Chronic kidney disease and risk of incident myocardial
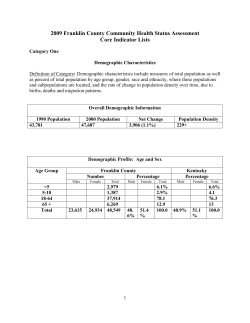
Clinical research European Heart Journal (2006) 27, 1245–1250 doi:10.1093/eurheartj/ehi880 Prevention and epidemiology Chronic kidney disease and risk of incident myocardial infarction and all-cause and cardiovascular disease mortality in middle-aged men and women from the general population Christa Meisinger1,2*, Angela Döring2, and Hannelore Löwel2 for the KORA Study Group 1 Central Hospital of Augsburg, MONICA/KORA Myocardial Infarction Registry, Stenglinstr. 2, D-86156 Augsburg, Germany; and 2 GSF National Research Center for Environment and Health, Institute of Epidemiology, Neuherberg, Germany Received 24 November 2005; revised 24 February 2006; accepted 23 March 2006; online publish-ahead-of-print 12 April 2006 Cohort study; Kidney function; Myocardial infarction; Mortality; Risk Aims Chronic kidney disease (CKD) was found to be an independent risk factor for all-cause mortality as well as adverse cardiovascular disease (CVD) events in high-risk populations. Findings from populationbased studies are scarce and inconsistent. We investigated the gender-specific association of CKD with all-cause mortality, cardiovascular mortality, and incident myocardial infarction (MI) in a populationbased cohort. Methods and results The study was based on 3860 men and 3674 women (aged 45–74 years) who participated in one of the three MONICA Augsburg surveys between 1984 and 1995. CKD was defined by an estimated glomerular filtration rate between 15 and 59 mL/min/1.73 m2. Hazard ratios (HRs) were estimated from Cox proportional hazard models. In this study, 890 total deaths, 400 CVD deaths, and 321 incident MIs occurred in men up to 31 December 2002; the corresponding numbers in women were 442, 187, and 102. In multivariable analyses, the HR for women with CKD compared to women with preserved renal function was significant for incident MI [HR 1.67; 95% confidence interval (CI) 1.07–2.61] and CVD mortality (HR 1.60; 95% CI 1.17–2.18). In men, CKD was also significantly associated with incident MI (HR 1.51; 95% CI 1.09–2.10) and CVD mortality (HR 1.48; 95% CI 1.15–1.92) after adjustment for common CVD risk factors. In contrast, men and women with CKD had no significant increased risk of all-cause mortality. Conclusion CKD was strongly associated with an increased risk of incident MI and CVD mortality independent from common cardiovascular risk factors in men and women from the general population. Chronic kidney disease (CKD) is a worldwide public health problem with an increasing incidence and prevalence.1 The increase in the number of persons with CKD is reflected in the rising number of people with end stage renal disease (ESRD) treated by dialysis or kidney transplantation.2 In the past, the incidence of ESRD reached about 135 new patients per million in Europe and 336 new patients per million in the USA.3 Furthermore, in several studies it was shown that a decreased level of kidney function is an independent risk factor for all-cause mortality as well as adverse cardiovascular disease (CVD) events, such as myocardial infarction (MI) and stroke.4–7 These findings were, in particular, based on studies conducted in high-risk populations, for example in patients with CVD or CVD risk factors.4–7 However, data from the general population on this issue are scarce and the findings are less consistent.8–12 In addition, very few population- * Corresponding author. Tel: þ 49 821 400 4373; fax: þ 49 821 400 2838. E-mail address: [email protected] based data are available in Europe.13 In the present study, we investigated the association between CKD and incident MI, CVD mortality, and all-cause mortality in persons aged 45–74 years from the general population. To answer the question whether CKD is likewise a risk factor for the different outcomes in both sexes, all analyses were performed separately for men and women. Methods The presented data were derived from the population based MONICA (monitoring trends and determinants on cardiovascular diseases) Augsburg (southern Germany) studies conducted between 1984 and 1995. The MONICA Augsburg project was part of the multinational WHO MONICA project and the design of the project has been described in detail elsewhere.14,15 Three independent crosssectional surveys were carried out in the city of Augsburg and the counties Augsburg and Aichach–Friedberg in 1984/85 (S1), 1989/90 (S2) and 1994/95 (S3) to estimate the prevalence and distribution of cardiovascular risk factors among men and women. Altogether 13 427 persons (6725 men, 6702 women, response 77%) aged & The European Society of Cardiology 2006. All rights reserved. For Permissions, please e-mail: [email protected] Downloaded from http://eurheartj.oxfordjournals.org/ by guest on June 9, 2014 KEYWORDS 1246 Data collection Baseline information on socio-demographic variables, smoking habits, physical activity level, medication use, and alcohol consumption were gathered by trained medical staff during a standardized interview. In addition, all the participants underwent an extensive standardized medical examination including the collection of a blood sample. All measurement procedures have been described elsewhere in detail.14 Body mass index (BMI) was calculated as weight in kilograms divided by height in square metres. Participants were classified as active during leisure time if they regularly participated in sports in summer and winter and if they were active for at least 1 h per week in either season. Actual hypertension was defined as blood pressure values 140/90 mmHg and/or use of anti-hypertensive medication given that the subjects were aware of being hypertensive. Dyslipidaemia was defined as the ratio of total cholesterol to high density cholesterol 5.0. History of CVD was defined as prevalent MI or prevalent stroke at baseline. Clinical chemical measurements A non-fasting venous blood sample was obtained from all study participants while sitting. Total serum cholesterol analyses were carried out using an enzymatic method (CHOD-PAP, Boehringer Mannheim, Germany). HDL cholesterol was also measured enzymatically after precipitation of the apoprotein B-containing lipoproteins with phosphotungstate/Mg2þ (Boehringer Mannheim, Germany). Serum creatinine was determined using an automated Jaffe method in S1 and S2 (Technicon, SMAC autoanalyzer; Tarrytown, NY) and using an enzymatic method in S3 (creatinine PAP, Boehringer Mannheim, Germany). The enzymatic method was calibrated according to the Jaffe method. Serum uric acid was measured by the uricase method in S1 and S2. In S3, serum uric acid was determined with an enzymatic colorimetric reaction (Uric Acid PAP, Boehringer Mannheim). Internal and external quality control was performed according to the WHO MONICA Manual.14,15 Assessment of renal function The abbreviated Modification of Diet in Renal Disease Study Group equation1 was used to calculate eGFR: eGFR (mL/min/1.73 m2) ¼ 186.3 (serum creatinine21.154) (age20.203) 0.742 (if female) 1.212 (if black), where serum creatinine is measured in mg/dL, and age in years. The study population was stratified into two groups by the level of kidney function, namely, eGFR of 15–59 mL/min/1.73 m2, and eGFR of 60 mL/min/1.73 m2. This cut-point was chosen as an eGFR of 15–59 mL/min/1.73 m2 represents a moderate to severe decrease of GFR defined by the NKF K/DOQI guidelines.16 Thus, the term CKD was used for an eGFR between 15 and 59 mL/min/1.73 m2 in the present study. Outcomes The endpoints used in this study were incidence of fatal or non-fatal MI including sudden cardiac death, mortality from any CVD, and allcause mortality. Mortality was ascertained by regularly checking the vital status of all sampled persons of the MONICA surveys through the population registries inside and outside the study area; this procedure guaranteed that the vital status of cohort members who had moved out of the study area could also be assessed. Death certificates were obtained from local health departments and coded for the underlying cause of death by a single trained person using the 9th revision of the International Classification of Diseases (ICD-9). MIs were identified through the population-based MONICA/KORA Augsburg coronary event registry for the 25 to 74-year-old study population and censored at the 75th year of age.17 This registry monitors the occurrence of all in- and out-of-hospital fatal and nonfatal MIs among the 25 to 74-year-old inhabitants of the study region.17 An MI was considered as incident if it was the first during follow-up in a person without a history of heart attack in the baseline survey. Up to 31 December 2000, the diagnosis of a major nonfatal MI was based on the MONICA algorithm taking into account symptoms, cardiac enzymes, and ECG changes.17 Since 1 January 2001 all patients with MI diagnosed according to ESC and ACC criteria were included.18,19 Coronary deaths were validated by death certificates, autopsy report, chart review, and information from the coroner or the last treating physician. Statistical analyses For analyses of MI, event times were computed as the time from baseline examination to the occurrence of the first event and for analyses of total and cardiovascular mortality, event times were calculated as times to death. For all-cause and CVD mortality (ICD-9: 390–459), subjects without events were censored at their last date of follow-up. For incidence estimates, that is non-fatal MIs and fatal coronary events, the follow-up times were censored for men and women at death or when they reached the age of 75 years after which the register-based monitoring of coronary events ceases. Means or proportions for baseline demographic and clinical characteristics were computed for men and women with and without CKD. The x 2 test was used to test the differences in prevalences. The t-test was used to compare means. The interquartile range (IQR) was defined as the interval from the 25%-quantile to the 75%-quantile. Hazard ratios (HRs) were computed for persons with a moderate to severe decrease of eGFR (15–59 mL/min/1.73 m2) as compared with persons with an eGFR of 60 mL/min/1.73 m2 in Cox proportional hazards models. The first model included eGFR and in addition age (continuous) and survey. The second model included all previous factors plus actual hypertension (yes/no), dyslipidaemia (yes/no), level of physical activity (active/inactive), smoking status (regular smoking, that is a subject who smoked at least one cigarette per day at baseline, yes/no), alcohol intake (men: 0, .0, and ,40 or 40 g/day; women: 0, .0, and ,20 or 20 g/day), BMI (continuous), and history of diabetes (yes/no and Downloaded from http://eurheartj.oxfordjournals.org/ by guest on June 9, 2014 25–74 years participated in at least one of the three cross-sectional studies. All persons who took part in more than one survey were included once only with data collected at the first visit. All subjects were prospectively followed within the framework of the Cooperative Health Research in the Region of Augsburg (KORA). The present study was restricted to 45–74 year old study participants (n ¼ 7823; 3993 men, 3830 women). Up to 31 December 2002, 890 men and 442 women in this age-range had died. None of the study participants were excluded from analysis due to insufficient follow-up. For the present analyses using mortality as outcome, we excluded all subjects with incomplete data on any of the included variable (n ¼ 285). Furthermore, we excluded four study participants with an estimated glomerular filtration rate (eGFR) ,15 mL/min/ 1.73 m2, because such a GFR is defined as kidney failure in the National Kidney Foundation (NKF) Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines.16 Finally, the prospective analyses comprised 3860 men and 3674 women aged 45–74 years at baseline for the outcomes of all-cause and CVD mortality. For the analyses using incident MI as outcome, we excluded 277 study participants with incomplete data on any of the included variables, four persons with an eGFR ,15 mL/min/1.73 m2, and 249 persons with a prevalent MI at baseline. Furthermore, for these analyses, 142 men and 120 women who moved outside the study area during follow-up were censored at the date of the move. Thus, these analyses comprised 3662 men and 3631 women aged 45–74 years at baseline. Written informed consent was obtained from each study participant and the study was approved by the local Ethics Committee. C. Meisinger et al. CKD and cardiovascular events 1247 unknown). For the mortality outcomes fully adjusted models 2 were also adjusted for history of CVD. The above analyses were repeated by including eGFR as a continuous variable. HRs were computed for an increase of 10 mL/min/ 1.73 m2 of eGFR. The assumption of proportionality of hazards was assessed by fitting models stratified by risk factor categories, then plotting the log (-log(survival)) curves to check parallelism. No severe deviations from parallelism were evident. The assumption of linearity was assessed graphically by studying the smoothed martingal residuals from the null model plotted against the covariate variables. Kaplan–Meier survival plots of eGFR groups in relation to the different outcomes were examined. Comparisons between survival curves were performed using Log Rank test. Results are presented as HRs and 95% confidence interval (CI). Significance tests were two tailed and P-values ,0.05 are stated as statistically significant. All analyses were performed using the Statistical Analysis System (Version 8.2, SAS Institute Inc., Cary, NC, USA). In Table 1, gender specific differences in the baseline characteristics between persons with and without CKD are given. Men and women with CKD were more likely to be older, to have dyslipidaemia, and a history of diabetes and CVD. They were more likely to be hypertensive, to be nonsmokers, and less likely to have a high daily alcohol intake. These men and women were also more likely to have a higher BMI, higher uric acid, and serum creatinine levels. During follow-up (median follow-up period 12.5 years; IQR: 7.8–13.1), 890 total deaths, 400 CVD deaths, and 321 incident MIs occurred in men; the corresponding numbers in women were 442, 187, and 102 (Table 2). Table 2 also describes the observed crude incidence rates for the different outcomes by categories of kidney function. Men and women with CKD had higher crude rates for allcause mortality, CVD mortality, and first ever MI compared with men and women without CKD. In all categories and Discussion The present large population-based study confirmed associations of reduced eGFR and increased risk of CVD mortality. The risk associated with CKD was apparent in men and women from the general population. In addition, this study showed a strong association between CKD and first ever coronary heart disease event in men and women without a history of MI independent of traditional Table 1 Baseline characteristics by gender and level of kidney function eGFR Group (mL/min/1.73 m2) Age (years) Education (,12 years, %) BMI (kg/m2) History of diabetes (%) History of CVD (%) Actual hypertension (%) Use of anti-hypertensive agents (%) Alcohol intake (%) 0 g/day 0.1–19.9 g/day (women), 0.1–39.9 g/day (men) 20 g/day (women), 40 g/day (men) Regular smoking (%) Physically active (%) Dyslipidaemia (%) Serum creatininea Serum uric acid eGFR a Geometric mean. Men (n ¼ 3860) Women (n ¼ 3674) 15–59 (n ¼ 480) 60 (n ¼ 3380) P-value 15–59 (n ¼ 753) 60 (n ¼ 2921) P-value 62.4 (8.2) 70.8 28.2 (3.5) 9.4 11.5 62.3 39.6 57.2 (7.9) 70.7 27.8 (3.5) 6.8 6.0 54.7 19.1 ,0.0001 0.9557 0.0269 0.0379 ,0.0001 0.0017 ,0.0001 61.5 (7.2) 88.2 28.4 (4.6) 6.9 4.1 55.5 35.2 56.6 (7.8) 88.5 27.6 (4.8) 5.5 1.8 46.5 21.2 ,0.0001 0.8087 0.0001 0.1340 0.0002 ,0.0001 ,0.0001 21.9 57.5 16.6 49.0 ,0.0001 52.7 33.9 47.8 35.0 20.6 15.8 33.5 54.6 1.5 (1.2) 6.4 (1.4) 52.4 (7.2) 34.4 24.8 37.3 48.1 1.0 (1.1) 5.7 (1.3) 80.9 (13.7) 13.4 8.5 30.0 32.5 1.1 (1.2) 5.0 (1.3) 51.9 (7.5) 17.2 12.9 30.4 24.3 0.8 (1.1) 4.1 (1.1) 77.6 (12.8) ,0.0001 0.1122 0.0079 ,0.0001 ,0.0001 ,0.0001 0.0144 0.0008 0.8509 ,0.0001 ,0.0001 ,0.0001 ,0.0001 Downloaded from http://eurheartj.oxfordjournals.org/ by guest on June 9, 2014 Results for all outcomes, the crude incidence rates were higher in men than in women. Kaplan–Meier survival analysis showed a greater probability of an incident MI, CVD mortality, and all-cause mortality in men and women with CKD (Figures 1–3). In Cox proportional hazards analyses the age- and survey-adjusted HRs were significantly increased for incident MI and CVD mortality in women with CKD compared with women with preserved renal function. In men, CKD was also significantly associated with incident MI and CVD mortality in age- and survey-adjusted analysis. After multivariable adjustment, the independent associations remained significant in both sexes (Table 3). In contrast, men and women with CKD had no significantly increased risk of all-cause mortality. When eGFR was included as a continuous variable in the Cox proportional hazard models, in men an increment of 10 mL/min/1.73 m2 of eGFR was associated with a significant decrease in the risk of an incident MI (HR 0.91; 95% CI 0.84–0.99), but not with a significant decrease in CVD mortality (HR 0.96; 95% CI 0.89–1.03) and all-cause mortality (HR 1.04; 95% CI 0.99–1.08) after multivariable adjustment. In women, an increase of 10 mL/min/1.73 m2 of eGFR was significantly associated with incident MI (HR 0.88; 95% CI 0.77–1.00) and CVD mortality (HR 0.85; 95% CI 0.78–0.94), but not with all-cause mortality (HR 0.97; 95% CI 0.91–1.04) in multivariable adjusted analyses. 1248 C. Meisinger et al. Table 2 Outcomes by level of kidney function eGFR (mL/min/1.73 m2) Men 15–59 Women 60 15–59 60 Incident MI Number of participants 441 3 221 737 2 894 Events 46 275 31 71 Person-years (PY) 3 141 32 703 6 438 30 975 Events/10 000 PY 146.5 84.1 48.2 22.9 All-cause mortality Number of participants 480 3 380 753 2 921 Events 144 746 128 314 Person-years (PY) 4 373 38 321 8 270 34 886 Events/10 000 PY 329.3 194.7 154.8 90.0 CVD mortality Number of participants 480 3 380 753 2 921 Events 83 317 72 115 Person-years (PY) 4 373 38 321 8 270 34 886 Events/10 000 PY 189.8 82.7 87.1 33.0 Figure 1 (A) Survival curves for incident MI by eGFR category. MONICA/ KORA Cohort Study, men aged 45–74 years at baseline. (B) Survival curves for incident MI by eGFR category. MONICA/KORA Cohort Study, women aged 45–74 years at baseline. cardiovascular risk factors. However, the present findings did not provide support for a significant relationship between CKD and all-cause mortality in both sexes. Prior studies including subjects at high risk for CVD consistently demonstrated an independent association between reduced level of kidney function and CVD events, as well as CVD mortality.7,20–22 However, previous community-based studies have shown discordant results.8–12 Because of the different methods of estimating GFR used in the hitherto existing studies direct comparisons between the investigations are difficult. Some studies used serum creatinine levels as a marker of renal function,8,9,23 other examinations were based on the Cockcroft–Gault equation.13 In accordance with some recent studies,10–12 in the present study the modification of Diet in Renal Disease (MDRD)Study equation for GFR was used, because it has been thoroughly validated in adults.1 The Framingham Heart Study9 showed that serum creatinine levels between 136 and 265 mmol/L for men and between 120 and 265 mmol/L for women were associated with all-cause mortality in men, but not in women. Furthermore, in multivariable analyses baseline kidney disease was not associated with incident CVD events or CVD mortality.9 Also, the National Health and Nutrition Examination Survey (NHANES) I follow-up study8 observed a significant association between moderate renal insufficiency, defined as a creatinine of 122 to 177 mmol/L in men and 104 to 146 mmol/L in women, and all-cause as well as CVD mortality in unadjusted analyses. However, after adjustment for traditional cardiovascular risk factors both associations lost significance. Therefore, the authors concluded that the relationship between moderate renal insufficiency and CVD, demonstrated in other epidemiologic studies, appears to be due to co-occurrence of renal insufficiency with traditional cardiovascular risk factors. In contrast to these studies, the British Regional Heart Study observed an association between serum creatinine and CVD mortality in middle-aged men with a baseline serum creatinine level of 130 mmol/L (HR 1.4, 95% CI 1.0–2.1) when compared with men with baseline serum creatinine values ,116 mmol/L.23 Muntner et al.11 investigated the association between MDRD-calculated GFR, and CHD and CVD mortality among NHANES II participants. Compared with subjects with a GFR 90 mL/min subjects with a baseline GFR ,70 mL/min had a significantly increased risk of Downloaded from http://eurheartj.oxfordjournals.org/ by guest on June 9, 2014 Figure 2 (A) Survival curves for CVD mortality by eGFR category. MONICA/ KORA Cohort Study, men aged 45–74 years at baseline. (B) Survival curves for CVD mortality by eGFR category. MONICA/KORA Cohort Study, women aged 45–74 years at baseline. CKD and cardiovascular events 1249 Table 3 HRs (95% CI) for outcomes in men and women with CKD Variable Incident MI (fatal and non-fatal) Men Women All-cause mortality Men Women CVD mortality Men Women Age- and survey-adjusted Multivariableadjusteda 1.50 (1.09–2.08) 1.75 (1.13–2.71) 1.51 (1.09–2.10) 1.67 (1.07–2.61) 1.17 (0.97–1.41) 1.16 (0.94–1.44) 1.17 (0.97–1.41) 1.12 (0.90–1.39) 1.55 (1.20–2.00) 1.74 (1.28–2.35) 1.48 (1.15–1.92) 1.60 (1.17–2.18) a Adjusted for age, survey, history of diabetes, regular smoking, BMI, alcohol intake, actual hypertension, physical activity, and dyslipidaemia; outcomes all-cause and CVD mortality: additional adjustment for history of CVD. both CHD mortality (HR 1.68, 95% CI 1.23–2.30) and CVD mortality (HR 1.68, 95% CI 1.33–2.13) in multivariable analysis. Moreover, the level of GFR was an independent risk factor for atherosclerotic cardiovascular disease (ASCVD) and de novo ASCVD in the Atherosclerosis Risk in Communities (ARIC) Study.12 The Hoorn Study showed that mild-to-moderate loss of renal function is strongly associated with an increased risk of cardiovascular mortality even after adjustment for traditional cardiovascular risk factors, markers of inflammation, and markers of endothelial dysfunction.13 Finally, recently a pooled analysis of four community-based longitudinal studies (ARIC, Cardiovascular Health Study, Framingham Heart Study, and Framingham Offspring Study) found that in adjusted analyses CKD was a risk factor for the composite outcome of all-cause mortality and CVD in the general population (HR 1.19; 95% CI 1.07–1.32). In contrast to the present study, that study was very large, and therefore it had sufficient power to investigate the effect of CKD on all outcomes in subjects without CVD at baseline.10 The present results are in line with the hypothesis that renal function itself is implicated in the association with cardiovascular disease. Because we did not observe a significant relationship between CKD and all-cause mortality it can be assumed that CKD is a specific independent predictor of cardiovascular events and not an unspecific marker of health status or unhealthy lifestyle. The reasons for the high cardiovascular risk in persons with CKD remain unknown.24 A possible explanation could be that a decrease in renal function may be associated with other non-traditional risk factors that were not taken into consideration in this study. Such factors include for example, changes in coagulation, lipids, endothelial Downloaded from http://eurheartj.oxfordjournals.org/ by guest on June 9, 2014 Figure 3 (A) Survival curves for all-cause mortality by eGFR category. MONICA/KORA Cohort Study, men aged 45–74 years at baseline. (B) Survival curves for all-cause mortality by eGFR category. MONICA/KORA Cohort Study, women aged 45–74 years at baseline. dysfunction, homocysteine and/or the presence of anemia, oxidative stress, and inflammation.24,25 On the other hand, CKD may be the result of both duration and severity of other causes of cardiovascular disease, such as hypertension. Thus, reduced kidney function may reflect residual confounding from CVD risk factors. Furthermore, it is thinkable that CKD may exacerbate the effect of CVD risk factors and may, therefore, promote the atherosclerotic process. The MONICA/KORA Augsburg Study has several limitations that need to be considered. Although we adjusted for a variety of confounders, confounding by unmeasured variables cannot be excluded. Particularly, no data on recently identified CVD risk factors, such as CRP and homocysteine, could be taken into consideration. Prior studies have shown that estimates of GFR depend critically upon the accuracy and precision of the creatinine measurement used in their calculation.26 In the present study, the definition of CKD was based on a single measurement of serum creatinine at baseline examination; thus, misclassification bias cannot entirely be ruled out. Because the study was limited to men and women of German nationality between 45 and 74 years of age, caution should be used in generalizing these results to other populations and other age-groups, respectively. The strengths of the MONICA/ KORA Augsburg Cohort Study are primarily its prospective design, the representativeness of the cohort, based on a random sample of the general population and the availability of data on lifestyle and multiple cardiovascular risk factors. In conclusion, the present study showed that CKD is strongly associated with an increased risk of incident MI and CVD mortality in men and women from the general population. The underlying mechanism behind this relationship is unclear but seems to be independent from common risk factors such as hypertension, diabetes, smoking, BMI, alcohol intake, physical activity, and dyslipidaemia. Thus, estimation of GFR in addition to the consideration of present conventional risk factors may be a valuable tool for individual cardiovascular risk assessment. Further studies are needed to investigate the pathophysiological mechanisms underlying this association. 1250 C. Meisinger et al. Acknowledgements The KORA research platform and the MONICA Augsburg studies were initiated and financed by the GSF—National Research Center for Environment and Health, which is funded by the German Federal Ministry of Education, Science, Research and Technology and by the State of Bavaria. Morbidity and Mortality follow-ups in 1997/ 98 and 2002/03 were in addition supported by grants from the Federal Ministry of Education, Science, Research and Technology (01 ER 9701/4) and the German Research Foundation (DFG) (TH 784/2-1), respectively. We thank all members of the GSF Institute of Epidemiology and the field staff in Augsburg who were involved in the planning and conduct of the study. Finally, we express our appreciation to all the study participants. 13. 14. 15. 16. 17. Conflict of interest: none declared. 18. References ‘. 19. 20. 21. 22. 23. 24. 25. 26. Downloaded from http://eurheartj.oxfordjournals.org/ by guest on June 9, 2014 1. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G. National kidney foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 2003;139:137–147. 2. Lysaght MJ. Maintenance dialysis population dynamics: current trends and long-term implications. J Am Soc Nephrol 2002;13:37–40. 3. El Nahas AM, Bello AK. Chronic kidney disease: the global challenge. Lancet 2005;365:331–340. 4. McCullough PA, Soman SS, Shah SS, Smith ST, Marks KR, Yee J, Borzak S. Risks associated with renal dysfunction in patients in the coronary care unit. J Am Coll Cardiol 2000;36:679–684. 5. Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol 2000;35:681–689. 6. Best PJM, Lennon R, Ting HH et al. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol 2002;39:1113–1119. 7. Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med 2001;134:629–636. 8. Garg AX, Clark WF, Haynes RB, House AA. Moderate renal insufficiency and the risk of cardiovascular mortality: results from the NHANES I. Kidney Int 2002;61:1486–1494. 9. Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int 1999;56:2214–2219. 10. Weiner DE, Tighiouart H, Amin MG, Stark PC, Macleod B, Griffith JL, Salem DN, Levey AS, Sarnak MJ. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. J Am Soc Nephrol 2004;15:1307–1315. 11. Muntner P, He J, Hamm L, Loria C, Whelton PK. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol 2002;13:745–753. 12. Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem DN, Griffith JL, Coresh J, Levey AS, Sarnak MJ. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol 2003;41:47–55. Henry RMA, Kostense PJ, Bos G, Dekker JM, Nijpels G, Heine RJ, Bouter LM, Stehouwer CDA. Mild renal insufficiency is associated with increase cardiovascular mortality: the Hoorn study. Kidney Int 2002; 62:1402–1407. Keil U, Liese AD, Hense HW, Filipiak B, Döring A, Stieber J, Löwel H. Classical risk factors and their impact on incident non-fatal and fatal myocardial infarction and all-cause mortality in southern Germany. Results from the MONICA Augsburg cohort study 1984–1992. Eur Heart J 1998;19:1197–1207. WHO MONICA project: objectives and design. Int J Epidemiol 1989;18(Suppl. 1):29–37. Clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. Am J Kidney Dis 2002;39(Suppl. 1):S17–S31. Loewel H, Lewis M, Hoermann A, Keil U. Case finding, data quality aspects and comparability of myocardial infarction registers: results of a south German register study. J Clin Epidemiol 1991;44:249–260. American College of Cardiology Committee. Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology for the redefinition of myocardial infarction. J Am Coll Cardiol 2000;36:959–969. Luepker R, Apple FS, Christenson RH, Crow RS, Fortmann SP, Goff D, Goldberg RJ, Hand MM, Jaffe AS, Julian DG, Levy D, Manolio T, Mendis S, Mensah G, Pajak A, Prineas RJ, Reddy S, Roger VL, Rosamond WD, Shahar E, Sharrett R, Sorlie P, Tunstall-Pedoe H. Case definitions for acute coronary heart disease in epidemiology and clinical research studies. A statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation 2003;108: 2543–2549. Al Suwaidi J, Reddan DN, Williams K, Pieper KS, Harrington RA, Califf RM, Granger CB, Ohman EM, Holmes DR. Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation 2002;106:974–980. Ruilope LM, Salvetti A, Jamerson K, Hansson L, Warnold I, Wedel H, Zanchetti A. Renal function and intensive lowering of blood pressure in hypertensive participants of the hypertension optimal treatment (HOT) study. J Am Soc Nephrol 2001;12:218–225. Schillaci G, Reboldi G, Verdecchia P. High-normal serum creatinine concentration is a predictor of cardiovascular risk in essential hypertension. Arch Intern Med 2001;161:886–891. Wannamethee SG, Shaper AG, Perry IJ. Serum creatinine concentration and risk of cardiovascular disease: a possible marker for increased risk of stroke. Stroke 1997;28:557–563. Sarnak MJ, Levey AS. Cardiovascular disease and chronic renal disease: a new paradigm. Am J Kidney Dis 2000;35(Suppl.):S117–S131. McCullough PA. Cardiorenal risk: an important clinical intersection. Rev Cardiovasc Med 2002;3:71–76. Lamb EJ, Wood J, Stowe HJ, O’Riordan SE, Webb MC, Dalton RN. Susceptibility of glomerular filtration rate estimations to variations in creatinine methodology: a study in older patients. Ann Clin Biochem 2005;42:11–18.
© Copyright 2026