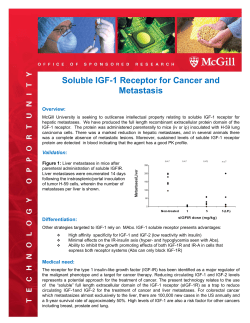
Review Alternative Activation of Macrophages: Mechanism and Functions Immunity
Immunity Review Alternative Activation of Macrophages: Mechanism and Functions Siamon Gordon1,* and Fernando O. Martinez1,* 1Sir William Dunn School of Pathology, University of Oxford, South Parks Road, Oxford OX1 3RE, UK *Correspondence: [email protected] (S.G.), [email protected] (F.O.M.) DOI 10.1016/j.immuni.2010.05.007 The concept of an alternative pathway of macrophage activation has stimulated interest in its definition, mechanism, and functional significance in homeostasis and disease. We assess recent research in this field, argue for a restricted definition, and explore pathways by which the T helper 2 (Th2) cell cytokines interleukin4 (IL-4) and IL-13 mediate their effects on macrophage cell biology, their biosynthesis, and responses to a normal and pathological microenvironment. The stage is now set to gain deeper insights into the role of alternatively activated macrophages in immunobiology. Introduction The concept of an alternative pathway of macrophage activation induced by the T helper 2 (Th2) cytokines interleukin-4 (IL-4) and IL-13, distinct from interferon-g (IFN-g)-mediated classical activation, has gained considerable ground over the past decade. Analysis of marker molecules in the mouse has revealed a stereotypic signature of expressed genes induced by IL-4 and IL-13, contrasting with characteristic changes induced by IFN-g, which mediates Th1 cell-type activation of macrophages. Phenotypes associated with alternative activation of macrophages (AAMs) and classical activation of macrophages (CAMs) can be distinguished from the direct effects of microbial stimuli, such as lipopolysaccharide, which induce innate macrophage activation, often through Toll-like receptors (TLRs). Innate stimuli are able to synergize with CAMs, to achieve full expression of macrophage effector pathways. Investigators have implicated AAMs in a range of physiologic and pathological processes, including homeostasis, inflammation, repair, metabolic functions, and malignancy. This is in addition to their established role in immunity, hypersensitivity, allergy, parasitic infections, and their sequelae, such as fibrosis. Recent genome-wide analysis, although broadly supporting earlier studies with limited numbers of markers, has underscored the heterogeneity and plasticity of macrophage gene expression, adding to the confusing nomenclature of monocyte and tissue macrophage subpopulations (Geissmann et al., 2010). In this review, we assess current knowledge, point to the need to restrict the concept of AAM, and consider newer findings regarding mechanisms and therapeutic potential. Our own interest in IL-4 modulation of the macrophage phenotype arose in the late 1980s from experiments with human blood monocyte-derived macrophages and mouse peritoneal macrophages. At the time, the role of this cytokine was believed to be mainly anti-inflammatory, resulting from its ability to suppress TNF and IL-6 production in macrophages. Whereas macrophage mannose receptor (MRC1) expression and its endocytic function were selectively downregulated by IFN-g (Mokoena and Gordon, 1985), it was upregulated by IL-4 (Stein et al., 1992) and IL-13 (Doyle et al., 1994) and depended in vitro and in vivo on IL4Ra1, the common IL-4 and IL-13 receptor alpha chain (Linehan et al., 2003). Others showed a critical role for the transcrip- tion factor STAT6 in their signaling (Heller et al., 2008). These and other experiments showed that these Th2 cytokines were not simply inhibitory, but subtle modulators of macrophage functions. We proposed that IL-4 induced an ‘‘alternative’’ form of activation in macrophages (Stein et al., 1992). Subsequently, other workers introduced the term M1 and M2 to parallel macrophage activation with T helper cell polarization, subdivided M2 classes into subgroups, and in some cases, termed all nonclassical activation phenotypes as ‘‘alternative’’ (discussed in Gratchev et al., 2001; Mantovani et al., 2008; Mosser and Edwards, 2008). We have argued that too loose a definition obscures the study of mechanism and discovery of potential therapeutic agents. Even a restricted definition of IL-4 and IL-13 dependence needs to take into account the complex effects of cell differentiation, interactions with other receptors, and signaling pathways, and the role of tissue microenvironment in modulating the macrophage phenotype. Monocyte and macrophage heterogeneity and nomenclature are discussed below and elsewhere (Gabrilovich and Nagaraj, 2009; Geissmann et al., 2010). Analytic Approaches There are two distinct, complementary approaches to the study of AAMs. The first, ‘‘forward analysis,’’ flows from receptor-dependent recognition, through signal transduction, gene expression, and protein production. The second, ‘‘reverse analysis,’’ deduces from phenotypic markers the mechanism of initiation. Studies with isolated macrophages and in situ analysis in wild-type and genetically modified mice made it possible to combine these approaches. Forward analysis utilizes cytokine, receptor, or signaling-deficient animals to define an AAM phenotype, including Arginase 1 (ARG1), Ym1 and Ym2, Fizz1, MRC1, and selected chemokines (Loke et al., 2002). Signature markers, in combination, have then been used to infer an AAM pathway and mechanism (reverse analysis). There are obvious caveats to the use of reverse analysis alone, as required in human studies in situ: substantial species differences exist in available markers, and established markers such as Arg1 can be induced by other pathways (El Kasmi et al., 2008). Even clusters of multiple signature markers can be independent of the IL-4 and IL-13 receptor pathway (Daley et al., Immunity 32, May 28, 2010 ª2010 Elsevier Inc. 593 Immunity Review 2010; Stout, 2010). We lack markers for human AAM, but these should become available with current microarray and proteomic studies. Combined forward and reverse analysis in the mouse will validate the link between recognition and response. With humans, our dilemma mimics the problem of diagnosis in clinical medicine, where a cluster of symptoms and signs cannot be assigned to a particular cause without supportive evidence. Toward an Integrated Approach Before turning to the pathways and functions of AAM, we summarize general features of monocyte and macrophage heterogeneity (Gordon, 2008). Macrophages arise from hemopoietic progenitors (Geissmann et al., 2010), which differentiate, directly or via circulating monocytes, into subpopulations of tissue macrophages and closely related myeloid dendritic cells (Steinman and Idoyaga, 2010), the latter specialized to present antigens to naive T helper lymphocytes. Osteoclasts arise from monocyte precursors to form multinucleated giant cells, implicated in resorption of bone. Monocyte and macrophages share properties with granulocytes, especially neutrophils, and to lesser extent with B lymphocytes. Monocyte and macrophages migrate through several body compartments, including bone marrow, blood, lymphoid, and all nonhematopoietic tissues. Resident macrophages are present in organs constitutively, in the absence of overt inflammation, and perform trophic as well as homeostatic roles in the removal of apoptotic cells, serving as sentinels of injury and infection. Tissue macrophages can replicate locally, but are terminally differentiated, turning over at different rates, depending on the stimulus and tissue environment. Macrophages differ morphologically and phenotypically in organs such as liver, spleen, lung, gut, and brain, interacting with matrix and other cell types. They are active in biosynthesis and express a wide range of receptors, recognizing foreign as well as normal and abnormal cells and host-derived products. Through constitutive and induced endocytosis, phagocytosis, and secretion of various products, including cytokines, growth factors, and metabolites, they perform both trophic and toxic functions, serving as a widely dispersed mononuclear phagocyte system during development and throughout adult life. They contribute to tissue remodeling, host defense in innate and adaptive immunity, and many disease processes. Monocytes are the main source of newly recruited tissue macrophages in infection, granulomata, atherosclerosis, Alzheimer’s disease, and tumors. Differentiation and activation of macrophages depend on specific growth and differentiation factors, their receptors, signaling pathways, and transcription factors. Macrophages migrate to local sites of injury and infection, contributing to acute and chronic inflammation, locally and systemically. In addition they acquire enhanced cytotoxic, antimicrobial, and inhibitory activities, initiate repair, and resolve inflammation. Macrophages express opsonic and a range of nonopsonic receptors, TLRs, RIG-I-like and Nod-like sensing receptors, on their surface and in vacuolar and cytosolic compartments. Other receptors include families of regulatory molecules, lectins, and scavenger receptors. Their secretory repertoire includes antibacterial and proteolytic enzymes, chemokines, and anti-inflam594 Immunity 32, May 28, 2010 ª2010 Elsevier Inc. matory cytokines, such as IL-10 and TGF-b. Proinflammatory cytokines include IL-1b, TNF, and IL-6. Through potent membrane protein assemblies they generate reactive oxygen, nitrogen, and arachidonate metabolites. The study of chromatin structure and epigenetic control of gene expression in macrophages is in its infancy. Given the range of receptors and potential ligands, it may be invidious to single out IFN-g, IL-4, and IL-13 receptor pathways as central regulators of macrophage activation. However, given their often polarized production in the immune response, these contrasting states of activation provide an important conceptual framework. Other receptors participate in forming signaling platforms and complexes, e.g., G protein-coupled receptors and integrins. Crosstalk at all levels impinges on altered transcription. It is therefore possible to conceive an infinite number of potential phenotypes; however, the conserved, stereotypic macrophagespecific signature for IFN-g versus IL-4- and IL-13-dependent activation provides useful insights into physiologic and pathologic mechanisms. Figure 1 presents a schematic model of macrophage activation. The first stage, differentiation, depends on growth factors such as GM-CSF or M-CSF; the second, priming by IFN-g (CAMs) or IL-4 and IL-13 (AAMs); and the third, a localizing stimulus delivered by a TLR or analogous receptor. This additional stimulus promotes induction of a full complement of classical or alternative activation functions. In the case of AAMs, this may arise in a Th2 cell-biased environment, e.g., chronic parasitic infection, followed by a secondary microbial challenge. Counteracting negative controls contribute to a fourth stage of resolution and repair. Once established, some properties of full alternative activation can be reversible (plasticity) whereas others may be irreversible (Stout et al., 2005). Cytokines in AAM Induction IL-4 and IL-13 are the prototypical direct inducers of AAMs, but other cytokines such as IL-33 and IL-25 amplify AAM induction indirectly, through Th2 cells (for review on CD4+ T cell heterogeneity, see O’Shea and Paul, 2010). IL-4 and IL-13 are produced by various innate cells, including non-B non-T cells (Moro et al., 2009; Neill et al., 2010), mast cells, basophils, eosinophils, NKT cells, and even macrophages themselves. Apart from activated Th2 cells and B cells, epithelia and tumor cells are potential sources in tissues. The availability of reporter mice has contributed to the analysis of IL-4 production in vivo, during allergic inflammation and infection (Mohrs et al., 2005). The role of IL-5, another Th2 cell cytokine that binds to distinct receptors on macrophages, is unclear. IL-10, produced by CD4+ Th2 cells, macrophages, and B cells as well as tumor cells, is a potent downregulator of macrophage gene expression, modulating IL-4 and IL-13 and IFN-g actions. IL-21 enhances AAMs by driving IL-4R expression (Pesce et al., 2006). IL-33, a Th2 cell product, binds to ST2L, a subunit of the IL-33 receptor, to amplify Th2 cytokine production and AAM induction (Kurowska-Stolarska et al., 2009). IL-25, a member of the IL-17 family also produced by Th2 cells, induces production of multipotent hemopoietic progenitors in bone marrow and at sites of extramedullary hemopoiesis, giving rise to a range of myeloid cells, including monocytes and macrophages (Saenz et al., 2010). IL-25 activates antigenspecific responses in mucosal tissues, such as the colon. In Immunity Review RESOLUTION IL-10, TGF-β, lipoxins ACTIVATION TLR stimuli PRIMING IFN-γ<-> IL-4 DIFFERENTIATION M-CSF <-> GM-CSF Figure 1. Paradigm of Macrophage Activation Macrophages undergo activation to fulfill specific functional roles during inflammation and its resolution. The phenotype is imparted by the complex mixture of cytokines, metabolites, plasma proteins, and microbial ligands present in the inflammatory milieu. The development into mature and fully activated macrophages can be artificially divided into successive stages. In this scheme we have placed these stimuli in a hierarchical order. A first phase is envisaged in which the recruited monocytes mature into macrophages. In vitro experiments suggest that the balance of MCSF, GMCSF, retinoic acids, and lipoproteins determines substantial differences in the phenotype of the mature macrophage. During continuous recruitment, monocytes are exposed to varying concentrations of mediators, inducing a second phase of priming by cytokines. The priming term derives from the fact that these stimuli per se are not very strong, but influence the inflammatory potential of macrophages and their response to other stimuli. During the third phase of activation, macrophages reach a mature functional phenotype in response to microbial and opsonic stimuli such as antibody complexes. If the macrophage survives its inflammatory task, it should undergo the final phase commonly referred as to deactivation. We have chosen the term resolution, because while the macrophage proinflammatory potential is deactivated, it also undergoes functional changes that allow it to clear debris and express general repair functions. IL-10, TGF-b, and a multitude of anti-inflammatory mediators such as nucleotides, lipoxins, and glucocorticoids are included in this category. principle, all cytokines that regulate Th1 and Th2 cell responses can affect AAMs indirectly. The IL-4 and IL-13 Receptors, Signaling, and Function Although IL-4 and IL-13 have many overlapping activities on macrophages, they have distinct functions. Receptors for IL-4 are mainly expressed on hematopoietic cells, whereas IL-13 receptors are also present on nonhematopoietic cells (Figure 2). IL-4 and IL-13 receptors share a common alpha chain, but there are specific IL-13Ra1 and IL-13Ra2 subunits (Kawashima et al., 2006). The IL-4Ra1 can signal through the common gamma chain (Type I IL-4R) or partner IL-13Ra1 (Type II IL-4R). The IL-13Ra2 chain, thought to form a decoy receptor with extraordinary affinity for IL-13 (Lupardus et al., 2010), but with little signaling capacity, has been implicated in STAT6-independent fibrogenesis and tumor-host interactions (Fichtner-Feigl et al., 2006, 2008b). There are therefore three distinct subtypes of AAMs, depending on specific ligand-receptor interactions, and their interplay is largely unexplored. The signaling pathways activated by the Type I and II receptors involve STAT6, although other STATs can participate (Bhattacharjee et al., 2006). STAT6 plays a central role in gene regulation by IL-4 and IL-13, including the differentiation of Th2 cells, production of IgE, chemokines, and mucus at sites of allergic inflammation. The differential effects of IL-4 and IL-13 on different macrophage populations from mice and humans have been examined by correlating the magnitude of response with the expression of each receptor (Junttila et al., 2008). Early, low amounts of IL-4 promote a Th2 cell type response; as the stimulus persists, IL-13 becomes sufficient to induce responses in both hemopoietic and nonhemopoietic cells, making it the dominant Th2 effector cell cytokine. Type I and Type II receptor complexes have also been compared in mouse bone marrow-cultured macrophages and human monocytoid cells (Heller et al., 2008). IL-4 action via the Type I receptor was more potent with subtle differences in signaling and target gene activation, which bear on the contribution of each cytokine to pathophysiology, e.g., in the airway. Type I IL-4R selectively activated IRS-2, which interacts with the adaptor Grb-2 and with PI-3 kinase, thereby initiating multiple signaling pathways. IL-4 more readily induced a subset of commonly used mouse AAM signature genes (Arg1, Fizz1, Ym1), whereas Mrc1 mRNA was induced comparably by IL-4 and IL-13. The expression of each receptor polypeptide influenced its affinity for each cytokine. IL-13Ra1-deficient cells were used to define distinct requirements for IL-13 and IL-4 in AAM induction by parasitic infection (Ramalingam et al., 2008). Whereas IL-4 could stimulate both Type I and Type II receptor signaling, the Type II receptor was essential for protection against schistosomiasis and resistance to Nippostrongylus braziliensis and its expulsion from the gut. Allergen-induced airway hyperreactivity, mucus secretion, and fibrosis were IL-13Ra1 dependent, whereas this receptor was redundant for AAM and fibroblast activation. Expression of a subset of genes, however, was reduced in the IL-13Ra1-deficient mice, including IL-13Ra2, Muc5a, Ccl11, and Ccl3. Surprisingly, the Th2 cell response was exacerbated, possibly because of lack of feedback inhibition. These results show that IL-13 is the more pathogenic cytokine, while consistent with the notion that IL-4 contributes most to expansion of a Th2 cell response. The role of epithelial and fibroblast receptors in vivo requires further study. IL-13 induced phosphorylation of IL-13Ra1 and IL-4Ra1, but not of the IL-13Ra2 or IL-2Rgc (Bhattacharjee et al., 2006; Roy et al., 2002). Phosphorylated Jak2 associated with IL-4Ra1 and phosphorylated Tyk2 with IL-13Ra1. STAT1, STAT3, STAT5A and B, and STAT6 were all tyrosine phosphorylated and activated in response to IL-13. Furthermore, IL-13 induction of the gene that encodes 15-LO (15 lipoxygenase) expression required p38 MAP kinase-mediated phosphorylation of STAT1 and STAT3. 15-LO was regulated by a signaling complex with PKCd kinase and both tyrosine and serine phosphorylation of STAT3. PKCd was thus required for IL-13-induced 15-LO expression and subsequent inhibition of the lipid mediator leukotriene B4. IL-4 has substantial effects on SHIP1 and SHIP2, phosphatases that skew macrophage polarization (Rauh et al., 2005). Immunity 32, May 28, 2010 ª2010 Elsevier Inc. 595 Immunity Review Type I Figure 2. IL-4 and IL-13 Signaling Machinery Type II IL-4 IL-13 IL-4 IL-13 IL-4Rα Jak1 STAT6 IL-2Rγ IL-4Rα Jak3 IL-13Rα1 Jak1 IRS-2 Tyk2 STAT3 (?) STAT6 PI3K P ? STAT6 Grb2 STAT6 IL-13Rα2 P Hematopoietic cell Nonhematopoietic cell STAT6 STAT6 PP PP IL-4 binds IL-4Ra and then recruits either IL-2Rg chain (to form the type I receptor) or the IL-13Ra1 chain (to make the type II receptor), depending upon the cell type (Heller et al., 2008). However, IL-13 can only signal through type II receptor as it binds IL-13Ra1 and recruits IL-4Ra (LaPorte et al., 2008). The common signaling pathways shared by both the cytokines involve phosphorylation of STAT6, which leads to dimerization and translocation of STAT6 to the nucleus where it regulates the transcription of a number of genes. The type I receptor is predominantly found in cells of hemopoietic origin such as lymphocytes and granulocytes, resulting from restricted expression pattern of the IL-2Rg chain. The type II IL-4 receptor is mainly expressed by cells of nonhemopoietic origin such as epithelial cells and fibroblasts. Some cell types, such as macrophages, express both receptor types. IL-13 also binds IL-13Ra2, with an extraordinarily high affinity (Lupardus et al., 2010), which is thought to function as a decoy receptor (Chiaramonte et al., 2003), though evidence exists for its potential to signal in selected circumstances (Fichtner-Feigl et al., 2006). STAT6 PP IL-4 triggers proteosomal degradation of both of these phosphatases in bone marrow-cultured mouse macrophages, enhancing the PI3K and Akt kinase pathways (Ruschmann et al., 2010). SHIP represses IL-4 production from basophils, thereby indirectly controlling the AAM phenotype (Kuroda et al., 2009). The mTOR adaptor is an evolutionarily conserved member of the PI3K family that forms the core of distinct TORC1 and TORC2 signaling complexes, broadly responsible for the regulation of metabolism, growth, and proliferation (Delgoffe et al., 2009). Recent studies have shown that mTOR is essential in dictating T helper cell differentiation, TORC1 for Th1 and Th17, and TORC2 for Th2 cell differentiation. It would be interesting to examine macrophage polarization in mice after genetic ablation of these distinct pathways. There are few reports of epigenetic modification or microRNA analysis in AAMs. Signature marker genes of IL-4-treated mouse macrophages, Arg1, Ym1, Fizz1, and MRC1, revealed reciprocal changes in histone H3K4 and H3K27 methylation; the latter methylation markers were removed by the H3K27 demethylase Jmjd3 (Ishii et al., 2009). These changes depended on activation of STAT6, which bound to consensus sites at the Jmjd3 promoter, contributing decreased di- and trimethylation of H3K27, as well as transcriptional activation of AAM marker genes. In vivo studies with Schistosome egg granulomas were consistent with evidence of chromatin remodeling in AAM. The kinase Akt regulates LPS-induced microRNA in macrophages and is implicated in LPS tolerance (Androulidaki et al., 2009). The isoforms Akt1 and Akt2 have differential effects on TLR4 and SOCS1 signaling in macrophages, depending on the microRNAs let7e and miR155. The effect of IL-4 and IL-13 on Akt isoforms has not been reported. Other studies have implicated microRNAs in regulation of macrophage activation (Taganov et al., 2006; Tili et al., 2007). 596 Immunity 32, May 28, 2010 ª2010 Elsevier Inc. Before global mRNA and protein repertoire analysis, knowledge of AAM markers was restricted to a few molecules. MRC1, MHC class II, FN1, and CCL22 were upregulated in common in both human and mouse macrophages, leading to the impression that they responded similarly to IL-4 (Gratchev et al., 2001; Mantovani et al., 2005; Martinez et al., 2009). Subsequent reports showed that important AAM markers in mouse, such as Fizz1, Ym1, and Ym2, lacked homologs in humans, and others such as Arg1 were not upregulated in human macrophages by IL-4, despite gene homology. Microarrays have made it possible to investigate effects of IL-4 in macrophages of both species; however, given the limited number of published studies in human or mouse macrophages, a consensus of markers is hard to establish, particularly for humans (Syed et al., 2007; Martinez et al., 2006; Scotton et al., 2005). Genes that appear to be modulated in common by IL-4 in macrophages, monocytes, and perhaps circulating precursors include ALOX15, FN1, CD23a, MAO-A, GAS6, FXIIIA1, CCL26, CCL22, and IL-17RB. Many of the expected AA markers could also be regulated by M-CSF, while a proportion of the genes were uniquely regulated by IL-4. Cell Biology and Membrane Dynamics in AAM Apart from their effects on specific receptors and antigen markers, IL-4 and IL-13 profoundly alter membrane flow in macrophages (Kzhyshkowska and Krusell, 2009; Montaner et al., 1999; Varin and Gordon, 2009). Human blood monocytederived macrophages displayed enhanced flow from the plasma membrane, through early endosomes into an expanded vacuolar compartment, accompanied by enhanced fusion with lysosomes (Montaner et al., 1999). These effects are distinct from those induced by other cytokines, such as IFN-g and TNF. Apart from receptor-mediated endocytosis, e.g., via mannose, transferrin, and folate receptors (Puig-Kroger et al., Immunity Review 2009), fluid phase endocytosis is also enhanced. The effects of IL-4 and IL-13 on phagocytosis have been variable (Varin et al., 2009). In our hands, with mouse peritoneal macrophages, these cytokines selectively downregulate phagocytosis of a range of particles, by approximately 50%, independent of specific receptor expression (Varin et al., 2009). Uptake of Neisseria meningitidis via Class A Scavenger receptors, of zymosan particles via Dectin-1, and of latex particles is similarly decreased. Reduced uptake is associated with reduced Akt phosphorylation, phagocytic cup closure, and PI3 Kinase activation. The mechanism and functional significance of these observations require further study. In contrast with reduction of phagocytosis in AAMs, IL-4 is required for the efficient uptake of apoptotic neutrophils by macrophages from murine gp91 phox-deficient mice, a model of chronic granulomatous disease (Fernandez-Boyanapalli et al., 2009). Another feature of IL-4 and IL-13 effects on macrophages is the induction of homokaryon formation by macrophage fusion (Helming and Gordon, 2009; Moreno et al., 2007). Foreign body giant cell formation depends on IL-4, whereas osteoclast formation, induced by RANKL cytokine, is inhibited by IL-4 (Moreno et al., 2003). Independent studies have demonstrated murine multinucleated giant cell formation by IL-4 and IL-13 and studied its mechanism. Fusion depends on STAT6 signaling and is homotypic, i.e., both fusing partners need to express STAT6 (Moreno et al., 2007). Several surface molecules have been implicated in fusion, including E-Cadherin, DC-STAMP (dendritic cell-specific transmembrane protein), and CD36, which is thought to interact with patches of exposed PS on fusion partners (Helming and Gordon, 2009). Other molecules such as DAP-12 induce a fusogenic phenotype required on both fusion partners (Helming et al., 2008). The effects of IL-4 and IL-13 are not necessarily associated with enhanced expression of fusogenic surface molecules, but may result from clustering in the plasma membrane or altered signaling. With human monocyte-derived macrophages, IL-4 and IL-13 accelerate fusion in vitro, but other culture variables, e.g., substratum, growth factors, and serum, also play a role. The significance of giant cell formation in granulomatous inflammation is obscure, nor is it known whether IL-4 and IL-13 play a role in macrophage fusion in nonparasitic infections, such as the prototypical Langhans giant cells of tuberculosis. Function of Signature Markers in AAM In the case of enzyme markers such as Arg1, there has been extensive investigation of its possible role in alternative versus classical activation (De’Broski et al., 2010; El Kasmi et al., 2008; Herbert et al., 2004; Pesce et al., 2009a). Although its upregulation in the mouse can be a useful indicator of IL-4 and IL-13 effects on macrophages, it can be upregulated by other pathways. Its demonstration in human macrophages has been problematic. Its possible role in fibrosis is described below. Enhanced expression and endocytosis of MRC1 are conserved features in both mouse and human macrophages; enhanced uptake of pathogens through carbohydrate recognition may contribute to infection. However, its immunologic role is unknown. A possible clue is via a role in Th17 cell differentiation (van de Veerdonk et al., 2009). Ym1 and Ym2 belong to a family of chitinase-like molecules. Chilectins are strongly induced by Th2 cell stimuli on macrophages as well as epithelium. Chilectins have undergone considerable diversification during evolution, in many cases losing enzyme activity, as with Ym1 and Ym2. These molecules bind chitin in insects, Helminth eggs, and Nematode pharynx. Chitin induces Th2 cell responses (Reese et al., 2007; Voehringer et al., 2006) and can be degraded by glucanases, and MRC1 contributes to chitin binding. Fizz1, also known as Relma or Retnla, a secreted protein produced by macrophages, epithelium, and eosinophils, is highly induced by IL-13. Fizz1 found in lung allergy and asthma may inhibit inflammation (Nair et al., 2009) Fizz / AAM display exaggerated antigen-specific Th2 cell differentiation. Fizz1 protein binds to macrophages and effector CD4+ Th2 cells, inhibiting Th2 cytokine production via Bruton’s tyrosine kinase. Fizz1 plays a role in metabolism, as well as regulating T cell differentiation and eosinophil migration. Others have reported a proinflammatory role for Fizz1 and related resistin-like molecules (Munitz et al., 2008). Involvement of AAMs in Selected Pathological Processes Role of AAM in Inflammation and Immunity AAMs are influenced by, and act upon, many processes associated with inflammation, immunity, and hypersensitivity. AAMs counteract proinflammatory and cellular immune effector mechanisms, serving regulatory as well as inhibitory functions, to shape the nature of the response. For example, IL-4 induces expression of SOCS1 in human and mouse macrophages via STAT6. SOCS1 feedback inhibits IL-4 signaling to limit expression of STAT6 responsive genes and the AAM pathway (Dickensheets et al., 2007). Although intimately associated with IL-10, TGF-b, and other agents of more profound deactivation, IL-4 and IL-13 promote a distinctive inflammation and cellular immune response. For example, NO generated by IFN-g-induced iNOS is shut down in macrophages (it is induced in epithelial targets), with a shift to Arg1. Interactions with mast cells, basophils, eosinophils, and NKT cells, as well as IgE and selected subclasses of IgG, promote allergy and hypersensitivity. Together they influence vascular permeability, angiogenesis, cell recruitment, smooth muscle contraction, goblet cell secretion, mucus production, and collagen deposition by myofibroblasts (Locksley, 2010). Several questions remain understudied. For example, the interactions between AAMs and other cells of the innate and acquired immune system, by contact, and secretion, require attention. Do AAMs influence DCs, which themselves are affected by Th2 cytokines, and can AAMs function as antigenpresenting cells (Loke et al., 2000; Rodriguez-Sosa et al., 2002)? Is the reported upregulation of MHCII significant? Apart from modulating inflammation, can AAM kill microbial and host targets, particularly parasites? Arg1 has been put forward as a candidate. Do IL-4-induced homokaryons participate in this process? Perhaps killing is indirect through eosinophils or neutrophils. In sum, the metabolic and secretory activities of AAM favor trophic rather than lytic functions, clearance of apoptotic corpses rather than induction of necrosis, and induction of tolerance rather than autoimmunity. Immunity 32, May 28, 2010 ª2010 Elsevier Inc. 597 Immunity Review Inflammasome Activation Little is known about inflammasome activation and IL-1b release by AAMs, compared with CAMs. Decrease of caspase 1 expression and pro-IL-1b processing has been described for human monocytes stimulated with IL-13 (Scotton et al., 2005). A similar downregulation is observed in some human macrophage models. An intriguing study by Pelegrin and Surprenant examined the role of extracellular ATP and purinergic receptors in a spectrum of polarized macrophages. In intermediate, but not fully AAMs, P2X7R activation uncouples NLRP3 inflammasome maturation (Pelegrin and Surprenant, 2009). ATP acts, instead, through pyrophosphate to inhibit IL-1b release. Role of AAMs in Infection, Fibrosis, and Immunopathology The generation and role of AAMs has been studied extensively in parasitic disease models (e.g., Anthony et al., 2006; Fallon et al., 2006; Hesse et al., 2001; Holscher et al., 2006; Reece et al., 2006), providing the best evidence for a regulatory, protective role of AAMs in these Th2 cell-dominated infections. Earlier studies, culminating in macrophage-specific genetic ablation experiments, implicated the common IL-4Ra1 chain in Nippostrongylus resistance. IL-13 is critical for worm expulsion and also plays an important role in Schistosome egg granuloma formation and fibrosis. Murine markers of AAMs have provided a remarkably conserved signature of gene expression, considering the diversity of organisms studied. Parasite-specific features are associated with particular sites of migration during complex life cycles, e.g., in skin, lung, gut, and liver, illustrating the importance of tissue microenvironment in tuning the Th2 cell response. AAMs respond to Th2 cytokines and in turn regulate T helper cell functions. Delayed healing or excessive fibrosis occurs in mice with dysfunctional AAMs (Wilson and Wynn, 2009). Major questions remain unresolved regarding the role, if any, of AAM in parasite killing and in activation or suppression of different T cell subsets. Can AAM serve as parasite antigen-presenting cells for T cells? Chemokines produced by AAMs promote recruitment and activation of eosinophils, mast cells, and basophils, themselves sources of Th2 cytokines, as well as neutrophils. Interactions of AAMs with antibody subclasses promoted by Th2 cytokines have received less attention, but include upregulation of FcR epsilon for IgE. The range of organisms studied in the mouse includes H. polygyrus and flatworms, and wellstudied unicellular parasites include Leishmania and Trypanosoma brucei. In humans, filariasis has attracted investigators, but the lack of reliable AAM markers has hampered progress. Further details on the diversity of host responses to parasitic infection can be found in excellent reviews (Jenkins and Allen, 2010; Wilson and Wynn, 2009). A striking example of the way in which a bacterial pathogen can subvert the host response to favor its intracellular survival is provided by Francisella tularensis (Ft), the causal agent of tularaemia (Shirey et al., 2008), illustrated in Figure 3A. This highly virulent coccobacillus has been studied in the form of a vaccine LVS strain, attenuated for humans but still pathogenic for mice. It enters macrophages by a TLR-2-dependent mechanism, utilizing mannose and scavenger receptors, and initiates a transient inflammatory response, but the host CAM reaction is then 598 Immunity 32, May 28, 2010 ª2010 Elsevier Inc. subverted by pathogen-induced reprogramming of the macrophage to acquire an AAM phenotype. Instead of the host-protective CAMs, it induces many characteristics of AAMs, by unknown sensing receptors within the phagocytic vacuole and, on escape into the cytoplasm, by additional cytosolic sensors. The macrophages are induced to produce IL-4 and IL-13, which amplify the AAM phenotype through autocrine and paracrine mechanisms. The canonical signature markers are induced, depending on the IL-4 and IL-13 common alpha chain receptor and STAT6, incapacitating the cell’s antimicrobial responses, and allowing FT to replicate freely. Similar though less dramatic exploitation of AAMs may contribute to persistent mycobacterial infection (Kahnert et al., 2006). Another issue is the secondary infection of Th2 cellbiased infected hosts with opportunistic or pathogenic bacteria. Challenge of IL-4 or IL-13 pretreated macrophages with Neisseria meningitidis can potentiate the release of proinflammatory cytokines (Varin et al., 2009); AAMs can thus contribute to septic shock. Pathogens such as Aspergillus and Candida utilize TLR-2 and TLR-6 and the beta glucan receptor Dectin-1 to infect macrophages (Brown, 2006). AAMs express enhanced Dectin-1 as well as mannose receptor, which is delivered to the nascent phagosome intracellularly (Heinsbroek et al., 2009). Dectin-1 contains a hemi-ITAM (immunoreceptor tyrosinebased activation) motif in its cytoplasmic domain, essential for signaling, through Syk kinase and CARD9, thus inducing proinflammatory cytokines and activating a respiratory burst. The receptor contributes to host resistance to Candida and Pneumocystis. However, it is not clear whether AAMs are beneficial or deleterious to the host, because other innate (complement, neutrophils) and adaptive mechanisms, including classical activation by IFN-g and Th17 cell activation, come into play. Respiratory syncytial virus (RSV), a major cause of morbidity in children, employs a similar mechanism of AAM induction to that described for Francisella, although in this instance the outcome is beneficial to host repair and diminishes host pathology (Figure 3B; Shirey et al., 2010). Studies with mouse macrophages in vitro and with cotton rats in vivo show that AAMs play a role in the response to infection. The macrophages are induced to express the marker signature of AAMs, which depends on the IL-4 and IL-13 receptor common alpha chain and STAT6, as well as TLR-4 and IFN-b. Infection in humans may also involve Th2 cytokines and AAMs. Although markers are insufficient to establish their role, other cell types, including innate and adaptive immune and epithelial cells, also modulate the host response. Since the earliest reports on AAMs, it has been assumed that these cells promote repair of host tissues after inflammation. Induction of Arg1 by IL-4 and IL-13 has been implicated in collagen deposition (Hesse et al., 2001) and degradation (reviewed in Wilson and Wynn, 2009). Imbalance in production and catabolism, associated with prolonged IL-13 effects on macrophages, promotes excessive fibrosis. Wynn and his colleagues and Murray, who has produced a conditional macrophage-specific deficiency of Arg1, provide evidence to support as well as question these hypotheses (El Kasmi et al., 2008; Pesce et al., 2009a, 2009b). Immunity Review A Ft IL-4, IL-13 TLR2 IL-4, IL-13 (requires IL-4Rα and STAT6) Inhibit Ft replication TLR2-dependent increase in: FIZZ1, Ym1, mannose receptor, arginase 1 Macrophage Alternatively activated macrophage Exogenous and endogenous IFN-β IL-10 Proinflammatory cytokines B Promotes Ft replication Kills host RSV IL-4, IL-13 Antiviral Increase IL-4Rα IFN-β TLR4-dependent increase in: FIZZ1, Ym1, mannose receptor, arginase 1 IL-4, IL-13 (requires IL-4Rα and STAT6) Lung macrophage Steroids COX-2 Repair of tissue damage IL-10 Parecoxib PGs Alternatively activated macrophage Pathology ? Predisposition to airway hyperreactivity Figure 3. Alternative Activation Amplification Loops in Infection (A) Model for the role of AAMs during Francisella tularensis (Ft) LVS infection. Ft infection of macrophages results in an initial proinflammatory response through a TLR2-dependent pathway (Cole et al., 2007), as well as an unknown intracellular sensor that leads to IFN-b production (Cole et al., 2008) and activation of caspase-1 through AIM2 and ASC sensors (Cole et al., 2008; Rathinam et al., 2010). IFN-b acts to inhibit bacterial replication, but production of IL-4 and IL-13 differentiates the macrophages to an AAM phenotype through an IL-4Ra- and TLR2-dependent mechanism that results in a microenvironment that promotes Ft replication, which is ultimately detrimental to the host. (B) Model for the role of AAM during RSV infection. RSV infection of macrophages leads to an early induction of proinflammatory cytokines and COX-2, which has been shown to mediate the observed lung pathology (Richardson et al., 2005). After this early proinflammatory period, macrophages produce their own IL-4 and IL-13 and differentiate into AAM through an IL-4Ra-, TLR4-, and IFN-b-dependent mechanism. This is thought to promote repair of damage caused by the earlier inflammatory process by inducing AAM markers including Arg1, FIZZ1, and Ym1. IL-10 acts to downregulate production of inflammatory cytokines. Figure adapted from Shirey et al. (2010) with permission. Although sterile foreign body reactions can depend on IL-4, IL-4Ra1 chain, and STAT6, repair of surgical wounds was independent of this pathway (Daley et al., 2010). The IL-13-specific receptor was not investigated although it has been shown to be essential for fibrosis in a parasitic model of S. mansoni granuloma formation (Ramalingam et al., 2008). As noted, Arg1 can be induced by a variety of different pathways, and cells other than macrophages also express receptors for IL-13. The reduction of fibrosis in egg granulomata in macrophage-selective ablation of the IL-13Ra1, in which induction of AAM is unaffected, confirms the existence of AAM-independent pathways of fibrogenesis, and also independent of TGF-b or MMP9, which are enhanced in this model. Macrophage-specific ablation of Arg1 enhances S. mansoni egg-induced fibrosis, an unexpected result. In wild-type mice, granulomata appear in liver after 7–10 weeks and diminish subsequently by Arg1-dependent downregulation, which is absent in Arg1-deficient mice. Macrophages express several transporters such as Cat2 (Thompson et al., 2008) as well as enzymes involved in L-arginine uptake and metabolism, but not a complete urea cycle. Ornithine decarboxylase, hydroxyproline, and polyamines have been implicated in additional properties of AAMs. Polyamines contribute to induction of Cadherin-1, after IL-4 treatment in vitro or Taenia crassiceps or allergen-induced activation in vivo (Van den Bossche et al., 2009). Cadherin-1 expression at the macrophage surface, together with catenin, mediates homotypic (cell fusion) and heterotypic interactions with CD103+ T cells. Alternative activation of macrophages has also been implicated in fibrosis after gamma herpes virus infection in mice (Gangadharan et al., 2008). It is not clear to what extent Th2 cytokines, AAMs, or fibroblasts contribute to noninfectious causes of fibrosis or whether combined targeting of IL-13 and TGF-b might prevent or reverse fibrosis. A remarkable example of a pathogenic role of IL-13 in chronic obstructive pulmonary disease (COPD) has been reported (Holtzman et al., 2009; Kim et al., 2008). COPD is a major cause of morbidity and mortality, in which lung failure is associated with chronic inflammation, mucous cell metaplasia, bronchial hyperreactivity, and fibrosis. The condition is often attributed to allergens and adaptive immune mechanisms, but this study provides convincing evidence that an initial transient acute viral infection in the lung can be followed after a period by activation of NKT cells, production of IL-13 by these cells, and by macrophages Immunity 32, May 28, 2010 ª2010 Elsevier Inc. 599 Immunity Review themselves. The macrophages upregulate IL-13Ra1 expression and become alternatively activated by an autocrine or paracrine mechanism. In an experimental mouse model of Sendai virus infection, bronchiolitis is associated with mucus production and airway hyperreactivity to methacholine. After the virus becomes barely detectable, NKT cells expressing semi-invariant Valpha14-Jalpha 18 TCR produce IL-13 through a CD1d-glycolipid-dependent mechanism, initiating a vicious circle of AAM amplification. In the mouse, the characteristic signature markers Arg1, Ym1 and Ym2, Fizz1, Mmp12, and Alox12e are now present. An analogous mechanism has been proposed for human COPD, with patient transplant-derived material to demonstrate the presence of NKT cells and IL-13 message and protein in macrophages (Holtzman et al., 2009). The critical role of IL-13 in the mouse model was demonstrated by macrophage depletion studies and blockade with soluble IL-13R2 protein. This provocative study shifts the pathogenic mechanism to the innate immune system. Improved AAM markers are needed for human tissue analysis and prospective studies in human subjects. Plasma Chitinase-1, a member of the chitinase family, allows quantitative stratification of COPD patients (Agapov et al., 2009). The question arises of genetic susceptibility to these sequelae of common virus infections, as does the possibility of therapeutic targeting of the IL-13 pathway. LPS tolerance, a refractory state in responses of the host and macrophages to repeated challenge with LPS, is known to involve NF-kB. Patients with sepsis can display features resembling alternative activation of monocytes. Porta and colleagues have shown that tolerance and alternative activation (M2 polarization) are related processes mediated by p50 homodimers, which lack a transcription activation domain of members of the NF-kB pathway (Porta et al., 2009). Studies were performed with human monocyte-derived macrophages and with mouse primary macrophages, in vitro and in vivo. P50 was shown to be a negative regulator of classical, M1 polarization and of IFN-b production, but played a positive, nonredundant role in induction of several signature M2-associated genes. Markers included selected chemokines (CCL2, CCL17, and CCL22), Arg1, Ym1, and Fizz1. There were some discrepancies between human and mouse phenotypes, however, and no reported involvement of IL-4 and IL-13 expression or of their receptors. P50 / mice lacked the characteristic AAM phenotype associated with Taenia crassiceps infection, consistent with the overall hypothesis. In another model, the prototypical proinflammatory function of TLR4 can be subverted by house dust mite allergen, which mimics MD2, its coreceptor, to induce IL-4 production (Trompette et al., 2009). Although IL-13 has been associated with disease-promoting activities, it can also play a protective role by virtue of its ability to regulate macrophages in an autoimmune myocarditis model of disease (Cihakova et al., 2008). Infection of mice with Coxsackie virus B3 induces a self-limiting myocarditis in most mouse strains, but a few strains develop severe myocardiopathy, with Th1 cell type inflammation, myosin antibodies, and fibrosis, especially in IL-13 / , but not IL-4 / , BALB/c mice. T cells are not known to express IL-13Ra, and the protective role of IL-13 has been attributed to macrophages. MRC1 expression was 600 Immunity 32, May 28, 2010 ª2010 Elsevier Inc. reduced in macrophages from the hearts of IL-13 or doubly deficient IL-13 and IL-4, but not IL-4-deficient, mice. PPARs and AAMs: Role in Metabolism, Inflammation, and Atherosclerosis Since the early observation by Glass and colleagues that PPAR gamma is strongly induced by IL-4, PPARs have been investigated in relation to lipid metabolism, macrophage polarization, obesity and insulin resistance, and atherogenesis (reviewed by Glass [Glass and Saijo, 2010] and Chawla [Chawla, 2010]). Macrophages express PPARg and PPARd; macrophage-specific deficient mice have been utilized in bone marrow chimera experiments of experimental atherosclerosis. Although there has been progress in analyzing the control of inflammation, the therapeutic application of PPAR ligand agonists via these receptors remains elusive. Macrophages in white adipose tissue in obese versus lean mice differ in phenotype, with features of CAMs in the former and of AAMs in the latter. By contrast, lipid-laden foam cells in atherosclerotic plaques have a distinct phenotype, not necessarily corresponding to the binary classification of M1- and M2-polarized cells. AAMs could play a role in smooth muscle cell migration and plaque rupture. IL-4 enhances uptake and oxidation of fatty acids and biogenesis of mitochondria, via STAT6, regulating programs controlled by PPARg and the coactivator protein PGC-1b. PPARg is dispensable for induction of AAM but required to sustain it. It plays a more complex role in limiting proinflammatory gene expression by LPS, preventing turnover of NCoR corepressor complexes and keeping such genes in the ‘‘off’’ position in AAMs, thus controlling the initiation, magnitude, and duration of inflammation. PPARg regulates primarily the metabolic phenotype of AAMs, whereas PPARd regulates the immune repertoire. PPARd is a sensor of triglyceride VLDL and contributes to macrophage numbers and phenotype in liver as well as adipose tissue. Mono-unsaturated fatty acids, such as oleic acid, synergize with IL-4 to enhance expression of AAM signature genes; PPARd may also play a role in the proliferative and anti-inflammatory effects of IL-4 on macrophages. Role of AAMs in Tumorigenesis Macrophages are a prominent component of the stroma and leukocyte infiltrate in human and experimental mouse tumors (DeNardo et al., 2009; Gocheva et al., 2010; Grivennikov et al., 2010; Hallam et al., 2009; Joyce and Pollard, 2009; Mantovani et al., 2008; Sinha et al., 2007). They interact with malignant epithelial, blood vessels and lymphatics, lymphocytes, innate cells, and extracellular matrix. They have been implicated in carcinogenesis, the angiogenic switch, local invasion, and metastasis. Systemic features of malignancy have also been ascribed to macrophages, locally and outside the actual tumor bed. It is established that they contribute trophic functions to the emergence of nascent tumor clones, phagocytose apoptotic tumor cells, influence the tissue response to hypoxia and, together with regulatory T lymphocytes, suppress Th1 cell and cytotoxic T lymphocyte antitumor responses. The nature of tumor-associated macrophages (TAMs) has become of great interest, though confusing because of phenotypic heterogeneity. TAMs have many properties of AAMs; myeloid-derived suppressor cells (MDSC) are less defined and Immunity Review in mouse contain infiltrating GR-1 intermediate CD11b+ monocytes, as well as GR-1 high CD11b+ granulocytic cells (Gabrilovich and Nagaraj, 2009). Some MDSC express F4/80 in the mouse and IL-4Ra, enabling them to respond to both IL-4 and IL-13. Innate and adaptive T cells as well as tumor cells can produce these cytokines, and some tumors also express the IL-4 and IL-13 alpha receptor (Mandruzzato et al., 2009). Several recent studies with experimental tumors in mice (transplantable as well as oncogene-induced) provide striking evidence that TAMs have much in common with AAMs. They contribute to local invasion through cathepsin B and S, promote angiogenesis and tumor growth through VEGF, and induce recruitment of other hemopoietic cells, through chemokines (Gocheva et al., 2010). AAMs as well as tumor cells themselves orchestrate tumor growth and spread through M-CSF, TNF, IL-10, TGF-b, and other products. The evidence that alternative activation of macrophages is important in promoting tumorigenesis includes expression of murine signature markers and dependence on the IL-4 and IL-13 common receptor alpha chain. Blockade of this receptor or its genetic ablation may therefore shift the host-tumor balance toward tumor rejection by Th1 cell-dependent effector mechanisms, such as IL-12 versus IL-10 production. A recent study (Weiss et al., 2009) combined treatment with IL-2 and anti-CD40 to induce a switch from M2 to M1 macrophage functions, depending on CCR2 and IFN-g. The contribution of TAM to this balance varied in different tumor models and could affect either primary or secondary growth. B cell-dependent mechanisms have been demonstrated in selected tumors (Andreu et al., 2010), with possible interactions with AAM Fc receptors. IL-13 and its receptors have been implicated in a different model of suppression of host immune effector responses to tumors (Fichtner-Feigl et al., 2008a). IL-4 or IL-13, acting through the IL13Ra1, is able to upregulate expression of the IL-13Ra2 polypeptide. TNF and NF-kB contribute in parallel to the STAT6 pathway. IL-13 acts on GR1 intermediate CD11b high monocytic cells, through variant AP1 transcription factor, to produce TGF-b. This pathway is responsible for suppression of tumor rejection by Th1 cell-type immune response. Treatment with anti-TNF or siRNA to block IL-13Ra2 reduces metastasis and promotes survival. In summary, AAMs are important candidates for therapeutic modulation of the tumor-host inflammatory interaction. However, AAM markers are urgently required to establish their contribution in naturally occurring human malignancy. Therapeutic Interventions As knowledge of the pathophysiologic pathways of IL-4 and IL-13 in human disease has grown, attempts are being made to achieve therapeutic blockade. In a well-controlled phase 2a trial (Wenzel et al., 2007), recombinant human pitrakinra showed promising results in ameliorating late-phase asthmatic response to allergen challenge in patients, by aerosol and subcutaneous routes. This agent, previously tested in cynomolgus monkeys, is a potent inhibitor of binding of both IL-4 and IL-13 to IL-4R receptor complexes, offering an advantage over previous attempts to inhibit IL-4 alone, IL-5, or IgE. Selective blockade of IL-13 signaling could offer further advantages, e.g., in a subpopulation of asthma patients (Wood- ruff et al., 2009). Various strategies have been employed to target IL-13 through receptor-specific antibodies, chimeric proteins, or soluble receptor (Blease, 2008). Proof-of-concept animal and early human studies have been undertaken, to ameliorate asthma and idiopathic lung fibrosis. Species differences need to be borne in mind, because in contrast with the mouse, human decoy IL-13 receptor is not secreted from cells (O’Toole et al., 2008). Novel strategies include functional variants based on analysis of human SNPs that demonstrate altered affinity for IL-13Ra2 and cell penetrant proteins or small molecules that target the signaling pathway through STAT 6. Structure-function studies should aid in the development of IL-13-specific therapeutic agents (LaPorte et al., 2008; Mitchell et al., 2010; Lupardus et al., 2010). Conclusion and Further Questions Although there has been striking progress in understanding the mechanisms and functions of AAM, much remains to be discovered. We have argued in favor of a restricted definition, shown the value of in situ analysis in mouse and man, and pointed to the possibility of selective targeting of pathogenic pathways through IL-13. Major human diseases, including infection, inflammation, fibrosis, and malignancy, demonstrate the twoedged nature of AAM function at different stages of disease. The need for validated human markers is apparent. Perhaps less obvious is a clearer understanding of what determines the spectrum of innate, classical, alternative, and other activation phenotypes in macrophage populations and individual cells. The trophic, antigen-presenting, and killing functions of AAMs need better characterization. Finally, does alternative activation of macrophages extend to other innate cells, in particular dendritic, NKT, and even nonhematopoietic cells? As in other fields of immunobiology, the alternative may indeed be the antecedent path in evolution. ACKNOWLEDGMENTS We thank colleagues for sharing unpublished results, Stefanie Vogel and Keri Ann Shirey for Figure 3, and Thiru Ramalingam for Figure 2. This review was prepared while S.G. was a visiting NCI/NIAID scholar and he thanks Giorgio Trinchieri and Alan Sher for their hospitality. F.O.M. was supported by the British Heart Foundation. REFERENCES Agapov, E., Battaile, J.T., Tidwell, R., Hachem, R., Patterson, G.A., Pierce, R.A., Atkinson, J.J., and Holtzman, M.J. (2009). Macrophage chitinase 1 stratifies chronic obstructive lung disease. Am. J. Respir. Cell Mol. Biol. 41, 379–384. Andreu, P., Johansson, M., Affara, N.I., Pucci, F., Tan, T., Junankar, S., Korets, L., Lam, J., Tawfik, D., DeNardo, D.G., et al. (2010). FcRgamma activation regulates inflammation-associated squamous carcinogenesis. Cancer Cell 17, 121–134. Androulidaki, A., Iliopoulos, D., Arranz, A., Doxaki, C., Schworer, S., Zacharioudaki, V., Margioris, A.N., Tsichlis, P.N., and Tsatsanis, C. (2009). The kinase Akt1 controls macrophage response to lipopolysaccharide by regulating microRNAs. Immunity 31, 220–231. Anthony, R.M., Urban, J.F., Jr., Alem, F., Hamed, H.A., Rozo, C.T., Boucher, J.L., Van Rooijen, N., and Gause, W.C. (2006). Memory T(H)2 cells induce alternatively activated macrophages to mediate protection against nematode parasites. Nat. Med. 12, 955–960. Bhattacharjee, A., Xu, B., Frank, D.A., Feldman, G.M., and Cathcart, M.K. (2006). Monocyte 15-lipoxygenase expression is regulated by a novel Immunity 32, May 28, 2010 ª2010 Elsevier Inc. 601 Immunity Review cytosolic signaling complex with protein kinase C delta and tyrosine-phosphorylated Stat3. J. Immunol. 177, 3771–3781. Blease, K. (2008). Therapeutics targeting IL-13 for the treatment of pulmonary inflammation and airway remodeling. Curr. Opin. Investig. Drugs 9, 1180–1184. Brown, G.D. (2006). Dectin-1: A signalling non-TLR pattern-recognition receptor. Nat. Rev. Immunol. 6, 33–43. Chawla, A. (2010). Control of macrophage activation and function by PPARs. Circ. Res. 106, 1559–1569. Chiaramonte, M.G., Mentink-Kane, M., Jacobson, B.A., Cheever, A.W., Whitters, M.J., Goad, M.E., Wong, A., Collins, M., Donaldson, D.D., Grusby, M.J., and Wynn, T.A. (2003). Regulation and function of the interleukin 13 receptor alpha 2 during a T helper cell type 2-dominant immune response. J. Exp. Med. 197, 687–701. Cihakova, D., Barin, J.G., Afanasyeva, M., Kimura, M., Fairweather, D., Berg, M., Talor, M.V., Baldeviano, G.C., Frisancho, S., Gabrielson, K., et al. (2008). Interleukin-13 protects against experimental autoimmune myocarditis by regulating macrophage differentiation. Am. J. Pathol. 172, 1195–1208. Cole, L.E., Shirey, K.A., Barry, E., Santiago, A., Rallabhandi, P., Elkins, K.L., Puche, A.C., Michalek, S.M., and Vogel, S.N. (2007). Toll-like receptor 2-mediated signaling requirements for Francisella tularensis live vaccine strain infection of murine macrophages. Infect. Immun. 75, 4127–4137. Cole, L.E., Santiago, A., Barry, E., Kang, T.J., Shirey, K.A., Roberts, Z.J., Elkins, K.L., Cross, A.S., and Vogel, S.N. (2008). Macrophage proinflammatory response to Francisella tularensis live vaccine strain requires coordination of multiple signaling pathways. J. Immunol. 180, 6885–6891. Daley, J.M., Brancato, S.K., Thomay, A.A., Reichner, J.S., and Albina, J.E. (2010). The phenotype of murine wound macrophages. J. Leukoc. Biol. 87, 59–67. De’Broski, R.H., Orekev, T., Roloson, A., Ilies, M., Perkins, C., O’Brien, W., Cederbaum, S., Christianson, S.W., Zimmermann, N., Rothenberg, M.E., and Finkelman, F.D. (2010). Arginine I suppreses IL-12/IL-23p40-driven intestinal inflammation during acute schistosomiasis. J. Immunol., in press. Published online May 5, 2010. 10.4049/jimmunol.0902009. Delgoffe, G.M., Kole, T.P., Zheng, Y., Zarek, P.E., Matthews, K.L., Xiao, B., Worley, P.F., Kozma, S.C., and Powell, J.D. (2009). The mTOR kinase differentially regulates effector and regulatory T cell lineage commitment. Immunity 30, 832–844. DeNardo, D.G., Barreto, J.B., Andreu, P., Vasquez, L., Tawfik, D., Kolhatkar, N., and Coussens, L.M. (2009). CD4(+) T cells regulate pulmonary metastasis of mammary carcinomas by enhancing protumor properties of macrophages. Cancer Cell 16, 91–102. Dickensheets, H., Vazquez, N., Sheikh, F., Gingras, S., Murray, P.J., Ryan, J.J., and Donnelly, R.P. (2007). Suppressor of cytokine signaling-1 is an IL-4-inducible gene in macrophages and feedback inhibits IL-4 signaling. Genes Immun. 8, 21–27. Doyle, A.G., Herbein, G., Montaner, L.J., Minty, A.J., Caput, D., Ferrara, P., and Gordon, S. (1994). Interleukin-13 alters the activation state of murine macrophages in vitro: Comparison with interleukin-4 and interferon-gamma. Eur. J. Immunol. 24, 1441–1445. El Kasmi, K.C., Qualls, J.E., Pesce, J.T., Smith, A.M., Thompson, R.W., HenaoTamayo, M., Basaraba, R.J., Konig, T., Schleicher, U., Koo, M.S., et al. (2008). Toll-like receptor-induced arginase 1 in macrophages thwarts effective immunity against intracellular pathogens. Nat. Immunol. 9, 1399–1406. Fichtner-Feigl, S., Terabe, M., Kitani, A., Young, C.A., Fuss, I., Geissler, E.K., Schlitt, H.J., Berzofsky, J.A., and Strober, W. (2008a). Restoration of tumor immunosurveillance via targeting of interleukin-13 receptor-alpha 2. Cancer Res. 68, 3467–3475. Fichtner-Feigl, S., Young, C.A., Kitani, A., Geissler, E.K., Schlitt, H.J., and Strober, W. (2008b). IL-13 signaling via IL-13R alpha2 induces major downstream fibrogenic factors mediating fibrosis in chronic TNBS colitis. Gastroenterology 135, 2003–2013. Gabrilovich, D.I., and Nagaraj, S. (2009). Myeloid-derived suppressor cells as regulators of the immune system. Nat. Rev. Immunol. 9, 162–174. Gangadharan, B., Hoeve, M.A., Allen, J.E., Ebrahimi, B., Rhind, S.M., Dutia, B.M., and Nash, A.A. (2008). Murine gammaherpesvirus-induced fibrosis is associated with the development of alternatively activated macrophages. J. Leukoc. Biol. 84, 50–58. Geissmann, F., Manz, M.G., Jung, S., Sieweke, M.H., Merad, M., and Ley, K. (2010). Development of monocytes, macrophages, and dendritic cells. Science 327, 656–661. Glass, C.K., and Saijo, K. (2010). Nuclear receptor transrepression pathways that regulate inflammation. Nat. Rev. Immunol. 10, 365–376. Gocheva, V., Wang, H.W., Gadea, B.B., Shree, T., Hunter, K.E., Garfall, A.L., Berman, T., and Joyce, J.A. (2010). IL-4 induces cathepsin protease activity in tumor-associated macrophages to promote cancer growth and invasion. Genes Dev. 24, 241–255. Gordon, S. (2008). Macrophages and phagocytosis. In Fundamental Immunology, W.E. Paul, ed. (Philadelphia, PA: Lippincott Raven), p. 547. Gratchev, A., Schledzewski, K., Guillot, P., and Goerdt, S. (2001). Alternatively activated antigen-presenting cells: Molecular repertoire, immune regulation, and healing. Skin Pharmacol. Appl. Skin Physiol. 14, 272–279. Grivennikov, S.I., Greten, F.R., and Karin, M. (2010). Immunity, inflammation, and cancer. Cell 140, 883–899. Hallam, S., Escorcio-Correia, M., Soper, R., Schultheiss, A., and Hagemann, T. (2009). Activated macrophages in the tumour microenvironment-dancing to the tune of TLR and NF-kappaB. J. Pathol. 219, 143–152. Heinsbroek, S.E., Kamen, L.A., Taylor, P.R., Brown, G.D., Swanson, J., and Gordon, S. (2009). Actin and phosphoinositide recruitment to fully formed Candida albicans phagosomes in mouse macrophages. J. Innate Immunol. 1, 244–253. Heller, N.M., Qi, X., Junttila, I.S., Shirey, K.A., Vogel, S.N., Paul, W.E., and Keegan, A.D. (2008). Type I IL-4Rs selectively activate IRS-2 to induce target gene expression in macrophages. Sci. Signal. 1, ra17. Helming, L., and Gordon, S. (2009). Molecular mediators of macrophage fusion. Trends Cell Biol. 19, 514–522. Helming, L., Tomasello, E., Kyriakides, T.R., Martinez, F.O., Takai, T., Gordon, S., and Vivier, E. (2008). Essential role of DAP12 signaling in macrophage programming into a fusion-competent state. Sci. Signal. 1, ra11. Herbert, D.R., Holscher, C., Mohrs, M., Arendse, B., Schwegmann, A., Radwanska, M., Leeto, M., Kirsch, R., Hall, P., Mossmann, H., et al. (2004). Alternative macrophage activation is essential for survival during schistosomiasis and downmodulates T helper 1 responses and immunopathology. Immunity 20, 623–635. Fallon, P.G., Ballantyne, S.J., Mangan, N.E., Barlow, J.L., Dasvarma, A., Hewett, D.R., McIlgorm, A., Jolin, H.E., and McKenzie, A.N. (2006). Identification of an interleukin (IL)-25-dependent cell population that provides IL-4, IL-5, and IL-13 at the onset of helminth expulsion. J. Exp. Med. 203, 1105–1116. Hesse, M., Modolell, M., La Flamme, A.C., Schito, M., Fuentes, J.M., Cheever, A.W., Pearce, E.J., and Wynn, T.A. (2001). Differential regulation of nitric oxide synthase-2 and arginase-1 by type 1/type 2 cytokines in vivo: Granulomatous pathology is shaped by the pattern of L-arginine metabolism. J. Immunol. 167, 6533–6544. Fernandez-Boyanapalli, R.F., Frasch, S.C., McPhillips, K., Vandivier, R.W., Harry, B.L., Riches, D.W., Henson, P.M., and Bratton, D.L. (2009). Impaired apoptotic cell clearance in CGD due to altered macrophage programming is reversed by phosphatidylserine-dependent production of IL-4. Blood 113, 2047–2055. Holscher, C., Arendse, B., Schwegmann, A., Myburgh, E., and Brombacher, F. (2006). Impairment of alternative macrophage activation delays cutaneous leishmaniasis in nonhealing BALB/c mice. J. Immunol. 176, 1115–1121. Fichtner-Feigl, S., Strober, W., Kawakami, K., Puri, R.K., and Kitani, A. (2006). IL-13 signaling through the IL-13alpha2 receptor is involved in induction of TGF-beta1 production and fibrosis. Nat. Med. 12, 99–106. 602 Immunity 32, May 28, 2010 ª2010 Elsevier Inc. Holtzman, M.J., Byers, D.E., Benoit, L.A., Battaile, J.T., You, Y., Agapov, E., Park, C., Grayson, M.H., Kim, E.Y., and Patel, A.C. (2009). Immune pathways for translating viral infection into chronic airway disease. Adv. Immunol. 102, 245–276. Immunity Review Ishii, M., Wen, H., Corsa, C.A., Liu, T., Coelho, A.L., Allen, R.M., Carson, W.F., IV, Cavassani, K.A., Li, X., Lukacs, N.W., et al. (2009). Epigenetic regulation of the alternatively activated macrophage phenotype. Blood 114, 3244–3254. Martinez, F.O., Helming, L., and Gordon, S. (2009). Alternative activation of macrophages: An immunologic functional perspective. Annu. Rev. Immunol. 27, 451–483. Jenkins, S.J., and Allen, J.E. (2010). Similarity and diversity in macrophage activation by nematodes, trematodes, and cestodes. J. Biomed. Biotechnol. 2010, 262609. Mitchell, J., Dimov, V., and Townley, R.G. (2010). IL-13 and the IL-13 receptor as therapeutic targets for asthma and allergic disease. Curr. Opin. Investig. Drugs 11, 527–534. Joyce, J.A., and Pollard, J.W. (2009). Microenvironmental regulation of metastasis. Nat. Rev. Cancer 9, 239–252. Mohrs, K., Wakil, A.E., Killeen, N., Locksley, R.M., and Mohrs, M. (2005). A two-step process for cytokine production revealed by IL-4 dual-reporter mice. Immunity 23, 419–429. Junttila, I.S., Mizukami, K., Dickensheets, H., Meier-Schellersheim, M., Yamane, H., Donnelly, R.P., and Paul, W.E. (2008). Tuning sensitivity to IL-4 and IL-13: Differential expression of IL-4Ralpha, IL-13Ralpha1, and gammac regulates relative cytokine sensitivity. J. Exp. Med. 205, 2595–2608. Mokoena, T., and Gordon, S. (1985). Human macrophage activation. Modulation of mannosyl, fucosyl receptor activity in vitro by lymphokines, gamma and alpha interferons, and dexamethasone. J. Clin. Invest. 75, 624–631. Kahnert, A., Seiler, P., Stein, M., Bandermann, S., Hahnke, K., Mollenkopf, H., and Kaufmann, S.H. (2006). Alternative activation deprives macrophages of a coordinated defense program to Mycobacterium tuberculosis. Eur. J. Immunol. 36, 631–647. Montaner, L.J., da Silva, R.P., Sun, J., Sutterwala, S., Hollinshead, M., Vaux, D., and Gordon, S. (1999). Type 1 and type 2 cytokine regulation of macrophage endocytosis: differential activation by IL-4/IL-13 as opposed to IFNgamma or IL-10. J. Immunol. 162, 4606–4613. Kawashima, R., Kawamura, Y.I., Kato, R., Mizutani, N., Toyama-Sorimachi, N., and Dohi, T. (2006). IL-13 receptor alpha2 promotes epithelial cell regeneration from radiation-induced small intestinal injury in mice. Gastroenterology 131, 130–141. Moreno, J.L., Kaczmarek, M., Keegan, A.D., and Tondravi, M. (2003). IL-4 suppresses osteoclast development and mature osteoclast function by a STAT6-dependent mechanism: Irreversible inhibition of the differentiation program activated by RANKL. Blood 102, 1078–1086. Kim, E.Y., Battaile, J.T., Patel, A.C., You, Y., Agapov, E., Grayson, M.H., Benoit, L.A., Byers, D.E., Alevy, Y., Tucker, J., et al. (2008). Persistent activation of an innate immune response translates respiratory viral infection into chronic lung disease. Nat. Med. 14, 633–640. Moreno, J.L., Mikhailenko, I., Tondravi, M.M., and Keegan, A.D. (2007). IL-4 promotes the formation of multinucleated giant cells from macrophage precursors by a STAT6-dependent, homotypic mechanism: Contribution of E-cadherin. J. Leukoc. Biol. 82, 1542–1553. Kuroda, E., Ho, V., Ruschmann, J., Antignano, F., Hamilton, M., Rauh, M.J., Antov, A., Flavell, R.A., Sly, L.M., and Krystal, G. (2009). SHIP represses the generation of IL-3-induced M2 macrophages by inhibiting IL-4 production from basophils. J. Immunol. 183, 3652–3660. Moro, K., Yamada, T., Tanabe, M., Takeuchi, T., Ikawa, T., Kawamoto, H., Furusawa, J., Ohtani, M., Fujii, H., and Koyasu, S. (2009). Innate production of T(H)2 cytokines by adipose tissue-associated c-Kit(+)Sca-1(+) lymphoid cells. Nature 463, 540–544. Kurowska-Stolarska, M., Stolarski, B., Kewin, P., Murphy, G., Corrigan, C.J., Ying, S., Pitman, N., Mirchandani, A., Rana, B., van Rooijen, N., et al. (2009). IL-33 amplifies the polarization of alternatively activated macrophages that contribute to airway inflammation. J. Immunol. 183, 6469–6477. Mosser, D.M., and Edwards, J.P. (2008). Exploring the full spectrum of macrophage activation. Nat. Rev. Immunol. 8, 958–969. Kzhyshkowska, J., and Krusell, L. (2009). Cross-talk between endocytic clearance and secretion in macrophages. Immunobiology 214, 576–593. Munitz, A., Waddell, A., Seidu, L., Cole, E.T., Ahrens, R., Hogan, S.P., and Rothenberg, M.E. (2008). Resistin-like molecule alpha enhances myeloid cell activation and promotes colitis. J. Allergy Clin. Immunol. 122, 1200–1207. LaPorte, S.L., Juo, Z.S., Vaclavikova, J., Colf, L.A., Qi, X., Heller, N.M., Keegan, A.D., and Garcia, K.C. (2008). Molecular and structural basis of cytokine receptor pleiotropy in the interleukin-4/13 system. Cell 132, 259–272. Nair, M.G., Du, Y., Perrigoue, J.G., Zaph, C., Taylor, J.J., Goldschmidt, M., Swain, G.P., Yancopoulos, G.D., Valenzuela, D.M., Murphy, A., et al. (2009). Alternatively activated macrophage-derived RELM-{alpha} is a negative regulator of type 2 inflammation in the lung. J. Exp. Med. 206, 937–952. Linehan, S.A., Coulson, P.S., Wilson, R.A., Mountford, A.P., Brombacher, F., Martinez-Pomares, L., and Gordon, S. (2003). IL-4 receptor signaling is required for mannose receptor expression by macrophages recruited to granulomata but not resident cells in mice infected with Schistosoma mansoni. Lab. Invest. 83, 1223–1231. Neill, D.R., Wong, S.H., Bellosi, A., Flynn, R.J., Daly, M., Langford, T.K., Bucks, C., Kane, C.M., Fallon, P.G., Pannell, R., et al. (2010). Nuocytes represent a new innate effector leukocyte that mediates type-2 immunity. Nature 464, 1367–1370. Locksley, R.M. (2010). Asthma and allergic inflammation. Cell 140, 777–783. O’Shea, J.J., and Paul, W.E. (2010). Mechanisms underlying lineage commitment and plasticity of helper CD4+ T cells. Science 327, 1098–1102. Loke, P., MacDonald, A.S., and Allen, J.E. (2000). Antigen-presenting cells recruited by Brugia malayi induce Th2 differentiation of naive CD4(+) T cells. Eur. J. Immunol. 30, 1127–1135. Loke, P., Nair, M.G., Parkinson, J., Guiliano, D., Blaxter, M., and Allen, J.E. (2002). IL-4 dependent alternatively-activated macrophages have a distinctive in vivo gene expression phenotype. BMC Immunol. 3, 7. Lupardus, P.J., Birnbaum, M.E., and Garcia, K.C. (2010). Molecular basis for shared cytokine recognition revealed in the structure of an unusually high affinity complex between IL-13 and IL-13Ralpha2. Structure 18, 332–342. Mandruzzato, S., Solito, S., Falisi, E., Francescato, S., Chiarion-Sileni, V., Mocellin, S., Zanon, A., Rossi, C.R., Nitti, D., Bronte, V., and Zanovello, P. (2009). IL4Ralpha+ myeloid-derived suppressor cell expansion in cancer patients. J. Immunol. 182, 6562–6568. Mantovani, A., Sica, A., and Locati, M. (2005). Macrophage polarization comes of age. Immunity 23, 344–346. Mantovani, A., Allavena, P., Sica, A., and Balkwill, F. (2008). Cancer-related inflammation. Nature 454, 436–444. Martinez, F.O., Gordon, S., Locati, M., and Mantovani, A. (2006). Transcriptional profiling of the human monocyte-to-macrophage differentiation and polarization: New molecules and patterns of gene expression. J. Immunol. 177, 7303–7311. O’Toole, M., Legault, H., Ramsey, R., Wynn, T.A., and Kasaian, M.T. (2008). A novel and sensitive ELISA reveals that the soluble form of IL-13R-alpha2 is not expressed in plasma of healthy or asthmatic subjects. Clin. Exp. Allergy 38, 594–601. Pelegrin, P., and Surprenant, A. (2009). Dynamics of macrophage polarization reveal new mechanism to inhibit IL-1beta release through pyrophosphates. EMBO J. 28, 2114–2127. Pesce, J., Kaviratne, M., Ramalingam, T.R., Thompson, R.W., Urban, J.F., Jr., Cheever, A.W., Young, D.A., Collins, M., Grusby, M.J., and Wynn, T.A. (2006). The IL-21 receptor augments Th2 effector function and alternative macrophage activation. J. Clin. Invest. 116, 2044–2055. Pesce, J.T., Ramalingam, T.R., Mentink-Kane, M.M., Wilson, M.S., El Kasmi, K.C., Smith, A.M., Thompson, R.W., Cheever, A.W., Murray, P.J., and Wynn, T.A. (2009a). Arginase-1-expressing macrophages suppress Th2 cytokinedriven inflammation and fibrosis. PLoS Pathog. 5, e1000371. Pesce, J.T., Ramalingam, T.R., Wilson, M.S., Mentink-Kane, M.M., Thompson, R.W., Cheever, A.W., Urban, J.F., Jr., and Wynn, T.A. (2009b). Retnla (relmalpha/fizz1) suppresses helminth-induced Th2-type immunity. PLoS Pathog. 5, e1000393. Porta, C., Rimoldi, M., Raes, G., Brys, L., Ghezzi, P., Di Liberto, D., Dieli, F., Ghisletti, S., Natoli, G., De Baetselier, P., et al. (2009). Tolerance and M2 Immunity 32, May 28, 2010 ª2010 Elsevier Inc. 603 Immunity Review (alternative) macrophage polarization are related processes orchestrated by p50 nuclear factor kappaB. Proc. Natl. Acad. Sci. USA 106, 14978–14983. Steinman, R.M., and Idoyaga, J. (2010). Features of the dendritic cell lineage. Immunol. Rev. 234, 5–17. Puig-Kroger, A., Sierra-Filardi, E., Dominguez-Soto, A., Samaniego, R., Corcuera, M.T., Gomez-Aguado, F., Ratnam, M., Sanchez-Mateos, P., and Corbi, A.L. (2009). Folate receptor beta is expressed by tumor-associated macrophages and constitutes a marker for M2 anti-inflammatory/regulatory macrophages. Cancer Res. 69, 9395–9403. Stout, R.D. (2010). Editorial: Macrophage functional phenotypes: No alternatives in dermal wound healing? J. Leukoc. Biol. 87, 19–21. Stout, R.D., Jiang, C., Matta, B., Tietzel, I., Watkins, S.K., and Suttles, J. (2005). Macrophages sequentially change their functional phenotype in response to changes in microenvironmental influences. J. Immunol. 175, 342–349. Ramalingam, T.R., Pesce, J.T., Sheikh, F., Cheever, A.W., Mentink-Kane, M.M., Wilson, M.S., Stevens, S., Valenzuela, D.M., Murphy, A.J., Yancopoulos, G.D., et al. (2008). Unique functions of the type II interleukin 4 receptor identified in mice lacking the interleukin 13 receptor alpha1 chain. Nat. Immunol. 9, 25–33. Syed, F., Huang, C.C., Li, K., Liu, V., Shang, T., Amegadzie, B.Y., Griswold, D.E., Song, X.Y., and Li, L. (2007). Identification of interleukin-13 related biomarkers using peripheral blood mononuclear cells. Biomarkers 12, 414–423. Rathinam, V.A., Jiang, Z., Waggoner, S.N., Sharma, S., Cole, L.E., Waggoner, L., Vanaja, S.K., Monks, B.G., Ganesan, S., Latz, E., et al. (2010). The AIM2 inflammasome is essential for host defense against cytosolic bacteria and DNA viruses. Nat. Immunol. 11, 395–402. Taganov, K.D., Boldin, M.P., Chang, K.J., and Baltimore, D. (2006). NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc. Natl. Acad. Sci. USA 103, 12481–12486. Rauh, M.J., Ho, V., Pereira, C., Sham, A., Sly, L.M., Lam, V., Huxham, L., Minchinton, A.I., Mui, A., and Krystal, G. (2005). SHIP represses the generation of alternatively activated macrophages. Immunity 23, 361–374. Thompson, R.W., Pesce, J.T., Ramalingam, T., Wilson, M.S., White, S., Cheever, A.W., Ricklefs, S.M., Porcella, S.F., Li, L., Ellies, L.G., and Wynn, T.A. (2008). Cationic amino acid transporter-2 regulates immunity by modulating arginase activity. PLoS Pathog. 4, e1000023. Reece, J.J., Siracusa, M.C., and Scott, A.L. (2006). Innate immune responses to lung-stage helminth infection induce alternatively activated alveolar macrophages. Infect. Immun. 74, 4970–4981. Reese, T.A., Liang, H.E., Tager, A.M., Luster, A.D., Van Rooijen, N., Voehringer, D., and Locksley, R.M. (2007). Chitin induces accumulation in tissue of innate immune cells associated with allergy. Nature 447, 92–96. Richardson, J.Y., Ottolini, M.G., Pletneva, L., Boukhvalova, M., Zhang, S., Vogel, S.N., Prince, G.A., and Blanco, J.C. (2005). Respiratory syncytial virus (RSV) infection induces cyclooxygenase 2: a potential target for RSV therapy. J. Immunol. 174, 4356–4364. Rodriguez-Sosa, M., Satoskar, A.R., Calderon, R., Gomez-Garcia, L., Saavedra, R., Bojalil, R., and Terrazas, L.I. (2002). Chronic helminth infection induces alternatively activated macrophages expressing high levels of CCR5 with low interleukin-12 production and Th2-biasing ability. Infect. Immun. 70, 3656– 3664. Roy, B., Bhattacharjee, A., Xu, B., Ford, D., Maizel, A.L., and Cathcart, M.K. (2002). IL-13 signal transduction in human monocytes: Phosphorylation of receptor components, association with Jaks, and phosphorylation/activation of Stats. J. Leukoc. Biol. 72, 580–589. Ruschmann, J., Ho, V., Antignano, F., Kuroda, E., Lam, V., Ibaraki, M., Snyder, K., Kim, C., Flavell, R.A., Kawakami, T., et al. (2010). Tyrosine phosphorylation of SHIP promotes its proteosomal degradation. Exp. Hematol. 38, 392–402. Saenz, S.A., Siracusa, M.C., Perrigoue, J.G., Spencer, S.P., Urban, J.F., Jr., Tocker, J.E., Budelsky, A.L., Kleinschek, M.A., Kastelein, R.A., Kambayashi, T., et al. (2010). IL25 elicits a multipotent progenitor cell population that promotes T(H)2 cytokine responses. Nature 464, 1362–1366. Scotton, C.J., Martinez, F.O., Smelt, M.J., Sironi, M., Locati, M., Mantovani, A., and Sozzani, S. (2005). Transcriptional profiling reveals complex regulation of the monocyte IL-1 beta system by IL-13. J. Immunol. 174, 834–845. Shirey, K.A., Cole, L.E., Keegan, A.D., and Vogel, S.N. (2008). Francisella tularensis live vaccine strain induces macrophage alternative activation as a survival mechanism. J. Immunol. 181, 4159–4167. Shirey, K.A., Pletneva, L.M., Puche, A.C., Keegan, A.D., Prince, G.A., Blanco, J.C., and Vogel, S.N. (2010). Control of RSV-induced lung injury by alternatively activated macrophages is IL-4Ra-. TLR4-, and IFN-b-dependent. Mucosal Immunol. 3, 291–300. Sinha, P., Clements, V.K., Bunt, S.K., Albelda, S.M., and Ostrand-Rosenberg, S. (2007). Cross-talk between myeloid-derived suppressor cells and macrophages subverts tumor immunity toward a type 2 response. J. Immunol. 179, 977–983. Stein, M., Keshav, S., Harris, N., and Gordon, S. (1992). Interleukin 4 potently enhances murine macrophage mannose receptor activity: A marker of alternative immunologic macrophage activation. J. Exp. Med. 176, 287–292. 604 Immunity 32, May 28, 2010 ª2010 Elsevier Inc. Tili, E., Michaille, J.J., Cimino, A., Costinean, S., Dumitru, C.D., Adair, B., Fabbri, M., Alder, H., Liu, C.G., Calin, G.A., and Croce, C.M. (2007). Modulation of miR-155 and miR-125b levels following lipopolysaccharide/TNF-alpha stimulation and their possible roles in regulating the response to endotoxin shock. J. Immunol. 179, 5082–5089. Trompette, A., Divanovic, S., Visintin, A., Blanchard, C., Hegde, R.S., Madan, R., Thorne, P.S., Wills-Karp, M., Gioannini, T.L., Weiss, J.P., and Karp, C.L. (2009). Allergenicity resulting from functional mimicry of a Toll-like receptor complex protein. Nature 457, 585–588. van de Veerdonk, F.L., Marijnissen, R.J., Kullberg, B.J., Koenen, H.J., Cheng, S.C., Joosten, I., van den Berg, W.B., Williams, D.L., van der Meer, J.W., Joosten, L.A., and Netea, M.G. (2009). The macrophage mannose receptor induces IL-17 in response to Candida albicans. Cell Host Microbe 5, 329–340. Van den Bossche, J., Bogaert, P., van Hengel, J., Guerin, C.J., Berx, G., Movahedi, K., Van den Bergh, R., Pereira-Fernandes, A., Geuns, J.M., Pircher, H., et al. (2009). Alternatively activated macrophages engage in homotypic and heterotypic interactions through IL-4 and polyamine-induced E-cadherin/ catenin complexes. Blood 114, 4664–4674. Varin, A., and Gordon, S. (2009). Alternative activation of macrophages: Immune function and cellular biology. Immunobiology 214, 630–641. Varin, A., Mukhopadhyay, S., Herbein, G., and Gordon, S. (2009). Alternative activation of macrophages by IL-4 impairs phagocytosis of pathogens but potentiates microbial-induced signalling and cytokine secretion. Blood 115, 353–362. Voehringer, D., Reese, T.A., Huang, X., Shinkai, K., and Locksley, R.M. (2006). Type 2 immunity is controlled by IL-4/IL-13 expression in hematopoietic noneosinophil cells of the innate immune system. J. Exp. Med. 203, 1435–1446. Weiss, J.M., Back, T.C., Scarzello, A.J., Subleski, J.J., Hall, V.L., Stauffer, J.K., Chen, X., Micic, D., Alderson, K., Murphy, W.J., and Wiltrout, R.H. (2009). Successful immunotherapy with IL-2/anti-CD40 induces the chemokine-mediated mitigation of an immunosuppressive tumor microenvironment. Proc. Natl. Acad. Sci. USA 106, 19455–19460. Wenzel, S., Wilbraham, D., Fuller, R., Getz, E.B., and Longphre, M. (2007). Effect of an interleukin-4 variant on late phase asthmatic response to allergen challenge in asthmatic patients: results of two phase 2a studies. Lancet 370, 1422–1431. Wilson, M.S., and Wynn, T.A. (2009). Pulmonary fibrosis: Pathogenesis, etiology and regulation. Mucosal Immunol. 2, 103–121. Woodruff, P.G., Modrek, B., Choy, D.F., Jia, G., Abbas, A.R., Ellwanger, A., Koth, L.L., Arron, J.R., and Fahy, J.V. (2009). T-helper type 2-driven inflammation defines major subphenotypes of asthma. Am. J. Respir. Crit. Care Med. 180, 388–395.
© Copyright 2026