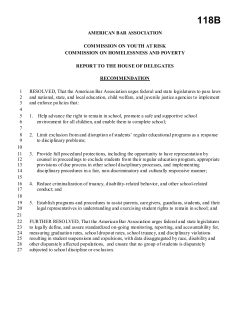
The Joint Commission and Patient Safety Outcomes: By
The Joint Commission and Patient Safety Outcomes: Have Accreditor Policies Improved Patient Safety? By Elaine Kenniston, B.S.N, R.N., O.C.N Capstone Project Presented to the Faculty of the Graduate Program of The University of California at San Diego and California Western School of Law In Partial Fulfillment Of the Requirements For the Degree of Master of Advanced Studies February 2011 The Joint Commission and Patient Safety Outcomes: Have Accreditor Policies Improved Patient Safety? Elaine Kenniston, MAS The University of California at San Diego-California Western School of Law, 2010 Supervisors: Bryan A. Liang (Committee Chair), Steven R. Smith, Lori Johnson The goal of this study is to determine the relative effectiveness of The Joint Commission (TJC) and its efforts to reduce patient deaths and preventable medical errors as recommended by the Institute of Medicine’s (IOM) ground-breaking report, To Err is Human: Building a Safer Health System. This publication originated from an independent review by its Committee on Quality of Health Care in America, which found that up to 98,000 patients die each year from preventable errors with an estimated annual cost between $17-29 billion. Based on these staggering findings, the IOM asked that a concerted effort be made among providers, organizations, purchasers, consumers, regulators and policy-makers to correct this broken system. TJC is a national health care accreditation organization with a vision that all people always experience the safest, highest quality, best-value health care across all settings. TJC has evaluated over 17,000 organizations and their standards enforce the Center for Medicare and Medicaid Services’ (CMS) Conditions of Participation. This work analyzes the role and potential impact of TJC in the patient safety effort since the IOM Report. It finds that the TJC is a major player in this system with many industry related and financial ties. Further, however, although there has been some progress in the past 10 years to protect patients in the safety realm, patients continue to die and billions of dollars have been lost because health care organizations have failed to implement the recommendations as outlined by the IOM. In particular, given current estimates on patient deaths and medical costs related to preventable errors, TJC compliance does not necessarily translate into improved patient safety. Table of Contents I. Introduction…………………………………………………………………..……..1-2 II. The Scope of Harm from Preventable Medical Errors – Past and Present…….…. 3-17 Implications from the Institute of Medicine’s 2000 Publication “To Err is Human: Building a Safer Health System” A. Medical Errors and Adverse Events B. Strategies for Improvement 1. Institute of Medicine 2. The Joint Commission a. National Patient Safety Goals b. ORYX Core Performance Measures c. Universal Protocol for Preventing Wrong Site, Wrong Procedure and Wrong Person Surgery TM C. Other Private Sector Efforts 1. Institute for Healthcare Improvement 2. National Quality Forum 3. Michigan Keystone ICU Project III. The Joint Commission…………………………………………………….……...18-27 A. Brief History B. Deemed Status C. The Office of Inspector General and The Government Accountability Office D. Survey Process and Fees for Accreditation VI. Alternative Accreditation Organizations and Quality Guidelines………………..28-33 1. Healthcare Facilities Accreditation Program 2. Del Norske Veritas Healthcare, Inc. including the International Organization for Standardization (IOS) 9001 Standards V. Recommendations…………………………………………………………...…...34-41 1. Outcomes Based versus Inspection Focused Surveys 2. Recommendations VI. Conclusion………………………………………………………………….……42-43 VII. Bibliography………………………………………………………………….....44-49 VIII. Vita…………………………………………………………………………………50 I. Introduction The Joint Commission (TJC) is a national health care accrediting organization that has deemed status1 through the Centers for Medicare and Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services (DHHS). TJC’s standards correspond to CMS’s Conditions of Participation (CoPs), which hospitals must meet in order to begin and continue participating in the Medicare and Medicaid programs.2 TJC’s mission is to continuously improve health care for the public, in collaboration with other stakeholders, by evaluating health care organizations and inspiring them to excel in providing safe and effective care of the highest quality and value. Its vision is that all people always experience the safest, highest quality, best-value health care across all settings.3 TJC has been the primary accreditor ensuring quality and safety in health care. Yet in 1999, the Institute of Medicine (IOM)4 published its report “To Err is Human,” which found that thousands of patients die each year from preventable errors with an estimated annual medical error costs in the billions.5 After this report, an 1 The Free Dictionary by Farflex, Medical Dictionary, deemed status, http://medical-dictionary.thefreedictionary.com/deemed+status (last visited Feb. 18, 2011) Deemed status is “conferred on a hospital or other organization by a professional standards review organization in formal recognition that the organization's review, continued-stay review, and medical care evaluation programs meet certain effectiveness criteria”. 2 Centers for Medicare and Medicaid Services, Conditions for Coverage (CfCs) & Conditions of Participations (CoPs), (10/25/2010), available at https://www.cms.gov/CFCsAndCoPs/01_Overview.asp 3 The Joint Commission, http://www.jointcommission.org (last visited Oct. 30, 2010) 4 Institute of Medicine, About the IOM, http://www.iom.edu/About-IOM.aspx (last visited Feb. 18, 2011) Established in 1970, the IOM is an independent, nonprofit organization that “works outside of government to provide unbiased and authoritative advice to decision makers and the public the health”; it is one arm of the National Academy of Sciences. Many of their studies begin as specific mandates from Congress while others are requested by federal agencies and independent organizations. 5 Id., Shaping the Future of Health, To Err is Human: Building a Safer Health System, (1999), available at http://www.iom.edu/Reports/1999/To-Err-is-Human-Building-A-Safer-Health-System.aspx 1 important question to assess is: has safety improved under TJC accreditation? In fact, in 2009, Arthur Levin, member of the IOM’s Committee on Quality of Health Care in America stated “One decade later, we can’t say whether we are any better off today than when the IOM first sounded the alarm about medical errors in 1999”.6 In Part II, the scope of harm from medical errors including estimated deaths, monetary and non-monetary costs, and how they relate to other leading cause of death statistics will be discussed. Preventable medical errors will be defined as well as the IOM’s goal to reduce medical errors and their strategies for improvement. TJC and other private sector responses to the report will also be outlined. Part III will review TJC’s history, deemed status and congressional response. Alternatives to TJC accreditation are discussed in Part IV. These include Del Norske Veritas Healthcare, Inc., the International Organization for Standardization (ISO) 9000 quality improvement guidelines for the health care sector, and the Healthcare Facilities Accreditation Program. Part V will asses TJC’s activities in context to the IOM’s recommendations to promote patient safety and reduce preventable medical errors. After summarizing, recommendations on solutions will be outlined. Finally, concluding thoughts will be presented in Part VI. 6 Consumers Union, U.S. Health Care System Fails to Protect Patients From Deadly Medical Errors, (May 19, 2009), available at http://www.consumersunion.org/pub/2009/05/011324print.html 2 II. Medical Errors: Past & Present “It may seem a strange principle to enunciate as the very first requirement in a Hospital that it should do the sick no harm”.7 Florence Nightingale - 1859 A. Medical Errors and Adverse Events In the Institute of Medicine’s (IOM) 2000 publication, To Err is Human: Building a Safer Health System,8 an error is defined as the failure of planned action to be completed as intended (i.e., error of execution) or the use of a wrong plan to achieve and aim (i.e., error of planning).9 An adverse event (AE) is an injury caused by medical management rather than by the underlying disease or condition of the patient. An AE attributed to an error is a preventable adverse event.10 A large proportion of AE’s are the result of errors. The IOM report estimated at least 44,000 people and as many as 98,000 people die in hospitals each year as a result of medical errors.11 These figures are attributed to the eighth-leading cause of preventable death, exceeding those related to motor vehicle accidents, breast cancer or AIDS.12 Another significant toll from preventable medical errors is its financial costs, which IOM estimated to be between $17 billion and $29 billion per year in hospitals 7 About.com, Women’s History, Selected Florence Nightingale Quotations, available at http://womenshistory.about.com/cs/quotes/a/qu_nightingale.htm (last visited Jan. 30, 2011) 8 Institute of Medicine, To Err Is Human: Building a Safer Health System, (Linda T. Kohn, et al. eds. 1999) 9 Id. 10 Id. at 29 11 Id. at 26 12 Id. 3 nationwide.13 Costs included the expense of additional patient care caused by the error, lost income and household productivity, and disability. Non-monetary costs include distrust of patients and their families that have been harmed by an error and provider dissatisfaction and loss of morale from not being able to provide the best care possible due to faulty systems, processes and conditions that lead to mistakes.14 In 2010, the Millennium Research Group estimated total medical error costs in the U.S. to be $19.5 billion during the year 2008.15 Of this amount, $17 billion was associated with the medical treatment and prescription drugs services delivered to patients who were directly affected by medical errors; indirect costs included $1.4 billion related to increased mortality rates and $1.1 billion related to decreased productivity from short-term disability claims.16 Compounding the problem, a 2007 study found that the U.S. ranked last out of seven nations (Australia, Canada, Germany, Netherlands, New Zealand and the United Kingdom) among expenditures per capita ($7,290).17 The U.S. has the most expensive health system in the world and ranked last on dimensions of access, safe care, efficiency, equity and long, healthy, productive lives in 2009.18 13 See supra note 5 at 27 Id. at 2 15 Milliman, The Economic Measurement of Medical Errors, Sponsored by Society of Actuaries’ Health System, (June 2010), 5, available at http://www.soa.org/files/pdf/research-econ-measurement.pdf (last visited Feb. 18, 2011) 16 Id. 17 Karen Davis, Cathy Schoen and Kristoff Stremikis, Mirror, Mirror on the Wall How the Performance of the US. Health Care System Compares Internationally 2010 Update, Executive Summary, Commonwealth Fund, (June 2010) available at http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2010/Jun/1400_Davis_ Mirror_Mirror_on_the_wall_2010.pdf 18 Id. 14 4 B. Strategies for Improvement 1. IOM As a result of their findings, the Quality of Health Care in America Committee of IOM outlined a comprehensive strategy in their 1999 report to reduce preventable medical errors. They also challenged the government, health care providers, industry related businesses and consumers with a goal to reduce errors by a minimum of 50% over the next five years.19 The recommendations for improvement were designed to balance efforts among regulatory and private sector initiatives and between the roles of professionals and organizations. The strategy included a four-tier approach which included establishing a national focus to strengthen the knowledge base about safety through research, tools and protocols; identifying and learning from errors by developing a public mandatory reporting systems; raising performance standards; and implementing safety systems in organizations at the level of delivery.20 The IOM also reported that the main sources of standards for health care organizations and professionals at the time was through licensing and accreditation activities, but medical errors and patient safety were not their main focus.21 Accreditation standards did speak to quality improvement, patient safety and medical error reduction; however, fully accredited organizations had yet to implement the most rudimentary systems and process to ensure patient safety.22 The report recommended that the existing regulatory organizations should increase attention to patient safety issues and that they 19 See supra note 3 at 4. Id. 21 See supra note 8 at 151 22 Id. 20 5 must hold health care organizations accountable for creating and maintaining safe practices.23 2. TJC a. Standards Prior to the IOM report, TJC’s standards emphasized optimal achievable levels of quality and performance improvement concepts.24 Starting 2001, after the IOM’s recommendations that accreditation agencies should increase their efforts in the patient safety realm, TJC introduced new standards that would focus directly on patient safety and medical care error reduction in hospitals.25 The standards went into effect on July 1st and required leaders to implement an integrated patient safety program throughout the organization with specific key provisions. That same year, TJC formed a 20-member Standards Review Task Force to identify the standards that were relevant to the safety and quality care that contributed to good outcomes and eliminate or revise those that did not.26 TJC also indicates that its commitment to patient safety is evident as almost 50 percent of their patient safety-related standards address issues in medication use, infection control, surgery and anesthesia, transfusions, restraint and seclusion, staffing and staff competence, fire safety, medical equipment, emergency management and security.27 Specific requirements include how the organization responds to adverse events 23 See supra note 8 at 151 and 152 See supra note 3, The Joint Commission History, 6, 1-14, (July, 2010) available at http://www.jointcommission.org/assets/1/18/Joint_Commission_History.pdf (last visited Jan. 17, 2011) 25 Id. at 3 26 See supra note 21 27 Id. 24 6 and the prevention of accidental harm through the root-cause-analysis of vulnerable patient systems, e.g., ordering, preparation and dispensing of medications.28 b. National Patient Safety Goals (NPSGs) In 2002, TJC established its first set of NPSGs designed to improve the safety of patients care in health care organizations.29 The goals included improving the accuracy of patient identification, improving the effectiveness of communication between caregivers, improving the safety of high-alert medications, the safety of using infusion pumps and the effectiveness of alarms used in the clinical setting. Organizations were also to develop processes to eliminate wrong-site, wrong-patient and wrong-procedure surgery.30 After the NPSGs went into effect on in January 2003, the Patient Safety Advisory Group31 has worked with TJC staff to perform reviews of the literature and databases to identify potentially new NPSGs. Over the years, goals were revised and new goals developed.32 In 2009, after determining that the goals had become too specific and detailed, revisions were made to clarify certain elements of performance and delete or 28 See supra note 21 See supra note 3, Facts about the National Patient Safety Goals, available at http://www.jointcommission.org/assets/1/18/National_Patient_Safety_Goals_12_09.pdf (last visited Jan. 17, 2011) 30 Id. 31 See supra note 3, Topic Library Item, Facts about the Patient Safety Advisory Group, available at http://www.jointcommission.org/facts_about_the_patient_safety_advisory_group/ (last visited Feb. 18, 2011) In April 2002, The Joint Commission appointed a group of experienced physicians, nurses, pharmacists and other patient safety experts to help advise and the development TJC’s first set of National Patient Safety Goals, the Patient Safety Advisory Group, (formerly called the Sentinel Event Advisory Group) 32 See supra note 24 29 7 move requirements into other standards. 33 As a result, the hospital NPSGs for 2011 have been revised and include correct identification of patients, improving staff communication, safe use of medications, infection prevention, checking patient medicines and identifying patient safety risks. c. ORYX Core Performance Measures In July 2002, accredited hospitals began collecting data on the first set of ORYX Core Performance Measures.34 TJC considered ORYX the next evolution in accreditation, and was first implemented in 1997 to integrate the use of performance measures and outcomes into the accreditation process.35 Core Measures and their outcomes are intended to balance the organization’s activities to improve patient care.36 Accredited hospitals were required to collect data on at least two of the four measures including acute myocardial infarction (AMI), heart failure (HF), community acquired pneumonia (CAP) and pregnancy and related conditions (PR). Each Core Measure has a set of performance measures. For example, the AMI set has 10 measures, including Aspirin at Arrival, Adult Smoking Cessation Advice/Counseling, Beta Blocker and Statin Prescribed at Discharge.37 Each measure set has an indicator in which performance is scored and can be compared to other hospitals. Scores are published and available to the public at 33 See supra note 24 See supra note 21 at 7 35 Id. at 4 36 UC San Diego Health System, What Are Core Measures?, available at http://www-ucsdhealthcare.ucsd.edu/clinical/pdf/pips/what%20are%core%20measures.pdf (last visited Jan. 16, 2011) 37 See supra note 3, Core Measure Sets – Acute Myocardial Infarction, available at http://www.jointcommission.org/assets/1/6/Acute%20Myocardial%20Infarction.pdf (last visited Jan. 16, 2011) 34 8 www.hospitalcompare.hhs.gov (CMS) and www.qualitycheck.org (TJC). Participation in collection and reporting of this data is linked to financial reimbursement from CMS.38 Currently, there are over 3,000 Joint Commission accredited hospitals that provide data from a selection of 57 inpatient measures. Of these, 31 are publicly reported with plans to add the remaining newly implemented measures over time.39 d. A TJC Example: Universal Protocol for Preventing Wrong Site, Wrong Procedure and Wrong Person Surgery As an example of TJC efforts to improve patient safety, the Joint Commission Board of Commissioners approved the Universal Protocol for Preventing Wrong Site, Wrong Procedure and Wrong Person Surgery.40 The protocol was created in 2003 as incidences of wrong site, wrong procedure and wrong person surgery continued to occur in organizations accredited by TJC. Critical components to the protocol included a preprocedure verification, site marking and a time out.41 e. Disappointing Results However, despite standards and safety measures that hundreds of hospitals have implements as a result of the TJC protocol, major mistakes still occur.42 Despite TJC efforts to improve safety, challenges remain. For example, efforts to decrease infections 38 See supra note 31 Mark Chassin, Jerod Loeb, Stephen Schmaltz, Robert Wachter , Accountability Measures – Using Measurement to Promote Quality Improvement, 363(7), N Engl J Med, 683, (Aug. 12, 2010), available at http://www.nejm.org/doi/pdf/10.1056/NEJMsb1002320?ssource=hcrc (last visited Jan. 17, 2011) 40 See supra note 3, Facts about Patient Safety, 1, 1-4, available at http://www.jointcommission.org/assets/1/6/Patient_Safety_1_4_11.pdf (last visited Jan. 15, 2011) 41 See supra note 42 42 abc NEWS, Surgical Errors Continue Despite New Safety Guideline, New Study Finds Doctors Continue to Make Major Surgical Mistakes, available at http://abcnews.go.com/Health/Wellness/study-finds-medical-mishaps-universal-protocolera/story?id=11910796 (last visited Jan. 17, 2011) 39 9 through the TJC infection control standards have not been successful. Hand washing failures continue to contribute to hospital-acquired infections (HAIs) that kill nearly 100,000 each year and cost hospitals $4 billion to $29 billion annually.43 As a result, TJC recently partnered with other private sector organizations to develop the Center for Transforming Healthcare. The center’s first initiative is to assess, develop and implement standards to address HAIs.44 Further, in a recent study between January 1, 2002 and June 1, 2008, from a database that contained 27,370 physician self-reported adverse events, a total of 25 wrong-patient and 107 wrong-site procedures were identified.45 The main root causes leading to the wrong patient procedures were errors in diagnosis (56%) and errors in communication (100%) and wrong-site procedures were related to errors in judgment (85%) and the lack of performing a ‘time-out’ (72%).46 Of note, performing a “time-out” prior to the procedure is part of TJC’s protocol.47 C. Other Private Sector Efforts Recognizing weaknesses in TJC processes, other organizations have attempted to promote patient safety. Below are examples of other, non-TJC initiatives created by the private sector as a response to the IOM’s strategy for improvement and the effective impact they have had on improving patient safety. 43 Joint Commission Center for Transforming Healthcare Newsroom, Creating Solutions for High Reliability Health Care, Joint Commission Center for Transforming Healthcare Takes Aim at Patient Safety Failures, (September 10, 2009), available at http://www.centerfortransforminghealthcare.org/news/display.aspx?newsid=6 44 Id. 45 Philip F. Sahel et al., Wrong-Site and Wrong-Patient Procedures in the Universal Protocol Era, Analysis of a Prospective Database of Physician Self-reported Occurrences, 145(10)Arch Surg, (Oct. 2010), 978, 978984, available at http://www.cascacolorado.com/wp-content/uploads/2010/10/Never-event-selfreporting-in-CO-AMA-article-Oct-10.pdf (last visited Feb. 19, 2011) 46 Id. 47 See supra note 42 10 1. The Institute for Healthcare Improvement (IHI) IHI is an independent, not-for-profit organization. It estimates that nearly 15 million instances of medical-harm occur in the U.S. each year, i.e., over 40,000 per day.48 Its goals focus on the IOM’s six improvement aims for the health care system (safe, effective, patient-centered, timely, efficient and equitable). IHI’s No Needless List illustrates its focus, which includes no needless deaths, no needless pain for suffering, no helplessness in those served or serving, no unwanted waiting, no waste and no one left out.49 A voluntary safety initiative from the IHI was the 18 month 100,000 Lives Campaign, which encouraged hospitals to adopt six best practices to reduce harm and deaths.50 The interventions included deployment of rapid response reams at the first sign of patient decline, delivering reliable evidence based care for acute myocardial infarction to prevent death from heart attacks, implementing a medication reconciliation process to prevent adverse drug events, implementing a central line management process to prevent central line infections, administering antibiotics at a specific time to prevent surgical site infections, and using a ventilator protocol to minimize ventilator associatedpneumonia.51 The IHI announced on June 14, 2006 that they surpassed their campaign goal with the 3,100 participating hospitals saving an estimated 122,000 lives within an 18 48 Institute for Healthcare Improvement, http://www.ihi.org/IHI/About/VisionValues/ (last visited Oct. 25, 2010) 49 Id. 50 Id., Campaign Overview, 1, 1-3, available at http://www.ihi.org/IHI/Programs/Campaign/100kCampaignOverviewArchive.htm (last visited Feb. 11, 2011) 51 Id. 11 month period.52 In 2008, TJC criticized the saved lives results and offered their own interpretation of items that they consider important in understanding possible inaccuracies including the science of mortality risk adjustments.53 Despite TJC criticisms, and based on the well-recognized success of the campaign, the IHI expanded its focus with a new campaign - The 5 Million Lives Campaign.54 The objective of this initiative was to reduce five million incidences of errors that resulted in non-fatal medical harm in a two-year period (December 2006 and December 2008).55 The campaign added six new interventions including preventing harm from highalert medications, reducing surgical complications, preventing pressure ulcers, reducing Methicillin-Resistant Staphylococcus aureus (MRSA) infection, evidence-based care for congestive heart failure and informing hospital Board of Directors on best practices to expedite organizational safe patient care.56 Currently, IHI is analyzing the results of its 5 Million Lives Campaign to determine if they met their goal.57 Data that has been gathered from this and earlier campaigns resulted in implementation of the IHI Improvement Map, which includes 73 processes and suggestions for implementation, expected outcomes and metrics to measure each 52 Id. Andrew D. Hackbarth et al, Interpreting the “Lives Saved” results of IHI’s 100,000 Lives Campaign, 8(5), Joint Commission Benchmark,1, September/October 2006, available at http://www.ihi.org/NR/rdonlyres/A3552730-6841-4269-A783BF73E125401E/0/JointCommisionBenchmarkSeptOct06.pdf 54 See supra note 48, Frequently Asked Questions about the 5 Million Lives Campaign, available at http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=6 (last visited Feb. 21, 2011) 55 Id. at 2, The 5 Million Lives campaign defines medical harm as “Unintended physical injury resulting from or contributed to by medical care (including the absence of indicated medical treatment), that requires additional monitoring, treatment or hospitalization, or that, results in death. Such injury is considered harm whether or not it is considered preventable, resulted from a medical error, or occurred within a hospital.” 56 Id. 57 See supra note 54 53 12 process.58 The map was launched in September 2009 and is provided as a free resource tool for organizations to use in their quality management and efforts to improve patient care.59 The elements in IHI’s Improvement Map are categorized by patient care, support care and leadership and management processes and were developed according to IOM’s six improvement aims.60 They also provide reasons and implications, resources and attributes including cost, time, and difficulty to implement and as levels of evidence. The attributes are rated on a scale of 0-3. For example, Level of Evidence (the degree to which the actions of the process are supported by research and experience) and can be rated by a 0=uncertain, 1=provides strong evidence, 2=provides some evidence and 3=opinion (those experienced in a few case studies).61 IHI represents a vastly improved approach over TJC’s. IHI’s approaches in reducing adverse events are focused on best practices, while TJC’s standards and NPSG’s, at times, lack strong supporting evidence.62 For example, TJC converted the CDC and World Health Organization hand hygiene guidelines and mandated hospitals to measure compliance without specific methods or procedures to ensure validation of compliance rates.63 Unlike TJC, IHI’s initiatives provide measurable results that can be 58 See supra note 39, Improvement Map, http://www.ihi.org/IHI/Programs/ImprovementMap/ImprovementMap.htm?TabId=1 (last visited Feb. 10, 2011) 59 Id. 60 Id., Quick Reference Guide; Exploring a Process, available at http://www.ihi.org/NR/rdonlyres/6D5C6093-5C17-41D5-BA9EEDB7AF0C4B1E/13179/ImprovementMapQuickReference.pdf (last visited Feb. 26, 2011) 61 Id. 62 Michael Edmond and Theodore C. Eickhoff, Who is Steering the Ship? External Influences on Infection Control Programs, CID 46, Healthcare Epidemiology, 1748, 1746-1750, (June 1, 2008), available at http://cid.oxfordjournals.org/content/46/11/1746.full.pdf+html (last visited Feb. 26, 2011) 63 Id. 13 traced to their interventions. TJC provides no mandate for hospitals to report outcomes from the NPSGs to ensure the interventions are actually improving outcomes. 2. The National Quality Forum (NQF) NQF is a nonprofit organization that aims to improve the quality of healthcare for all Americans through fulfillment of its three-part mission including setting national priorities and goals for performance improvement; endorsing consensus standards for measuring and reporting; and promoting attainment of the national goals through education.64 They estimate that, despite all efforts, medical-related harm is now the third leading preventable cause of death in America.65 In 2002, NQF published its first report on Serious Reportable Events in Healthcare, which identified 27 preventable adverse events that should never occur in hospitals and if they did occur, what events would need to be reported.66 The report was updated in 2006, which provided a summary of progress by organizations using the list and guidelines for those who would be implementing a reporting system. This program is contracted through the Department of Health and Human Services (HHS) and is now due for review with a new report to be published in 2011.67 64 The National Quality Forum, http://www.qualityforum.org/About_NQF/About_NQF.aspx (last visited Oct. 25, 2010) 65 Id., Safe Practices for Better Healthcare-2010 Update, A Consensus Report, iii, i-ix, (April 24, 2010), available at http://www.qualityforum.org/Publications/2010/04/Safe_Practices_for_Better_Healthcare_%E2%80%93 _2010_Update.aspx 66 See supra note 64, Patient Safety: Serious Reportable Events Healthcare, http://www.qualityforum.org/projects/hacs_and_sres.aspx (last visited Feb. 10, 2011) 67 Id. 14 Presently, there are 27 states and the District of Columbia that have implemented reporting systems to analyze and learn from their mistakes.68 Most have incorporated some of the NQF’s serious reportable events (SREs), also known as Never Events.69 SREs are devastating and preventable, and healthcare organizations are under pressure to completely eliminate them. In 2007, CMS announced that Medicare would no longer pay for treatment that is necessary as a result of 10 specific costly or common events effective October 1, 2008.70 In 2003, NQF released its set 30 of safe practices that were designed for use in clinical care areas to reduce the risk of medical-related harm to patients.71 The 2010 report presents 34 practices, all of which have demonstrated to reduce the incidences of adverse events, including creating and sustaining a culture of safety, informed consent, matching healthcare needs with service delivery capability, information transfer and clear communication, medication management, prevention of HAIs, condition and site-specific practices.72 NQF’s focus in efforts to achieve quality is employing uniform standards, then reporting and measuring performance of the standards to analyze and determined where 68 Id., The Power of Safety: Sate Reporting Provides Lessons in Reducing Harm, Improving Care, http://www.qualityforum.org/Publications/2010/06/Quality_Connections__The_Power_of_Safety__State _Reporting_Provides_Lessons_in_Reducing_Harm,_Improving_Care.aspx 69 Agency for Healthcare Research and Quality, AHRQ Patient Safety Network – Patient Safety Primers, Never Events, available at http://psnet.ahrq.gov/primer.aspx?primerID=3 (last visited Feb. 10, 2011) 70 OEI-06-09-00360, Adverse Events in Hospitals: Public Disclosure of Information About Events, 17, 1-19, available at http://oig.hhs.gov/oei/reports/oei-06-09-00360.pdf (last visited Feb 21, 2010) The 10 events include foreign object inadvertently left in patients after surgery, air embolism, transfusion with wrong type of blood, stage II, IV pressure ulcers, falls, poor glycemic control, catheter-associated urinary tract infection, vascular catheter-associated infection, deep vein thrombosis/pulmonary embolism related to knee or hip replacement surgery, surgical site infections 71 See supra note 63, Safe Practices2003, at http://www.qualityforum.org/Publications/2003/05/Safe_Practices_2003.aspx 72 See supra note 64 15 patient care is falling short.73 Once again, there is approach evidence-based and outcomes can be traced to their standards, while some of TJCs standards lack the same capability or grounding. 3. Michigan Keystone ICU Project In 2002, HHS estimated that HAIs were among the leading causes of death in the United States, accounting for 1.7 million infections and 99,000 deaths and another 1.6 million to 3.8 million infections occurring in long-term care facilities.74 HHS also estimated that patients admitted into hospitals with antimicrobial resistant microorganisms continue to increase, more than tripling since 2000.75 In an effort to improve patient safety, the Michigan Health and Hospital Association Keystone ICU project was developed by researchers from Johns Hopkins University, undertaking a state-wide initiative that adopted evidence-based interventions for improving mortality rates from HAIs.76 Funding for the project was provided by AHRQ and was initiated in October 2003 ending December 2006.77 73 See supra note 64, Setting Priorities, NQF in the Quality Landscape, available at http://www.qualityforum.org/Setting_Priorities/NQF_in_the_Quality_Landscape.aspx (last visited Feb. 26, 2011) 74 U.S Department of Health & Human Services, Healthcare-Associated Infections, 1, 1-2, available at http://www.hhs.gov/ash/initiatives/hai/index.html (last visited Feb. 11, 2011) 75 Id. 76 Allyson Lipitz-Snyderman et al, Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis, 342:d219 doi:10.1136/bmj. d219, BMJ, 1, 1-7, (2011), available at http://www.bmj.com/content/342/bmj.d219.full.pdf The project took a comprehensive approach to improving patient safety including promoting a culture of safety, improving communication between providers and implementing evidence based practices to decrease rates of catheter related bloodstream infections (promoting hand washing, full barrier precautions, skin antisepsis with chlorhexidine, avoiding the femoral site during catheter insertion, removing unnecessary catheters)and ventilator associated pneumonia (mechanical ventilator “bundle” using semi-recumbent positioning, daily interruption of sedation infusions and prophylaxis for peptic ulcers and deep venous thrombosis). 77 Id. at 2 16 After base-line data was gathered, the project was initiated in Michigan’s ICUs and those patients receiving Medicare benefits. After 22 months, the researchers found that a patient’s chance of dying of HAIs decreased by almost 24% compared to surrounding states where the program was not implemented.78 This ground-breaking voluntary initiative is also founded upon evidence-based efforts, and has led to substantially improved patient safety outcomes. In comparison, TJC efforts on HAIs have not yet resulted in reduced iatrogenic infections while total costs continue to rise. The Centers for Disease Control and Prevention (CDC) estimates that approximately 1 out of every 20 hospitalized patients will contract an HAI79 with annual direct medical costs between from $35.7 to $45 billion,80 despite TJC focused efforts in this realm. 78 AHRQ Medical Errors & Patient Safety Update, Landmark Initiative to Reduce Healthcare-Associated Infections Cuts Deaths Among Medicare Patients in Michigan Intensive Care Units, (February 1, 2011) available at http://www.ahrq.gov/news/press/pr2011/haimiicupr.htm 79 Centers for Disease Control and Prevention, Healthcare-associated Infections, HAIs, The Burden, available at http://www.cdc.gov/HAI/burden.htmlt (last visited Feb. 26, 2011) 80 Id., R. Douglas Scott II, The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention, (March 2009), available at http://www.cdc.gov/ncidod/dhqp/pdf/Scott_CostPaper.pdf (last visited Feb. 26, 2011) 17 III. The Joint Commission “Accidents will occur in the best regulated families.” 81 John Dos Passos ________________________________________________________________________ A. Brief History In 1910, Ernest Codman, M.D., developed a system called the End Result Theory that would allow hospitals to track every patient it treated to determine if the treatment was effective.82 At the time, he was on staff at the Massachusetts General Hospital but left to start his own private hospital, which he named the End Result Hospital.83 His hospital differed from others in that he admitted his errors, believing that covering up errors was not in the best interest of the public.84 In 1913, Dr. Codman, with Drs. George W. Crile and Charles H. Mayo, founded the American College of Surgeons (ACS); and the end result system became an ACS stated objective.85 Four years later, the ACS developed the Minimum Standard for Hospitals and began on-site inspections in 1918 and only 89 of the 692 hospitals met the requirements of the standards.86 In 1926, the first standard manual was printed which 81 Brainy Quote, Accidents Quotes, http://www.brainyquote.com/quotes/keywords/accidents.html (last visited Feb. 11, 2011) 82 See supra note 3, A Journey Through the History of the Joint Commission, 1, 1-12, (August 2009) available at http://www.ncamss.org/AnnualMtg2009/Dengler%20-%20Joint%20Commission%20History.pdf 83 D Neuhauser, Heroes and Martyrs of Quality and Safety, Ernest Amory Codman MD, 11, Qual Saf Health Care 104, 104-105, (2002) available at http://qshc.bmj.com/content/11/1/104.full.pdf 84 Id. 85 See supra note 82 at 1 86 See supra note 82 at 2 18 consisted of 18 pages. By 1950, more than 3,200 hospitals achieved approval based on the ACS standards.87 In 1951, the American College of Physicians (ACP), the American Hospital Association (AHA), the American Medical Association (AMA), and the Canadian Medical Association (CMA) joined with the ACS to create the Joint Commission on Accreditation of Hospitals (JCAH), an independent, not-for-profit organization whose primary purpose is to provide voluntary accreditation.88 The ACS transferred its Hospital Standardization Program to JCAH in 1952. They began offering accreditation to hospitals using their Standards for Hospital Accreditation the following year and began charging for their surveys in 1964.89 In 1987, JCAH changed its name to the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) to indicate its expanded scope of activities and new set of initiatives designed to place emphasis of the accreditation process on actual performance of the organization.90 On January 1, 2007, JCAHO changed its branding to The Joint Commission (TJC) in support of its efforts to continually improve the value of accreditation.91 B. Deemed Status In order for health care organizations to participate in Medicare and Medicaid programs, they must meet the Center for Medicare & Medicaid Services (CMS) Conditions of Participations (CoPs). The requirements meet the minimum health and safety standards are the foundation for improving quality and protecting the health and 87 See supra note 82 Id. 89 Id. 90 Id. at 4 91 Id. at 9 88 19 safety of patients that are enrolled in public programs.92 Through a process called “deeming”, CMS ensures that the standards of accrediting organizations meet or exceed the Medicare standards set forth in the CoPs.93 Health care organizations have the options of using CMS, State, or other accreditation agencies that have deemed status. Most of the nation’s hospitals choose TJC to demonstrate their fulfillment of CoP.94 TJC (JCAH at the time) was originally granted exclusive deeming status in the Medicare provisions of the Social Security Amendments of 1965.95 At the time, other national organizations were coming together to form voluntary, non-for-profits accreditation organizations.96 Congress, being new to the health care quality business, deferred to the expertise of TJC as they had been accrediting hospitals based on quality standards for the past 14 years.97 Also, through this law, congress granted this deemed status while limiting CMS’ oversight of TJC as well the executive branch’s authority in the accreditation process.98 In 1966, TJC’s board decided to redefine their role and made a decision to revise their standards to reflect an optimal achievable rather than a minimal essential level of 92 See supra note 2 Id. 94 See supra note 3, Facts about Joint Commission Accreditation and Certification, 1, 1-2, “The Hospital Accreditation Program has been in existence in some form for more than 60 years. Today, it accredits approximately 4,250 general, children’s, long term acute, psychiatric, rehabilitation and surgical specialty hospitals. Approximately 88 percent of the nation's hospitals (including critical access hospitals) are currently accredited by The Joint Commission.” http://www.jointcommission.org/assets/1/6/Accreditation_and_Certification_10_09.pdf (last visited Feb. 11, 2011) 95 Juliet Battard Menendez, The Impetus for Legislation Revoking the Joint Commission’s Deemed Status as a Medicare Accrediting Agency, 12(3), JONAS Healthc Law Ethic Regul., 70, 69-76, (Jul-Sep 2010), available at http://www.nursingcenter.com/prodev/ce_article.asp?tid=1062299 96 Id. 97 Id. 98 Id. 93 20 care.99 This decision was made for two reasons. First, the majority of hospitals in the nation achieved and was maintaining the minimum standards. The standards were no longer a challenge for hospitals to reach for at the levels of quality care that the board thought could be attained.100 The second reason was that federal conditions and the regulatory codes that the states were writing closely resembled those of TJC.101 TJC realized that the changes were needed to remain the primary accreditator in the nation. C. Office of Inspector General and Government Accountability Office Reports 1. Office of Inspector General Report In 1999, in response to industry related criticism regarding the rigidity and quality of the hospital surveys conducted by then-JCAHO, the Office of Inspector General of the Department of Health and Human Services (OIG) published a report that concluded TJC surveys provided an important vehicle for reducing risk and fostering improvement.102 The report found, however, that although the current system of hospital oversight had significant strengths that help protect patients, there were also major deficiencies including the fact that TJC’s surveys were unlikely to detect practitioners with questionable or substandard skill sets.103 Also, the quick paced, structured survey process 99 James S. Roberts et al, A History of the Joint Commission on Accreditation of Hospitals, 258(7), JAMA 938, 936-940, (Aug 21, 1987), downloaded from www.jama.com at University of California – San Diego (last visited Nov., 1, 2010) 100 Id. 101 Id., “In the mid 1960’s the Joint Commission found itself no longer the advanced and lonely leader. The Federal government wrote its conditions for participation in Medicare. State after state with new refurbished licensing authority wrote regulatory codes where there had been few or none before…and it is more than coincidence that the federal conditions and, more particularly, the state codes bore a strong family resemblance to the Joint Commission’s accreditation standards…the Joint Commission seemed almost overnight to be struggling to stay even in the vanguard of progress. And it was challenged, most seriously as being no longer necessary because now everybody was beginning to do what it had once done alone.” Dr. John Porterfield, TJC Director at the time 102 OEI-01-97-00050, The External Review of Hospital Quality, A Call for Greater Accountability, (July 1999), 2, 1-7, available at http://oig.hhs.gov/oei/reports/oei-01-97-00050.pdf 103 See supra note 102 21 left limited opportunities to perform an in-depth examination of the hospitals conditions of practice; and instead of random selection of medical records for review, surveyors tended to rely on staff to choose the records.104 The report also found that the then Health Care Financing Administration (HCFA), now CMS, did little to hold TJC or state agencies accountable for their performance in overseeing hospitals, and that feedback on their performance was limited.105 Public disclosure also played a minimal role in holding TJC and State agencies accountable.106 As a result of their findings, the OIG recommended that HCFA steer external reviews of hospital quality so that they ensure a balance between collegial and regulatory modes of oversight, including continued presence of on-site surveys, both announced and unannounced.107 The OIG also recommended that HCFA should periodically assess the justification for JCAHO’s deemed status authority.108 2. Government Accountability Office Report TJC launched its new accreditation process in January 2004, Shared Visions-New Pathways, and moved from using announced to unannounced surveys starting in 2006. In July 2006, the Government Accountability Office (GAO) also reviewed TJC activities. It focused its study on the extent to which TJC’s pre-2004 hospital accreditation process, 104 Id. See supra note 102 at 3 106 Id. at 4 107 Id. at 5 108 Id. 105 22 identifying hospitals not complying with Medicare requirements, the potential of the new TJC process, and the effectiveness of CMS’s oversight of TJC’s hospital accreditation program.109 In contrast to the OIG, the GAO found that TJC’s pre-2004 hospital accreditation process did not identify serious deficiencies in Medicare standards found by state survey agencies. In a sample of 500 TJC accredited hospitals, state agency validation surveys from 2000 through 2002 found 31 percent (157) with deficiencies. Of these 157 hospitals, TJC did not find deficiencies of Medicare requirements in 123 (78 percent).110 Based on the study findings, the GAO advised the congressional committees that TJC was missing too many serious problems in its surveys and was failing as a consumer advocate for patients.111 The GAO’s remedy to this problem was to give CMS more authority over TJC’s accreditation process. TJC responded to the GAO’s key recommendation to Congress providing CMS increased authority over TJC in a letter from TJC President Dennis S. O’Leary, M.D. dated July 12, 2004: The Joint Commission interposes no objection to this suggested statutory change but takes great exception to the fact that the GAO arrives at this conclusion based upon a flawed study methodology and erroneous, alarming statistics that seriously mislead the public and do a great disservice to the Joint Commission …. The Joint 109 GAO-04-850, CMS Needs Additional Authority to Adequately Oversee Patient Safety in Hospitals, 2, 1-58, (July 2004), available at http://www.gao.gov/new.items/d04850.pdf 110 Id 111 See supra note 95 at 74 23 Commission never sought this deemed status relationship nor was it even aware of the framing of the statutory provision respecting hospital accreditation.112 Despite these TJC statements, four years after the GAO’s recommendations, the 110th Congress passed the Medicare Improvements for Patients and Providers Act of 2008, in which Section 125 revoked the unique deeming authority of TJC.113 After participating in a new hospital deeming authority process, CMS announced in December 2009 that TJC could continue to hold a non-exclusive deeming authority for hospitals through at least 2014.114 D. Survey Process and Fees for Accreditation 1. Survey Process All of TJC’s surveyors are employees of TJC and many remain employed in hospitals or private practice.115 All surveyors must pass a certification exam while training is on-going, keeping them up-to-date on changes in survey, performance evaluations, and standards.116 TJC conducts unannounced surveys between 18-39 months after an organization’s prior survey.117 Timing of the survey is based on pre-survey data provided to TJC from the organization’s Priority Focus Process (PFP).118 Information 112 See supra note 109 at 46 See supra note 95 at 74 114 Fierce Healthcare, Daily News for Healthcare Executives, CMS approves Joint Commission’s hospital deeming authority, (Dec 3 2009), available at http://www.fiercehealthcare.com/story/cms-extends-relationship-joint-commission/2009-12-03 115 Diane Meldi et al, The Big Three: A Side by Side Matrix Comparing Hospital Accrediting Agencies, NAMSS Industry & Government Relations Committee, 13, 12-14, Synergy, (January/February 2009), available at http://www.hfap.org/mediacenter/NAMSS%20Synergy%20JanFeb09_Accreditation%20Grid.pdf (last visited Feb. 20, 2011) 116 Id. 117 See supra 2, Facts about the unannounced survey process, (Sept. 2009), available at http://www.jointcommission.org/assets/1/18/Unannounced_Survey_Process_2010.pdf (last visited Feb. 27, 2011) 118 Id., Facts about the Priority Focus Process, (Sept. 2009), available at 113 24 supplied from the PFP tool helps surveyors to focus on issues that are significant to patient safety and quality of care provided by the facility and to evaluate performance more consistently.119 In 2004, TJC developed a new system for on-site surveys called the tracer methodology which was designed to follow and evaluate the quality of a patient’s healthcare experience while offering patient-centered and process-focused survey instead of a paper labored process.120 Using this method, the surveyors select a patient and use that individual’s medical record to track the patient’s movement through the different areas in the facility to assess and evaluate compliance with TJC standards and the organization’s systems for delivering safe, quality care.121 TJC’s survey process strives to ensure that scoring and decision process are congruent with the organization’s performance and TJC standards, transparent and easily understood by all involved and based on the criticality of the standards (those that more directly impact the patient than others).122 The elements of performance (EPs) are those expectations that determine if a standard is in compliance.123 Those that receive a partially or insufficiently compliant EPs must be addressed through the Evidence of http://www.jointcommission.org/assets/1/18/Priority_Focus_Process_2010.pdf (last visited Feb. 27, 2011) 119 See supra note 118 120 See supra note 115 121 See supra note 3, Facts about the Tracer Methodology, (Sept. 2010), available at http://www.jointcommission.org/assets/1/18/Tracer_Methodology_2010.pdf (last visited Feb. 27, 2011) The number of tracers completed during a survey depends on the patient’s length of stay. Patients are selected from the facility’s active patient list and most-likely received multiple or complex services during their inpatient stay and any prior outpatient activity related to that stay (continuum of care) 122 See supra note 3, Facts about scoring and accreditation decisions for 2011, (Dec. 2010), available at http://www.jointcommission.org/assets/1/18/Scoring_Accreditation_Decisions_2011.pdf (last visited Feb. 27, 2011) Compliance of EPs are scored on a three-point scale with 0=insufficient, 1=partial and 2=satisfactory. visited Feb. 27, 2011) 123 Id. 25 Standards (ESC) process, time-line for completions (45 or 60 days) depends on how critical the findings how immediate the risk is.124 Accreditation decisions125 are made once TJC receives the organization’s ESC along with their Measures of Success (MOS) which shows how they have corrected the sufficiency and their track record for maintaining compliancy.126 Also, in regards to deficiencies, CMS CoPs are embedded in their core standards; however, TJC does expand beyond those standards127 which may lead to deficiencies during a survey that may not occur with an actual CMS site survey. 2. Fees for Accreditation Annual fees are based on the size and the service complexity of the organization with the average cost being $33,000.128 Additional revenues for TJC inspections include those associated with the number of surveyors and total number of days spent at the site.129 TJC’s also receives revenues (and accreditation hopefuls pay) for preparing and maintaining accreditation include services that are provided by TJC’s for profit affiliate, Joint Commission Resources (JCR).130 JCR sells TJC’s accreditation manuals, consulting services such as mock surveys to assess current accreditation status as well as other publications to hospitals to help them prepare and maintain their accreditation status.131 124 See supra note 122 Id. The five accreditation decisions are Preliminary, Accreditation, Accreditation with Follow-up Survey Contingent, Preliminary Denial of Accreditation and Denial. 126 See supra note 121 127 Patricia Kienle, Speaking of Accreditation Options, PPP Mag, Vol.7 No. 12, 2, (December 2010), available at http://www.pppmag.com/article/801/December_2010/Speaking_of_Accreditation_Options/ 128 See supra note 115 at 14 129 See supra note 3, About the Joint Commission, available at http://www.jointcommission.org/about/JointCommissionFaqs.aspx?faq#372 (last visited Feb. 27, 2011) 130 Joint Commission Resources, Products and Services, available at http://www.jcrinc.com/Products-and-Services/ (last visited Feb. 27, 2011) 131 Id. 125 26 JCR’s revenue for these services totaled over $51 million in 2008.132 However, conflict of interest issues have arisen since TJC created JCR in 1986 and creation of their firewall policies in 1987. Of particular interest has been the relationship between JCR’s consulting services and TJC’s accreditation process. 133 In 2006, the GAO was asked to study this relationship by the congress and report its findings. In December 2006, the GAO published its findings that beginning in 2003, TJC and JCR reviewed their policies and revised and implemented new guidelines to strengthen the firewall between the two organizations including oversight of implementation and compliance with the firewall policies to ensure JCR’s consulting services did not affect or be perceived to affect TJC’s accreditation process.134 However, substantive questions remain as to the influence of surveyor findings on anticipated future consulting. There have been no assessments of TJC/JCR’s method to mitigate these conflicts, and institutional conflicts of interest have not been evaluated. 132 DNV Managing Risks, DNV Accreditation Program Frequently Asked Questions, 2, 1-9, available at http://dnvaccreditation.com/pr/dnv/document/FAQ.pdf (last visited Jan. 22, 2011) 133 GAO-07-79, Hospital Accreditation, Joint Commission on Accreditation of Healthcare Organizations’ Relationship with Its Affiliate, 2, 1-37, (December 2006), available at http://www.gao.gov/new.items/d0779.pdf (last visited Feb. 28, 2011) 134 Id. at 4 27 IV. Alternative Accreditation Organizations and Quality Guidelines “The absence of alternatives clears the mind marvelously.” 135 Henry A. Kissinger ________________________________________________________________________ Although TJC is the main source for accreditation in the industry, medical errors continue to rise, billions of dollars are being wasted and deaths relating to needless adverse events is now the third leading preventable cause of the in the nation. TJC has had limited effectiveness in its accreditation approach in improving patient safety outcomes. However, there are two other alternatives that are authorized by CMS to survey hospitals for compliance with the Medicare CoPs that may promote patient safety and quality management processes with different survey processes than TJC. A. Healthcare Facilities Accreditation Program (HFAP) HFAP, under the American Osteopathic Information Association, was originally created in 1945 to provide an objective review of services conducted by osteopathic hospitals.136 They have maintained deeming status since 1965 and last received renewed deeming authority in 2009 that is effective through September 2013.137 HFAP meets or exceeds CMS standards and provides accreditation services to hospitals and their clinical 135 “Quote DB”, http://www.quotedb.com/quotes/1468 (last visited Feb. 13, 2011) Healthcare Facilities Accreditation Program, Overview, available at http://www.hfap.org/about/overview.aspx (last visited Jan. 22, 2011) 137 42 CFR § 488, Medicare and Medicaid Programs; Application of the American Osteopathic Association for Continued Deeming Authority for Hospital, (2009) available at http://www.hfap.org/pdf/CMSFederalReg2009.pdf 136 28 laboratories, ambulatory care/surgical, mental health, substance abuse and rehabilitation facilities as well as critical access hospitals and stroke centers.138 There are nearly 200 hospitals and over 200 other healthcare facilities and laboratories accredited by HFAP.139 Their standards are incorporated from a variety of sources including CMS CoPs, NQF 30 Safe Practices, along with endorsing the IHI 5 Million Lives Campaign.140 Unlike TJC, HFAP’s surveyors are not employed by the organization. The survey teams are paid volunteers that consist of physicians, nurses and administrators with significant, demonstrated experience. They represent leadership in their own organizations that bring a current understanding of the healthcare industry to the survey process.141 The survey process includes a comprehensive, non-biased, thorough review of patient-centered processes and is conducted in the least disruptive way as possible.142 They are educationally focused and success on these surveys is based on the organization’s ability to correct deficiencies. If deficiencies are identified, the surveyors draw from their own experiences and offer feasible solutions, many times at the point of discovery.143 Discrepancies are reported to the HFAP office and the facility is sent a comprehensive report for which they must submit a Plan of Correction within 30-60 138 See supra note 115 Id. 140 See supra note 115 141 Id. at 13 142 Id. at 14 143 Id. at 12 139 29 days.144 HFAP has three categories of accreditation decisions including Full, Interim or Denial.145 Their survey cycle is every three years and the average cost for their services is $25,000, depending on the size and complexity of the facility. This pricing structure has tremendous advantages, since it varies only by the size and volume of the organization. Further, because their standards are so clearly written, additional consults or workshops are not required like under TJC and sold by JCR. Total HFAP fees include a triennial registration fee, purchase of the accreditation standards manual, and reimbursement for direct costs including the number of surveyors and their travel costs.146 This system has advantages over TJC efforts. Beyond clarity of accreditation costs, their standards are closely cross-walked to and do not go beyond CMS CoPs. This avoids confusion when assessing and addressing requirements from the HFAP standards manual.147 HFAP also incorporates the NFQ safe practices, which have proven to be effective in improving patient safety outcomes. Hence, reduced costs, regulatory clarity, and integration of important successful initiatives are the basis for HFAP accreditation and advantages over TJC patient safety efforts. B. Del Norske Veritas Healthcare Inc. (DNV) and International Organization for Standardization (ISO) 9001 Standards DNV’s accrediting program is called the National integrated Accreditation for Healthcare Organizations (NIAHO) and was given deeming status for hospitals effective 144 Id. at 13 Id. 146 See supra note 109, Working with HFAP, 2, 1-2, available at http://www.hfap.org/WhyHfap/workingwithhfap.aspx (last visited Feb 21, 2011) 147 Id. at 1 145 30 September 26, 2008.148 It is the first new hospital accreditation program in the United States in 40 years, and has accredited close to 100 hospitals since its inception.149 DNV developed their program by integrating the CMS CoPs and the ISO 9001 Quality Management System. The ISO was founded in Geneva in 1947 to provide standardized technical specifications for products being traded in the international market.150 There are now members in over 150 countries and more than 10,000 ISO standards being used worldwide.151 The ISO 9001 quality management standards were developed in 1987 and the first draft of standards for healthcare were developed in 2001 and published by the American Society for Quality in partnership with the Automotive Industry Action Group, who first brought the ISO concepts to the US in the late 1980’s.152 Currently, of the approximately 100 healthcare facilities in the US that are certified, there are 12 hospitals and 10 medical groups.153 Hospitals do not need to be ISO compliant before receiving DNV accreditation; instead, they have three years to become compliant after the initial survey.154 The term “compliant” means the hospital has implemented the ISO standards; certification is a 148 David Gourley, Competitor to Joint Commission approved by CMS, Accreditation News, Journal for Respiratory Care & Sleep Medicine, 1, 1-3, (July 1, 2009), available at http://www.thefreelibrary.com/_/print/PrintArticle.aspx?id=207360830 149 DNV Annual Report, We’ve waited 40 years for a new choice. If you’re still waiting, it’s your patience that is winning, not your patients, available at http://www.ebookdnv.com/hcannualreport/ (last visited Feb. 14, 2011) 150 James M. Levett, Implementing and ISO 9001 Quality Management System in a MultiSpecialty Clinic, Nov., Dec. 2005, 1, 1-5, available at http://dnvaccreditation.com/pr/dnv/document/dr._levett_tcm4-321304.pdf (last visited Feb. 13, 2011) 151 Id. 152 Id. 153 Id. 154 See supra note 132 at 2 31 process that requires significant additional documentation apart from CMS requirements and an additional fee for the certification survey.155 DNV uses the same tracer methodology as TJC. Surveyors include physicians, registered nurses, and Physical Environment Specialists that come with a facilities and safety background, and who must complete NIAHO Surveyor and ISO 9001 Lead Auditor didactic training.156 Unlike TJC’s survey scoring process that evaluates elements of performance on a scale of satisfactory, partial or insufficient compliance, DNV does not use an aggregated system. The organization is responsible for developing and implementing corrective actions plans with facilities to address all nonconformities identified.157 DNV’s accreditation categories include Accredited, Jeopardy Status and Not Accredited.158 The cost for a DNV survey depends on the number of surveyors, length of survey, size of the facility, average daily census, and complexity of the services offered, special care units, and off-site locations. The average cost for their annual survey is $23,100,159 with the number of full time equivalents (FTEs) being the driving factor when estimating total costs.160 Their quotes include all survey fees, travel and other expenses with no hidden charges unlike those associated with TJC’s accreditation process, i.e., JCR consulting and manual fees.161 Advantages to using DNV accreditation are that surveys are outcome-based instead of inspection focused, the quantity of findings does not determine the 155 Id. at 5 Id. 157 See supra note 152 at 13 158 Id. 159 Id. at 14 160 Id. at 8 161 Id. 156 32 accreditation status, and an innovative, coordinated and cooperative approach to patient safety is encouraged instead of a narrow path to TJC compliance.162 It also has a global reputation for quality in certifications, standards development, and risk management in several types of industries.163 DNV has issued 1,200 ISO certificates to healthcare facilities worldwide including hospitals, outpatient clinics, diagnostic centers, laboratories, nursing homes and home care organizations.164 Outcomes relating to decreased events of preventable medical errors for organizations accredited by DNV are too early to determine as its approaches have been in place for approximately two years. 162 See supra note 132, Advantages of DNV Accreditation, 1, 1-2, available at http://www.dnv.com/industry/healthcare/hospital_accreditation/niaho_advantages/ (last visited Feb. 13, 2011) 163 See supra note 152 at 13 164 See supra note 160 at 2 33 V. Recommendations “You give them recommendations. You throw different angles at them where, hopefully, they can get something out of it.”165 Mike Butcher ________________________________________________________________________ Over a decade ago, the IOM published their four-tiered strategy to reduce preventable medical errors by a minimum of 50% within the next five years. Still, billions of dollars have been lost and millions of patients continue to die because our health care industry has failed to meet the key recommendations set forth by the IOM.166 While the recommendations were designed to balance efforts among the regulatory and private sectors, response at the federal level has been slow. Since the 2000 report, Congress introduced five medical error bills but none were adopted, which indicates that Congress has a lack of urgency about the problem.167 Yet studies show that preventable medical errors kill four times as many people as the lack of medical insurance.168 Instead of a policy focus on this key medical and public health concern, countless hours and debate instead has centered on the Affordable Health Care for America Act that was signed by President Obama in March 2010. 165 See supra note 65, Quotes on Recommendations, available at http://www.brainyquote.com/quotes/keywords/recommendations.html (last visited Feb. 14, 2011) 166 Consumers Union, Safe Patient Project, To Err is Human – To Delay is Deadly Ten Years Later, a million lives lost, billions of dollars wasted, (May 2009), 1, 1-13, available at http://www.safepatientproject.org/2009/05/to_err_is_humanto_delay_is_dea.html 167 Id. 168 Eric Nalder, Cathleen F. Crowley, Dead by Mistake, Health care bills sidestep medical errors issue, Hearst Newspapers, (Oct. 1, 2009), 1, 1-2, available at http://www.chron.com/disp/story.mpl/deadbymistake/6669310.html 34 Despite lack of effort at the federal level, the private sector has put-forth several initiatives that provide important insight. By combining the advantages of each, a more robust system of safety can accompany accreditation efforts. A. Outcomes Based versus Inspection Focused Surveys Accreditation agencies such as TJC have the power to mandate change. Yet the toll of preventable medical errors remains high. TJC’s check box approach to safety and accreditation (in the industry known as “blunt tools”) has limited potential to understand and unearth key aspects of institutional cultures and instead treats all facilities homogeneously.169 An example of TJC’s one-size fits all solution is evident in the roll out of their 2005 National Patient Safety Goal on medication reconciliation in an effort to prevent medication errors in hospital facilities. But the goal does not address important differences across facilities (e.g., academic center; community hospital; long term care acute hospitals; etc.), across geographic locales (e.g., rural, urban, suburban; Midwest, east coast, west coast, etc.), nor across resource availability (e.g., physicians, nurses, and other human resources; CT, MRI, PET scanners and other hard asset resources). Since that time, hospitals have understandably had difficulties in implementing effective processes to meet this goal.170 Only after 4-5 years of provider complaints did TJC revise the goal in 2009; however, TJC did not apparently respond effectively. After more 169 Robert M. Wachter, Understanding Patient Safety, McGraw Hill Medical,2008, 222, 3-298 American Society of Medication Safety Officers, admin’s blog, TJC: Medication reconciliation National Patient Safety Goal to be reviewed, refined, (February 6, 2009), available at http://www.asmso.org/node/19 (last visited Feb. 21, 2011) 170 35 criticism arose again from the field, TJC approved another streamed-lined and more focused version that will go into effect July 1, 2011.171 Another example of TJC’s blunt tools approach was in 1996 when its Sentinel Event Policy was established.172 In February 1998, TJC sent its first Sentinel Event Alert (SEA) to announce its new periodical that would provide important information on occurrence, management and prevention of sentinel events and ongoing information on TJC’s Sentinel Event Policy and Procedures.173 The first issue also provided a Medical Error Prevention Alert for Potassium Chloride (KCl). After reviewing more than 200 sentinel events, TJC found that the most common events were related to medication errors, and of those, the most frequent from the use of KCl.174 TJC’s Issue for Consideration suggested that health care organizations not make concentrated KCl available outside of the pharmacy unless appropriate 171 See supra note 3, Topic Library Item, National Patient Safety Goal on Reconciling Medication Information (NPSG.3.06.01), (December 7, 2010), available at http://www.jointcommission.org/npsg_reconciling_medication/ (last visited Feb. 21, 2011) 172 See supra note 3, Sentinel Event Alert, Board of Commissioners Affirms Support for Sentinel Event Policy, 1, 1-3, Issue 3, (May 1, 1998),available at http://www.jointcommission.org/assets/1/18/SEA_3.pdf (last visited Feb. 21, 2011) The Sentinel Event Policy applies to events that result in an “unanticipated death or major permanent loss of function, not related to the natural course of the patient’s illness or underlying condition..or a suicide of a patient in a setting where the patient receives around-the-clock care, infant abduction or discharged to the wrong family, rape, hemolytic transfusion reaction involving administration of blood or blood products having th major blood group incompatibilities, surgery on the wrong patient or wrong body part”. On May 11 , 1998, in Issue 4, the Board of Commissioners published revised and approved examples of sentinel events considered voluntarily reportable under TJC’s Sentinel Event Policy as well as examples of sentinel events that were not considered reportable under the policy. 173 See supra note 3, New Publication, Issue 1, (February 28, 1998), available at http://www.jointcommission.org/assets/1/18/SEA_1.pdf (last visited Feb. 21, 2011) 174 Id. (noting 10 incidences of patient deaths related to misadministration with eight from direct infusion of concentrated KCl). 36 safeguards were in place.175 However, no processes for implementing the safeguards were recommended and nothing addressed change in different institutional cultures. 176 In May of 1998, just three months after the policy was implemented, a SEA was issued announcing TJC’s approval of a more detailed definition of voluntary reporting of sentinel event occurrences reportable to TJC. This included procedural revisions to help organizations comply with the policy, strategies to minimize the risk of discoverability of information related to sentinel events, continued exploration of processes to close identified gaps in confidentiality protection, and provisions for on-site root causes analysis (RCA) and a 30-day period to submit RCAs for organizations that chose to not voluntarily self report.177 However, criticism also emerged from the health law field on the premise that mandating healthcare organizations to voluntary report SEAs showed inattention to the legal culture of discovery and absence of immunity.178 Currently, accredited organizations are encouraged, but not required, to report reviewable sentinel events; if TJC does become aware of an event by some other means such as from a patient, family member, employee or through the media, the organization must meet the expectations of the Sentinel Event Policy.179 Documents related to a sentinel event, including the RCA and action plan, are restricted to specially trained TJC 175 Id. On April 21, 2000, Issue 13 of the SEA was published including TJC’s response to its suggestions for improvement stating “TJC and various experts have provided recommendations on how other health care organizations can prevent the adverse events from happening in the future….some readers have interpreted these suggestions as being Joint Commission requirements. That was never the intention. These suggestions should be considered for implementation, but, if not appropriate for the individual health care organization, alternatives should be considered. The Joint Commission recognizes that other acceptable practices or approaches exist”. 177 See supra note 150 at 1 178 Bryan A. Liang & Kristopher Storti, Creating Problems as Part of the “Solution”: The JCAHO Sentinel Event Policy, Leal Issues, and Patient Safety, 33(2), J Health Law, 263, (Spring 2000) 179 See supra note 3, Facts about the Sentinel Event Policy, 1, 1-3, (Sept. 2009), available at http://www.jointcommission.org/assets/1/18/Sentinel%20Event%20Policy.pdf (last visited Feb. 21, 2011) 176 37 staff following policies and procedures designed to protect the confidentiality of the documents.180 Once data is reviewed by TJC, it is entered into the Sentinel Event Database, information that was electronically submitted will be de-identified and any provided paper documents will be destroyed or returned to the hospital.181 Given the fact that there has been little improvement over the past decade on incidences of preventable medical errors, current accreditation processes must be reviewed by entities that govern them in collaboration with the federal and private sectors. The customary approach using prescriptive standards that frequently change or are difficult to implement does little to foster a collaborative accreditation effort between surveyors and healthcare organizations interested in improving patient safety. B. Recommendations To address the issues surrounding medical errors, prevention is the key. Over a decade ago, the IOM recommended a four-tier approach which included developing a mandatory public reporting system to identify where and how errors occur and what interventions should be implemented for providers to provide the safest care possible. Until this is accomplished, it is impossible to research effectively the anatomy of medical errors. Some progress is being made at the state level with the NQF Never Event reporting initiatives; however, disclosure of privileged information is a barrier. Also, there still remains reluctance on the part of physicians, nurses and other care providers to report medical errors and near misses, one that is deeply rooted in the health care culture. 180 Id. Id. at 3 181 38 Deeming authorities must work at a state and federal levels to develop a system that can break the barriers to a mandatory reporting system. CMS has adopted the policy that is will no longer pay for care or treatment relating to 10 hospital-acquired conditions (HACs). Deeming authorities should participate with CMS to analyze the data to compare those hospitals with higher rates of HACs with those with lower rates to determine best practices and incorporate monitoring into their accreditation standards. Once these systems are in place, the accreditation agencies should be audited by CMS to ensure that their focus is on regulation rather than collegiality. Recommendations should also be made that deeming organizations should have a system in place to show aggregate safety results over a three-year period to determine their effectiveness in reducing errors and improving patient safety. CMS should then assess these approaches, act to identify key lessons on safety, and integrate successful approaches into updated CoPs for healthcare organizations to fulfill using successful accreditor approaches. Recommendations must also take into consideration an approach that focuses on the institution’s culture and their patient safety and quality management priorities while still complying with CMS CoPs. DNV’s approach to drive quality transformation from the point of care and up to the organization’s leadership and senior management teams is a key, successful, cooperative approach to doing so. This approach should be the focus of CMS evaluation efforts to determine best practices on improving safety in a timely way that takes entity structure and culture into account when evaluating outcomes.182 This will 182 See supra note 132, Comparison of Accreditation Organizations, 2, 1-3, available at http://www.dnvaccreditation.com/pr/dnv/document/comparison-dnvhc_to_tjc_tcm4-358498.pdf (last visited Feb. 27, 2011) 39 address the inappropriate use of blunt tools employed by TJC and also promote a culture of learning and internal promotion rather than a punitive “inspection” type system of TJC. Also, when an accreditation agency creates new standards or revisions to existing policies and procedures, the processes must be evidence-based, with clear guidance whenever possible, to negate ambiguity between surveyors, healthcare leaders and practitioners. Instead of a single accreditation entity requiring change that may or may not be evidenced based, entities that will be comparing treatment comparative effectiveness and innovation183 should also be given responsibility for issuing new safety standards. These standards should be uniform, evidence-based, and provide for models of implementation for differing institutional cultures, locales, and systems, with feedback to be incorporated in new standards and systems. In this manner, a justified, consistent, and uniform set of standards can emerge that is dynamically responsive to the individual locales while continuously improving on the basis of field experience, not TJC or other accreditor assumptions of standard applicability in all contexts. What is key in promoting patient safety is an avoidance of the very compliance driven, top down mandates that TJC in its present and earlier iterations have represented. TJC was the patient guard for quality and safety in health care, yet its almost 50 years of efforts culminated in critical OIG, GAO, and, of course, IOM Reports. CMS, employers, insurers, and patients should demand that policymakers work to create and improve systems that substantively improve safety dynamically and continuously using the experience of providers and the knowledge from research. Continuous loops of 183 These include Center for Medicare and Medicaid Innovation, Patient Centered Outcomes Research Institute, Center for Quality Improvement and Patient Safety. See Bryan A. Liang & Tim Mackey, Quality and Safety in Medical Care: What Does the Future Hold? ARCH. PATH. LAB. MED. (2011); forthcoming. 40 information and improvement using existing and available systems will provide the basis for improving safety, as they have done in other industries.184 184 See, e.g., William Riley, Bryan A. Liang, William Rutherford, & William Hamman, Structure and Features of a Care Enhancement Model Implementing the Patient Safety and Quality Improvement Act. ADVANCES IN PATIENT SAFETY: NEW DIRECTIONS AND ALTERNATIVE APPROACHES Vol. 1: Assessment (Kerm Henriksen, James B. Battles, Margaret A. Keyes, Mary L. Grady, eds.) 59-70 (2008) (discussing care enhancement model employing aviation systems); and Bryan A. Liang, William Riley, William Hamman, & William Rutherford, The Patient Safety and Quality Improvement Act of 2005: Provisions and Potential, 22(1) AM. J. MED. QUAL. 8 (2007) (discussing use of Patient Safety Organizations to promote quality and safety in healthcare). 41 VI. Conclusions “How much of a problem is patient safety? The unsettling fact is that no one knows.”185 Dr. Lucian Leape ________________________________________________________________________ Despite the initiatives that have been put forward since the IOM report in 1999, medical errors have gone from the 8th to the 3rd leading cause of preventable death in a nation that has the most expensive health care system in the world. In a recent study, the cost of avoidable medical errors in 2008 was estimated at $19.5 billion including 6.3 million medical injuries, relating 1.5 million to medical errors.186 TJC accredits close to 90% of hospitals nationally. When reviewing the current statistics on preventable medical errors, it is clear that correlation between TJC accreditation and improved patient safety outcomes is not strong. TJC must evaluate its standards, initiatives and survey process to rise to their vision statement that all people always experience the safest, highest quality, best-value health care across all settings. More importantly, however, for the nation’s patients, accreditation and safety efforts must be taken seriously at the federal level. Congress should take heed at the increasingly difficulty and intractable problem represented by preventable medical errors. The status quo of allowing a single accreditor to dominate the field that was also that same accreditor that allowed the current patient safety situation to occur should raise 185 See supra note 128 at 2 Cheryl Clark, HealthLeaders Media, Top 10 Most Costly, Frequent Medical Errors, (August 11, 2010) 1, 1-4, available at http://www.healthleadersmedia.com/page-1/PHY-254873/Top-10-Most-CostlyFrequent-Medical-Errors (last visited Feb. 14, 2011) 186 42 policymaker attention to other entities and methods that should be considered for patient safety. It is a truism that continuous improvement requires continuous effort. However, a corollary is that continuous improvement also requires dynamic feedback of accurate data and best practices. The emergence of innovative systems and approaches such as HFAP, DNV, and others should be brought forward by CMS and others to showcase advantages and preferences for accreditation and safety purposes. Only by this comparative approach can transparency in strategies, approaches, conflicts of interest, and other issues that impact safety can be addressed, and entities can make informed choices as to the most appropriate systems of meeting CoPs. The challenges for patient safety remain. TJC has been criticized in the past for its limited effectiveness in being the nation’s guardian of safety. It has continued its limited impact after these reports. It is time to move beyond TJC efforts and assess, plan, integrate, and provide continuously feedback using other systems in a coordinated, dynamic manner so as to improve safety. The lessons of history should not elude us; a new system of safety review must be put into place so that the next generation of patients will not have to address these same safety concerns that have plagued the health delivery system for more than half a century. 43 VII. Bibliography 1. The Free Dictionary by Farflex, Medical Dictionary, deemed status, http://medical-dictionary.thefreedictionary.com/deemed+status (last visited Feb. 18, 2011) 2. Centers for Medicare and Medicaid Services, Conditions for Coverage (CfCs) & Conditions of Participations (CoPs), available at https://www.cms.gov/CFCsAndCoPs/01_Overview.asp (last visited Oct. 25, 2010) 3. The Joint Commission, http://www.jointcommission.org (last visited Oct. 30, 2010) 4. Institute of Medicine, About the IOM, http://www.iom.edu/About-IOM.aspx (last visited Feb. 18, 2011) 5. Consumers Union, U.S. Health Care System Fails to Protect Patients From Deadly Medical Errors, (May 19, 2009), available at http://www.consumersunion.org/pub/2009/05/011324print.html 6. About.com, Women’s History, Selected Florence Nightingale Quotations, available at http://womenshistory.about.com/cs/quotes/a/qu_nightingale.htm (last visited Jan. 30, 2011) 7. To Err Is Human: Building a Safer Health System, Linda T. Kohn, Janet Corrigan, Molla S. Donaldson, eds., National Academy Press, 1-273, (2000) 8. Milliman, The Economic Measurement of Medical Errors, Sponsored by Society of Actuaries’ Health System, (June 2010), 5, available at http://www.soa.org/files/pdf/research-econ-measurement.pdf (last visited Feb. 18, 2011) 9. Karen Davis, Cathy Schoen and Kristoff Stremikis, Mirror, Mirror on the Wall How the Performance of the US. Health Care System Compares Internationally 2010 Update, Executive Summary, Commonwealth Fund, (June 2010) available at http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2010/Jun/140 0_Davis_Mirror_Mirror_on_the_wall_2010.pdf 44 10. UC San Diego Health System, What Are Core Measures?, available at http://www-ucsdhealthcare.ucsd.edu/clinical/pdf/pips/what%20are%core%20measures.pdf (last visited 1/16/2011) 11. Mark Chassin, Jerod Loeb, Stephen Schmaltz, Robert Wachter , Accountability Measures – Using Measurement to Promote Quality Improvement, 363(7), N Engl J Med, 683,683-688, (Aug. 12, 2010), available at http://www.nejm.org/doi/pdf/10.1056/NEJMsb1002320?ssource=hcrc (last visited Jan. 17, 2011) 12. abc NEWS, Surgical Errors Continue Despite New Safety Guideline, New Study Finds Doctors Continue to Make Major Surgical Mistakes, available at http://abcnews.go.com/Health/Wellness/study-finds-medical-mishaps-universal-protocolera/story?id=11910796 (last visited Jan. 17, 2011) 13. Joint Commission Center for Transforming Healthcare Newsroom, Creating Solutions for High Reliability Health Care, Joint Commission Center for Transforming Healthcare Takes Aim at Patient Safety Failures, (September 10, 2009), available at http://www.centerfortransforminghealthcare.org/news/display.aspx?newsid=6 14. Philip F. Sahel et al., Wrong-Site and Wrong-Patient Procedures in the Universal Protocol Era, Analysis of a Prospective Database of Physician Self-reported Occurrences, Arch Surg, Vol 145 No. 10, (Oct. 2010), 978, 978-984, available at http://www.cascacolorado.com/wpcontent/uploads/2010/10/Never-event-self-reporting-in-CO-AMA-article-Oct-10.pdf (last visited Feb. 19, 2011) 15. Institute for Healthcare Improvement, http://www.ihi.org/IHI/About/VisionValues/ (last visited Oct. 25, 2010) 16. Andrew D. Hackbarth et al, Interpreting the “Lives Saved” results of IHI’s 100,000 Lives Campaign, Joint Commission Benchmark, September/October 2006, Volume 8, Issue 5, 1, 1-11, available at http://www.ihi.org/NR/rdonlyres/A3552730-6841-4269-A783BF73E125401E/0/JointCommisionBenchmarkSeptOct06.pdf 45 17. Michael Edmond and Theodore C. Eickhoff, Who is Steering the Ship? External Influences on Infection Control Programs, CID 46, Healthcare Epidemiology, 1748, 1746-1750, (June 1, 2008), available at http://cid.oxfordjournals.org/content/46/11/1746.full.pdf+html (last visited Feb. 26, 2011) 18. The National Quality Forum, http://www.qualityforum.org/About_NQF/About_NQF.aspx (last visited Oct. 25, 2010) 19. Agency for Healthcare Research and Quality, AHRQ Patient Safety Network – Patient Safety Primers, Never Events, available at http://psnet.ahrq.gov/primer.aspx?primerID=3 (last visited Feb. 10, 2011) 20. U.S Department of Health & Human Services, Healthcare-Associated Infections, 1, 1-2, available at http://www.hhs.gov/ash/initiatives/hai/index.html (last visited Feb. 11, 2011) 21. Allyson Lipitz-Snyderman et al, Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis, 2011:342:d219 doi:10.1136, bmj, 1, 1-7, available at http://www.bmj.com/content/342/bmj.d219.full.pdf 22. AHRQ Medical Errors & Patient Safety Update, Landmark Initiative to Reduce HealthcareAssociated Infections Cuts Deaths Among Medicare Patients in Michigan Intensive Care Units, (February 1, 2011) available at http://www.ahrq.gov/news/press/pr2011/haimiicupr.htm 23. Centers for Disease Control and Prevention, Healthcare-associated Infections, HAIs, The Burden, available at http://www.cdc.gov/HAI/burden.htmlt (last visited Feb. 26, 2011) 24. Brainy Quote, Accidents Quotes, http://www.brainyquote.com/quotes/keywords/accidents.html (last visited Feb. 11, 2011) 25. D Neuhauser, Heroes and Martyrs of Quality and Safety, Ernest Amory Codman MD, 11, Qual Saf Health Care 104, 104-105, (2002) available at http://qshc.bmj.com/content/11/1/104.full.pdf 26. Centers for Medicare & Medicaid Services, Conditions for Coverage (CfCs) & Conditions of Participations (CoPs), Overview, http://www.cms.gov/CFCsAndCoPs/ (last visited Nov. 12, 2010) 46 27. Juliet Battard Menendez, The Impetus for Legislation Revoking the Joint Commission’s Deemed Status as a Medicare Accrediting Agency, 12(3), JONAS Healthc Law Ethic Regul., 69, 70, (Jul-Sep 2010), available at http://www.nursingcenter.com/prodev/ce_article.asp?tid=1062299 28. James S. Roberts et al, A History of the Joint Commission on Accreditation of Hospitals, 258(7), JAMA 938, 936-952, (Aug 21, 1987), downloaded from www.jama.com at University of California San Diego (last visited Nov. 11, 2010) 29. OIG No. OEI-01-97-00050, The External Review of Hospital Quality, A Call for Greater Accountability, (July 1999), 2, 1-7, available at http://oig.hhs.gov/oei/reports/oei-01-97-00050.pdf 30. GAO-04-850, CMS Needs Additional Authority to Adequately Oversee Patient Safety in Hospitals, (July 2004), available at http://www.gao.gov/new.items/d04850.pdf 31. Fierce Healthcare, Daily News for Healthcare Executives, CMS approves Joint Commission’s hospital deeming authority, (Dec 3 2009), available at http://www.fiercehealthcare.com/story/cms-extends-relationship-joint-commission/2009-12-03 32. Diane Meldi et al, The Big Three: A Side by Side Matrix Comparing Hospital Accrediting Agencies, NAMSS Industry & Government Relations Committee, Synergy, 12, 12-14 (January/February 2009), available at http://www.hfap.org/mediacenter/NAMSS%20Synergy%20JanFeb09_Accreditation%20Grid.pdf 33. Patricia Kienle, Speaking of Accreditation Options, PPP Mag, Vol.7 No. 12, 2, (December 2010), available at http://www.pppmag.com/article/801/December_2010/Speaking_of_Accreditation_Options/ 34. Joint Commission Resources, Products and Services, available at http://www.jcrinc.com/Products-and-Services/ (last visited Feb. 27, 2011) 35. DNV Managing Risks, DNV Accreditation Program Frequently Asked Questions, 2, 1-9, available at http://dnvaccreditation.com/pr/dnv/document/FAQ.pdf (last visited Jan. 22, 2011) 47 36. GAO-07-79, Hospital Accreditation, Joint Commission on Accreditation of Healthcare Organizations’ Relationship with Its Affiliate, 2, 1-37, (December 2006), available at http://www.gao.gov/new.items/d0779.pdf (last visited Feb. 28, 2011) 37. “Quote DB”, http://www.quotedb.com/quotes/1468 (last visited Feb. 13, 2011) 38. Healthcare Facilities Accreditation Program, Overview, available at http://www.hfap.org/about/overview.aspx (last visited Jan. 22, 2011) 39. 42 CFR § 488, Medicare and Medicaid Programs; Application of the American Osteopathic Association for Continued Deeming Authority for Hospital, (2009) available at http://www.hfap.org/pdf/CMSFederalReg2009.pdf 40. David Gourley, Competitor to Joint Commission approved by CMS, Accreditation News, Journal for Respiratory Care & Sleep Medicine, 1, 1-3, (July 1, 2009), available at http://www.thefreelibrary.com/_/print/PrintArticle.aspx?id=207360830 41. DNV Annual Report, We’ve waited 40 years for a new choice. If you’re still waiting, it’s your patience that is winning, not your patients, available at http://www.ebookdnv.com/hcannualreport/ (last visited Feb. 13, 2011 42. James M. Levett, Implementing and ISO 9001 Quality Management System in a MultiSpecialty Clinic, Nov., Dec. 2005, 1, 1-5, available at http://dnvaccreditation.com/pr/dnv/document/dr._levett_tcm4-321304.pdf (last visited Feb. 14, 2011) 34. Consumers Union, Safe Patient Project, To Err is Human – To Delay is Deadly Ten Years Later, a million lives lost, billions of dollars wasted, (May 2009), 1, 1-13, available at http://www.safepatientproject.org/2009/05/to_err_is_humanto_delay_is_dea.html 35. Eric Nalder, Cathleen F. Crowley, Dead by Mistake, Health care bills sidestep medical errors issue, Hearst Newspapers, (Oct. 1, 2009), 1, 1-2, available at http://www.chron.com/disp/story.mpl/deadbymistake/6669310.html 36. Robert M. Wachter, Understanding Patient Safety, McGraw Hill Medical,2008, 222, 3-298 48 37. American Society of Medication Safety Officers, admin’s blog, TJC: Medication reconciliation National Patient Safety Goal to be reviewed, refined, (February 6, 2009), available at http://www.asmso.org/node/19 (last visited Feb. 21, 2011) 38. Bryan A. Liang & Kristopher Storti, Creating Problems as Part of the “Solution”: The JCAHO Sentinel Event Policy, Leal Issues, and Patient Safety, 33(2), J Health Law, 263, (Spring 2000) 39. Cheryl Clark, HealthLeaders Media, Top 10 Most Costly, Frequent Medical Errors, (August 11, 2010) 1, 1-4, available at http://www.healthleadersmedia.com/page-1/PHY-254873/Top-10Most-Costly-Frequent-Medical-Errors (last visited Feb. 14, 2011) 49 VIII. Vita Elaine Kenniston attended Chula Vista High School in Chula Vista, CA. In 1995, she entered San Diego State University in San Diego, CA. She received her Bachelor of Science in Nursing in 1997. Since that time, Elaine has worked for the University of California San Diego Medical Center as a Registered Nurse. Her duties included Clinical Nurse III, Quality Resource Manager and currently the BMT Administrative Nurse Manager for the Blood & Marrow Transplant Program. She has held her Oncology Nursing Certification since 1999. In 2007, she entered the Master of Advanced Studies in Health Law program from the University of California, San Diego and California Western School of Law. Permanent Address: 24365 Saddlebag Ct., Murrieta, CA 92562 This ISP was typed by the author. 50
© Copyright 2026