Read a sample issue of Health Plan Week
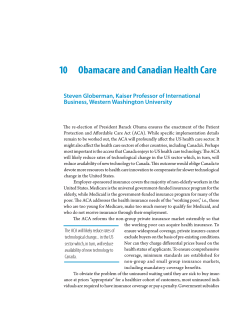
Volume 25, Number 16 May 11, 2015 Strategic Business, Financial and Regulatory News of the Health Insurance Industry Contents 3 Health Net, WellCare Post Solid Starts; MLRs Are Mostly Tempered 3 Molina Revenues Soar, Pumping Up a Strong 1Q Earnings Season 4 Table: Health Plan Stock Performances Weaken at Close of First Quarter 5 Table: Insurers With the Highest Risk-Corridor Receivables in 2014 7 Health Plan Briefs S&P Sees Market Unease Heading Into ’16 As Plans Weigh Risk of Exchange 3R Hole The likelihood CMS will not be able to make good on 100% of the risk corridors payments owed to health plans that lost significant amounts of money on Affordable Care Act (ACA) exchanges in 2014 will create market instability in 2016, a new report by Standard & Poor’s Ratings Services says. Market consultants say the lack of certainty about these payments, from the so-called 3Rs (reinsurance, risk corridors and risk adjustment) risk-mitigation programs under the ACA, will lead plans to hike exchangebased premiums next year as aggressive pricing gives way to the hard realities of the marketplace. Deep Banerjee, an associate director at Standard & Poor’s and lead author of the report, tells HPW that because of budget neutrality, which requires the risk-corridors pool to be funded by payments insurers make into the pool, there are major shortfalls in store. This is because many insurers are incurring big losses in their exchange business. “Our study indicates that the risk corridor payables are less than 10% of the receivables insurers reported in 2014,” he says. A receivable refers to the amount a health plan expects to get in payment as a result of the risk corridor. On the other hand, payables are the amount an insurer expects to pay into the corridor pool based on the risk-corridor formula. continued on p. 5 Cigna Moves Value-Based Collaborative Care Into New Areas; Feds Tout Pioneer There’s no need to wait for your next issue to stay on top of the latest industry news! The “From the Editor” postings at your subscriberonly Web page will keep you updated all week long. Log in at www.AISHealth. com/newsletters/ healthplanweek. Managing Editor Patrick Connole [email protected] Assistant Editor Lauren Clason Executive Editor Jill Brown Marching ever forward, value-based contracting saw significant positive news when on May 4 HHS said independent auditors found that its Pioneer Accountable Care Organization (ACO) Model coaxed more than $384 million in savings for the Medicare program in its first two years, an average of $300 per participating beneficiary per year. On the commercial side of the payer spectrum, Cigna Corp. on May 4 and 5 trumpeted its forays into the specialty physician practice space with its ACO-equivalent Cigna Collaborative Care and payment model, which was once reserved for only large physician groups. These announcements come at a time that the near-daily stream of activity by payers and providers to move more of their risk to value-based models continues unabated. But as these encouraging news stories come out, is there enough evidence to support the positive spin for accountable care? Harriett Wallsh, R.N., director of Cigna Collaborative Care clinical operations, tells HPW that generally it takes two to three years to determine whether a specific initiative is a success, but that timetable is shortening, with the ramp-up a little faster these days. Her broad statistics do indicate much progress in the value-based model for Cigna. “At the end of the calendar year 2014, for the 86 CACs [Collaborative Accountable Care] with us one year or more, there were 1.05 million customers. And for those people, over a million customers, 77% were in CACs that achieved quality or cost success,” she says. continued Published by Atlantic Information Services, Inc., Washington, DC • 800-521-4323 • www.AISHealth.com An independent publication not affiliated with insurers, vendors, consultants or associations 2 Health Plan Week The numbers also show that the absolute medical cost was in general 1% better than the market, Wallsh adds. As far as proof that the move away from fee-forservice (FFS) can pay dividends, Bruce Landon, M.D., a professor in the Department of Health Care Policy at Harvard Medical School, tells HPW that the year-in, year-out findings by Blue Cross and Blue Shield of Massachusetts and its Alternative Quality Contract (AQC) are exhibit A (HPW 11/11/13, p. 1). “The most developed piece of evidence is from the work we have done with the AQC in Blue Cross and Blue Shield of Massachusetts. It started in 2009 as a commercial ACO on an HMO population and has seen increasing rates of savings over time of participation in the program,” he says. “For the 2009 cohort, in the first year they had savings of $21 per patient per quarter, and that grew to $121 per patient per quarter for the fourth year. It is not like they are seeing 30% off spending, but they are making significant inroads.” And the Blues plan has widened the scope of its AQC, declaring in March that it will make the model available to PPO customers as well, increasing the breadth of the program to more than 1 million members from its current 680,000 (HPW 3/9/15, p. 7). Health Plan Week (ISSN: 1937-6650) is published 45 times a year by Atlantic Information Services, Inc., 1100 17th Street, NW, Suite 300, Washington, D.C. 20036, 202-775-9008, www.AISHealth.com. Copyright © 2015 by Atlantic Information Services, Inc. All rights reserved. On an occasional basis, it is okay to copy, fax or email an article or two from HPW. But unless you have AIS’s permission, it violates federal law to make copies of, fax or email an entire issue, share your AISHealth.com subscriber password, or post newsletter content on any website or network. To obtain our quick permission to transmit or make a few copies, or post a few stories of HPW at no charge, please contact Eric Reckner (800-521-4323, ext. 3042, or [email protected]). Contact Bailey Sterrett (800521-4323, ext. 3034, or [email protected]) if you’d like to review our very reasonable rates for bulk or site licenses that will permit weekly redistributions of entire issues. Contact Customer Service at 800-521-4323 or [email protected]. Health Plan Week is published with the understanding that the publisher is not engaged in rendering legal, accounting or other professional services. If legal advice or other expert assistance is required, the services of a competent professional person should be sought. Managing Editor, Patrick Connole; Assistant Editor, Lauren Clason; Executive Editor, Jill Brown; Publisher, Richard Biehl; Marketing Director, Donna Lawton; Fulfillment Manager, Tracey Filar Atwood; Production Coordinator, Lauren Yoffe Subscriptions to HPW include free electronic delivery in addition to the print copy, quarterly Key Financial Indicators for major health plans (in print and posted on the subscriber Web page), e-Alerts when timely news breaks, and extensive subscriber-only services at www.AISHealth. com that include a searchable database of HPW content and archives of past issues. To order an annual subscription to Health Plan Week ($667 bill me; $567 prepaid), call 800-521-4323 (major credit cards accepted) or order online at www.AISHealth.com. May 11, 2015 Rosemarie Day, president of Day Health Strategies, based in Somerville, Mass., tells HPW these success stories are real bottom-line material, generated by payers and providers being able to “truly share information on a patient,” like through electronic medical records. “But is also a cultural change for them [physicians],” she adds. And, Day stresses, there is a need to have insurers take the impetus to effect new attitudes about care management. “Insurers are trying to move in the right direction and reset incentives, and there are some docs already there. But others are slower on the adoption curve and need a push,” she says. For Ellen Lukens, a vice president at Avalere Health LLC, a Washington, D.C.-based consultant, the trick is for insurers and physicians working under these new models to determine the medical necessity of what they are doing and to deal with the bigger picture. “Whether it is under FFS or a value-based system, what has really changed now is this sense that the providers have a much more longitudinal focus. It is not just about the hospital but what impacts how the patient transitions back home and the impact on overall spending,” she tells HPW. Carrier Spreads Its Value-Based Designs Cigna, a veteran in the value-based space, has long held the goal of expanding collaborative care programs from large physician groups to small groups, hospitals and specialty practices. In that vein, recently the carrier said early results from OB/GYN medical practices in Florida and Texas taking part in the Cigna ACO-like model have recorded improved quality and lower medical costs. Wallsh says the key is that the initiatives have specific clinical targets that go beyond simple cost savings. “The OB/GYN program aims to reduce primary cesarean deliveries and inductions of labor prior to 39 weeks gestation for non-medical reasons, increase the use of generic drugs and shift certain gynecologic surgical procedures to less-costly sites of service. The program also focuses on the identification and referral of at-risk pregnant women, safety certification for office-based procedures and maternal mental health screening,” according to the carrier. OB/GYN practices taking part are compensated for their successful quality and cost efforts with a patient care management payment that varies based on how well the group performs. After its first year in the program, Women’s Care Florida, LLC, with offices in Tampa and Orlando, showed a 15.2% improvement in its primary cesarean delivery rate, 6.4% increase in generic dispensing rate and 3.7% rate for early elective deliveries, below the national rate of 5%, Wallsh says. Call Bailey Sterrett at 202-775-9008, ext. 3034 for rates on bulk subscriptions or site licenses, electronic delivery to multiple readers, and customized feeds of selective news and data…daily, weekly or whenever you need it. May 11, 2015 Health Plan Week Separately, Southwest Women’s Health Alliance (formerly Obstetrical & Gynecological Associates) in Houston improved total medical cost performance by 3%, experienced a 7.6% improvement in generic dispensing rate and had 93% overall patient satisfaction. Cigna has pilot programs with four other OB/GYN groups and estimates the launch of up to six more like efforts this year. Cigna also said on May 5 that Hackensack, N.J.based Regional Cancer Care Associates LLC (RCCA) is now working with the carrier to improve care for chemotherapy patients. Also part of the Cigna Collaborative Care brand, “the arrangement encourages RCCA to follow evidence-based medicine guidelines for cancer care and to use COTA, Inc., an industry-leading oncology analytics company that tracks the quality of care and associated costs. In addition, the practice will expand access to daily acute care with same day appointment availability, after-hours access and after-hours clinical advice, including 24/7 access to clinical triage staff,” Cigna said. This is more of what Wallsh calls valuable, realworld changes that a collaborative, value-based care program can bring. Another will be that RCCA will designate a registered nurse or an advanced care practitioner as the specialty group’s oncology care coordinator for as- sisting patients and managing coordinated care. In turn, Cigna will compensate the New Jersey medical group with a one-time care management payment for each of its member patients undergoing chemotherapy treatment. Contact Wallsh via Mark Slitt at mark.slitt@cigna. com, Lukens at [email protected], Day at rosemarie@ dayhealthstrategies.com and Landon at landon@hcp. med.harvard.edu. G Health Net, WellCare Post Solid Starts; MLRs Are Mostly Tempered Health Net, Inc. and WellCare Health Plans, Inc. are both off to “good” starts for 2015, according to securities analysts who point to positive first-quarter earnings underpinned by effective cost management programs, robust enrollment growth and sensible strategies for commercial and government-sponsored market segments moving forward. First out of the gate was Health Net, which on May 4 told investors that it recorded net income of $30 million or 39 cents a share for the first quarter, compared with $28.8 million or 36 cents a share for the same quarter of 2014. But taking into account one-time events, Health Net said adjusted net income stood at 74 cents a share for Molina Revenues Soar, Pumping Up a Strong 1Q Earnings Season Medicaid managed care specialist Molina Healthcare, Inc. on May 7 said its business is doing very well, reporting significant gains in first-quarter 2015 net income, revenue and enrollment as the carrier benefits from the expansion of coverage eligibility for low-income Americans under the Affordable Care Act (ACA). The insurer said first-quarter net income was $28.2 million, or 56 cents a share, up from $4.5 million, or 9 cents a share, for the same period of 2014. Year-on-year revenues for the quarter grew to $3.2 billion from $2.1 billion, a 53% jump from 2014. Wall Street analysts had expected net earnings of 49 cents per share, giving Molina a clear beat to start the year. Enrollment stood at nearly 3 million members as of March 31, 38% higher than the same period of 2014. A sharp rise in customers buying Molina coverage on public exchanges aided the carrier’s performance. As of March 31, Molina said it had 266,000 customers enrolled in ACA marketplaces, compared with only 15,000 at the end of the first quarter in 2014. 3 Chris Carter, an analyst with Credit Suisse, in a May 7 research note said the positive results for Molina came despite some headwinds generated by the lack of reimbursement from states for the ACA insurer fee that is typically passed on to the states under Medicaid contracts. Molina said in its earnings release that the company’s results continue to be adversely affected by the delays. “Due to progress made in securing agreements for the reimbursement of the HIF [health insurance fee] with various state Medicaid agencies in 2014, the company recognized approximately 73% of the Medicaid-related reimbursement revenue associated with HIF expense in the first quarter of 2015, compared with only 51% in the first quarter of 2014,” the insurer said. “[But the] delay in recognition of the HIF expense reimbursement from California, Michigan and Utah reduced income from continuing operations before income tax expense by approximately $16 million, or 20 cents per diluted share in the first quarter of 2015.” Contact Carter at [email protected]. Web addresses cited in this issue are live links in the PDF version, which is accessible at HPW’s subscriber-only page at http://aishealth.com/newsletters/healthplanweek. 4 Health Plan Week May 11, 2015 the quarter, 5 cents better than the pre-release expectations of financial analysts. The insurer logged a $47 million pretax charge tied to its outsourcing agreement with Cognizant Healthcare Services, LLC. Last November, Health Net CEO Jay Gellert said the insurer had finalized a master services agreement with Cognizant, a subsidiary of Cognizant Technology Solutions Corp., and the deal was expected to produce $150 million to $200 million in savings by 2017. Cognizant provides information technology, consulting and business process services, and Health Net contracted with it to help shrink administrative costs (HPW 11/10/14, p. 7). Health Net also increased its full-year earnings guidance by 10 cents to a range of $3.25 to $3.35 a share. “This is a result of better medical cost experience in government programs,” Gellert said in a May 4 conference call after the earnings release. He also cited the individual market on the California public exchange as one of the key drivers of the company’s positive results. “In 2014, we experienced substantial growth in this business resulting in a 17% market share statewide and a 31% market share in Southern California at the end of the year. We’ve maintained that market share in the first quarter of 2015,” Gellert said. “Our subsidized silver plan continues to be an attractive option, evident by the enrollment of 47,000 new individual exchange members in the first quarter of this year. While we grew in California, we lost some less-profitable individual members as expected on the Arizona exchange. This loss in membership was primarily due to a migration of membership to a lower-priced co-op plan.” Ralph Giacobbe, a securities analyst for Credit Suisse, said in a May 4 research note that Health Net’s consolidated medical loss ratio (MLR) of 84.5% “came in relatively in-line with consensus of 84.4%.” But he said commercial MLR was better than forecast at 82.1% versus the consensus 82.5%. “However, MA [Medicare Advantage] MLR was higher than expected at 92.9% (vs. consensus 91.4%) primarily due to prior year changes to risk adjuster estimates [MA risk adjustment under CMS rules.]. Medicaid MLR was in-line at 81.9%.” Also commenting on the MLRs, Scott Fidel, securities analyst for Deutsche Bank, in a May 4 report said the impact of the insurer’s revisions to its 3Rs estimates under the Affordable Care Act provisions on public exchanges lowered pretax income by $11.4 million. “Health Net’s commercial MLR would have been 81.2% excluding the revised 3R’s assumptions,” he said. Health Plan Stock Performances Weaken at Close of First Quarter Health plan stock prices fell an average of 7.4% in April, effectively negating March’s average gain of 7% to end the quarter on a sour note. Of the 10 plans HPW tracks, WellCare Health Plans, Inc. and Health Net, Inc. fared the worst, posting 15.3% and 12.6% losses, respectively, and pushing their year-to-date numbers into the red. Aetna Inc. broke even for the month, preserving its 20.3% full-year gain, with the same percentage boost as Anthem, Inc., even though Anthem had a 2% decline in its stock price last month. Closing Stock Price on 4/30/2015 April Gain (Loss) Full-Year Gain (Loss) Consensus 2015 EPS* Consensus 2015 P/E Ratio* COMMERCIAL Aetna Inc. $106.87 0.0% 20.3% $7.35 14.6 x Cigna Corp. $124.64 (4.4%) 21.2% $8.49 14.7 x $52.65 (12.6%) (0.7%) $3.21 16.4 x UnitedHealth Group $111.40 (5.2%) 10.5% $6.26 17.8 x Anthem, Inc. $150.93 (2.0%) 20.3% $9.94 (5%) 14% $165.60 (6.8%) 15.8% $8.83 $9.99 (4.9%) 10.9% $0.25 (6%) 13% 18.7% $2.68 23.2 x 23.8 x Health Net, Inc. Commercial Mean 15.2 x 15.7 x MEDICARE Humana Inc. Universal American Corp. Medicare Mean 18.8 x 39.3 x 29.0 x MEDICAID Centene Corp. $61.99 (12.0%) Molina Healthcare, Inc. $59.23 (10.7%) 13.0% $2.49 WellCare Health Plans, Inc. $77.43 (15.3%) (4.3%) $3.40 Medicaid Mean (13%) 9% 23.3 x Industry Mean (7.4%) 12.6% 20.7 x 22.8 x * Estimates are based on analysts' consensus estimates for full-year 2015. SOURCE: Bank of America Merrill Lynch. Compiled by Atlantic Information Services, Inc., April 2015. Subscribers who have not yet signed up for Web access — with searchable newsletter archives, Hot Topics, Recent Stories and more — should click the blue “Login” button at www.AISHealth.com, then follow the “Forgot your password?” link to receive further instructions. May 11, 2015 Health Plan Week On membership, Health Net said that as of March 31, 2015, total enrollment in its Western Region increased by 20% from the same time last year to 3.2 million members. Western Region commercial enrollment gained 7% to 1.2 million members. On May 6, WellCare also beat Wall Street estimates with its first-quarter 2015 results but did not revise its 2015 guidance. The carrier posted net earnings of $17.5 million, or 39 cents a share for the quarter, lower than the $44.1 million, or $1 a share, it had a year earlier. But in the first quarter of 2014, WellCare benefited from its acquisition of Windsor Health Group, Inc. (HPW 5/12/14, p. 5). Financial analysts had expected net income of 28 cents a share. WellCare also said its total membership expanded by 8.3% year to year to 3.8 million as of March 31. In looking at both insurers’ results, Steve Zaharuk, senior vice president at Moody’s Investors Service, tells HPW that it is clear the carriers had strong quarters, extending the trend set by most of the top-tier publicly traded carriers like UnitedHealth Group (HPW 4/20/15, p. 1), Aetna Inc. and Anthem, Inc. (HPW 5/4/15, p. 1). “It shows a continuation of what we are seeing, with the medical trend under control. Companies are tightening their belts on expenses and focusing on managed care,” he says. For WellCare, Zaharuk says new management seems to have corrected course in its key Medicaid business and improved cost-utilization strategies. WellCare on Feb. 17 informed investors of a turnaround plan by its new CEO, Kenneth Burdick. The insurer on Dec. 15, 2014, named then-President and Chief Operating Officer Burdick its new CEO, succeeding Chairman and Interim CEO David Gallitano (HPW 2/23/15, p. 7). Contact Fidel at [email protected], Zaharuk at [email protected] and Giacobbe at ralph. [email protected]. G 3R’s Underfunding Triggers Unease continued from p. 1 Insurers do not have to make payments if their risk-corridor ratio (i.e., costs as a share of revenues) is between 97% and 100%, and no payments will be made to insurers if their ratio is between 100% and 103%. But if the risk-corridor ratio falls between 92% and 97%, the health plan will pay into the corridor 50% of the excess. If the ratio is below 92%, the plan will pay about 80% of the excess into the corridor. These amounts will then be paid out in similar proportion to plans between 103% and 107% and to those at above 107%. CMS is likely to announce these risk-corridor payments in late June. Banerjee says larger insurers will be able to take any lost receivables under the risk-corridor program (see 5 table, below) in stride, but smaller players with a larger proportion of their business tied to ACA exchanges will experience a tougher hit. And for all insurers, the fact CMS may be unable to fulfill the promise of the risk-mitigation programs is a wake-up call. “The reinsurance and risk-corridor programs are temporary [expiring at the end of 2016], and after they are gone eventually rational pricing will have to come back to the market,” he says. “With the programs, however, you can afford to be a little aggressive in your pricing to pick up members and grow scale, but once these programs are gone, you probably have to price more conservatively than now.” Christopher Condeluci, a principal at CC Law & Policy, tells HPW that 2016 premium increases are in store because of this rethinking by insurers on their individual-market pricing due to the uncertainties of 3R payments. “I don’t want to be a sky is falling type of person, but more new entrants may exit because they cannot cope, unlike the big guys. And separately, you are going to have a premium spike by those new entrants that are Insurers With the Highest Risk-Corridor Receivables in 2014 Insurer Net ACA ACA corridor risk-corridor receivables as State of receivables % of reported domicile (mil. $) capital Health Care Service Corp. IL 115 1 Select Health Inc UT 105 24 Health Net, Inc. National Insurer 87 5 Moda Health Plan OR 82 68 Kentucky Health Cooperative Inc. KY 76 117 PreferredOne Insurance Co. MN 72 149 Blue Cross and Blue Shield of North Carolina NC 61 3 Humana Inc. National Insurer 51 1 Health Republic Insurance of New York Corp. NY 58 54 Common Ground Healthcare Cooperative WI 25 69 Geisinger Insurance Group PA 19 9 Neighborhood Health Plan, MA Inc. 18 14 Independence Health Group Inc. PA 16 1 Oscar Insurance Co. NY 15 57 Rocky Mountain Health Group CO 13 18 SOURCE: Standard & Poor’s Ratings Services, “The Unfunded ACA Risk Corridor May Make The U.S. Insurance Market Less Stable, Not More.” http://www.globalcreditportal.com. NAIC annual statutory filings and SEC 10K filings. Copyright © 2015 by Atlantic Information Services, Inc. All rights reserved. Please see the box on page 2 for permitted and prohibited uses of Health Plan Week content. 6 Health Plan Week May 11, 2015 still able to see if they can weather the storm, and the big guys will still charge higher premiums,” he says. This interplay between insurer pricing strategies in the new public exchanges and expectations for riskmitigation payments is a factor in all markets. But Humana Inc.’s experience in the Georgia individual market, where the carrier has admitted to pricing problems, is to brokers that operate in the state a prime example of this phenomenon. ACA exchanges were virgin territory for insurers when they opened for business about a year and a half ago. And in some cases, like Humana in Georgia, and in a much more drastic way for smaller insurers like the failed CoOportunity Health, Inc. in Iowa and Nebraska (HPW 1/12/15, p. 1), the purpose of the safety net offered by the 3Rs has become especially important because of mistakes in setting premiums for individual policies. Executives of Humana, which is best known for its major presence in the Medicare market, spoke on April 29 during a first-quarter 2015 earnings conference call about how Georgia’s individual market has hurt the bottom line of its Humana One individual plan offering. Humana CEO Bruce Broussard, on the earnings call, told investors that even as Humana One membership has grown nationally, and continues to be a break-even business, the insurer projects an increased reliance on the 3Rs. Humana Senior Vice President and Chief Financial Officer Brian Kane said the ACA exchange business is akin to what a startup deals with, and that has meant some successes and some stumbles. As a result, he said, “We have increased our net 2015 3R guidance range to $450 million to $550 million with reinsurance accounting for approximately 75% and risk adjustment and risk corridors accounting for approximately 25% of the total. As we have discussed in the past, there is an interplay between risk adjustment and risk corridors in that if we don’t get the risk adjustment exactly right, a meaningful part of the balance, either positive or negative, is captured through the risk corridors.” Kane said that in Georgia the insurer’s limited claims experience and an unexpected “less healthy state population” resulted in Humana accruing both a risk-adjust- AIS’s Management Insight Series Improving Medicare Star Ratings: Practical Strategies for Health Plans and Providers Go to the “Marketplace” at www.AISHealth.com and click on “Books, Insight Series.” ment and risk-corridor receivable. But this trial and error for the start of ACA exchanges is exactly the point of the premium stabilization programs, “namely early-year protection in this circumstance,” he added. Brokers Detail Humana Pricing Strategies Early protection or not, Rick Bailey, president of insurance brokers Rick Bailey & Company, Inc., based in Woodstock, Ga., tells HPW it seems Humana simply overplayed a low pricing move it undertook for open enrollment for 2014. “They came out with some very aggressive pricing last year for their first exchange open enrollment. And they were killing it. They were so much lower than everybody,” he says. “For this year, we kind of expected a price correction from them and someone else to come in and take them on, but it really didn’t happen. Humana’s pricing is still underneath everybody in metro Atlanta again for a second year. I was kind of shocked on how they could do that. My guess is maybe they have been aggressive in pricing in thinking the money from government for the first three years would help offset that.” Concurring with Bailey is Russ Childers, an insurance agent based in Americus, Ga., and past president of the Georgia Association of Health Underwriters. He tells HPW that Humana priced “real low in the market” for the first year of exchanges, offering plans in major metro areas centered in north Georgia (Atlanta), with exceptions made for Savannah and Macon. “They were significantly lower than anyone else for 2014, probably 10% to 15% under Blue Cross [Anthem, Inc.’s Blue Cross Blue Shield of Georgia], the primary competition. Their idea was to secure market share,” he says. For Childers, this extremely low pricing strategy struck him as a “little strange,” given the inevitable in the health plan world, which is that enrollees likely will be filing plenty of claims at some point. Now, from what he saw for 2015, Humana did adjust its pricing, raising premiums on the order of 10% on average. But other carriers adjusted as well, like the Blues plan, which did the opposite and reduced premiums. “And United [UnitedHealth Group unit UnitedHealthcare] entered at about the same price point as Blue Cross,” Childers adds. He says that he thinks the way Humana started off in 2014, with its aggressive approach, made other large carriers nervous and resulted in the twitches by Aetna Inc. and UnitedHealth that saw both carriers file to enter the Georgia exchange but then withdraw. Humana had no comment on the Georgia market. Contact Condeluci at [email protected], Banerjee at [email protected], Childers at [email protected] and Bailey at rick@ rickbaileycompany.com. G Web addresses cited in this issue are live links in the PDF version, which is accessible at HPW’s subscriber-only page at http://aishealth.com/newsletters/healthplanweek. May 11, 2015 Health Plan Week 7 HEALTH PLAN BRIEFS u Aetna Inc. said starting on May 15 it will stop covering the routine use of the laparoscopic power morcellator in removal of uterine fibroids, reacting to FDA concerns that the medical device can spread hidden cancer in women. The insurer will require that doctors obtain prior approval for any medical procedure that uses a morcellator. “Myomectomy and hysterectomy procedures that use a power morcellator will not be covered in most circumstances because the safety and efficacy of this approach has not been demonstrated,” Aetna said. Doctors can ask for exceptions for pre-menopausal women who want to remain fertile and have no other clinical option or in cases where a woman’s life is in danger without the procedure. The Aetna decision is one of a string taken by insurers. For instance, UnitedHealth Group last month imposed tighter restrictions for its coverage of hysterectomies (HPW 3/2/15, p. 7). The trade group America’s Health Insurance Plans on April 14 said the federal government and medical societies need to do more to help guide health plans on how to handle the morcellator issue (HPW 4/27/15, p. 8). Visit http://tinyurl.com/m2tsac7. u Arlington, Va.-based Evolent Health, Inc. on May 6 registered for an initial public offering (IPO) with the Securities and Exchange Commission to raise $100 million and operate as a public company. The population and health management company was founded in 2011 by UPMC (the University of Pittsburgh Medical Center) and The Advisory Board Company (HPW 12/24/12, p. 1). Visit http://tinyurl. com/kgcbchm. u New York City-based Assurant, Inc. on May 6 released its first-quarter 2015 earnings, detailing “worse than expected” results from its Milwaukeebased Assurant Health unit that just one week before on April 28 it said it was looking to sell, along with its employee benefits subsidiary (HPW 5/4/15, p. 4). The parent company, which is strongest in the home and life insurance segments, had said that the long-term prospects for the insurance unit were not sufficient to continue operations. During the conference call after earnings were released, Christopher Pagano, Assurant chief financial officer, said the net operating loss for Assurant Health was $84 million for the first quarter of 2015. “Approximately half was due to a reduction in our estimated recoveries under the ACA [Affordable Care Act] risk-mitigation programs for 2014 policies,” he said. Assurant said ACA policies now make up 60% of the health insurer’s premiums compared to 18% last year. Pagano said absent a sale of Assurant Health, “we will begin the process to exit the market and will not participate in the 2016 ACA open enrollment.” On the same call, Assurant CEO Alan Colberg said the sale of the health and employee benefits units would be separate and not a package deal. Visit http://tinyurl.com/ml3bvtp. u Kansas Gov. Sam Brownback (R) on May 4 said he would file an amicus brief in support of the lawsuit filed by Florida Gov. Rick Scott (R) on April 28 against the Obama administration over its attempt to convince Florida to expand Medicaid by refusing to fund its Low-Income Pool (HPW 5/4/15, p. 8). “CMS has indicated that Low Income Pool funding to the states will be cut off unless they expand Medicaid. The Supreme Court ruled in 2012 that the federal government is prohibited from coercing the states to expand Medicaid,” Brownback said. “Kansas intends to join Texas through an amicus brief supporting Florida’s effort to stop the Obama administration from cutting off health care dollars for the Low Income Pool in an effort to force Obamacare upon the states.” Visit http://tinyurl.com/othr6jk. u U.S. District Judge William Yohn Jr. in Philadelphia ruled that a surgical clinic’s counterclaims for payment against Aetna Inc. should stand, rejecting the insurer’s arguments that the outpatient center can’t enforce a network reimbursement agreement. In Aetna Life Insurance Co. v. Huntingdon Valley Surgery Center et al., case number 2:13cv-03101, in the U.S. District Court for the Eastern District of Pennsylvania, Yohn on April 30 mostly sided with the surgical center. “Put simply, in the counterclaims, Huntingdon Valley contends that Aetna has consistently underpaid it for its services to Aetna members and also interfered with its prospective contractual relations with Aetna members and with doctors in Aetna’s network. Aetna has moved to dismiss all eight counterclaims on a variety of grounds….I will dismiss Huntingdon Valley’s claim for ERISA benefits but otherwise deny the motion,” he said. Huntingdon filed its counterclaims in response to a 2013 lawsuit from Aetna alleging improper referrals stemming from kickbacks. In granting Aetna a win on the ERISA part of its argu- Subscribers who have not yet signed up for Web access — with searchable newsletter archives, Hot Topics, Recent Stories and more — should click the blue “Login” button at www.AISHealth.com, then follow the “Forgot your password?” link to receive further instructions. 8 Health Plan Week May 11, 2015 HEALTH PLAN BRIEFS (continued) ment, Yohn ruled that Huntingdon Valley wrongly failed to use all of its possible administrative remedies before bringing its claim. Visit http://tinyurl. com/797xzrm. u Health insurance premiums on the Small Business Health Options Program (SHOP) exchanges were 7% less on average than premiums offered outside the exchanges, according to a study in the May issue of Health Affairs. The journal cited the low premiums and high provider participation rates as indicators of continued success in the program, but said complicated enrollment procedures and the lack of broker participation could be causes for concern. Visit http://tinyurl.com/k9auwqf. u CMS on May 4 released an interim final rule (42 CFR Part 423) requiring Medicare Part D insurers to cover prescriptions written by all state-licensed prescribers, even if they are not enrolled in Medicare. A previous rule set to take effect in December specifically required insurers and pharmacy benefit managers to reject prescriptions from prescribers not enrolled in Medicare. The new interim rule includes state-authorized prescribers unable to enroll in Medicare, who essentially fall into a loophole of the program, and also provides provisional coverage and individualized written notices to members who fulfill a prescription from non-Medicare physicians. Visit http://tinyurl.com/noe3l9g. u Approximately 75% of emergency-room doctors said ER visits have increased since January 2014, when major provisions of the Affordable Care Act took effect, according to The Wall Street Journal. That number is up from a survey in 2013, when less than half of ER doctors said visits had grown. The new study, conducted by the American College of Emergency Physicians, said new Medicaid patients are failing to find doctors and instead seek help through the ER. Twenty-eight percent of respondents said visits had increased greatly, while 47% said they had risen only slightly. Visit http://tinyurl.com/op3kzso. u Medicaid and the Children’s Health Insurance Plan (CHIP) added more than 560,000 lives to their rolls in February, CMS said on May 1. The Affordable Care Act extended Medicaid or CHIP coverage to 11.7 million additional individuals total since enrollment efforts for the federal marketplace launched in October 2013. The total for Medicaid and CHIP enrollment across the U.S. is more than 70 million. Expansion states experienced a 27% enrollment bump compared with the period from July to September 2013, whereas enrollment in non-expansion states grew by 8%. Visit http://tinyurl.com/lcjgxy9. u The National Association of Insurance Commissioners has adopted new guidelines regarding cybersecurity and patient privacy. The document released last month details eight principles governing insurance commissioners’ responsibilities in the defense of protected health information, including conducting risk reviews, establishing incident response procedures, verifying third-party security controls and collaborating with insurers to develop regulations. Visit http://tinyurl.com/oaa8w9h. u Medicare star quality ratings have little impact on seniors’ choices in Blue Cross Blue Shield plans, according to data released by HealthPocket Inc. The April study found seniors paid little attention to star ratings, instead choosing plans based on brand familiarity, premiums, out-of-pocket costs and provider access. The Blues plans’ branding power and wide variation in star ratings led HealthPocket to suggest seniors should be more aware of quality when selecting coverage. Visit http://tinyurl.com/ prgseww. u PEOPLE ON THE MOVE: Aetna Inc. named Cain Hayes president of Mid-America operations. He is based in Columbus, Ohio. Previously, Hayes was president of Aetna’s government-sector business…. Minnesota’s state-based public exchange, MNsure, said CEO Scott Leitz is resigning to become the chief transformation officer with the Health Care Cost Institute, a Washington, D.C.-based think tank. Allison O’Toole, the exchange’s deputy director of external affairs, will take over as MNsure’s interim head starting on May 22....Centene Corp. named Ken Yamaguchi, M.D., executive vice president and chief medical officer. Yamaguchi is the founder of the Shoulder and Elbow Service at Washington University in St. Louis. The insurer also appointed Mary Mason, M.D., senior vice president and chief medical officer of specialty companies. For the past nine years Mason has served as Centene’s chief medical officer….Gold Coast Health Plan in Camarillo, Calif., named Dale Villani CEO. Before Gold Coast, Villani was chief operating officer for Arizona Priority Care, a physician network in the Phoenix area. Call Bailey Sterrett at 202-775-9008, ext. 3034 for rates on bulk subscriptions or site licenses, electronic delivery to multiple readers, and customized feeds of selective news and data…daily, weekly or whenever you need it. If You Don’t Already Subscribe to the Newsletter, Here Are Three Easy Ways to Sign Up: 1. Return to any Web page that linked you to this issue 2. Go to the MarketPlace at www.AISHealth.com and click on “Newsletters.” 3. Call Customer Service at 800-521-4323 If you are a subscriber and want to provide regular access to the newsletter — and other subscriber-only resources at AISHealth.com — to others in your organization: Call Customer Service at 800-521-4323 to discuss AIS’s very reasonable rates for your on-site distribution of each issue. (Please don’t forward these PDF editions without prior authorization from AIS, since strict copyright restrictions apply.)
© Copyright 2026