THE PREVALENCE AND CONTROL OF HYPERTENSION AMONG
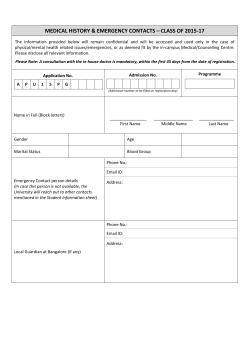
THE PREVALENCE AND CONTROL OF HYPERTENSION AMONG PATIENTS WITH TYPE 2 DIABETES MELLITUS IN NIGERIA http://dx.doi.org.10.4314/jcm.v17i2.2 Anakwue RC1,2, Arodiwe EB1, Ofoegbu EN1 1 Department of Medicine, College of Medicine, University of Nigeria, Enugu Campus, Nigeria. 2 Department of Pharmacology & Therapeutics, College of Medicine, UNEC, Nigeria. Corresponding author: Dr RC Anakwue Email: [email protected], Phone number : +2348033343044 SUMMARY Background: Diabetes Mellitus (DM) is an endocrine disease with profound vascular morbidity and mortality, and hypertension is known to play a prominent role in this regard. The aim of this study is to determine the prevalence of hypertension and to assess drug control of hypertension among DM patients seen in Enugu, Nigeria. Methods: The medical records of 420 adult patients with diagnosis of type 2 DM and hypertension, managed consecutively in the outpatient unit of University of Nigeria Teaching Hospital Enugu were studied. Results: Sixty percent of the diabetic patients had hypertension. Only 12% of these patients had their blood pressure controlled to ≤ 130mmHg and ≤ 80mmHg. About 12.3% of the patients who had hypertension were not on anti hypertensive drug treatment. Most of the patients were placed on 1 or 2 drugs. Angiotensin converting enzyme inhibitors were the most frequently prescribed drug. Conclusion: This study and similar ones from other parts of Nigeria indicate that the prevalence of hypertension among Nigerians with type 2 DM is high. Clinicians and patients should be reminded that even though blood glucose control is important, aggressive blood pressure control in diabetics is top priority in preventing adverse cardiovascular events which causes the highest mortality in the average population of type 2 diabetics. Appropriate antihypertensive regimen optimizes nonpharmacological therapies, reduces adverse effects on glucose control, minimizes the risk of medication-related side-effects, and provides much needed cardiac and renal protection. Key words: Hypertension, Prevalence, Diabetes Mellitus, Drug control, Nigerians 11 J. College of Med, Dec 2012;17(2) Prevalence and Control of Hypertension Anakwue RC, Arodiwe EB , Ofoegbu EN INTRODUCTION Diabetes mellitus (DM) is an endocrine disease, defined by high blood glucose levels, but with a prominent vascular component. The major cause of death in treated diabetic patients is due to cardiovascular problems (70%), followed by renal failure (10%), and infections (6%).1 The underlying vascular component is so significant that the complications of diabetes mellitus are usually divided according to macrovascular (coronary artery disease, cerebrovascular disease, peripheral vascular disease) and microvascular events (retinopathy, 2 nephropathy, neuropathy). One of the extremely common cardiovascular risk factors in patients with type 2 diabetes is hypertension. Hypertension may precede diabetes mellitus, be diagnosed at same time as diabetes or may be as a result of diabetic nephropathy. Whenever it occurs, it is the greatest contributor to increased morbidity and mortality in macro-vascular and microvascular events in type 2 DM.3 Macro-vascular complications are more common; up to 80% of patients with type 2 diabetes will develop or die of macrovascular disease4-12 and the costs associated with macro-vascular disease are greater than those associated with micro-vascular disease13 However, while some observational evidence suggests that the level of glycemia is a risk factor for macrovascular disease,14-18 experimental studies to date have not clearly shown a causal relationship between improved glycemic control and reductions in serious cardiovascular outcomes.3 Hypertension is one of the highly prevalent risk factors for macro-vascular events affecting up to 60% of patients with type 2 DM. Hypertension is known to increase morbidity and mortality among patients with diabetes mellitus. The control of hypertension is dramatically effective in reducing risk for cardiovascular events and 12 mortality and does so within a 4- to 6-year period.19-25 Glucose control is clearly effective only in reducing microvascular end points, but to date only intermediate outcomes have been shown to be reduced. The UKPD study demonstrated that intensive hypertension control is more effective than intensive glycemic control in reducing macro-vascular and micro-vascular events as well as all cause mortality.3 The benefits of intensive hypertension control (diastolic blood pressure, 87 mm Hg vs. 82 mm Hg) dramatically outweighed those of intensive glucose control (mean hemoglobin A1c level, 7.9% vs. 7.0%), with substantially greater (by two- to fivefold) absolute risk reductions for all published outcomes.3 It is not just the UKPD but also the Hypertension Optimal Treatment (HOT )26 Trial, has demonstrated that cardiovascular mortality and total mortality were reduced by 43% when blood pressure is reduced to <130/80mmHg in diabetic patients with hypertension. The interruption of the rennin-angiotensinsystem (RAS) is considered to be the cornerstone of pharmacologic therapy to reduce macrovascular and microvascular complications in hypertensive type 2 DM patients, mediated by antihypertensive, antiinflammatory, antiproliferative, and 27 oxidative stress lowering properties. There is evidence, that ACE inhibitors, angiotensin-receptor blockers and diuretics, , may be superior to ß-blockers and calciumchannel blockers and the latter are probably best used as second- or third-line treatments for hypertension in diabetes 28-31 Other antihypertensive drugs may have a role in achieving desired blood pressure targets in patients with type 2 diabetes. However, there is little information on the effectiveness of these drugs in reducing micro-vascular and macro-vascular outcomes. J. College of Med, Dec 2012;17(2) Prevalence and Control of Hypertension Previous studies have noted that the antihypertensive drug compliance as well as optimal blood pressure control in diabetic patients is poor and sub optimal in sub Saharan countries, including Nigeria.32 There are few reports of hypertension and its control among DM patients from south western(Ibadan and Benin city), 32,33central (Ilorin) 34and north eastern belts of Nigeria,35 but non from the south east. The aim of this study is to determine the prevalence of hypertension and to assess anti hypertensive drug control among DM patients seen in Enugu, south east, Nigeria. METHODOLOGY The medical records of 420 adult patients of both sexes (253 females, 167 males) aged between 23 and 81 years with diagnosis of type 2 DM who were seen consecutively in the outpatient unit of University of Nigeria Teaching Hospital Enugu from January 2009 were studied. The first 420 patients that satisfied the inclusion criteria-adult patients of both sexes, with diabetes mellitus type 2, whose blood pressure was > 140/90mmHg or on antihypertensive drugs, were selected. The anthropometric data- age, sex, weight, height, fasting blood sugar, blood pressure of the patients were documented. Diagnosis of diabetes mellitus was made using a fasting blood sugar of 7.0 mmol/liter (126mg/dl) according to the World Health Organization guidelines.35 The last clinic blood pressure was recorded, observing the usual standard by taking measurements in the sitting position on two occasions at least 15 minutes apart and the average recorded. Assessment of BP control was based on the American Diabetes Anakwue RC, Arodiwe EB , Ofoegbu EN Association guidelines36 for optimal BP control in patients with diabetes. The Accousson’s mercury sphygmomanometer was used. Hypoglycaemic and antihypertensive drugs given in the last visit were recorded and classified. RESULTS Out of 420 DM patients studied, those with a combination of diabetes and hypertension were significantly more than those with diabetes only (p<0.001). There were also more females than males. The diabetic hypertensives were also significantly older than the non diabetic patients ( p<0.001) (table 1). Sixty percent of the diabetic patients had hypertension with systolic and diastolic blood pressures > 140/90mmHg with mean systolic and diastolic blood pressures of 152.6mmHg ±22.2 and 96.6mmHg±9.9 respectively. The blood pressure control pattern is shown in figure 1. Only 18.3% (46) and 21% (53) of these patients had their mean systolic and diastolic blood pressure controlled to ≤ 130mmHg and ≤ 80mmHg respectively. Altogether 12% (51) DM patients had their blood pressure controlled to below 130/80mmHg. About12.3% (31) of the patients who had blood pressure of more than 135/85mmHg±9.2 were not on anti hypertensive drug treatment. Forty percent of all the diabetic patients had normal blood pressure with mean systolic and diastolic blood pressures of 123.4mmHg ±3.4and 72.4mmHg ±10.6 respectively. The frequency of antihypertensive drugs is shown in table 2. Most patients were on 1 and 2 drugs (63%) and only very few (about 20%) were on 3 and 4 drugs. TABLE 1 :Characteristics of Patients Studied No studied Mean Age(yrs) All Patients Diabetes Only 420 59.9± 10.2 176 (42%) 52.6 ±9.5 Diabetic hypertensive 244(58%) 57.9 ±12.7 P value 0.001 0.001 Prevalence and Control of Hypertension M/F Mean Dur(yrs) Mean BMI(kg/m2) Mean SBP(mmHg) Mean DBP(mmHg) Anakwue RC, Arodiwe EB , Ofoegbu EN 167/253 8.2± 6.2 27.4 ±4.5 137.4 ±11.3 84.4 ±10.6 70/98 8.6 ±8.7 26.7± 5.5 121.5± 4.8 73.4 ±10.4 97/155 9.1 ±5.8 27.9± 4.7 152.6± 22.2 96.6 ±9.9 0.24 0.68 0.022 0.00 0.00 TABLE 2 : Frequency of antihypertensive drug combination in diabetic patients studied Number of different drug classes 0 1 2 3 4 Number of diabetic patients (%) 31 (12.3) 68 (27) 103 (40.9) 45 (17.8) 5 (2%) The classes and pattern of antihypertensive pharmacotherapy are depicted in figure 2. Angiotensin converting enzyme inhibitors was the most frequently prescribed drug for the hypertensive diabetics (64%). Angiotensin receptor blocker was prescribed in only 12% of hypertensive diabetics. Diuretics, calcium channel blockers and central acting agents were prescribed in 35%, 17% and 8% of hypertensive diabetics respectively. No beta blockers were given. Angiotensin converting enzyme inhibitors and angiotensin receptor blockers were also prescribed in 15% of diabetics who had normal blood pressure for renal protective effects. The study showed that the average prescribed dose of Angiotensin converting enzyme inhibitors (ACEI) and Angiotensin receptor blockers (ARB) were on the low side of recommended dose. The percentage of hypertensive diabetics that achieved the median recommended doses of ACEI/ARB were very low, ranging from 12 to 20%.(table 3) 70 60 50 % of Patients on Drugs 40 30 20 FIGURE 1: The pattern of antihpertertensive drugs prescribed in percentages:ACEI-Angiotensin Converting enzyme inhibitors, ARB-Angiotensin receptor blockers, CCB-Calcium channel blockers, DIU-Diuretics, CENTRAL-Central acting drugs. 10 0 ACEI ARB CCB DIU CENT Antihypertensive Drug Classes TABLE 3 : The recommended ACEI/ARB target dose in Hypertensive patients and the prescribed doses in the study group ACEI/ARB drugs Lisinopril Enalapril Ramipril Valsartan Losartan Recommended dose range in mg(median dose in mg) 10-40(25) 5-40(22.5) 5-20(12.5) 80-320(200) 50-100(75) 13 Average Prescribed dose in mg 8 7 5 160 50 J. College of Med, Dec 2012;17(2) % of study patients achieving the median dose 20 15 12 18 16 Prevalence and Control of Hypertension Anakwue RC, Arodiwe EB , Ofoegbu EN DISCUSSION Hypertension is a major cardiovascular disease risk factor and when present in diabetic patients increases the cardiovascular disease burden substantially. It has been documented that hypertension in diabetic patients markedly increases the risks of coronary heart disease, stroke, nephropathy and retinopathy.37,38,39Indeed, when hypertension coexists with diabetes, the risk of CVD is increased by 75%37,40 Reports of prevalence of hypertension in diabetic patients help to assess the added risks it poses in management. It also exposes the weaknesses and shows the vigour in implementing already recommended guidelines. The prevalence of hypertension among diabetics in this study, done in Enugu, south eastern Nigeria (60%) is comparable to that obtained in Ibadan, south western Nigeria (57%) 32 and Benin city (59%)33 ,Ilorin (63%)34 and Sweden (56%), 41but understandably lower than that of United kingdom(73%)3 and USA (77%)2 were diet, physical inactivity and obesity have combined to place hypertension and diabetes as competing risk factors of cardiovascular disease in these two countries. The Swedish and American studies were nationwide surveys. Our study and that from Ibadan were hospital based and we await a nation-wide survey to provide the true prevalence of diabetes in Nigeria. Diabetic patients in Cameroon exhibit a very high prevalence of hypertension (66%) and are about three times more affected than the general population42. A study conducted in Kenya during the year 2005 to determine the proportion of specific cardiovascular risk factors in ambulatory patients with type 2 DM reported that 50% of the patients had HTN 43. The recent EPIDIAM Study conducted in 525 type 2 individuals in three Moroccan regions reported that 70.4% of the individuals had HTN 44.In India about 50% of diabetic patients have hypertenson45. In a cohort study in China the age- and sex-adjusted prevalence of hypertension among diabetic subjects was twice that of non diabetic subjects (30.6 vs. 16.4%, P < 0.0005). 46 Globally, the frequency of diabetic hypertension in diabetic population is almost twice as compared to non-diabetic general population.2 Hypertension and diabetes mellitus are really deadly cardiovascular duets. Generally, hypertension in type 2 diabetic persons clusters with other CVD risk factors such as microalbuminuria, central obesity, insulin resistance, dyslipidaemia, hypercoagulation, increased inflammation and left ventricular hypertrophy. 47 This clustering risk factor in diabetic patients ultimately results in the development of CVD, which is the major cause of premature mortality in patients with type 2 diabetes. In all there is now considerable evidence for an increased prevalence of hypertension in diabetic persons. 48 Blood pressure goals in diabetics are lower and thus more difficult to control. Globally, 25% of hypertensive diabetics achieve control. 39 The control achieved in this study(12%) is comparable to that in Ibadan-Nigeria (12%) 32, Ilorin-Nigeria(11%)34 but lower than that of United Kingdom (<27%),3Sweden (33.3%)41 and USA (35.5%).3 were there are better care for patients with cardiovascular risk factors such as hypertension and diabetes mellitus. The mean systolic and diastolic blood pressure for the hypertensive diabetic patients in our study was high (153/97mmHg). The poor rate of control of hypertension among hypertensive diabetics in this study may be due to inadequate optimization of the antihypertensive agents. The same reason was also adduced for the control in Ibadan and Ilorin studies. Majority of the antihypertensive prescriptions in this study were 1 or 2 drugs in combination but studies have recommended 3 drugs as required for optimal control of hypertension in diabetics 16 J. College of Med, Dec 2012;17(2) Prevalence and Control of Hypertension Anakwue RC, Arodiwe EB , Ofoegbu EN particularly in those whose systolic blood pressure is 25-30mmHg above target goal.3 In fact the United Kingdom Prospective Diabetic study found out that one-third of patients needed three or more antihypertensive drugs in combination, and two-thirds of treated patients needed two or more for control of blood pressure.3 It should be emphasized that blood pressure targets in diabetics should be aggressive. For example, a four point blood pressure difference in the HOT trial (84 to 81mmHg) resulted in a decrease by 50% in cardiovascular events in patients with DM. The study noted that the risk reduction seen with hypertension control in patients with diabetes is substantially greater than that seen in persons in the general population who have similar blood pressure levels26 The ACE inhibitors and particularly the ARB are underutilized in this study (64% and 12% respectively) gave rise to the poor control of hypertension. The Ibadan and Ilorin studies 32,34 had also recorded ACE inhibitors in only 52% and 44.3% respectively of their prescriptions. The Ibadan study pointed at the high cost of ACE inhibitors/ARB as possible reason for its low patronage. It has been recommended that treating people with diabetes and at least one other major cardiovascular risk factor with an ACE-inhibitor produces a 25-35% lowering of the risk of heart attack, stroke, overt nephropathy or cardiovascular death. 39 It has been noted that in patients with bilateral renal artery stenosis, ACE inhibitors can cause renal insufficiency. To help detect the presence of undiagnosed bilateral renal artery stenosis, physicians should monitor the serum creatinine level at baseline and one week after initiation of ACE inhibitor therapy. Diuretics were not used optimally in this study. This finding is in keeping with the Ibadan study. 33 Diuretics are however recommended in the multiple regimen required to control hypertension inspite of their diabetogenic potential. Diuretics, particularly, hydrochlorothiazides when used in low doses, have no significant disturbance on glucose metabolism and are useful in blacks in the control of hypertension. Thiazide diuretics have been shown to benefit patients with diabetes and systolic hypertension and lower dosages of thiazides (e.g., hydrochlorothiazide 12.5 mg per day) are generally well tolerated and not associated with adverse metabolic effects. 4 Thiazide diuretics are not as effective in patients with renal insufficiency; in such patients, loop diuretics are preferred. In general, diuretics are effective, affordable and available for the treatment of hypertension in diabetes mellitus. Calcium channel blockers were prescribed in 17% of the diabetic hypertensive patients studied. Non-dihydropyridine calcium channel blockers were not prescribed in this study and in other studies in Nigeria. Both the non DHP (diltiazem and verapamil) and the DHP CCBs (amlodipine, felodipine, and others) reduce CVD events in people with diabetes and hypertension. 49,50 NonDHP CCBs significantly reduce albuminuria and may slow the progression of proteinuric renal disease.51 In contrast, DHP CCBs inconsistently reduce albuminuria and are less effective than ACE inhibitors or ARBs in slowing the progression of diabetic nephropathy. 51However, DHP CCBs effectively lower blood pressure and can be safely combined with an ACE inhibitor or ARB to slow the progression of diabetic nephropathy. 51 B-blockers were not prescribed in this study unlike in the Ibadan study were it was used in 7% of the patients. 33 17 J. College of Med, Dec 2012;17(2) Prevalence and Control of Hypertension Anakwue RC, Arodiwe EB , Ofoegbu EN Beta blockers worsen hyperglycemia and block adrenergic symptoms. This may produce dangerous hypoglycemia without giving the patient enough time to react by taking food to increase the blood glucose level. It is however useful in post myocardial infarction patients and as an antiarrhythmic agent. The effectiveness of beta blockers was demonstrated in the UK Prospective Diabetes Study Group, where atenolol was comparable with captopril in reduction of CVD outcomes52,53. Although these agents have been associated with adverse effects on glucose and lipid profiles and implicated in new onset diabetes in obese patients, 4 they are not absolute contraindication for use in diabetic patients. In fact, carvedilol, which has both alpha and beta receptor blocking properties, has been shown to induce vasodilatation and improve insulin sensitivity52. Blood pressure lowering with carvedilol or metoprolol reduces microalbuminuria by 43 and 30%, respectively, when added to ACE inhibitors or ARBs. 47 However, carvedilol is nearly 50% more effective than metoprolol for preventing progression from normoalbuminuria to microalbuminuria.54 Central acting drugs were used in only 8% of diabetic hypertensive studied. This drug was not used in any of the centers in Nigeria. This group of drugs are prescribed because they are cheap and affordable. Our study noted that thirteen percent of the diabetic patients who were hypertensive were not placed on antihypertensives. The reason for this is not clear except that the patients had mild hypertension (135/85mmHg±9.2) and may have been erroneously classified as non hypertensive. These patients are under the threat of renal impairment and other end organ damage. Our study also showed inertia in the attainment of target doses for the ACEI and ARB was only 12-20% of median doses of ACEI and ARB. It is not clear if the distraction of treating diabetes mellitus and the adverse effects of these drugs contributed to the below target dose prescription of these drugs. CONCLUSION It is clear from this study that blood pressure control in hypertensive diabetic patients is unsatisfactory even in a tertiary hospital in Nigeria. The study found out that inspite of high prevalence of high blood pressure, hypertension was managed less intensively in patients with diabetes. Findings of other tertiary health institutions in Nigeria and other parts of Africa run parallel to that of our study. This is inspite of the consensus that blood pressure control in diabetic patients has dramatic effects in reducing cardiovascular morbidity and mortality. Clinicians and patients should be reminded that even though blood glucose control is important, aggressive blood pressure control in diabetics is top priority in preventing adverse cardiovascular events which causes the highest mortality in the average population of type 2 diabetics. 30 Apart from issues on pharmacotherapy, poor control of hypertension in diabetic patients may be traced to non pharmacological factors which include inadequate recognition of the role of therapeutic life style changes, poverty and proper health education. These non drug measures are obviously not the focus of this study but they can not escape being mentioned here. Availability of generic drugs and health insurance scheme may help to place antihypertensive drugs at the reach of the patients. 18 J. College of Med, Dec 2012;17(2) Prevalence and Control of Hypertension Anakwue RC, Arodiwe EB , Ofoegbu EN REFERENCES 1. Gale EAM, Anderson JV. Diabetes Mellitus and other disorders of metabolism. Kumar P, Clark M, In Clinical Medicine, 6th edition, Elsevier Saunders 2005;1101-1152. 2. Diabetes in America. 2nd ed. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 1995. 3. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group Lancet. 1998; 352:837-53. 4. Harris MI. Epidemiology of diabetes mellitus among the elderly in the United States Clin Geriatr Med. 1990;6:703-719. 5. Meigs JB, Singer DE, Sullivan LM, Dukes KA, D'Agostino RB, Nathan DM, et al. Metabolic control and prevalent cardiovascular disease in non-insulin-dependent diabetes mellitus (NIDDM): The NIDDM Patient Outcome Research Team Am J Med. 1997;102:38-47. 6. Morrish NJ, Stevens LK, Fuller JH, Keen H, Jarrett RJ. Incidence of macrovascular disease in diabetes mellitus: the London cohort of the WHO Multinational Study of Vascular Disease in Diabetics Diabetologia. 1991; 34:584-589. 7. Wingard DL, Barrett-Connor EL, Scheidt-Nave C, McPhillips JB. Prevalence of cardiovascular and renal complications in older adults with normal or impaired glucose tolerance or NIDDM. A population-based study Diabetes Care. 1993; 16:1022-1025. 8. de Grauw WJ, van de Lisdonk EH, van den Hoogen HJ, van Weel C. Cardiovascular morbidity and mortality in type 2 diabetic patients: a 22-year historical cohort study in Dutch general practice Diabet Med. 1995;12:117-122. 9. Garcia MJ, McNamara PM, Gordon T, Kannel WB. Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up study Diabetes. 1974;23:105-111. 10. Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study JAMA. 1979; 241:2035-2038. 11. Kleinman JC, Donahue RP, Harris MI, Finucane FF, Madans JH, Brock DB. Mortality among diabetics in a national sample Am J Epidemiol. 1988; 128:389-401. 12. Królewski AS, Czyzyk A, Janeczko D, Kopczyski J. Mortality from cardiovascular diseases among diabetics Diabetologia. 1977; 13:345-350. 13. Economic consequences of diabetes mellitus in the U.S. in 1997. American Diabetes Association Diabetes Care. 1998; 21:296-309. 14. The effect of intensive treatment of diabetes on the development and progression of longterm complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group N Engl J Med. 1993; 329:977-986. 15. Andersson DK, Svärdsudd K. Long-term glycemic control relates to mortality in type II diabetes Diabetes Care. 1995; 18:1534-1543. 20 J. College of Med, Dec 2012;17(2) Prevalence and Control of Hypertension Anakwue RC, Arodiwe EB , Ofoegbu EN 16. LaaksoM. Glycemic control and the risk for coronary heart disease in patients with noninsulin-dependent diabetes mellitus. The Finnish studies Ann Intern Med. 1996; 124:127130. 17. Lehto S, Rönnemaa T, Haffner SM, Pyörälä K, Kallio V, Laakso M. Dyslipidemia and hyperglycemia predict coronary heart disease events in middle-aged patients with NIDDM Diabetes. 1997; 46:1354-1359. 18. Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Predictors of stroke in middle-aged patients with non-insulin-dependent diabetes Stroke. 1996; 27:63-68. 8553405]. 19. Curb JD, Pressel SL, Cutler JA, Savage PJ, Applegate WB, Black H, et al. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic Hypertension in the Elderly Program Cooperative Research Group JAMA. 1996; 276:1886-1892. 20. Tuomilehto J, Rastenyte D, Birkenhäger WH, Thijs L, Antikainen R, Bulpitt CJ, et al. Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. Systolic Hypertension in Europe Trial Investigators N Engl J Med. 1999; 340:677-684. . 21. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study Investigators Lancet. 2000; 355:253-259. 22. Ravid M, Brosh D, Levi Z, Bar-Dayan Y, Ravid D, Rachmani R. Use of enalapril to attenuate decline in renal function in normotensive, normoalbuminuric patients with type 2 diabetes mellitus. A randomized, controlled trial Ann Intern Med. 1998; 128:982-988. 23. Hypertension in People with Type 2 Diabetes (non-insulin dependent diabetes) knowledge - based diabetes – specific guidelines, International Diabetes Federation (European Region) on behalf of the St Vincent Declaration Initiative. 24. Hypertension Control - Report of a WHO – Expert Committee World Health Organisation, 39, 6th Cross Wilson Garden, Banglore-560027. Panther Publishers Private Limited, 1996; 42. 25. Mogensen CE. Combined high blood pressure and glucose in type 2 diabetics: double jeopardy. British trials show clear effects of treatment, specially blood pressure reduction. Selections from Br Med J 1999; 14: 984-989. 26. Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group Lancet 1998; 351:1755-1762. 27. Candido R, Bernardi Stella; Fabris Bruno. Hypertensio and Diabetes: Emphasis on the Renin-Angiotensin System in Atherosclerosis, Current Hypertension Reviews,2009 :5:3:181-201. 21 J. College of Med, Dec 2012;17(2) Prevalence and Control of Hypertension Anakwue RC, Arodiwe EB , Ofoegbu EN 28. Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with noninsulin-dependent diabetes and hypertension N Engl J Med. 1998;338:645-652. 29. Tatti P, Pahor M, Byington RP, Di Mauro P, Guarisco R, Strollo G, et al. Outcome results of the Fosinopril Versus Amlodipine Cardiovascular Events Randomized Trial (FACET) in patients with hypertension and NIDDM Diabetes Care. 1998; 21:597-603. 30. Lindholm LH, Hansson L, Ekbom T, Dahlöf B, Lanke J, Linjer E, et al. Comparison of antihypertensive treatments in preventing cardiovascular events in elderly diabetic patients: results from the Swedish Trial in Old Patients with Hypertension-2. STOP Hypertension-2 Study Group J Hypertens. 2000;18:1671-1675. 31. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and LipidLowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002; 288:29812997. 32. Arije A, Kuti M, Fasanmade A, Akinlade K, Ashaye A, Obajimi M, Adeleye J. Control of hypertension in Nigerians with Diabetes Mellitus: A report of the Ibadan Diabetic / Kidney Disease Study Group. Int J Diabetes & Metabolism 2007; 15: 82-86 33. Unadike BC, Eregie A, Ohwovoriole AE. Prevalence of hypertension amongst persons with diabetes mellitus in Benin City, Nigeria. Niger J Clin Pract 2011; 14:300-2 34. Okoro E, Oyejola B. Inadequate control of blood pressure in Nigerians with diabetes. Ethn Dis 2004; 14:82-86. 35. The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997; 20: 1183–1197 36. American Diabetes Association-Position statement. Treatment of hypertension in adults with diabetes. Diabetes Care 2002; 25: supplement 1: S71–S73. 37. Sowers J R, Epstein M, Frohlich E D, “Diabetes, hypertension, and cardiovascular disease: an update”, Hypertension 2001; 37:4: 1053–1059. 38. Bakris G, Williams M, Dworkin L, Elliott W, Epstein M, Toto R et al. Preserving renal function in adults with hypertension and diabetes: A consensus approach. Journal of Kidney Diseases 2000; 36:3: 646. 39. Sowers J R, Haffner S. Treatment of cardiovascular and renal risk factors in the diabetic hypertensive. Hypertension 2002; 40: 6: 781–788. 40. Adler A I, Stratton I M, Neil H A W, Yudkin J S, Matthews D R, Cull C A et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes ,UKPDS 36 : prospective observational study. BMJ 2000; 321:7:258: 412–419. 41. Nilsson PM, Gudbjörnsdottir S, Eliasson B, Cederholm J et al.Hypertension in diabetes: trends in clinical control in repeated large-scale national surveys from Sweden. Journal of Human Hypertension 2003; 17:37–44. 22 J. College of Med, Dec 2012;17(2) Prevalence and Control of Hypertension Anakwue RC, Arodiwe EB , Ofoegbu EN 42. Choukem SP, AP,Kengne AP, Dehayem, YM, Simo NL, Mbanya JC Hypertension in people with diabetes in sub-Saharan Africa: Revealing the hidden face of the iceberg Diabetes Research and Clinical Practice 2007; 77: 2 : 293-299. 43. Otieno CF, Vaghela V, Mwendwa FW et al “Cardiovascular risk factors in patients with type 2 diabetes mellitus in Kenya: levels of control attained at the outpatient diabetic Clinic of Kenyatta National Hospital, Nairobi,” East African Medical Journal, 2005; 82 : 12 : S184–S190. 44. Berraho M, Achhab YE, Benslimane A, et al “Hypertension and type 2 diabetes: a crosssectional study in Morocco (EPIDIAM Study),” The Pan African Medical Journal 2012:11:52. 45. Jain S, Patel JC. Diabetes and hypertension. J Diab Assoc India 1983; 23: 83-6. 46. Tong-Yuan Tai, Lee-Ming Chuang, Chien-Jen Chen, Boniface J Lin. Link between Hypertension and Diabetes Mellitus Epidemiological Study of Chinese Adults in Taiwan. Diabetes Care November 1991; 14: 11; 1013-1020 47. Arauz-Pacheco C, Parrott M A, Raskin P. The Treatment of Hypertension in Adult Patients with Diabetes. Diabetes Care 2002; 25: 1: 134–147. 48. Ravid M, Lang R, Rachmani R, Lishner M. Long-term renoprotective effect of angiotensin-converting enzyme inhibition in non-insulin-dependent diabetes mellitus. A 7year follow-up study. Arch. Intern. Med. 1996; 156: 3: 286–289. 49. Tuomilehto J, Rastenyte D, Birkenhager WH et al. Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. N Engl J Med 199; 340:677 –684. 50. Bakris GL, Gaxiola E, Messerli FH et al. Clinical outcomes in the diabetic cohort of the International Verapamil SR-Trandolapril Study 2004; Hypertension 44:643 –648. 51. Nathan S, Pepine CJ, Bakris GL: Calcium antagonists: effects on cardio-renal risk in hypertensive patients. Hypertension 2005;46 : 637–642. 52. Group UKPDS. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ 1998; 317:7160: pp. 713–720. 53. Giugliano D, Acampora R, Marfella R, De Rosa N, Ziccardi P, Ragone R et al. Metabolic and Cardiovascular Effects of Carvedilol and Atenolol in Non-Insulin-Dependent Diabetes Mellitus and Hypertension: A Randomized, Controlled Trial. Ann. Intern. Med 1997; 126:12: 955–959. 54. Bakris GL, Fonseca V, Katholi RE et al : for the GEMINI Investigators: Differential effects of β-Blockers on albuminuria in patients with type 2 diabetes. Hypertension 2005; 46:1309 –1315. 23 J. College of Med, Dec 2012;17(2)
© Copyright 2026