AG Koch/Schölch: Mechanisms of Tumor Cell Dissemination in
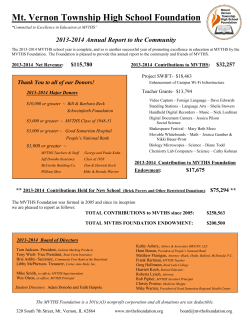
AG Koch/Schölch: Mechanisms of Tumor Cell Dissemination in Gastrointestinal Tumors Members: Prof. Dr. med. Moritz Koch (Senior PI) Dr. med. Sebastian Schölch (PI) Dr. rer. nat. Lahiri Nanduri (PostDoc) Dr. med. Sebastian Garcia (Physician Scientist) Dr. med. Alexander Betzler (Physician Scientist) May-Linn Thepkaysone (PhD) Catherine Herzig (MD student) Maria Rudolf (MD student) Marlena Baumann (MD student) Doreen Werchau, BSc (Technician) Annett Heinrich (Technician) Stefanie Ufer (Technician) In localized stages, most gastrointestinal tumors are curable by surgical resection. Once the disease has spread to distant organs, the tumors are generally considered a systemic disease and are incurable in the majority of cases. Systemic spread is a consequence of tumor cell seeding into the blood stream. Tumor cells in circulation are called circulating tumor cells (CTC), single tumor cells found in distant organs are called disseminated tumor cells (DTC). CTC and DTC are the biological correlate of metastasis and are therefore the main reason for the high mortality of GI tumors. Our group is interested in the biological traits of CTC and DTC and the mechanisms enabling these cells to perform the complex mechanism of metastasis. To investigate these mechanisms we are using patient samples as well as state-of-the-art preclinical models such as genetically engineered mouse models and 3D organoid culture. In the past we were able to identify differentially regulated surface proteins in CTC which enable these cells to escape the immune system while in circulation. Future goals include the identification of druggable targets on CTC to develop drugs which may be used to prevent metastatic spread of GI tumors in patients. Another research focus of our group is genetic diversity in colorectal cancer (CRC). We are able to remodel multiple subtypes of CRC in vitro and in vivo and are aiming to eventually be able to tailor the treatment of CRC to the patient’s individual tumor genotype. Our group harbors subproject 1 of Klinische Forschergruppe 227 (Deutsche Forschungsgemeinschaft, (www.kfo227.de). Further funding is generously provided by Roland-Ernst-Stiftung für Gesundheitswesen. Key publications: Schölch S*, Rauber C*, Tietz A, Rahbari NN, Bork U, Schmidt T, Kahlert C, Haberkorn U, Tomai MA, Lipson KE, Carretero R, Weitz J, Koch M* and Huber PE*. Radiotherapy combined with TLR7/8 activation induces strong immune responses against gastrointestinal tumors. Oncotarget 2015 [Epub ahead of print] Steinert G*, Schölch S*, Niemietz T*, Iwata N, García SA, Behrens B, Voigt A, Kloor M, Benner A, Bork U, Rahbari NN, Buechler MW, Stoecklein N, Weitz J and Koch M. Immune Escape and Survival Mechanisms in Circulating Tumor Cells of Colorectal Cancer. Cancer Res 2014;74:1694–704. Van Noort V*, Schölch S*, Iskar M*, Zeller G, Ostertag K, Schweitzer C, Werner K, Weit J, Koch M* and Bork P*. Novel Drug Candidates for the Treatment of Metastatic Colorectal Cancer through Global Inverse Gene-Expression Profiling. Cancer Res 2014;74: 5690–5699. Schölch S, Bork U, Rahbari NN, García S, Swiersy A, Betzler AM, Weitz J and Koch M. Circulating tumor cells of colorectal cancer. Can Cell Microenviron 2014;1: e323 Rahbari NN, Bork U, Kircher A, Niemietz T, Schölch S, Kahlert C, Schmidt T, Steinert G, Ulrich AB, Reissfelder C, Koch M and Weitz J. Compartmental differences of circulating tumor cells in colorectal cancer. Ann Surg Oncol 2012;19:2195–202. Steinert G, Schölch S, Koch M and Weitz J. Biology and significance of circulating and disseminated tumour cells in colorectal cancer. Langenbecks Arch Surg 2012;397:535–42. *equal contribution Fig 1: Circulating tumor cell in the isolation pipet (EpCAM-FITC merge). Fig 2: Murine CRC organoid. Fig 3: Group picture. From left to right: M. Koch, D. Werchau, C. Herzig (front), A. Heinrich (middle), L. Nanduri (back), M. Thepkaysone (front), S. Garcia (back), S. Ufer, M. Baumann, S. Schölch, M. Rudolf, A. Betzler
© Copyright 2026