CPD: Setting up a weight loss management service
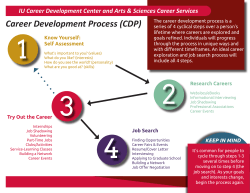
CPD Tom Maher MPSI Reflection and self-assessment Evaluation RECORD (e.g. portfolio) Learning plan Action (e.g. CE) CPD: Setting up a weight loss management service We’ve all seen the statistics countless times. We have been reminded about the obesity epidemic for years through the papers, radio, TV and online. The strange thing is, despite everybody’s knowledge and awareness, Ireland’s obesity levels have still doubled in the last 10 years. Is there an opportunity for pharmacy? “Almost one in four Irish adults are obese, a rate worse than most of Europe” – The Journal (May 2014) “Four out of five over 50s in Ireland are overweight or obese” – Irish Longitudinal Study on Ageing (July 2014) “We now know that obesity causes every disease and makes every disease worse. Nothing does that bar ageing,” – Prof Donal O’Shea, Consultant Endocrinologist (May 2014) Why set a Weight Loss Management Service? There are many different weight loss products and services out there already, with varying degrees of success but how many of them empower people to make significant permanent changes to their lifestyle? A weight loss management service is easily set up and, if done correctly, can bring additional custom and revenue to your pharmacy. IPUREVIEW DECEMBER 2014/JANUARY 2015 Background and preparation 1. Motivation What is motivation? I believe it’s when a person needs to see and feel a real reason to them to do anything, especially anything challenging. So, for example, your house needs tidying but you couldn’t be bothered, it will do as it is. You get a call that Barack Obama is on his way over and, in a flash, you have found all the energy and determination you need to have the place spotless. How can you create that for any given circumstance? How can you create that for your patients? This is where Motivational Interviewing (MI) plays a key role in dealings with your patients. If an asthma patient can’t see why he/she should bother about using the preventer inhaler, what are the chances it will be used correctly going forward? Similarly, smokers must see and feel for themselves why they should quit. The same also applies for weight loss. Changing long-standing bad eating habits and lack of exercise can be difficult to accomplish, but is possible if you create your own motivation and, as pharmacists, we can help our patients do that. Motivational Interviewing Questions Motivational interviewing is a style of counselling developed to identify and engage the patient’s intrinsic motivation for changing health-related behaviours. The technique takes practice, but it can be a very effective tool for identifying realistic goals, feasible approaches and opportunities for progress with all patients, especially those who are resistant to change or struggle to acknowledge their health problem. The method is non-judgemental, nonconfrontational and allows the patient and pharmacist to assess readiness to change together, instead of being directed by the pharmacist. Five general principles of motivational interviewing: 1. Express Empathy – see the world through patient’s eyes. Be non-judgemental; leave aside your own views and values. 2. Develop Discrepancy – facilitate patient to identify the discrepancy between current behaviour and future goals. 3. Avoid Argument – it’s counterproductive. Look for inconsistencies and consequences that conflict with important goals. 4. Roll with Resistance – defuse the resistance. Be empathetic and nonjudgemental and encourage patient to develop their own solutions and examine new perspectives. 5. Support Self-Efficacy – patient is responsible for choosing and carrying out personal change. Belief in the possibility of change is a good motivator and previous efforts and successes can be elicited to build self-confidence. 33 CPD overview Reflect and Self-Assessment o Is there a need in my locality for this service? o Have I sufficient pharmacist cover to provide this service? o Have I a good working relationships with local GPs, Public Health Nurse, etc.? o Have I a SOP in place for this service? o Is the consultation area adequate? o How will I record this patient service – paper or electronically? o Have I identified the appropriate equipment, professional and patient resources materials? Learning Plan Including a list of desired learning outcomes in a personal learning plan is a helpful self-analytical tool. o Create a list of desired learning outcomes, e.g. MI techniques, healthy eating, physical activity, body measurements. o Identify professional resources available to achieve learning objectives. o Identify patient support material and online patient resources. o Develop a realistic time line for plan. Action Activities chosen should be outcomes based to meet learning objectives. o Read this article. o Create SOP for weight loss management service. o Evaluate professional resource materials available in the pharmacy and source additional material if necessary. o Evaluate patient support material and source additional material if necessary. o Promote this new patient service. Evaluate Consider outcomes of learning and impact of learning. o Do I now feel confident to set up a weight loss management service? o Do I now feel confident to engage with my patient about weight loss? o Should I consider including cardiovascular screening as part of weight loss management service? ] o Have I met my desired learning outcomes? o Have further learning needs been identified? Record o Create a record in my CPD portfolio. As part of this record, complete an evaluation, noting whether learning outcomes were achieved and identifying any future learning needs. 34 Effective motivational interviewing encompasses the following communication techniques commonly referenced by the acronym OARS: • Some people talk about part of them wanting to change their eating patterns and part of them not really wanting to change. Is this true for you? n Open ended questions – allows patient to express their perspective and provides insights for the consultation. • On a scale from one to ten, how ready are you to make changes in your eating patterns? n Affirmations – shows appreciation and support for the patient’s statements. They can be verbal or non-verbal. n Reflective listening – adds direction to the consultation and helps focus on change statements. n Summarising – draws a number of strands together and clarifies and reflects the patient’s own thoughts back to them. Asking permission has also been shown to be a powerful tool. It communicates respect for the patient and results in increased likelihood of discussing change. In motivational interviewing, the focus shifts from giving information and advice, to helping patients explore concerns, uncertainties, reasons for change and ideas and strategies to make change happen. What does Motivational Interviewing look like? Subtle differences in how pharmacists elicit information from patients can make very meaningful differences. As an example, instead of asking closed questions such as, “Do you want to lose weight?” or “How much weight do you want to lose?” an MI approach would instead ask, “How ready do you feel to change your eating patterns?” or “How is your current weight affecting your life right now?” • How much of you is not wanting to change? • What was your life like before you gained weight? • What do you think will happen if your health behaviours don’t change? • What are your hopes for the future if you are able to become healthier? • How would your life be different if you lost weight or adopted a healthier lifestyle? • What kinds of healthy changes do you think you could make this week? 2. Collaborative goal setting Patients who need to lose weight are often asked to make a lot of changes to their diet and activity levels. There is evidence that if patients are given the opportunity to choose one behaviour change goal to focus on, success is more likely. When patients achieve a goal, their selfefficacy and confidence goes up and then more ambitious goals are set; for example, patients who set a goal to walk half a mile each day and succeed are likely to set a higher goal, for example to walk one mile each day. Other MI type questions: • What kinds of changes have you made in the past to improve your eating (or physical activity)? • What strategies have worked for you in the past? IPUREVIEW DECEMBER 2014/JANUARY 2015 Collaborative goal-setting is a process where both the pharmacist and patient negotiate a health-related goal. Research has shown that when patients participate in decisions, they are more likely to adopt the behaviours decided upon. Collaborative goal-setting does not involve the pharmacist telling the patient what to do. Telling a patient that their goal “should be to lose 10kg” is not collaboration. Instead, it is better to explore how much weight loss the patient can realistically achieve and to work on achieving that goal. 3. Considerations n Time – do you have the time to put a service like this into place? n Drop-in service or by appointment? In my view, scheduled appointments on one particular day of the week works best, as both pharmacist and patient will be prepared. n Adequate consultation room? n Advertise – posters and flyers in the pharmacy, also online, in GP surgeries, community halls, local Spar, Centra, etc. n Are you familiar with all the activities in your local area to suggest to patients who may be unaware and might consider, e.g. walking group, ramblers, exercise IPUREVIEW DECEMBER 2014/JANUARY 2015 classes in parish halls, aqua aerobics, etc. n Is this a free service, or are you going to charge? Bear in mind that organisations such as Weight Watchers and Slimming World have a joining and weekly fee – does this help focus some motivation? n Can this service have added value by adding in a Blood Pressure check also? n Knowledge and information – become familiar with motivational interviewing techniques, healthy waist measurement, BMI, ideal weight, average calories per day required for men and women, food calorie counting, detail on healthy eating, alcohol intake, recommended physical activity levels. n Documentation – create a SOP for a Weight Loss Management Service. Equipment needed n Print out leaflets on healthy eating, exercise, suggested diet plans, e.g. Healthy Eating and Active Living for Adults, Teenagers and Children over 5 Years available on www.fsai. ie, Lose weight and reduce your risk of heart disease and stroke available on www.irishheart.ie Structure n Appointment once a week for 12 weeks followed by review thereafter. n Week 1 – Assessment (40 minutes). 1.Measurements - height, weight, waist measurement. Calculate BMI and pinpoint on the chart. Explain about significance of waist measurement. 2. Motivational Interviewing technique (aiming to find out about eating habits and physical activity). n Digital weighing scales 3. Collaborative goal setting (aiming for a maximum weekly weight loss of 0.5kg1kg / 1lb-2lb). n BMI chart – available on www.healthpromotion.ie 4. Review and agree next meeting. n Waist and height measure – available from e.g. Fleming Medical n Record patient consent, details, measurement statistics and progress. (Choose paper or electronic format) n Weeks 2-12 Ongoing support (20 minutes) 1.Measurements, review and reaffirm motivation. 2. Topics, e.g. food diary, reading food labels, increasing physical activity, calorie counting. 3. Collaborative goal setting. 4. Encouragement and set rewards for goals achieved, e.g. buying music, new clothes, book a massage. Remember! An effective weight loss programme: n Addresses the reasons why someone might find it difficult to lose weight n Is tailored to individual needs and choices n Is sensitive to the person’s weight concerns n Is based on a balanced, healthy diet n Encourages regular physical activity References Safefood – Stop the Spread Healthy Eating and Active Living for Adults, Teenagers and Children over 5 Years – www.fsai.ie NHS 12 week weight loss pack – www.nhs.uk/LiveWell Weight Management Treatment Algorithm, Reference guide & Support Information – HSE/ICGP www.healthpromotion.ie Medscape – Motivational Interviewing of Obese Patients 35
© Copyright 2026