Concussion Management E-book - Kings Park Physical Therapy
631-269-5170
277 Indian Head Rd., Unit A
Kings Park, NY 11754
www.kingsparkpt.com
Concussions: The Invisible Injury
Student and Parent Information Sheet
Concussion definition
A concussion is a reaction by the brain to a jolt or force that can be transmitted to the head by an impact or blow occurring anywhere
on the body. Essentially a concussion results from the brain moving back and forth or twisting rapidly inside the skull.
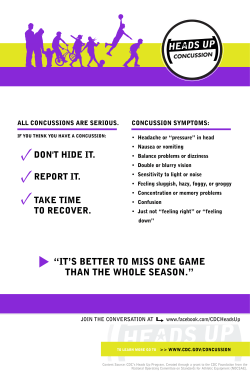
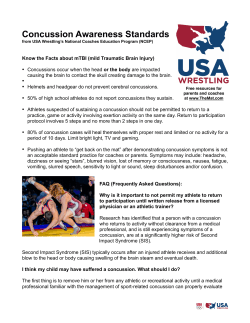
Facts about concussions according to the
Center for Disease Control (CDC)
l
l
l
An estimated 4 million people under age 19 sustain a head
injury annually. Of these approximately 52,000 die and
275,000 are hospitalized.
An estimated 300,000 sports and recreation related
concussions occur each year.
Students who have had at least one concussion are at
increased risk for another concussion.
In New York State in 2009, approximately 50,500 children
under the age of 19 visited the emergency room for a traumatic
brain injury and of those approximately 3,000 were hospitalized.
Requirements of School Districts
Education:
l
Each school coach, physical education teacher, nurse, and
athletic trainer will have to complete an approved course on
concussion management on a biennial basis, starting with the
2012-2013 school year.
j School coaches and physical education teachers must
complete the CDC course.
(www.cdc.gov/concussion/HeadsUp/online_training.html)
j School nurses and certified athletic trainers must complete
the concussion course. (http://preventingconcussions.org)
Information:
l
Provide concussion management information and sign off
with any parental permission form.
l
The concussion management and awareness information or
the State Education Department’s web site must be made
available on the school web site, if one exists.
Removal from athletics:
l
Require the immediate removal from athletic activities of any
pupil that has or is believed to have sustained a mild
traumatic brain injury.
l
No pupils will be allowed to resume athletic activity until
they have been symptom free for 24 hours and have been
evaluated by and received written and signed authorization
from a licensed physician. For interscholastic athletics,
clearance must come from the school medical director.
j Such authorization must be kept in the pupil’s permanent
heath record.
j Schools shall follow directives issued by the pupil’s
treating physician.
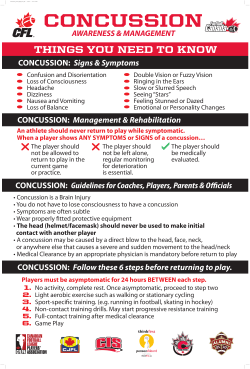
Symptoms
Symptoms of a concussion are the result of a temporary
change in the brain’s function. In most cases, the symptoms of a
concussion generally resolve over a short period of time; however,
in some cases, symptoms will last for weeks or longer. Children
and adolescents are more susceptible to concussions and take
longer than adults to recover.
It is imperative that any student who is suspected of having
a concussion is removed from athletic activity (e.g. recess, PE
class, sports) and remains out of such activities until evaluated and
cleared to return to activity by a physician.
Symptoms include, but are not limited to:
l
l
l
l
l
l
l
l
l
l
l
l
l
Decreased or absent memory of events prior to or immediately after the injury, or difficulty retaining new information
Confusion or appears dazed
Headache or head pressure
Loss of consciousness
Balance difficulties, dizziness, or clumsy movements
Double or blurry vision
Sensitivity to light and/or sound
Nausea, vomiting and/or loss of appetite
Irritability, sadness or other changes in personality
Feeling sluggish, foggy or light-headed
Concentration or focusing problems
Drowsiness
Fatigue and/or sleep issues – sleeping more or less than usual
Students who develop any of the following signs, or if signs
and symptoms worsen, should be seen and evaluated immediately
at the nearest hospital emergency room.
l
l
l
l
l
l
l
l
l
l
l
l
Headaches that worsen
Seizures
Looks drowsy and/or cannot be awakened
Repeated vomiting
Slurred speech
Unable to recognize people or places
Weakness or numbing in arms or legs, facial drooping
Unsteady gait
Change in pupil size in one eye
Significant irritability
Any loss of consciousness
Suspicion for skull fracture: blood draining from ear or
clear fluid from the nose
State Education Department’s Guidance for
Concussion Management
Schools are advised to develop a written concussion management policy. A sample policy is available on the NYSPHSAA web
site at www.nysphsaa.org. The policy should include:
l A commitment to reduce the risk of head injuries.
l
A procedure and treatment plan developed by the district
medical director.
l A procedure to ensure proper education for school nurses,
certified athletic trainers, physical education teachers,
and coaches.
l A procedure for a coordinated communication plan among
appropriate staff.
l
A procedure for periodic review of the concussion
management program.
Return to Learn and Return to Play
protocols
Cognitive Rest: Activities students should avoid include, but are
not limited to, the following:
l
Computers and video games
l
Television viewing
l
Texting
l
Reading or writing
l
Studying or homework
l
Taking a test or completing significant projects
l
Loud music
l
Bright lights
Students may only be able to attend school for short periods of
time. Accommodations may have to be made for missed tests and
assignments.
Physical Rest: Activities students should avoid include, but are
not limited to, the following:
l
Contact and collision
l
High speed, intense exercise and/or sports
l
High risk for re-injury or impacts
l
Any activity that results in an increased heart rate or
increased head pressure
Return to Play Protocol once symptom free for 24 hours and
cleared by School Medical Director:
Day 1: Low impact, non strenuous, light aerobic activity.
Day 2: Higher impact, higher exertion, moderate aerobic activity.
No resistance training.
Day 3: Sport specific non-contact activity. Low resistance weight
training with a spotter.
Day 4: Sport specific activity, non-contact drills. Higher resistance
weight training with a spotter.
Day 5: Full contact training drills and intense aerobic activity.
Day 6: Return to full activities with clearance from School Medical
Director.
Any return of symptoms during the return to play protocol, the
student will return to previous day’s activities until symptom free.
Concussion Management Team
Schools may, at their discretion, form a concussion management
team to implement and monitor the concussion management policy
and program. The team could include, but is not limited to, the
following:
l
Students
l
Parents/Guardians
l
School Administrators
l
Medical Director
l
Private Medical Provider
l
School Nurse
l
Director of Physical Education and/or Athletic Director
l
Certified Athletic Trainer
l
Physical Education Teacher and/or Coaches
l
Classroom Teachers
Other Resources
l
New York State Education Department
New York State Department of Health
http://www.health.ny.gov/prevention/injury_prevention/
concussion/htm
l
New York State Public High School Athletic Association
www.nysphsaa.org/safety/
l
Center for Disease Control and Prevention
http://cdc.gov/TraumaticBrainInjury
l
National Federation of High Schools
www.nfhslearn.com – The FREE Concussion Management course
does not meet education requirement.
l
Child Health Plus
http://www.health.ny.gov/health_care/managed_care/consumer_
guide/about_child_health_plus.htm
l
Local Department of Social Services – New York State
Department of Health
http://www.health.ny.gov/health_care/medicaid/ldss/htm
l
Brain Injury Association of New York State
http://www.bianys.org
l
Nationwide Children’s Hospital – Concussions in the
Classroom
http://www.nationwidechildrens.org/concussions-in-theclassroom
l
Upstate University Hospital – Concussions in the Classroom
http://www.upstate.edu/pmr/healthcare/programs/concussion/
classroom.php
l
ESPN Video – Life Changed by Concussion
http://espn.go.com/video/clip?id=7525526&categoryid=5595394
l
SportsConcussions.org
http://www.sportsconcussions.org/ibaseline/
l
American Association of Neurological Surgeons
http://www.aans.org/Patient%20Information/Conditions%20
and%20Treatment/Concussion.aspx
l
Consensus Statement on Concussion in Sport – Zurich
http://sportconcussions.com/html/Zurich%20Statement.pdf
l
Division of KPPT
Greg Rahn, PT, CSCI
631-269-5170 (Tel)
631-269-5283 (Fax)
Director/Owner
www.kingsparkpt.com
277 Indian Head Road, Unit A, Kings Park, NY 11754
Greg Rahn, PT,MoveForwardPT.com
CSCI
Director/Owner
631-269-5170 (Tel)
631-269-5283 (Fax)
www.kingsparkpt.com
Move Forward Guide
Physical Therapist's Guide to Concussion
Created: March 24, 2011 | Revised: March 24, 2011 | Last Reviewed: March 24, 2011
Jump to:
In the past few years, concussion has received a great deal of attention as people in the medical
and sports worlds have begun to speak out about the long-term problems associated with this injury.
The Centers for Disease Control estimate that in sports alone, more than 3.8 million concussions
occur each year. Recent scientific evidence highlights the need for proper care to prevent
complications from concussion.
If you think you might have a concussion:
• Seek medical care immediately.
• Avoid any additional trauma to your head—don't engage in any activity that carries a risk of
head injury.
• Limit activities of all kinds, including school and work.
•
What Is
Concuss
•
Signs an
Symptom
•
How Is It
Diagnose
•
How Can
Therapis
•
Real Life
Experien
•
What Kin
Physical
Do I Nee
•
Further R
What Is Concussion?
Concussion is a brain injury that occurs when the brain is shaken inside the skull, causing changes
in the brain's chemistry and energy supply. A concussion might happen as a result of a direct blow to
the head or an indirect force, such as whiplash. You might or might not lose consciousness.
Concussion: See More Detail
277 Indian Head Road, Unit A, Kings Park, NY 11754
Signs and Symptoms
Signs and Symptoms
There are many symptoms related to concussion, and they can affect your physical, emotional, and mental well-being.
Physical symptoms may include:
• Headache
• Dizziness
• Difficulty with balance
MoveForwardPT.com
• Nausea/vomiting
MoveForwardPT.com
MoveForwardPT.com
Fatigue with sleeping
• Difficulty
•• Difficulty
sleeping
Difficultyorwith
with
sleeping
Double
blurred
vision
•
Double
or
blurred
vision
http://www.moveforwardpt.com/Print.aspx
Double or blurred
vision
• Sensitivity
to light and
sound
•• Sensitivity
to
light
and
Sensitivity to light and sound
sound
Cognitive (thinking) symptoms may include:
Cognitive
Cognitive (thinking)
(thinking) symptoms
symptoms may
may include:
include:
• Difficulty with short-term or long-term memory
•• Difficulty
Difficulty with
with short-term
short-term or
or long-term
long-term memory
memory
Confusion
•• Confusion
Confusion
Slowed
"processing" (for instance, a decreased ability to think through problems)
•• Slowed
Slowed "processing"
"processing" (for
(for instance,
instance, a
a decreased
decreased ability
ability to
to think
think through
through problems)
problems)
"Fogginess"
"Fogginess"
"Fogginess"
•• Difficulty
with concentration
•• Difficulty
Difficulty with
with concentration
concentration
Emotional symptoms may include:
Emotional
Emotional symptoms
symptoms may
may include:
include:
• Irritability
Irritability
Irritability
•• Restlessness
•• Restlessness
Restlessness
Anxiety
•• Anxiety
Anxiety
Depression
•• Depression
Depression
Mood
swings
•• Mood
Mood swings
swings
Aggression
Aggression
Aggression tolerance of stress
•• Decreased
•• Decreased
Decreased tolerance
tolerance of
of stress
stress
Page 2 of 4
Page
Page 22 of
of 44
7/10/2012
Back to Top
Back
Back to
to Top
Top
How Is It Diagnosed?
How
How Is
Is It
It Diagnosed?
Diagnosed?
Concussion is easy to miss because diagnostic imaging, such as such as magnetic resonance imaging (MRI) or a computed tomography
Concussion
is
miss
Concussion
is easy
easyisto
tonormal.
miss because
because diagnostic
diagnostic imaging,
imaging, such
such as
as such
such as
as magnetic
magnetic resonance
resonance imaging
imaging (MRI)
(MRI) or
or a
a computed
computed tomography
tomography
(CT)
scan, usually
(CT)
scan,
usually
is
normal.
(CT) scan, usually is normal.
Because of the variety of possible symptoms that can interfere with day-to-day activity, seek coordinated medical care immediately.
Because
of
of
can
with
activity,
seek
care
Because
of the
the
variety
of possible
possible
symptoms
that
can interfere
interfere
with day-to-day
day-to-day
activity,
seek coordinated
coordinated medical
medical
care immediately.
immediately.
Your
health
carevariety
professionals
maysymptoms
include a that
physician
with expertise
in concussion,
a neuropsychologist,
and a vestibular
physical
Your
health
care
professionals
may
include
a
physician
with
expertise
in
concussion,
a
neuropsychologist,
and
a
vestibular
Your health
care professionals
mayspecializes
include a physician
expertise
in concussion,
a neuropsychologist, and a vestibular physical
physical
therapist
(a physical
therapist who
in treatingwith
balance
disorders
and dizziness).
therapist
therapist (a
(a physical
physical therapist
therapist who
who specializes
specializes in
in treating
treating balance
balance disorders
disorders and
and dizziness).
dizziness).
After a concussion, limit any kind of exertion. The brain won't have time to heal if you increase physical exertion too soon—such as
After
limit
kind
The
won't
time
ifif you
increase
physical
exertion
soon—such
as
After a
a concussion,
concussion,
limit any
any
kind of
of exertion.
exertion.
The brain
brain
won't have
have
time to
to
heal
you
increase
physical
exertion
too
soon—such
as
returning
to social activities
or sports—or
if you increase
cognitive
demands
tooheal
soon,
such
as returning
to school
or too
work.
You can slowly
returning
to
social
activities
or
sports—or
if
you
increase
cognitive
demands
too
soon,
such
as
returning
to
school
or
work.
You
can
slowly
returningnormal
to social
activities
oronce
sports—or
if you increase
too soon, such as returning to school or work. You can slowly
resume
activities
only
your symptoms
have cognitive
improved demands
and stay improved.
resume
resume normal
normal activities
activities only
only once
once your
your symptoms
symptoms have
have improved
improved and
and stay
stay improved.
improved.
Back to Top
Back
Back to
to Top
Top
How Can a Physical Therapist Help?
How
How Can
Can a
a Physical
Physical Therapist
Therapist Help?
Help?
Physical therapists can evaluate and treat many problems related to concussion. Because no 2 concussions are the same, the physical
Physical
can
evaluate
and
many
problems
related
to
Because
2
the
same,
physical
Physical therapists
therapists
can is
evaluate
and
treat
many
problems
related
to concussion.
concussion.
Because
no
2 concussions
concussions
are
thedesigns
same, the
the
physical
therapist's
examination
essential
totreat
assess
your
individual
symptoms
and limitations.
Theno
physical
therapistare
then
a treatment
therapist's
therapist's examination
examination is
is essential
essential to
to assess
assess your
your individual
individual symptoms
symptoms and
and limitations.
limitations. The
The physical
physical therapist
therapist then
then designs
designs a
a treatment
treatment
program.
program.
program.
Help Stop Dizziness and Improve Your Balance
Help
Help Stop
Stop Dizziness
Dizziness and
and Improve
Improve Your
Your Balance
Balance
If you have dizziness or difficulty with your balance following a concussion, vestibular physical therapy may help. The vestibular system,
If
dizziness
or
your
following
a
vestibular
physical
may
help.
vestibular
system,
If you
you have
have
dizziness
or difficulty
difficulty
with
your balance
balance
following
a concussion,
concussion,
vestibular
physical
therapy
may keeping
help. The
The
vestibular
system,
which
includes
the inner
ear and with
its connections
with
the brain,
is responsible
for sensing
headtherapy
movement,
your
eyes focused
which
includes
the
inner
ear
and
its
connections
with
the
brain,
is
responsible
for
sensing
head
movement,
keeping
your
eyes
focused
which you
includes
inner
earand
andhelping
its connections
brain, isAresponsible
for sensing
headtherapist
movement,
eyesexercises
focused and
when
movethe
your
head,
you keepwith
yourthe
balance.
qualified vestibular
physical
cankeeping
provide your
specific
when
head,
and
you
your
A
when you
you
move
your
head,
and helping
helping
you keep
keepbalance
your balance.
balance.
A qualified
qualified vestibular
vestibular physical
physical therapist
therapist can
can provide
provide specific
specific exercises
exercises and
and
training
to move
reduceyour
or stop
dizziness
and improve
and stability.
training
training to
to reduce
reduce or
or stop
stop dizziness
dizziness and
and improve
improve balance
balance and
and stability.
stability.
Reduce Headaches
Reduce
Reduce Headaches
Headaches
Your physical therapist will examine you for neck problems following a concussion. Neck injuries can cause headaches and contribute to
Your
will
examine
you
for
problems
following
a
Neck
can
Your physical
physical
therapist
will
examine
you also
for neck
neck
problems
following
a concussion.
concussion.
Necktoinjuries
injuries
can cause
cause headaches
headaches and
and contribute
contribute to
to
some
forms oftherapist
dizziness.
Your
therapist
can assess
your
back for
possible injuries
your spine.
some forms of dizziness. Your therapist also can assess your back for possible injuries to your spine.
when you move your head, and helping you keep your balance. A qualified vestibular physical therapist can provide specific exercises and
training to reduce or stop dizziness and improve balance and stability.
Reduce Headaches
Your physical therapist will examine you for neck problems following a concussion. Neck injuries can cause headaches and contribute to
some forms of dizziness. Your therapist also can assess your back for possible injuries to your spine.
As symptoms due to concussion improve, your physical therapist will help you resume physical activity gradually, to avoid overloading the
brain and nervous system that have been compromised by concussion.
It's important that you follow the recommendations of all health care professionals so that you can achieve the greatest amount of recovery
in the shortest amount of time.
MoveForwardPT.com
Back
to Top
Page
3 of
4
Real Life Experiences
You've just come home from a soccer game where your 15-year-old daughter was star goalie. She admits to you that she "dinged"7/10/2012
her
http://www.moveforwardpt.com/Print.aspx
head during a play in the second half and did not tell anyone. She's complaining of headache and dizziness, and she's sensitive to light.
What do you do next?
You monitor the next 24 hours closely, seeking care immediately in the local emergency department if your daughter has or you observe
any of the following:
•
•
•
•
•
•
•
•
•
•
•
Headache that gets worse and does not go away
Weakness, numbness or decreased coordination
Repeated vomiting or nausea
Slurred speech
Extreme drowsiness or cannot be awakened
One pupil (the black part in the middle of the eye) larger than the other
Convulsions or seizures
Inability to recognize people or places
Increased confusion, restlessness, or agitation
Unusual behavior
Loss of consciousness
During the next couple of days, she's frequently in the nurse's office due to headaches and dizziness. She reports difficulty concentrating
and remembering during school and is having trouble falling asleep at night. What do you do next?
• Have the concussion evaluated by a licensed medical professional with expertise in treating concussion. Some communities have
concussion or mild traumatic brain injury clinics. Evaluation should include an assessment of symptoms, neurologic screening,
testing of thinking ability ("cognition"), and testing for balance problems.
• Do NOT allow your daughter to participate in sports or any other activity with risk of head injury until she is cleared by a licensed
medical professional with expertise in treating concussion. Repeated concussions can result in many problems.
• Do NOT allow your daughter to engage in physical activity—such as exercise, sports practice, gym class—until she has recovered
from her concussion or has been advised by a licensed medical professional with expertise in treating concussion. Physical activity
during early stages of concussion robs your brain of the energy it needs for healing.
• Limit thinking ("cognitive") activity until you have recovered from your concussion or have been advised by a licensed medical
professional with expertise in treating concussion. Your brain requires additional energy to heal from a concussion, and excessive
thinking interferes with recovery.
• Get plenty of sleep and rest. This will help your brain to recover from the concussion.
This story was based on a real-life case. Your case may be different. Your physical therapist will tailor a treatment program to your specific
case.
Back to Top
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat a variety of conditions or injuries. You may want to consider:
• A physical therapist who is experienced in treating people with neurological problems. Some physical therapists have a practice
with a neurological or vestibular rehabilitation focus.
• A physical therapist who is a board-certified clinical specialist or who completed a residency or fellowship in neurologic physical
therapy. This therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists who have these and other credentials by using Find a PT, the online tool built by the American Physical
Therapy Association to help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you're looking for a physical therapist (or any other health care provider):
• A physical therapist who is a board-certified clinical specialist or who completed a residency or fellowship in neurologic physical
therapy. This therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists who have these and other credentials by using Find a PT, the online tool built by the American Physical
Therapy Association to help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you're looking for a physical therapist (or any other health care provider):
• Get recommendations from family and friends or from other health care providers.
• When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience in helping people with
concussion.
• During your first visit with the physical therapist, be prepared to describe your symptoms in as much detail as possible, and say
what makes your symptoms worse.
MoveForwardPT.com
Back to Top
Page 4 of 4
Further Reading
The American Physical Therapy Association (APTA) believes that consumers should have access to information that could help them
make health care decisions and also prepare them for their visit with their health care provider.
http://www.moveforwardpt.com/Print.aspx
7/10/2012
The following articles provide some of the best scientific evidence related to physical therapy treatment of problems related to concussion.
The articles report recent research and give an overview of the standards of practice for treatment both in the United States and
internationally. The article titles are linked either to a PubMed abstract of the article or to free full text, so that you can read it or print out a
copy to bring with you to your health care provider.
Alsalaheen BA, Mucha A, Morris LO, et al. Vestibular rehabilitation for dizziness and balance disorders after concussion. J Neurol Phys
Ther. 2010;34:87–93. Article Summary on PubMed.
McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on Concussion in Sport 3rd International Conference on Concussion in
Sport held in Zurich, November 2008. Clin J Sport Med. 2009;19:185–200. Article Summary on PubMed.
Centers for Disease Control and Prevention
Acknowledgments: Anne Mucha, PT, NCS, and the APTA Neurology Section
Back to Top
The ImPACT of Concussion on Our Young Athletes: The Concussion Management Program - Junior Ho... Page
Greg Rahn, PT, CSCI
In The News
Director/Owner
631-269-5170 (Tel)
631-269-5283 (Fax)
www.kingsparkpt.com
The ImPACT of Concussion on Our Young Athletes: The
Concussion Management Program - Junior Hockey News
March 8, 2012, 5:00am
Salvatore Trazzera, www.juniorhockey.com
Dr. Salvatore Trazzera, a Board Certified Cardiologist, Internal Medicine Specialist and Sports Medicine
Physician has rapidly established himself as the athletes and fitness conscious individual's physician. He has
extensive experience in coronary angiography, non invasive vascular imaging and state of the art cardiac and
vascular computed tomography. His life long experience as a competitive athlete combined with his extensive
medical training, knowledge and clinical experience provide an uncommon combination of skills which allow
him to relate to his athletes in a way unique to few physicians. He is owner and supervising team physician of
professional, Jr. A and youth hockey programs for NYTEX Sports, Suffolk PAL and the Texas Brahmas of the
Central Hockey League he has introduced a concussion prevention and management program utilizing state of
the art clinical neurocognitive (ImPACT@) and neurophysical (Biodex Balance SD@) assessment. This
program will help to guide athletes to safer timing of return to play minimizing recurrent and long term injury
further decreasing post concussive cognitive impairment. To date he has over 250 competitive athletes
baseline tested with ImPACT and Biodex Balance-SD and experience and expertise in returning athletes to
competition
safely
post
traumatic
brain
injury
(concussion).
Below is an overview of concussion (Traumatic Brain Injury, TBI) prevention, recognition, assessment and
treatment which will serve as a general outline for any school or club programs "Concussion Management
Program".
Recently much over due attention has been focused by the media on the epidemic of concussion or Traumatic
Brain Injury in sports (we will use concussion, TBI or Traumatic Brain Injury interchangeably). A concussion is
in fact just that. A functional brain injury sustained after direct or indirect head or brain trauma. Annual
incidence of sports related concussion is estimated to be over 300,000 per year according to the Center for
Disease Control. FACT: There need not be loss of consciousness to have sustained a concussion. FACT:
The developing brain, in our younger athletes, is much more susceptible to functional brain injury. FACT:
Recovery from TBI takes longer in the developing brain. FACT: The long term effect of repeated concussion in
the younger athlete is incrementally worse than in older athletes. FACT: In a University of Pittsburgh Medical
Center (UPMC) study of high school and college athletes with concussion, on-the-field amnesia, not loss of
consciousness, as long thought, was predictive of post-injury symptom severity and neurocognitive (brain
function) deficits.
Common signs of TBI include the athlete appearing to be dazed or stunned, confused about assignments,
forgets plays, is unsure of game, score, or opponent, moves clumsily, answers questions slowly, loses
consciousness (even temporarily), shows behavior or personality change, forgets events prior to hit (retrograde
amnesia) or forgets events after hit (anterograde amnesia).
Signs frequently reported by the athlete include headache, nausea, balance problems or dizziness, double or
fuzzy vision, sensitivity 277
to light
or noise,
feeling
sluggish,
feeling
"foggy",
change in sleep pattern and
Indian
Head R
oad, U
nit A, Kings
Park
, NY 11754
concentration or memory problems.
The overwhelming majority of athletes that sustain a concussion recover fully but unfortunately the number of
consciousness (even temporarily), shows behavior or personality change, forgets events prior to hit (retrograde
amnesia) or forgets events after hit (anterograde amnesia).
Signs frequently reported by the athlete include headache, nausea, balance problems or dizziness, double or
fuzzy vision, sensitivity to light or noise, feeling sluggish, feeling "foggy", change in sleep pattern and
concentration or memory problems.
The overwhelming majority of athletes that sustain a concussion recover fully but unfortunately the number of
athletes that go on to experience chronic cognitive and neurobehavioral difficulties is difficult to estimate, or for
that fact accurately know especially if the athlete is reluctant to report symptoms to coaches, parents or trainers
for fear of being removed from competition.
Post concussive symptoms can be quite debilitating to the athlete and may include a combination of any of the
following symptoms; chronic headaches, fatigue, sleep difficulties, personality changes (e.g. increased
irritability, emotionality), sensitivity to light or noise, dizziness when standing quickly, deficits in short-term
memory, problem solving and general academic functioning and unfortunately such difficulties can be
permanent and disabling.
In addition to Post-Concussion Syndrome, suffering a second blow to the head while recovering from an initial
concussion can have catastrophic consequences as in the case of "Second Impact Syndrome," which has led
to approximately 30-40 deaths over the past decade.
Concussion Assessment
In the event of a witnessed blow to the head or the remotest of suspicion of a coach or trainer considering the
possibility of TBI to one of his/her athletes, the athlete should be removed from competition until further
evaluated by a clinician specializing in sports concussion management.
Upon ruling out more severe injury, acute evaluation continues with assessment of the concussion. First, the
clinician should establish the presence of any loss or other alteration of consciousness (LOC). LOC is relatively
rare and occurs in less than 10% of concussions.
The identification of LOC can be very tricky, as the athlete may lose consciousness very briefly and this event
may not be directly observed by others. By definition, LOC represents a state of brief coma in which the eyes
are typically closed and the athlete is unresponsive to external stimuli. LOC is most obvious when an athlete
makes no attempt to brace his or her fall following a blow to the head. Any athlete with documented LOC
should be managed conservatively, and return to play is contraindicated.
Although helpful in identifying more serious concerns (e.g. skull fracture, hematoma, contusion), traditional
neurological and radiologic procedures, such as CT, MRI, and EEG, are not useful in identifying the effects of
concussion. Such tests are typically unremarkable or normal, even in athletes sustaining a severe concussion.
The reason for this issue is that concussion is a metabolic rather than structural injury. Thus, structural
neuroimaging techniques are insensitive to the effects of concussion.
Concussion Management Guidelines
At the forefront of proper concussion management is the implementation of baseline and/or post-injury
neurocognitive and neurophysical (balance, proprioception) testing. Such evaluation can help to objectively
evaluate the concussed athlete's post-injury condition and track recovery for safe return to play, thus
preventing the cumulative effects of concussion. In fact, neurocognitive testing has recently been called the
"cornerstone" of proper concussion management by an international panel of sports medicine experts.
Current management guidelines (i.e. Grade 1, 2, 3 of concussion) are not evidenced-based and little to no
scientific data support the arbitrary systems that are in place to manage concussion. As a result, there are
currently 19 different management criteria available for concussion management, which are often misused and
misinterpreted.
Concussion Recommendations
According to the Vienna Concussion Conference Recommendations, athletes should complete the following
step-wise process prior to return to play following concussion:
Removal from contest following signs and symptoms of concussion
No return to play in current game
Medical evaluation following injury
misinterpreted.
Concussion Recommendations
Concussion
According
to Recommendations
the Vienna Concussion Conference Recommendations, athletes should complete the following
According
to
the Vienna
Recommendations, athletes should complete the following
step-wise process
prior to Concussion
return to playConference
following concussion:
step-wise process prior to return to play following concussion:
Removal from contest following signs and symptoms of concussion
Removal
contest
following
No
return from
to play
in current
gamesigns and symptoms of concussion
No
returnevaluation
to play in following
current game
Medical
injury
Medical
evaluation
following
injury pathology
Rule out more serious intracranial
Rule out more
serious
Step-wise
return
to playintracranial pathology
1.
No activity
until asymptomatic
Step-wise
return- rest
to play
2.
aerobic
exercise
1. Light
No activity
- rest
until asymptomatic
3.
training
2. Sport-specific
Light aerobic exercise
4.
3. Non-contact
Sport-specificdrills
training
5.
4. Full-contact
Non-contact drills
drills
6.
Competition
5. Game
Full-contact
drills
6. Game Competition
The ImPACT of Concussion on Our Young Athletes: The Concussion Management Program - Junior Ho... Page 3
Concussion
The ImPACT
of Concussion
on Our
Management
Program -differs
Junior Ho... Page 3
The
goal of Treatment
concussion
treatment
is toYoung
allow Athletes:
the brain The
injuryConcussion
to heal. Treatment
of concussions
Concussion
depending
onTreatment
the level of severity.
treatment
may
include:
The goal of
concussion
treatmentConcussion
is to allow
the brain
injury
to heal. Treatment of concussions differs
depending
on the adequate
level of severity.
treatment
may include:
Rest. Provide
time forConcussion
recovery from
a concussion.
Do not rush back into daily activities for work
or school.
Rest. Provide adequate time for recovery from a concussion. Do not rush back into daily activities for work
Preventing
or school. re-injury. Avoid activities that might jolt or jar your head. Never return to a sports activity until
your doctor has given you clearance. Ask when it's safe to drive a car, ride a bike, work or play at heights,
Preventing re-injury. Avoid activities that might jolt or jar your head. Never return to a sports activity until
or use heavy equipment.
your doctor has given you clearance. Ask when it's safe to drive a car, ride a bike, work or play at heights,
Observation
a responsible adult. Ask someone to awaken you every few hours as advised by your
or use heavyby
equipment.
doctor. The doctor will explain how to watch for complications such as bleeding in the brain.
Observation by a responsible adult. Ask someone to awaken you every few hours as advised by your
Limiting
exposure
drugs.
Dohow
not take
medicines
without yoursuch
doctor's
permission.
is especially true
doctor. The
doctorto
will
explain
to watch
for complications
as bleeding
in theThis
brain.
with aspirin, blood thinners, and drugs that cause drowsiness. Avoid the use of alcohol or illicit drugs.
Limiting exposure to drugs. Do not take medicines without your doctor's permission. This is especially true
Consult
with blood
a Credentialed
ImPACT
a full recovery.
with aspirin,
thinners, and
drugsConsultant
that causefor
drowsiness.
Avoid the use of alcohol or illicit drugs.
Consult with a Credentialed ImPACT Consultant for a full recovery.
Concussion Recovery
Concussion
Athletes whoRecovery
are not fully recovered from an initial concussion are significantly vulnerable for recurrent,
cumulative,
andare
even
consequences
of a second
concussion.
Athletes who
notcatastrophic
fully recovered
from an initial
concussion
are significantly vulnerable for recurrent,
cumulative,
and
even
catastrophic
consequences
of
a
second
concussion.
Such difficulties are prevented if the athlete is allowed time to recover from a concussion and return to play
decisions
are carefully
made. No
should
return totime
sport
other at-risk
symptoms
of
Such difficulties
are prevented
if athlete
the athlete
is allowed
toorrecover
from aparticipation
concussion when
and return
to play
concussion
are
present
and
recovery
is
ongoing.
decisions are carefully made. No athlete should return to sport or other at-risk participation when symptoms of
concussion
andtorecovery
ongoing.with concussion is to manage the injury properly when it does
In summary,are
thepresent
best way
prevent is
difficulties
occur.
In summary, the best way to prevent difficulties with concussion is to manage the injury properly when it does
occur.
References;
Overview
of Adult Traumatic Brain injuries, Copyright 2011 Orlando Health Education & Development
References;
Measurement
of Symptoms
Following
Sports
Related
Concussions:
Reliability
and Normative
Data for the Post Concussion Symptom Scale,
Overview of Adult
Traumatic Brain
injuries,
Copyright
2011
Orlando Health
Education
& Development
Applied
Neuropsychology,
Lovell
et al, May
2006
Measurement
of Symptoms
Following
Sports
Related Concussions: Reliability and Normative Data for the Post Concussion Symptom Scale,
Neurocognitive
and Symptom
predictors
of Recovery;
Brian Lau, BS, Clin J Sports Med, Vol 0 Num 0, 2009
Applied
Neuropsychology,
Lovell
et al, May
2006
Concussions
in and
the News
Feb predictors
12, 2012; http://www.stopconcussions.com/2012/02/dr-salvatore-trazzera/
Neurocognitive
Symptom
of Recovery; Brian Lau, BS, Clin J Sports Med, Vol 0 Num 0, 2009
Concussion
Management
recommendations;
http://dev.impacttest.com/index.php/concussion/management
Concussions in the News Feb 12, 2012; http://www.stopconcussions.com/2012/02/dr-salvatore-trazzera/
Salvatore
Trazzera,
MD, FACC,
FACP, RPVI,http://dev.impacttest.com/index.php/concussion/management
RTV, RPhS, March 7, 2012
Concussion
Management
recommendations;
Center
for
Athletic
Medicine
&
Phys
Salvatore Trazzera, MD, FACC, FACP, RPVI, RTV, RPhS, March 7, 2012
Center for Athletic Medicine & Phys
Related Program:
Biodex Concussion Management Program
Related Program:
Related Product: Balance System SD
Biodex Concussion Management Program
BioSway, Portable
Related Product: Balance System SD
Biodex Concussion Manager Software v2.0
BioSway, Portable
Biodex Concussion Manager Software v2.0
631-269-5170 (Tel) 631-269-5283 (Fax)
277 Indian Head Road, Unit A
Kings Park, NY 11754
www.kingsparkpt.com
631-269-5170 (Tel) 631-269-5283 (Fax)
277 Indian Head Road, Unit A
Kings Park, NY 11754
www.kingsparkpt.com
© Copyright 2026