Accreditation - The Hemophilia Alliance
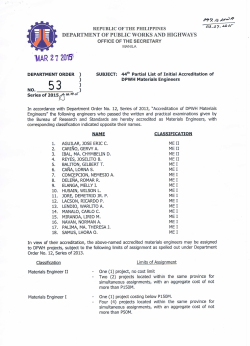
The Hemophilia Alliance Members Meeting n o i t a t i d e Accr Washington, DC Monday, April 27th Ralph Woods – BloodCenter of Wisconsin Mark Plencner – Sanford Health‐Roger Maris Cancer Center Dan Dalton – UNC HTC Pharmacy …or, “How to wrap you head around this without losing it” Getting Your Head Wrapped Around It…. • Do I need to become accredited? • Which accreditation organization is best for my program? • Which accreditation best represents my payer mix? • Which accreditation can I afford? • Can I afford not to be accredited? Our Mascot . . . Sparky Accreditation is nothing new . . . UL provides safety‐related certification, validation, testing, inspection, auditing, advising and training services to a wide range of clients, including manufacturers, retailers, policymakers, regulators, service companies, and consumers. . . . it’s just a ticket to the dance Accreditation – Def. The act of accrediting or the state of being accredited, especially the granting of approval by an official review board after the organization has met specific requirements ‐ Wikipedia Navigating the process 1.Provide a high quality service that meets industry standards 2.Write it all down – Policies and Procedures 3.Have documentation to prove you do what you say you do Do I really HAVE to ??? For the big companies . . . the marketing books call it “Barriers to Entry” The compelling result . . . Payors will require it Suppliers will require it Regulators may require it Choosing an Accrediting Agency • Joint Commission • Organization type • ACHC • Your organization’s experience • CHAP • Your organization’s support • URAC • Time commitment • NABP • Payor requirements • CPPA • Supplier requirements • EIEIO etc. • Cost and now . . . JC ACHC URAC Mark Ralph Danny Why Do We Accredit? Why Do We Accredit? Why Do We Accredit? The Joint Commission • Founded in 1951 • The Joint Commission seeks to continuously improve health care for the public, in collaboration with other stakeholders, by evaluating health care organizations and inspiring them to excel in providing safe and effective care of the highest quality and value. • The Joint Commission evaluates and accredits more than 20,500 health care organizations and programs in the United States. • An independent, not‐for‐profit organization, The Joint Commission is the nation's oldest and largest standards‐setting and accrediting body in health care. • To earn and maintain The Joint Commission’s Gold Seal of Approval™, an organization must undergo an on‐site survey by a Joint Commission survey team at least every three years. (Laboratories must be surveyed every two years.) The Joint Commission • Roots back to 1910 • Ernest Codman, M.D. • the acknowledged founder of what today is known as outcomes management in patient care • Proposed the end result system of hospital standardization.” • American College of Surgeons is founded. • The “end result” system becomes an ACS objective. • 1926 ‐ The first standards manual is printed, consisting of 18 pages. The Joint Commission • 1950‐1951 • The American College of Physicians, the American Hospital Association, the American Medical Association, and the Canadian Medical Association join with the ACS as corporate members to create the Joint Commission on Accreditation of Hospitals (JCAH), an independent, not‐for‐profit organization, in Chicago, Illinois, whose primary purpose is to provide voluntary accreditation. The Joint Commission • 1964‐1965 • The Joint Commission on Accreditation of Hospitals begins charging for surveys. • Congress passes the Social Security Amendments of 1965 with a provision that hospitals accredited by JCAH are “deemed” to be in compliance with most of the Medicare Conditions of Participation for hospitals and, thus, able to participate in the Medicare and Medicaid programs. The Joint Commission • 1975‐1977 • The Accreditation Council for Ambulatory Health Care is established and accreditation for ambulatory health care facilities begins. The Joint Commission The Joint Commission • 1978‐1979 • JCAH establishes an agreement with the College of American Pathologists to recognize CAP accreditation of a laboratory in a JCAH‐accredited hospital in lieu of the Commission’s accreditation of the laboratory. • The American Dental Association (ADA) becomes a JCAH corporate member. • A Professional and Technical Advisory Committee is established for each accreditation program, and the Accreditation Councils are disbanded. The Joint Commission • 1982‐1983 • The accreditation cycle is changed from two years to three years for hospitals, psychiatric facilities, alcoholism and substance abuse programs, community mental health centers, and long term care organizations. • Accreditation for hospice care organizations begins. (Folded into the Home Care Accreditation program in 1990.) The Joint Commission The Joint Commission • 1987‐1989 • The organization name changes to the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) to reflect an expanded scope of activities. • The Agenda for Change is launched, placing the primary emphasis of the accreditation process on actual organization performance. • Development of the Indicator Measurement System®(IMSystem®) – an indicator‐based performance monitoring system –gets underway. • Accreditation for home care organizations and managed care begins. (Managed care is folded into the Ambulatory Care Accreditation Program in 1990). The Joint Commission • 1992‐1993 • The Joint Commission issues a standard requiring all accredited hospitals to have a policy prohibiting smoking in the hospital. • The number and nature of confirmed substantive complaints filed against accredited facilities and the existence of type I recommendations becomes public information. • The federal government announces that home health agencies accredited by the Joint Commission after an unannounced survey will be “deemed” to meet the Medicare Conditions of Participation The Joint Commission • 1995 • The federal government recognizes Joint Commission laboratory accreditation services as meeting the requirements for Clinical Laboratory Amendments of 1988 (CLIA) certification. • As part of an Action Plan, the Joint Commission launches the Orion Project in Pennsylvania and Arizona as a series of experiments designed to test innovations to improve the delivery of accreditation services. • Accreditation for freestanding laboratories begins. The Joint Commission • 1996 • The Centers for Medicare & Medicaid Services announces that ambulatory surgical centers accredited by the Joint Commission will be “deemed” as meeting or exceeding Medicare certification requirements. • The Sentinel Event Policy is established. • The Joint Commission launches its website at www.jcaho.org (now www.jointcommission.org). The Joint Commission • 2002 • The Joint Commission establishes its first annual National Patient Safety Goals. • The Joint Commission and the Centers for Medicare and Medicaid Services launch Speak Up™. • The Disease‐Specific Care Certification Program launches. • The Centers for Medicare and Medicaid Services announces the granting of deeming authority for critical access hospitals to The Joint Commission. • The Joint Commission and the National Quality Forum announce the establishment of the John M. Eisenberg Patient Safety Awards. • The Joint Commission and the American Case Management Association announce the establishment of the Franklin Award of Distinction. The Joint Commission • 2003 • The Joint Commission announces a Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery™, effective July 1, 2004. • The Joint Commission creates a Gold Seal of Approval™ that is displayed on all certificates of accreditation. • The Joint Commission develops a Primary Stroke Care Certification Program with the American Stroke Association, providing the first nationwide certification program to evaluate stroke care provided by hospitals. The Joint Commission • 2006 • The Joint Commission begins conducting on‐site accreditation surveys and certification reviews on an unannounced basis, with certain exceptions. • An Advanced Inpatient Diabetes Care Certification Program is announced. • The Standards Improvement Initiative launches, with a goal to eliminate non‐essential standards and to ensure that the remaining standards are understandable and relevant to the care setting to which they apply. The Joint Commission • 2013 • The Joint Commission debuts its new Nursing and Rehabilitation Center Accreditation program, and for the first time offers a Rehabilitation and Advanced Care Certification option. • The Joint Commission begins offering a Primary Care Medical Home certification option for accredited hospitals and critical access hospitals. Joint Commission Standards • ACCREDITATION PARTICIPATION REQUIREMENTS(APR) • ENVIRONMENT OF CARE (EC) • EMERGENCY MANAGEMENT (EM) • EQUIPMENT MANAGEMENT (EQ) • HUMAN RESOURCES (HR) • INFECTION PREVENTION AND CONTROL (IC) • INFORMATION MANAGEMENT (IM) • LEADERSHIP (LD) • MEDICATION MANAGEMENT (MM) • NATIONAL PATIENT SAFETY GOALS (NPSG) • PROVISION OF CARE, TREATMENT AND SERVICES (PC) • PERFORMANCE IMPROVEMENT (P) • RECORD OF CARE, TREATMENT, AND SERVICE (RC) • RIGHTS AND RESPONSIBILITIES OF THE INDIVIDUAL (R) Joint Commission Standards – an example Medication Management ‐ Standard MM.07.01.01 The organization monitors patients to determine the effects of their mediation(s) Elements of Performance: • THE ORGANIZATION MONITORS THE PATIENT’S PERCEPTION OF SIDE EFFECTS AND THE EFFECTIVENESS OF HIS OR HER MEDICATION(S). NOTE: THIS ELEMENT OF PERFORMANCE IS ALSO APPLICABLE TO SAMPLE MEDICATIONS. • THE ORGANIZATION MONITORS THE PATIENT'S RESPONSE TO MEDICATION(S) BY TAKING INTO ACCOUNT CLINICAL INFORMATION FROM THE PATIENT RECORD, RELEVANT LAB VALUES, CLINICAL RESPONSE, AND MEDICATION PROFILE. NOTE: THIS ELEMENT OF PERFORMANCE IS ALSO APPLICABLE TO SAMPLE MEDICATIONS. • THE CLINICAL OR CONSULTANT PHARMACIST REVIEWS EACH PATIENT’S MEDICATION REGIMEN AT LEAST MONTHLY. • THE CLINICAL OR CONSULTANT PHARMACIST COMMUNICATES TO THE PRESCRIBER PROBLEMATIC FINDINGS AND RECOMMENDATIONS FROM THE MEDICATION REGIMEN REVIEW. Most common deficiencies . . . • Patient Education • Assessment and Care Planning • Safety Cost ESTIMATED ANNUAL SUBSCRIPTION FEE PROGRAM ESTIMATE (THESE FEES ARE DUE EVERY YEAR). AMBULATORY HEALTH CARE ACCREDITATION PROGRAM $4,810.00 HOME CARE ACCREDITATION PROGRAM $2,470.00 (THIS IS THE PORTION OF THE ANNUAL FEES THAT COVERS THE PHARMACIES AND OPTICAL SHOPS ON SANFORD CLINIC NORTH ACCREDITATION APPLICATION. IT INCLUDES MULTIPLE LOCATIONS ACROSS THE FARGO REGION). TOTAL ESTIMATED ANNUAL FEE $7,280.00 ESTIMATED ON‐SITE FEE PROGRAM ESTIMATE (THE ON‐SITE SURVEY OCCURS EVERY THREE YEARS). AMBULATORY HEALTH CARE ACCREDITATION PROGRAM $39,430.00 HOME CARE ACCREDITATION PROGRAM $19,260.00 (THIS IS THE PORTION OF THE ON‐SITE SURVEY FEE THAT COVERS PHARMACIES AND OPTICAL SHOPS ACROSS THE REGION). TOTAL ESTIMATED ON‐SITE FEE $58,690.00 A long winter in Wisconsin . . . Choosing an Accrediting Agency • Joint Commission • Organization type • ACHC • Your organization’s experience • CHAP • Your organization’s support • URAC • Time commitment • NABP • Payor requirements • CPPA • Supplier requirements • EIEIO etc. • Cost BloodCenter of Wisconsin From a payor’s provider network agreement . . . “Provider shall have accreditation . . . from one of the following: The Joint Commission (JC) Community Health Accreditation Program (CHAP) Accreditation Commission for Health Care (ACHC) From a manufacturer’s Specialty Pharmacy agreement . . . “Pharmacy represents and warrants that it is . . . Accredited by one of the major specialty pharmacy accrediting organizations (URAC, ACHC, or JC” BloodCenter selected… • Limited our consideration to JC, ACHC, URAC • Alignment: JC Hospitals ACHC Homecare and small providers URAC Health plans, disease & case management • Shortest time frame • Lowest cost • Recent experience of The Alliance Pharmacy, UNC BloodCenter selected… • Assembled a project team October 20 • Applied for accreditation February 17 • On site survey April 13 • Approved for Accreditation April 17 Accreditation Programs • • • • • • • • Home Health Care Hospice Private Duty DMEPOS Pharmacy Sleep Behavioral Health Hospital Accreditation • • • • • • • Infusion Pharmacy Ambulatory Infusion Center Specialty Pharmacy Infusion Nursing Community Retail Pharmacy Non‐sterile Compounding Sterile Compounding Step one . . . Dig into the details ACHC Standards • ORGANIZATION AND ADMINISTRATION • PROGRAM/SERVICE OPERATIONS • FISCAL MANAGEMENT • HUMAN RESOURCE MANAGEMENT • PROVISION OF CARE AND RECORD MANAGEMENT • QUALITY OUTCOMES/PERFORMANCE IMPROVEMENT ACHC Accreditation ACHC Standards – an example Organization and Administration ‐ Standard DRX1‐1B The organization is an established entity . . with the appropriate licensure, Articles of Incorporation, or other documentation of legal authority Surveyor might request to see pharmacy license and Articles of Incorporation for the parent organization ACHC Accreditation ACHC Standards – another example Human Resource Management ‐ Standard DRX4‐7A Written Policies and Procedures .. all personnel receive training .. to competently perform the task .. prior to being assigned to work independently Surveyor might request training records for a pharmacy technicians to verify that she had been trained on the proper packaging of factor for shipping ACHC Accreditation ACHC Standards – one more Human Resource Management ‐ Standard DRX5‐2C Written plan of care for each client/patient accepted for pharmacy services Surveyor might pick a random patient or three and ask the pharmacist to open the patient’s record in the pharmacy system and show the POC ACHC Accreditation Most common deficiencies . . . • Personnel records incomplete – orientation, training records • Performance reviews, etc. • Plan of Care documentation • Education – not having minimum education of staff, and/or staff cannot answer questions correctly • Not performing performance improvements (PI), not documenting them, not having them ACHC Accreditation Back home in South Carolina . . . ? ? ? UNC HTC Pharmacy • University‐based program • NC Medicaid 340B Hemophilia Specialty Pharmacy • Among the requirements to participate…be accredited by one of three organizations….JCAHO, ACHC, URAC • ACHC Accredited 1/17/2014 • URAC Accreditation in process • BCBS of NC requirement for participation in SP network • BCBS of NC does not recognize ACHC accreditation ACCREDITATION PROGRAMS • • • • • • • • • • • • • • • Accountable Care Accreditation Case Management Claims Processing Clinical Integration Accreditation Community Pharmacy Comprehensive Wellness Consumer Education & Support Credentials Verification Organization Dental Network Disease Management Drug Therapy Management Health Call Center Health Content Provider Health Network Health Plan • Health Plan with Health Insurance Marketplace • Health Plan Quality Measures • Health Web Site • Health Utilization Management • HIPAA Privacy & Security • Independent Review Organization • Mail Service Pharmacy • Medicare Advantage • Patient Centered Medical Home • Pharmacy Benefit Management • Provider Credentialing • Specialty Pharmacy • Transitions of Care Designation • Workers Compensation Property & Casualty Pharmacy Benefit Management SPECIALTY PHARMACY • • • • • • • • • • • Pharmacy Core Standards Organization Structure Policies and Procedures Regulatory Compliance Inter‐Departmental Coordination Oversight of Delegated Functions Marketing and Sales & Communications Business Relationships Information Management Quality Management Staff Qualifications • Staff Management • Clinical Staff Credentialing and Oversight Role • Health Care System Coordination • Consumer Protection and Empowerment • Customer Service, Communications & Disclosures • Specialty Drug Management • Pharmacy Operations • Patient Management • Measures Reporting URAC ‐ Mandatory Standard: Measure Number SP‐3 Measure Name Call Center Performance Measure Developer/ Steward URAC Measure Description Numerator Denominator This measure has two parts: Part A measures 30‐second response rate: Part B measures call abandonment rate. Part A: The number of calls answered by a live customer service rep within 30 seconds of being placed in the organization's ACD call queue. Part B: The number of calls abandoned by callers after being placed in the ACD call Queue and before being answered by a live customer service rep Part A: The total number of calls received by the organization’s call service center during normal business hours during the measurement period. This measure is to be reported for each of the Specialty Pharmacy’s books of business that is included Part B: The total number of calls received by the organization’s call service center during normal business hours during the measurement period. COMPARISON AT A GLANCE JC • • • • • High complexity Time: > 6 months Costs: $60,000.00* Standards:149 Elements:Many ACHC • • • • • • Moderate complexity Time: < 6 months Costs: $4,500.00 Standards: 68 Elements: 142 Requires a PER upload URAC • • • • • • High complexity Time: > 6 months Costs: $28,500.00* Standards:96 Elements: 405 Requires Accredinet upload Getting Your Head Wrapped Around It…. • Do I need to become accredited? • Which accreditation organization is best for my program? • Which accreditation best represents my payer mix? • Which accreditation can I afford? • Can I afford not to be accredited? Questions?
© Copyright 2026
![National University Virtual High School [2014-2015]](http://cdn1.abcdocz.com/store/data/000348438_1-3a80ae3134ab49395c6a7578fe5bdf0b-250x500.png)