Afferent Dysgraphia after Right Cerebral Stroke: An
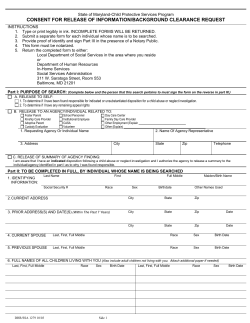
Brain and Cognition 44, 629–644 (2000) doi:10.1006/brcg.2000.1239, available online at http://www.idealibrary.com on Afferent Dysgraphia after Right Cerebral Stroke: An Autonomous Syndrome? Roberto Cubelli,* Antonella Guiducci,* and Patrizia Consolmagno† *Dipartimento di Psicologia dello Sviluppo e della Socializzazione, Universita` di Padova, Padua, Italy; and †Casa di Cura Sol et Salus, Torre Pedrera, Rimini, Italy Published online November 9, 2000 Afferent dysgraphia is an acquired writing deficit characterized by deletions and duplications of letters and strokes. The commonly accepted interpretation states that afferent dysgraphia is associated with three main clinical features: production of spatial writing errors; the presence of left unilateral neglect; and no deterioration in performance when writing blindfolded. In order to test whether these symptoms necessarily co-occur with afferent dysgraphia, we studied the writing performances of a series of eight right brain-damaged patients. In sentence copying, spontaneous handwriting, and writing to dictation they showed afferent dysgraphia. However, signs of left neglect and spatial dysgraphia were evident only in some cases. Furthermore, the frequency of afferent errors increased when patients were required to write without vision. The present study demonstrates that afferent dysgraphia is an autonomous clinical entity and that it results from a selective impairment of a mechanism whose function is that of comparing the information about the number of letters and strokes specified at the level of letter motor programs and the actual number of movements already realized. 2000 Academic Press Key Words: afferent dysgraphia; left spatial neglect; brain damage; right hemisphere; spatial disorders. INTRODUCTION Afferent dysgraphia is an acquired deficit of handwriting characterized by omissions and duplications of strokes and letters (Lebrun, 1976). When writing in cursive, patients may add a fourth downstroke to the letter m or omit the second downstroke of the letter n (Lebrun & Rubio, 1972; Cubelli & Lupi, 1999); when writing in uppercase print, they may produce the letter E with four horizontal lines or the letter B with only one arch (Ellis, This study was supported by NIH Grant NS 34073 to Alfonso Caramazza. Address correspondence to Roberto Cubelli, Dipartimento di Psicologia dello Sviluppo e della Socializzazione, Universita` di Padova, Via Venezia, 8, 35131 Padova, Italy. Fax: (49) 8276511. E-mail: [email protected] 629 0278-2626/00 $35.00 Copyright 2000 by Academic Press All rights of reproduction in any form reserved. 630 CUBELLI, GUIDUCCI, AND CONSOLMAGNO Young, & Flude, 1987). Further, they may write ‘‘ladder’’ with three d’s or hammer with only one m (Ellis et al., 1987). Afferent dysgraphic errors occur mainly in writing sequences of duplicated letters or letters with repeated strokes (Hecaen & Marcie, 1974; Margolin, 1984). Most stroke errors involve the letters m, n, w, and u (Cubelli & Lupi, 1999). Cursive handwriting is usually more impaired than writing in uppercase print (Ellis et al., 1987; Lebrun, 1985; but see Silveri, 1996). Direct copying is as affected as spontaneous writing (Lebrun, 1985). Afferent dysgraphia is a ‘‘peripheral’’ form of writing impairment (Ellis, 1988). The term ‘‘peripheral’’ is a cognitive metaphor and indicates a disorder of a processing mechanism which follows the computation of the abstract graphemic description of words. Indeed, current cognitive models of spelling and writing distinguish between ‘‘central’’ and ‘‘peripheral’’ processes (Margolin, 1984; Shallice, 1988). While the former compute the orthographic representation corresponding to the semantic or phonological content of a linguistic input (either by retrieving the stored lexical information or by applying the phoneme-to-grapheme conversion procedures), the latter translate the abstract orthographic forms into the motor commands necessary for the actual realization of the response (handwriting, typing, or oral spelling). Consequently, depending on the locus of the cognitive impairment, ‘‘central’’ and ‘‘peripheral’’ dysgraphias may occur following an acquired brain damage (Shallice, 1988; Shallice & Warrington, 1980). Impairment at the level of central processes produces a spelling disorder in all the output modalities but involves mainly one class of words (e.g., irregular or novel); on the contrary, impairment at the peripheral level causes a deficit in only one modality but affects all kinds of stimuli to the same extent. Among ‘‘peripheral’’ dysgraphias, the disorders of handwriting are the most studied (Ellis, 1988): patients show a selective impairment of writing coupled with a preserved ability to spell orally, to type on a keyboard, or to assemble preformed letters. Depending on the affected level of the handwriting process, three classes of impairment may be observed (Margolin & Goodman-Schulman, 1992). The first reflects a disorder in the selection of the appropriate allographic form of the letters according to case and style (Patterson & Wing, 1989; De Bastiani & Barry, 1989). The second comprises deficits in accessing the stored graphic motor programs which specify direction, relative size, position, and appropriate strokes needed to form each letter (Valenstein & Heilman, 1979). The third consists of a defective control of the actual motor execution for some specific details, such as force regulation (Margolin & Wing, 1983) or direction of writing (Chan & Ross, 1988). Copying performance is spared if the impairment occurs prior to selecting the letter motor programs, while it is impaired if the deficit occurs later (Zettin, Cubelli, Perino, & Rago, 1995). In afferent dysgraphia the underlying disorder is located at the last level and reflects the impairment of a control mechanism which processes incom- AFFERENT DYSGRAPHIA 631 ing information to keep track of position in stroke and letter sequences (Margolin, 1984; Cubelli & Lupi, 1999). In the course of handwriting, this mechanism has to ‘‘know’’ the identity and the number of graphic elements which have already been realized. Any failures in this updating operation will result in duplication or omission errors: for example, if in writing the letter m the first arch is interpreted as the second, the letter n will result; on the contrary, if the second arch is interpreted as the first, an m with four arches will be produced (Ellis et al., 1987). Even if central and peripheral dysgraphias usually follow lesions located in the posterior regions of the left (dominant) hemisphere (Bub & Chertkow, 1988), afferent dysgraphia follows focal lesions located in the right parietal lobe (Assal & Zander, 1969; Hecaen & Marcie, 1974).1 Since afferent dysgraphia may appear in the context of visuospatial disorders, Lebrun (1976, 1985) conceived this deficit as a part of a more general ‘‘spatial dysgraphia’’ (Hecaen, Angelergues, & Douzenis, 1963; McCarthy & Warrington, 1990; Margolin & Goodman-Schulman, 1992; Ardila & Rosselli, 1993). Besides deletion and duplication errors, four main features define ‘‘spatial dysgraphia’’ (Ardila & Rosselli, 1993; Hecaen & Marcie, 1974; Lebrun, 1985): (i) overwriting: words are written one over the other; (ii) word splitting (gap errors): patients leave a space between normally attached letters, thus leading to the fragmentation of the words into small segments; (iii) sloping lines: patients fail to write horizontally and produce oblique or wavy lines; (iv) ‘‘right-page’’ preference: writing is crowded onto the right side of the page leaving an excessively wide ‘‘margin’’ on the left side. The latter symptom reflects the presence of left spatial neglect (Ardila & Rosselli, 1993), another cognitive deficit usually caused by right parietal lesions (Robertson & Marshall, 1993). A closed association between left neglect and afferent dysgraphia has recently been pointed out: Hillis and Caramazza (1995), for example, suggested that omissions and repetitions of strokes and letters are one manifestation of the neglect syndrome. The term ‘‘afferent dysgraphia’’ was first introduced by Lebrun (1976). He observed that the errors produced by dysgraphic patients were similar to those made by normal subjects when requested to write with their eyes closed or with delayed visual feedback (van Bergeijk & David, 1959; Kalmus, Fry, & Denes, 1960; Smith, McCrary, & Smith, 1960; Tamada, 1995). However, unlike normals, dysgraphic patients appeared not to be more defective when vision was prevented. Lebrun (1976) assumed that even under standard 1 Afferent dysgraphia may also be observed in Alzheimer’s disease (De Vriees, Neri, Motta, Toschi, & Vecchi, 1988; Neils-Strunjas, Shuren, Roeltgen, & Brown, 1998); in this case, perseverations are the most frequent errors, while deletions rarely occur. The underlying deficit seems to be attentional in nature. Such errors are also made by normal controls while performing a simultaneous articulatory task (Smyth & Silvers, 1987). 632 CUBELLI, GUIDUCCI, AND CONSOLMAGNO conditions they behaved as if visual feedback was not available for handwriting. Therefore he proposed the term ‘‘afferent dysgraphia’’ to refer to a disturbance of afferent information in monitoring writing movements. In sum, the common widely accepted notion of afferent dysgraphia implies three main characteristics: 1. Spatial dysgraphic errors, such as letter overlapping, word splitting, and line wandering, are always associated with afferenttype errors. In most papers (e.g., Seki, Ishiai, Koyama, Sato, Hirabayashi, Inaki, & Nakayama, 1998) and textbooks (e.g., Margolin, 1992), the terms ‘‘spatial dysgraphia’’ and ‘‘afferent dysgraphia’’ are considered equivalent and interchangeable; 2. evidence of left spatial unilateral neglect is always present in patients with afferent dysgraphia (Ardila & Rosselli, 1993; Hecaen & Marcie, 1974); 3. no decrement of performance occurs when patients write with their eyes closed (Lebrun, 1976). However, such a description is not consistent with the clinical data one can glean from the literature. Ellis et al. (1987) described two patients with left neglect and spatial dysgraphia, but only one of them showed omissions and duplications of strokes and letters (i.e., afferent dysgraphia). Seki et al. (1998) studied the writing performances of a group of right brain-damaged patients and found no significant correlation between the presence of left neglect on screening tests (line bisection, line cancellation, and picture copying) and the occurrence of afferent dysgraphic errors in writing and copying kanji letters. In a fleeting comment they reported the existence of two cases showing a double dissociation. Recently, Cubelli and Lupi (1999) described a patient who presented a pure form of afferent dysgraphia with no evidence of left spatial neglect in a series of clinical tests.2 In spontaneous writing and in writing to dictation she produced frequent omissions and duplications of letters and strokes, but no spatial-type errors. In contrast with Lebrun’s (1976) hypothesis, her performance worsened when she wrote with her eyes closed. These findings seem to suggest that afferent dysgraphia is an autonomous clinical entity, that it is independent of spatial dysgraphia and left neglect, and that visual feedback is still available, even if not effective, to these patients. With the aim of ascertaining the independence of afferent dysgraphia, we examined the writing performance of a series of eight patients with acquired dysgraphia due to vascular lesions in the right cerebral hemisphere. Furthermore, to explore the role of visual afferent information we compared the performance of the patients and that of matched normal controls writing blindfolded versus their performance when writing with their eyes open. 2 A similar pattern of performance has been recently reported by Crosile and Hibert (1998); their patient, however, produced mostly badly-formed letters, suggesting a form of ‘‘apractic agraphia’’ (Roeltgen & Heilman, 1983) rather than an afferent dysgraphia. 633 AFFERENT DYSGRAPHIA TABLE 1 Demographic and Clinical Data of the Right Brain-Damaged Patients Patients BM GE BV NM MO SG MP AM Sex Age at testing Level of education (years) Lesion site Distance from onset (days) Male Female Male Male Female Male Male Male 33 65 71 65 67 55 64 16 17 5 10 10 5 5 8 10 FT FTP FP Tha FT FTP FPO FP 62 46 58 45 33 31 67 132 Note. F, frontal lobe; T, temporal lobe; P, parietal lobe; O, occipital lobe; Tha, thalamus. METHOD Participants The following criteria were set for entering the patients in the study: they should be righthanders, younger than 80, with at least 3 years of full-time education, affected by a focal CTdemonstrated vascular lesion limited to the right hemisphere, not affected by other neurological or psychiatric diseases or alcoholism, take any drug which could potentially interfere with the testing results, and perform above the age- and education-adjusted cutoff score on the Mini Mental State Examination (Folstein, Folstein, & McHugh, 1975). A continuous series of 27 patients affected by clinical signs indicative of a right hemisphere stroke, admitted to the Rehabilitation Centre of the Clinic ‘‘Sol et Salus’’ of Torre Pedrera (Rimini) between May and November 1997, were considered for the study. Five patients were excluded because they performed poorly on the Mini Mental State Examination; 1 had attentional problems too severe to allow reliable testing; 3 showed disorders of language and speech; finally, 2 were illiterates. Of the remaining 16 patients, 8 (50%) showed difficulties in the writing subtest of the Mini Mental State Examination and entered the present study. Their individual demographic and clinical data are reported in Table 1. A control group of 17 men and 5 women participated in the experimental investigation. For each individual patient, two or three controls, matched for age, sex, and education, were selected. The mean age of the normal participants was 49.9 (SD 18.3, range 16–70), their mean education was 8.8 years (SD 4, range 5–17). Neuropsychological Investigation Unilateral spatial neglect. A series of standardized tests assessing the presence of left spatial neglect was administered. The clinical battery comprised four tasks: Line cancellation (Albert, 1973), Bells’ Test (Gauthier, Dehaut, & Joanette, 1989), Copying of Geometrical Figures (Arrigoni & De Renzi, 1964), and Drawing Familiar Objects (daisy, clock, house) from memory. Moreover, the patients were asked to read aloud 40 words of different lengths (from 4 to 11 letters) and 20 numbers (from 3 to 6 digits). Finally, an index of position preference was computed (Colombo, De Renzi, & Faglioni, 1976) on the basis of the performance on Raven’s Coloured Progressive Matrices (Raven, 1965). 634 CUBELLI, GUIDUCCI, AND CONSOLMAGNO Handwriting. Writing performance was assessed under three different conditions: writing to dictation, direct copying, and spontaneous production. In the writing-to-dictation task, the patients were asked to write 40 concrete and high-frequency words (ranging from 4 to 11 letters in length) and six sentences (51 words in total) read aloud by the examiner. In the copying task, the patients were shown six printed sentences (44 words in all) on two occasions. On the first they had to copy the stimuli in cursive style and on the second in uppercase print. The spontaneous production was evaluated by asking patients to write a letter to a relative or a friend. Experimental Investigation The 8 patients and the 22 normal controls were asked to write 30 words in two different styles (cursive or uppercase print) in two different ‘‘vision’’ conditions (with eyes open or blindfolded). Experimental conditions were balanced across participants. The stimulus length ranged from 4 to 7 letters. The words were presented orally, and the participants were instructed to write at normal handwriting speed and if a mistake was made not to correct it. After completing all the writing tasks, the patients were asked to spell each stimulus orally. By definition, in afferent dysgraphics oral spelling should be normal or better preserved than handwriting. RESULTS Assessment of Neglect Table 2 reports the performance of the patients on the clinical battery for left spatial neglect. Three patients showed no evidence of neglect, while the remaining five failed at least one test. Only in one case (MO) was neglect so severe as to be evident in all tasks. The Bells’ Test appeared to be the TABLE 2 Performance of Patients in the Screening Tests (Neglect Scores in Bold) Patients BM GE BV NM MO SG MP AM a Line cancellation (omissions) a Bells’ Test (omissions) b Right Copying of shapes (neglect errors) c Drawing from memory (neglect errors) d Word and number reading (neglect errors) e Raven CPM (position preference) f Left Right Left 0 0 0 0 18 0 0 0 0 0 0 0 3 0 0 0 7 3 0 0 15 5 0 5 0 0 1 0 3 1 1 1 2 4 0 0 7 0 0 0 0 0 0 0 1 0 0 0 2 0 0 0 14 0 0 0 2 8 6 2 29 7 3 5 Range 0–18. Range 0–15. c Range 0–11; neglect score ⱖ 1. d Range 0–3; neglect score ⱖ 1. e Range 0–60; neglect score ⱖ 1. f Range 0–36; neglect score ⱖ 8. b 635 AFFERENT DYSGRAPHIA most sensitive task, thus supporting that asking the cancellation of targets among distracters is a powerful way to elicit left visuospatial neglect (Halligan, Marshall, & Wade, 1989). Assessment of Handwriting The patients made errors in all the tasks (Table 3). After the transformation in arcsign of the percentage of incorrectly written words, an analysis of variance was carried out. No significant effect of testing conditions was found [(F[4, 28) ⫽ 1.635; n.s.]. In the copying tasks, only MO omitted words placed at the beginning of the stimulus sentences. Left visuospatial neglect appeared to be unrelated to the occurrence of writing errors. Taking the number of tests failed as an index of neglect severity, no significant correlation between the degree of neglect and the percentage of words incorrectly written was found (Rho ⫽ .381; n.s.). For example, SG, who failed only the Bells’ Test, produced significantly more incorrect words (43%) than BM (18.9%), who failed three of the clinical tests for neglect [χ 2 (1) ⫽ 30.215; p ⬍ .001]. Furthermore, MP, who was normal in the neglect battery, had a percentage of wrong responses (20.62%) higher than that of GE (12.5%), who showed clear evidence of neglect in three tests of seven [χ 2 (1) ⫽ 5.321; p ⬍ .05]. These findings TABLE 3 Number (and Percentage) of Words Incorrectly Written in the Screening Battery for Handwriting Patients BM GE BV NM MO SG MP AM Total Dictation of words Dictation of sentences Copying in cursive Copying in print Writing of a letter 9/40 (22.5) 5/40 (12.5) 6/40 (15) 5/40 (12.5) 26/40 (65) 21/40 (52.5) 10/40 (25) 4/40 (10) 86/320 (26.9) 10/51 (19.6) 10/51 (19.6) 5/51 (9.8) 11/51 (21.6) 21/51 (41.2) 16/51 (31.4) 10/51 (19.6) 7/51 (13.7) 90/408 (22.1) 8/44 (18.2) 7/44 (15.9) 3/44 (6.8) 4/44 (9.1) 11/17 (64.7) 21/44 (47.7) 7/44 (15.9) 2/44 (4.5) 63/325 (19.4) 7/44 (15.9) 4/44 (9.1) 8/44 (18.2) 6/44 (13.6) 8/14 (57.1) 23/44 (52.3) 12/44 (27.3) 1/44 (2.3) 69/322 (21.4) 10/54 (18.5) 5/73 (6.8) 3/47 (6.4) 2/13 (15.4) 8/19 (42.1) 8/28 (28.6) 1/15 (6.7) 36/185 (19.5) 73/434 (16.8) Total 44/233 (18.9) 31/252 (12.3) 25/226 (11.1) 28/192 (14.6) 74/141 (52.6) 89/207 (43) 40/194 (20.6) 50/364 (13.7) 636 CUBELLI, GUIDUCCI, AND CONSOLMAGNO TABLE 4 Different Types of Errors Produced by the Right Brain-Damaged Patients Patients Errors BM GE BV NM MO SG MP AM Afferent-type (letters and strokes) Unnecessary gaps Overlapping letters Sloping words Left neglect 45 29 18 26 106 108 31 46 0 0 0 ⫹ 0 0 0 ⫹ 11 0 64 ⫺ 0 1 0 ⫺ 3 2 65 ⫹ 0 0 23 ⫹ 4 0 0 ⫺ 0 0 9 ⫹ Note. The signs ‘‘⫹’’ and ‘‘⫺’’ indicate the presence and the absence of left neglect. In the other cases the total number of errors is reported. Words were classified as misoriented independently of accuracy at letter level. conclusively point to afferent dysgraphia as a primary disorder of handwriting independent of the neglect syndrome. Table 4 reports the individual patterns of performance according to the five categories of errors which constitute the syndrome of ‘‘spatial dysgraphia’’ (Ardila & Rosselli, 1993; Hecaen & Marcie, 1974). Besides the afferenttype errors (involving the erroneous production of letters and strokes), four other incorrect responses were considered: overwriting (overlapped letters), sloping lines, word splitting, and neglect for the left half of the page. An overwriting error was produced when one letter was written over another one, even if only partially. An unnecessary gap within a word (word splitting error) was identified when the space between two adjacent letters was larger than 2 mm in cursive style and larger than 3 mm in uppercase print. The deviation from the horizontal in writing one individual word was defined as a sloping error when the absolute vertical shift from the beginning to the end was larger than 10 mm. Words were classified as misoriented independently of accuracy at letter level. The preference for the right half of the page was identified as a neglect-related error when the distance between the left margin of the paper and the first produced letter was larger than 30 mm. While the afferent-type errors were produced by all the patients, the other defective phenomena were found only in some cases. Given the different patterns of dissociation shown by the patients, each error category should be considered as an expression of different underlying cognitive deficits (for a discussion on this point, see Cubelli & Lupi, 1999). The lower frequency of overwriting and gap errors with respect to afferent-type errors can be explained by considering that while the latter may occur at stroke level and involve each individual letter, the former reflect a difficulty in maintaining the correct relative distance between adjacent letters within words. It is noteworthy that only the five patients showing neglect in at least one of the clinical tests used exclusively the right side of the paper in writing tasks. 637 AFFERENT DYSGRAPHIA The right-page preference, therefore, does not seem to be specific to afferent dysgraphia but rather a manifestation of a more general attitude of ignoring the contralateral space. Among the afferent-type errors, the most frequent responses were stroke repetitions (26%), stroke deletions (25%), letter repetitions (22%), letter deletions (14%), and letter substitutions (10%). The remaining errors (3%) comprised letter additions, letter exchanges, and stroke additions. It is worth noticing that many errors classified as occurring at the letter level were ambiguous. Indeed, a letter substitution error like pallone (ball) → pallome (nonword) could be interpreted as a stroke repetition, whereas a letter duplication error like ombrello (umbrella) → ommbrello (nonword) could be scored as a three-stroke repetition. Of the 104 errors classified as repetition of letters, 42 (40%) involved repeated letters (e.g., BICCHIERE (glass) → BICCCHIERE). In sum, most of the afferent-type errors consisted of the production of an incorrect number of letters and strokes. The analysis of the individual patterns of performance reveals a high level of variability. SG and BM made mainly repetitions (70 and 76%, respectively), while GE and AM produced mainly deletions (58 and 56%, respectively). MO, on the contrary, produced the same number of repetition and deletion errors (46 and 44%, respectively). Experimental Investigation Table 5 allows one to compare the patients’ performance in the oral spelling task to that of written spelling with eyes open. Obviously, the correct comparison is with writing errors at the letter level. SG, MP, and AM made no errors in the oral task, confirming the diagnosis of ‘‘peripheral’’ dysgraphia. MO made only one error in the oral spelling despite her severe writing disorder. On the contrary, NM was more impaired in the oral spelling TABLE 5 Total Number of Errors Made by the Patients in the Spelling Tasks Written spelling (letters) Patients BM GE NM MO SG MP AM Written spelling (strokes) Oral spelling Cursive Uppercase print Cursive Uppercase print 6 4 20 1 0 0 0 4 1 1 9 2 2 1 4 1 0 14 3 5 0 10 3 0 44 10 4 4 1 0 0 11 12 3 1 Note. Case BV was discharged before the administration of the oral spelling task. 638 CUBELLI, GUIDUCCI, AND CONSOLMAGNO FIG. 1. Total number of errors made by the patients and by the normal participants under the four experimental conditions. task than in the written spelling one. The discrepancy between the two performances allows to assume different underlying deficits. BM and GE made a similar number of errors in both tasks; however, a central dysgraphia is ruled out by the presence of errors at the stroke level, which reflect a postgraphemic disorder. Figure 1 shows the total number of errors made by the patients and by the matched normal controls in writing single words to dictation in cursive and uppercase print under the two experimental conditions. A significant effect of Group [F(1, 28) ⫽ 29.151; p ⬍ .001] was found: the patients were more impaired than the controls. Also the effect of Condition [F(1, 28) ⫽ 55.974; p ⬍ .001] was significant: the performances of both groups were more defective when writing blindfolded rather than with eyes open. The interaction Group X Condition was significant [F(1, 28) ⫽ 15.475; p ⬍ .001]: the brain-damaged patients were more greatly disrupted by the absence of visual feedback. Also the interaction Group X Condition X Style was significant [F(1, 28) ⫽ 8.373; p ⫽ .01]. 639 AFFERENT DYSGRAPHIA TABLE 6 Total Number of Afferent and Spatial (Word Splitting and Overwriting) Errors Made by the Patients in the Experimental Investigation Afferent errors Eyes open Patients Cursive BM GE BV NM MO SG MP AM 14 4 4 1 38 12 6 5 Spatial errors Blindfolded Eyes open Blindfolded Uppercase Uppercase Uppercase Uppercase print Cursive print Cursive print Cursive print 5 1 0 0 21 15 8 1 31 15 12 7 33 21 8 15 36 11 5 3 26 22 12 0 0 0 0 0 1 0 0 0 0 2 0 0 5 0 1 0 0 2 0 0 5 1 6 0 7 14 1 4 6 2 11 0 Table 6 reports the frequency of afferent and spatial writing errors under the four experimental conditions. The performance was significantly less accurate in the ‘‘no vision’’ condition [F(1, 7) ⫽ 8.217; p ⬍ .05]. Neither the effect of style [F(1, 7) ⫽ 4.2; n.s.), nor the interaction Condition X Style [F(1, 7) ⫽ .072; n.s.] was found. Some examples of errors made by the patients are given in Fig. 2. The letters most involved in errors were m, n, r, t, u, and v when writing in cursive3 (in both eyes open and blindfolded conditions) and the letters E, M, and N when writing in uppercase print (but only in the ‘‘no vision’’ condition).4 Word splitting and overwriting errors were made only by some patients. These errors were more frequent in the blindfolded condition [F(1, 7) ⫽ 9.134; p ⬍ .05] and, differently from the afferent-type ones, they involved mainly uppercase printed letters [F(1, 7) ⫽ 8.805; p ⬍ .05]. To write a word in cursive one single, continuous movement can be made without lifting the pen from the page, whereas to write in print each individual letter has to be formed separately. Visual control is crucial to maintain the space between the constituent letters constant, so as to avoid unnecessary gaps or overlapped letters. 3 The letters m, n, r, u, and v differ for the number of identical strokes. In writing the letter t, the patients tended to omit the horizontal bar. 4 In the stimulus words the different letters did not appear with the same frequency. Other multiple-stroke letters, such as F or H, could have been frequently involved in errors in both styles, but too few instances of these letters were present in the words to be written. A future study will be devoted to testing whether multiple-stroke letters are differentially affected by afferent dysgraphia. 640 CUBELLI, GUIDUCCI, AND CONSOLMAGNO FIG. 2. Examples of handwriting errors made by the patients in the experimental investigation. DISCUSSION In this paper we have studied the writing performances of a series of eight patients who showed a written production disorder following a right brain stroke. In sentence copying, spontaneous handwriting, and writing to dictation they produced frequent deletions and duplications of letters and strokes, fulfilling the criteria for ‘‘afferent dysgraphia’’ (Lebrun, 1976, 1985; Ellis et al., 1987). No difference among tasks was found, thus confirming a disorder at a functional level subsequent to that of the selection of letter motor programs. Most errors occurred at the stroke level and involved mainly letters differing for number of identical strokes. Some patients produced mostly deletion errors, while others produced mainly repetitions. This pattern variability suggests that letter and stroke errors cannot be attributed to a general tendency to perseverate (Ardila & Rosselli, 1993), but require a different and unitary explanation. Since most errors involved strokes within letters the defect should be located at the level of the actual realization of the correct AFFERENT DYSGRAPHIA 641 letter shape. The production of ill-formed letters is also a typical feature of apraxic dysgraphia (Zettin et al., 1995). However, differently from those observed in afferent dysgraphia, apraxic errors involve any letter and result in unrecognizable shapes. Venneri, Cubelli, and Caffarra (1994) reported a patient with Alzheimer’s disease who produced perseverative errors only in writing adiacent repeated letters: he produced farfallla (nonword) instead than farfalla (butterfly). Sequences containing nonrepeated letters were always well written. To explain these errors the functional impairment was located at the level of motor program selection, where orthographic information about double letters (Caramazza & Miceli, 1990) is still represented and acts as a motor command signaling the duplication of a given letter. In patients with attentional disorders this information could induce a selective perseverative behavior limited to the letters to be doubled. Even if afferent dysgraphia requires a different explanation, in this case the source of errors could also be related to the information represented at the level of the graphic–motor programs. Besides the number of individual letters for a given word [one or two to distinguish between words like rosa (rose) and rossa (red)], the number of the appropriate strokes for a given letter (two or three to distinguish between letters n and m) is also represented. This information about the number of units to be written (either letters or strokes) is necessary for the correct execution of the handwriting movements. Consequently, a constant comparison between the represented information specifying the motor programs and that coming from the actual movements is crucial for realizing the correct number of strokes and letters. We postulate the existence of a mechanism whose function is that of signaling the perfect match between the information about the number represented in long-term stored motor programs and the actual number of movements already realized. If that mechanism is not functioning, duplications as well as omissions of letters and strokes will follow. In normal subjects a simultaneous concurrent task can interfere with the activity of such a comparison mechanism (Ellis, 1982), whereas a lesion in the right parietal lobe can damage it, causing inability to monitor the handwriting movements under standard conditions also. Such a deficit should be more evident in writing words with duplicated letters or letters with multiple or repeated strokes. In particular, the frequency of errors should depend on the number of strokes in the individual letters: while letters requiring only a single movement, for example ‘‘e,’’ ‘‘o,’’ ‘‘l’’ in cursive style or ‘‘I,’’ ‘‘O,’’ and ‘‘C’’ in uppercase print, should be less vulnerable, letters with two or more separate strokes should be more frequently wrong. BV, NM, MP, and AM showed afferent dysgraphia but no left neglect, either in writing tasks or in other clinical tests. In copying they did not omit the initial words of sentences or the initial letters of words; in spontaneous writing they did not use only the right half of the paper. Further, they performed within the normal limits in a six-test battery for neglect. As predicted 642 CUBELLI, GUIDUCCI, AND CONSOLMAGNO by Ellis et al. (1987) and confirmed by Cubelli and Lupi (1999) and Seki et al. (1998), the production of duplications and omissions of letters and strokes may be observed independently of the presence of left neglect. Afferent dysgraphia also appears to be independent of spatial writing errors. BM and GE showed no evidence of overwriting, line sloping, or unnecessary gaps. Furthermore, afferent-type and spatial-type errors are differentially affected by the absence of vision: spatial errors were more frequent in writing in uppercase print than in writing in cursive; afferent errors, on the contrary, increased in both styles. In our opinion, afferent dysgraphia and spatial dysgraphia are not different verbal labels for the same clinical syndrome; on the contrary, they refer to different writing errors which reflect independent underlying deficits. Spatial dysgraphia, which is characterized by the production of wandering lines, overlapping letters, and word splitting, reflects a difficulty in elaborating the spatial relationships among letters within words: they can be well formed but they are realized misaligned, one over the other, or too distant. Afferent dysgraphia, instead, is characterized by the production of an incorrect number of repeated strokes for a given letter or identical letters for a given word; it is a disorder in monitoring the actual handwriting movements in order to compare what is written with the abstract representation of letters and words. Hereafter, afferent dysgraphia and spatial dysgraphia should be considered clinical manifestations of different handwriting disorders. In sum, following a right cerebral lesion three different classes of writing disorders can be observed (for a discussion, see Cubelli & Lupi, 1999): (i) neglect-related writing deficits; (ii) spatial errors; (iii) afferent-type errors. In the present study patients’ writing performances worsened when they wrote without vision. This finding rules out the possibility that for patients with afferent dysgraphia visual information is not available (Lebrun, 1976). In our opinion, the deficit in afferent dysgraphia does not derive from a reduced afferentation, but from the impairment of a specific mechanism, fed by visual information, whose role is that of comparing feedback information with information specified in the letter motor programs. In the Introduction we reported that the main features commonly assumed to be closely associated with afferent dysgraphia are three: the production of spatial writing errors; the presence of left unilateral neglect; and no deterioration in performance when writing without vision. The present study has demonstrated that afferent dysgraphia is an autonomous clinical entity and that none of these three features has been confirmed as a necessary manifestation of afferent dysgraphia. REFERENCES Albert, M. L. (1973). A simple test of visual neglect. Neurology, 23, 658–664. Ardila, A., & Rosselli, M. (1993). Spatial agraphia. Brain and Cognition, 22, 137–147. Assal, G., & Zander, E. (1969). Rappel de la symptomatology neuropsychologique des lesions AFFERENT DYSGRAPHIA 643 hemispheriques droites. Archives suisses de Neurologie, Neurochirurgie et de Psychiatrie, 105, 217–239. Arrigoni, C., & De Renzi, E. (1964). Constructional apraxia and hemispheric locus of lesion. Cortex, 1, 170–197. Bub, D., & Chertkow, H. (1988). Agraphia. In F. Boller and J. Grafman (Eds.), Handbook of neuropsychology, Vol. 1. New York: Elsevier. Caramazza, A., & Miceli, G. (1990). The structure of graphemic representations. Cognition, 37, 243–297. Chan, J. L., & Ross, E. D. (1988). Left-handed mirror writing following right anterior cerebral artery infarction: Evidence for nonmirror transformation of motor programs by right supplementary motor area. Neurology, 38, 59–63. Colombo, A., De Renzi, E., & Faglioni, P. (1976). The occurrence of visual neglect in patients with unilateral cerebral disease. Cortex, 12, 221–231. Croisile, B., & Hibert, O. (1998). Spatial or afferent agraphia without left-sided neglect. Aphasiology, 12, 147–159. Cubelli, R., & Lupi, G. (1999). Afferent dysgraphia and the role of vision in handwriting. Visual Cognition, 6, 113–128. De Bastiani, P., & Barry, C. (1989). A cognitive analysis of an acquired dysgraphic patient with an ‘‘allographic’’ writing disorder. Cognitive Neuropsychology, 6, 25–41. De Vriees, L. P., Neri, M., Motta, M., Toschi, A., & Vecchi, G. P. (1988). The right hemisphere syndrome and Alzheimer’s disease: A case report. In A. Agnoli, J. Cahn, N. Lassen, & R. Mayeux (Eds.), Senile dementias. Paris: J. Libbey Eurotext. Ellis, A. W. (1982). Spelling and writing (and reading and speaking). In A. W. Ellis (Ed.), Normality and pathology in cognitive functions. London: Academic Press. Ellis, A. W. (1988). Normal writing processes and peripheral acquired dysgraphias. Language and Cognitive Processes, 3, 99–127. Ellis, A. W., Young, A. W., & Flude, B. M. (1987). ‘‘Afferent dysgraphia’’ in a patient and in normal subjects. Cognitive Neuropsychology, 4, 465–486. Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatry Research, 12, 189–198. Gauthier, L., Dehaut, F., & Joanette, Y. (1989). The Bells’ Test: A quantitative and qualitative test for visual neglect. International Journal of Clinical Neuropsychology, 11, 49–54. Halligan, P. W., Marshall, J. C., & Wade, D. T. (1989). Visuospatial neglect: Underlying factors and test sensitivity. The Lancet, 25, 517–522. Hecaen, H., & Marcie, P. (1974). Disorders of written language following right hemisphere lesions: Spatial dysgraphia. In S. J. Dimond & J. G. Beamont (Eds.), Hemisphere function in the human brain. London: Elek. Hecaen, H., Angelergues, R., & Douzenis, J. A. (1963). Les agraphies. Neuropsychologia, 1, 179–208. Hillis, A. E., & Caramazza, A. (1995). A framework for interpreting distinct patterns of hemispatial neglect. Neurocase, 1, 189–207. Kalmus, H., Fry, D. B., & Denes, P. (1960). Effects of delayed visual control on writing, drawing and tracing. Language and Speech, 3, 96–108. Lebrun, Y. (1976). Neurolinguistic models of language and speech. In H. Whitaker & H. A. Whitaker (Eds.), Studies in neurolinguistics, Vol. 1. New York: Academic Press. Lebrun, Y. (1985). Disturbance of written language and associated abilities following damage to the right hemisphere. Applied Psycholinguistics, 6, 231–260. 644 CUBELLI, GUIDUCCI, AND CONSOLMAGNO Lebrun, Y., & Rubio, S. (1972). Reduplications et omissions graphiques chez des patients atteints d’une lesion hemispherique droite. Neuropsychologia, 10, 249–251. Margolin, D. I. (1984). The neuropsychology of writing and spelling: Semantic, phonological, motor, and perceptual processes. Quarterly Journal of Experimental Psychology, 36A, 459–489. Margolin, D. I. (1992). Cognitive neuropsychology in clinical practice. New York: Oxford Univ. Press. Margolin, D. I., & Wing, A. (1983). Agraphia and micrographia: Clinical manifestations of motor programming and performance disorders. Acta Psychologica, 54, 263–283. Margolin, D. I., & Goodman-Schulman, R. (1992). Oral and written spelling impairments. In D. I. Margolin (Ed.), Cognitive neuropsychology in clinical practice. New York: Oxford Univ. Press. McCarthy, R. A., & Warrington, E. K. (1990). Cognitive Neuropsychology. A clinical introduction. San Diego: Academic Press. Neils-Strunjas, J., Shuren, J., Roeltgen, D., & Brown, C. (1978). Perseverative writing errors in a patient with Alzheimer’s Disease. Brain and Language, 63, 303–320. Patterson, K. E., & Wing, A. M. (1989). Processes in handwriting: A case for case. Cognitive Neuropsychology, 6, 1–23. Raven, J. C. (1965). Guide to using the Coloured Progressive Matrices. London: Lewis. Robertson, I., & Marshall, J. C. (1993). Unilateral neglect: Clinical and experimental studies. Hove: Erlbaum. Roeltgen, D. P., & Heilman, K. M. (1983). Apractic agraphia in a patient with normal praxis. Brain and Language, 18, 35–46. Seki, K., Ishiai, S., Koyama, Y., Sato, S., Hirabayashi, H., Inaki, K., & Nakayama, T. (1998). Effects of unilateral spatial neglect on spatial agraphia of kana and kanji letters. Brain and Language, 63, 256–275. Shallice, T. (1988). From neuropsychology to mental structure. Cambridge: Cambridge Univ. Press. Shallice, T., & Warrington, E. K. (1980). Single and multiple component central dyslexic syndromes. In M. Coltheart, K. E. Patterson & J. C. Marshall (Eds.), Deep dyslexia. London: Routledge and Kegan Paul. Silveri, M. C. (1996). Peripheral aspects of writing can be differentially affected by sensorial and attentional defect: Evidence from a patient with afferent dysgraphia and case dissociation. Cortex, 32, 155–172. Smith, W., McCrary, J., & Smith, K. (1960). Delayed visual feedback and behavior. Science, 132, 1013–1014. Smyth, W. M., & Silvers, G. (1987). Functions of vision in the control of handwriting. Acta Psychologica, 65, 47–64. Tamada, T. (1995). Effects of delayed visual feedback on handwriting. Japanese Psychological Research, 37, 103–109. Valenstein, E., & Heilman, K. M. (1979). Apraxic agraphia with neglect-induced paragraphia. Archives of Neurology, 36, 506–508. Van Bergeijk, W. A., & David, E. E. (1959). Delayed handwriting. Perceptual and Motor Skills, 9, 347–357. Venneri, A., Cubelli, R., & Caffarra, P. (1994). Perseverative dysgraphia: A selective disorder in writing double letters. Neuropsychologia, 32, 923–931. Zettin, M., Cubelli, R., Perino, C., & Rago, R. (1995). Impairment of letter formation: The case of ‘ideomotor’ apraxic agraphia. Aphasiology, 9, 283–294.
© Copyright 2026