Management of Hyponatremia in Hospitalized Patients Role of Pharmacists in Improving Patient Care
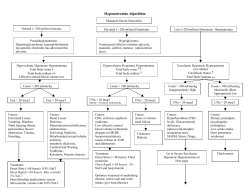
ASHP Advantage e-Newsletter March March2012 2011 Management of Hyponatremia in Hospitalized Patients Role of Pharmacists in Improving Patient Care Educational Initiative Targets Need for Improved Management of Hyponatremia ASHP Advantage is coordinating a series of learning opportunities on the management of hyponatremia in hospitalized patients. The learning opportunities are designed to build upon each other to educate pharmacists about the characteristics and treatment of hyponatremia of varying degrees, as well as to provide pharmacists with practical strategies for improving the management of hyponatremia for inpatients and after discharge. The series is supported by an educational grant from Otsuka America Pharmaceutical, Inc. The educational activities included both live and ondemand formats, and faculty members are nationally recognized experts in critical care and electrolyte disturbances. A live symposium was conducted on December 5, 2011, during the 46th ASHP Midyear Clinical Meeting and Exhibition in New Orleans, Louisiana. The symposium was simultaneously webcast, enabling a total of more than 1000 individuals to participate. Attendees submitted questions about unresolved issues related to the management of hyponatremia, and these were addressed by Initiative Chair Joseph F. Dasta, M.S., FCCM, FCCP, and faculty member Michael J. Cawley, Pharm.D., RRT, CPFT, in a live webinar on February 15, 2012. These frequently asked questions also serve as the basis of content explored in the two e-newsletters that are part of the educational initiative. If you missed the Midyear symposium, it is now available as a web-based activity and is approved for two hours of continuing pharmacy education credit. Downloaded from www.ashpadvantage.com/hyponatremia Its on-demand format is convenient since it may be completed at any time. For more information and to access the web-based activity, go to the web portal at www.ashpadvantage.com/hyponatremia. Faculty Roundtable Visit the Hyponatremia web portal or click here to listen to Professor Joseph Dasta and fellow faculty Drs. Michael Cawley and Henry Cohen discuss important aspects of managing hyponatremia in hospitalized patients. The discussion is available in three parts, each lasting 10 to 12 minutes: Overview of Hyponatremia Issues Related to Treatment Options Role of Pharmacists Why Focus on Hyponatremia? While there is not uniform agreement in the range for normal serum sodium concentration, in general hyponatremia is considered to be a serum sodium concentration less than 135 mEq/L.1 Hyponatremia is the most common electrolyte disorder in hospitalized patients, affecting 6-15% of patients at the time of admission and an additional 5% of patients during their hospital stay.2,3 One in four patients in the intensive care unit is hyponatremic. If not treated appropriately, hyponatremia can lead to substantial morbidity and mortality.4,5 Even small reductions in serum sodium concentration are associated with prolonged hospital lengths of stay and increased costs.6 Page 1 ASHP Advantage e-Newsletter Figure 1. Classification of Hyponatremia1 Dilutional Hyponatremia Total body sodium near normal Total body water increased Hypervolemic (edema) Heart failure Cirrhosis Nephrotic syndrome Depletional Hyponatremia Hypovolemic Sodium lost Total body water reduced Euvolemic (no edema) SIADH = syndrome of inappropriate antidiuretic hormone Hyponatremia can be classified as either depletional or dilutional (Figure 1).1 Depletional hyponatremia is relatively uncommon. It is characterized by hypovolemia with reduced total body water and sodium. The majority of cases of hyponatremia are dilutional and characterized by increased total body water and near normal total body sodium. Dilutional hyponatremia may be further classified as hypervolemic or euvolemic.1,7 Heart failure is a common cause of hypervolemic hyponatremia, and edema typically is present. Edema usually is absent in euvolemic hyponatremia, the most common cause of which is syndrome of inappropriate antidiuretic hormone (SIADH).7 Tumors and a wide variety of disorders, conditions, and medications (e.g., carbamazepine, selective serotonin-reuptake inhibitors) can lead to SIADH.3 The management of hyponatremia in the hospital setting is based on the severity of the electrolyte abnormality and neurologic symptoms3,7,8: Asymptomatic: fluid restriction to 500-1000 mL/day Moderate symptoms (e.g., confusion, altered mental status): 3% sodium chloride ± loop diuretic or vasopressin receptor antagonist followed by fluid restriction Severe (<120 mEq/L) symptoms (e.g., seizures, coma): 3% sodium chloride ± loop diuretic followed by fluid restriction ± vasopressin receptor antagonist This e-newsletter features frequently asked questions (FAQs) addressed by the faculty pertaining to current Downloaded from www.ashpadvantage.com/hyponatremia March 2012 information about the use of traditional therapies, such as hypertonic saline, for the management of hyponatremia in hospitalized patients. Answers to FAQs about new and emerging therapies and cost considerations related to the use of these therapies for the management of hyponatremia in hospitalized patients will be provided in the next e-newsletter. Frequently Asked Questions Q A What is known about the real-world use of therapies for hyponatremia? There is a paucity of information about the treatment of hyponatremia. Data from a prospective observational hyponatremia registry may provide insight into how various therapies are used in hospital settings.9 This first of its kind registry includes clinical and laboratory findings from patients either admitted with hyponatremia or with hyponatremia developing during hospitalization within or outside the United States. As of December 2011, almost 1800 patients had been enrolled in the registry, with a target enrollment of 2500 patients in the United States. Preliminary analysis of the findings reveals that 40% of patients were discharged from the hospital with a serum sodium concentration less than 130 mEq/L (i.e., hyponatremia), which may reflect problems with the use of currently available therapies for hyponatremia (e.g., failure to recognize and treat hyponatremia, improper use of currently available therapies, or lack of efficacy of currently available therapies despite attempts at optimal use of these therapies). Further insight is anticipated as additional data are collected in the registry. Q Can you provide information about the proper use of hypertonic sodium chloride to treat hyponatremia, including how to determine the amount of sodium chloride needed and the infusion rate? Is there a maximum recommended rate of infusion? A Hypertonic saline (i.e., 3% sodium chloride) is appropriate for patients with hyponatremia who are symptomatic (i.e., with an altered neurologic examination, confusion, seizure, or coma) or in a critical care unit.10-12 Overly rapid correction of hyponatremia can result in osmotic demyelination syndrome (ODS), a brain demyelinating disease that causes significant Page 2 ASHP Advantage e-Newsletter morbidity and mortality.7,8,13 The rate of infusion of sodium chloride for patients with severe symptoms should not exceed 1-2 mEq/L/hr.1 Furthermore, the sodium correction should not exceed 12 mEq/L over a 24-hour period or 18 mEq/L over the first 48 hours.1,7 These rate limits minimize the risk for ODS. The need for complex calculations to determine the sodium deficit and sodium chloride infusion rate is a potential problem related to the use of hypertonic saline. More than one method is available to perform these calculations, and no one method is the gold standard. The sodium deficit calculation provides only a rough estimate because its accuracy depends on the frequency of serum sodium monitoring.14 The onset of effect of hypertonic sodium chloride depends on the sodium concentration of the infusate and the rate of infusion because its bioavailability is 100% by the intravenous route. Sodium Deficit Method The sodium deficit method entails determining the difference between the current and desired serum sodium concentrations (mEq/L) and multiplying the result by the total body water (TBW). A serum sodium of 120 mEq/L is a suitable goal for patients with severe hyponatremia. The TBW (L) can be estimated by multiplying the body weight (kg) by a correction factor of 0.6 L/kg for men and 0.45 L/kg for women. Here is an example. Consider a 45-kg woman with an acute seizure and a serum sodium concentration of 106 mEq/L in whom a sodium of 120 mEq/L is desired. For this patient, the sodium deficit is 284 mEq, which was determined as follows: (120 mEq/L–106 mEq/L) x 45 kg x 0.45 L/kg = 284 mEq March 2012 Faculty Joseph F. Dasta, M.S., FCCM, FCCP Initiative Chair Professor Emeritus The Ohio State University College of Pharmacy Columbus, Ohio Adjunct Professor The University of Texas College of Pharmacy Austin, Texas Michael J. Cawley, Pharm.D., RRT, CPFT Associate Professor of Clinical Pharmacy Philadelphia College of Pharmacy University of the Sciences Philadelphia, Pennsylvania Henry Cohen, M.S., Pharm.D., BCPP, FCCM, CGP Professor of Pharmacy Practice Arnold & Marie Schwartz College of Pharmacy and Health Sciences Long Island University Chief Pharmacotherapy Officer Kingsbrook Jewish Medical Center Brooklyn, New York of sodium, the initial rate of infusion would be 58 mL/hr (determined by dividing 30 mEq/hr by 0.513 mEq/mL). If sodium chloride 0.9%, which contains 154 mEq/L (0.154 mEq/mL) of sodium, were used, an infusion rate of 195 mL/hr would be needed to correct the same 284mEq deficit. Adrogué-Madias Equation Another method used to guide the administration of hypertonic saline is the Adrogué-Madias equation, which allows estimation of the effect of infusing 1 L of an infusate on serum sodium concentration15: How should the deficit of 284 mEq in this patient be corrected? As noted previously, the rate of sodium correction for patients with severe symptoms should not exceed 1-2 mEq/L/hr. Using the midpoint of that range (1.5 mEq/L/hr) for this patient and TBW of 20.25 L (calculated as 45 kg x 0.45 L/kg), the rate would be 30 mEq/hr (calculated as TBW x 1.5 mEq/L/hr). This rate would be used only for the first several hours, checking the serum sodium frequently (every two hours) to avoid overcorrection and to stay within the maximum increase of 12 mEq/L in 24 hours. Using sodium chloride 3%, which contains 513 mEq/L (0.513 mEq/mL) Consider the patient used in the previous example. Using the correction factor of 0.45 L/kg for the 45kg woman with an acute seizure and serum sodium concentration of 106 mEq/L who will receive 3% sodium chloride, which contains 513 mEq/L of sodium, the change in serum sodium would amount to 19.1 mEq/L. Because 12 mEq/L over a 24-hour period is the maximum recommended increase in serum Downloaded from www.ashpadvantage.com/hyponatremia Page 3 Change in serum sodium = (infusate sodium – serum sodium) (total body water + 1) ASHP Advantage e-Newsletter March 2012 sodium to avoid neurological sequelae, 632 mL is the maximum volume of 3% sodium chloride that should be administered to this patient over a 24-hour period (this amount is calculated by dividing 12 mEq/L by 19.1 mEq/L per L of infusate = 0.632 L). Since 1.5 mEq/L/hr is the maximum recommended rate of sodium correction for the first several hours in patients with severe symptoms (e.g., 6 mEq/L for 4 hours, with frequent monitoring of serum sodium at 2-hour intervals), the 3% sodium chloride could be administered to this patient at a rate of approximately 80 mL/hr for 4 hours (determined by dividing 6 mEq/L by 19.1 mEq/L per L of infusate = 0.314 L or 314 mL), followed by a rate of approximately 16 mL/hr for 20 hours (determined by subtracting the 320 mL of infusate delivered over the first 4 hours from the 632 mL needed for the 24-hour period). If 0.9% sodium chloride, which contains 154 mEq/L of sodium, were used instead of 3% sodium chloride in this patient, the Adrogué-Madias equation predicts a change in serum sodium of 2.3 mEq/L per liter of infusate, and 5217 mL would be the calculated maximum volume that would be administered to this patient over a 24-hour period. This could work in theory using an initial rate of 652 mL/hr for 4 hours, followed by approximately 130 mL/hr for 20 hours. Administering 5 L in 24 hours, however, would not be an appropriate treatment of hyponatremia and potentially may lead to significant adverse effects. A more concentrated form of sodium chloride is needed. “ These are just two of many strategies for determining the sodium deficit of patients with hyponatremia and recommended administration rates of hypertonic saline. The primary reason pharmacists should be familiar with equations like these is not to calculate a precise administration rate for a patient but rather to determine whether the prescribed initial rate of hypertonic sodium chloride is reasonable and safe and then to monitor serum sodium closely to avoid overcorrection. -- Michael J. Cawley, Pharm.D., RRT, CPFT ” Q A Should 3% sodium chloride be administered only via central venous access? The maximum recommended osmolarity for a solution administered into a peripheral vein is 900 mOsm/L because the use of solutions with a higher osmolarity can lead to thrombophlebitis. The osmolarity Downloaded from www.ashpadvantage.com/hyponatremia of 3% sodium chloride is approximately 1026 mOsm/L, so central venous access is preferred.16 However, central venous access is not always feasible in the pre-hospital and emergency department settings. The vessel size, volume to be infused, and rate of infusion must also be taken into consideration in making decisions about how to administer 3% sodium chloride. Q A Can hypertonic sodium chloride be administered as a bolus in an emergent situation? Rapid infusion of hypertonic sodium chloride has been used for patients with seizures, coma, acute water intoxication (e.g., marathon runners), or traumatic brain injury.17 Based on this experience, infusion of 100 mL of 3% sodium chloride over 10 minutes to raise the serum sodium concentration by 2-4 mEq/L or 250 mL of 3% sodium chloride infused over 30 minutes to raise the serum sodium concentration by 4-6 mEq/L is recommended.18 Serum sodium concentrations should be monitored every 2-3 hours for the first 12-24 hours during 3% sodium chloride administration. Q A Is there a role for oral sodium chloride in the management of hyponatremia? In theory, oral sodium chloride might be an option for patients with chronic hyponatremia. However, randomized trials comparing oral with intravenous sodium chloride for the management of hyponatremia have not been performed. Traditionally 1-2 g three times daily has been used when sodium chloride was given orally, but no consistent dosing strategy for oral sodium chloride in patients with hyponatremia is available in the published literature. Gastrointestinal intolerance (e.g., nausea, vomiting, diarrhea) is a potential problem with oral therapy. Oral sodium chloride is not mentioned as an option in hyponatremia treatment guidelines released in 2007.7 Sign up to be notified of updates related to this educational initiative. The second e-newsletter in this series will focus on FAQs about the clinical and economic impact of newer agents on the management of hyponatremia. www.ashpadvantage.com/hyponatremia Page 4 ASHP Advantage e-Newsletter March 2012 References 1. Cawley MJ. Hyponatremia: current treatment strategies and the role of vasopressin antagonists. Ann Pharmacother. 2007; 41:840-50. 2. Deitelzweig S, McCormick L. Hyponatremia in hospitalized patients: the potential role of tolvaptan. Hosp Prac. 2011; 39:87-98. 3. Upadhyay A, Jaber BL, Madias NE. Epidemiology of hyponatremia. Sem Nephrol. 2009; 29:227-338. 4. Wald R, Jaber BL, Price LL et al. Impact of hospitalassociated hyponatremia on selected outcomes. Arch Intern Med. 2010; 170:294-302. 5. Zilberberg MD, Exuzides A, Spalding J et al. Epidemiology, clinical and economic outcomes of admission hyponatremia among hospitalized patients. Curr Med Res Opin. 2008; 24:1601-8. 6. Callahan MA, Do HT, Caplan DW et al. Economic impact of hyponatremia in hospitalized patients: a retrospective cohort study. Postgrad Med. 2009; 121:186-91. 7. Verbalis JG, Goldsmith SR, Greenberg A et al. Hyponatremia treatment guidelines 2007: expert panel recommendations. Am J Med. 2007; 120(suppl 1):S1S21. 8. Kumar S, Berl T. Diseases of water metabolism. In: Berl T, Bonventre JV, eds. Atlas of diseases of the kidney. Vol 1. Philadelphia: Current Medicine, Inc.; 1999:1.1-1.22. 9. Dasta J, Amin A, Chiong et al. Trends in hyponatremia management and associated outcomes in hospital settings: interim results from an observational, prospective, multicenter, global registry in hospitalized 10. 11. 12. 13. 14. 15. 16. 17. 18. patients. Presented at American College of Clinical Pharmacy Annual Meeting. Pittsburgh, PA; 2011 Oct 18. Poster 95E. Laureno R, Karp BI. Myelinolysis after correction of hyponatremia. Ann Intern Med. 1997; 126:57-62. Achinger SG, Moritz ML, Ayus JC. Dysnatremias: why are patients still dying? Med J. 2006; 99:353-62. Goldsmith SR. Current treatments and novel pharmacologic treatments for hyponatremia in congestive heart failure. Am J Cardiol. 2005; 95(suppl):14B-23B. Janicic N, Verbalis JG. Evaluation and management of hypo-osmolality in hospitalized patients. Endocrinol Metab Clin N Am. 2003; 32:459-81. Mohmand HK, Issa D, Ahmad Z et al. Hypertonic saline for hyponatremia: risk of inadvertent overcorrection. Clin J Am Soc Nephrol. 2007; 2:1110-7. Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000; 342:1581-9. Roche e Silva M, Velasco IT, Porfirio MF. Hypertonic saline resuscitation: saturated salt-dextran solutions are equally effective, but induce hemolysis in dogs. Crit Care Med. 1990; 18:203-7. Noakes T, IMMDA. Fluid replacement during marathon running. Clin J Sport Med. 2003; 13:309-18. Sterns RH, Nigwekar SU, Hix JK et al. The treatment of hyponatremia. Semin Nephrol. 2009; 29:282-99. Additional ASHP Advantage Educational Activities Visit the ASHP Advantage website to browse listings of convenient on-demand continuing education (CE) activities, as well as publications, podcasts, and live webinars. More than 40 hours of free ondemand CE programming are available. Learn more and find a full listing of topics and activities at http://www.ashpadvantage.com. For complete information about educational activities that are part of this initiative, visit www.ashpadvantage.com/hyponatremia. There is no charge for the activities, and ASHP membership is not required. Planned and coordinated by ASHP Advantage and supported by an educational grant from Otsuka America Pharmaceutical, Inc. Contact ASHP Advantage for assistance or questions. Downloaded from www.ashpadvantage.com/hyponatremia Copyright 2012 Trademark ASHP Privacy Policy Page 5
© Copyright 2026