Document 11580
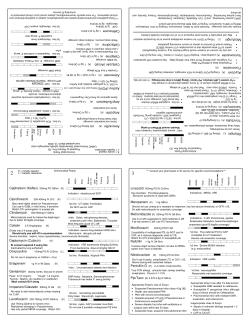
“arguably the greatest risk … to human health comes in the form of antibiotic-resistant bacteria. We live in a bacterial world where we will never be able to stay ahead of the mutation curve. A test of our resilience is how far behind the curve we allow ourselves to fail.” World Economic Forum, 2013 First, do no harm HIV Review of 162 HIV pts hospitalized at Cleveland Clinic in 2011 50% errors in prescriptions for ARV 65% of these errors not corrected by discharge ▪ E.Neuner. Abstract #36170, ID Week, San Diego 2012 Postulated reasons Complexity of regimens Unfamiliarity re HIV Rx by hospital MD’s ▪ Shift of therapy to outpatient setting ART should be offered regardless of CD4 count ART is recommended to persons during acute phase of primary HIV infection regardless of symptoms ART should be started as soon as possible in pts with opportunistic infections TB and Cryptococcus can be exceptions * JAMA. 2012; 308(4): 387-402 ART should be offered regardless of CD4 count There is a steady decrease in AIDS-free survival as CD4 threshold for initiation of Rx decreased. The higher the CD4 achieved after ART, the greater the survival benefit ART reduces likelihood of HIV transmission ▪ Cohen MS, et al. N Engl J Med 2011;365:493-505 ART is recommended to persons during acute phase of primary HIV infection regardless of symptoms. Early Rx associated with: Conserved lymphocyte function Lowered cell-associated HIV DNA Reduction in viral set point Delayed rate of CD4 cell decline Theoretical decline in transmission because of high viral load in newly infected individuals Pneumocystis ART should be started as soon as possible in pts with opportunistic infections Usually start within 2 weeks of diagnosis Cryptococcal meningitis is less certain because of association of increased mortality with early Rx In TB, may delay ART Rx when CD4 > 50 to avoid immune reconstitution syndrome What to start Prior to Rx should check genotype susceptibility Always treat with multiple agents (usually minimum of 3) Convenience of regimen is important as compliance is key to good outcome Specialist involvement improves patient outcomes The desire to take medicine is perhaps the greatest factor which distinguishes man from animals. Sir William Osler Indications for screening for ASB in adults includes: Pregnancy Prior to urologic procedures where mucosal bleeding is anticipated. No other adults with ASB should be treated CID. 2005;40:643-54 Screening for or treatment of ASB is not recommended for the following: Presence of pyuria Nonpregnant women Diabetic women Elderly persons, whether or not institutionalized Spinal cord injuries Catheterized patients Renal or other solid organ transplant The Role of Asymptomatic Bacteruria in Young Women With Recurrent Urinary Tract Infections: To Treat or Not to Treat? 673 young women with ASB 312 not treated, 361 treated 13.1% not treated had recurrence at 12 mos 46.8% treated group had recurrence at 12 mos Cai T. Clin Infect Dis. 2012;55:771-777 Table 2. Prevalence of asymptomatic bacteriuria in selected populations. Population Healthy, premenopausal women Pregnant women Postmenopausal women aged 50–70 years Diabetic patients Women Men Elderly persons in the community Women Men Elderly persons in a long-term care facility Women Men Patients with spinal cord injuries Intermittent catheter use Sphincterotomy and condom catheter in place Patients undergoing hemodialysis Patients with indwelling catheter use Short-term Long-term Prevalence, % 1.0–5.0 1.9–9.5 2.8–8.6 9.0–27 0.7–11 10.8–16 3.6–19 25–50 15–40 23–89 57 28 9–23 100 Patients in nursing homes are frequently evaluated for lethargy/stupor These patients frequently have ASB In the absence of fever and/or leukocytosis, the depressed mental status is seldom due to UTI. (Dr. Pontzer’s observations – unpublished) Many other factors, including dehydration, medications and metabolic factors are common causes The downside for treatment of ASB include: C. diff C. diff C. diff Colonization/infection with multidrug-resistant bacteria in both the index patient and those patients surrounding him/her. Other adverse drug reactions If your patient is afebrile and hemodynamically stable, recommend in most cases refrain from antibiotic treatment for ASB 246 pts with CDI reviewed 141 received non-CDI ABX Rx during and/or shortly after their CDI Rx totaling 445 courses 77% received at least 1 unnecessary ABX dose 26% of ABX Rx was totally unnecessary Leading indications for unnecessary Rx were putative UTI or pneumonia Shaughnessy MK, et al. Infect Control Hosp Epidemiol 2013;34:109-116 HIGH RISK MEDIUM RISK LOW or NO RISK Cephalosporins ß-lactam Sulfonamides 3rd & 4th gen Narrow Tigecycline spectrum Quinolones Carbapenems Vancomycin Clindamycin TMP/SMX Broad Spectrum Tetracyclines Penicillins Macrolides Metronidazole Linezolid & Daptomycin Nitrofurantoin Discontinue the inciting antibiotic therapy Mild disease → po metronidazole 500 mg tid or vanco 125 mg qid for 10-14 days Moderately severe disease → po vancomycin with or without IV metronidazole Cohen SH, et al. Infect Control Hospit Epidiemol. 2010; 31: 421-55 Fulminant disease → po vanco (500 mg qid) &/or intraluminal vanco (500 mg 3-4 x day) with IV metronidazole (500 mg q 8h) Criteria for subtotal colectomy: age >65 with a WBC >50,000 and/or lactate > 5 mmol/L Right-sided colonic lavage as substitute for subtotal colectomy may be viable option* IVIG reported effective in some case reports ▪ Controlled studies remain to be done *Lamontagne et al. Ann Surg. 2007;245:267 Fidaxomicin Narrower spectrum than vanco or metronidazole ▪ Less disruption of colonic flora Lower recurrence (10% v 28%) with non NAP1 strains ▪ No difference with NAP1 strains Expensive ~$3000 per course Louie et al. N Engl J Med. 2011;364:422 “No antimicrobial agent is clearly superior for the initial cure of C. difficile infection” Dimitri, DM. et al. Ann Intern Med 2011;155:839-847 My current favorite po vancomycin pulse taper regimen: Week 1: 125 mg po qid Week 2: 125 mg po bid Week 3: 125 mg po daily Week 4-7: 125 mg po every other day Fecal transplant following 4 days po vanco vs. po vancomycin 500 mg po qid X 14 days 81% cure with transplant 2 of 3 who failed were cured with 2nd transplant 27% cure with standard vanco Rx Donor screening included risk factor questionnaire, parasites, C. diff, pathogenic bacteria, HIV, hepatitis A,B,C, CMV, EBV, Syphilis, serologies for Strongyloides & Amoeba Nood, E. et al. N Engl J Med 2013;368:407-15 Synthetic stool – RePOOPulate Mixture of 33 different intestinal bacteria isolated in pure culture Treated 2 patients who had failed at least 3 courses of Rx for hypervirulent CDI Both were asymptomatic at 6 month follow-up Eliminates concern for disease transmission Eliminates ‘yuk’ factor Petrof, E O, et al. Microbiome 2013; 1: 3 S. aureus 20-40 % mortality Leading cause of both community and hospital acquired bacteremia Complications include endocarditis, osteomyelitis, discitis, joint infection , endopthalmitis and many others Recurrence of bacteremia is common Sexton, D. et al. Treatment of Staphylococcus aureus bacteremia in adults UpToDate Jan 2013 Endocarditis frequency 25-32% TEE often indicated since presence of vegetation can impact management Occasional exceptions may include rapid clearance of bacteremia in the presence of a removable focus (i.e. vascular catheter) TTE is inadequate for ruling out IE Vancomycin Dose must be adjusted based upon patient mass and creatinine clearance Follow trough vanco levels ▪ For sepsis target 15-20 ug/ml ▪ Should be obtained at steady state Consider shift to another agent if MIC is > 2 ug/ml Change to beta-lactam if organism is MSSA ▪ Superiority supported by multiple studies Daptomycin (Cubicin®) Effective against most MRSA & MSSA Not indicated for pneumonia Monitor CPK weekly Linezolid (Zyvox®) Effective against most MSSA & MRSA Lack of cidality suboptimal for endocarditis Not FDA approved for SAB Ceftaroline (Teflaro®) 5th generation cephalosporin Active against MRSA It is bactericidal Not FDA approved for bacteremia/sepsis ▪ Only for SSI (MRSA and MSSA) and community acquired pneumonia (not MRSA) Overuse may well lead to resistance Q 12 hr dose may be suboptimal for sepsis Removable focus Retaining an IV foreign body greatly reduces probability for cure – ideally remove infected devices Presence of cardiac devices decrease cure rate ▪ Chamis AL, et al. Circulation 2001; 104:1029 Patients who have a removable focus may be treated with a 14 day course of IV ABX Rx if all of the following are present: Blood cultures clear within 4 days of onset Rx No valvular abnormalities No indwelling devices: prosthetic joints, heart valves or vascular grafts No evidence for metastatic infection All others should receive 4-6 wks IV ABX Rx Multiple studies conclude that patients with SAB have improved outcomes with an ID consult Forsblom E, et al. CID 2013;56:527 Jenkins TC, et al. CID 2008; 46:1000 Honda H, et al. Am J Med 2010;123:631 Lahey T, et al. Medicine 2009; 88: 263
© Copyright 2026