DRESS Syndrome: Drug Rash with Eosinophilia and Systemic
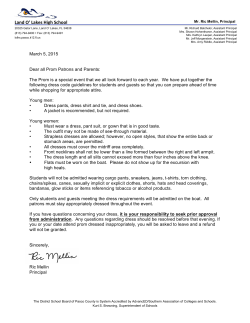
78 Journal of The Association of Physicians of India ■ Vol. 63 ■ May 2015 Case Report DRESS Syndrome: Drug Rash with Eosinophilia and Systemic Symptoms Hemant Thacker1, Manish Shah2, Rahul Tulle3 Abstract DRESS Syndrome is caused by exposure to certain medications that may cause fever, rash, inflammation of internal organs, lymphadenopathy and characteristic hematologic abnormalities such as eosinophilia, thrombocytopenia and atypical lymphocytosis. We herein report a case of DRESS syndrome who presented with fever and rash, secondary to sulfasalazine ingestion. Diagnosis of DRESS is often delayed, as several diseases have clinical and laboratory features similar to DRESS syndrome. Case History A 51 year old female came to our institution with complaints of high grade fever since 3 days, dry cough and prostration. Patient had a history of rheumatoid arthritis for which she was advised Sulfasalazine 500 mg bid for the last one month. On admission, the patient looked sick, flushed and febrile. Systemic examination was not contributory. Laboratory studies revealed a leukocyte count of 10,330/ cumm with 67% neutrophils and 17% eosinophils, hemoglobin of 11.3 gm% and platelet count of 1 2 9 , 0 0 0 / c u m m . L i ve r e n z y m e s we r e e l e va t e d w i t h a S G P T o f 157 U/L and SGOT of 124 U/L. Te s t s f o r m a l a r i a a n d d e n g u e were negative; Blood culture sent on admission was subsequently negative. Ultrasound abdomen revealed a mild hepatomegaly. Two days following admission, the patient developed a red macular rash with pruritus. The rash initially appeared on the face and trunk and within the next 36 hours had spread in a descending fashion to all over the body. The rash finally evolved to appear as erythematous maculopapular with edematous confluent lesions involving entire body with more severity over the face and limbs (Figure 1). Despite starting the patient on ceftriaxone, broad spectrum antibiotic, the fever was persistent. A dermatologic consultation was advised. The constellation of erythematous edematous rash on face, trunk and distal extremities with eosinophilia and atypical lymphocytosis and raised transaminases; temporal relation of rash occurring 4 weeks after commencement of oral sulfasalazine, clinched the diagnosis in favour of DRESS, also called drug-induced hypersensitivity syndrome (DIHS). A skin biopsy was advised for histopathological conformation of DRESS syndrome, but this was refused by the patient. S u l f a s a l a z i n e wa s p r o m p t l y discontinued and the patient was started on oral prednisolone (1 mg/kg). The patient responded dramatically with defervescence f r o m t h e ve r y n e x t d a y a n d a reduction in the rash. The liver enzymes also began declining t o n o r m a l i t y . T h e p a t i e n t wa s discharged with gradual tapering of steroid over a period of 6 weeks. Discussion Drugs incriminated commonly for DRESS syndrome include aromatic anticonvulsants (phenobarbital, carbamazepine, phenytoin, lamotrigine), sulfonamides, allopurinol, antiretroviral drugs etc. It has been suggested that concomitant Human Herpes Virus-6 (HHV-6) infection increases the risk to develop DRESS syndrome. The exact pathophysiologic mechanism of DRESS syndrome is not fully understood. Postulated mechanisms include defective detoxification of drug- Fig. 1: Erythematous maculopapular with edematous confluent lesion over upper limb Consultant Physician and Cardio Metabolic Specialist, 2Consultant Dermatologist, 3DNB Medicine Resident, Bhatia Hospital, Mumbai, Maharashtra Received: 05.07.2013; Revised: 16.01.2014; Accepted: 17.01.2014 1 Journal of The Association of Physicians of India ■ Vol. 63 ■ May 2015 reactive metabolites resulting in modification of cellular proteins, targeting an autoimmune response. There are 7 J-SCAR criteria for diagnosis of DRESS syndrome: 2 (1) maculopapular rash developing 3 weeks after beginning treatment with the causative drug; (2) prolonged clinical symptoms after discontinuing the causative drug; (3) fever >38°C (4) hepatic abnormalities (5) leukocyte abnormalities: leukocytosis, eosinophilia (6) lymphadenopathy ( 7 ) H H V - 6 r e a c t i va t i o n . I f a l l 7 points are present then it is termed as typical DIHS, if only first 5 are present, atypical DIHS is diagnosed. 79 Once the diagnosis of DRESS syndrome has been established, the next step in management is immediate cessation of the medication(s). Immediate withdrawal of the causative drug and initiation of systemic corticosteroids is the mainstay in the management of DRESS syndrome. Thyroiditis has been reported to develop in a subset of patients as long-term sequelae. drug reaction with a 10% mortality rate. Clinicians must be aware of this potentially fatal reaction and its common culprit medications. Prompt diagnosis using clinical criteria, laboratory values, and histopathology is imperative. The aim of this article is to review the available data regarding the diagnosis and the management of this probably underrecognised subset of drug reaction. Conclusion References DRESS syndrome is a drug hypersensitivity reaction with cutaneous and systemic manifestations. DRESS syndrome is a potentially fatal cutaneous 1. Chauhan A, Anand S, Thomas S, et al. Carbamazepine induced DRESS Syndrome; J Assoc Physicians India 2010; 58. 2. J o u r n a l o f Am e r i c a n Ac a d e my o f Dermatology; 2013.
© Copyright 2026