providing patient care services and those involved solely in dispensing activities. The survey will compare and contrast both groups of pharmacists’ motivations to perform patient care services. Job satisfaction will also be assessed in both groups of pharmacists. The data collected from the survey will be used to implement new recruitment and advancement strategies to increase Kroger community pharmacist involvement in pharmaceutical care services. In addition, the information will be disseminated to other community pharmacies for use in increasing pharmacist involvement with pharmaceutical care. Results: Data collection began in November 2003. Conclusions: This project will enable corporate management of community pharmacy establish- 250 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 ments to identify motivational forces that contribute to a pharmacist’s decision to perform pharmaceutical care services and factors that contribute to job satisfaction. Also, this project is expected to provide information regarding how best to reward pharmacists for their participation in pharmaceutical care services. 97—USING ADVANCED PRACTICE COMMUNITY CLERKSHIP STUDENTS TO PROVIDE CONTINUING EDUCATION FOR RURAL PHARMACISTS. Hastings J, University of Arkansas for Medical Sciences College of Pharmacy, West D, University of Arkansas for Medical Sciences. E-mail: [email protected] Objective: The goal of this project is to describe how senior pharmacy students are used in the delivery of live continuing education (CE) to pharmacists in a remote region of a small southern state. Methods: The community clinical clerkship is a cooperative rotation taught by the college of pharmacy in conjunction with 24 pharmacies located throughout Arkansas. One of the assignments that senior students enrolled in this advanced community practice clerkship must complete is a clinical or management project. The board of pharmacy in this state requires pharmacists to obtain 12 hours of live, disease-related CE over a biennial licensing period. One preceptor in a rural area of the state requires each student who rotates through his site to deliver a CE presentation related to drug-therapy to pharmacists in the southeast region of the state. Results: NA. Conclusions: This unique use of students to help pharmacists comply with licensing requirements benefits everyone involved. The students have an opportunity to complete an assignment for their rotation while at the same time benefiting from the experience of researching, preparing and presenting a CE program. Pharmacists in the region benefit from the information presented by the student about the selected drug topic, are able to obtain live CE credit in a convenient manner and have the opportunity to network with their local peers on a regular basis. 98—ANALYSIS OF HYPERTENSION CONTROL IN A MIDWESTERN CARDIOLOGY CLINIC. Glosner S, Pfizer Inc, Tynan S, Alsip D, Cline K, Midwestern University, Konczal M, Faaborg J, Marcinkowski L, Midwestern University. E-mail: [email protected] Objective: Coronary heart disease (CHD) remains the number 1 killer in the United States. CHD also costs more than $100 billion a year to treat. CHD is both financially and clinically important. Risk factors for developing CHD are elevated blood pressure (BP), tobacco use, low HDL cholesterol, family history, and age. Our purpose was to assess BP control, treatment options and comorbidities that increase CHD risk in hypertensives patients. Methods: A retrospective, chart review was performed at an Illinois cardiology practice during October 2002. The study population consisted of patients taking either antihypertensives alone (N = 401) or those taking antihypertensive agents in conjunction with medications for heart failure (N = 359). A total fo 120 patients were randomly selected and evaluated from the study population. Patient demographics, blood pressures, laboratory test results, and medications were collected. Results: Overall, 56% of participants were women. The average age for the overall population was 68 years. More than 75% of patients had a body mass index of greater than 25 kg/m2. Some 70% of the population had a dyslipidemia, 29% had CHD, 23% had arrhythmias, and 15% had diabetes mellitus (DM). Beta blockers (24%) and calcium-channel blockers (23%) were the most frequently used medications. BP control was noted in 47.1% of men and 51.5% of women. BP control was observed in less than 50% of each drug class except for diuretic medications (52%). A total of 62% of CHD patients had elevated BPs, and 42% of patients with CHD or DM were not at their LDL cholesterol goal of less than 100 mg/dL. Within the last year, 15% of reported patient hospitalizations were cardiac related. Conclusions: Cardiologists generally treat more complicated cardiovascular patients, yet nearly 50% of patients in this study had BPs that were uncontrolled while on medications. Practitioner education by pharmacists on national guideline attainment should help improve health outcomes (e.g., BP and cholesterol control). 99—ASSESSMENT OF MEDICATION NONADHERENCE AND DISEASE STATE KNOWLEDGE IN A COMMUNITY PHARMACY. Self T, University of Kentucky, Chou C, Pfizer, Inc. E-mail: [email protected] Objective: The purpose of this project was to (1) identify patients at risk for medication nonadherence using a validated scale and to report any trends; (2) determine the need for further counseling in patients with risk behaviors for nonadherence on the benefit of prescription medications, and (3) evaluate disease knowledge and awareness of their personal laboratory values in patients indicating a history of hypertension, hyperlipidemia, or diabetes. Methods: Surveys were randomly distributed to patients 18 years of age and older at a local Kroger Pharmacy. Collected information included demographics (age and gender), chronic disease states, and self-reported medication-taking behaviors. The survey consisted of four questions (Morisky scale) in a validated tool that is used to identify and address barriers to medication adherence. Patients were considered nonadherent if one or more questions on the Morisky scale was answered “yes,” and they were then counseled on ways to increase adherence as well as the benefit of prescription medication. In addition, halfway through the survey, the method was improved by asking patients that indicated a history of hypertension, hyperlipidemia, or diabetes if they knew their current laboratory values and goals for their blood pressure, cholesterol, or blood glucose. Patients were then counseled appropriately about their diseases and goals of therapy. Results: All data will be analyzed using www.japha.org March/April 2004 Vol. 44, No. 2 FEATURE Annual Meeting Abstracts 2004 25–A REPRODUCIBLE MODEL FOR DISEASE STATE MANAGEMENT AND PHARMACEUTICAL ACCESS FROM A FEDERALLY FUNDED URBAN COMMUNITY HEALTH CENTER. Talsania S, University of Illinois at Chicago, Assam A, University of Illinois at Chicago, Mile Square Health Center. E-mail: [email protected] Objective: To develop an effective model for expanded clinical pharmacy services and increased access to pharmaceuticals in an underserved community. Methods: The Bureau of Primary Health Care provided grant funding for clinical pharmacy demonstration projects to meet the needs of underserved communities. One of the 2002 recipients was a federally qualified urban community health center with an in-house pharmacy. To achieve the goals of the grant, the pharmacy created three integrated processes: diabetes disease state management, 340B drug program utilization, and manufacturer assistance program expansion. Before the grant was funded, pharmacists provided disease state management on a sporadic basis depending on pharmacy staffing needs. Funding from the grant enabled the pharmacy to hire a pharmacotherapist to implement structured clinical pharmacy services on a consistent basis. The focus was on patients who had type 2 diabetes mellitus with or without comorbidities. Patients were seen in a one-on-one session, and drug therapy was adjusted through a collaborative practice agreement and established protocols. An educational assessment was performed, and education was tailored to meet individual patient needs. Increased access to pharmaceuticals was achieved through the 340B drug program and expansion of manufacturer assistance programs. Clinical indicators measured included change from baseline in glycosylated hemoglobin, blood pressure, and serum lipid levels. Data on economic, education, and humanistic outcomes are also being collected, and validated instruments will be used to analyze this information. Results: Analysis for year 1 data has started and will be completed by the APhA annual meeting. Conclusions: Based on preliminary data analysis, this model will demonstrate improvement in diabetic patient outcomes and cost savings for the health center’s drug budget. The hope is that pharmacists will implement this model in their practice settings. 26—A SURVEY OF PHARMACISTS’ ACTIVITIES SUPPORTING MEDICATION ADHERENCE. Possidente C, Pfizer, Inc, Anzisi L, Pfizer, Algozzine T, Buckley T, Weathermon R, Pfizer, Inc. E-mail: [email protected] Objective: Nonadherence to prescribed drug therapy is a common and serious health care problem. The study objectives were to determine what activities were provided by pharmacists to improve medication adherence and to review pharmacists’ attitudes related to medication adherence. Methods: A 15-question written survey was distributed to pharmacists attending educational programs conducted in New York, Connecticut, New Hampshire, and Vermont from February through June 2003. The survey response rate was approximately 65%. 232 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Results: The majority of the 937 respondents were men (65%) who had been in practice for more than 20 years (58%) and were working in community practice (60%). A total of 73% of pharmacists stated they performed adherence activities. Activities most commonly provided included: verbal counseling for new prescriptions, verbal counseling not related to prescriptions, telephone consultations, and distributing written materials. Community pharmacists (86.4%) provided more activities to improve adherence than did hospital pharmacists (50.8%), (P < .0001); however, they had less time available. Hospital pharmacists tended to target patients with specific diseases more than community pharmacists. Time spent performing adherence activities did not vary between independent and chain community pharmacists. Pharmacists in practice less than 5 years provided activities to improve adherence more frequently than their peers. Time spent performing these activities decreased as years in practice increased. The most common barrier was limited time, reported by 78% of pharmacists. Some 76% of respondents agreed pharmacists have a responsibility to improve medication adherence, but 17% of pharmacists stated improving medication adherence was not their responsibility, an attitude more common with men in community practice for longer than 10 years. Overall, 92% of respondents were interested in learning more about adherence. Conclusions: Pharmacy organizations and the pharmaceutical industry have an opportunity to educate pharmacists and the public on the importance of optimizing medication adherence. 27—A UTILIZATION REVIEW OF OAB AGENTS IN A WISCONSIN MEDICAID POPULATION. Conner C, Cherayil G, Pfizer, Inc. Email: [email protected] Objective: Current estimates suggest that 17 million Americans are affected by overactive bladder (OAB). The available agents for the treatment of OAB differ with respect to formulation (immediate versus extended-release), selectivity for the bladder, and adverse effect profile. Our objective was to describe the costs and explore the use patterns of specific OAB agents in the Wisconsin Medicaid population. Methods: The claims data used for analysis included all Wisconsin Medicaid paid prescription claims data from January 1, 2002 to December 31, 2002. These data were obtained directly from the Centers for Medicare & Medicaid Services Web site. National Drug Codes were used to extract use data for tolterodine immediate and extended-release, oxybutynin immediate and extended-release, and flavoxate. Descriptive analysis of claims included calculation of total expenditures, number of claims reimbursed, and mean cost per claim across products and formulations. Results: In 2002, the Wisconsin Medicaid program reimbursed for OAB agent claims totaling $3,423,458.30, representing 55,864 claims. Within the OAB category, oxybutynin extended-release (14,899 claims), tolterodine extended-release (14,852 claims) and oxybutynin immediate-release (13,343 claims) represented the most frequently used products. Extended-release products constituted 47% of total prescription claims expenditures in 2002. Cost per claim values within the extendedrelease OAB agents were $77.67 for tolterodine and $82.44 for oxybutynin. Conclusions: In the Wisconsin Medicaid population, the top three most frequently used OAB agents in 2002 were oxybutynin (extended-release), tolterodine (extended-release), and oxybutynin (immediate-release). Among extended-release OAB products tolterodine exhibits a more favorable cost per claim ratio than did oxybutynin. 28—ADHERENCE MEASURES OF PSYCHOSTIMULANTS USED IN THE TREATMENT OF ATTENTION-DEFICIT/HYPERACTIVITY DISORDER IN CHILDREN AND ADOLESCENTS. Sanchez R. E-mail: [email protected] Objective: The purpose of this study was to examine adherence measures of various psychostimulants in school-aged children with attentiondeficit/hyperactivity disorder (ADHD). Methods: Paid prescription claims from May 1, 2001 to May 31, 2002 were extracted from the Texas Medicaid prescription claims database. Adherence measures included persistence, medication possession ratio (MPR), and consistence. Adherence was evaluated based on drug, age, and gender. Results: Subjects initiated on Concerta performed better on all three adherence measures. Mean persistence, MPR, and consistence were 0.50, 0.76, and 0.81, respectively. Subjects aged 5–9 years exhibited better persistence and consistence than did those aged 10–14 years and 15–18 years. Mean persistence and consistence were 0.45 and 0.78, respectively, for subjects aged 5–9 years. No gender-related adherence differences were found among the groups. Conclusions: Separation between Concerta and the other stimulants was statically significant. However, this significance may not be clinically meaningful. Younger children tended to perform better on adherence measures than older children. As medical advances continue to improve, physicians, pharmacists, managed care organizations, and other health care-related workers should develop strategies to identify and improve adherence to medications. Further investigation into the clinical relevance of these findings should be explored. 29—AN EVALUATION OF THE MANAGEMENT OF HYPERLIPIDEMIA IN COMMUNITY BASED OUTPATIENT CLINICS WITH A CENTRALLY BASED CLINICAL PHARMACIST (“VIRTUAL CLINICAL PHARMACIST”). Evanko T, Jones W, Southern Arizona VA Health Care System. E-mail: [email protected] Objective: The objective of this project was to evaluate the impact of a clinical pharmacist in a hyperlipidemia disease state management program using telephone contact and follow-up for a Veterans Affairs (VA) Community Based Outpatient Clinics (CBOCs). Methods: This was a prospective open study of patients with hyperlipidemia approved by the local www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 30—ANALYSIS OF A MEDICAID COX-2 PRIOR AUTHORIZATION PROGRAM. Hermansen E, Gunning K, University of Utah. E-mail: [email protected] Objective: (1) To examine criteria used for denial or acceptance in determination of Medicaid prior authorization for COX-2 inhibitors and to evaluate appropriateness of these requests. (2) To evaluate costs shifts and use of nonselective NSAIDs in response to the implementation of the prior authorization program. Methods: All patients whose physicians submitted requests for prior authorization for COX-2 inhibitors from July 1, 2003 to December 31, 2003 will be examined. Baseline demographic data will be collected. Medication profiles will be compared with patients’ profiles before implementation of the prior authorization program (January 1, 2003 to May 31, 2003). Results: NA. Conclusions: Based on these results, the prior authorization process may be able to be improved Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 such that quality care is provided while costs within Medicaid are contained. 31—COLLABORATIVE PRACTICE AGREEMENTS: PERCEPTIONS OF PHARMACISTS AND PHYSICIANS. Causey L, Causey’s Rx Solutions, Ramsey L, University of Mississippi. E-mail: [email protected] Objective: To determine provider perceptions and barriers to implementation of pharmacy disease management programs using physician–pharmacist collaborative practice agreements (CPAs). Methods: Nonexperimental, descriptive-correlational design using surveys mailed to 4,991 Mississippi-licensed pharmacists and physicians. Primary outcome measures included perceived barriers and benefits to CPAs, support level of CPAs, and interest level in establishing CPAs. Results: Response rate was 13.5%; 70% of respondents were men; respondents were between 30 and 60 years of age; most were private practice physicians or independent community pharmacists. A total of 95% of pharmacists and 74% of physicians supported CPAs. Similarly, 94% of pharmacists and 68% of physicians felt CPAs were within a pharmacist’s scope of practice. Age of individuals surveyed had no impact on pharmacist’s support level; however, support differed in varying age groups of physicians. Physicians in satellite clinics expressed the greatest interest in establishing CPAs, while physicians in private groups expressed the least. The impact of training medical and pharmacy students together was evident only when the highest degree of co-training was achieved, with support rate increasing by 12%. Approximately 45% of practitioners deemed training beyond an entry-level pharmacy degree necessary. Pharmacists and physicians identified different disease states for which they believed pharmacists could play a paramount role. The majority of physicians (74%) were unfamiliar with pharmaceutical care (PC) data. Physician support increased by 14.9% as knowledge of PC increased. Pharmacists’ greatest concerns were adequate reimbursement, training, and time to deliver PC. Pharmacist competency, scope of practice, and protocol adherence were identified as physician’s primary concerns. Perceived benefits of CPAs were similar between both groups, but they differed in order of importance. Conclusions: Physician support for CPAs with pharmacists is positive. Most providers perceive CPAs as positively affecting patient care; however, concerns exist that negatively affect CPA establishment. Understanding provider perceptions allows initiatives to be pursued leading to increased CPA implementation and improved patient care. 32—COMPARISON OF KNOWLEDGE AND ATTITUDES OF PHARMACISTS VERSUS DIETITIANS REGARDING HERBS AND DIETARY SUPPLEMENTS. Mehta B, Ohio State University, Giannamore M, Pfizer, Inc. E-mail: [email protected] Objective: The goals of this project were to determine: (1) differences in knowledge between pharma- cists and dietitians, (2) changes in attitudes toward the professional responsibility of patient education, and (3) the level of confidence within each profession regarding patient education. Methods: Pharmacists and dietitians who attended Ohio pharmacy association annual meetings completed a knowledge and attitude survey before and after attending a continuing education (CE) program on herbs and dietary supplements. Pharmacists and dietitians listened to the same presentation. The pretest included the following questions about herbal supplements: demographic information, access to information, previous CE program attendance, attitudes regarding use of supplements, and knowledgebased questions about commonly used products. The posttest repeated pretest knowledge-based and attitude questions. Data from the survey were entered and analyzed using Microsoft Access. Results: Of the 130 dietitians and 85 pharmacists who attended each program, 60% of dietitians and 69% of pharmacists had attended previous herbal CE programs. Dietitians had a lower average baseline knowledge score of 5.3, compared with 7.4 for pharmacists (P < .01; maximum score 15). Posttest scores improved significantly to scores of 10.3 and 10.5, for dietitians and pharmacists, respectively (P < .01 for pretest-to-posttest comparisons within each group). Attitudinal scores (pretest versus posttest) regarding professional responsibility for patient education decreased from 24% to 14% for dietitians (P < .02) and 8% to 5% for pharmacists (P > .05). The confidence level (pretest versus posttest) in providing patient information decreased from 62% to 25% for dietitians (P < .01) and 43% to 21% for pharmacists (P < .04). Conclusions: Pharmacists had higher baseline knowledge scores, compared with dietitians. Both groups significantly increased their scores following the CE presentation. The majority of respondents had attended previous CE sessions on this subject, but they did not consider provision of patient education about herbal products within the realm of their professional responsibilities. Attitudinal scores regarding professional responsibility for patient education differed significantly between pretest and posttest surveys for dietitians but not pharmacists. Both groups were less comfortable discussing herbal products in the posttest versus pretest presentation period. Future research may identify educational needs of pharmacists and dietitians to increase confidence about patient education on herbal supplements. 33—COMPARISON OF PHARMACY REFILL HISTORY VERSUS SPIROMETRY AS AN INDICATOR OF ASTHMA CONTROL IN COMMUNITY PHARMACY PRACTICE. Dugan B, Palm Beach Atlantic University, Buie B, Walgreens Pharmacy, Weitzel K, University of Florida, Van Riper B, Walgreens Pharmacy, Asmus M, Hendeles L, Chesrown S, University of Florida. E-mail: [email protected] Objective: To determine if community pharmacist performed spirometry would assist in identifying Journal of the American Pharmacists Association 233 2004 Abstracts of Contributed Papers Institutional Review Board. All patients were cared for by one of five CBOCs, with nurse practitioners or physicians being the primary care providers. Patients entering the study were referred to a clinical pharmacist via E-mail or telephone communication. The clinical pharmacist reviewed the medical records of the patient and made recommendations for drug therapy and adjustments to therapy based upon laboratory results. Patients agreeing to this program had their lipid lowering drugs adjusted according to the Pharmacologic Management of Hyperlipidemia clinical practice guidelines published by the Department of Veterans Affairs. Follow-up laboratory testing was scheduled by the clinical pharmacist and medication changes were suggested to the primary care provider and implemented when approved. The target LDL cholesterol was less than 130 mg/dL for primary and less than 100 mg/dL for secondary prevention. All contact between the clinical pharmacist, primary care provider, and patients was via the telephone, E-mail, or electronic progress notes. The primary endpoint was to determine the change in the lipid profile before and after enrollment in the hyperlipidemia project. Results: A total of 47 adult patients (44 men/3 women) enrolled in the study. The respective mean total and LDL cholesterol concentrations were 251 and 164 mg/dL at the time of enrollment. After enrollment, these respective values decreased to 191 and 114 mg/dL. Follow-up was completed for 44 patients (94%). The three who did not complete the study did not have laboratory testing (1) or died of causes unrelated to hyperlipidemia (2). Conclusions: These results show that having hyperlipidemia patients managed by a “virtual clinical pharmacist” who recommends, implements, and monitors therapy can be very successful. Many VA medical centers are operating CBOCs but may not have clinical pharmacist involvement in drug therapy management. Further evaluation of alternative practice models needs to be undertaken. FEATURE FEATURE Annual Meeting Abstracts 2004 patients with poorly controlled asthma who had a refill history indicative of good control and asthma medication adherence. Methods: Design: Prospective, pilot project. Setting: Four community pharmacies in Gainesville, Florida. Patients: Those identified as having a refill history suggestive of good asthma medication adherence and asthma control. Parameters defining good asthma control were based on NHLBI asthma guidelines and were: (1) receipt of not more than 12 shortacting beta-2 agonists or not more than 6 short-acting beta-2 agonists if using long-acting beta-2 agonists concomitantly in the past year, (2) receipt of not more than 12 long-acting beta-2 agonists in the past year, (3) receipt of inhaled corticosteroids at least one half as often as prescribed in the past year. Selected patients then underwent spirometry testing. Data Collection: Forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and the ratio of these two measures. Patients with a FEV1/FVC ratio of less than 0.8 of predicted were identified as having poor asthma control. Analysis Plan: Descriptive analysis and statistics. Other Measures: Not applicable. Results: A total of 145 patients were identified as having a refill history suggestive of good asthma control. Of these, seven patients met study criteria and underwent spirometry. The mean age of participants was 26.6 years. Subjects were primarily Caucasian and women, with a 6:1 ratio for race and gender. FEV1/FVC ratio was less than 0.8 of predicted for 57% of the subjects. Conclusions: NHLBI guidelines recommend community pharmacists use patients’ refill history to identify those with poorly controlled asthma. This study tested a mechanism by which community pharmacists could identify patients with poor asthma control who would not be identified by refill history alone. Results indicate that spirometry may have a role in further identifying poorly controlled asthma patients in the community pharmacy setting. A larger, controlled analysis is warranted. 34—EVALUATION OF PHARMACIST INTERVENTIONS IN DIABETIC PATIENTS FROM RURAL COMMUNITY HEALTH CENTERS. Pinto S, Segal R, Winterstein A, Annis L, Robinson D, Yates D, University of Florida, Pederson L, Palatka Community Health Center, Willis M, Trenton Medical Center. E-mail: [email protected] Objective: The focus of this clinical pharmacy demonstration project is on improving the drug-use process in the management of vulnerable patients with chronic diseases, especially diabetes. The program includes the education and training of pharmacists in five community health centers funded by the Health Resources and Service Administration (HRSA) about specific disease therapies, monitoring, and management. The targeted disease is diabetes, but the program also addresses diabetic patients’ comorbidities, including hypertension and hyperlipidemia. The study hypotheses are (1) patients exposed to the intervention will have improved medical and patient outcomes based on 234 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 changes in glycosylated hemoglobin, diabetic symptoms, LDL, blood pressure, and health related quality-of-life; and (2) process measures consistent with best practices will improve for patients exposed to the intervention. Methods: The project uses a prospective design to determine whether exposure to the intervention over a 2-year period leads to improved outcomes and processes of care. Patients are the unit of analysis and serve as their own controls. Subjects include adult patients who have a diagnosis of type 2 diabetes mellitus and whose glycosylated hemoglobin values are above 8 mg/dL within a 3-month period of the enrollment date. Subjects who meet the inclusion criteria were consecutively drawn from a subset of clinic patients. Medical outcome data are being collected from medical and laboratory records, pharmacy records, and patient self-report. Study measures include clinical indicators, quality-of-life, satisfaction, and HEDIS diabetes-related process measures. Outcomes and process data is collected at baseline and every 6 months. Results: Currently, 142 patients are enrolled in the study, with 137 at the 6-month level and 104 at the 12-month level. Study findings for approximately 135 patients followed for 12 months will be presented. Conclusions: Conclusions will be presented based on the analysis of data comparing baseline, 6month, and 12-month results. 35—HYPERCHOLESTEROLEMIA: A SURVEY OF PATIENTS’ UNDERSTANDING OF THE CONDITION AND ITS TREATMENT. Ong C, Liew S, Changi General Hospital. E-mail: [email protected] Objective: To determine: (1) patients’ perceptions of the causes and consequences of hypercholesterolemia, and (2) the level of understanding of their current pharmacological treatment for hypercholesterolemia. Methods: A random survey on hypercholesterolemic patients who consented to participate in completing a pharmacist-assisted questionnaire was conducted. These subjects were from specialist outpatient clinics and wards. Results: A total of 73 patients were interviewed for the survey. Only 45.2% of participants were able to describe briefly a physical feature of cholesterol. While 39.7% of patients had heard of the term “high cholesterol,” only 24.7% of respondents were aware of the differences between “high density-lipoprotein cholesterol” and “low density-lipoprotein cholesterol.” Participants most commonly associated hypercholesterolemia with unhealthy diets (80.8%), lack of exercise (58.9%), and obesity (28.8%), and they believed that hypercholesterolemia led mainly to heart attacks (58.9%) and strokes (43.8%). Although most respondents understood the importance of lowering their serum cholesterol, they were largely unaware of their target serum cholesterol levels. The results of this study also suggested that the patients’ degree of understanding of hypercholesterolemia was proportional to the level of education but inversely related to their age. Treatment-wise, patients demonstrated familiarity with the physical appearance and dosing regimen of their medication; however, few patients could accurately remember the names of their medication and their potential adverse effects. Eight patients (11%) reported experiencing drug-related adverse effects such as muscle weakness and constipation. Conclusions: Although patients were generally aware of the influence of social lifestyle on the development of hypercholesterolemia, overall knowledge about this condition was poor. More than one half of the patients surveyed knew how to take their medication, but most were unaware of potential adverse effects. Health professionals are well placed to better educate patients, especially older patients, in understanding their condition, treatment goals, and medication profile. 36—IMPACT OF DIABETES EDUCATION AND MANAGEMENT ON PATIENT OUTCOMES. Assam A, University of Illinois at Chicago, Mile Square Health Center, Talsania S, Lin S, Jackson T, University of Illinois at Chicago, Ntowe F, Chessky A, University of Illinois at Chicago, Mile Square Health Center. E-mail: [email protected] Objective: To determine the impact of clinical pharmacy services on diabetes outcomes in an urban community health center. Methods: Patients 18 years of age or older with type 2 diabetes, with or without comorbidities, were enrolled in the program through physicians, pharmacists, or self-referral. Enrollment was on an ongoing basis. A total of 92 patients were evaluated by clinical pharmacists during year 1. Patients were seen in a one-to-one session by appointment or walk-in basis. Before the visit, the pharmacist reviewed patient’s medical and laboratory records via an integrated electronic medical record system. Initial visits lasted 30 minutes to 1 hour, and the patient’s knowledge, adherence to drug therapy, and glycemic control were assessed. All patients enrolled were provided with a free blood glucose monitor and were taught proper testing technique. Based on the initial assessment, patients were referred to a nutritionist, podiatrist, or optometrist/ophthalmologist, as needed. An individualized educational plan was also developed at this time. Educational sessions included, but were not limited to: importance of self-monitoring blood glucose, medication use, diet and exercise, complications of diabetes, and importance of laboratory values and patient involvement in disease management. A collaborative practice agreement with the medical providers and standards of care for the American Diabetes Association were used to adjust drug therapy and monitor disease states. Subsequent visits lasted 20 to 30 minutes, and patients were assessed for adherence to prior interventions. Results: Year 1 data analysis will be presented at APhA2004. Clinical markers collected to evaluate the program objective include glycosylated hemoglobin, blood pressure, lipid profile, and improvement in knowledge from baseline. Conclusions: We anticipate the results will www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 demonstrate clinical pharmacy services can improve patient knowledge base and diabetes outcomes. 38—IMPACT OF PHARMACIST INTERVENTION THROUGH A TELEPHONE RUN SMOKING CESSATION CLINIC. Foust S, Porter J, Drake University College of Pharmacy. Email: [email protected] Objective: To determine the impact of a pharmaVol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 39—MEDICATION UTILIZATION EVALUATION OF HMG-COA REDUCTASE INHIBITORS IN LIPID CLINIC. Booth H, Tomich D, Kassebaum P, Madigan Army Medical Center. E-mail: [email protected] Objective: (1) To identify patients in lipid clinic who are being treated with a 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitor (statin) other than our formulary agent, simvastatin, and to document the reason behind starting on or switching to a nonformulary statin, (2) to identify trends in prescribing pattern of HMG-CoA reductase inhibitors, and (3) to document the rate of discontinuation of simvastatin and to assess for the opportunities for clinical interventions to improve patient care. Methods: This is a retrospective analysis of use of HMG-CoA reductase inhibitors in a pharmacistmanaged lipid clinic. A query from Access-based database used in the lipid clinic enabled identification of patients who were being treated with a HMGCoA reductase inhibitor between January 1, 2002 and September 30, 2003. A retrospective chart review was conducted in patients who were identi- fied as being treated with a HMG-CoA reductase inhibitor other than simvastatin. Results: A total of 565 patients were identified as being treated with HMG-CoA reductase inhibitors. Of these patients, 403 patients were being treated with simvastatin, 114 patients with atorvastatin, 42 patients with pravastatin, and 1 patient with lovastatin. Retrospective analysis of prescribing pattern of HMG-CoA reductase inhibitors, rate and rationale behind discontinuation of simvastatin, and potential opportunities for clinical interventions will be presented. Conclusions: NA. 40—MEDICATION UTILIZATION REVIEW OF ALENDRONATE. Seah J, Lim W, Wee I, Changi General Hospital. E-mail: [email protected] Objective: To determine the prescribing patterns, drug-related problems, range of patient monitoring, and daily calcium intake associated with oral alendronate amongst inpatients. To recommend appropriate measures for rational prescribing of alendronate and improvements in patient monitoring. Methods: A retrospective review of clinical case notes, laboratory data, and pharmacy medication records was performed for all ward patients prescribed alendronate during a 5-week study period. Results: A total of 44 patients receiving either once-daily or once-weekly alendronate were identified. Alendronate was prescribed most commonly to treat postmenopausal osteoporosis. Six patients were switched from alternative pharmacological treatments for osteoporosis to alendronate therapy. Seven patients were also prescribed concomitant intranasal calcitonin, with two being on long-term combination treatment. One patient was given alendronate despite the drug being contraindicated; two tube-fed patients and another patient with dysphagia received crushed tablets. No significant drug interactions were noted, though many patients were on multiple medications. Approximately one third of patients had their baseline bone mineral density (BMD) assessed, but none received follow-up BMD scans. Calcium levels were checked in 56.8% of patients, and none was hypocalcemic. Constipation was the most common adverse event; other less common adverse effects included esophagitis, gastric ulcers, and gastritis. None of the patients received the recommended 1,500 mg/day of elemental calcium, although almost one half of them had a total calcium intake (meals plus supplements) of 800–1000 mg/day. Conclusions: Alendronate was generally prescribed appropriately for registered indications. The use of long-term concomitant intranasal calcitonin should be reviewed as clinical evidence for this practice is lacking. Alendronate was generally well tolerated; however, its contraindications and precautions should be closely noted before initiating therapy. Increased use of BMDs, more frequent serum calcium level determinations, and adequate calcium intake should also be considered. Journal of the American Pharmacists Association 235 2004 Abstracts of Contributed Papers 37—IMPACT OF PHARMACEUTICAL CARE: A RANDOMIZED, CONTROLLED TRIAL OF BLOOD PRESSURE CONTROL IN HYPERTENSIVE PATIENTS. Amruso N, Eckerd PatientCARE Network. E-mail: [email protected] Objective: To determine the ability of pharmacists within community pharmacies to manage hypertensive patients. Methods: Design/Setting: Randomized, prospective, controlled study within community pharmacies. Patients: Patients were included if they had an average blood pressure (BP) reading above goal based on the sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI) guidelines. Patients were excluded if they had one or more of the following conditions: status-post–transplant procedure requiring long-term immunosuppressive therapy, terminal illness, end-stage renal disease, renal artery stenosis, or other unstable condition potentially contributing to hypertension. Patients were excluded if they were participating in another hypertension management program or refused to consent to the conditions of the study. Patients were randomized into high intensity (HI) or low intensity (LI) groups. HI patients met individually with the pharmacist for BP measurements, medication assessment, and education. Patients were scheduled for visits at 2 to 4 week intervals until BP was controlled, then periodically until the end of 12 months. LI patients were mailed educational materials quarterly and had their BP measured at 12 months. Data Collection: A progress note was developed to ensure complete data collection at each visit. The completed note was sent to the study coordinator for input into a database. Outcomes measures: Change in systolic blood pressure (SBP) and diastolic blood pressure (DBP), percentage of patients who achieved goal BP and percentage on first-line therapy. Analysis: A statistician performed the data analysis. Results: Overall, 109 patients were randomized into HI and 103 into LI, and 35 HI and 13 LI patients completed the study. Among HI patients, SBP declined by an average of 17 mm Hg, compared with a 1 mm Hg decrease for LI patients. Among HI patients, DBP declined by an average of 3 mm Hg, compared with a 1 mm Hg increase for LI patients. A total of 66% percent of HI patients and 8% of LI patients achieved goal BP; 57% of HI patients and 23% of LI patients were on first-line therapy. Conclusions: Patients enrolled in a hypertension management program conducted by pharmacists in the community setting achieved BP control to a greater extent than patients not enrolled. cist-run, telephone smoking cessation clinic on patient success. Methods: Patients were obtained based upon patient interest and primary care referral at the Department of Veterans Affairs. Inclusion criteria included patients at either the precontemplation or contemplation stages of the Transtheoretical Model. Duration of patient enrollment was 1 year from patient’s quit date. The pharmacist contacted patients 2 weeks and again 7 days before the quit day. Patients were also contacted on quit day (Day 0) and on days 3, 7, 14, 21, 28, 42, 56, 70, 84, 114, 144, 174, and 365. Counseling consisted of behavioral and pharmacological cessation methods, such as proper use of nicotine-replacement therapy (NRT) and trigger, stress, and weight management. Data collected will include patient self-reported frequency and duration of tobacco use throughout the program and response to initial assessment questionnaire. The initial assessment questionnaire will be used to obtain Fagerstrom Tolerance Scores, previously used NRT therapy by the patient, patient-perceived negative effects of smoking, patient concerns, and planned methods to be used in smoking cessation. The primary outcome is participants’ abstinence rate 1 year from quit date. Secondary outcomes include initial Fagerstrom Tolerance Scores compared with quit rate, duration of NRT or bupropion therapy, number of telephone calls placed to patient, and number of patient-reported relapses. Results: Preliminary results show that subjects were all men with a mean age of 55. Descriptive statistics will be used to evaluate primary and secondary outcomes for presentation at APhA2004. Conclusions: If favorable outcomes result from this research, this study will show that pharmacists can have an impact on patient success in smoking cessation through the use of a telephone smoking cessation clinic. FEATURE FEATURE Annual Meeting Abstracts 2004 41—NATIONWIDE DISSEMINATION OF THE RX FOR CHANGE TOBACCO CESSATION CURRICULUM: IMPACT OF A TRAINTHE-TRAINER PROGRAM FOR PHARMACY FACULTY. Corelli R, Fenlon C, Kroon L, Lem K, Sullivan M, Hudmon K, University of California, San Francisco. E-mail: [email protected] Objective: Research consistently demonstrates that students in the health professions receive inadequate training for assisting patients with tobacco cessation. In response to this need, the California schools of pharmacy collaborated to develop Rx for Change, a 6- to 8-hour comprehensive tobacco cessation curriculum that is being disseminated to schools of pharmacy across the U.S. via a faculty train-the-trainer model. The purpose of this study is to assess pharmacy faculty members’ posttraining perceptions regarding adoptability of the Rx for Change curriculum. Methods: Pharmacy faculty attended one of three train-the-trainer conferences offered during summer 2003. Participants completed an eight-page posttraining survey that assessed key factors potentially associated with adoption of the program. Participants rated their pretraining and posttraining ability to teach comprehensive tobacco cessation on a 5-point scale (1 = poor; 2 = fair; 3 = good; 4 = very good; 5 = excellent). Results: A total of 132 faculty members representing 76 pharmacy schools participated in the trainthe-trainer program and completed a posttraining survey. Before the training, 48.5% of the faculty had received no formal training for treating tobacco use and dependence, and 82.2% had not taught students about this subject. Participants’ self-rated abilities to teach tobacco cessation to pharmacy students significantly increased on the posttest, compared with the pretest (2.77 versus 4.39; P < .001), with 25.7% and 96.2% rating their abilities as either very good or excellent before and after the training, respectively. Nearly all participants believed the Rx for Change curriculum materials were either moderately (47.3%) or highly (50.4%) compatible for integration into their existing curricula, and 69.5% of the participants indicated they were highly likely to adopt Rx for Change at their school. A total of 96% of attendees said they would recommend the train-the-trainer program to other pharmacy faculty members. Conclusions: Participation in a train-the-trainer program significantly increased pharmacy faculty confidence to provide comprehensive tobacco cessation education to pharmacy students. The majority of participants are highly likely to adopt the Rx for Change curriculum at their school, which will eventually translate into an increased proportion of pharmacists who are adequately trained to treat tobacco use and dependence. 42—OXYMORPHONE EXTENDED RELEASE PROVIDES SAFE AND EFFECTIVE ANALGESIA FOR CANCER PATIENTS: A RANDOMIZED,. Ahdieh H, Endo Pharmaceuticals, Inc., Dvergsten C, INC Research, Inc., Ma T, Frailey A, Endo Pharmaceuticals, Inc., Nashat G, not applicable. E-mail: [email protected] 236 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Objective: To compare the analgesic efficacy and tolerability of oxymorphone extended release (ER) and oxycodone controlled release (CR) in moderate to severe cancer pain. Methods: In this Phase III, randomized, doubleblind, two-way crossover study, patients were stabilized with oral opioid medication during a 7- to 10day titration/stabilization phase, followed by 7 to 10 days of double-blind treatment with oxycodone CR or oxymorphone ER (estimated conversion ratio of 2:1 for oxycodone CR:oxymorphone ER). Dosages remained fixed from days 4 to 7; two rescue doses of morphine sulfate 15 mg/day were allowed. Patients then crossed over to the alternate treatment for 7 to 10 days. Efficacy was assessed by pain intensity and relief (via the Brief Pain Inventory), global evaluations, and Karnofsky performance status. Routine safety evaluations were performed. During doubleblind treatment, the ratio of the average total daily dose from the last 2 days of each treatment period was calculated for each patient. Results: A total of 44 patients received at least 1 dose of study drug. Mean pain intensity following double-blind treatment was 2.8 for oxycodone CR and 2.5 for oxymorphone ER. Results of all other efficacy parameters were equivalent, indicating equianalgesia was achieved. The mean daily dose of oxycodone CR was 91.9 mg versus 45.9 mg for oxymorphone ER, an equianalgesic dose ratio of 2:1. Karnofsky scores were 81% for patients taking oxycodone and 82% for patients taking oxymorphone ER, equating to normal activity with effort. Rescue medication use was low in both groups; however, fewer patients receiving oxymorphone ER required rescue. Opioid adverse events were similar between groups. Conclusions: Patients taking oxycodone CR can convert to oxymorphone ER at one half the dose and rapidly achieve a stable dose that provides adequate pain relief with similar opioid adverse events. Nearly 90% of patients rated oxymorphone ER as “good,” “very good,” or “excellent.” Original Citation: Poster Presentation; American Society of Clinical Oncology, May 28–June 3, 2003, Chicago, IL. 43—PREDICTING EMETOGENICITY OF NEW CANCER CHEMOTHERAPY AGENTS. Terenzi L, Waddell J, Walter Reed Army Medical Center. E-mail: [email protected] Objective: Serotonin receptor antagonists are standard of care for prevention of acute cancer chemotherapy induced nausea and vomiting. To guide the use of serotonin receptor antagonists, Hesketh et al. classified cancer chemotherapy agents according to frequency of acute emesis. Their classification remains unchanged since 1997 and several new agents are on the market since then. Our objective is to classify new cancer chemotherapy agents by emetogenicity according to the Hesketh nomogram. Methods: Literature searches will be conducted to find emetogenicity data from the serotonin antagonist era for a subset of agents in the Hesketh nomogram. This data will be used to determine ratios of pre-serotonin versus serotonin era emetogenicity for these agents. If there is a consistent ratio for all agents or consistent ratios within drug classes, this information will be used to predict the emetogenicity of new agents. Literature searches and data analysis will be conducted by the oncology pharmacy residency program director and oncology pharmacy resident at an academic military medical center. Results: NA. Conclusions: NA. 44—THE CHALLENGE: ACHIEVING ADEQUATE ORAL ANTICOAGULATION IN ONCOLOGY PATIENTS WITH DEEP VEIN THROMBOSIS. Swenson C, Shaw D, Berry J, Madigan Army Medical Center. E-mail: [email protected] Objective: Recently published studies suggest higher rates of both recurrent deep-vein thrombosis (DVT) as well as bleeding in oncology patients treated with warfarin. To help assess the risk–benefit ratio of warfarin versus low molecular weight heparin or other options for this population, the rate of therapeutic anticoagulation in patients with DVT with or without an oncology diagnosis at our institution was needed. Methods: A retrospective, comparative study of patients receiving oral anticoagulation with a diagnosis of DVT and an oncology diagnosis versus no oncology diagnosis was undertaken. A query of the institutional database for the 800 active anticoagulation clinic patients who also carried an oncology diagnosis yielded 150 patients. A further screen for DVT diagnosed within the last 12 months yielded 27 patients. A control group of 27 patients with DVT but without an oncology diagnosis was identified using the anticoagulation clinic database. The diagnosis of DVT was confirmed by usual tests (ultrasonography). The demographics of the groups were similar: Average age (years): nononcology = 66.6, oncology = 61.6; sex (men/women): nononcology = 10/17, oncology = 13/14. The international normalized ratio (INR) values for analysis were included after the patient was in the 2.0–3.0 range for two values and the percentage of values in range calculated. Results: The percentage of INR values in range was much higher for the nononcology DVT patients versus oncology DVT patients: 70.7% (220 of 311 patients) versus 42% (268 of 636 patients). The range and median for the percentage of therapeutic INRs for the nononcology DVT patients versus oncology DVT patients: 25–90%, median 72%; 0–80%, median 47%. Conclusions: This retrospective comparative study of the rate of therapeutic anticoagulation in patients with DVT with or without an oncology diagnosis at our institution demonstrated results similar to those in the published literature. These data will be key in assessing other therapeutic options for these patients. 45—USE OF MIXED-EFFECT MODELING TO DETERMINE THE INFLUENCE OF ALBUMIN, BILIRUBIN, VALPROIC ACID, WARFARIN, AND ASPIRIN ON PHENYTOIN UNBOUND FRACTION AND PHARMACOKINETICS. Bauer L, University of Washington. www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 46—USING THE OUTCOMES PHARMACEUTICAL HEALTH CARE CASE MANAGEMENT SYSTEM AS A DATA COLLECTION TOOL FOR RESEARCH. Zillich A, Purdue University, Kumbera P, Outcomes Pharmaceutical Health Care, Carter B, University of Iowa. E-mail: [email protected] Objective: To describe a system for collecting research-based data from community pharmacy programs. Methods: The Outcomes Case Management System (OCMS) is a Web-based patient care system. The system assists payers in implementing disease management programs while simultaneously offering pharmacists a method to bill for services provided. For pharmacists, patient-specific information can be captured, enabling pharmacists to maintain progress notes and document patient care services. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 OCMS identifies patients who qualify for services and reminds pharmacists about the types of assessments needed at each visit. A variety of reporting capabilities track clinical and service data for individual patients or groups. For payers, researchers and program managers, OCMS captures service data for quality assurance monitoring. Advanced administrative features of OCMS offer customized patient care protocols that detail patient visit frequency, types of services needed, and specific monitoring parameters (i.e., blood pressure, blood glucose, cholesterol). Pharmacist fees are calculated using a unit rate set by the payer for various services and clinical assessments. Fees can also be adjusted based upon percent or fixed dollar patient copayments. These data can be used for research purposes to evaluate pharmacy-based services. No additional data entry is required, and the system interfaces with a relational database. Data are captured via an encrypted and password-protected hyperlink. Recently, OCMS was tailored for use during a clinical research study conducted in 12 community pharmacies. The study evaluated a pharmacist-based home blood pressure monitoring program. The program consisted of four face-to-face visits with a trained pharmacist. In general, the visits lasted 15 to 60 minutes. Pharmacists were required to document all patient care activities and submit data via OCMS. As data were submitted, a claim was generated by the pharmacist to receive reimbursement for the service. Pharmacists were paid a set fee for each service visit. All claims data were instantly transferred to a relational database. The database was queried to provide researchers with the data collected in the pharmacies. Results: A total of 398 visit claims were submitted. Appropriate data, without specific patient identifiers, were transferred to researchers for analysis. Research personnel reported that the data were clean and easy to manage for analyses. Conclusions: OCMS can be used effectively for collection of research-based data. 47—VALUE OF SPECIALTY CERTIFICATION IN PHARMACY. Pradel F, Palumbo F, Flowers L, Mullins C, Haines S, Roffman D, University of Maryland at Baltimore. E-mail: [email protected] Objective: The purpose of this project was to develop a white paper addressing the value of Board of Pharmaceutical Specialties (BPS) certification. Our work primarily focused on the value of pharmacy specialty certification as perceived by different stakeholders (pharmacists, employers, government, and academia). We also examined specialization and certification in medicine to draw a parallel between the two disciplines. Methods: We searched electronic databases (Medline, International Pharmaceutical Abstracts, Sociological Abstracts), association/health care organization Web sites, and outside reports. Finally, clinical pharmacists involved in certification processes were consulted. Results: Board certification is perceived as valuable in a number of instances. Certified pharmacists report enhanced feelings of self-worth, improved competence, and greater marketability. Other values of certification include increased acceptance by health care professionals, salary increases, and job promotion. Employers acknowledge board-certified pharmacists through public recognition, increases in responsibility, and some type of monetary compensation. In a few governmental organizations, certified pharmacists receive salary raises and are granted prescribing authority. About one third of colleges of pharmacy in the United States also consider board certification as a criterion for promotion and tenure, and, to a lesser extent, for salary increases. In contrast, the overall value of specialty certification in pharmacy as perceived by the public or payers lags behind when compared with the status of specialty certification in medicine. Conclusions: The Board of Pharmaceutical Specialties needs to, in collaboration with pharmacists, further document and promote the value of certification to various stakeholders. 48—WOMEN’S USE OF INFORMATION SOURCES IN THE TREATMENT OF MENOPAUSE. Jackowski R, Kirking D, Huston S, University of Michigan. E-mail: [email protected] Objective: Recent studies regarding hormonereplacement therapy (HRT) have caused women to rethink decisions regarding its use. In light of the controversy surrounding HRT use, we sought to explore what sources women use for information regarding their decision to treat menopause. Thus, the objectives of this study were to (1) identify sources women use, ascertain their understanding of those sources, and assess how helpful sources were in influencing decisions to use HRT and (2) determine how these factors vary by patient characteristics, including HRT user status and presence of diabetes mellitus. Methods: A cross-sectional mail survey was used. Data were collected from women with and without diabetes mellitus aged 45 to 60 years who met specified inclusion criteria and were enrolled in a southeastern Michigan health-maintenance organization. Results: A total of 765 usable responses were obtained from 1,812 eligible, deliverable surveys (42.2%). The most frequent information source was physicians, followed by magazines/print publications, friends, and family, (80%, 57%, 48% and 43%, respectively). Pharmacists were used as an information source by 17% of respondents. The most trusted sources were physicians, pharmacists, and other health care professionals (82%, 59%, and 56%, respectively), with similar results for the most knowledgeable and helpful sources. Least trusted were print ads, television ads, television programs and the Internet (34%, 34%, 25%, and 13%, respectively). These sources were also most thought to be biased or to have a vested interest in promoting a particular view. Results show differences in trust among sources by various personal characteristics, including diabetes status. Three distinct groups were shown to be trusted differently by respondents: health providers, family and friends, and various media. Journal of the American Pharmacists Association 237 2004 Abstracts of Contributed Papers E-mail: [email protected] Objective: Because phenytoin is a drug with a low hepatic extraction ratio, the unbound fraction of drug in the serum influences its pharmacokinetics and interpretation of serum concentrations. The objective of this study was to use NONMEM to determine the effects of the above characteristics on phenytoin pharmacokinetics. Methods: A total of 637 hospital inpatients taking phenytoin for seizures were studied; 57% of the patients took one or more of the other drugs, and 32% of the patients had abnormal albumin (<2.5 g/dL) and/or total bilirubin (>1.5 mg/dL). Steadystate phenytoin total and unbound concentrations were measured using the TDx assay system (coefficient of variation <7%); ultrafiltration was performed at 25º C. NONMEM was used to fit concentration data to pharmacokinetic (steady-state Michaelis–Menten equation) and statistical models. Regression equations that related patient characteristics and other drug doses to population pharmacokinetic parameters were constructed using standard NONMEM techniques. Statistical significance was determined by computing changes in the objective function (chi square >3.841, P <.05). Clinically relevant changes were determined for each factor by when unbound fractions exceeded 15% or changes in pharmacokinetic parameters exceeded 25%. Results: These patient covariates were statistically significant and caused unbound fractions of more than 15%: albumin <2.7 g/dL, total bilirubin >2.1 mg/dL, warfarin >4 mg/day, valproic acid >750 mg/day, aspirin >1,300 mg/day. These patient covariates were statistically significant and decreased the maximum rate of metabolism (Vmax) by more than 25%: albumin <2.5 g/dL plus total bilirubin >3 mg/dL, valproic acid >500 mg/day. Conclusions: Unbound concentrations and unbound fractions of phenytoin should be measured in patients with characteristics that alter protein binding. When patients have more than two covariates present, the unbound fraction can be as high as 30% to 40%. Phenytoin doses should be reduced by 25% or more in patients with characteristics that decrease Vmax values. FEATURE FEATURE Annual Meeting Abstracts 2004 Conclusions: Except for physicians, sources used most frequently by women were not always considered to be the best sources of information regarding treatment of menopause. 49—WORK AND COST ANALYSIS OF PHARMACEUTICAL CARE DELIVERED BY PHARMACISTS IN PRIMARY CARE CLINICS. Helou L, Sorensen T, University of Minnesota. E-mail: [email protected] Objective: (1) Identify the amount of revenue generated by clinical pharmacists in primary care settings and compare this amount with the pharmacy personnel cost of service delivery and (2) model potential patient-care revenues using a resourcebased relative value scale (RBRVS) for reimbursement of pharmaceutical care. Methods: Clinical pharmacists practicing in four Minnesota primary care clinics will record workload and clinical data for patients evaluated during a 4week period in October and November 2003. Billing in these clinics is accomplished via cash payment, “incident-to” billing, and/or institutional provider fees. Data collected will include but are not limited to: reason for pharmacist assessment, time committed to encounter, number of drugs and medical conditions reviewed during assessment, and number of drug therapy problems identified. Revenue collected, as cash or from third-party payers, from each encounter will be identified and compared with workload data. Workload and clinical data collected will be used to model projected revenues using a RBRVS for pharmaceutical care reimbursement that models the RBRVS applied to medical reimbursement for medical care. Results: Results of this project will allow determination of the cost–revenue differential for the delivery of pharmaceutical care in a primary care setting. Data collected will allow for a prospective modeling of the cost–revenue differential using a RBRVS for pharmaceutical care. Conclusions: The mechanism by which pharmacists will be reimbursed for pharmaceutical care, should these services be included in Medicare insurance plans, is unknown. Reimbursement may model the RBRVS of medical provider reimbursement. This project will allow prospective evaluation of one proposed RBRVS for pharmaceutical care. 50—EMERGENCY CONTRACEPTION PILLS—EDUCATING PHARMACISTS UTILIZING A CONTINUING EDUCATION PROGRAM. Morawiec K, Northeastern University, Dougherty T, Presbyterian Medical Center, Penn Family Care. E-mail: [email protected] Objective: To develop, conduct, and assess the effectiveness of an interactive, multidisciplinary continuing education (CE) program about emergency contraception pills (ECPs). Methods: A unique CE program about ECPs, practice guidelines and state/federal legislation was created for pharmacists practicing in Massachusetts. Pharmacists were invited to attend through pharmacy associations, E-mails, faxes, and site visits. A variety of learning methods were used: lecture, case- 238 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 based discussions, and video-counseling sessions. Pamphlets in English and Spanish were developed and distributed to participants to facilitate patient counseling in their practice settings. The presenters panel consisted of a physician, faculty pharmacist, and assistant director for the Massachusetts Health Department family planning program. Participants completed a voluntary pretest survey to assess knowledge, medical practices, attitudes, and patient encounters. A posttest survey was mailed 3 months later. A comparison of the pretests and posttests were used to assess the program’s effectiveness. Results: The program was attended by 21 pharmacists—12 community, 6 hospital, and 3 faculty pharmacists. Of 19 participants, 37% felt confident, 56% felt unconfident, and 5% felt very unconfident in the accuracy of ECP information they were providing. Of the 12 community pharmacists, 67% rarely or never discussed ECPs when counseling patients receiving prescription contraceptives. Among all participants, 81% knew ECPs were most effective when used within 72 hours after unprotected sex, and 43% did not know that progestin-only ECPs are more effective than combined ECPs. Results of the posttest survey will be presented and compared. Conclusions: The program may be an effective method of education as measured by the increased number of pharmacists counseling patients about ECPs and improved confidence in knowledge accuracy about ECPs. 51—PRESCRIPTION ASSISTANCE AND MEDICATION MANAGEMENT FOR SENIORS. Herndon A, School of Pharmacy, Roth M, University of North Carolina at Chapel Hill. Email: [email protected] Objective: Senior Care, a prescription drug program for North Carolina seniors, covers 60% of the first $1,000/year for select prescription drugs. This includes medications used to treat cardiovascular disease, chronic obstructive pulmonary disorder (COPD), and diabetes. The program also funds 23 Medication Management Centers across the state to assist seniors in appropriate medication use. One of these centers, the University of North Carolina (UNC) School of Pharmacy, is responsible for providing medication assistance by telephone to seniors in 41 counties not covered by a local Medication Management Center. Methods: Senior Care eligibility requirements are age 65 years or older; annual income less than $17,720 (single individuals) and $23,880 (couples); medications used to treat cardiovascular disease, COPD, and diabetes; Medicaid ineligible; and no third-party prescription coverage. Interested individuals submit an application to Senior Care headquarters. Approved applications are mailed to the Medication Management Center in the senior’s respective county or to UNC. Upon receiving an application, UNC initiates patient contact. The senior is given an opportunity for a telephone interview to determine prescription assistance eligibility and learn more about his or her medications from a pharmacist. After completing the interview, a phar- macist documents the medication history in a letter to the patient. Additionally, a prescription assistance coordinator searches for prescription assistance programs for which the patient may qualify. The pharmacist’s letter along with applications for assistance programs are mailed to the patient. This concludes the patient encounter. Results: To date, 354 individuals have been contacted. Of these, 162 (46%) have been interviewed, and 98% of interviewed individuals received a pharmacist’s letter and applications. Some 2% were ineligible for prescription assistance, but received a pharmacist’s letter. The remaining 54% were unreachable or declined participation. Conclusions: Although 50% of Senior Care-eligible individuals are reached and the majority receive application packets, the program has limited ability to reach those in need and to detect meaningful outcomes because of lack of follow-up. APhA–APPM Community & Ambulatory Practice 52—ADHERENCE TO ANTIDEPRESSANT MEDICATIONS. Krueger M, Asher C, Mancuso L, U.S. Army Medical Department, Chou C, Pfizer, Inc. E-mail: [email protected] Objective: To assess medication adherence rates in an ambulatory setting. Methods: Design: A convenience sample of 98 patients completed a four-question validated survey (Adhere Rx). As a follow-on study, we conducted a retrospective analysis of antidepressant prescription data using the Standardized Therapy Adherence Research Tool (START). Participants: Military health care beneficiaries receiving new prescriptions during the pilot study and 5,830 patients receiving 16,800 prescriptions in the follow-on study. Analysis: After being stripped of patient identifiers, antidepressant (bupropion, citalopram, fluoxetine, mirtazapine, nefazodone, paroxetine, sertraline, trazodone, venlafaxine) prescription data from January 2002 through June 2003 were placed into a Microsoft Access 97 database. We employed a washout period to avoid bias and to be reasonably certain that all first instances of prescriptions included in the transformed database were new starts, leaving a population of 2,571 patients. Results: During the pilot study, the majority of respondents (84.7%) self-reported adherence scores in the medium or high categories. There was no correlation between medication adherence score and the number of medical conditions. There was, however, a correlation between medication adherence score and the type of medical condition, namely depression, anxiety, allergy, and asthma. Having a concern with antidepressants, we decided to examine general population results using START. The average length of therapy for SSRIs was 130.3 days, compared with 111.1 days for non-SSRIs. There was a higher median gap (44.8) for SSRIs versus non-SSRIs (30.7). Persistence on SSRI therapy at 3, 6, and 12 months was 74, 63, and 42 percent, respectively, while persistence on non-SSRI therapy at 3, 6, and 12 months www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 was 58, 41, and 18 percent, respectively. Fluoxetine, trazodone, and nefazodone had higher switch rates. A limitation is that our database likely did not include solely those with depression since some of these medications were being used to treat insomnia, migraine headache prophylaxis, or anxiety. Conclusions: Medication adherence is the use of the right drug in the correct dose at the right interval. Brief questionnaires can help pharmacists target individual patients for additional counseling. START is a powerful statistical tool to examine pharmacy claims databases to determine rates of medication adherence. Assessment of adherence rates uncovers opportunities for improvement in pharmaceutical care. 54—BILINGUAL OVER-THE-COUNTER PRODUCT LABELS TO ENHANCE PRODUCT USE. Sansgiry S, University of Houston. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 55—BLOOD PRESSURE CONTROL OF ELDERLY HYPERTENSIVE PATIENTS WITH PHARMACEUTICAL CARE INTERVENTION AND HOME BLOOD PRESSURE MONITORING. Christian M, Johnson & Johnson. E-mail: [email protected] Objective: To assess the effectiveness of pharmaceutical care intervention, medication-use review, and home blood pressure monitoring for blood pressure control in elderly hypertensive patients. Methods: Eligible patients were entered into this prospective, controlled 4-month, two-phase study. Blood pressure was recorded and quality of life (QOL) assessments made using the 36-item short form (SF-36). During the initial (control) phase, blood pressure was monitored monthly by a trained health care professional without pharmaceutical care interventions. Weight and pulse were measured monthly. Patients were maintained on their medication regimen, adjustments only made as per standard of care. At the start of the second (intervention) phase of the trial, patients were administered the QOL survey. Monthly, patients received medication counseling, disease education, lifestyle modification counseling, and instruction on using a home blood pressure monitor. Monthly, patients had blood pressure monitored by a health care professional. Weight and pulse were measured monthly. At the conclusion of the trial, the QOL assessment was administered once again. Results: During the control phase, patients exhibited a mean elevation in both systolic and diastolic blood pressure from baseline. Heart rate remained virtually unchanged, and weight was reduced an average of 2 pounds, corresponding to a mean reduction of BMI. QOL assessment, using SF-36, showed an improvement in six of eight categories in the intervention group over the control group. General health category scores were improved 31.7% over baseline in the intervention group, compared with a 17.8% decline in general health score for the control group. During the intervention phase, systolic and diastolic blood pressures were reduced by an average of 3.25 and 0.4 mm Hg, respectively. Heart rate remained stable, and weight loss was observed in 7 of 12 patients for a mean reduction of 3 pounds (a mean reduction in BMI of 3.8%). Conclusions: Data presented demonstrate that active, monthly pharmaceutical care intervention along with home blood pressure monitoring was effective in blood pressure control of elderly hypertensive patients. Patient QOL can be significantly improved after pharmaceutical care intervention. Weight reduction was also enhanced with active pharmaceutical care intervention. 56—CHANGING BEHAVIOR TOWARDS OSTEOPOROSIS PREVENTION: DOES SCREENING LOCATION MATTER? Scolaro K, Stamm P, Lloyd K, Auburn University. E-mail: [email protected] Objective: To determine if adherence to pharmacist recommendations for osteoporosis prevention differs by screening setting. Methods: Nonrandomized prospective analysis conducted in two chain community pharmacies (CP) and one nondispensing pharmaceutical care center (PCC) in suburban Alabama. The sample consists of 200 adult men and women. CP recruitment efforts include flyers, pharmacy staff referrals, and patient self-referrals. PCC patients are recruited during routine visits. Eligible patients complete an intake form collecting demographic data, basic medical information, osteoporosis risk factors, and current preventative behaviors (calcium and vitamin D use and exercise). Patients are then screened using the Achilles Express Ultrasound, educated about their results, and given recommendations to reduce osteoporosis risk. Follow-up surveys are mailed to each patient screened. Surveys are used to determine patient adherence to recommendations and patient satisfaction. Results will be compared to see if adherence or satisfaction differs according to screening setting. Nominal data (e.g., gender) will be analyzed using descriptive statistics. Differences in nominal data Journal of the American Pharmacists Association 239 2004 Abstracts of Contributed Papers 53—AN EVALUATION OF THE IMPACT OF A PHARMACY BASED LATENT TUBERCULOSIS INFECTION COMPLIANCE CLINIC ON COMPLETION RATES OF ISONIAZID IN A COLLEGE STUDENT POPULATION. Goad J, Johnson K, University of Southern California, Milani H, Longs Drug Stores. E-mail: [email protected] Objective: To determine if a pharmacist-managed latent tuberculosis infection (LTBI) clinic in a university community pharmacy improves the completion rate of isoniazid (INH) therapy for students. Methods: Data were retrospectively collected from pharmacy and medical records at the campus pharmacy and student health center. Using pharmacy records, all students receiving INH between January 1999 and May 2003 were identified. Those patients on antituberculosis medications other than INH were excluded. The resulting set of patients was matched to student health center medical records. Students were excluded if they did not meet CDC guidelines for low INH toxicity risk. A community pharmacybased LTBI compliance clinic for INH therapy had been initiated in August 2000. The pre-LTBI pharmacy clinic group A (January 1999 to July 2000) was managed completely by student-health clinicians, and the pharmacy-managed group B (August 2000 to May 2003) was referred by student health for all follow-up care at the pharmacy. Before June 2000, LTBI in non-HIV patients was treated with a 6month course of INH, while later patients received the currently recommended 9 months of therapy. Results: A total of 86 patients were included in group A, while 118 patients were in group B. The average age in both groups was 25 years, and the ethnicity of group B was primarily Asian. The completion rate in group A (6 months or 180 doses in 9 months) was 36%, compared with 65% in group B (9 months or 270 doses in 12 months). The rate of adverse drug reactions to INH in group A was 1.2%, while in group B it was 11%, most likely reflecting the infrequent visits with clinicians in group A. Conclusions: A community pharmacy-based compliance clinic may significantly increase the rate of INH completion for LTBI treatment. E-mail: [email protected] Objective: The objective of this study was to develop and evaluate bilingual (Spanish and English) product information labels (PILs) for overthe-counter (OTC) medication products to enhance comprehension of product-use information. Methods: A randomized experimental study design was developed using three different label formats: new OTC labels, old OTC labels, and PILs. Data were collected from consumers in the process of selecting OTC medications from the pharmacy stores in the Houston area. Participants were classified into three groups—English monolinguals, Spanish monolinguals, and English/Spanish bilinguals. Each participant evaluated three label designs in random order after which they completed a questionnaire that measured dependent variables such as ease of use, product knowledge, attitude toward product label, product evaluation, and purchase intention. The questionnaire was provided in both English and Spanish languages. Demographic variables measured include age, gender, marital status, race, income, education, employment status, and prior medication use. Data were coded and analyzed to evaluate the effect of PILs as compared with other label designs. Results: A total of 336 subjects participated in the study. Participants had a mean age of 38.7 (± 12.2) years with a higher distribution of women (59.2%) and Hispanics (69%). The multivariate analysis of variance (MANOVA) test showed significant effect of label design on all dependent measures (P < .001). Scheffé post-hoc tests showed that PILs were significantly superior to the current OTC label formats, and the results were consistent across all dependent variables measured. Conclusions: This study highlights the need for better information sources for OTC medications, especially for the growing Hispanic population. PILs provide a valuable solution to the concerns of the Spanish-speaking communities who may have difficulty reading or understanding current OTC labels. FEATURE FEATURE Annual Meeting Abstracts 2004 will be assessed using chi square analysis. Interval data will be analyzed using means, standard deviations, and Student’s t test for paired data. Results: Screenings are ongoing; the following data are aggregate. A comparison by setting will be presented. A total of 92 patients (81 CP, 11 PCC) have been screened, including 88 (96%) women. Mean (± SD) age is 48 ± 18 years. Patients average 2.7 ± 1.6 risk factors for osteoporosis, and the mean (± SD) T score is –0.2 ± 1. A total of 221 osteoporosis-specific recommendations have been made: 67 to increase calcium, 53 to increase vitamin D, 50 to initiate or increase weight-bearing exercise, 25 to obtain a diagnostic scan, 6 to reduce modifiable risk factors, and 20 miscellaneous. Some 54 (59%) patients returned evaluable surveys, and 16 of 37 (43%) responders had followed calcium recommendations, and 14 of 30 (47%) responders followed the exercise recommendations. On a scale of 1 to 10 (1 = very dissatisfied; 10 = very satisfied), patients rated the screening service at 8.9 ± 2.5, and all reported that they would recommend the service to a friend. Conclusions: Preliminary results indicate patients do change behavior, are highly satisfied with osteoporosis screenings conducted by pharmacists in the community setting and in nondispensing pharmaceutical care centers, and would recommend the service to others. 57—COMPARING THE RISK FOR OSTEOPOROSIS IN HISPANIC AND CAUCASIAN WOMEN BASED UPON BONE DENSITY MEASUREMENTS OBTAINED FROM COMMUNITY HEALTH SCREENINGS. Alvarez G, Nova-Southeastern University, Marsh W, Hunter T, Droege M, Nova Southeastern University. E-mail: [email protected] Objective: The objective of this study was to determine whether Caucasian–Hispanics are at a significantly lower risk than are non-Hispanic Caucasians for development of osteoporosis. Osteoporosis, a debilitating bone disease defined by decreased mass and altered bone micro-architecture, results in increased bone fragility and increased risk of fracture. The World Health Organization defines osteoporosis as a T score 2.5 standard deviations below the mean for young adult controls. All women, regardless of race, are at risk of developing osteoporosis; however, Caucasian or Asian women are commonly considered being at higher risk. Hispanics in the United States are of Mexican, Puerto Rican, Cuban, Dominican Republic, Central American, or South American descent; many Hispanics in South Florida are of Caucasian heritage. Whether osteoporosis risk differs based upon heritage within the Hispanic population is unknown. If health care providers mistakenly believe that some are not at risk for this disease, opportunities for appropriate prevention may be forfeited. Methods: Bone density measurements were used to assess the osteoporosis risk in 627 men and women in South Florida. Each subject self-reported gender, age, and race. Bone density measurements were obtained using a Hologic Sahara Bone 240 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Sonometer and T scores were calculated. Data are presented for 353 (209 Hispanic and 144 Caucasian) women over the age of 55. Results: The overall mean T score for the group was –1.229 with a standard deviation of 1.0385. The mean T score obtained for Hispanic women was –1.194, compared with –1.280 for Caucasian women. An independent Student’s t test for paired data confirmed that there was no statistically significant difference between the groups (t = 0.76, P = .47). As expected, the correlation between the obtained T score and age was negative (r = –.36), reflecting bone loss with increasing age. Conclusions: This study indicates that Hispanic women of Caucasian heritage are at equal risk of developing osteoporosis as Caucasian women. 58—CONSUMER ATTITUDES TOWARD THE OVERALL VALUE OF THE PHARMACIST AS A DRUG INFORMATION SOURCE. Rollins B, Sullivan D, Ohio Northern University. Email: [email protected] Objective: Consumers consistently view the pharmacist as one of the most trusted and respected professionals, but do they truly view the pharmacist as a valuable source of drug and medical information? The pharmacist, especially in the community setting, is the one of the most accessible and reliable sources of drug information for the consumer. However, are there barriers preventing consumers from seeking the pharmacist’s advice? The purpose of the study is to assess consumer attitudes toward the overall value of the pharmacist as a drug information source. The researchers will attempt to answer the following research questions: (1) Consumer attitudes toward the availability and approachability of the pharmacist; (2) is the pharmacist seen as a true patient advocate; (3) who do consumers seek to answer their drug information questions; and (4) do consumers prefer written drug information or pharmacist counseling? The fourth research question is based on the results of a previous study in which consumers slightly to moderately agreed they would rather have a voluntary package insert versus personal instruction from the pharmacist regarding the use of a corticosteroid nasal spray (mean = 4.49 ± 1.268; scale: 1 = strongly disagree to 6 = strongly agree). Methods: Consumers were selected for inclusion in the study from a database of Ohio residents between the ages of 18 and 70. A sample size of approximately 140 consumers was calculated based on a priori alpha of .05, beta of .20, and power of .80. Based on an estimated response rate of 35%, 400 consumers will be randomly selected through simple random sampling from this database. The survey instrument is a self-administered mailed questionnaire. The questionnaire uses approximately 35 questions to assess the four research questions. Data will be analyzed using descriptive statistics and Student’s t test for paired data. Demographic differences (gender, age, education level) will also be analyzed. Results: Data collection ongoing. Conclusions: Data collection ongoing. 59—CREATING THE CAPACITY FOR CASE MANAGEMENT IN A COMMUNITY PHARMACY. McDonough R, Doucette W, Musick J, Klepser D, McCarthy R, University of Iowa. E-mail: [email protected] Objective: Main at Locust Pharmacy Clinic developed and implemented a process to provide case management services for the Iowa Medicaid Pharmaceutical Case Management (PCM) Program. The objective of this report is to describe the patient care processes and forms that were developed to provide case management services for eligible patients. Methods: Design: A descriptive overview of the patient care processes developed and implemented at the pharmacy to provide efficient and effective care to eligible Medicaid patients. Setting: An independent community pharmacy Patients: Medicaid recipients who were taking four or more long-term oral medications and had one or more of the 12 disease states that are costly to Iowa Medicaid (heart failure, coronary artery disease, diabetes mellitus, hypertension, hyperlipidemia, asthma, depression, atrial fibrillation, osteoarthritis, gastroesophageal reflux disease, peptic ulcer disease, and chronic obstructive pulmonary disease) Data Collection: A description of the patient care process that evolved over the 2year period is provided. Patient care forms and physician communication tools that were developed to improve the efficiencies of the patient care process are discussed and shared. The number of patients enrolled, the number of drug therapy problems found, and the physician response to pharmacists’ recommendations is described. Analysis Plan: Description of the patient care process Results: Over a 2-year period, 259 patients met eligibility criteria. The clinic enrolled 153 patients into the program. Patient care processes were developed and patient care forms created. Communication forms were developed that improved the physician response rate to the pharmacists’ recommendations. Pharmacists found 901 drug therapy problems over the 2-year period. Physicians responded to pharmacists’ recommendations approximately 60% of the time. In 48% of the cases, pharmacists’ recommendations led to a documented change in patients’ medications. Conclusions: Pharmacists at Main at Locust Pharmacy Clinic were successful in developing and implementing case management services in a patient population considered at high risk for drug therapy problems. 60—DETERMINING THE EFFECT OF MEDIA RELATIONS ON PHARMACISTS. Ferreri S, University of North Carolina at Chapel Hill, Coffey C, Mercer University Southern School of Pharmacy. E-mail: [email protected] Objective: (1) To address if pharmacists have interacted with media. (2) Report if pharmacists receive communication or media training. (3) Identify how pharmacists could improve their interaction with the media. Methods: The members of the OTC Media Advisors network were chosen based on the criteria of knowledge of OTC medications, availability to www.japha.org March/April 2004 Vol. 44, No. 2 FEATURE Annual Meeting Abstracts 2004 the need to regulate was different from that in 1906. In 1962, the Kefauver–Harris amendments to the FFDCA transferred regulatory authority over prescription drug advertising from the FTC to the FDA. The FTC retained regulatory authority over advertising of nonprescription products. The first U.S. direct-to-consumer (DTC) advertisements for prescription medications were issued by Boots Pharmaceuticals for Rufen in 1981. This was followed by advertisements for Merck’s Pneumovax vaccine. The FDA Commissioner issued a formal request to the industry for a moratorium on DTC advertisements while FDA considered its position. Subsequently, FDA issued a Federal Register notice asserting its jurisdictional authority and stating that DTC ads must meet the same legal requirements as other prescription drug advertising. In 1997, FDA issued a draft guidance on consumer-directed broadcast advertisements and subsequently issued a final guidance on this in 1999. This opened the door to the plethora of DTC advertisements presently seen in the United States. This paper presents the history and current regulation of DTC advertising in the United States, DTC activities in other countries, and legislative activities designed to control DTC advertising. 290—WASHINGTON’S UNIFORM HEALTH CARE INFORMATION ACT: A STRONG EXAMPLE OF STATE LAWS THAT ARE NOT PRE-EMPTED BY HIPAA. Fassett W, Washington State University, Hazlet T, University of Washington. E-mail: [email protected] Objective: To compare the requirements of Washington state’s Uniform Health Care Information Act of 1991 with the provisions of the Federal Health Information Portability and Accountability Act (HIPAA) of 1996, and with the requirements of the U.S. Department of Health and Human Services’ Privacy Procedural Enforcement Rule adopted in 2003; and to assess potential compliance issues for practicing pharmacists and pharmacies. Methods: Design: Comparative legal analysis. Setting: Single state law and regulation compared with federal law and regulation. Analysis: Provisions of the laws and regulations were compared to identify any standards in Washington that were more stringent and not pre-empted by federal law. Samples of pharmacy notices of privacy practices were collected at independent and chain pharmacy sites or via the Internet to examine whether the statements conformed with Washington law as well as federal law. Results: The basic provisions of Washington law and HIPAA are similar. Certain provisions of Washington law are more stringent than HIPAA, particularly in the handling of requests by patients to view their records, consent by minors, and handling of military record requests. Washington Board of Pharmacy rules preclude certain disclosures without written consent that would be allowed under HIPAA rules. Considerable variation exists among Notices of Privacy Practices regarding the particulars of Washington laws, and pharmacies that do mention Washington specifics have not consistently interpreted the Washington statute. 300 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Conclusions: Procedural compliance with Washington law will likely result in compliance with HIPAA. However, compliance with HIPAA procedures, particularly in dealing with requests for records, will not assure compliance with Washington state rules. These results suggest that notices of privacy practices in other states may also inconsistently accord with more stringent rules in those jurisdictions. American Institute of the History of Pharmacy (AIHP) 291—“ALWAYS AND EVERYWHERE”— QUININE IN THE AMERICAN CIVIL WAR. Flannery M, University of Alabama at Birmingham. E-mail: [email protected] Hardtack and Coffee (1887), John D. Billings‘ amazingly detailed account of the soldier’s life in the Civil War, states, “Quinine was always and everywhere prescribed with a confidence and freedom which left all other medicines far in the rear” (p. 176). This 15-minute slide presentation will discuss the curious history of quinine during the Civil War from therapeutic and economic standpoints. The paper argues that quinine and its cinchona variants not only played a significant role in therapeutics but its prevalent use in the war provided a proving ground for the remedy of unprecedented proportions. Quinine, it will be argued, was also a catalyst to the wartime boom of pharmaceutical mass production, making Rosengarten & Sons and Powers & Weightman major players in the pharmaceutical market. The talk is supplemented with illustrations of the firms and men who played a major role in its manufacture and distribution along with graphs tracking various economic aspects of quinine during the war years, 1861–1865. 292—18TH AND 19TH CENTURY PRINTED MATERIALS ABOUT THE PURSUIT OF HEALTH AT MINERAL SPRINGS. Lane A, University of Wyoming. E-mail: [email protected] The tradition of people going to special places to restore or maintain their health is a long one, dating from ancient times up to the present. Some natural locations offer bathing and drinks of “healing” spring water; some health resorts offer other attractions. Through the eighteenth and nineteenth centuries, aspects such as increased middle and upper middle class wealth, greater leisure time, and more efficient transportation allowed more people to travel further to seek relief. Promoters emphasized both scientific facts and subjective testimonials in stressing the legitimacy of their establishments. This study will focus on eighteenth and nineteenth century materials in the Toppan Rare Books Library that explain just how, and why, certain diseases and physical problems were said to be helped at particular places. Books and pamphlets to be discussed include: A treatise on the three medicinal mineral waters at Llandrindod, in Radnorshire, South Wales, by Diederick Wessell Linden, MD, 1761; A Sketch of Lebanon Springs (New York), by Daniel Gale, 1872; America’s Baden-Baden, where it is, what it is, and how to get there (Hot Springs, Arkansas), 1879; Invalids & Tourists Hotel, Buffalo, N.Y., by Ray Vaughn Pierce, MD, 1879; Asheville, Western North Carolina, nature’s trundle-bed of recuperation for tourist & health seeker, by Hinton, A. Helper, 1886; Souvenir of Poland Springs (Maine) by Hiram Ricker and Sons, 1890; and Health resorts of the South and summer resorts of New England, 1896. The association, if any, of physicians and pharmacists with these places will be considered. 293—AMERICA’S SECOND OLDEST PHARMACY? Weart C, Karig A, Medical University of South Carolina. E-mail: [email protected] Virtually forgotten in the pages of pharmacy history is one of America’s oldest pharmacies, perhaps the second oldest, which operated in Charleston, South Carolina. Founded in 1781, the pharmacy was operated by a continuous succession of owners until closing in 2002. The pharmacy became known as “Apothecaries Hall” in 1816 and later would be known as “Schwettmann’s,” a name associated with the business until its end. In 1781, Dr. Andrew Turnbull set up an apothecary shop in Charleston. He imported, prescribed, prepared, and dispensed his own medicines acting as both pharmacist and physician. In 1792, Dr. Joseph Chouler took over the practice as physician and apothecary. Dr. Chouler was succeeded by Mr. William Burgoyne who practiced as an apothecary until 1816. Dr. Jacob De la Motta, a prominent Charleston physician, purchased the establishment, enlarged the shop and named it “Apothecaries Hall.” A large golden mortar and pestle sign became its hallmark. In 1845, Dr. William Trott took over Apothecaries Hall from Dr. De la Motta. In 1849 he hired Christian Frederick Schwettmann as a pharmacist’s clerk. From 1863 to 1865 the business was temporarily relocated because of shelling from Fort Sumter. The business narrowed its focus to retail pharmacy and compounded a number of specific remedies under Dr. Trott’s name. In 1870, Dr. Trott sold the pharmacy to his one-time pharmacist’s assistant, Dr. Christian Frederick Schwettmann. Associating with his son, Dr. F. W. Schwettmann, the business became C. F. Schwettmann and Son, Pharmacists and operated until 1915 when it was purchased by Dr. John Hutching. In 1920, the pharmacy moved to a new location. It was renamed the Poulnot Drug Company and managed by Dr. Frederick Poulnot, grandson of the late Dr. C. F. Schwettmann. The pharmacy underwent several ownership and location changes before closing in 2002. 294—AN ILLUSTRATED HISTORY OF THE STERLING DRUG COMPANY. Wendt D, National Museum of American History. E-mail: [email protected] In 2001, the National Museum of American History acquired an outstanding collection of artifacts and archival material from Sterling Drug Inc. This material had been housed and processed by www.japha.org March/April 2004 Vol. 44, No. 2 FEATURE Annual Meeting Abstracts 2004 and counseling provided by a clinical pharmacist on outpatients receiving cancer chemotherapy. Methods: A two-way mixed-design experimental study was conducted during September 2002 to February 2003 at Oncology Unit, Department of Internal Medicine, Rajavithi Hospital, Bangkok, Thailand. A total of 44 subjects were randomly stratified and assigned into experimental and control groups based on the number of cycles of chemotherapy and educational levels. An experimental group of 23 patients received education and counseling, while a control group of 21 patients did not. Outcomes variables were evaluated in terms of: (1) knowledge about disease and treatment, adverse drug reactions, and self-care of patients receiving chemotherapy; (2) clinical changes in the severity of adverse drug reactions and the effectiveness of selfcare when patients had adverse drug reactions; and (3) changes in the quality of life. Data were collected using standardized survey interview and selfassessment questionnaire at baseline and during the first and second follow-up visits while receiving chemotherapy. Two-way ANOVA with repeated measure on one factor and chi-square test were used to analyze data. Results: No statistically significant differences were observed in demographic data, cancer types, and chemotherapy treatment regimen between experimental and control groups at baseline. Results indicated that providing education and counseling had significant effects on knowledge of patients (P < .05), especially concerning knowledge of adverse drug reactions and self-care. The effectiveness of self-care in the experimental group was higher than in the control group significantly (P < .05). However no significant differences in severity of adverse drug reactions and the quality of life emerged between the groups (P > .05). Conclusions: Providing education and counseling by a clinical pharmacist can significantly improve patients’ knowledge and effectiveness of self-care of adverse cancer chemotherapy reactions. 65—EFFECT OF PHARMACIST EDUCATION ON PATIENT KNOWLEDGE OF NOSEBLEED MANAGEMENT: AN ANTICOAGULATION CLINIC INTERVENTION. Hassenplug K, Burkiewicz J, Jackson T, Peppers L, Midwestern University. E-mail: [email protected] Objective: To assess patient knowledge of management of nosebleeds of patients receiving anticoagulation therapy at an ambulatory care clinic in a managed care setting. Our objectives are to determine if pharmacist intervention improves proper management and to decrease risks of complications among patients. Methods: Studies have documented the widespread unawareness of patient management of nosebleeds. Few studies document the improved response in patient management after pharmacist education of patients. Further, these studies did not specifically study higher-risk anticoagulation patients. Paired evaluations of patient knowledge were conducted before and after patient education by 242 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 a pharmacist. The survey included approximately six demographic-based and four knowledge-based questions. Included patients were receiving anticoagulation therapy at the time of presurvey administration (July–August 2003). Patients unable to communicate written or verbally and those who discontinued therapy were excluded. Postsurvey evaluation began approximately 6 weeks after a pharmacist education. The Wilcoxon Signed Rank Test and Bonferroni Correction were used to evaluate data. Results: Of 264 patients in the anticoagulation clinic, 171 patients completed the presurvey (65%), and 148 post surveys have been completed to date. Demographic data reveal that 60% of the patients surveyed were women. The mean (± SD) age of the patients was 71 ± 12.03 years. Significant improvement occurred in the before and after surveys in the following knowledge-based areas: pinching nose (P < .001), placement of pinch (P < .001), plugging nostrils (P < .001), and tilting head forward (P = .01). Final results will be presented at APhA2004. Conclusions: Patient education by a pharmacist increases patient knowledge of proper nosebleed management. Pharmacist intervention has been successful in improving proper compliance of nosebleed management. 66—ESTABLISHMENT OF PHARMACIST CONSULTATION SERVICES AND COLLABORATION BETWEEN HIV CLINICS AND A NONPROFIT PHARMACEUTICAL CARE CENTER SPECIALIZING IN HIV CARE IN ORANGE COUNTY CALIFORNIA. Sherman M, Gotterer H, Center for Advanced Pharmaceutical Care. E-mail: [email protected] Objective: To improve therapeutic outcomes and quality of life for individuals with human immunodeficiency virus (HIV) infections through specialized pharmaceutical care services provided through a collaboration between HIV clinics and a nonprofit pharmaceutical care center. Methods: The Center for Advanced Pharmaceutical Care (CAPC) is a unique, innovative nonprofit facility, specializing in pharmaceutical care services for patients with HIV. The HIV specialist pharmacist collaborates and works with providers at HIV clinics, providing services that have improved outcomes such as: improved adherence, decreased drug–drug interactions, improved understanding of HIV medications and complex regimens, improved health and better quality of life. The collaboration is funded by Ryan White Title I and Title III funding. CAPC is also a rotation site for pharmacy student clerkships from the University of California–San Francisco and University of Southern California pharmacy schools. Future plans include collaboration with an HIV clinic in Long Beach, California, and the University of the Western Cape Pharmacy School in South Africa, to educate pharmacists about HIV and HIV drug therapies and to create a pharmacist consultation program similar to that at the Center for Advanced Pharmaceutical Care in Khayamandi, a township of about 25,000 people near Stellenbosch, South Africa, where 40% of the residents in this township are unemployed. One half of the township is composed of women, and most individuals are from 29 to 49 years of age. Of those with tuberculosis, an estimated 35% are HIV positive. Results: During 2002 the HIV pharmacist had 792 face-to-face patient contacts and 931 other contacts (physicians, nurses, and case managers). The collaboration between the pharmacist and health care team has resulted in improved patient outcomes. Specific outcomes include: improved adherence with drug therapies, improved health, and better quality of life. Conclusions: Pharmacist involvement in the care of HIV-infected individuals is critical especially in the areas of drug therapy counseling, drug interaction monitoring, and adherence. Pharmacist collaboration with the HIV health care team has completed the continuum of care for patients and allowed for effective management of HIV drug therapies, which is the key component to successful outcomes for HIV patients. 67—EVALUATION OF A COMMUNITY PHARMACY NUTRITIONAL EDUCATION PROGRAM FOR PATIENTS WITH DIABETES. Dinh Q, Zgarrick D, Cornell S, Midwestern University. E-mail: [email protected] Objective: To evaluate the effect of a diabetes education program on patient knowledge of the impact of nutrition on their diabetes and their desire to self-manage their disease. Methods: All patients with diabetes who were enrolled in an American Diabetes Association (ADA) recognized Diabetes Education Program at a grocery store pharmacy were invited to participate. Two Certified Diabetes Educator pharmacists (one is also a licensed dietitian) instructed small groups of patients on how nutrition affects their disease in an hour-long session. A quiz was developed to evaluate patient knowledge of the impact of nutrition on their diabetes and their desire to self-manage their disease. The quiz was administered to patients immediately before, immediately after, and 6 months after the educational session. A total of 39 patients were enrolled into the study. Results: Student’s t tests for paired data showed significant increases in patient diabetes knowledge both immediately after and 6 months after their educational session (P < .05). Patients’ ability to pick out carbohydrate-containing foods improved after their session. Patient motivation to self-manage their condition also increased after their session. Conclusions: We conclude that this pharmacistmanaged diabetes education program significantly improve patient knowledge and willingness to selfmanage their condition. 68—EVALUATION OF A MEDICAID PHARMACEUTICAL CARE PROGRAM WITHIN AN INDEPENDENT COMMUNITY PHARMACY IN RURAL IOWA. Belger A, University of Iowa, Osterhaus M, Bullock T, Osterhaus Pharmacy, Currie J, Farris K, University of Iowa. E-mail: [email protected] Objective: We plan to: (1) identify processes required to expand the Pharmaceutical Case www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 69—EVALUATION OF BENZODIAZEPINE UTILIZATION IN A FAMILY MEDICINE OFFICE. Santee J, Howell J, University of Missouri-Kansas City. E-mail: [email protected] Objective: This study was performed to determine whether benzodiazepines are commonly misused, abused, or underprescribed and whether a patient–physician contract changes benzodiazepine utilization in a family medicine office. Methods: The investigators queried a billing database to identify patients of a family medicine office who had been diagnosed with generalized anxiety disorder, insomnia, and/or panic disorder. The charts of identified patients were retrospectively reviewed to gather information on patient characteristics and benzodiazepine utilization since 2001. Patients were classified as misusing if at least twice, they requested a refill for benzodiazepines more than 5 days early. Abuse was defined as sufficient documentation to meet DSM-IV criteria for substance abuse. Underutilization was assessed by identifying patients who had not received benzodiazepine prescriptions despite being appropriate candidates. Impact of the patient–physician contract was deterVol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 mined by comparing the frequency of early refills before and after the contract was signed. Results: A total of 147 patients were identified through the billing database. None could be classified as abusing benzodiazepines, while seven (22%) were identified as misusing these agents. The mean daily dose in terms of diazepam equivalents was 8 mg overall and 26 mg for those who were classified as misusing. Impact of the patient–physician contract could not be assessed as only two of five patients who signed the contract did so after 2001. Some 114 patients had not received a benzodiazepine prescription despite being diagnosed with one or more of these conditions, but only one patient was an appropriate candidate for benzodiazepine therapy. Conclusions: The percentage of patients classified as misusing benzodiazepines was higher than that reported in other studies. The doses of benzodiazepines used, however, were well within the recognized dosing range for these indications and lower than what was seen in the before-mentioned studies. Misuse may therefore be more reflective of an ineffective dose rather than abuse. Underuse of benzodiazepine prescriptions was not common, but the criteria for what was an appropriate candidate for benzodiazepine therapy was strict. 70—EVALUATION OF CARDIOVASCULAR RISK AMONG PARTICIPANTS OF A VIETNAMESE HEALTH AWARENESS PROGRAM. Wong N, Merrigan D, Pfizer. E-mail: [email protected] Objective: Coronary heart disease (CHD) is the leading cause of death in the United States. Major risk factors for the development of CHD are elevated blood pressure, elevated total (TC) and LDL cholesterol, low serum HDL cholesterol, diabetes mellitus, cigarette smoking, and obesity. The objectives of this evaluation were to assess control of blood pressure according to the sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI) guidelines; assess management of hyperlipidemia according to the National Cholesterol Education Program (NCEP) guidelines; and identify participants with undiagnosed hypertension and hyperlipidemia. Methods: Methods included offering cholesterol (TC, LDL-C, HDL-C, TG), blood pressure and glucose screenings to participants at a Vietnamese health awareness program. A questionnaire was used to collect information regarding health plan, treatment for hypertension and hypercholesterolemia and risk factors such as smoking, diabetes and prior history of CHD. Values were recorded in CHD Risk Calculator using scanner technology. Results: A total of 54 participants were screened. The majority of participants (74.1%) described their ethnicity as Asian/Pacific Islander. Results of the screenings showed that 54.4% of participants had a systolic blood pressure greater than 120 mm Hg and 25.9% had a diastolic blood pressure greater than 80 mm Hg, yet only 3.5% reported receiving treatment for hypertension. Cholesterol screenings revealed that 83.3% of participants had a TC greater than 200 mg/dL and 40.7% had a TC greater than 240 mg/dL. LDL-C level of 130 mg/dL or higher was found in 55.7% of participants. However, only 5.4% of participants reported receiving lipid-lowering therapy. Conclusions: The American Heart Association statistics report the median percentage of Asian/Pacific Islander adults who have been informed by a health professional that they have high blood pressure is 16.3% and the median percentage of those informed that they have high blood cholesterol is 27.3%. Findings of the Vietnamese Health Awareness Program suggest a possible gap between disease prevalence and diagnosis and treatment. The results demonstrate a need for improvement in diagnosis and treatment of CHD risk factors among the Asian/Pacific Islander population. Original Citation: American Society of HealthSystem Pharmacists Midyear Clinical Meeting, New Orleans, La., December 7–11, 2003. 71—EVALUATION OF MEDICATION ADHERENCE IN A LOCAL COMMUNITY PHARMACY. Rosiak B, Pfizer, Akinsowon W, Howard University. E-mail: bonnie.jean.rosiak@ pfizer.com Objective: To review general medication adherence taking behavior in patients at a community pharmacy. To determine the relationship between adherence level and other factors (age, sex, payment method, number of prescriptions, costs and adverse effect). Methods: Patients were asked to complete a selfassessment survey tool that included de-identified data on patient’s demographics (sex and age), the Morisky scale, and questions on medication cost. Four patients were excluded from the study due to incomplete data. Descriptive statistics were performed using Microsoft Access and Minitab 12 for Windows. Results: The population includes 65 women and 35 men, ranging in age from 18 to 75 years (mean = 43.5 years). According to the Morisky scale, 19% of patients had low medication adherence, 37% had medium adherence, and 44% had high adherence. About 21% of women had low adherence, compared with 14% of men. Older adults (aged 50 years and older) who were on more than four medications scored higher for adherence to medications than those younger than 38 years of age and on one or two medications. Of all patients, 25% said they stopped taking their medications when they feel worse. Adherence level did not differ by payment type. Of 26 patients not filling their medications because of cost, 39% scored as highly adherent according to the Morisky scale. Conclusions: The Morisky scale can help assess medication-taking behavior but has limitations related to cost issues (e.g., not filling a prescription because of costs). Pharmacists have an opportunity to play an active role to help improve patient’s adherence by assessing patients’ medication-taking behavior and addressing cost-related issues. Journal of the American Pharmacists Association 243 2004 Abstracts of Contributed Papers Management (PCM) program within an independent pharmacy; (2) evaluate patient satisfaction with this program; and (3) evaluate cost effectiveness of this program for this pharmacy. Methods: The Iowa PCM program was implemented in 2000 to serve Medicaid patients with at least four maintenance medications and one of 12 disease states. Pharmacists and physicians collaborate to maximize patients’ care. A 2002 evaluation of the program found improvement in the quality of care patients received and in medication safety. It found no net increase in health care costs. Design: Program implementation and evaluation. Subjects: All individuals receiving PCM in the pharmacy. Program implementation: Participation in PCM will be expanded within a community pharmacy. Program evaluation: An impact and cost-effectiveness evaluation will be conducted. Patient satisfaction surveys using validated questions will be mailed to all PCM patients seen between September 2003 and February 2004. The 15-item survey will use a 5point Likert response scale. Patients will be provided a return envelope and a reminder postcard to obtain high response rates. Costs will be determined using pharmacist salary and benefit expenses for pharmacist time delivering and documenting care. Fees received for care provision will be compiled. Results: Methods used to expand care provision will be described. Satisfaction results will be analyzed using t tests and ANOVA statistics as appropriate. The cost-effectiveness evaluation will describe all revenues generated and expenses incurred in the provision of PCM. Fees received for care provision will be compared with costs and evaluated to determine cost effectiveness. Conclusions: Patient satisfaction and cost effectiveness results will be evaluated to determine where improvements can be made in patient care and if continuation of effort in the program is beneficial. FEATURE FEATURE Annual Meeting Abstracts 2004 72—EVALUATION OF REIMBURSEMENT METHODS UTILIZED BY PHARMACISTS PERFORMING DISEASE STATE MANAGEMENT SERVICES. Beatty S, Mehta B, Rodis J, Ohio State University. E-mail: [email protected] Objective: For pharmacists performing disease management services: (1) determine billing and reimbursement techniques being used, (2) assess the amount pharmacists are being reimbursed, and (3) propose an effective billing and reimbursement technique. Methods: After performing a literature review of pharmacist-based billing and reimbursement techniques, a comprehensive survey will be created to determine geographic location, practice setting, disease management services, billing techniques, and amount of reimbursement for each service. Following survey development, local pharmacists performing disease management services will beta-test the survey and appropriate adjustments will be made. Approximately 1,000 surveys will be sent to all pharmacists with mailing information available through the following lists: APhA Community Pharmacy Residency Preceptors, Anticoagulation Forum, and ACCP Ambulatory Practice and Research Network. Data entry into Microsoft Access will assure avoidance of duplicate mailings. In October, pharmacists will receive an introductory postcard, the survey and postage-paid self-addressed envelope 2 weeks later, and a reminder postcard 2 weeks after that. All surveys will be returned by December 31, 2003. As surveys are returned, responses will be recorded into the Microsoft Access database. Results: Statistical analysis will be performed to assess which practice settings are billing, what type of billing techniques are being used, what disease management services are receiving reimbursement, who is paying for the services, and the approximate amount of reimbursement being received. Conclusions: Results from this survey will provide an overall assessment of the billing techniques currently being used and the approximate amount of reimbursement being received by pharmacists performing disease state management services. It is anticipated that these results will be presented in a publication that proposes an effective way for pharmacists to bill for services to receive reimbursement. 73—HEALTH SCREENING: THE ROLE OF PHARMACISTS IN ASSESSING HEART DISEASE RISK. Glosner S, Pfizer Inc, Tynan S, Lee M, Midwestern University. E-mail: scott. [email protected] Objective: Coronary heart disease (CHD) is the number 1 killer in the United States. Illinois has a higher heart disease death rate than the national average. A health care center in Chicago wanted to help promote preventive cardiovascular disease management. We evaluated patient CHD risk factors (e.g., blood pressure [BP], cholesterol profile, glucose level, tobacco utilization, family history and age) and determined 10-year CHD risk. Methods: Each participant attended an ambulatory care health fair on September 13, 2003. The health fair took place in a southwestern Chicago communi- 244 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 ty. They completed a survey, which captured their CHD risk factors. Their values were scanned into CHD Risk 2001 Software. A health care professional (e.g., pharmacist, physician) reviewed each participant’s CHD risk factors and his or her 10-year CHD risk. All patients received a printed CHD risk health report. A copy of each de-identified health survey was captured into a Microsoft Access database and aggregately analyzed. Results: BP and cholesterol levels were collected on 38 participants. Of the attendees 47% were African American, while 45% and 8% were Caucasian and Hispanic, respectively. The average age was 69.3 years. Body mass index of greater than 25 mg/k2 was noted in 82% of participants. Nearly 8% of those screened smoked tobacco. Three participants had CHD, while six had diabetes. Elevated BP, as defined in the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) guidelines, was present in 42% of participants, while 45% were in the new JNC VII classification of prehypertension. The average BP was 133/76 mm Hg. Total cholesterol level of greater than 200 mg/dL was documented in 82% of participants, and 53% did not meet their NCEP goals. A majority (89.5%) of participants were considered “unhealthy,” with a relative CHD risk higher than standard risk for their age and gender. Conclusions: A majority of the participants (89.5%) were deemed “unhealthy” because of elevated BP, elevated cholesterol, and/or concomitant disease states (e.g., diabetes, CHD). Participants were counseled on lifestyle changes and appropriate BP and lipid-goal attainment by a pharmacist or physician. In addition, patients received their own personalized health report, which contained CHD risk factors and their risk of developing CHD over the next 10 years. Preventive follow-up and education are paramount to controlling and treating patients at risk for CHD. 74—IMPACT OF PHARMACEUTICAL CARE INTERVENTION ON PATIENT ADHERENCE. Mutha N, Unterwagner W, Coffey C, Mercer University, Thurman S, Eckerd Drug Company, Norton A, Mercer University. E-mail: [email protected] Objective: (1) To define reasons for nonadherence; (2) to perform pharmaceutical care intervention to improve patient adherence; (3) to assess improvement in patient adherence before and after pharmaceutical care intervention; and (4) to compare glycosylated hemoglobin A1C (A1C) levels, blood pressure (BP), and number of refills before and after intervention. Methods: Study participants will be selected from Eckerd’s central computer database system. Subjects will be contacted via telephone and asked to participate in the study. Patient will be considered as a nonadherent to their therapy if they have not filled 30-day supply of their medication within last 3 months. All of the participants will be asked to come into the Eckerd’s pharmacy or schedule a visit at another Eckerd location for initial assessment and baseline A1C and BP checks. The initial assessment will consist of a complete medical history and a survey to define patient’s reasons for being nonadherent. The program will consist of defining the reasons for nonadherence (cost, poor education, adverse effects, accessibility, forgetfulness, difficult regimen, multiple pharmacies/samples) as well as finding a pharmaceutical care intervention (cost improvement, education, prevent/treat adverse effects, convenience, memory aid, simplifying regimen, contacting pharmacist) for each individual. The pharmacist will have performed pharmaceutical care interventions for each individual within a period of 3 months. Patients may be followed further to determine improvement in compliance by telephone or bringing them back to Eckerd. At a 6month follow-up visit, the participants will be asked to complete the initial survey assessing improvement in adherence, and their A1C and BP will be measured. At this time, evaluation will be made based on A1C and BP levels before and after the intervention. Improvement in number of refills will be evaluated via rerunning Eckerd’s central computer database by each participant name. The A1C and BP readings will be provided to the patient and to their physicians. The research study will involved approximately 500 participants who have met the criteria. Results: All of the data accumulated will be evaluated via STATISTIX analytical software. Conclusions: Research study in progress. 75—IMPLEMENTATION OF A BREAST CANCER RISK ASSESSMENT AND EDUCATION SERVICE IN A COMMUNITY PHARMACY. Bumgardner M, University of Minnesota, Duluth College of Pharmacy, Giles J, University of Colorado Health Sciences Center. E-mail: mbumgar2 @d.umn.edu Objective: This project evaluated the impact of a community pharmacy-based service for breast cancer risk assessment, education, and risk communication on knowledge of and adherence to American Cancer Society (ACS) guidelines for mammograms and clinical breast exams (CBE). Methods: Design: Women were invited to receive a free breast cancer risk assessment at select community pharmacies and health fairs. Subjects provided informed consent, knowledge of current ACS breast cancer screening guidelines, and a description of current screening practices. Risk assessment was performed using the National Cancer Institute Breast Cancer Risk Assessment software program. Results were discussed with each subject and education regarding 2002 ACS screening guidelines and breast cancer risk was provided. Results were then communicated to the subjects’ health care providers. Subjects completed a telephone interview 6 months later to assess changes in screening behaviors. Setting: Five Denver community pharmacies and four community health fairs. Participants: 103 women age 25 to 78 years completed the risk assessment, 62 completed the follow-up telephone interview. Results: Knowledge of ACS screening guidelines for mammogram and CBE increased 5% (P = .61) and 9% (P = .36), respectively, after the initial encounter. Adherence to guidelines for mammogram in subjects www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 older than 40 years increased by 5% (P = .61). Conclusions: This community pharmacy-based breast cancer education program increased knowledge of and adherence to ACS guidelines, and may serve as a model for other programs. However, these improvements were not statistically significant, possibly because of a high baseline knowledge of and adherence to ACS guidelines, lack of control for outside factors influencing screening behavior, and the brief follow-up period. This project was supported by an APhA Foundation Incentive Grant for Practitioner Innovation in Pharmaceutical Care. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 77—IMPLEMENTING MOTIVATIONAL STRATEGIES TO EMPOWER PATIENTS IN DIABETES MANAGEMENT. Heller K, Palm Beach Atlantic University, Greck B, Kerr Drug and Campbell University. E-mail: katherine_heller @pba.edu Objective: The best way to improve treatment adherence among patients with diabetes is unclear. This preliminary study investigated the development of a motivationally focused program empowering patients with diabetes who were previously uncontrolled to achieve therapeutic goal. Methods: Design: Qualitative, cross-sectional descriptive study. Setting: Asheville Project Diabetes Wellness Program in Asheville, N.C. Patients: The sample frame included all patients enrolled in the Diabetes Wellness Program who had not achieved two consecutive glycosylated hemoglobin values of 8.0% or lower. Data Collection: Patients were identified by retrospective chart review or by referral. After patient identification, the intervention pharmacist met with the provider pharmacist to review the following: (1) patient’s perspective regarding value of glycemic control, (2) provider pharmacist’s perception of patient’s self-efficacy and locus of control, (3) areas of need for referral, (4) patient’s short- and longterm health goals, (5) plan of action for achieving these goals, and (6) identify barriers to achieving glycemic goals. Analysis Plan: Qualitative and descriptive analysis of these reviews Results: Reviews of five patients were studied. External locus of control was identified in two of four patients. Pharmacist provider short- and long-term health goals were clearly outlined in three of four charts, with patient-identified goals outlined in all four charts from enrollment data but identified in recent visits in only 2 charts. A pharmacist provider plan of action was apparent in 4:4 cases while a patient plan of action was apparent in 2:4. Areas of need for referral were primarily psychological (n = 3) but also nutrition (n = 2) and fitness (n = 1). The predominant barrier identified was psychological (n = 3). Conclusions: For patients who have not achieved goal control of their diabetes, pharmacists will need to better assess and enhance their patients’ psychological readiness for change. Pharmacy training will need to include an individualized approach to using motivational strategies. 78—IMPROVING HEALTH AMONG RURAL MONTANANS: MOBILE PHARMACIST-CONDUCTED DISEASE SCREENING IN FRONTIER COMMUNITIES. Stratton T, University of Minnesota, Williams R, Meine K, University of Montana. E-mail: marimbafan@ yahoo.com Objective: To describe the provision of pharmacist-conducted disease screening services in remote frontier and rural Montana communities. Methods: A federal telehealth grant was awarded to this unique demonstration project, Improving Health Among Rural Montanans (IPHARM) in which a motor home was converted into a mobile office, and a recent doctor of pharmacy graduate was hired to use it in providing disease screening to residents of frontier and rural Montana counties. A satellite transmitting/receiving dish on the motor home provides wireless Internet access for researching drug information questions. The motor home also contains an ultrasound unit for testing heel bone density, a spirometer for testing lung function, and CLIA-waived devices to measure glycosylated hemoglobin and serum lipid levels. Pharmacist-conducted screening clinics are held in conjunction with county health departments, tribal health authorities, community pharmacies, county agricultural extension agents, community health centers, and migrant health centers. Employee wellness clinics are also conducted for public and private sector employers. Pharmacy students in advanced practice experiences assist with the screenings when the motor home is nearby. Descriptive statistics are generated for each clinic, and nonparametric statistical analyses are conducted for each screening test to compare results from rural and nonrural communities. Results: During the project’s first 6 months, the IPHARM pharmacist logged almost 6,000 miles, conducting 1,830 tests for 944 patients, 85% of whom live in rural communities. More than 34% of patients were referred to their primary-care providers for follow-up concerning out-of-normalrange test results. The age-corrected prevalence of low bone density was found to be statistically greater among rural residents tested than among nonrural residents tested. Some 40 pharmacy students, including more than one half of all students engaged in advanced practice experience rotations, participated in the clinics. In excess of $27,000 has been generated by the project in operating revenue and donations. Conclusions: Pharmacists and pharmacy students are capable of providing disease-screening services in remote frontier and rural communities. Obtaining sufficient payment for these services in rural communities to cover operational costs remains a challenge. 79—IMPROVING INDIGENT PATIENT MEDICATION ADHERENCE THROUGH PHARMACIST INTERVENTIONS USING MANUFACTURER PATIENT ASSISTANCE PROGRAMS. Hoyt C, Ohio State University. Email: [email protected] Objective: Despite rising costs and complexity of medication regimens, pharmacists are the key professionals to improve access to medications. The primary goal of this project is to increase medication adherence by decreasing drug costs to low income patients through the use of pharmacist-managed manufacturer assistance programs (MAPs). Journal of the American Pharmacists Association 245 2004 Abstracts of Contributed Papers 76—IMPLEMENTATION OF A LIPID MANAGEMENT PROGRAM IN A COMMUNITY PHARMACY. Nesbitt K, Ferris State University/Pfizer/Meijer, Durst S, Ferris State University, Detloff R, Pfizer, Ruhlman B, Vanlente H, Meijer, Inc.. E-mail: [email protected] Objective: Approximately one in five Americans have one or more types of cardiovascular disease (CVD), including stroke, myocardial infarction (MI), angina pectoris, and congestive heart failure (CHF). Risk factors for CVD include: dyslipidemia, age, family history, cigarette smoking, hypertension, obesity, diabetes mellitus, and physical inactivity. High blood cholesterol is strongly related to the risk of CVD. The recommendations for screening for CVD include a fasting lipid profile consisting of high-density lipoprotein cholesterol (HDLC), low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC), and triglycerides (TGs). Measuring blood pressure and fasting blood glucose levels is also important when screening for cardiovascular disease. This study investigates the impact of a community pharmacy-directed lipid management program (LMP) on the clinical outcomes associated with lipid management. The LMP will be offered each year in January and July over a 6month timeframe. Monthly group sessions will be conducted that will provide the patient with intense education. Topics discussed will include risk factors for cardiovascular disease, diet, therapeutic lifestyle changes, and lipid-lowering drug therapy. Individual consultations will take place during refill visits to the pharmacy. The pharmacist will be notified when the patient picks up the refill and will keep track of when the refills are due. The patient will also be afforded the opportunity to call and schedule a visit with the pharmacist on an as-needed basis to allow the patient the opportunity to discuss issues with the pharmacist in private. Methods: Following approval by an investigational review board, the LMP will enroll patients by physician referral or patient interest. Recruitment will take place during monthly cholesterol screenings held at the Meijer Pharmacy. During these screenings risk assessment will be performed for every patient using coronary heart disease risk calculator software. Physicians in the area will be educated about the program for patient-referral purposes. Results: Data collection at baseline will include a patient self-knowledge survey of cholesterol and CVD, self-reported patient medication adherence survey, and full lipid profile to assess LDL-C goal attainment. These outcomes will be re-measured at the month 6 completion visit and compared with baseline to determine the effectiveness of the lipid management program. Conclusions: NA. FEATURE FEATURE Annual Meeting Abstracts 2004 Secondary goals are to encourage patients to proactively manage their medications by decreasing prescription drug coverage through continued MAP use and to decrease cost burden on the health center. Methods: Adult indigent patients on five or more medications will be recruited to the study from Columbus Neighborhood Health Center, Inc. (CNHC) through two methods, either patient selfreferrals or if patients are deemed unable to pay their copayments for medications by health centers or providers. These patients are “waived” copayments with CNHC paying the cost and will be asked to make a pharmacist appointment to assess their medications. Patients will complete a preintervention Morisky adherence survey. At the initial appointment, patient eligibility for MAPs will be determined and MAP education and paperwork provided. Patients will be responsible to complete forms and bring back for physician signatures. The pharmacist will also assess medication regimens for simplification, therapeutic substitution, and other potential interventions. Medication change recommendations will be left in the chart for provider approval if not available during the patient appointment. A follow-up chart review will be completed 3 months after the initial appointment to reassess whether the patient has refilled their next MAP order. At this time, a patient satisfaction questionnaire and post-Morisky adherence survey will be distributed to study participants. Results: Data analysis will include: before and after number of MAPs used, number of medications per patient, changes in adherence survey, and cost savings to the patient and CNHC per month. Pharmacist intervention acceptance rate, pharmacist time and salary versus cost to CNHC, and patient refills of next MAP orders will also be evaluated. Conclusions: By increasing MAP usage and decreasing patients cost burden, we anticipated that this program will improve medication adherence. Further research will need to be performed to assess long-term impact on savings to the health care system and medication adherence. 80—INCORPORATION OF ANIMAL THERAPY INTO THE PHARMACY SCHOOL CURRICULUM: ANIMAL THERAPY AS AN ADJUNCT TO PHARMACOTHERAPY IN CLINICAL PHARMACY PRACTICE. Coffman R, Allison W, Nevada College of Pharmacy. E-mail: [email protected] Objective: To expose pharmacy students to adjunctive therapies, and raise pharmacy students’ awareness of the importance of treating not only the disease, but the psychological and emotional manifestations of disease through an elective course that combines animal-assisted therapy with the tenets of the pharmaceutical care model (PCM). Methods: Students who sign up for the elective follow trained therapy dogs providing adjunctive therapy to patients in hospitals and hospices. Students are assessed on their ability to articulate tenets of the pharmaceutical care model and their knowledge of the use of animal-assisted therapy in various diseases. Students make a formal presenta- 246 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 tion on their observations of the impact on animalassisted therapy in patients followed during the 4week elective. Results: Students taking the elective demonstrated a more complete understanding of the pharmaceutical care model as well as the positive impact that animal-assisted therapy can have on therapeutic outcomes for patients. Conclusions: Bringing together the pharmaceutical care model and animal-assisted therapy as a component of pharmacy education is logical and can be of great benefit to the practicing clinical pharmacist as well as their patients. By incorporating this novel and innovative elective into the Nevada College of Pharmacy curriculum, the college raises student awareness of adjunctive therapies and can serve as a resource for the increasing number of undergraduate and graduate students who are interested in both research and applied clinical aspects of the field of animal-assisted therapy and clinical pharmacy practice. 81—MORBIDITY AND MEDICATION PREFERENCES OF HEADACHE PATIENTS IN A COMMUNITY PHARMACY. Wenzel R, Diamond Headache Clinic Inpatient Unit, Schommer J, University of Minnesota, Marks T, Martin Avenue Pharmacy. E-mail: rwenz@ hotmail.com Objective: A complaint of headache has always been among the foremost reasons people have sought the help of a pharmacist. In 2000 and 2001 the number 1 over-the-counter (OTC) product recommendation pharmacists performed was for a “headache product,” more than 53,000 times daily. This project quantified the degree of morbidity (via Migraine Disability Assessment, or MIDAS, a validated disability assessment tool) and the treatment views of headache patients presenting to a community pharmacy. Methods: Pilot project of 22 self-administered surveys of individuals presenting to a community pharmacy with a complaint of headache and seeking a pharmacist’s recommendation Results: A total of 13 patients had MIDAS scores of Grade III or Grade IV (highest levels). Of the sample population, a substantial minority (41%) did not believe their headaches can be effectively managed with OTC medications, 72% did not feel OTC agents are safer than prescription products, 96% did not indicate that OTC drugs are more effective than prescription items, and 50% disagreed that a physician’s evaluation was not necessary. Only one half of the population was satisfied with their current therapy, and patients overwhelmingly (91%) wished they could prevent their headaches. Conclusions: The majority of headache patients presenting to a community pharmacy had high levels of morbidity and are in need of education regarding the proper role of OTC products, the advantages of prescription agents, and the benefits of a physician’s referral. These preliminary results indicate that community pharmacies are potentially important locations of headache patient identification, education, and referral. 82—PATIENT AND PHYSICIAN RESPONSE TO BONE MINERAL DENSITY MEASUREMENT IN COMMUNITY PHARMACY. Mcfee J, University of Illinois at Chicago. E-mail: [email protected] Objective: Osteoporosis contributes to more than 1.3 million fractures in the United States each year. Early detection of low bone mineral density (BMD) is the best fracture risk predictor. In recent years, the early detection of low BMD has become more accessible through use of portable units. Few studies have focused on low BMD detection in community pharmacies using portable ultrasound technology. Also, little tracking of the impact of pharmacist intervention on outcomes has been completed. The purpose of this study is to identify and enroll women at risk for osteoporosis in a pharmacist-managed intervention that aims to improve awareness and patient health in these subjects. Methods: Women will be recruited through marketing strategies available at approximately 20 chain pharmacies in the Chicagoland area. Subjects will complete a questionnaire, and their BMD will be assessed by quantitative ultrasound of the calcaneus. Pharmacist recommendations will be made regarding calcium intake, weight-bearing exercise, fall prevention, and further follow up with diagnostic technology. BMD results and pharmacist recommendations will be mailed to each subject’s physician. Physicians will be asked to complete a survey instrument that asks them to evaluate and assess the services provided by the osteoporosis monitoring program. Study subjects will be contacted by telephone 6 months after the intervention and asked questions from a survey designed to evaluate patient adherence with pharmacist recommendations and follow-through with their physicians. Results: Responses to the two instruments will be analyzed using the Rasch rating scale model. Conclusions: Increased patient and physician awareness and positive attitudes about the community pharmacists’ role in osteoporosis management are anticipated. 83—PHARMACEUTICAL CARE EVALUATION OF NON-ENGLISH SPEAKING PATIENTS. Westberg S, Sorensen T, University of Minnesota. E-mail: [email protected] Objective: (1) Identify and publicize foreign language services available at pharmacies near a medical clinic serving a large immigrant population; and (2) determine whether the type of drug therapy problems experienced differ between English and non-English speaking patients. Methods: Language services were identified by contacting pharmacies in the neighborhood served by the clinic via telephone survey. A pharmacist provided pharmaceutical care to clinic patients, working with interpreters when necessary. Patientspecific data and the results of the pharmacist’s assessment were recorded in a patient management database. Results: Of the six primary languages spoken by clinic patients, written or verbal information was available for five languages in one or more area www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 pharmacies. A reference card outlining available foreign language services was prepared in multiple languages and disseminated to patients and clinic staff. The clinic pharmacist completed comprehensive assessments for 91 patients via 230 patient encounters, identifying 186 drug therapy problems (DTPs). Problems related to adherence were more prevalent in non-English speaking patients compared with English speaking patients (69% versus 23%). Of adherence-related DTPs, 54% resulted from lack of understanding instructions in nonEnglish speaking patients, compared with 14% in English speaking patients. Adherence DTPs related to a patient’s desire to not take a medication were twice as frequent for non-English speakers versus English speakers (14% versus 7%). In these 91 patients, the number achieving desired drug therapy outcomes improved by 24% after a pharmacist joined the team of clinic providers. Similar outcomes were recognized in both English and nonEnglish speaking groups. Conclusions: Despite the availability of clinicbased interpreters and foreign language services in pharmacies, compliance-related problems are substantially more common in non-English speaking patients. Pharmacists committed to providing pharmaceutical care must consider the impact of language barriers when working to optimize drug therapy outcomes. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 85—PHARMACY PARTICIPATION IN AND NATURE OF CLAIMS SUBMITTED TO THE WISCONSIN MEDICAID PHARMACEUTICAL CARE PROGRAM. Hermansen–Kobulnicky C, University of Wyoming, Kreling D, Mott D, University of Wisconsin–Madison. E-mail: [email protected] Objective: The study objectives were to examine (1) pharmacy participation and intensity of claims submission and (2) characteristics of claims submitted in the Wisconsin Medicaid Pharmaceutical Care Program, an ongoing program initiated in 1996 that reimburses pharmacies for patient-care activities. Methods: Pharmaceutical care claims data for the first 6 years of program operation were analyzed to examine the number of pharmacies submitting a claim and the number of claims submitted by each pharmacy. We also examined the characteristics of claims submitted overall and for each year of the program, including the reason for providing pharmaceutical care, the action taken by the pharmacist, the result of action, and the level of time required to provide the intervention. Results: A total of 16,557 claims were submitted and paid. Except for 1998 and 1999, the number of claims submitted increased every year from 1,438 in 1996 to 4,667 in 2002. The number of pharmacies participating annually has varied; 154 pharmacies submitted at least one claim in 1996 (averaging 9.3 claims per pharmacy) and 88 pharmacies submitted claims in 2002 (averaging 53.0 claims per pharmacy). In 2002, 10 pharmacies submitted more than 80% of all claims. Between 1996 and 2003, the most common reason, action, and result were late refill (n = 3,035), patient education (n = 5,165), and instructions understood (n = 6,881), respectively. The most common level of time required was 6 to 12 minutes (n = 6,554). Conclusions: Although the number of claims has increased over time, a consolidation of pharmacies responsible for the vast majority of claims has occurred, suggesting that some pharmacies have incorporated the program into their routine of practice. Although more than 40% of reasons for pharmaceutical care interventions dealt with compliance issues, pharmacists are detecting and solving a vari- ety of problems with therapy. 86—PREDICTING AND UNDERSTANDING THE INTENTION TO USE HERBAL MEDICINES AMONG HISPANIC AND NONHISPANIC OLDER ADULTS.. Abhyankar U, Gupchup G, Worley–Louis M, University of New Mexico, Raisch D, VA Cooperative Studies Program, Marfatia A, Namdar R, University of New Mexico. E-mail: [email protected] Objective: (1) Identify predictors of intention to use herbal medicines for health problems in the next 6 months among Hispanic and non-Hispanic older adults using the Theory of Planned Behavior and (2) to compare the beliefs underlying the significant predictors of intention to use herbal medicines for health problems in the next 6 months between these two ethnicities. Methods: Design: Cross-sectional survey. Setting: Senior Health Clinic and the Veterans Affairs Hospital outpatient pharmacy. Patients: 251 ambulatory patients; age 65 years and above (Hispanics = 80; non-Hispanics = 171). Data Collection: Self-administered questionnaire. Outcome Measure: Intention to use herbal medicines in the next 6 months. Analysis Plan: Multiple regression analysis was used to identify the significant predictors of intention to use herbal medicines in the Theory of Planned Behavior within each ethnicity. Independent t tests were used to compare the beliefs underlying the significant predictors of intention to use herbal medicines across the two ethnic groups. Results: For both Hispanic and non-Hispanic patients, attitudes towards using herbal medicines was the only significant predictor of the intention to use herbal medicines in the next six months (Hispanics, adjusted R2 = .59, β = .78, P < .001; non-Hispanics, adjusted R2 = .57, β = .66, P < .001). Using the method suggested by Netter et al., magnitude of the beta coefficients did not differ significantly between the two ethnicities. Behavioral beliefs underlying attitudes towards the use of herbal medicines differed significantly by ethnicity. Compared with non-Hispanics, Hispanics believed that herbal medicines are cheaper, have fewer side effects, work better, and are more convenient to use than other medicines. Conclusions: Understanding ethnic differences in behavioral beliefs underlying attitudes towards the use of herbal medicines can help pharmacists in educating and formulating appropriate counseling strategies specific to older patients of different ethnicities. 87—RECOMMENDATIONS FROM IOWA PRIORITY’S BROWN BAG MEDICATION REVIEWS: A COMPARISON OF STUDENT PHARMACISTS AND PHARMACISTS. Freml J, Farris K, Currie J, Fang G, University of Iowa. Email: [email protected] Objective: In the Iowa Priority Brown Bag Medication Reviews: (1) Determine the percentage of drugs that could have been generically substituted or therapeutically interchanged and (2) compare types of recommendations (i.e., cost saving versus Journal of the American Pharmacists Association 247 2004 Abstracts of Contributed Papers 84—PHARMACIST AND PHARMACY STUDENT KNOWLEDGE AND ATTITUDES REGARDING EMERGENCY CONTRACEPTION. Maniscalco M, Daniel K, Marsh W, Nova Southeastern University. E-mail: maniscal@ nova.edu Objective: To assess general knowledge, attitudes, and beliefs of Florida pharmacists and pharmacy students concerning the administration and provision of emergency contraception (EC). Background: The American College of Obstetricians and Gynecologists supports EC as a safe and efficacious method for prevention of unintended pregnancy. Effective use of EC could prevent 2 million unintended pregnancies per year in the United States; however, many patients and providers are unaware of the availability of EC or have misconceptions concerning the use of EC. Provision of EC is based on a time-sensitive protocol. Pharmacists maintain working hours when physicians are typically unavailable and are ideal providers for consulting patients who may be in need of EC. Several states have passed legislation that authorizes trained pharmacists to consult patients and prescribe EC, and at the time this abstract went to press, FDA was considering a petition that would make EC available without a prescription. Methods: A confidential two-page survey was administered to pharmacists during continuing education programs in south Florida and to pharmacy students attending classes at Nova Southeastern University. Questions addressed knowledge of EC administration as well as ethical and social issues regarding its use. Descriptive statistics and chi- square cross analysis were used to analyze the data. Results: A total of 719 surveys were completed by 319 practicing pharmacists and 400 pharmacy students. In general, 59% responded that they believed they were somewhat informed on the topic of EC. When asked whether EC is a public concern, 48% indicated EC was a major public concern. The majority of responders (68%) indicated a positive or neutral attitude towards the use of EC for prevention of unintended pregnancy. Approximately 50% believed EC was not safe and efficacious. Overall, 86% responded they would be willing to prescribe and/or dispense EC. Conclusions: Florida pharmacists and pharmacy students who participated in this survey viewed themselves as somewhat informed concerning the topic of EC, and most indicated they would be willing to be providers of EC. FEATURE FEATURE Annual Meeting Abstracts 2004 therapeutic) made by pharmacists or student pharmacists. Methods: Design. A retrospective cohort study of the Iowa Priority Brown Bag Medication Reviews was completed. Subjects. A random sample of 100 reviews performed by pharmacists and 50 by student pharmacists was drawn from a pool of 2,060 reviews. Data collection. To calculate the percentage of medications that could be generically substituted or therapeutically interchanged, all medications from the 150 brown bag reviews were identified and each medication was coded based upon availability for generic substitution or therapeutic interchange. Determining generic availability was done via the Multum Lexicon database updated as of March 2003 and through use of DrugStore.com. To be considered for therapeutic interchange, drugs needed to be in the same medication class and available generically. The total number of brown bag medications for each patient was the denominator. For objective 2, each of eight recommendation types was counted for each patient. Recommendation types were also classified as cost saving or therapeutic. Analysis. Comparability of the study groups was determined. Student’s t test was used for comparisons of mean data, and the Chi-square test was used to compare nominal data. Results: No differences were identified by study groups in the demographic, disease, or medicationuse variables. Student pharmacists made significantly more total, cost saving, generic substitution, alternate brand, and stop-prescription medication recommendations than did pharmacists. More than 50% of all medications identified in the medication reviews could have been generically substituted or therapeutically interchanged. Conclusions: This study showed student pharmacists make a significant number of recommendations to decrease health care expenses, a finding that should encourage other pharmacists and pharmacy settings to use student pharmacists. 88—REDUCTION OF PRESCRIBING ERRORS IN COMMUNITY PHARMACY. Cottrell J, Cerulli J, Albany College of Pharmacy. E-mail: [email protected] Objective: To determine the impact of a pharmacy-initiated, systems-based reporting tool on the percentage of prescribing errors and the perception of the tool among prescribers in the community setting. Methods: During January to May 2002, potential prescribing errors that occurred in community pharmacies during four collection periods lasting 2 weeks each were documented by pharmacy students. All data collected was reviewed by the investigators and if determined to be a prescribing error, the information was entered into an Access database. After each collection period, a newsletterstyle report with the most common errors for that period and methods to reduce errors was distributed to the most common prescribers of each participating pharmacy. A survey assessing the perception of the newsletter was sent to the participating prescribers at the end of the study. Results: Two independent and four chain partic- 248 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 ipated in at least one data collection period. Four participated during every interval. A total of 397 errors (1.6%) were detected during the study. The most common errors identified were incorrect dosing (22%), incomplete order (20%), and suboptimal dosage form (15%). The total number of errors decreased from 110 (2.2%) to 69 (1.3%) during the study (P = .42). A total of 25 (17%) surveys were returned; 83% of respondents stated that the newsletter was either very useful or useful, and 65% stated they either acted upon the newsletter or shared it with colleagues. Conclusions: Increasing awareness of prescribing errors in community pharmacy via a newsletter is one proposed mechanism to reduce the error rate. Because of a small response rate and sample size, this study was unable to demonstrate significant improvement, however, a trend toward error reduction was evident. Pharmacists need to more actively communicate with prescribers about medication errors that occur in this setting to prevent drug misadventures. 89—RETROSPECTIVE REVIEW OF HYPERTENSIVE PATIENTS IN A POPULATION WITH A HIGH RATE OF DIABETES ACCORDING TO THE NEW JNC-7 GUIDELINES. Feldman L, Zuni Comprehensive Community Health Center, Binning R, Christensen K, University of Wisconsin–Madison. E-mail: [email protected] Objective: To assess the treatment of hypertension at the Zuni Comprehensive Health Center, using the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) guidelines to interpret proper therapy. Methods: At the Zuni Comprehensive Health Center, 173 patients with a diagnosis of hypertension between January and March 2003 were reviewed to categorize them into special populations, review medication usage, and assess blood pressure goals. Monitoring of therapy, laboratory values, glomerular filtration rate (GFR), pregnancy, compliance, medication allergies, and pulse was also performed. Results: The majority of the patients (120 patients, or 69%) received an ACE inhibitor. Thiazide diuretics were used in 42 (26%) patients. Some 78 (45%) patients were only taking one medication, while 52 patients (30%) were taking two medications. Most of the patients (128 or 74%) were diabetic, and 64 (37%) patients had chronic kidney disease. Some patients were in both groups. Only 24 (23.5%) of the patients had blood pressure monitored monthly until their goal was reached, but 84 (98.8%) of those patients at goal were checked again in the next 6 months. Electrolytes and serum creatinine were monitored in 162 (94.2%) of the patients, and no medications were given to any patient with a contraindication. Only 1 patient (2.2%) on a thiazide diuretic had a GFR less than 30 mL/min. A total of 119 (70.4%) patients were noncompliant with their medication regimen. Finally, blood pressure goals were reached in 70 (40%) of the patients and 108 (62.4%) of the patients were within 10 mm Hg of their goal systolic blood pressure. Conclusions: A higher percentage of patients (40%) reached their goal blood pressure compared with the national percentage listed in the JNC-7 guidelines (34%). Diabetic patients receiving an ACE inhibitor may benefit from the addition of a thiazide-type diuretic to help reach the blood pressure goal. 90—SCREENING PATIENTS FOR RISK OF NONSTEROIDAL ANTI-INFLAMMATORY DRUG INDUCED COMPLICATIONS IN COMMUNITY PHARMACY SETTINGS. Anzisi L, Lee A, Algozzine T, Brady G, Pfizer Inc. E-mail: [email protected] Objective: The study objective was to identify patients at risk for gastrointestinal (GI) and cardiovascular complications receiving a nonspecific nonsteroidal anti-inflammatory drug (NSAID). Up to 50% of patients have intolerance to nonspecific NSAIDs, and more than 100,000 patients are hospitalized annually with NSAID-associated GI complications. NSAID use in the elderly is an independent risk factor for developing hypertension and may contribute to poor blood pressure control in those receiving antihypertensive medications. Methods: A questionnaire consisting of 13 questions was developed and administered to patients in community pharmacies who presented with a prescription for an NSAID. The questionnaire assessed: age; need for help with self-care; previous stomach upset, ulcer, or bleeding from NSAIDs; concomitant use of antiplatelet agents, gastroprotective medications, corticosteroids, or nonprescription NSAIDs; cigarette and alcohol consumption; and presence of hypertension. Patients were classified as having mild, moderate, or severe risk for GI complications based upon their responses, and pharmacists recorded any interventions made after assessing the patient’s risk level. Results: More than 200 patients were screened in community pharmacies in Maine, New York, and New Hampshire. Preliminary results estimate that 56% of patients screened were at moderate or severe risk for GI complications. A total of 25% of patients were over 60 years of age, placing them at moderate or severe risk. Regardless of age, 31% of patients had a history of GI upset or bleeding, and 30% were receiving gastroprotective medications. Of hypertensive patients 57% were receiving nonspecific NSAIDs, and 27% were receiving both prescription and over-the-counter NSAIDs. Conclusions: The use of this screening tool enabled pharmacists to identify NSAID users at greatest risk for GI and cardiovascular complications and should be incorporated into more community pharmacy practice settings. 91—SERVING CHRONIC PAIN PATIENTS IN THE MILLENNIUM. Guilherme A, Humphrey J, Kaiser Permanente, Northwest Region, Vancouver, Washington. E-mail: [email protected] Objective: To improve the efficiency of serving www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 92—STUDYING THE PROFESSIONAL INTERRELATIONSHIP BETWEEN COMMUNITY PHARMACISTS AND PHARMACY TECHNICIANS. Akiyode O, Bullard W, Karodeh Y, Cao T, Howard University. E-mail: oakiyode@ howard.edu Objective: To understand the professional relationship between pharmacists and pharmacy technicians. To identify the supporting and inhibiting factors toward the professional behaviors demonstrated by the two entities. Methods: Community pharmacists and pharmacy technicians will complete a survey tool that assesses their interaction with each other. The survey tool is designed to evaluate the attitudes, behaviors, perceptions, and expectations among the aforementioned entities. A total of 50 surveys will be randomly distributed to local community pharmacies. Pharmacists will receive one half of the surveys, while pharmacy technicians will receive the other half. Upon completion of the surveys, a pair of fivemember focus groups (one involving pharmacists, the other technicians) will convene to discuss the survey results and ways to improve the professional relationship. The participants of the focus group discussions will be randomly selected from the pool of the study participants. Upon completion of the focus group discussions, all participants will be asked to complete a postdiscussion questionnaire to assess Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 what they have learned from the discussion session, and how they plan to improve their own professional relationships. Results: The outcome of the surveys, focus group discussions, and postdiscussion questionnaires will be analyzed using descriptive statistics. The study is expected to educate participants and generate ideas to improve further the relationship between pharmacists and technicians, hopefully improving the efficiency of the pharmacy and overall patient care. Conclusions: NA 93—SURVEY OF PHARMACISTS DESIRE AND READINESS FOR DISEASE STATE MANAGEMENT IN OHIO. Dorsch M, Riverside Methodist Hospital, Kier K, Mraz S, Ohio Northern University. E-mail: [email protected] Objective: Prescription drugs remained the fastest growing health expenditure, increasing by 15.7%. The state of Ohio follows a similar trend. Currently medications account for 15.1% of the Ohio Medicaid budget, while physician billing only comprises 6%. Due to the increasing cost of health care and medications, the Ohio Pharmacists Association (OPA) started discussions with the state about the concept of disease state management (DSM). The objective was to determine pharmacists desire and readiness to start DSM programs within the state. Methods: OPA put together a task force to discuss issues relevant to starting a statewide program in DSM. Based on task force discussions, a survey was designed and pilot tested to look at DSM issues. The survey was sent to a random selection of licensed pharmacists within the state of Ohio. The survey asked questions relating to demographics, current practice settings, current DSM practices, and preparation and desire to provide DSM services. Descriptive statistics will be used to analyze the data. Results: Initial results from the survey provided interesting feedback, especially in the area of pharmacist training and preparation for DSM. In general, pharmacists were most comfortable with the area of diabetes management. Most pharmacists indicated a willingness to take more training or certification in areas of DSM. Data analysis is ongoing. Conclusions: The results will be used by the task force to make decisions relating to pharmacist interest, training, and potentially areas for reimbursement. 94—THE DEVELOPMENT OF A PAIN SERVICE BY THE PHARMACY DEPARTMENT IN A UNIVERSITY MEDICAL CLINIC. Jacobson S, Massachusetts College of Pharmacy and Health Sciences, Debay G, Massachusetts Institute of Technology. E-mail: [email protected] Objective: To provide pain management education and reference information to health care providers and patients in an outpatient ambulatory clinic and inpatient unit. Methods: A pharmacist was identified to lead an educational initiative helping pharmacists, nursing staff, physicians and other health care providers learn about effective pain management. All pharmacists were required to read and successfully complete posttests associated with journal articles. Case study discussions were also an integral part of their pain management competency training. Ongoing education for the pharmacists helped to ensure consistent communication in their clinical assistance to the medical staff and in patient counseling. Health care practitioners were provided pain management information and guidance on how to identify and refer patients to the pain service. Assessment tools such as flow sheets and narcotic conversion charts were developed by the pharmacy for use in both the inpatient and outpatient setting. Frequent meetings with the inpatient and outpatient clinical staff regarding up-to-date pain management information, assistance on the proper use of pain management assessment tools, approved formulary medications for pain, appropriate prescribing, outpatient prescription and inpatient order writing for medications, and documentation in the medical chart were imperative for the success of this service. The pharmacy department is beginning to collect data in both the inpatient and outpatient records to monitor the proper use of pain assessment tools, appropriate prescribing, and patient compliance. Results: The medical and nursing staffs have reported a positive outcome for patients involved with the pharmacy pain service. The pharmacists are finding that providing clinical information to health care providers and counseling patients receiving pain medications is a rewarding experience. Conclusions: A pharmacy-centered pain management program is beneficial to the university health system. 95—THE PHARMACIST’S ROLE IN PUBLIC HEALTH: A SURVEY OF HEALTH DEPARTMENT OFFICIALS. Cottrell J, Albany College of Pharmacy, Blumenschein K, University of Kentucky, Paavola F, None. E-mail: [email protected] Objective: To examine services provided by state and local health departments, determine areas into which health departments would like to expand, and examine the public health officials’ perceptions of partnering with community pharmacists. Methods: In December 1999, 25 state health department Web sites were reviewed to determine the areas of focus that public health agents were attempting to address. From this assessment, a three-page survey was developed and sent to directors of 300 health departments, randomly selected from the National Association of County and City Health Officials (NACCHO) mailing list. Each packet contained a cover letter, a survey, and a selfaddressed stamped envelope. Surveys were approved under expedited review by the University of Kentucky Medical Institutional Review Board and contained 13 questions: 4 addressing staff composition and responsibilities, 4 addressing current and future programs, and 5 concerning perceptions of partnering with pharmacists and pharmacy serJournal of the American Pharmacists Association 249 2004 Abstracts of Contributed Papers chronic pain patients by establishing a collaborative project via pharmacy and primary care providers. Methods: The Kaiser Permanente Cascade Park clinic is one of 22 ambulatory care locations in the Pacific Northwest Region. In the past years, improvements were needed to provide a more methodical approach to serve chronic pain patients who required therapy with controlled substances. The collaborative project created set out to decrease workload of providers and increase patient satisfaction. The new system operates on patient lists. One week before medications are due, a pharmacist sends a message to the provider stating the following: date medication is due, the last fill of the medication, the quantity that the prescription was filled for, last patient appointment, and any special requests or concerns. An order for the patient’s medication is also created. Once the provider receives the message, the order can be approved if continued therapy is intended, and a signed prescription is sent back to the pharmacy. Pharmacy staff then files the prescription for the date that the patient is due for medication and then on date in question, the prescription is processed by pharmacy staff. Results: All clinic providers who care for chronic pain patients on controlled substances have been participating in this project, and more than 250 patients have been enrolled. Conclusions: Since this project began, provider, patient, and pharmacy satisfaction with the method of processing controlled substances for chronic pain patients has been overwhelming. A need for change was identified and satisfied with a technological update on method of service. FEATURE FEATURE Annual Meeting Abstracts 2004 vices. Surveys were anonymous and were collected from January to March of 2001. Results: A total of 153 surveys were returned for a response rate of 49%. Nurses were the most common health care provider on staff at health departments, and the most frequently additional personnel requested. The most common service offered by health departments was immunizations. Most respondents desired to establish preventive services such as disease management, indigent care clinics, and health information libraries. Only 13% had a pharmacist on staff, and an additional 11% partnered with their local pharmacist. Approximately 60% had not considered partnering with their local pharmacists; most stated that cost was the barrier preventing an alliance. Officials identified indigent care clinics, dispensing medications, and drug-use review as the main services they would like to see provided by pharmacists. Conclusions: Pharmacists appear to be underused in public health plans for meeting goals of Healthy People 2010. 96—MOTIVATION AND JOB SATISFACTION OF COMMUNITY PHARMACISTS INVOLVED WITH PHARMACEUTICAL CARE. Swensgard L, Ohio State University. Email: [email protected] Objective: Community pharmacists are becoming increasingly involved with direct patient care services as a way to expand their role as health care professionals. The future success of these services depends in part on the ability of community pharmacies’ corporate management to keep the participating pharmacists motivated to continue their roles as pharmaceutical care providers and motivate other community pharmacists to become involved. The purpose of this study is to assist Kroger corporate management in identifying what motivational factors contribute to the decision of central Ohio Kroger pharmacists to become involved in or abstain from pharmaceutical care services. Also, the study will identify what barriers central Ohio Kroger pharmacists perceive to becoming involved in pharmaceutical care. Factors contributing to job dissatisfaction and job satisfaction will also be assessed. Methods: Mail surveys will be sent to two groups of central Ohio Kroger pharmacists, those actively providing patient care services and those involved solely in dispensing activities. The survey will compare and contrast both groups of pharmacists’ motivations to perform patient care services. Job satisfaction will also be assessed in both groups of pharmacists. The data collected from the survey will be used to implement new recruitment and advancement strategies to increase Kroger community pharmacist involvement in pharmaceutical care services. In addition, the information will be disseminated to other community pharmacies for use in increasing pharmacist involvement with pharmaceutical care. Results: Data collection began in November 2003. Conclusions: This project will enable corporate management of community pharmacy establish- 250 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 ments to identify motivational forces that contribute to a pharmacist’s decision to perform pharmaceutical care services and factors that contribute to job satisfaction. Also, this project is expected to provide information regarding how best to reward pharmacists for their participation in pharmaceutical care services. 97—USING ADVANCED PRACTICE COMMUNITY CLERKSHIP STUDENTS TO PROVIDE CONTINUING EDUCATION FOR RURAL PHARMACISTS. Hastings J, University of Arkansas for Medical Sciences College of Pharmacy, West D, University of Arkansas for Medical Sciences. E-mail: [email protected] Objective: The goal of this project is to describe how senior pharmacy students are used in the delivery of live continuing education (CE) to pharmacists in a remote region of a small southern state. Methods: The community clinical clerkship is a cooperative rotation taught by the college of pharmacy in conjunction with 24 pharmacies located throughout Arkansas. One of the assignments that senior students enrolled in this advanced community practice clerkship must complete is a clinical or management project. The board of pharmacy in this state requires pharmacists to obtain 12 hours of live, disease-related CE over a biennial licensing period. One preceptor in a rural area of the state requires each student who rotates through his site to deliver a CE presentation related to drug-therapy to pharmacists in the southeast region of the state. Results: NA. Conclusions: This unique use of students to help pharmacists comply with licensing requirements benefits everyone involved. The students have an opportunity to complete an assignment for their rotation while at the same time benefiting from the experience of researching, preparing and presenting a CE program. Pharmacists in the region benefit from the information presented by the student about the selected drug topic, are able to obtain live CE credit in a convenient manner and have the opportunity to network with their local peers on a regular basis. 98—ANALYSIS OF HYPERTENSION CONTROL IN A MIDWESTERN CARDIOLOGY CLINIC. Glosner S, Pfizer Inc, Tynan S, Alsip D, Cline K, Midwestern University, Konczal M, Faaborg J, Marcinkowski L, Midwestern University. E-mail: [email protected] Objective: Coronary heart disease (CHD) remains the number 1 killer in the United States. CHD also costs more than $100 billion a year to treat. CHD is both financially and clinically important. Risk factors for developing CHD are elevated blood pressure (BP), tobacco use, low HDL cholesterol, family history, and age. Our purpose was to assess BP control, treatment options and comorbidities that increase CHD risk in hypertensives patients. Methods: A retrospective, chart review was performed at an Illinois cardiology practice during October 2002. The study population consisted of patients taking either antihypertensives alone (N = 401) or those taking antihypertensive agents in conjunction with medications for heart failure (N = 359). A total fo 120 patients were randomly selected and evaluated from the study population. Patient demographics, blood pressures, laboratory test results, and medications were collected. Results: Overall, 56% of participants were women. The average age for the overall population was 68 years. More than 75% of patients had a body mass index of greater than 25 kg/m2. Some 70% of the population had a dyslipidemia, 29% had CHD, 23% had arrhythmias, and 15% had diabetes mellitus (DM). Beta blockers (24%) and calcium-channel blockers (23%) were the most frequently used medications. BP control was noted in 47.1% of men and 51.5% of women. BP control was observed in less than 50% of each drug class except for diuretic medications (52%). A total of 62% of CHD patients had elevated BPs, and 42% of patients with CHD or DM were not at their LDL cholesterol goal of less than 100 mg/dL. Within the last year, 15% of reported patient hospitalizations were cardiac related. Conclusions: Cardiologists generally treat more complicated cardiovascular patients, yet nearly 50% of patients in this study had BPs that were uncontrolled while on medications. Practitioner education by pharmacists on national guideline attainment should help improve health outcomes (e.g., BP and cholesterol control). 99—ASSESSMENT OF MEDICATION NONADHERENCE AND DISEASE STATE KNOWLEDGE IN A COMMUNITY PHARMACY. Self T, University of Kentucky, Chou C, Pfizer, Inc. E-mail: [email protected] Objective: The purpose of this project was to (1) identify patients at risk for medication nonadherence using a validated scale and to report any trends; (2) determine the need for further counseling in patients with risk behaviors for nonadherence on the benefit of prescription medications, and (3) evaluate disease knowledge and awareness of their personal laboratory values in patients indicating a history of hypertension, hyperlipidemia, or diabetes. Methods: Surveys were randomly distributed to patients 18 years of age and older at a local Kroger Pharmacy. Collected information included demographics (age and gender), chronic disease states, and self-reported medication-taking behaviors. The survey consisted of four questions (Morisky scale) in a validated tool that is used to identify and address barriers to medication adherence. Patients were considered nonadherent if one or more questions on the Morisky scale was answered “yes,” and they were then counseled on ways to increase adherence as well as the benefit of prescription medication. In addition, halfway through the survey, the method was improved by asking patients that indicated a history of hypertension, hyperlipidemia, or diabetes if they knew their current laboratory values and goals for their blood pressure, cholesterol, or blood glucose. Patients were then counseled appropriately about their diseases and goals of therapy. Results: All data will be analyzed using www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 Microsoft Access. Conclusions: NA 101—DEVELOPMENT OF A HELICOBACTER PYLORI RAPID SCREENING PROGRAM IN THE COMMUNITY PHARMACY SETTING. Kurpius M, University of Iowa, Sommers Hanson J, Dominick’s Pharmacy. E-mail: [email protected] Objective: To implement a Helicobacter pylori screening program in the community pharmacy setting to (1) identify patients with untreated H. pylori infection, (2) initiate appropriate drug therapy for treatment of H. pylori infections, and (3) evaluate patient symptom improvement as the result of the interaction with the pharmacist. Methods: Patients for program participation were identified through patient prescription profile review for antisecretory medications and patient requests for nonprescription medication recommendations for the treatment of ulcer symptoms. Exclusion criteria included: patients younger than 18 years of age, pregnant, older than 50 years with new onset of symptoms, patients with gastroesophageal reflux disease-like symptoms, alarm symptoms, long-term use of nonsteroidal antiinflammatory medications, and previous infection or treatment of H. pylori. Those patients who did not Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 102—NATIONAL PATTERNS OF ASPIRIN PROPHYLAXIS IN PATIENTS WITH DIABETES. Holness P, Lee E, Hogue V, Lombardo F, Howard University. E-mail: [email protected] Objective: To describe the patterns of aspirin prescription in diabetic population using the 2000 National Ambulatory Medical Care Survey (NAMCS) and to evaluate the need for intervention by community pharmacists. Methods: Design: Cross-sectional descriptive study. Setting: Standalone office-based physician visits in ambulatory care settings. Participants: 22,224 NAMCS visit records made by patients 21 years of age and older. Results: Mean (± SD) age of the population was 54.3 (± 18) years. About 5% of the visits (1,046) were made by patients with diabetes. Mean age of patients making the diabetes visits (62.9 ± 13.8 years) was higher than that of the total population. Of the diabetes visits, 7.2% involved recommendations for aspirin were noted in the record. Visits made by diabetic patients were highly associated with aspirin record (odds ratio [OR], 3.6; 95% CI, 2.8–4.7). Although women patients were less likely to have aspirin records in the general population (OR, 0.4; 95% CI, 0.4–0.5), no gender difference was observed in the diabetic population (OR, 0.8; 95% CI, 0.5–1.3). Patients who were 65 years and older were approximately 4 times as likely to have aspirin record than patients who were younger than 65 years of age (OR, 3.7; 95% CI, 3.1–4.4). In addition, certain visit characteristics were associated with aspirin records among diabetic population. Cardiovascular specialists were more likely to be associated with aspirin records than were other physician specialties (OR, 5.2; 95% CI, 3.1–8.8). Physicians located in the Midwest were less likely to prescribe aspirin than were physicians in the Northeast (OR, 0.4; 95% CI, 0.2–0.9). No difference was observed by gender, race, metropolitan status, or counseling. Multivariate analyses will be conducted to describe factors predicting aspirin use. Conclusions: Status of aspirin use among patients with diabetes was suboptimal in 2000. More educational prevention programs focusing on aspirin prophylaxis are needed by community pharmacists. 103—PHARMACY STUDENTS’ EXPECTATIONS OF COLLABORATIVE WORKING RELATIONSHIPS (CWRS) AMONG PHARMACISTS, PHYSICIANS, AND PATIENTS. Stehling D, Gaebelein C, St. Louis College of Pharmacy. E-mail: [email protected] Objective: A major trend in pharmacy education is the promotion of a collaborative role for pharmacists in patient care. This effort involves the establishment of CWRs among pharmacists, physicians, and patients. Currently, however, little research is available on the dynamics of these relationships. The objective of this study was to adapt an existing survey tool, the Health Role Expectations Index (HREI), to study pharmacist–physician–patient interactions. The success was measured in terms of the statistical reliability and sensitivity of the resulting survey, the HREI-Pharmacist. Methods: The HREI, originally developed to study role expectations among nurses, physicians, and patients, was modified by substituting the term “pharmacist” for “nurse” in the 16-item questionnaire. The resulting items reflected the degree of collaboration expected among physicians, pharmacists, and patients in the health care setting. The survey also provided a general index of egalitarianism. The statistical reliability and sensitivity of the HREI–Pharmacist were assessed with a convenience sample of 55 students in their second year of professional studies at St. Louis College of Pharmacy. Survey data were analyzed using the Statistical Package for the Social Sciences (SPSS), release 10.0, and Microsoft Excel. An alpha level of .05 was used for all statistical decisions. Effect size estimations were calculated according to Cohen. Results: The statistical reliability of HREI–Pharmacist was determined by calculating a Generalizability Coefficient according to the principles of Generalizability Theory. A value of 0.68 was obtained, indicating that the HREI displayed adequate statistical reliability. The sensitivity of the HREI–Pharmacist was assessed by dividing respondents into two groups based upon the median egalitarianism score, and then comparing responses on the three collaborative dimensions. Students with high CWR scores expected much collaboration with physicians, while those with low CWR scores did not. However, both groups expected much collaboration with patients. Based on effect size estimations, the group difference in collaboration among physicians was large, and that among pharmacists was moderate. Conclusions: The HREI–Pharmacist is a reliable and sensitive tool for the study of the health role expectations of pharmacists, physicians, and patients. Current work with the tool involves benchmarking the CWR attitudes of pharmacy students and rural pharmacists. Journal of the American Pharmacists Association 251 2004 Abstracts of Contributed Papers 100—BRANDING PHARMACEUTICAL CARE SERVICES USING THE BRAND CLARITY PYRAMID. Abraham J, Bircea E, Stubbings J, University of Illinois at Chicago. Email: [email protected] Objective: (1) To alter the public image of pharmacy from the traditional dispensing role to the current patient-focused role, (2) to develop an image for pharmaceutical care using a proven professional tool used in the marketing and advertising industry, and (3) to help the public understand the role of pharmaceutical care in health care. Methods: To better represent the population, participants who interact with various types of pharmacy settings will be used. There will be multiple focus groups, each containing six to eight participants from a wide variety of backgrounds in each group. The brand clarity pyramid is the marketing tool chosen to create a new image of pharmaceutical care. Each session will last about 60 to 90 minutes and, with the permission of the participants, will be tape-recorded; the facilitator will ask the participants a series of questions to build a brand clarity pyramid for each session. After all the focus groups have done their brand clarity pyramids, a fifth focus group will be used to analyze the previous groups’ results and to develop a cohesive brand image. Results: Each brand pyramid from the focus groups will be presented. The results from the last focus groups will be used to determine if an effective image for pharmaceutical care has been developed; patient demographics from all focus groups will be included as well. Conclusions: This project is expected to promote an increased public understanding of pharmaceutical care. meet the exclusion criteria were screened for H. pylori using a rapid whole blood test. Patients who tested negative were provided with drug therapy recommendations, suggestions for lifestyle modifications, and educational handouts. Patients who tested positive had a letter sent to the physician stating the patient’s symptoms, test results, and pharmacist’s recommendations for drug therapy. Follow-up with both groups of patients was made 1 month later via telephone call. Results: The pharmacist used a gastrointestinal symptom survey to assess the resolution of symptoms, outcomes of the pharmacist’s interventions, and implementation of recommendations made to the patient and the physician. Conclusions: This program is expected to benefit patient care as a result of pharmacist identification of patients requiring screening and treatment of H. pylori, and relieving symptoms associated with this infection. FEATURE FEATURE Annual Meeting Abstracts 2004 104—PROVIDING MEDICATIONS TO UNDERSERVED POPULATIONS UTILIZING 340B. Reid C, Jackson T, Langridge S, Midwestern University. E-mail: [email protected] Objective: To increase awareness of the 340B program by educating pharmacist and other health care professionals in a community health care (CHC) setting. Methods: This is a two-hour continuing education (CE) program that is designed to educate health care professionals about 340B pricing. The main speaker of the program, a consultant for the Office of Pharmacy Affairs, will discuss barriers of access to pharmaceutical care in the working poor, 340B pricing, benefits of implementing the program, entities eligible for 340B pricing and who to contact for assistance when starting 340B. The group demographics will differ in gender, age, health care background, employment experience and education level. Each health care provider that attends the CE program will be asked to respond to a retrospective pre/post test. The survey is designed to assess participants’ knowledge of 340B pricing and the intent to implement the 340B pricing program. Results: The retrospective before–after test answers will be analyzed using the Wilcoxon Singed Rank analysis to measure the difference in the participant’s pretest and posttest knowledge of the 340B pricing program. Rasch analysis will determine the probability of answering a question correctly and measure the difference between the participant’s intent to implement the program before and after the retrospective pre/post test. Demographic variables will be analyzed using descriptive statistics. Conclusions: This CE program is expected to increase knowledge of 340B pricing among participants and gauge the intent to implement the program. 105—THE UNAVAILABILITY OF PRESCRIBED MEDICATIONS IN THE COMMUNITY PHARMACY SETTING. Rodriguez I, NOVA Southeastern University, Lai L, Nova Southeastern University. E-mail: [email protected] Objective: To evaluate if there is a relationship between the unavailability of prescribed medications and patients’ deserting the pharmacy. Methods: A convenience sampling method was used to recruit the study subjects at three community pharmacies in the Pembroke Pines and Miami area in Florida. The unavailability of a prescription is defined as a medication not available until next day. “patients’ deserting the pharmacy” was defined as a patient not returning to pick up the medication within the next 7 days. The patients who were not permanent residents of Florida or who did not agree to interchange the medication for one that is available were excluded from the study. Data will be obtained from the pharmacy computer database including: age, gender, race, type of medication prescribed, if the medication is used for acute or chronic conditions, type of insurance, and if the medication was picked up or not. A total of 154 study subjects was estimated to be the minimum sample size 252 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 to provide results with a confidence interval of 95% and a power of .70. Results: This study is expected to identify that patients with new prescriptions for acute conditions will be less willing to wait or come back for the medication. Elderly patients and customers with insurance are expected to be less willing to order the medication for next day. Conclusions: NA. APhA–APPM Hospital & Institutional Practice 106—APPROPRIATE TREATMENT OF SYSTOLIC HEART FAILURE IN THE PRIMARY CARE CLINICS. Worrall T, Ralph H. Johnson Veterans Affairs Medical Center, Simpson K, Medical University of South Carolina, Jenrette D, Ralph H. Johnson Veterans Affairs Medical Center. E-mail: [email protected] Objective: Heart failure is a common medical condition affecting more than five million people in the United States. Many experts believe that suboptimal pharmacological treatment contributes significantly to hospitalizations and deaths. This study was designed to quantify the percentage of patients in the primary care clinics receiving appropriate therapy for systolic heart failure (SHF) and to potentially improve prescribing practices in this patient population. Methods: Male veterans with SHF from three primary care teams were evaluated. Patients with SHF were randomly selected from the fourth quarter of 2001. The primary end points evaluated were the percentage of patients on ACE inhibitors, betablockers, or combination therapy. The secondary end point evaluated was the percentage of patients on spironolactone. Following an initial retrospective chart review, two educational interventions were performed to increase compliance with the SHF treatment guidelines. The effectiveness of this education was assessed through a review of SHF patient charts using the same methods described in the initial retrospective evaluation. Logistic regression modeling was used to assess the effect of the educational interventions. The Likelihood Ratio was used to assess overall model significance, and each variable was assessed using the chi-square test. The Wald Confidence Interval (CI) for the odds ratio estimates was also calculated. Results: A total of 148 patients were evaluated (75 before and 73 after education). The mean (± SD) age of the patients was 65 ± 11.3 years, the mean ejection fraction was 29 ± 9.5%, and the mean number of drugs prescribed per patient (other than study drugs) was 9.5 ± 4.8. The New York Heart Association (NYHA) functional class distribution was similar between groups. The percentages of patients prescribed ACE inhibitor in the before and after education groups were 90.7% and 89%, respectively. After education, beta-blocker and spironolactone prescribing increased by 12,8% and 6.2%, respectively. Spironolactone prescribing increased 10% in NYHA class III and IV heart fail- ure patients. These patients were also 3.7 times more likely to receive appropriate therapy (95% CI, 1.16–11.63, P = .026). Conclusions: These results indicate that pharmacists’ educational interventions significantly improved the appropriate pharmacological treatment of SHF in primary care clinics. Original Citation: American College of Clinical Pharmacy 2003 Annual Meeting. November 5, 2003. Atlanta, Georgia. 107—COUNSELING MONOAMINE OXIDASE INHIBITOR PATIENTS. Wenzel R, Diamond Headache Clinic Inpatient Unit, Schommer J, U. of Minnesota, Diamond S, Diamond Headache Clinic. E-mail: rwenz@ hotmail.com Objective: Assess whether a classroom-based pharmacy education service for hospitalized patients newly prescribed a monoamine oxidase inhibitor (MAOI) results in (1) higher self-perceived medication knowledge or (2) lower perceived risk of using MAOIs. Methods: Quasi-experimental self-administered patient survey given before the education service and repeated 24–72 hours after the service. Results: A total of 78 individuals completed the study. Paired-sample t tests showed that for each of the four items related to self-perceived medication knowledge, the scores reflected higher knowledge after the MAOI class compared with before the class (P < .05). For three of four items related to perceived risk of using MAOIs, the scores reflected a lower level of perceived risk after the MAOI class, compared with before the class (P < .05). One item did not significantly change: “The MAOI prescribed for me is just as good as other products available for treating headache.” Conclusions: Our results demonstrate a classroom-based teaching structure for newly prescribed MAOI patients can result in higher self-perceived medication knowledge and lower perceived risk of using MAOIs. The utility of this personnel-efficient method of counseling hospitalized patients prescribed other medications warrants further investigation. 108—DEVELOPMENT OF A CLINICAL PATHWAY TO OPTIMIZE EPOETIN THERAPY IN THE TREATMENT OF ANEMIA IN CHRONIC RENAL FAILURE PATIENTS. Canney T, Kindred Hospital. E-mail: [email protected] Objective: The objective of the project was to increase the utilization of iron supplementation and of the subcutaneous administration of epoetin in chronic renal failure patients through the design and implementation of a clinical pathway. Methods: Protocol developed based on literature and practice guidelines from the National Kidney Foundation (approved by renal specialists and the Medical Executive Committee of the hospital). Data were collected for 30 inpatients in an acute respiratory-care hospital who were prescribed epoetin. Dialysis and nondialysis patients were included and www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 109—EXPERIENCE WITH A SYMPTOMTRIGGERED ALCOHOL WITHDRAWAL SYNDROME PRACTICE GUIDELINE IN HOSPITALIZED PATIENTS. Worrall C, Padgett S, Medical University of South Carolina, Stanley K, Medical University of South Carolina. E-mail: [email protected] Objective: We developed a symptom-triggered alcohol withdrawal syndrome (AWS) Practice Guideline and piloted its use in general surgery and medicine patients. Our primary and secondary objectives were to improve outcomes in hospitalized patients at risk for AWS and to evaluate the safety and efficacy of the guideline to determine whether hospital-wide implementation would be appropriate. This report summarizes our experience using the guideline in 106 hospitalized patients. Methods: An evidence-based AWS Practice Guideline was developed by a multidisciplinary team of practitioners. After appropriate staff education, the guideline was piloted in a general surgery and a general medicine group. Control data were Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 collected retrospectively, while guideline data were collected concurrently for each group. Primary outcome measures included milligrams of drug administered, presence of AWS seizures or QTc prolongation, transfer to an intensive-care unit (ICU), use of restraints or sitters, and length of stay (LOS). Continuous data were assessed using a two-tailed t test, and proportional data were assessed using chisquare and Fisher‘s exact test. Multivariate logistic regression was used to assess LOS. Results of each individual analysis and a combined analysis are described below. Results: Demographics of the surgery or combined analysis groups were similar, but the medicine analysis demonstrated significantly more women in guideline group (P = .02). Lorazepam use decreased significantly across all guideline-managed patients (surgery P = .01, medicine P < .01, combined P < .01). Clonidine use increased significantly in the guideline-managed surgery and combined groups (P < .01 in both groups). There was no difference in haloperidol use in any group. The medicine and combined analyses demonstrated a significant number of guideline-managed patients requiring no drug therapy (P = .01 and P < .01, respectively). Withdrawal seizures, QTc prolongation, transfers to an ICU, restraint hours, and LOS were similar between groups. Sitter hours decreased significantly in the guideline combined analysis (P = .01), but the surgery and medicine analyses did not reach significance. Conclusions: The AWS Practice Guideline significantly decreased benzodiazepine use in guideline-managed general surgery and medicine patients. Many patients required no drug therapy when managed using this symptom-triggered approach. We are currently working with our hospitalists to expand the use of this practice guideline hospitalwide. 110—GABAPENTIN: A POOLED ANALYSIS OF ADVERSE EVENTS FROM THREE POSTHERPETIC NEURALGIA CLINICAL TRIALS. Parsons B, Pfizer, Tive L, Huang S, Pfizer, Inc. E-mail: [email protected] Objective: Gabapentin has been shown to effectively and safely manage the pain of postherpetic neuralgia (PHN). Adverse events are often doserelated, with frequency and severity increasing with increasing dosage. Here, we assessed the relationship between gabapentin dose and adverse events using data from studies of patients with PHN. Methods: Data were pooled from three randomized, double-blind, placebo-controlled, parallelgroup studies (N = 599 PHN patients). Three treatment category groups were included in the analysis: patients receiving placebo (N = 243); patients receiving less than 1,800 mg/day (N = 356) and patients receiving 1,800 mg/day gabapentin or more (N = 321). Gabapentin was initiated at 300 mg and titrated to maintenance doses of 1,800–3,600 mg/day by days 12–24. Patients receiving higher doses had received lower doses. An adverse event was scored at dose of first onset, and scored again at a higher dose if it worsened in severity. Results: The three most common adverse events were dizziness, somnolence, and peripheral edema. Patients had a higher incidence of peripheral edema with gabapentin in doses of 1,800 mg/day or more (7.5%) compared with lower gabapentin doses (1.4%). The incidence at the higher (P = .0014) but not the lower (P > .05) doses was significantly different from the placebo rate of 1.6%. By contrast, patients did not have a higher incidence of dizziness and somnolence with higher gabapentin doses. Patients receiving less than 1,800 mg/day of gabapentin reported dizziness (20.2%) and somnolence (14.9%) at a significantly greater frequency than the respective placebo rates of 7.4% and 5.8% (P = .005). However, at less than 1,800 mg/day, the 9.7% and 6.9% rates of dizziness and somnolence were both comparable to placebo (P > .05). Discontinuation rates were comparable between patients receiving placebo and gabapentin. Conclusions: These data demonstrate that although a mild increase in the incidence of peripheral edema is observed when patients receive greater than or equal to 1,800 mg/day of gabapentin, dizziness and somnolence are transient and do not occur more frequently or worsen when patients are titrated to doses of 1,800 mg/day or more by days 12–24. Therefore, safety concerns should not limit titration to achieve optimal efficacy. 111—RAPID ONSET OF ABSORPTION WITH OLANZAPINE ORALLY DISINTEGRATING TABLETS. Houston J, Bergstrom R, Mitchell M, Hill A, Taylor C, Liu-Seifert H, Yadav Marya R, Jones B, Witcher J, Eli Lilly and Company. E-mail: [email protected] Objective: A clinical perception exists suggesting more rapid onset of action with olanzapine orally disintegrating tablet (ODT) versus olanzapine standard oral tablet (SOT). Olanzapine bioavailability data were evaluated to assess early plasma concentration time profiles for olanzapine ODT versus SOT. Methods: In three crossover bioequivalence studies of olanzapine ODT (5, 10, or 20 mg) versus SOT (1 × 5 mg, 2 × 5 mg, 4 × 5 mg), approximately 20 healthy subjects received single-dose ODT and the corresponding dose of SOT (13 or more days between treatments). Olanzapine plasma concentrations, area under the serum concentration– time curve (AUC) and peak concentrations (Cmax) values were evaluated to assess bioequivalence. Early onset of absorption was assessed using comparative absorption profiles. Results: Olanzapine ODT and SOT are bioequivalent based on AUC and Cmax. Overall plasma concentration-time profiles and absorption rate constants were nearly identical between formulations. Nonetheless, with 5 mg olanzapine, 79% of ODT versus 0% of SOT patients had measurable olanzapine concentrations at 15 minutes. Significantly more subjects receiving ODT had higher plasma concentrations over the first hour versus SOT (e.g., 63% versus 10% with 1 ng/mL or more at 45 minJournal of the American Pharmacists Association 253 2004 Abstracts of Contributed Papers treated identically. Fifteen patients were evaluated before and after implementation of the protocol to assess preexisting ordering practices for laboratory tests, epoetin route of administration (subcutaneous versus intravenous) and iron supplements (yes or no). As per the protocol, subcutaneous injections were used in all patients unless the volume (>1 mL) required use of the intravenous route and/or the patient refused the subcutaneous injection. All 15 patients in the intervention group had laboratory monitoring done to assess iron deficiency anemia. Iron supplements were ordered (iron sulfate 300 mg three times daily) for patients with transferrin saturation less than 20% and/or serum ferritin less than 100 ng/mL. The primary end points of the project included: utilization of the subcutaneous route for epoetin, monitoring of baseline iron laboratory values, and increased use of iron when appropriate. Results: Epoetin therapy was not optimized in the host institution before the implementation of the protocol. Before pharmacist intervention, the subcutaneous route was not the primary route of administration, and the intravenous route was used routinely when it was not indicated. In addition, iron store studies were not done consistently to assess for irondeficiency anemia. Even when laboratory values were available and iron was indicated, supplementation was often not ordered with epoetin. In the postpharmacy intervention group, all epoetin orders were changed to subcutaneous where feasible. Iron stores were checked with every new order for epoetin, and iron supplements were consistently ordered if indicated. Conclusions: Pharmacist intervention and pharmacy-managed programs can help optimize drug use. A pharmacy-initiated protocol was shown to improve the use of the appropriate route for administration of epoetin (usually subcutaneous) in chronic renal failure patients. In addition, the protocol improved laboratory monitoring of iron stores and led to increased iron use in patients receiving epoetin. FEATURE FEATURE Annual Meeting Abstracts 2004 utes). Small early concentration differences at become indistinguishable before reaching Cmax. Conclusions: Olanzapine ODT yields a more rapid onset of absorption than SOT as significantly more subjects given ODT achieved slightly higher olanzapine concentrations immediately after administration. The small differences are likely attributable to more rapid onset of ODT gastrointestinal absorption. These differences do not change the conclusion of bioequivalence. The relevance of earlier onset of absorption to clinical treatment has not been tested. Original Citation: U.S. Psychiatric Congress, November 6–9, 2003, Orlando, Fla. 112—STANDARDIZED CHEMOTHERAPY ORDER FORMS. Sano H, Waddell J, Doulaveris P, Myhand R, Walter Reed Army Medical Center. E-mail: [email protected] Objective: To develop standardized chemotherapy order forms (SCOFs) for our institution’s most commonly prescribed cancer chemotherapy regimens and determine if the use of these SCOFs is associated with a decrease in prescribing error rate and a decrease in antiemetic costs. Methods: Of the most commonly used chemotherapy regimens from medical and gynecologic oncology, 60 were identified from textbooks, handbooks, primary literature, and consultation with experts. The medication doses, schedules, routes and durations of administration, cycles, required laboratory tests, and recommended supportive measures were extracted from primary literature. Antiemetic needs were drawn from standard nomograms. For each regimen, all of the above data were incorporated into a one-page SCOF in standard word-processing software. Final approval of each SCOF was obtained from the Chief, Oncology Pharmacy Service, the Director, Oncology Pharmacy Residency Program, and the Chief, Hematology-Oncology Service. The 60 SCOFs were developed over a 4-month control period, during which antiemetic cost and prescribing error data were monitored. After the control period, all 60 SCOFs were fielded during a 4-month intervention period, which is ongoing. Antiemetic cost and prescribing error data are being monitored. Differences in prescribing error rate and antiemetic cost between the control and intervention periods will be calculated. Prescribing error rate in the intervention period will also be compared with a historical prescribing error rate for this service. Results: NA. Conclusions: NA. APhA–APPM Nuclear Pharmacy Practice 113—ENHANCED LIVER UPTAKE OF TC99M–LABELED RED BLOOD CELLS DURING GASTROINTESTINAL BLEED SCINTIGRAPHY USING TRANSFUSED RBC COMPARED TO AUTOLOGOUS RBC. Melchior W, Wong K, Beauvais M, Snyder S, 254 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 William Beaumont Hospital. E-mail: wmelchior@ beaumonthospitals.com Objective: To report two cases of altered distribution of Tc-99m–labeled red blood cells (RBC) to the liver during GI studies. Methods: GI bleed studies were performed on two occasions for a 91-year-old woman and one occasion for a 96-year-old man. The in vitro method of RBC labeling with Tc-99m was used (Ultratag, Mallinckrodt Medical, following the package insert directions). For the woman, the first study used autologous blood, while her second study was performed using cells from donor packed cells infused the day of the study. The study for the man was performed using cells from donor packed cells infused the day of the study. Quality control was performed following the package insert directions for all lots of labeled RBC. Binding of Tc-99m to the RBC was 98.0% to 99.4%. Results: All studies were negative for a GI bleed. Using the heart as the reference organ, the relative degree of liver uptake for the woman was 45% using autologous blood and 97% using transfused blood, and 91% for the man using transfused blood. Conclusions: Increased liver uptake of Tc99m–labeled RBC obtained from a unit of transfused packed RBC was demonstrated compared with Tc-99m–labeled autologous RBC. Liver uptake of Tc-99m–labeled RBC is normally 50% or less using the heart as the reference organ. Although survival of transfused RBC is normal in cells surviving beyond 24 hours, a small but unknown percentage of transfused RBC is not expected to survive the transfusion process. The basis of the increased liver uptake of Tc-99m–labeled RBC obtained from a unit of transfused packed RBC seen in these cases is unknown. When using Tc99m–labeled transfused RBC for the evaluation of gastrointestinal bleeding increased uptake in the liver may be anticipated. 114—EXPECTED QUALITY OF LIFE AND COST IMPLICATIONS OF R-CHOP AND RADIOIMMUNOTHERAPY REGIMENS FOR INDOLENT NON-HODGKIN´S LYMPHOMA. Chumney E, Kit S, Cheng K, Chris B, Hall P, Medical University of South Carolina. E-mail: [email protected] Objective: The recent introduction of radiolabeled antibodies (radioimmunotherapy) has offered a promising new therapy for indolent nonHodgkin’s lymphoma (NHL), though with varying efficacy estimates. The major objective of this study is to examine the effect of these varying estimates on patient outcomes, costs, and quality of life. Methods: A Markov model was used to simulate the experience of newly diagnosed indolent NHL patients treated with the conventional course of rituximab and cyclophosphamide/doxorubicin/vincristine/prednisone (R-CHOP) followed by radioimmunotherapy and then palliative care. The model comprises 10 health states including complete, partial, and no response to each treatment course, and then death. Patients transition through at 1-month intervals with transition probabilities based on pub- lished estimates; the literature searches included Medline, ScienceDirect, general Internet searches, and company information. Quality of life estimates were based on expert pharmacist opinion using visual analog scales, and cost estimates were based on the average wholesale price (AWP). Results: Our base model with a 26% complete response rate to radioimmunotherapy has total treatment costs of $212,233 per patient. Median survival time after diagnosis is 7.8 years, with 41% of patients still alive at the end of the ten-year period. Mean quality-adjusted life-years (QALYs) are 2.89. We next programmed the model with a 76% complete response rate and found total treatment costs of $211,639 per patient with mean QALYs of 3.54. We will also report on potential benefits if the order of treatment is reversed so that patients have radioimmunotherapy as their front-line therapy. Conclusions: Although the efficacy estimates of radioimmunotherapy vary widely in the literature, we found they produced only a slight difference in the resulting 10-year cost estimates. This is primarily attributed to the treatment sequence of the base model. The different assumptions of efficacy had a large effect on the patients’ overall quality of life. 115—ORGANIZATION OF LYMPHOSCINTIGRAPHY PROTOCOLS. Beauvais M, William Beaumont Hospital, Dobish D, William Beaumont Hospital, Melchior W, William Beaumont Hospital. E-mail: mbeauvais@ beaumonthospitals.com Objective: Various lymphoscintigraphy protocols are ordered by the surgical physicians in a large teaching hospital. To clarify the instructions of the physicians, a nuclear medicine department unfiltered Tc-99m sulfur colloid breast lymphatic mapping request form was developed. The purpose of this project was to create a simplified method for drawing up and dispensing the requested doses. This led to the creation of a nuclear pharmacy preparation guideline form. Methods: Physician requests were reviewed and a Tc-99m sulfur colloid breast lymphatic mapping request form was devised. The form describes the Tc-99m sulfur colloid activity required for each protocol, the size and number of syringes the dose should be dispensed in, the gauge of needle to attach to the syringes, the radiopharmaceutical concentration and volume as well as injection instructions for the physician. Tc-99m sulfur colloid syringes for the subareolar and peritumoral protocols were measured before and after injection to determine the residual activity in the syringes. The postinjection activity was decay corrected to the time of the preinjection measurement. The appropriate concentrations for each protocol were determined and a nuclear pharmacy preparation guideline form was developed. Results: A nuclear pharmacy preparation guideline form was devised based on preinjection and postinjection Tc-99m sulfur colloid syringe measurements to aid radiopharmacy personnel to prepare the necessary concentration for each lymphoscintigraphy protocol. www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 Conclusions: In a busy 1,000-bed teaching hospital, various physician orders for lymphoscintigraphy doses required organization. A nuclear pharmacy preparation guideline chart provides a useful guide to accurately dispense Tc-99m sulfur colloid for lymphoscintigraphy procedures. 117—QUALITY CONTROL OF [F18]FACBC: A NON-NATURAL AMINO ACID TUMOR IMAGING AGENT. Crowe R, Yu W, Goodman M, Emory University. E-mail: [email protected] Objective: FACBC, anti-1-amino-3-[F-18]fluorocyclobutyl-1-carboxylic acid, is a non-natural amino acid that has shown promise for PET tumor imaging. An improved method of synthesis has been Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 118—RADIOPHARMACISTS’ SATISFACTION WITH THEIR EDUCATION/TRAINING, JOB SATISFACTION, AND PROFESSIONAL PRACTICE PATTERNS: RESULTS OF A NATIONAL SURVEY. Wittstrom K, Norenberg J, Borrego M, University of New Mexico. E-mail: [email protected] Objective: This study assessed radiopharmacists’ satisfaction with their radiopharmacy training and education (T&E) and job satisfaction. The study also identified factors that have influenced radiopharmacists’ decision to enter, continue, or exit this specialty practice. Methods: A 20-item, self-administered survey was developed and pilot-tested using a convenient sample of practicing radiopharmacists. The study sample included all U.S. radiopharmacists identified through databases of licensed pharmacists, radiopharmacy continuing education program subscribers, and alumni records (N = 789). Follow-up surveys were mailed to nonrespondents. Results: Overall usable response rate was 41% (N = 327). Of those respondents practicing radiopharmacy, 64% were Board Certified Nuclear Pharmacists (BCNPs), 81% were men, 64% listed BS Pharmacy as their highest degree, and 54% received their T&E through a certificate program. Respondents trained in an academic setting felt more prepared to perform radiopharmacy practice functions, compared with those completing a certificate program. Board certification did not influence preparedness to perform radiopharmacy practice functions. Overall, most radiopharmacists were satisfied with their current position. Of the respondents practicing pharmacy, the most frequently cited reasons for leaving radiopharmacy practice, included family reasons, difficult hours, and management issues. Conclusions: The results of the survey provide information regarding radiopharmacists´ satisfaction with their T&E, and job satisfaction with their current radiopharmacy position. Results of this study can be used to improve existing radiopharmacy educational program curricula and to develop new continuing radiopharmacy education programs to address perceived T&E deficiencies. 119—STABILITY OF FILTERED TC-99M SULFUR COLLOID. Ponto J, University of Iowa. E-mail: [email protected] Objective: Filtered Tc-99m sulfur colloid has recently gained popularity for use in lymphoscintigraphic mapping of lymphatic flow and identification of sentinel lymph nodes. This study was undertaken to evaluate the stability of filtered Tc-99m sulfur colloid stored in glass vials over a period of 8 hours. Methods: About 100 mCi of routinely prepared Tc-99m sulfur colloid was passed through a 0.1micron filter (Millex-VV, Millipore Corp, Bedford, Mass.). The filtrate was collected in a sterile glass vial (Hollister-Stier, Spokane, Wash.) and diluted to a concentration of about 4 mCi/mL. Samples were withdrawn from this stock vial at 2-hour intervals and subjected to the following testing: (1) thin-layer chromatography to assess radiochemical purity; (2) measurement of specific activity (mCi/gram) as assayed in a dose calibrator and weighed on an analytical balance, to indirectly assess sedimentation/adsorption to container walls; and (3) measurement of specific activity (mCi/gram) following re-filtration through another 0.1-micron filter to indirectly assess changes in particle size (e.g., aggregation or clumping). This procedure was repeated on a total of ten separate preparations of filtered Tc-99m sulfur colloid. Results: Results are expressed as mean (range) values. (1) Radiochemical purity of the filtered Tc99m sulfur colloid in the stock vial decreased slightly from 99.3% (98.7–99.7%) at the time of preparation to 98.6% (98.3–99.5%) at 8 hours. (2) The specific activity of filtered Tc-99m sulfur colloid in the stock vial decreased slightly to 97% (94–101%) of its original value at 8 hours. (3) The specific activity of refiltered samples decreased slightly to 94% Journal of the American Pharmacists Association 255 2004 Abstracts of Contributed Papers 116—PREPARATION OF [C-11]-CFT FOR PET MEASUREMENT OF CEREBRAL DOPAMINE TRANSPORT ACTIVITY. Moerlein S, Perlmutter J, Patel P, Welch M, Washington University in St. Louis. E-mail: [email protected] Objective: Positron emission tomography (PET) is used to assess changes in degenerative disorders such as Parkinson’s disease or Huntington’s disease. With the goal of developing a more sensitive tracer for measurement of these changes, we have optimized the preparation of carbon-11 labeled β-CFT [(-)-2-β-carbomethoxy-3-β-(4 fluoropheny)tropane] suitable for clinical application in human subjects. Methods: [C-11]Carbon dioxide was produced using the 16-MeV proton beam of a JSW 16/8 medical cyclotron. The target was emptied into a PETtrace MeI MicroLab. This microprocessor-controlled device catalytically converts [C-11]carbon dioxide to [C-11]methane, which is subsequently iodinated to yield [C-11]methyl iodide. Approximately 12 minutes after target emptying, the [C-11]methyl iodide is bubbled into a solution of 0.5 mg of (nor-methyl)β-CFT in 200 µL of dimethylformamide cooled in an ice bath. The reaction mixture is heated at 70º C for 3 minutes. The crude product mixture is diluted with 4 mL of HPLC solvent and purified using semipreparative HPLC (Partisil 10 ODS-3; acetonitrile/10 mM monobasic potassium phosphate (40/60); 5 mL/min). The product fraction is diluted with 150 mL of 4 µM sodium hydroxide, and passed through a SepPak C18 extraction cartridge, which is then rinsed with 10 mL Sterile Water for Injection, USP. The radiopharmaceutical is eluted from the SepPak with 1.1 mL of Ethyl Alcohol, USP, through a 0.2 µ Acrodisc filter into a 10 mL sterile empty vial. The solution is diluted with 10 mL of Saline for Injection, USP to give the reformulated [C-11]βCFT in a 10% ethanolic solution. Results: Batch yields of [C-11]β-CFT prepared in this manner are 28.3 ± 10.1 mCi (N = 41), with specific activity >1000 Ci/mmol and radiochemical purity >97%, and are sterile and apyrogenic. The overall preparation time is 60 minutes EOB. Conclusions: This methodology is a reliable method for the clinical production of [C-11]β-CFT for PET studies of human subjects. reported that demonstrates high stereoselectivity and possible suitability for larger scale preparation. Determine and develop potential quality control (QC) methods to ensure safe intravenous administration and begin data collection in anticipation of IND submission. Methods: Design: FACBC was synthesized using an automated chemical process control unit (CPCU) with a computer interface (CTI, Inc.). Upon completion of synthesis, the FACBC is purified by passage through an Ion Retard column assembly and 0.22-µm sterilizing filter before collection. The QC of FACBC included analysis for sterility, pyrogenicity, pH, clarity, and purity. Purity is evaluated using TLC with radiometric detection, GC analysis, and timed radioactive decay. Sterility is evaluated per USP guidelines, and PET is performed using the LAL gelclot method. Setting: All procedures performed in a licensed radiopharmacy laboratory. Patients: Limited to patients presenting probable metastatic brain carcinoma and referred by neurosurgery services of the Emory Healthcare System. Results: For all lots of FACBC, radiochemical and radionuclidic purity have been greater than 99%. Sterility and endotoxin testing have been negative. pH range has been 5.5–6.0. GC analysis has shown only trace amounts of organic solvents. FACBC has been used in 12 people at Emory with no local, neurologic, or systemic toxicities observed. Additional QC testing procedures have been identified as potential requisites for release. Conclusions: QC results have exceeded established in-house limits of acceptability. However, more investigation into the characterization of major nonradioactive species present and evaluation of the potential toxicity of FACBC must be completed to obtain regulatory approval for extensive human use. The Emory FACBC study is a pilot study to determine subsequent broad study feasibility and generate pilot data and is under the oversight of the Emory Radioactive Drug Research Committee. FEATURE FEATURE Annual Meeting Abstracts 2004 (89%–100%) of the corresponding specific activity of filtered Tc-99m sulfur colloid in the stock vial at 8 hours. Conclusions: Filtered Tc-99m sulfur colloid stored in glass vials appears to maintain acceptable stability, in terms of radiochemical purity, sedimentation and adsorption to container walls, and particulate size, throughout a period of 8 hours. APhA–APPM Specialized Pharmaceutical Services 120—ASSESSMENT OF A COMMUNITY PHARMACY-BASED DISEASE-STATE MANAGEMENT PROGRAM. Cuellar D, Dodd M, University of New Mexico. E-mail: [email protected] Objective: To describe a community pharmacybased disease-state management (DSM) program in the areas of diabetes and cardiovascular risk reduction in an ethnically diverse population and describe the effectiveness of this program in achieving national treatment guideline goals. Methods: This study reports outcomes from a recently developed community pharmacy-based DSM program in an ethnically diverse community. A retrospective review of patient data collected through January 2004 is presented. All patients seen in the community pharmacy-based DSM program for diabetes or cardiovascular risk reduction are included in this analysis. Physicians or pharmacists refer their patients to this community pharmacybased DSM clinic, or patients self-refer. All patients receive oral and written DSM education during every visit with the pharmacist. A complete medical history is collected at the initial visit. Additionally, blood pressure, glycosylated hemoglobin, fasting glucose, and a fasting lipid panel are obtained at baseline and every 6 weeks after enrollment. A plan is developed with the patient and assessed at each visit. Therapy recommendations are made to the patients’ primary provider after every visit. The analysis includes a description of patient demographics, including number of cardiovascular risks and number of patients at treatment goals by ethnicity, gender, age, type of physician, and type of insurance. Student’s t test is used to analyze differences in blood pressure, glycosylated hemoglobin, fasting glucose, and lipid panel values between visits. Acceptance of treatment recommendations by patients’ primary providers is also described. Results: NA. Conclusions: NA. 121—DEVELOPMENT AND IMPLEMENTATION OF A WEB-BASED TOOL TO ALERT, DOCUMENT, AND COMPENSATE CONSULTANT PHARMACISTS UNDER A POLYPHARMACY DRUG USE REVIEW PROGRAM. Trygstad T, University of North Carolina at Chapel Hill, Thorpe J, AccessCare Inc. E-mail: [email protected] Objective: To describe and demonstrate a Webbased product that alerts consultant pharmacists to 256 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 potential drug-related problems among nursing home patients and documents responses to problem alerts. Methods: A polypharmacy intervention project targeting North Carolina Medicaid recipients in nursing homes was launched in November 2002. The initiative developed rapidly and now serves more than 300 nursing facilities and 18,000 Medicaid patients. The intervention was developed by pharmacists under the auspices of a nonprofit network of physicians serving Medicaid recipients (AccessCare). Consultant pharmacists are paid separately by the network for their response to potential drug therapy problem alerts generated from Medicaid claims data. Early experiences with a paper-based profile alert and documentation system stimulated the development of ConsultRx, a Webbased application. The software was developed in 6 months and involved two programmers and two pharmacists. The program allows consultant pharmacists to access and download patient drug profile data from claims databases for purposes of identifying possible drug-related problems. The database is updated monthly with the most recent claims available that include drug name, amount paid, prescriber, and a host of other associated claims information. Additionally, the program allows for “flagging” of possible drug-related problems and suboptimal therapy. The flagging criteria can be updated whenever desired. The application also allows the pharmacist to document interventions and submit them for payment. Results: The success of ConsultRx is being evaluated after 6 months’ usage. Criteria for success include: (1) number of consultants who elect to use the system to identify and resolve potential drug therapy problems, (2) cost savings associated with editing and submitting claims for payment for drug therapy problem and resolution activities, (3) User satisfaction as measured by user response to a questionnaire administered after 6 months, and (4) efficiency of documentation, as measured by average intervention time from initiation to final submission, number of interventions per user per month, and response to flagging criteria as measured by rates of interventions regarding any of the given criteria. Conclusions: NA 122—EDUCATING PHARMACY STUDENTS ABOUT END-OF-LIFE CARE THROUGH A CLERKSHIP ROTATION. Amerson A, University of Kentucky, Kelley D, Hospice of the Bluegrass. E-mail: [email protected] Objective: Describe the benefit to one hospice in providing rotation experiences for pharmacy students and discuss services that pharmacy students can provide as part of their learning experience. Methods: A 1-month rotation in end-of-life care was begun for pharmacy students at hospice in 1995. Because there was no pharmacist at the hospice site, a college of pharmacy faculty member and the student coordinator for hospice (a nurse) jointly precepted the rotation. The student coordinator coordinated the activities for the student at hospice, and the pharmacy faculty member met with the stu- dent weekly for discussions on topics and review of patients and assignments. The hospice now employs a full-time pharmacist who helps precept students with the faculty member. An experience is provided for 8 –10 students per year. Results: Benefits for hospice are that the student provides in-service education for nursing staff, answers drug information questions as needed, works on medication use evaluation projects, counsels patients/caregivers on medication use, develops written information for patients/caregivers, newsletters, and the pharmacy and therapeutics committee, and extends existing pharmacy personnel for team meetings/rounds. Students benefit in that they learn the philosophy of hospice care, see roles of different team members (e.g., chaplain, social worker), address difficult symptom management issues (pain, dyspnea, nausea, vomiting), counsel patients and caregivers, prepare and present written drug information, and see patients in both home and inpatient settings. Specific student projects and activities are described. Comments from student evaluations have been very positive about the experience and indicate that students perceive a benefit from participating in end-of-life patient care. Conclusions: Students learn about opportunities to provide pharmacy services in end-of-life care. Original Citation: This poster was presented at the National Hospice and Palliative Care Organization’s 18th Management and Leadership Conference, September 7, 2003, Phoenix, Ariz. 123—EFFECTS OF A ONE-YEAR PHARMACIST MANAGED CORONARY HEART DISEASE RISK REDUCTION PROGRAM AT AN AIR FORCE BASE CLINIC. Nicholson S, Benefis Healthcare, Great Falls, Montana. E-mail: [email protected] Objective: To reduce the risk for coronary heart disease (CHD) in identified patients. Therapeutic targets included attainment of National Cholesterol Education Program (NCEP) LDL cholesterol goals, modification of CHD risk factors, and reduction of 10-year CHD risk estimates. Methods: Patients with diabetes or elevated cholesterol were identified from clinic records and invited to participate. Additional patients were enrolled through physician referrals. A total of 32 patients participated for varying periods up to 14 months. Charts, laboratory reports, and lifestyle questionnaires were used to collect risk data. Appointments were conducted individually with a clinical pharmacist, and these consisted of atherosclerosis education, CHD risk assessment, setting of therapeutic goals, and treatment planning. Intervention targets included nutrition, exercise, smoking, weight, blood pressure, stress level, and medication use. If appropriate, patients were referred to established diabetes, cholesterol, and tobacco cessation programs on base. Medication recommendations were made to the patient’s primary care provider (the pharmacist did not have prescriptive authority). Visits were documented in the patient’s medical record using a standardized charting form cosigned by a physician. Follow-up visits www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 and laboratory visits were generally scheduled at 3month intervals. Computer software was used to calculate 10-year CHD risk estimates. Results: Enrollees who attended less than three appointments did not have significant changes in CHD parameters. A total of 23 enrollees attended three or more appointments. Among these patients, four attained NCEP LDL cholesterol goals, two eliminated major risk factors by increasing HDL cholesterol, nine attained triglyceride goals, two attained waist-reduction goals, and two attained body mass index goals. The mean estimated 10-year absolute risk of CHD decreased from 12.6% to 10.8% in this group. Conclusions: This project demonstrates that a pharmacist managed CHD risk reduction program can reduce LDL cholesterol levels, modify CHD risk factors and reduce the estimated 10-year risk of CHD in patients who attend more than two appointments. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 125—SUCCESSFUL INCLUSION OF PHARMACY PRACTICE INTO THE HOME CARE SETTING. Macklin L, University of Montana. E-mail: [email protected] Objective: A multiservice, small home care agency wanted to elevate its standard of care by having a pharmacist help the home health and hospice nurses provide optimal drug therapy management for its patients. The local school of pharmacy needed more ambulatory care advanced practice experiences (APEs) and instructors for its expanding pharmacy program. In 1995, the two organizations collaborated to fund a full-time, split consultant pharmacist position to determine if such a position would meet their joint needs. Methods: The position was evaluated annually for integration of the pharmacist into the patient care teams and effectiveness of the pharmacist meeting predetermined educational, clinical, operational, and financial objectives. Results: The university secured not only a needed ambulatory care APE but also a clinical instructor to help teach didactic and experiential courses. The position is cost-effective because the agency has access to a full-time pharmacist and yet is only paying for a half-time position. The pharmacist helps with patient care by performing medication reviews and pain consults, participating in weekly team meetings, answering drug information questions, developing patient medication teaching materials, and going on home visits. To help with operational needs, the pharmacist coordinates pharmacy needs between hospice and the home infusion program, as well as with outside contract pharmacies. The pharmacist also serves as a mini-case manager for medication needs for rehabilitation patients. To help with quality improvement, the pharmacist performs drug-use reviews, helps develop agency policies and procedures when related to medications, and serves on the agency’s pain committee. Lastly, the pharmacist financially helps the hospice program by overseeing the medication formulary, contracting with local pharmacies, and reviewing pharmacy bills for accuracy. Conclusions: Since the inclusion of the consultant pharmacist/clinical professor position 8 years ago, the joint venture has been successful. Original Citation: “How to Succeed by Adding Pharmacy Services,” at the National Association of Home Care’s Meeting in Salt Lake City, UT. Session speaker, 10/28/2002. 126—INFORMED CONSENT FORMS— GOBBLEDYGOOK? Colucci N, Massachusetts College of Pharmacy and Health Sciences–Worcester, Donahue M, Lahoz M, Massachusetts College of Pharmacy and Health Sciences–Worcester. E-mail: nancy.colucci@ students.mcp.edu Objective: An informed consent form (ICF) is intended to provide potential recruits to a clinical research trial (CRT) with details of the nature of the study, risks and benefits involved, and a recruit’s rights and responsibilities. We conducted a project to meet the requirements of an elective course, “Addressing the Health Literacy Challenge.” Studies have shown that language used in ICFs is not comprehensible to most people. The primary objective of our project was to measure the gap between the readability of ICFs and the literacy skills of CRT participants. Our secondary objectives were to raise awareness of this gap and to offer a solution for bridging this gap. Methods: We conducted our project at an outpatient CRT center over a 6-week period. We used the Fry formula and SMOG grading to assess the readability of 15 ICFs, and the Rapid Estimate of Adult Literacy in Medicine (REALM) test to measure the reading skills of a sample of 26 CRT participants. Results: The average readability score of the ICFs was 14th grade on the Fry chart and 12th grade on the SMOG. The REALM test showed that the average reading skill of the CRT participants was at the 11th grade level, which is higher than the reported average of 8th- to 9th-grade level for adult Americans. We presented our findings to the research coordinators. To help bridge the observed gap, we developed a seven-item test of comprehension that coordinators could use to help pinpoint specific ICF parts that may need further clarification with a potential CRT recruit. Conclusions: ICFs are written at readability levels that may be above the literacy skills of many CRT participants. Efforts should be made to simplify ICFs or supplement them with other forms of instruction so CRT recruits can really make an informed choice. APhA–APPM Miscellaneous 127—ATTITUDES AND OPINIONS ON CONTINUING EDUCATION, TRAINING, AND READINESS TO ASSUME NEW PROFESSIONAL RESPONSIBILITIES BY CERTIFIED PHARMACY TECHNICIANS. Jacobson S, Steere P, Foye L, Massachusetts College of Pharmacy and Health Sciences. E-mail: sjacobson@ mcp.edu Objective: To survey technicians certified by the Pharmacy Technician Certification Board in Massachusetts regarding such elements of practice as preferred channels for receipt of continuing education, perceptions of their present professional status, relationships between job training and actual duties performed in the course of practice, and their readiness to take on new or expanded roles. Methods: A grant application was submitted and accepted in 2002 supporting a 43-question survey that was approved by an institutional review board. The survey was mailed to 1,815 certified pharmacy technicians. The survey questions addressed pharJournal of the American Pharmacists Association 257 2004 Abstracts of Contributed Papers 124—ESTABLISHMENT OF A PHARMACIST CONSULTING TEAM FOR STATEWIDE BIOTERRORISM PREPAREDNESS. Feret B, Bratberg J, University of Rhode Island, Curzake J, CVS Pharmacy, Kogut S, Low G, University of Rhode Island, Cordy C, Orsini M, Rhode Island Department of Health. E-mail: [email protected] Objective: The objective of this program was to develop, test, and maintain a statewide bioterrorism preparedness plan in collaboration with a core group of pharmacy consultants. Methods: The Department of Health and Board of Pharmacy for the State of Rhode Island developed a plan for bioterrorism preparedness after the terrorist events of 2001. This included plans for the receipt, distribution, and dispensing of the Strategic National Stockpile (SNS) of medications and supplies from the Centers for Disease Control and Prevention (CDC). Since pharmaceuticals and dispensing of medications to the public constitute an important portion of a bioterrorism plan, the state recognized the importance of having pharmacists involved in the planning process. Five pharmacy consultants were recruited by the Board of Pharmacy through an application process. The five pharmacists hired were a community pharmacist, three faculty members from the University of Rhode Island with specialties in community pharmacy, infectious diseases, and pharmacoepidemiology, and a graduate student with expertise in pharmacoinformatics. The five consultants developed a plan for the local municipalities for the mass distribution of antibiotics to the public, drug selection algorithms, and the development of patient assessment tools. Results: To date the five pharmacy consultants, along with the Department of Health, have developed a plan for the mass-distribution municipal clinics for a bioterrorist event involving a bacterial agent, including drug selection algorithms based on current recommendations and a patient assessment form. This plan was recently exercised in August 2003, including the receipt of a SNS training package from CDC. Conclusions: Collaboration between the pharmacy consultants and the Department of Health has been very successful in improving the preparedness for the state of Rhode Island and its local municipalities in the event of a bioterrorist event. FEATURE FEATURE Annual Meeting Abstracts 2004 macy technicians’ training, aspects of their present responsibilities, and topics relevant to job satisfaction. It also examined their preferences regarding continuing education credit. Results: A total of 288 (16%) usable responses were returned. Data will be presented on broad opinions of respondents on issues such as salary commensurate with job duties, training, perceptions of their value to the profession, and desired channels and subject matter for continuing education. Information is being tabulated according to years of experience, practice setting and employment status, and the analysis will correlate impressions of continuing education with the technicians’ developmental needs toward assuming expanded roles within the profession of pharmacy. Conclusions: NA. 128—CREATION, IMPLEMENTATION, AND ASSESSMENT OF A WEIGHT MANAGEMENT ELECTIVE COURSE IN A PHARMACY CURRICULUM. Ahrens R, Ciardulli L, Shenandoah University. E-mail: [email protected] Objective: To develop, implement, and evaluate an interactive and interdisciplinary weight management course. Methods: Course objectives were designed to give students a background in weight management issues and to develop skills needed to assess and manage the overweight/obese patient. These skills were taught in a classroom and field exercise format. Students actively participated in applying skills taught through the use of diet/exercise histories and weekly health goals. As an interdisciplinary approach to learning, a dietitian and an athletic trainer were invited to share their ideas on lifestyle modifications. Field exercises included a grocery store and fitness center informational tour. Students were evaluated by presentations and the development of portfolios. Knowledge tests and physical assessments (cholesterol panel, weight, body fat percentage, waist circumference, blood pressure, and blood glucose) were administered before the course and upon course completion. The formal course evaluation included open-ended and closeended assessments. Results: The course was initially offered in fall 2002 as a 1-hour elective with an enrollment of 16. Students were actively involved in the course format with open discussions of weight management issues on an individual and global level. Overall evaluations of the course were strongly positive. Open-ended comments were also positive and indicated a growth in knowledge of health issues and awareness of obesity as an epidemic. In addition, class participants indicated they would recommend the course to other students. Conclusions: Results indicate satisfaction with course design and content. Further expansion of course topics within the school’s curriculum will be explored. Original Citation: American Association of Colleges of Pharmacy Annual Meeting, Minneapolis, Minn., July 2003. 258 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 129—HERBAL AND SUPPLEMENT USE IN A MILITARY HEALTH CARE SETTING AND THE ASSOCIATED DRUGHERBAL/SUPPLEMENT AND DISEASEHERBAL/SUPPLEMENT INTERACTIONS. Lagasse C, United States Air Force, Halperin T, University of the Pacific School of Pharmacy and Health Sciences, Johnson J, United States Air Force. E-mail: [email protected] Objective: To describe the percentage of military outpatient pharmacy patrons who use herbal products and/or supplements and describe the associated potential drug-herbal/supplement or herbal/supplement-disease state interactions Methods: Design: Prospective and descriptive. A convenience sample of patients will be surveyed regarding their use of herbal and/or supplement products. Patient surveys will be conducted at three outpatient pharmacies while patients are waiting to pick up their medications. The patient’s medication profile and medical record (when possible) will be reviewed to assess for drug-herbal/supplement or disease-herbal/supplement interactions. Setting: Three outpatient pharmacies of a west coast Air Force base. Patients: This study will include 385 English-speaking patients at least 18 years of age. Results: Age, gender, active duty/dependent status, and number of patrons using herbal products and supplements will be reported and analyzed. Herbal products and supplements used and associated drug-herbal/supplement and herbal/supplementdisease state interactions will also be categorized by number and type. In addition, the number of patients using these products who have informed their doctor, the patient’s self-assessed knowledge level of the products they are using, and the patient’s information sources will be recorded. Conclusions: The results of this study will provide an estimate of military pharmacy patrons who use herbals and supplements and the associated potential drug and disease interactions. This will give military health care providers a better idea of the scope of herb and supplement use, related drugherbal/supplement and disease-herbal/supplement interactions, and may suggest a need for increased education in this area. APhA–APPM Pharmacy Residents 130—A COMPARISON OF THE VALIDITY AND RELIABILITY OF AUTOMATIC BLOOD PRESSURE MONITORS. Warburton S, Daniel K, Marsh W, Nova Southeastern University. E-mail: [email protected] Objective: The objective of this study is to determine if there is a difference in the validity and reliability of four automatic blood pressure monitors when compared with the gold standard mercury sphygmomanometer in measuring blood pressure. The primary outcome of the study is the validity of blood pressure readings taken by each automatic blood pressure monitor when compared with blood pressure readings from the mercury sphygmo- manometer. The secondary outcome of the study is reliability of each of the automatic blood pressure monitors. Methods: Thirty normotensive people are being recruited to participate in the study at Nova Southeastern University Clinic Pharmacy, Fort Lauderdale, Florida. Normotensive subjects are being chosen to reduce the variability within the measurements to better evaluate validity and reliability. Participants are at least 18 years of age and able to sign the written consent for participation. Each subject has his or her blood pressure measured by each of the four automatic blood pressure monitors and by the mercury sphygmomanometer two separate times with a two-minute interval between each measurement. All patients are asked to be seated with their arm at heart level and feet flat on the floor. The order of testing with each monitor is being randomized for each patient. For the primary outcome, the percent of times that each automatic monitor produces a result within 4 mm Hg of the measured blood pressure by the mercury sphygmomanometer will be used. Similarly, for the secondary outcome, the test–retest reliability of each automatic machine will be measured. If the two readings on any monitor differ by greater than 4 mm Hg, then a third measurement will be taken on that monitor. Before the study began, all researchers performed blood pressure measurements on a sample of subjects to check interrater reliability using the kappa coefficient, and then to resolve differences between researchers. Data will be analyzed using SPSS version 11.1. Results: Data are currently being collected. Preliminary results indicate a lack of validity with at least one of the store brand monitors. Final results will be presented at the meeting. Conclusions: NA. 131—A CROSS-SECTIONAL SURVEY OF COMMUNITY PHARMACISTS AND LEVEL OF COMFORT IN ANSWERING QUESTIONS ABOUT HERBS. Cormier L, Texas Southern University. E-mail: [email protected] Objective: To assess the comfort level of community pharmacists in answering questions about herbs and to compare comfort levels with corresponding demographics, education, and pharmacy practice experience. Methods: Design: Community pharmacists in a particular district of a retail chain in Houston, Texas will be surveyed between December 2003 and February 2004. The survey sheet will contain the following items: demographics, all previous and current practice settings, year graduated from pharmacy school, type of pharmacy degree obtained, average number of times the pharmacist is asked a question about herbs, which herbs have the most frequent questions, how comfortable they are to answer herbal questions, and the factors attributed to that comfort level. Setting: The survey will be conducted in the pharmacies of a particular district of a retail chain in Houston, Texas. Patients/Participants: Pharmacists in the pharmacies www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 of a particular district of a retail chain in Houston, Texas. Data Collection: Surveys with questions about demographics, pharmacy practice experience, graduation date from pharmacy school, pharmacy degree obtained, average number of herbal questions asked, herbs asked about most frequently, and comfort level in answering questions about herbs will be analyzed. Analysis Plan: The surveys will be analyzed to determine the average comfort level of community pharmacists in relation to answering questions about herbal products and if there is any correlation between comfort level and demographics, clinical education, and pharmacy practice experience. Other appropriate qualitative methods: NA. Results: It is hypothesized that most pharmacists will be slightly apprehensive in answering questions about herbs. Conclusions: NA. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 133—AN EVALUATION OF SENIOR CITIZEN PATIENT COMPLIANCE IN A COMMUNITY GROCERY CHAIN PHARMACY AFTER INITIATING A REFILL REMINDER SYSTEM. Morales C, Hampton K, Safeway Pharmacy. E-mail: [email protected] Objective: To assess the impact of a refill reminder system on senior citizen medication compliance by evaluating changes in medication compliance as well as patient and pharmacy staff satisfaction. Methods: The refill reminder system will be implemented in two pharmacy locations. Patients will be selected to participate based on certain inclusion and exclusion criteria. The inclusion criteria includes patients at least 60 years of age, patients having at least two refills for one “chronic” medication in the last year, and a Morisky score of 0 to 3. A baseline analysis will be conducted to determine each enrolled patient’s refill compliance over the past 6 months. Pharmacy personnel will call each patient 3 to 5 days prior to the refill date and inform them to call in that refill using our automated refill system. After a period of at least 3 months and up to 6 months, refill compliance and poststudy Morisky scales will again be assessed and then compared with baseline. At the conclusion of the study, all participating patients and pharmacy staff will be given a survey to assess their satisfaction with the program. Results: The effectiveness of this program in improving patient compliance will be evaluated using a comparison of pre- and post-Morisky scales and an analysis of the time between prescription refills using appropriate statistical tests. In addition, patient and pharmacy staff satisfaction will be evaluated using descriptive statistics. Conclusions: It is expected that this refill reminder system will increase patient compliance and that both the patients and pharmacy staff will be satisfied with the program. 134—ANALYSIS OF REIMBURSEMENT PATTERNS FOR PHARMACISTS WHO PROVIDE DIABETES CARE SERVICES. Wells A, Campbell University, Steiner G, Campbell University/Kerr Drug. E-mail: we2apothecary@ yahoo.com Objective: The primary objective of this study is to identify professional characteristics of pharmacists who are currently obtaining reimbursement for the provision of diabetes care services. The secondary objectives are to identify which third party payers are reimbursing pharmacists for these services and to determine the mechanism by which pharmacists working in physicians’ offices are being reimbursed. Methods: A questionnaire will be administered via the Internet. The population sample will include the 6,109 male and female pharmacists who maintain an active license on record with the state Board of Pharmacy (BOP) and have a current E-mail address. There are no anticipated risks for the population sample being studied. Data will be collected during the community pharmacy practice residency of the principal investigator. Each E-mail will consist of an informative letter requesting pharmacists who provide diabetes care to participate in the survey. A link to the survey web site will be provided at the bottom of each E-mail. Each participant will be provided a unique identifier located within the Email, which the individual must enter at the beginning of the Internet survey. This unique identifier will help the investigator identify information entered multiple times by the same user and keep data anonymous throughout the analysis. If duplicate information is collected, only the first submission will be used, all additional submissions will be discarded prior to data analysis. A limitation of the study is that there may be pharmacists who do not have a current E-mail address on file with the BOP. These subjects will be excluded from the study. Descriptive statistics will be used to examine the data collected in the survey. The Internet-based questionnaire will consist of 16 items and is designed to be completed in approximately 5 minutes. The survey will be located on a nonsearchable web site. The pharmacists will be categorized based upon various criteria, including gender, practice setting, and credentials. Pharmacists will be asked to identify diabetes care services offered, the setting in which these services are offered, collaborative efforts with other health care professionals, and reimbursement procedures. In addition, the questionnaire will examine respondents’ billing practices. Results: NA. Conclusions: NA. 135—ANALYSIS OF THE GROWTH TRENDS IN INDUSTRY-BASED POSTGRADUATE TRAINING PROGRAMS FOR PHARMACISTS. Lam A, Rutgers, The State University of New Jersey, Brady P, Eli Lilly & Company, Chow W, Crivera C, Goyal V, Rutgers, The State University of New Jersey, Patel A, Xavier University of Louisiana, Shprecher A, Toma S, Alexander J, Barone J, Rutgers, The State University of New Jersey, Hill B, Auxilium Pharmaceuticals, Suh D, Rutgers, The State University of New Jersey, Ramseyer K, Smith N, Eli Lilly & Company, Williams E, University of North Carolina at Chapel Hill, Romney M, GlaxoSmithKline. E-mail: [email protected] Objective: The objectives of this project are to: (1) conduct a retrospective analysis of the proliferation of industry-based postgraduate training programs over a 20-year period (1983–2003) to better understand the implications of growth, (2) evaluate trends within specific training disciplines, (3) Journal of the American Pharmacists Association 259 2004 Abstracts of Contributed Papers 132—AN EVALUATION OF A MICROABLUMINURIA SCREENING AND EDUCATION PROGRAM IN PATIENTS WITH DIABETES IN A COMMUNITY CHAIN PHARMACY. Olbricht T, Purdue University. E-mail: [email protected] Objective: To screen patients with diabetes for microalbuminuria and educate them about diabetic nephropathy. Additional goals are to: determine if pharmacists in a community pharmacy setting can identify patients at elevated risk of developing diabetic nephropathy (i.e., positive microalbumin test); and evaluate the program by conducting patient surveys to measure knowledge gained, suggestions for improvement, and satisfaction. Methods: Microalbuminuria screenings and education will be conducted in five community pharmacy locations and will involve 23 patients. The primary researcher will provide all educational and testing services, which will be free of charge to the patient. The educational component and the microalbumin protocol will be developed from the American Diabetes Association Guidelines and medical literature. Patient recruitment will be conducted by asking patients on diabetic medications to fill out a survey-test, which will evaluate their knowledge about diabetic nephropathy and find out if they are interested in joining the study. The education component will include such topics as a definition of diabetic nephropathy, what is microalbuminuria, and how to prevent progression into diabetic nephropathy. The microalbumin protocol will consist of three separate screenings using a Accubase ì Alb microalbumin test kit over a 12week period, with educational components during the first and last screenings. Patients will be referred to their doctor if they test positive for microalbuminuria at any of the three screenings. All patients enrolled in the study will be asked to complete a pre- and postknowledge test as well as a satisfaction survey. Results: The effectiveness of this study will be evaluated in two parts. The first part will evaluate how many study patients are at high risk for developing diabetic nephropathy (i.e., positive for microalbuminuria). The second part will be an evaluation of the education component using a comparison of the pre- and postknowledge tests. Conclusions: It is expected that patients will gain knowledge about the pathogenesis, risk factors, and recommended goals associated with diabetic nephropathy and high-risk patients will be identified for referral to their physician. FEATURE FEATURE Annual Meeting Abstracts 2004 improve awareness of the opportunities available to pharmacists within the pharmaceutical industry. Industry-based postgraduate training programs for pharmacists (e.g., residencies, visiting scientists, and fellowships) have experienced substantial growth over the past 20 years. Many companies have established these training programs for pharmacists within key disciplines, including Clinical Research, Drug Information, Medical Affairs, Marketing, Pharmacoeconomics, and Regulatory Affairs, to better prepare pharmacists for a career within the industrial practice setting. Methods: A 20-year retrospective analysis of industry-based postgraduate training programs will be conducted on data obtained from multiple sources. Data will be collected from electronic and printed sources published by professional pharmacy and industry-related associations (AACP, ACCP, APhA, ASHP, DIA, ISPOR), and data contributed from program sponsors. Due to the historical component of this project, programs that have been discontinued may also be accounted for through anecdotal evidence. In this analysis, industry-based postgraduate training programs include residencies, visiting scientist programs, and fellowships that recruit pharmacists for training within pharmaceutical research and manufacturing companies, biotechnology companies, and industry-affiliated consulting companies. Whenever possible, these programs will be quantified based on the number of participants that completed the program. Results: Based on preliminary data, we expect to see a growth in the number of postgraduate industry-based training programs for pharmacists over the last 20 years. The scope of this project also allows for the development of a comprehensive directory of industry-based postgraduate training programs available for pharmacists. Conclusions: NA. 136—ANALYZING SUN-DAMAGED SKIN AND EDUCATION ON PREVENTING FUTURE DAMAGE. Magnus L, Walgreens. Email: [email protected] Objective: This year, the American Cancer Society estimates that 9,800 people will die from skin cancer, the most prevalent cancer in the United States. The primary goal of this study is to help decrease skin cancer deaths through screening and education. A pharmacist will use a Dermaview to show patients the present condition of their skin and provide education. The impact of the pharmacist on patients’ knowledge of sun protection/skin cancer and patient satisfaction with skin screening will be assessed. Methods: The screening will be primarily performed at two different locations within a large chain community pharmacy. About 200 patients will be targeted for enrollment. The patient begins by filling out a risk assessment survey to determine potential risk for skin cancer. Screening with the Dermaview machine can be performed on patients ranging from 13 to 80 years of age. The Dermaview uses a harmless black light to locate and identify dry, oily, and sun-damaged areas of the face. After 260 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 the screening, the pharmacist provides recommendations and education. A pre- and postscreening quiz is administered to test the patients’ knowledge of the sun, tanning, and skin cancer. A survey is also completed by the patient to document the amount of satisfaction and willingness to pay for this type of screening. All patient materials will be approved by the Investigational Review Board. All data collected from the quiz and survey will be analyzed using appropriate statistical tests and then compiled into a written discussion of the project. Results: Preliminary results show that the screenings lead to an increase in skin care awareness and patient satisfaction. Such data are consistent with a single skin screening conducted in Massachusetts by dermatologists. Results from a site-specific needs assessment show patients are interested in skin screening. Conclusions: To be determined. 137—ASSESSING PUBLIC KNOWLEDGE OF SAFE AND APPROPRIATE USE OF ACETAMINOPHEN. Dyer A, Whitaker A, Goode J, Virginia Commonwealth University. E-mail: [email protected] Objective: The purpose of this project is to compare the general public knowledge of safe and appropriate use of acetaminophen between prescription and nonprescription uses of acetaminophen product and to identify areas of education and counseling that need to be addressed through a standardized educational message designed to improve the safe and appropriate use of acetaminophen. Methods: This is a 3-month prospective study conducted in an independent pharmacy. A survey will be used to evaluate acetaminophen knowledge including dosing, interaction with alcohol, and liver toxicity. The survey will also identify individuals and/or places where consumers may have learned information about acetaminophen. All patients receiving an acetaminophen prescription product and nonprescription product will be asked to voluntarily complete the survey. After the respondents have completed their surveys, they will receive an educational pamphlet on acetaminophen. The data collected will be compared between the two groups to assess deficiencies in knowledge and education. After identifying potential problem areas with the knowledge of acetaminophen, an educational program will be developed for the pharmacy. The program will include staff development with a standardized approach to counseling and education of patients receiving acetaminophen. Results: The survey instrument and educational pamphlet have been developed for the project. Conclusions: By assessing the public knowledge of acetaminophen use, the pharmacy will be able to incorporate a standardized delivery of acetaminophen education. 138—ASSESSING THE IMPACT OF A COMMUNITY PHARMACY–BASED RAPID HIV PREDIAGNOSTIC TESTING PROGRAM. Akhtar A, Childress J, Berry T, St. Louis College of Pharmacy. E-mail: [email protected] Objective: The objectives of this study are to (1) identify patients with multiple risk factors for contracting HIV, (2) educate individuals about appropriate strategies that may reduce their risk of contracting HIV, (3) provide preliminary results of HIV status, and (4) evaluate the impact of the availability of HIV screening in the setting of a community pharmacy. Methods: The study will be conducted at one primary community pharmacy with an opportunity to expand to other locations (within the same chain pharmacy) in the metropolitan area. The following subjects will be included: males and females ages 18 years and older who possess risk factors for contracting HIV. Tests will be conducted using a rapid HIV-1 antibody test. Results of the test will be provided and subjects will receive pre- and posttest counseling. Subjects with negative test results will receive counseling on reducing high-risk behaviors. If these subjects engaged in high-risk behaviors in the 3 months prior to the test, a second test will be required in 3 months for confirmation. Subjects with a positive test result will receive counseling on preventing the transmission of HIV and be referred immediately to the local department of health for confirmatory testing and evaluation. All subjects will be contacted after 3 months to determine if further testing was needed and performed and to discuss implementation of risk reduction strategies. Results: Subject recruitment will begin in January 2004 and enrollment is anticipated to continue until 50 subjects are included. Evaluation of objectives will consist of documenting risk factors, giving subjects a posttest to assess understanding of risk reduction strategies, detection of HIV status, and completion of a survey to determine their attitude and receptivity toward HIV screening in this environment. Preliminary data will be evaluated and analysis of these data will be presented. Conclusions: NA. 139—ASSESSING THE IMPACT OF PERFORMING BODY COMPOSITION ANALYSIS ON OVERWEIGHT AND OBESE INDIVIDUALS IN A COMMUNITY PHARMACY. Paulson K, Walgreens. E-mail: kellipaulson@ yahoo.com Objective: The primary objective of this study is to provide overweight and obese patients with education and motivation for proper weight management. Body composition analysis will be provided as a pharmacy service along with the education and motivation for appropriate weight management. Methods: The project is designed to assess the knowledge and motivation of patients in a community pharmacy setting. Throughout the study, patients will have their body composition measured twice. At the initial screening, the patients will have their body composition measured and will be provided with education about their current body composition status. They will also be provided with techniques for appropriate weight management and their motivation will be assessed. Throughout a 3month period, the patient will monitor their weight at home. When the patient returns to the site after 3months they will have their body composition rewww.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 measured and will have their knowledge and motivation reassessed. The patients will also be surveyed about their satisfaction with the service and their willingness to pay for future visits. The data collected will be assessed for any changes in body composition, weight, and motivation. All of the data will be analyzed for statistical significance, with a written report to be submitted for publication. Results: Preliminary results show positive patient satisfaction in body composition analysis performed in a community pharmacy setting as well as an increase in overall weight management knowledge among this population. Conclusions: Conclusions of this study will be determined upon completion. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 141—COMMUNITY PHARMACISTS’ USE OF INTERNET RESOURCES CONTAINING PATIENT EDUCATION MATERIALS. Cruse E, University of Tennessee and Chase Drugs, Johnson S, Hill L, Chase Drugs and Clinical Services, Timpe E, University of Tennessee, Hardin M, Chase Drugs and Clinical Services. E-mail: [email protected] Objective: Community pharmacists are accessible to patients and are in a position to provide valuable education regarding a multitude of disease states and therapeutic modalities. The Internet has become a useful tool for health information, but using it to retrieve information can be daunting for patients and health care professionals alike. Several reliable sources for patient education materials are available on the Internet; these resources are often underused by pharmacists. The objectives of this study are to: (1) determine community pharmacists’ use of Internet resources containing patient education materials, (2) identify barriers to community pharmacists’ use of Internet resources containing patient education materials, and (3) educate community pharmacists about patient education materials on the Internet by distributing written materials that can assist them in the utilization of Internet resources to enhance patient care. Methods: Surveys asking questions about the use of and barriers to using patient education materials from the Internet will be mailed to the attention of the pharmacist-in-charge at 217 pharmacies in the state of Tennessee. The pharmacies will be randomly identified using an alphabetical list provided by the State Board of Pharmacy. The pharmacist-incharge at every seventh pharmacy on the list will receive a survey. A self-addressed, stamped envelope will be provided for return of surveys. Responses to each question will be recorded into tables and a statistician will assist in determining statistical significance. Results: The deadline for completion of surveys is January 15, 2004. Data analysis will be completed by February 15, 2004. The follow-up resource, currently being developed with the assistance of a faculty member at the University of Tennessee Drug Information Center, will be mailed March 1, 2004. Results from this study will be available at the time of the APhA annual meeting and exposition in 2004. Conclusions: NA. 142—EFFECTS OF A PHARMACY-BASED PHYSICAL ACTIVITY EDUCATION PROGRAM USING STEP-COUNTERS. Cole R, Leesburg Pharmacy, Ahrens R, Shenandoah University. E-mail: [email protected] Objective: The purpose of this study is to: (1) create and implement a pharmacist-directed physical activity education program in a community pharmacy setting, (2) educate patients about the importance and benefits of physical activity, and (3) measure the effectiveness of a pharmacist-directed physical activity program in increasing patient activity levels and improving clinical measurements. Methods: This pharmacist-directed study will take place in a community pharmacy in Northern Virginia, enrolling 35 patients. The physical activity program, consisting of walking only, will be a structured 6-week program, of which weeks 0–2 are the control period and weeks 2–6 are the active period. Patients will return to the pharmacy weeks 2, 4 and 6 for a total of four study visits. At their initial visit, a patient history and clinical measurements, including blood pressure, height, weight, and waist circumference, will be taken. Patients will be given a free step-counter, instructed on its use, and asked to record daily number of steps taken to determine their approximate daily activity level prior to the educational intervention. At week 2, activity logs will be collected and clinical measurements retaken. Education will be given by the pharmacist on the benefits of physical activity, exercise techniques, and behavior modification. During weeks 2–6, patients will continue to record daily number of steps taken and return at weeks 4 and 6 for visits with the pharmacist. These visits will consist of clinical measurements and collection of daily activity logs. Results: The effectiveness of the education program will be evaluated by comparing activity levels, as measured by the step-counter, pre- and posteducational intervention. Clinical measurements will be evaluated to assess changes Conclusions: It is anticipated that patients’ physical activity will increase and clinical measurements will improve. 143—ELDERLY HOME CARE MEDICATION MANAGEMENT SERVICE BY COMMUNITY PHARMACISTS. Haughaboo A, Community Pharmacy Care. E-mail: haughaam@ E-mail.uc.edu Objective: In the United States, adverse drug events are a major problem for the elderly. The purpose of this study is to provide home medication management to the elderly and to provide patient education on medications, disease states, and wellness in an effort to decrease adverse drug events and deliver a pleasing patient interactive service. Methods: Candidates for the service will be recruited from senior residential facilities via presentation of the service. Brochures and word-ofmouth will be additional mechanisms of recruitment. Approximately 25 patients will be selected for this program. Initial and follow-up visits will be conducted to provide medication management and patient education on the treatment and prevention of high-risk disease states. Each patient will receive a portfolio including disease state information and their medication profile. The portfolio will be routinely updated. Recommendations to physicians for changes in medication therapy, such as inappropriate patient use of medication, inappropriate prescribing, duplicate therapy, therapy with no indicaJournal of the American Pharmacists Association 261 2004 Abstracts of Contributed Papers 140—ASSESSMENT OF THE CONSUMER’S SELF-CARE AND OVER-THECOUNTER MEDICATION KNOWLEDGE WITH AND WITHOUT PHARMACIST INTERVENTION IN A COMMUNITY PHARMACY POPULATION. Downing J, Kerr Drug/UNC Chapel Hill School of Pharmacy, Brown L, Kerr Drug Clinical Services, Ferreri S, University of North Carolina. E-mail: [email protected] Objective: The primary objective of this study is to assess the knowledge of self-care and over-thecounter (OTC) medications in the community pharmacy population. The secondary objective of this study is to evaluate the effects of the pharmacist’s educational intervention on self-care and OTC medications. Methods: In this pilot study, volunteers complete a survey at the drop-off window in Kerr Drug pharmacy or before attending a scheduled educational program. The survey consists of five questions with multiple choice answers. Surveys 1 and 2 are general self-care and OTC medications questionnaires. Survey 3 is a self-care and OTC medication questionnaire designed specifically for consumers with diabetes. Customers who wish to attend an educational program on self-care indicate this desire my checking a box on the survey. Surveys will be collected at the drop-off window in a collection box. Only the investigators will read and analyze the data and will subsequently determine the self-care knowledge base of the community pharmacy population. Subjects will be recruited to attend a free educational program at Kerr Drug by the surveys, flyers, and word-of-mouth advertising. The educational program will consist of 10 subjects per program in a private classroom within Kerr Drug. At least 20 persons from surveys 1 and 2 and at least 10 persons from survey 3 will be recruited for the educational program. Incentive to attend the program will consist of a coupon for $10 off any of the services offered in the Kerr Health Care Center. The community pharmacy resident will present a 20–30 minute walking education tour of the OTC medication aisles followed by a 10–15 minute question and answer session. Subjects will then be asked to complete the same survey that was filled out before the educational program. Data will be collected and pre- and postprogram surveys will be compared by the community pharmacy resident. Results: NA. Conclusions: NA. FEATURE FEATURE Annual Meeting Abstracts 2004 tion, indication with no therapy, drug–drug interactions, and drug–disease interactions will be recorded. The number of interventions will be used to measure the ability of the community pharmacist to decrease adverse drug events. Results will be used to asses the impact of a community pharmacist on the pharmacotherapy of elderly patients. A patient satisfaction survey will be used to determine the value of the service and an individual’s willingness to pay out of pocket. Results: Data collection will begin in January 2004. Conclusions: It is anticipated that the preliminary data will demonstrate the impact of community pharmacists’ ability to provide a pharmaceutical care home service and potentially a new method for reimbursement. This service is expected to improve elderly satisfaction with pharmacists and decrease the number of adverse drug events an elderly individual may incur. 144—ENHANCING PATIENT SAFETY BY IMPROVING A CQI PROGRAM WITH EDUCATION AND TECHNOLOGY IN A SUPERMARKET CHAIN PHARMACY. Jones K, Goode J, Virginia Commonwealth University, Swiger K, Beckner J, Ukrop’s Super Markets, Inc., Hermann K, Virginia Commonwealth University. E-mail: [email protected] Objective: To observe and assess workflow processes to determine trends, significance, frequency and outcomes on near-miss prescription incidents (incidents caught before reaching patient) and prescription incidents with the current CQI program. To evaluate if an education and reminder program and/or system change with improved dispensing technology will increase pharmacists’ comfort with the current CQI program and decrease near-miss prescription incidents. Methods: This is a prospective, matched control, year-long study conducted in eight super market pharmacies in Richmond, Virginia with an active CQI program. The CQI program includes documentation and analysis of prescription incidents. The pharmacies will be divided into two groups (an active and control group) consisting of four stores each. The initial phase of the study will include a 4hour system analysis conducted by the investigators to assess workflow processes and adherence to the current CQI program. From the system analysis information, a continuous education program and Email reminder system will be developed for all staff. All sites will receive the education component, while only the active sites will receive new technology for the dispensing system. Data will be collected for 6 months and prescription incidents will be compared between stores and with the previous year’s data. Pharmacists’ comfort and confidence with the CQI program will be assessed with a preand postsurvey. Results: Observations have been made in four of the eight stores. The same problem areas were discovered in the workflow process and will be targeted for system change and education. Conclusions: It is anticipated that this project 262 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 will result in improvement of pharmacists’ comfort with the CQI program and additional lowering of near-miss and prescription incidents. 145—EVALUATING THE COST-EFFECTIVENESS OF THE FLORIDA MEDICAID QUALITY-RELATED EVENTS STUDY: A COMMUNITY PHARMACY PERSPECTIVE. Agboh B, Eckerd/Ohio Northern University Community Pharmacy Practice Residency, Sullivan D, Ohio Northern University. E-mail: [email protected] Objective: Recognizing the need for proper counseling among Medicaid patients, the Florida Agency for Health Care Administration has organized a pilot project to encourage pharmacists from all community pharmacies located in certain counties to identify, resolve, and document quality-related events (QREs) and also to provide patient education and follow-up for new prescriptions. Proper documentation will allow pharmacies to be reimbursed $7 for education and follow-up of each new prescription, $10 for each QRE involving patient compliance, and $15 for each QRE requiring physician consultation. The amount of reimbursement for cognitive services has not been adequately evaluated for cost-effectiveness. The primary objective of this study is to determine if it is cost-effective for a community pharmacy to participate in the Florida Medicaid Quality-Related Events program. A secondary objective is to determine if cost-effectiveness changes based on the class of medication. Methods: Ten Eckerd pharmacists actively participating in the Florida Medicaid Quality-Related Events Study will be selected to record the amount of time spent counseling, following up on new prescriptions, documenting and submitting QREs, correcting QRE claims that have been rejected, and time spent on miscellaneous events related to processing claims. A data collection sheet will be designed for documentation of time spent for each activity and the medication involved for each claim. A total of 10–15 QRE claims from each pharmacist will be evaluated for time spent and medication involved. Ancillary and administrative personnel responsible for inputting claims will also record the time spent in completing this task and medication involved. All costs associated with each QRE claim including salary, computer time, etc. will be evaluated. These costs will be compared with the reimbursement fees to determine if participation in Florida Medicaid’s QREs program is cost-effective and to determine if the medication class changes cost-effectiveness. Results: NA. Conclusions: NA. 146—EVALUATION OF AN INCENTIVE PROGRAM ON ADHERENCE RATES IN A COMMUNITY PRACTICE SETTING. Frasco A, Whitaker A, Goode J, Virginia Commonwealth University. E-mail: [email protected] Objective: The purpose of this study will be to evaluate the effect of an incentive program on adherence rates. The study will focus on medica- tions specifically related to the treatment of blood pressure, diabetes, cholesterol, and depression. Methods: We will be conducting reviews of patient medication profiles in a mass-merchandise, community pharmacy setting. An experimental aspect will be introduced in the form of a financial incentive to determine changes in adherence. The study’s primary endpoints will be increased Medication Possession Ratio (MPR) and analysis of on-time refills. Patients will be asked to sign consent forms to participate in the study, after being selected from refill history profiles established by pharmacy reports. These reports are generated periodically by the pharmacy on all prescription department patients. Patients who have a 3-month refill history for medications from our indicated therapeutic categories will be targeted for our incentive program. We will exclude medications with a reminder system built into the packaging. When patients enroll in the study, they will receive a gift card in exchange for permission to review their medication profile. After the study begins, 3-month prospective refill history will be assessed and compared with a 3-month retrospective refill history in order to assess any adherence changes that may have been affected by the incentive program. Patients will be categorized based on class of medication, as defined by computer disease-state codes. This data will be used to subdivide the study population by disease state. With this information, we will calculate the Medication Possession Ratios (MPR). The goal is to assess MPR for the 3 months prior to the receipt of the gift card, and compare it with the MPR for the 3 months after implementation of the incentive. By comparing the MPRs for preand post-gift card receipt, we hope to determine the impact of an incentive on patient adherence. Results: When the study concludes, data will be analyzed by various methods of categorization and comparison statistics. All data will be de-identified, so that only medication name, dose and regimen, therapeutic class, and refill history will remain attached to the records. Conclusions: The adherence reports previously published reveal an alarming trend. It is our hope that an incentive will encourage patients to increase medication adherence. 147—EVALUATION OF EXISTING PATIENT DATA FROM A COMMUNITY PHARMACY-BASED ASTHMA PROGRAM. Ward M, University of Florida/Walgreens, Weitzel K, University of Florida, Brad V, Walgreens, Leslie H, Asmus M, University of Florida. E-mail: [email protected] Objective: The role of the community pharmacist in patient care has evolved beyond traditional medication dispensing to include clinical responsibilities such as disease state management in diabetes, hypertension, dyslipidemia, and asthma. This project will analyze data already being collected through an asthma patient care service in a community pharmacy. The analysis will focus on whether measuring pulmonary function identifies a greater proportion of patients with poor asthma control than symptom analysis alone. www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 148—EVALUATION OF PHARMACIST INTERVENTIONS IN A COMMUNITY PHARMACY–BASED OSTEOPOROSIS SCREENING PROGRAM. Capka M, Happy Harry’s Discount Drugs. E-mail: dragonmount4@ hotmail.com Objective: To determine the outcomes of pharmacist intervention on screened patients at risk for osteoporosis and to determine the percentage of screened patients that are initiated on medications. Methods: Patients at increased risk for hip fracture (defined as any postmenopausal woman satisfying one of the following criteria: age older than 65 years, personal history of fracture, first degree relative with history of fracture, currently smoking, oral corticosteroid treatment lasting longer than 3 months, thyroid medication use, and anticonvulsant use) will be included in the study. Exclusion criteria include those patients already on bisphosphonates, selective estrogen receptor modulators, calcitonin or estrogen therapy as well as those with a history of fractures in both ankles. Patients will be recruited by Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 on-site promotional materials, senior center visits and identification through prescription profiles with a goal of attaining 50 screened patients. These patients will be scanned in a community pharmacy setting using a Lunar Achilles Express bone densitometer. All screened patients will receive educational materials containing general information regarding osteoporosis and its management as well as strategies to help lower the risk of fracture. Those patients who receive a Stiffness Index T-score or Stiffness Index Z-score of < –1.0 will be referred to the primary care physician and for completeness, the physician will be made aware of both the T- and Z-scores via fax. Patients will be followed up via telephone interviews at 1-month and 3-month intervals post screening. Primary endpoints of the study include the percentage of screened patients who are referred to their physician, the percentage of referred patients who see their physician, the percentage of screened patients placed on medication to treat osteoporosis or osteopenia, the percentage of referred patients placed on medication to treat osteoporosis or osteopenia and the percentage of referred patients who have increased their calcium intake or amount of weight-bearing exercises. Results: NA. Conclusions: NA. 149—EVALUATION OF PHARMACY STUDENTS’ ATTITUDES AND INTEREST ON ADMINISTERING ADULT IMMUNIZATIONS AS A HEALTH CARE SERVICE. Akala F, Powers M, University of Toledo. E-mail: [email protected] Objective: To gain a better understanding and determine the attitudes and interest of pharmacy students toward the administration of adult immunizations. The study will also determine how receptive pharmacy students are toward providing this valuable health care service. Methods: A survey questionnaire evaluating the attitudes and interest of students will be conducted during December 2003 to PharmD students at a college of pharmacy. 209 students (n = 105 first professional year and n = 104 second professional year) are expected to participate in the survey. Surveys will be distributed in a classroom setting in which participation is voluntary. The survey consists of questions that either require responses in the form of a 5-point Likert scale (A = strongly agree, E= strongly disagree) or are dichotomous questions that require either a “Yes” or “No” response. The questions are divided into three subcategories (1) perceived barriers to immunization; (2) knowledge and interest; and (3) student demographics. The data collected will be analyzed using SPSS to determine correlations and compare differences and similarities in the interest and attitudes of students in the two classes. Results: Once data collection is complete and analyzed, the results will be used as a tool in designing an immunization-training course to be incorporated in the pharmacy curriculum. Conclusions: Pharmacists are the most accessi- ble health care professionals in the community and because they are so accessible they can provide a range of health services, including immunizations. Since many pharmacy students will become the new practitioners in community pharmacies, it is essential to train and prepare pharmacy students to be competent in providing pharmaceutical care services. To prepare these students, their attitudes and interest in providing these services must be understood. 150—EVALUATION OF THE EFFECTIVENESS OF COMPUTER-GENERATED MEAL PLANNING WITH BEHAVIORAL COUNSELING SESSIONS TO PROMOTE WEIGHT LOSS. Devizia R, Kerr Drug and Campbell University, Greck B, Kerr Drug. E-mail: [email protected] Objective: The primary outcome is to evaluate the change in weight and body mass index among participants. Secondary outcomes will include changes in fasting blood glucose, waist circumference, blood pressure, and cholesterol. Methods: A single-center randomized, quasiexperimental, longitudinal pre–post cohort study conducted in Asheville, NC. DIME (Diabetes Information Management and Evaluation Program) is the computer-generated meal planning program that will be used. During the first visit all baseline measurements will be obtained. These measurements consist of a cholesterol panel using the Cholestech LDX, weight, height, waist circumference, blood pressure using an automated Omron blood pressure monitor, and a fasting blood glucose using the One Touch Ultra glucometer. Each patient will generate a 2-week patient specific meal plan with assistance from a pharmacist. During the initial session, the participants in the intervention group will develop goals to be met throughout the 12week period. Participants in the intervention group will receive training in behavior modification, exercise routine establishment, and meal planning in order to meet these goals. After the initial session, the intervention group will return every 4 weeks for the opportunity to adjust meal plans. Measurements of weight, waist circumference, and blood pressure will be collected at each of these sessions. Cholesterol and fasting blood glucose will be done at the end of the 12-week period. The goals developed in the initial session will be assessed at each 4week session and adjusted as necessary. Long-term weight management assessment will be assessed at 24 weeks. This will be done only if time allows and the 24th week does not fall after July 1, 2004. Results: To be collected, assessed, and presented at the March 2004 APhA meeting and the Southeastern Residency Conference in May 2004. Conclusions: This study should demonstrate the effectiveness of community pharmacists in helping patients set attainable weight loss goals that are safe and effective. 151—EVALUATION OF THE IMPACT OF A CLINICAL PHARMACIST ON FAMILY MEDICINE RESIDENTS’ DRUG KNOWLJournal of the American Pharmacists Association 263 2004 Abstracts of Contributed Papers Methods: Design: Retrospective chart analysis Setting: Four community chain pharmacies in Gainesville, Florida. Patients: Those offered an existing asthma education service. Data Collection: Currently, asthma patients are evaluated by National Heart, Lung, and Blood Institute (NHLBI) Symptom Assessment, spirometry, and NHLBI control classification by symptoms to determine whether their asthma is controlled or uncontrolled. Patients with a ratio < 0.8 for forced expiratory volume in 1 second (FEV1) over forced vital capacity (FVC) predicted demonstrate airway obstruction and are classified as having poor asthma control. Based on symptom assessment and spirometry measurement, patients are classified into four different categories (i.e., mild intermittent, mild persistent, moderate persistent, and severe persistent). A drug therapy assessment is performed on patients who are determined to be uncontrolled upon evaluation. Patients’ primary care providers are contacted by phone and by mail with recommendations for changes in therapy. After 6 months of providing the asthma service, patient charts will be reviewed. Analysis Plan: The primary outcome measures will be asthma control based on symptoms versus symptoms and FEV1 and whether pharmacist contacting physician resulted in change in therapy. Data collection will include: comparison of the number of patients controlled by symptoms versus those controlled by symptoms and FEV1; comparison of mean FEV1 in controlled and noncontrolled patients; and comparison of the number of recommendations for changes to therapy versus the number of those accepted. Other Appropriate Qualitative Measures: NA. Results: Pending. Conclusions: We hypothesize that the use of spirometry in the community setting may increase the number of patients detected with poor asthma control and result in changes to therapy that may improve patient outcomes. FEATURE FEATURE Annual Meeting Abstracts 2004 EDGE BASED ON A NATIONAL STANDARDIZED EXAM. Craft K, Mehra Harris I, University of Minnesota. E-mail: [email protected] Objective: The objective of this study is to evaluate the impact of regular interactions with a clinical pharmacist on family medicine residents’ drug knowledge based on a national standardized exam. Pharmacists are actively involved in 26.7% of family medicine residency programs. The effect of clinical pharmacists’ involvement on a resident’s understanding of drug therapy is unknown. Family medicine residents are required to take a yearly standardized exam, with a passing requirement, in preparation for the board exam. This In-Training Exam, from the American Board of Family Practice, is a general exam encompassing all areas of family medicine, including pharmacotherapy. Methods: The In-Training Exam does not have a separate category for drug-related questions. The exams for the past 3 years will be reviewed to determine which questions are drug related. The performance on the drug-related questions relative to the composite exam score will be compared between groups. Our family medicine residency program, which has pharmacist involvement, will be compared with a control group of residents in two other programs in areas that do not have pharmacist involvement. A separate analysis will compare performance in each of the 3 years of training the resident is in with fellow residents in the programs without a pharmacist. Results: NA. Conclusions: NA. 152—IMPACT ON MEN’S HEALTH: COADMINISTRATION OF A STANDARDIZED SCREENING TOOL AND DIRECT PATIENT CARE SERVICES. Hammond J, American Pharmacy Services Corporation/ University of Kentucky, Mcintosh T, American Pharmacy Services Corporation, Freeman T, APSC Foundation for Education and Research, Inc., Blumenschein K, University of Kentucky. E-mail: [email protected] Objective: To determine if independent community pharmacists can identify men at risk for chronic disease and impact their access to health care, quality of life (QOL), and general satisfaction with pharmacy services using a standardized screening tool in combination with direct patient care services. Methods: Two pharmacy sites will be identified for subject recruitment; a control site and an intervention site. At each site, patients will be recruited and asked to complete an SF-12 to assess QOL and a questionnaire to obtain demographics and information on health care access and patient satisfaction. Recruited patients will be screened using a standardized screening tool—the Men’s Health Risk Assessment Tool (MHRAT) until 25 patients at each site are identified at risk for chronic disease. Intervention-site patients determined to be at risk will be asked to schedule an appointment with the pharmacist within 2 weeks of screening for education and direct patient care services using CLIAwaived testing devices. Intervention patients will be 264 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 encouraged to schedule physician visits based on MHRAT results and objective test results. Controlsite patients identified at risk will be counseled to schedule a physician visit after completing the initial MHRAT screening; they will not receive any additional patient care services or education from the pharmacist. Six weeks postscreening, pharmacists at both sites will call patients to schedule appointments for completion of postintervention surveys and questionnaires. The pharmacists’ interventions will be considered a success if patients identified at risk accessed health care services or scheduled appointments to access care. Results: Pharmacist-intervention success rates between groups will be analyzed using the chisquare statistic; results from the SF-12 and patient questionnaire assessing access-to-care and satisfaction with pharmacy services will be analyzed using appropriate statistical tests. Conclusions: It is anticipated that independent community pharmacists can positively impact men’s access to health care, QOL and satisfaction with pharmacy services by administering MHRAT screenings. It is also anticipated that those pharmacists providing direct patient care services in addition to MHRAT screenings will have a greater impact than those providing screening services alone. 153—IMPLEMENTATION AND EVALUATION OF A SMOKING CESSATION PROGRAM FACILITATED BY COMMUNITY PHARMACISTS. Wilhelm M, Balls Food Stores, Kerner S, Balls Foods. E-mail: [email protected] Objective: The goals of the project are to: (1) assist patients to quit smoking, (2) measure patient success rate, and (3) evaluate patient satisfaction of the program. Methods: The American Lung Association’s Freedom from Smoking program offers a systematic approach to quitting by progressing patients from awareness of the smoking habit to behavioral changes. Two community pharmacists will facilitate the program on a corporate campus. Marketing techniques will include: (1) campus television ads, (2) tabletop cafeteria ads, (3) break area posters, and (4) a counter sign in the campus pharmacy. Patients will enroll in the seven-session program. A survey will be conducted during the last session, at 3 weeks, and 6 weeks after completion of the program. Data from the survey will be evaluated for quitting success rate and patient satisfaction of the program. Results: The study is expected to assist patients in becoming smoke free. Patient acceptance of the program will be determined. Conclusions: The results will provide information to community pharmacists on the success of implementing and evaluating a smoking cessation program. 154—IMPLEMENTATION OF EXPANDED PHARMACIST-PROVIDED CARE IN A FAMILY PRACTICE CLINIC. Bratten S, University of Iowa, Shepley A, Shepley Pharmacy, Currie J, University of Iowa, Brandt K, Mt. Vernon Family Practice, Ernst M, University of Iowa, Farris K, University of Iowa, Jackson A, Clark R, Shepley Pharmacy. E-mail: [email protected] Objective: This paper describes and evaluates the expansion of pharmacist-provided care services in a family practice clinic. Methods: Design: A process and impact evaluation will be conducted after program implementation. This study will take place in a family practice clinic currently utilizing a clinical pharmacist to manage anticoagulation services. Program Development: A community pharmacy initiated discussions with a local family practice clinic to expand the scope and extent of services being offered. After introductory discussions, pharmacy staff members outlined potential services to be delivered. Gaps in clinical services, patient education opportunities and patient groups who could benefit from working with pharmacists were identified. Pharmacists began working with the current clinical pharmacist in the practice to become familiar with clinic procedures. Clinic times and administrative procedures are in development. Program Implementation: Program implementation began September 2003. Evaluation: To describe the processes of the new service(s), data will be collected on number and type of patients seen, types of drug therapy problems identified, recommendations made and accepted, estimates of cost savings for patients by resolved drug therapy problems and time required for service provision. The impact of the service will be evaluated by quantifying revenues generated, the percent of patients with controlled disease states, and patient and physician satisfaction. Results: To be presented. Conclusions: Collected data will be used to describe the program and assess the impact of the enhanced physician–pharmacist relationship in the comprehensive care of patients in a family practice clinic. 155—OUTCOMES OF A DIABETES CARE PROGRAM IN A CHAIN COMMUNITY PHARMACY SETTING. Patel U, University of Maryland, Baltimore, Rodriguez De Bittner M, University of Maryland at Baltimore, Layson-Wolf C, University of Maryland, Baltimore. E-mail: [email protected] Objective: (1) Measure the clinical and humanistic outcomes of a pharmacist-managed diabetes care program in a chain community pharmacy. (2) Assess the economic impact of a diabetes care program for a chain community pharmacy. Methods: This is a retrospective study. Data from the Diabetes Care Program at Giant Pharmacy collected between November 1998 and September 2003 will be evaluated. Participating patients are greater than 18 years of age and have type 1 or type 2 diabetes. All patients included in the study have completed the eight-session diabetes care program. Patients who did not complete all eight sessions will be excluded. The outcomes measured include both clinical and humanistic. Clinical outcomes include hemoglobin A1c, blood pressure, weight, total www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 cholesterol, LDL, and HDL. Outcomes will be measured pre- and postprogram. Humanistic outcomes include patient’s pre- and postprogram quality of life, knowledge, and satisfaction. The quality-of-life survey from the Diabetes Control and Complications Trial was used for this study. Economic impact will be assessed from the income generated and expenses incurred for the program. The income generated from the program includes the fee for services, prescription sales, and sales of monitoring supplies. The pharmacy’s prescription database will be used to assess prescription sales. A survey will be sent to patients who completed the program to determine their use of monitoring supplies. Expenses incurred for the program includes pharmacist’s time, marketing supplies, and other expenses incurred during the sessions. Results: NA. Conclusions: It is anticipated that a pharmacistbased diabetes education program will improve patients’ clinical and humanistic outcomes. The results of this study will confirm or reject this conclusion. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 157—PERFORMNG A PHARMACY CARE SERVICE NEEDS ASSESSMENT IN AN INDEPENDENT COMMUNITY PHARMACY. Cinelli E, Cerulli J, Albany College of Pharmacy. Email: [email protected] Objective: To determine pharmacy care services desired and patients’ willingness to pay out-ofpocket for those services. A secondary objective is to receive feedback from the pharmacy staff on the effectiveness of current marketing strategies. Methods: A self-administered needs assessment was developed to determine pharmacy care services desired. It is being distributed to patients with prescriptions accompanied by a self-addressed, stamped reply envelope. The survey asked patients to identify pharmacy care services that interest them and indicate the fee they would be willing to pay for those services. A separate survey was developed to obtain staff input regarding the effectiveness of current marketing strategies such as usefulness of bag stuffers and the resident and staff roles in recruiting patients to the programs. Results: The needs assessment was piloted in late August. To date, about half of the responders were willing to pay out-of-pocket for some services. The most requested service was a weight loss program. Final numbers of services requested and willingness to pay will be reported. Staff survey responses were received by 9 out of 18 of the employees. Staff suggestions will be used to implement new marketing strategies, including providing pharmacy care service menus in physician’s offices and improving pharmacy signs to attract customers, remind staff and stimulate interest. Conclusions: Patient response to the survey will aid in determining the need for certain services and the patients’ willingness to pay. It is also projected that both surveys will help develop new or improved marketing strategies to expand patient and staff participation in the programs. 158—PHARMACIST MANAGED DIABETES CLINIC: IMPROVING OUTCOMES FOR UNDERPRIVILEGED HISPANIC WOMEN. Gardner J, University of Houston, Adkison J, Memorial Hermann Southwest Hospital, Sansgiry S, University of Houston. E-mail: [email protected] Objective: The incidence of diabetes mellitus (DM) is reaching epidemic proportions in the United States. The growing Hispanic American population is particularly affected, given their high number of risk factors and greater incidence of complications. Delivering health care to a patient with limited resources presents even more of a challenge in treating DM, because of his/her inability to afford medications, lack of transportation to the health care provider, psychosocial factors, etc. Diabetes melli- tus is a complicated disease state that requires active participation from both the health care provider and the patient for optimal control and minimal complications. Clinical pharmacists are in the unique position to assist to this end, by suggesting alternative, more cost-effective medications, providing counseling to patients and families, and assisting with medical and financial issues as needed. The objective of this retrospective study is to examine clinical outcomes in Hispanic women who are patients in a pharmacist-managed indigent DM clinic. These results will be compared with a similar population receiving health care in a clinic not having clinical pharmacy involvement. Methods: Populations will include Hispanic females receiving care at the Memorial Family Practice Fort Bend pharmacist-managed clinic and those who are patients at the Memorial Family Practice Southwest clinic. Health outcomes examined will include glycosylated hemoglobin levels, lipids (LDL, HDL, triglycerides, and total cholesterol) levels and blood pressure readings. In addition, the study will obtain data to compare results at baseline and after pharmacist intervention. Pharmacist interventions include, but are not limited to, medication management, diabetic and dietary education, and medication counseling. In addition, satisfaction with care received at the clinic postintervention will be obtained. Results: Data collection is currently in progress and will be analyzed using SAS. It is anticipated that knowledge provided about the benefit of a pharmacist-managed diabetes clinic on controlling diabetes and improving heath outcomes, especially in Hispanic women, will enhance future interventions. Conclusions: NA. 159—PHARMACIST MANAGEMENT OF DIABETES IN AN ACUTE CARE SETTING USING A BASAL-BOLUS SUBCUTANEOUS INSULIN ORDER SET. Deloria G, Sampsel E, Lum G, Sharp Chula Vista Medical Center, Howard J, Sharp Grossmont Hospital. E-mail: [email protected] Objective: Optimizing glucose control in hospitalized diabetic patients has lead to decreased mortality, decreased postoperative infections, and decreased sternal wound infections. Whether the implementation of a standardized subcutaneous insulin order set (SIOS) will improve patient outcomes compared with conventional sliding scale insulin (SSI) and/or oral antidiabetic agents is unknown. Methods: Sharp Chula Vista Medical Center is a 330-bed, tertiary care, nonteaching community hospital located in San Diego County. Up to 30% of patients admitted have a past medical history significant for diabetes. This standardized SIOS incorporates the use of long-acting insulin glargine (Lantus), as basal insulin, and rapid-acting insulin aspart (NovoLog), as prandial insulin to cover calories from meals via a sliding scale. The pharmacist will adjust insulin doses based upon patient-specific factors and individual needs in the acute care setJournal of the American Pharmacists Association 265 2004 Abstracts of Contributed Papers 156—OUTCOMES OF A PHARMACISTMANAGED TOBACCO-CESSATION PROGRAM IN A PRIVATE, RETAIL PHARMACY CLINIC. Haskins J, Pope N, University of Texas at Austin. E-mail: [email protected] Objective: To measure the effectiveness of a tobacco-cessation program through pharmacist’s intervention in a private clinic. Methods: Setting: The Patient Care Center is a two-room clinic within a Walgreens store in Austin, Texas. Methods: Subjects will be recruited through referrals from health care professionals, advertisements, and patients in other programs conducted at the clinic. Included subjects will be men and women, age 18 years or older, who currently use tobacco products. Pregnant females and those currently enrolled in a tobacco cessation program will be excluded. Informed consent will be obtained from each participant prior to enrollment. Subjects will be enrolled in a 6-week tobacco cessation program with a fee paid on the initial visit. The program module will follow the U.S. Department of Health and Human Services Treating Tobacco Use and Dependence, Clinical Practice Guidelines. At enrollment, the initial 1-hour visit will consist of demographic collection, determining a quit date, education about techniques for quitting, recommendations for OTC cessation product use, and necessity for physician referral. One 30-minute visit will occur on the quit date, and a second 30-minute follow-up visit will occur 1 week after the quit date. Subjects will be contacted by phone weekly for the remainder of the program. Outcomes of intervention will be collected by phone after the end of the program every 2 weeks for 3 months. Data collection will consist of changes from baseline demographics, length of cessation, and assessment of successful intervention techniques in this setting. Results: To be determined. Conclusions: The role of community pharmacist intervention in tobacco cessation in this unique setting will provide a model for community pharmacists in the future. Outcomes of this study will provide information to determine successful intervention techniques, lower health care costs, and improve quality of life. FEATURE FEATURE Annual Meeting Abstracts 2004 ting. We are performing a prospective, open-label pilot study of patients admitted to the telemetry unit and placed on the SIOS pursuant to a physician order. Our goal blood glucose range is 90–180 mg/day. The control group will be randomized diabetic patients on the same unit who fit the same inclusion criteria, but did not receive the SIOS. Measured patient outcomes will include rates of infection, glucose control during hospitalization, and patient length of stay. Patient outcomes between the two groups will then be assessed and evaluated throughout hospital course until discharge. Results: We anticipate that optimizing glucose control through the implementation of a pharmacistmanaged SIOS will reduce the rates of infection during hospitalization, decrease patient length of stay, and improve glycemic control. Conclusions: NA. 160—PHARMACISTS’ PERCEPTIONS AND CONCERNS ABOUT BECOMING IMMUNIZATION PROVIDERS AND ISSUES AFFECTING PATIENTS’ ACCEPTANCE OF COMMUNITY PHARMACIST PROVIDERS. Johnson P, Barnett C, Mercer University. E-mail: [email protected] Objective: (1) To identify factors that pharmacists believe are barriers to provision of immunizations. (2) To measure the willingness of pharmacists to provide immunization services. (3) To measure pharmacists’ perceptions of factors for patients that present barriers to seeking immunization services. (4) To determine the factors that patients’ indicate affect their willingness to seek immunization services. Methods: Two groups of Kroger pharmacists will be selected. One group will consist of 200 pharmacists who have received training in immunization and another group of 200 will consist of pharmacists who have not received training. Kroger will provide a list of pharmacists in the Atlanta area who have and have not received training. A random sample of 200 names will be selected from each list. The research design is a mail survey questionnaire. Both groups of pharmacists will be sent the same survey. The questionnaire will not be coded, so results will be anonymous. A replacement questionnaire will be sent to all the pharmacists after 2 weeks requesting that they complete the survey if they have not already done so. A list of Kroger pharmacies in the Atlanta area that do not participate in immunization services will be obtained. A random sample of 10 pharmacies will be selected. The subjects are adult patrons of Kroger pharmacies where immunizations are not provided. The research design of this aspect of the study is an on-site questionnaire. A group of items on this questionnaire are the same as a group of items on the pharmacist questionnaire so that comparisons between the pharmacists and patients can be made. The principal investigator will provide each of these pharmacies with 50 questionnaires via a personal visit to the pharmacy. The pharmacists working at these pharmacies will be asked to give a survey with cover letter to adult patients waiting for prescriptions to be filled. The survey questionnaires 266 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 will not be coded. A box will be provided for the patients to drop their completed surveys into. This will further ensure anonymity. Project Timeline: October 2003, selection of pharmacists (subjects) for pharmacist survey; selection of pharmacies for distribution of patient survey. November 1, 2003, mail pharmacist survey; deliver patient surveys to pharmacies. Nov 14, 2003, mail replacement pharmacist survey. December 2003–February 2004, data analysis. March 2004–May 2004, write-up results. Results: NA. Conclusions: NA. 161—PHARMACY EXPERIENCES AND PERCEPTIONS OF NEWLY ENROLLED PHARMACY STUDENTS. Huh J, Sorensen T, University of Minnesota. E-mail: [email protected] Objective: In newly enrolled pharmacy students: (1) identify the degree and type of pre-enrollment pharmacy experience; (2) analyze the impact of previous experience on perceptions of the role of pharmacists in health care. Methods: First-year pharmacy students at three Midwestern colleges of pharmacy were surveyed regarding previous pharmacy-related work experience. Surveys were distributed during school orientation or early in the first semester of enrollment. The survey instrument evaluated work experience and its relation to whether this was completed prior to choosing to pursue pharmacy as a career or after applying to schools. It also addressed the type of setting in which pharmacy-related experience was gained, observations of the type of work completed by pharmacists, and the perceptions of pharmacists’ responsibilities to medication dispensing and overall patient care. Results: Approximately 250 first-year pharmacy students received the survey in fall 2003. Data analysis will include assessment of whether previous experience and/or the setting of this experience affect perceptions of the role of pharmacists. Conclusions: When a profession is in the midst of changing its professional role, applicants to its schools may be basing their decision on observations of a role somewhat inconsistent with the profession’s desired future. It is prudent to determine the message the profession is sending potential pharmacy school applicants to ensure that those entering the profession are prepared to accept the expanding role of pharmacists in the health care system. 162—PHYSICIANS’ PERCEPTIONS OF PHARMACISTS AS VACCINATORS. Welch A, Ferreri S, Caiola S, University of North Carolina at Chapel Hill. E-mail: [email protected] Objective: The objectives are to assess the awareness and support of physicians regarding pharmacists as vaccinators. This study also identifies the physicians’ common reasons for lack of support. Methods: A mail survey will be sent to the family practice physicians in North Carolina. Physician offices will be identified by the State Medical Board’s Web site using the physician locator function. Target areas will be the 255 towns and cities in the state with a local government. The survey will include a letter describing the intent of the study and return postage. The survey identifies how long the physician has been in practice, if vaccines are currently administered in their practice, and if the physician works closely with a pharmacist. A series of questions will be asked to assess physicians’ perceptions of pharmacists as vaccinators using a Likert scale. A follow-up letter will be sent in 3weeks if no response. Results will be assessed using descriptive statistics. Results: Results are pending. Conclusions: The intent of the study is to provide pharmacists with a tool to use when approaching physicians on administering vaccines. With state regulations changing to favor pharmacists as vaccinators, the results may serve useful in marketing vaccination services. 163—PROMOTING COLORECTAL CANCER AWARENESS AND SCREENING IN A RURAL COMMUNITY PHARMACY PRACTICE SETTING. Dolin D, Rite Aid Pharmacy, Meredith B, West Virginia University, Jacknowitz A, West Virginia University. E-mail: danipharmd@ aol.com Objective: This project will attempt to (1) increase colorectal cancer awareness and prevention through a community pharmacy-based education and screening program, (2) provide average and high-risk individuals with fecal occult blood tests (FOBT) for home use upon counseling and education by a pharmacist, (3) encourage colorectal screenings at appropriate intervals and foster communication between the patient and health care provider regarding colorectal cancer, and (4) determine if screening and education promote positive lifestyle modifications. Methods: Study participation will be offered to all pharmacy patrons and interested persons in the community. Colorectal cancer literature will be available in the pharmacy with pharmacists trained to answer patient inquiries. Participants will be individually educated in the pharmacy’s private counseling area regarding colorectal cancer, risk factors, and options for screening. FOBT will be distributed to average risk and high-risk individuals for home use upon providing instruction to the participant. Participants will contact the pharmacist with their results, and a brief questionnaire will be completed to determine whether colorectal cancer education and screening have influenced their health attitudes and practices. Providers will be notified of the test results and follow-up evaluated. Results: The objectives of this program will be evaluated for effectiveness by determining the number of participants who (1) receive literature on colorectal cancer, (2) rank as average and high risk according to American Cancer Society guidelines, receive FOBT through this initiative, (3) provide the results of their FOBT to the pharmacist, and followup with their health care provider for appropriate care/intervention, as well as (4) whether participants have improved their health practices and attitudes as a result of colorectal cancer education and screening. Conclusions: It is anticipated that knowledge of www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 colorectal cancer and its prevention will be increased with many patients receiving FOBT screening and education. Participants will establish appropriate screening habits, although continued education and reinforcement may be needed for enhancement of health attitudes and beliefs to occur. 165—REDUCING SENIORS’ DRUG EXPENDITURES THROUGH MEDICATION REGIMEN REVIEW AND REVISION IN A COMMUNITY PHARMACY. Owen J, Fry’s Pharmacy/University of Arizona, Herrier R, University of Arizona, Spencer J, Fry’s Pharmacy. E-mail: [email protected] Objective: To provide seniors with an economically viable alternative to purchasing medications outside the United States by reducing out-of-pocket expenditures through eliminating unnecessary drug therapy, switching to generic or the cheapest brand Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 166—RETROSPECTIVE ASSESSMENT OF LONG-TERM OUTCOMES IN A COMMUNITY-BASED PHARMACEUTICAL CARE PROGRAM. Leighty J, Eckerd Corporation, Sullivan D, Ohio Northern University. E-mail: [email protected] Objective: The role of a pharmacist is changing dramatically from dispenser of prescription drugs to a provider of patient care and medication management. Over the last few years, the value of pharmaceutical care has been evaluated in hospital, medical clinics, and community pharmacy settings. However, much of the research demonstrating the value of pharmaceutical care programs has been limited to short-term outcomes. One of the few projects that have evaluated long-term outcomes of pharmaceutical care was the Asheville Project. Unfortunately, there was a significant drop-out rate for its patients over the course of 3 years, which made the evaluation of long-term outcomes somewhat difficult. This leads us to the question of whether pharmaceutical care programs sustain positive patient outcomes over longer periods of time. The objective of this study is to assess the long-term outcomes of a community-based pharmaceutical care program for patients with diabetes, hypertension, and dyslipidemia. Methods: Patient charts will be randomly select- ed from all persons that have been enrolled in the Eckerd PatientCARE network for the last 3 years in the Tampa area. A total of 50 cases for each of the three disease states will be assessed for adherence to the nationally recognized clinical guidelines. Due to the overlap of some disease states within patients, the total number of patients evaluated will be between 80 and 120. For hypertension, the variables assessed will include the percentage of goal blood pressures, and proper choice of recommended medication. For diabetes, the variables assessed will include hemoglobin A1c, body mass index, and the ability to reach recommended goals. Preprandial and postprandial blood glucose values will also be included for those patients for whom the data is available. For dyslipidemia, the variables assessed will include triglycerides, total cholesterol, HDL, LDL, and the ability to reach recommended goals. Results: NA. Conclusions: NA. 167—RETROSPECTIVE COST–BENEFIT ANALYSIS OF A WELLNESS CENTER FROM AN INDEPENDENT COMMUNITY PHARMACY PERSPECTIVE. Kent K, McDonough R, Doucette W, University of Iowa, Ploehn L, Main at Locust Pharmacy Clinic. E-mail: [email protected] Objective: Main at Locust Pharmacy Clinic developed and implemented a wellness center that provides health risk assessments and health screenings to interested patients. The purpose of the wellness center is to provide an advanced level of patient care as well as provide an additional revenue source for the practice. The objectives of this study are to (1) determine the revenues and costs associated with the delivery of the wellness center services, and (2) perform a cost–benefit analysis of the wellness center. Methods: Design: Retrospective review of the clinic’s wellness center records over a 2-year period. Setting: An independent community pharmacy wellness center. Data collection: Wellness center records for nine different services (blood pressure, blood glucose [BG], bone density, body fat, hemoglobin A1c, ALT, total cholesterol [TC]/HDL, TC/BG, full lipid panel) will be analyzed beginning October 1, 2001 thru September 30, 2003. Revenues will be determined by reviewing cash register receipts for that period. Direct and indirect costs associated with the delivery of the services will include the staff’s time involved with each service, equipment and supply costs, advertising, and the overhead costs associated with the practice. Data Analysis: Frequencies of each service will be tabulated. Revenues and costs will be determined for each service and discounted to October 2001 levels. A cost–benefit and sensitivity analysis will be performed. Sensitivity analyses will vary personnel costs and service volume. Results: Preliminary analysis of Main at Locust Pharmacy Clinic records demonstrates that more than 1,000 patient interactions have used the wellness center during the defined 2-year period. Journal of the American Pharmacists Association 267 2004 Abstracts of Contributed Papers 164—PROVISION OF WEIGHT MANAGEMENT SERVICES BY A PHARMACIST IN A GROCERY STORE COMMUNITY PHARMACY. Hussein S, Briggs A, Dominick’s Pharmacy/Midwestern University, Zgarrick D, Midwestern University. E-mail: [email protected] Objective: The primary objective of the weight management program is for patients to safely lose weight, maintain lower body weight, and reduce risk of obesity-related disorders. The secondary objective is to assess patients’ satisfaction with the program, pharmacist, and pharmacy; likelihood of returning for other clinical services and prescription needs; and income generated from the program. Methods: Inclusion criteria: Men and women between the ages of 18 and 64 with a body mass index (BMI) of 25 to 34.9 kg/m2. Exclusion criteria: Pregnancy, lactation, psychiatric illness, bulimia, anorexia nervosa, substance abuse, cancer, severe gastrointestinal disease, renal or hepatic dysfunction, and recent start of a thyroid hormone. A medical release form authorizing the start of the program and physical activity regimen will be obtained from the physician. The program will involve an initial, individualized consultation with counseling on a low calorie diet, physical activity, and behavior therapy and the development of a practical treatment plan for each patient. At follow-up group meetings, the treatment strategy will be evaluated and modified. NIH guidelines will be followed when considering and recommending pharmacotherapy. Outcome measures: Weight, BMI, waist circumference, blood pressure, fasting and/or 2hour postprandial blood glucose, and lipid profile. In addition, patients will be surveyed concerning secondary objective variables 3 months from the commencement of the program. Results: Intention to treat analysis and paired t test will be used to compare baseline with last visit values and determine if a statistically significant improvement in outcome measures occurred. Descriptive analysis will be performed for the results of the satisfaction survey. Conclusions: NA. medications when possible, and using manufacturer and store discount plans. Methods: The medication regimen review will be piloted at a pharmacy located within an hour of the Mexican border. Patients will be targeted via instore and newspaper advertising. Additionally, patients who might benefit from this service will be identified using the pharmacy computer system. Targeted patients will include those who are paying cash for their prescriptions, members of Medicare HMOs, or using discount cards. The clinical recommendations to alter the therapeutic regimen will be based on published drug literature and the relative cost of alternative medications. The suggestions for change will be presented to the patient’s primary care doctor for approval and/or modification. Data will be collected and analyzed for loss in prescription sales revenue, changes in patient purchases in other parts of the store, changes in patient expenditures for medications including those medications obtained from outside the United States, physician acceptance rates, types of changes made, pharmacy expenses to perform the service, changes in disease control, and patient satisfaction. A fee schedule for services provided will be determined based on the evaluation of collected data. Results: The effectiveness of the medication regimen review will be assessed by evaluating profitability, patient health status, and patient satisfaction. Conclusions: It is expected that the medication review will maintain or improve disease control, reduce patient out-of-pocket expenses, and provide a viable alternative to purchasing medications outside the United States. FEATURE FEATURE Annual Meeting Abstracts 2004 Conclusions: The wellness center has generated new revenue for the clinic. A cost–benefit analysis will determine the profitability and sustainability of the service. 168—SUCCESS RATE OF A PHARMACIST-MANAGED SMOKING CESSATION PROGRAM IN A COMMUNITY PHARMACY SETTING. Free H, Rodriguez De Bittner M, Layson-Wolf C, University of Maryland at Baltimore, Fairfax, CVS Pharmacy. E-mail: [email protected] Objective: To assess the effectiveness of a pharmacist-managed smoking cessation program, in a community pharmacy setting, on patients’ ability to remain smoke free after quitting, and assess patients’ knowledge about the consequences of smoking and its treatment. Methods: The study design is a single-center, prospective, pilot study. Phase I involves training pharmacists to serve as the smoking cessation facilitators. The pharmacists will be trained using the American Lung Association, “Freedom from Smoking” program. Procedures will be developed that define the roles and responsibilities of the facilitators using the tobacco dependence guidelines. Phase II will involve the implementation of the smoking cessation program. The program will begin with three individualized (patient and pharmacist) appointments followed by three group sessions and a 3-month group follow-up. Throughout the program, patients will be educated on smoking consequences, how to incorporate behavior modifications, and how to prevent relapse. Pharmacotherapy may also be used. At every session, monitoring parameters will be assessed, including blood pressure, pulse, weight, adverse drug reactions, and carbon monoxide levels. Written education materials will be supplied at every session. Results: Analysis of the pre- and postknowledge tests will be conducted. Quality of life at baseline and completion of the program will be measured. A Kaplan Meier survival curve will be used comparing the percent abstinence and relapse at weeks 1, 4, and 12 and will be compared with other published studies. In addition, patient satisfaction surveys will be reported. Conclusions: It is anticipated that a pharmacistmanaged smoking cessation program in a community pharmacy setting will be successful in helping patients quit and maintaining smoking abstinence. 169—TARGET INTERVENTION PROGRAM TO PROMOTE CALCIUM SUPPLEMENT USE IN COMMUNITY PHARMACY. Cinelli E, Cerulli J, Albany College of Pharmacy. Email: [email protected] Objective: To determine if a Target Intervention Program (TIP) developed for community pharmacy can increase appropriate calcium supplement intake in patients receiving prescription osteoporosis therapy. A secondary objective is to determine baseline calcium supplement use in this population. Methods: Eligible patients will be identified by pharmacists and/or PharmD candidates based on a 268 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 prescription (new or refill) for a medication to treat and/or prevent osteoporosis at six Community Pharmacy Advanced Practice Experience sites that include chain and independent settings. All eligible patients identified will be documented on an enrollment log. An assessment tool will be used by the students to determine baseline supplement use either in person or via telephone. Students will determine if patients presently on a calcium supplement are receiving the appropriate dose and/or are using the correct administration technique and will intervene as needed. A recommendation for an appropriate calcium supplement will be made to the patient and their physician if patients are not currently receiving a calcium supplement. Two months following any intervention, students will perform a follow-up phone call to patients to determine if the recommendations were accepted. Results: The percent of patients taking a calcium supplement with their prescription at baseline will be reported. The impact of the intervention will be determined by the number of recommendations made to add calcium supplementation or improve administration/dose. The number of patients who purchased a calcium supplement following the intervention and the number of patients reporting use on follow-up will be documented. Conclusions: Assuming baseline calcium supplementation is low, a recommendation by a pharmacist or pharmacy student is anticipated to increase calcium supplement intake in patients receiving osteoporosis medications. 170—THE EVALUATION OF JNC VII ADHERENCE IN AN INTERDISCIPLINARY OUTPATIENT SETTING. Wylie K, Green C, Medow M, Ohio State University. E-mail: [email protected] Objective: (1) Evaluate percentage of patients at target blood pressure according to the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) guidelines, (2) determine areas in need of intervention, and (3) develop a patient assessment form to address deficits. Methods: Research will be conducted retrospectively at an interdisciplinary primary care clinic. Patients will be identified via ICD-9 codes signifying a hypertension diagnosis (401.X). Exclusion criteria include pregnancy, less than 18 years of age, and/or primarily managed by nephrologists. The primary end point is the percentage of patients achieving their blood pressure goal according to JNC VII guidelines. Secondary end points include assessment of drug selection, risk factors, comorbidities, and interventions. Individual charts will be pulled onsite and reviewed since the initiation of JNC VII (on May 14, 2003) using a self-created data collection sheet. The data collected will identify the patient’s goal, if the patient has met his/her goal, risk factors for major cardiovascular disease, relevant family history, comorbidities, and receipt of appropriate follow-up, laboratory tests, medications, and interventions. Upon completion of each chart review, a patient assessment sheet will be added to each chart as a reminder to health care providers of monitoring parameters. Results: Once data collection is complete, the percentage of clinically diagnosed hypertensive patients at goal and not at goal will be documented and reported. For those not at goal, the following will be taken into consideration and reported: treatment, follow-up, interventions, assessment of risk factors, and comorbidities. Conclusions: We anticipate that these results will accurately identify the percentage of patients at their target blood pressure and identify areas in need of intervention. The results will provide feedback to team members to determine whether we need to reengineer workflow to optimize hypertension management. 171—THE EVALUATION OF PHARMACISTS’ ATTITUDES TOWARDS PROVIDING SMOKING CESSATION COUNSELING IN A CHAIN PHARMACY SETTING. Hendrickson J, Jackson T, University of Illinois at Chicago. E-mail: [email protected] Objective: The U.S. Public Health Service has published guidelines for treating tobacco use. A goal of these guidelines is to change practice patterns of health care professionals in identifying and offering treatment to tobacco users. While numerous smoking cessation programs exist, barriers prevent pharmacists from implementing them. The primary objective of this study is to objectively evaluate pharmacists’ knowledge and attitudes regarding smoking cessation counseling. Additionally, the frequency of identifications and interventions made will be evaluated. Methods: Pharmacists in the Chicago metropolitan area will be invited to attend a smoking cessation training program. The program will be developed using medical literature and U.S. Public Health Service guidelines. Pharmacists will be trained to identify smokers visiting the pharmacy and to apply the transtheoretical model to individually tailor counseling based upon information about a patient’s smoking behavior. Pharmacists will provide brief counseling on health consequences of smoking, behavioral strategies in quitting, and the use of nicotine replacement therapy. Investigators will assess pharmacists’ perceived knowledge and attitudes regarding the provision of smoking cessation counseling using an 11-item retrospective pretest/posttest administered 12 weeks after the training program. Additionally, program effectiveness and the number of smoking cessation interventions by pharmacists will be evaluated. Results: Responses to the assessment instrument will measure pharmacists’ knowledge and attitudes towards providing smoking cessation counseling. These data will be analyzed using the Rasch rating scale model. Conclusions: It is expected that pharmacists participating in this program will gain skills and confidence in counseling patients on smoking cessation. It is predicted that attitudes toward providing smoking cessation interventions will improve, and the frequency of the interventions will increase accordingly. www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 173—THE IMPACT OF PHARMACIST CONSULTATION FOR LIFESTYLE MODIFICATION IN PREHYPERTENSIVE SUBJECTS IN A COMMUNITY PHARMACY. Patthanacharoenphon D, Dominick’s Pharmacy/University of Illinois at Chicago, Sommers Hanson J, Dominick’s Pharmacy, Jackson T, University of Illinois at Chicago. E-mail: [email protected] Objective: This pilot study will assess the impact of monthly educational visits of subjects identified by community pharmacists as prehypertensive according to the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) . Subjects will be encouraged by the pharmacist to Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 make lifestyle modifications such as weight loss, weight maintenance and increased activity in order to decrease their blood pressure to normal as defined by JNC VII. Methods: Subjects will be selected from a convenience sample through both in-pharmacy and community blood pressure (BP) screenings. Subjects will be eligible if two BP readings on two separate occasions are in the range of 120–139/80–89 mm Hg. Subjects will be excluded if they are less than 18 years old, are taking antihypertensive medications, or have been diagnosed as hypertensive according to JNC VII. Subjects will receive monthly pharmacist counseling on lifestyle modification and written educational information on hypertension and lifestyle modification to supplement the pharmacists education. Monitoring will occur over a 12-week period. Monthly consultations will include BP measurement, weight measurement and lifestyle assessment. Dependent variables included in analysis will be BP, weight and selfreported activity level. Independent variables included will be race, age, gender, and pre-existing conditions. The dependent Student t test will be used to compare group means for continuous variables. Rasch analysis will be used to measure attitudinal components of a retrospective pretest/posttest survey. Results: The designation of a new category of prehypertension is an opportunity to expand the role of the pharmacist in the prevention of hypertension. It is anticipated that patients receiving pharmacist consultation for lifestyle modifications will experience a reduction in blood pressure by the end of the 12-week study. Conclusions: NA. 174—THE NORTH CAROLINA MEDICAID POLYPHARMACY INITIATIVE. Smith K, Mission St. Joseph’s Hospital–Asheville, NC, Bunting B, Mission St. Joseph’s/City of Asheville. E-mail: [email protected] Objective: Access II Care provides case management services for North Carolina Medicaid recipients with chronic illnesses through participating primary care offices. The Prescription Advantage List (PAL) is a statewide formulary for preferred medications that are considered the most cost-effective for Medicaid patients. The major goal of the study was to determine the initial cost-savings with the implementation of medication recommendations from the PAL list at a participating primary care setting. Methods: A retrospective chart review was performed for patients who were prescribed more than eight prescriptions a month, received North Carolina Medicaid, participated in the Access II Care program, and had a primary care physician (PCP) at the Buncombe County Health Center. Medication records were reviewed to determine the most appropriate and cost-effective medications from the PAL list. These written medication recommendations were communicated with the PCP and implemented with their approval. Results: Among the 37 charts reviewed, 57 recommendations were made to change drug therapy. Thirty-five of the 57 recommendations (61%) were accepted, 19 of the 57 recommendations (34%) were denied, and there was no response on 3 of the recommendations (5%) made. One physician refused to participate in the initiative and denied all of the recommendations made concerning his/her patients. These denials accounted for 75% of the total denied recommendations. The 35 accepted recommendations accounted for an estimated cost-savings of $800 per month and $10,000 per year. Assuming that 90% of the recommendations were accepted, cost-savings estimations increased to $1,200 per month and $14,000 per year. Conclusions: Implementation of a polypharmacy initiative that incorporated drug therapy review by a pharmacist improved appropriate prescribing of cost-effective medications for Medicaid patients in a primary care setting. Original Citation: Presented at the Southeastern Residency Conference, Athens, GA, May 2, 2003. 175—THE USE OF PATIENT-CONTROLLED ANALGESIA WITH OR WITHOUT BASAL INFUSION FOR POSTORTHOPEDIC SURGERY PAIN MANAGEMENT. Phan T, Luong K, Lum G, Sharp Chula Vista Medical Center, Elington M, Sharp Memorial Hospital–Security Trailer. E-mail: [email protected] Objective: Patient-controlled analgesia (PCA) has become a widely used method of pain relief following major orthopedic surgery. PCA is effective because it allows the patient control of their pain management by self-administering doses depending on their level of pain. Adding a basal infusion to PCA is believed to sustain the level of drug in the body, thereby maintaining constant analgesia. However, patients who are on PCA with basal infusion are reported to experience more sedation and are less able to ambulate postoperatively than their counterparts, resulting in slower recovery and increased length of stay. Methods: This is a comparison study looking at recovery in patients who are on morphine PCA with or without basal infusion status postorthopedic surgery. It is a 3-month observational study of patients who are admitted to the medicine/orthopedic floor following orthopedic surgery such as joint replacement or fracture. Patients are excluded if they have nonorthopedic surgery or are on analgesia other than morphine PCA. Data are collected from documentation charted by anesthesiologists, nurses, physical therapists, and pharmacists. We are evaluating levels of sedation, ambulation, respiratory function, pain, nausea/vomiting, incidence of deep vein thrombosis, and length of stay. Results: Based on prior anecdotal observation, we expect to see patients who are on morphine PCA without basal infusion be less sedated, ambulate earlier, have less nausea/vomiting and have a shorter length of stay. Additionally, we may find less respiratory depression and fewer episodes of DVT. We Journal of the American Pharmacists Association 269 2004 Abstracts of Contributed Papers 172—THE IMPACT OF COMMUNITY PHARMACISTS’ INTERVENTION ON PATIENTS’ LIPID PROFILES, KNOWLEDGE OF DISEASE STATE, AND QUALITY OF LIFE. Taylor C, Divine H, University of Kentucky. E-mail: [email protected] Objective: To determine the impact on patients’ cholesterol levels after being educated by a community pharmacist about their lipid profiles and disease state compared with patients not receiving a 12week education program from the pharmacist. The secondary objective is to improve patients’ quality of life and satisfaction with the services offered at the pharmacy. Methods: 100 patients taking medication for hyperlipidemia will be randomly assigned to one of two groups. The control group will not receive any special education sessions with the pharmacist. The intervention group will receive biweekly educational sessions with the pharmacist. At the beginning of the study, all 100 patients will have their fasting lipid profile measured by the pharmacist using a point-of-care device at the pharmacy. In addition, each patient will be asked to fill out three surveys; the SF 12 for quality of life, a quiz to measure knowledge of cholesterol, and a patient satisfaction with pharmacy services survey. For 12 weeks, the intervention group will receive biweekly educational sessions with a pharmacist. There will be a number of topics covered in each of the six sessions including evaluating each person’s risk of a coronary event in the next 10 years, dietary improvements, and lifestyle modifications. The patient’s information will be documented using Pfizer’s Lipid Goal Manager. With this program, the patient can see visually through graphs the impact small changes can have on their future. At the conclusion of the project, each of the 100 patients will be brought back in to the pharmacy to have their lipid profiles tested again. Each patient will also receive the three surveys to take again. Results: Data such as lipid profiles, quality-oflife survey, knowledge survey, and patient satisfaction survey will be analyzed for statistically significant differences between the control and intervention groups. Conclusions: NA. FEATURE FEATURE Annual Meeting Abstracts 2004 anticipate no significant difference in pain control. Conclusions: NA. 176—THERAPEUTIC SUBSTITUTION WITH GENERIC LISINOPRIL: EVALUATION OF COST SAVINGS AND CLINICAL OUTCOMES FROM THE COMMUNITY PHARMACY SETTING. Vinti A, Caiola S, Coker H, Futrell D, Futrell W, University of North Carolina at Chapel Hill, Gouveia-Pisano J, Pfizer, Inc., Jones M, McDowell J, University of North Carolina at Chapel Hill. E-mail: [email protected] Objective: (1) Identify medical providers’ willingness to accept a therapeutic substitution recommendation as suggested by a community pharmacist. (2) Maintain blood pressure (for all patients) and kidney function (for diabetic patients) after therapeutic substitution of a brand name ACE inhibitor with generic lisinopril. (3) Maintain JNC VII blood pressure goals for those patients who are at goal prior to the intervention. (4) Achieve JNC VII blood pressure goals for those patients who are not at goal prior to the intervention. (5) Record outof-pocket costs incurred by the patient and health care system. (6) Discuss reimbursement for a community pharmacist’s pharmaceutical care services. Methods: This study enrolled adult male and female patients with a diagnosis of hypertension who had no change in antihypertensive medication regimen (agents or dosages) for the last 4 weeks, which included therapy with a brand name ACE inhibitor. Patients were identified through a drug utilization review of all patient medication profiles at two community pharmacies. Potential subjects were contacted via telephone to inform them briefly of the project and to request an initial screening. All subjects were assessed for demographics, current medications (prescription, over-the-counter, and herbal), past medical and surgical histories, and medication compliance with the Morisky Scale. Upon informed consent, dose conversion from the patient’s brand name ACE inhibitor to generic lisinopril was conducted by the pharmacist, and recommended to the patient’s medical provider by telephone or fax. Upon approval from the medical provider, the recommended dose of lisinopril was taken as a call-in prescription and dispensed. At dispensation, patients had their blood pressure checked, received counseling on their new medication and scheduled 12 follow-up appointments. Follow-up visits at the pharmacy occurred every 7 days and included assessment of compliance, adverse events, and measurement of blood pressure. Those subjects who had a documented medical history significant for diabetes mellitus with microalbuminuria or proteinuria were asked to give urine samples for assessment of urine microalbumin/creatinine ratio. Results: NA. Conclusions: NA. 177—THROUGH A SELF-ASSESSMENT SURVEY, AT WHAT POINT OF SEVERITY OF SYMPTOMS, DOES AN ASTHMA PATIENT SEEK MEDICAL CARE? Heaton R, 270 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Moose J, Caiola S, Brock T, Spencer S, University of North Carolina at Chapel Hill. E-mail: [email protected] Objective: The objective of this research survey is to qualify and quantify how patients perceive their symptoms and when they should seek medical attention. The objective at the conclusion of this survey is to educate asthma patients on how to manage their asthma, including when seeking health care is appropriate. Methods: A letter of intent, a retrospective survey and consent form will be mailed to 128 patients. The patients were selected through a drug recall report off of the database at Moose pharmacies’ computers. The drug recall selected patients that were prescribed and filled steroid inhalers and albuterol inhalers for the months of June, July, and August. The survey is to be filled out by participating patients and mailed back to Moose Pharmacies. A follow-up survey, letter of intent and consent form will be mailed to the same 128 patients if there is no response. A stamped envelope will be included in the package for the patient to return the survey and signed consent form. Children under the age of 18, pregnant women, and patients with other respiratory diseases will not be included. Results: Pending. Conclusions: Pending. 178—UNDERSTANDING OVER-THECOUNTER DRUG USE AND MISUSE IN HIVINFECTED PATIENTS. Ngo C, Sansgiry S, University of Houston College of Pharmacy. Email: [email protected] Objective: This pilot study was designed to understand the involvement of HIV-infected patients in self-medication practices that may lead to drug misuse in order to optimize future drug therapy. Drug misuse is defined as self-reported experiences of excessive or inadequate use of over-thecounter (OTC) products as well as nonrecommended uses of the product with other medications. The advent of new drugs in treating HIV infection has decreased disease progression and imposed new challenges for health care providers. The significance of this study is to evaluate and understand OTC drug use and misuse in HIV-positive patients. Methods: A cross-sectional study will be conducted to understand self-medication practices that may lead to drug misuse in HIV-infected patients. A sample of approximately 120 patients will be selected randomly from a local HIV-care clinic in Houston, Texas. Patients between 18–55 years of age who are HIV positive will be considered as potential participants. Information on OTC drug use and misuse along with demographics will be obtained by using a combination of self-administered questionnaire and personal interview. A previously validated questionnaire will be administered by a trained and qualified data collection assistant with clinical knowledge on OTC drug use and misuse in HIV-infected patients. Data will be analyzed using descriptive and comparative analysis, including t test and Spearman correlation, to determine the extent of OTC drug use and misuse in HIV-infected patients. Results: NA. Conclusions: The study is currently in progress and will help researchers gain further understanding of the factors that should to be considered in optimizing self-medication practices for HIV-infected patients in order to optimize future drug therapy. Drug misuse may lead to adverse drug events and eventually affect health-related quality of life of patients. 179—WEIGHT MANAGEMENT IN A PHARMACIST-RUN CLINIC: PATIENT SATISFACTION AND OUTCOMES. Michalcik L, Randolph R, Marcrom R, University of Tennessee. E-mail: [email protected] Objective: The objective of this study is to evaluate patient satisfaction with a pharmacist-run weight management program and the effects the program has on patient’s weight loss. Patients will complete a survey at the end of the study to determine their satisfaction with the program. Methods: Subjects will be recruited through posters, bag stuffers, and an informational radio program. Subjects who meet inclusion criteria will be chosen on a volunteer basis. The subject population will consist of approximately 20 volunteers with a body mass index greater than 25 kg/m2 who are interested in improving their health through diet and exercise. Exclusion criteria will include patients who are currently taking weight loss medications, who are taking medications that commonly lead to weight gain, who do not have a health care provider, whose condition prevents them from performing moderate exercise, who are pregnant or lactating, who are less than the age of 21, who have uncontrolled psychiatric illness, who have active substance abuse, or who have a history of anorexia nervosa or bulimia nervosa. At the initial visit, a thorough medication review will be performed to determine these criteria. Motivation to lose weight will also be determined at this visit via a motivation questionnaire adapted from the NIH Practical Guidelines, A Brief Behavioral Assessment. Weight, body mass index, waist circumference, and blood pressure will be measured. The weight loss program being offered follows national guidelines provided by the National Heart, Lung, and Blood Institute and the American Dietetic Association. Emphasis on gradual weight loss through calorie reduction and increased exercise will be taught in seven educational follow-up sessions. Discussion topics will include: adding exercise, components of food, eating triggers, dining at restaurants, fiber, vitamins, minerals, getting the most from exercising, and maintaining weight loss. At the end of the program, the patient will be asked to complete a questionnaire to see if their weight loss goals and expectations of the program were met. Patients will be asked specifically what parts of the program with which they were pleased or displeased, and point values will be assigned to different levels of satisfaction. Data will be evaluated to determine the success of the program based on point values. Results: Weight loss of 5% to 7% is expected by the 14th week. Conclusions: NA. www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 APhA–APRS Basic Sciences 181—EVALUATION OF ACACIA AND SEMISYNTHETIC POLYMERS AS AN EMULSIFYING AGENT. Carp E, Wilkes University–Nesbitt School of Pharmacy, Lee C, Kibbe A, Wilkes University. E-mail: [email protected] Objective: To find a substitute for acacia in emulsions. Preliminary experiments were undertaken, and the decision to compare acacia, semisynthetic polymers, and semisynthetic polymers and a surfactant was made. Methods: The test samples were prepared on the same day using various methods to ensure quality emulsions. Physical appearance and viscosity was tested from day 0 (baseline) to day 29. There were three samples of each emulsion at different temperVol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 APhA–APRS Clinical Sciences 182—EXAMINATION OF MEDICATION ERRORS OCCURRING IN THE PATIENT’S HOME REPORTED TO USP’S MEDICATION ERROR REPORTING PROGRAMS. Camp S, United States Pharmacopeia. E-mail: [email protected] Objective: To examine reports submitted to USP’s medication error reporting programs, in which the error occurred in the patient’s home. Understanding the characteristics of these medication errors can contribute to the development of strategies to improve the safe use of medications. From these data, we hope to identify safe practices that health care professionals and consumers can use to prevent these errors from occurring in the patient’s home. Methods: Reports submitted to the USP MEDMARX and the USP/ISMP Medication Errors Reporting Programs, where the location of the error is in the patient’s home, are identified. Data are summarized using Microsoft Access and Excel to present information about the severity, type(s), cause(s), contributing factor(s), and product(s) associated with these errors. Information about where in the medication use process the errors initiated (node) and the level(s) of staff involved in the errors is also displayed. Finally, a review of action(s) taken in response to the errors is summarized. Results: The findings from this study will be used by USP’s Safe Medication Use Expert Committee to develop practice recommendations for health care professionals and/or safe medication use recommendations for consumers. Conclusions: NA. 183—A NEW ORAL OPIOID, OXYMORPHONE EXTENDED RELEASE, DOES NOT AFFECT HUMAN METABOLIC ENZYMES CYP 2C9 AND CYP 3A4. Adams M, SFBC New Drug Services, Inc., Ahdieh H, Gammaitoni A, Endo Pharmaceuticals, Inc., Pieniaszek H, HPP Consulting & Services, Inc. E-mail: livinginpa135@ yahoo.com Objective: To investigate the clinical significance of in vitro data linking suprapharmacologic concentrations of oxymorphone (> 3,000 times therapeutic levels) with induction of the human cytochrome P450 drug metabolizing enzymes CYP 2C9 and CYP 3A4. Methods: Two single-center, randomized, openlabel, parallel-group studies compared the effects of high and low dosages of oxymorphone extended release (ER) on the metabolism of substrates of CYP 2CP and CYP 3A4. On days –1, 7, and 14, healthy adults received 1 dose of either a CYP 2C9 probe (tolbutamide 500 mg, study 1) or CYP 3A4 probes (midazolam and intravenous [14CH3 Nmethyl]-erythromycin for the erythromycin breath test [ERMBT], study 2). Five groups were randomized to 14 days of treatment with either (a) highdose oxymorphone ER (3 × 20 mg every 12 hours) plus naltrexone (50 mg every 24 hours to minimize opioid effects); (b) low-dose oxymorphone ER (10–20 mg every 12 hours); (c) rifampin (2 × 300 mg every 24 hours) to induce CYP 2C9 and CYP 3A4 activities; (d) naltrexone (50 mg every 24 hours); or (e) CYP probes alone (controls). All treatments except erythromycin were oral. Tolbutamide AUC, midazolam AUC, and change from baseline in expired 14CO2 were determined on days –1, 7, and 14. Results: In the oxymorphone ER and naltrexone groups, changes from baseline to days 7 and 14 in tolbutamide and midazolam AUCs and the percentage of expired 14CO2 per hour in the ERMBT were not significantly different from the untreated control values. The positive control rifampin significantly decreased tolbutamide and midazolam AUCs and increased the percentage of 14CO2 expired per hour on days 7 and 14. Conclusions: Oxymorphone ER did not affect the metabolism of CYP 2C9 or CYP 3A4 substrates, indicating that it has a low potential for altering the plasma levels of other drugs metabolized via these enzymes. This may result in fewer dosage adjustments in patients taking oxymorphone with other drugs metabolized by CYP 2C9 or CYP 3A4. 184—SINGLE- AND MULTIPLE-DOSE PHARMACOKINETIC AND DOSE-PROPORTIONALITY STUDY OF OXYMORPHONE IMMEDIATE-RELEASE TABLETS. Adams M, SFBC New Drug Services, Inc., Ahdieh H, Endo Pharmaceuticals, Inc. E-mail: [email protected] Objective: To investigate the pharmacokinetics and dose proportionality of oxymorphone immediate release (IR) and its metabolites (6-OH-oxymorphone and oxymorphone-3-glucuronide) following single- and multiple-dose administration. Methods: A randomized, three-way crossover study of oxymorphone IR (5, 10, and 20 mg) was performed in 24 healthy adults (18–45 years). Subjects received all three dosage levels of oxymorphone IR. A single dose of 5, 10 or 20 mg was administered on day 1; beginning on day 3, subjects received the same dose every 6 hours through the morning of day 8 (22 total doses). Treatment periods were separated by a 7-day washout. Naltrexone hydrochloride was administered to prevent opioidrelated adverse events. Blood was collected up to 48 hours after day 1 to determine single-dose pharmacokinetics and up to 6 hours after the day-8 dose for steady-state data. Results: Twenty-three subjects (12 men; 11 women) completed the study. Following single Journal of the American Pharmacists Association 271 2004 Abstracts of Contributed Papers 180—A QUICK AND SIMPLE HPLC METHOD FOR THE DETERMINATION OF CRYPTOLEPINE IN A COMMERCIAL SAMPLE OF CRYPTOLEPIS SANGUINOLENTA HERB TEA. Ononiwu I, Howard University, Fakorede F, Walter Reed Army Institute of Research, Kumar K, Howard University, Iwu M, Bioresources Development and Conservation Programme. E-mail: [email protected] Objective: Cryptolepine is the antimalarial, antidiabetic, and cytotoxic substance in Cryptolepis sanguinolenta, a herb that is commercially available in alternative medical practice for the treatment of malaria and diabetes. As part of an ongoing program to develop methods for the standardization of herbal remedies with proven efficacy and safety, using chemical markers identified in the plant materials, a simple, quick, sensitive and robust high-performance liquid chromatographic method with simultaneous photodiode array and fluorescence detection for the identification and determination of cryptolepine has been developed. Methods: Isocratic elution was carried out using Waters 2690D separation module with a reversephase Zobrax SB C18 5 mm (4.6 × 250 mm) column. The mobile phase consisted of acetonitrile and 10 mM potassium phosphate buffer in the ratio 30:70 at pH 3 and 35°C. Detection was with a Waters photodiode array detector (PDA996) at a wavelength of 366 nm and 474 fluorescence detector at 366 excitation and 673 emission wavelengths, respectively. Data analyses was performed using Waters Empower software. Results: The average retention time for cryptolepine was found to be 2.8 minutes. Calibration curves for cryptolepine were linear with correlation coefficients (r2) of > .999. Limits of detection and quantitation were, respectively, 4.5 and 10 ng/mL. The method was applied in the determination of cryptolepine in different batches of commercial herb tea samples of Cryptolepis sanguinolenta used in the treatment of malaria in Ghana. Conclusions: This selective and sensitive method can be used for high-throughput determination of cryptolepine in commercial and /or medicinal herbal preparations containing this indoloquinoline alkaloid. atures (32° C, 22° C, and 4° C). Results: In the pivotal experiment there were differences between the acacia emulsions and the semisynthetic emulsions. The semisynthetic polymers appeared to be more stable over time in their viscosity. Conclusions: Only the methylcellulose semisynthetic polymer made an acceptable, easy to use, and stable emulsion. FEATURE FEATURE Annual Meeting Abstracts 2004 doses of 5, 10, or 20 mg, the oxymorphone IR mean AUC (4.5, 9.1, and 20.1 ng•h/mL, respectively) and Cmax (1.1, 1.9, and 4.4 ng/mL, respectively) confirmed dose proportionality. Metabolites levels also increased in a linear fashion. Steady-state dosing data also showed proportional increases in the AUC and Cmax of oxymorphone and its metabolites. Adverse events generally were mild, and no clinically relevant changes in laboratory or other safety variables were noted. For all doses of oxymorphone IR, the single dose and steady state Tmax was 0.5 hours. The terminal half-life of oxymorphone IR was measured at 7.25 to 9.43 hours. Conclusions: For oxymorphone IR tablets, the single-dose and steady-state pharmacokinetic profiles of oxymorphone and its metabolites were linear and dose proportional across the dosage range from 5 mg to 20 mg. The short Tmax predicts a rapid onset of analgesia. Original Citation: American Pain Society Annual Meeting; March 18–23, 2003; Chicago, Ill. Poster Presentation. 185—BIOASSAY FOR DIRECT ANTIMICROBIAL ACTIVITY OF LANSOPRAZOLE AGAINST VAGINAL LACTOBACILLI. Rue K, UHS-COM, MSIV, Herndon B, Dempsey D, University of Missouri–Kansas City, Marinac J, The University of Health Sciences, Mathews T, Williams C, University of Health Sciences. E-mail: [email protected] Objective: Determine the antimicrobial effect of lansoprazole on vaginal Lactobacillus. Background: Fourteen days of 30 mg lansoprazole reversibly increases vaginal pH and significantly reduces vaginal lactobacilli in healthy women. No data exists on antimicrobial effects of lansoprazole on vaginal lactobacilli. Methods: Lactobacillus was obtained from vaginal swabs of eight healthy female volunteers. Lactobacilli were inoculated onto an MRS agar plate surface and stored in sterile sleeves at 4°C. Lansoprazole 20 microliters was added to 6.3 mm sterile discs on the culture plate mimicking average human serum concentrations (765 ng/mL) following chronic oral administration. Three additional tests were also run on the specimens: lansoprazole dissolved in sterile water (control); lansoprazole dissolved in a series of low pH buffers (to determine influence of surrounding pH on antimicrobial activity); and lansoprazole at 10× and 100× average therapeutic serum concentrations. Cultures were anaerobically incubated for 30 hours at 37°C. Antimicrobial activity was evaluated by measuring the diameter of the clear area (lactobacillus kill) around the drug discs. Results: Minimal killing of lactobacilli was demonstrated at both the 10× (7.65 mcg/mL) and 100× (765 mcg/mL) therapeutic lansoprazole concentrations. However, no vaginal lactobacilli were killed by the typical human serum concentrations of lansoprazole, the control solution, or the pH manipulation studies. Conclusions: Data suggest lansoprazole exhibits a small direct bactericidal effect on vaginal lactobacilli at high serum concentrations, but this is not 272 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 likely to be of clinical importance because it only occurs well outside the typical therapeutic range. Based upon these in vitro findings, the reduction in vaginal lactobacilli following lansoprazole administration we previously reported is not a result of direct antimicrobial activity of the drug. Further studies are underway to determine the causal relationship. 186—CLINICAL EXPERIENCE WITH A PHARMACIST-COMPOUNDED NALTREXONE IMPLANTABLE PELLET IN OPIOID ADDICTS. Baker J, Barr W, Virginia Commonwealth University, Coleman P, Coleman Institute. E-mail: [email protected] Objective: The development of naltrexone (NTX) for the treatment of opioid addiction (OA) has been financially supported by the National Institute on Drug Abuse (NIDA) for over three decades. In 1984 FDA approved oral NTX for OA in only highly motivated patients because clinical trials proved compliance to be a significant drawback. Since realizing the limitation of oral NTX, NIDA has been supporting the development of sustained-release (SR) forms of NTX. Still waiting for FDA approval of SR forms of NTX, clinicians have turned to pharmacist-compounded preparations. This report describes 3-, 6- and 9-month follow-ups on patients who have received at least one compounded NXT implant, which has a duration of effect of about 6 weeks. There are no similar reports available in the literature. Methods: The Coleman Institute in Richmond, VA is an OA treatment center providing detoxification and long-term treatment. Follow-up consultations at 3-, 6-, and 9-month with patients who have received at least one NTX implant at the Coleman Institute between March 2003 and September 2003 will be retrospectively reviewed. We will review opioid use, if patients are in behavioral therapy, and pellet complications. Also of interest is the incidence of pain problems that would normally require narcotic treatment and how these problems were treated. Last, we will review items that would relate to a patient’s quality of life, such as depression, arrests, and employment/student status. Baseline and follow-up characteristics will be compared. This study has been approved by Virginia Commonwealth University Health System’s institutional review board. Results: This retrospective review will describe the results obtained for all the study variables described above for up to 9 months after NTX implantation. Important to the possible increase in the future use of implants, this report will document complications that may arise in a nonresearch/clinical setting. A primary concern with implantable NTX therapy is how to deal with acute pain requiring narcotics. This descriptive review will detail the frequency of these circumstances and how they were resolved. Conclusions: The hypothesis to be tested is that the majority of patients using the NTX implant will remain abstinent from opioid use and will be employed or seeking education at each of their follow-ups. A description of pellet complications and treating emergent pain while a virtually nonremovable narcotic antagonist is in place will be detailed. Supported in part by T32-DA07027. 187—COMPARISON OF ANTICOAGULATION PARAMETERS BETWEEN PATIENTS SEEN AT A PHARMACIST-MANAGED CLINIC AND ROUTINE MEDICAL CARE. Conner C, Pfizer, Inc., Pauly D, Dean Medical Center. E-mail: [email protected] Objective: The primary objective of this analysis was to compare INR goal attainment among patients seen in a pharmacist-managed (PM) and a physician-managed or routine medical care (RMC) setting. Methods: Patients included in the RMC or physician-managed clinic (East clinic) were identified using CPT codes for INR laboratory tests. To be identified for inclusion, patients had to have at least two INR values documented. After identification of a list of all eligible patients, based on more than two INR determinations, one of the investigators manually screened each patient chart to ensure that the INRs corresponded to a valid indication for longterm anticoagulation therapy. Patients in the PM clinic were identified by a screening of anticoagulation clinic records. INR lab data were extracted for all included patients. These lab data included all documented INR lab results from January 1, 2002 through December 31, 2002. Valid indications for anticoagulation and target INR ranges were derived from the Chest guidelines. One of the studies’ primary investigators scanned a listing of unique patient ICD-9 codes and translated these into INR target ranges using the Chest guidelines. Results: An initial harvesting of the database yielded 969 patients for the analysis. Preliminary results will be presented. Conclusions: Though published evidence mounts on the topic of whether pharmacists operating an anticoagulation clinic perform as well as or better than primary care physicians, there remains some doubt in the minds of some health care decision makers as to the real-world effectiveness of these clinics. Published analyses comparing pharmacist-managed clinics to physician-managed clinics may exhibit characteristics that cause decision makers to feel that published results fail to generalize to their specific patient populations. Consequently, there is a need to conduct these outcomes analyses locally, so that conclusions can be drawn with regard to quality of care produced at these clinics within an individual health care system. This analysis represents such an endeavor. 188—COMPARISON OF SEXUAL FUNCTIONING IN PATIENTS RECEIVING DULOXETINE OR PAROXETINE: ACUTEAND LONG-TERM DATA. Gonzales J, Eli Lilly and Company, Brannan S, Cyberonics, Detke M, Mallinckrodt C, Tran P, Eli Lilly and Company, Delgado P, Case Western Reserve University. Email: [email protected] Objective: Evaluate sexual functioning following acute- and long-term treatment with duloxetine, www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 189—DULOXETINE FOR THE TREATMENT OF MAJOR DEPRESSIVE DISORDER: SAFETY AND EFFICACY ASSOCIATED WITH RAPID DOSE ESCALATION (60–120 MG QD). Gonzales J, Wohlreich M, Mallinckrodt C, Watkin J, Prakash A, Eli Lilly and Company. Email: [email protected] Objective: Duloxetine, a dual reuptake inhibitor of serotonin/norepinephrine (5-HT/NE), has demonstrated efficacy for the treatment of emotional and painful physical symptoms of major depressive disorder (MDD) in double-blind, placebo-controlled trials at 60 mg QD. While the expected starting and therapeutic dose is 60 mg QD, we further investigated duloxetine’s pharmacologic profile by examining its safety and tolerability during dose escalation from 60 mg QD to 120 mg QD. Methods: Patients with MDD (N = 128), blinded to timing of dose escalations, received placebo for 1 week followed by duloxetine (60 mg QD) titrated after 1 week to 90 mg QD and after a further week to 4 weeks of 120 mg QD. Efficacy measures included 17-item Hamilton Rating Scale for Depression (HAMD17) total score, Clinical Global Impression of Severity (CGI-S) scale, Patient Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 Global Impression of Improvement (PGI-I) scale, and Visual Analog Scales (VAS) for pain. Safety was assessed using spontaneously reported treatment-emergent adverse events, changes in vital signs, and laboratory analytes. Results: Significant improvements were observed in all efficacy measures at end point (P < .001). The rate of discontinuation due to adverse events (16.3%) was comparable to rates observed in previous placebo-controlled trials. The most frequently reported treatment-emergent adverse events (TEAEs) were nausea, headache, dry mouth, dizziness, and decreased appetite. The majority of TEAEs were associated with initial duloxetine dosing—escalations in dose produced few additional TEAEs. Mean changes from baseline to end point in supine systolic and diastolic blood pressure were 1.2 and 0.6 mmHg, respectively, with no reports of sustained hypertension. Mean change in heart rate was 1.7 bpm, while mean changes in QTcB and QTcF were 1.8 and –5.4 msec, respectively. Conclusions: These results establish the safety and tolerability of duloxetine at once-daily doses above 60 mg, and demonstrate that rapid dose escalation can be achieved without incurring additional adverse events. Original Citation: European College of Neuropsychopharmacology, Prague, Czech Republic, September 2003. 190—EFFECT OF LANSOPRAZOLE ON IL-6 IN HEALTHY WOMEN. Rue K, UHSCOM, MSIV, Marinac J, The University of Health Sciences, Mathews T, University of Health Sciences, Herndon B, University of Missouri–Kansas City, Williams C, Sun C, University of Health Sciences. E-mail: [email protected] Objective: Determine the effect of 14 days of lansoprazole 30 mg (Prevacid) on serum interleukin-6 (IL-6) concentrations in healthy women. Background: Lansoprazole, a commonly prescribed proton pump inhibitor (PPI), has been shown to modulate the inflammatory response. Previous work has shown that PPIs possess antiinflammatory activity. PPIs may attenuate the oxidative burst of neutrophils (PMNs), downregulate the expression of adherence molecules on both PMNs and endothelial cells, as well as decrease circulating monocyte concentrations. Because lansoprazole modulates the inflammatory response, we hypothesized its usage may produce effects in IL-6, a cytokine that reflects inflammation. An increase in circulating IL-6 is indicative of an acute systemic inflammatory response. The effect of long-term lansoprazole administration on circulating plasma IL-6 concentrations is unknown. Methods: Twenty-one healthy, premenopausal women (mean age 30.6 years) were enrolled. Women taking hormones, those with acute infection, diabetes, or immunosuppressed conditions or who were taking confounding immune-modulating medications were excluded. Blood samples were obtained at baseline (V1) after 7 (V2) and 14 (V3) days of lansoprazole, and at washout (V4), 14 days after lansoprazole was discontinued. Human IL-6 concentrations were determined using ELISA. Data are reported as mean (± SD) pg/mL. Results: A significant depression of IL-6 concentrations was found at V4 as compared with V1: 2.2 (2.6) versus 1.6 (1.9); P = .02. IL-6 concentrations were similar at V1, V2, and V3: 2.2 (2.6), 2.3 (1.9) and 2.9 (3.6) pg/mL, respectively. Conclusions: Following discontinuation of drug given to healthy women for 14 days, IL-6 concentrations were significantly lower than before drug therapy. However, administration of lansoprazole results in no acute change in IL-6 concentrations. This finding suggests a delayed reduction in one marker of inflammation. Further work is needed to determine the causal relationship and clinical importance of this finding. 191—EFFECT OF LANSOPRAZOLE ON PMN ACTIVITY AND CHEMOKINES IN HEALTHY WOMEN. Rue K, UHS-COM, MSIV, Marinac J, The University of Health Sciences, Mathews T, University of Health Sciences, Herndon B, University of Missouri–Kansas City, Williams C, Sun C, University of Health Sciences. E-mail: [email protected] Objective: Determine the effect of 14 days lansoprazole 30 mg on serum interleukin-8 (IL-8) concentrations, PMN chemotaxis, and PMN superoxide production in healthy women. Background: Lansoprazole is well known to modulate extracellular and intracellular acid in gastric mucosa. Neutrophils (PMNs) use similar ionic processes. Lansoprazole binds within PMN lysosomes, attenuating free radical production from activated PMNs. We hypothesized lansoprazole may also act indirectly by attenuating chemokines activating PMNs. IL-8 serum concentrations were measured in subjects’ whose PMNs were isolated and evaluated. Methods: Twenty-one healthy, premenopausal women (mean age 30.6 years) were enrolled. Women taking hormones, with acute infection, taking confounding medications, diabetics, and otherwise immune suppressed were excluded. Blood samples were obtained at baseline (V1), after 7 (V2) and 14 (V3) days of lansoprazole, and at washout (V4), 14 days after lansoprazole discontinuation. Human IL-8 ELISA was performed on the serum while PMN chemotaxis to fMLP and sod-cyto c assays were performed on PMNs isolated from the subjects’ blood. Data are reported as mean (± SD) pg/mL. Results: A significant increase in IL-8 concentrations was demonstrated at V4 as compared with both V1 and V3: V1 13.7 (11.0), V4 17.9 (24.4) P = .04; V3 15.0 (12.3), V4 17.9 (24.4) P =.04. However, no significant change in IL-8, chemotaxis to fMLP, nor superoxide production was demonstrated by subject PMNs while taking lansoprazole. V1, V2, and V3 IL-8 concentrations were similar: 13.7 (11.0), 21.1 (22.2), 15.0 (12.3) pg/mL respectively. Conclusions: Upon discontinuation of lansopraJournal of the American Pharmacists Association 273 2004 Abstracts of Contributed Papers paroxetine or placebo. Methods: Acute-phase data obtained from four 8-week, double-blind studies, with patients randomized to duloxetine (20–60 mg BID; N = 736), paroxetine (20 mg QD; N = 359), or placebo (N = 371). Long-term data obtained from extension phases, in which acute treatment responders received duloxetine (40 or 60 mg BID; N = 297), paroxetine (20 mg QD; N = 140), or placebo (N = 129) for 26 additional weeks. Sexual function evaluated using the Arizona Sexual Experience Scale (ASEX). Results: In patients without initial sexual dysfunction, the probability of acute phase sexual dysfunction onset was significantly lower for duloxetine-treated patients compared with those receiving paroxetine (P = .015), although both rates were significantly higher than placebo (P = .007 and P < .001, respectively). Long-term data revealed that sexual function improved (ASEX total score reduced) in 70.9% of duloxetine-treated patients between baseline and end point, compared with 57.6% for paroxetine (P = .060). For ASEX questions 1 and 2, a significantly greater proportion of duloxetine-treated patients reported improvement compared with paroxetine (P = .050 and P = .037, respectively). No significant differences were found in Questions 3, 4, or 5. Conclusions: In these studies, the incidence of acute phase sexual dysfunction development among patients receiving duloxetine across its dose range (40–120 mg/day) was significantly lower than that of paroxetine at the low end of its dose range (20 mg/day). On certain ASEX questions, a significantly higher percentage of duloxetine-treated patients reported improvement in sexual functioning compared with paroxetine. Original Citation: American Psychological Association, May 2003. FEATURE FEATURE Annual Meeting Abstracts 2004 zole given to healthy women for 14 days, IL-8 concentrations were significantly higher than before or during drug therapy. However, subjects’ PMNs showed no attenuation of free radical production nor a decrease in chemotaxis to fMLP. This is the first study to relate chemokines to PMN activity in subjects treated with a proton-pump inhibitor. Further work is needed to determine the causal relationship and clinical importance of these findings. 192—EXAMINATION OF A SERVICELEARNING–BASED PHARMACEUTICAL CARE PROGRAM DELIVERED BY THE PHARMACEUTICAL ACCESS PROJECT OF THE NESBITT SCHOOL OF PHARMACY. McManus M, Nesbitt School of Pharmacy and Nursing–Wilkes University, Graham B, Nesbitt School of Pharmacy and Nursing–Wilkes University. E-mail: [email protected] Objective: Examination of the impact of pharmacy student involvement on the delivery of pharmaceutical care to indigent and underserved patient populations and reflection on the impact of the service learning experience on the student’s perception of the professional role of the pharmacist. Methods: Data has been collected from three independent, free health care clinics. Each clinic has a distinct patient population and mission. Clinic data collection includes identification of the number of pharmaceutical care interventions by the students, patient diagnosis, tracking of the total number and type of medications prescribed. A student survey has been designed to assess student perception of the professional roles of pharmacists both before and after the service-learning experience. Final analysis of the data will be accomplished using SPSS. Results: Pharmaceutical care (as measured by number of direct patient contacts and medication dispensed) for indigent patients has steadily increased. The patient diagnoses that appear to have the most improved access are associated with asthma, hypertension and diabetes. Student perceptions of the professional role of the pharmacist demonstrated an increased appreciation for the skills and expertise the pharmacist brings to the health care team. Conclusions: The Pharmaceutical Access Project has evolved into a premier service-learning outreach program and research opportunity for the Nesbitt School of Pharmacy. It has rapidly grown over the past 3 years, from four free clinics to six. The program provides pharmaceutical services and medications (with the school of pharmacy acting as a restricted formulary warehouse) to the local indigent rural community. All of the services are provided by the students and faculty of the School of Pharmacy. Over the past 3 years, 40 students have had the unique experience of active involvement in ambulatory-based, collaborative efforts to improve health care delivery to the homeless and undeserved. The almost universal response of the students to the service-learning experience is one of compassion, increased confidence in professional skills, enhanced pride in the practice of pharmacy, 274 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 and increased delivery of pharmaceutical care to the underserved individuals of the area. 193—INCIDENCE AND MANAGEMENT OF ANTIDEPRESSANT-INDUCED NAUSEA: EXPERIENCE WITH DULOXETINE. Gonzales J, Eli Lilly and Company, Greist J, Healthcare Technology Systems, Mallinckrodt C, Rayamajhi J, Eli Lilly and Company, Raskin J, Eli Lilly Canada. E-mail: [email protected] Objective: Gastrointestinal disturbances, particularly nausea, are the most frequently reported adverse events for many antidepressants. Consequently, management of nausea is important for patient adherence. We investigated the incidence of nausea in patients with major depressive disorder (MDD) who were treated with the new antidepressant duloxetine, a potent dual reuptake inhibitor of serotonin and norepinephrine. Methods: Data were from eight double-blind, randomized, placebo- and active comparator-controlled trials of patients with MDD. The treatment arms were: placebo (N = 777), duloxetine 40 mg/day (N = 177), duloxetine 60 mg/day (N = 251), duloxetine 80 mg/day (N = 363), duloxetine 120 mg/day (N = 348), paroxetine 20 mg/day (N = 359), and fluoxetine 20 mg/day (N = 70). Results: In acute (8–9 week) placebo-controlled trials of duloxetine (40–120 mg/day), treatmentemergent nausea was reported by 19.9% of duloxetine-treated patients and 6.9% of patients receiving placebo (P < .001). Onset of duloxetine-induced nausea occurred primarily within the first 2 days of treatment with a median duration of 7 days. The incidence of nausea did not differ from placebo rates after 1 week. In paroxetine-controlled and fluoxetine-controlled studies, the incidence of treatmentemergent nausea in patients receiving duloxetine did not differ significantly from paroxetine (14.1% versus 12.0%) or fluoxetine (17.1% versus 15.7%). Most duloxetine-treated patients reported nausea to be mild (52.9%) or moderate (41.4%) in intensity. Treatment discontinuation secondary to nausea occurred in 1.4% of duloxetine-treated patients and 0.1% of patients receiving placebo. The incidence of treatment-emergent nausea during 6-month continuation of duloxetine treatment (80 mg/day: 2.1%; 120 mg/day: 1.3%) was similar to placebo (1.6%). Conclusions: These data indicate the new antidepressant duloxetine induces mild-to-moderate nausea in a subset of patients during treatment initiation. Nausea resolved rapidly with continued treatment. The incidence of duloxetine-induced nausea resembled that produced by the SSRIs paroxetine and fluoxetine. Duloxetine-induced nausea should have little impact on patient satisfaction and adherence. 194—LEVEL OF DEPRESSIVE SYMPTOMS AMONG PATIENTS WITH A PRIOR HISTORY OF DEPRESSION TREATED WITH VERAPAMIL SR-LED VERSUS ATENOLOL-LED TREATMENT STRATEGIES. Ried L, University of Florida/Department of Veterans Affairs, Tueth M, Department of Veterans Affairs, Handberg E, Pepine C, University of Florida. E-mail: [email protected] Objective: INVEST demonstrated equivalence for clinical outcomes between a verapamil SR (Ve)led strategy and an atenolol (At)-led strategy in 17,131 U.S. patients with hypertension and coronary artery disease. The study objective was to compare depressive symptoms between strategies among those with a previous diagnosis of depression. Methods: A subset of consecutively randomized INVEST patients living in the United States (N =2,317) were enrolled between April 1, and October 31, 1999. Patients were mailed a survey within 24 hours of randomization and 1 year later. The surveys contained a depression (CES-D) scale and questions about self-reported prior diagnosis of depression. Nearly 50.2% of patients returned both the randomization and follow-up surveys. Results: Among patients with a prior diagnosis of depression, the difference in CES-D scores between the At-led and Ve-led strategies after 1 year was 1.85 points (22.03 versus 20.18, t = 1.01, P = .31). Among patients without a prior diagnosis of depression, the difference was 1.43 points (12.12 versus 10.69, t =2.29, P = .02). The baseline CES-D scores were similar when the two treatment groups were compared. Baseline (23.5 versus 12.0, P < .001) and follow-up (21.0 versus 11.4, P < .001) depressive symptoms were significantly higher among those with a prior diagnosis of depression (N = 201) when compared with those without a prior diagnosis of depression (N = 951). Patients with a prior diagnosis of depression improved by 2.5 points after 1 year (t = 3.45, P = .001), whereas those without a prior history of depression improved by 0.6 points (t = 2.33, P = .02). Conclusions: Prior history of depression is consistently one of the most significant predictors of future depression. In INVEST, the treatment choice effected patients’ depressive symptoms similarly whether or not they had a prior diagnosis of depression, although the verapamil SR strategy had less mood-related impact than the atenolol strategy. 195—LIPID MANAGEMENT AND FACTORS AFFECTING GOAL ATTAINMENT IN LATIN AMERICA. Alemao E, Merck and Co., Meaney E, Cardiovascular Unit Head, ISSSTE Regional Hospital 1º de octubre, Armaganijan D, Chief of Caronariopaty Medical Session, Dante Pazzanese Institute of Cardiology, Ramos A, Innoval, S.A. de C.V, Yin D, Merck and Co. E-mail: [email protected] Objective: Despite proven value of cholesterol reduction in coronary heart disease (CHD) prevention, many studies in Europe and the United States suggest that majority of patients receiving treatment do not achieve the efficacy needed for CHD prevention. The objective of this study was to evaluate treatment of hyperlipidemia patients in Mexico and Brazil and determine factors associated with attaining goals as defined in the Third Report of the Adult Treatment Panel of the National Cholesterol Education Program (ATP-III) in CHD/CHD-equivwww.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 196—NOVEL, EPIDURAL, SUSTAINEDRELEASE MORPHINE PROVIDES 48-HOUR POSTOPERATIVE PAIN RELIEF. Viscusi E, Thomas Jefferson University, Martin G, Duke University Medical Center, Hartrick C, William Beaumont Hospital, Singla N, Huntington Memorial Hospital, Manvelian G, SkyePharma, Inc. E-mail: [email protected] Objective: Rationale: Epidural morphine provides good postoperative analgesia, but requires use of an indwelling catheter for pain relief beyond 24 hours. Obviating the need for an indwelling catheter with a single dose of sustained-release morphine could eliminate complications associated with indwelling epidural catheters, especially in patients receiving anticoagulants. Objective: To evaluate DepoMorphine, a novel, single-dose, sustainedVol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 release formulation of epidural morphine, in providing pain relief for 48 hours postoperatively. Methods: Adults (N = 194) undergoing total hip arthroplasty were randomized to receive an epidural injection of placebo (normal saline) or DepoMorphine 15, 20, or 25 mg for postoperative pain management. All patients had access to IV fentanyl via a PCA pump for breakthrough pain relief as needed. Postoperative fentanyl consumption through 48 hours was the primary efficacy end point. Pain intensity and pain relief were also assessed. Results: DepoMorphine reduced mean (± SD) fentanyl use versus placebo (510 ± 708 mcg versus 2,091 ± 1,803 mcg; P < .0001) and delayed median time to first rescue with fentanyl (21.3 hours versus 3.6 hours; P < .0001). DepoMorphine patients had lower mean (± SD) pain intensity scores with activity as measured by the VAS (0–100 mm) at 24 and 48 hours (30 ± 28 versus 52 ± 29 and 29 ± 28 versus 39 ± 27; P < .001 and P = .06). DepoMorphine patients were also more likely to rate pain relief as “good” or “very good” (90% versus 65%; P < .05). More DepoMorphine-treated patients did not require postoperative fentanyl at 12 (57% versus 2%; P < .001) and 48 hours (25% versus 2%; P = .001). The incidence of adverse events was similar across treatment groups except for a higher incidence of vomiting and pruritus (P < .05) with DepoMorphine. Respiratory depression occurred in 5 (4%) of DepoMorphine patients and no placebo patients (NS). Conclusions: Single-dose DepoMorphine provided postoperative pain relief for 48 hours, while avoiding complications associated with indwelling epidural catheters. 197—ONSET OF IMPROVEMENT IN EMOTIONAL AND PAINFUL PHYSICAL SYMPTOMS OF DEPRESSION WITH DULOXETINE TREATMENT. Gonzales J, Wohlreich M, Eli Lilly and Company, Brannan S, Cyberonics, Mallinckrodt C, Detke M, Lu Y, Watkin J, Tollefson G, Eli Lilly and Company. Email: [email protected] Objective: Duloxetine, a potent reuptake inhibitor of serotonin (5-HT) and norepinephrine (NE), is expected to show robust and rapid efficacy in treating emotional symptoms of depression. 5-HT and NE also play an important role in modulation of pain via a descending inhibitory pain pathway in the spinal cord. Therefore we hypothesized that duloxetine would also demonstrate efficacy in painful physical symptoms, which are commonly associated with depression. We examined the temporal pattern of efficacy of duloxetine 60 mg QD in both the emotional and painful physical symptoms associated with major depression. Methods: Data were pooled from two, 9-week randomized, double-blind, clinical trials of duloxetine 60 mg QD (N = 244) and placebo (N = 251). Emotional symptom outcomes included the 17-item Hamilton Rating Scale for Depression (HAMD17) total score and its subfactors and items, as well as the Clinical Global Impression of Severity (CGI-S), and Patient Global Impression of Improvement (PGI-I) scales. Painful physical symptom outcomes included Visual Analog Scales (VAS) for pain. Results: For all emotional symptom outcomes, meaningful and significant advantages of duloxetine over placebo were observed at week 1 or 2, and continued to increase throughout the trial. In physical symptom outcomes, meaningful and significant advantages were again observed at week 1 or 2; however, maximal improvement was observed by week 3. For example, at weeks 1 and 9 the advantage of duloxetine over placebo in mean changes on HAMD17 item 1 were 0.19 and 0.57, respectively. For back pain, the advantage of duloxetine over placebo at weeks 1 and 9 in mean percent improvement was 23.1% and 25.1%, respectively. Conclusions: In these studies, duloxetine (60 mg QD) demonstrated rapid onset of robust and sustained antidepressant efficacy across a wide range of emotional and physical symptom outcomes. Original Citation: Society of Biological Psychiatry Annual Meeting, May 2003. 198—OPEN-LABEL TREATMENT WITH DULOXETINE 60 MG ONCE-DAILY IN THE ACUTE TREATMENT OF MAJOR DEPRESSIVE DISORDER. Gonzales J, Detke M, Wang F, Wiltse C, Prakash A, Wohlreich M, Eli Lilly and Company. E-mail: [email protected] Objective: Open-label studies may better mimic normal clinical practice and may offer a better approximation of clinical practice results with duloxetine 60 mg QD than those seen in placebocontrolled studies. Together with data from placebocontrolled studies, the information from this study may help clinicians to determine the place for duloxetine among current pharmacotherapy choices for the treatment of major depressive disorder (MDD). Methods: Results were obtained from an openlabel, 12-week, multinational clinical trial in MDD outpatients (age ≥ 18) receiving duloxetine at 60 mg (administered once daily.) Results: A total of 533 patients enrolled in this study. Mean changes in the HAMD17 total score, HAMD subfactors, CGI-Severity, and Visual Analog Scales for pain all showed highly significant (P < .001) improvements at all assessment times. Response and remission rates at end point were 67.9% and 52.8%, respectively. Adverse events led to discontinuation in 11.3% of patients. The most frequently reported treatment-emergent adverse events were nausea (35.8%), headache (20.3%), dry mouth (18.0%), somnolence (13.5%), insomnia (10.5%), and dizziness (10.1%). Mean changes for pulse, systolic and diastolic blood pressure, and body weight were 1.72 bpm, 1.35 mm Hg, 0.71 mm Hg, and –.08 kg, respectively. Conclusions: Results from this study were generally consistent with previously reported doubleblind placebo-controlled studies that had established the safety and efficacy of duloxetine in the treatment of major depression. The results reported herein Journal of the American Pharmacists Association 275 2004 Abstracts of Contributed Papers alent patients (LDL-C goal ≤ 100 mg/dL) and non–CHD 2+ risk factor patients (LDL-C goal ≤130 mg/dL). Methods: Retrospective observational study at randomly selected 25 specialist and 15 general practice (GP) centers in Mexico and Brazil. Physicians at the centers selected at random adult (age ≥ 18) patients that were prescribed lipid lowering drug (LLD) for minimum 12 weeks. Date of first LLD was the index prescription date; patients were followed for minimum 3 months (study period) from index date. Medical records were reviewed by physicians to collect patient-level data. A lipid profile was done in a centralized laboratory at end of the study. Results: Two hundred and forty patients were included for study, 38% from GP practice and 62% from specialist practice: 43% were CHD/CHD–equivalent patients, 35% 2+ risk factor patients and 22% < 2 risk factor patients. Mean (± SD) age was 57 (± 12) years, 53% were female. Median reduction in LDL-C required to attain ATPIII goals was 48% for CHD patients and 25% for 2+ risk factor patients. There was no significant difference in LDL-C reduction required at initiation of LLD in Mexico and Brazil. For CHD group, 27% were prescribed low-dose statins (simvastatin 10 mg or equipotent), 36% medium-dose statins (atorvastatin 10 mg or equipotent) and 19% high-dose statins (atorvastatin 20 mg or equipotent) as initial LLD. Physicians in Brazil prescribed higher equipotent statin doses compared with Mexico (MH chisquare < .05). Overall 44% patients attained ATPIII recommended LDL-C goals. After controlling for age, gender, country, baseline LLD, titration and comorbidities, patients with baseline LDL-C ≥ 190 mg/dL (OR = 0.41; 95% CI, 0.23–0.72), 3+ risk factors (OR = 0.51; 95% CI, 0.27–0.98) and CHD (OR = 0.38; 95% CI, 0.21–0.68) were less likely to achieve LDL-C goal. Conclusions: Majority (56%) of hyperlipidemia patients did not attain recommended ATP-III LDLC goals. More aggressive lipid management is required in patients with high baseline LDL-C, CHD and multiple CHD risk factors in order to achieve recommended lipid goals in these patients. FEATURE FEATURE Annual Meeting Abstracts 2004 provide a useful estimation of the outcomes that will be seen in normal clinical practice. Original Citation: U. S. Psychiatric & Mental Health Congress, November 2003. 199—PREVALENCE OF COMORBIDITIES IN DVT AND PE PATIENTS. Yin H, University of Illinois at Chicago, Vogenberg R, Aon Consulting. E-mail: [email protected] Objective: Deep vein thrombosis (DVT) and pulmonary embolism (PE) patients tend to have multiple comorbidities that need to be considered when evaluating pharmacotherapy outcomes. DVT patients may have different comorbidities from PE patients, and until now this comparison had not been examined in the literature. This study aims to identify the prevalence of comorbidities in DVT and PE patients and to compare comorbidity prevalence of the DVT group to that of the PE group. Methods: The study is based on an administrative database from eight U.S. hospitals. There are 2,506 DVT patients and 1,973 PE patients’ records in the pooled database. Patients with both DVT and PE were considered only as PE patient in the analysis. Comorbidities were categorized and summarized according to ICD-9-CM codes. A comorbidity was included in the analysis only when prevalence in DVT or PE group was greater than 1%. A chisquare test was performed to analyze whether the comorbidity burdens were similar or different between the two groups. Results: There are 29 comorbidities with prevalence greater than 1% in either DVT or PE group. DVT patients are found to be more likely to have peripheral vascular disease, anemia, cerebrovascular disease, and renal disease. PE patients are more likely to have cardiac arrhythmias, congestive heart failure, mild to moderate diabetes, chronic pulmonary disease, and cases of drug abuse. Further, a PE patient tends to have more comorbidities overall compared with a DVT patient. Conclusions: Prevalence of comorbidities differs between DVT and PE patients. Additional study is needed to address the reasons why PE patients are more likely to have certain comorbidities. DVT patients who have these comorbidities should be identified in effort to prevent PE development through pharmacotherapy prophylaxis. 200—PROLONGED EPIDURAL ANALGESIA WITH SINGLE-DOSE, ENCAPSULATED MORPHINE VERSUS STANDARD EPIDURAL MORPHINE FOR POSTOPERATIVE PAIN AFTER HIP SURGERY. Viscusi E, Thomas Jefferson University, Kopacz D, Virginia Mason Medical Center, Hartrick C, William Beaumont Hospital, Martin G, Duke University Medical Center, Manvelian G, SkyePharma, Inc. Email: [email protected] Objective: To evaluate the analgesic efficacy and safety of a single, preoperative, epidural injection of sustained-release morphine (DepoMorphine) compared with standard preservative-free morphine sulfate (MS) in patients undergoing total hip arthroplasty with intrathecal anesthesia. 276 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Methods: A prospective, open-label, serial cohort, dose-ranging trial at six U.S. sites enrolled 39 patients scheduled for total hip arthroplasty with intrathecal anesthesia. Patients were assigned to receive DepoMorphine 10 (N = 4), 15 (N = 1), 20 (N = 12), 25 (N = 1), or 30 mg (N = 8) or a control of MS 5 mg (N = 13) as a single injection via epidural catheter 30 minutes preoperatively. Regional anesthesia was then administered with an intrathecal injection of bupivacaine (12.5–17.5 mg). Patients had postoperative access to intravenous patient-controlled analgesia using fentanyl for treatment of breakthrough pain. Efficacy parameters were total fentanyl consumption, time to first fentanyl use, pain intensity rated by 100 mm visual analog (VAS), and 4-term categorical (CAT) scales. Safety was evaluated through clinical assessments and laboratory testing. Results: Mean total fentanyl use for DepoMorphine 10, 20, and 30 mg groups were 598 ± 230 mcg, 261 ± 95 mcg, and 143 ± 101 mcg, respectively, and 1,095 ± 280 mcg for MS (P = .01). Median times to first fentanyl dose were 18, 36, and 35 hours for DepoMorphine 10, 20, and 30 mg, respectively, and 6 hours for MS (P < .001). VAS and CAT scores were comparable among all groups. Pain medication was rated “excellent” by 46% of DepoMorphine-treated patients and 15% of MStreated patients. The most common postoperative adverse effects for both groups were pruritus, fever, and nausea; respiratory effects were mild to moderate in severity and similar for both groups. Conclusions: DepoMorphine provided prolonged dose-dependent postoperative analgesia versus MS 5 mg in patients undergoing total hip arthroplasty with intrathecal anesthesia. This new treatment modality offers clinicians a new option that may simplify postoperative pain management. 201—SUSTAINED-RELEASE EPIDURAL MORPHINE REDUCES POSTOPERATIVE PCA FENTANYL USE FOR 48 HOURS AFTER LOW ABDOMINAL SURGERY. Gambling D, Sharp Mary Birch Hospital for Women, Hughes T, Woodland Memorial Hospital, Martin G, Duke University Medical Center, Manvelian G, SkyePharma, Inc. E-mail: [email protected] Objective: Rationale: Complications can arise from epidural catheterization, especially when anticoagulants are administered. A new, sustainedrelease morphine (DepoMorphine [DM]) may obviate the need for an indwelling epidural catheter and provide prolonged analgesia. Objective: To compare analgesic efficacy and safety of four dosage strengths of DM with a single dose of DM 5 mg (dose-control) and with standard epidural morphine sulfate (MS) 5 mg after elective low abdominal surgery. Methods: 519 adults were randomly assigned to receive preoperative epidural injection of MS 5 mg or DM 5, 10, 15, 20, or 25 mg. Patients had patientcontrolled analgesia (PCA) using intravenous fentanyl for postoperative pain control. Fentanyl consumption through 48 hours was the primary effica- cy endpoint. Pain intensity (VAS: 0–100 mm) and overall pain control (very good, good, fair, or poor) were also assessed. Adverse events were recorded. Results: Mean (± SD) total fentanyl use through 48 hours decreased from 995.1 ± 987.0 mcg to 682.5 ± 620.0 mcg, respectively, with DM 10 and 25 mg compared with 1,213.3 ± 1079 mcg and 1217.1 ± 894.0 mcg, respectively, with DM 5 mg and MS 5 mg (P< .05). In the DM 10, 15, 20, and 25 mg groups, 15% of patients required no supplemental fentanyl through 48 hours compared with 6% and 2%, respectively, in DM 5 mg and MS 5 mg groups (P < .01). VAS scores were better with DM for 48 hours postdose. On Day 2, pain control was rated significantly better in the 15 and 25 mg DM groups versus the MS group (P < .05). Urinary retention and pruritus occurred more frequently in DM patients (9% versus 3% and 54% versus 39%, respectively; P < .05); other adverse events were similar across groups. Conclusions: A single epidural injection of DM provides prolonged postoperative analgesia, improved pain control, and decreased need for postoperative PCA fentanyl, thereby simplifying postoperative pain treatment. 202—WEIGHT CHANGES DURING LONG-TERM TREATMENT WITH DULOXETINE AND PAROXETINE. Gonzales J, Mallinckrodt C, Detke M, Eli Lilly and Company, Raskin J, Eli Lilly Canada, Tran P, Watkin J, Wohlreich M, Eli Lilly and Company. E-mail: [email protected] Objective: Weight gain during long-term antidepressant treatment is a common concern and may interfere with compliance with pharmacotherapy. Methods: Data were pooled from two doubleblind studies. Patients received placebo (N = 192), duloxetine 80 mg/day (40 mg BID; N = 188), duloxetine 120 mg/day (60 mg BID; N = 196), or paroxetine 20 mg QD (N = 183) for 8 weeks. Acute treatment responders (≥ 30% reduction from baseline HAMD17 total score) continued double-blind therapy for an additional 26 weeks. Data from a 52week open-label study of duloxetine 80–120 mg/day (40–60 mg BID; N = 1,279) were analyzed separately. Results: Following acute treatment, mean changes in weight for patients receiving duloxetine 80 mg/day (–0.2 kg), duloxetine 120 mg/day (–0.2 kg), or paroxetine 20 mg QD (–0.1 kg) did not differ significantly from placebo (0.1 kg). After 34 weeks, mean weight changes for duloxetine (80 mg/day: 0.8 kg; 120 mg/day: 1.0 kg) did not differ significantly from placebo (0.1 kg), while patients receiving paroxetine 20 mg QD had a mean weight change significantly greater than the placebo group (1.2 kg; P = .020). Incidences of weight gain ≥ 7% during the 34-week study were: placebo (3.0%), duloxetine 80 mg/day (3.2%), duloxetine 120 mg/day (8.8%), and paroxetine 20 mg QD (11.5%). In the open-label study, mean changes in weight at weeks 8, 32 and 52 were –.2 kg, 1.5 kg, and 2.1 kg, respectively. Conclusions: In these studies, changes in body www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 weight during long-term treatment with duloxetine (80–120 mg/day) were intermediate to the changes observed for placebo and paroxetine 20 mg QD. Original Citation: U. S. Psychiatric and Mental Health Congress, November 2003. APhA–APRS Economic, Social & Administrative Sciences influence the patients’ positive or negative affect or somatic symptoms, but patients assigned to the Veled treatment strategy endorsed fewer depressive symptoms for all four factors. 204—A CONFIRMATORY FACTOR ANALYSIS OF THE CENTER FOR EPIDEMIOLOGIC STUDIES DEPRESSION SCALE OF VERAPAMIL SR-LED AND ATENOLOL-LED HYPERTENSION TREATMENT STRATEGIES. Wilson D, Mueller M, Meng X, Ried L, University of Florida. E-mail: [email protected] Objective: To determine whether the fit of the Center for Epidemiologic Studies depression scale (CES-D) factor analytical model is similar for patients assigned to verapamil SR-led (Ve-led) and atenolol-led (At-led) hypertension treatment strategies. Methods: A subset of consecutively randomized patients involved in an international high blood pressure treatment clinical trial (N = 2,317) was enrolled between April 1, 1999, and October 31, 1999. These patients were mailed a survey that contained the CES-D scale within 24 hours of randomization and after 1 year. All 20 items were completed by 1,019 patients at 1 year. The four-factor CESD model initially used to fit the data included somatic-retarded activity, depressed affect, positive affect, and interpersonal relationship factors. Multigroup confirmatory factor analysis procedures tested differences in the fit of the two treatment groups’ data after 1 year. Mean differences in CES-D scores from the four derived factors were compared between the At-led and Ve-led treatment groups using Student’s t-tests. Results: The data for the combined sample fit the postulated four-factor model. However, the item factor loadings were different between patients assigned to the Ve-led and At-led groups. The patients assigned to the At-led treatment group had scores indicative of higher depressive symptoms when compared with those assigned to the Ve-led treatment on all four factors. Conclusions: The four-factor CES-D model was confirmed. However, patients in the two high blood pressure treatment strategies endorsed the items in the four factors differently. This difference in endorsing the items may reflect the medications’ different pharmacological properties and side effects. Choice of treatment did not preferentially 205—A FIVE-YEAR COMPARISON STUDY OF ARIZONA PHARMACISTS IN RURAL AND URBAN COUNTIES. Eng H, University of Arizona. E-mail: aeng@ahsc. arizona.edu Objective: Similar to many states, Arizona is facing a shortage of pharmacists in both urban and rural settings. There is a growing concern about whether the state can keep up with the demands for pharmacists. The goal of this study is to answer the following question: Are the shortages greater in the rural counties than the urban counties in the state? Methods: Pharmacist data for 5 years (1997–2001) were obtained from the Arizona Board of Pharmacy. Only those with active pharmacist licenses residing in one of Arizona’s 15 counties were examined. An active licensed pharmacist could be a person who is not currently practicing pharmacy or a person who is a part-time practitioner. Pharmacists licensed in other states who were working in federal pharmacies were not examined. A comparison of the number of pharmacists and number of pharmacists per 100,000 residents for the two urban counties, two rural–urban counties, and the remaining 11 rural counties was performed during the 5-year study. Results: In 2001, a total of 3,743 individuals held active Arizona pharmacist licenses, an increase of 843 pharmacists (29%) over 1997. During this 5year period, the ratio of Arizona pharmacists per 100,000 residents increased from 63 to 71. Most of the increases occurred in the two urban counties (30%). Maricopa County had higher pharmacist percentage increases than did Pima County (32% versus 27%). The 13 other counties had similar percentage increases, 20% in the two rural–urban counties and 21% in the remaining 11 rural counties. Conclusions: Examination of the Arizona pharmacist data shows that over the study period, greater increases in the number of pharmacists occurred in the urban counties. The ratio of pharmacists per 100,000 residents increased from 71 in 1997 to 80 in 2001. By contrast, the ratio of pharmacists to 100,000 residents increased from 44 to 45 in the rural-urban counties and 36 to 37 in the rural counties. These data indicate that the shortage of pharmacists is greater in the rural counties than in the urban counties. Mean (± SD) PIF (L/minute) Age Group (years of age) Diskus Aerolizer Turbuhaler 2 29.2 ± 4.1 30.5 ± 6.1 20.2 ± 2.8 3 43.8 ± 17.1 44.7 ± 10.3 37.9 ± 26 4 41.6 ± 14 51.1 ± 20.9 35.0 ± 15.8 5 51.1 ± 15.6 54.6 ± 18.3 44.6 ± 23.1 6–9 58.5 ± 18.7 65.5 ± 27.6 39.7 ± 13.2 10–12 58.6 ± 22.7 75.0 ± 28 47.9 ± 15.6 Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 206—A STUDY OF FACTORS RELATED TO PATIENTS’ SHARING OF SIDE EFFECT AND SYMPTOM SELF-MONITORING INFORMATION WITH THEIR ONCOLOGISTS. Hermansen-Kobulnicky C, University of Wyoming. E-mail: [email protected] Objective: To explore the potential reasons as to why some cancer patients used intervention-based self-monitoring side effect and symptom information when talking with their oncologists, while others did not. Variables of Self-Efficacy for Participating with, Journal of the American Pharmacists Association 277 2004 Abstracts of Contributed Papers 203—INSPIRATORY FLOW THROUGH DRY-POWDER INHALERS (DPI) IN ASTHMATIC CHILDREN 2 TO 12 YEARS OLD. Monske M, McNutt DH, Raissy H, University of New Mexico. E-mail: [email protected] Objective: To measure peak inspiratory flow (PIF) generated through Turbuhaler, Aerolizer, and Diskus dry-powder inhalers (DPIs) in children 2 to 12 years old. Methods: An open-labeled, stratified, randomized, crossover comparison of the three DPIs in asthmatic children presenting to the Pediatric Pulmonary Clinic, University of New Mexico Hospital. All the patients had used MDIs previously, but were excluded if they had used a DPI previously or were experiencing an asthma exacerbation during their visit. Patients were instructed on how to use one device at a time and were asked to demonstrate the use without coaching from the study coordinator or parents. For patients aged 2 and 3 years who were unable to manually activate the device, parents were asked to help the patient and this was noted by study coordinator. Results: A total of 60 patients completed at least one part of the study. The PIF results are presented in the table. Conclusions: The majority (87%) of children less than 5 years old could not generate a PIF of 60 L/minute, whereas the majority (85%) of children older than 2 years of age could generate a PIF of 30 L/minute. When asked which device they preferred overall, a greater percentage (41%) chose Diskus. FEATURE FEATURE Annual Meeting Abstracts 2004 and perceived Interpersonal Relationship Quality of, the oncologist in addition to patient age and education were compared across whether or not patients reported using self-monitoring information in this way after being instructed to do so. Methods: A longitudinal, descriptive design was employed using experimental subject data from a larger study. Subjects were adult cancer outpatients beginning chemotherapy at three cancer clinics, randomly assigned to an intervention designed to teach them to self-monitor side effects and symptoms and to use such information with their oncologists. Data collection was via pretest, posttest, and clinic chart. Variables for hypothesis testing are patients’ SelfEfficacy for Participating with, and perceived Interpersonal Relationship Quality of, the oncologist, measured as multi-item summated scales, and patient age and education. Other variables are used for sample description. Analysis for hypothesis testing includes Student’s t-, matched-pair, and chisquare tests. Results: Data were analyzed from 39 of 61 experimental group subjects (63.9%) who completed the larger study and self-monitored using the intervention materials. Most subjects were women (79.5%), white (94.9%), and educated (48.5% had a college degree). Significant findings include higher Interpersonal Relationship Quality ratings of oncologists among those who reported using their selfmonitoring information with their oncologists (112.5 > 97.4, t = –2.120, P < .05). Conclusions: Study results suggest better provider–patient relationships may improve patient sharing of side effect and symptom information. Provider training, including that of pharmacists, should include how to better elicit patients’ side effect and symptom concerns. Future research is needed to determine how patient self-monitored information can be incorporated into the routine of ambulatory care. 207—ACTIONS OF COMMUNITY PHARMACISTS IN RESPONSE TO CONCURRENT USE OF PRESCRIBED MEDICINES WITH COMPLEMENTARY AND ALTERNATIVE MEDICINE. Shah S, Brown C, Barner J, University of Texas at Austin. E-mail: [email protected] Objective: (1) To determine how often pharmacists inquire about complementary and alternative medicine (CAM) use among their patients; (2) to identify actions pharmacists take in response to patients’ use of CAM along with prescribed medications; and (3) to examine if demographic, professional, or setting characteristics predict differences in pharmacists’ rate of inquiry about CAM use and in the actions taken. Methods: A survey was mailed to 400 Texas community pharmacists. The questionnaire collected information on pharmacists’ inquiries about CAM, their actions in response to patients’ concurrent use of CAM and prescription medications, and their demographic, professional, and setting characteristics. Pharmacists’ responses were analyzed both descriptively and inferentially. Chi-square analyses, 278 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Student’s t-tests, and analysis of variance (ANOVA) were used to examine the differences in pharmacists’ responses. Results: A total of 107 completed surveys were analyzed. Pharmacists rarely to sometimes (mean ± SD, 2.5 ± 0.9) inquired about a patients’ use of CAM. Most pharmacists (72.9%) either encouraged the use of CAM if appropriate or neither encouraged nor discouraged the use of CAM. Pharmacists who had additional training in CAM (P = .002) and those who had a place on patients’ profiles to document CAM use (P = .04) were more likely to inquire about CAM use than others. Pharmacists who stocked herbals or homeopathic products would more often encourage (P = .02) or recommend (P = .03) use of CAM therapies than others. Pharmacists who worked in independent pharmacies were less likely to encourage or discourage use of CAM than pharmacists in other settings (P = .004). Conclusions: The rate of inquiry about patients’ CAM use was rare among pharmacists. They most often encouraged CAM use if deemed medically appropriate. Pharmacists’ actions and rate of inquiry varied based on professional and practice setting characteristics. 208—AN ASSESSMENT OF FRESHMAN PHARMACY STUDENTS’ CONSUMPTION OF AND PERCEPTIONS ABOUT DRUG AND ALCOHOL USE. Patwardhan P, Mukherjee K, Siganga W, Lundy J, University of Toledo. E-mail: [email protected] Objective: Pharmacy students will become providers of pharmaceutical care services and will have easy access to potentially abusive drugs and alcohol. The goals of this study were to determine from first-year pharmacy students the following about themselves and their peers: (1) reasons for alcohol consumption, (2) the frequency of binge drinking, (3) perceptions about illegal drug use, (4) types of illegal drugs commonly used, and (5) perceptions about the effect of current and future drug or alcohol consumption on their future professional integrity. Methods: A 25-item questionnaire was administered to 353 first-year pharmacy students over a 1week period during the fall semester 2002. Questionnaires were distributed to students in 17 sections of a freshman pharmacy class. The data were analyzed using SPSS version 11.5. Results: A total of 329 students responded (93%). Almost all were under 21 years of age. Enhancement of social activity was reported as the main reason for alcohol consumption by 62% of students. Forty-four percent of the students thought that 51%–75% of their peers consumed alcohol at least once every 2 weeks. Forty-four percent reported binge drinking more than two times in the month before the survey. Sixty-two percent of the students thought that 1%–25% of first-year pharmacy students used drugs illegally. Marijuana was the most commonly used illegal drug. Fifty-nine percent of the students thought that use of drugs or alcohol would affect their future professional integrity as health care providers. Conclusions: Having a majority of underage freshman pharmacy students involved in drug and alcohol use should be a concern for the College of Pharmacy. Students must be educated about the hazards of drug and alcohol use. Alcohol abuse prevention and treatment programs could help change the drinking behavior of the students over a period of time. Original Citation: Date: July 2003 Location: Ohio Pharmacist Journal, Volume 52, No. 7, pages 16 and 17. 209—AN EVALUATION OF MANAGING THE RISK OF GLUCOCORTICOIDINDUCED OSTEOPOROSIS. McDonough R, Doucette W, Kumbera P, Klepser D, University of Iowa. E-mail: [email protected] Objective: To assess the impact of risk-management activities on patient risk of glucocorticoidinduced osteoporosis. Methods: This was a randomized control study, set in 15 Iowa community pharmacies, of patients 18 years of age or older who had been on the equivalent of at least 7.5 mg of prednisone for at least 6 months. Patients in the control group received usual and customary care. Patients in the treatment pharmacies received education and a take-home educational pamphlet about the risks of glucocorticoidinduced osteoporosis. In addition, the treatment group pharmacists monitored the patients’ drug therapy and identified and addressed any drug-related problems. Data on the glucocorticoid taken by the patient, other medications, and osteoporosis risk factors were collected at baseline and after 9 months of monitoring, via a Web-based survey completed in the pharmacy. Patients also reported use of osteoporosis preventive therapies, whether anyone had discussed osteoporosis risk from glucocorticoids or the need for a bone mineral density test, and whether they had had a bone mineral density test. Results: When the pre–post frequencies changes were compared between the groups, the contrasts were significant in favor of the treatment pharmacies for the frequency of patients taking a calcium supplement (control, –4 [–6.9%]; treatment, 7 [17.1%], P < .05). Education by the treatment pharmacies also raised patient awareness of bone mineral density testing. Conclusions: Community pharmacists are capable of identifying patients at risk for glucocorticoidinduced osteoporosis. Pharmacists who educate atrisk patients can positively affect the self-care of these patients, including the use of calcium supplements. 210—ASSESSING THE STATE OF DISEASE STATE MANAGEMENT PROGRAMS IN COMMUNITY PHARMACY SETTINGS IN CALIFORNIA. Law A, Western University, Okamoto M, Western University of Health Sciences. E-mail: [email protected] Objective: The purpose of the study was to assess the prevalence, types, and characteristics of disease state management (DSM) programs in the community pharmacy setting in the state of California. www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 211—COLLEGE STUDENTS AND STRESS: WHAT IS THE CONNECTION? A HUMANISTIC OUTCOMES ASSESSMENT. White A, University of Florida, Xiao H, Florida A&M University. E-mail: [email protected] Objective: The objectives of this study are to determine the top three stressors for college students and to explore how different demographics affect those stressors. Methods: Primary Data Collection, CrossSectional Study Items for the questionnaire were obtained from the Brief College Student Hassles Scale (BCSHS), Erindale College University of Toronto. Students responded to a Likert-type scale that ranged from 1 (never) to 5 (extremely often) and ranked stressors in terms of frequency and the extent to which they were bothered by the stressor. The sample consisted of 122 students in pharmacy school at Florida A & M University. Frequencies, Student’s t-test, correlation, regression, and oneway ANOVA were conducted using SPSS. Results: t-Tests: For men (P < .01), the five highest ranked items were (1) parking problems (µ = 4.13), (2) preparing for examinations (µ = 4.11), (3) lack of money (µ = 3.48), (4) schoolwork (working on term papers, reading tedious hard material; µ = Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 3.42), and (5) unavailable resources (µ = 3.18). For women (P < .01), the five highest ranked items were (1) parking problems (µ = 4.36), (2) examination (µ = 4.20), (3) schoolwork (µ = 3.83), (4) lack of money (µ = 3.39), and (5) waiting in lines, appointments (µ = 3.22). Pearson’s Correlation: A negative relationship between age and the stressor appearance of self (P = .021). A positive relationship between female and the stressor health physical symptoms of self (e.g., headache, premenstrual syndrome, allergies) (P = .001). A positive relationship between female and the stressor roommates/house mates relationship (P = .020). A positive relationship between female and the stressor weight/dietary management (P = .007). One-Way ANOVA: Significant differences were identified between age groups with regard to finding or moving into housing and parking problems; between races with regard to bills/overspending; and between men and women with regard to health–physical symptoms. Regression Analysis: Males, age 26 and up (P = .029) and age 17–22 years (P = .016) were less stressed by money than those ages 23–25 years. Whites were less stressed out by money than other races (P = .043). For women, no significant differences were identified among demographics and stressors. Conclusions: Demographics and stress are related, according to the results of this study. Areas in which efforts should be focused for improvement in the future are identified. Original Citation: International Society for Pharmacoeconomics and Outcomes Research, 8th International Meeting, May 2003, Arlington, Va. 212—COMMUNITY PHARMACISTS’ PERCEPTIONS OF COMPUTERIZED DRUG–DRUG INTERACTION ALERTS. Malone D, Abarca J, Skrepnek G, Rehfeld R, Armstrong E, Murphy J, Grizzle A, Woosley R, University of Arizona. E-mail: malone@ pharmacy.arizona.edu Objective: To evaluate community pharmacists’ attitudes toward computerized drug–drug interaction (DDI) alerts, self-perceived ability to interact with physicians, and perceived physician receptiveness to DDIs. Methods: A survey was mailed to pharmacy managers of 3,000 randomly selected community pharmacies in 17 distinct Metropolitan Statistical Areas. A 31-item survey instrument was developed for this study. Of these, seven attitudinal questions using a 6-item Likert scale (1: strongly disagree to 6: strongly agree) were included to obtain pharmacists’ attitudes towards DDI alerts and their self-perceived ability to handle DDIs. Another item collected information on the ability to obtain detailed DDI information from the pharmacy computer system. Each pharmacy was sent an announcement postcard, a cover letter and survey instrument, a reminder postcard, and a follow-up survey for nonresponders. Results: A total of 718 usable surveys were returned (24% response rate). Pharmacy managers reported that they had confidence in the ability of their computer system to identify DDIs (mean ± SD, 4.49 ± 1.23). Most did not think that DDI alerts were a waste of time (mean ± SD, 2.14 ± 1.13). Pharmacy managers agreed with the statement that they had confidence in their own ability to identify DDIs (mean ± SD, 4.91 ± 0.91) and that DDIs are easily differentiated from other DUR alerts (mean ± SD, 4.14 ± 1.42). When responses were analyzed with respect to whether the pharmacy computer system provided detailed information about DDIs or not, those pharmacists with pharmacy systems that provided detailed information were more likely to agree that they were confident that their computer system provided meaningful alerts, less likely to agree that DDI alerts were meaningless, more confident in their ability to identify DDIs, and less likely to agree that the volume of alerts makes it difficult to differentiate clinically meaningful interactions from unimportant interactions (P < .01). Conclusions: The results of this study suggest that pharmacy managers in a community setting are confident in the ability of their computer system to identify DDIs and their ability to contact physicians about DDIs. Most pharmacists did not feel the DDI alerts were useless or a waste of time. Pharmacists working in stores with computer systems that provide detailed information about DDIs were more likely to agree with statements that DDI alerts were meaningful. 213—COMPARING OKLAHOMA MEDICAID RX REIMBURSEMENT RATE VERSUS THE OFFICE OF INSPECTOR GENERAL’S REPORT OF ACQUISITION COST. Phung Q, Oklahoma State University, Jacobs E, University of Oklahoma Health Sciences Center. E-mail: [email protected] Objective: The objective of this study is to estimate the reimbursement rate to Oklahoma pharmacies based on the discount off of average wholesales price (AWP) and compare it to the four tier system suggest by the Office of Inspector General (OIG) to determine how well Oklahoma’s reimbursement rates match the OIG’s report of acquisition cost. We also incorporate the State Maximum Allowable Cost (SMAC) and narrow therapeutic index (NTI) drugs into the analysis to reflect the state’s current Medicaid policies. Methods: The study population was derived from the Oklahoma Healthcare Authority (OHCA) Medicaid prescription database for the year 2002. This database was combined with Medi-Span Master Drug Database (MDDB) and a SMAC dataset to obtain pricing information such as AWP, the federal upper limit (FUL), and SMAC. The data were classified into a tier system reflective of the OIG report and the mean discount off of AWP was calculated for each tier. The results were compared with the OIG report for significance. The data were further reclassified into a different tier system to incorporate SMAC and NTI into the analysis. Results: The results indicated that OHCA reimbursement rate was comparable to the estimated acquisition cost of pharmacy. For Brand, OHCA Journal of the American Pharmacists Association 279 2004 Abstracts of Contributed Papers Methods: The study used an exploratory telephone survey and targeted all 5,270 community pharmacies in California. Pharmacies willing to participate were surveyed about current or past DSM programs in the pharmacy. The reasons for closure of past DSM programs were also obtained. For pharmacies with no DSM programs, interest as well as perceived barriers in developing DSM programs were examined. The pharmacies with existing DSM programs were sent a follow-up survey about the characteristics of the DSM program, including challenges faced in establishing DSM programs, DSM protocols used, measurement of outcomes, reimbursement patterns, and documentation of success of the program. Demographic information was obtained from all participating pharmacies. Results: Data from a total of 1,299 pharmacies had been analyzed when this abstract was prepared. Only about 4% (51) of the sample had a DSM program currently in place; a substantial proportion (37) were in independent pharmacies. Diabetes care was the most prevalent program, followed by asthma and hyperlipidemia. Seven pharmacies had a program that closed down because of either limited patient acceptance or exit of directing pharmacist. About 20% of the pharmacies who did not have a program were interested in implementing a DSM program. Interest was highest for diabetes care. Commonly perceived barriers to new programs were limited time and staff. Conclusions: Independent pharmacies tended to have more DSM programs and more autonomous decision making about developing such programs. The most prevalent and the most desired type of DSM program appeared to be diabetes. Data from the remaining pharmacies and DSM programs are being analyzed and tabulated. FEATURE FEATURE Annual Meeting Abstracts 2004 reimbursement rates were only 3.27% lower off of AWP than the OIG estimated acquisition cost. For generic, the difference ranged from 8.5% to 12.45% (P < .001). The results from the second analysis were also consistent with OIG’s rates. Conclusions: NTI drugs had a higher discount rate as it incorporated both brands and generics into the analysis. Accounting for SMAC resulted in an increased in discount rate. The State’s SMAC reimbursement system appears to be successful in further minimizing cost by reimbursing pharmacy closer to their acquisition cost. 214—CONTENT ANALYSIS OF PRINT DIRECT-TO-CONSUMER DRUG ADVERTISEMENTS TO DETERMINE NUMBER AND SPECIFICITY OF RISK STATEMENTS. Valluri S, Pedersen C, Ohio State University. Email: [email protected] Objective: Our objective for the current study is to determine the number and the specificity of the risk factors (side effects, specific side effects, contra indications, total number of sentences) disclosed in typical direct-to-consumer print advertisements published in 2002. Methods: Content analysis of all product-specific prescription drug advertisements appearing in seven consumer magazines from January 2002 to December 2002 was done. The variables measured were “side effects, specific side effects, contraindications, and the number of sentences containing risk statements.” Sets of operational guidelines were developed to define these variables. Other than the author, two judges independently coded the advertisements. The judges were trained for this purpose. Since the data obtained was of interval type it was recoded into a nominal scale. This was done to determine interrater agreement using Cohen’s Kappa. Each brand name drug advertisement served as the unit of analysis. Descriptive statistics were the primary tool for analytical procedures. Results: A total of 349 advertisements were identified representing 40 distinct brand drugs. Multiple advertisements for the same brand drug were not analyzed as they had the same risk information. Of the total advertisements analyzed, 28 (70%) of the 40 drugs were for long-term use. An average of 4.6 side effects per advertisement were listed. Of these, 0.7 specific side effects were mentioned per advertisement. Each advertisement contained 1.7 contraindications and a total of 2.55 sentences. The interrater agreement between “judge 1” and “judge 2” for side effects, specific side effects, contraindications, and number of risk statements was 0.89, 0.50, 0.849, and 0.498 respectively. Conclusions: The risk statements in direct-toconsumer print advertisements tend to be limited. Overall, advertisements contained only 2.55 risk statements. The average number of side effects disclosed in a typical advertisement is less than 5. Also, drugs for long-term use were more likely to be advertised than those for acute conditions. Future studies on risk disclosure in direct-to-consumer print advertisements should take into account the current risk disclosure in such advertisements. 280 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 215—COST-EFFECTIVENESS ANALYSIS OF A CONTRACEPTIVE PATCH: AN EMPLOYER’S PERSPECTIVE. Patkar A, Holdford D, Virginia Commonwealth University. E-mail: [email protected] Objective: To compare the costs and effectiveness of a new combined hormonal contraceptive transdermal patch with a combined hormonal oral contraceptive pill from an employer’s perspective. Methods: Design: A cost-effectiveness model was developed using decision tree software. Setting: Randomized controlled trials. Participants: Women of childbearing age. Data collection: Data were collected from a variety of public sources including clinical trial data, the Alan Guttmacher Institute, the Kaiser Family Foundation, and databases that provide cost and effectiveness associated with pregnancy outcomes. Analysis plan: The outcome of treatment was failure characterized by pregnancy and subsequent pregnancy-associated childbirths, induced abortions, or spontaneous abortions. The model examined direct and indirect costs to employers associated with unintended pregnancies and pregnancy-related outcomes. Key variables considered in the model were the failure rate (effectiveness) associated with each contraceptive, cost of each contraceptive, and lost workforce productivity. All the costs were estimated for a 1-year period for 1,000 contraceptive users. Data analyses: Data analyses included incremental cost-effectiveness ratio estimation and sensitivity analyses across a range of the key variables. Results: For an employer, the cost of covering the contraceptive patch to prevent an additional pregnancy would be $3.44 more per employee per year than for oral contraceptives. Sensitivity analyses demonstrated that effectiveness of oral contraceptives and costs of the patch were the most important variables that had an impact on the choice of treatment. Conclusions: Contraceptive patch can be costeffective in preventing unintended pregnancies when compared with oral contraceptives. Employers should consider covering the contraceptive patch to avoid further costs of pregnancy-related outcomes. 216—DECISION-MAKING PREFERENCE AMONG COMPLEMENTARY AND ALTERNATIVE MEDICINE USERS AND NONUSERS. Shah B, Chewning B, University of Wisconsin–Madison, Sleath B, University of North Carolina at Chapel Hill, Rubin R, Department of Internal Medicine, University of New Mexico. Email: [email protected] Objective: To examine decision-making preference patterns of complementary and alternative medicine (CAM) users and nonusers. Methods: Data involving use or nonuse of CAM, decision-making preferences of participants, and general demographics were extracted from a data set collected during 1995 at the family practice and general medicine clinics at the University of New Mexico Health Sciences Center in Albuquerque. Descriptive statistics and cross-tabs were carried out using SPSS version 11.0. Results: A little more than one fourth of the patients reported using CAM in the past month. More than two thirds of the CAM users and nonusers preferred shared decision making. While about one sixth of CAM users preferred patients only to make decisions, a lesser number of nonusers (about 10%) preferred patients to make the decisions. There was no evidence that CAM use was greater among patients who were more dissatisfied with care, less confident in care, or felt their feelings were not considered by the physician in prescribing medicines compared with satisfied, confident patients and patients who felt their feelings had been considered by the physician. Lastly, while 14.3% of those who rated their health as poor used CAM, a larger number of those who rated their health as excellent (35.7%) had used CAM in the last month. Conclusions: This study has major implications for pharmacist training and continuing education. Given that more than 25% of respondents had used CAM in the past month, pharmacists need to be prepared to assist those patients who prefer shared decision making. Background and information resources are needed to train pharmacists for counseling regarding CAM. Second, communication skills training is needed to help pharmacists assess and adapt to a patient’s preferred degree of shared decision making. While some patients may not want assistance in the actual decision, the pharmacist can still help a patient be a well-informed and safer decision maker. 217—DEPRESSIVE SYMPTOMS AMONG PATIENTS WITH A HISTORY OF DEPRESSION SIX MONTHS AFTER INITIATING BETA-BLOCKER TREATMENT. Taylor M, Sauer B, Munyer T, Ried L, University of Florida. E-mail: [email protected] Objective: To determine whether prior depression diagnosis is associated with higher depressive symptoms in coronary artery disease patients 6 months after initiating beta-blocker (atenolol) therapy. Methods: A subset of consecutively randomized patients (N = 2,317) involved in an international high blood pressure treatment trial was enrolled between April 1, 1999, and October 31, 1999. Patients were mailed a survey within 24 hours of randomization and again 6 months later. The surveys contained a measure of current depressive symptoms. Patients also reported whether a physician or psychiatrist had previously diagnosed them with depression. Logistic regression was performed to examine the association between depression history and high risk of current depression 6 months after initiating beta-blocker therapy, controlling for age, gender, race, and baseline depressive symptoms. Results: Surveys were sent to 1,134 patients assigned to receive a beta-blocker. Baseline and 6month surveys were returned by 824 (73%) and 657 (58%) patients, respectively. At baseline, 19% of the patients reported an earlier depression diagnosis, and 24.6% had currently high depressive symptoms. Six months later, 22.4% had high depressive symptoms (McNemar’s chi-square = 3.32, P = .082). After controlling for covariates, patients with a prior www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 depression diagnosis were more likely to have high depressive symptoms 6 months after initiating betablocker therapy (OR = 2.04, 95% CI = 1.02, 4.08). Conclusions: Beta-blocker therapy for hypertension may be indicated for patients with coronary artery disease (e.g., myocardial infarction). There was a statistically nonsignificant decrease in the proportion of patients with high depressive symptoms among those prescribed atenolol. Patients with a depression diagnosis before initiating hypertension therapy were at greater risk of depressive symptoms after 6 months when compared with those without prior history of depression. Clinicians should screen for onset or worsening of depressive symptoms after initiating atenolol therapy, especially among those with a history of depression. However, it probably is not a reason to avoid prescribing atenolol when indicated. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 219—DETERMINANTS OF PERCEIVED NEED AND INTENTION TO ADOPT HEALTHIER LIFESTYLE CHOICES IN INDIVIDUALS WITH DIABETES. Maddigan S, Institute of Health Economics/University of Alberta, Johnson J, University of Alberta. E-mail: [email protected] Objective: The purpose was to assess factors associated with perceived need and subsequent intention to adopt healthier lifestyle choices in diabetes (i.e., increase exercise, weight loss, change eating habits, or smoking cessation). Methods: The study sample included 4,125 respondents from the 2000–2001 Canadian Community Health Survey who reported having diabetes diagnosed by a health care provider. Respondents were dichotomized according to perceived need for lifestyle change (yes/no) and intention to make such a change in the next 12 months (yes/no). Logistic regression analysis was used to determine demographic, health status, and current lifestyle factors associated with the perceived need and behavioral intention. Results: Approximately 57% of respondents felt they should do something to improve their health in the next 12 months. Most frequently cited improvements were to increase exercise (38.5%), lose weight (18.0%), and quit smoking (7.2%). Younger individuals (P < .001), those with higher levels of education (P < .001), with higher incomes (P = .005), with higher body mass indexes (P < .001), who were inactive (P = .002), or who drank regularly (P < .001) were more likely to perceive they needed to make lifestyle changes. Health-related quality of life (HRQL) (P < .001) and greater impact of health problems (P = .010) were also significant. Approximately 68% of individuals intended to make a lifestyle change in the next 12 months. Intention was associated with higher levels of HRQL (P = .048), lack of perceived barriers to change (P = .028), lower age (P < .001), being physically inactive (P < .001), being a regular drinker (P < .001) or holding a college or university degree (P < .001). Conclusions: The majority of people with diabetes perceived they needed to make lifestyle changes and intended to do so in the next 12 months. Lack of intention to make lifestyle changes was associated with relatively poor health status, greater perceived barriers to change, and lack of education. Original Citation: The Canadian Diabetes Association Meeting, Ottawa Ontario, October 15–18, 2002. Podium Presentation. 220—DEVELOPING OLDER DIABETICS’ MEDICATION-RELATED KNOWLEDGE, BELIEFS, AND PERCEIVED ABILITIES: IS THE PHARMACIST–PATIENT RELATIONSHIP IMPORTANT? Worley-Louis M, University of Minnesota. E-mail: [email protected] Objective: Diabetes and diabetes-related complications affect older adults (65 years and older) more than other age groups in the population. Diabetic patients engage in sustained interactions with health care professionals, as well as self-management. The study purpose was to investigate the association of pharmacist–patient relationship characteristics with aspects of the medication use process from older diabetic patients’ perspectives. The theoretical framework used in this study consisted of antecedents to building pharmacist–patient relationship quality and outcomes of pharmacist–patient relationships. Antecedents to building pharmacist–patient relationship quality are: (1) pharmacist participative behavior/patient-centeredness of the relationship, (2) patient participative behavior, and (3) pharmacist–patient interpersonal communication. Using self-efficacy theory as a framework, the following medication use outcomes are investigated: (1) medication-related knowledge, (2) medicationrelated outcome expectations (beliefs), and (3) medication-related self-efficacy (perceived abilities). Methods: Design: Cross-sectional and descriptive. Setting: United States. Participants: Systematic random sample of 600 noninstitutionalized adults, 65 years and older with type 1 or 2 diabetes, and using at least one prescription medication to treat diabetes. Data Collection: Mailed questionnaire. Data Analysis Plan: All study constructs will be assessed for reliability using Cronbach coefficient alpha. Discriminant validity will be assessed via exploratory factor analysis. Associations between pairs of study constructs will be assessed using Pearson Product Moment correlations and will be tested for significance at an alpha level of .05. Results: Data collection is complete. The overall response rate is 52.9% (311 responses out of 588 questionnaires mailed). Currently, the data analysis plan is being conducted for this phase of the research project. Conclusions: Study results will be discussed as implications for pharmacy practitioners as they develop counseling and relationship building strategies for older patients with diabetes. Implications for researchers who investigate the medication use process in older patients with diabetes will be discussed. The American Foundation for Pharmaceutical Education, through the American Association of Colleges of Pharmacy New Investigators Program for Pharmacy Faculty, provided funding for this research. 221—DIRECT-TO-CONSUMER ADVERTISING OF PRESCRIPTION DRUGS: MEASURING EFFECTIVENESS AND EDUCATIONAL VALUE ACROSS DIFFERENT MEDIA. Sullivan D, Ohio Northern University. E-mail: [email protected] Objective: To assess the educational value, information, understandability, and consumer attitudes toward direct-to-consumer (DTC) advertising in television, print, and Internet ads. Journal of the American Pharmacists Association 281 2004 Abstracts of Contributed Papers 218—DEPRESSIVE SYMPTOMS AND THE IMPACT ON PHYSICAL FUNCTIONING: ARE MALES AND FEMALES DIFFERENT? Gerhard T, Ballentine A, Nyanteh H, Tueth M, Ried L, University of Florida. E-mail: [email protected] Objective: Major depression occurs in 1%–3% of the elderly population and an additional 8%–16% have clinically important depressive symptoms. These symptoms often result in lower physical functioning. However, whether this relationship is similar for men and women has not been established. This study examined whether men and women are equally sensitive to the physical impact of depressive symptoms. Methods: A subset of consecutively randomized patients (N = 2,317), living in the United States and enrolled in an international hypertension clinical trial between April 1 and October 31, 1999, was mailed surveys within 24 hours of randomization and more than 72% were returned. The survey included a measure of depressive symptoms and the physical functioning and role physical domains of the MOS SF36. Of the returned surveys, approximately 81% (N = 1,359) contained complete data regarding depressive symptoms and were included in the analysis. Results: Older women with high depressive symptoms (Center for Epidemiologic Studies–Depression [CES-D] >20) were more likely to report limitations in daily activities such as work, household chores, and self-care (physical functioning). However, the negative impact of depression on physical functioning was 1.7 times greater for men. While depressed women (N = 181) scored 15.5 points lower on the physical functioning scale than nondepressed women (N = 392), depressed men (N = 159) scored 26.5 points lower than nondepressed men (N = 627). Patient age, baseline CES-D score and the interaction between gender and depression were significant predictors of patients’ role limitations due to physical health (role physical). The negative impact of depression on patients’ work and other daily activities as a result of their health is about 40% greater for men than for women (a decline of 37.3 versus 28.2 points, respectively). Conclusions: Although depression occurs more frequently among older community-dwelling women, it has a larger negative impact on men’s performance of everyday physical activities. Health care practitioners should increase their efforts to detect later-life depression among their older patients and assess its effect on their independence. FEATURE FEATURE Annual Meeting Abstracts 2004 Methods: A total of 480 Ohio consumers were randomly selected for inclusion in the study. The survey instrument was a self-administered, mailed questionnaire using a Likert-type scale, with 1 = strongly disagree to 6 = strongly agree. Consumers were asked to compare the three types of media on risk–benefit information, educational value, drug information quality, understandability, and usefulness. Results: Of the 187 (39% response rate) respondents, 25% indicated they had talked to their doctor about an advertised drug within the past year; 15% had asked their doctor for a prescription for an advertised product; and 13% had saved an ad from a magazine/newspaper. Respondents slightly to moderately agreed that both print and television ads were written at a level they could understand (mean ± SD = 4.44 ± 1.29 and 4.51 ± 1.24, respectively). However, respondents slightly agreed that print and television ads lacked information on side effects and risks. Consumers felt that prescription drug ads in magazines and newspapers had more educational value that those on television (t = –2.86, df = 179, P = .005) and Internet ads had more educational value than television ads (t = 3.51, df = 159, P = .001). Consumers felt that information in Internet ads was more useful (mean = 3.82 ± 1.42) than television ads (mean ± SD = 3.65 ± 1.45) (t = –2.136, df = 146, P = .034). Consumers indicated that ads on television (mean ± SD 4.36 ± 1.40) and in magazines/newspapers (mean = 4.19 ± 1.59) lacked important information more so than ads on the Internet (t = 4.45, df = 148, P < .001) and (t = 2.752, df = 148, P = .007), respectively. Finally, consumers found magazine/television ads more truthful (mean ± SD = 3.64 ± 1.37) than television ads (mean ± SD = 3.42 ± 1.38) (t = 2.54, df = 172, P = .012). Conclusions: NA. 222—DISABILITY IN STROKE OUTCOMES RESEARCH. Kwon S, Hartzema A, Duncan P, University of Florida, Lai S, University of Kansas Medical Center. E-mail: [email protected] Objective: Residual disability after stroke presents a major economic and humanistic burden. To quantify disability in patients, three disability instruments are globally used: Barthel Index (BI), Motor component of Functional Independence Measure (M-FIM), and Modified Rankin Scale (MRS). The purpose of this study is to understand the relationship among these disability measures by examining the differentiating ability of the BI and the M-FIM to the global disability scale MRS. Methods: Kansas City Stroke Study data were used for the current study. Polytomous logistic regression analysis was applied to produce probabilistic distributions of BI and M-FIM corresponding to MRS. Model-fit statistics were examined to verify logistic regression appropriateness. A categorization scheme, which minimized the false positive rate, was selected as the optimal categorizing system. Results: Three measures were highly correlated. BI and M-FIM do not differentiate disability well in higher level of functioning. BI differentiated four 282 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 levels with the following categorization scheme: 0 ≤ MRS5 < 15, 15 ≤ MRS4 < 70, 70 ≤ MRS3 < 95, and 95 ≤ MRS(0,1,2) ≤ 100, and M-FIM differentiated three levels with the scheme: 13 ≤ MRS5 < 26, 26 ≤ MRS4 < 62, and 62 ≤ MRS(0,1,2,3) ≤ 91. These cutoff points were consistent for baseline, 1, 3, and 6 months. Conclusions: The proposed categorization scheme can serve as a translation between measures. However, due to the ceiling effect of BI and M-FIM, the translation could not be completed for all six distinct levels of MRS. No apparent variation over time in the categorization scheme was observed. 223—DO DIABETIC PATIENTS’ MEDICATION USE BELIEFS AND PERCEIVED ABILITIES VARY BY ACTUAL, PREFERRED, AND POTENTIAL SOURCES OF MEDICATION HELP? Worley-Louis M, University of Minnesota, Hermansen-Kobulnicky C, University of Wyoming. E-mail: [email protected] Objective: Diabetic patients’ medication use involves both self-management and sustained interaction with health care providers. This pilot study’s purpose is to explore how diabetic patients’ beliefs (outcome expectations) and perceived abilities (selfefficacy) for medication management and monitoring vary by patients’ preferred, actual, and potential sources of diabetes medication-related help. Methods: Design: Cross-sectional and descriptive. Setting: United States. Participants: Random sample of 300 noninstitutionalized adults (18 years and older) with type 1 or 2 diabetes, and using at least one diabetes prescription medication. Data Collection: Mailed questionnaire. Patients’ beliefs and perceived abilities for medication management and monitoring are measured using multi-item scales. These will be assessed for reliability using Cronbach coefficient alpha, refined using interitem and item-to-total correlations, and assessed for discriminant validity using principal component analysis. Patients’ actual and preferred sources for diabetes medication help are measured as two categorical variables. Patients’ potential for using a pharmacist as a source for help is measured by evaluating the likely presence of a pharmacist–patient relationship. Data Analysis Plan: Means comparisons will evaluate beliefs and perceived abilities across actual, preferred and potential sources for obtaining help about diabetes medication use and monitoring. Cross tabulations will be used to compare actual, preferred and potential sources. Results: Data collection is ongoing. Overall response rate to date is 42.5% (124 of 292). Conclusions: Study results may include finding differences among patients’ self-report of actual, preferred, and potential sources of help, as well as differing beliefs and perceived abilities across patients’ whose report of actual, preferred, and potential sources of help match, versus those patients that do not match. Evidence of a pharmacist–patient relationship may support opportunities for pharmacists to assist diabetic patients in the areas of medication management and monitoring, and helping to build patients’ beliefs and perceived abilities in these areas. Research implications also will be discussed. 224—DOES OWNERSHIP TYPE RELATE TO MANAGERIAL TIME CULTURE IN COMMUNITY PHARMACIES? Gurney M, Mount J, University of Wisconsin–Madison. Email: [email protected] Objective: (1) Describe how ownership relates to strategic and operational management in community pharmacies. (2) Examine relationships between ownership and strategic and operational management, controlling for organizational factors that may covary. Methods: Cross-sectional, multimethod study of stratified random sample of community and ambulatory pharmacies involved in a school of pharmacy’s experiential learning program. Data were collected via telephone interviews with pharmacy managers and mail-back surveys from manager and staff pharmacists. Of 173 surveys sent, 82 (47.4%) surveys (39 pharmacy managers; 43 pharmacists) were analyzed. Data on management activities were collected using a series of 25 questions. A strategic management index (SMI) and an operational management index (OMI) were constructed to measure temporal aspects of planning functions (in SMI) and organizing, implementing, and controlling functions (in OMI). Data on other pharmacy factors were gathered during telephone interviews. Ordinary least squares regression was used to analyze relationships between ownership and strategic management and operational management. Results: While ownership is not a significant predictor of SMI for the total sample, it is a significant predictor of SMI for both the manager and staff pharmacist subgroups. This is in opposite directions, with independent managers reporting significantly lower involvement in strategic activities than their staff pharmacist colleagues of their chair pharmacy counterparts. Results remain similar when covariates are entered into the analysis. In contrast, ownership is largely unrelated to OMI for the total sample, mangers, and staff pharmacists. Although having no direct effects, ownership appears to have an indirect effect on OMI through its effects on SMI, particularly for staff pharmacists. Conclusions: Independent, health-system, and corporate chain pharmacies have markedly different management approaches, with involvement being the most manager-centered in corporate chain pharmacies and most devolved to staff pharmacists in independent pharmacies. In study pharmacies, managerial time orientation was not uniformly held, suggesting that the time aspect of organizational culture is fragmented. Further research is needed into how cultural content and structure relate to efforts to change pharmacy’s model of patient care. 225—DRUG THERAPY COST SAVINGS AND QUALITY INITIATIVES DIRECTED TO MEDICAID RECIPIENTS IN NORTH CAROLINA. Trygstad T, Christensen D, University of North Carolina at Chapel Hill, Thorpe J, AccessCare Inc. E-mail: [email protected] www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 226—EFFECT OF AN AUTOMATED PRESCRIPTION FILLING SYSTEM AND INSPECTION ENHANCEMENT TOOL ON DISPENSING ACCURACY. Flynn E, Barker K, Auburn University. E-mail: [email protected] Objective: To compare the rate of dispensing errors before and after the implementation of an automated dispensing system providing two levels of control. Methods: Design: Explanatory study. Participants: One independent and one chain pharVol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 macy. Data collection: A pharmacist–researcher evaluated the accuracy of prescriptions filled during 2-week periods before and after the installation of an automated dispensing system in each pharmacy. A robotic device filled the top 200 oral solid dosage forms, and all drugs were subject to bar code verification. A dispensing error was defined for new prescriptions as any deviation from a prescriber’s written order, and for refills as any deviation between the prescription content and the label. Data analysis: A paired two-sample t test for means was employed to compare daily error rates before and after system implementation. Results: At the independent pharmacy the dispensing error rate was 2.8% before (99 errors on 3,427 prescriptions) and 2.1% after (68 errors on 3,241 prescriptions) the automated system was installed, a statistically significant decrease (P = .099). At the chain pharmacy, the dispensing error rate was 1.9% before (64 errors on 3,424 prescriptions) and 2.4% after the new system (74 errors on 3,028 prescriptions), which was not a statistically significant difference (P = .225). Conclusions: The implementation of the automated dispensing system was associated with a statistically significant decrease in the overall dispensing error rate in the independent pharmacy but not the chain pharmacy. A close inspection of the processes and specific errors revealed much about the challenges of reducing prescription dispensing errors via automated dispensing systems. 227—EVALUATING THE INSTRUCTIONAL DESIGN OF A WEB-ENHANCED PROGRAM FOR TEACHING THE PRACTICE OF PHARMACEUTICAL CARE. Droege M, Nova Southeastern University. E-mail: [email protected] Objective: The objectives of this study were to design a new, Web-enhanced educational tool to teach students and practitioners the fundamental principles of pharmaceutical care practice and to evaluate the extent to which it might be effective. Methods: A Web-enhanced educational tool for teaching the practice of pharmaceutical care was designed applying principles of problem-based learning (PBL) and a formative evaluation of the learning materials was performed aimed at the usability of the software and its content. The method used in the evaluation of the instructional design was an inspection method similar in style to the heuristic method for usability testing described for the evaluation of computer interfaces. This expertise-oriented evaluative approach involved having 11 evaluators examine the interface and judge its compliance with the stated objectives. Evaluators were recruited who possessed expertise in software development; instructional design as well as pharmaceutical care practice. Results: Evaluation data suggest that a valid and reliable instrument for evaluating the educational tool was developed. In addition, evaluator comments led to the identification of a small number of problems that need to be addressed before the release of the educational tool. These deficiencies pertained to three general areas: interface design, instructional design, and content of the design. No major problems were identified that would question the release of the educational multimedia program. Conclusions: The problem-based, Webenhanced approach appears to be a practical tool to support an effective learning experience for teaching the fundamental principles of pharmaceutical care practice. 228—EVALUATION OF VITALITY AND DEPRESSIVE SYMPTOMS ON PHYSICAL FUNCTIONING IN A COHORT OF ELDERLY PATIENTS WITH CORONARY ARTERY DISEASE. Mayhew D, Schiller K, Telfair T, Ried L, University of Florida. E-mail: mayhew@ cop3. health.ufl.edu Objective: The objective is to investigate if vitality effects physical functioning after considering depressive symptoms in coronary artery disease patients. Methods: A subset of consecutively randomized patients enrolled in an international high blood pressure clinical trial and who were living in the United States (N = 2,317) were enrolled into a concomitant substudy between April 1, 1999. and October 31, 1999. These patients were mailed surveys within 24 hours of randomization; 1,359 patients returned the baseline survey, and 1,116 patients returned 1-year surveys. The survey included the Center for Epidemiologic Studies—Depression scale, a measure of depressive symptoms, and the vitality and physical functioning domains of the Medical Outcome Study Short Form 36. The temporal ordering of the depressive symptoms and vitality variables and their direct and indirect influence on 1year physical functioning were examined using path analysis. Results: Persons with lower energy and vitality were more limited in their daily activities (standardized regression coefficient [beta] = 0.332, P < .001). Patients reporting more depressive symptoms were more limited in their daily activities (beta = –0.352, P < .001). Higher baseline depression scores were associated with more fatigue and tiredness (beta = 0.418, P < .001), whereas baseline vitality had little impact on depressive symptoms 1 year later (beta = –0.002, P = .233). The effect of 1-year depression scores on 1-year vitality was significant (beta = –0.882, P < .001), even after controlling for baseline levels of vitality and depressive symptoms. Conclusions: Higher levels of depressive symptoms directly limit patients’ work, exercise and other daily activities. Depressive symptoms also indirectly limit these activities because of its impact on patients’ vitality and energy levels. While depressive symptoms and vitality are associated, depressive symptoms seem to be more associated with lower energy levels and fatigue rather than patients interpreting their lower energy levels and fatigue as depressive symptoms. Journal of the American Pharmacists Association 283 2004 Abstracts of Contributed Papers Objective: The aim of this study is to develop, demonstrate, and evaluate a structured retrospective DUR and intervention project aimed at North Carolina Medicaid nursing home residents. Consultant pharmacists in nursing homes were provided patient drug profiles that targeted/flagged potential drug therapy problems. Specific objectives are to assess the impact of this intervention in terms of (1) the type and frequency with which potential drug therapy problems were reported, (2) the impact of changes in terms of the quality and cost of drug therapy received by residents, and (3) the downstream impact of changes in use of services and associated medical costs. With Phase 1 only recently completed (March 2003), we present results related to objective 1 and partially for objective 2. As 6month follow-up data become available, we will use pharmacy claims to validate pharmacist reports of drug cost savings (objective 2), and use hospital and physician services claims to report downstream impact on quality. Phases 2 and 3 will incorporate another 15,000 or more residents and will be analyzed when their respective claims become available. Methods: This is a cohort study with comparison group. The study group consists of 9,310 nursing home residents in 253 nursing homes. The comparison group consists of 13 geographically separated nursing homes. The impact of pharmacist activities, in terms of numbers and types of interventions as well as projected cost savings, are reported and discussed. Additionally, 6 months of claims data before and after the date of intervention will be used to validate the drug and medical care cost impact. Results: An average of 1.22 recommendations were made per resident. An average drug cost savings of approximately $40 per patient per month was achieved for each intervention. There was evidence that drug-related quality was improved as a result of interventions. For example, 936 drugs were found to have a potential for serious adverse drug reactions, 631 recommendations were made to change therapy for Beers’ list drugs, and 448 recommendations were made to discontinue duplicative drug therapy. Conclusions: A program of medication profile review of Medicaid nursing home residents by pharmacist consultants collaborating with physicians is projected to be cost-beneficial based solely on drug cost savings. We estimate the cumulative savings potential of the program to be in excess of $14 million through December 2004. FEATURE FEATURE Annual Meeting Abstracts 2004 229—EXAMINING THE RELATIONSHIPS WITHIN AND PRESENCE OF THE SERVICE PROFIT CHAIN IN INDEPENDENT COMMUNITY PHARMACY. Bonnarens J, University of Wisconsin–Madison, Wilkin N, University of Mississippi Medical Center, McCaffrey D, Garner D, University of Mississippi. E-mail: [email protected] Objective: The intent of this study is to explore whether satisfied and loyal employees provide quality service, to explore whether this service is related to satisfied and loyal customers, and to explore if satisfied and loyal customers are correlated with revenue growth and profitability. Methods: This exploratory study was designed to use primary data collection techniques to examine the each of the seven “links” proposed in the service profit chain model. The study was to test the applicability of the model in community pharmacy, specifically independent community pharmacies. Recruitment efforts focused on a national pharmacy franchise corporation. A sample of pharmacies (N = 40) was recruited. To collect the necessary data dictated by the service profit chain model, three groups of participants were identified: owners/managers, employees, and customers. A multistage data collection method was implemented using a total of three different instruments, one for each participant group, to collect the varied amount of data identified in the model. Scale measures were adapted from the literature. Reliabilities were measured using Cronbach and factor, when appropriate, and results showed similar reliabilities found in the literature. Then, correlation coefficients were calculated for each link in the chain model. Results: Based on specific criteria, 47.5% of pharmacies were eligible for analysis, including a usable response rate of 61.5% for employees and 29.8% for customers. Based on correlation analyses, five of the possible seven relationships predicted by the service profit chain were found to be significant. In addition, the significant relationships that were identified support previous empirical testing of the model in other industries. Conclusions: Although further research is needed, the service profit chain holds potential as a management tool useful in explaining the link between customer satisfaction, employee satisfaction and financial performance of an independent community pharmacy. 230—EXPERIENCE WITH A WORKSITE EDUCATIONAL PROGRAM ON ARTHRITIS AND MUSCULOSKELETAL DISORDERS. Gianarkis D, Pfizer. E-mail: dean.gianarkis@ pfizer.com Objective: The objectives of the program were to measure the impact of arthritis on work productivity, assess the effectiveness of treatments, and educate participants about arthritis. Methods: Workshops were conducted at 13 different sites at 6 different companies nationwide. Participants were provided with educational materials, attended a lecture, and were then asked to complete a survey. A total of 798 surveys were evaluat- 284 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 ed, 648 contained 11 questions, and 150 had 39 questions. Results: Overall, 71% (106/150) of participants experienced symptoms of arthritis. 32% (48/150) had the disease for at least 5 years, 20% (26/133) had symptoms greater than 6 months, and 33% (46/140) experienced 10 or more episodes per year. Further, 61% (85/139) rated their symptoms as moderate to severe. 28% (31/111) of the population reported missing 5 or more work days in the last 12 months and more than 70% (87/124) reported working 6 months or more with arthritis symptoms in the past year. When the total impact of presenteeism was considered, arthritis reduced workforce productivity by 16.2%. The survey also included questions on medication use. 33.6% (45/140) of the sample did not take any medication for their arthritis symptoms, 33.6% (47/140) take nonprescription products, and only 18.6% (26/140) reported taking prescription NSAIDs. Lastly, control of arthritis symptoms was measured. 38% of participants rated their symptom control as fairly poor, poor, or very poor and 29% (23/80) were dissatisfied or very dissatisfied with their current medication. After attending the workshop, 60% (303/506) of attendees plan to speak to their doctor about arthritis treatments and 94% (615/657) indicated the ability to have a productive discussion with their doctor about arthritis. Conclusions: This workshop was successful in increasing awareness of the signs and symptoms of arthritis and knowledge of treatment options. 231—FACTORS AFFECTING BARGAINING POWER OF DRUG-PURCHASING GROUPS IN THAILAND. Ngorsuraches S, Saichol S, Faculty of Pharmaceutical Sciences, Prince of Songkla University. E-mail: [email protected] Objective: To examine the effects of purchasing volume, purchasing group size, purchasing time, history of contract, and geographic location on bargaining power of the drug-purchasing groups in Thailand. Methods: Design: The bargaining model developed by Brooks, Doucette, and Sorofman (1999) is applied to the situation between drug-purchasing groups and manufacturers. Data Sources/Setting: This study uses retrospective analysis of two national databases, which are drug price information and hospital information for 2002, established by Ministry of Public Health. Data Collection: The drug price information database comprises two types of drug price lists, which are reference price and bid purchasing price for drug products. The reference price list is set as maximum allowable cost of each product that public hospitals can possibly buy, while the bid purchasing price list is bid prices agreed between a purchasing group and a manufacturer. The reference price list is composed of generic name, package size, and unit price, while the bid purchasing price list contains generic name, trade name, package size, manufacturer, volume of purchased products, purchasing time, and bid purchasing price from each purchasing group. Enalapril 20 mg tablets, gemfibrozil 300 mg tablets, hyoscine nbutylbromide 10 mg tablets, and ceftriaxone 1 gram vials are chosen in the study because they have high purchase volumes and represent either short- or long-term treatment. The hospital database contains numbers of beds of the hospitals in each purchasing group and health care zones, which are geographically assigned by Thai government. Main Outcome Measure: Bargaining power of drug-purchasing groups. Analysis Plan: Multiple regression analysis is planned for estimating coefficients in the bargaining model, which will reflect the effects of studied factors on the bargaining power. Results: Descriptive statistics show evidence of different bargaining power across the drug-purchasing groups. Conclusions: NA. 232—FACTORS AFFECTING UTILIZATION OF NEW PRESCRIPTION DRUGS. Agarwal S, Ye X, Cline R, University of Minnesota. E-mail: [email protected] Objective: The objective of the present research is to analyze factors affecting utilization of new prescription drugs. Methods: The household component and prescribed medicines event files from the Medical Expenditure Panel Survey (MEPS) 2000 were used for this study. The analysis was limited to the antiarthritic therapeutic category. Elderly people over the age of 65 with arthritis were selected and COX-2 or NSAID prescriptions for these individuals were identified using National Drug Codes (NDC). The outcome variable was classified into two separate categories: (1) ever-use of a COX-2 inhibitor and (2) never-use of a COX-2 but with a prescription for NSAID. Those who had at least one prescription of COX-2 were coded as having used newer drugs (Y = 1), while others with prescriptions of only NSAIDS were coded as not having tried newer drugs (Y = 2). The independent variables selected were guided by Andersen’s Health Services Utilization Model, which include predisposing variables (age, gender, and ethnicity), need variables (comorbidity, health status) and enabling variables (income, insurance status, copayment for a prescription drug). The difference in utilization rates was modeled using all the independent variables in a multivariate logistic regression equation model and the effects of each independent variable on the prescription of COX-2 were tested at the significance level of .05. Results: Preliminary results suggest a relationship between utilization of newer drugs and co-payments. Higher out-of-pocket prescription drug expenditures are associated with lower newer prescription drug use regardless of health status and comorbidities. Conclusions: People with higher copayments are deterred from using higher-priced newer prescription drugs. In addition, lower copayments could introduce moral hazard and lead to unnecessary use of expensive drugs. Insurers should introduce strategies that reduce needless consumption of new drugs while ensuring adequate access to appropriate therapy. www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 234—FUNCTIONAL HEALTH LITERACY AMONG CHINESE POPULATION IN CHICAGO. Ko Y, University of Arizona, Lin S, Salmon J, Crawford S, University of Illinois at Chicago. Email: [email protected] Objective: (1) Measure functional health literacy (FHL) among a Chinese population in Chicago using the shortened version of the Test of Functional Health Literacy in Adults (S-TOFHLA). (2) Determine relationships between FHL and sociodemographic variables. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 Methods: A convenience sample of Chinese adults was recruited in the city of Chicago in May 2003. A sociodemographic questionnaire and the STOFHLA were administered by face-to-face interview. The S-TOFHLA tests the participant’s ability to perform basic reading and numerical tasks required to function in health care environments, such as the ability to interpret instructions on prescription bottles and an appointment card. Summary statistics, bivariate analyses, and multiple regression were conducted to meet the study objectives. Results: A total of 50 Chinese adults participated in this study. Overall, 34% of the participants had inadequate or marginal FHL. About 25% of the participants could not correctly interpret information provided on prescription bottles and the test result card. Bivariate analyses indicated that lower FHL was significantly associated with older age, less education, owning a residence, and using English as second language (P < .05). However, education was the only significant predictor of FHL in multiple regression model after controlling for other covariates, with subjects having more years of education also having a higher FHL score. Conclusions: This is the first study to examine the FHL level of a Chinese population. About one third of the participants in this study had inadequate or marginal FHL, and a significant portion had problem interpreting frequently encountered medical information and instructions. As non–Englishspeaking population in the United States is increasing, there is an urgent need to identify patients without adequate FHL and to develop appropriate intervention. Pharmacists should be aware of the difficulty their patients may encounter in understanding health information and instructions. 235—GENERIC DRUG UTILIZATION PATTERNS AMONG ELDERY AND NONELDERLY INDIVIDUALS. Agarwal S, Zhang D, Schondelmeyer S, University of Minnesota. E-mail: [email protected] Objective: The objective of the present study was to determine and compare the generic drug-utilization rates amongst elderly and nonelderly Americans. Methods: The household component and prescription drug event files of Medical Expenditure Panel Survey (MEPS) 1998 were used for this descriptive research. The generic availability status of a drug was obtained from multisource codes available in Medi-Span’s Master Drug Database (MDDB). Analyses on generic drug-utilization rates categorized according to age, sources of payment, out-of-pocket spending, therapeutic category and income were conducted. Generic drug utilization was defined in three ways: (1) generic prescribing rate, (2) generic dispensing rate, and (3) generic consumption rates. Generic prescribing rate was the ratio of the number of multiple-source brand and generic drugs used to the total number of drugs used. Generic dispensing rate was the ratio of the number of generics used to the total number of drugs that had the opportunity to be generically used (multiple-source brand + generics). Generic consumption rate was the ratio of the total number of generics used to the total number of drugs used. Results: Seniors had poorer rates of insurance coverage of prescription drugs than the younger individuals. The older cohort with no prescription drug coverage had lower generic dispensing rates, generic prescribing rates and generic consumption rates than the nonelderly group. In situations where medications could be generically substituted, the elderly had lower generic dispensing rates than did the nonelderly (i.e., a cheaper generic drug was dispensed less often for the elderly). Conclusions: The preliminary results of this study indicate that seniors in certain circumstances tend to use generics at a lower rate than do nonseniors. Higher utilization rates of generic drugs would result in lower drug expenditures for the elderly. 236—GETTING PHARMACISTS TO RESPOND: A COMPARISON BETWEEN MAIL AND TELEPHONE SURVEYS. Chamnanmoh S, Mount J, University of Wisconsin– Madison. E-mail: [email protected] Objective: The main goal of this study was to evaluate the effectiveness of mail and telephone surveys. Three specific objectives were to (1) evaluate the level of study participation and quality of response between mail and telephone surveys; (2) compare the costs for data collection in mail and telephone surveys; and (3) assess the pattern of response between mail and telephone survey participants. Methods: A short postcard-length and a brief telephone survey were used to collect data concerning pharmacy-based immunization activities in Washington State. First, a mail census of community pharmacies was conducted. Next, a 5-minute follow-up telephone survey, using the same questions contained in the mail survey, was conducted with 110 randomly selected pharmacies that did not respond to the mail survey. Results: Of the 1,143 mail surveys, 328 were returned and 2 were undeliverable, yielding the cooperation rate of 28.7%. For the telephone survey, of 110 pharmacies contacted, 92 agreed to participate and 3 were ineligible, yielding the cooperation rate of 86%. Using completeness of answer to survey questions as a measure of quality of response, the response quality was greater for the telephone survey. Additionally, costs for each usable survey was compared. The mail survey was the most expensive, the telephone survey using an advanced notification letter was the second most expensive, and the telephone method not using an advanced letter was the least expensive method. The results also revealed that the type of pharmacy and the existence of an immunization protocol did not affect participation for either the mail or telephone survey. However, participating pharmacies in the mail and telephone surveys were different in their involvement in some immunization activities. These differences were due to nonresponse bias. Conclusions: The telephone survey achieved a Journal of the American Pharmacists Association 285 2004 Abstracts of Contributed Papers 233—FORECASTING THE IMPACT ON COX-2 NSAID UTILIZATION IN A MEDICAID PROGRAM USING PRIOR AUTHORIZATION CRITERIA. Vuchetich P, Juracek J, Jorgensen A, Creighton University. E-mail: [email protected] Objective: Prior Authorization in the Nebraska Medicaid program is designed primarily to promote appropriate use of medication, and secondarily as a cost-containment tool. The goal of this project was to forecast the impact on COX-2–specific NSAID utilization based on a draft set of prior authorization criteria. These estimates would be used by the Nebraska Medicaid DUR Board as part of the discussion about specific prior authorization criteria and would aid in the development of final prior authorization criteria recommendations to the state. Methods: A draft version of the prior authorization criteria, including seven specific criteria sequenced in a stepwise order, was created by the drug-use review board. The researchers used these draft criteria to estimate the impact on utilization and cost using actual pharmacy and medical claims paid over the previous 12-month period (April 2001 through March 2002). The reporting and statistical analysis was based on the most recent actual claims data for the population impacted by the prior authorization. Results: The results of this study identified that a majority of patients who had received COX-2–specific NSAIDs in the 12-month period immediately preceding the study would receive prior authorization according to the draft criteria. Approximately 70% of the 13,898 patients who received a COX2–specific NSAID would be approved using the draft criteria based on the data available. Of the patients who would be denied, more than one-half (52%) did not have a medical claim with a diagnosis for which an NSAID is indicated. Conclusions: The forecasting of the impact of the prior authorization criteria, both as individual criteria and as an algorithm was possible using available claims and administrative data that were already captured as part of the normal business processes. This forecasting was used as part of the decision-making process by a drug-use review board, and was available for program administrators to help predict the impact on utilization and cost of implementing a prior authorization program. This initial study will serve as a foundation for evaluating the actual impact on pharmacy and medical utilization, program costs, and clinical impact of the prior authorization program. FEATURE FEATURE Annual Meeting Abstracts 2004 higher level of participation as well as high response quality, with a reduced cost per response. Future researchers should consider using a telephone survey as a: (1) screening tool to document prevalence of pharmacy/pharmacists’ activities, (2) survey method to replace a mail survey, or (3) follow-up method with mail survey nonrespondents to examine nonresponse bias. A telephone survey is a viable data collection method that holds many promises in pharmacy research. 237—HEALTH CARE DECISIONS UNDER BUDGET CONSTRAINT IN THAILAND. Kasemsup V, Schommer J, Hadsall R, Cline R, Dowd B, University of Minnesota. E-mail: [email protected] Objective: To improve access to health care, in 2001, the Thai government launched a new policy named the “30-baht-per-visit” program in an attempt to provide health insurance coverage to Thai people who had not been covered by other public insurance plans. Because the cost of providing coverage for high-cost treatments such as renal replacement therapy (RRT) for end-stage renal disease (ESRD) and antiretroviral drugs for people living with HIV/AIDS would undermine financial viability of the 30-baht-per-visit program, these therapies have not been included in the program’s benefit package. As a result, almost all ESRD patients have not received RRT and people living with HIV/AIDS have not been optimally treated with antiretroviral drugs. Under limited resources, we assert that it is better to provide some treatments for selected patients than not providing any care at all. From this perspective, we propose that rationing criteria will be used for decision making under budget constraint and that these criteria should be established with input from the general public. Therefore, the specific aims of this study are as follows: (1) Determine rationing criteria that would be accepted by Thai citizens for selecting patients for high-cost therapies; and (2) investigate the extent to which “five principles” of rationing [(a) lottery principles or “not playing god”; (b) distribution according to immediate need or “rule of rescue”; (c) health maximization; (d) equalizing lifetime health or “fair inning”; and (e) equalizing opportunity for health or “choicism”] are related to rationing decisions. Methods: Data will be collected from three focus groups and from a household survey of 500 respondents in Thailand. Methods of analysis are descriptive analysis, one-sample t test, ANOVA, factor analysis, and multinomial logistic regression. Results: Results of the study will be used for policy decisions related to high-cost treatments in Thailand. Conclusions: NA. 238—HEALTH-RELATED QUALITY OF LIFE AMONG URBAN INDIGENT PERSONS WITH HIV INFECTION. Viswanathan H, Purdue University, School of Pharmacy and Pharmacal Sciences, Anderson R, New Century Medical Imaging (at the time of the study, Dr. Anderson was Director of Health and Education Services at the 286 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Damien Center), Thomas J, Purdue University, School of Pharmacy and Pharmacal Sciences. Email: [email protected] Objective: To assess health-related quality of life (HRQOL) among urban indigent persons with HIV/AIDS, to compare participants’ HRQOL scores to general population norms and those for chronic conditions, and to examine relationships between patient characteristics, nonadherence, and HRQOL. Methods: A cross-sectional written survey of HIV/AIDS infected individuals currently taking antiretroviral medication was conducted at an HIV/AIDS service center. The Medical Outcomes Study Short Form 12 Version 1 (SF-12) was used to assess HRQOL. Nonadherence was assessed using the 9-item Morisky Adherence Scale. Data also were collected on social support, number of antiretroviral medications, CD4 counts, and time since diagnosis. Statistical analyses were conducted using t-tests and linear regression. Results: Of the 112 surveys received, 86 surveys were analyzed because 2 survey codes were not discernible, 11 did not meet inclusion criteria, and 13 had missing data on the SF-12. Approximately 84% of participants were men, and 50% were white. The mean ± SD physical component summary (PCS) score of 41.0 ± 12.5 and mental component summary (MCS) score of 41.9 ± 11.0 were lower than population norms (P < .001). Participants’ PCS scores were lower than those of individuals with hypertension (44.3 ± 10.8) and depression (45.0 ± 12.0). Participants also had lower MCS scores than individuals with hypertension (52.2 ± 9.3) and diabetes (51.9 ± 9.5). In multivariate analyses, employment and higher social support were positively associated with PCS scores (P <.05) and nonadherence was negatively associated with MCS scores (P <.05). Conclusions: Participants had significantly lower HRQOL scores compared with population norms, poorer physical health than patients with hypertension and depression, and poorer mental health than patients with hypertension and diabetes. Employed participants and those with higher social support had higher PCS scores. Participants reporting higher nonadherence had lower MCS scores. Identifying strategies for increasing social support and adherence for economically disadvantaged persons with HIV/AIDS may improve their HRQOL. 239—HIPAA COMPLIANCE PROCEDURES: IMPACT AND PERCEPTIONS AMONG COMMUNITY PHARMACISTS. Kavookjian J, Mamidi S, West Virginia University. E-mail: [email protected] Objective: New Health Insurance Portability and Accountability Act of 1996 (HIPAA) compliance regulations became effective in April 2003 for the purpose of ensuring security of patient health information (PHI). The regulations call for training, compliance procedures (CPs), and potential equipment that may pose burdens on community pharmacies. The objectives of this pilot study were to explore and describe the state of HIPAA CPs in community pharmacy, including impact of train- ing/staffing issues, privacy statements and compliance methods, the burden of time spent gaining patient consent, patient reactions to new HIPAA CPs, and pharmacy staff utilization and perception of HIPAA CPs. Methods: The study was exploratory and descriptive; it included an examination of HIPAA regulations literature and open-ended interviews with eight community pharmacists in four types of practice settings (chains, independents, grocery stores, mass merchandise stores). A semistructured interview protocol was generated, pretested, and implemented via 96 telephone interviews among community pharmacists in West Virginia, Pennsylvania, and Ohio. Pharmacists were identified through semirandom selection, with eight pharmacies representing each of the four categories per state. Analyses included descriptive statistics and ANOVA. Results: Respondent pharmacists were 61.8% women, had been practicing an average 13.16 years, and experienced an average daily prescription volume of 206. Nearly all staff (96.8%) were HIPAA trained at the time of the study, predominantly using in-store computerized training. All pharmacies had HIPAA CPs in place, including logbook or electronic signature “box”. Time spent explaining privacy to patients was a mean 1.81 minutes, conducted an average 31.16 times per day. 42.2% of pharmacists agreed that HIPAA CPs took time away from patient counseling, with independent pharmacists being more concerned about this than chain pharmacists. Most patients were receptive; some were appreciative. Pharmacist and staff reaction was mixed, with the cons for HIPAA CPs being more salient than the pros. Conclusions: These findings suggest implications for future research to expand the study of the impact of HIPAA compliance procedures, and could perhaps lay the groundwork for exploration of cost impact variables in community pharmacy. 240—HYPERTENSION OUTCOMES THROUGH BLOOD PRESSURE MONITORING AND EVALUATION BY PHARMACISTS (HOME STUDY). Zillich A, Purdue University, Carter B, University of Iowa, Kumbera P, Outcomes Pharmaceutical health Care. E-mail: [email protected] Objective: To evaluate the effectiveness of a community pharmacist–based home blood pressure monitoring program. Methods: This was a randomized, controlled trial conducted in 12 community pharmacies. Six intervention pharmacies provided a pharmacist-based home blood pressure (BP) monitoring program. Six additional pharmacies served as control sites. Patients with uncontrolled BP were eligible to participate. The program comprised four face-to-face visits with a trained pharmacist. Pharmacists provided patient specific education about hypertension including: (1) disease process and complications, (2) medication use and adherence, (3) lifestyle modification, and (4) proper home BP monitoring. Following the first and third visits, patients were www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 241—IMPACT OF MEDICATION MANAGEMENT ON INFORMAL CAREGIVERS OF PATIENTS WITH DEMENTIA AND ALZHEIMER’S DISEASE. Byrd J, Sleath B, University of North Carolina at Chapel Hill, Clipp E, Doyle M, Richard L, Duke University Medical Center. E-mail: [email protected] Objective: To compare the amount of time spent helping with medicines versus other caregiving tasks for informal caregivers who provide care for elderly relatives with progressive dementia. To determine the caregiver and patient characteristics that are related to the amount of time that caregivers help with their medications. To examine whether increased time spent managing medication is associated with lower emotional health status of the informal caregiver. Methods: The data are from the National Longitudinal Caregiver Sample, a survey of 2,279 informal caregivers of elderly male veterans diagnosed with probable Alzheimer’s disease or vascular dementia. All variables were measured using caregiver self-report on a mailed survey. Time spent managing medicines is reported in average minutes per day, as are the other caregiving tasks. Emotional Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 health of the caregivers was measured and categorized using a modified version of the Center for Epidemiological Studies – Depression (CES-D) scale and a combined version of the Short Psychiatric Evaluation Schedule (Pfeiffer) and the Langer Twenty-Two Item Screening scale to measure stress and psychological distress. Results: Medication management requires more time (mean, 19.5 minutes per day) than the majority of the seven personal management tasks and all eight physical care tasks. Results of the regressions of time spent helping with medicines on caregiver and patient characteristics and of caregiver emotional health on medication management time are currently being conducted. Conclusions: This study has found, thus far, that more time is spent by caregivers helping with medicines than on the majority of other personal management tasks and all of the physical care tasks provided to patients with dementia. This suggests that the caregiver’s role in medication management for demented adults is important in the overall caregiving process and that pharmacists can develop interventions to decrease the time spent by caregivers and enhance their overall emotional health. 242—IMPACT OF SUSTAINED-RELEASE LINE EXTENSIONS ON GENERIC DRUG UTILIZATION. Agarwal S, Schondelmeyer S, University of Minnesota. E-mail: agar0040@ umn.edu Objective: The objectives of the study were to: (1) determine the generic utilization rate of drugs with sustained-release line extensions, and (2) describe the effect of sustained-release line extensions on price competition in the post–generic drug market. Methods: This descriptive study used a longitudinal secondary database from IMS Health on sales of prescription drugs that had first generic entry between 1993 and 2001. Oral solid drug products that had a sustained-release line extension introduced within a year of generic entry were included in the study. Line extensions without any generic substitutes constituted the nonsubstitutable portion of the market. Dosage forms with generic alternatives formed the substitutable component. Defined daily doses sold for each drug product were calculated to obtain a measure of units used. Generic utilization rates were calculated using two different denominators: (1) total chemical entity market (substitutable and nonsubstitutable), and (2) substitutable section of the chemical entity market. Price competition in the substitutable and nonsubstitutable markets was assessed. Results: Separate analyses were performed with the inclusion and exclusion of fluoxetine in the sample. In the market with substitutable drugs, the generic utilization rate was almost 30% (50% with fluoxetine) 6 months after generic entry. The total chemical entity market had approximately 25% (42% with fluoxetine) generic penetration 6 months after generic entry. The price of the nonsubstitutable section of the market was about 50% more than the price of generics at 24 months after generic entry. Conclusions: The generic penetration rates for the total chemical entity market were lower than the utilization rates for the substitutable component. Sustained-release extensions introduced at the time of generic entry acquired a significant portion of the post–generic drug market. 243—JUDGING A BOOK BY ITS COVER: THE PREDICAMENT WITH CANADIAN PHARMACY ADVERTISEMENTS AND AMERICAN CONSUMERS. Ballentine A, Lipowski E, University of Florida. E-mail: [email protected] Objective: To gauge the adequacy of Canadian pharmacy advertisement content by comparing the information contained within the advertisement to the information consumers are recommended to obtain prior to forming a judgment about a pharmacy’s quality and authenticity. Methods: The U.S. Food and Drug Administration (in conjunction with 14 other organizations including the American Pharmacists Association), the National Association of Boards of Pharmacy, and the American Association of Retired Persons have each published consumer guidelines on how to safely and securely purchase prescription medication from Internet and foreign pharmacies. The guideline sets were compared and main themes extracted. These themes were then compared with a pretest sample of pharmacy advertisements from two Florida newspapers during June 1–30, 2003. Content analysis will be performed on Canadian pharmacy advertisements appearing in 10 Florida newspapers over a 1-month period, from September 1–30, 2003. Results: The consumer guidelines contained 10 unique themes, such as provision of pharmacist access, pharmacy address, phone and license number, patient privacy policy, an explanation of Canadian and American drug and labeling differences, along with the requirement of the patient’s medical history and prescriptions from the consumer’s personal doctor. In the pretest sample, not a single pharmacy advertisement mentioned consumer access to a pharmacist and only one mentioned licensure and provided a nonresident pharmacy license number. The greatest number of guideline themes addressed in any one advertisement was four. Conclusions: According to the pretest sample content analysis, Canadian pharmacy advertisements do not contain an adequate amount of information for consumers to accurately judge the authenticity and quality of a Canadian pharmacy. The public policy implications may be that new educational campaigns or regulatory changes need to be implemented if Americans are to follow specified guidelines intended to safeguard their well-being. 244—MEDICATION SAFETY IN THE PHYSICIAN’S OFFICE—OPPORTUNITIES FOR COMMUNITY PHARMACISTS. Galt K, Clark B, Rule A, Bramble J, Moores K, Creighton University. E-mail: [email protected] Journal of the American Pharmacists Association 287 2004 Abstracts of Contributed Papers provided with a home BP monitoring device and instructed to measure their BP at least once daily for the next month. Home BP readings were used by the pharmacists to develop treatment recommendations for the patient’s physician. Recommendations were discussed with the physician and, if approved, implemented by the pharmacist. Control pharmacies did not provide patient education, home BP monitoring, or physician recommendations. These patients were referred to their physician for evaluation. The primary outcome measure was the difference in systolic BP (SBP) between the intervention and control patients at program conclusion. BP measurements were performed in the pharmacies using a uniformly dedicated, automatic electronic device. A trained pharmacist recorded the average of two BP readings separated by 5 minutes of rest. Secondary study end points include hospitalizations, emergency department visits, physician office visits, medication adherence, and quality of life. Data were submitted via a secured Web-based claims processing system, the Outcomes Case Management Program. Analyses of differences in SBP will be performed using t tests. Chi-square tests will be used for analyses of secondary end points. Results: 120 patients have been enrolled, with 64 completing the study. The study population is an average of 64.1 (SD = 12.2) years old and 59% women. For patients completing the study, baseline SBP was not significantly different between the control group (N = 37) and the intervention group (N = 27) (154 versus 153.6 mm Hg, respectively; P = .892). At study completion, SBP was significantly reduced in the intervention group compared with the control group (133.9 versus 141.6 mm Hg, P = .05). Conclusions: Preliminary results suggest this model can improve BP control. Final results will be presented. FEATURE FEATURE Annual Meeting Abstracts 2004 Objective: To study the safety aspects of the medication use process in primary care office practice, and to recommend practical improvements to enhance patient safety. Methods: A 154-item written survey was developed to assess medication safety practices in primary care office practice. Safety domains were identified and items developed. The survey was piloted on two offices to assure content and face validity, and reduce item ambiguity. The survey was administered using the interviewer-assisted technique to 31 primary care office managers in the Nebraska and Iowa region. Direct observation and on-site interviews were conducted to assess the environment, facilities, technologies, and office behaviors related to the medication use process. Results: 44% of the practices report no specific procedure to respond to a serious medication error, 56% report no established procedure for providing prescription drug samples to patients, 36% report that pharmacists repeat back the prescription when they telephone prescriptions in to minimize errors associated with verbal transmission, 33% report updating the patient’s chart when they renew medications by phone, 24% report dismissing individuals from employment because of errors. The prescribing process itself was studied to determine areas for practice improvement for safer prescribing. Information is presented on practices related to maintaining current patient charts, collecting timely medication histories from patients, the generation of new prescriptions, the processes associated with prescription renewal, methods of prescription transmission, and prescription clarification once received by the pharmacists. Conclusions: Improving the medication use process initiated in primary care offices is an important step to improving medication safety for the public. This research contributes new knowledge to our understanding of outpatient medication safety, supports evidence-based decisions about improvement practices, and helps to define where inter-professional efforts between primary care physicians and pharmacists are necessary, add value, and how successful they may be in a wide scale effort to improve patient medication safety in the local community. 245—OSTEOPOROSIS BELIEFS AND ANTIRESORPTIVE MEDICATION CHOICES: RESULTS OF A SURVEY IN MINNESOTA. Cline R, Farley J, University of Minnesota, Hansen R, University of North Carolina at Chapel Hill, Schommer J, University of Minnesota. E-mail: [email protected] Objective: Osteoporosis is a disease that causes deterioration in bone strength and often results in fractures of the hip, wrist, and vertebra. Although a number of prescription medications are effective in the treatment and prevention of osteoporosis, little is known about the factors influencing women’s decisions to use medications such as the antiresorptives. The objectives of this study were (1) to better understand how beliefs regarding osteoporosis and antiresorptive drugs are associated with decisions to use these drugs and (2) to assess the utility of the health 288 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 belief model (HBM) in predicting choices among hormone replacement therapy (HRT), newer antiresorptives, and no prescription drug therapy for osteoporosis. Methods: A cross-sectional survey design was used. Survey forms were mailed to 1,700 community-dwelling women aged 45 and older residing in Minnesota. Respondents completed measures of HBM constructs, as well as medication profiles and demographics. Data were analyzed using multivariable logistic regression models. Results: A total of 990 usable survey forms were returned, yielding an adjusted response rate of 61.1%. Higher perceptions of susceptibility to osteoporosis were associated with the choice of newer antiresorptives over no therapy as were some cues to action (having been diagnosed with osteoporosis or ever having a test for the disease). Women attributing strong benefits to these drugs were more likely to use them, as were women who perceived few barriers to their use. Respondents were likely to choose HRT relative to no therapy if they had ever been tested for osteoporosis and if they perceived few barriers to the use of prescription medicines for its treatment. Conclusions: Several HBM constructs were associated with the decision to use newer antiresorptive drugs relative to no prescription therapy. However, few HBM components were operative in the choice of HRT relative to no therapy. Although the HBM appears to provide a plausible model of the decision to undertake newer antiresorptive drug therapy, it explains little about women’s use of HRT. 246—PATIENT EXPECTATIONS, PERCEPTIONS ON PERFORMANCE AND SATISFACTION WITH PHARMACIST DIRECTIVE GUIDANCE. Stroud L, Bharmal M, Thomas J, Purdue University. E-mail: [email protected] Objective: The study objectives were to: (1) assess patients’ expectations, perceptions on performance, and satisfaction with directive guidance provided by pharmacists, (2) assess associations between patient expectations and perceived satisfaction with pharmacists’ services, (3) examine correlations between disconfirmation of expectations and patient satisfaction. Methods: Based on review of literature, a survey was developed to assess patients’ expectations, perceptions on pharmacists’ performance and satisfaction with pharmacist directive guidance. Some items assessed perceptions regarding pharmacists providing medication-related instructions (i.e., more basic care), while the remainder assessed perceptions regarding pharmacists providing feedback and goal setting (i.e., more advanced care). Disconfirmation was calculated by subtracting individuals’ expectation ratings from their rating of pharmacists’ performance on individual items. The initial survey was mailed to 1,000 randomly selected Indiana residents. To increase the survey response rate, two follow-up mailings were made at approximately 4week intervals. Data were analyzed using SAS for Windows version 8.2. Kruskal–Wallis tests were used to assess associations between demographic variables and expectations, performance, disconfirmation, and satisfaction. Spearman rank correlation coefficients were used to assess associations between expectations, performance, disconfirmation, and satisfaction. An a priori alpha level of .05 was used for all statistical tests. Results: A total of 306 completed surveys were returned, a response rate of 30.6 percent. Cronbach’s alpha reliabilities of the all the scales were good, and ranged from 0.74 to 0.92. There was a low nonsignificant negative correlation (–0.12, P = .069) between expectation and satisfaction. The correlation between satisfaction and performance was moderate (0.41, P < .05). However, the correlation between disconfirmation and satisfaction was highest (0.51, P < .05). Conclusions: The results of the study support application of expectation-disconfirmation theory to examining patients’ attitudes toward pharmacy services. Although expectations were low for higher level services (i.e., feedback and goal setting), disconfirmation of those expectations had significant associations with satisfaction. The findings should reinforce pharmacies’ efforts to advance higher level services. 247—PATIENT SELF-MANAGEMENT BEHAVIOR ADOPTION IN CHRONIC CONDITIONS BASED ON TRANSTHEORETICAL MODEL READINESS STAGE OF CHANGE PROFILES FOR SELF-MANAGEMENT. Sankaranarayanan J, Mason H, Purdue University. E-mail: [email protected] Objective: To determine the: (1) distribution of readiness stages for Transtheoretical Model Readiness Stage of Change Profiles for SelfManagement (TTMSM) and its significance in identifying patient type (risk status), and (2) associations among sociodemographic, psychosocial (coping, stress, self-efficacy, goal setting), self-management behavior, and perceived health status outcome (using the Medical Outcomes Study Short Form 12 Version 2 [SF-12]) variables with TTMSM-stage. Methods: Prospective, cross-sectional random mail survey of Indiana-based managed care enrollees, 18 years and older with asthma, diabetes, hyperlipidemia, or hypertension included 4,040 low-risk and 700 high-risk patients. The study protocol was approved by Purdue University’s Institutional Review Board. Results: The usable survey response rate was 13%. Patients with a mean of two chronic conditions, maximum disease duration of 12 years, and a majority wanting self-management advice distributed into TTMSM-stages (precontemplation, contemplation, preparation, action, or maintenance). The evaluable patients (N = 607) were distributed across all five TTMSM-stages for three self-management domains of participation with doctor, general, and lifestyle management, but not for the medical care domain. More patients (36.9%) were in precontemplation–contemplation for general self-management. In ANOVA models, association between the TTMSM summated score and chronic conditions www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 were not significant (P = .5590). The TTMSM-stage of lifestyle management was significant (ordinal logistic-regression, P = .007) in classifying a patient as low- or high-risk user. Only goal setting had significant association with TTMSM summated score (ANOVA, 10.2%, P < .05). The TTMSM summated score was explained by self-management behavior, age, goal setting and number of information support sources (ANOVA, 36.8%, P < .05). Patient type, the four TTMSM domains, diabetes, coexistence of asthma, high cholesterol and hypertension and all four medical conditions, were significant in explaining SMBI (ANOVA, 41.7%, P < .05). Conclusions: More patients reported advanced TTMSM-stage for medical care than for general self-management. Independent of chronic conditions, the TTMSM-stage appears to indirectly impact health status through patient self-management behavior. In the delivery of effective self-management education programs, health providers need to consider patients’ TTMSM-stage in addition to their chronic conditions. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 249—PDA PRESCRIBING IN OUTPATIENT SETTINGS: BARRIERS AND SOLUTIONS. Galt K, Bramble J, Rule A, Clark B, Siracuse M, Taylor W, Lust E, Creighton University, Schwartz A, University of Nevada, Moores K, Creighton University. E-mail: [email protected] Objective: Successful adoption of the personal digital assistant (PDA) use by primary care physicians in office practice may result in improved safety when prescribing takes place. However, introducing of new technologies may meet with user adoption barriers. This research identifies adaptation and adoption barriers perceived by physicians using PDAs as a prescribing tool in outpatient practice and the strategies physicians employed to overcome these barriers. Methods: Forty primary care physicians were provided PDAs with both a drug information and prescription writing software package. After successful completion of training, subjects used the PDA as a drug information source and prescriptiongeneration tool. We conducted qualitative interviews 2 weeks after initiation of the PDAs to elicit the barriers experienced and how they overcame these barriers. Five experts identified themes and patterns that emerged using a content analysis process employing human factors, organizational theory and technology diffusion theory as a framework. Results: Four major themes emerged related to inhibition of full adoption of PDA use and applications: Technology, Time/Workload, Environment, and Personal. Physicians reported the software did not always meet their needs and that the time to learn, the speed of the PDA, and the work environment were not conducive to full adoption. Four themes related to responses to these barriers emerged: self-help, seeking assistance, avoidance, and partial adoption. Physicians either “gave up” and returned to their “old” ways or partially adopted the piece of technology that was easiest to learn and efficient. When PDA use interfered with “seeing” patients the technology was deemed “not worth it.” Conclusions: Barriers and solutions to PDA use exist on both an individual and system level. Technology adoption for individual users requires adaptation at both levels. Users need to have the time to learn how to implement the technology so it is an asset and not an inhibitor to daily practice. 250—PHARMACEUTICAL CASE MANAGEMENT: A CASE OF IDENTIFYING AND RESOLVING DRUG-RELATED PROBLEMS IN THE COMMUNITY. Klepser D, Doucette W, McDonough R, McCarthy R, University of Iowa. Email: [email protected] Objective: The Iowa Medicaid program has initiated a pharmaceutical case management (PCM) program in which community pharmacists and physicians work together to manage the drug therapy for ambulatory patients taking at least four chronic medications. The objective of this project was to describe the drug-related problems identified at one pharmacy during the first 2 years of the PCM program. Methods: In the PCM program pharmacists make written recommendations to the patient’s physician after assessing a patient’s drug therapy. For 153 patients who had at least one documented visit during the first year of the PCM program, data were abstracted from the pharmacy records. Collected data included patient demographics, number of chronic conditions and medications at first visit, type and number of drug-related issues, pharmacist recommendations, and physician acceptance of the recommendations. Results: The patients had an average age of 54.2 (SD, 19.3) years and nearly 74% were women. They were taking a mean of 9.3 (SD = 4.5) medications and had 6.2 (SD = 2.9) medical conditions at the start of PCM. A total of 901 drug-related issues were classified into nine categories: inappropriate compliance, 232 (25.8%); needs additional therapy, 200 (22.2%); wrong drug, 122 (13.5%); unnecessary drug therapy, 113 (12.6%); adverse drug reaction, 98 (10.9%); dosage too low, 85 (9.4%); dosage too high, 47 (5.2%); and two types less than 1% each (drug duplication, drug interaction). The pharmacists made 672 recommendations regarding the drug-related issues, which resulted in 323 changes in drug therapy for the patients. Specifically, pursuant to a pharmacist’s recommendation physicians changed dosage 87 times, changed to a different medication 84 times, stopped a medication 78 times, and added a medication 74 times. Conclusions: The PCM program showed that the safety of drug therapy for ambulatory patients can be improved through collaboration between physicians and pharmacists. 251—PHARMACIST COLLABORATIVE PRACTICE IN HOSPITALS. Bharmal M, Purdue University, Lin S, University of Michigan Hospital, Thomas J, Purdue University. E-mail: [email protected] Objective: The objectives of this study were to: (1) identify the extent and scope of collaborative practice (CP) occurring in U.S. hospitals, (2) identify perceived facilitators and barriers for CP, (3) assess perceptions of pharmacy directors regarding support for CP, and (4) assess the perceived strategic impact and financial impact of CP. Methods: A mail survey was developed and pretested in January 2002 with 30 hospital pharmacy directors in Illinois, Indiana, and Michigan. A national random sample of 1,000 hospital pharmacy directors stratified by state were mailed surveys. Pharmacy directors’ perceptions regarding support for CP and impact of CP were obtained through ratings of statements on a 5-point Likert scale (1 = Journal of the American Pharmacists Association 289 2004 Abstracts of Contributed Papers 248—PATIENTS’ EVALUATION OF CARE FOLLOWING A DENIAL OF AN ADVERTISEMENT-RELATED PRESCRIPTION DRUG REQUEST: THE ROLE OF EXPECTATIONS, SYMPTOM SEVERITY AND PHYSICIAN DECISION-MAKING STYLE. Shah M, Bentley J, McCaffrey D, University of Mississippi. E-mail: [email protected] Objective: To assess the influence of physician decision-making style, patients’ expectations of receiving a prescription, and perceived symptom severity on patients’ evaluation of care following a physician denial of a prescription drug request stimulated by direct-to-consumer advertising. Methods: This study uses a 2 × 2 × 2, betweensubjects, experimental design. Physician decisionmaking style, patients’ expectations of receiving a prescription medication, and patients’ perceived symptom severity were manipulated using vignettes. Manipulations were reviewed by experts and pretested. Patients’ postvisit evaluation of care was assessed by measuring trust in the physician, visit-based satisfaction with the physician, and commitment towards the physician. University staff members were randomly assigned to read one of the eight vignettes and then responded to a Web-based, self-administered survey. Factorial analysis of variance procedures for a three-way design were used to test the hypotheses and propositions. Results: Postvisit patient evaluation of care was significantly associated with physician decisionmaking style (partnership response led to better evaluation of care). Prior expectations and perceived symptom severity were not significant predictors of evaluation of care; however, nonsignificant trends in mean scores were in the predicted direction. No significant interactions were detected. Conclusions: Physicians attempting to minimize the effect of request denials on patient evaluations should attempt to make the patient feel involved in the decision-making process. The manner in which a physician communicates with the patient is an important determinant of patient evaluation of care following a denial of a patient’s request. Prior expectations of patients and symptom severity need to be further explored as determinants of patient evaluation of care. The results have implications for other health care professionals, including pharmacists, who commonly respond to patient requests. FEATURE FEATURE Annual Meeting Abstracts 2004 strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, and 5 = strongly agree). SAS for Windows version 8.2 was used for descriptive statistics and t tests comparing responses from CP and non-CP institutions. Results: Usable responses were received from 318 hospitals, a 31.8% usable response rate. A total of 155 respondents, 49.2%, indicated some pharmacist(s) in their hospital were engaged in CP. Infectious disease (79.3%), anticoagulation (60.6%), and parental nutrition (55.6%) were most frequently mentioned CP disease state/therapeutic areas. Payment or reimbursement for some CP was received in 12.7% of hospitals with CP. Upper hospital administration support for CP was rated higher in CP hospitals (mean ± SD = 3.85 ± 0.78) than in non-CP hospitals (2.98 ± 0.91) (P < .0001). CP hospitals’ pharmacy directors also perceived a favorable strategic impact of collaborative services through enhancing upper administration’s perceptions of the value of the pharmacists (4.25 ± 0.67) and physicians asking staff to provide more advanced services because of CP (3.91 ± 0.88). Conclusions: Pharmacy directors of CP hospitals perceived upper hospital administration, physicians, management staff, and nurses as more supportive of CP compared with non-CP hospitals. CP has provided positive strategic benefit to pharmacists practicing in hospitals. 252—PHARMACISTS’ ORGANIZATIONAL COMMITMENT: AFFECTIVE, CONTINUANCE, AND NORMATIVE. Kahaleh A, Ohio Northern University, Gaither C, University of Michigan. E-mail: [email protected] Objective: To distinguish between three dimensions of pharmacists’ organizational commitment. Methods: The study has a cross-sectional design. Self-administered questionnaires were mailed to a national random sample of 1,200 pharmacists. Data were coded, entered, and analyzed using SPSS 10.0 for Windows statistical software. Descriptive statistics were used to examine demographics. Validity and reliability of multiple-item measures were assessed using factor analysis and Cronbach’s coefficient alpha. Given the hyperdemand for pharmacy services, employers are working hard to recruit pharmacists. Organizational commitment is becoming more important to consider in recruiting and retaining qualified pharmacists. Organizational commitment was measured as (1) affective (attachment to the organization); (2) continuance (perceived costs associated with leaving the organization); and (3) normative (obligation to remain in the organization). Results: Factor analysis revealed that the three dimensions were distinguishable from one another. Reliability tests for affective (AC), continuance (CC), and normative (NC) commitment showed that Cronbach’s alphas were 0.87, 0.50, and 0.86 respectively. Using a 7-point Likert scale, NC had the highest mean (± SD) 4.25 ± 1.5, followed by AC, 3.75 ± 1.7, and CC, 3.50 ± 1.8. Also, 67% of the pharmacists indicated that they are willing to spend the rest of their careers with their organizations, 51% said 290 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 that they are staying in the organization because of sense of obligation to the people in it, and 48% stated that staying with the organization is a necessity. Conclusions: Consistent with theoretical considerations, the results provided evidence that organizational commitment has three distinct dimensions: affective, continuance, and normative. Employers can help their organizations by increasing pharmacists’ affective commitment. Pharmacists who have a high level of affective commitment tend to have a high interest in achieving the organization’s goals. 253—PHARMACISTS’ VIEWS OF DEVELOPING COLLABORATIVE WORKING RELATIONSHIPS WITH PHYSICIANS. Nevins J, McDonough R, Doucette W, University of Iowa. E-mail: [email protected] Objective: A conceptual model of collaborative working relationships between physicians and pharmacists states that collaboration is affected by three sets of characteristics: individual, context, and exchange. The objective of this study was to test the conceptual model to empirically determine which sets of characteristics influence collaboration. Methods: Data were collected through a survey mailed to a national sample of 321 pharmacists identified by state pharmacy associations as being innovative practitioners. Individual variables included demographics and personality measures. Context variables included practice environment and professional interactions between pharmacists and physicians. Exchange characteristics were measured using the three domains of the Physician/Pharmacist Collaboration Instrument (PPCI): trustworthiness, role specification, and relationship initiation. Four items asked about the pharmacist’s collaborative care with a physician and were rated using a 7-point Likert scale. A linear regression analysis was performed with collaborative care as the dependent variable and the individual, context, and exchange characteristics as the independent variables. Results: A total of 166 usable surveys (53.4%) were returned. About 64% of the respondents were men with a mean age of 43.7 (SD, 11.2) years. Independent pharmacy owners were the most common respondents, while family practice was the most common specialty of collaborating physicians. Linear regression analysis of the model produced an R2 = 0.790 (P < .001). Significant predictors in the model included professional interaction, trustworthiness, and role specification. Conclusions: Overall, the collaborative working relationship model explained the development of collaborative care between pharmacist and physicians. The exchange characteristics trustworthiness and role specification were positively correlated with collaborative practice. In addition, the scope of professional interactions, a context variable, had a positive influence on the level of pharmacist–physician collaboration. Further work is needed to extend our understanding of collaboration between pharmacists and physicians. 254—PHARMACY-BASED IMMUNIZATION PROGRAMS IN WASHINGTON STATE. Chamnanmoh S, Mount J, University of Wisconsin–Madison, Rochon J, Washington State Pharmacy Association. E-mail: schamnanmoh@ wisc.edu Objective: Describe the level of pharmacy involvement in and trends related to pharmacybased immunization programs in the State of Washington. Methods: Using a postcard-length survey, a census of community pharmacies in Washington was conducted during August and September 2003 to identify the prevalence of and changes in immunization programs. Specific programs to be considered were immunization consultation, immunization promotion, out-sourced immunization service, pharmacist-administered immunization service under a collaborative drug therapy agreement protocol and pharmacist-administered immunization service pursuant to prescribers’ order. A follow-up telephone survey with nonrespondents was conducted during late September and October 2003 to examine nonresponse bias. Results: Results were based on the returned postcard-length survey. Of the 1,143 survey packages sent, 2 were undeliverable; 328 (28.7%) were returned. Of the returned surveys, 315 were usable. Results show that more than 50% of pharmacies reported that their pharmacies were involved in immunization consultation and promotion activities. Approximately one third of the respondents reported that their pharmacies provided pharmacistadministered immunization service under a protocol. Almost 30% of pharmacies were involved in an out-sourced immunization service and vaccine administration for patients with prescription orders. Additionally, there is an increasing trend for all immunization programs, except for out-sourced immunization service. Conclusions: Pharmacy-based immunization programs, including consultation/promotion activities and delivery services are important to the community as they help increase immunization rates. Washington State pharmacists are actively involved in these immunization activities. Further research is needed to examine reasons why pharmacies offer (or do not offer) immunization delivery service, to facilitate greater pharmacy/pharmacist involvement in this practice. Original Citation: Chamnanmoh S, Mount JK, Rochon J. Pharmacy-based immunization programs in Washington State. Poster presentation at the Washington State Public Health Association 10th Annual Joint Conference on Health, Yakima, Wash., October 13–15, 2003. 255—PHYSICIAN ADAPTABILITY TO HANDHELD COMPUTER USE: A PATH ANALYSIS OF CORRELATES WITH EXPECTED BEHAVIORS. Siracuse M, Galt K, Clark B, Rule A, Taylor W, Creighton University. E-mail: [email protected] Objective: The objective was to determine human factors (attitudes, beliefs, and abilities) assowww.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 256—PHYSICIAN ATTITUDES TOWARD DIRECT-TO-CONSUMER ADVERTISING OF PRESCRIPTION DRUGS: A CONTENT ANALYSIS OF OPINION-BASED PUBLICATIONS. Zhang D, Carlson A, University of Minnesota. E-mail: [email protected] Objective: Increases in spending on direct-toconsumer advertising (DTCA) have coincided with a sharp rise in the number of prescriptions being written and in spending on prescription drugs. Although the physicians’ role in prescribing is central, only a few studies have attempted to identify physician attitudes toward the value and effect of DTCA on the patient care process. The objective of this study was to: (1) identify physician attitudes toward DTCA of prescription drugs using opinionbased articles published in professional journals and other mass media sources and (2) compare these published opinions with the results of two very recent surveys of physicians regarding DTCA. Methods: Opinion-based publications such as letters to the editor, editorials, comments, controversies, or manuscripts that present information about DTCA without original data collection were identified using MEDLINE, CINAHL, and Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 International Pharmaceutical Abstracts supplemented by hand search of secondary references. Articles must be published after 1985 and have at least one physician (with MD or DO degree) as an author. Content analysis was used to group statements about the influence of DTCA on patient and physician behaviors into relevant themes. Results: A total of 40 eligible publications have been identified, and 29 have been reviewed. Eight (27.6%) expressed positive views of DTCA, and 21 (72.4%) expressed negative views. Some 94 statements have been catalogued and grouped into five positive and eight negative themes. Positive themes include the educational value to patients and DTCA’s role in improving patient compliance. Negative comments are related to the quality of discussions between physicians and patients and the negative influence of DTCA on the patient–physician trust relationship. None offer evidence that DTCA has contributed to poor patient outcomes. Conclusions: Review of opinion-based literature identifies concerns about DTCA that are supported by results of national surveys of physicians. Evidence connecting concerns with negative patient outcomes is lacking. 257—PREDICTING DISCONTINUATION OF TREATMENT AMONG PATIENTS WITH MULTIPLE SCLEROSIS: AN APPLICATION OF THE TRANSTHEORETICAL MODEL OF CHANGE. Berger B, Auburn University, Hudmon K, University of California, San Francisco, Liang H, Florida Atlantic University. E-mail: [email protected] Objective: To delineate factors associated with discontinued use of Avonex, a medication for treatment of multiple sclerosis (MS), a chronic disease affecting the central nervous system. These factors would serve as a basis for the development of an intervention to promote treatment persistency. Methods: In-depth telephone interviews with 56 patients followed by a 12-page written questionnaire mailed to 946 patients with MS. The Transtheoretical Model of Change provided the theoretical framework for the study. Setting: United States. Participants: 531 completed questionnaires (56%) were returned; 79% were currently using Avonex for treatment of MS. Main outcome measure: discontinuation of Avonex treatment. Results: A series of four key variables accurately identifies 82% of patients who discontinue drug use while also correctly identifying 81% of patients who stay on the drug. These variables are pros of Avonex use, cons of Avonex use, highest level of education completed, and level of disability. Conclusions: Constructs from the Transtheoretical Model of Change were effective in differentiating patients who had discontinued their Avonex treatment versus patients who continued treatment. This behavioral model likely would be an effective framework for a medication persistency software intervention program that would be stage and patient specific. 258—PREDICTING THE TREATMENT OF MENTAL HEALTH PROBLEMS–COMPARISONS BETWEEN LOGISTIC REGRESSION AND CHAID MODELS. Lin S, Tan H, University of Illinois at Chicago. E-mail: [email protected] Objective: The objectives are to (1) estimate the prevalence of mental health (MH)–related symptoms, diagnoses and treatments in ambulatory visits made to office-based physicians in the United States, (2) evaluate the discrepancy between symptom reporting and the diagnosis and treatment of MH-related problems, and (3) compare models from traditional logistic regressions and CHAID (classification-tree analysis with the chi-square automatic interaction detection) on their performance to predict and explain the treatment of mental health problems. Methods: Data from the 1997 to 2000 National Ambulatory Medical Care Survey were used for the study. Visits made by adults to primary care physicians or psychiatrists were selected for analysis. Dependent variables were the probabilities to report symptoms and receive diagnoses and treatments of MH-related problems. Independent variables include patient demographics, payment and health plan types, physician specialty, and proportion of MH-related symptoms encountered by each physician. Logistic regressions and Exhaustive CHAID are statistical methods used. Results: A total of 26,043 visits met the inclusion criteria, among them 17% reported at least one MHrelated symptom, 24% were given MH-related diagnoses, and 27% received MH-related treatments. Ten percent of the visits did not report a MH-related symptom but were given a MH diagnosis, and 6% had neither a MH-related symptom nor a diagnosis but were prescribed a MH-related treatment. Results from the logistic regressions indicated that females and whites (as compared with African Americans) were more likely to report symptoms, and to be diagnosed and treated with their MH problems. Compared with visits made by private insured patients, Medicaid visits were not associated with a higher probability to report symptom but were more likely to be diagnosed and received MH-related treatments. Conclusions: MH-related symptoms, diagnoses and treatments were prevalent. Considerable inconsistency was found in diagnosing MH problems and prescribing MH treatments. 259—PREDICTORS OF STUDENT SATISFACTION AND COMMITMENT TO THEIR PHARMACY SCHOOL. Holdford D, Patkar A, Virginia Commonwealth University. E-mail: [email protected] Objective: To test a service quality framework that presents seven educational quality inputs that influence four outcomes and examine the predictive validity of an educational service quality instrument. Methods: Design: Self-administered survey. Instrumentation: A 68-item instrument using a 5point Likert scale was selected to assess seven Journal of the American Pharmacists Association 291 2004 Abstracts of Contributed Papers ciated with the use of computers in general and handheld devices in particular (specifically, personal digital assistants [PDAs]). Methods: The population of study was primary care office-based practice physicians who were new or relatively inexperienced learners of handheld technologies. Our study involved 78 primary care physicians in 32 office-based practices located in the Eastern Nebraska–Western Iowa region. The initial instrument assembled a total of 60 items, with an equal distribution of items requiring a positive or negative response. All of the items were scored on a 5-point Likert scale. The instrument was completed by physicians in their routine office practice setting using self-administered, interviewer-assisted technique. The instrument was administered to the study population after it was piloted on six physicians to confirm face validity and to reduce ambiguity. Results: Of the 78 physicians surveyed, 73% did not use a PDA at work, and only 3% specifically received formal training in the use of PDAs. Exploratory factor analysis resulted in the following eight subscales being identified: (1) emotional reaction toward computers (0.93); (2) learning related attitudes toward computers (0.88); (3) dexterity limitations to computer use (0.77); (4) physical sensory barriers and computers (0.90); (5) beliefs about utility of PDA use in prescribing (0.90); (6) expectations of being slowed down by PDAs (0.84); (7) fear of loss (0.86); and (8) belief that PDAs increase efficiency (0.84). Conclusions: Path analysis will be done to analyze the association between the aforementioned subscales and physician attitude regarding current and future use of handheld devices. Ultimately, the association between successful adaptation to handheld technology by individual physicians and human factors will be determined. FEATURE FEATURE Annual Meeting Abstracts 2004 inputs (i.e., service quality, courses, student friendships, faculty friendships, workload, perceived accomplishment, and student organizations) and four outcomes (i.e., overall satisfaction, school commitment, perceived value, and willingness to serve). Participants: Pharmacy students in their final year of school before graduation (P-4). Data collection: Four graduating classes of students (2000 to 2003) at an Southeastern University were surveyed during P-4 clerkships. Data Analysis: Descriptive and regression analyses were conducted. Results: Four separate stepwise models showed substantial explanatory power of overall satisfaction (73%), school commitment (42.4%), perceived value (50.5%), and willingness to serve (33.6%). Five of the seven educational quality inputs in the proposed framework had a significant impact on at least three of the four outcomes. Service quality had the greatest impact on overall satisfaction (R2 = .619) and school commitment (R2 = .307). Courses had the greatest impact on perceived value (R2 = .384) and willingness to serve (R2 = .200) and significant influence on overall satisfaction (R2 = .101) and school commitment (R2 = .064). Other important predictors were student organizations, faculty friendships, and academic accomplishments. Student friendships had no impact on any outcome, and workload had marginal impact on perceived value. Conclusions: This research demonstrates that student perceptions of the school are based upon a broad range of educational inputs including but not limited to service quality. Most important are the courses and the way they are delivered. Extracurricular activities such as participation in student organizations and interactions with faculty also influence perceptions. 260—RANDOMIZED TRIAL OF A PHARMACIST CONSULTATION PROGRAM FOR FAMILY PHYSICIANS AND THEIR ELDERLY PATIENTS: 17-MONTH FOLLOW-UP. Sellors C, Kaczorowski J, Sellors J, Goeree R, Dolovich L, Willan A, Woodward C, Howard M, Blackhouse G, McMaster University. E-mail: [email protected] Objective: To report the longer term (17 months) health and economic impacts of the Seniors Medication Assessment Research Trial (SMART). Methods: The study was a pairedcluster, randomized, controlled trial. A total of 48 randomly selected pair-matched physicians and 889 of their randomly selected senior patients taking five or more medications participated and were randomized to the intervention (pharmacist consultation) group (N = 24) or the control group (N = 24). For each senior in the intervention group, a pharmacist completed a medication assessment, then discussed the written recommendations with the physician. Outcomes included health care and medication utilization and costs determined by administrative databases, control of blood pressure (BP), blood glucose, glycosylated hemoglobin, and cholesterol (by chart audit), medication appropriateness measured by a published tool, and quality of life. 292 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Analyses are based on the 12 months (phase 2) after the 5-month intervention period and took account of the cluster design. Results: A total of 779 seniors (374 intervention group, 405 control group) participated in phase 2. Seniors in both groups were 74 years of age on average, and approximately two thirds were female. Pharmacists identified 1,093 drug-related problems in the intervention group. During the 12 months of phase 2, seniors in the intervention and control groups filled a similar average number of prescriptions (34.6 versus 33.9, respectively, P = .81), and had a similar number of hospitalizations (0.27 versus 0.33, respectively, P = .38). The total average cost (including the pharmacist consultation in that group) in the intervention and control groups over the 12 months was $5,042.72 versus $4,781.49, P = .67. The proportions of seniors with hypertension, hypercholesterolemia, and diabetes, who had uncontrolled (including an absence of any readings in the chart) BP, cholesterol, and blood glucose were high in both groups (58%–95%), and were not statistically significantly different between groups after taking account of baseline group imbalances. Conclusions: The one-time pharmacist consultation intervention did not result in changes in health care utilization or clinical management of hypertension, diabetes, or hyperlipidemia, but demonstrated a need to address drug-related problems and a successful collaboration process between pharmacists and physicians. Original Citation: Canadian Association for Population Therapeutics, Quebec City, Quebec, Canada, March 31, 2003. 261—RATES AND IMPLICATIONS OF DRUG COST IMPUTATIONS IN THE MEDICARE CURRENT BENEFICIARY SURVEY. Mott D, Kreling D, Chou C, University of Wisconsin–Madison. E-mail: damott@pharmacy. wisc.edu Objective: The objectives of this study were to examine trends in the rates of statistical imputation for drug cost data in the MCBS data, determine how those rates vary by drug coverage source, and explore potential implications of those imputations on resulting drug cost and out-of-pocket cost estimates. Methods: Data on prescription drug use and spending for persons age 65 and older from the Medicare Current Beneficiary Survey (MCBS) Cost and Use Files from 1994 to 1999 were used. A variable identifying whether drug cost information for prescribed medicine events was statistically imputed was used to track rates of imputation. The effects of statistical imputation were examined with data from 1994 by comparing summary cost variables calculated using all prescribed medicine events, using only prescribed events that did not have imputed costs and using prescribed medicine events only for persons with no imputed medicine events. Results: The general trend for out-of-pocket was an increase in the rate of statistical imputation each year. The least amount of imputations occurred among the no coverage group. In terms of total spending, the rates of statistical imputation were more consistent across the years, and lower than those for out-of-pocket costs except for the Medicaid-covered group. Imputation effects on estimates of drug use and cost occurred when prescriptions with imputation were removed or persons with imputation were removed. Conclusions: Variation in rates of statistical imputation for drug cost information in the MCBS data among seniors with different drug coverages, a trend toward more statistical imputations over time, and higher amounts of out-of-pocket cost and drug costs in cases of imputation suggests caution is warranted by users of these data and the results of studies based on these data. 262—RESORPTIVE DRUG USE PATTERNS AMONG MINNESOTA FEMALES: RESULTS OF A STATEWIDE SURVEY. Farley J, Cline R, University of Minnesota, Hansen R, University of North Carolina at Chapel Hill. E-mail: [email protected] Objective: A number of drugs (referred to as resorptive medications) including antiepileptics, loop diuretics, and corticosteroids can reduce bone mineral density in users and ultimately increase their risk of osteoporosis. Although the use of resorptive medications can positively affect the health of users, few studies have examined their prevalence or predictors of use. Primary objectives were to (1) establish the prevalence of use of resorptive medications in Minnesota women aged 45 or older and (2) describe factors associated with resorptive medication use. Secondary objectives were to explore the occurrence of osteoporosis and osteopenia as well as the use of newer antiresorptive medications, calcium, and hormone-replacement therapy (HRT) among women using resorptive drugs. Methods: Design: Secondary data analysis of a cross-sectional mailed survey. Instrumentation: 75item questionnaire with 5 sections including health belief model constructs, medication profiles, and demographics. Participants: Survey forms were mailed to 1,700 community-dwelling women aged 45 and older residing in Minnesota. Analyses: Chisquare analysis and logistic regression were used to test bivariate and multivariate relationships between demographic variables, health characteristics, resorptive medications, and use of newer antiresorptives, calcium, and HRT. Results: A total of 990 usable survey forms were returned (adjusted response rate of 61.1%). Eightyfour respondents (8.5%) reported use of a resorptive medication. Age, health status, and health care utilization (monthly physician visits and prescription use) were all associated with resorptive medication use, controlling for other variables in the model. Women using resorptive drugs were more likely to report osteopenia or osteoporosis, were more likely to report using an antiresorptive medication but were not more likely to report using HRT or calcium. Conclusions: Resorptive medication use was common among respondents and was correlated with diagnoses of osteoporosis or osteopenia. www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 Identification of risk factors such as health status, health care utilization, and age may be helpful to clinicians targeting interventions of women using resorptive medications. 264—SURVEY OF PHARMACY STUDENT WORK EXPERIENCE. Siracuse M, Creighton University, Schondelmeyer S, Hadsall R, Schommer J, University of Minnesota. E-mail: [email protected] Objective: The objective of this study was to survey pharmacy students to determine the type of pharmacy work environments they have experiVol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 265—TALKING TO PHARMACISTS ABOUT DIABETES: HOW TO ASK ABOUT MONITORING CLINICAL TARGETS. Guirguis L, Chewning B, University of Wisconsin–Madison. E-mail: lmguirguis@ pharmacy.wisc.edu Objective: To (1) discuss the development of an interview instrument to assess community pharmacists’ use and beliefs about clinical targets such as blood glucose, cholesterol levels, and blood pressure, for their patients with diabetes and (2) present pharmacist perceptions of outcome monitoring in response to pilot questions. Methods: Twelve pharmacists were asked to participate in one of four stages of the development of a paper instrument for face-to-face interviews: (1) developmental interview, (2) behavioral item pretesting, (3) subjective item pretesting, and (4) cognitive testing. Results: In the developmental interview, pharmacists used medications rather than patients to recall routine interactions with patients, talked about clinical targets primarily when changes occurred, and had differing reasons for asking about blood sugars. In the development of behavioral items, pharmacists found it easier to describe a recent interaction with a patient when they named the product involved. They asked routine questions about whether patients had any concerns instead of asking about clinical targets and used estimation to report how often they asked about clinical targets. Because so few pharmacists monitored clinical outcomes, it became important to structure the interview to minimize respondent embarrassment by allowing them to comment on the busyness of their practice and their usual questions to patients prior to questions regarding rates and importance of asking about clinical targets. Conclusions: The combination of a developmental interview, pretesting, and cognitive testing helped create a detailed interview to understand how and why pharmacists do or do not talk to patients with diabetes about clinical targets. 266—THE SPREAD AS A SOURCE OF PBM REVENUE. Clark B, Creighton University, Garis R, Creighton University School of Pharmacy & Health Professions. E-mail: [email protected] Objective: To conduct a pilot study that develops valid methodology for documenting the spread in drug ingredient cost between what PBMs charge employers and what PBMs pay dispensing pharmacies for the drug ingredient portion of prescription transactions. Spread is defined as the difference between the drug ingredient cost billed to an employer by a PBM and the drug ingredient cost that is paid to the dispensing pharmacy by the PBM on behalf of the employer. Methods: Researchers conducted a retrospective review of two sets of financial records issued by each of two PBMs. These financial records were: (1) line-item prescription transactions billed to employers and (2) line-item transaction data accompanying PBM payment to dispensing pharmacies. Drug ingredient cost amounts billed to employers were compared with the amounts paid to pharmacies for 129 prescription transactions. Nonparametric analyses were used for comparisons of these non–normally distributed outcome variables. Results: Taking both PBMs together, the average spread of $12.29 per prescription ranged from –$1.67 to $201.65. Considering all 129 transactions together, there was a significant difference between brand-name drugs and generics with mean spreads of $4.65 and $23.45 per prescription, respectively. The spread difference between PBMs on generic drugs was suggestive (P < .09). A significant difference between PBMs was found only in the spread percentage charged on brandname drugs (P < .02). Conclusions: For the PBMs and prescriptions analyzed, results indicate dramatic differences in spread and spread percent when comparing generic and brand-name drugs, but essentially no difference between PBMs. Wider ranges in spread opportunities available with generic drugs are, in part, explained by the disparity between generic drug Journal of the American Pharmacists Association 293 2004 Abstracts of Contributed Papers 263—RESPONSE QUALITY OF INFORMATION FROM “ASK THE PHARMACIST” SERVICES ON INTERNET PHARMACY SITES. Nath D, Duquesne University, Holmes E, University of Mississippi, Markuss J, Desselle S, Duquesne University. E-mail: [email protected] Objective: There is concern over the veracity and comprehensiveness of information provided by Internet pharmacy sites. Some sites offer an “Ask the Pharmacist” service whereby consumers E-mail questions to a pharmacist who subsequently returns a response. The objectives of this study are to (1) compare the quality of responses from questions submitted to “Ask the Pharmacist” services among Verified Internet Pharmacy Practice Sites (VIPPS) and non-VIPPS pharmacy practice sites and among standalone, brick-and-mortar chain community, and brick-and-mortar independent community practice sites; and (2) determine if the quality of responses services differ among the sources providing the drug information (i.e., drug information specialist versus community pharmacist). Methods: Design: Content Analysis. VIPPS sites were acquired through the NABP’s current listing of sites provided on www.nabp.org. Other sites are obtained though in a WebFerret 5.0 metasearch engine query. Professional pharmacy students are submitting five drug information questions to each of the pharmacy practice sites sampled using fictitious Internet E-mail accounts. The drug information questions and scoring schemata for each question were developed by a focus group panel comprising pharmacists and academicians who were guided by information from resources typically available to practicing pharmacists. Trained professional pharmacy student judges will score the responses obtained from the sites. Each response will be scored by three judges working independently. Interrater reliability among the judged will be determined from the calculation of intraclass correlation coefficients. Student t tests and analyses of variance with Tukey’s HSD posthoc tests will be used to determine differences in response quality. Results: A panel of five pharmacists and academicians have developed questions and constructed scoring templates for standard items to assure these met predetermined criteria. Submission of questions has been initiated. Conclusions: All responses will have been evaluated and the analysis completed by the time of presentation. enced and their attitudes towards these experiences. Methods: A total of 533 third-year (in a four-year program) PharmD students from eight colleges and schools of pharmacy in the Midwest volunteered to participate in this study using a written survey. The students were surveyed as a group at their respective institutions. Data collection included demographics, workplace descriptive information, and Likert scales to determine student attitudes toward their work environment. Data cleansing resulted in 509 usable surveys. Statistical analysis included determination of frequencies and means for descriptive data and Likert scale mean item scores for the attitudinal data. Results: Overall, 496 (97.4%) students reported at least one pharmacy work experience. Of these students, the most frequently reported work sites for their most recent or current positions were: 331 (65.0%) in chain pharmacies; 74 (14.5%) in hospital pharmacies; 58 (11.4%) in independent community pharmacies; and 12 (2.4%) in long-term care pharmacies. Overall, students spent most of their time (69.0%) in dispensing, distribution, and compounding activities. Students spent considerably less time in direct patient care/pharmaceutical care (10.5%) activities and providing drug information to patients (11.6%), but not in the same depth that would be expected from a pharmaceutical care consultation. Students spent the least amount of time (4.2%) providing consultative services to other health care professionals. Other activities such as cashiering and clerical duties took up 4.7% of student time. A 5-point Likert scale used to analyze student attitude toward resulted in: 390 (78.6%) students either agreed or strongly agreed their current work experience was favorable; 290 (58.6%) students either agreed or strongly agreed they would have a fulfilling career working in a pharmacy that is similar to their current work experience. Conclusions: NA. FEATURE FEATURE Annual Meeting Abstracts 2004 acquisition cost and the published generic AWP. Results presented, and their statistical significance in this small sample, have severe limitations clearly associated with the extremely limited number of prescription transactions and PBMs studied. 267—THE ECONOMIC BURDEN OF HYPERPHOSPHATEMIA-RELATED ENDSTAGE RENAL DISEASE IN FLORIDA MEDICAID PATIENTS. White A, University of Florida, Odedina F, Florida A&M University. Email: [email protected] Objective: The purpose of this study was to determine whether end-stage renal disease (ESRD) associated with hyperphosphatemia had a significant impact on health care costs from a third party payers’ perspective. Study objectives were to: (1) describe the characteristics of these patients in terms of demographics, comorbidities, and utilization, (2) evaluate the primary cost drivers in the treatment of these patients, and (3) assess the economic burden associated with treating hyperphosphatemia-related ESRD patients. Methods: Retrospective study using secondary data from the Florida Medicaid database provided by the Agency for Health Care Administration. Patient inclusion criteria consisted of recipients taking either Renagel or Phoslo, verification of continuous eligibility, time period of July 1, 1999 to December 31, 2002 (July 1 through December 31, 1999, was a washout period). Patient exclusion criteria consisted of diagonosis of with HIV or hemophilia. Data frequencies were examined using regression and quarterly trend analyses. Results: Results of the cost analysis showed that patients with hyperphosphatemia-related ESRD impose an economic burden of $228 million. Facility claims expenditures represented the largest proportion of increase in total direct costs, increasing from $56 million in 2000 to $78 million in 2002. Results showed that the major cost driver for 2000–2002 in the treatment of hyperphosphatemiarelated ESRD among Medicaid patients was dialysis center visits with a total cost of $95 million, followed by general hospital visits with a total cost of $92 million, and prescription medication with a total cost of $11 million. Health care for the study population was most often used through facility visits (78.1%), followed by pharmacy-related services (17.2%), and then medical services (4.7%). Based on medical claims utilization patterns, ambulance service contributed the most to health care utilization by patients with hyperphosphatemia-related ESRD (8.7%), followed by recipient home visits (3.3%) and inpatient visits (2.1%). Facility claim utilization was dominated by dialysis center visits (48.5%), followed by general hospital visits (43.3%) and lastly nursing home visits (7.4%). Conclusions: This study has shown that health care costs for this population of patients had a substantial impact on the Florida Medicaid budget. Additional efforts should be undertaken to further enhance the diagnosis, treatment, and recovery of these patients. 294 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 268—THE EFFECT OF DIRECT-TO-CONSUMER ADVERTISING ON PRESCRIPTION DRUG USE AMONG THE INSURED. Hansen R, University of North Carolina at Chapel Hill, Schommer J, Cline R, University of Minnesota. Email: [email protected] Objective: Direct-to-consumer advertising (DTCA) has become a common promotional technique among the pharmaceutical industry. The relative effect of DTCA on prescription drug utilization and spending is unknown, in part because of the effect of insurance on consumers’ marginal cost. The objective of this study was to determine if the effect of DTCA is moderated by cost-sharing incentives among insured individuals. Methods: Design: retrospective cohort study. Study population: 396,500 employees and dependents with employer-sponsored health insurance continuously enrolled in a contributing plan during July 1997 through December 1998. Data: Personlevel enrollment and claims data were provided by MEDSTAT MarketScan. DTCA data were provided by Competitive Media Reporting (CMR) and linked to the MEDSTAT enrollment files by metropolitan statistical area. Analysis plan: Localized DTCA levels for one class of medication were evaluated and matched with prescription claims for MEDSTAT contributors residing in one of 47 defined advertising markets. Product use within the advertised medication class was evaluated by the intensity of the advertising campaign for various types and levels of cost-sharing incentives, controlling for health status and other covariates. Results: The effectiveness of DTCA was modified by the type and amount of beneficiary out-ofpocket payments for provider visits and prescription drugs. Significant relationships were observed for use of the advertised product as well as its competitor. When high levels of DTCA were present, increased product use of the advertised product was observed for those with high provider out-of-pocket costs, and decreased use was observed among those with high prescription costs. Conclusions: Insured individuals may respond differently to DTCA, depending on the type and level of cost-sharing incentives employed by their insurance plan. More research is needed in this area to verify the findings of this study and explore the interactive effects of insurance coverage and pharmaceutical promotion. 269—THE EFFECT OF DIRECT-TO-CONSUMER AD CONTENT ON BELIEF TENACITY: A STUDY OF APPEALS, ARGUMENT TYPES, AND JUDGMENTS. Jalnawala N, University of Mississippi, Wilkin N, University of Mississippi Medical Center. E-mail: nekshanj@ olemiss.edu Objective: This study was conducted to evaluate the usefulness of inoculation theory (sidedness of appeals) and theory of belief formation (argument types and judgments) in understanding belief tenacity. Direct-to-consumer advertisements (DTCAs) and negative experiences were used to study these theories. Methods: A 2 (one-sided versus two-sided) × 2 (causal versus authoritative) factorial study design was employed. A total of 263 undergraduate students were nonsystematically assigned to view one of the four mock influenza medication advertisements and complete a questionnaire. Subjects were then presented with a negative scenario and were asked to fill out a questionnaire based on the information in the ad and in the negative scenario. The dependent measures included belief change, change in purchase intent and standardized price change. Data were analyzed using two-way analysis of variance. Results: Subjects exposed to two-sided appeals showed lower belief change, standardized price change, and change in purchase intent following a negative experience than subjects exposed to onesided appeals (P < .05). No significant difference was found between subjects who received causal and authoritative arguments. A significant interaction effect was observed between sidedness of appeal and argument type on initial belief and initial purchase intent. Belief change was correlated with the change in information reliability (r = .525, P = .01) and the change in information relevance (r = .583, P = .01). Changes in relevance and reliability also were significantly greater in those subject exposed to one-sided appeals (P < .05). Conclusions: Some support for aspects of inoculation theory and theory of belief formation was found. The findings suggest that complying with the “fair-balance” requirement may be beneficial to pharmaceutical marketers as two-sided appeals increase the tenacity of consumers’ beliefs. Higher initial belief and purchase intent when causal arguments are used in two-sided promotional messages suggest that evidence-based advertising may result in enhanced beliefs about the merits of advertised products (P < .05). 270—THE EFFECTS OF PHARMACISTS’ POSITIONS ON EMPOWERMENT AND ORGANIZATIONAL BEHAVIORS. Kahaleh A, Ohio Northern University, Gaither C, University of Michigan. E-mail: [email protected] Objective: To assess the impact of pharmacists’ position on antecedents and consequences of psychological and structural empowerment. Methods: The study has a cross-sectional design. Self-administered questionnaires were mailed to a national random sample of 1,200 licensed pharmacists. Descriptive statistics, reliability and validity tests, analyses of variance, and path analyses using structural equation techniques (SEM) were used to analyze the data. The theoretical model examines the effects of need for achievement and power factors on psychological and structural empowerment that in turn affect loyalty, organizational commitment, identification, and job turnover intention. Power factors are structural elements that enhance empowerment. Psychological empowerment is defined as the affective state that individuals must experience for managerial interventions to be successful. It has four dimensions: meaning, competence, self-determination, and impact. Structural empowerment is defined as having access to knowlwww.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 edge, resources, opportunity, and support in an organization. Results: Findings of ANOVA showed that managers had significantly higher levels of psychological and structural empowerment. They had significantly higher levels of competence, self-determination, and impact. Similarly, they had significantly higher levels of opportunity, knowledge, support, and resources. Although SEM revealed similar patterns, there were differences between managers and staff pharmacists. Power factors had stronger effects on psychological and structural empowerment among staff pharmacists compared with managers. Also, working in management positions resulted in significant impacts of psychological empowerment on commitment. Similarly, loyalty and commitment had stronger impact on job turnover among staff pharmacists in comparison with managers. Conclusions: Consistent with other studies in the business and nursing literature, managers had higher levels of psychological and structural empowerment. Managers are more likely to have autonomy, confidence in their skills, and control over what happens in their departments than staff pharmacists. Administrators may strengthen their relationships with staff pharmacists by increasing their level of empowerment. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 272—THE EXPERIENCE OF COMMUNITY PHARMACISTS WITH MEDICATION INTENDED FOR USE IN PRIMARY AND SECONDAY SCHOOLS. Reutzel T, Holtorff M, Midwestern University Chicago College of Pharmacy. E-mail: [email protected] Objective: The purpose of this research was to observe the degree to which community pharmacists are aware of and involved in issues related to the use of medications in primary and secondary schools and to identify the interventions they use to deal with these issues. Methods: A short questionnaire was mailed to a random sample of 3,333 Illinois pharmacists selected from the Illinois Department of Professional Regulation roster of registered pharmacists. Subjects with current or recent (within the last year) community pharmacy experience were asked to return a completed questionnaire. A total of 569 returned questionnaires met inclusion criteria and were used in the research (a 17% overall response rate and a 34% estimated community pharmacist response rate). Results: Almost all subjects (97%) reported that they have dispensed medications for use in school, and two-thirds thought taking medications at school creates the potential for special problems (e.g., missed dose, social stigma). Of nine interventions that could help minimize these problems, respondents used an average of 3.33. The most common intervention (used by 94% of subjects) was providing separate, labeled containers for school. Respondents who believed medication use in school causes special problems used significantly more interventions than those that did not think so. Conclusions: This is the first study of pharmacists’ views on this important area of drug therapy. The results show that many pharmacists are aware of and involved in this phenomenon and make use of interventions available to all community pharmacists. Still, pharmacists overall could do much better, and further efforts to raise their awareness levels are warranted. For example, colleges of pharmacy might wish to develop student interest in this important area of drug therapy by providing more coverage of it within and outside the curriculum. 273—THE IMPACT OF ANTIDEPRESSANT EDUCATION AND MONITORING BY COMMUNITY PHARMACISTS ON MULTIPLE CONSUMER OUTCOMES. Rickles N, Long Island University, Svarstad B, University of Wisconsin–Madison. E-mail: nathaniel.rickles@ liu.edu Objective: The study explores the impact of consistent antidepressant education and monitoring by community pharmacists on multiple consumer outcomes. Methods: A total of 63 consumers presenting new antidepressant prescriptions at eight Wisconsin community pharmacies were randomized to receive either three monthly telephone calls from pharmacists providing pharmacist-guided education and monitoring (PGEM) or usual pharmacist’s care. At the end of the 3-month study, consumers reported their antidepressant knowledge, beliefs, frequency of patient feedback with pharmacist (FPFP), orientation toward treatment progress (OTTP), and antidepressant adherence at 3 months. To evaluate improvement in depression, consumers completed a Beck Depression Inventory-II (BDI-II) at baseline and at the end of the study. Pharmacy and health system records were used to objectively measure antidepressant adherence during and 3 months after the study. Data were analyzed using descriptive statistics, analysis of variance, chi-square, linear and logistic regressions. Results: Overall, 60 consumers completed the study: 28 received PGEM and 31 received usual pharmacist’s care. PGEM had a significant and positive impact on the consumer’s antidepressant knowledge (P ≤. 05), beliefs (P ≤ .01), FPFP (P ≤ .001), OTTP (P ≤ .001), and adherence at 6 months (P ≤ .05). PGEM did not have a significant impact on either adherence at 3 months or improvement in depression. Multivariate analyses indicated that (1) antidepressant knowledge (P ≤ .05) and beliefs (P ≤ .001) are significant predictors of adherence at 3 months, (2) consumer’s education (P ≤ .01) and adherence at 3 months (P ≤ .01) were significant predictors of improvement in depression, (3) antidepressant beliefs (P ≤ .05) and adherence at 3 months (P ≤ .001) were significant predictors of adherence at 6 months, and (4) FPFP mediated the relationship between PGEM and the patient’s OTTP. Conclusions: This is the first experimental study to demonstrate that antidepressant education and monitoring by community pharmacists can have a significant impact on the consumer’s antidepressant knowledge, adherence, FPFP and OTTP, pharmacists can also have a significant and sustainable impact on antidepressant adherence by facilitating more positive antidepressant beliefs. More research is needed using larger and more diverse samples to explore how collaboration between prescribers and community pharmacists impact consumer outcomes. 274—THE PROVISION OF CARE AND RETIRED OHIO PHARMACISTS. Birdwell S, NA. E-mail: [email protected] Objective: This study assessed attitudes and perceptions of retired pharmacists regarding an increased level of care and identified aspects of pharmaceutical care that were provided. Methods: A questionnaire was sent to a random sample of 171 retired pharmacists registered in Ohio. The questionnaire measured attitudes and perceptions toward provision of an increased level of Journal of the American Pharmacists Association 295 2004 Abstracts of Contributed Papers 271—THE EFFECTS OF WORK SETTING ON PHARMACISTS’ EMPOWERMENT. Kahaleh A, Ohio Northern University, Gaither C, University of Michigan. E-mail: a-kahaleh@ onu.edu Objective: To assess the impact of work setting on pharmacists’ psychological and structural empowerment. Methods: The study has a cross-sectional design. Self-administered questionnaires were mailed to a national random sample of 1,200 licensed pharmacists in United States. Descriptive statistics, reliability and validity tests, and analyses of variance were used to analyze the data. Psychological empowerment is defined as the affective state that individuals must experience for managerial interventions to be successful. It has four dimensions: meaning, competence, self-determination, and impact. Structural empowerment is defined as having access to knowledge, resources, opportunity, and support in an organization. Results: Results of the analyses of variance revealed that significant differences in the levels of empowerment among independent, chain, and hospital pharmacists. Results of the analyses showed that pharmacists who worked in independent settings had significantly higher levels of psychological and structural empowerment than those who worked in chains or hospitals. Specifically, pharmacists who worked in independent settings had significantly higher levels of self-determination and impact than those who worked in chains or hospitals. In the same vein, those who worked in independent settings had significantly higher levels of knowledge and support than did their counterparts in chain or hospital settings. Conclusions: Managers in independent settings appears to foster a more empowering work environment than did those in chain or hospital settings. Pharmacists in independents described their work environment as a low-stress setting due to having adequate personnel. Administrators may enhance the quality of work life for pharmacists in chains and hospitals by empowering them through increasing their participation in the decision-making processes and their access to knowledge, support, and opportunity in their organizations. FEATURE FEATURE Annual Meeting Abstracts 2004 care and provision of various services associated with pharmaceutical care. Results: The majority of respondents indicated that they did not know if automation assisted in the provision of an increased level of care but agreed that technology did assist in the provision of an increased level of care. Respondents disagreed that incentives were used to provide an increased level of care and that inadequate personnel and high workload pressures prevented the provision of an increased level of care. While the majority agreed that they had the appropriate amount of information, the majority indicated that they lacked the confidence to obtain needed additional information. The majority agreed that pharmacist should provide clinical services, advice on medications, and immunizations and disagreed that an increased level of care would have been provided if properly reimbursed and that physicians in their area disapproved of spending more time with patients. The majority worked in an organization that kept patient profiles and screened for problems with medications and allergies and sometimes or always developed patient-specific education programs; however, many respondents indicated that the profile did not include the pregnancy or breast-feeding status. Conclusions: The respondents in this study agreed that pharmaceutical care is necessary and many of the services associated with pharmaceutical care were provided. Many respondents lacked the confidence needed to obtain needed additional information; therefore, educational programs should consider the age of the target group and provide the necessary tools for providing the appropriate services. 275—THE RELATIONSHIP BETWEEN ADHERENCE TO ANTIDEPRESSANT CLINICAL GUIDELINES AND DIABETES MEDICATION ADHERENCE AMONG MANAGED CARE ENROLLEES. Chao J, University of Michigan, Nau D, University of Michigan, Aikens J, University of Michigan. E-mail: [email protected] Objective: The objectives of this study were to: (1) determine the proportion of patients with diabetes within a managed care organization who received an antidepressant medication; (2) examine the adequacy of antidepressant use among patients with diabetes; and (3) examine the relationship between adequacy of antidepressant use and oral antihyperglycemic medication adherence. Methods: Administrative claims data were extracted from a managed care database for January to December 2001 to identify patients who used oral antihyperglycemic medications, indicating a diagnosis of diabetes. Based on Agency for Healthcare Research and Quality guidelines for treatment of major depression, the adequate use of antidepressants in the acute phase was defined as filling at least 90 days of therapy during the 118 days from the first antidepressant fill, while adequacy in the long-term phase was filling at least 120 days of therapy within 155 days of the initial fill. The medication possession ratio (MPR) for antihyperglycemic 296 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 medications was compared among patients with adequate use of antidepressants, those with inadequate use of antidepressants, and those who did not receive an antidepressant. Results: Among 2,027 patients who used oral diabetes medications, 497 (24.5%) had at least one claim for an antidepressant medication. Of the 497 patients who used an antidepressant, 295 (59.4%) received an adequate trial of medication for the acute phase, while 269 (54.1%) met the adequacy criteria for the long-term phase of treatment. Patients with inadequate use of antidepressants had a mean antihyperglycemic MPR that was significantly lower than patients with adequate antidepressant use, as well as significantly lower than those diabetes patients without antidepressant use. Conclusions: Many patients with diabetes and depression may not receive adequate medication therapy for depression. Inadequate treatment for depression among patients with diabetes was associated with lower antihyperglycemic medication adherence. 276—THE RELATIONSHIP BETWEEN WANTING AND DOING: THE EFFECTS OF GOAL COMPATIBILITY ON CONSUMERS’ RESPONSES TO PRESCRIPTION DRUG ADVERTISING. Sumpradit N, Ascione F, University of Michigan, Bagozzi R, Rice University. E-mail: [email protected] Objective: The aim was to determine how directto-consumer advertising (DTCA) of prescription drugs motivates consumers to take particular actions, based on the combined framework of selfregulatory focus and self-construal orientation. Selfregulatory focus posits that behavior is regulated by two systems: promotion (emphasizing achievements) and prevention (emphasizing safety/obligations). Self-construal orientation suggests that behavior is guided by two self-views: independentself (emphasizing self-fulfillment/uniqueness) and interdependent-self (emphasizing family/social relationships). The independent-self emphasizes selffulfillment and therefore is compatible with promotion focus. The interdependent-self emphasizes maintaining relationships and avoiding mistakes and therefore is consistent with prevention focus. First, we hypothesized that goal-compatible advertisements would lead to more favorable advertisement/brand attitudes, greater intention-to-act, greater likelihood-of-action, higher perceived drug benefits, and lower perceived drug risks. Second, we hypothesized that prevention-focused advertisements would elicit better risk information recall and more negative emotional responses to the advertisement. Conversely, promotion-focused advertisements would elicit more positive emotional responses to the advertisement. Methods: A two (independence versus interdependence) × two (promotion versus prevention) factorial design was used. A random sample of 220 women aged 40 years or older was randomly assigned to view a mock antihyperlipidemia drug advertisement and completed a questionnaire. Main outcome measures included advertisement/brand attitudes, intention-to-act, likelihood-of-action, per- ceived drug benefits and risks, emotional responses, and risk information recall. Data were examined using analyses of variance/covariance. Results: Results partially supported the hypotheses regarding goal-compatibility and emotional responses to the advertisement. Surprisingly, results for risk information recall were in the opposite directions to those hypothesized. Subgroup analysis showed that positive/neutral DTCA-attitude individuals reacted to goal-compatible advertisements consistent with our predictions, whereas negative DTCA-attitude individuals reacted to the same message in the opposite directions to what we predicted. Conclusions: The motivational themes in DTCA affect consumer behavior. The impact is a function of the interaction between the themes and the preexisting beliefs and attitudes of the consumer. 277—THE ROLE OF INFORMATION RELEVANCE AND RELIABILITY IN DIRECTTO-CONSUMER ADVERTISING. West D, University of Arkansas for Medical Sciences, Bentley J, Wilkin N, University of Mississippi Medical Center. E-mail: westdonnas@ exchange.uams.edu Objective: To describe patients’ judgments of information relevance and reliability with respect to direct-to-consumer advertising (DTCA) and to examine the role of information relevance and reliability judgments in persuasion. Methods: Patients at community pharmacies in a southern state were randomly selected; a total of 118 people participated in the study. Upon agreement to participate, each patient was asked to complete a self-administered questionnaire. The questionnaire included four DTCAs, specifically ones for Avandia, Zyrtec, Lipitor, and Prevacid. The questions following each advertisement measured persuasion, information relevance, information reliability, likelihood of asking a physician about a medication, and demographics. Summated scale scores were used as measures of information relevance, information reliability, persuasion, and likelihood of asking for the medication. Descriptive statistics were calculated. Multiple regression was then used to determine the relationship between relevance and reliability and persuasion. Results: The investigators used multiple regression to test the relationship among persuasion, information reliability, and information relevance, controlling for demographics (race, age, gender) and medication use variables (heard of medication, use/used medication, use medication in the therapeutic class). Persuasion was the dependent variable. For each DTCA, multiple regression yielded a significant model with information reliability and/or information relevance as predictors in the model. The findings indicated that consumers are more likely to be persuaded as they deem the information to be relevant and reliable. The model is supported in the DTCAs of Lipitor, Prevacid, and Zyrtec. Conclusions: The results of this study provide insight into the role of judgments of relevance and reliability in persuasion. Regardless of a person’s demographics or past experience, judgments of relwww.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 evance, and reliability significantly predict persuasion. Understanding these relationships will provide a better understanding of how to design promotional pieces and how to manipulate information relevance and reliability to influence persuasion. 279—TREATMENT PATTERNS AND COSTS FOR AFRICAN AMERICAN PATIENTS WITH TYPE 2 DIABETES WHO ARE POORLY CONTROLLED ON ORAL HYPOGLYCEMIC AGENTS AT BASELINE. Ernst F, Eli Lilly and Company, Coons S, University of Arizona, Hayes C, Eli Lilly and Company, Draugalis J, University of Arizona, Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 280—TRENDS IN PRESCRIPTION COST SHIELDING FOR MEDICARE BENEFICIARIES BY DRUG COVERAGE: 1994 TO 1999. Kreling D, Mott D, Chou C, University of Wisconsin–Madison. E-mail: dhkreling@ pharmacy.wisc.edu Objective: The objective of this study was to examine trends in out-of-pocket costs for seniors and the proportion of total spending that the out-ofpocket costs represented across different sources of drug coverage. Methods: Data on prescription drug use and spending for persons age 65 and older from the Medicare Current Beneficiary Survey (MCBS) Cost and Use Files from 1994 to 1999 were used. Drug coverage source was derived from a summary variable (Medicaid) or a systematic iterative process identifying drug coverage as a part of health insurance coverage for respondents and was classified as Medicaid, Private HMO, Medicare HMO, employer-sponsored, individually purchased, other coverage, and no coverage. To examine the extent of cost shielding we calculated the ratio of out-of-pocket drug costs to total spending per prescription. Results: The percentage of respondents with drug coverage increased between 1994 and 1999 as did the number of prescriptions per person. Seniors with employer-sponsored drug coverage had the largest increase in total spending per prescription across time and seniors with no drug coverage had the largest increase in out-of-pocket costs per prescription across time. Over time, other than seniors with Medicaid drug coverage, seniors with employer-sponsored drug coverage were shielded the most for the cost of their drug use. Conclusions: Overall, between 1994 and 1999 seniors paid a decreasing proportion of total spending for prescription drugs out-of-pocket; however, this trend was mainly due to seniors with employersponsored drug coverage. Closer examination of the differences in benefit structures and cost-sharing provisions and how those differences influence the extent of cost shielding for seniors is an important consideration for potential drug benefit programs under Medicare. 281—UTILIZATION OF SUPPLEMENTAL MEDICINE IN U.S. ADULTS: WHO ARE THE USERS AND WHAT ARE THEY USING? Mazyck-Brown J, Mazyck P, Medical University of South Carolina. E-mail: [email protected] Objective: In recent years, supplemental products have been increasingly used by consumers in the United States, either as alternative or adjunctive therapy. Health care professionals need to engage their patients in open communication about the use of these therapies and remain informed about the potential risks and benefits of these treatments. The objective of this study was to describe the utilization patterns for dietary supplements and nonprescription products in adults in the United States with regard to age, race, gender, and disease state. Methods: The National Health and Nutrition Examination Survey (NHANES) is a populationbased survey designed to collect information on the health and nutrition of the U.S. household population. Data from the NHANES III national survey (N = 20,050) were analyzed and estimates of dietary supplements were determined among patients. Statistical analysis was conducted using SAS. Analysis was conducted on the newly released Journal of the American Pharmacists Association 297 2004 Abstracts of Contributed Papers 278—THEORY OF PLANNED BEHAVIOR AND WOMEN’S DECISIONS ABOUT HORMONE-REPLACEMENT THERAPY. Huston S, Kirking D, Shimp L, University of Michigan, Bagozzi R, Rice University. E-mail: [email protected] Objective: (1) Determine the proportion of women with and without diabetes intending to initiate or continue HRT. (2) Evaluate the relative importance of the modified Theory of Planned Behavior (TPB) variables on HRT intention. (3) Determine if an identity variable “menopause is natural” (MN) increases variance in HRT intention explained. (4) Determine differences in variable influences between current, previous and never HRT users, and women in early or late stages of menopause. Methods: Data were collected via a survey mailed to 821 women with and 1,065 women without diabetes between the ages of 46 and 60 who met specific inclusion/exclusion criteria and were enrolled in a southeastern Michigan health maintenance organization (HMO). Data were analyzed using ANOVA, chi-square, t tests, and multiple regression. Confirmatory factor analysis through structural equation modeling (SEM) verified variable structure. Results: Overall usable response rate was 42.2%. Mean intention to initiate or continue using HRT was 3.27, (1 = extremely unlikely, 7 = extremely likely). There was no significant difference in mean intention between women with and without diabetes overall, but never HRT users with diabetes were significantly more likely to be undecided (chi square 7.2, P = .027) than those without diabetes. Previous users with diabetes were more likely to intend to not use HRT compared with those without diabetes. Model variables explained 67.4% of variance. Attitude (ATT), subjective norm (SN), perceived control over behavior (PCB), and self-efficacy (SE) were all significant. Physicians (independent from SN) were one of the most significant predictors of intention. In all groups SE was positively associated with intention to use HRT and MN was significant, adding 0.5% to explained variance. Interactions were found between HRT status and PCB, ATT, SN, and diabetes status. Conclusions: Study variables do significantly influence HRT decisions. This information can be used to help provide women with targeted information. Ziemer D, Caudle J, Emory University. E-mail: [email protected] Objective: To evaluate 1-year treatment patterns, resource utilization, and costs for African American adults with type 2 diabetes poorly controlled on oral antihyperglycemic agents. Methods: Patients were poorly controlled (glycosylated hemoglobin [A1c] ≥7 %, random plasma glucose [RPG] > 150 mg/dL, or fasting plasma glucose [FPG] > 120 mg/dL) at an index visit to a Grady Health System clinic from July 1999 through June 2000 and were taking oral antihyperglycemic medications. Patients were grouped on 1-year antihyperglycemic treatment patterns. Retrospective demographic, clinical, laboratory, hospital, pharmacy, and provider data were analyzed. Statistical comparisons included ANOVA, t tests, and logistic and multiple linear regression. Results: Of 606 patients, 36% took a sulfonylurea–metformin combination at index and end (SM–SM), followed by 18% taking only sulfonylureas (S–S). The most frequently used treatments also had the longest durations. The S–S and metformin-only (M–M) groups had disproportionately more controlled patients, but improvement was usually small and incremental. Short-term costs and resource utilization varied significantly by treatment group. Treatment patterns, duration of diabetes, body mass index, Charlson Comorbidity Index score, A1c tests, and number of treatment changes were associated with total costs, but overall total costs did not differ by treatment group. Medication costs were greatest for patients receiving combinations, such as SM–SM, and lowest among patients taking S–S. No differences in total hospital, office/clinic visit, or laboratory testing costs were found. Microvascular complication-associated total costs were highest for the SM–SM group and lowest for the M–M group. The treatment pattern groups contributing most to total costs, relative to the least-contributing S–S group, were SM–SM, sulfonylurea–metformin at index and sulfonylurea–metformin–insulin at end (SM–SMI), and then M–M. Conclusions: No optimal treatment pattern emerged, as each had different effects on outcomes and costs. Thus, treatment choice cannot be based on a single comparator, such as glycemic control achievement or cost. Rather, there are multiple clinical and economic effects produced by the choice of one treatment choice over another. Original Citation: Drug Information Association/Agency for Healthcare Research and Quality 5th Annual Workshop on Pharmaceutical Outcomes Research; Tucson, Ariz., January 21–23, 2004. FEATURE FEATURE Annual Meeting Abstracts 2004 1999–2000 NHANES data to determine if utilization rates among U.S. adults have increased since 1988. Logistic regression was performed controlling for age, gender, race and socioeconomic status. Results: Of the 20,050 participants surveyed, 7,381 (37%) stated that they have used vitamin/mineral products within the last month. The mean supplement usage intake was 1.7 products/month. In regard to race, 73% of the participants were Caucasian, 24% African American, and 3% other. Women consumed more vitamin/mineral products than did men (60% versus 40%). When analyzed, by region, the percentage of supplement users was greater in the Southeast. Diseases among the supplemental respondents were unspecified hypertension, unspecified heart disease, fluid overload, and diabetes without complications, unspecified arthropathy, and postmenopausal hormone-replacement therapy. Vitamin C, multivitamins, vitamin E, calcium, and iron were among the vitamins/mineral supplement with the highest usage. Other than those previously stated, garlic, fish oil, chromium, alfalfa, and lecithin were frequently used among the supplement users. Conclusions: Based on the available evidence, adults in the United States commonly report use of dietary supplements products. 282—DIRECT-TO-CONSUMER ADVERTISING OF PRESCRIPTION VERSUS NONPastakia S, PRESCRIPTION DRUGS. Wertheimer A, Temple University. E-mail: [email protected] Objective: The purpose of this article is to analyze the differences in economic implications and impact on patient care between prescription and nonprescription drug advertising to consumers. Methods: The current medical literature was researched using both the Medline and International Pharmaceutical Abstracts databases. Due to a paucity of information regarding nonprescription drugs, consumer groups such as the National Consumer’s League, Consumer Healthcare Products Association, and Kaiser Family Foundation were used to provide data and statistics on the public’s perception of DTCA. Results: The economic statistics describing prescription drug advertising illustrate the vast market share that advertised drugs have (advertised drugs are responsible for approximately 48% of the increase in spending on pharmaceuticals). Studies analyzing patient care have shown that patients have an increased interest in acquiring information on prescription drugs, while inquiries regarding nonprescription drugs have increased at a much lower rate. Patient surveys have also shown patients rely heavily upon the convenience and relief nonprescription drugs provide. Conclusions: All these factors have left patients in a precarious position as they attempt to treat themselves with nonprescription drugs based on the limited information they receive from health care providers and nonprescription drug advertisements. 298 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 283—PREVALENCE OF ANTIDEPRESSANT USE IN CHILDREN AND ADOLESCENTS: WHO PRESCRIBES AND WHAT ARE THE DIAGNOSES? Legorreta A, University of California, Los Angeles, School of Public Health/Health Benchmarks, Inc, Hassan M, West Virginia University, Pharmaceutical Systems and Policy/Health Benchmarks, Inc. E-mail: [email protected] Objective: To determine prevalence trend of antidepressant utilization among children and adolescents and to characterize antidepressant utilization in terms of the patient’s age, gender and medical diagnosis, subclass of antidepressant, and physician prescribing patterns. Methods: Retrospective analysis of all antidepressant prescription claims between 1998 and 2001 of members less than 20 years of age using an employer-based managed care claims data. Prevalence trend was studied by categorizing all claims into four 1-year cross-sectional datasets. Results: Antidepressant prevalence was about 7.2 to 7.6 per 1,000 children and adolescents between 1998 and 2000 but decreased to 5.2 per 1,000 in 2001. Greater proportion of antidepressant users were found in higher age categories. Though depression was the most common diagnosis throughout 1998 to 2001, a considerable proportion of antidepressants were being used for attention-deficit/hyperactivity disorder (ADHD). However, antidepressant users with ADHD had decreased from 19% in 1998 to 12% in 2001. About 63% of children and adolescents receiving antidepressants did not have any record of a psychiatric diagnosis in the claims data. Highest proportion of antidepressant prescriptions were for selective serotonin reuptake inhibitors (SSRIs) followed by miscellaneous antidepressants. Greater number of SSRI and miscellaneous antidepressants were prescribed by psychiatrists, whereas greater number of tricyclic antidepressants were prescribed by pediatricians. Zoloft, Prozac, and Paxil were among the most frequently prescribed antidepressants throughout the 4 years. About 66% of children and adolescents had received antidepressants without any consultation with a psychiatrist. Most of the patients receiving antidepressants without a psychiatric diagnosis (74%) had received the prescription from a nonpsychiatrist. Conclusions: Though the clinical evidence regarding efficacy and safety of antidepressant use among children and adolescents is lacking, antidepressant use is prevalent among this population. Nonpsychiatrists are responsible for a large proportion of antidepressant prescriptions in this population. Such widespread “off label” prescribing of antidepressants by physicians should be monitored. American Society for Pharmacy Law (ASPL) 284—DETERMINANTS OF PATENTING IN THE U.S. PHARMACEUTICAL INDUSTRY BASED ON RECENT CAFC CASE LAW. Rumore M, Scully, Scott, Murphy & Presser. Email: [email protected] Objective: Life-cycle management of pharmaceuticals involves a wide range of patents that may be obtained before as well as after approval of a new drug. The intersection between Hatch–Waxman and patent laws has spawned a great deal of litigation involving “Orange Book” patents. This paper analyzes recent Court of Appeals for the Federal Circuit (CAFC) decisions involving patents on metabolites, polymorphs, purity, off-label uses, dosing regimens, and “submarine patents” and explores ramifications on patenting of pharmaceuticals in the United States. Methods: Various strategies for extending exclusivity for blockbuster drugs have evolved since passage of the Hatch–Waxman law and are discussed herein. One such strategy involves patenting metabolites and listing them in the Orange Book, sometimes on the eve of patent expiration. This strategy worked merely because the ensuing litigation itself was effective in preventing generic competition. Another strategy involves the patenting of polymorphs. Such patents may be listed in the Orange Book without actually being used in the commercial drug product. Recent decisions are of import in future use of these strategies. Results: The decision in Andrx Pharmaceuticals, Inc. v. Biovail Corp. suggests that suits against FDA under the Administrative Procedures Act when FDA has improperly listed a patent is an appropriate mechanism to pursue. Additionally, the decision in Bristol-Myers Squibb Co. v. Mylan Pharmaceuticals Inc. reflects that improper patent listing in the Orange Book may subject the holder of a New Drug Application to enormous liability under antitrust laws. In Schering v. Geneva Pharmaceuticals, the CAFC held that a patent on a drug that does not explicitly describe a metabolite inherently discloses the metabolite if it teaches administration of the drug to the patient and it necessarily follows that the metabolite is formed. In some cases companies are seeking delisting of Orange Book patents to avoid being the target of antitrust lawsuits from states, the Federal Trade Commission, and patients. Conclusions: A unique hybrid of food, drug, and cosmetic law and patent law continues to be carved from recent CAFC decisions. Additionally, FDA’s newly issued regulations on criteria for listing certain types of patents in the Orange Book will have far reaching effects on patenting of pharmaceuticals in the United States. 285—EXTERNAL TAGGING PRACTICES ON OTC MEDICATION PRODUCTS: POTENTIAL RISK AND LIABILITIES FOR PHARMACISTS. Pawaskar M, Sansgiry S, University of Houston, Bix L, Clark R, Michigan State University. E-mail: [email protected] Objective: The objective of this study was to make pharmacists aware of potential risk and liabilities associated with external tagging practices with respect to over-the-counter (OTC) products. The study examined information concealed by antitheft tags and price tags affixed on OTC medication labels. Methods: The study was conducted in two cities www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 286—LEGAL, ECONOMIC AND ETHICAL ISSUES INVOLVING REIMPORTATION OF DRUGS. Djuric M, University of Illinois at Chicago. E-mail: [email protected] The elderly population of the United States is limited in its options to pay for its prescriptions and need other options. Some qualify for programs like Circuit Breaker and Senior Care, which allow for a small copayment for many prescription medications. For the rest of the elderly population that do not qualify for these programs, the choice for some individuals each month is between buying food and buying medicine. As a result of this economic pressure, many people have started to get their prescriptions filled in Canada, where prescription drug prices are lower. Canadian “pharmacies” buy prescription drugs from U.S. pharmaceutical companies and sell them in Canada at lower, governmentfixed prices. U.S. citizens travel to Canada or go through a “pharmacy” in the United States to buy their prescriptions at this lower price. From a legal, economic, and health care standpoint, the reimportation of drugs from Canada to the United States is unacceptable because it is illegal. FDA has not regulated Canadian pharmacies, and therefore safety of products dispensed by them cannot be guaranteed. Most importantly, if this continues, pharmacists in the United States will not be providing pharmaceutical care nor practicing the art and science of pharVol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 macy: they will simply be running an importing business. The solutions provided by lawmakers have included circumventing U.S. authority over importation of foreign drugs by allowing pharmacists and wholesalers to import drugs from Canada, negotiating with health provider plans to reimburse patients for drugs bought in Canada, and fining manufacturers who refuse to sell their drugs to Canadian pharmacies that dispense to U.S. patients. Continuing to allow and even assist the elderly of the United States in getting their prescriptions from Canada is not a solution. Possible solutions to the problem of prescription coverage for the elderly will be presented. 287—MEDICAL ERROR AND THE LAW: LEGAL ISSUES FOR PHARMACISTS IN PERFORMING SAFETY WORK. Liang B, University of Houston. E-mail: baliang@ alum.mit.edu Objective: To determine legal risks for pharmacists performing patient safety and medical error reporting and research. Methods: A review of error reporting statutes, the sentinel event policy of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), peer review/quality assurance privilege law, attorney–client privilege law, Medicare Quality Improvement Organization (QIO) statutes, federal medical privacy law, and mediation confidentiality rules to identify potential holes that may allow patient safety information to be used to support lawsuits rather than be limited to safety efforts. Results: Significant legal risks are associated with participating in medical error reporting and patient safety research. Error reports may be used to sanction providers, JCAHO sentinel event policy information may be discoverable, Medicare QIO laws may allow for broad litigation support, privilege law appears inapplicable to safety information, the federal privacy law may inhibit patient safety research and subject participants to significant penalties, and mediation communications to engage patients in safety efforts are likely not confidential. Conclusions: Significant legal risks are involved in reporting medical error and engaging in patient safety work. Attention to these risks is essential to avoid unintended liability and to encourage patient safety efforts. 288—PHARMACIST PROVISION OF IMMUNIZATIONS: ANALYSIS OF STATE LAWS AND REGULATIONS IN 7 UPPER MIDWESTERN STATES. Chamnanmoh S, Mount J, University of Wisconsin–Madison. Email: [email protected] Objective: (1) To compare laws related to pharmacist provision of immunizations of 7 upper Midwestern States (Indiana, Illinois, Iowa, Michigan, Minnesota, Ohio, and Wisconsin) in terms of their forms (i.e., statutory versus regulatory) and sources, pharmacists’ ability to immunize, scope of laws (i.e., vaccine types and age of recipients), and additional requirements (i.e., training and liability insurance); (2) To explore implications of these laws for immunization delivery service implementation and public health outcomes. Methods: State statutes and regulations from all study states were systematically reviewed. Key informants of the seven state boards of pharmacy were invited for a brief telephone interview using a structured interview format. Five key informants completed the telephone interview, and two others completed it in writing (100% response). Results: Among the selected states, Illinois is the only state that does not allow pharmacists to administer vaccines. Most states had established state statutes allowing pharmacists to administer vaccines before establishing regulations. Two mechanisms for pharmacists to administer vaccines are practicing under a collaborative agreement protocol (Iowa, Michigan, Minnesota, Ohio, and Wisconsin) and administering vaccines pursuant to written prescriptions (Indiana, Iowa, Minnesota, and Wisconsin). Additionally, some states restrict the types of vaccines that may be administered (Iowa, Minnesota, and Ohio) and/or the age of vaccine recipients (Iowa, Minnesota, Ohio, and Wisconsin). Lastly, states also vary greatly in terms of training and liability insurance requirements. Conclusions: States vary widely with respect to the forms of immunization laws and their sources, pharmacists’ ability to immunize, scope of laws and additional requirements. These variations may influence pharmacists’ receptivity to and participation in pharmacy-based immunization services. Further research is needed to examine the effects of state laws on pharmacists’ behaviors and on public health outcomes. This understanding can help policy-makers plan effective strategies for involving pharmacists in addressing immunization-related goals of Healthy People 2010. Original Citation: Chamnanmoh S, Mount JK. Pharmacist provision of immunizations: analysis of state laws and regulations in 7 upper midwestern states. Poster presentation at the Wisconsin Public Health and Health Policy Institute Bi-Annual Conference, Madison, Wis., October 3, 2003. 289—THE DEVELOPMENT OF DIRECTTO-CONSUMER PRESCRIPTION DRUG ADVERTISING REGULATION. Palumbo F, Mullins C, University of Maryland at Baltimore. Email: [email protected] Historically, prescription drug advertising in the United States was directed primarily to prescribers. The 1906 Pure Food and Drug Act was directed toward product labels and contained no provisions regarding advertising Primarily because, at the time of its enactment, the labels under which drugs were sold were the primary medium for drug promotions. Moreover, the Federal Trade Commission (FTC) Act of 1914 gave the FTC jurisdiction over advertising practices. In addition, at that time the FTC did not have the authority to regulated deceptive advertisements unless it could prove that they injured another company. By the time the 1938 Federal Food Drug and Cosmetic Act (FFDCA) was passed, advertising media such as radio had emerged, and Journal of the American Pharmacists Association 299 2004 Abstracts of Contributed Papers Houston, Tex. (24 stores) and East Lansing, Mich. (33 stores) by examining labels of OTC products containing acetaminophen. Four products from each store were selected, and five packages for each of these products were evaluated for presence of external tags. Data with respect to type of tags and the information concealed on these labels were coded and analyzed to report information obscured. Results: From the 57 stores, 124 products and 718 packages were evaluated. There were more price tags (N = 515, 63.1%) as compared with antitheft tags (N = 178, 21.8%). Information concealed by antitheft tags was predominantly from the Drug Facts Panel (44.4%), namely warnings (15.3%), active ingredients (3.7%), inactive ingredients (3.3%), and product use (1.1%), which is required by the FDA to be clearly visible on each package. Price tags were predominately on the face of packages and concealed mainly information such as brand name (38.5%), product description (24%), and various sections of the Drug Facts Panel (27.5%). Conclusions: Results indicate that inappropriate tagging by retailers and manufacturers evidently obscure important information mandated by the FDA on OTC medication labels. These external tags could make it difficult for consumers to make informed decisions regarding product selection and use. Pharmacists should realize the importance of consumer rights to access vital information from OTC medication labels and be aware of lawsuits and liabilities associated with such issues. Recommendations for improvement and/or change in practice are suggested. FEATURE FEATURE Annual Meeting Abstracts 2004 the need to regulate was different from that in 1906. In 1962, the Kefauver–Harris amendments to the FFDCA transferred regulatory authority over prescription drug advertising from the FTC to the FDA. The FTC retained regulatory authority over advertising of nonprescription products. The first U.S. direct-to-consumer (DTC) advertisements for prescription medications were issued by Boots Pharmaceuticals for Rufen in 1981. This was followed by advertisements for Merck’s Pneumovax vaccine. The FDA Commissioner issued a formal request to the industry for a moratorium on DTC advertisements while FDA considered its position. Subsequently, FDA issued a Federal Register notice asserting its jurisdictional authority and stating that DTC ads must meet the same legal requirements as other prescription drug advertising. In 1997, FDA issued a draft guidance on consumer-directed broadcast advertisements and subsequently issued a final guidance on this in 1999. This opened the door to the plethora of DTC advertisements presently seen in the United States. This paper presents the history and current regulation of DTC advertising in the United States, DTC activities in other countries, and legislative activities designed to control DTC advertising. 290—WASHINGTON’S UNIFORM HEALTH CARE INFORMATION ACT: A STRONG EXAMPLE OF STATE LAWS THAT ARE NOT PRE-EMPTED BY HIPAA. Fassett W, Washington State University, Hazlet T, University of Washington. E-mail: [email protected] Objective: To compare the requirements of Washington state’s Uniform Health Care Information Act of 1991 with the provisions of the Federal Health Information Portability and Accountability Act (HIPAA) of 1996, and with the requirements of the U.S. Department of Health and Human Services’ Privacy Procedural Enforcement Rule adopted in 2003; and to assess potential compliance issues for practicing pharmacists and pharmacies. Methods: Design: Comparative legal analysis. Setting: Single state law and regulation compared with federal law and regulation. Analysis: Provisions of the laws and regulations were compared to identify any standards in Washington that were more stringent and not pre-empted by federal law. Samples of pharmacy notices of privacy practices were collected at independent and chain pharmacy sites or via the Internet to examine whether the statements conformed with Washington law as well as federal law. Results: The basic provisions of Washington law and HIPAA are similar. Certain provisions of Washington law are more stringent than HIPAA, particularly in the handling of requests by patients to view their records, consent by minors, and handling of military record requests. Washington Board of Pharmacy rules preclude certain disclosures without written consent that would be allowed under HIPAA rules. Considerable variation exists among Notices of Privacy Practices regarding the particulars of Washington laws, and pharmacies that do mention Washington specifics have not consistently interpreted the Washington statute. 300 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 Conclusions: Procedural compliance with Washington law will likely result in compliance with HIPAA. However, compliance with HIPAA procedures, particularly in dealing with requests for records, will not assure compliance with Washington state rules. These results suggest that notices of privacy practices in other states may also inconsistently accord with more stringent rules in those jurisdictions. American Institute of the History of Pharmacy (AIHP) 291—“ALWAYS AND EVERYWHERE”— QUININE IN THE AMERICAN CIVIL WAR. Flannery M, University of Alabama at Birmingham. E-mail: [email protected] Hardtack and Coffee (1887), John D. Billings‘ amazingly detailed account of the soldier’s life in the Civil War, states, “Quinine was always and everywhere prescribed with a confidence and freedom which left all other medicines far in the rear” (p. 176). This 15-minute slide presentation will discuss the curious history of quinine during the Civil War from therapeutic and economic standpoints. The paper argues that quinine and its cinchona variants not only played a significant role in therapeutics but its prevalent use in the war provided a proving ground for the remedy of unprecedented proportions. Quinine, it will be argued, was also a catalyst to the wartime boom of pharmaceutical mass production, making Rosengarten & Sons and Powers & Weightman major players in the pharmaceutical market. The talk is supplemented with illustrations of the firms and men who played a major role in its manufacture and distribution along with graphs tracking various economic aspects of quinine during the war years, 1861–1865. 292—18TH AND 19TH CENTURY PRINTED MATERIALS ABOUT THE PURSUIT OF HEALTH AT MINERAL SPRINGS. Lane A, University of Wyoming. E-mail: [email protected] The tradition of people going to special places to restore or maintain their health is a long one, dating from ancient times up to the present. Some natural locations offer bathing and drinks of “healing” spring water; some health resorts offer other attractions. Through the eighteenth and nineteenth centuries, aspects such as increased middle and upper middle class wealth, greater leisure time, and more efficient transportation allowed more people to travel further to seek relief. Promoters emphasized both scientific facts and subjective testimonials in stressing the legitimacy of their establishments. This study will focus on eighteenth and nineteenth century materials in the Toppan Rare Books Library that explain just how, and why, certain diseases and physical problems were said to be helped at particular places. Books and pamphlets to be discussed include: A treatise on the three medicinal mineral waters at Llandrindod, in Radnorshire, South Wales, by Diederick Wessell Linden, MD, 1761; A Sketch of Lebanon Springs (New York), by Daniel Gale, 1872; America’s Baden-Baden, where it is, what it is, and how to get there (Hot Springs, Arkansas), 1879; Invalids & Tourists Hotel, Buffalo, N.Y., by Ray Vaughn Pierce, MD, 1879; Asheville, Western North Carolina, nature’s trundle-bed of recuperation for tourist & health seeker, by Hinton, A. Helper, 1886; Souvenir of Poland Springs (Maine) by Hiram Ricker and Sons, 1890; and Health resorts of the South and summer resorts of New England, 1896. The association, if any, of physicians and pharmacists with these places will be considered. 293—AMERICA’S SECOND OLDEST PHARMACY? Weart C, Karig A, Medical University of South Carolina. E-mail: [email protected] Virtually forgotten in the pages of pharmacy history is one of America’s oldest pharmacies, perhaps the second oldest, which operated in Charleston, South Carolina. Founded in 1781, the pharmacy was operated by a continuous succession of owners until closing in 2002. The pharmacy became known as “Apothecaries Hall” in 1816 and later would be known as “Schwettmann’s,” a name associated with the business until its end. In 1781, Dr. Andrew Turnbull set up an apothecary shop in Charleston. He imported, prescribed, prepared, and dispensed his own medicines acting as both pharmacist and physician. In 1792, Dr. Joseph Chouler took over the practice as physician and apothecary. Dr. Chouler was succeeded by Mr. William Burgoyne who practiced as an apothecary until 1816. Dr. Jacob De la Motta, a prominent Charleston physician, purchased the establishment, enlarged the shop and named it “Apothecaries Hall.” A large golden mortar and pestle sign became its hallmark. In 1845, Dr. William Trott took over Apothecaries Hall from Dr. De la Motta. In 1849 he hired Christian Frederick Schwettmann as a pharmacist’s clerk. From 1863 to 1865 the business was temporarily relocated because of shelling from Fort Sumter. The business narrowed its focus to retail pharmacy and compounded a number of specific remedies under Dr. Trott’s name. In 1870, Dr. Trott sold the pharmacy to his one-time pharmacist’s assistant, Dr. Christian Frederick Schwettmann. Associating with his son, Dr. F. W. Schwettmann, the business became C. F. Schwettmann and Son, Pharmacists and operated until 1915 when it was purchased by Dr. John Hutching. In 1920, the pharmacy moved to a new location. It was renamed the Poulnot Drug Company and managed by Dr. Frederick Poulnot, grandson of the late Dr. C. F. Schwettmann. The pharmacy underwent several ownership and location changes before closing in 2002. 294—AN ILLUSTRATED HISTORY OF THE STERLING DRUG COMPANY. Wendt D, National Museum of American History. E-mail: [email protected] In 2001, the National Museum of American History acquired an outstanding collection of artifacts and archival material from Sterling Drug Inc. This material had been housed and processed by www.japha.org March/April 2004 Vol. 44, No. 2 Annual Meeting Abstracts 2004 The History Factory (a private archival management company) for Sterling Drug since 1991, but became “orphaned” after the divestiture of Sterling in 1995. The collection (225 linear feet of archival material and 850 artifacts) includes product samples and packaging, advertising, sales and marketing material, and corporate history files. Sterling Drug originated in 1901, when boyhood friends William E. Weiss and Albert H. Diebold established the Neuralgyline Company in Wheeling, W.V., for the purpose of manufacturing the pain-reliever product Neuralgine. Over the next 85 years the company expanded through the acquisition, both directly and indirectly, of about 130 companies. Some of the earliest acquired products included Dandarine, No-ToBac, Cascarets, and California Syrup of Figs. During World War I, Sterling set up the Winthrop Company to manufacture German drugs made unavailable by Allied blockade, and after the armistice, Sterling bought the American Bayer Company at an auction of alien property. Through licensing agreements, Sterling–Winthrop continued to produce drugs developed by Bayer and Hoechst, including Demerol, Prontosil, Atabrine, Salversan, and Luminal. Weiss and Diebold headed up the company until forced to resign in 1941. Using the artifacts and archives of the Smithsonian collection, this presentation will take a look at the first 40 years of Sterling Drug—its roots in the “patent medicine” business, expansion through aggressive acquisition, and entry into pharmaceutical manufacturing during World War I and its aftermath. Vol. 44, No. 2 March/April 2004 www.japha.org Downloaded From: http://japha.org/ on 06/09/2014 297—JAMES O. MAY, CONNECTICUT DRUGGIST AND ENTREPRENEUR. Brodeur D, Sacred Heart University. E-mail: [email protected] James O. May (1853–1904) a life-long resident of Naugatuck, Conn., was a druggist, pharmaceutical manufacturer, real estate developer, and politician. For many years, he was the proprietor of The Naugatuck Drug Company, one of several drugstores in town. He later established The Diamond Laboratory Company, which was known for the manufacture of Diamond Ginger Ale as well as several successfully marketed proprietary products. The best known and most widely advertised of these products was May’s Marshmallow Cream, which, according to its label, was “unexcelled as a curative agent in diseases of the lungs and throat.” May also was one of the largest real estate owners in the Borough of Naugatuck and was a Burgess from the First Ward. That he left a positive mark on the town is borne out by the headline of his obituary which read, “Sad Demise of Burgess May: Naugatuck Loses One of Her Best Citizens.” 298—MARMOLA, THE FTC, AND THE BATTLE OVER AUTHORITY AND OBESITY IN THE 1920s AND 1930s. Swann J, US Food and Drug Administration. E-mail: [email protected] This paper examines the history of Marmola, a preparation of desiccated thyroid and other ingredients sold to consumers for weight reduction. Introduced in the first decade of the twentieth century, Marmola became a widely—and some argued, wildly—advertised medicine for the masses in an era that increasingly prized the sleek, trim, and even emaciated figure. Seen as an unsafe and unscientific remedy thriving beyond the reach of the Food and Drugs Act, the Federal Trade Commission took issue with Marmola’s claims and ordered its manufacturers, the Raladam Company, to cease advertising that it was a harmless medicine for self-medication. Raladam appealed this ruling, and eventually the Supreme Court ruled in favor of Raladam. The FTC moved against Marmola again in the mid1930s, with similar results. However, Marmola’s existence was short-lived once the 1938 Federal Food, Drug, and Cosmetic Act was passed. In the two cases between Raladam and the FTC, both sides marshaled scientific evidence on the use of thyroid in the treatment of disease. Their arguments, framed in the context of what was known and recommended concerning obesity management at the time, will be analyzed, as will the subsequent history of Marmola under the 1938 Act. 299—MEDICINE IN THE TIME OF AULUS CORNELIUS CELSUS, 1st CENTURY ROME VERSUS MEDICINE TODAY. Ali M, Emory University, Warren F, University of Georgia. Email: [email protected] Aulus Cornelius Celsus, who lived in the first century A.D., was a great Roman medical writer and the author of De Medicinia, a classic source of information about medicinal practices before and during that time period. Celsus was a nobleman who headed his household, and as such, was responsible for the medical care of both the members of the household and the slaves who served them. De Medicinia consists of eight books, which consider prescriptives for healthy living, and descriptions of various disease states, along with their treatments. The treatments might include food, drink, adjustments to the body, plant pharmaceuticals, or surgery. For example, he gave specific directions for amputation of a limb, necessarily cutting off some of the good tissue as well as the bad, to ensure that no diseased tissue remained in the body. This paper will present some examples of Celsus’s writings and compare them with modern day conditions and their treatments. 300—THE EARLY HISTORY OF PHARMACY IN OUACHITA PARISH, LOUISIANA. Sirmans S, University of Louisiana at Monroe. Email: [email protected] Objective: The early history of pharmacy in Ouachita Parish, La., was greatly influenced by social, economic, and political issues that differ from those found in the southern part of Louisiana. Through most of the nineteenth century residents were relatively isolated and economic development was hampered; roads were poor, railroads were nonexistent, and steamboats were not able to travel to the area until 1819. The first advertisements for a drugstore did not appear until 1852. Most of the early pharmacists of the area were involved in multiple pursuits including publishing, agriculture, fraternal organizations, civic organizations, real estate, and elected office. The first college of pharmacy graduate in Monroe was George Washington McFee, an 1855 graduate of the Philadelphia College of Pharmacy. He and Jethro Moore of Trenton operated the only two drugstores in the area Journal of the American Pharmacists Association 301 2004 Abstracts of Contributed Papers 295—COD AND THE CONSUMPTIVE: A HISTORY OF COD-LIVER OIL IN THE TREATMENT OF PULMONARY TUBERCULOSIS. Grad R, University of Alabama at Birmingham. E-mail: [email protected] In 1841, Dr. John Hughes Bennett, of Edinburgh, published a treatise extolling the great benefit of cod-liver oil in the treatment of consumption. Within 10 years, cod-liver oil had entered the United States Pharmacopoeia and had become “one of the most esteemed remedies in the whole catalogue of the Materia Medica.” (United States Dispensatory [USD], 1851, p. 509). The agent quickly became regarded as the most effective remedy ever in the treatment of consumption, and its use was widespread during the second half of the nineteenth century. More than a simple food, it was thought to stimulate nutrient uptake, resulting in weight gain, and production of healthy lung tissue. The major drawback was its foul taste and smell. Although enthusiasm for the use of the agent for consumption waned at the dawn of the twentieth century, individuals still advocated its use in consumption, and the USD included a tuberculosis indication as late as 1960. This 15-minute slide presentation will discuss the history of cod-liver oil as a remedy for consumption in the United States, using successive editions of the USD, textbooks of medicine, pediatrics and materia medica, and journal articles of the period. 296—CORA DOW 1868–1915, PHARMACIST, ENTREPRENEUR, PHILANTHROPIST. Henderson M, Independent Scholar, Worthen D, Lloyd Library and Museum. E-mail: [email protected] Cora Dow took over her father’s patent medicine store in Cincinnati when he became ill. She hired a clerk while she attended the Cincinnati College of Pharmacy, graduating in 1888. By 1890 she opened a second store and began her career as a pioneer owner of a chain of discount drug stores. This business philosophy made her unpopular with other Cincinnati pharmacists and some manufacturers. However, she was well regarded by her employees and the community. She set high standards for quality of goods in her stores. When the dairy did not meet her expectations she opened her own ice cream factory. She received 150 trademarks for her line of cosmetics and toiletries. She built a drugstore with fixtures and services specifically for the woman shopper. Cora Dow sold her 11 stores shortly before her early death from tuberculosis in 1915. She never wanted to be a pharmacist; she wanted to be a musician. The major benefactor in her will was the Cincinnati Symphony Orchestra. She was a very successful entrepreneur. FEATURE FEATURE Annual Meeting Abstracts 2004 until after the Civil War. These businesses continued operations into the 1880s and were joined by no more than two other interests during the Reconstruction Period. During and for 20 years following Federal occupation, East-West and NorthSouth railroad routes were established or extended through the area and fueled economic growth. By the turn of the century at least five pharmacies were in operation, most solely or partly owned by physicians. Physician ownership of pharmacies decreased during the early 1900s and the number of pharmacist owned pharmacies exploded with the large increase in population related to discovery of gas and oil in the area in 1916. The number of pharmacies kept pace with population growth despite the economic depression of the 1930s and a national pharmacist shortage during World War II. During this period the first female pharmacist of Monroe, Arnetta Pierce, joined her father’s practice, and first and second generation Italian American pharmacists established pharmacies in Monroe. 301—THE NATURAL HISTORY OF PLINY VERSUS CURRENT ALTERNATIVE THERAPY. Warren F, University of Georgia, Ali M, Emory University. E-mail: [email protected] Pliny the Elder was author of The Natural History, an encyclopedic work that served as an authority on medical and scientific matters up to the Middle Ages. The Natural History, containing 37 books, was completed in A.D. 77. Pliny explained his purpose as the study of “the nature of things.” Previously, no author had collected the older, scattered material that belonged to encyclical culture. The Natural History covers most subjects, including humans (Book VII), botany (Books XII to XIX) and medicine and drugs (Books XX to XXXII). Reading The Natural History became a substitute for a general education, and many monastic libraries possessed copies. Pliny’s authority was unchallenged, partly because of a lack of reliable information and partly because his assertions often could not be tested. The first attack on Pliny’s work came in 1492, and Pliny’s influence diminished as more writers questioned his statements. By 1700, The Natural History had been rejected by leading scientists. This paper will present some of Pliny’s descriptions of diseases and their Roman treatments and compare them with those recommended by present-day alternative therapy practitioners. 302—THE NISEI PHARMACY STUDENTS. Worthen D, Lloyd Library and Museum. E-mail: [email protected] In post-Pearl harbor 1942 a number of students were forced from four West Coast colleges of pharmacy, not for poor grades, but because of their ethnicity. Frequently the students were forced to leave despite the wishes of the school to keep them. Some of the students were forced into assembly centers and relocation camps before finding another pharmacy school that would allow them to return to their professional studies. Other students were able to gain admittance quickly and avoided the camps altogether. Some schools, notably Idaho State 302 Journal of the American Pharmacists Association Downloaded From: http://japha.org/ on 06/09/2014 University, the University of Nebraska, and the St. Louis College of Pharmacy, admitted a number of these transfer students. Other schools were precluded from accepting Nisei students, frequently because of military contracts with the University. This paper draws on school records and materials in the National Archives to document the story of both individuals and institutions during the internment of the Nisei students. selling advertising space for the Washington Post. The presentation uses advertisements, city directories, newspaper articles, and objects from museum collections to examine the history of the Roach store. Since the store opened at a time when southeastern Washington was a thriving area, and closed as the neighborhood fell into disarray, the paper will reveal how city history is reflected through the history of the store. 303—THE PROVENANCE OF THE MEDICINA PENSYLVANIA, CA. 1770. Wilson R, Johns Hopkins University. E-mail: [email protected] This presentation examines the provenance of a large and complex German–English dispensatory at the College of Physicians in Philadelphia compiled by George de Benneville, a physician trained in Germany and practicing in the North American colonies. Of particular interest is the selective use of seventeenth and eighteenth century German and English sources, suggesting that more than one author was involved. Current findings confirm a mixed provenance. The section on spagyrical diseases and uroscopy draw on a Paracelsian tract by a sixteenth century German court physician, Johannes Hayne. By contrast, the section on medicinal simples, including some of the oils, wines, and salts, is a fairly verbatim condensed extract of the 1753 New Dispensatory of William Lewis. The more complex tinctures and balsams and the numerous prescriptions for specific conditions appear to introduce yet another set of sources, probably the recipe collections of German chemiatrists such as Johann Schroeder. The presentation also inquires into the commercial expectations underlying the compilation and publication plans for this manuscript. Absent American dispensatory imprints before the 1770s, its author or authors may have wished to address colonial medical markets and their providers. Here, a major question is whether the inclusion of disparate sources was intended to serve concrete therapeutic objectives or marketing strategies, or represents a synthetic approach in a new multicultural environment. 305—THE TRADING WITH THE ENEMY ACT OF 1917 AND ITS AFFECT ON DRUG REGULATION. Cooper D, Independent Scholar. E-mail: [email protected] This paper discusses how the Trading with the Enemy Act of 1917 affected drug regulation through its authorization of the seizure of German patents. An Executive Order created the Office of the Alien Property Custodian and authorized the Federal Trade Commission (FTC) to issue licenses for the patents. The FTC was given the authority to set the terms of the licenses along with the power of revocation. Because of shortages, high prices, and health significance, the most critical patents were for synthesized drugs, especially the antisyphilitic agent Salvarsan. The FTC recognized the potential quality problem new non-German suppliers posed. The FTC, with the advice and support of the National Research Council, the U.S. Public Health Service, and the American Medical Association, developed an evaluation and control procedure. Generic names and price control provisions were established. The Alien Property Custodian’s sale in 1919 of all German patents to the Chemical Foundation, a private organization, weakened FTC’s control. The U.S. Public Health Service grew uneasy about the loss of government control over arsphenamine (the generic name for Salvarsan). However, the agency gained control over the medication when the Solicitor of the Treasury issued an opinion that arsphenamine was subject to the 1902 Biologics Control Act as an analogous product. 304—THE ROACH DRUGSTORE, WASHINGTON, D.C. Jentsch E, National Museum of American History. E-mail: [email protected] Many remember the elaborate 1890s Drugstore Exhibit in the National Museum of American History’s old Medical Sciences Hall. The fixtures for this display were taken from the Roach Drugstore, a pharmacy that sat on 8th and G streets in southeast Washington, D.C., for almost 50 years. This paper presents information on the Roach drugstore, its owners, and the community it served. The store was one owned by the O’Donnell family. Under patriarch James O’Donnell, this family ran at least eight other pharmacies in the Washington area. The paper discusses the leadership of the O’Donnell family among Washington’s pharmacists and shows how their pharmacies became valuable community spaces, from serving as ballot places for Washington’s most popular Irishman contests to 306—TINS AND PHARMACY. Silberman H, Independent Scholar. E-mail: aihp@ facstaff.wisc.edu Tin collecting is a widespread hobby. The beauty and richly decorated metal boxes attract collectors. This talk focuses on small boxes in which drugs, especially throat medications, were and are sold. Slides show boxes of American and European origin. Emphasis is on early manufacturing practices in producing and decorating tin-clad iron containers. A variety of narcotics (alkaloids) were incorporated into cough medications. Extended claims were made in the early part of the twentieth century as to the benefits of such over-the-counter preparations, promising for instance the cure from lung diseases such as tuberculosis and whooping cough. A handout lists a bibliography of European and American books and articles on the subject. Modern equipment of a production line in a leading metal box manufacturing company is presented. www.japha.org March/April 2004 Vol. 44, No. 2
© Copyright 2026