Read the Central West CCAC 2015/2016 Quality Improvement Plan
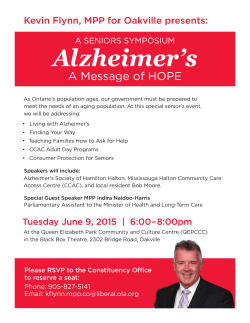
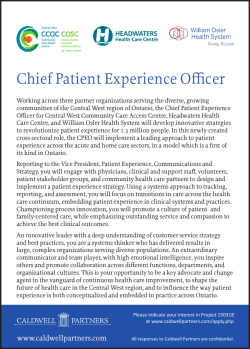
Quality Improvement Plan (QIP) Narrative for Health Care Organizations in Ontario April 1, 2015 This document is intended to provide health care organizations in Ontario with guidance as to how they can develop a Quality Improvement Plan. While much effort and care has gone into preparing this document, this document should not be relied on as legal advice and organizations should consult with their legal, governance and other relevant advisors as appropriate in preparing their quality improvement plans. Furthermore, organizations are free to design their own public quality improvement plans using alternative formats and contents, provided that they submit a version of their quality improvement plan to Health Quality Ontario (if required) in the format described herein. 1 Overview In 2014, the Central West Community Care Access Centre (CW CCAC), Headwaters Health Care Centre (Headwaters) and William Osler Health System (Osler) committed to an innovative partnership to integrate nonclinical (administration or back-office) support functions across the three organizations. This cross-sector partnership is the first of its kind in the Province and will accelerate a regional approach to planning to support the delivery of quality, timely health care services to those we serve. This year, our quality improvement plans (QIPs) reflect this bold, new partnership and present a more in-depth and systematic approach to setting improvement targets and developing change initiatives. Our QIPs also highlight key strategies for quality improvement within our organizations and across our local health care system and are key components of our comprehensive quality programs. Collectively we have placed patients at the core of our strategies to help create consistently exceptional patient experiences. Together, we will work to enhance the safety and effectiveness of the system as a whole, through our innovative practices and focused QIPs. What does quality mean to the CW CCAC, Headwaters and Osler? Quality is the foundation of everything we do and it shapes how we interact with and care for patients, their families and the communities we serve. To the CW CCAC, Headwaters and Osler, quality means taking a system-wide approach to ensuring patients get the care they need, when and where they need it. We are committed to working with our strategic partners to provide the best experiences, treatments and outcomes for patients and families every day. Together, we believe quality means: • • • • • Patients are informed about healthy lifestyle choices so they can stay healthy or better manage their chronic diseases at home or in the community. Health care providers in our communities can easily identify and access services at our hospitals, so patients do not make avoidable trips to the emergency department. When emergency care is required, patients have timely access to services and experience seamless transitions between hospital departments, between hospitals in our region, and between the care they receive in hospital and the care and support they receive in the community through the CW CCAC. Our services are inspired and shaped by patients and the care they receive is personalized to their needs so it is in keeping with a patient’s belief and values. Information flows easily between care providers to support clinical decision-making about care and treatment. We support staff in continuously developing their skills so they can provide the best possible care and services that are safe, effective and reflective of best practices. Quality also means investing in innovation and striving for improvements to not only provide the exemplary care that patients and the community expect but lead the way in creating inspired new approaches that are at the forefront of care delivery. How will our 2015-16 QIPs improve care for patients? The CW CCAC, Headwaters and Osler are committed to evidence-based practices and to providing the best possible care to meet the unique needs of each patient. In addition, we are focused on improving how patients transition through programs and services within our hospitals, and as they return home with support from the CW CCAC or to another destination, such as long-term care, so their journey is a seamless one. 2 We believe we can make a significant impact on improving care for patients in our region by having shared accountability for success on the following measures: • Voice of the Patient. We will infuse the voice of the patient in all that we do to create ideal experiences that are inspired and shaped by patients and personalized to their needs. • Patient Satisfaction. There is a significant opportunity to transform and improve care across our region by improving the experience for patients and their families. By listening to patients we understand that satisfaction is largely based on their experience of how service is delivered, rather than the technical aspects of the medical care they receive. Every touch point of patient care, whether in the home or an acute care setting, leaves a lasting impression on how well patients feel they were served. To help us identify opportunities to create the best possible patient experience, CW CCAC, Headwaters and Osler will continue to measure how patients rate the care and services they receive at our organizations using our NRC Canada Patient Satisfaction Surveys. To gather as much information as possible, we will also make phone calls to patients after they leave our hospitals and, where applicable, as their care transitions to the CW CCAC, to inquire about their experience. Measuring patient satisfaction with the transition between acute care and the CW CCAC is unique in Ontario. • 30-day Readmission. Readmission to hospital within 30 days of discharge can be challenging for patients, their families and the overall health care system. To improve the health, safety and quality of care for our community, as health care providers, we have a unique opportunity to work together to reduce preventable hospital readmissions by ensuring patients get the care they need, when they need it and in the most appropriate setting. • Wait Times. For many people in the community, the Emergency Department (ED) is the gateway to health care and as more patients come through our doors the impacts are felt across Headwaters and Osler and in the community. While Osler continues to navigate through the highest ED volumes in the province, patients coming to Headwaters through their ED typically experience shorter wait times than others. With consistently increasing numbers of patients visiting our EDs, Headwaters and Osler will build on past accomplishments and focus on new opportunities to ensure exceptional care continues. And, as increasing demand extends wait times, the CCAC is instrumental in supporting the safe and timely discharge of patients once their acute care needs have been met, helping to reduce hospital wait times further. • Falls. Falls pose a significant risk to patient safety and wellbeing. The CW CCAC will strive to reduce the number of patient falls in the home, by working with patients to increase their knowledge, confidence and independence. Headwaters and Osler play vital roles in supporting the CW CCAC’s improvement focus on falls prevention by creating consistent documentation standards to better record and share falls-related information, including fall risk assessment results and fall prevention strategies. To make improvements in these areas with our partners and to address improvement initiatives specific to each organization, the CW CCAC, Headwaters and Osler have each developed comprehensive quality improvement strategies and specific targets in the areas which are highlighted below. 3 CW CCAC How will we improve? How will we achieve this? We will innovate with our partners to ensure patients continue to receive coordinated care in a timely manner. • We will infuse the voices of both patients and caregivers in all that we do to create optimum experiences that are inspired and shaped by patients and personalized to their needs. • • • • • • We will implement new and leading best practice initiatives to enhance the safety of our patients at home. • We will work together as health care providers to reduce preventable hospital readmissions by ensuring patients get the care they need, when and where they need it. • • • • • • • Optimize our role in care coordination, system navigation, and timely service delivery by more closely aligning CW CCAC staff with primary care providers and local hospitals. Strengthen partnerships with our contracted service providers to develop more effective processes and remove barriers to reducing wait times. Bring the voice of the patient and caregiver to the forefront through enhancement of the Patient and Caregiver Advisor role. Define the “Patient and Caregiver Experience” so we can better measure and monitor our actions to improve it. Gain a comprehensive understanding of the transitions across the partners and determine what drives satisfaction across the region through the regionalization of a call centre with our local hospital partners. Partner with our contracted service provider organizations to ensure outstanding care through quality-based performance. Develop and implement a “Patient and Caregiver-Centered Framework” to ensure their voices are central to everything we do. Collaborate with hospital partners to improve communication regarding patients who are at risk for falls as they are discharged from hospital to CW CCAC. Require contracted service providers to complete regular fall risk assessments and share results with the CW CCAC. Expand the implementation of the Home Independence Program to reduce falls and maintain patients’ independence and safety. Optimize the CW CCAC’s falls prevention and exercise classes to ensure they benefit as many people as possible. Select, implement and evaluate the use of a validated hospital readmission predictor tool. Connect patients without a primary care provider with one in their community. Complete cross-sector case reviews on patients who experience avoidable hospital readmissions within 30 days of discharge. Continue to develop formal care plans for Health Links patients. Embed our Home Visiting Pharmacist, Rapid Response Nursing and Mental Health and Addiction Nursing programs further into our evolving models of service delivery. 4 Headwaters How will we improve? Reduce the wait time for patients to be transferred to an inpatient bed from the emergency department. Work together with patients, families and other providers to ensure accurate and comprehensive medication information is communicated when the patient leaves the hospital. Continue to reduce the risk of patients contracting a hospital acquired infection. How will we achieve this? • Improve existing processes and technologies to facilitate easier access to information, inform decision-making and communication to transition admitted patients faster. • Develop an effective process built on knowledge and experiences when medication information is gathered on patients upon their arrival at the hospital and implement tools based on patient, staff, physician and community partner feedback. • Implement new practices and auditing tools to improve practices and enhance compliance to keep patients, visitors, staff, physicians and volunteers safe. Continue to enhance antibiotic microbial stewardship. • Osler How will we improve? We will work directly with patients to better serve their needs and create the ideal patient experience. We will reduce the wait time for patients to be transferred to an inpatient bed from the emergency departments. We will introduce innovative models of care to better meet patient needs, deliver the same or better outcomes and, at the same time, shorten or avoid hospital stays. We will reduce the risk of patients getting a hospital acquired infection or being prescribed the wrong medication. How will we achieve this? • Continue to capture patient feedback and action improvements to enhance services. • Introduce a new ED customer service model to proactively engage with patients/families and conduct customer service education and training for specific roles to enhance the patient/family experience. • Regionalize the call centre to get a comprehensive understanding of the transitions across the partners and to determine what drives satisfaction across the region. • Continue to implement technology to facilitate easier access to patient information to inform clinical decision-making. • Continue to focus on sustainable improvement strategies to better align and optimize our capacity with demand and improve access for patients in high-need areas. • Engage community-based mental health and addiction services and improve processes in the ED to address mental health patients’ needs and effectively transition patients to community resources. • Continue developing Health Links across the care continuum in CW LHIN to improve the coordination of care for medically complex patients. • Increase the number of medically complex patients who access Telehomecare and expand enrollment of diabetic patients in the Centre for Complex Diabetes Care to effect a decrease in readmission rates for these patients. • Continued engagement of proper hand hygiene practices and compliance to keep everyone at Osler safe from harm. • Continued focus on improving the collection and documentation of patient medication information and sharing it with other health care providers through care transitions. • Continued expansion of the antimicrobial stewardship program to reduce the risk of hospital acquired infections directly linked to antibiotic usage. 5 Integration & Continuity of Care How does the QIP align with other planning processes and strategies? Our QIPs take into account the priorities and common directions of our three organizations, as well as our other health system partners, the Ministry of Health and Long-Term Care (MOHTLC), and the Central West Local Health Integration Network (LHIN). These strategic themes are woven through our various quality, safety and improvement plans to ensure patients and families within our region get the care they need, when and where they need it, today and into the future. Our QIPs fully align with each of our corporate directions and goals outlined in our multi-year Strategic Plans, Annual Business Plans and Regional Information Management and Information Technology Plan. For Headwaters and Osler, our QIPs also align with our respective Clinical Priorities Plans. Priorities identified by Accreditation Canada were also taken into consideration in the development of our QIP. By aligning our improvement agendas with our corporate strategies and plans, we sharpen our focus on quality, and strengthen our ability to successfully achieve the Vision of each of our organizations as we embed innovation and best practice into the quality and safety culture within our and among our partners’ organizations. As one means of measuring our success, in 2016, the organizations will also seek to maintain its Accreditation with Exemplary Standing through Accreditation Canada. To view the Strategic Plan, Annual Business Plan, Accreditation Report and other quality and safety indicators of CW CCAC, Headwaters or Osler, please visit our web sites: • • • www.healthcareathome.ca/centralwest www.headwatershealth.ca www.williamoslerhs.ca Thanks to the dedication of staff, hospital physicians and hospital volunteers, the commitment of our Boards of Directors and leadership, and the support from and collaboration with our community partners, we are confident we will achieve the goals outlined in our 2015-16 QIPs. How will we work with our health care partners? By working with our partners more closely than ever before, we are creating new opportunities to improve the quality of patient experience across the Central West region. Our dynamic new non-clinical administration partnership is a catalyst for further collaboration, joint investment opportunities, system-level planning and improves our combined ability to meet the health care needs of our community. Our collective Vision, Mission, Values and corporate priorities demonstrate a strong degree of existing organizational alignment which will help us successfully achieve our goal of improving care for patients in our region. We are creating new opportunities to leverage the strengths and expertise of our organizations. Health Links is a great example of where we’ve taken a leadership role in our region to work with health care providers across the Central West LHIN, to improve access to health care services and make it easier for patients and families to get the appropriate level of care in their home, community or in the hospital. As partners, we believe our 2015-16 QIPs demonstrate our combined commitment to enhancing the quality of care across the care continuum. 6 Challenges, Risks & Mitigation Strategies How will we overcome challenges to ensure success? The CW CCAC, Headwaters and Osler have established innovative strategies and stretch targets for each of our organizations. Our QIPs will require the collective efforts of our staff, physicians, hospital volunteers, partners throughout the system, and for the CW CCAC, the engagement of their contracted service providers. In order to be successful, we have identified solutions to help us overcome the challenges we face today. CW CCAC Challenges Demand for services Our region is home to one of the fastest growing and most diverse populations in the province. Solutions • Partner with hospitals, primary care providers and other community sector partners optimize access to services in our community, so patients get the care they need, when they need it and in the most appropriate setting. • Actively seek to gain better insight into the unique health care needs of our diverse population and link them to appropriate care in a timely manner. Increased complexity of patient needs As people age, the complexity of their health care needs also increases. • • • • Work with local hospitals to help patients stay safely at home longer with CCAC services. Improve communication between providers to promote effective, safe care transitions. Continue to collaborate with primary care providers and other partners to support high-needs patients though Health Links and other key initiatives. Focus on efficiency improvements and standardization within our region so we can support as many complex patients possible in the community once their acute care needs are met. Tailor our programs and services to best meet the needs of patients. Streamline processes to avoid duplication and improve the flow of patients through the health care system. • Continue to identify Health Links patients and create outcome-based care plans to best manage their chronic conditions. More chronic conditions Our region has an increased number of people with complex chronic health conditions. • • Economic constraints Health funding reforms have changed the way health care providers are funded. • Patient preferences There is a need for a deeper understanding of the patient and caregiver experience. • • • • Support funding shifts to promote care delivery in the most appropriate setting. Improve efficiency by utilizing quality improvement tools and applying leading practices so we can provide more care with our available resources. Continue to engage patients through existing channels and implement new ways of reaching out to patients and caregivers even further. Involve patients and families at all touch points in their health care journey so that care is personalized. Implement leading global practices in customer service and improving the patient experience. 7 Headwaters and Osler Challenges Demand for services Our region is one of the fastest growing with aging populations. Headwaters, as a mediumsized hospital, is dependent on its partners to help deliver the right care, when and where it is needed. More chronic conditions Our region has an increased number of people with complex chronic health conditions. Economic constraints Health funding reforms have changed the way health care providers are funded. Organizations are doing more with less. Patient preferences Many aspects of patient experience need more consideration and understanding. Solutions • Partner with health care providers to identify and access services so patients get the care they need, when and in the most appropriate setting • Improve communication between providers to promote effective, safe care transitions. • • • • • • • • Streamline processes to avoid duplication of services and implement improvements for better flow of patients through our system Tailor our programs and services to meet the needs of patients in our community. Specific to Osler-Create specialized services and centres of excellence in order to better meet the needs of patients. Focus on efficiency improvements and standardization within our region so that we can provide more with the same resources Support shifts in funding to promote delivery of care in the most appropriate setting. Find effective new ways to communicate with patients. Involve patients and families at all touch points in the health care journey so that care is personalized. Implement leading global practices in customer service and improving the patient experience. Information Management Systems How will we harness technology? Technology helps to facilitate exemplary patient care. Through the development of a Regional Information Management and Information Technology Plan with our strategic partners, we will create an integrated roadmap to leverage technology solutions such as a patient portal and other information sharing platforms to improve quality of care for patients in our region and quality of the work environment for our staff members. To inform the targets in our QIPs and corporate scorecards, each of our organizations leverages data from our own information systems, provincial data sets and information from health care partners. Data quality is a focus for all of us to ensure data is accurate, complete, timely, reliable and relevant for clinical, statistical and financial information to support decision-making and performance management. In keeping with our commitment to quality, we use technology and its tools to regularly monitor, measure, assess and evaluate our targeted improvement plans to proactively deliver care to enhance health, treatment and outcomes. 8 Engagement of Clinicians & Leadership Quality improvement is deeply ingrained in each of our cultures and at every level of our organizations, by those who deliver and support exemplary care. At Headwaters and Osler, our QIPs were individually developed with the involvement of our respective Boards of Directors, Quality Committees, senior leadership, clinicians, physicians and staff. By using performance huddles with aligned quality measures and indicators, as well as a daily access reporting tool, clinicians, staff, physicians and leadership are frequently engaged in, measured on, and share in the quality goals and commitments at our hospitals. In setting its strategic directions for 2013-2016, the CW CCAC’s Board o f D i r e c t o r s articulated a desired future state that is patient-centric and fueled by fabulous people, engagement and innovation. Staff from throughout the organization are regularly engaged in the creation, prioritization and implementation of programs that support the realization of the CW CCAC’s strategic directions, drive quality and add value. To ensure Headwaters’ continued success on its journey of quality improvement and innovation, clinicians, staff, physicians and leadership receive training and education opportunities to enhance their capacity for change, innovation and improvement. This year, the CW CCAC and Osler will work closely with Headwaters to standardize and implement an evidence-based leadership development framework across all our organizations. Patient/Resident/Client Engagement To create the best possible patient experience and achieve the Visions for our organizations, the voice of the patient is infused throughout our organizations. Continuous patient feedback helps shape our plans and initiatives, including our QIPs in order to improve the quality and safety of care. We directly engage patients to seek input on the quality of their care and their experience, through NRC Canada Patient Satisfaction Surveys and by connecting with patients directly via phone calls after they are discharged from hospital or from home care. In addition, for Headwaters and Osler, our QIPs were developed with the involvement of our communities, through our Community Advisory Councils. Our non-clinical integration has allowed for the cross-sector development of quality improvement goals that will impact our shared patients and provide opportunity to support each other in new ways. As part of our bold, new partnership, we have created a new cross-appointed position, Chief Patient Experience Officer (CPEO), to ensure the patient is at the heart of everything we do and to support our collective focus on being leaders and innovators in the area of patient experience. Through our collective efforts we will create bold, new strategies that transform the patient experience across the hospital and community settings. Our passion for quality and philosophy of continuous quality improvement is greater than ever before and is evidenced by the way in which we are engaging patients and families at all touch points in the health care journey. Accountability Management & Performance Based Compensation Through the Excellent Care for All Act, hospitals in Ontario have a requirement to tie compensation of the Chief Executive Officer (CEO) and other executives to the achievement of performance targets laid out in the QIP. While this same regulatory requirement does not extend to the CCAC sector at present, Central West 9 CCAC believes the linkage between performance and compensation is an important measure of accountability. It is a linkage that the organization has decided to implement in keeping with its firm commitment to being accountable for outcomes, as well establishing yet another means of bringing about closer alignment between the CCAC and its acute care partners, Headwater Health Care Centre and William Osler Health System. The purpose of performance based compensation is: • To drive performance and improve quality of care. • To establish clear performance expectations and expected outcomes. • To ensure consistency in application of the performance incentive, accountability and transparency. • To enable teamwork and a shared purpose. Central West CCAC’s Executive Team Composition and Portion of Compensation Linked to Performance: Members of the Executive Team who report to the CEO have their compensation linked to achieving specific QIP targets as well as other individual performance targets. The amount of compensation that is performancebased for each Vice President is determined as a percentage of that member’s base salary. The performancebased compensation percentages at risk for the 2015/16 fiscal year are set out below: Vice President, Patient Care, Quality and Safety: 3% Joint Vice President, Facilities & Redevelopment: 3% [across a joint portfolio] Joint Vice President, Finance: 3% [across a joint portfolio] Joint Vice President, Human Resources & Organizational Development: 3% [across a joint portfolio] Joint Vice President Information Management & Information Technology: 3% [across a joint portfolio] Joint Vice President, Patient Experience, Communications & Strategy: 3% [across a joint portfolio] Application of Improvement Targets to Individual Executives Targets identified in the QIP form the basis for several performance goals for the leadership team and staff. Vice Presidents will have their performance-based compensation tied to the achievement of three key indicators identified for improvement from within the QIP. Specifically, performance on the following indicators will be the focus for the year: falls for long-stay patients; hospital readmissions within 30 days of discharge and; patient experience. At the conclusion of the 2015/16 QIP period, performance on each of the QIP targets will be evaluated. For the key QIP indicators in the performance model, it will be determined what compensation has been earned based on performance against target. If an executive joins or leaves the organization mid-year, his or her performance-based compensation will be paid following the conclusion of the fiscal year, pro-rated according to the position of the year worked at the CCAC. Accountability Sign-off CW CCAC I have reviewed and approve our organization’s Quality Improvement Plan: Carmine Domanico Board Chair Elizabeth Hull Client Services & Quality Committee Chair Cathy Hecimovich Chief Executive Officer 10
© Copyright 2026