Document 15560
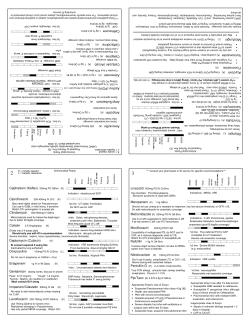
Susan Fryters Susan Fryters, BScPharm., ACPR NPAA Conference June 2013 Objectives To review key changes in the Bugs & Drugs book with a focus on: antimicrobial resistance and how it is affecting the treatment of common infections principles of antimicrobial stewardship in treating infections and preventing antimicrobial resistance. Bugs & Drugs 2012 Authors Dr. Edith Blondel-Hill, MMID Susan Fryters, BScPharm, ACPR > 40 editorial contributors and reviewers Literature search from 2005-August 2011 → Almost 1900 references (1/3 new) Key references/guidelines cited throughout Supported by: Alberta Health Services (AHS) Alberta Health (AH) BC Ministry of Health Do Bugs Need Drugs? program Bugs and Drugs 2012 Sections Antibiotics Treatment Recommendations Prophylaxis Recommendations Dental Pregnancy/Lactation Organisms References – available on-line only Susan Fryters Vancomycin Dosing/Monitoring Guidelines Antibiotics Antimicrobial Spectrum of Activity Pharmacodynamics Dosing Guide and Daily Costs Adult Paediatric Aminoglycosides - Dosing/Monitoring Guidelines High-Dose Extended Interval Conventional Vancomycin Dosing/Monitoring Guidelines Adult Dosing Guidelines in Renal/Hepatic Impairment Loading Dose: 25-30mg/kg (ABW; no maximum) single dose followed by MD at appropriate dosing interval, e.g. q8h, q12h, etc. Severe infections - where rapid attainment of target g of 15-20mg/L g needed,, e.g.: g trough Vertebral osteomyelitis Epidural abscess MRSA pneumonia Septic shock Patients with significant renal dysfunction - to decrease time to target trough level Rybak M, Lomaestro B, Rotschafer JC, et al. Therapeutic monitoring of vancomycin in adult patients: A consensus review of ASHP, IDSA, SIDP) Am J Health Syst Pharm 2009;66:82-98.. Vancomycin Dosing/Monitoring Guidelines Maintenance Dose (MD): 15mg/kg (ABW; empiric max of 2g/dose) at dosing interval based on Clcr and target trough q8h dosing in patients with good renal function Calculated Clcr (mL/min) Dosing Interval for trough 10-20mg/L Dosing Interval for trough 15-20mg/L ≥ 80 q12h q8h 40 - 79 q24h q12h 20 - 39 q36h q24h 10 - 19 q48h q48h < 10 Consider loading dose. Obtain pharmacist consult. Consider loading dose. Obtain pharmacist consult. Vancomycin Dosing/Monitoring Guidelines Desired trough levels: Serious MRSA infection CNS infections Endocarditis Osteomyelitis Pneumonia Bacteremia All other infections 15 20 mg/L 15-20 10-20 mg/L Rybak M, Lomaestro B, Rotschafer JC, et al. Therapeutic monitoring of vancomycin in adult patients: A consensus review of ASHP, IDSA, SIDP) Am J Health Syst Pharm 2009;66:82-98.. Antibiotics Antimicrobial Generic/Trade Name Listing IV to PO Switch Recommendations CSF Penetration of Antimicrobials β-lactam Allergy Susan Fryters β-Lactam Allergy Accurate allergy history important: to determine nature of reaction to decrease use of broad spectrum alternatives Cross-reactivityy between p penicillin &: cephalosporins 1% (2.55% if confirmed pen allergy) negligible between penicillin &: 2nd generation cephs (except cefaclor & cefprozil) 3rd and 4th generation cephs carbapenems ~1% Frumin J, Gallagher JC. Allergic cross-sensitivity btwn pen, carbapenem, monobactam abx. AnnPharmacother 2009;43:304-15 Management of β-Lactam Allergy If documented severe non-lgE-mediated reaction to penicillin, such as: interstitial nephritis Avoid all β-lactams (penicillins, hepatitis cephalosporins, carbapenems) hemolytic anemia serum sickness severe cutaneous reactions If documented severe lgE-mediated reaction to penicillin, such as: Avoid penicillins, firstgeneration and secondurticaria (hives) laryngeal edema, angioedema generation cephalosporins Solensky R, Khan DA, eds. Drug allergy: an updated practice parameter. Ann Allergy, Asthma & Immunol 2010;105:273.e1-78. Frumin J, Gallagher JC. Allergic cross-sensitivity btwn pen, carbapenem, monobactam abx. AnnPharmacother 2009;43:304-15 Management of β-Lactam Allergy TREATMENT RECOMMENDATIONS Treatment options for pts with severe IgEmediated pen allergy include: Non-β-lactam β antibiotic or 3rd or 4th -generation cephalosporin or carbapenem via graded challenge* or 3rd or 4th -generation cephalosporin or carbapenem after drug desensitization* Recommended Empiric Therapy of Selected Infections Neonates/Paediatrics Adults Ophthalmic Fungal Enteric Parasitic Solensky R, Khan DA, eds. Drug allergy: an updated practice parameter. Ann Allergy, Asthma & Immunol 2010;105:273.e1-78. TREATMENT RECOMMENDATIONS Recommended Therapy of Culture-Directed Infections Pneumonia CAPD Peritonitis Adult - ISPD 2010 Guidelines Pediatrics - ISPD 2012 Guidelines Meningitis Endocarditis - gent synergy for native valve MSSA/MRSA endocarditis no longer recommended due to increased nephrotoxicity, and no difference in cure, mortality, or relapse Culture- negative Endocarditis MRSA Methicillin-resistant S. aureus resistant to all β-lactams (cloxacillin, cefazolin, other cephs, carbapenems) Community-associated MRSA (CA-MRSA) 56% of MRSA isolates in Edmonton may be susceptible (S) to TMP/SMX, doxycycline, clindamycin all S to vancomycin Healthcare/hospital associated MRSA (HA-MRSA) usually only susceptible to vancomycin, [linezolid, daptomycin] Susan Fryters MRSA MRSA Significant M&M in both CA & HA infections - SSTI, pneumonia, bacteremia 20-25% of S. aureus clinical isolates in western Canada are MRSA Edmonton – 13%, UAH ~20% Calgary – 19% Resistance to clindamycin (and quinolones) very % Susceptible common Clindamycin Tetra/Doxy TMP/SMX Vancomycin 63 vs. MSSA 76% 96 97 100 Calgary – S. aureus 62-77 97 96-97 100 Central – MSSA 80 97 99 100 Edmonton – MRSA Empiric therapy of serious infections – vancomycin or linezolid Switch to β-lactam if appropriate and susceptible (MSSA) as better outcome – next slide Increased vancomycin MICs → clinical failure Linezolid preferred over vancomycin if: vancomycin MIC ≥ 1.5µg/mL concurrent nephrotoxins pre-existing renal dysfunction Drugs for Serious MRSA Infections cSSSI Drug Daptomycin Bactericidal vs. (MR)SA • Once daily • Potential for cross-resistance with vancomycin • Not for use in lower RTIs • ADRs: dose-dependent dose dependent ↑ CK, CK rhabdomyolysis Vancomycin • Slowly bactericidal vs (MR)SA • Twice-thrice daily, IV only Linezolid IV/PO • Bacteriostatic vs. (MR)SA • ADRs • Twice daily • Oral formulation Bacteremia/IE Dosage Dosage 4mg/kg IV Q24h 6mg/kg IV Q24ha 15mg/kg IV Q12H 15mg/kg IV Q8-12H 600 mg Q12H 600 mg Q12Hb • a. Although daptomycin is approved at this dosage, higher doses (up to 12 mg/kg/day) are being used due to its concentration dependent activity to increase its antibacterial activity and potentially prevent the development of resistance. b. Linezolid is not indicated for bacteremia or infective endocarditis specifically although there are limited clinical data on its use in bacteremia & infective endocarditis. Skin/Soft Tissue Infections Skin/Soft Tissue Infections MRSA Superficial – when to use systemic therapy vs. topical Impetigo Folliculitis/furunculosis Carbuncles Cellulitis – differential diagnosis Clindamycin – significant Strep/Staph resistance – use only if β-lactam allergy – monitor clinical response Empiric therapy: Carbuncles – unresponsive to clox or cephalexin I&D +/TMP/SMX or Doxycycline Purulent cellulitis Mild: I&D if abscess +/Cephalexin (for MSSA/Strep) + [TMP/SMX or Doxycycline (for MRSA/MSSA)] Moderate-severe: I&D if abscess + Vancomycin Susan Fryters Bone & Joint Infections Diabetic Foot Infections Added section on Vertebral OM: Most common type of OM in adults S. aureus most common; MRSA especially if: preceding trauma multifocal lesions disease in adjacent muscle Empiric coverage of P. aeruginosa IF: tropical/warm climates soaking of feet failed nonpseudomonal therapy limb threatening infection limb-threatening Rx: Cloxacillin 2g IV q4h MRSA/β-lactam allergy Vancomycin 25-30mg/kg once then 15mg/kg IV q8-12h Empiric coverage of MRSA IF: previous (prior 12 months)/current colonization/infection with MRSA recent antibiotic use recent hospitalization Alternative Linezolid or TMP/SMX Lipsky BA, et al. IDSA clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis 2012;54:132-73. Zimmerli W. Vertebral osteomyelitis. N Engl J Med 2010;362:1022-9. Sinusitis S. pneumoniae Penicillin resistance has stabilized – still very low rates of pen R in Western Canada justifying: continued use of oral amoxicillin (best activity of any oral β-lactam agent) for mild-moderate infections & Ceftriaxone for more serious infections Pen IV can be used if penicillin S confirmed Significant resistance to macrolides (21-29%), clindamycin (14%), and (6-32%) TMP/SMX (6-32%). Empiric therapy with these agents no longer recommended for majority of RTIs New IDSA guidelines: Chow AW, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis 2012:x:e1-41. 70% spontaneous resolution; only treat IF: Symptoms >10 days Worsening after 5-7 days Severe - ≥ 39 C and purulent nasal discharge or facial pain x 3-4 consecutive days Immunocompromised % Susceptible Pen PO* Pen IV NM* Pen IV M** Amox * Cefuroxime Ceftriax one** Clindamycin Erythromycin Tetracycline TMP/ SMX Levofloxacin Edmonton 87 91 85 100 91 100 86 76 83 83 99 Calgary NA NA 82-96 NA NA 91-98 NA 71 86 68 100 Central NA NA NA NA NA 100 NA 79 NA 94 NA Local S. pneumoniae resistance ⇒ Macrolides, TMP/SMX and second generation cephalosporins no longer recommended empirically Rx: Amoxicillin – high dose if antibiotic use in past 3 months Alternative: Doxycycline *NM = nonmeningeal breakpoint **M = meningeal breakpoint AECB First line: Amoxicillin or Doxycycline or TMP/SMX Second line: Amoxicillin-clavulanate or Cefuroxime axetil or Levofloxacin NB: Macrolides only as alternative to these due to poor Haemophilus coverage and significant S. pneumoniae resistance Outpatient CAP Imperative to adequately cover S. pneumoniae - add Amoxicillin to Doxycycline if: lobar pneumonia with fever or rigors recent antibiotic therapy tetracycline y resistance > 15% Cover MRSA (Doxycycline or TMP/SMX) IF: S. aureus/GPC clusters on Gram stain diabetes recent influenza Duration: minimum of 5 days and until afebrile 4872h Mandell LA, et al. IDSA/ATS consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007;44:27-72. Susan Fryters Hospitalized & Severe/ICU CAP HAP/VAP Cover MRSA IF: coma DM head injury recent influenza IVDU antibiotics in past 3 months lung disease (bronchiectasis/CF) immunosuppression Cover MRSA (Vancomycin or Linezolid) IF: rapid onset necrotizing process on CXR recent influenza colonization/recent infection with MRSA S. aureus/GPC clusters on Gram stain Duration: 7 days 14 days if MRSA, Pseudomonas, Acinetobacter NHAP Gram Negative Resistance Imperative to adequately cover S. pneumoniae – Amoxicillin 1g PO tid COPD or post-influenza – use Amoxicillin(plus Doxycycline y y or Azithromycin y or clavulanate (p Clarithromycin if underlying pulmonary disease) as better coverage of : M. catarrhalis/H. influenzae S. aureus Duration: 7 days FQ and TMP/SMX resistance in enteric GNB (E. coli, Proteus mirabilis, Morganella morganii, Serratia marcescens) > 20% → empiric therapy with FQs & TMP/SMX no longer recommended for infections where GNs are predominant pathogens – GI, UTI % Susceptible Amp/ Amox Amox clav Cefixime Ceftria xone TMP/ SMX Cipro NTF (urine) Gent 38 68 92 94 76 77 99 92 Calgary 39-44 NA NA 86-89 71-78 71-77 93-96 83-91 Central 63 NA NA 99 80 83 98 94 E. coli Edmonton Gram Negative Resistance ESBL & AmpC Increased β-lactam (pen/ceph) resistance due to ESBL (3.5% of Enterobacteriaceae) and Amp C β-lactamases Typically associated with multi-resistance to other antibiotic classes including TMP/SMX, FQs, tetracyclines, aminoglycosides ESBL increasingly seen in community-acquired infections, especially UTIs (90% of ESBLs are seen in urine) C b Carbapenems often ft only l class l lleft ft tto ttreatt serious i ESBL and d Amp A C infections, and NTF or fosfomycin for uncomplicated UTIs But now carbapenemase–producing organisms (KPC) UTI Increased FQ, TMP/SMX and amoxicillinclavulanate resistance of E. coli first line empiric therapy with these no longer recommended if used, confirm S by culture % Susceptible E. coli Amp/ Amox Amox clav Cefixime Ceftria xone TMP/ SMX Cipro NTF (urine) Gent % Susceptible ESBL E. coli TMP/ SMX Cipro NTF (urine) Gent Erta Mero Imip Edmonton 40 11 96 63 100 100 100 Central* 40 12 89 78 NA 100 NA * Piperacillin-tazobactam susceptibility listed but shouldn’t be used even if documented S as clinical failures have been reported. Carbapenem best option. Edmonton 38 68 92 94 76 77 99 92 Calgary 39-44 NA NA 86-89 71-78 71-77 93-96 83-91 Central 63 NA NA 99 80 83 98 94 Susan Fryters UTI Fosfomycin (Monurol) Monurol) Use cefixime, nitrofurantoin*†, fosfomycin*† * For uncomplicated UTI only; not for complicated, pyelonephritis, or urosepsis as poor renal tissue and serum concentrations / lack of clinical data † Effective against majority of ESBL E. coli Once only drug for uncomplicated UTI Spectrum of activity: E coli E. coli* * including ESBL P. mirabilis* Citrobacter spp* E. faecalis NOT S. saprophyticus Back on the market through Triton Under consideration for listing on AH DBL Gupta K, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the IDSA and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 2011;52:e103-20. Complicated or catheter catheter-associated UTI Add gentamicin if: Septic shock Recent antibiotic use Suspected p ESBL,, AmpC p or carbapenemase p producing organism Duration: If prompt response (48-72h): 7 days If delayed response or structural abnormality: 14 days Hooton TM, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 international clinical practice guidelines from the IDSA. Clin Infect Dis 2010;50:625-63. Clostridium difficile infection (CDI) Anaerobe Resistance Increased resistance and clinical failures Clindamycin R common in both GP and especially GN anaerobes Increased R to moxifloxacin, especially Bacteroides and Prevotella M t id Metronidazole l and d carbapenem b R still till relatively l ti l rare b butt have been found with increasing frequency % Susceptible Edmonton Pen Clinda Anaerobic GPC 100 49 Metro 99 B. fragilis / B. fragilis group 3 51 100 Clostridium spp 94 78 100 Fidaxomicin (Dificid) Dificid) New class of drug for CDI 2 RCTs: Noninferior to vancomycin PO for cure; superior in reducing CDI recurrences 200mg PO bid x 10 days $231.00/day Common Drug Review recommendation: DO NOT LIST at submitted price Cohen SH, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by SHEA and IDSA. Infect Control Hosp Epidemiol 2010;31:431-55. Susan Fryters GI infections Intra--abdominal infections Intra Updated H. pylori to include sequential therapy Increased FQ and cefazolin resistance: Empiric therapy for peritonitis and cholecystitis now ceftriaxone + metronidazole, metronidazole not cefazolin* * If cefazolin is reported as S, can use but at 2g/dose Ciprofloxacin only if severe β-lactam allergy STI/Genital STI/Genital Updated as per 2010 Canadian PHAC guidelines Neisseria gonorrhoeae Increased FQ R → quinolones no longer recommended d d [PHAC D Dec 2011] Increased ceph R: ⇒ higher doses of cephalosporins recommended ⇒ Ceftriaxone recommended in: MSM or pharyngeal infection Genital Ulcers Table on Clinical Features and Diagnosis Central Nervous System Added section on Recurrent/chronic meningitis Empiric coverage of MRSA IF: Post-trauma or postop meningitis Shunt/EVD meningitis/ventriculitis B il skull Basilar k ll ffracture t and d prolonged l dh hospitalization it li ti Colonized with MRSA and brain abscess 2 to IE or epidural abscess Greatly expanded section on Encephalitis including: Epidemiology Investigations Etiology Susan Fryters Fungal Infections Cardiovascular Candida [Pappas PG, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the IDSA. Clin Infect Dis 2009;48:503-35.] Added section on Cardiac device related infections/ endocarditis (CDRIE) Empiric coverage of MRSA recommended in: Purulent pericarditis Endocarditis CDRIE Fungal Infections Prophylaxis Recommendations C. albicans and C. glabrata - > 80% of all Candida from sterile sites: % Susceptible Oropharyngeal Esophageal y p g risk Candiduria – onlyy treat symptomatic or high patients Invasive candidasis/Candidemia: Hemodynamically stable, no azoles past 3 months – fluconazole Hemodynamically unstable or azoles in past 3 months – echinocandin (micafungin) or ampho B Hepatosplenic Candidiasis/Chronic disseminated candidiasis Ampho B Fluc Vori Mica C. albicans 100 93 92 100 C. glabrata 100 NA 90 96 Source: UAH 2011 Antibiogram PCP now in Fungal section as re-classified as a fungus Prevention of Perinatal Infection Intrapartum Antimicrobial Prophylaxis of Group B Strep Penicillin/Ampicillin 1st line Non severe β-lactam allergy: Cefazolin Increased erythromycin and clindamycin resistance of Group B Strep ⇒ Erythromycin no longer recommended ⇒ Clindamycin only if susceptibility confirmed Vancomycin now recommended if severe pen allergy and clindamycin resistance or susceptibility unknown Centers for Disease Control and Prevention. Prevention of perinatal Group B streptococcal disease. Revised guidelines from CDC, 2010. MMWR 2010;59(No. RR-10):1-31. Surgical Prophylaxis → iPhone, AHS on-line Endocarditis Prophylaxis – AHA 2007 guidelines Blood/Body Fluid Exposure Sexual Assault Prophylaxis for Contacts of Communicable Diseases Infection Prevention and Control MRSA/VISA/VRSA VRE CDI ESBL AmpC Carbapenemases ORGANISMS Antibiograms (no longer in book) Calgary Zone Antibiograms 2012 (CLS) p g y http://www.calgarylabservices.com/files/LabTests/Micro biologyNewsletters/2012_Antibiogram.pdf Edmonton Zone Antibiograms 2011 – UAH & Stollery Children’s Hospital Antibiograms 2011 – Edmonton Hospitals (DynaLIFE) Central Zone 2011 South Zone 2010 http://www.albertahealthservices.ca/3294.asp Susan Fryters Antimicrobial Stewardship Appropriate use of antibiotics is critical since: Antimicrobial resistance is increasing, leading not only to increased costs of patient care but also to increased morbidity and mortality In the hospital setting: Over 50% of patients in hospital receive antibiotics during their stay – at least 50% unneeded in most studies Antimicrobials comprise the single largest category of drug expenditures in AHS hospitals at approximately 20% of the drug budget Antimicrobial Stewardship Appropriate: 1. Selection: Empiric – B&D Definitive – B&D and C&S results Streamlining or de-escalation 2. Dosing – PK/PD 3. Route – IV to PO 4 Duration 4. D ti – reduces d selective l ti pressure on b bacteria t i preventing emergence of resistance of antimicrobial therapy to: optimize clinical outcomes minimize: toxicity superinfections, e.g. CDI resistance reduce health care costs – drug, HCAI, resistance www.bugsanddrugs.ca Antimicrobial Stewardship Appropriate Duration Louis Rice: “reduction in length of antibiotic therapy is the antibiotic strategy most likely to be effective in reducing antibiotic resistance.” [Rice LB, Maxwell Finland ICAAC lecture. Clin Infect Dis 2008;46;491-6] Clin Infect Dis 2011;52:1232-40. J Antimicrob Chemother 2012;67:2570-5. Bugs and Drugs For more information: [email protected] Susan Fryters, BScPharm., ACPR Edmonton Oliver PCN April 2013 Susan Fryters THANK YOU
© Copyright 2026