Time to Refocus Your Strategy on Creating Value
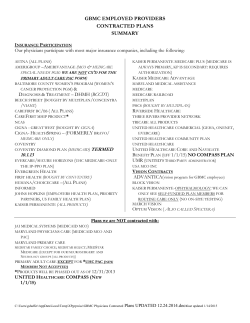
BDC Insights March 2015 Launching 1,000 Ships? Time to Refocus Your Strategy on Creating Value Steve Weylandt and Dave Anderson What Follows: Value Transition Underway Market Segmentation Growing More Complex “A successful transformation strategy requires focusing on the growth and alignment of programs that create value for consumers.” Launching 1,000 Ships Building Transient Advantage in Healthcare Markets Value Theory Must Underpin Strategy Strategic Focus, Innovative Culture & Effective Execution Keys to Success Value Transition Underway The transformation of the nation’s healthcare system to a value-based, consumercentered model from a volume-based, system-centered model is well underway. It is being fueled by government reforms, technology development, commercial market innovations, and a growing retail healthcare market. CMS’s Innovation Center has launched more than 50 different demonstration program initiatives in the past five years to test new value payment and service delivery mechanisms. These programs range from the Medicare Shared Savings Program (MSSP), PatientCentered Medical Home programs, and Bundled Payments to initiatives focused on Medicaid-Medicare Dual Eligible Enrollees. These innovation efforts all share a common goal of improving quality and reducing costs. In January, HHS Secretary Sylvia Burwell tied all these value improvement activities together by announcing a goal of tying 50 percent of all Medicare payments to value-based 1 models of care such as Accountable Care Organizations (ACOs), Medicare Advantage, Medical Homes/Medical Neighborhoods, and bundled payments by 2018. Coupled with this, HHS also set a goal of tying 90% of all payments under the remaining fee-for-service Medicare to measures of quality or value by the end of 2018. Along with reform-based efforts to control costs and improve the value of care, the ACA significantly expanded access. The Congressional Budget Office (CBO) projects that as many as 38 million previously uninsured persons will receive healthcare benefits by 2018 from the Insurance Exchanges or through Medicaid and CHIP. During this same period, CBO projects that the number of people with employer-based coverage will rise modestly from 156 million to 165 million. As a result of these trends, provider systems need to look at government programs as their major source of future organic volume growth. Given HHS’s recent announcements raising the bar on value-based payments, many systems are challenged in developing the right value-based strategies for successful participation in these government programs, as well as positioning themselves for key commercial markets that are also moving rapidly to valuebased contracts. Market Segmentation Growing More Complex Market segmentation and the financial models underlying this transformation are becoming increasingly complex. In the past, the payer market’s main segments were commercial insurance, Medicare, Medicaid, and the uninsured. Now, commercial insurance has been segmented into several sub-markets ranging from traditional large group products to direct employer contracts, to new public and private health insurance marketplaces (exchanges). Health systems must develop multiple network configurations to deal with new narrow, tailored, and high-performance network products designed for these various segments, as illustrated in Figure 1. Figure 1: Market Pressures & Responses 2 Segmentation is also growing in the public sector. In addition to traditional Medicare and Medicaid, we now have the Medicare Shared Savings Program, Medicare Advantage, a variety of Medicare Special Needs Plans, Medicaid Managed Care, and Managed Care for Dual Eligibles. Another important trend is the accelerating shift from inpatient to ambulatory care. A host of new ambulatory and outpatient competitors are beginning to compete in primary care and urgent care markets, with in-store clinics priced below the physician’s office and far below hospital clinics and emergency rooms. Health systems that fail to adapt could lose their profitable ambulatory business to Target, Walmart or CVS. Looking ahead, ambulatory care is under attack by phone consults and e-visits, home monitoring, and rapid growth in telemedicine. What is delivered in a clinic today will be delivered in the home tomorrow. As market complexity has increased, the lines between payers and providers have blurred. A recent survey reported that 13% of the nation’s provider systems now own health plans. An additional 20% are planning to secure insurance licenses in the next five years.1 At the same time, insurers are entering the provider space. United HealthCare and Humana have both acquired numerous physician practices, and Anthem, Humana, Aetna, Cigna, United, and others (including many regional Blue Cross plans) are partnering with health systems to manage risk. Most provider systems have bought into the notion, intellectually at least, that the core requirement of market reform is to maximize value to patients while maintaining the financial viability of their delivery systems. This means changing their business model from a volume- driven system to a much more complex model where providers take responsibility for numerous population segments with varying demands and payment approaches, all shifting rapidly to value-based incentives. Launching 1,000 Ships To date, most health systems’ response to today’s complex market and government pressures has been to “launch 1,000 ships,” hoping some of them will find a passage to the promised land of value-based care. (See Figure 2.) Figure 2: Cost & Quality Pressure Requires Focus Health systems must address market pressures while transitioning to value. Launch a 1,000 Ships? Cost & Quality Pressures Private/Public Exchanges 1 High Deductible Plans Direct to Employer Reference Pricing Network Affiliations Centers of Excellence Narrow Networks & Tiered Network Value Based Benefits/Risk Contracts • • • • Segments • • • • • • • Services • • • • Unique Mission Medicaid TANF Medicare/Medicaid Duals Medicare FFS Medicare MA Commercial ASO Commercial Fully Insured Commercial HIX/Private Inpatient Outpatient Surgical Routine Outpatient Surgical Specialized Outpatient Diagnostic Ancillary Cancer Care Clinic Rehab ED Treat & Release Transplant Academic, Research Non-Profit Private Complexity of Cases Subsidization of Medicare/Medicaid • Payer/Broker/Employer/ Consumer Dynamics • • • • • McGrath, Rita Gunther, “Transient Advantage,” Harvard Business Review, June 2013. 3 For health systems that can afford to launch 1,000 ships, this is a reasonable response to a chaotic environment. No amount of business planning can predict exactly which ships will find safe harbors, so diversification is appropriate. In some ways, the business of healthcare is becoming like the oil business: If you want to strike oil, you need to drill a lot of wells. But a business strategy based on launching 1,000 ships has its own challenges. New programs launched to meet specific government reform efforts, or to market directly to consumers, can miss the mark, squandering resources without contributing to the mission or profitability of the system. Building Transient Advantage in Healthcare Markets The traditional strategy playbook for health systems, as for most industries, has been to develop and implement strategies that build “sustainable competitive advantage” through physician alignment, new technology, superior brand position, and the like. But, long-range planning aimed at creating sustainable competitive advantage is unlikely to yield as much as it has in the past. As boundaries between market segments become porous, competitive position can be challenged and put at risk from unexpected sources, or simply because of unanticipated market shifts. Sustaining competitive advantage over a long period of time in this type of competitive environment is becoming a fool’s errand. As an alternative, healthcare systems may want to adopt what Professor Rita Gunther McGrath of the Columbia Business School describes as a strategy of building “Transient Advantage.” This involves bringing new business initiatives to scale rapidly, managing short life cycles to maximize near-term benefits, and unsentimentally “disengaging” from them when life cycles start trending down.1 Building transient advantage requires a portfolio manager’s mindset. You will win if you make good shortterm bets, maximize benefits from these investments, get out at the right time, and move on. Success in today’s healthcare markets requires health systems to cycle rapidly through the planning and development of new programs and to manage a pipeline of initiatives aimed at meeting market needs, some of which may be short lived. Most systems will need to operate in a market with a variety of different contract models, with varying degrees of risk while the value transition plays out. Building a business based on transient advantage is not just a matter of throwing out traditional concepts of business strategy. Building transient advantage has its own playbook, and over the years, many companies have prospered by following these rules. They include: • Pick the right “arenas” for your investments. The question of where to invest for transient advantage requires an understanding of the “value theory” of your health system – i.e., how it delivers value to customers.2 This is discussed below. To build transient advantage, McGrath believes that the most fertile arenas are likely to be those that meet immediate needs of healthcare consumers (“customer experiences and solutions”). “Go-to-market” initiatives – new risk contracts with employers, new retail care delivery vehicles, etc. – are likely to be less risky and more productive than large, expensive infrastructure development projects. 2 Zenger, Todd, “What Is the Theory of Your Firm?”, Harvard Business Review, June 2013. 4 • Choose champions wisely. Introducing new products or process innovations is an entrepreneurial activity, and you need to put natural entrepreneurs in charge of your key initiatives. Traditionally, health systems have been havens for administrators, not risktakers and “intrapreneurs.” One potential source of champions is independent physicians on your medical staff who do business in the chaotic healthcare marketplace every day. In academic health systems, good researchers with strong clinical practices can also make good champions, since they compete daily in the fast-moving, highly competitive market for ideas. • Set up champions for success. Entrepreneurs need clear accountability, relevant metrics, and appropriate carrots and sticks to guide their efforts. Traditional metrics like 10-year discounted cash flow forecasts are more likely to kill off innovations than support them. Measuring new revenue, on the other hand, or tangible cost reduction, is useful for both project leaders and executive “portfolio managers.” And, while champions need to be rewarded when they succeed, punishing them for good tries that fail – e.g., by pulling them out of the game – is no way to develop their skills. • Make small initial investments and condition future $ on success. One of the most innovative U.S. companies over many years has been 3M Corporation, whose culture is defined by the motto, “Make a little. Sell a little. Make a little more.” This incrementalist philosophy is especially important for health systems pursuing early- stage innovations (which, as McGrath points out, is where you need to play to build transient advantage). Because the risk is great, initial investments must be contained until the initiatives prove to have “legs.” • Develop a sponsorship culture. Champions need sponsors. In the venture market, this role is played by venture capitalists who have a direct financial stake in the success of their entrepreneurs. In health systems, senior leaders need to play this role, providing release time and seed funding, candid advice and counsel, and protection from traditional organizational processes that could undermine their efforts. A company culture that develops champions also needs to develop sponsors, and incentive compensation for senior executives should recognize this as an important institutional priority. One final requirement for building transient advantage is scale and market reach. Larger organizations with more resources and greater ability to take risks have a significant advantage (as long as they don’t let their size get in the way). The most recent economic forecasts for the hospital industry from the rating agencies – Fitch, Moody’s and Standard & Poor’s – continue to favor the largest and most geographically dispersed health systems. As a result, we expect the pace of mergers to continue to be brisk, since smaller systems that lack scale, physician networks, or capital to grow, are expected to be less profitable, with operating margins of -0.5% to 1.5% – a level of financial performance insufficient to fund a “1,000 Ships” transition strategy. Mergers are not the only way to achieve scale. An increasing number of organizations are banding together in alliances or “Super ACOs” to engage in joint population health management.3 Over 30 Super ACO alliances have been formed in the past three years, with the goal of building common infrastructure and programs necessary for population health management. As alliances, they offer an alternative to asset mergers or acquisitions and may be a way for smaller community hospital systems to play in larger markets while maintaining their independence. Since they are not formal mergers, they also meet the “transient advantage” test of being easier to take apart if the business opportunity they are designed around proves short-lived.4 3 Anderson, Dave and Hogan, Neal, “Emerging Super ACOs Fill Unique Needs,” hfm Magazine, Oct 2013. The development of “Super ACOs” Regional Health Care Alliances designed to promote population health management has been growing with more than 30 alliances nationally. While promising developments, most are still in the organizational phase and have yet to report concrete results. 4 5 Value Theory Must Underpin Strategy As Todd Zenger has pointed out, successful organizations need a “value theory” that defines how they will combine their unique resources and assets with external assets. For health systems, a working value theory comprises: • foresight into the future health system market • vision of how the system can optimize future growth • insight into which internal capabilities will best enable growth • critical analysis of how assets can be leveraged to create value for consumers • willingness to move out of established program(s) and move into something new Michael Porter and Tom Lee believe that health systems need to adopt a consumerdriven “Value Agenda” – improving what matters to patients relative to the cost of providing it – as their value theory.5 In their view, successful healthcare transformations will be those that grow and align programs to create value for consumers. Strategic Focus, Innovative Culture, & Effective Execution Keys to Success Launching 1,000 ships in today’s healthcare marketplace requires strategic focus, a culture that encourages innovation, and effective execution. Together, these success factors will enable you to: • Make sure you are addressing the right problems (i.e., make sure your ships are heading in the right direction) • Sharpen your understanding of consumer needs • Conduct productive experiments, learn from them, and realize benefits while they are valuable • Remain agile and able to shift resources to rebuild transient advantage as the market shifts In addition to improving your chances of success, taking these steps will raise the bar for other healthcare providers, and play an important role in revitalizing U.S. healthcare for all of us. 5 Porter, Michael E. and Lee, Thomas H., “The Strategy That Will Fix Health Care,” Harvard Business Review, October 2013. 6
© Copyright 2026