Physical examination of the chest. Inspection. Chest pain.
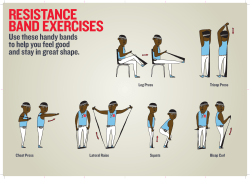
Physical examination of the chest. Inspection. Chest pain. Inspection Landmark on chest wall. Physical examination of the chest Traditional physical examination of the chest includes four methods. Inspection Palpation Percussion Auscultation - warm circumstance, well light - sitting or supine position (according to the need for the examination or the ill condition) Breath movement: healthy subject is steady and regular. Inspiration: active movement, leading to the expansion of the lung (air flowing into the lung). Expiration: passive movement, depending on the elastical recoil of the lung and chest---air in the lung is exhaled. Males and children: diaphragmatic respiration. Female: thoracic respiration Respiratory rate: 16-20/min (in newborn and children higher). Tachypnoe: >24/min (fever, pain, anemia, hyperthyreoidism and heart failure), bradypnoe<12/min (overdose anesthetics or sedatives or elevated intracranial pressure). Chest wall deformities Pectus excavatum Sternum sunken into the chest Pectus carinatum sternum protruding from the chest Pectus excavatum Scoliosis Kyphosis Kyphoscoliosis Inspection Nutrition, skin, lymph nodes, development of skeleton muscles - Vein: normally the vein on chest wall is not obviuos. (if v. cava or their branches are blocked---veins become full form varicose) Chest wall deformities IMPORTANT: Affects the percussion Affects the breath and circulation Palpation Retraction of hemithorax Obstruction of free air flowing into the respiratory tract (atelectasis, pulmonary fibrosis, extensive thickening fibrotic pleura) Bulging of hemithorax Massive pleural effusion, tension pneumothorax, severe emphysema Palpation Subcutaneous emphysema: air enters and stores in subcutaneous tissue (pressing the skin produce „crepitation” or grasping snow). Tenderness: normally ther is no tenderness on chest wall (intercostal neuritis, costal cartilagitis, soft tissue inflammation, rib fractures, pain on sternum occurs in leukemia, myelodysplasia). Respiratory expansion-check whether expansion is equal (place your thumbs along each costal margin, and your hands along the lateral rib cage). Tactile fremitus-the patient says „ninety-nine”, whilst physician sense with ulnar aspect of hand for changes in sound conduction. Pleural friction fremitus (inspiration and expiration too) Examination of the breast Inspection: symmetry (enlargement of one breast may denote congenital deformation, cyst formation, inflammation, or tumor). Superficial appearance: skin erythema, ulceration, pigmentation and scars (inflammation, breats cancer). Nipple: size, location, symmetry, inversion and secretion (tumor). Skin retraction (trauma, inflammation, tumor). Palpation: sitting position, patient’s arms at side first then overhead or pressed on both hips. Supine position: shoulders can be elevated by a small pillow putted under them to allow the breasts. Palpation: from the upper lateral quadrant with a procedure of clockwise direction for thorough examination (superficially and deeply palpation) If a MASS exist, it should be characterized as the following features: Location Size (length, width and thickness) Contour (regular or irregular, margin is dull or acute) Consistency (soft, cystic, moderatly firm or extremely hard) Tenderness (if tender, what degree) Mobility (movable or fixed) Chest pain Pleuralgic pain, or nerve compression pain Many causes of chest pain arise from the pleura (parietal pleura (pain sensory nerve)). Conditions of the lung are less likely to cause chest pain unless they involve the pleura. (This is certainly true of pneumonia and neoplasm). Pleuritis: stich (mordant pain), it worsen with breath (tyni breath). Pleura-, lung tumor --- intercostal nerve or plexus brachialis Chest pain Modality Location Emission (to left shoulder: angina or AMI, to back: aorta dissection) Temporal modality (acute or chronic) Connection with other factors (eating, high blood pressure, breath) Suggestibility (drugs) Other factors (fever, weight loss etc.) Exams ECG Blood cell count Sedimentation rate (pneumonia, infarction) Sputum smear and culture (pneumonia) Serum cardiac troponin levels [myocardial infarction (MI)] d-Dimer testing (pulmonary embolism) Gastro-esophagoscopy (reflux esophagitis) X-ray (pneumonia, pleuritis, radiculopathy) Echocardiograph (pericarditis) 24-hour Holter monitoring (coronary insufficiency) Gallbladder ultrasound
© Copyright 2026