Controversies in The Treatment of Hyponatremia Hilmer O. Negrete MD
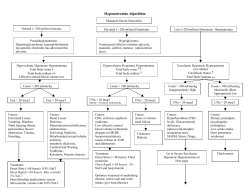
Controversies in The Treatment of Hyponatremia Hilmer O. Negrete MD The Renal Group Boardman, OH May 2, 2013 Learning Objectives • To recognize the conditions that are associated with complications of hyponatremia and its treatment • To better understand and apply the goals of therapy in hyponatremia • To understand new options in preventing complications of the treatment of hyponatremia • To understand the role of use of Vaptan in the treatment of Hyponatremia Mortality after hospitalization with mild, moderate, and severe hyponatremia Waikar, SS et al Am J Med 2009 Sep;122(9): 857-65 Renal Division, Brigham and Women's Hospital, Harvard Medical School • Hyponatremia (Na <135 mEq/L) was observed in 14.5% of patients • Patients were older (67.0 vs. 63.1 years, P <.001) • Had more comorbid conditions (P <.001) • Increased risk of death • in hospital (odds ratio 1.47) • at 1 year (hazard ratio 1.38) • at 5 years (hazard ratio 1.25) • Resolution of hyponatremia during hospitalization attenuated the increased mortality risk conferred by hyponatremia. Hyponatremia in the Elderly • Overall incidence of hyponatremia, Na < 137 mEq/L ~ 7% (Caird et al, Brit Heart J 35:527, 1973) • Prevalence as high as 18-20% in chronic care facilities, with 53% of incidence of one or more episodes of hyponatremia (Kleinfeld et al, J Am Geriatr Soc 43:1410, 1995) • Mortality rate 16% for patients over 65, versus 8% for those with normal Na on admission (Terzian et al, J Gen Int Med 9:89, 1994) Joseph Verbalis, MD,“Improving Hyponatremia Outcomes in the Hospitalized Patient” Society of Hospital Medicine (SHM) Annual Meeting, April 8-11, 2010 Increasing risk for hyponatremia with age at admission and acquired at hospital Hawkins RC Clin Chim Acta 337: 169–172, 2003 Osmotic Determinants of Body Water Distribution Intracellular Extracellular 40% Body Wt 20% Body Wt H2O K+ H2O Prot Na+ H2O H2O Interstitium Plasma Serum Sodium Concentration and Hyponatremia • Reflects body fluid tonicity • Abnormal sodium concentration usually means disorder of water balance Serum [Na+] = Total Na+E + Total K+E Total Body Water Maintenance Water Homeostasis • Osmotic regulation – – – – Plasma tonicity Hypothalamic osmoreceptors ADH (AVP- vasopressin) Thirst • Hemodynamic regulation – Arterial filling (Effective circulatory volume) – Aortic arch, carotid sinus, cardiac atria • Kidney – Water excretion (urine dilution) Plasma and Urine Osmolality and Vasopressin Underfilling Arterial Circulation Renin, Angiotensin II Aldosterone Sympathetic Nervous System Vasopressin (ADH) Increase Renal Sodium Reabsorption Increase Renal Water Reabsorption Low Urine Sodium UNa < 30 mEq/L High Urine Osmolality Uosm > 100 mOsm/kg (Exceptions: Diuretics, Adrenal insufficiency, Renal salt wasting, Cerebral salt wasting?) Hyponatremia Serum OSM Low Hypotonic Hyponatremia Normal High Marked hyperlipidemia (lipemia, TG >35mM) Hyperproteinemia (Multiple myeloma) “Pseudohyponatremia” Hyperglycemia Mannitol “Translocation Hyponatremia” *Note: all have ↑ADH •SIADH: inappropriate •Rest: appropriate ECFv * Low Renal loss (UNa > 20) Extra-renal loss (UNa <10) •Diuretics •Bleeding •Thiazide •Burns •K-sparing •GI (N/V, diarrhea) •ACE-I, ARB •Pancreatitis •IV RTA, Hypoaldo • Cerebral salt wasting Normal •Hypothyroidism •AI •SIADH •Reset Osmostat •Water Intoxication 1° Polydipsia TURP post-op High •CHF •Cirrhosis •Nephrosis Pathogenesis of hypotonic hyponatremia as derived from the Edelman equation Adrogué H J , and Madias N E JASN 2012;23:1140-1148 Generation of hypotonic hyponatremia in function of Electrolytes and water Net IC Net Free water Nae+ Ke+ TBW [Na]s Normal State 0 0 Normal Normal Normal Normal CHF (early) Positive 0 Increased Normal Increased Normal CHF (late) 0 Positive Increased Decreased Increased Decreased Diarrhea (early) Negative 0 Decreased Decreased Decreased Normal Diarrhea (late) 0 Positive Decreased Decreased Decreased Decreased SIADH 0 Positive Normal Normal Increased Decreased Psychogenic Polydipsia 0 Positive Normal Normal Increased Decreased Hypokalemia Negative Positive Normal/In creased Decreased Normal Decreased Adrogué H J , and Madias N E JASN 2012;23:1140-1148 Hypovolemic Hyponatremia • Key Point – Driven by both Sodium and water losses – The net loss of Sodium > Water • Causes – – – – GI Losses (Diarrhea, emesis) Diuretic use Adrenal Insufficiency Salt wasting nephritis • Treatment: – Restoration of volume with Isotonic fluid Euvolemic Hyponatremia • Key Point: – Water retention without significant change in total sodium • Causes – Syndrome of Inappropriate antidiuretic hormone secretion (SIADH) – Thiazide use – Hypothyroidism – Beer-drinker’s potomania – Reset Osmostat Hypervolemic Hyponatremia • Key Point – Gain of both sodium and water – Water > sodium • Decrease effective circulating blood volume • Causes – Congestive Heart Failure – Cirrhosis – Nephrotic Syndrome Diagnostic and Therapeutic Approach to the Hyponatremic Patient Schrier R W JASN 2006;17:1820-1832 Effect of water on sodium concentration Intracellular Extracellular 40% Body Wt 20% Body Wt WATER H2O H2O Prot [K +] [Na+] Cell swelling H2O H2O Interstitium Plasma Post operatively Hyponatremia A woman with postoperative hyponatremia Adrian Schreiber, MD et al American Journal of Kidney Diseases Volume 44, Issue 1 , Pages e3-e6, July 2004 Central Pontine Myelinolysis John D. Fleming, M.B., B.S., and Suresh Babu, M.B., B.S. N Engl J Med 2008; 359 December 4, 2008 Effects of Hyponatremia on the Brain and Adaptive Responses Effects of Hyponatremia on the Brain and Adaptive Responses. Adrogué HJ, Madias NE. N Engl J Med 2000;342:1581-1589. Controversies in the Treatment of Hyponatremia What is the optimal rate of correction of Hyponatremia? What is the Optimal Rate of correction? • Is the hyponatremia acute or chronic? • Does the patient have severe symptoms or intracranial pathology? Acute versus chronic hyponatremia • In practice the duration of hyponatremia is often unknown • Patients with chronic hyponatremia may develop acute reductions in the serum sodium concentration • The clinical approach to the patient should be primarily determined by the severity of symptoms How aggressive? How Fast? • Level 1: No or minimal symptoms – Headache, irritability, inability to concentrate, altered mood, depression OK TO CORRECT SLOWLY Joseph Verbalis, MD,“Improving Hyponatremia Outcomes in the Hospitalized Patient” Society of Hospital Medicine (SHM) Annual Meeting, April 8-11, 2010 How aggressive? How Fast? • Level 3: Severe symptoms – Seizures, obtundation, respiratory distress, coma Emergency! CORRECT RAPIDLY Joseph Verbalis, MD,“Improving Hyponatremia Outcomes in the Hospitalized Patient” Society of Hospital Medicine (SHM) Annual Meeting, April 8-11, 2010 How aggressive? How Fast? • Level 2: Moderate symptoms –Nausea, confusion, disorientation, altered mental status WHAT IS THE BEST PLAN? Joseph Verbalis, MD,“Improving Hyponatremia Outcomes in the Hospitalized Patient” Society of Hospital Medicine (SHM) Annual Meeting, April 8-11, 2010 Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective. R H Sterns, J D Cappuccio et al. JASN February 1, 1994 vol. 4 no. 8 1522-1530 • 56 patients with serum Na levels of < or = 105 mmol/L collected from ASN Members • Results: – 14 developed post-therapeutic complications (10 permanent, 4 transient) after correction to a serum sodium > 120 mmol/L. – No neurologic complications were observed among patients corrected by < 12 mmol/L per 24 h or by < 18 mmol/L per 48 h or in whom the average rate of correction to a serum sodium of 120 mmol/L was < or = 0.55 mmol/L per hour How Urgent Is the Need for Intervention? • The vast majority of hyponatremic patients do not require urgent management. • Conversely, patients with severely symptomatic hyponatremia and those with neurologic or neurosurgical conditions at risk of worsening intracranial hypertension represent medical emergencies. • When violation of the correction threshold appears likely, urgent measures to slow or halt further correction are required. • Overcorrection should be treated as a medical emergency; prompt relowering of the serum sodium concentration is in order • Urgent intervention might also be required for coexisting conditions (severe volume depletion might have caused circulatory shock and AKI, hypokalemia). Adrogué H J , and Madias N E JASN 2012;23:1140-1148 Symptomatic versus asymptomatic hyponatremia • Severe symptoms are most likely to occur – Acute (especially less than 24 hours) – Marked reduction in the serum sodium concentration (Na <120 mEq/L) • Neurologic manifestations, including seizures, impaired mental status or coma, and death Risk factors for development of hyponatremia encephalopathy Moritz ML and Carlos Ayus J (2007) Nat Clin Pract Nephrol 3: 374–382 Risk Factor Mechanism Childhood Higher brain to intracranial volume ratio Female sex Estrogens inhibit brain adaptation to hyponatremia Higher vasopressin levels than males Hypoxemia Impairs adaptation of brain to hyponatremia Decrease cerebral perfusion Causes brain injury Brain injury Vasogenic cerebral edema Cytotoxic cerebral edema Conditions associated with severe symptoms of hyponatremia • Exercise-associated hyponatremia, as in marathon runners • Hyponatremia associated with the use of ecstasy (3,4methylenedioxyamphetamine) • Self-induced water intoxication in psychogenic polydipsia, water drinking contests. • Postoperative hyponatremia due to SIADH • Patients with known intracerebral pathology • Recent administration of thiazides • Induction of delivery with oxytocin *Young women and children are particularly vulnerable to hyponatremic brain damage. Risk factors for the development of Exercise Associated Hyponatremia (EAH) • Exercise duration > 4 h or slow running/exercise pace • Female gender (may be explained by lower body weight) • Low body weight • Excessive drinking (>1.5 L/h) during the event • Pre-exercise overhydration • Abundant availability of drinking fluids at the event • Nonsteroidal anti-inflammatory drugs (not all studies) • Extreme hot or cold environment Mitchell H. Rosner and Justin Kirven Exercise-Associated Hyponatremia CJASN January 2007 2): (1) 151-161 Reversal of Transtentorial Herniation (TTH) With Hypertonic Saline Koenig MA, et al Neurology. 2008 Mar 25;70(13):1023-9 • To evaluate the role of 23.4% saline in the management of TTH • Results: – Reversal of TTH was predicted by a >/=5 mmol/L rise in serum sodium concentration (p = 0.001) hour after 23.4% saline – No evidence of central pontine myelinolysis was detected on post-herniation MRI Effect of increasing Na concentration on brain water content during Hyponatremia and Normonatremia Berl T. Treating hyponatremia: damned if we do and damned if we don’t. Kidney Int 1990; 37: 1006–1018. Re-induction of hyponatremia after rapid overcorrection of hyponatremia reduces mortality in rats Group 1 Group 2 NaCl alone NaCl+DXM (n=12) (n=16) Group 3 NaCl + SNa re-lowering (n=16) SNa at day 4 (mEq/l) 108 +/-2* 107 +/-1* 104 +/-2* SNa 12 h after correction — — 133 +/-2* ,† SNa at 24 h 137 +/-2* ,† 136 +/-1* ,† 117 +/-2 Change in SNa at 12 h — — 29 +/-1* Change in SNa at 24 h 29 +/-1* 29 +/-1* 14 +/-1 Neurological manifestations at day 5 12/12 8/16‡ 1/16‡ Mortality at day 10 12/12 13/16§ 1/16§ Fabrice Gankam Kengne, Alain Soupart, Roland Pochet, Jean-Pierre Brion and Guy Decaux Kidney International (2009) 76, 614–621 Outcome of Central Pontine and Extrapontine Myelinolysis Menger H, Jörg J, J Neurol. 1999;246(8):700. • The findings in 44 patients (42 of whom were chronic alcoholics) with central pontine myelinolysis • Results: • 34 patients for whom follow-up data were available, 32 survived, 11 completely recovered, 11 had some deficits but were independent, 10 were dependent (4 through disorders of memory or cognition, 3 with tetraparesis, 2 with cerebellar ataxia, 1 with polyneuropathy). • Magnetic resonance imaging had no prognostic significance. • Outcome was independent of the severity of neurological deficits during the acute phase, degree of hyponatremia or MRI initial or persistent findings Clinical and Radiologic Correlations of Central Pontine Myelinolysis Syndrome Mayo Clin Proc. 2011 November; 86(11): 1063–1067. • PATIENTS AND METHODS: 24 Patients Diagnosed with CPM from January 1, 1999, through December 31, 2010. • RESULTS: – Of 24 patients, 14 (58%) had only CPM, and 10 (42%) had extrapontine involvement. Hyponatremia was documented in 18 patients (75%), with median sodium nadir of 114 mmol/L. – Eighteen patients (75%) had alcoholism, and malnutrition was documented in 12 (50%). – Presenting symptoms included encephalopathy (n=18 [75%]), ataxia (n=11 [46%]), dysarthria (n=7 [29%]), eye movement abnormalities (n=6 [25%]), and seizures (n=5 [21%]). – Favorable outcome was seen in 15 patients (63%) at last follow-up. • CONCLUSION: Clinical outcome in patients with CPM is not predicted by the volume of radiologic T2 signal abnormality on MRI or the severity of hyponatremia Causes of Hyponatremia Associated With Unintentional Overcorrection Cause of Hyponatremia Mechanism of Escape From Antidiuresis Hypovolemia Volume repletion reverses baroreceptor-mediated vasopressin secretion Beer potomania, tea and toast diet Increased solute intake enhances delivery of glomerular filtrate to distal diluting sites Thiazide diuretics Discontinuation of diuretic restores diluting function of the distal tubule SSRI Discontinuation of antidepressant eliminates drug-induced SIADH Desmopressin Discontinuation of synthetic vasopressin eliminates antidiuretic state Hypopituitarism Cortisol replacement restores ability to suppress vasopressin secretion Addison disease Volume and cortisol replacement Hypoxemia Correction of hypoxemia eliminates non-osmotic stimulus for vasopressin Nausea, surgery, pain, or stress Spontaneous resolution of SIADH Richard. H. Stern et al American Journal of Kidney Diseases Volume 56,Issue 4, 774-779, October 2010 Hypertonic versus Isotonic saline • Hypertonic saline is required for patients with severe hyponatremic encephalopathy and concentrated urine. • In view of the high potential for overcorrection, its prescription should be based on a quantitative approach guided by a simple formula • Isotonic saline will correct volume depletion and the associated hyponatremia. However, great vigilance is required to prevent overcorrection, because brisk diuresis can ensue when extracellular fluid volume nears restitution. • Isotonic saline is unsuitable for correcting the hyponatremia of the SIADH culminating in worsening of the serum sodium. Potassium Supplementation and Hyponatremia • Hyponatremia associated with potassium depletion requires prompt but cautious repletion. • Prescribing multiple doses of potassium without close monitoring of both serum potassium and sodium values is fraught with risk for hyperkalemia and osmotic demyelination. • Catastrophic overcorrection of the serum sodium is well documented in such settings, especially because potassium depletion is a risk factor for osmotic demyelination. Adrogué H J , and Madias N E JASN 2012;23:1140-1148 Correction Goals for Severe Chronic Hyponatremia (Na <120 mEq/L) Rule of Sixes: • For all patients with chronic hyponatremia, the goal is 6 mEq/L during the initial 24 hours. • For those with severe symptoms (seizure, severe delirium, and unresponsiveness), the goal is preloaded in the first six hours, postponing subsequent efforts to increase serum sodium level until the next day. • This is not a target of therapy, but rather a therapeutic threshold that should not be crossed. Can re-lowering Na levels prevent complications of overcorrection? What strategies do we have to prevent overcorrection? Treating Profound Hyponatremia: A Strategy for Controlled Correction Richard H. Sterns et al. American Journal of Kidney Diseases Volume 56,Issue 4, 774-779, October 2010 • A 45-year-old man with a history of alcoholism (1/2 bottle of vodka and 15-24 cans of beer daily) with recurrent alcohol withdrawal seizures and delirium was found unresponsive in his apartment. • On arrival at the emergency department, he was combative and disoriented, requiring sedation • Medications: thiazide diuretic, a selective serotonin reuptake inhibitor (SSRI) for depression 2 weeks earlier after discharge from the hospital for an alcohol withdrawal seizure. • Laboratory Data: Serum Na: 96 mEq/L, Urine Osmolality 732 mOsm/kg , Urine Sodium 7 mEq/L • Diagnosis: Profound hyponatremia caused by the combination of thiazide diuretic, SSRI, beer potomania, alcohol withdrawal, and hypovolemia. Treating Profound Hyponatremia: A Strategy for Controlled Correction Richard H. Sterns et al. American Journal of Kidney Diseases Volume 56,Issue 4, 774-779, October 2010 DDAVP Is Effective in Preventing and Reversing Inadvertent Overcorrection of Hyponatremia Perianayagam A , Sterns RH et al. Clin J Am Soc Nephrol . 2008;3(2):331–336 • Objective: To assess the effectiveness and safety of desmopressin acetate – Avoid overcorrection of hyponatremia and – To lower the plasma sodium concentration after inadvertent overcorrection. • Methods: – Six patients (group 1) were given desmopressin acetate after the 24-h limit of 12 mmol/L had already been reached or exceeded – Fourteen patients (group 2) were given desmopressin acetate in anticipation of overcorrection DDAVP Is Effective in Preventing and Reversing Inadvertent Overcorrection of Hyponatremia Perianayagam A , Sterns RH et al. Clin J Am Soc Nephrol . 2008;3(2):331–336 • Results: – In all 14 patients correction was prevented from exceeding either the 24- or 48-h limits. – Plasma sodium concentration of 14 of the 20 patients fell by 2 to 9 mmol/L. – In all six group 1 patients (already overcorrected) and in five of the group 2 patients (prevention) , the plasma sodium concentration was actively lowered again by the concurrent administration of desmopressin acetate and 5% dextrose in water DDAVP Is Effective in Preventing and Reversing Inadvertent Overcorrection of Hyponatremia Perianayagam A , Sterns RH et al. Clin J Am Soc Nephrol . 2008;3(2):331–336 DDAVP Is Effective in Preventing and Reversing Inadvertent Overcorrection of Hyponatremia Perianayagam A , Sterns RH et al. Clin J Am Soc Nephrol . 2008;3(2):331–336 Group 1 Patients Precorrection Na Levels Peak Na level Before Correction Lowest Na levels after Correction Amount of Relowering Time of Relowering Rate of ReLowering (mmol/h) 1 122 138 134 4 4.5 0.89 2 115 135 129 6 20 0.3 3 109 121 112 9 17.5 0.51 4 108 125 118 7 8.25 0.85 5 129 142 134 8 14.5 0.55 6 112 124 120 4 10 0.40 ** All patients received D5W after the administration of DDVAP Hypertonic Saline and Desmopressin: A Simple Strategy for Safe Correction of Severe Lonika Sood, Richard H Sterns et al American Journal of Kidney Diseases 61:4, 571-578 April 2013 • 25 patients admitted to a community teaching hospital between October 1, 2008, and September 30, 2011, who were treated for serum sodium level <120 mEq/L with concurrently administered desmopressin and hypertonic saline solution. • Desmopressin was administered prior to the initiation of hypertonic saline, and the dose varied from 1-2 µg at approximately 6- to 8-hour intervals either intravenously or subcutaneously, except for one patient weighing 120 kg who was given 4 µg. Hypertonic Saline and Desmopressin: A Simple Strategy for Safe Correction of Severe Lonika Sood, Richard H Sterns et al American Journal of Kidney Diseases 61:4, 571-578 April 2013 • To determine dose-response relationships, the increase in serum sodium level prior to the start of the hypertonic saline solution infusion was estimated to the closest values 4, 24, and 48 hours later by using the Adrogué HJ , Madias Formula. • Salt tablets and/or potassium were converted to 3% saline solution equivalents: 1 g of salt tablets was taken to equal 34 mL, 1 mEq of oral potassium chloride elixir was taken equal to 2 mL, 1 mEq of 400 mmol/L of intravenous potassium chloride was taken to equal 2 mL. Hypertonic Saline and Desmopressin: A Simple Strategy for Safe Correction of Severe Lonika Sood, Richard H Sterns et al American Journal of Kidney Diseases 61:4, 571-578 April 2013 • Mean increase in serum sodium levels: – First 4 hours: 2.6 ± 2.0 mEq/L – First 24 hours: 5.8 ± 2.8 mEq/L – Second 24 hours: 4.5 ± 2.2 mEq/L • No patient had correction by >12 mEq/L in 24 hours or >18 mEq/L in 48 hours Hypertonic Saline and Desmopressin: A Simple Strategy for Safe Correction of Severe Lonika Sood, Richard H Sterns et al American Journal of Kidney Diseases 61:4, 571-578 April 2013 Hypertonic Saline and Desmopressin: A Simple Strategy for Safe Correction of Severe Lonika Sood, Richard H Sterns et al American Journal of Kidney Diseases 61:4, 571-578 April 2013 Hypertonic Saline and Desmopressin: A Simple Strategy for Safe Correction of Severe Lonika Sood, Richard H Sterns et al American Journal of Kidney Diseases 61:4, 571-578 April 2013 • In conclusion, combined infusion of 3% saline solution and desmopressin appears to be a valid strategy for correcting severe hyponatremia effectively and safely. • This approach appears to reduce the chance of inadvertent overcorrection. • It still requires substantial oversight by the nephrologist, who must identify patients who are poor candidates for the protocol What is the best formula to calculate the rate of correction in Hyponatremia? Formulas for calculating initial infusion rates in Hyponatremia Ellison DH, Berl T. N Engl J Med 2007;356:2064-2072. Does the Adrogue–Madias formula accurately predict serum sodium levels in patients with dysnatremias? • Prospective study to evaluate the utility or/and the accuracy of the Adrogue-Madias formula in managing patients with hyponatremia (Na <130 mEq/L) and hypernatremia (Na>148 mEq/L) • Methods: out of 317 patients, 189 patients (59.6%) had administration of intravenous solutions for the correction of dysnatremias. Liamis G, Kalogirou M et al Therapeutic approach in patients with dysnatraemias. Nephrol Dial Transplant 2006 Jun;21(6):1564-9 Formulas for estimating the effect of infusates and fluid losses on [Na+]s Infusate Formula Projects the effect of gaining 1 L of any infusate (inf) on sodium levels [Na +]s Fluid-Loss Formula Projects the effect of losing 1 L of any fluid (fl) on sodium levels [Na+]s Adrogué H J , and Madias N E JASN 2012;23:1140-1148 Does the Adrogue–Madias formula accurately predict serum sodium levels in patients with dysnatremias? Na levels at 12 hours Anticipated Na level Achieved Na level Number P value Volume depletion 130.2 +/- 4.1 131.3 +/- 5.2 45 NS SIADH 127.4 +/- 5.7 128.9 +/- 5.9 10 NS 123.8 +/- 6 125.5 +/- 5.6 9 NS Primary Polydipsia 122.5 +/- 0.7 129 +/- 1.4 2 P: 0.02 Hypernatremia 153.6 +/- 7.5 156.5 +/- 8.9 92 P: 0.021 Diuretic induced hyponatremia Liamis G, Kalogirou M et al Therapeutic approach in patients with dysnatraemias. Nephrol Dial Transplant 2006 Jun;21(6):1564-9 Does the Adrogue–Madias formula accurately predict serum sodium levels in patients with dysnatremias? Na levels at 24 hours Anticipated Na level Achieved Na level Number P value Volume depletion 130 +/- 4 135.6 +/- 3.3 15 0.002 Diuretic induced hyponatremia 128.1 +/- 4.8 130 +/- 4.5 15 NS Hypernatremia 151.5+/- 6.4 153.3 +/- 8.3 67 NS Liamis G, Kalogirou M et al Therapeutic approach in patients with dysnatraemias. Nephrol Dial Transplant 2006 Jun;21(6):1564-9 Estimating the Effect of Infusates and Fluid Losses on Serum Sodium • Implementation of case-specific therapeutic measures requires information derived from the quantitative projections on the patient’s serum sodium – prescribed fluid therapy – ongoing fluid losses • Easily applicable formulas based on the Edelman equation allow estimation of the effect of infusates (infusate formula) and fluid losses (fluid-loss formula) on the serum sodium What is the roles of Vaptans in the Treatment of Hyponatremia? AVP Regulation of Water Reabsorption Joseph Verbalis, MD,“Improving Hyponatremia Outcomes in the Hospitalized Patient” Society of Hospital Medicine (SHM) Annual Meeting, April 8-11, 2010 Non-Peptide AVP Receptors Antagonist (Vaptans) Conivaptan Tolvaptan Lixivaptan Satavaptan Receptor V2/V1a V2 V2 V2 Route of administration Intravenous Oral Oral Oral FDA approved Available in USA Available in USA Formulation 20 mg/100 cc D5W Tablets 15, 30 mg Treatment of SIADH with Conivaptan Decaux G, Am J Med 110 : 582 –584, 2001 Long-term effect of tolvaptan on serum sodium in the SALTWATER trial Berl T, Quittnat-Pelletier F, Verbalis JG, Schrier RW,Bichet DG,Ouyang J, Czerwiec FS; for the SALTWATER Investigators et al. Oral tolvaptan is safe and effective in chronic hyponatremia. J Am Soc Nephrol 21:705–712, 2010 Where Vaptans do and do not fit in The Treatment of Hyponatremia Anna J Jovanovich and Tomas Berl Kidney International April 2013 83:4, 563–567 • “Upon analysis of the available literature, we conclude that there is presently no role for vaptans in acute symptomatic hyponatremia” • Vaptans are efficacious in raising serum sodium in long-standing ‘asymptomatic’ hyponatremia. • However, the cost of the only Food and Drug Administration-approved oral agent (tolvaptan) makes its use prohibitive for most patients in this setting. AVP Receptors Antagonists in the Treatment of Hyponatremia • Further studies are needed to assess the proper use of AVP Receptors Antagonists in the following areas: – Correction of symptomatic hyponatremia alone or with Hypertonic saline – To assess the benefits of correction of hyponatremia in hospitalized patients (outcomes and length of stay) – To assess the long term use in minimally symptomatic hyponatremia in order to reduce the risk of neurocognitive dysfunction and gait instability Does Treatment of chronic hyponatremia change Outcomes? Relationship between serum Na and mortality Arun Chawla, Richard H. Sterns, et al Mortality and Serum Sodium: Do Patients Die from or with Hyponatremia? CJASN May 2011 vol. 6 no. 5 960-965 Populations in Which Hyponatremia Is Associated With Mortality (Odds ratio) • • • • General Population (1.17-8.0) Hospitalized patients (1.37-1.55) Patients in the ICU (1.3) Pre-operative hyponatremia (1.4) Patie Hoorn et al "Hyponatremia and Mortality: Moving Beyond Associations." American journal of kidney diseases : (2013)doi:10.1053/j.ajkd.2012.09.019 Diseases in Which Hyponatremia Is Associated With Mortality (Odds ratio) • • • • • • • Congestive Heart Failure (1.8) Cirrhosis (2.1) Myocardial Infarct (2.0) Pulmonary embolism (1.53) Pulmonary hypertension (3.6-10.2) Pneumonia (1.3) CKD (1.12-1.32) Patie Hoorn et al "Hyponatremia and Mortality: Moving Beyond Associations." American journal of kidney diseases : (2013)doi:10.1053/j.ajkd.2012.09.019 Hyponatremia and mortality: How innocent is the bystander? Hoorn EJ , Zietse R . Clin J Am Soc Nephrol . 2011;6(5):951–953 Hyponatremia and Mortality • Hyponatremia increasingly is being recognized as an independent predictor of mortality • Prospective studies are necessary to determine whether hyponatremia in itself contributes to mortality and whether correcting hyponatremia improves outcomes. • Until such studies are available, the presence of hyponatremia should be regarded as a risk factor for adverse outcomes and patients should be monitored accordingly. Patie Hoorn et al "Hyponatremia and Mortality: Moving Beyond Associations." American journal of kidney diseases : (2013)doi:10.1053/j.ajkd.2012.09.019 Mild hyponatremia and risk of fracture in the ambulatory elderly F. Gankam Kengne QJM: Volume 101, Issue 7 Pp. 583-588 • Case control study of 513 cases of bone fracture after incidental fall in ambulatory patients aged 65 or older • Prevalence of hyponatremia (serum Na <135 mEq/l,): – Patients with bone fracture: 13.06% – Controls patients: 3.90% • Hyponatremia was associated with bone fracture after incidental fall in ambulatory elderly (OR: 4.16). Options of Therapy in Hyponatremia Options of Therapy Comments/Limitations Normal saline Ok for hypovolemic hyponatremia but may cause overcorrection, ineffective in SIAD and hypovolemic hyponatremia Hypertonic Saline No consensus in infusion rate, can cause overcorrection, not indicated in hypovolemic hyponatremia Fluid restriction Slow to correct, poor compliance Salt tablets Need to be use with fluid restriction, not indicated in hypovolemic hyponatremia Urea Effective in SIADH, no USP formulation, not approved for hyponatremia, poor palatability, available in Europe Demeclocycline Inconsistent response, nephrotoxic in cirrhosis and CHF AVP Receptor Antagonist Effective in chronic SIAD and hypovolemic hyponatremia, very expensive Fluid Restriction • Fluid restriction remains the cornerstone of managing oligosymptomatic patients with euvolemic or hypervolemic hyponatremia. • Although variably effective, fluid restriction does not pose a risk as long as the defect of water excretion persists. • On the other hand, repair of the aquaretic defect can lead to overcorrection and thus risk development of osmotic demyelination. • Prescription of stringent sodium restriction in patients with liver cirrhosis or heart failure helps control volume overload but counters correction or even aggravates hyponatremia. Adrogué H J , and Madias N E JASN 2012;23:1140-1148 Repairing the Abnormal State of the Determinants of Hyponatremia • Fluid restriction (up to <800 ml/d), excluding those with ongoing aquaresis • Increased solute intake (protein, sodium, and potassium), but limited Na intake in hypervolemic hyponatremia • Use of Loop diuretic (in euvolemic and hypervolemic hyponatremia) • Use of Vaptans in euvolemic or hypervolemic patients can be consider Urine/serum (U/S) electrolyte ratio • Can point out the effect of Urine output on the serum Na Levels – Ratio of 1: Urine output is not affecting the serum sodium – Ratio >1, urine contributes to lowering the serum sodium (perpetuating hyponatremia) – Ratio ≤0.5, urine contributes to raising the serum sodium (water diuresis present) • The larger the urine output, the greater the effect on serum sodium. Hospital-acquired hyponatremia—why are hypotonic parenteral fluids still being used? • Hospitalized patients have numerous stimuli for arginine vasopressin production and are at risk of developing hyponatremia • Routine administration of hypotonic parenteral fluid to hospitalized patients can result in fatal hyponatremia encephalopathy • 0.9% NaCl (154 mmol/l) should be administered as prophylaxis against hyponatremia, except in the setting of a free water deficit or ongoing free water losses • Patients at greatest risk of developing neurological complications secondary to hyponatremia are children, premenopausal females, postoperative patients, and those with brain injury, brain infection or hypoxemia Michael L Moritz and Juan Carlos Ayus Nature Clinical Practice Nephrology (2007) 3, 374-382 Managing Profound Hyponatremia Teaching Points – Part 1 • Prompt correction in symptomatic hyponatremia enough to improve symptoms • Correct hyponatremia rapidly in the first few hours and then slow down, 4-6 mEq/L increased in Sodium levels is enough correction regardless of the severity of the hyponatremia • The use of Adrogue-Madias formula in the calculation of the rate of correction seem to be very helpful but does not replace the real-life close monitoring of Serum Na measurements. Managing Profound Hyponatremia Teaching Points – Part 2 • Limited correction to prevent neurologic injury (osmotic demyelination syndrome) – <10 mEq/L in a 24-hour period – <18 mEq/L in a 48-hour period • Stay well below these limits in patients at high risk of osmotic • Anticipate and manage reversible causes of hyponatremia • Vaptans are an option for the treatment of euvolemic and hypervolemic hyponatremia • Prospective studies are needed to clarify the role of treatment of chronic hyponatremia in Mortality • References: • 1. Hoorn EJ, Zietse R. Hyponatremia and Mortality: Moving Beyond Associations. Am J Kidney Dis. 2013. Published online doi:10.1053/j.ajkd.2012.09.019 2. Sood L, Sterns RH, Hix JK, Silver SM, Chen L. Hypertonic Saline and Desmopressin: A Simple Strategy for Safe Correction of Severe Hyponatremia. Am J Kidney Dis. 2013;61:571-578. 3. Berl T. An Elderly Patient with Chronic Hyponatremia. Clin J Am Soc Nephrol. 2013; 8: 469-475. 4. Jovanovich AJ, Berl T. Where vaptans do and do not fit in the treatment of hyponatremia. Kidney Int. 2013;83: 563-567. 5. Gankam-Kengne F, Ayers C, Khera A, de Lemos J, Maalouf NM. Mild hyponatremia is associated with an increased risk of death in an ambulatory setting. Kidney Int. 2013; 83: 700-706. 6. Adrogué HJ, Madias NE. The challenge of hyponatremia. J Am Soc Nephrol. 2012; 23:1140-1148. 7. Chawla A, Sterns RH, Nigwekar SU, Cappuccio JD. Mortality and serum sodium: do patients die from or with hyponatremia? Clin J Am Soc Nephrol. 2011;6:960965. 8. Gross PA, Wagner A, Decaux G. Vaptans are not the mainstay of treatment in hyponatremia: perhaps not yet. Kidney Int. 2011;80:594-600. • • • • • • • • • • • • • • • • • • • 9. Sterns R, Hix J. Hyponatremia: Vasopressin antagonists in hyponatremia: more data needed. Nature Reviews Nephrology. 2011;7:132-133. 10. Rozen-Zvi B, Yahav D, Gheorghiade M, Korzets A, Leibovici L, Gafter U. Vasopressin Receptor Antagonists for the Treatment of Hyponatremia: Systematic Review and Meta-analysis. Am J Kidney Dis. 2010; 56:325-337. 11. Sterns RH, Hix JK, Silver S. Treating Profound Hyponatremia: A Strategy for Controlled Correction. Am J Kidney Dis. 2010;56:774-779. 12. Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170:294-302. 13. Vaidya C, Warren HO, Freda BJ. Management of hyponatremia: Providing treatment and avoiding harm. Cleve Clin J Med. 2010;77:715-726. 14. Greenberg A, Lehrich RW. Treatment of chronic hyponatremia: now we know how, but do we know when or if? J Am Soc Nephrol. 2010;21:552-555. 15. Kamel KS, Halperin ML. Managing overly rapid correction of chronic hyponatremia: an ounce of prevention or a pound of cure? J Am Soc Nephrol. 2010;21:2015-2016. 16. Schrier RW. Does 'asymptomatic hyponatremia' exist? Nature Reviews Nephrology. 2010; 6:185. 17. Ireland R. Hyponatremia: Prolonged use of the vasopressin antagonist tolvaptan is a safe and effective treatment for hyponatremia. Nature Reviews Nephrology. 2010;6:315. 18. Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122:857-865. 19. Sterns RH, Hix JK. Overcorrection of hyponatremia is a medical emergency. Kidney Int. 2009; 76:587-589. 20. Gankam Kengne F, Soupart A, Pochet R, Brion J-P, Decaux G. Re-induction of hyponatremia after rapid overcorrection of hyponatremia reduces mortality in rats. Kidney Int. 2009;76:614-621. • • • • • • • • • • • • • • • 21. Liamis G, Milionis H, Elisaf M. A Review of Drug-Induced Hyponatremia. Am J Kidney Dis. 2008;52:144-153. 22. Perianayagam A, Sterns RH, Silver SM, et al. DDAVP is effective in preventing and reversing inadvertent overcorrection of hyponatremia. Clin J Am Soc Nephrol. 2008;3:331-336. 23. Decaux G, Musch W. Clinical laboratory evaluation of the syndrome of inappropriate secretion of antidiuretic hormone. Clin J Am Soc Nephrol. 2008;3:1175-1184. 24. Hew-Butler T, Ayus JC, Kipps C, et al. Statement of the Second International Exercise-Associated Hyponatremia Consensus Development Conference, New Zealand, 2007. Clin J Sport Med. 2008; 18:111-121. 25. Sterns RH, Silver SM. Cerebral salt wasting versus SIADH: what difference? J Am Soc Nephrol. 2008; 19:194196. 26. Berl T. Impact of solute intake on urine flow and water excretion. J Am Soc Nephrol. 2008; 19:1076-1078. 27. Shea AM, Hammill BG, Curtis LH, Szczech LA, Schulman KA. Medical Costs of Abnormal Serum Sodium Levels. J Am Soc Nephrol. 2008; 19:764-770. 28. Lehrich RW, Greenberg A. When Is It Appropriate to Use Vasopressin Receptor Antagonists? J Am Soc Nephrol. 2008; 19:1054-1058. 29. Gankam Kengne F, Andres C, Sattar L, Melot C, Decaux G. Mild hyponatremia and risk of fracture in the ambulatory elderly. QJM. 2008; 101:583-588. 30. Verbalis JG, Goldsmith SR, Greenberg A, Schrier RW, Sterns RH. Hyponatremia Treatment Guidelines 2007: Expert Panel Recommendations. Am J Med. 2007; 120:S1-S21. 31. Rosner MH, Kirven J. Exercise-associated hyponatremia. Clin J Am Soc Nephrol. 2007; 2:151-161. 32. Mohmand HK, Issa D, Ahmad Z, Cappuccio JD, Kouides RW, Sterns RH. Hypertonic saline for hyponatremia: risk of inadvertent overcorrection. Clin J Am Soc Nephrol. 2007; 2:1110-1117. 33. Ellison DH, Berl T. The Syndrome of Inappropriate Antidiuresis. New England Journal of Medicine. 2007;356:2064-2072. 34. Halperin ML, Kamel KS. A new look at an old problem: therapy of chronic hyponatremia. Nat Clin Pract Nephrol. 2007; 3:2-3. 35. Chen S, Jalandhara N, Batlle D. Evaluation and management of hyponatremia: an emerging role for vasopressin receptor antagonists. Nat Clin Pract Nephrol. 2007; 3:82-95. • • • • • • • • • • • • • • • • • • 36. Moritz ML, Ayus JC. Hospital-acquired hyponatremia—why are hypotonic parenteral fluids still being used? Nat Clin Pract Nephrol. 2007; 3:374382. 37. Upadhyay A, Jaber BL, Madias NE. Incidence and Prevalence of Hyponatremia. Am J Med. 2006; 119:S30-S35. 38. Verbalis JG. AVP receptor antagonists as aquaretics: review and assessment of clinical data. Cleve Clin J Med. 2006;73 Suppl 3:S24-S33. 39. Schrier RW, Gross P, Gheorghiade M, et al. Tolvaptan, a Selective Oral Vasopressin V2-Receptor Antagonist, for Hyponatremia. New England Journal of Medicine. 2006; 355:2099-2112. 40. Almond CS, Shin AY, Fortescue EB, et al. Hyponatremia among Runners in the Boston Marathon. New England Journal of Medicine. 2005; 352:1550-1556. 41. Verbalis JG. Vasopressin V2 receptor antagonists. J Mol Endocrinol. 2002; 29:1-9. 42. Gross P, Reimann D, Henschkowski J, Damian M. Treatment of severe hyponatremia: conventional and novel aspects. J Am Soc Nephrol. 2001; 12 Suppl 17:S10-S14. 43. Schwartz WB, Bennett W, Curelop S, Bartter FC. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. 1957. J Am Soc Nephrol. 2001; 12:2860-2870. 44. Baker EA, Tian Y, Adler S, Verbalis JG. Blood-brain barrier disruption and complement activation in the brain following rapid correction of chronic hyponatremia. Exp Neurol. 2000;165:221-230. 45. Lauriat SM, Berl T. The hyponatremic patient: practical focus on therapy. J Am Soc Nephrol. 1997;8:1599-1607. 46. Sterns RH, Cappuccio JD, Silver SM, Cohen EP. Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective. J Am Soc Nephrol. 1994; 4:1522-1530. 47. Clark BA, Shannon RP, Rosa RM, Epstein FH. Increased susceptibility to thiazide-induced hyponatremia in the elderly. J Am Soc Nephrol. 1994; 5:1106-1111. 48. Soupart A, Penninckx R, Crenier L, Stenuit A, Perier O, Decaux G. Prevention of brain demyelination in rats after excessive correction of chronic hyponatremia by serum sodium lowering. Kidney Int. 1994; 45:193-200. 49. Soupart A, Penninckx R, Stenuit A, Perier O, Decaux G. Treatment of chronic hyponatremia in rats by intravenous saline: Comparison of rate versus magnitude of correction. Kidney Int. 1992; 41:1662-1667. 50. Verbalis JG, Martinez AJ, Drutarosky MD. Neurological and neuropathological sequelae of correction of chronic hyponatremia. Kidney Int. 1991; 39:1274-1282. 51. Berl T. Treating hyponatremia: Damned if we do and damned if we don't. Kidney Int. 1990; 37:1006-1018. 52. Ayus JC, Krothapalli RK, Arieff AI. Treatment of Symptomatic Hyponatremia and Its Relation to Brain Damage. New England Journal of Medicine. 1987; 317:1190-1195. 53. Arieff AI. Hyponatremia, Convulsions, Respiratory Arrest, and Permanent Brain Damage after Elective Surgery in Healthy Women. New England Journal of Medicine. 1986; 314:1529-1535.
© Copyright 2026