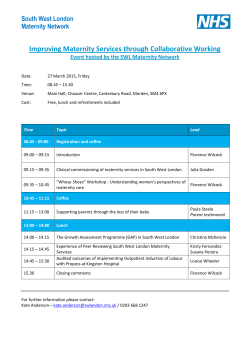
update on the transition of maternity and interrelated services from
North West London Collaboration of Clinical Commissioning Groups UPDATE ON THE TRANSITION OF MATERNITY AND INTERRELATED SERVICES FROM THE EALING HOSPITAL SITE Ealing CCG Governing Body 18th March 2015 Version no: 0.998 CONTENTS 1 BACKGROUND AND DECISIONS TAKEN TO DATE 3 1.1 Decisions taken to date for the transition of maternity and neonatology services 3 1.2 Improving the model of care for residents in North West London 5 1.3 Ealing CCG’s Role in the decision making process 6 2 OVERVIEW OF SYSTEM WIDE ASSURANCE UNDERTAKEN TO DATE 6 2.1 NHS England Led Assurance 7 2.2 North West London CCG Led assurance 7 3 RESOLUTIONS FOR AGREEMENT 9 3.1 Resolutions for agreement on 18th March 2015 9 A DIRECTORY OF APPENDIX MATERIALS 10 1 PURPOSE OF THIS PAPER The purpose of this paper is to: – Summarise the decisions taken to date in relation to the proposed timing of the transition of maternity and interrelated services from Ealing Hospital – Outline the role of Ealing CCG in this ongoing process – Provide an overview of the assurance work undertaken to date in relation to the planning of the transition – Set out for Ealing CCG the initial outputs of the assurance reviews undertaken by NHS England Attached to this paper are a number of Appendices for the consideration of Ealing CCG Governing Body members. 2 1 BACKGROUND AND DECISIONS TAKEN TO DATE 1.1 Decisions taken to date for the transition of maternity and neonatology services 1.1.1 Background to the decision to transition maternity and neonatal services from Ealing hospital The SaHF programme, through its work with hospital doctors, midwives, nurse leaders, providers of community care, volunteer groups and charities, commissioners in North West London developed a set of proposals in 2012 to transform the way healthcare is delivered for local people. Clinical leaders from across NW London proposed changes to create fewer, more comprehensive and better staffed hospitals, able to provide the best quality care throughout the whole week, whilst developing out of hospital services to allow co-ordinated integrated care for people with less severe acute illness and those with chronic conditions. The proposals are aimed at helping NW London meet the challenge of the NHS mandate, save lives and improve clinical outcomes. The NHS in NW London is facing a range of pressures and challenges. From a clinical view, there is increased demand caused by the ageing population and increased prevalence of long term conditions and co-morbidities. There are also unacceptable variations in the quality of care provided, evidenced by higher mortality rates for patients who are treated in hospital at night or during the weekend. Alongside this, there are financial pressures which require the NHS to deliver efficiency savings for reinvestment. As such, doing nothing is not an option. The SaHF Case for Change was developed with clinicians, who looked at the current and future demands on the NHS in NW London, and showed that a new configuration of services was necessary to deliver high quality care within the financial constraints on the system In order to significantly improve the maternity, neonatal and paediatric services provided to women, children and families in NW London, these proposals include the intention to close the maternity, neonatal and paediatrics services currently delivered on the Ealing Hospital site. The full set of proposals were presented to the Joint Committee of Primary Care Trusts (JCPT) in February 2013 with the full recommendations set out in the accompanying Decision Making Business Case. The JCPCT met and agreed as a statutory decision making body to accept the proposals included within the DMBC 1.1.2 IRP Review and Secretary of State Statement to Parliament The agreed changes were referred to the Independent Reconfiguration Panel in 2013 for review. In October 2013, the Secretary of State for Health accepted the Independent Reconfiguration Panel (IRP) recommendations to implement all of the SaHF proposals due to the compelling evidence for how services will be improved. For maternity and neonatal services this included the consolidation of maternity (delivery) and neonatal services from seven sites to six sites (Chelsea and Westminster, Hillingdon, Northwick Park, Queen Charlotte’s, St Mary’s and West Middlesex). For paediatric services, this included the consolidation of paediatric inpatient services from six sites to five sites (Chelsea and Westminster, Hillingdon, Northwick Park, St Mary’s and West Middlesex). While no implementation timeframe was set, there was a clear recommendation that: 3 “Commissioners and providers of acute hospital services across North West London must ensure that changes required to secure safety and quality for patients are made without delay” In his letter to the London Borough of Ealing Health and Adult Social Services Standing Scrutiny Panel, the Secretary of State for Health wrote: “I support the panel’s recommendation that maternity and paediatric inpatient services should be concentrated on the sites identified by Shaping a Healthier Future” 1.1.3 Ealing CCG decision to commence contingency planning In March 2014, Ealing CCG Governing Body made a decision to invest in contingency plans to allow the potential acceleration of transition of maternity services from the Ealing Hospital site. This was in response to concerns raised by Ealing Hospital to the Medical Director of NHS England (London region) highlighting the issue of a reduction in deliveries and the subsequent challenges to sustainability and quality. Ealing CCG Governing Body agreed to meet again to discuss the issue in autumn 2014. It was agreed that a number of factors would need to be considered in detail before a decision on the timing of the maternity transition can be made. These included: Maintenance of clinical quality and access to care – all women and their families have access to a comprehensive range of maternity services which are equitably and appropriately resourced and comply with safeguarding policies and procedures Impact on staff – disruption for Ealing Hospital staff must be kept to a minimum, including impact on training rotas. Alignment with Out of Hospital (OOH) commitments - sufficient capacity should exist in the community to provide care as close to home as possible, where this is clinically appropriate and GPs must be engaged and informed in the development and implementation of any models of care that have an impact on their patients. Financial and operational viability – the transition must be managed as cost effectively as possible, although there will be some double running necessary to ensure a smooth transition. 1.1.4 Ealing CCG Governing Body Decision of 8th October 2014 On 8th October 2014, Ealing CCG Governing Body met in public to discuss the possible next steps in the implementation of these changes. The Governing Body agreed: That there is a need to plan for the transition of maternity and any other necessary, clinically interdependent services from Ealing Hospital as soon as possible, noting that the earliest that any service transition could take place is March 2015 when additional system capacity will be available. To seek the views of the Maternity and Neonatal and Paediatric Project Delivery Boards on the optimum approach to this planning exercise and timing of any change, including those changes which may be required to associated or interdependent clinical services both at Ealing and other hospitals To Seek ‘Delegated Authority’ from any other CCG with a material interest in this change in order to ensure Ealing CCG can progress this work and, whilst addressing their concerns, take any decisions on their behalf as required. 4 1.2 Improving the model of care for residents in North West London 1.2.1 Current model of care and deficiencies arising For the majority of women living in Ealing, the current model of care does not provide continuity of care across the maternity pathway The majority of women who live in Ealing borough choose not to deliver at Ealing Hospital (~60% in 2013/14). These women receive fragmented maternity care, with different parts of the maternity pathway delivered by different providers. There are different acceptance criteria between maternity providers in NWL - most prioritise women from their own ‘host’ CCG boroughs. In addition, there is currently no sector wide Management Information (MI) which results in: Lack of understanding of the proportion of women from NWL that receive their first choice which makes it difficult for the sector to manage capacity appropriately Women book at more than one site in NWL; this makes it difficult for trusts to accurately and effectively plan their services and workload 1.2.2 Proposed model of care and benefits Work has continued on the development of new models of care, such as the proposed approach to delivering services in community settings and the benefits to our local population. For the first time, there will be a consistent sector wide community model with all providers in NWL that aims to improve access, choice and continuity of care for women in NWL. The sector will have a standardised service across the whole area with a common approach to manage the system and common acceptance criteria at each site. This, alongside the development of both midwifery and consultant led community care aims to provide greater access to, choice and continuity of care A summary of the further work on models of care to date is attached to this paper as Appendix A. 1.2.3 Review of the forecast demand and activity flows The modelling document shows that there is sufficient capacity across NWL to meet demand in births across the system and at individual sites. Each trust has confirmed that it is confident that the planned bed and staffing capacity will meet the predicted activity that will transfer from Ealing Hospital. Further, most trusts forecast that they could take further deliveries if needed. A summary of this report is attached to this paper as Appendix B. 1.2.4 Communications and Engagement activities As a part of this work, further consideration will be given to the communications and engagement approach required. More detail on this is included in Appendix D which is attached to this paper. 5 1.3 Ealing CCG’s Role in the decision making process The Joint Committee of Primary Care Trusts which met in February 2013 contained representation from the eight Primary Care Trusts (PCTs) which comprised ‘North West London’ as well as Camden, Richmond and Wandsworth PCTs. Following the implementation of the Health and Social Care Act (2012) the successor Clinical Commissioning Groups (CCGs) covering the same geographical area took responsibility for the implementation of the Shaping a Healthier Future programme. Ealing CCG, as the commissioner with the closest proximity to, and largest volume of patients using, the Ealing Hospital service met on 8th October and requested delegated authority from the other CCGs with a material interest in the proposed transition of services to take all necessary decisions on their behalf to determine the timing of the agreed service changes. All of those CCGs in turn agreed this request and the following table shows the dates on which they made their decisions to delegate. CCG Governing Body Date Agreed Central London CCG 12th November 2014 West London CCG 4th November 2014 Hammersmith & Fulham CCG 11th November 2014 Hounslow CCG 11th November 2014 Brent CCG 26th November 2014 Harrow CCG 24th February 2015 Hillingdon CCG 24th October 2014 Table 1: Delegations received from CCGs in North West London Camden, Wandsworth and Richmond CCGs each reviewed the documentation which was presented to the Ealing CCG Governing Body on 8th October. Following this review, each of them wrote to the Senior Responsible Officer (SRO) of the Shaping a Healthier Future programme to acknowledge the decisions which would be required to effect the proposed transition of services, and in doing so each confirmed that it did not believe it had a material interest in that decision making process. As a result of these letters, no delegations for decision making were requested or required from these CCGs. Ealing Hospital also currently provides a Special Care Unit (SCU) as part of its neonatal service. Following the implementation of the Health and Social Care Act (2012), responsibility for the commissioning of Specialised Services such as this was transferred to NHS England. For the SCU service at Ealing Hospital, NHS England in its role as commissioner for Specialised Services will take its own decision regarding the future of this service at a later date. 6 OVERVIEW OF SYSTEM WIDE ASSURANCE UNDERTAKEN TO DATE 2 To inform the Ealing CCG Governing Body, an extensive array of assurance has been undertaken by NHS organisations. 2.1 NHS England Led Assurance NHS England have undertaken a three stage assurance process. Stage 1: areas for assurance before a decision is made by Ealing Governing Body on the timing of the transition Stage 2: areas for assurance prior to the transition of services Stage 3: areas for assurance in the year following transition of maternity services This process is currently in Stage 1 and the outcome of Stage 1 assurance is summarised in a letter received from NHS England. This letter is attached to this paper as Appendix C. 2.1.1 Further work arising from NHS England led assurance Before a decision can be made on the timing of the transition of maternity services, NHS England seeks further assurance on the following: Confirmation that number of midwives, consultants, sonographers, as set out in the SaHF workforce plan place at each receiving site by the time of transition Director of Operations and Trust Liaison posts filled Estates work at Queen’s Charlotte will be completed in advance of transition Testing of maternity booking system for monitoring booking at Trusts Details of gynaecology emergency model at Ealing Hospital 2.2 North West London CCG Led assurance Following the decision by the NWL CCGs to delegate decision making authority to Ealing CCG Governing Body for the timing of the transition of Ealing maternity services, provider focused assurance reviews have been arranged through December 2014, January 2015 and February 2015. The objective of these reviews has been to provide assurances to CCGs on the clinical and operational planning and preparations Trusts are leading on to support the transition of maternity and neonatal services from Ealing Hospital. The outputs and recommendations from these sessions are expected to be actioned in preparation for decision making and to support the final decision by Ealing CCG around the timing and implementation of the transition of maternity services. The provider focused assurance reviews have been led by the lead commissioner for each Trust in NWL and have comprised of two parts: Part one: An CCG led assurance review session at a private meeting of the CCG Governing Body Part two: A CCG led clinical site visit 7 The reviews commenced in December 2014 and focused on assuring the provider implementation plans for receiving maternity and neonatal activity from Ealing Hospital, rather than assurance on provider readiness to handle the additional activity at that point. All of the provider assurance review sessions have now been completed and the findings are broadly consistent with the work undertaken by NHS England and the TDA. Assurance will continue and a full suite of materials presented to Ealing CCG Governing Body at a future meeting. 2.2.1 Further work arising from CCG led assurance Before a decision can be made on the timing of the transition of maternity services, CCGs seek further assurance on the following: Workforce readiness and recruitment plans Confirmation that the required physical capacity to handle additional maternity and neonatal activity from Ealing will be in place at the point of transition Plans for providing community maternity care within the new geographic boundaries Clinical governance and quality metrics to ensure quality of service is maintained during and after transition 8 3 3.1 RESOLUTIONS FOR AGREEMENT Resolutions for agreement on 18th March 2015 Ealing CCG Governing Body is asked to: (1) NOTE that it has received Delegated Authority from the statutory bodies referenced in Table 1 and is therefore vested with the authority to take decisions on timing with regard to the agreed maternity, paediatric and gynaecology service changes at Ealing Hospital on their behalf. (2) NOTE Appendix B, the document titled "Update on the maternity activity and capacity modelling" (3) NOTE Appendix C, the letter received from NHS England dated 11th March 2015 "Re: NHS England assurance on changes to Ealing maternity services" and the recommendations contained within this letter. (4) NOTE the further assurance work which is recommended to be undertaken as detailed in sections 2.1.1 and 2.2.1 and AGREE this work should be progressed. 9 A DIRECTORY OF APPENDIX MATERIALS Appendix A: Model of care for maternity and neonatal services in NWL Appendix B: Update on the maternity activity and capacity modelling Appendix C: Letter from NHS England Re: NHS England assurance on proposed changes to Ealing maternity services Appendix D: Communications and engagement – update for Ealing CCG: 18th March 2015 10 APPENDIX A Model of care for maternity and neonatal services in NWL 18th March 2015 Background and context Maternity, neonatal and paediatrics will be consolidated across fewer sites in NWL The SaHF programme, led by local clinicians, proposed changes to services in NWL that would provide high quality care through better services for the local population. This included: 1. Consolidation of maternity and neonatal services from seven to six sites to provide comprehensive obstetric and midwife-led delivery care and neonatal care. 2. Consolidation of paediatric inpatient services from six sites to five sites to incorporate paediatric emergency care, inpatients and short stay /ambulatory facilities. The key hospital sites for these services would be Chelsea and Westminster, Hillingdon, Northwick Park, Quuen Charlotte’s and St Mary’s Hospiatls and West Middlesex which will become major hospitals with better services. The Joint Committee of Primary Care Trusts decision was reviewed by the Independent Reconfiguration Panel (IRP) on 13 September 2013, who made the following recommendations relevant to the transition of maternity services: “Commissioners and providers of acute hospital services across north west London must ensure that changes required to secure safety and quality for patients are made without delay.” “Maternity and paediatric inpatient services should be concentrated on the sites identified by Shaping a Healthier Future.” “The NHS’s implementation programme must demonstrate that, before each substantial change, the capacity required will be available and safe transition will be assured.” The Secretary of State accepted the recommendations of the IRP in his statement to Parliament in October 2013. 4 Clinicians and commissioners in NWL are committed to improving the quality and delivery of maternity and neonatal services in NWL through reconfiguration of existing services • The new service configuration for maternity and neonatal care will see birthing units and labour ward activity concentrated across six sites in upgraded facilities, with expectant mothers able to choose between midwife-led or obstetric-led units. • Antenatal and postnatal care will still be provided on the Ealing hospital site as well as in children’s centres, Health centres and GP surgeries in Ealing • • • • Northwick Park The new service configuration will enable choice of the environment in which expectant mothers give birth with all units able to provide higher quality and safer maternity care and improved access to home delivery. The case for consolidating the number of maternity units remains strong as it will enable all Trusts in NWL to provide significantly more consultant-led care than currently, working closer towards the London quality standard for obstetric units to provide 168 hour consultant presence every week. 250 Imperial 1000 800 Ealing Hillingdon In addition, it will enable Trusts to provide more individualised midwifery care through making it easier for maternity units to work towards the standard for 1:30 midwife to birth ratio. 600 350 Chelsea and Westminster Neonatal services will expand on all six sites in NWL. This will West Middlesex provide for a greater number of cots across NWL. At Hillingdon and West Middlesex Hospital seperate consultant rota for paediatrics and neonatal Figure 1: Summary of agreed additional maternity activity services will be implemented providing dedicated cover for neonatal receiving Trusts can handle upon closure of Ealing Hospital services. maternity unit 5 The Secretary of State approved the proposals for reconfiguration of maternity and neonatal services, the SAHF programme are now planning for implementation • The outcome of the Independent Reconfiguration Panel (IRP) in September 2013 supported the proposals for maternity and neonatal services and emphasised that ‘any changes required to secure safety and quality for patients are made without delay’. • The announcement of the Secretary of State on 30 October 2013 committed the programme to proceeding with the changes to maternity services at Ealing Hospital. • On 19th March 2014, Ealing CCG Governing Body made a decision to invest in early implementation of the transition of maternity and neonatal services from Ealing hospital. This was in response to a letter from the medical director of Ealing Hospital to the Medical Director of NHS England outlining the risks associated with the declining birth activity and maintaining safe services. The clinical risks associated with a precipitate unplanned closure prompted this decision. • A Maternity and Neonatal Transition Project was launched in April 2014 to develop plans for each of the receiving trusts in NWL. Planning for implementation is underway and all of the receiving Trusts are implementing plans to accommodate the re-provision of activity from Ealing hospital both in terms of physical and workforce capacity. • The critical path for the implementation plan is based on: ensuring physical and workforce capacity exists at the other receiving Trusts; implementing a revised clinical model to reflect the changes to pathways while protecting antenatal/postnatal care for the women of Ealing; delivering clear and targeted communications with stakeholders and the public and ensuring staff at Ealing transition effectively to receiving Trusts. • The recent decline in bookings and deliveries at Ealing and increased attrition of their maternity staff, make implementation of this plan more urgent. 6 Model of care for maternity and neonatal services in NWL Model of care for maternity services in NWL – key principles In line with recommendations from the Shaping a Healthier Future (SaHF) Maternity and Neonatal Project Delivery Board and national standards and guidance, the core philosophy behind maternity and newborn care in NWL is a localised and normalised pathway. Pregnancy is a normal physiological event and maternity services should be nonmedicalised where possible. Care should be delivered in the community where appropriate, in partnership with GPs and embedded within wider community provision of healthcare, social and emotional support services. Women with more complex medical and/or social or obstetric needs and babies who require neonatal services will have access to specialist services. The clinical assessment criteria for care will be consistent across all maternity services in the sector. Key principles for the maternity services in NWL include: • More choice must be offered to woman over antenatal care, birth setting and postnatal care • More women should be supported to give birth at home or in midwife-led birthing units. • There should be a midwife-led unit alongside every obstetric-led unit. These units are described as ‘alongside midwifery units’ (AMUs). • Women require active 1:1 support from a midwife during active labour, regardless of their chosen place of birth. • The most senior medical staff must be available on site to support high-risk births and women who develop complications during labour with the aim of ultimately achieving cover 24 hours a day, 7 days a week. 8 Model of care for maternity services in NWL - objectives and expected outcomes Objectives To introduce a consistent model of care for maternity and newborn services in NWL to: • improve equity of access • provide care closer to home e.g antenatal care will be provided in the community supported by structured GP involvement (via an agreed shared care arrangement) • offer a choice in ante-natal care, delivery setting and post-natal care. • Improve continuity of care for women throughout their antenatal and postnatal pathway. Expected Outcomes • Women have increased choice of where they receive their antenatal and postnatal care and choice of birth setting. • 90% of pregnant women who are referred by 10 +6 will receive a full medical and social needs assessment with a healthcare professional before the 12th completed week of pregnancy. • Enhanced patient safety and clinical outcomes by ensuring that patients have access to the most skilled and specialist staff when needed 24/7 • Help avoid unnecessary referrals and admissions to hospital or specialist services through offering 24/7 day assessment and triage facilities. • Reduction in inappropriate intervention through development of Alongside Midwifery Led Units • Improve patient experience and satisfaction • Modernise services in line with new and developing technologies and evidence. 9 Implementation of SaHF maternity proposals will enable the following clinical and quality benefits can be expected Workforce • Overall improvement in midwifery to birth ratios across all five Trusts in NWL, following transition, with improvement as a sector reaching the target of 1:30 overall (from 1:32 in 2014/15) and an additional 105 midwives being recruited across the sector. • Overall improvement in consultant hours on labour ward across all five trusts in NWL from an average of 101 hours in 2014/15 to 126 hours in 2015/16 (an additional 12 WTE consultants) and on a trajectory towards 168hrs by 2017/18. • Better alignment between numbers of medical trainees and overall delivery activity to address historical misalignment Collaborative working across NWL Model of care • Improved community model of care for women – for the first time a consistent model of care will be implemented across NWL. This will also enable standardised development of the which creates greater resilience to build and develop the home birth service across offer in NWL • More women will have a named midwife that provides their antenatal and postnatal care across NWL • Improved continuity of care across the whole pathway as providers extend their community midwifery boundaries and offer to women • Increase in midwifery led services, with all six maternity units providing alongside midwifery led births options • Increased awareness of choice across NWL and improved compliance for 12+6 week bookings target • Facilitates the creation of sector wide posts for perinatal mental health, domestic violence and safeguarding Physical estates and infrastructure • Facilitates sector approach to community breastfeeding support. NWL aims to be one of the first sectors to achieve sector wide accreditation in • Improved maternity and neonatal estates for women in NWL as a Breastfeeding Initiative. result of the reconfiguration. All units in NWL now have Midwifery • Development of sector wide model for transitional care, with a sector Led Unit and Transitional Care beds. approach to multi-disciplinary education, aiming to reduce the number of babies separated from mothers • Facilitates a sector wide review of community obstetric provision supported by consultants and providers – Northwick park and Hillingdon already have plans to run this model out of the Ealing hospital site following transition and following an evaluation of the success this may be extended to all providers in the future • Partnership working with GPs and CCGs to improve maternity referral patterns across NWL 10 Model of care for maternity services in NWL – summary of pathway Choice Access Early pregnancy Continuity of care Antenatal Delivery Postnatal Choice from six maternity providers, supported via advice from GPs, providers and a maternity booking service in NWL Choice of setting with more care close to home (children’s centres, health centre's, GP surgeries, community hubs) Choice of birth setting – home, midwifery led or obstetric led Choice of setting - care either in home or close to home in community settings Early access to maternity services by 12+6 weeks Shared care between GP/Midwives/Obstetrician as appropriate Access to translation, interpreting and advocacy services based on an assessment of need Access to advice and support on lifestyle, breastfeeding, diet, diagnostics etc Triage, treat and transfer protocols to avoid unnecessary admissions Access to 24/7 Day Assessment, early pregnancy and emergency gynaecology services for women should problems occur 1:1 Midwifery care in established labour Increase in midwife to birth ratios in line with Birthrate Plus recommendations (target 1 Midwife to 30 births) Increase consultant obstetric presence on the delivery ward (target for 168hrs presence) A model of Transitional Care for babies Clear handover protocols and communication with identified healthcare professional for the transition to parenthood Enhanced children's safeguarding through development of provider:borough protocols Neonatal All babies needing on-going neonatal care have rapid access to the appropriate level of care as close to home as possible. Key elements include: • A specialist neonatal transport service • Established care pathways that allow mothers and babies to access rapidly a unit offering the appropriate level of neonatal care • Adequate assessment of need and provision of appropriate capacity 11 The proposed model of care for promotes access, choice and continuity of care for Ealing women Women Receiving Trusts • Can choose their delivery unit from six maternity providers in NWL • Will extend their current community boundaries to ensure the majority of maternity care can be provided locally • Can choose the location for their antenatal and postnatal care - either at Ealing Hospital, one of the children's centres, health centre’s, their local GP clinic for GP appointments or their host provider site in NWL • Will offer women a choice of where to receive their antenatal and postnatal care depending on ongoing assessment of their clinical/social risk and needs. • Will work out of the Ealing Hospital site and Ealing Children's Centres/health centres to deliver: • will need to travel to their host provider site for scanning appointments for their two scans (the first scan will be combined with their first visit to the unit) • Antenatal care (including booking appointment & phlebotomy) • requiring specialist antenatal care may need to travel to their host provider or will receive care locally at the Ealing hospital site • Breastfeeding clinics • Hillingdon and London North West Healthcare Trust will offer consultant led antenatal clinics from the Ealing Hospital site. • will still be able to access the Early Pregnancy Assessment Unit at Ealing Hospital Trust • Will offer scanning services at the host provider site (the first scan to be combined with first visit). • Will be able to stay with their babies if they require transitional care • Will continue effective local services where appropriate e.g. diabetes clinic • Postnatal care • Parent education classes 12 Proposed changes to community maternity services in NWL Context and executive summary The purpose of this paper is for Ealing CCG to review and agree the plans for community maternity services in NWL. Proposed antenatal and postnatal catchment areas in and around Ealing borough This paper outlines: • The current and proposed model • The benefits of the proposed model • Examples of patient stories The proposed changes to community maternity services were codeveloped by the SaHF Maternity & Neonatal Project Delivery Board and NWL commissioners. They have been endorsed by SaHF Clinical Board and SaHF Programme Board. Northwick Park Hillingdon Hospital St Mary’s It should be noted that the proposed NWL community model is highly flexible and can be adapted and enhanced over time as patterns of activity for women in NWL emerge. This will be regularly monitored via data received by the Maternity Booking Service and feedback from patients and individual Trusts on demand for community services. Chelsea & Westminster West Middlesex Alongside this, there will be a detailed review undertaken within three months of the transfer of Ealing Hospital’s maternity services to develop an enhanced community model The proposed changes aim to benefit most Ealing women, by increasing women's awareness of the choices they have for maternity provider and where they receive their care., It also aims to improve continuity of care along their maternity pathway Queen Charlotte’s Ealing Hospital London North West Chelsea & Westminster Imperial Hillingdon London North West/Imperial West Middlesex The new community model of care will be implemented in phases: • Phase 1 – Testing community model for operational readiness • Phase 2 - Implement transitional community model ( transfer existing Ealing community model of care to receiving units) • Phase 3 - Review transition model • Phase 4 – Ongoing performance improvement 14 S M The current model Current postnatal catchment areas in and around Ealing borough For the majority of women living in Ealing, the current model of care does not provide continuity of care across the maternity pathway Northwick Park The majority of women who live in Ealing borough choose not to deliver at Ealing Hospital (~60% in 2013/14). These women receive fragmented maternity care, with different parts of the maternity pathway delivered by different providers. For example: • For example, both Hillingdon and Imperial offer ante-natal and delivery services to Ealing women, but post-natal treatment for these women is always delivered by Ealing Hospital. Hillingdon Hospital • For women choosing other sites, such as West Middlesex,, Northwick Park and Chelsea & Westminster ,their ante-natal care and delivery care is delivered at the host provider site and there is no option for care delivered locally St Mary’s Queen Charlotte’s Ealing Hospital • Women in Ealing who currently choose another NWL maternity provider, may not get into their chosen units due to preferential treatment for women from their host CCG boroughs (this is currently the case for Ealing women choosing QCCH) Chelsea & Westminster West Middlesex • The majority of women in the Kilburn area of Brent currently choose Imperial and therefore receive their antenatal and delivery care from Imperial but their postnatal care from London North West Healthcare London North West Hillingdon Imperial West Middlesex There are different acceptance criteria between maternity providers in NWL - most prioritise women from their own ‘host’ CCG boroughs London North West/Imperial Ealing Chelsea & Westminster Ealing borough There is currently no sector wide Management Information (MI) which results in: • Lack of understanding of the proportion of women from NWL that receive their first choice which makes it difficult for the sector to manage capacity appropriately • Women book at more than one site in NWL; this makes it difficult for trusts to accurately and effectively plan their services and workload Women’s stories – what currently happens… • Currently, a women booking at Ealing Hospital receives all her care from Ealing Hospital, either at the hospital or at one of the children’s centres/health centres in the community • If a women from Ealing chooses West Middlesex for delivery, she will have all of her antenatal and delivery care at the West Middlesex hospital and her postnatal care will be delivered by Ealing. There is limited choice over where women access their care. 15 S M The future model For the first time, there will be a consistent sector wide community model with all providers in NWL that aims to improve access, choice and continuity of care for women in NWL NWL’s providers, through the Maternity Network and Maternity & Neonatal Project Delivery Board have collaborated on the development of a new community transitional model There are two key aspects of the model of care which will change: 1. Expansion of catchment areas for all trusts delivering maternity services • Receiving trusts’ midwifery teams will offer care in the new community as per the catchment areas map on the right • Receiving Trusts will utilise the Ealing Hospital site, Children Centres (CC) and Health Centres (HC) in Ealing to provide routine antenatal and postnatal care. • Hillingdon will also provide obstetric appointments at the Ealing site • Chelsea and Westminster will offer routine antenatal and postnatal care in Chiswick (currently an Imperial catchment area) enabling Imperial to expand further into Ealing. If demand requires, then Chelsea & Westminster can expand further into Ealing in the future 2. Common framework across all trusts in NWL • The Maternity Booking Service in NWL will give sector wide MI, enabling joint decisions across the system on demand, capacity and service improvement • Acceptance criteria will be the same for all women (prioritised as below) 1) Women from the Trusts local community area (as defined in figure in the previous slide) 2) Women with medical or social need 3) Women that have previously given birth at the hospital 4) Women in NW London 5) All other women Proposed antenatal and postnatal catchment areas in and around Ealing borough Northwick Park Hillingdon Hospital St Mary’s Queen Charlotte’s Ealing Hospital Chelsea & Westminster West Middlesex London North West Chelsea & Westminster Imperial Hillingdon London North West/Imperial West Middlesex Women’s stories – what will happen in the future… • If a woman living in the blue (West Midd) area of Ealing chooses Queen Charlotte's, she has the option to have her antenatal care at Ealing Hospital, a children's centre in the red Imperial area or Queen Charlotte's site if she requires specialist input or a scan. She can receive her post natal care from either Queen Charlotte's (at Ealing Hospital or a children's centre) or from West Middlesex (either in her home or a local children's centre in the blue area.) • If she chooses West Middlesex, she will receive the full pathway from West Middlesex, choosing between at home, locally at a children's centre or at Ealing hospital or at West Middlesex Hospital itself. 16 S M Detailed description of the changes in Ealing borough Services to be provided at HC and CC will mirror (or be enhanced from ) existing service provision (session/days) Overview of service changes by Trust and site: Proposed antenatal and postnatal catchment areas in and around Ealing borough Northwick Park Petts Hill CC West Middlesex University Hospital (WMUH)Trust: • Featherstone Road HC (Midwife led AN, PN care) • Ealing hub (Midwife led AN, PN care) • Scans at WMUH site (combined with first visit) • WMUH will review need for Borough consultant-led clinics following implementation Horsenden Lane CC Islip Manor CC Perivale CC Grand Union Village HC Jubilee Gardens HC Southall Broadway HC Featherstone Road HC Hathaway CC Mattock Lane HC Ealing Hospital Maples CC Log Cabin CC Ealing Hub (Obstetric-led AN care, diabetes clinic) • Scans at Hillingdon and Ealing hub (high risk women only), use of phlebotomy services at Ealing hub for obstetric –led clinics West Middlesex London North West Imperial College Hospital Trust (ICHT): Acton Park CC Queen Charlotte’s Grange CC South Acton CC Islip Manor CC, Southall Broadway HC, Jubilee Gardens HC, Grand Union Village HC (Midwife led AN, PN care) • St Mary’s John Perryn CC Laurel Gardens CC The Hillingdon Hospital Foundation Trust (THHFT): • West Twyford CC Windmill Lane CC Hillingdon Hospital Imperial Chelsea & Westminster Duke Meadows CC Chelsea & Westminster Hillingdon West Middlesex Sites for community care • Windmill Lane CC,(shared with London North West Hospital Trust (LNWHT)), Laurel Gardens CC, Grange CC, Mattock Lane CC (Midwife led AN, PN care, Parent education) • Hathaway CC, Log Cabin CC, (Midwife led AN, PN care) London North West Hospital Trust (LNWHT): • Ealing Hub (Midwife led AN, PN care) • • Existing service provision out of Ealing centres will remain (Acton Park CC, John Perryn CC, Maples CC, South Acton CC and West Twyford CC) Horsenden Lane CC, Perivale CC, Petts Hill CC, Windmill Lane CC (shared with ICHT) (Midwife-led AN, PN care) • Ealing Hub (Midwife-led AN, PN care, Obstetric-led AN care) • Scans at Northwick Park or Ealing Hospital sites • Scans at Queen Charlottes and St Marys (combined with first visit) ICHT will provide obstetric-led care at hospital sites above and will review need for Borough consultant-led clinics following implementation London North West/Imperial 17 S M Detailed description of the changes outside Ealing borough Alongside the expansion of community maternity services in Ealing borough, two community boundaries outside of Ealing are being modified. These were developed as part of a wider review of the maternity community model across NWL. This was an opportunity to redefine historical boundaries across NWL and better align to current and future referral patterns. Both proposed boundary changes are in areas where there is already a strong referral pattern to the proposed new provider. Increasing bookings to the new provider will be facilitated through the offer of full continuity of care to women in those areas and targeted GP engagement. Brent – reallocates area from Northwick Park to St Marys • After the publication of Northwick Park’s CQC report, commissioners decided to limit the flow of births from Ealing at Northwick Park to 250 births (as discussed at the Clinical Board on the 4th December 2014)* Proposed antenatal and postnatal catchment areas in and around Ealing borough Northwick Park Petts Hill CC Horsenden Lane CC Islip Manor CC Perivale CC Grand Union Village HC Jubilee Gardens HC Southall Broadway HC Featherstone Road HC Hathaway CC Mattock Lane HC Ealing Hospital Maples CC Log Cabin CC Acton Park CC Queen Charlotte’s Grange CC West Middlesex London North West Imperial Chiswick – reallocates area from Queen Charlotte’s to Chelsea & Westminster Hospital St Mary’s John Perryn CC Laurel Gardens CC • The Maternity Project Delivery Board (PDB) decided to use this opportunity to redress historic boundaries as part of a wider review of community maternity model in NWL • Parts of Brent (specific parts of NW2, NW6 and NW10) were considered as appropriate for the transfer due to existing referral patterns. Across the specific postcodes, over 70% of women already choose ICHT. The intention, post implementation, is that this rises to 80% West Twyford CC Windmill Lane CC Hillingdon Hospital London North West/Imperial South Acton CC Chelsea & Westminster Duke Meadows CC Chelsea & Westminster Hillingdon West Middlesex Sites for community care • Chelsea and Westminster’s expansion of its MLU and Labour Ward has increased their capacity by 1,000 births. Due to its location with respect to Ealing and other Ealing sites, the forecast demand at Chelsea & Westminster from Ealing has been far lower than their capacity to absorb additional births • To spread the Ealing births across NWL’s providers, the Maternity PDB looked to increase the activity to Chelsea & Westminster through the redrawing of community maternity service boundaries outside of Ealing • Parts of Chiswick were considered as appropriate for the transfer due, through discussion with CCGs. Across the postcodes, women currently choose approximately 50% Queen Charlotte’s and 50% Chelsea & Westminster; after the implementation, we intend for this to be approximately 25% Queen Charlotte’s and 75% Chelsea & Westminster * It should be noted that it was felt that no action was necessary after the publication of Hillingdon’s CQC because their report did not highlight anything ‘Inadequate” (red in the report) and the key concerns raised related to the poor estate, which is being addressed as part of the planned refurbishment to support the transition 18 S M Benefits of the proposed community model For the first time, North West London will have a standardised service across the whole sector with common MI to manage the system and common acceptance criteria at each site This, alongside the development of both midwifery and consultant led community care aims to provide greater access to, choice and continuity of care Current Future Women in Ealing who choose to deliver at another hospital in NWL (~60% in 13/14) can’t access their antenatal care locally • Ealing women currently have variable continuity of care across the antenatal & postnatal pathway • Women will experience improved continuity of care as a result of NWL units providing antenatal and postnatal care in Ealing Hospital and children’s centres in the Ealing borough Queen Charlotte’s currently cannot accommodate Ealing demand and are turning Ealing women away • Queen Charlotte’s will be able to accommodate more women from Ealing due to the expansion of its maternity unit on both the QCCH and SMH sites Units, including Queen Charlotte’s, will treat women from Ealing the same as women that live in their host CCG borough, thereby increasing the number of women from Ealing able to access their first choice provider • • Women will be able to choose to have their antenatal care at Children’s centres, Health centres in Ealing, Ealing Hospital, community venues in their chosen providers borough or on the hospital site of their chosen provider. Those choosing Hillingdon or LNWHT will be able to access consultant led antenatal care from the Ealing hospital site To explain to GPs how the new system will operate, example patient journeys have been developed to describe the continuity care aspect of the proposed community model. These are documented in the following pages. Simplified patient journeys and explanations that can be used with women are in development to help explain how the new community model will operate. 19 Patient story 1: Cynthia, Northolt, Standard pathway Cynthia is 26 years old and lives in Northolt (UB5). She is having her first child and she has no underlying health condition. Cynthia’s pregnancy is considered to be on the standard care pathway (low risk). Cynthia has various options for her maternity care. Two are explored below. Choosing a unit Booking After considering advice from her GP, Cynthia chooses Northwick Park as her first choice. Because she lives within London North West Healthcare Trusts (LNWHT’s) new catchment area, she is accepted to the unit (under 1st admission criteria) Cynthia meets her named midwife at Pett’s Hill Children’s Centre (nearest LNWHT site to her home). The midwife undertakes Cynthia’s booking appointment and will be her point of contact for her care going forward After discussions with friends who live nearby, Cynthia decides to have her baby at Hillingdon Hospital. Although she is not within Hillingdon Hospital Trust (THHFT’s) new catchment, she is accepted under the 4th admission criteria (women within NWL) Cynthia meets her named midwife at Islip Manor Children’s Centre (nearest Hillingdon site to her home). The midwife undertakes Cynthia’s booking appointment and will be her point of contact for her care going forward Cynthia’s receives her antenatal care at Islip Manor Children’s Centre by the Hillingdon midwifery team Antenatal care Cynthia’s receives her antenatal care at Pett’s Hill Children’s Centre by the LNWHT midwifery team Antenatal care ultrasound scan Cynthia goes to Ealing Hospital for her ultrasound scans (1012 weeks and 20 weeks) as it is on a direct bus route (282) from her home. Cynthia goes to Hillingdon Hospital for her ultrasound scans, the first one of which is combined with a tour of the unit Cynthia has her baby at Northwick Park’s maternity unit Cynthia has her baby at Hillingdon Hospital Delivery Postnatal care Cynthia is visited by a midwife from LNWHT midwifery team at her home for postnatal follow up Cynthia is visited by a midwife from LNWHT midwifery team at her home for Postnatal follow up 20 Patient story 2: Amal, Southall, Intermediate pathway Amal is 33 year old Somali woman who lives in Southall (UB1). She recently moved to Southall from another part of the UK and has type 2 diabetes. Amal is pregnant with her second child and her pregnancy is considered to be on an intermediate care pathway (medium risk). Amal has various options for her maternity care. Two are explored below. Choosing a unit After conversations with her GP, Amal decides on Hillingdon as her first choice. Amal lives in Hillingdon’s new catchment area so is accepted by the unit (under 1st criteria) After discussions with her GP and friends who have recently had children, Amal chooses St Mary’s Hospital. There is availability so Amal is accepted under 4th admission criteria (women in NWL). Booking Amal meets her named Hillingdon midwife at Southall Broadway Healthcare centre (nearest Hillingdon site to her home) The midwife undertakes Amal’s booking appointment and will be her point of contact for her care going forward Amal meets her named Imperial midwife at the Ealing Hospital Hub (nearest Imperial site to her home). The midwife undertakes Amal’s booking appointment and will be her point of contact for her care going forward Antenatal care Amal receives her Antenatal care at Southall Broadway Healthcare Centre. The midwife also provides intermediate diabetes care. Amal receives her antenatal care at the Ealing Hospital Hub. The midwife also provides intermediate diabetes care Amal goes to Hillingdon Hospital for her ultrasound scans (1012 weeks and 20 weeks) Amal goes to St Mary’s Hospital for her ultrasound scans (1012 weeks and 20 weeks) Amal has her baby at Hillingdon Hospital Amal has her baby at St Mary’s hospital Amal is visited by a midwife from Hillingdon team at her home for postnatal follow up Amal is able to request a Postnatal follow up by Imperial midwifery team at the Ealing Hub or by the Hillingdon midwifery team at her own home Antenatal care ultrasound scan Delivery Postnatal care 21 Patient story 3: Jackie, Greenford, Intermediate pathway Jackie is a 22 year old woman who lives in Greenford (UB6). She is expecting her first child. She has previous history of substance/alcohol misuse. Jackie’s pregnancy is considered to be on the intermediate care pathway (medium risk). Jackie has various options for her maternity care. Two are explored below. Choosing a unit Jackie’s GP refers her to Northwick Park for delivery. Due to capacity restraints, Jackie is unable to book her delivery at the site. Jackie is contacted by the Maternity Booking Service and decides to choose Queen Charlotte’s as she can obtain care locally and is likely to see continuity of care across the pathway. As she lives in Imperial Trusts catchment area, she is accepted into Queen Charlotte’s (under 1st admission criteria) Jackie’s GP refers her to Northwick Park for delivery. As she lives in London North West Healthcare Trust (LNWHT) catchment area, she is accepted into Northwick Park (under 1st admission criteria) Booking Jackie undertakes her booking appointment at Windmill Lane Children’s centre by a named midwife from the Imperial team Jackie undertakes her booking appointment at Windmill Lane Children’s centre by a named midwife from the LNWHT team Antenatal care Jackie receives all of her antenatal care at the Windmill Lane Children’s Centre by her named Imperial midwife Jackie receives all of her antenatal care at the Windmill Lane Children’s Centre by her named LNWHT midwife Jackie attends Queen Charlotte’s Hospital site for her ultrasound scans (10-12 weeks and 20 weeks) Jackie attends Ealing Hospital site for her ultrasound scans (10-12 weeks and 20 weeks) as it is closer to her home (number 92/282 bus) Jackie has her baby at Queen Charlotte’s maternity unit Jackie has her baby at Northwick Park maternity unit Jackie is visited by a midwife from Imperial midwifery team at her home for postnatal follow up Jackie is visited by a midwife from LNWHT midwifery team at her home for postnatal follow up Antenatal care ultrasound scan Delivery Postnatal care 22 Patient story 4: Priya, Southall, Intensive pathway Priya is a 30 year old Asian woman who lives in Southall (UB2). She is expecting her third child. She has high blood pressure and developed pre-eclampsia in a previous pregnancy. Priya’s pregnancy is considered to be on the intensive care pathway (high risk and therefore requires specialist medical input). Priya has various options for her maternity care. Two are explored below. Priya decides on West Middlesex (WMUH) as her first choice of delivery site as closest to her home. As she lives in WMUH’s catchment area, she is accepted into WMUH (under 1st admission criteria) Priya decides on Hillingdon as her first choice of delivery site. She is accepted to Hillingdon under the 2nd criteria (medical or vulnerable need) Priya undertakes her booking appointment at the West Middlesex Hospital site with an obstetrician. Priya undertakes her booking appointment at the Ealing Hospital site with an Hillingdon obstetrician. Antenatal care As Priya is on the intensive care pathway, she receives all of her antenatal care within the West Middlesex Hospital setting, by an obstetrician (takes bus route 195/267, approx. 30 mins) As Priya is on the intensive care pathway, she receives all of her antenatal care within the Ealing Hospital setting, by a Hillingdon consultant obstetrician Antenatal care ultrasound scan Priya attends West Middlesex Hospital site for her ultrasound scans (10-12 weeks and 20 weeks, plus any additional scans) Priya attends Ealing Hospital site for her ultrasound scans (1012 weeks and 20 weeks, plus any additional scans) Priya has her baby at West Middlesex’s maternity unit Priya has her baby at Hillingdon maternity unit Priya is visited by a midwife from West Middlesex midwifery team at her home for postnatal follow up Priya is visited by a midwife from West Middlesex midwifery team at her home for postnatal follow up Choosing a unit Booking Delivery Postnatal care 23 APPENDIX B Update on the maternity activity and capacity modelling 9th March 2015 Context and purpose of this document The purpose of this document is to explain the capacity modelling that has been undertaken to test how maternity activity currently delivered at Ealing can be absorbed at other sites. NWL Clinicians developed the Bed Model and Ealing Allocation Model. These have been stress tested and subjected to external review which highlighted a number of areas that require further clarification. This document provides final updated analysis. We have stress tested trust capacity plans using the Bed Model developed by the NWL Maternity Network and we have used headroom analysis to understand the potential impact on women’s choice. The development of this document provides an opportunity to update three aspects of the assumptions in the modelling: • Since the original modelling, we now have additional data of actual deliveries in 2014/15. This have been used to create a forecast for 2014/15. • A potential capacity concern at Hillingdon Hospital was discussed at the SaHF Implementation Programme Board on the 29th January 2015 and 2 postnatal beds have been added into Hillingdon’s plans for 2015/16 to address these capacity concerns • The trusts have been asked to confirm their maximum capacity in terms of births (based on their own internal trust estimates of capacity) Key Messages Each trust has confirmed that it is confident that the planned bed and staffing capacity will meet the predicted activity that will transfer from Ealing Hospital. Further, most trusts forecast that they could take further deliveries if needed. 3 Executive summary (1 of 2) Context • The Bed Model used by SaHF was originally built to give a highly cautious recommended number of beds. Alongside this, flexible bed usage in practice allows units to flex their capacity further than the model suggests • The Ealing Allocation Model estimates how Ealing Hospital’s deliveries will split between the receiving sites across NWL by trying to understand the impact of different drivers of women’s choice of unit • Birth rates across NWL have declined each year since 2011/12, with this trend continuing in 2014/15. The predicted outturn for 2014/15 is 29,297 births (270 births below 2013/14) • The number of beds since 2011/12 has increased slightly and in 2015/16, trusts are planning on having exactly the same total number of beds as 2013/14 at 423 beds • North West London managed in 2011/12 to deliver a higher number of births than we are estimating for any scenario for 2015/16 with fewer beds than the planned bed base in 2015/16. • Benchmarking (see right) suggests that there are units across the country who are managing with fewer beds per 1000 births than is proposed in any 2015/16 Scenario for NWL Scenarios used for stress testing the model • Two scenarios of the number of deliveries at NWL sites are used to stress test the model. They are: – Scenario 1 – 29,297 births (the same number of births as predicted outturn for 2014/15). This is based on the ONS prediction of no growth – Scenario 2 – 30,565 births (predicted outturn for 2014/15 + 4.3%). This includes an allowance of 3,000 births for Ealing Hospital, which is 15% above the forecast outturn for 2014/15 plus the planning assumptions used by trusts. • These two Scenarios are tested with the different possible Allocations of Ealing’s births NWL historic beds to births ratio beds/1000 births NWL 2013/14 14.3 NWL 2012/13 13.8 NWL 2011/12 13.3 NWL 2015/16 scenarios against other units nationally beds/1000 births Wythenshaw (S Manchester) 15.8 Bolton 15.5 Birmingham Women's 15.4 NWL 15/16 (Scenario 1) 14.4 Royal Free 14.3 NWL 15/16 (Scenario 2) 13.8 Liverpool Women's 13.4 St George's 13.2 North Middlesex 12.8 Guy's & St Thomas' 12.7 Barnet 11.8 4 Executive summary (2 of 2) Stress testing bed plans • Stress testing each scenario, the NWL system has sufficient capacity using all allocations of Ealing’s deliveries – Scenario 1 base case – there is a surplus of 24-27 beds across NWL compared to the bed model recommendations (equivalent of 1,890 – 2,120 births) – Scenario 2 high growth case – there is a surplus of 3-11 beds across NWL compared to the bed model recommendations (equivalent of 270 – 870 births) • • • are flexible. A surplus of DAU beds allows the trust to flex antenatal beds and Hillingdon is able to transfer women in maternity HDU to our main hospital HDU ward. Under permutations of the Scenarios and Allocations of Ealing Hospital’s births, Chelsea & Westminster and Hillingdon are planning on having fewer beds than the bed model recommends, but both trusts have historically been more efficient than the number the bed model recommends Chelsea & Westminster has 6-7 fewer beds than the bed model recommends. The main contributor is having 6 fewer transitional care beds than the bed model recommends. Chelsea & Westminster operates a different transitional care model to other trusts. Postnatal beds are used flexibly with transitional care beds, enabling beds to be flexed based on need. Since the opening of the Midwifery Led Unit, there has been increased capacity in beds across intra partum and postnatal and the trust has more recovery beds which relieve pressure from the postnatal ward. Transitional care is supported by nursery nurse lead on the postnatal ward. There will be additional capacity for transitional care on the neonatal unit which will be co-located with the postnatal ward as part of the planned expansion of the neonatal unit. The trust has also secured funding to expand the neonatal unit and add additional cots if required during 2015/16. This will allow for shared workforce, more efficient working between the two areas, and promote mother and baby early bonding by not separating them. As a result, the trust have confirmed that they are able to manage with their bed base Under Scenario 2, Hillingdon’s planned number of beds is 3-5 beds fewer than the number the bed model recommends. Hillingdon has the physical space for 4 additional antenatal beds on its antenatal ward or overflow ward if required. Alongside this, the site has an additional labour ward room that can be used flexibly with MLU and its bereavement, recovery and HDU beds Headroom and women’s choice • Most trusts are able to take more births than they are planning for 2015/16 • Under Scenario 1, with most allocations of Ealing’s births including those with strongest weighting, all trusts have sufficient capacity to serve the women who choose them • Under Scenario 2, there are permutations in which trusts potentially do not have the capacity to serve the women who choose them. These women, however, can be accommodated at other sites in NWL • In the allocations with the strongest weightings, at least 99% of NWL women receive their first choice of unit. In the worst case allocation under Scenario 2, 2.4% of NWL women do not receive their first choice, driven by a shortage at West Middlesex. This allocation (women who deliver at Ealing Hospital chose to deliver at the unit closest to their GP’s surgery) is not seen as likely by NWL clinicians (reflected in the Clinical Board weighting of allocations). Maternity Booking Service • Maternity is a planned service and the Maternity Booking Service being introduced across NWL will track deliveries and bookings across NWL, enable the system to manage excess demand for any particular site in NWL and enable specific sites and the wider system to respond early to changes in demand Additional • There is additional physical capacity in neonatal cots being developed and, while neonatal staffing remains an issue for NWL and the nation as a whole, each of the units are improving their neonatal staffing following the transition so will be better positioned than currently • Trusts have developed detailed workforce and recruitment plans for 2015/16 that are being monitored by the programme as part of the assurance process 5 Context and modelling methodology Historic and planned capacity for maternity and neonatal services The table below shows that compared to 2011/12, when units experienced a peak in birth activity yet managed their maternity services, NWL is planning to have more beds to handle fewer deliveries forecast in 2015/16. Deliveries Beds Neonatal cots 2011/12 2012/13 2013/14 2014/15 2015/16 31,600 30,700 29,600 419 423 423 432 423 - - 158 158 165 29,300* 29,300** * Predicted outturn for 2014/15 based on 8 months of data ** Forecast for 2015/16 applying ONS growth forecast 7 The modelling approach considers the system capacity in terms of both births and beds Different demand scenarios are tested against the maximum number of births that trusts can take to understand the headroom at each trust and the impact on women’s choice Demand in births for NWL sites Scenarios for births across NWL + Different ways of allocating Ealing’s births to receiving trusts Different permutations of Scenarios and Allocations give a distribution of births across NWL sites The Bed Model recommends a number of inpatient beds, by type, for each site under different permutations. These are tested against the planned number of beds at each site in 2015/16 Recommended number of beds for each site Different permutations of Scenarios and Allocations give a distribution of births across NWL sites Recommended number of beds for each site under each permutation This uses the Ealing Allocation Model developed by NWL Clinicians, which uses six different ways (allocations) of understanding where the women currently choosing Ealing Hospital may choose to go, based on historic activity, proximity to sites, GP referrals, and women’s preferences. This uses the Bed Model which was developed by the NWL Maternity Network, using best practice sources including Safer Childbirth (RCM) and Royal Colleges guidance. It recommends a number of inpatient beds for each site depending on acuity and the number of births it is expected to receive. Alongside this, different Scenarios for total numbers of births across NWL sites are tested. Each permutation of Scenarios and Allocations gives a distribution of births across receiving NWL sites. For each permutation of Scenarios and Allocations, the Bed Model recommends a number of beds for each site, by type of bed. Headroom and first choice analysis is conducted by comparing the number of births sites are allocated in each permutation of Scenarios and Allocations by the Ealing Allocation Model with the maximum number of births that each site can accommodate Bed numbers are stress tested by comparing the number the Bed Model recommends under each permutation of Scenarios and Allocations with the planned number of beds for 2015/16 Maximum number of births that each site can accommodate The planned number of beds at each site for 2015/16 Scenarios – the overall demand Scenarios for NWL births that have been used Allocations – the different ways of understanding where the women currently choosing Ealing Hospital may choose to go 8 The Bed Model developed by SaHF provides generous capacity The NWL bed model was developed by the NWL Maternity Network, using best practice sources including Safer Childbirth (RCM) and Royal Colleges guidance. The result is a recommended inpatient bed model for a 6000 birth unit, dependent on the acuity of the unit: Unit acuity Level 1 Level 2 Level 3 Triage/ OPD induction 6 4 6 4 6 4 Mid-wifery Led Unit DAU Ante-natal 4 4 4 15 18 20 Labour ward 11 11 12 Bereavement 2 2 2 Theatres 2 2 2 HDU Recovery Post-natal 2 2 2 4 4 4 27 28 29 Transitional Care 6 6 6 Total beds 73 77 81 There are various factors which contribute to the bed model recommending more beds than sites need Model reviewed and signed off by The model was deliberately built to be highly cautious in its recommended number of beds for sites and therefore • Heads of Midwifery provides an overestimate of the required capacity at sites: across NWL • The bed model rounds up the required number of resources. Therefore, for a unit delivering 3000 births, the bed • Maternity Network model recommends 1 theatre, but for a unit delivering 3001 births, the bed model recommends 2 theatres (because it rounds 1.0003 up to 2). • Maternity & Neonatal Project Delivery • Beds are used flexibly in practice, based on adjacency and trust operating models but this is not reflected in the Board model • The model does not factor in site efficiency (beds to births ratios or length or stay), so those sites which are more • SaHF Clinical Board efficient potentially have fewer beds than the bed model recommends • SaHF Programme Board • A very low level of home births is assumed and units are proactively encouraging women to chose home births so this is expected to rise • There are various types of beds which have been catered for in the model which are unlikely to be used in practice in the same numbers. This is shown most clearly with bereavement beds. Currently, all receiving sites apart from Northwick Park have 1 bereavement bed. Northwick Park use a labour ward room suitable for bereavement. If an additional bereavement room are needed, then trusts use a appropriate delivery room • Labour ward beds are the least flexible beds and therefore the model builds in occupancy at just 60% to allow for surge. 9 Clinicians developed an Ealing Allocation Model to estimate how Ealing Hospital’s deliveries will split between receiving sites in NWL The Ealing Allocation Model uses six different ways (allocations) of understanding where the women currently choosing Ealing Hospital may choose to go, based on historic activity, proximity to sites, GP preferences, and women’s preferences. NWL clinicians (SaHF Clinical Board) agreed a weighting of these based on confidence in the different allocations to use as the best available predictor of where women will choose to go. Description Approach Weighting agreed by Clinical Board 1 2 3 4 5 6 Practice proximity Referral patterns / practice proximity Current referral patterns GP survey Children’s centre survey Ealing Hospital survey All Ealing CCG women deliveries are redistributed based on women's practice proximity to their nearest provider Women who deliver at Ealing hospital transfer to next closest provider to the women's practice. Women who currently deliver elsewhere remain unaffected. Visitors at Ealing children’s centres gave second choices and these are applied based on where they are resident Women who deliver in Ealing Hospital transfer in accordance to the surveyed women's response in each respective postcode 0% 10% 10% 40% Women who deliver at A GP survey provided Ealing hospital transfer locality based according to the preferences. proportions of women at each practice who use the alternate providers Two modifiers are applied to the outputs of this • Firstly, the implementation of Imperial’s site and clinical strategy allocates 80% of Imperial’s Ealing birth allocation to Queen Charlottes and 20% of Imperial's Ealing allocation to St Mary’s • Certain boundaries for community services between trusts are re-drawn in Chiswick and Brent, reallocating 264 births from Northwick Park to Imperial’s two sites (mainly St Marys) and 282 births from Imperial (mainly QCCH) to Chelsea & Westminster 30% 10% The weighted allocation • • • Model reviewed and signed off by The SaHF Clinical Board developed a Weighted allocation • Heads of Midwifery from these using the weightings above across NWL They agreed that: Allocations (3) and (6) have the • Maternity & Neonatal strongest weighting with the others having reduced Project Delivery weighting due to (1) ignores existing referral patterns (2) Board uses straight line distance rather than travel time and (4) • SaHF Clinical Board and (5) have low sample size surveys • SaHF Programme Therefore, the Weighted Allocation was agreed to produce Board an allocation that was considered the best available predictor of where Ealing women will choose to go Henceforth, these are referred to as Allocations in the remainder of this document 10 Detailed analysis While number of deliveries has declined in NWL since 2011/2012, the number of beds has increased slightly over this time period Number of births Number of births at NWL sites 40k - 4% - 1.5% 31.6k 30.7k 30k Current outturn for 2014/15 suggests the trend of declining births across North West London’s hospitals will continue - 1% 29.6k 29.3k Ealing St Mary's • Over the past 3 years, we have seen a year on year decline in the number of births across North West London, since the sector’s peak in 2011/12 • Using the first eight months of the year, we forecast that outturn for the year is expected to be 29,297 a 1% reduction on 2013/14 deliveries Hillingdon 20k West Midd. Northwick Park 10k Queen Charlotte's Chel West k 2012/13 2013/14 2014/15 (F) The bed base has remained relatively consistent over the past few years • • • The number of beds has remained consistent over the past few years, with growth in 2014/15 as a result of an increase in MLU beds at Chelsea & Westminster, providing the system with capacity for an additional 1000 births The result of the slight growth in beds with the decrease in births has seen the number of beds per 1000 births increase from 13.3 in 2011/12 to 14.7 in 2014/15 (F). None of the units across NWL has delivered their full capacity in births in any of these years. Number of beds at NWL sites Number of beds 2011/12 The increase in capacity in 14/15 supports us to prepare to transition Ealing’s service while retaining the same number of total beds in 13/14. The increased bed number for 14/15 is driven by the opening up of MLU and Labour Ward beds at Chelsea & Westminster, providing the system capacity for an additional 1000 births. Alongside this, West Middlesex has beds ready to open. 500 419 423 423 432 423 Ealing 400 St Mary's 300 Hillingdon West Midd. 200 Northwick Park 100 Queen Charlotte's Chel West 0 2011/12 2012/13 13.3 13.8 2013/14 2014/15 (F) 2015/16 Planned 14.3 14.7 14.4* Beds per 1000 births * Based on Scenario 1 12 Two scenarios for deliveries are used to stress test the capacity of the system • • Scenario 1 – 29,297 births (the same number of births as predicted outturn for 2014/15). This is based on the ONS prediction of no growth in births in NWL Scenario 2 – 30,565 births (Scenario 1 + 4.3%). This was arrived at by asking trusts for their likefor-like planning figures for 2015/16 and including an allowance of 3,000 from Ealing Hospital (compared to 2,614 births forecast at Ealing Hospital in 2014/15) The number of births in Scenario 2 (30,565) is fewer than the number of births seen in 2011/12 (31,600) in North West London and NWL is planning a higher bed base (423 compared to 419). Total number of births at NWL sites – historic and applying ONS growth forecasts Number of births Two scenarios are used in testing the capacity in the system for 2015/16: 40k Two scenarios used 40k 31.6k 30.7k 29.6k 29.3k 29.3k 29.2k 29.2k 30k 30k Based on ONS growth forecasts 20k Actuals for NWL (inc. 14/15 forecast based on first 8 months) 10k k 11/12 12/13 13/14 14/15 (F) 15/16 (ONS) 16/17 (ONS) 17/18 (ONS) 29.3k 30.6k 20k 10k k Scen 1 Scen 2 Each of the two Scenarios is applied to different possible Allocations of Ealing births to the receiving sites • Allocations (2) to (6) are used because they were the components of the Weighted allocation the SaHF Clinical Board agreed • The Weighted allocation, agreed by SaHF Clinical Board, is used • (1) is not used as it did not form part of the Weighted allocation signed off by Clinical Board • We therefore stress test the total system with 12 permutations of Scenarios and Allocations • See slide for 9 for an overview of the Ealing Allocation Model 13 Stress testing each scenario demonstrates that the NWL system capacity will be sufficient using all allocations of Ealing’s births Beds/1000 births NWL-wide bed capacity will be sufficient to handle demand in all permutations of Scenario 1 and Scenario 2 • 11/12 13.3 12/13 13.8 13/14 14.3 14/15 (F) 14.7 15/16 Scen 1 14.4 15/16 Scen 2 13.8 Scenario 1 – Across the different allocations of Ealing’s births, there are 24-27 more beds planned across NWL than recommended by the bed model – With the Weighted allocation, considered by NWL clinicians as the most likely allocation, there is a surplus of 24 beds across the NWL system • Scenario 2 – Across the different allocations of Ealing’s births, there are 3-11 more beds planned across NWL than the bed model recommends – With the Weighted allocation, there is a surplus of 10 beds • While there are differences between the planned number of beds and the recommended by the bed model for different types of bed, each service is able to flex beds differently (dependent on adjacency and operating model) The programme has sought confirmation from each trust that individual sites are able to flex beds appropriately to manage demand and each trust has confirmed it is confident it will be able to meet anticipated demand Inpatient beds by type Total beds The best and worst for each scenario is based on the different ways of allocating Ealing births between receiving sites. These are given with the Weighted allocation The variation between the different allocations (even with splitting the same number of births between sites) is driven by two factors in the bed modelling – the rounding up and the difference in acuity in sites Midwifery Led Unit Antenatal Labour ward Not inpatient beds Bereavement HDU Recovery Scen. Allocation 2015/16 planned 423 31 97 66 7 11 22 Scenario 1 - Difference between beds planned and recommended by bed model 24 Worst (All. 3) 0 7 6 -5 -1 -1 27 Best (All. 2) 0 8 8 -5 -1 0 24 Weighted -1 6 9 -5 -1 -1 Scenario 2 - Difference between beds planned and recommended by bed model 3 Worst (All. 4) -3 2 5 -6 -2 -2 11 Best (All. 3) -2 4 5 -5 -1 -1 10 Weighted -2 4 5 -5 -1 -1 Postnatal Transitional Care Triage/ OPD induction DAU Theatres 157 32 24 26 12 17 16 17 1 1 0 1 2 1 3 4 3 0 0 0 11 12 11 -2 -1 -1 0 1 1 2 3 3 -1 0 0 Currently, all receiving sites apart from Northwick Park have 1 bereavement bed. Northwick Park use a labour ward room suitable for bereavement. If an additional bereavement room are needed, then trusts use a appropriate delivery room. The model recommends that any unit between 3000-6000 births has 2 bereavement beds i.e. 12 in total for NWL, which is 9 more than the current number of 4 bereavement beds and 6 more than the planned 7. 14 While there is sufficient capacity across NWL, there are two trusts which are planning fewer beds than the model recommends For each Scenario, the worst, best and weighted allocations (in terms of difference between the planned number of beds and the bed model recommendations). The breakdown by trust is shows for each of these allocations. Scenario 1 – difference between planned and recommended beds 2013/14 ACTUAL NWL SYSTEM St Mary's Queen Charlotte's Chelsea & West. West Middlesex Northwick Park Hillingdon Scenario 1 Worst (All. 3) Best (All. 2) Weighted 24 27 24 7 4 -5 3 5 -3 3 9 -7 11 7 1 5 19 -6 2 3 4 4 11 -6 8 6 1 Scenario 2 – difference between planned and recommended beds 2013/14 ACTUAL NWL SYSTEM St Mary's Queen Charlotte's Chelsea & West. West Middlesex Northwick Park Hillingdon Scenario 2 Worst (All. 4) Best (All. 3) Weighted 3 11 10 7 4 -5 3 5 -3 2 -1 -6 7 6 -5 2 7 -7 7 5 -3 2 8 -6 6 3 -3 Stress testing indicates that there will be sufficient capacity under all scenarios, but some choice may be decreased • Under Scenario 1, the bed model recommends more beds for Chelsea & Westminster than the trust is planning • Under Scenario 2, the bed model recommends more beds for Chelsea & Westminster and Hillingdon than either trust is planning • Operational models at Chelsea & Westminster and Hillingdon are different from other trusts. For both trusts, we see (from the first column) that when we compare this to actual births and beds for 2013/14, the bed model recommends more beds than the trusts used to manage their services. • Chelsea & Westminster has 6-7 fewer beds than the bed model recommends, the main contributor being 6 fewer transitional care beds. Chelsea & Westminster operates a different transitional care model to other trusts. Postnatal beds are used flexibly with transitional care beds, enabling beds to be flexed based on need. Since the opening of the Midwifery Led Unit, there has been increased capacity in beds across intra partum and postnatal and the trust has more recovery beds which relieve pressure from the postnatal ward. Transitional care is supported by nursery nurse lead on the postnatal ward. There will be additional capacity for transitional care on the neonatal unit which will be co-located with the postnatal ward as part of the planned expansion of the neonatal unit. The trust has also secured funding to expand the neonatal unit and add additional cots if required during 2015/16. This will allow for shared workforce, more efficient working between the two areas, and promote mother and baby early bonding by not separating them. As a result, the trust have confirmed that they are able to manage with their bed base • Under Scenario 2, Hillingdon’s planned number of beds is 3-5 beds fewer than the number the bed model recommends. Hillingdon has the physical space for 4 additional antenatal beds on its antenatal ward or overflow ward if required. Alongside this, the site has an additional labour ward room that can be used flexibly with MLU and its bereavement, recovery and HDU beds are flexible. A surplus of DAU beds allows the trust to flex antenatal beds and Hillingdon is able to transfer women in maternity HDU to our main hospital HDU ward. The programme has confirmed local plans from both trusts to ensure that they have sufficient flexibility in their bed base to deal with potential demand. 15 99-100% of North West London women receive their first choice of maternity unit in all likely permutations Trusts have indicated that they would be able to accommodate more births than they have assumed in their capacity planning (see chart right for the maximums). These have been used to understand headroom at each site and the impact on choice*. In most permutations of Scenarios and Allocations, at least 99% of women receive their first choice (see table below) • The number of women in NWL who currently receive their first choice is unknown. The introduction of a Maternity Booking Service in North West London will enable this to be tracked and help the system to manage peaks in demand across trusts. • The worst case for both scenarios is under Allocation (2), in which women who deliver at Ealing Hospital choose to instead deliver at the unit closest to their GP’s surgery. This scenario is not seen as likely by NWL clinicians (reflected in the Clinical Board weighting of allocations). • Using the allocations of Ealing’s births considered good predictors by NWL clinicians – (3), (6) and the Weighted – the proportion of women who do not receive their first choice is 0.0% in Scenario 1 and 0.2-0.6% in Scenario 2 In all permutations where women do not receive their first choice there is enough capacity across NWL to accommodate them. The impact on women’s choice is therefore expected to be minimal for all women across NWL including women from the Ealing. 40k 29.3k 30.6k 30k 31.8k 5,500 5,300 20k West Mid 5,000 Northwick Park 4,000 Hillingdon 10k 6,000 6,000 St Mary's Queen Charlotte's Scen 1 Scen 2 Maximum trusts can take The modelling suggests the following proportion of women will not receive their first choice unit under different permutations of scenarios and allocations of Ealing’s births: Scenario 1 Scenario 2 In both Scenarios 1 and 2, using Allocation (2), the women’s whose choice may be affected are those who choose West Middlesex (regardless of where they are from in NWL) 2 1.2% 2.4% 3 0.0% 0.2% The women’s whose choice may be affected are those who choose Hillingdon (regardless of where they are from in NWL) 4 0.0% 0.9% 5 0.0% 0.0% The women whose choice may be affected are those who choose primarily Hillingdon (regardless of where they are from in NWL). In this permutation, some women who choose Queen Charlotte may not receive their first choice (10% of those whose choice might be affected) 6 Weight. 0.0% 0.0% 0.6% 0.3% The women’s whose choice may be affected are those who choose Hillingdon (regardless of where they are from in NWL) The women’s whose choice may be affected are those who choose Hillingdon (regardless of where they are from in NWL) * Method applied - The total number of women who may not able to deliver at their chosen site from the headroom analysis are considered as a proportion of the total women in North West London. These are calculated using the maximum number of births that each site can take and comparing to the number that each site is allocated under each permutation of allocation and scenario. These are then represented below as a proportion of the total number of women. 16 Ealing women will also have increased choice in community care There will be more choice for Ealing women about where they access their care and greater continuity of care during their antenatal and postnatal pathway • The majority of women who live in Ealing borough choose not to deliver at Ealing Hospital (~60% in 2013/14) • Continuity of care is currently limited and women may not get into their chosen units due to preferential treatment of those from more traditional boroughs (this is currently the case for Ealing women choosing QCCH today) • Those who would have chosen Ealing Hospital will be treated by the same principles as are currently applied across London. The extension of community services into Ealing will enable better continuity of care for Ealing women (see example on right) • For the first time, all NWL providers have agreed common acceptance criteria for women and these will help to ensure that all women in North West London, including Ealing women, are treated equally. Benefits of the new proposed community model Current Future Women in Ealing who choose to deliver at another hospital in NWL (~60% in 13/14) cant access their antenatal care locally • Ealing women currently have variable continuity of care across the antenatal & postnatal pathway • Women will experience improved continuity of care as a result of NWL units providing antenatal and postnatal care in Ealing Hospital and children’s centres in the Ealing borough Queen Charlotte’s currently cannot accommodate Ealing demand and are turning Ealing women away • • Queen Charlotte’s will be able to accommodate more women from Ealing Units, including Queen Charlotte’s, will treat women from Ealing the same as women that live in their host CCG borough • Women will be able to choose to have their antenatal care at Children’s centres, Health centres in Ealing, Ealing Hospital, community venues in their chosen providers borough or on the hospital site of their chosen provider. Those choosing Hillingdon or LNWHT will be able to access consultant led antenatal care from the Ealing hospital site Worked example of what will happen to Ealing women Northwick Park • Hillingdon Hospital St Mary’s Queen Charlotte’s Ealing Hospital Chelsea & Westminster West Middlesex • London North West Chelsea & Westminster Imperial Hillingdon London North West/Imperial West Middlesex If a woman living in the blue (West Midd) area of Ealing chooses Queen Charlotte's, she has the option to have her antenatal care at Ealing Hospital, a children's centre in the red Imperial area or Queen Charlotte's site if she requires specialist input or a scan. She can St receive her post natal care from either Queen Mary’s Charlotte's (at Ealing Hospital or a children's centre) or from West Middlesex (either in her home or a local children's centre in the blue area.) Chelsea & Westminster If she chooses West Middlesex, she will receive the full pathway from West Middlesex, choosing between at home, locally at a children's centre or at West Middlesex Hospital itself. 17 There will be additional physical capacity in neonatal cots with all receiving trusts implementing robust recruitment plans There will be an additional physical capacity of 15 neonatal cots Special care cots 120 Number of cots 100 87 89 86 92 104 5 99 92 80 • There will be additional physical capacity across the system with 7 more cots planned and a potential additional 11 if required (across both Special Care and HD/IC) • The 11 additional cots are made up of 6 HD/IC cots at Chelsea at Westminster (budget approved and can be used as SC if necessary) and 5 SC cots at West Middlesex (they have space but subject to commissioning) • Trust plans to increase transitional care beds across North West London will reduce the demand on special care neonatal cots • The capacity planning for neonatal cots has been reviewed and signed off by: Potential additional cots if necessary 60 40 Physical Capacity 20 0 2011/12 2012/13 2013/14 2013/14 2014/15 2015/16 Cot usage (activity at 80% occupancy) Physical Capacity High dependency and intensive care cots 80 66 Number of cots 62 60 51 56 66 72 6* 66 40 Potential additional cots if required 20 Physical Capacity 2013/14 2014/15 2015/16 Cot usage (activity at 80% occupancy) Physical Capacity Neonatal leads from each Trust – The Maternity & Neonatal Project Delivery Board – NHS England’s specialist commissioners for Neonatology – SaHF Clinical Board – SaHF Programme Board Specialist nurses staffing levels have been considered in the transition planning • The shortage of neonatal specialist nurses is a concern that has been raised and reviewed nationally • The transfer of Ealing’s neonatal nurses has been planned to broadly follow activity, which will enable trusts to meet the potential increase in activity • Alongside this, the Neonatal network is sharing demand management approaches between trusts, which will support the introduction of transitional care, which in turn will reduce demand 0 2011/12 2012/13 2013/14 – * Chelsea & Westminster has budget approved for up to 6 neonatal HD/IC cost if needed. 18 All trusts are making progress in 2015/16 towards meeting target Total numbers across NWL quality standards for workforce levels Trusts have comprehensive workforce and recruitment plans which are supported by the transfer of Ealing staff • All the trusts have developed workforce plans based on their capacity planning assumptions (Scenario 2) and the weighted allocation of 3000 Ealing births • The implementation of SaHF (including the transfer of Ealing Hospital’s maternity services) is an enabler for trusts working towards achieving London Quality Standards (LQS) by 2017/18 • 2014/15 in post Role Midwives 935 1040 + 11% O&G consultants 97 109 + 13% Neonatal nurses 259 322 + 25% Including Ealing transfer and local recruitment plans All trusts are making progress in 2015/16 towards the achievement of LQS (a midwife to birth ratio of 1:30 and consultant presence on labour ward of 168 hours) Midwifery ratios 14/15 in- 15/16 planned post ratio ratio Trust Midwifery ratios • 4 out of 6 sites are expected to achieve the midwifery ratio of at least 1:30 in 2015/16 • Hillingdon and West Middlesex, the two sites not achieving the ratio in 2015/16 are significantly improving their midwife to birth ratios as a result of the transition and have plans to work towards meeting 1:30 midwife to birth ratio by 2017/18 • As a sector, NWL will achieve an overall average of 1 midwife to 30 births following transition. 2015/16 planned Change Chelsea & West. Imperial Northwick Park Hillingdon West Middlesex Ealing NWL 1:32 1:33 1:25 1:33 1:36 1:30 1:32 1:30 1:30 1:27 1:32 1:33 1:30 2015/16 ratio based on Scenario 2 births – trust plans Obstetrics & Gynaecology consultant cover • 5 out of 6 sites are planning to increase their Consultant cover in 2015/16 • All of the trusts are committed to working towards meeting the 168 hour consultant cover target by 2017/18 • As a sector, the average will increase from 101 hours to 122 hours in 2015/16 Neonatal nurses • The shortage of neonatal specialist nurses is a concern that has been raised and reviewed nationally and the changes by SaHF will not affect this negatively • The transfer of Ealing’s neonatal nurses has been planned to broadly follow activity, which will enable trust to meet the potential increase in activity • Alongside this, the Neonatal network is sharing demand management approaches between trusts, which will support the introduction of transitional care, which will reduce demand. Consultant cover in 2014/15 and 2015/16 (planned) Chelsea and West. Queen Charlotte's St Mary's 110 to 115 98 to 134 98 to 108 Hillingdon 96 to 114 West Middlesex AVERAGE Hrs cover in 2015/16 (planned) stays at 98 Northwick Park Ealing Hrs cover in 2014/15 144 to 164 60 hrs in 2014/15 101 to 122 19 APPENDIX C Simon Weldon NHS England London Southside 4th Floor 105 Victoria Street London SW1E 6QT Dr Mohini Parmar Chair Ealing CCG Cc: Clare Parker Chief Officer CWHHE CCGs Rob Larkman Chief Officer BHH CCGs Thirza Sawtell SRO SaHF Programme 11 March 2015 Dear Mohini Re: NHS England assurance on changes to Ealing maternity services As you know, as part of Shaping a Healthier Future to transition Ealing maternity services to other Trusts in NW London, NHS England has set out a three stage assurance process: Stage 1: areas for assurance before a decision is made by Ealing Governing Body on the timing of the transition Stage 2: areas for assurance prior to the transition of services Stage 3: areas for assurance in the year following transition of maternity services I am writing to let you know the outcome of our Stage 1 assurance. As part of our Stage 1 assurance, we commissioned a number of external reviews and worked with NHS Trust Development Authority colleagues reviewing documentation provided by the SaHF team. Set out below is a summary of the recommendations from: 1. The London Clinical Senate Review 2. Outcome of clinical conversations with lead clinicians in NW London Trusts 3. Review of SaHF demand and capacity modelling 4. Outcome of Stage 1 assurance. 1. The London Clinical Senate Report In December 2014, NHS England commissioned the London Clinical Senate to advise on: Has there been any substantive change to the case for change since it was accepted by Secretary of State in October 2013 Do the clinical models remain appropriate The proposed timing of these changes. NHS England received the London Clinical Senate report on 6 February 2015. The Review Team found no material issues that alter the strategic case for change presented in 2013. At an operational level, they found the drivers for change have accelerated since the case for change was accepted especially in maternity, increasing risks to clinical quality and safety. 1 Overall, the Review Team found the clinical models remain appropriate. They found the model for maternity services will improve quality and choice and is consistent with the recently published guidance from NICE and the NHS Five Year Forward View. With regard to timing, the Review Team advised very strongly that maternity services at Ealing should move in line with a proposed transition date of June 2015. Retaining the service beyond this timescale would significantly increase the risk of unplanned closure of the unit. The Review Team also recommended that NHS England sought assurance on the following: 1. Further detail on the emergency gynaecology service at Ealing Hospital 2. Satisfactory arrangements were in place for transitional and outreach neonatal services 3. Development of an innovative paediatric service model at Ealing. 2. Clinical conversations between London Strategic Clinical Network Clinical Director and North West London clinicians from Trusts affected by SaHF proposals In February 2014, NHS England commissioned the Clinical Senate to undertake conversations with maternity, neonatology, gynaecology and paediatric clinicians in NW London Trusts. Views were unanimous from maternity and neonatology clinicians that Ealing services needed to transition to the planned timetable. Paediatric and gynaecology clinicians at Ealing were confident about the services planned to remain at Ealing following the transition of maternity services. All clinicians at London North West Healthcare, Imperial College Healthcare, West Middlesex, Chelsea and Westminster and Hillingdon Hospital Trusts were supportive of increased service provision at these sites and the timetable proposed. 3. Review of capacity and demand models In December 2014, NHE England commissioned Ernst and Young LLP (EY) to review SaHF demand and capacity modelling for maternity and neonatal services underpinning the plans. EY provided a report with recommendations. These recommendations together with SaHF’s response formed the basis of a workshop held on 12 February and a final workshop held on 19 February. The conclusions arising from the EY review and workshops are contained in 4.II below. 4. Outcome of Stage 1 assurance The Stage 1 assurance was undertaken in three sections: I. Case for change II. Impact of activity moving to receiving sites III. Impact on paediatric and gynaecology services remaining at Ealing Hospital post maternity transition The outcome of the assurance is summarised below with further detail given in the following paragraphs. Assurance section Case for change Impact of activity moving to receiving sites Impact on paediatric and gynaecology services remaining at Ealing Hospital post maternity transition NHS England decision Assured Partly assured Partly assured 2 Case for change As a result of the Clinical Senate Report and Clinical Conversations, NHS England are assured there is a clear, well-articulated case for change that is supported by Trust clinicians, strategic clinical network leaders and the London Clinical Senate. The risks of delaying the transition of maternity services are clearly identified. The planned transition is consistent with NICE guidelines and the Five Year Forward View. NHS England is fully assured on the case for change. Impact of activity moving to receiving sites Demand On behalf of the CCGs and providers, SaHF developed an allocation model to understand how Ealing births may be distributed to receiving sites and developed a bed model which recommended maternity impatient bed numbers based on acuity of site and number of deliveries. The SaHF programme also developed a workforce model. EY reviewed the distribution and capacity models for maternity and neonatal services. EY’s final report confirmed that overall modelling was robust. The first workshop concluded that flat growth for births was the most realistic assumption to model capacity on. Capacity plans for Trusts include excess capacity for growth of 1300 births. NHS England is therefore assured that sufficient capacity has been built into the plans. Workforce Detailed workforce modelling linked to demand planning, has been undertaken. Receiving Trusts have comprehensive workforce and recruitment plans in place which are supported by the transfer of Ealing staff. NHS England is partly assured on workforce. Further assurance is sought that the numbers of staff as set out in the February 2105 workforce plan, will be in place at all receiving sites before implementation.. Posts to support Trust implementation have been established including an Operations Director and Trust liaison posts. As part of Stage 3, further assurance will be sought on continued movement towards London and national standards for improved staffing levels, where appropriate. Physical capacity Sufficient physical space is available at Northwick Park, West Middlesex, Chelsea and Westminster, Hillingdon and St Mary’s to receive the transfer of maternity and neonatal services. Sufficient space at Queen Charlotte’s is dependent on estates work being completed in May 2015. NHS England is partly assured on physical capacity. Confirmation is sought that work at Queen Charlotte’s will be completed in May. Managing capacity and demand and supporting women’s choice NW London CCGs have put in place a maternity booking system that helps women who may not get their first choice of maternity unit and supports system wide monitoring of demand and capacity to manage potential surges in demand. Based on an independent review that the maternity booking system is well thought through with defined clear objectives and lines of accountability, NHS England is partly assured that the maternity booking system is fit for purpose. Further testing for Stage 1 is required on the flow of data between Trusts and the system to ensure it can support monitoring and surge management. It is recommended for Stage 2 assurance that the ability of the system to support women’s choice is tested. Impact on paediatric and gynaecology services at Ealing Hospital Based on the Senate Review and the Clinical Conversations, NHS England is assured that the proposed retention of paediatric and gynaecology services on the Ealing site post maternity transition are supported by London North West Trust clinicians, strategic clinical network leaders and the London Clinical Senate. In line with the Senate Report recommendations, further detail is sought on the emergency gynaecology model for Stage 1 assurance. For Stage 3 assurance, further detail will be sought on the paediatric model of care in relation to day surgery, rapid access clinic and transition arrangements for young people. 3 Summary of recommendations from Stage 1 My letter has identified those areas where NHS England is fully assured in Stage 1 and those areas where further assurance is required. Areas for assurance in Stages 2 and 3 have also been identified in Stage 1 where relevant. It should be noted this is not an exhaustive list of assurance activities for Stages 2 and 3. A summary of all recommendations relating to further assurance is set out in the table below. Table of recommendations for further assurance Stage 1 Pre decision 1 Confirmation that number of midwives, consultants, neonatal nurses and sonographers, as set out in the SaHF workforce plan in February 2015, will be in place at each receiving site by the time of transition 2 Director of Operations and Trust Liaison posts filled 3 Estates work at Queen’s Charlotte will be completed in advance of transition 4 Testing of maternity booking system for monitoring booking at Trusts 5 Details of gynaecology emergency model at Ealing Hospital Stage 2 Pre Transition 6 Testing of maternity booking system to support women’s choice is tested by women who are booked in at Ealing Hospital and may need to transition provider 7 Individual communication to women who are likely to be most affected by the transition 8 Communication to women about the importance of booking early and choices available and information to women about the maternity booking system Stage 3 Following transition 9 Continued movement towards London and national standards on improved staffing levels, where relevant. 10 Detail on the paediatric model of care at Ealing Hospital in respect day care and day surgery, rapid access clinic and transition arrangements for young people. 11 External peer review of all affected services within the hospitals providing the additional maternity, neonatal and gynaecology capacity is strongly recommended before, during and up to 18 months after transition We will be in touch shortly about the additional information we need to conclude Stage 1. NHS England acknowledges the considerable work the SaHF programme, Ealing CCG and Trust clinicians and managers have put into developing these proposals. We are aware that there are other issues Ealing Governing Body may wish to consider in making a decision on the timing of the transition. If so, please let us know and we will be happy to assist you. Yours sincerely, Simon Weldon Chief Operating Officer NHS England London Region 4 APPENDIX D Communications and engagement – update for Ealing CCG: 18th March 2015 Objectives Raise awareness of changes and how they will improve maternity services in NW London Help women make informed choices about maternity units Provide reassurance about the changes Provide information on maternity units in NW London Hear feedback and answer questions Ensure women and their families have access to information Ensure regular and consistent information to women Planned products 1. Booklet – includes information on the changes, map of NWL showing the 6 sites post closure and information on each of these units (mini prospectuses) 2. Travel map – Our Travel Advisory Group are working with TfL to develop a bus map showing links between key localities around Ealing and maternity units in NW London 3. Accessible materials as appropriate – to be agreed in discussion with lay partners and community groups 4. FAQs – For midwives and GPs Planned activity A – Direct to women currently booked at Ealing maternity unit Phase 1 – pre-timing decision Regular letters to provide updates Phase 2 – timing decision until closure THOSE UNAFFECTED: Dedicated phone line for any queries Letter x 2: to confirm date means no change to birth plan. Phase 3 – post closure Relevant Trusts to decide if further communications required to women who have moved from Ealing. THOSE AFFECTED: Letter to confirm they will no longer be able to give birth at Ealing and to explain the next steps. Booklet included with letter Phone call to ensure receipt and understanding of letter Contact from maternity booking service to discuss 2 rd and 3 preference location B – Clinicians (GPs, midwives, HVs) Regular contact to provide update and remind to continue booking to Ealing until date known nd Confirmation letter from MBS once re-booking and appointments confirmed Letter to provide confirmation of closure date, next steps and to confirm bookings cease. FAQs Booklets delivered to all GP surgeries, Ealing Hospital and available to community midwives Staff-engagement with Ealing midwives regarding their roles Posters delivered to all GP surgeries showing maternity units in NW London Letter to confirm unit now closed and to remind of maternity units in NWL Updates at Practice Manager forums Updates at Network meetings & Council of Members Restock booklets if required Updated FAQs provided Electronic leaflet uploaded to computer system Updates at Practice Manager forums Updates at Network meetings & Council of Members MBS/Trust (tbc) confirm new booking for individual patients as appropriate C – Children’s centres and NCT Meetings with leaders Update email to all contacts Face to face sessions at all centres and all NCT groups as appropriate to provide reassurance and answer questions Booklets and posters delivered to all sites Continuing face to face engagement on all health and social care in NW London Information provided for websites and newsletters Provision of newsletters, leaflets and materials as appropriate Update email/letter to all contacts providing update and offering meetings Continuing face to face engagement on all health and social care in NW London Booklets and posters delivered to all sites Provision of newsletters, leaflets and materials as appropriate Testing of planned materials D – Wide community groups Letter to all groups to provide update, point of contact and copy for newsletters/website Face to face meetings to provide update on progress and next steps Information provided for websites and newsletters Updates on relevant NHS websites Press release in local media Testing of planned materials E – Hard to reach communities Tender out to identify community groups to undertake work with groups where there are language or cultural barriers Update email/letter to all contacts Booklets and posters delivered to all sites Information provided for websites and newsletters Meetings with leaders to identify languages and accessible materials required Continuing face to face engagement on all health and social care in NW London Chosen provider to undertake intensive engagement with hard to reach communities Provision of newsletters, leaflets and materials as appropriate
© Copyright 2026