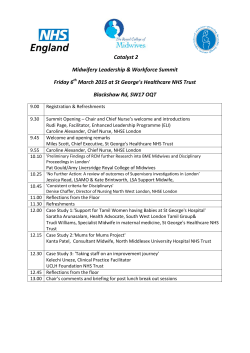
Schedule Schedule
Schedule Schedule 08:30 – 9:00 Registration 10:50 – 11:20 Refreshments 9:00 – 9:30 Opening and Introduction 11:20 – 13:00 Robin Daly Chairman, Yes to Life Morning session 2: Re-examining our evidence base and the barriers to cheap, effective solutions Dr Vijayendra Murthy Bach. Ayurvedic Med & Surgery, Master of Surgery (India), B.Nat, Master of Public Health (New Zealand) Opening address and introduction to the Think Tank Summit About the Think Tank. The main drivers of the healthcare crisis. Introduction to the morning speakers. Robert Verkerk PhD How can we better evaluate clinical practice, outcomes and experience? Executive & scientific director, Alliance for Natural Health International Evidence-based medicine (EBM) does not always best serve the public or health professionals. Comparative Effectiveness Research and other collaborative approaches add a critically important dimension to evidence, particularly as it relates to determining best clinical practice and evaluating multi-modality interventions. How can we take into account clinical experience and improve on clinical decisionmaking based on the existing evidence hierarchy system? Opening and introduction to the Think Tank Summit content Highlighting consensus, uncertainties and challenges; identifying quick-fixes to improve primary and secondary care outcomes in the face of an ageing population and spiraling chronic disease crisis. Robert Scott Bell Presenter & broadcaster, Robert Scott Bell Show, NaturalNews Radio, UK Health Radio Prof Karol Sikora 9:30 – 10:50 Morning Session 1: Chronic disease and healthcare systems – new directions Ben van Ommen PhD Principal Scientist, TNO (Netherlands Organisation for Applied Scientific Research) The need for flexibility in clinical practice aimed at optimising outcomes The guideline-based protocols developed by the National Institute for Health and Care Excellence (NICE) currently used by NHS doctors relies heavily on pharmaceutical prescription and surgery and do not sufficiently take into account key factors such as patient individuality, epigenetics and clinical experience. Prevention and treatment protocols need to be more flexible, take into account a whole-body perspective, consider the individual’s epigenetic background and be geared to effectiveness, as distinct from efficacy, as determined in RCTs. How systems flexibility changes medicine to personalised healthcare By applying the concept of systems flexibility to all drivers of health and disease, personalised approaches to prevention and treatment have emerged. These require new diagnostics and pave the way for the new paradigm of personalised lifestyle medicine. Most importantly, they encourage self-empowerment and aim to resolve underlying causes of disease, so replacing the disease management and symptom control practices that typify current mainstream healthcare. Dr Jonathan Wright Ralph Moss PhD With specific focus on cancer, validated approaches to delivery of more effective, yet significantly less costly, primary and secondary care are discussed, along with the need for a sea change in the training of oncologists and related health professionals, as well as the associated medico-legal framework. After 45 years practicing lifestyle medicine… Michael Ash Which areas of the science are emerging, which are well established, and which are yet to be adequately recognised? The central role of the gut microbiome, how selfcare/disease prevention approaches could be encouraged and healthcare education reformed, with a view to reducing demand and costs of mainstream healthcare. Facilitator Robert Scott Bell Dr Rangan Chatterjee Think tank discussion session 1 NHS GP and functional medicine practitioner Conventional vs functional medicine clinical practice models: Perspectives from a UK general practitioner Challenges for effective primary healthcare in a mainstream setting; comparing conventional and functional medicine models of clinical practice; and lessons on continuing professional development, patient empowerment and self-responsibility. Adjunct Faculty Member, Institute for Functional Medicine (USA); NL Education (UK) Listening to the science with deaf ears. Principal, Cancer Decisions, USA Insights on cost-effective, patient-centred oncology Medical Director, Tahoma Clinic, USA A sea change in healthcare practice is required if non-pharmaceutical and integrative approaches are to be more widely adopted. Dr Wright draws from nearly half a century of clinical experience and discusses the potential for dramatic improvements in outcome using integrative interventions for a diverse range of common and debilitating diseases. Medical Director, Cancer Partners UK; Dean of Medicine, University of Buckingham (UK) Facilitator: Dr Rangan Chatterjee Think tank discussion session 2 13:00 – 14:00 Lunch break Schedule 14:00 – 15:40 Dr Robin Youngson Afternoon session 1: Patient-centred care, business and politics – towards effective and sustainable healthcare Schedule 16:10 – 17:15 Afternoon Session 2: Discussion & summaries Facilitator: Robert Scott Bell Structured think tank discussion 4 (plenary) Issues for discussion: challenges facing improved adoption of lifestyle medicine; cost and accessibility; benefits of individualised, whole body, multi-modality, functional approaches; making epigenetics matter; equalities and inequalities; comparison between the UK’s NHS and the US healthcare system; priorities for mainstream health renewal Director, Hearts in Healthcare, NZ Compassion and empathy in healthcare Compassionate care saves time, money and lives. Approaches that could help to facilitate improved integration of compassionate care into mainstream healthcare are discussed. Robert Scott Bell Smriti Singh Personal Health Budgets, Regional Lead for London, NHS England Presenter & broadcaster, Robert Scott Bell Show Speaker Soundbites: “The biggest shift in your perspective today” Putting the patient at the centre Much lip-service has been given to patient-centred healthcare. Smriti Singh shows how Personalised Health Budgets can encourage autonomy and self-care, increase personal choice significantly and place the patient at the centre of their own chronic disease management or prevention programme. Vivienne Lyfar-Cissé PhD Principal Clinical Biochemist, Brighton and Sussex University Hospitals NHS Trust, Chair – NHS BME Network Towards a healthcare solution for all Despite the rhetoric around patient-centred care, which is firmly embedded in the NHS Constitution, inequality is rampant. Services often inadequately account for social and economic causes of disease or accounting for the cultural and individual needs of both patients and healthcare providers. We need to urgently move towards a more flexible, non-discriminatory healthcare system that extends into communities and families, is relevant both to patients and frontline health professionals and caters for all needs, irrespective of social strata, cultural background, ethnicity or genetic predisposition. Robert Verkerk PhD Executive & scientific director, Alliance for Natural Health International Bottom-up and top-down reform of healthcare Excessive drug dependency, conflicting healthcare paradigms and information, medical training biases, a regulatory environment that stifles innovation and insufficient individualisation are among the factors limiting adoption of personalised lifestyle medicine approaches. While top-down policy shifts are necessary, sea changes are required to the medical curriculum, to clinical decision-making and practice models, and to individual and corporate responsibility in healthcare. Public engagement in this process is vital. Facilitator: Vivienne Lyfar-Cissé PhD Think tank discussion session 3 15:40 – 16:10 Refreshments Robert Verkerk PhD Summary and conclusions from the day Robin Daly Dr Rangan Chatterjee Vivienne Lyfar-Cissé PhD Robert Scott Bell Robert Verkerk PhD Robin Daly Closing remarks 17:15 Close
© Copyright 2026