Charles T Costello and Arthur H Jeske 1995; 75:554-563. PHYS THER.
Iontophoresis: Applications in Transdermal
Medication Delivery
Charles T Costello and Arthur H Jeske
PHYS THER. 1995; 75:554-563.
The online version of this article, along with updated information and services, can be
found online at: http://ptjournal.apta.org/content/75/6/554
Collections
This article, along with others on similar topics, appears
in the following collection(s):
Electrotherapy
Pharmacology
e-Letters
To submit an e-Letter on this article, click here or click on
"Submit a response" in the right-hand menu under
"Responses" in the online version of this article.
E-mail alerts
Sign up here to receive free e-mail alerts
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
Pharmacology Series
Iontophoresis: Applications in Transdermal
Medication Delivery
This article presents a review of the literature relating to iontophoresis. This
technique has been used in physical therapy to introduce ionic medications
through the skin, primarily for a local effect. Recently, there has been increased
interest in using this technique for the transdermal delivery of medications,
both ionic and nonionic. This article includes an ovenjiew of the histov of
iontophoresis and a discussion of thephysico-chemical and biological factors
affecting iontophoretic drug transferfor both local and systemic effects. Factors
affecting skin injury and techniquesfor optimizing iontophoretic drug delivery
through the use of current modulation, electrode construction, and skin permeation enhancers are also discussed. Clinical applications of iontophoresis in
physical therapy and the pharmacology of selected medications are presented.
Thoughtsfor future potential uses of this technique and needs for further research are also discussed. [Costello CT, Jeske AH. Iontophoresis: applications in
transdermal medication delivery. Phys Ther. 1995; 753554-563.1
Charles T Costello
Arthur H Jeske
Key Words: Contmlled drug delivery, Drug delivery, EElectmosmos& Iontophoresis,
Pharmacology, Transdermal drug delivery.
Iontophoresis is the introduction of
various ions into the skin by means of
e1ectricity.l This definition, however,
should be expanded because many
nonionic materials such as polypeptides can be delivered into the body
by iontophoresis. Physical therapists
use iontophoresis with the objective of
delivering a locally higher, therapeutic
concentration of an ion or other medication, while minimizing the systemic
concentration caused by circulatory
removal of the material from the area.
The use of iontophoresis has fluctuated over the years, partly due to
concerns about chemical burns of the
skin that can accompany iontophore-
sis treatment and the lack of research
demonstrating the efficacy of the technique. Recently, there has been a
resurgence in the use of iontophoresis,
particularly for the delivery of antiinflammatory medications. Interest has
also grown in the use of iontophoresis
for the percutaneous delivery into the
body of systemically active drugs and
maintenance of therapeutic levels. This
approach has been termed "controlled
release."
According to Chien et a1,2there are
several advantages of an effective,
controlled percutaneous drug delivery
system such as iontophoresis. These
CT Costello, PhD, PT, CHT, is Assistant Professor, Deparrment of Physical Therapy, The University
of Texas Medical Branch, Galveston, TX 77555-1028 (USA). Address all correspondence to Dr
Costello.
AH Jeske, PhD, DMD, is Professor, Deparrment of Basic Sciences/Pharmacology, Dental Branch,
The University of Texas, Houston-Health Science Center, Houston, TX 77225.
104 / 554
advantages are listed in the Table. Use
of iontophoresis easily overcomes
some of the major impediments to
other passive transdermal drug delivery mechanisms, including requirements such as low molecular weight,
low dose, and balanced oil-water
partition coefficient (implying that the
material is equally soluble in both
water and organic solvents).3
The interests of the pharmaceutical
and physical therapy professions in
iontophoresis are often dlferent. Many
medical practitioners are interested
primarily in the delivery of medication
to achieve a systemic concentration
sufficient for a desired effect (although
medication uptake may occur preferentially in a specific target organ),
whereas physical therapists are interested in directing larger quantities of a
medication into a localized treatment
region (under the electrode) and mini-
Physical Therapy / Volume 75, Number 6 /June 1995
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
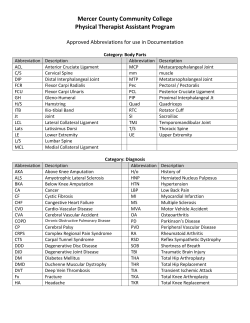
Table. Advantages of a n Effective, Controlled Percutaneous Drug Delivery System, Such as ~ontophoresi?
1. Avoids the risks and inconveniences of parenteral (injection/intravenous)therapy
2. Prevents the variation in the absorption and metabolism seen with oral administration
3,Increases therapeutic efficacy by bypassing hepatic "first-pass"elimination-the reduction in the amount of the drug entering the systemic circulation,
due to metabolism by the liver as the drug passes through the hepatic circulation after absorption from the gastrointestinal tract
4. Reduces the chance of overdosing or underdosing by providing continuous delivery of the drug, programmed at the required therapeutic rate
5. Permits the use of a drug with a short biological half-lifebecause (1) the drug is delivered directly to the target organ without the need to circulate and
recirculate in the blood or (2) the drug is delivered directly into the bloodstream without delays due to absorption through the gastrointestinaltract
6. Provides a simplified therapeutic regimen, leading to better patient compliance
7. Permits a rapid termination of administration of the medication, if needed, by simply turning off the iontophoretic delivery system
mizing systemic levels of the
medication.
The purposes of this article are to
present what is known about the
mechanisms of iontophoresis and to
review the past and present clinical
applications of this technique.
disciplines, most notably dermatology,
otorhinolaryngology,ophthalmology,
and dentistry.5 Iontophoresis is also
used in some research methods, particularly in neuroscience either to
administer small quantities of neuroactive substances or to create small lesions within the central nervous
sy~tem.~
History of lontophoresis
A comprehensive historical review of
electrotherapy until 1965, including
iontophoresis, is provided by Licht4; a
more recent overview has been published by Chien and Banga.3 According to Chien and Banga,3 claims of
medication transfer by electricity have
been made as early as 1745. Not until
1879, however, did Munck truly demonstrate the ability to deliver ions, by
delivering strychnine into a rabbit with
an electric current.*A few years later,
in 1898, hlorton published a book in
which he described an experiment in
which he drove finely powdered
graphite into his slun.3
The first scientific experiments relating
to the mechanism of iontophoresis
were performed by LeDuc in 1908.3
Using two rabbits placed in series, he
introduced strychnine into one and
cyanide into the other, each depending on the polarity. He was able to
determine which ions were introduced
by observing the signs preceding
death.
Experimental and clinical trials have
continued to establish a role for iontophoresis in clinical practice, in physical therapy and other health-related
Factors Influencing
lontophoresis
Ionization and Electm&sis
The primary factors in iontophoresis
relate to the movement of ions. In
aqueous solution, an inorganic compound dissociates into positively
charged cations and negatively
charged anions. When a direct electric
current is passed through this solution,
the cations move toward the negative
electrode (the cathode) and the anions
move toward the positive anode
where the ion either picks up or releases electrons. When a direct current
is passed through the body, electrolysis of sodium chloride takes place.
This electrolysis results in the formation of sodium hydroxide and a rise in
the pH at the cathode and in the formation of hydrochloric acid and a
lowering of the pH at the anode.6
When the electrodes contain solutions
of ions, negatively charged anions are
repelled from the cathode into the
body. Positively charged cations are
repelled into the body from the anode. This effect is specific for ions of
the same polarity as the electrode.
Ions of the opposite polarity are not
transferred into the body.' If ionto-
Physical Therapy / Volume 75, Number 6 /June 1995
phoretic medication delivery were
dependent solely on this mechanism,
nonionized drugs, including most
organic compounds, would not be
appropriate for delivery with this
technique.
Electmosmosis
Another primary means by which ions
and other substances traverse the skin
during iontophoresis is via the passage
of a solvent, carrying with it other
dissolved substances, through the skin
under the Influence of direct current.
This process been termed iontohydmkinesis.8 This effect and its dependence on the pH were first demonstrated by Rein.9 The relevance of this
effect to medical iontophoresis was
later discussed by HarpuderloJ and
was more recently studied by
Praissman et all2 and Gangarosa et al.8
The skin is isoelectric (cames no
charge) at a pH of between 3 and
4.13914 At a physiologic pH (around 7),
the slun cames a negative charge,
which enhances the migration of cations at the an0de.~,9,'~
This greater
migration seems to drag the solvent
through the skin, carrying with it any
dissolved s u b s t a n c e ~ . ~If ~the
9 ~pH
~ ~is
lowered below 3, this effect can happen at the cathode.12
Effect of pH
The pH is a critical variable in iontophoresis because, as was noted, it
affects skin charge and electroosmotic
f l o ~ . ~During
J~1~
iontophoresis,
~
as a
result of ionic exchange between the
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
electrode and the body fluids, oxidation and reduction reactions take place
at the anode and cathode, respectively. These reactions produce a lowering of the pH at the anode and an
increase of the pH at the cathode.15In
his dissertation, Mandleco reported
that at the cathode, following direct
current flow of 2 or 4 rnA for up to 30
minutes, the pH changed from 7 to
10.1.~
Changes in the pH are also
considered responsible for the discomfort and skin irritation sometimes associated with iontophoresis.l'j Histamine
release probably mediates the redness
of the skin that usually occurs after
treatment.I6
These pH changes at the electrodes
can alter the transfer of medications
due to changes in the electroosmotic
effect. The pH also alters the degree of
ionization of organic compounds,
which usually exist in a solution in a
pH-dependent equilibrium between
their ionized and nonionized
states.lS15An optimal iontophoretic
effect occurs when a material is maximally ionized.17J8 Other conditions
may also be pH dependent. For example, Chien et a12 showed that iontophoretic transfer of insulin is greatest
at a pH of 3.7, because at hlgher values, the molecules aggregate.
Because of these effects of the pH,
there has been interest in developing
electrode systems that will provide a
stable pH.15J6 This research on electrode design will be discussed in later
sections.
Pore Transport
Another interesting observation from
these s t ~ d i e s l 7 -is~that
~ the material
delivered by iontophoresis stays in the
skin for several days following treatment. There also appears to be some
physical narrowing or plugging of
these skin pores, which begins to
resolve after about 5 days.25
The ability of the skin, when iontophoresis is applied, to allow the passage of some ions and to restrict that
of others reflects the "permselective"
properties of the skin. Studies7-9-26327
have shown that transport across the
skin is dependent on the valence of
the ion, its polarity, and its transport
number (related to its size). Small,
monovalent cations pass through the
skin most readily. Larger ions and
anions pass through the skin less
readily. Bivalent ions (both anions and
cations) appear to bind to receptors
on the walls of the pores and thus do
not traverse the skin.
Concentration and Mixture
of Sdutes
If the concentration of ions in a solution is too great, it causes a bottleneck
effect as the ions attempt to pass
through the available pores.26~28If
several ions or other substances are
mixed in the solution, the ions compete, and those that are best capable
of carrying the charge will be transported preferentially across the
skin.24.26,29
Penetration and Distribution
of Ions
The stratum comeum of human skin is
normally quite impervious. This part
of the epidermis, however, is punctured by pores, particularly those of
the sweat glands, as well as those of
the hair follicles and sebaceous glands.
Electric current-mediated ion transfer
occurs primarily through these pores.
This ion transfer was first demonstrated by Morton in 1898.l9 More
recent studies20-24 have venfied that
electric current traverses the skin by
passing primarily through sweat
glands and, to a lesser extent, through
hair follicles and sebaceous glands.
The physical therapy use of iontophoresis is largely based on the penetration and distribution of ions. Some
researchers3O-32 have proposed that all
the material delivered through the skin
with iontophoresis is removed by the
subcutaneous circulation and distributed around the body (ie, there is no
local concentration). Other researchers3535 have shown with animal studies and direct measurement that ions
and other substances do penetrate and
concentrate in the deeper tissues under the medication electrode. In addi-
tion, several studies2"36-38 have indicated sufficient penetration of ions to
produce deep cutaneous anesthesia.
Other studies on h~rnans39-~2
have
indicated that ions penetrate and have
therapeutic effects on deeply situated
structures.
Costello recently reported, in his dissertation, on his in vivo studies of
lidocaine iontophoresis with an animal
(rabbit) model.35 He reported penetration of lidocaine to at least 1 cm into
the gluteal muscles. He found that the
ideal variables for depth of ionic penetration were a current of 4 rnA, applied for 10 minutes, with a 4% lidocaine solution.35
Skin Injury
The pH changes that occur with direct
currents have long been considered
the cause of the skin injuries associated with treatments using such currents.5 Bums under the cathode generally are more serious, being deeper
and slower to heal than burns under
the anode.s2Molitor and Femandez43
found that burns occurred in areas of
high current density, even though the
electrode solution was continuously
replaced (so that the pH did not
change). Lewis and Zottermanbl and
Leerning et a145reported that gas bubbles disrupt the stratum comeum,
causing areas of higher current density
where the pH changes occur to the
greatest degree. Because twice as
much hydrogen is produced at the
cathode, compared with oxygen at the
anode, the disruption is greater
there." Gas bubbles seem to occur
mostly at the periphery of electrodes,
because pressure under the center of
the electrodes appears to trap the gas
and impedes the current flow there,
reducing the electrolytic effe~t.~5
The likelihood of skin injury with
direct current can be decreased by
thoroughly cleansing the s h prior to
treatment, using only well-saturated
absorbent pads (or other material) for
electrodes, ensuring that there is no
contact between the metal or carbonrubber components and the skin,
ensuring even skin contact with no
skin blemishes (any small skin lesions
Physical The1-apy/ Volume 75, Number 6 /June 1995
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
should be protected with petroleum
jelly), and keeping the current density
at the cathode at 1es.sthan 1 mA/in2.6
Instrumentation
Currents Used in lontophoresis
Constant direct curr~mthas been used
in iontophoresis applications, but we
contend that a constant-current generator should be used to provide consistent current flow while the skin resistance is changing. Eiecause of concerns about skin chiarge accumulation
and skin irritation and bums due to
pH changes, however, modulated
currents have been used with success
in in vitro and in vivo studies on laboratory animals for the transdermal
delivery of drugs for a systemic effect.'.G-j2 Pulsed currents have proved
to be as effective or more effective in
the delivery of small, yet systemically
effective, quantities of drugs, including
insulin.2-45-5O Okabe et a146 reported
drug transfer with pulse durations as
short as 4 microsecc>nds.In all of
these studies, very low amplitude
currents, as low as :25 pA,50were
used. We believe the amplitude of the
currents used in these studies is too
small to meet the needs of physical
therapists to cause primarily a local
effect. The results of these studies,
however, indicate the need for physical therapists to consider the use of
currents other than the traditional
continuous monophasic current for
iontophoresis.
Su et al,52 for example, reported recently on a study involving in vivo
iontophoresis of tetraethylammonium
(TEA). By placing tlne TEA in both
electrodes and reversing the 100-pA
current every 6 hours over a 24-hour
period, the pH change was only 0.2 at
both electrodes, compared with
changes of 0.55 at the anode and 1.3
at the cathode without current
reversal .j2
Electrodes
There have been few published studies concerning the construction of
electrodes for iontophoresis. Until
manufacturers started marketing spe-
cific iontophoretic drug delivery systems, therapists and others made their
own electrodes from lint cloth, orthopedic felt, paper towels, or gauze.
These electrodes were then connected
by a soft metal or alloy electrode to
the direct-current generator. In an
attempt to maintain a stable pH,
Phipps et allj used a buffer solution
separated from the medication solution by an anion-permeable membrane in their electrode. Sanderson et
all6 used a silver anode, which reacted
with chloride ions from the body to
form insoluble silver chloride. Both
these studies demonstrated a stable
pH and an increased rate of drug
transfer. The buffer ions must be restrained, because if they were mixed
in solution with the medication, the
buffer ions would compete with the
medication ions for transport across
the skin.
Su et alj2 reported enhanced drug
delivery with use of a skin permeation
enhancer. The plasma levels of the
drug more closely followed the theoretical prediction and the plasma levels with tape-stripped skin (with the
stratum corneum removed). The authors also reported that the drug was
delivered with less voltage needed to
generate the current.
Applications in Physical
Therapy
Corticostemids
(Glucocorticostemids)
Pharmacology. Corticosteroids are
the primary drugs used with iontophoresis in physical therapy. Corticosteroids are widely used because they
possess a profound anti-inflammatory
effect and are available in relatively
inexpensive forms designed both for
oral and topical administration. Several
corticosteroids are available as watersoluble salts, rendering the corticosteroid molecule negatively charged and
therefore available to move under the
Influence of a negative current field.
Another type of electrode available
today is the gel electrode. Although it
appears that this type of electrode may
provide a more even distribution of
current,53the hydrophilic nature of the
gel of these electrodes binds the solvent, thus inhibiting the electroosmotic
effect and reducing the total amount of
Two water-soluble steroids have
drug transferred at the anode, comgained widespread popularity in physpared with other electrode de~igns.~~,i4ical therapy: dexamethasone sodium
phosphate (Decadron and various
Pore Dilation
generic forms) and methylprednisolone sodium succinate (SoluBecause of the relatively impervious
Medrol and various generic forms).
nature of the stratum corneum, and
Methylprednisolone must be reconstibecause drug transport through the
tuted immediately before use. Dexamethasone is available in a somewhat
skin occurs primarily via pores, it
appears logical that the use of a pore
more stable, dissolved form. In either
case, corticosteroid solutions should
dilator may enhance iontophoretic
transport across the slun. However,
be kept at room temperature to ensure
stability. Methylprednisolone must be
little has been published about the use
used within 48 hours of mixing, acof pore dilation in combination with
iontophoresis. In his dissertation,35
cording to the manufacturer's instrucCostello reported that with lidocaine
tions, because the solution loses stabiliontophoresis, using menthol as a pore
ity after that time.
dilator, there was no enhancement of
the amount of drug transferred or
Dissolution of the sodium phosphate
depth of penetration into the tissues.
salt results in formation of positively
There was a reduced tendency for the
charged sodium ions and negatively
lidocaine to pool in the skin, probably
charged dexamethasone molecules.
secondary to the enhanced blood flow
Decadron injectable solutions contain
due to the vasoactive effects of the
both bisulfite and paraben preservamenthol.
tives and should not be administered
to patients with sensitivity to either
substance (bisulfite sensitivity is occa-
Physical Therapy / Volume 75, Number
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
sionally seen in steroid-dependent
persons with asthma). Solu-hledrol, in
its powder form, contains no preservatives and can be used with patients
who are allergic to preservatives. The
solvent provided with some forms of
powdered methyl prednisolone, however, should be substituted by distilled
water when used with iontophoresis,
because this solvent may contain other
competing ions.
Corticosteroids inhibit the inflarnmatory process, in part by reducing the
migration of neutrophils and monocytes into the inflamed area and reducing the activity of these white
blood cells.56 Corticosteroids have
recently been shown to reduce
"sprouting"that occurs in sensory
nerves in association with tissue injury.57 This "sprouting" may be one
factor increasing the sensitivity of
Inflamed tissues to painful stimuli.
However, corticosteroids should not
be applied to infected areas or to
open wounds, because steroids tend
to Inhibit the immunologic defense
process.
Clinical applications. In selecting
patients for treatment with steroids,
the therapist must determine that the
patient has a condition that is amenable to relief by application of a corticosteroid and that the patient is not
allergic to the medications or their
preservatives. In the case of joint pain,
one additional factor should be considered: steroid resistance. This condition is seen in a small number of patients with rheumatoid arthritis and
other conditions treated by long-term
steroid u ~ e . In
5 ~cases in which patients are being treated with systemic
corticosteroids, the patients' physician
should be consulted prior to the administration of any additional form of
steroid to minimize any further adrenocortical suppression.
Dexamethasone is often administered
by iontophoresis, in combination with
lidocaine, in the treatment of musculoskeletal disorders. This corticosteroid
has frequently been administered from
the positive electrode (it presumably is
camed through the skin by the electroosmotic effect, because it is a nega-
tively charged ion). DeLacerda40used
dexamethasone (1 mL of 0.4% dexamethasone mixed with 2 mL of 4%
lidocaine in aqueous solution administered from the anode at a dosage of 5
mA for 10 minutes) to treat patients
with myofascial shoulder girdle syndrome and found that iontophoresis
produced the most rapid improvement
in range of motion, compared with
treatment with ultrasound or muscle
relaxants. He used a current of 5 mA
for 15 minutes, applied over trigger
points.
Bertolucci41reported reduction of pain
and increased range of motion in a
group of patients with shoulder tendinitis treated with the same mixture of
dexamethasone and lidocaine iontophoresis, applied for 10 minutes at 2
mA, for 5 minutes at 3 mA, and for 5
minutes at 4 mA, compared with a
control group. He reported that the
results were similar to those seen with
steroid injections. He used a current of
2 to 4 mA, progressed over a 20minute treatment period. Similarly,
Hasson and colleagues have reported
a delay in the onset of postacute exercise muscle soreness with the use of
dexamethasone iontophoresis,59and
an improvement in knee joint range of
motion and a reduction in knee circumference following dexamethasone
iontophoresis, applied using the same
protocol as Berto1ucci.m
Other glucocorticoids administered by
iontophoresis have been used in the
treatment of patients with temporomandibular trismus and paresthesiab'
and for Peyronie's disease.62
drug administered in this manner are
rather small, the systemic effects of
lidocaine are not seen. In certain conditions (eg, facial pain syndrome with
trigger points), the application of local
anesthesia prior to administration of
the corticosteroid appears to be beneficial. Because lidocaine and other
local anesthetics dilate blood vessels,
however, they enhance their own
clearance from the tissues being
treated, requiring the addition of a
drug to constrict blood vessels and
localize subsequent drugs to the
treated area. G a n g a r ~ s areported
~~
increased depth of penetration and
longer duration of anesthesia when
epinephrine (epinephrine:total solution dilution of 1:50,000)was coadministered with 2% lidocaine in iontophoresis. Recently, Silcox et a163
confirmed that cutaneous vasoconstriction with iontophoresis enhanced the
accumulation of topically applied,
radiolabeled compounds.
Clinical applications. Russo et aF4
reported that lidocaine applied by
iontophoresis was more effective for
producing skin anesthesia than when
it is applied by swabbing. Iontophoresis, however, was not as effective as
injection.@Although these investigators examined skin anesthesia for
injection or minor surgical procedures,
they demonstrated that lidocaine had a
deeper, longer-lasting effect when
applied by iontophoresis than when it
was swabbed on. The method of
application could be a consideration
when cutaneous anesthesia is used in
physical therapy to modulate kinesthesia from skin or superficial joint
receptors.
Lidocaine
Epinephrine
Pharmacology. Lidocaine is an injectable, arnide-type local anesthetic that
is widely used in medicine and dentistry. In its injectable form, it is a
hydrochloride salt that dissociates into
a positively charged molecule. Therefore, lidocaine is applied iontophoretically under the anode. When applied
in this manner, lidocaine produces
dilation of blood vessels and a rather
profound topical anesthesia of the
skin, to depths of several millimeter~.~~,%
Because
- % the amounts of
Epinephrine is the vasoconstrictor
most widely used in conjunction with
lidocaine. In dentistry, where the local
anesthetic is injected, relatively small
amounts of the vasoconstrictor are
used (eg, epinephrine:total solution
dilutions of 1:50,000-1:200,000, or
0.02-0.005 mg/mL). In iontophoresis,
higher concentrations are required to
produce sufficient vasoconstriction and
to counteract the rapid deterioration of
epinephrine after it is mixed and ex-
Physical Therapy / Volume 75, Number 6 /June 1995
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
posed to oxygen, light, and body
temperatures. Epinephnne acts on
alpha- and beta-adrenergic receptors
throughout the body, producing a
number of syrnpathmnimetic effects
when administered ~ystemically.~5
These effects are well known and
include cardiovascular stimulation,
elevations in blood glucose, and dilation of bronchioles. In some patients,
even small amounts of epinephrine
may produce uncomfortable and potentially harmful side effects, such as
cardiovas~ularstimulation and palpitations, and this drug should not be
used in such patients. Epinephnne is
only available in a water-soluble, injectable form and must be diluted
prior to use. Because epinephrine is
also positively charged in this form, it
can be administered along with lidocaine under the positive iontophoretic
electrode.
Historical Uses iin Physical
Therapy
Although use of lidocaine and dexamethasone represents the majority of
clinical applications of iontophoresis
currently used in physical therapy,
there are reports on the use of other
materials, particularly inorganic anions
and cations. Much of the historical
applications of these are well surnrnarized by Harris.'3 Other published
reports are discusse:d in the following
sections. Readers must realize, however, that most of these reports are
poorly substantiated or are reports of
clinical trials that lacked controls. The
reported results of these studies, therefore, should be vie-wed with caution.
Hyalumnidase
Hyaluronic acid, a gelatinous substance that exists in, many body tissues, is a major constituent of the
"ground substance" of connective
tissue. It restricts dihsion of certain
substances through the tissues. Hyaluronidase is an enzyme that hydrolyses
hyaluronic acid, reducing its viscosity.66 Hyaluronidast?carries a positive
charge and migrates most rapidly at a
pH of 5.4. For these reasons, it is
applied in 0.1-mol/L solution with an
acetate buffer by iontophoresis to an
edematous limb.&-GB
Hyaluronidase has been shown to be
effective in reducing acute66 and
chroni@@ edema. It has also been
used to reduce joint swelling due to
hemarthro~is.@.~9
Additionally, PopkinG7 reported on two patients with
scleroderma to whom he applied
hyaluronidase iontophoresis. These
patients improved by having increased
slun softness and flexibility and reduced cold sensitivity.
In spite of the apparent clinical effectiveness of hyaluronidase, we encourage caution in its use because it is
indiscriminate in breaking down the
intercellular ground substance matrix.
In so doing, it may open a path for
mfection or other toxins, and may
damage articular cartilage. Until further
studies support its safe use, we contend that hyaluronidase should not be
used routinely as a component of
iontophoretic therapy. This caution,
however, does not rule out the careful
use of hyaluronidase in selected cases.
Two potent vasodilators, histamine
and mecholyl (acetyl-beta-methylcholine chloride), have been adrninistered by iontophoresis for a variety of
~iisorders.~0-73
Kling and Sashin70 compared the eficacy of these two vasodilators and determined that mecholyl
produced less vasodilation. They also
used histamine iontophoresis for patients with a number of conditions,
particularly arthritis. The authors reported reduced pain and increased
range of motion. Because there was
no change in joint swelling, it is possible that the improvements noted were
largely due to pain modulation. Kling
and Sashin also reported improvement
in patients with conditions associated
with vasospasm, such as Raynaud's
disease.
K o ~ a c susing
, ~ ~ mecholyl, and later
Abrarnson et
using histamine,
reported enhanced healing of longstanding, trophic ulcers. More recently,
DeHaan and Stark73 experimented
with using histamine iontophoresis to
improve the viability of large, composite skin grafts. Histamine enhanced
venous flow, but apparently did not
improve overall blood flow or the
establishment of new circulation that
would allow the grafts to "take"
sooner.
Inorganic Cations
Inorganic cations carry a positive
charge and are delivered from the
anode. Zinc has been used in the
treatment of patients with ischemic
ulcers, applied from a 0.1-moVL solution of zinc
In this case presentation, zinc appeared to promote
healing and prevent infection.
Silver ions were used in the treatment
of a series of patients with osteomyelitk75 The ions were from a silver wire
electrode, connected to the wound
through saline-soaked gauze. Because
this was a case report, however, there
were no controls to determine
whether the beneficial effects were
due to the use of silver ions or merely
the passage of a low-intensity direct
current. Silver iontophoresis has also
been used with some success in the
treatment of patients with rheumatoid
arthritis.' 3
Copper iontophoresis has been used
to treat chronic fungal mfections of the
feet.76A 0.2% solution of copper sulphate was used. Most patients were
cured, without recurrence of the infection, following an average of six to
seven treatments.
Weinstein and Gordon77reported on
the use of magnesium iontophoresis
from a solution of 2% magnesium
sulphate in the treatment of a series of
50 patients with subdeltoid bursitis.
Thirty-four of the patients showed
good results (resolution of all clinical
signs and symptoms and restoration of
full active range of motion), and another 14 patients were improved. The
authors felt that these results were
satisfactory, better than could be
achieved by other methods available.
Kahn78reported a case study that
showed improvement in a patient with
gout following treatment with lithium
Physical Therapy / Volume 75, Number
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
iontophoresis. The rationale was that
the lithium would replace the insoluble sodium urate in the joint with
soluble lithium urate. The patient
reported hours of relief after the first
treatment and complete relief after
four weekly treatments. There was no
change in radiologic signs, although
no gouty tophi developed and swelling was reported to decrease. The
author reported that previous, similarly
treated patients did demonstrate reduction of tophi. Given the time period of the study, during which remission is likely to occur, and that other
pain-reducing treatments were administered, however, the conclusions can
be questioned.
Inorganic Anions
Inorganic anions are administered
under the cathode. Acetic acid iontophoresis has been described in case
reports for the treatment of patients
with calcium deposits around the
shoulder79 and for myositis ossdicans
affecting the quadriceps femoris muscle.80 In both case reports, the authors
reported resolution of the calcium
deposition, with reduction in symptoms and improved function.
Clinical Applications in Other
Disciplines
been used for the treatment of patients
with allergic rhiniti~.l3!9~
Dentistry
Ophthalmology
Dentistry, probably to an even greater
extent than physical therapy, has used
iontophoresis. Beginning in the late
19th century, dentists applied local
anesthetics to their patients prior to
oral surgical procedures. Gangarosa85
described the use of iontophoresis for
three basic applications in dentistry:
(1) treatment of hypersensitive dentin
(eg, in teeth sensitive to air and cold
liquids) using negatively charged fluoride ions; (2) treatment of oral ulcers
("canker sores") and herpes orolabialis
lesions ("fever blisters") using negatively charged corticosteroids and
antiviral drugs, respectively; and (3)
the application of local anesthetics to
produce profound topical anesthesia,
as is done in some physical therapy
appli~ations.~,~~
Iontophoresis has been used experimentally to deliver antibiotics into the
eye." The principal disadvantage of
this technique is the time required for
direct contact of the electrode with the
eye.
CoyeP1 reported on the use of citrate
iontophoresis for patients with an
exacerbation of rheumatoid arthritis
affecting the hands. He used a 2%
solution of sodium citrate and reported increased grip strength in these
patients, compared with similar control groups treated with anodal or
cathodal galvanism, with tap water
electrodes.
A review of iontophoresis in dermatology was provided by Sloan and
S ~ l t a n iMany
. ~ ~ of the uses of iontophoresis discussed in this article are
also used in physical therapy and
dentistry. Except for the use of lidocaine for anesthesia and the treatment
of patients with hyperhidrosis, however, most uses of iontophoresis in
dermatology have largely been abandoned. Iontophoresis with tap water
or anticholinergic compounds has
been used for the treatment of patients
with hyperhidrosis of the palms, feet,
and a~illae.~9-9"
Salicylate ions from a 2% solution of
sodium salicylate have been shown to
be effective in treating a series of five
patients with plantar warts.e2The
warts disappeared after two or three
weekly treatments.
In patients with bums, iontophoresis
of antibiotics has been shown to be
more effective for treating superficial
~nfectionsthan systemically administered antibiotics that would not penetrate eschar.95
Iodide iontophoresis, using "Iodex"
ointment, has been reported as useful
in the management of problems related to scar tissue, such as Dupuytren's contracture,B3 and release of
scar adhesion of tendon to bone.*
Iontophoresis is a preferred method
for obtaining anesthesia of the tympanic membrane prior to simple surgical procedures involving that structure.Ns97 Iontophoresis of zinc has also
Diagnostic Applications
Iontophoretic application of the drug
pilocarpine produces intense sweating,
allowing sufficient amounts of sweat
to be collected and analyzed. This is
now accepted as the primary test in
the diagnosis of cystic f i b r o s i ~ . ~ ~ ~ - ~ ~ ~
Conclusions and Future
Applications
For the reasons outlined by Chien et
a1,2the use of iontophoresis in medicine is likely to increase, because it
offers a convenient, safe, noninvasive
route for the administration of many
compounds that are capable of penetrating the skin, but are difficult to
administer in other ways. This applies
particularly to the administration of
hormones and other polypeptide
medications.47.48 Other recent applications are for the systemic management
of pain. Thysman and Preat,1°3 for
example, reported on the iontophoretic administration of fentanyl and
sufentanil (opiate analgesics) in rats,
with the production of analgesia for
up to 4 hours. It is questionable to
what extent physical therapists will be
involved in this expanded use of iontophoresis for the delivery of systemically active drugs.
Miniaturized, unit-dose iontophoretic
systems may become available for the
long-term administration of medically
useful drugs that are effective at low
plasma concentrations and that would
otherwise be ineffective or produce
serious side effects if given orally or by
injection. The "minisets" would likely
be self-contained, with a built-in battery. They would provide low current
levels for sustained administration. The
currents may be pulsed to reduce skin
Physical Therapy / Volume 75, Number 6 /June 1995
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
irritation and charge accumulati0n,~,&-50
or the current may be reversed intermittently, with the medication in both electrodes, to provide
continuous administration while lessening the pH changes associated with
unidirectional fl0w.5~It may even be
possible for the patient to selectively
apply different drugs from the same
iontophoretic delivery system (''Dial A
Drugn).17-4 permeation enhancer will
most likely be used to reduce skin
resistance and accumulation of the
drug in the skin. Much work, however, still needs to be done to validate
the clinical efficacy of this form of
drug administration.
For most physical therapy applications, we recommend treatment with a
current of 4 rnA for 10 minutes. This
current is needed to penetrate into the
deeper tissues; treatment times greater
than 10 minutes are not likely to
achieve any greater tissue concentration due to circulatory removal of the
medication (possibly unless a vasoconstrictor were used). An electrode
system that uses a silver or silver-silver
chloride electrode would probably be
the most cost effective to minimize pH
changes.16
In spite of the many years that iontophoresis has been used by physical
therapists, very little has been done in
the way of research to demonstrate
the efficacy of this treatment. There
are strong indications that this treatment technique is clinically effective,
but this effectiveness must be proven
by controlled studies, both in the
clinic and the laboratory. These studies should include demonstration
(where possible) of the ability of the
medications to penetrate to the target
tissues in sufficient quantity to produce
a clinical effect, as well as controlled
trials of clinical efficacy. There are
several applications of iontophoresis
that have been used in the past and
that are believed based on clinical
judgment and experience to be effective. It would be worthwhile to subject
these applications to scientific scrutiny
in controlled trials to determine
whether they can meet the criteria of
being more clinically effective and cost
efficient compared with alternative
treatment techniques.
References
1 Thomas CL, ed. Tubers Cyclopedic Medical
Dictionary. 13th ed. Philadelphia, Pa: FA
Davis Co; 19773-47.
2 Chien YW, Siddiqui 0 , Shi W-M, et al. Direct current iontophoretic transdermal delivery
of peptide and protein drugs. J Phann Sci.
1989;78:376-383.
3 Chien YW, Banga AK. lontophoretic (transdermal) delivery of drugs: overview of historical development. J Phann Sci. 1989;78:35>
354.
4 Licht S. History of electrotherapy. In: Licht
S, ed. Therapeutic Electricity and Ultraviolet
Radiation. New Haven, Conn: Elizabeth Licht
Publisher; 1967:l-70.
5 Mandleco CF. Application of Zontophoresis
for Noninvasive Administration of Lidocaine
~ ~ d r o c h l o r i in
d e the Ionized FO&. Salt
Lake City, Utah: University of Utah; 1978.
Dissertation.
6 Shriber WJ. A Manual of Electrotherapy. 4th
ed. Philadelphia, Pa: Lea & Febiger; 1975:
chap 11.
7 O'Malley EP, Oester YT, Warnick EG. Experimental iontophoresis: studies with radioisotopes. Arch Phys Med Rehabil. 1954;35:
500-507.
8 Gangarosa LP,Park N-H, Wiggins CA, Hill
JM. Increased penetration of nonelectrolytes
into mouse skin during iontophoretic water
transport (iontohydrokinesis). J Phannacol
Ther. 1980;212:377-381.
9 Rein H. Experimentalle studien iiber elektroendosmose an iiberiebender menschlicher
haut. Z Biol. 1924;81:124-130.
10 Harpuder K. Electrophoresis in physical
therapy. Arch Phys Ther X-Ray Radium. 1937;
18:221-225.
11 Harpuder K. Electrophoresis in physical
therapy. N m York JMed. 1938;38:176-180.
12 Praissman M, Miller IF, Berkowitz JM. Ionmediated water flow, I: electroosmosis.
JMembr Biol. 1973;11:139-151.
13 Harris R. Iontophoresis. In: Licht S, ed.
7berapeutic Electricity and Ultraviolet Radiation. New Haven, Conn: Elizabeth Licht
Publisher; 1967:156-178.
14 Tyle P. Iontophoretic devices for drug delivery. Phannacol Res. 1986;3:318-326.
15 Phipps JB, Padmanabhan RV, Lanin GA.
Iontophoretic delivery of model inorganic and
drug ions. J Phann Sci. 1989:78:365-369.
16 Sanderson JE, DeRiel S, Dixon R. Iontophoretic delivery of nonpeptide drugs: formulation optimization for maximum skin permeability. J Phann Sci. 1989;78:361-364.
17 Behl C, Kumar S, Malick WA, et al. Iontophoretic drug delivery: effects of physiochemical factors on the skin uptake of nonpeptide
drugs. J Phann Sci. 1989;78:355-360.
18 Siddiqui 0 , Roberts MS, Polack AE. The
effect of iontophoresis and vehicle pH on the
in vitro permeation of lignocaine through human stratum corneum. Phann Phannacol.
1985;37:732-735.
Physical Therapy i Volume 75, Number 6 /June 1995
19 Morton WJ. Cataphoresis or Electrical Medicamental Surgery. New York, NY: American
Technical Book Co; 1898.
20 Abramson HA, Gorin MH. Skin reactions,
MI: relationship of skin permeability to electrophoresis of biologically active materials into
the living human skin. Phys C h a . 1939;43:
335-346.
21 Abramson HA, Gorin MH. Skin reactions,
IX. the electrophoretic demonstration of the
patent pores of the living human skin; its relation to the charge of the skin. Phys Chem.
1940;44:1094-1102.
22 Abramson HA, Engel MG. Skin reactions,
XII: patterns produced in the skin by electrophoresis of dyes. Arch Dennatol Syphilol.
1941;44:190-200.
23 Grimnes S. Pathways of ionic flow through
human skin in vivo. Acta Denn Vmereol
(Stockh). 1984;64:93-98,
24 Burnette RR, Ongpipananakul B. Characterization of pore transport properties of excised human skin during iontophoresis.
J Phann Sci. 1988;77:132-137.
25 Dobson RL, Lobitz WC. Some histochemical observations on the human eccrine sweat
glands. Arch Dennatol Syphilol. 1957;75:653666.
26 O'Malley EP, Oester YP. Influence of some
physical chemical factors on iontophoresis
using radio-isotopes. Arch Phys Med Rehabil.
1955;36:310-315.
27 Burnette RR, Marrero D. Comparison between the iontophoretic and passive transport
of thyrotropin releasing hormone across nude
mouse skin. JPhann Sci. 1986;75:738-745.
28 Gangarosa LP. Defining a practical solution for iontophoretic local anesthesia of the
skin. Methods Find E q Clin Phannacol. 1981;
3:83-94.
29 Abramson HA. Alley A. Mechanisms of
histamine iontophoresis from aqueous media.
Arch Phys Ther X-Ray Radium. 1937;18:327333.
30 Turrell WJ. The therapeutic action of constant current. Proc R Soc Med. 1920-1921;
14(1-2):41-52.
31 Turrell WJ. The action of the constant current with special reference to its action on the
subcutaneous tissues. Arch Radiol Electtother.
1922-1923;27:130-135.
32 Challiol MM, Laquierriere. Action of the
constant galvanic current on tissues in health
and disease. Arch Radiol Electrother. 19221923;27:135-139,
33 Finzi NS. Cited by: Turrell WJ. The therapeutic action of constant current. Proc R Soc
Med. 1920-1921;14(1-2):41-52.
34 Glass JM, Stephen RI,Jacobsen SC. The
quantity and distribution of radiolabeled dexamethasone delivered to the tissues by iontophoresis. Znt J Dermatol. 1980;19:519-525.
35 Costello CT. Optimization of Drug Delivery With Zontophoresis. Houston, Tex: Texas
Woman's University; 1993. Dissertation.
36 Morton WJ. Guaiacol-cocaine cataphoresis
and local anesthesia: a new cataphorecic electrode and the Wheeler fractional volt selector.
Dental Cosmos. 1896;38:48-53.
37 Druffel C, Fox A, Sabbahi M. Do joint
receptors change h e excitability of motor
neurons. Phys Ther. 1986;66:796-797.
Abstract.
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
38 Sabbahi MA, Fox AM, Druffle C. Do joint
receptors modulate motoneuron excitability?
Electromyogr Clin Neuropbysiol. 1990;30:3873%.
39 Kahn J. Acetic acid iontophoresis for
calcium deposits. Pbys Ther. 1977;57:658660.
40 DeLacerda FG. A comparative study of
three methods of treatment for shoulder girdle
myofascial syndrome. J Orrhop Sports Phys
Ther. 1982;4:51-54.
41 Bertolucci LE. Introduction of antiinflammatory drugs by iontophoresis: doubleblind study. J Ortbop Sports Pbys Ther. 1982;4:
103-108.
42 Hams PR. Iontophoresis: clinical research
in n~usculoskeletalinflammatory conditions.
J Orthop Sports Pbys Ther. 1982;4:109-1 12.
43 Molitor H, Fernandez L. Studies on iontophoresis, I: experimental studies on the
causes and prevention of iontophoretic bums.
Am J Med Sci. 1939;198:778-785.
44 Lewis T, Zotterman Y. Vascular reactions
of the skin to injury, part VIII: the resistance
of the human skin to constant currents, in relation to injury and vascular response.
J Pbysiol. 1926-1927;62:280-288.
45 Leeming MN, Cole R, Howland WS. Low
voltage direct-current bums. JAMA. 1970;214:
1681-1684.
46 Okabe K, Yamaguchi H, Kawai Y. New
iontophoretic transdermal administration of
the beta blocker metoprolol. Journal of Controlled Release. 1986:4:79-85.
47 Siddiqui 0 , Sun Y, Liu J-C, Chien YW. Facilitated transdermal transport of insulin.
J Pbarm Sci. 1987;76:341-345.
48 Chien YW, Siddiqui Y, Shi WM, Liu JC.
Transdermal iontophoretic delivery of therapeutic peptides/proteins. Ann NYAcad Sci.
1987;507:32-51.
49 Burnette RR, Bagniefski TM. Influence of
constant current iontophoresis on the impedance and passive Naf permeability of excised
nude mouse skin. J Pbarm Sci. 1988;77:492497.
50 Bagniefski TM, Burnette RR. A comparison
of pulsed and continuous current iontophoresis. Journal of Controlled Release. 1990;ll:
113-122.
51 Sabbahi MA, Costello CT, Ernran A. A
method for reducing skin irritation by iontophoresis. Pbys Ther 1%4;74(suppl):S156.
Abstract.
52 Su M-H, Srinivasan V, Ghanem A-H, Higuchi WI. Quantitative in vivo iontophoretic
studies. J Pbarm Sci. 1994;83:12-17.
53 Iorned Inc. Visualizing uneven DC current
distribution by fiber electrodes. Pborum.
1992:5.
54 Petelenz TJ, Buttke JA, Bonds C, et al. Iontophoresis of dexamethasone: laboratory studies. Journal of Controlled Release. 1992;20:55
66.
55 Bush RK, Taylor SL, Holden K, et al. Prevalence of sensitivity to sulphiting agents in
asthmatic patients. Am JMed. 1986;81:816820.
56 Wingard LB, Brody TM, Larner J. Schwartz
A. Glucocorticoids and other adrenal steroids.
In: Human Pbanacology. St Louis, Mo:
Mosby-Year Book; 1991:484-493.
57 Hong D, Byers MR, Oswald RJ. Dexamethasone treatment reduces sensory neuropep-
tides and nerve sprouting reactions in injured
teeth. Pain. 1993;55:171-181.
58 Bames PJ, Adcock I. Anti-inflammatory
actions of steroids: molecular mechanisms.
Trends Pbanacol Sci. 1993;14:436-441.
59 Hasson SM, Wible CL, Reich M, et al.
Dexamethasone iontophoresis: effect on delayed muscle soreness and muscle function.
Can JSport Sci. 1992;17:8-13.
60 Hasson SH, Henderson GH, Daniels JC,
Scheib DA. Exercise training and dexamethasone iontophoresis in rheumatoid arthritis: a
case study. Physiotherapy Canada. 1991;43:
11-14.
61 Kahn J. Iontophoresis and ultrasound for
postsurgical temporomandibular trismus and
paresthesia. Phys Ther. 1980;60:307-308.
62 Rothfield SH, Murray W. The treatment
of Peyronie's disease by iontophoresis of
esterified glucocorticoids. J CTrol.1967;97:
874-875.
63 Silcox G, Parry G, Bunge A, et al. Percutaneous absorption of benzoic acid across human skin, 11: prediction of an in vivo, skin
flap system using in vitro parameters. Pbarm
Res. 1990;7:352-358.
64 Russo J, Lipman AG, Cornstock TJ, et al.
Lidocaine anesthesia: comparison of iontophoresis, injection and swabbing. Am J Hosp
Pbarm. 1980;37:843-847.
65 Weiner N. Norepinephrine, epinephrine,
and the sympathomimetic amines. In: Gilman
AG, Goodman LS, Rall TW, Murad F, eds.
Goodman and Gilman's The Pathologic Basis
of Therapeutics. 7th ed. New York, NY: Macmillan Publishing Co; 1985:145-180.
66 Magistro CM. Hyaluronidase by ionto
phoresis in the treatment of edema. Pbys
Ther. 1964;44:169-175.
67 Popkin R. The use of hyaluronidase by
iontophoresis in the treatment of generalized
scleroderma. JInuest Denatol. 1951;16:97102.
68 Schwartz MS. Use of hyaluronidase by iontophoresis in treatment of lymphedema. Arcb
Intern Med. 1955:95:662-668.
69 Boone DC. Hyaluronidase iontophoresis.
Pbys Ther. 1969;49:139-145.
70 Kling DH, Sashin D. Histamine iontophoresis in rheumatic conditions and deficiencies of peripheral circulation. Arcb Pbys Ther
X-rav Radium. 1937;18:333-338.
71 Kovacs J. Iontophoresis of varicose ulcers.
Arcb Phys Ther X-ray Radium. 1937;18:103106.
72 Abramson DI, Tuck S, Chu LS, Buso E.
Physiologic and clinical basis for histamine
iontophoresis. Arcb Pb-ys Med Rebabil. 1967;
48:583-591.
73 DeHaan CR, Stark RB. Changes in efferent
circulation of tubed pedicles and in the transplantability of large composite grafts produced
by histamine iontophoresis. Plast Reconsa
Surg. 1961;28:577-583.
74 Comwall MW. Zinc iontophoresis to treat
ischemic skin ulcers. Pbys Ther. 1981;61:359360.
75 Becker RO, Spadaro JA. Treatment of orthopedic infections with electrically generated
silver ions. J Bone Joint Surg /Am/. 1978;60:
871-881.
76 Haggard HW, Strauss MJ, Greenberg LA.
Fungous infections of the hands and feet
treated by iontophoresis of copper. JAMA.
1939;112:1229-1232.
77 Weinstein MV, Gordon A. The use of magnesium sulphate iontophoresis in the treatment of subdeltoid bursitis. Pbys Ther Rev.
1958;38:96-98.
78 Kahn J. A case report: lithium iontophoresis for gouty arthritis. J Orthop Sports Phys
Ther. 1982;4:113-114.
79 Kahn J. Acetic acid iontophoresis for
calcium deposits. Pbys Ther. 1977;57:658660.
80 Wieder DL. Treatment of traumatic myositis ossificans with acetic acid iontophoresis.
Pbys Ther. 1992;72:133-137.
81 Coyer AB. Citrate iontophoresis in rheumatoid arthritis of the hands. Ann Pbys Med.
1955;2:16-19.
82 Gordon AH, Weinstein MV. Sodium salicylate iontophoresis in the treatment of plantar
warts. Pbys Ther. 1969;49:869-870.
8 3 Kovacs R. Electrotherapy and Light Therapy. 3rd ed. Philadelphia, Pa: Lea & Febiger;
1938: chap X.
84 Tannenbaum M. Iodine iontophoresis in
reducing scar tissue. Pbys Ther. 1980;60:792.
85 Gangarosa LP. Iontophoresis in Dental
Practice. Chicago, Ill: Quintessence Publishing
CO; 198317-20.
86 Gangarosa LP. Iontophoresis in pain control. Pain Digest. 1993;3:162-174.
87 Henley-Cohn T, Hausfeld JN. Iontophoretic treatment of oral herpes. hryngoscope. 1984;94:118-121.
88 Sloan JB, Soltani K. Iontophoresis in
dermatology: a review. J Am Acad Dermatol.
1986;4:671-684.
89 Grice K, Sattar H, Baker H. Treatment of
idiopathic hyperhidrosis with iontophoresis of
tap water and poldine methosulphate. BrJ
Dermatol. 1972;86:72-78.
90 Abell E, Morgan K. The treatment of idiopathic hyperhidrosis by glycopyrronium bromide and tap water iontophoresis. BrJDermatol. 1974:91:87-90.
91 Shrivastava SN, Singh G. Tap water iontophoresis in palmo-plantar hyperhidrosis. Br J
Dermatol. 1977;96:189-195.
92 Morgan K. The technique of treating hyperhidrosis by iontophoresis. Pbysiotbera~.
1980;66:45.
93 Midtgaard K. A new device for the treatment of hyperhidrosis by iontophoresis. BrJ
Dermatol. 1986;114:48%488.
94 Akins DL, Meisenheimer JL, Dobson RL.
Efficacy of the Drionic unit in the treatment of
hyperhidrosis. J Am Acad Denatol. 1986;16:
828-832.
95 Rapperport AS, Larson DL, Henges DF,
et al. Iontophoresis: a method of antibiotic
administration in the bum patient. Plast Reconstr Surg. 1965;36:547-552.
96 Comeau M, Brummett R, VernonJ. Local
anesthesia of the ear by iontophoresis. Arcb
Otolaryngol. 1973;98:114-120.
97 Echols DF, Noms CH, Tabb HG. Anesthesia of the ear by iontophoresis of lidocaine.
Arcb Otolaryngol. 1975;101:418-421.
98 Vaudin J. Ionization and rhinitis. Physiotherapy. 1973;59:222.
99 Fellner R, Glawogger F. Penicilliniontophoresis in der augenheikunde. Klin
Montasbl Augenbeilkd. 1972;160:300-303.
Physical Therapy / Volume 75, Number 6 /June 1995
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
100 Gibson LE, Cooke RE. A test for concentration of electrolytes in sweat in cystic
fibrosis of the pancreas utilizing pilocarpine
by iontophoresis. Pediatrics. 1959;23:545549.
101 Shwachman H, Mahmoodian A. Pilocarpine ionrophoresis sweat testing: results of
seven years' experience. Bihlio Pediatr. 1967;
86:158-182.
102 Report of the Committee for a Study for
Evaluation of Testing for Cystic Fibrosis.
J Pediatr. 1976;88:711-750.
103 Thysman S, Preat V. In vivo iontophoresis of fentanyl and sufentanil in rats: phamacokinetics and acute antinociceptive effects.
Anesth Analg. 1993;77:61-66.
PHARMACOLOGY
For an in-depth understanding of how
medications influence your patient's
I
I
I
This collection of 13 articles, from a two-part
special series published in Physical Therapy,
such as iontophoresis and phonophoresis; pharmacologic techniques used to manage pain and
reflex activity; and practice issues related to the
prescription of medications by therapists in a
I
I
1
I
Bv PHONE:Call 1-800/999-2782, ext 3395, Monday-Friday between 8:30 am and 5:30 pm Eastern time. Please
have your Mastercard or VISA information ready.
Bv FAX: Fax a copy of this coupon to 703/706-3396.
BV E-MAIL:
E-mail your order and credit card information
to
US via
Internet:[email protected]
clrv
j
I
I
I
DAMIME PHONE
o CnEc,
EmosEo PAvABLr To APTA
o MASTERCARDo VISA
CREDITCARDd
I
GUEST
EDITED BY CICCONE,
WITH 31 CONTRIBUTORS.
(APPROXIMATELY
132 PACES, 13 ARTICLES, 1995).
Physical Therapy / Volume 75, Number 6 /June 1995
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
563 / 113
Iontophoresis: Applications in Transdermal
Medication Delivery
Charles T Costello and Arthur H Jeske
PHYS THER. 1995; 75:554-563.
This article has been cited by 7 HighWire-hosted articles:
Cited by
http://ptjournal.apta.org/content/75/6/554#otherarticles
http://ptjournal.apta.org/subscriptions/
Subscription
Information
Permissions and Reprints http://ptjournal.apta.org/site/misc/terms.xhtml
Information for Authors
http://ptjournal.apta.org/site/misc/ifora.xhtml
Downloaded from http://ptjournal.apta.org/ by guest on September 9, 2014
© Copyright 2026