Managing scoliosis in a primary-care setting
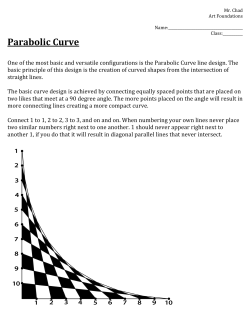
FEATURE: BY ERIN S. HART, RN, MS, CPNP, AND BRIAN E. GROTTKAU, MD Managing scoliosis in a primary-care setting Most often, clinicians are the first to diagnose this common spine condition. Two orthopedic specialists tell how you can help prevent disease progression. coliosis, the most common disorder of the spine encountered by primary-care clincians, is defined as a lateral curvature >10 degrees on x-ray accompanied by vertebral rotation (Figure 1).There are five categories of scoliosis: degenerative (adult onset), neuromuscular, congenital,secondary,and idiopathic. Degenerative scoliosis, generally seen in middle-aged and older patients,results from wear and tear on the vertebral elements over time. Neuromuscular scoliosis is a spinal curvature seen in those with cerebral palsy, muscular dystrophy, myelodysplasia (spina bifida), syrinx, diastematomyelia, or intraspinal tumor (Figure 2). There is also a very high incidence of scoliosis in neuromuscular patients who have a spinal-cord injury and are paraplegic/quadriplegic at a young age. Such patients can develop curve patterns similar to those seen with neuromuscular conditions but characterized by abnormal neurologic examination.* Spinal deformities caused by neuromuscular etiologies generally progress more rapidly than idiopathic scoliosis and are more difficult to manage without surgery. Congenital scoliosis is a fixed curvature that is present at birth (Figure 3).This form is caused by either the failure of certain vertebral bony anatomy to form, failures of segmentation, or a combination of the two. Curves may be noted on physical examination, but they often present as incidental findings on x-rays taken for other purposes.Once discovered,congenital hemivertebra, bars, or butterfly vertebrae need to be further characterized. The patient should also be S FIGURE 1. Typical x-ray of a patient with scoliosis, showing lateral curvature >10 degrees and vertebral rotation. . 1 THE CLINICAL ADVISOR • FEBRUARY 2006 THE CLINICAL ADVISOR • FEBRUARY 2006 1 SCOLIOSIS FIGURE 2. Neuromuscular scoliosis, seen in a patient with XXX. FIGURE 3. Congenital scoliosis seen on (type of imaging) evaluated for other developmental abnormalities that occur during embryogenesis. For example, genitourinary and cardiac abnormalities are frequently associated with spinal abnormalities because they all develop during the first six weeks of embryonic formation. The most common cause of secondary scoliosis is leglength discrepancy.This form of the disease often appears as lumbar scoliosis on physical examination; however, the asymmetry will disappear when the leg-length discrepancy is blocked and vertebral rotation will not be seen on radiographs. Other conditions that can give the clinical appearance of secondary scoliosis include muscle spasm, herniated nucleus pulposus,and postural faults. The most common category of scoliosis is idiopathic. It can be further subdivided into infantile (presenting at 3 years of age or older), juvenile (3-10 years of age) and adolescent (older than 10 years).Adolescent idiopathic scoliosis (AIS) accounts for 70%-85% of all cases of scoliosis,1 and it is the primary focus of this article. AIS generally presents in children aged 10-16 years and oftentimes is first noted either at school screenings or at wellchild visits with the primary-care clinician.There are no associated underlying congenital or neurologic abnormalities. Approximately 2%-3% of all adolescents will develop a curve >10 degrees on x-ray. However, the overall prevalence of curves measuring >30 degrees decreases to 0.3%. At this magnitude,the female-to-male ratio is 10:1. Although most patients with pediatric spinal deformities are referred to a pediatric orthopedic surgeon for definitive treat- ment,the conditions is usually diagnosed first by the primarycare clinician.Therefore, it is important to have a thorough understanding of scoliosis, including recognition and screening techniques, physical examination findings, and current surgical and nonsurgical treatment options. In addition, clinicians must determine which patients should be referred for pediatric orthopedic evaluation. Detecting scoliosis during adolescence has been shown to have a significant positive impact on the initial treatment plan and final outcome.2 2 THE CLINICAL ADVISOR • FEBRUARY 2006 History and physical examination: After a complete general history and physical examination,a focused musculoskeletal and neurologic-spine examination should be performed. It is important to obtain the patient’s standing height and weight at each visit so that growth can be assessed and monitored over time. Start the exam with a general inspection of the patient in the standing position. Look for obvious asymmetries, especially an elevated scapula, uneven shoulder height, unequal leg length, rib hump, thoracic and/or lumbar prominence, or an uneven waist crease. Cutaneous lesions should also be noted, including any café au lait spots, midline hairy patches, sinuses, or clefts. These may be indicative of other underlying disorders, including neurofibromatosis or spinal dysraphism. Although there is no single ideal screening test, the Adam’s forwardbend test is considered to be the most accurate and reliable. In this test, the patient bends forward at the hip, with the knees parallel and straight, both arms hanging toward the floor, and palms together.The back, side, and front of the THE CLINICAL ADVISOR • FEBRUARY 2006 2 SCOLIOSIS TABLE 1. Risser staging system Monitoring ossification of the iliac apophysis on x-ray can assess skeletal maturity. Normal ossification begins laterally and progresses medially as a child matures. By dividing the crest into quadrants, five stages of maturation can be assigned. Complete ossification requires approximately one year. Grade Criterion 0 No visible apophysis 1 Ossification of the lateral one fourth 2 Ossification of the lateral one-half 3 Ossification of the lateral three-fourths 4 Complete ossification without fusion 5 Complete fusion 3 4 5 2 1 horizontal plane of the spine is examined for any asymmetry in the contour of the back. An inclinometer (scoliometer) may be used in conjunction with the forward-bend test. Both the scoliometer and bend test measure truncal rotation, not scoliosis. During the bend test, an inclinometer is placed along the spine, and any deviation >5-7 degrees in a growing child should be referred to a pediatric orthopedic surgeon for further evaluation and radiographs. The side should also be examined during a forward-bend test to determine sagittal spinal balance.Any increase in normal thoracic kyphosis or lumbar lordosis should be noted. If a deformity appears structural rather than postural,the patient should be referred for further evaluation. A patient with possible scoliosis should also receive a thorough neuromuscular examination. Gait should be assessed as the patient walks into the exam room, while motor strength in the lower extremities can be evaluated by having the patient stand on the heels and toes.Complete motor and sensory examinations should include both the upper and lower extremities. Deep tendon reflexes are elicited at the biceps, triceps, brachioradialis, patella, and Achilles tendon. Any increase (hyperreflexia), asymmetry, or absence of reflexes that may indicate a neurologic cause for the scoliosis should be noted. Babinski’s reflex and superficial abdominal reflexes should also be elicited. The superficial abdominal reflex is elicited by lightly stroking the skin on each side of the umbilicus with the index finger or back of a reflex hammer.An asymmetric or a unilaterally absent reflex suggests an upper motor neuron abnormality, such as a syrinx, intraspinal tumor,or diastematomyelia. Hamstring flexibility should be assessed with a straight-leg raise or forward bending.Tight hamstrings may be associated with Scheuermann's kyphosis, spondylolysis, or spondylolisthesis,as well as musculoskeletal low back pain.3 Prognosis FIGURE 5. To determine the angle of curvature using the Cobb method, angles are drawn from the vertebral bodies above and below the apex of the curve with the greatest tilt. 3 THE CLINICAL ADVISOR • FEBRUARY 2006 The three main determinants of scoliosis curve progression are gender (progression is more common in females), future growth potential (patients who are skeletally immature experience greater progression), and curve magnitude at time of diagnosis (larger curves more likely to progress).Most cases of AIS occur in females, and curve progression often coincides with the growth spurt of puberty. Assessing the amount of growth remaining is a key predictor in determining the likelihood of curve progression.Traditionally, growth potential is determined by chronological age (growth is generally completed in girls at age 14 and boys at age 16), age at onset of menstruation (growth typically is complete two years after THE CLINICAL ADVISOR • FEBRUARY 2006 3 SCOLIOSIS onset of menarche), and Tanner staging (Tanner 2-3 usually occurs following onset of pubertal growth spurt). Skeletal maturity is also assessed with Risser staging on x-ray. The Risser system estimates remaining skeletal growth by assigning a grade of 0-5 to the progress of bone fusion over the iliac apophysis (Table 1).4 The iliac apophysis ossifies in a predictable fashion from anterolateral to posteromedial along the iliac crest. Progression takes about one year,and fusion an additional two years.The lower the Risser grade at curve detection,the greater the risk of progression.1 The magnitude or size of the curve also has a direct impact on progression.Scoliosis <30 degrees is unlikely to progress once the patient is skeletally mature; curves 30-50 degrees will usually progress 10-15 degrees over a lifetime; and curves >50 degrees will usually progress 1-2 degrees every year.5 FIGURE 6. A nighttime Providence brace is worn only when sleeping. Radiographic assessment Although spinal deformity can be strongly suspected on physical examination, a definitive diagnosis requires a standing posteroanterior x-ray of the entire spine. X-rays are necessary when the inclinometer determination is ≥7 degrees.6 The Cobb method can be used to quantify the amount of scoliosis, kyphosis, or lordosis.To obtain the angle, intersecting lines are drawn on the x-ray from the vertebral bodies above and below the apex of the curve with the greatest tilt (Figure 5). Cobb angles >10 degrees are considered scoliosis. Smaller angles are classified as spinal asymmetry.The clinician should note whether the curve or asymmetry is in the cervical, thoracic, or lumbar spine, and whether the apex of the curve is to the left or right.A thoracic curve will often cause rotation of the ribs and will therefore be more obvious on physical examination than a lumbar curve.More than 90% of the adolescent idiopathic curves in the thoracic region have curve apices that are to the right.7 Left thoracic curves are considered atypical and feature a 20% incidence of neurologic or spinal-cord abnormalities, such as syrinx, hydromelia, tethered cord,or tumor.Most specialists will obtain a screening spinal MRI in patients with left thoracic scoliosis curves. Additional indications for MRI screening include neurologic deficits, unusually rapid progression of curve, and complaints of severe back pain.8 Treatment algorithm There are only three options for patients with AIS: observation, bracing, and surgical correction. Physical therapy, chiropractic adjustment, biofeedback, and electrical stimulation of muscle have not been shown to alter the natural history of 4 THE CLINICAL ADVISOR • FEBRUARY 2006 FIGURE 7. An allograft helps stablize the spine. scoliosis. Because most cases are detected when the curvature is mild or moderate,they can be treated successfully with nonoperative management.8 When the curve measures between 10 and 25 degrees, most pediatric orthopedic surgeons will recommend observation with scheduled follow-up/radiographs every four to six months. Bracing is indicated when the curve progresses to 25-40 degrees in a growing child (Risser 0-3).The goal of this therapy THE CLINICAL ADVISOR • FEBRUARY 2006 4 SCOLIOSIS Surgical intervention, such as a bone graft, is generally needed when the curve progresses to 40-45 degrees in a skeletally immature patient. is to prevent disease progression, and it is currently the only accepted nonsurgical treatment modality. It is important for patients and families to understand that bracing will not make a curve disappear; it is prescribed to prevent the curve from getting worse.The most widely used brace is the Boston lowprofile thoracolumbar-sacral orthosis. Brace fit and curve measurements are re-evaluated every six months in growing patients, and the brace is used until skeletal growth is completed. Compliance is an important factor in preventing curve progression,as research has shown that braces should be worn for 18-23 hours a day for effectiveness.Although difficult to assess, bracing used for the required length of time has an overall success rate of 70%-75% at stopping curve progression.9 Brace technology has improved significantly, lessening the psychosocial impact and improveing overall compliance. In certain circumstances (e.g., poor compliance, single curve), nighttime bracing may be an option.The nighttime Providence brace overcorrects a curve and is worn only while sleeping (Figure 6).Although more research needs to be done,early studies of this brace are very promising.10 Surgical intervention is generally needed when the curve progresses 40-45 degrees in a skeletally immature patient. The goal of surgery is to correct spinal deformity and to reduce the risk of progression. Currently, most pediatric orthopedic surgeons use segmental instrumentation for the posterior fusion. A bone graft (autograft or allograft) is placed to create a solid column of bone (Figure 7).Spinal instrumentation is used to stabilize the spine while the fusion consolidates, which usually takes 6-12 months.6 Surgery can be accompanied by spinal-cord monitoring using somatosensory and motor-evoked potentials, decreasing the rate of neurologic injury to one in 7,000 procedures.11 The typical hospital stay following spinal arthrodesis is four to six days. Most patients will not have to wear a postoperative brace,and the majority will return to school within five to six weeks. Conclusion Primary-care clinicians are in a unique position to anticipate, evaluate, and correctly refer patients with suspected scoliosis. All well-child visits should include a careful examination of the spine because early detection is the key to successful management. ■ Ms. Hart is a nurse practitioner in the Department of Pediatric Orthopaedics, Massachusetts General Hospital, in Boston, where Dr. Grottkau is department chief. References 1. Miller NH. Cause and natural history of adolescent idiopathic scoliosis. Orthop Clin North Am. 1999;30:343-352. 2. Renshaw TS. (1988). Screening school children for scoliosis. Clin Orthop Relat Res. 1988:229:26-33. 3. Chin KR, Price JS, Zimbler S.A guide to early detection of scoliosis. Contemp Pediatr. 2001;9:77-85. 4. Reamy BV, Slakey JB.Adolecent idiopathic scoliosis: review and current concepts. Am Fam Physician. 2001;64 :111-116. 5. Staheli LT (2001). Practice of pediatric orthopaedics. Philadelphia: Lippincott Williams and Wilkins. 6. Dennis AL. Scoliosis:A straightforward approach to the curved spine. JAA- AT A GLANCE ● ● ● ● PA. 2003;16:17-24. 7. Rinsky RA, Gamble JG.Adolescent idiopathic scoliosis. West J Med. Scoliosis is the most common spine disease seen in primary care, and adolescent idiopathic scoliosis accounts for 70%85% of all cases. 1988;148:182-191. Approximately 2%-3% of all adolescents will develop a curve >10 degrees on x-ray; that number decreases to 0.3% with curves measuring >30 degrees.. 9. Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in Definitive diagnosis requires x-rays, and the Cobb method will quantify the amount of scoliosis, kyphosis, or lordosis. Am. 1995;77:815-822. Bracing, indicated when the curve progresses to 25-40 degrees in a growing child, is currently the only accepted nonsurgical treatment for scoliosis. Providence brace in adolescent girls with idiopathic scoliosis. Spine. 2001;26: 8. King EC, Sarwark JF (2002).A look at scoliosis. The Child’s Doctor: Journal of Children’s Memorial Hospital of Chicago. girls who have idiopathic scoliosis.A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg 10. D'Amato CR, Griggs S, McCoy B. (2001). Nighttime bracing with the 2006-2012. 11. Roach JW.Adolescent idiopathic scoliosis. Orthop Clin North Am. 1999;30:353-365. 5 THE CLINICAL ADVISOR • FEBRUARY 2006 THE CLINICAL ADVISOR • FEBRUARY 2006 5
© Copyright 2026