A Comparative Study of Anemia among Pregnant Women in Rural
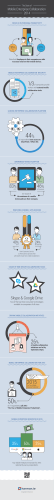
Sciknow Publications Ltd. Health Care ©Attribution 3.0 Unported (CC BY 3.0) HC 2015, 3(2):21-26 DOI: 10.12966/hc.05.01.2015 A Comparative Study of Anemia among Pregnant Women in Rural and Urban Areas of Ogun State, Southwest, Nigeria Oluwafolahan O. Sholeye1,2,*, Olubukunola A. Jeminusi1,2, Tessie O. Shorunmu2, Albert A. Salako1,2, Ramota Ademola-Raheem2 1 Department of Community Medicine and Primary Care, Olabisi Onabanjo University Teaching Hospital, Sagamu, Ogun State, Nigeria Faculty of Clinical Sciences, Olabisi Onabanjo University, Ogun State, Nigeria 2 *Corresponding author (Email: [email protected]) Abstract - A major contributor to the high levels of pregnancy – related morbidity and mortality, is anemia in pregnancy, often precipitated by poor dietary intake of iron and other mineral elements. Anemia in pregnancy is a global problem requiring concerted efforts to reduce its impact on maternal morbidity and mortality. A cross-sectional comparative study on the prevalence of anemia was carried out among 720 pregnant women at selected Primary Health Centers in rural and urban areas of Ogun state, southwestern Nigeria, using multi-stage sampling technique. Severe anemia was found in 1.7% of rural participants and 2.8% of urban participants; 17.2% of rural participants and 12.2% of urban participants had moderate anemia. More respondents in the rural (51.1%) and urban areas (62.2%) had normal hemoglobin concentration values. There was a significant difference (p=0.009) between the hemoglobin concentrations of rural and urban respondents. Regular dietary intake of iron, folate and other mineral elements in form of supplements should be encouraged. Keywords - Anemia, Pregnant, Rural, Urban, Ogun 1. Introduction In many developing countries of the world, particularly in Southeast Asia and sub-Saharan Africa, the maternal mortality and morbidity ratios are unacceptably high. Several strategies have been put in place to correct the anomaly, at international, country and local levels (Cohen and Richards, 1994; World Bank, 1994). A major contributor to the high levels of pregnancy – related morbidity and mortality, is anemia in pregnancy, often precipitated by poor dietary intake of iron and other mineral elements (Madukosiri and Adoga, 2011). The World Health Organization has identified anemia in pregnancy as a global problem requiring concerted efforts to reduce its impact on maternal morbidity and mortality (WHO, 1992). It is more common in developing countries than in developed ones. Studies show that prevalence of anemia in pregnancy in developing countries of Africa, Asia and Latin America, range from 35% to 75% in contrast to less than 30% in the United States (Vanderjagt et al, 2007; Brahin et al, 2001; Van den Broek, 1998). According to the World Health Organization, about 42% of all pregnant women worldwide are anemic, with 90% of these living in Africa and Asia (McLean et al, 2009). Pregnant women are at an increased risk for iron and multi-nutrient deficiency, as well as iron deficiency anemia (Mungen, 2003) - Maternal deaths from anemia in the developing world have been documented to vary significantly from 34 per 100,000 live births in Nigeria, to 194 per 100,000 live births in Pakistan (Vanderjagt et al, 2007; WHO, 1996). About 20% of maternal deaths in Africa have been attributed to anemia (Harrison, 1975).Severe anemia may directly cause death and even mild anemia may increase the probability that hemorrhage or exhaustion will be fatal (Ross, 1998; Nnaem and Udofia, 2010).An association has been shown to exist between maternal hemoglobin concentration and birth weight, as well as between maternal hemoglobin concentration and preterm birth (Ramussen, 2001; Scholl, 2005).In northern Tanzania, the prevalence of anemia among study participants was 47.4%; mild anemia accounted for 35.3%; moderate anemia was found in 9.9% of subjects; only 2.1% of the women had severe anemia. Analysis of pregnancy outcomes showed that anemic women were more likely to have low birth weight infants, compared with their non-anemic counterparts (Msuya et al, 2011). A study of the hematocrit levels of 530 gravid women in Enugu, south eastern Nigeria, found a prevalence of 40.4% for anemia in pregnancy. Of these, 90.7% were mildly anemic; 9.3% were moderately anemic; while no case of severe anemia was reported (Dim and Onah, 2007). A total of 735 pregnant women participated in a study on maternal hematocrit and pregnancy outcome in Ibadan. These women were followed up from the booking clinic until delivery. At booking, 15% of the women were anemic, while in labor, only about 10.4% remained anemic. Mild anemia was reported in 6.6% of study participants, while moderate anemia was found in only 3.8% 22 Health Care (2015) 21-26 of the women studied. The proportion of mothers with negative birth outcomes like stillbirths was higher among patients with moderate anemia (Aimakhu et al, 2003). A cross-sectional study carried out in Abeokuta, Ogun State, reported about 76.5% of the pregnant women studied to be anemic at one trimester or the other. Of these, 57.8% were moderately anemic; 40.3% were mildly anemic; while 7% were severely anemic. Anemia was of a higher prevalence (80.6%) among primigravidae compared with the multigravidae (74.5%). All severely anemic women were aged less than 30 years. More women in the second trimester of pregnancy were anemic than in any other trimester (Idowu et al, 2005). Rural – urban differences in the prevalence of anemia in pregnancy have been documented in literature. In Owerri, southeast Nigeria, a study of the predisposing factors to iron deficiency anemia among 910 urban and 477 rural pregnant women, found an overall prevalence of 67.1% for iron deficiency anemia. Rural women had a significantly higher prevalence of anemia and significantly lower mean hemoglobin concentration compared with the urban subjects. Less-educated women, those aged 24 years and younger, as well as women with child spacing less than one year had significantly lower mean hemoglobin concentration and a significantly higher prevalence of anemia, compared with other study participants (Okwu and Ukoha, 2008). Nutritional factors, including multi-nutrient deficiency, have been associated with anemia in pregnant women in Nigeria and other developing countries of the world. Folate, Vitamin B12, Iron and other mineral elements have been found to be deficient among these groups of women (Vanderjagt et al, 2007; Abdelrahim et al, 2009; Al Khalib et al, 2006). This study therefore determined the prevalence of nutritional anemia among pregnant woman utilizing rural and urban Primary Health Centers. 2. Methodology Ogun state is located in the southwest geo-political zone of Nigeria. It was created in 1976 from the defunct Western Region and has twenty Local Government Areas, grouped into three senatorial districts in the state. It is bounded in the north by Oyo and Osun states, in the east by Ondo state, in the south by Lagos state and in the west by the Republic of Benin. The Ogun-East Senatorial zone is made up of nine Local Government Areas; Ogun Central senatorial zone is made up of five LGAs, while Ogun West senatorial zone has six LGAs comprising it. A cross-sectional comparative study was carried out among pregnant women at selected Primary Health Centers in rural and urban areas of Ogun state, between 4th December 2012 and 6th May 2013. The following categories of women were excluded from the study: a. Pregnant adolescents younger than 18 years and women older than 49 years of age; and, b. Women with bleeding disorders, peptic ulcer disease and chronic medical conditions, including hemoglob in pathies. The sample size was derived with a formula for the comparison of two independent proportions, N = (Z1-α/2 + Z1-β)2 [P1(1-P1) + P2(1-P2)] / (P1-P2)2 Using a prevalence of 30% for nutritional anemia in pregnancy, from a facility-based study in northern Nigeria(V anderjagt et al, 2007) and considering P1 – P2 to be 10%; N = (1.96 + 0.84)2 [0.3(0.7) + (0.2(0.8)] / (0.3 – 0.2)2 N = 290.008 Taking into account a 20% non-response rate, incompletely-filled questionnaires and other unforeseen challenges with data collection, the calculated sample size (N) was rounded up to 360, per group. A total of 720 pregnant women were studied in all. Multi – stage sampling technique was used for the selection of study participants. The first stage involved the selection of a senatorial district/zone, from the three zones present in the state, by simple random sampling resulted in the selection of Ogun-East senatorial zone. The second stage involved the selection of one rural and one urban LGA, by simple random sampling. Sagamu LGA was selected as the urban study location, out of the two urban LGAs, while Remo-North LGA was selected from a list of six LGAs, as the rural study location, by simple random sampling. Odogbolu LGA, which is classified as semi-urban, was exempted from the sampling frame. The third stage of sampling involved the selection of two wards, from each of the selected LGAs, by simple random sampling. In Remo-North LGA, wards 7 and 9 were selected from the 15 existing wards, by simple random sampling (balloting). The PHCs, located within the selected wards, constituted the rural study sites. In Sagamu LGA, wards 5 and 8 were selected through a process of simple random sampling (balloting). The PHCs, located within the two selected wards, constituted the urban study sites. Therefore, a total of four PHCs were utilized for the study in both LGAs. All pregnant women, who met the inclusion criteria and were willing to participate in the study, constituted the sampling frame. They were recruited consecutively till the desired sampling size was reached. Interviewer-administered, semi–structured questionnaires, pretested in Ikenne and Ijebu-Ode LGAs, were used to collect data on respondents’ socio-demographic characteristics, record Hb and PCV values. Hemoglobin (Hb) level was assessed using the hemoglobin meter. The finger prick technique was used. Participants had their first fingers cleaned with methylated spirit, which were allowed to dry up, after which a sterile lancet was used to pierce the skin. Blood samples measuring about 2.5millilitres in volume, were collected into the microcurvettes and loaded into a chamber in the hemoglobin meter. The Hb values were displayed on the monitor of the portable machine. New batteries were used for each PHC visited, in order to ensure the reliability of test results. Participants also had their packed cell volume (PCV) Health Care (2015) 21-26 measured using capillary tubes and a centrifuge, into which the tubes were loaded, prior to the measurement of the PCV, as documented in literature (Dim and Onah, 2007; Adinma et al, 2002; Gonzales et al, 2009). Data Analysis was done using the International Business Machines (2004) Statistical Package for the Social Sciences (SPSS) version 14.00. Anemia was defined as hemoglobin concentration less than 11g/dl and a Packed Cell Volume of less than 33%. Proportions, means and frequencies were calculated, presented as tables and charts, and compared between the two groups using the appropriate statistical tests. Chi square test and Fisher’s exact test were used to test for association between categorical variables, while t test was used for comparison of means. Level of significance was placed at p = 0.05. Ethical approval was obtained from the Ogun State Primary Health Care Board, Ogun State Ministry of Health, as well as the Health Research and Ethics Committee of Olabisi Onabanjo University Teaching Hospital, Sagamu. Written approval was also sought from the Local Government Health Authorities in Sagamu LGA and Remo-North LGA, through the Medical Officer for Health/Director, Primary Health Care Department. Participants’ informed consent was obtained verbally and by thumb printing, prior to the commencement of the study. Strict confidentiality was ensured throughout the course of the research. Participants were free to withdraw from the study, if they deemed it necessary and were assured that such would not affect the quality of care received at the facility. All hemoglobin concentration and packed cell volume results were made available to the respective participants, through the nursing staff on duty, at the four PHCs utilized for the study. 3. Results 3.1. Age of respondents 51.7% of rural and 53.9% of urban respondents were aged between 26 and 33 years. This was followed by those aged 18 – 25 years, comprising 27.2% and 26.4% of rural and urban respondents respectively. Only 19.4% of rural women and 17.8% of urban respondents were aged between 34 and 41years.The mean age of rural women (28.14 ± 5.49 years) was not significantly different (p=0.553) from that of the urban women (28.38 ±5.53 years). 3.2. Marital Status of respondents Almost 96% of respondents in both urban and rural areas were married. Both areas had only 3.1% of single respondents. Divorced and separated respondents constituted 1.3% and 1.1%of study participants at the rural and urban locations respectively. There was no significant association (p=0.945) between marital status and respondents’ location. 3.3. Respondents’ Parity More than a quarter (28.3%) of rural respondents had no 23 previous pregnancy greater than 28 weeks, compared with 23.3% of their urban counterparts. The proportion of respondents with more than five previous pregnancies, were 10.8% for rural and 13.3% for urban areas. The mean parity of respondents was 3.13 for rural and 3.32 for urban respondents. There was no significant difference (p=0.329) between both means. 3.4. Respondents’ Average Monthly Income Most respondents in the rural areas (62.5%) and urban areas (66.4%) earned NGN 2,000.00 or less monthly. About a third (34.4%) of respondents in the rural areas and 21.1% of respondents in the urban areas earned no income. The mean income of rural respondents (NGN 120.49 ± 37.17) was significantly lower (p=0.021) than the mean income of urban respondents (NGN 450 ±16.47). 3.5. Sewage Disposal Method About sixty-seven percent (67.2%) of rural respondents and 60.6% of urban respondents used water closets; 5.3% of rural respondents had no toilet facilities in their homes, while only 1.9% in the urban areas lacked toilet facilities. 3.6. Vegetable Consumption Pattern of Respondents Vegetable consumption pattern among respondents was found to be occasional among 21.7% of rural and 27.8% of urban women: three times or more a week for 34.4% of rural respondents compared with 31.1% for urban respondents; weekly among 30.0% of rural and 27.8% of urban respondents; daily among 13.9% and 13.3% of respondents. There was no significant difference (p=0.298) between the frequency of vegetable consumption of rural and urban participants. 3.7. Medical History and Use of mineral supplements (Table 1) Respondents with medical conditions like gestational Diabetes, Pregnancy – Induced Hypertension and Asthma accounted for 1.9% of rural women and 2.8% of urban study participants. About 85.0% of respondents in both rural and urban areas used Folic acid, Vitamin B Complex, Multivite, Iron and Vitamin C tablets daily. There was no significant difference (p=0.917) between both groups of study participants. 3.8. Hemoglobin Concentration and Packed Cell Volume (Table 2) Severe anemia was found in 1.7% of rural participants and 2.8% of urban participants; 17.2% of rural participants and 12.2% of urban participants had moderate anemia. More respondents in the rural (51.1%) and urban areas (62.2%) had normal hemoglobin concentration values. There was a significant difference (p = 0.009) between the hemoglobin concentratio ns of rural and urban respondents. The mean PCV of rural participants (33.1 ± 4.4) was significantly lower (p = <0.001) than the mean for urban participants (34.6 ± 4.6). Slightly 24 Health Care (2015) 21-26 higher proportions of normal participants (52.8% rural; 63.1% classification, there was also a significant difference between urban) were reported using the packed cell volume the PCV readings of both groups of women. Table 1. Medical History and Drug Use among Respondents Presence of medical conditions Yes No Use of mineral supplements Yes No Prescribed at antenatal clinic Yes No Location Rural (n=360) Urban (n=360) Frequency (%) Frequency (%) 7 (1.9) 10 (2.8) 353 (98.1) 350 (97.2) Rural ( =360) Urban (n=360) Frequency (%) Frequency (%) 305 (84.7) 306 (85.0) 55 (15.3) 54 (15.0) Rural (n=305) Urban (n=306) Frequency (%) Frequency (%) 266 (87.2) 278 (90.8) 39 (12.8) 28 (9.2) Test Statistic X2=0.542; p=0.462. X2 =0.071; p=0.917. X2=2.069; p=0.150. Table 2. Respondents’ Hemoglobin Concentration and Packed Cell Volume Hemoglobin concentration (g/dl) Severe anemia (less than 7.0) Moderate anemia (7.0 – 9.9) Mild anemia (10.0 – 10.9) Normal (11.0 and above) Packed Cell Volume (%) Severe anemia (less than 21.0) Moderate anemia (21.0 – 29.9) Mild anemia (30.0 – 32.9) Normal (33.0 and above) Mean (%) Location Rural (n=360) Urban (n=360) Frequency (%) Frequency (%) 6 (1.7) 10 (2.8) 62 (17.2) 44 (12.2) 108 (30.0) 82 (22.8) 184 (51.1) 224 (62.2) Rural (n=360) Urban (n=360) Frequency (%) Frequency (%) 5 (1.4) 62 (17.2) 103 (28.6) 190 (52.8) 33.1 ±4.4 9 (2.5) 43 (11.9) 81 (22.5) 227 (63.1) 34.6 ±4.6 4. Discussion The mean age of rural respondents was 28.14 ± 5.49 years while that of urban respondents was 28.38 ± 5.33 years, a finding that is different from a similar study in Balasore District India, where the mean age of all respondents was 24.2 years (Sahoo and Panda, 2006). There was no statistically significant difference between both means (p=0.553), There was a significant difference between the waste disposal methods of rural and urban respondents (p =0.002). The poor waste disposal practices is an established predisposing factor to parasitic infections and the resultant malnutrition, as reported in studies conducted in Nigeria and the Ghana (ORC Macro,2005;Egwunyenga et al,2001).Vegetable consumption was fair among study participants, with less than 14% of respondents reporting a daily consumption pattern; 34.4% and 31.1% consuming vegetables at least three days a week in rural and urban study locations respectively. This is consistent with findings from other studies in Nigeria and other countries, which reported sub-optimal dietary intake of vegetables and folate (Huybregs et al, 2009; Oguntona and Akinyele, 2002; Test statistic X2= 11.536; df = 3; p=0.009 X2=10.494; df=3; p=0.015. t=4.369; p=<0.001 Chang et al, 2009; Esmailzadeh et al, 2008).It is however different from the vegetable consumption patterns reported by researchers in the Vararian district of India and Osun State, southwest, Nigeria, where consumption of vegetables along with its folate content, were adjudged optimal (Ojofeitimi et al, 2008; Mehrotra and Tiwari, 2009). The slightly better vegetable consumption pattern among rural women compared to their urban counterparts could be as a result of availability of home-grown vegetables in rural areas in contrast to urban settlements. The hematological indices of respondents, in form of hemoglobin concentration and packed cell volume, were measured to determine the presence or otherwise of anemia, as documented in medical literature (Koryo-Dabrah et al, 2012;Saxena et al, 2000; Story and Alton, 1995). Hemoglobin concentration of respondents, classified according to World Health Organization guidelines, showed that 1.7% of rural participants and 2.8% of their urban counterparts were severely anemic, with Hb concentration less than 7.0g/dl. This is higher than previously reported findings from Sagamu, Health Care (2015) 21-26 where only 0.7% of the pregnant women were severely anemic (Lamina and Shorunmu, 2003). The observed difference between the proportions could be due to the fact that the previous study was carried out among women accessing the teaching hospital’s ANC services, while this study was strictly limited to women accessing PHC services. The time interval of 10 years, since the research was published, could also account for the difference observed between both results from the urban LGA. Although the proportion of severe anemia was higher among the urban respondents (2.8%), the values reported in this study are far lower than that reported by researchers in another urban LGA of Ogun State, where 7.0% of the women were severely anemic (Idowu et al, 2005).These findings contrast sharply with those from Enugu, Ibadan, and some other southeastern states and outside the Nigeria, where no case of severe anemia was reported among all their pregnant subjects (Msuya et al, 2011; Van den Broek et al, 2000; Dim and Onah, 2007; Adinma et al, 2002; Aimakhu et al, 2003). Moderate anemia was found in 17.2% of rural and 12.2% of urban respondents. These proportions are higher than findings from previous studies in Sagamu, Ibadan, Enugu and other countries, but lower than those from Orissa, India and Abeokuta, southwest, Nigeria (Lamina and Shorunmu, 2003; Aimakhu et al, 2003; Dim and Onah, 2007; Adinma et al, 2002; Idowu et al, 2005; Sahoo and Panda, 2006). More rural respondents (30.0%) were mildly anemic, compared with their urban counterparts with a prevalence of 22.8% for mild anemia. The prevalence of mild anemia among the rural pregnant women is similar to that reported in Abeokuta, where 30.8% of study participants were mildly anemic (Idowu et al, 2005). It however, contrasts with findings from Ibadan, where only 6.6% of study participants were mildly anemic (Aimakhu et al, 2003). Among the rural respondents, 51.1% had normal Hb concentrations, compared with 62.2% of urban women.This implies that 48.9% of rural respondents were anemic, while 37.8% of the urban women were anemic. These findings are consistent with WHO report on vitamins and minerals consumption, which states that 42% of pregnant women worldwide are anemic (McLean et al, 2009).The prevalence of anemia in this study is similar to those from studies in Enugu, Tanzania and Malawi, but lower than findings from Sagamu and Abeokuta (Msuya et al, 2011; Van den Broek et al 2000; Dim and Onah, 2007; Lamina and Shorunmu, 2003; Idowu et al, 2005). It is however much lower than findings from Sudan, where 80.3% of the pregnant women studied were anemic, with 14.3% having iron deficiency (Abdelrahim et al, 2009).The higher prevalence of anemia in the rural subjects is similar to results obtained in Owerri, southeast Nigeria (Okwu and Ukoha, 2008). Hemoglobin concentration was significantly associated with location (p=0.009) in this study. This is similar to findings in Owerri, where rural pregnant women had a significantly higher prevalence of anemia than their urban counterparts (Okwu and Ukoha, 2008). The mean PCV of rural participants (33.1 ± 4.4) was 25 significantly lower (p=0.000) than the mean PCV (34.6 ±4.6) of urban participants. The prevalence of anemia based on PCV measurements was slightly lower than that obtained using the participants’ Hb concentration. With the PCV classification, there was also a statistically significant difference (p=0.015) between the blood levels of rural and urban participants. With the various limitations of the use of PCV as an indicator of nutritional status in pregnancy, several studies have reported it alongside other parameters, particularly the hemoglobin concentration (Lamina and Shorunmu, 2003). Researchers in Sagamu, investigated 2,650 pregnant women accessing antenatal care at the teaching hospital for the presence of anemia in pregnancy. A prevalence of 55.3% was reported for anemia among the study participants. Most (88.9%) of the anemic participants had mild anemia, while moderate anemia was found in 10.4% of them. Only 0.7% of the pregnant women studied were found to be severely anemic, with a hemoglobin concentration of less than 7g/dl (Lamina and Shorunmu, 2003). Researchers in Anambra, southeast Nigeria, studied 186 booked pregnant women and reported a prevalence of 35.5% for anemia at booking, using a PCV of 30% as cut off point for anemia in pregnancy (Adinma et al, 2002). Nigeria hopes to meet the 2015 deadline for attainment of the Millennium Development Goals, but the health indices suggest otherwise. Maternal and peri-natal mortality can be significantly reduced if adequate mineral and vitamin intake, as well as optimal hemoglobin concentrations are promoted and monitored among pregnant women. The PHCs provide a unique opportunity for providing the best of care to women by well trained personnel. Since the Ward Health System is operational in Nigeria, nutrition education, hygiene education, dietary supplementation and other strategies, aimed at improving the health status of pregnant women and ultimately their chances of survival will have a very wide coverage, thereby achieving the desired results. The study excluded pregnant teenagers less than 18years and therefore could not report on the differences in the prevalence of anemia between rural and urban gravid teenagers. This study also did not follow up the participants to determine pregnancy outcome, due to its cross sectional comparative nature. Therefore, it could not test for association between maternal anemia and pregnancy outcome. This could be a subject for further research in the near future. However, the findings of this study typify the hematological profile of the generality of pregnant women in both rural and urban areas of Ogun State, Nigeria. 5. Conclusion The prevalence of anemia was higher among the rural pregnant women than their urban counterparts. Regular dietary intake of iron, folate and other mineral elements in form of supplements should be encouraged. 26 Health Care (2015) 21-26 Acknowledgement We are most grateful to our colleagues, Dr Tope Ladi-Akiny emi, Dr Solomon Oyetoyan, Mrs Adebisi Orenuga, Mr. Lekan Aina, and Professor Olayinka Abosede, for their very useful contributions to the completion of this study. References Abdelrahim, H., Adam, G. K., Mohammed, A. A., Salih, M. M., Ali, N. I., Elbashier, M. I. et al (2009). Anaemia, folate and vitamin B12 deficiency among pregnant women in an area of unstable malaria transmission in Eastern Sudan. Trans R Soc Trop Med Hyg. 103(5), 493 – 496. Adinma, J. I. B., Ikechebelu, J. I., Onyejimbe, U. N., Amilo, G., Adinma, E. (2002). Influence of antenatal care on haematocrit values of pregnant Nigerian Igbo women. Trop J ObstetGyneacol. 19, 68 -70. Aimakhu, C. O., Olayemi, O. (2003). Maternal haematocrit and pregnancy outcome in Nigerian women. West Afr J Med. 22, 18-21. Al Khalib, L., Obeid, O., Sibai, A. M., Batal, M., Adra, N., Hwalla, N. (2006). Folate deficiency is associated with nutritional anaemia in Lebanese women of childbearing age. Public Health Nutr. 9(7), 921-927. Africa Nutrition Chart books (2005). Nutrition of young children and mothers in Ghana: findings from the 2003 Ghana Demographic and Health Survey. Calverton, Maryland. ORC Macro. Brahin, B. J., Hakimi, M., Pelletier, D. (2001). An analysis of anaemia and pregnancy-related maternal mortality. J Nutr. 131, 4-5. Chang, Y., Dibley, M. J., Zhang, X., Zeng, L., Yan, H. (2009). Assessment of dietary intake among pregnant women in a rural area of western China. BMC Public Health. 9, 222. Cohen, S. A., Richards, C. L. (1994). The Cairo Consensus: Population, Development and Women. Int. Fam. Plann. Persp. 20, 150-155. Dim, C. C., Onah, H. E. (2007). Prevalence of anaemia in pregnant women at booking in Enugu, southeastern Nigeria. Med Gen Med. 9(3),11-14. Esmailzadeh, A., Sarareh, S., Azadbaklit, S. (2008). Dietary patterns among pregnant women in western Iran. Pak J Biol Sci. 11(5), 793-796. Egwunyenga, A. O., Ajayi, J. A., Nmorsi, O. P., Duhlinska-Papova, D. D. (2001). Plasmodium intestinal helminth co-infection among pregnant Nigerian women. MemInst Oswaldo Cruz. 96(8), 1055-1059. Gonzales GF, Steenl and K, Tapia V (2009). Maternal haemoglobin level and foetal outcome at low and high altitudes. American Journal of Physiology. 297(5), 1477-1485. Harrison, K. A. (1975). Maternal mortality and anaemia in pregnancy. West Afr Med J. 23:27-31.Huybregs LF, Roberfroid DA, Kolsteren PW, Van Camp JH. Dietary behavior, food and nutrient intake of pregnant women, in a rural community in Burkina Faso. Maternal Child Nutr. 2009; 5(3), 211- 222. Idowu, O. A., Mafiana, C. F., Sotiloye, D. (2005). Anaemia in pregnancy: a survey of pregnant women in Abeokuta, Nigeria. Afr Health Sci. 5(4), 295-299. International Business Machines (2004). Statistical Package for the Social Sciences. Version 14.00. Koryo-Dabrah, A., Nti, C. A., Adanu, R. (2012). Dietary practices and nutrient intakes of pregnant women in Accra, Ghana. Curr Res J Biol Sci. 4(4), 358-365. Lamina, M. A., Shorunmu, T. O. (2003). Prevalence of anaemia in pregnant women attending the antenatal clinic in a Nigerian University Teaching Hospital. Niger Med Pract. 44(2), 39-42. Madukosiri, C. H., Adoga, G. I. (2011). Elemental status of pregnant and lactating women in Bassa LGA of Plateau State, Nigeria. Pak J Nutr; 10(5), 401-404. McLean, E., Cogswell, M., Egli, I., Wojdyla, D., de Benoist, B. (2009). Worldwide prevalence of anaemia: World Health Organisation Vitamin and Mineral Information System, 1993 – 2005. Public Health Nutr. 12, 444-454. Mehrotra, M., Tiwari, S. (2009). Energy and protein consumption by pregnant women of Varanasi district. Indian J Prev. Soc Med. 40(1/2), 58 -62. Mungen, E. (2003). Iron supplementation in pregnancy. J Perinat Med. 31(5), 420-426. Msuya, S. E., Hussein, T. H., Uriyo, J., Sam, N. E., Stray-Pedersen, B. (2011). Anaemia among pregnant women in northern Tanzania: prevalence, risk factors and effect on perinatal outcomes. Tanzan J Health Res. 13(1), 40 – 49. Nnaem, N. M., Udofia, U. S. (2010). Food-based strategy to improve iron status of pregnant women in Nigeria. International Journal of Food Safety, Nutrition and Public Health. 3(1), 64-68. Oguntona, C. R., Akinyele, I. O. (2002). Food and nutrient intake by pregnant Nigerian adolescents during the third trimester. Nutrition. 18(7/8), 673-679. Ojofeitimi, E. O., Ogunjuyigbe, P. O., Sanusi, R. A., Orji, E. O., Akinlo, A., Liasu, S. A. (2008). Poor dietary intake of energy and retinol among pregnant women: implications for pregnancy outcome in southwest Nigeria. Pak J Nutr. 7(3), 480-484. Okwu, G. N., Ukoha, A. I. (2008). Studies on the predisposing factors of Iron Deficiency Anaemia among pregnant women in a Nigerian community. Pak J Nutr, 7(1), 151-156. Ramussen, K. (2001). Is there a causal relationship between iron deficiency or iron deficiency anaemia and weight at birth, length of gestation and perinatal mortality? J Nutr. 131(2S-2), 590-601. Ross, J., Horton, S. (1998). Economic consequences of iron deficiency. Ottawa, Canada. The Micronutrient Initative. Sahoo, S., Panda, B. (2006). A study of the nutritional status of pregnant women of some villages in Balasore District, Orissa. J Human Ecol. 20(3), 227-232. Saxena, V., Srivastava, V. K., Idris, M. Z., Mahan, U., Bhushan, V. (2000). Nutritional status of rural pregnant women. Indian J Community Med. 25(3):104-107. Scholl, T. O. (2005). Iron status during pregnancy: setting the stage for mother and infant. Am J ClinNutr. 81(5), 1218 – 1222. Story, M., Alton, J. (1995). Nutrition issues and adolescent pregnancy. Nutr Today. 30, 142-151. Vanderjagt, D. J., Brock, S. H., Melah, G. S., El-Nafaly, A. U., Crossey, M. J., Glew, R. H. (2007). Nutritional factors associated with anaemia in pregnant women in Northern Nigeria. Journal of Health, Population and Nutrition. 25(1), 75-81. Van den Broek, N. R. (1998). Anaemia in pregnancy in developing countries. Br J Obstet Gynaecol. 105, 385-390. Van den Broek, N. R., Rogerson, S. J., Mhango, C. G. (2000). Anaemia in pregnancy in southern Malawi: prevalence and risk factors. British Journal of Obstetrics & Gyneacology. 107, 437-438. World Bank (1994). A new agenda for women’s health and nutrition. Washington DC. The World Bank. World Health Organisation (1992). The prevalence of anaemia in women: a tabulation of available information. Second Edition. Geneva, WHO. World Health Organisation (1996). Prevention and management severe anaemia in pregnancy: report of a technical working group. Geneva. WHO: 20-22.
© Copyright 2026