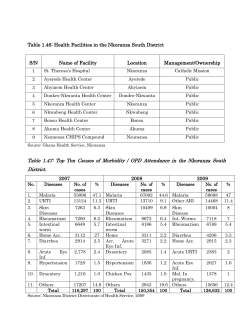
HEALTH/EPIDEMICS – 2009
HEALTH/EPIDEMICS – 2009 (January to December - 2009) Compiled & Edited By K. Samu, Human Rights Documentation, Indian Social Institute, Lodi Road, New Delhi Severe Malaria spread to 28 districts (3) Bhopal, Jan 1: Malaria is spreading fast in the state. It has already engulfed 28 districts of the state. People in other districts are also suffering from this disease but the situation is not alarming in them. The health department of the state has utterly failed to effectively control Malaria in the state. According to information reached here people of more than 50 per cent of the districts, including Gwalior division are under the grip of Malaria fever. During the last one and a half month the number of patients in Gwalior division has increased by five per cent. According to the unofficial reports 42 patients including 24 children died of Malaria fever in Chambal Division. All the districts of the state are affected by Malaria fever. The situation in Bhind, Morena, Guna, Shivpuri and Sheopur the situation is very alarming. Here the patients are not properly responding to the medicines. In districts like Chhattarpur, Tikamgarh, Sagar, Jabalpur, Bhopal, Indore, Betul, Khandwa the situation is not very bad. According to a report lakhs of people are attacked by Malaria fever every year. But government statistics tells a different story. (Central Chronicle 2/1/09) Latest polio victim also from UP (3) NEW DELHI: Delhi ushered in the new year by reporting a fresh case of P1 infection polio virus's most dangerous strain. One-and-a-half-year old boy Sonu, who lived for two weeks near Okhla railway station under the Modi Mill flyover, has become the city's latest victim to be infected with the crippling disease. Even though the infection was confirmed only on Friday, the case dates back to the first week of December. The latest infection takes last year's polio toll in the city to five, of which four are the deadly P1 cases. Interestingly, Sonu's family hails from Uttar Pradesh. They are nomads who travel across states, selling hand-made ropes. Sonu's father arrived in Delhi on November 22 and stayed here till December 5 before moving back to Unnao in UP. Sonu suffered paralysis while in Delhi. However, the confirmation that he was affected by polio came only when he was in Unnao. Genetic sequencing of the virus is presently being undertaken at Mumbai's Enterovirus Research Centre to pinpoint its origin. "The child contracted the virus while living in Delhi. During the peak of the virus's incubation period, the child was living next to open railway tracks in Okhla," state government officials told TOI. Multiple vaccination rounds are now being planned in Delhi to respond to the latest P1 importation reported from Okhla. In 2007, Delhi reported two polio cases while in 2006, five polio cases were confirmed from the Capital. P1 is the most dangerous form of polio virus as it can cause huge outbreaks and travel long distances. P1 accounted for 95% polio cases in the country till 2006. P1 causes paralysis in one out of every 200 children while P3 causes paralysis in one out of every 1,000 infections. Migrant populations are at greatest risk of getting infected with polio, having missed immunisation while on the move. In 2008, India recorded 549 polio cases of which 68 were caused by the P1 strain and 481 were P3 infections. UP has recorded 297 cases while Bihar has reported 232 polio infections. Delhi recorded the third highest number of cases five followed by two each in Rajasthan, West Bengal, Maharashtra, Haryana, Orissa, Assam, Uttarakhand and Punjab. Andhra Pradesh and Madhya Pradesh have recorded one case each. In 2007, India recorded 874 cases of polio. "The state's polio eradication programme should concentrate on eradicating P1 transmission while maintaining good control over the P3 strain. The programme objective should be to stop P1 transmission by the end of 2009 and P3 by the end of 2010," an official said. "We recorded 68 cases of P1 in 2008 compared with 83 in 2007 and 646 in 2006. The polio eradication programme in India has to continue prioritising P1 eradication, which caused 95% of the polio cases till 2006," the official added. (Times of India 4/1/09) 70.4 per cent of Jharkhand population suffer from anemia (3) Bokaro: Believe it or not! But it's the starling truth which came after a resent survey; indicates that more than ninety per cent girls in the Jharkhand are anemic and they are suffering from iron deficiency in their blood. Survey also indicates that 70.4 per cent of the state's populations are suffering from anemia. According to the survey report given by National Consultation on Control of National Anemia in India 77.7 per cent young children of the state are anemic, while 71 percent of the state population is suffering from anemia. Talking to the Pioneer Civil Surgeon of Bokaro district Dr Promad Kumar stated that fifty per cent of the anemic women of the world resides in India while in Jharkhand 90 per cent adolescent girls are anemic. “We should take proper steps to arrest the phenomena for which we need involvement of all stake holders like adolescent girls, teachers, health officers, parents, community leaders and assure a steady supply of Iron and Folic Acid tablets for the each children of the target group”, added the Civil Surgeon. He added, “Anemia is a deficiency of red blood cells, which can lead to a lack of oxygencarrying ability, causing unusual tiredness, complications in pregnancy, and many other health-related problems”. Elaborating about anemia Dr Sobha Kumari stated that Iron deficiency anemia is a serious public health problem that affects the ability to study and work as well as health and well being. It is one of the most prevalent nutritional deficiencies in the world, and more than half of the population in India is anemic. The prevalence of anemia is as high as 70 – 80 per cent among children and 60 per cent among pregnant women. In the northern states of Uttar Pradesh and Jharkhand, anemia prevalence among preschool children is 74 per cent and 82 per cent respectively, Stated Dr Sobha. She added, “Anemia is most often caused by iron or folate deficiency and is especially common during pregnancy. Although supplementation of diets with Iron and Folic Acid (IFA) tablets has been a part of Government programming for over three decades, levels of IFA intake remain low. But only 22 per cent of pregnant women reported consuming IFA for 90 days or more when they were pregnant. There are significant challenges in reaching the at-risk population as well as in managing the side effects of IFA consumption which discourage adequate intake”. Talking to the Pioneer Dr Randhir the President of Indian Medical Association (IMA) Bokaro stated that maternal malnutrition is a major cause for concern in the state of Jharkhand. Four of every 10 women in. Jharkhand are undernourished. About two-thirds of women in the childbearing ages are anemic and pregnant women experience the highest levels of anemia. “There is more than one reason for this development. Low social status of women, poor food quality, high cost of healthcare facilities and even some genetic problems are responsible for the problem,” added Dr Randhir. Among the States, Assam is the worst affected, with 72 per cent of its married women suffering from anemia, followed by Haryana (69.7 per cent) and Jharkhand (68.4 per cent). (Pioneer 5/1/09) Ansari expresses concern over healthcare in U.P. (3) LUCKNOW: Vice-President Mohammad Hamid Ansari on Tuesday expressed concern over the low level of human development in Uttar Pradesh and pointed out that deficiencies in the State’s health sector would have disastrous consequences for the poor. Mr. was delivering the convocation address at the fourth convocation of Chhatrapati Shahuji Maharaj Medical University (CSMMU) here.The health of the citizens was a component of the globally and nationally accepted parameters of human development. On this count, and as the State Planning Department has noted, “U.P. continues to languish at a low level of human development,” he said. The matter needed to be addressed in terms of perceptions, policy, proper infrastructure, budgetary allocations and administrative procedures. Mr. Ansari drew a parallel between life expectancy at birth in U.P. at 56 years with that of Kerala (74 years). “It seems that the State you are born determines how long you will live,” he said. The Vice-President’s observations were made in the presence of State Health and Family Welfare Minister Anant Kumar Mishra, who earlier expressed his gratitude to Chief Minister Mayawati for extending healthcare to the poor despite “severe financial constraints of the State government.” Mr. Ansari said there was a significant gap between the aspirations of the people for quality healthcare and the [ground] reality in Uttar Pradesh. Quoting from the National Family Health Survey of 2005-2006, he said 50 per cent of women in the 15-50 age group and 85 per cent children below three years suffered from anaemia, whereas around half of the children born in U.P. were stunted and underweight. While less than 25 per cent of the children were completely immunised, the infant mortality rate (IMR) in U.P. was 73 per 1,000, against the national average of 57. While emphasising that the focus should be on reduction in IMR, Mr. Ansari said that to achieve this objective explicit commitments in the policy and programmes should be made. Only 9 per cent of the State’s population were able to use government healthcare facilities for treatment of ordinary ailments with the rest depending on private health care. Proper attention should be given to preventive healthcare, with concomitant resource allocation. Over 11 per cent of the State’s population was unable to access medical care due to locational reasons, and even if they get access, there was no guarantee of sustained care. Mr. Ansari stressed the need to enhance human resource in the health sector to overcome the shortage of doctors and paramedics in U.P. The State should seek inspiration from other State governments on health insurance cover to the poor.Governor and Chancellor of the university T.V. Rajeswar, who presided over the function, said though India lagged behind in fund allocation for medical science, the situation had improved in the last five years. But much needed to be done. He also underlined the importance of stem cell research. The honorary degree of Doctor of Science was conferred on Purushottam Upadhyaya, Snehalata Deshmukh, Hargovind Laxmishanker Trivedi and R.K. Bali.(The Hindu 7/1/09) Delhi boy gets HIV during cancer treatment (3) NEW DELHI: A 12-year-old blood cancer patient being treated at Guru Teg Bahadur Hospital has been diagnosed as HIV-positive. His family has alleged that he contracted the infection during his treatment when he received several blood transfusions and chemotherapy at the hospital. Deepak, a lymphoblastic leukaemia patient, was undergoing treatment for the past two years at the hospital. ``He underwent a blood transfusion in November last year and his condition deteriorated in December. So, I took him to GTB for a check-up. I couldn't believe when the doctor told me that his report was positive for HIV and Hepatitis B. He has been undergoing treatment for cancer at this hospital only and I have never got him treated at any other hospital,'' said his father, Tilak Ram, who is a small-time painter in Shahdara. Deepak's blood sample has been sent to G B Pant Hospital for a re-test. The medical superintendent of the hospital, Dr P C Dikshit, denies responsibility. ``Firstly, we have not received any complaint from the boy's family in this regard. Secondly, it is very difficult to ascertain whether the boy contracted the infection during the blood transfusion at the hospital or not. He could have contracted the infection anywhere as he was not well and was being treated somewhere else.'' Deepak was diagnosed with lymphoblastic leukaemia in January 2007 and hospitalized for nearly eight months at GTB Hospital. ``He was initially being treated for tuberculosis of the lung but later I was told that he has cancer and that his treatment would continue for two years,'' said Tilak Ram. ``Till now, he has undergone 11 blood transfusions at the hospital. My wife and I were hoping that he would recover but this news has left us shattered. We have told him that he has some blood infection since he won't understand what HIV infection is.'' Tilak Ram has six children. A senior doctor in the hospital said: ``Deepak was undergoing chemotherapy outside. He could have contracted the infection from anywhere. It is difficult to pinpoint one source until there is a detailed investigation, and even then it will be a difficult call. This is a rare and unfortunate case.'' Though government blood banks have made their procedures very stringent to ensure that blood is HIV free, there is still a small possibility of the blood carrying the virus. ``A lot of precaution is taken while banking the blood,'' says Mohammad Shaukat, joint director, blood safety, National AIDS Control Organisation. ``We have various forms which a donor has to fill so that we can evaluate whether the donor is free from high-risk behaviour or not. There is though a small possibility of contracting infection from blood transfusion as the donor might be in the window period when he had donated the blood. The minimum time for the virus to be detected is at least 11 days. All blood banks follow high standards in testing for HIV but still it can't be said that the blood is 100% HIV infection free.'' Deepak's father is waiting for the blood test reports from GB Pant Hospital after which he says he will file a complaint against the hospital. (Times of India 9/1/09) 20,000 die of rabies every year: Experts (3) Bangalore, The Indian Public Health Association and Department of Community Medicine, Kempegowda Institute of Medical Sciences, had organised the CME programme, on Thursday, where issues pertaining to Community Medicine -- from prevention and control of rabies to tuberculosis was discussed on day one. Two speakers, Dr Madusudana, Additional Professor of Neuro Virology, NIMHANS and Dr Sudarshan M K, Principal and Dean KIMS, covered the topic -- Prevention and control of rabies. They informed that according to statistics, more than 1.7 million dog bites are recorded in the entire country. There are 20,000 rabies death every year, of which 90 per cent can be attributed to bites from stray dogs. They also covered the current mode of treatment for rabies which is widely in use. Treatment of dog bites typically starts with post exposure treatment which consists of wound wash with soap and water. This is followed by anti-rabies vaccination to produce active immunity and rabies immunoglobulin, an active ingredient will be injected into the bite site directly, to kill the viruses at site. However the drawback of the anti-rabies vaccine, which is modern tissue culture vaccine, is the cost. The speakers discussed alternative treatments at a lower cost. The anti-rabies vaccine which is intramuscular comes at a cost of Rs 350 per dose, making the entire course of treatment (five courses) on day 0, day 3, day 7 day 14 and day 28 amount to Rs 1,750. The alternative discussed was the intradermal rabies vaccination which is one fifth the cost. The other sessions for the day covered issues pertaining to tuberculosis and the avian influenza. Deccam Herald 9/1/09) Doctors protest ‘baseless statement’ by A.P. Human Rights Commission chief (3) CHENNAI: B. Subashan Reddy, chairman of the Andhra Pradesh Human Rights Commission (APHRC), has called for legislation to prosecute parents with diseases such as tuberculosis, HIV, leprosy and dyslexia should they, knowing that they have the disease, have children. His remarks in Hyderabad have drawn a sharp response from three doctors who say that “the statement is devoid of any substance or rationale” and that “making irresponsible and ill-considered statements like this could lead to further stigmatisation and ostracisation of an already marginalised population.” This is the text of the response: It was with great concern and disbelief that we read the statement made by the chairman of the Andhra Pradesh Human Rights Commission regarding criminal prosecution of persons with diseases such as tuberculosis, HIV, leprosy, or dyslexia if they had children. We would like to give reasons why this statement is devoid of any substance or rationale and point out that making irresponsible and illconsidered statements like this could lead to further stigmatisation and ostracisation of an already marginalised population. Neither tuberculosis nor leprosy is a genetic or inheritable disease. Further, both are curable with drugs and patients become non-infectious within a few weeks of starting treatment. Children with dyslexia, a common learning disability, only need recognition of their problem and educational and social support to be able to function as normal, self-reliant members of the community. Tuberculosis is an air-borne infection and anyone can get the disease at any stage in life. Half of adult Indians have latent TB infection, which can flare up to active TB in later life. Should all these people abstain from having children for fear that they may develop TB one day? HIV infection spreads by sexual contact, mother-to-child transmission, and use of unsafe needles and blood or blood products. Mother-tochild transmission accounts for less than 4 per cent of new infections in India — even these can be prevented by screening and timely treatment of pregnant women. …. (The Hindu 9/1/09) Infant mortality rate highest in K’mal: Study (3) Bhubaneswar: Violence-hit Kandhamal has yet another reason to worry. According to New Delhi-based Population Foundation of India’s (PFI) report, infant mortality rate (IMR) in Kandhamal is highest in India. PFI in its report “Infant and Child Mortality in India: District Level Estimates” says the infant mortality rate in Kandhamal is 121 per 1,000 live births.Despite the district having over 50 Government-run hospitals and healthcare centres, health services remain out of bounds for poor tribals in remote hilly tracts, as doctors skip their official duty. Scheduled tribes constitutes over 50 per cent of Kandhamal’s population and about two-thirds of the people are living below the poverty line. Though agriculture is the main occupation of the people, 70 per cent of the land is unproductive, as per official statistics. Among the country’s 593 districts, Kandhamal has the highest (121) IMR, while Kottayam in Kerala has the lowest (13), according to the PFI report. The national IMR stands at 54. Among the States and Union Territories, Madhya Pradesh has the highest IMR (94), followed by Orissa (90). Kerala has the lowest IMR at 18. As for the child mortality rate (CMR), the trend continues with Madhya Pradesh having the highest (102), followed by Uttar Pradesh (94) and Orissa (90). Kerala has the lowest (20). Female IMR is more pronounced than male in a few States like MP, Orissa, UP, Rajasthan and Bihar, says the PFI report. (Pioneer 13/1/09) Now, baby doom in Kandhamal (3) Bhubaneshwar: Kandhamal is once again in the news and this time too for the wrong reason. The impoverished district in Orissa has earned the dubious distinction of having the highest infant mortality rate (IMR) with 121 deaths per 1,000 live births. The figures were revealed in a report published by the New Delhi-based Population Foundation of India (PFI) in its publication, 'Infant and child mortality in India: district-level estimates'. "Among 593 districts in the country, Kandhamal has the highest IMR at 121 and Kottayam in Kerala has the lowest IMR at 13," the report stated. The national infant mortality rate is 54 per 1,000 live births. Orissa's planning minister Duryodhan Majhi said agriculture was the main occupation of the people of Kandhamal, but more than 70% of the land in the district fell in hilly areas. As a result, two-third of the population in the area falls in the below poverty line bracket. Among the states, Madhya Pradesh continues to lead the in terms of IMR. The state has the highest IMR at 94, followed by Orissa at 90. Kerala has the lowest IMR at 18. In case of child mortality rate (CMR), which includes toddlers below five, Madhya Pradesh takes the lead again. The state has the highest CMR at 102 followed by Uttar Pradesh at 94 and Orissa at 90. Kerala has the lowest CMR at 20. (DNA 14/1/09) Drop in infant mortality rate (3) PUDUCHERRY: Infant Mortality Rate (IMR) has dropped in the Union Territory, as per the latest SRS report of the Registrar-General of India. The IMR has come down from 28 per 1,000 live births to 25 per 1,000 live births in the last three years . Director of Health Dilip Kumar Baliga said that the reduction comes after efforts to increase institutional deliveries in the Union Territory. “We have a high percentage of institutional deliveries in the Union Territory. Nearly 99 per cent deliveries are at institutions now, that too at major hospitals such as government hospital and maternity hospital in Puducherry and government hospitals in Karaikal and Mahe,” he said. Neonatal care services had also increased over the years with death of infant within the first week of birth - neonatal death rate - considerably reduced . “We are taking efforts to bring in a further reduction in IMR. It is important to take care of the nutrition of pregnant mother, especially during the last three months to have a baby with good weight,” Dr. Baliga said. “The survival chances for a baby weighing 2.5 kg are good. At least 20 to 25 per cent babies are born weighing less than 2.5 kg. We are trying to improve this situation,” he said. The District Level Household Survey-3 for 2007-2008 found that 77 per cent mothers in Puducherry had registered in the first trimester. Nearly 98.6 per cent mothers had at least three ante-natal care visits and 96 per cent mothers received post natal care within 48 hours of delivery. Already, the Directorate was providing nutrition for pregnant mothers through anganwadis, self-help groups and Mahila Mandals for the last three to four years. “We are insisting on at least two ante natal check-ups during the last trimester. We have appointed specialists including gynaecologists at eight Primary Health Centres for consultation. Specialist services are available every day for pregnant mothers,” he said. (The Hindu 17/1/09) Women in LDCs 300 times more likely to die in childbirth (3) New York (PTI): Bearing a child remains one of the biggest health risks for women worldwide, particularly in the least developed countries (LDCs), who are 300 times more likely to die in childbirth or from pregnancy-related complications than women in developed countries, the UN Children's Fund has said. A child born in a developing country is almost 14 times more likely to die during the first month of life than a child born in a developed one, the 2009 edition of UNICEF's flagship publication "The State of the World's Children" said. "The divide between the industrialised countries and developing regions, particularly the least developed ones, is perhaps greater on maternal mortality than on almost any other issue," the report said. For example, a woman in Niger has a one in seven chance of dying during the course of her lifetime from complications during pregnancy or delivery, as against the risk faced by mothers in the United States, where it's one in 4,800 or in Ireland, where it's just one in 48,000. Following close behind Niger in terms of the highest lifetime risk of maternal death are Afghanistan, Sierra Leone, Chad, Angola, Liberia, Somalia, the Democratic Republic of Congo, Guinea-Bissau and Mali. The agency noted that both mothers and infants are vulnerable in the days and weeks after birth – a critical time for lifesaving interventions, such as post-natal visits, proper hygiene, and counseling about the danger signs of maternal and newborn health. While many developing countries have made excellent progress improving their child survival rate in recent years, there has been less headway in reducing maternal mortality. Niger and Malawi nearly cut their under-five death rates in half between 1990 and 2007. In Indonesia, underfive death rates fell to nearly a third of what they were in 1990, and in Bangladesh they fell by more than a half. The same progress, however, has not been made in addressing health risks for mothers, who are most vulnerable during delivery and in the first days after birth. And while the rate of survival for children under five years of age is improving globally, the risks faced by infants in the first 28 days remain at "unacceptably high levels" in many countries. Launching the report, UNICEF Executive Director Ann M Veneman noted that more than half a million women die every year as a result of pregnancy or childbirth complications, including about 70,000 girls and young women aged 15 to 19. "Since 1990, complications related to pregnancy and childbirth have killed an estimated 10 million women," she added. To lower the risks for pregnant women and newborns, the report recommends the provision of essential services that include a continuum of care at critical points – adolescence, pre-pregnancy, pregnancy, birth, post-natal and neonatal periods, infancy and childhood – as well as at key locations where they can be readily accessed by women and children. "Saving the lives of mothers and their newborns requires more than just medical intervention," noted Veneman. "Educating girls is pivotal to improving maternal and neonatal health and also benefits families and societies." Welcoming the new report, the UN Population Fund (UNFPA) called for more action to achieve universal access to reproductive health by 2015, which is the target date for achieving the globally agreed anti-poverty objectives known as the Millennium Development Goals (MDGs). (The Hindu 17/1/09) ‘India may have 60 pc of the world’s heart patients by 2010’ (3) London: An international group of researchers has warned that India may have 60 per cent of the world’s heart disease patients by 2010, for a study has shown that one in 25 individuals in the country carries a genetic mutation that raises risk of heart disease. Almost 1pct of the world’s population carries a genetic mutation that leads to heart problems, while in India the mutation reaches a frequency of 4 pct, say the researchers. "The mutation leads to the formation of an abnormal protein," Nature quoted lead researcher Kumarasamy Thangaraj from the Centre for Cellular and Molecular Biology, Hyderabad, India as saying. "Young people can degrade the abnormal protein and remain healthy, but as they get older it builds up and eventually results in the symptoms we see," he added. The mutation, a deletion of 25 letters of genetic code from the heart protein gene MYBPC3, is virtually restricted to people from the Indian subcontinent. But there, Caste and Tribe, Hindu, Muslim, Sikh, Christian and others are all united by this affliction. One in 25 people of Indians carry this mutation. "We think that the mutation arose around 30,000 years ago in India, and has been able to spread because its effects usually develop only after people have had their children. A case of chance genetic drift: simply terribly bad luck for the carriers," said Chris Tyler-Smith from The Wellcome Trust Sanger Institute, Hinxton, UK. "The bad news is that many of these mutation carriers have no warning that they are in danger," said Perundurai S. Dhandapany from Madurai Kamaraj University, Madurai, India, "but the good news is that we now know the impact of this mutation." People carrying the mutation can be identified at a young age by genetic screening and a healthier lifestyle. "This is a genetic finding of great importance," said Sir Mark Walport, Director of the Wellcome Trust. "Heart disease is one of the world’s leading killers, but now that researchers have identified this common mutation, carried by one in 25 people of Indian origin, we have hope of reducing the burden that the disease causes. “This research should lead to better screening to identify those at risk and may ultimately allow the development of new treatments," he added. (Indian Express 19/1/09) Malnutrition deaths invite HC ire (3) NAGPUR: The Bombay high court has come down heavily on the state government for failing to check malnutrition and infant deaths among tribals of Melghat in Amravati. "We have no hesitation in observing that the progress in preventing malnutrition and infant deaths is hardly satisfactory,'' said chief justice Swatanter Kumar and Justice D Y Chandrachud while hearing a public interest petition filed by Rajendra Burma and Ravindra Kolhe, two doctors who have been striving to address the malnutrition problem in the area. "...the picture is dismal. We are afraid the state is failing in its duty to protect the life of poor residents of this state,'' the court said during the hearing of the case held before the principal bench last week. The court also observed that the infant mortality rate was an alarming 74 per 1,000 in Melghat compared to the state average of 38. "This should be sufficient to wake up state authorities,'' the court stated. The court has further directed tribal department secretary N Aramugham, who was present in the court, to visit the malnutrition-hit areas and examine the facts. It also directed additional chief secretary (public health) to file an affidavit on points raised by the petitioners. The petitioners' counsel Jugal Kishore Gilda had contended that there were no anganwadi in Ghana and Makhala villages, while the one existing at Kohana catered to 114 children from a 10X18-ft room. Besides providing nutritious food to children below five years, the anganwadis are expected to provide basic education and day shelter to children. Referring to sorry state of affairs in five tribal-dominated districts of Amravati, Yavatmal, Gadchiroli Thane and Nandurbar, the court instructed the additional chief secretary to state the reasons of continued high rate of infant mortality there. It also wanted to know whether norms stated and schemes formulated by the state are actually being implemented, and if not, the action taken against the officials concerned. The court has also asked for details of the amounts received in last three years by the state government from The Central government under the integrated child development scheme (ICDS) and to what extent they were utilised. Directing that the orders be complied within a week, the court warned that in event of default, the chief secretary and the additional chief secretary shall remain present in the court. "We are compelled to pass these directions as orders passed by the division benches right from the year 2007 have failed to given any results. On the contrary, during the intervening period there was an increases in malnutrition and infant deaths and it appears that none of the competent authorities in the government are taking the above directions with seriousness," the court said in its scathing indictment of the government. (Times of India 21/1/09) ‘Cooking oil in market poses health hazard’ (3) New Delhi: Feb. 3: A new study by the Centre for Science and Environment (CSE) has revealed that the cooking vegetable oils available in the market have trans fats — commonly understood as bad cholestrol — and that the levels of trans fat in these products was much above the permissible limit, leading to serious health risks like infertility in women, diabetes and Alzheimer’s disease and even breast cancer. The body attributed the prevalence of such products in the market to weak regulation by the Central government. According to the report, which was released here on Tuesday, it was found that in all vanaspati brands, trans fat levels were five to 12 times higher than the world’s only standard for trans fats in oil, set in Denmark, at 2 per cent of the total oil. The CSE’s Pollution Monitoring Laboratory tested 30 samples of branded oil widely available in the market. The total fatty acid profile (saturated and unsaturated) comprising 37 components and nine trans fats was analysed. The samples comprised vegetable oils such as soyabean, sunflower, mustard and coconut, partially hydrogenated (vanaspati) oils, desi ghee and butter. Talking to the media after releasing the report, director, CSE, Sunita Narayan, said: "This happens because food regulatory bodies in India just have no stomach for setting stricter standards for the product or for the health claims on its labels, which allowed the companies to get away with literally anything, which was just not acceptable." Meanwhile, reacting to the report, Union health minister Anbumani Ramadoss described trans-fats as a "danger on the health of Indians". He added that while he had taken cognisance of the issue, imposing a ban on any product content required availability of substitutes. The report further said that the lowest trans fats — which are results of process of hydrogenation that gives the product longer shelf lives — level was found in desi ghee of Milk Foods Ltd and in Amul butter — 3.73 per cent. The highest percentage, 23.7 per cent, was found in "Panghat" brand of vegetable oil. It is particularly bad for the heart and can also infertility in women, diabetes, Alzheimer’s and even breast cancer. In 2004, the health ministry had begun discussions on a standard for trans fats. However, in September 2008, it came out with notification for labelling of trans fats on oil and food which helps companies get away by listing anything on the labels. (Asian Age 4/2/09) Hepatitis-B affecting Tripura's tribal population (3) Agartala (PTI): About 15 per cent of the tribal population in Tripura was affected by Hepatitis-B which was much above the national average, president of the Hepatitis Foundation of Tripura (HFT) Dr Pradip Bhowmick said on Wednesday. The tribals constitute one third of the state's population. However, the disease has affected only 4.5 per cent of the state's population as a whole, which is much less than the national average of 8 per cent, Bhowmick told PTI. The Hepatitis Foundation of Tripura, a non government organisation which works in collaboration with the state government, has vaccinated more than three lakh people in the state in last six years. The foundation would very soon conduct a survey through out the state to find out the level of awareness of the people about the disease, whether they were being vaccinated and the reason behind the high incidence of the disease in tribal areas, he said. Dr Bhowmick said, after the survey reports were available, the organisation would build up stringent awareness campaign and set up more vaccination centres depending on the requirments. (The Hindu 5/2/09) Explain deaths in tribal school: HC (3) MUMBAI: The Bombay high court on Friday ordered the secretary of the tribal development department to be present in court - in person - to explain the deaths of five tribal children in a state-run ashram school in Dahanu. A division bench of Chief Justice Swatanter Kumar and Justice Dhananjay Chandrachud upbraided the state and asked the secretary to visit government-run residential schools in Thane and submit a report by February 27. The court also asked the chief judicial magistrate of Thane to visit the said `ashram' schools. The court's direction came on a PIL that referred to newspaper reports on the deaths of the school children. In an affidavit, the state claimed that the children had died due to reasons beyond the control of the ashram school administration. The government had paid a compensation of Rs 15,000 to the families of the children. With regard to the allegations of rape levelled by a female student against the ashram school superintendent Vinod Shirsath, the government, much to the court's consternation, claimed it was the case of a "love affair'' between the two. Assistant government pleader Pradip Patil told the court that an inquiry has been initiated against one of the head masters and two superintendents. The court asked the additional solicitor general to ensure that the central government conducts an enquiry into the safety of food supplies given to the tribal students. (Times of India 7//2/09) 12 Tripura tribals die of unknown disease (3) Agartala, Feb. 8: Twelve tribals, including women and children, had died of an unknown disease in remote villages under Dhalai district of Tripura. Rumela Debbarma, 37, a tribal woman from remote Jamircherra, is battling for life at the ICU of GB Hospital, Agartala. The director of health services, Satya Ranjan Debbarma, said in the past one week the toll had risen to 12 in remote tribal-dominated Sarpakumar para, Laldinga Bari, Lalcherri, Chhaya Roaja para villages. “We have sent a medical team there and diagnosis will start soon. Since the woman admitted to the ICU of GB Hospital carries germs of meningitis, we assume that the deaths were caused either by meningitis or encephalitis,” Debbarma said. The villages had no primary hospital within a radius of 42km, he said. “Remoteness has always been a major problem but steps are being initiated to launch at least three primary health centres near these villages and before that medical teams will be visiting there as frequently as possible.” The health department is preparing to organise a five-day mega health fair at Agartala’s Children’s Park from Tuesday to Saturday. “There will be 150 stalls at the fair opened by the state health department, NGOs working in the health sector and institutions run on public-private partnership model,” commissioner for health Yashpal Singh said adding that organising the fair would cost Rs 15 lakh. Free medical check-ups and services, including pathological tests, will be provided to the people at the fair. “For access to services of an MRI machine, we will give a 20 per cent discount for each test but the rest will be free,” Singh said. He added that the health department was planning to launch new diagnostic centres on public-private partnership models in the government-run hospitals of the state. “The centres will be equipped with the latest and the most sophisticated machines and we will ensure that only reputed and responsible institutions working in the health sector are made partners,” Singh said.(Telegraph 9/2/09) Malnutrition kills 50 children in Madhya Pradesh: survey (3) Bhopal, Feb 10 : Malnutrition has killed over 50 children in Madhya Pradesh in less than six months, say NGOs. The government says it has no information about the deaths. The main reasons ascribed to the deaths are poorly-equipped government health centres and failure of government schemes to reach a majority of the impoverished, say NGOs after surveys in five districts. An NGO, Spandan, carried out a survey with support from Action Aid (India) in Burhanpur, Khandwa, Khargone and Hoshangabad districts and found that 22 children had died due to undernourishment in six months. Similarly, the Madhya Pradesh Right to Food campaign and Adiwasi Adhikar Manch reported 28 deaths in Satna district alone between October 2008 and January 2009. Twelve deaths were reported from Burhanpur district, between June and November 2008. "Six children died of malnutrition in five villages of Khandwa between October and December 2008, one child died in a village of Khargone in October while three children died in two villages of Hoshangabad," said the Spandan survey. Spandan claimed that 30 percent of the 216 children surveyed in Burhanpur, 23 percent of 116 children in Khandwa and 30 percent of 177 children in Khargone were "severely malnourished". It said that in Burhanpur 58.3 percent children do not attend anganwadis (women and chilcare centres), 7.5 percent families are landless, only 30.7 percent got employment under the National Rural Employment Guarantee Act (NREGA) and 25 percent families do not have ration cards. "This is the tip of the iceberg since these figures pertain to death of children in five districts. Just imagine the gravity of undernourishment considering there are 50 districts in the state," said Sachin Jain of the Right to Food Campaign. Kalpana Shrivastava, commissioner of women and child welfare department in the state government, expressed ignorance about the malnutrition deaths. She said the state could only provide supplementary nutrition. Shrivastava said: "The main problem is that whatever the state provides can only be supplementary nutrition. It is hard to tackle malnutrition if hunger is a chronic problem." According to the National Health Survey data, the number of malnourished children in the 0-5 years age group is 33,000, which is about 60 percent of the total child population in Madhya Pradesh. The state has with the assistance of the UNICEF and the World Food Programme unveiled schemes like the 'Bal Shakti Yojana', 'Shaktimaan' and 'Bal Sanjeevani Abhiyan' to treat severely malnourished children. "But one can make out the level of nourishment provided to children from the state of anganwadis. They lack basic facilities like seating arrangement, drinking water, separate toilets or space to cook nutritious food," Jain said. "The percentage of underweight children in Madhya Pradesh has increased from 54 in 1998-99 to 60.3 at present and the percentage of wasted (extremely malnourished) children has according to the National Family Health Survey (NFHS-3) gone up from from 20 to 33 despite UNICEF involvement," said an official of the women and child welfare department on condition of anonymity. According to the Comptroller Auditor General of India, government schemes do not reach 52-62 percent of children in the state. (New Kerala 11/2/09) Anbumani: awareness key to reducing infant mortality rate (3) NEW DELHI: Awareness and availability of affordable and equitable health care are the key to achieving better health indices in reproductive and child health areas, Union Health Minister Anbumani Ramadoss said on Wednesday. Speaking at a governing body meeting of the Jansankhya Sthirata Kosh (JSK) here, he underlined the need to keep the focus on spread of awareness and improving infrastructure to bring down infant mortality rate and maternal mortality rate. The Minister also launched the Virtual Resource Centre (VRC) of the JSK. The VRC provides access to films, posters and photos on gender, maternal and infant mortality, the waning sex ratio, and adolescent health spacing. The material is of use to teachers, researchers and students; non-governmental organisations, and the media. Inter-university and schoollevel quiz competitions are being planned to motivate young people to use the VRC that would heighten interest in maternal and child health issues. It is a virtual documentation centre and anyone can place orders and receive the material on CD free of cost and get easy access to advocacy material. Through this approach, the JSK also expects to motivate young people to refuse societal pressure to prove early fertility; to shun dowry and sex determination tests, and reject female foeticide. (The Hindu 12/2/09) Death toll in hepatitis outbreak rises to 16 (3) Ahmedabad: The Sabarkantha district health department has filed cases against seven doctors for negligence of duty after the death toll in hepatitis infection cases rose to 16 with most of them being reported from Modasa taluk here, a top official said on Sunday. “In all, 47 cases of hepatitis have been registered in the district with most of the cases in Modasa taluk,” Chief District Health Officer (CDHO), Sabarkantha, H.S. Patel, told PTI. “Of the 47 cases, 16 died of the hepatitis infection from the beginning of this month till date. — PTI (The Hindu 16/2/09) Nearly half of Guatemalan children suffer malnutrition (3) Guatemala City (IANS): Nearly half of Guatemala's children suffer from chronic malnutrition and their physical growth falls below the average established by the World Health Organisation (WHO), according to a study. The study carried out by the education and health ministries found that 45.6 percent of Guatemalan children suffer from chronic malnutrition, EFE reported Sunday. The nationwide study in schools has also found that children between the ages of eight and nine were most affected by malnutrition. Girls suffered the effects of poor nutrition disproportionately, accounting for 60 percent of all cases of children with lower than normal height for their age, the study said. On an average, Guatemalan girls are between eight and 12 cm shorter than the average set by the WHO. In rural areas, where poverty levels are highest, the study found that 49.7 percent of children suffer from malnutrition, mainly in the western provinces of Solola and Totonicapan. The study was conducted in August among 459,808 children at 15,076 public schools across the country. Experts from international organisations assisted the ministries in the study. Juan Aguilar, head of Guatemalan president's food security secretariat, told reporters that the lack of adequate food, poverty and a dearth of basic services are the primary causes of this scourge, adding that malnutrition not only limits biological growth among young people but also stunts their ability to learn. According to official figures, 52 percent of Guatemala's 13.3 million people live in conditions of poverty or extreme poverty (The Hindu 16/2/09) Death toll in Hepatitis outbreak in Gujarat rises to 24 (3) Ahmedabad, Feb 18 (PTI) Five more deaths have been reported today in Modasa taluk in north Gujarat due to Hepatitis, taking the toll to 24 in less than a fortnight, district health officials said. "Five people have lost their lives due to the diseases taking the number of deaths due to hepatitis infection to 24. Of those, who died today, three were undergoing treatment at the Civil hospital in Ahmedabad, while two were in Sarvajanik hospital in Modasa," Chief District Health Officer of Sabarkantha district H S Patel told PTI. According to Patel, there have been seven new cases reported taking the total number of cases registered to 77, off which 24 have died. Over 58 persons are undergoing treatment at various hospitals in different districts, he added. The State Health Department is working round the clock to control the outbreak of Hepatitis B and Hepatitis D, officials said adding that more than 135 teams comprising of 44 doctors are doing door-to-door survey to check for more infected people. A central team of National Institute of Communicable Disease, Delhi and Institute of Virology Pune had visited Modasa to take stock of the situation. PTI (PTI 19/2/09) Orissa fares worse than Bangla, Bhutan (3) BHUBANESWAR: Despite all tall claims of initiation of effective measures to curb the high maternal and neonatal mortality rate, Orissa continues to be among the highest incidence states, according to the State of World Children report 2009 (SoWC) released by Unicef recently. The maternal mortality rate (MMR) (deaths per lakh live births) in Orissa is at 358 against 301 nationally. The State fares poorer than countries like El Salvador, Dominican Republic and Guatemala. Similarly, the U-5 (under-five) mortality rate is 90 per 1,000 against 72 Nationally and poorer than Zimbabwe, Pakistan, Bangladesh and Bhutan. As far as neonatal mortality rate (death of a child before 28 days), with 52 deaths per 1,000 it tops the country that has 39. Though Unicef maintains that high MMR is linked to high neonatal mortality rate, in Orissa high MMR is not the sole factor behind the high neonatal mortality rate. Infections, asphyxia (suffocation) and preterm births are also major factors. The SoWC concludes that lack of proper antenatal care is responsible for the manifestation of these three lethal causes. It says as high as 82 per cent of newborn deaths in India is due to Preterm births (35 pc), infections (24 pc) and asphyxia (23 pc). High level of female illiteracy, poor maternal health care delivery apparatus, no all-weather roads, low per capita expenditure and no decisive role on their own health in the family are also the cardinal factors in MMR. The report has specially highlighted the fact that the need of medical care for the pregnant mothers was decided either by their husbands, mothers or mothers-in-law. It says haemorrhage after delivery is the major cause of high maternal mortality in Orissa followed by eclampsia, sepsis and anaemia. Early marriage too is a contributing factor. As much as 14 per cent mothers in Orissa are in the age group of 15-19 years. Sixty-eight per cent pregnant women in Orissa are anaemic. As high as 54 per cent births are not assisted by any health worker while the institutional deliveries constitute only 39 per cent. Thus, the need of the hour is to tighten the belt and take result-oriented interventions to ensure safe child delivery. (Express Buz 19/2/09) Guj hepatitis: Toll rises to 46, new cases detected (3) Ahmedabad: As Gujarat health officials stepped up the vaccination drive in hepatitis-hit Modasa town Sabarkantha district, the death toll due to the liver disease climbed to 46 with three more deaths on Tuesday. "Three more deaths were reported today. With this, the total death figure now stands at 46," said Chief District Health Officer (CDHO) Sabarkantha H S Patel. "Eleven new cases of hepatitis have been reported from different parts of the district and they have been shifted to hospitals," Patel said. The vaccination drive in the North Gujarat district continued for the second day on Tuesday, trying to cover as many people as possible, he said. Around 56,000 people were administered hepatitis-B vaccines in Modasa, the most affected area whose total population is estimated to be over 60,000. Meanwhile, a doctor, Govind Patel, and his son Chintan, who had been booked on the charge of culpable homicide by the Health Department for using contaminated syringes, are yet to be arrested. The district police said the father-son duo was evading arrest and had gone underground. An FIR was filed against Govind Patel and his son after investigation by the Health Department showed most of the people infected with hepatitis in Modasa had taken treatment from them in the last six months. The duo have been booked under Section 304 (culpable homicide not amounting to murder) of the IPC as several of the patients treated at their clinic were found positive for the viral disease and some of them died. They have also been booked under IPC Sections 269 (negligent act likely to spread infection of disease dangerous to life) and 278 (making atmosphere noxious to health). Police said when the Health Department officials had raided Patel's clinic they found used syringes and undisposed medical waste there. (Indian Express 25/2/09) Meningitis claims 17 lives in Tripura in one month (3) Agartala, February 25, 2009: A total 17 people have died of meningitis in Tripura's Dhalai district since January 22, government said on Wednesday. Replying to a question in the Assembly, Health and Family Welfare Minister Tapan Chakraborty said the 17 deaths were reported from different villages in Longterai valley subdivision from January 22 to February 24 this year and the government has taken all precautionary measures to check it. He said the state government wanted to undertake mass immunisation programme in the subdivision but the National Institute of Communicable Diseases has turned the proposal. It has asked the government to offer preventive tablets to the villagers living in and around the affected tribal hamlets, the minister said. Opposition leader Ratan Lal Nath, however, claimed that at least 57 tribal villagers have died of meningitis in Manu and Chawmanu blocks and criticised the health minister for not being able to control the disease. (Hindustan Times 26/2/09) Tribals: DNA trails to thalassaemia (3) JALPAIGURI, March 1: The medical director of Netaji Subhas Bose Cancer Research Institute Dr Ashis Mukharjee said today that the institute had solid evidence to suggest that the short life span of the people from the dwindling Toto tribal community could be attributed to the haunting spectre of Thalassaemia. In the wake of a project entitled "Prevalence and Awareness of Thalassaemia in Tribal Population of West Bengal with Special References to the Toto, Rava and Malpahari," initiated by the Centre, the institute organised a blood sample collection camp on 10 and 11 January at Toto Para in Jalpaiguri district where the officials collected 70 blood samples. “After DNA analysis and various other tests on the collected fluid samples of those blood samples we are now certain that the wide spread tentacles spread out by the blood-related malady are cutting short the normal life span of certain tribal communities. "A staggering 55 percent of those from whom the blood samples were collected are Thalassaemia carriers and around 18 percent are afflicted by the disease. We also arranged a similar blood test among the Rava tribe of North Bengal where we collected 85 blood samples. The results are staggering: 46.6 percent have been confirmed as carriers while 40 percent are Thalassaemia positive,” said Dr Mukharjee. The officials distributed Thalassaemia certificates among the Toto community at Toto Para today. “We used three colours to categorise the certificates. Green certificates have been provided to healthy people, red certificates to Thalassaemia carriers and brown ones to Thalassaemia positives. We advise sufferers to avoid red meat and alcohol and to eat vegetables as often as possible,” added Dr Mukharjee. The medical director said that they had received a positive response from the Toto. “We will arrange a similar program among the Malpahari population in Alipurduar in the last phase of the project” added Dr Mukharjee. (Statesman 1/3/09) Unhappy kids likely to have poor health (3) Children who are unhappy are more likely to get permanently sick or disabled later in life, according to a new study. Unhappy kids likely to have poor health (Getty images) For the study, researchers at the King's College London, looked at over 7,100 people born between 1950 and 1955. They found that those described as ‘miserable’ or ‘unhappy’ by teachers were five times more likely to be off work through illhealth in middle age. They said these kids were also likely to be more prone to depression. The study involved thousands of children who grew up in Aberdeen in the 1950s. Teachers were asked about their temperament and school attendance. The researchers tracked down many of the participants now in middle age to ask them about their employment status. The researchers found that around 392 were unable to work because of permanent disability or ill-health - 5.5 per cent of the total questioned. This could have included those retired through illness and those on incapacity benefit. The study showed that a quarter of those whose teachers had reported them as ‘often appearing miserable, unhappy, tearful or distressed’ were permanently sick or disabled. It was also found that a quarter of those who complained of aches and pain were also off sick through ill-health. However, those who were off school because of poor physical health were no more likely to end up as adults off work sick. "We can't say these childhood trends cause the ill-health later in life, but they certainly seem to be a contributing factor,” the BBC quoted lead author Dr Max Henderson, as saying. "Based on previous research, we suspect these groups are more susceptible to depression and anxiety, which of course is a major cause of being off work," he added. (Times of India 2/3/09) Fluoride victims stage demonstration (3) arriguda (NALGONDA): The fluoride victims of Marriguda staged a demonstration demanding Krishna waters to all the affected habitations to draw the attention of Yuvarajyam president Pawan Kalyan who visited the mandal on Tuesday. This mandal is worst -affected by fluorosis in the district. Charging politicians of all parties with touring their mandal in a rhetoric manner without initiating any concrete steps to find a permanent solution to their woes, the fluoride-affected persons vowed to contest the ensuing Parliament elections from Nalgonda and Bhongir under the banner of Fluoride Vimukthi Porata Samiti to bring their misery into focus. Displaying placards with slogans like ‘Protected drinking water is a constitutional right’, the victims staged a demonstration in front of Pawan Kalyan while he was on his way to address a public meeting in Marriguda in the afternoon. Speaking to media men Tirupathamma, 30, a fluoride victim, alleged that the politicians and VIPs have converted their fluoride-affected mandal as a virtual ‘jathara’. “All the top politicians visited our mandal and had photo sessions with us,” she recalled and deplored that their fate remained unchanged due to the denial of protected drinking water to several fluoride-hit areas. “If they were really concerned about our plight, they would have spent a part of the huge expenditure incurred on flexi boards and helicopter visits to mitigate our woes”, contended Swamy, another victim. Samiti president K. Subash said tha0074 22 fluoride-hit habitations were yet to receive Krishna water in the mandal. The Samiti has already fielded Tirupathamma and Swamy in the local body elections in the past to raise the voice of fluoride victims, he said. “We will field them in the coming Parliament elections to once again voice our concern and safeguard the interests of fluoride-affected people”, he stated. Yuvarajyam president Pawan Kalayan said that the Praja Rajyam will include fluoride mitigation strategy in its election manifesto and sincerely strive to check the menace with a holistic approach. Pawan Kalyan interacted with several fluoride-affected villagers including children at Kudabakshpalli village in Marriguda mandal on Tuesday. He enquired about the health condition of crippled children during an interactive session with parents. Heartrending scenes were witnessed in the meeting as the parents of the affected children poured out their miseries. Later, addressing a public meeting at Marriguda Mr. Pawan Kalyan deplored the fluoride menace which confined several youngsters including children to beds taking a heavy toll on their families due to the apathy of the successive governments since decades. (The Hindu 4/3/09) 98 p.c. public support for anti-smoking laws: Survey (3) NEW DELHI: Bollywood biggies might disagree, but a vast majority of Indians (98 per cent) support the ban on smoking in public places, including restaurants and bars, and an overwhelming 99 per cent favour enforcement of a smoke-free environment at the work place. These are the findings of a new survey released by Voluntary Health Association of India and Healis Sekhsaria Institute for Public Health. The survey was conducted through Synovate’s Global Omnibus to sense public attitudes and preferences in four major Indian cities: Delhi, Mumbai, Kolkata, Chennai. Ninety-nine per cent of the respondents in Delhi said the Government should strongly enforce rules prohibiting smoking at public places and 92 per cent believed exposure to second-hand smoke is a serious public health hazard. Ninety-four per cent supported the rights of non-smokers at public places. The smoke-free laws came into effect in the country on October 2 last year, envisaging all public and work places being rid of smoke in order to provide comprehensive protection from second-hand exposure to tobacco. Says Voluntary Health Association of India senior director Bhavna B. Mukhopadhyay: “It is the Government’s responsibility to protect people’s health and the citizens of this country are sending out a clear message to their elected representatives that they applaud the introduction of smoke-free public and work places. Clearing the air of tobacco smoke with stronger enforcement and compliance of the legislation can potentially turn this initiative into a major public health success story for India in the near future.” The majority of respondents said restaurants and bars are healthier and more enjoyable now that they are smoke-free. Eighty-five per cent of the respondents agreed to this, and 72 per cent agreed very strongly that these places are now healthier. Eighty-eight per cent agreed that it was nice to go out and visit local restaurants and bars without smelling like smoke when they got home. “The results of the survey have highlighted the fact that Indians have decisively spoken out against smoking in public, and….recognition of the fact that secondhand smoke is a health hazard. This clearly shows that there is ample scope for the ban on smoking in public places to succeed in the country, and it is the responsibility of civic bodies to ensure that the rules necessary to achieve this are uniformly enforced,” said the report. (The Hindu 5/3/09) Over 22,000 struck by jaundice in Nellore city (3) NELLORE: Nearly 23,000 people have been affected by jaundice in this city. This was revealed in a study conducted by Narayana Medical College, Nellore and Christian Medical College, Vellore with the help of Nellore Municipal Corporation. Doctors said the epidemic was caused due to drinking water contamination, poor hygienic conditions, connecting sewage into river and poor quality of food supplies in the city. However, there were no deaths. Gastroenterologists says that the pilot study was conducted in 50 divisions in Nellore city and not in the entire district. Dr. Lalit Nihal, Head of Gastroenterology, Narayana Medical College, said this was the largest outbreak of jaundice in South India in the last 50 years. Mr. Rosario Vivek, Department of Gastrointestinal Sciences, Christian Medical College, said the disease attack rate was maximum (6.3 per cent) in the residents consuming municipal water and minimum (2.8 per cent) among the people taking packaged drinking water. About 4.4 per cent of the people taking well water were affected by jaundice, he said. When contacted, Municipal Corporation Commissioner T. S. R. Anjaneyulu said that jaundice which was a seasonal and waterborne disease was alarming during October, November and December months in 2008. However, jaundice is in full control now and there were no cases of Hepatitis E virus now. Municipal Medical Officer P. V. C. Subba Raju said that instructions were given to the food inspectors to collect food samples from hotels to prevent serving of poor quality food and sub-standard food items, which was one of the reason of causing jaundice. A special drive would also be taken up to check the quality of packaged drinking in the city. (The Hindu 8/3/09) Malaria control drive suffers from official apathy (3) MANGALORE: Four people, three from north Karnataka and one from West Bengal, were found to be suffering from malaria symptoms during a visit of a voluntary agency to a construction site off Old Kankanady road here on aturday. They were immediately taken to the Government Wenlock Hospital by Suresh Shetty, an activist of a non-governmental organisation (NGO), for diagnosis and three of them tested positive. However, health workers, who had visited the site earlier in the day, could meet with only Sharanappa (19) from Bagalkot. “They were in a hurry. They checked only those whom they met in the ground floor, collected blood samples, and left after giving a few tablets of Chloroquin to one,” Johrul Seth (19), a construction worker from West Bengal, told The Hindu. Deepak Bolar, assistant health officer (malaria) of the Mangalore City Corporation, said the health workers were supposed to make enquiries with as many people as possible and look for malaria symptoms. The health workers were also supposed to spray fumigants at the construction site and neutralise the potential breeding sites for malaria-carrying mosquitoes. The migrant workers/people such as those found at the construction site were considered “high risk” groups by the National Vector Borne Disease Control Programme of the Ministry of Health and Family Welfare since these groups were most likely to carry the disease with them as they travelled. Mr. Bolar said. In order to prevent such groups from spreading the disease, a health worker was supposed to visit these people every 15 days. Johrul Seth and his co-workers from West Bengal said that they had been there for over two months and not a single health worker visited them. In two months, four Bengali labourers were treated for malaria. Residents of the nearby Dalit shanty of Kuthkori Gudda said that owing to the negligence of health workers, the disease had spread in their area. A random survey on Saturday among 38 children there showed that 28 of them had suffered from malaria in the last two months. The oldest among them was 17 years and the youngest less than one year. Anil Kumar (30), a resident of the area, said that Kuthkori Gudda did not have a long history of malaria. “It all started two years ago, when this construction site came up,” he said. Mr. Bolar said that the builders were fined Rs. 1,000, recently. “They have spent crores of rupees on the building. What is Rs. 1,000 for them? The damage is already done,” said Raju (36), a resident suffering from the disease, along with his two children aged 12 and six. In order to prevent Mr. Raju and his family from spreading the disease further, health workers were supposed to carry out vigorous fumigation inside his house. “Nobody has visited our house for over five months,” said Mr. Raju. Mr. Anil Kumar feels that if any other population from a posh locality of the city were exposed to such a grave risk the MCC and health officials would have rushed to their aid. “Is it because we are poor Dalits that nobody come to our aid?” he asks. The children at Kuthkori Gudda have formed a malaria control group, “Kuthkori Gudde Makkala Parisara Sangha”. The eight-year-old secretary of the organisation, Rahul Raj, eloquently explained the various ways in which malaria spreads and the manner in which it could be controlled. (The Hindu 9/3/09) Anthrax: Orissa told to take precautions (3) VISAKHAPATNAM: With the cutaneous anthrax cases having been reported from the Visakha Agency villages bordering Orissa, the Orissa Government has been asked to take precautions against the spread of the disease. The villages in Munchingput mandal from where the anthrax cases have been reported are a short distance away from Orissa border and people from both sides crossover the border frequently and are also sharing the meat of cattle carcasses, the eating of which is the main reason for the spread of cutaneous anthrax. Hence a letter has been faxed to the Orissa authorities to take precautions against the spread of anthrax, District Medical and Health Officer J. Sarojini said here on Monday. The situation in Korlapodor, Sutiguda, Mukkiputtu, Attikallu, Pillaganduva, Lakshmipuram, Adarladi and Tamidiputtu villages in Lakshmipuram and Barada panchayats in Munchingput mandal, inhabited by primitive tribal groups, from where the cutaneous anthrax cases have been reported, is under control, according to Dr. Sarojini. A total of 16 cases have been identified so far and none of them were bad cases. Five patients are undergoing treatment at King George Hospital here. Regarding the death of eight persons, reportedly due to anthrax during last week, she said that three of them might be due to anthrax but the reason could not be confirmed as clinical tests could not be carried out. Dr. Sarojini had visited the villages during the last two days along with Additional DMHO, Assistant Director of Veterinary Department and others. Active surveillance was still on in the area while the Veterinary Department was continuing with vaccination of cattle. District Collector has designated district-level officials to the 11 mandals of the Agency to take up precautionary measures. Tahsildars were also asked to take measures in their respective mandals. The Project Officer of ITDA, Paderu had banned sale of mutton in the 11 mandals as a precautionary measure. Dr. Sarojini said burial of carcasses was a problem. People were not readily willing to bury the carcasses and also the burial should follow a process. The panchayats in the area were asked to help the villagers in this regard, she added. (The Hindu 24/3/09) The world is watching Rural Health Mission: Sir Andrew (3) NEW DELHI: “The world is keenly watching developments in India following the implementation of the National Rural Health Mission [NRHM], billed as the single-most largest primary health care programmes being run in any country. What happens in India in the primary health care sector will be crucial,” Professor Sir Andrew Haines, Director, London School of Hygiene and Tropical Health, told The Hindu here. “The programme is getting close attention — its strengths as well as its weaknesses. Of particular interest are its features like recruiting women as Accredited Social Health Activists [ASHAs] and involving the community that would lead to accountability and transparency,” Sir Andrew said. Besides, ASHA would be excellent as an intermediary between the people and the formal health system, he said. Not willing to comment on the impact the Mission has had on the primary health care system as he was yet to study the outcomes, Sir Andrew, nevertheless, said the bigger challenge before India was to reduce inequalities that existed within the States. Sir Andrew, who delivered the Second Public Health Foundation of India Day lecture here on Saturday, said the strengths of any primary health care system were its cost-effectiveness and an increased money absorption capacity. He also stressed on the need to integrate population issues with the primary health care systems. “It was in 1978 that representatives from 134 countries gathered in Alma Ata and declared that primary health care was the key to delivering Health for All by the year 2000. Subsequently, however, attention shifted to promoting vertical, diseasespecific programmes. These may be efficient in tackling specific disease burden but are inadequate in addressing socio-economic determinants of health, resulting in a still high burden of preventable diseases, particularly in low and middle-income countries,” he said. According to Sir Andrew, recent years have seen a renewed interest in primary health care in these countries for various reasons, including inequities in health, inadequate progress towards the millennium development goals, major shortfalls in the human resource in health sectors and the fragmented and weakened state of health system in many countries. On whether India can achieve the goals set in the NRHM, he said there were variations within the States as some States were making strong progress while others lagged behind. “I am an optimist and believe a lot can be achieved by way of enhancing absorption capacity, pushing resources, improving the quality of services and establishing an interface between the formal health care at the primary level and workers,” he explained. The immediate expected outcomes would be a reduction in the child mortality rate while improving maternal mortality rate and chronic disease management would continue to be a challenge for some more time, he said. Advocating the need for factoring in environmental issues into public health policies, Professor Haines said India needed to respond to climate change through public health policies. “A simple thing like reducing the green house gases can reduce the disease burden immensely,” Sir Andrew added. (The Hindu 31/3/09) Medico-legal clinics in govt hospitals? (3) Bangalore: The Karnataka State Legal Services Authority is looking into the need of initiating medicolegal clinics in government hospitals across the state. Releasing the `People's Health Manifesto - 2009' on Tuesday, Justice Gopal Gowda heard presentation of case studies and testimonies of denial of health service to people. AIDS victim and peer counsellor Vijaya said she was denied gynaecological treatment in Belgaum district; Savitha, a sex worker, complained of ill-treatment and lack of sensitivity among health professionals; a patient suffering from spinal injury said there's a need for specialists at public health centres (PHCs) and that procurement of disability certificate is difficult. Health secretary M Madan Gopal agreed facilities at PHCs must improve. "We need one PHC for 30,000 people; now we have one PHC for every 14,000.'' According to a recent study by NGO Belaku on health services in Kanakapura, only 5 of 608 pregnant women interviewed had received free treatment. Another study, conducted in 13 districts, showed shortage of emergency medicines like anti-rabies and anti-venom drugs in PHCs and district hospitals, and HIV-infected pregnant mothers being deprived medical care in government hospitals. (Times of India 1/4/09) World must fight drug-resistant TB threat: WHO (3) Beijing (AP): The World Health Organization's chief warned Wednesday that emerging, hard-to-treat strains of tuberculosis are set to spiral out of control and urged countries to fight the growing threat to global public health. WHO Director-General Margaret Chan told health ministers and senior officials from 27 countries worst-affected by the new drug-resistant strains of TB that they must make dramatic improvements in detecting infections and build stronger health care systems. ``Call it what you may - a time-bomb or a powder keg,'' Chan said at the opening of a three-day meeting on drug-resistant TB in Beijing. ``Any way you look at it, this is a potentially explosive situation.'' TB is caused by germs that spread when a person with active TB coughs, sneezes or speaks. It's ancient and treatable but now has evolved into stronger forms: multidrug-resistant TB, which does not respond to two top drugs, and extensively drug-resistant TB, which is virtually untreatable. Left unchecked, people with drug-resistant TB could potentially spread the disease to others, creating an epidemic in the highly mobile global economy. Even when detected, the infected have to switch to more potent and expensive medicines, posing a problem for many countries with underfunded health care systems. Of the more than 9 million people around the world who contract tuberculosis every year, about 500,000 get multi-drug resistant TB. Nearly a quarter of them are in China, where legions of rural migrants face an inadequate health care system. It is also a problem in India, where rural health care is often poor and there is little control over the sale of anti-TB drugs; Russia, which faces a shortage of qualified medical staff and drugs; and South Africa, where the disease thrives amid an AIDS epidemic that has weakened the immune systems of people with HIV. ``I urge you to make the right policy decisions with appropriate urgency,'' Chan said to the officials. ``At a time of economic downturn, the world simply cannot afford to let a threat of this magnitude, complexity and cost spiral out of control.'' Chan said less than 5 percent of estimated cases of drug-resistant TB were being detected and fewer than 3 percent were being treated according to WHO standards. Countries attending the meeting are expected to start drawing up five-year national plans to prevent and control the spread of drug-resistant TB. Many countries have been slow to act, said Medecins Sans Frontieres, also known as Doctors Without Borders, in a statement ahead of the Beijing meeting. ``The slow progress in treating people'' was especially striking because many of the at-risk countries have thriving economies, said MSF's Tido von Schoen-Angerer. ``They have the capacity to act, and need to make this a priority and put people on treatment.'' TB is usually treated in six months with a $20 cocktail of four antibiotics, but its drug-resistant form takes up to two years to fight. Chan said the cost of treating drug-resistant TB can be as much as 200 times higher than normal TB. Detecting drugresistant TB quickly improves the chances a patient will survive and lowers the risk that the disease mutates further into an even more drug-resistant form of the disease. (The Hindu 1/4/09) Puducherry has over 48,000 known diabetics, says study (3) PUDUCHERRY: A community-based study in the Union Territory, the first of its kind, has revealed that about six per cent of the general population in the region are ‘known’ diabetics. The study includes both Type 1 and Type 2 diabetics, with the bulk being of the second category. The study conducted by the Pondicherry Institute of Medical Sciences (PIMS) estimated that there were 48,876 known diabetics living in Puducherry, which has a total population of 10 lakh. Associate Professor, Department of Community Medicine, PIMS, Anil Jacob Purty, said, “We undertook the study to estimate the prevalence of known diabetics in Muthialpet. It was conducted from 2002 to 2007. The data was then used to extrapolate the number of persons diagnosed with diabetes in Puducherry region.” The Urban Health Centre area that was surveyed covered a population living in 12 square kilometre area between Salai Street and Thidal Street along the East Coast Road. A total of 2,677 families resided in the area, accounting for 11,835 persons. Home visits were carried out to identify persons diagnosed with diabetes and taking treatment in the private and public health sectors. Laboratory reports and prescriptions/drugs taken for treatment at least for the last six months, were verified to confirm identity, Dr. Purty added. Researchers found that 684 individuals — 317 men and 367 women — in the study area were aware they had been diagnosed with diabetes. The youngest diabetic was a six-month-old girl child who was on treatment for Type 1 diabetes, he stated. Based on this data, the age-sex specific prevalence was extrapolated using the 2001 Census date for Puducherry. “The number of diabetics living in a small area was surprising. There are persons who remain undiagnosed,” he said. In people aged above 20 years, the prevalence of known diabetics was 8.2 per cent, he added. One of the critical findings of the study was that at least 30 per cent of the immediate family members of known diabetics were at high risk of diabetes, stressing the need for intervention and physical activity, the professor said. “We used the Indian Diabetes Risk Score developed by the Madras Diabetes Research Foundation, Chennai, to identify persons who were at high risk of diabetes. This group should be further screened for blood glucose level. We have already started the testing process. It is likely that 10 to 20 per cent of them will be diabetic,” he said. Results of the study have been published in the International Journal of Diabetes in Developing Countries in the March 2009 edition. (The Hindu 7/4/09) 'Maternal mortality is a silent emergency' (3) Ahmedabad: Dr Mira Shiva, a member of the health committee of the National Human Rights Commission, has been working on issues related to primary healthcare, the right to health, women's health and gender for 29 years. On the eve of World Health Day, she talks to DNA about matters close to her heart and issues affecting Gujarat. On World Health Day, what issues would you like to talk about in relation to women? We will be campaigning for maternal health as one woman in India dies in childbirth every seven minutes. In Gujarat, there are 132 deaths per one lakh live births. Maternal mortality is a silent emergency in India, and needs to be curbed.What are the causes of maternal death? Early marriage, nutrition, maternal health, proximity of healthcare facilities are some of the reasons for this, but a leading cause is the lack of knowledge. Pregnant women are susceptible to infection, obstructed labour, birth-related disabilities and other problems, which can lead to complications. A lack of knowledge leads to improper care, resulting in death.What health problems do women in Gujarat face? Cervical and breast cancer are on the rise in Gujarat. The rate of surrogacy here is the highest in the country, which is good. However, the rights of surrogate mothers need to be revised. For example, in case of multiple births, does the adopting party have to take only one child and leave the other/others for the surrogate mother to look after? What need be done if the child is born with a deformity? Surrogate mothers need rights to protect themselves. (DNA 7/4/09) On World Health Day, focus on safe hospitals (3) NEW DELHI: It is important to keep the health facilities in good stead, specially to deal with emergency situations effectively. This World Health Day April 7 the World Health Organisation (WHO) is creating awareness about safe hospitals by focussing on their importance during disaster situations. According to WHO, more than half-a-million people in south-east Asia lost their lives to natural disasters between 1996 and 2005. "Since in a disaster situation health facilities become the key centre, they have to be in good shape. However, we have seen in the past that health facilities too can get destroyed during such events. Thus, it becomes important to assess the existing facilities for disaster preparedness and all the new hospitals should be built such that they are not caused much damage during a disaster,'' said Poonam Khetrapal Singh, deputy regional director, WHO-SEARO. WHO has come up with `12 benchmarks for emergency preparedness', comprising a complete set of standards and checklists for making new and existing health facilities withstand disasters. "Slight changes in design can save a lot of lives in case of an emergency. The assessment has to be divided on three parameters: Structural, non-structural and functional. Under non-structural, one has to ensure water, electricity, road access, sanitation etc are not disrupted during a calamity,'' said Dr Roderico H Ofrin, regional advisor on emergency action, WHOSEARO. Experts also stressed on the importance of networking of hospitals that can prove beneficial during an emergency. "In India, there is no networking between government hospitals. During emergency situations, if there is communication between two hospitals, the patient load can be easily divided,'' said Dr Shakti Gupta, head of the department hospital administration, AIIMS. The Central government has plans to build mobile hospitals, which can be airlifted to the disaster areas and made operational within six hours. "The Central government has cleared the mobile hospitals project and we should soon have at least two such hospitals in place. A mobile hospital will have everything from an ICU to operation theatre to laboratory. It's a compact unit that can cater to a large number of disaster victims,'' added Dr Gupta. (Times of India 7/4/09) Health screening camps in villages (3) COIMBATORE: Isha Foundation along with PSG Medical College will organise a series of free health screening camps at Semmedu village as part of World Health Day celebrations on Tuesday. The first of the camps was launched on April 5. More than 300 people including children, women and elders, attended the camp. Their medical records would be maintained by the organisers. People were made aware of their illnesses and advised on ways to remain healthy. People who require secondary treatment were referred to the hospital and treated. The programme was also an initiative of Isha’Ws Action for Rural Rejuvenation project that aimed at creating model villages in and around Alandurai. Over the last six months, the Isha Foundation had introduced several activities that addressed health problems in the villages such as Gandhi Colony, Muttathuvayal and Semmedu. Educational assistance in the form of tuitions was offered to children of these villages. Training in tailoring and computers, were offered to the villagers. Toilets were constructed to improve sanitation facilities. Awareness programmes on prevention of diseases, nutrition, hygiene and sanitation were also conducted frequently. (The Hindu 9/4/09) At least 15 to 20 per cent of alcoholic liver diseases are in women, says doctor (3) CHENNAI: Liver is one of those organs that can take plenty of abuse before giving way. It can regenerate most of its cells even when they are damaged. But, constant abuse of the organ can end its unique ability to regenerate and when that happens, it is defined as end-stage liver disease that requires transplantation. Liver cirrhosis is most often caused by alcoholism, viral infections owing to Hepatitis B and Hepatitis C. The latter two, considered ‘silent killers,’ lead to permanent and serious liver damage ending in prolonged jaundice, blood vomiting and liver cancer in some cases. The Government General Hospital in the city also gets patients with Hepatitis A and E infection, says gastroenterologist Mohammed Ali. While Hepatitis A is most common in children, Hepatitis E is caused by consumption of contaminated water. Although hospitals also see patients with problems such as drug-induced hepatitis, gastroenterologists say that in India, consumption of alcohol contributes to the problem of cirrhosis in a larger number of people. Cirrhosis is a condition which impairs the liver’s ability to control infection; remove bacteria and toxins from the blood; process nutrients, hormones and drugs; make proteins that regulate blood clotting and produce bile to absorb fats. According to World Health Organisation, in 2006, around six per cent of the country’s population was categorised as alcoholic. About 35 to 40 million people are infected by Hepatitis B virus. The country also has 15 million Hepatitis C carriers. The disease remains dormant for 20 years and then manifests as life-threatening liver disease that shrinks the liver. At Government Stanley Hospital, 25 to 30 per cent of the cases of cirrhosis are because of alcohol consumption and another 40 per cent, due to viral infection, says R. Surendran, head of its Gastroenterology Department. Until recently liver diseases, especially cirrhosis of liver caused due to alcoholism, was confined to men but now hospitals receive women patients too. At least 15 to 20 per cent of alcoholic liver diseases are in women, Dr. Surendran says. At the Government General Hospital, of the 100 patients coming for treatment less than 10 are women but the trend “is slowly catching up,” Dr. Ali says. Persons suffering from cirrhosis are advised to eat nutritious food, reduce salt intake, and avoid consumption of alcohol and smoking. The treatment aims at slowing the progression of the disease and preventing further damage to the cells of the liver. Liver transplant is the last option and done only when all treatment options have been exhausted, doctors say. (The Hindu 10/4/09) Deadly cholera strain hits India (3) NEW DELHI: It's like an offspring that has picked up the worst qualities of both its parents. A highly virulent and deadly form of cholera strain — the El Tol hybrid — has now been found in India. First discovered in Bangladesh in 2006 and subsequently found in parts of Africa, this recombinant strain is more dangerous than all its predecessors, with the power to kill more people and cause prolonged outbreaks. What's worse, scientists at the National Institute of Cholera and Enteric Diseases (NICED) in Kolkata fear that almost 100% of all new cholera infections in West Bengal and Orissa are being caused by this "new bad boy". "Usually in cholera, with proper Oral Rehydration Therapy, case fatalities shouldn't exceed 1%. Alarmingly, with the El Tol hybrid, case fatalities in Ghana is 24% and 8% in Orissa," said NICED director Dr G B Nair, who had actually discovered the strain in Bangladesh in 2006. According to Dr Amit Ghosh from NICED, the world has seen seven major cholera pandemics since 1816. Till 1961, scientists knew that all the outbreaks were being caused by a classical cholera strain. In 1962, a new strain El Tol took over and continued to cause outbreaks till 2006. "The hybrid strain presently found in Bangladesh, Mozambique and now in India is a combination of both the previous strains. The dehydration caused by cholera is extremely severe when infected with the El Tol hybrid and hence mortality rates are higher," Dr Ghosh said. ICMR director general Dr V M Katoch said the present strain has better survival techniques in the environment. "El Tol hybrid has higher case fatality rates, higher surviving power in the environment and the ability to cause prolonged outbreaks," Dr Katoch said. The most severe warning about the risks of the El Tol hybrid, however, came from Dr Nair. According to him, the classical strain was more virulent and less infectious while El Tol was less virulent and more infectious. "The El Tol hybrid has picked up both attributes and is more virulent and more infectious," Dr Nair said. "The new strain has completely replaced the previous El Tol breed. Earlier, we used to see explosive outbreaks. Now, it is a staggered one, continuing over 5-6 months. That bothers us. We believe the strain came to Kolkata as way back as in 1994. However, any new strain takes time to adjust to its environment. The El Tol hybrid has become most active in India in the past two years," Dr Nair added. Cholera is an acute intestinal infection caused by ingestion of food or water contaminated with the bacterium Vibrio cholerae. It has a short incubation period, from two hours to five days, and produces an enterotoxin that causes a painless, watery diarrhoea that can quickly lead to severe dehydration and death if treatment is not promptly given. About 75% of people infected with cholera do not develop any symptoms. However, the pathogens stay in their faeces for 7-14 days and are shed back into the environment, potentially infecting other individuals. (Times of India 11/4/09) 'Safe' clinical practices unwittingly spur hepatitis B virus (3) London (IANS): Routine clinical practices, presumed safe, could spur patient-to-patient transmission of hepatitis B virus (HBV), one of the most lethal of its kind. A review of 33 HBV outbreaks has shown that the most frequent HBV transmission routes are administration of drugs using multi-vial compounds and capillary blood sampling (e.g. for glucose monitoring) using non-disposable devices. Simone Lanini led researchers from the Istituto Nazionale per le Malattie Infettive Lazzaro Spallanzani, Rome, who performed a systematic review of HBV outbreaks published between 1992 and 2007 within the European Union and the US. Lanini said HBV remains an important cause of liver disease in developed countries. Moreover, the virus has long been recognised as one of the most insidious viral agents within health care settings. The authors included 30 papers in their review, featuring information on 33 HBV outbreaks, involving 471 patients and 16 fatal cases. Sixteen out of the 33 outbreaks were from EU countries; the remaining 17 outbreaks were from the US. There were no significant differences in the main epidemiological parameters between the two areas. An epidemiological study is a statistical study on human populations, which attempts to link human health effects to a specified cause The majority of the outbreaks originated among patients already affected by one or more underlying conditions causing some degree of immuno-depression. "Firstly, we found that dialysis units accounted for the highest number of outbreaks (10 out of 33)" said Lanini, according to an Istituto Nazionale release. The authors conclude: "We have found that several breaches in infection control measures, related to some routine clinical practices thought to be risk-free (e.g. point of care blood glucose monitoring or preparation and administration of common parenteral drugs with multi-vial compounds) could result in patient-to-patient transmission of HBV." (The Hindu 13/4/09) WHO team reviews implementation of TB programme (3) SALEM: A six-member team from World Health Organisation (WHO) reviewed the implementation of Revised National Tuberculosis Control Programme at Salem Government Medical College Hospital and various other parts in the district on Friday. The team led by Haileyesus Getahun comprised Billy Stewart, Sangeeta Kaul, Puneer Dewan, Chen-Yuan Chiang and Rahul Thakur. The team members inspected facilities for the treatment of tuberculosis, interacted with doctors, paramedical staff and patients and discussed diagnosis, prevention and control measures. They advised doctors to act cautiously while treating patients. The team also visited some primary health centres and private hospitals which offer treatment for tuberculosis. Team members said they would submit a report based on the inspections. Based on the recommendations, the country might be able to get more financial assistance for the implementation of the programme. The team would also inspect primary health centres and hospitals in Namakkal and Nagapattinam districts shortly. (The Hindu 18/4/09) Global warming responsible for rising infections: study (3) PUNE: A recent study by city-based environmentalists shows perceptible rise in infectious diseases despite relative improvement in hygiene and potable water supply. They attribute this rise to global warming and subsequent change in climate. The study is based on the data of patients suffering from infectious diseases like diarrhoea and tuberculosis at a sub-district government hospital in Solapur district. It says that despite improvement in sanitation and quality of potable water over the years, occurrence of diarrhoea (a water-borne disease) has gone up by 43 per cent in this part of the district. "Many of the patients studied actually belong to villages which were awarded Gadge Maharaj Gram Swachhata Abhiyaan' and Jal Swachhata Abhiyaan' prizes for improving and maintaining hygiene in the village," said Amar Dhere, assistant professor in enviornmental science at the department of environment science of Indira College of Commerce and Science. "Many studies reveal that climate change and rise in temperature are among the most common causes for outbreak of infectious diseases. In India very less work has been done to explore the relation between the two. Our study done over the period of six years from 2000 to 2006 clearly indicates that despite improvement in living conditions, the outbreak of diarrhoea, instead of coming down, has increased by 43 per cent. This clearly shows the impact of global warming on human lives," said Dhere. Similarly, occurrence of tuberculosis (an infectious viral disease) has also gone up by 37 per cent during the same period. "Increasing patients of diarrhoea and TB are indicators of global warming which is not only affecting metropolitan population but also those living in towns and villages," said Dhere, who headed the study team. Substantiating his point, Dhanraj Patil, assistant professor in sociology at the Yashwantrao Chavan Academy of Development Administration (Yashada) said that the London School of hygiene and tropical medicine has also stated that outbreak of diarrhoea will continue till the global temperature continues to rise. "They also underlined that even afer providing clean drinking water and sanitation facilities in developing countries, diarrhoea cases are constantly on rise," said Patil. Our study is in congruence with the research done by the London School of hygiene and tropical medicine, he added. It is difficult to find a direct relationship between infectious disease and global warming. "At present, researchers are reviewing past studies and trying to establish a relationship between infections and global warming," said Dhere. Elaborating on the methodology of the study, Dhere said, "We collected the data of patients suffering from diarrhoea and TB from government sub-district rural hospital at Akluj in Solapur. This hospital covers three tehsils namely Malshiras, Madha, Sangola. Patients admitted with diarrhoea during 2000 to 2006 were studied," said Dhere. The data was analysed with statistical techniques such as frequency, mean, median and standard deviation. Confirming this, physician Radheshyam Lahoti said, "Many scientists are now convinced that ecological disruption, dramatic environmental change and poor handling of human and animal waste play an important part in spread of infectious diseases." (Times of India 23/4/09) Poor dalit woman dies inside CSMMU for want of proper treatment (3) LUCKNOW: In stark contrast to Mayawati government's claims of dalit emancipation, a dalit woman died writhing in pain near the gate of state's only medical university named after the dalit icon, Chhatrapati Shahuji Maharaj. There were reports that despite orders to provide treatment to her, doctors in CSMMU did not admit her. The woman, who died late on Sunday night, had been reportedly persuading for her treatment for the last three weeks. Gyanti Devi, 27, a dalit woman hailing from Mahdipatti village, Azamgarh was brought to CSMMU nearly three weeks ago by her husband, Harish Chandra. The man reportedly contacted a senior professor, who also belonged to his native district for helping him in arranging treatment for his wife. The professor used his connections to help the ailing woman. Gyanti was seen by doctors at the gynaecology department where she was diagnosed cervix cancer and referred her to the radiotherapy department. The doctors advised a series of tests including biopsy for which she had to rely on private labs, it being a drain on her little savings. Later, the doctors at Radiotherapy refused to admit her claiming non-availability of bed. After much persuasion, the doctors relented claiming that she will be admitted on Monday. But Gyanti Devi died of acute pain on the road inside CSMMU campus on Sunday night. "The radiotherapy department then asked us to go for number of pathological tests. After giving samples at pathology department, we went back to our village and came back on April 10. However, though tests confirmed cancer, doctors refused to admit my wife saying that there was no vacancy. We took shelter under `rain basera' and on Sunday night she died," Harish told TOI. He said that even the request made by the senior professor known to me failed to move hospital authorities. Sources said that apart from radiotherapy department, the woman could have been admitted in a special ward in gynaecology department. There are standing orders of the government and the CSMMU vicechancellor that no patient will be denied admission but Gynati's case shows that doctors care little for directions. When informed about the matter, vice-chancellor, Prof Saroj Chooramani Gopal said she would order a probe into the matter. "This is the height of insensitivity and the wrong-doers will not be spared," she told reporters. (Times of India 23/4/09) India issues travel advisory in wake of swine flu epidemic (3) NEW DELHI: As the Union health ministries' high-level meeting on swine flu outbreak ended on Monday, the government issued a travel advisory, asking Indians to restrict visits to Mexico, US, Canada, New Zealand and France. The health ministry called experts from National Institute of Communicable Diseases and Indian Council of Medical Research in the meeting to chalk out preliminary containment measures if the virus springs up in Asian countries. To ensure public safety, all travellers flying into India from Mexico, US, Canada, New Zealand and France would be individually checked for flu symptoms - like fever and upper respiratory tract infection. All passengers arriving from Mexico will especially be tested as fear gripped India over the spread of the killer virus across the world. At the meeting, it was decided that two doctors each will be stationed at 6 airports of Delhi, Mumbai, Kolkata, Chennai, Bangalore and Goa to check all passengers. Health officials have also been asked to locate all passengers who came into the country from Mexico in the last 10 days. Doctors will visit their local addresses for complete check-up. India has stockpiled 1 million doses of “Tamiflu” -- the only medicine that could be effective. Four labs will be set up in Delhi, Pune, Kolkata and Dibrugarh to test suspected human samples of swine flu. An official told TOI, "In case any passenger shows symptoms, we already have a quarantine centre at the international airport. We also have Delhi government's infectious disease hospital. During SARS, we had created isolation facilities in Safdarjung hospital and RML. We will take action only after WHO instructs us. At present, they have designated the outbreak as Phase III animal to human transmission. They have declared the outbreak as a public health concern and a disease that merits international health regulations. Countries will have to report in case a case of infection is reported within its borders." Human to human transmission of the virus is designated by World Health Organisation (WHO) at a phase IV level. More than 100 people in Mexico are believed to have died from the new flu and more than 1,600 sickened, prompting widespread school closures and other measures in the country. WHO DirectorGeneral Margaret Chan on Sunday said the outbreak had ``pandemic potential'' and held teleconferences with staff and flu experts around the world. She urged governments to step up their surveillance of suspicious outbreaks. Officials around the world are aacing to contain the swine flu outbreak as potential new cases were reported from New Zealand, Hong Kong and Spain, raising concerns about the potential for a global pandemic. China and Russia have set up quarantine centres for anyone possibly infected. In the United States, at least 11 cases of swine flu have been confirmed. Canada's chief public health officer Dr. David Butler-Jones said six cases had been confirmed there, and all had links to people who had travelled to Mexico. (Times of India 27/4/09) WHO focus on vivax malaria control (3) NEW DELHI: Ways of effectively controlling vivax malaria are at the centre of this year’s World Malaria Day activities in the WHO South-East Asia and Western Pacific Regions.Representatives from the Democratic People’s Republic of Korea, India, Indonesia, the Republic of Korea and Sri Lanka met here recently to discuss ways of containing the spread of vicax malaria. Plasmodium vivax causes malaria symptoms and relapses. Patients infected with this parasite suffer frequent relapses (mainly of fever) within one to three years of a single inoculation against parasites from mosquito bites. Though vivax malaria is not absolutely fatal and the parasites usually cause mild symptoms, compared to the “killer” Plasmodium falciparum, prevalent in sub-tropical Africa, recent evidence from India indicates that it occasionally causes severe manifestations and even death. Dr. Samlee Plianbangchang, Regional Director of the WHO South-East Asia Region, said: “Malaria in Asia is different from malaria in Africa. Vivax malaria is less known and we need to understand more about its epidemiology and control interventions.” The years 2000-2010 are a decade of “Roll Back Malaria.” (The Hindu 29/4/09) Swine flu spreads in 10 US states, Europe (3) WASHINGTON (AP): Virulent swine flu spread to 10 U.S. states from coast to coast on Wednesday and swept deeper into Europe, extending its global reach as the U.S. was hit with the first flu death outside of Mexico _ a Mexican toddler who had traveled with his family to Texas. Total American cases surged to nearly 100. The World Health Organization said the outbreak is moving closer to becoming a full-scale pandemic. But in Mexico City, the mayor said the outbreak there seemed to be stabilizing. Dr. Keiji Fukuda, WHO's top flu expert, told reporters in Geneva that the latest developments are moving the agency closer to raising its pandemic alert to phase 5, indicating widespread human-to-human transmission. That's just one step below level 6, a full-fledged pandemic. In Washington, Homeland Security Secretary Janet Napolitano was questioned closely by senators about whether the U.S. should close its border with Mexico, where the outbreak apparently began and the casualties have been the greatest, with more than 150 deaths. She repeated the administration's position that questioning of people at borders and ports of entry was sufficient for now and said closing borders ``has not been merited by the facts.'' Dr. Richard Besser, the acting chief of the Centers for Disease Control, said in Atlanta that there are confirmed cases now in ten states, with 51 in New York, 14 in California and 16 in Texas, where officials said Wednesday they were postponing all public high school athletic and academic competitions until May 11. Two cases have been confirmed in Kansas, Massachusetts and Michigan, while a single cases have been reported in Arizona, Indiana, Nevada and Ohio. State officials in Maine said laboratory tests also had confirmed three cases in that state, although those had not yet been included in the CDC count. In a possible outbreak north of the Mexican border, the commandant of the Marine Corps said a Marine lieutenant in southern California might have the illness and 39 Marines were being confined on their California base until tests come back. Marine General James Conway told a Pentagon briefing an initial test indicated the sick Marine _ who was not identified _ might have swine flu but his illness did not appear life-threatening. President Barack Obama said he wanted to extend ``my thoughts and prayers'' to the family of a nearly two-year-old Mexican boy who died in Houston, the first confirmed U.S. fatality among more than five dozen infections. Health officials in Texas said the child had traveled with his family from Mexico, to Brownsville on April 4 and was brought to Houston after becoming ill. He died Monday night. ``This is obviously a serious situation,'' and ``we are closely and continuously monitoring'' it, Obama said of the spreading illness. Laboratory testing shows the new virus is treatable by the anti-flu drugs Tamiflu and Relenza, and the first shipments from a federal stockpile arrived Wednesday in New York City and several other locations in the U.S.. The government was shipping to states enough medication to treat 11 million people as a precaution. Meanwhile, Egypt's government ordered the slaughter of all pigs in the country as a precaution, though no swine flu cases have been reported there. Egypt's overwhelmingly Muslim population does not eat pork, but farmers raise some 300,000-350,000 pigs for the Christian minority. The disease is not spread by eating pork, and farmers were to be allowed to sell the meat from the slaughtered animals. In fact, officials appeared to go out of their way on Wednesday to not call the strain ``swine flu.'' Obama called the bug the ``H1N1 virus.'' ``The disease is not a food-borne illness,'' Rear Adm. Anne Schuchat, CDC's interim science and public health deputy direct, told the Senate Homeland Security Committee. She said the strain is particularly worrisome because ``it's a virus that hasn't been around before. The general population doesn't have immunity from it.'' People have various levels of protection against other more common types of flu because they are exposed to it over time, and that protection accumulates. She suggested that some older people might have more resistance to this particular strain than younger people because its traits might resemble outbreaks of decades ago. Germany became the latest country to report swine flu infections. It reported four cases on Wednesday. New Zealand's total rose to 14. Britain had earlier reported five cases, Spain four. There were 13 cases in Canada, two in Israel and one in Austria. Obama said it is the recommendation of public health officials that authorities at schools with confirmed or suspected cases of swine flu ``should strongly consider temporarily closing so that we can be as safe as possible.'' He was underscoring advice that the CDC provided earlier to cities and states, and that some schools _ most prominently in New York City _ already have followed. ``If the situation becomes more serious and we have to take more extensive steps, then parents should also think about contingencies if schools in their areas do temporarily shut down, figuring out and planning what their child care situation would be,'' Obama advised. He advised people to take their own precautions _ washing hands, staying home if they are sick, and keeping sick kids home. (The Hindu 1/5/09) Concern over an Act lying dormant for 13 years (3) CUTTACK: After about 13 years of enactment of a Statute that aimed at providing safety, health and welfare measures to millions of building and construction workers, top judicial and administrative officials gathered here on Saturday to deliberate as to why the Act could not be implemented till date. After a daylong thought-provoking deliberation in two sessions of pondering, it was decided that all stakeholders would work towards sensitising the construction workers who are not affluent about the Act. The Building and Other Construction Workers’ (Regulation of Employment and Conditions of service) Act was enacted way back in August 1996, but due to alleged insensitiveness, the statute aimed at doing away with the miseries of one crore construction workers has not yet been implemented in the country, rued senior Supreme Court judge Justice Arijit Pasayat. (The Hindu 3/5/09) People with HIV more vulnerable to H1N1 flu (3) NEW DELHI: Patients suffering from HIV are at an increased risk from the deadly H1N1 flu virus. According to World Health Organisation, infection with the flu virus may have a more serious impact on people with immuno-deficiency diseases compared to otherwise healthy individuals. What's more worrying is if the two viruses -- HIV and H1N1 -- mix in the environment, much like what's happened with HIV and tuberculosis. Even people with heart disease, asthma and diabetes may face an increased risk of serious influenza-related symptoms. The WHO advisory should come as a serious warning for India which is home to an estimated 2.5 million HIV infected people -- third only to South Africa and Nigeria in the total number of cases. Guidelines issued by CDC Atlanta recently say, "It is known that adults and adolescents with HIV infection, especially persons with low CD4 cell counts, are at higher risk for viral and bacterial lower respiratory tract infections and for recurrent pneumonias." "Because adults and adolescents infected with HIV experience more severe complications of seasonal influenza, it is reasonable to assume that they are also at higher risk for H1N1 influenza complications." Reacting to a question on what a H1N1 outbreak's impact could be on HIV patients, WHO's assistant director-general Dr Keiji Fukuda told TOI from Geneva, "The world is made up of groups of people who have different medical conditions. Chronic heart or lung conditions make people more vulnerable to influenza viruses in general." "We also now know that people who have HIV infections can be susceptible to many infections and with influenza viruses HIV infected populations are one of the groups of people who can be somewhat more heavily impacted than people who are healthy. We need to know who are the different groups of people who are going to be disproportionately affected if a pandemic breaks out," Dr Fukuda said. WHO says regular seasonal flu kills between 250,000 and 500,000 such people a year. The apparent spread of the H1N1 influenza virus has many people living with HIV concerned about their health and safety in India. But a health ministry official said while there are reasons to be cautious, there's still no reason to panic. At present, the H1N1 is sensitive to two known drugs, Relenza and Tamiflu, and there is little evidence to suggest that these drugs cannot be safely combined with anti-retrovirals (ARVs) used to treat HIV. The flu medications work much like ARVs -- they prevent the influenza virus from reproducing in the body. According to WHO and CDC, people at high risk of serious influenza-related complications, including people living with HIV/AIDS, can take Relenza or Tamiflu as post-exposure prophylaxis (PEP) to prevent the flu. However, PEP is only recommended for HIV-positive people who have a known exposure to the virus if a household member is diagnosed with H1N1. Officials said HIVinfected persons should be considered as a high risk and a priority population for preventive and therapeutic strategies against H1N1. WHO recommends that patients at higher risk for complications of influenza should be among those prioritized for antiviral treatment with oseltamivir or zanamivir which shortens illness duration and severity in seasonal influenza. The WHO advises that it is best if people infected with the flu strain start taking the antivirals within 48 hours of the onset of symptoms. Because of the unique vulnerability of people living with HIV (PLWH), it is recommended that they consult the HIV clinical care provider during this heightened alert as a preventative action. If signs and symptoms of flu do occur, the PLWH should contact the HIV clinical care provider immediately, WHO says. (Times of India 7/5/09) TB, malaria rampant in commercial sex market in NE (3) GUWAHATI, May 7 – It may sound strange but is true. HIV/AIDS is no longer the gravest health hazard in the commercial sex market. Diseases like tuberculosis (TB) and malaria are becoming more rampant in the prostitution market of eastern India, including the North East. This eye-opening revelation has been made by Anindit Roy Choudhury of Sanlaap, a developmental organisation working against trafficking and commercial sexual exploitation of children and women while talking to The Assam Tribune. Sanlaap is a Kolkota-based NGO operating in entire eastern India. The new-found phenomenon has reportedly affected scores of people involved in the trade, especially women sex workers, who are facing untimely death in a frequent manner across the region. “At a time when too much emphasis is being paid on alleviating the menace of HIV/AIDS and other sexually-transmitted diseases, the menace of TB, malnutrition and malaria has started wreaking havoc,” he said. “Most of the brothels lack basic health and hygiene requirements — be it in terms of keeping the surroundings hygienic or having access to nutritious food, which has led to such a menace,” he divulged. Apart from TB, malaria and malnutrition are the other diseases, which are increasingly hitting the commercial sex workers. “Even the figures stated by the World Health Organisation indicated that TB has caused more deaths and so it is high time for the health organisations, NGOs and the Government to focus on these issues,” Arijit said. “In the North east where there are no red-light areas, and room-based prostitution is more prominent more so in the slum areas, the authorities and the activists have an uphill task in actually reaching out to those engaged in prostitution,” he said, calling for a mass campaign targeting the marginalised population. “Extra effort is needed on the part of the Government, which would now have to pump in more funds to alleviate these health issues,” he pointed out. Hasina Kharbih of Impulse, an NE-based NGO, while endorsing the statement of Arindit, said that most of the rescued victims are found affected by such diseases and there is a need to introduce a holistic approach to address the issue. “The problem here in Assam and Dimapur where street-based prostitution is more prominent, things should dealt with more effectively,” she further stated. (The Assam Tribune 7/5/09) 'Rising maternal & infant mortality rate worry' (3) KANPUR: Indian Academy of Paediatrics in joint effort with department of paediatrics, Ganesh Shankar Vidyarthi Memorial (GSCM) Medical College observed the `World Health Day,' keeping in mind `women and children and their welfare,' on Tuesday. Other issues highlighted during discussion by various organisation were to save lives - make hospitals safe in emergencies, preparedness of health institutions and hospitals for handling emergency situations. Issues of women and children, stigma attached to society like female foeticide, gender discrimination, early marriage which have been instrumental in poor health of females. There is need of programmes to check the increasing maternal and infant mortality rate in the country, emphasised professor and HoD paediatrics GSVM medical college, Dr VN Tripathi. The introduction of the anti-cancer vaccines for the females was also discussed. The maternal mortality rate in India is comparatively higher than western countries, it is 600 per 1 lakh population against the US and UK countries where the maternal mortality rate is 10 per 1 lakh population, a cause of concern. Meanwhile, at another public awareness and quality improvement programme organised at Indian Medical Association (IMA) it was pledged to provide medical facility to all in need of emergency. "Efforts are to make zonal teams of doctors available for the needy in their respective areas. Our efforts will to be to provide mother and child birth services and immunisation facilities affordable to all," assured the IMA members. (Times of India 8/5/09) P-1 virus detected in Saharsa district (3) SAHARSA: The polio eradication programme here suffered a severe jolt with the detection of one P-1 virus in Kathdumar village under Simri Bakhtiyarpur block of Saharsa district. The district administration, health department as well as WHO and UNICEF authorities are once again on their toes as the district has reported the much dreaded virus for the third consecutive year. The victim is a 14-month-old girl child, Chandni, daughter of Kapileshwar Sada. Recently, she developed some trouble in her limbs and the stool test report confirmed that she is a P-1 positive case. Talking to TOI on Friday, civil surgeon Dr Ajad Hind Prasad said that one P-1 case was detected in Mahishi block in 2007 while another in 2008 in Salkhua block of the district. Ironically, the flood-ravaged Kosi region remains the only area in Bihar where P-1 cases have been discovered in 2009 so far. Incidentally, polio cases are being discovered despite the much-publicised immunisation programme. The civil surgeon also admitted that the latest case came to light despite the fact that the girl child had been administered 11 doses of polio drops. (Times of India 10/5/09) Drop in infant mortality rate in the country (3) NEW DELHI: The infant mortality rate (IMR) in the country went down by two percentage points from 57 to 55 per 1,000 live births between 2006 and 2007. While the overall figure has shown a decrease, the number has gone up in Chandigarh, Uttarakhand, the Andaman and Nicobar Islands and some northeastern States, according to the latest figures released by the Registrar-General of India as per the Sample Registration System (SRS). The IMR has gone up from 23 to 27 per 1,000 live births in Chandigarh and from 31 to 34 in the Andaman and Nicobar Islands. In Uttarakhand, the number of children dying per 1,000 live births has gone up from 43 to 48, in Manipur from 11 to 12 and in Meghalaya from 53 to 56. Similarly, the IMR figure has shown an uptrend in Nagaland to 21 from 20 in the previous survey, from 33 to 34 in Sikkim, and from 36 to 39 in Tripura. Strangely, while Manipur has an IMR of 11, both in rural and urban areas, the latest statistics show that the figure has gone up to 13 in rural areas and slumped to nine in urban areas. However, it continues to have the lowest IMR followed by Kerala at 13. The worst performers, despite an improvement, continue to be Madhya Pradesh at 72 followed by Orissa at 71, Uttar Pradesh at 69, Assam at 66 and Rajasthan at 65. The other States whose performance is not so satisfactory are Chhattisgarh (59), Bihar (58), Haryana (55), Gujarat (52) and Jammu and Kashmir (51). The rural-urban divide is also visible in the data. The IMR in rural India is 61, while it is 37 in urban areas. The SRS is a large-scale demographic survey for providing reliable annual estimates of birthrate, death rate and fertility and mortality indicators at the national and sub-national levels. Initiated on a pilot basis by the Registrar-General in a few States in 1964-65, it became fully operational during 1969-70 with about 3,700 sample units. The field investigation consists of continuous enumeration of births and deaths in selected sample units by resident part-time enumerators, generally anganwadi workers and teachers, and an independent survey every six months by SRS supervisors. The data obtained by these two independent functionaries are matched and the unmatched or partially matched events re-verified in the field. The sample unit in a rural area is a village or a segment if the village population is 2,000 or more. In urban areas, the sample unit is a census enumeration block with a population ranging from 750 to 1,000. (The Hindu 13/5/09) 'Globally six lakh women die during childbirth' (3) The right to health is not new. For instance, a number of notable judgments of India's Supreme Court have linked the right to health with the right to life. I believe it is important to take Article 25 of the Universal Declaration of Human Rights and make it very practical. What this means is that we should evolve a system of security for the poorest so that they don't suffer the shocks of illness. The poor pay the most for food, they pay the most for health care. It is possible to set up a system to address this. But why has the right to health remained so under-legislated? Liberal economic philosophy approaches health as a cost, rather than seeing a healthy population as vital for development. It is important that governments recognise the value of health in terms of its contribution to the GDP. One of the great human rights violations, which doesn't get much attention is maternal mortality. In my own country, Ireland, if a mother dies during childbirth, the whole hospital mourns. It is a real tragedy. But globally 6,00,000 women die during childbirth. Recently, a newspaper columnist observed that when Madonna adopts a baby in Malawi, it points to high levels of maternal mortality there. Yes. There are more doctors from Malawi in Manchester, England, than in Malawi. How can you have good medical care under such circumstances? But Malawi is also one of the countries where we have evidence-based work on the effectiveness of midlevel providers, especially trained in emergency obstetric care. Today, they are effectively carrying out the majority of caesarean sections there. You have spoken about the asymmetrical movement of health workers from resource poor to resource rich countries. Take India: 75 to 80 per cent of medical schools here are publicly funded. India has the largest number of doctors of any nation migrating to Organisation for Economic Cooperation and Development (OECD) countries. The US alone has over 50,000. This means there is one Indian doctor available for every 1,325 Americans, but in India there is one doctor for every 2,200 Indians. Inevitably, public health services in rural India are understaffed by over 50 per cent. Of course, we must recognise the human right to migrate to further one's prospects. At the same time we need to address the imbalance this causes. (Times of India 13/5/09) Three more cases of swine flu? (3) HYDERABAD: Three passengers with suspected symptoms of influenza A (H1N1) flu virus were admitted to Government General and Chest Hospital, Erragadda on Wednesday. Throat and nasal secretions, swabs of sputum and serum samples of the three patients have been sent to National Institute of Communicable Diseases (NICD), New Delhi for confirmation. A 23-year old student from Hyderabad, studying in Indiana University, Bloomington, and flying from New York to Hyderabad via Dubai in an Emirates flight, was admitted to the hospital on early Wednesday morning. The patient had symptoms of cough, fever, sour throat and general weakness. The other two persons, both of them on a business trip to United States, reached Hyderabad from New York on Tuesday and after developing flu like symptoms volunteered to get admitted to Chest Hospital. The two had symptoms of cough, cold and sour throat. Both had travelled to California, Texas, Florida and New Jersey before reaching twin cities. The hospital authorities informed that there was no need to quarantine the family members of the both the passengers because they stayed in a guest house after reaching Hyderabad. “They had mild cold when they reached Hyderabad. After a day, the cold became severe,” informed Chest hospital doctor Dr. K. Subhakar. (The Hindu 14/5/09) Second phase of Arogya Kavacha to focus on reducing neonatal deaths (3) Bangalore: To reduce neonatal mortality and also promote institutional deliveries, the second phase of “108 Arogya Kavacha”, to be rolled out by this month-end, will keep track of the expected date of deliveries of all expecting women in rural areas. The State Government had signed a memorandum of understanding (MoU) with the Hyderabad-based Emergency Management and Research Institute (EMRI) for “Arogya Kavacha”, a scheme which provides free emergency services in the public private partnership (PPP) mode in rural and urban areas. As many as 180 ambulances equipped with all medical facilities will be added to the existing fleet of 150, which were pressed into service in the first phase. “Though we have been working towards safe deliveries and safe births, the second phase will focus more on reducing neonatal mortality and also promoting institutional deliveries. Presently, 33 per cent of the emergencies attended to by our ambulances are related to pregnancies,” Bharat C. Radhakrishnan, Chief Executive Officer (CEO) of EMRI told The Hindu. “Though these 150 ambulances are covering all the districts, we know that we have not been able to provide services to the remote areas. The additional ambulances will ensure better coverage,” he said. EMRI was also working along with the State Government towards meeting the goals set under the National Rural Health Mission (NRHM), he added. With 925 young mothers and 1,400 new born babies dying every year, the Directorate of Health and Family Welfare is going all out to reduce the Infant Mortality Rate (IMR) and Maternal Mortality Rate (MMR). “According to the figures released by the Registrar-General of India as per the Sample Registration System (SRS) in 2007, the IMR of Karnataka is 47 per 1,000 births. We have set a goal to reduce it to 30 for 1,000 by 2012. Likewise, the target is to reduce the MMR, which is 220 for every 1,000 to 100 by 2012,” Health Commissioner P.N. Sreenivasichari said. Pointing out that neonatal mortality was the major contributor for IMR, he said about 60 per cent of newborns in Karnataka died within seven days of their birth. “Hence, it has become very important to focus on reducing the neonatal deaths to bring down the IMR,” he told The Hindu from Uttaranchal, where he has been deputed as the election observer for the Assembly byelections. Principal Secretary (Health and Family Welfare) M. Madan Gopal said the plan was to replicate the Maharashtra model of establishing “home-based neonatal care” (HBNC) in rural areas to meet these goals. A team of health officials led by him recently visited Gadchiroli in Mahasrastra last month to study the functioning of a similar system there. The HNBC system, managed by the Society of Education, Action and Research in Community Health (SEARCH), a NGO in Gadchiroli, has contributed towards reducing the IMR of that remote and most backward district considerably, he said. The Government would train the Accredited Social Health Activists (ASHA) trained under NRHM for the homebased neonatal care, he added. (The Hindu 18/5/09) Gift lure to keep moms in hospital (3) Goalpara May 20: A government-funded pack of towels and nappies, the Goalpara administration is hoping, will help persuade new mothers to stay on in hospital for at least 24 hours after delivery — a necessity if the infant morality rate is to be brought down. In impoverished areas where awareness is low, newborns and their mothers often die of infection and lack of care, contributing to an astounding child mortality and post-delivery death rate, which the government has been trying to desperately curb. The simple gift pack, costing Rs 180 each, is part of a scheme being implemented through the District Health Society of which the deputy commissioner is the chairman and is supported by the National Rural Health Mission funds. Goalpara deputy commissioner Anurag Goel recently launched the scheme in Lakhipur and Rangjuli primary health centres — two blocks which have the highest infant and maternal mortality rates. “The first 24 hours are crucial. The newborn could get an infection and the mother could suffer from bleeding. At hospitals, they will be under expert supervision, which will help reduce the infant mortality rate. Our reports suggest that women of these areas leave the hospital within 24 hours of delivery. This stay is a must for the safety of both the child and mother and the gifts are one way of keeping the mothers in hospital,” Goel said. Another important reason to ensure the stay at the hospital is to teach new mothers how to tend to the baby. “Besides ensuring the safety of the mother and child, a woman can also learn how and what to feed the baby, clean the infant and look after its health. In areas where there is poverty and illiteracy, these small things make a lot of difference,” a source in the National Rural Health Mission said. Nine women in tribal-dominated Rangjuli and three in minority-dominated Lakhipur have already received the gifts. The scheme, however, is restricted only to those with two children and who opt for institutional delivery. Though the exact mortality rates in the district are not available, Assam has a maternal mortality rate of 490 per lakh and an infant mortality rate of 66 per thousand. A source in the National Rural Health Mission said this new plan had been put on hold because of the parliamentary elections. “The concept paper was submitted to Dispur in January. The health department is very supportive and if everything goes well, it will be replicated in all the 27 districts of the state,” the source said. (Telegraph 21/5/09) Death of young children down a third since 1990: WHO (3) New York (PTI): Death of children under five years of age have plummeted by almost one third since 1990, the U.N. health agency said today, while cautioning that greater action is necessary to achieve similar success in other areas, in particular maternal and newborn health. Some 9 million children under the age of five died in 1997, marking a sharp decline from the 12.5 million estimated to have died in 1990, according to "World Health Statistics", a first progress report by World Health Organisation (WHO) on the health-related MDGs — the eight globally-agreed anti-poverty targets with a 2015 deadline. "The decline in the death toll of children under five illustrates what can be achieved by strengthening health systems and scaling up interventions, such as insecticide-treated mosquito nets for malaria and oral rehydration therapy for diarrhoea, increased access to vaccines and improved water and sanitation in developing countries," said Ties Boerma, Director of WHO's Department of Health Statistics and Informatics. But the new study, which is based on over 100 health indicators collected from WHO's 193 Member States, cautioned that in many African nations and in low-income countries, the fourth MDG — slashing child mortality by two-thirds — may not be met. Mr. Boerma said that while encouraging progress has been made at the half-way point to the 2015 deadline, "there needs to be more effort to strengthen health systems in countries affected by high levels of HIV/AIDS, economic hardship or conflict." Additionally, he called for greater attention to be paid to the poorest groups within countries where progress is slowest and child mortality remains high. Maternal and newborn health has seen almost no improvement, Mr. Boerma said, with nearly 40 per cent of deaths among children under five occurring in the first month, even first week of life. "While the data are patchy and incomplete, it appears that the regions with the least progress are those where levels of maternal mortality are highest." Boosting these rates will involve addressing weak health systems, emerging health threats such as pandemics, and climate change, he added. (The Hindu 22/5/09) Gehlot lays emphasis on health care schemes (3) JAIPUR: Rajasthan Chief Minister Ashok Gehlot has called for immediate steps to reduce maternal and infant mortality ratios, execute heath care services and develop urban infrastructure and resources to benefit large sections of population. Presiding over two separate review meetings here over the weekend, Mr. Gehlot said while the health care schemes should benefit the people at the grassroots, the urban development schemes should aim at empowering the local bodies to enable them to improve the quality of life of city dwellers. Mr. Gehlot reviewed the progress of the Rajasthan Health System Development Project, National Rural Health Mission and medical education while observing that the Rajiv Gandhi Mobile Units arrangement should be strengthened to provide timely medical services in the remote areas. The Chief Minister underlined the significance of Janani Suraksha Yojana for safe institutional deliveries and issued instructions for supply of 5 kg of desi ghee to women after delivery as promised in the State Assembly election manifesto of the ruling Congress. For the expansion of urban infrastructure, Mr. Gehlot said proper arrangements should be made in the cities for parking and flyovers and railway over-bridges constructed while taking steps for conservation of cultural and architectural heritage. Mr. Gehlot said the urban local bodies should be evolved as agencies responsible for implementing the civic laws and added that a Heritage Development Authority would be established shortly in the State. He said new townships would be developed at the barren and unproductive land situated away from the existing towns. (The Hindu 2/6/09) Azad promises help to Kerala for prevention of fever outbreak (3) New Delhi/Kochi: Union Health Minister Ghulam Nabi Azad on Tuesday assured full support to the Kerala Government to prevent the outbreak of fever in Alappuzha district and other areas. He said the Central Government was ready to send an expert team to the State. The Union Government could provide more aid to help prevent fever outbreak after receiving intimation from the State Government, he said. As per the reports the Centre was receiving now from Kerala, the situation did not warrant the assigning of an expert team to Kerala, he said. However, the Centre would indeed send a team if the situation worsened, he added. Azad said certain long-time measures were necessary to prevent the outbreak of diseases in the Alappuzha region. He was speaking to the media after holding talks with Kodikunnil Suresh and KC Venugopal, MPs from Mavelikkara and Alappuzha respectively. The waterlogged region had reported several cases of cholera in the just started monsoon season. The increasing number of cholera cases had raised concerns about the public water supply system in the region. Though water-logged, drinking water had been a major dilemma for residents here, with the lake and river water hardly fit for consumption, due to salinity.At the same time, reports on Tuesday from different areas in Alappuzha district, especially the Alappuza town and the water-bound Kuttanad, suggested that viral fevers and cholera were spreading without cease. Eleven persons had o far confirmed to have contracted cholera while reports put the number of persons dead due to the disease between two and four. According to official sources, only two persons had contracted chikungunya in Alappuzha district, but voluntary health workers disputed this. As per the estimates of the Health Department, the number of fever-hit persons in the district was about 17,000 but health workers pointed out that this did not include the patients approaching private medical facilities. Even on Tuesday, more than 900 persons with symptoms of viral fevers approached various hospitals seeking medical assistance. The Health Department estimates showed that the State had a total of 70,000 viral fever cases presently, but officials said there was no reason for apprehensions as such fevers were normal at the start of monsoon. They said the incidence of fatal fevers like dengue was miniscule. Meanwhile, Health officials in Pathanamthitta, Kottayam, Kozhikode and Kasaragod districts said the fever situation had come under control. There had been a drop in the number of patients reaching medical facilities this week compared to last weekend, they said. Viral fevers had spread through villages in the hilly areas of Pathanamthitta, Kottayam, Kozhikode and Kasaragod districts. Reports of spread of rain-related communicable diseases had come from the coastal areas of Kollam, Ernakulam and Thrissur areas also. However, the district administration authorities in Ernakulam said that the incidence of fevers would come down in the coming days as the cleanliness and disease-prevention measures had now been implemented in full measure. At the same time, reports from Thiruvananthapuram said that one more person had died of Weil’s disease in the district. With this death, the number of deaths due to contagious diseases in the district rose to six, reports said. Apart from chikuingunya and dengue, malaria also had been reported from the rural areas of Thiruvananthapuram district. Health officials in Idukki asked people of the district not to fall into panic on the basis of the media reports about incidence of malaria. They said some cases of suspected malaria had been found in the district but assured that all measures had been taken to prevent its spread. Earlier reports had said that 18 cases of malaria had been found in Idukki, including a 12-year-old boy. This had created panic in the area as none of these persons had gone out of the State in a long time, which suggested that the disease had become endemic. Doctors also said that the disease could have arrived here through migrant workers from States like West Bengal and Bihar. (Pioneer 3/6/09) Four more suspected cases of swine flu in Coimbatore (3) Coimbatore, Jun 3 (PTI) Four more persons, including a lady doctor, suspected to be infected with swine flu, have been admitted to a government hospital here, even as officials made efforts to contact air passengers who travelled with the two confirmed flu patients on May 28. The doctor, who is treating two confirmed flu patients at the hospital, has developed fever and throat pain last evening. Her blood samples have been sent to the National Institute of Communicable diseases, Delhi, Dr Kumaran, Dean (incharge) of hospital told reporters here. Meanwhile, three members of a family--husband, wife and daughter, who returned from Atlanta to Coimbatore this morning also have been admitted for suspected flu symptoms, Kumaran said. Blood samples of the three would be sent to Delhi today, he said. A 34year-old woman and her five-year-old son, who had come from United States to Coimbatore on May 28, had tested positive for the H1N1 virus. They have been kept in a quarantine ward at the Coimbatore Government hospital. PTI (PTI 3/6/09) What is H1N1 (swine) flu?Influenza A H1N1 (3) Influenza A H1N1 is a contagious respiratory disease of pigs caused by type A strains of the influenza virus. The virus enters the human body through inhalation of contaminated droplets or transfers live virus from a contaminated surface to the eyes, nose or mouth of a person. It takes 3 to 5 days for symptoms to develop and it continues for nearly a week. One can pass the infection to others for nearly 8 days after getting infected* Symptoms Fever, Cough, Body ache, Chills, Sore throat, Acute gastrointestinal symptoms like vomiting, diarrhoea and nausea * See a doctor if you: Have the above mentioned symptomsHave visited an area where H1N1 flu cases have been reportedHave come in contact with a person with flu like symptoms and develop respiratory discomfort. High risk groups. Old people, People with pre-existing diseases like diabetes, kidney problems etc Cancer patients, HIV+ and AIDS patients and all immuno-compromised patients, * Treatment, H1N1 flu is sensitive to oseltamivir (Tamiflu) and zanamivir (Relenza). But these medicines should be taken under medical supervision. Over-the-counter sale of these drugs is banned in India* Precautions, Maintain oral and personal hygiene, If you eat pork, it should be well-cooked, Wash your hands before eating anything* Number of cases reported so farCountries affected: 73Confirmed H1NI cases worldwide: 25,288Deaths reported worldwide: 139 (Times of India 9/6/09) Infant mortality rate declines in Bellary (3) BELLARY: The infant mortality rate (IMR) has been on the decline in Bellary district with the number of institutional deliveries going up ever since the National Rural Health Mission (NRHM) was implemented in 2006. The IMR in the district, which was 36.93 for every 1,000 live births in 2003-04, has come down to 22.37 in 2008-09. As many as 52,121 deliveries took place in government health institutions during 200809 of which 51,009 live births have been reported. Even with regard to the Maternal Mortality Rate (MMR), the district recorded 1.23 deaths for every 64 deliveries out of as many as 52,121 deliveries in 2008-09, Jaikumar, District Health Officer, told The Hindu. He said that the main focus of the NRHM was to bring down the IMR and MMR by persuading women to opt for institutional deliveries. Apart from introducing several schemes such as the Janani Suraksha Yojana and Madilu, the department improved infrastructure at government health centres in rural areas by making them function round-the-clock. The required staff has also been appointed to attend to the postnatal health requirements of women. “As a result, the number of institutional deliveries went up and is now 49.76 per cent for this year. Of the 52,121 deliveries reported in the district during the previous year, around 50 percent (25,935) were carried out at government as well as private hospitals. The percentage of women in the district opting for institutional deliveries stood at 42.91 and 37.21 during 2007-08 and 2006-07 respectively,” he added. Following is the taluk-wise details of deliveries, live births, IMR and MMR respectively — Bellary (16,707), (16,394), (348) and (27); Sandur (5,192), (5,094), (139) and (03); Siruguppa (6,070), (5,894), (144) and (02); Hadagali (3,667), (3,596), (77) and (05); Hospet (10,280), (10,018), (193) and (15); Hagari Bommanahalli (4,474), (4,360), (137) and (06); and Kudligi (5,731), (5,653), (103), and (06). Dr. Jaikumar said that of the 54 public/community health centres in the district, 35 had been functioning round-the-clock and eight more centres would be asked to observe that schedule from this month. (The Hindu 10/6/09) Alarming rise in infant, maternal mortality rates, finds civic body (3) Ahmedabad: The city has seen an alarming rise in infant and maternal mortality rates as per the latest report compiled by the Ahmedabad Municipal Corporation (AMC). This is contrary to the records of the last five years with the AMC. Also, it is contrary to the state government records that claim that both the mortality rates have been contained. AMC officials say there is nothing wrong with the statistics and that there is nothing to be scared of or have ideas about the system. They say that surveys done so far were based only on figures available with four government hospitals; but for the last one year or so, deaths at home have also been included. This, they say, is the reason behind the phenomenal rise in the two vital mortality figures. So far, delivery at home was not taken into account and therefore, the figures were low. But now, with the inclusion of this segment, the data is near accurate, said the officials. There is no explanation as to why such an important marker (home delivery) was not included in the data earlier. (Indian Express 11/6/09) India reports three more swine flu cases, total 15 (3) NEW DELHI: With three more H1N1 influenza cases being reported on Thursday, two from Delhi and one from Goa, India now has 15 confirmed infections of swine flu. Five of these patients are from the capital. Both new cases reported from Delhi were those of women who had recently returned from New York. A senior official at the National Institute of Communicable Diseases (NICD) told TOI: ``The samples of these two women have tested positive and we have sent these for a second confirmatory test to National Institute of Virology (Pune).''A 41-year-old woman, who had visited Haiti and had came to India via New York, was admitted to the isolation ward at Ram Manohar Lohia (RML) Hospital on Wednesday. ``She was brought straight from the airport and her sample was sent to NICD for testing. She tested positive and has been kept in the isolation ward. We have given her Tamiflu and are monitoring her condition at regular intervals,'' said Dr N K Chaturvedi, medical superintendent, RML Hospital. The other confirmed case is that of a 28-year-old woman, who lives in south Delhi and had travelled from New York. She was admitted to Lok Nayak Hospital on Wednesday night. ``She had called our helpline and told us about her deteriorating health. A team of doctors went to her place and collected the sample, which was sent to NICD for testing. She has tested positive for H1N1 infection and we later got her admitted to Lok Nayak Hospital,'' said J P Singh, principal health secretary, Delhi government. Meanwhile, swine flu made its entry in Goa, when a 41-year-old man from south Goa tested positive for the virus and another suspected case surfaced in north Goa. State health officials said the infected man's blood sample had been sent to Delhi and Pune for re-confirmation. The man, who had recently arrived from London via Germany, was being kept in the isolation ward of the Chicalim Cottage Hospital. A 35-year-old woman arriving in Goa from Sharjah was stopped at the airport for flu-like symptoms. She is being tested for the virus. The samples of a French national, who had travelled to several countries and was in Hyderadad last Thursday, and the father of the 17-year-old NRI student from Boston have tested negative for the H1N1 infection. ``We discharged the Frenchman — with his reports negative for H1N1 infection — after giving him prophylactic treatment,'' said Dr Chaturvedi. The middle-aged man and his 60-year-old mother, who were the first human-to-human transmission case reported in the Capital, refused to get admitted to RML Hospital despite the strong advisory given by the city health department on Wednesday night. According to NICD officials, ``The son tested negative on Thursday as he has been on prophylactic treatment. But the mother is still positive.'' Meanwhile, Delhi health minister Prof Kiran Walia appealed to people not to panic. Hinting at the mother-son duo, who despite being infected refused to get admitted, Prof Walia said ``it is mandatory for swine flu patients to get admitted as our hospitals are well-equipped. The person suffering from H1N1 infection should not be allowed to stay at home.'' (Times of India 12/6/09) Malaria claims 17 lives in Mizoram (3) AIZAWL, June 11 – Seventeen people died of malaria during January to April this year in Mizoram, a Health department statement said here today.The statement said that the death toll during January to April surpassed last year's figure of seven by ten during the same period. April this year witnessed the highest malarial death toll as eight persons fell pery to the disease transmitted through the bite of female mosquitoes. Hospitals and health centres across the state, which tested 27,682 blood samples found as many as 893 positives out of which 615 were identified as positive malaria PF (plasmodium falciparum), the statement said. The Health department urged the people to take utmost preventive measures during the onset of monsoon as monsoon brings more pandemic malaria cases from almost all over the state and also asked the public to make maximum use of the 1,283 Drug Distribution centres from where malaria drugs are distributed to the affected people free of costs. – PTI Assam Tribune 12/6/09) 2.86 lakh incoming passengers screened for A(H1N1) flu (3) CHENNAI: Only two cases of A(H1N1) flu have been confirmed since the health authorities launched a 40-day-old vigil against the A (H1N1) virus during which over 2.86 lakh incoming passengers were screened at international airports and ports, Health Secretary V. K. Subburaj said. Addressing reporters on the sidelines of a function to launch a diabetes-tuberculosis prevention programme, Mr. Subburaj said no case of domestic A(H1N1) flu was reported in the State. All the 15 suspected cases to be quarantined and kept under observation so far were from the US. Patients reporting at the airport here with symptoms of flu are being quarantined at the airport and later referred for observation to the Communicable Diseases Hospital in Tondiarpet and kept there until the results of blood sample tests are received from the National Institute of Communicable Diseases, New Delhi. The two confirmed cases reported from Coimbatore were also passengers from the US. Health authorities are expecting by Monday the test result of the blood sample of a five-year-old girl who showed signs of flu on arriving in Chennai. All five members of the family will be under a 48-hour surveillance. The Health Secretary said there was no need to panic as there was no significant A(H1N1) flu pandemic threat in the State. Even the patients who tested positive for the A (H1N1) virus at the Coimbatore Government Medical College were treated and discharged from hospital after five days, he said. “Nevertheless, we are not lifting guard and round-theclock vigil will continue at the airports in Chennai, Tiruchi and Coimbatore as well as in key ports in Chennai and Tuticorin,” Mr. Subburaj said. The Health department has been instructed by the Government of India to mobilise itself to ensure that not a single A(H1N1) flu case gets past the surveillance net. It has trained and deployed 100 health workers at the three airports in the State. Airport authorities too have mobilised special masks and other personal protection equipment and medicines for the benefit of passengers. (The Hindu 15/6/09) Malaria kills more people than Maoists in Orissa (3) BHUBANESWAR: Killings by Maoists in Orissa attract a lot of attention, but malaria claims many more lives in the remote villages across the state and not much note is taken of them. Official sources said as many as 1255 people succumbed to malaria during the past 5 years, while 133 people became victims to Maoist violence in the state. Home department reports said during 2004-08 at least 49 civilians and 84 police personnel, including 36 from neighbouring Andhra Pradesh, had lost their lives in naxal attack and violence in the state. The situation was such that both malaria and Maoists have become serious problems in many parts of the state, a senior government official said. The Maoists are operating in 17 of the 30 districts of Orissa, while malaria deaths were reported from about 20 districts, he said. The highest number of 283 people died of malaria in 2004, followed by 257 deaths in 2006, 255 in 2005, 221 in 2007 and a spurt to 239 in 2008. ''So far 27 people have died of malaria in 2009'', Health and family welfare minister Prasanna Acharya said. Maoists on the other hand killed 82 persons in 2008, 11 in 2007, 8 in 2006, 15 in 2005 and 9 in 2004. Both home and health departments claimed to have stepped up activities to combat Maoist and malaria menaces. Acharya said measures to check malaria were in place in all the villages of Orissa. "Facilities have been created to detect the disease within 15 minutes," the minister said. On the ineffectiveness of chlroquine tablets in most places of the state, Acharya said new medicines like artesunate and sulphadoxin plus pyremethamine were being freely distributed among patients. Besides, long lasting insecticide treated mosquito nets were also being distributed and insecticides were being sprayed to control the spread of the disease. The awareness machinery has also been activated in vulnerale districts, the minister said. Stating that both World Bank and global funds are available for controlling malaria, the minister said tribal districts - Keonjhar and Mayurbhanj in the north and Malkangiri and Kandhamal in the south - have been identified as more vulnerable to it. Balangir district in western Orissa and Puri on the coast had no incidence of malaria deaths, while only one person died of the disease in 5 years in Jajpur district. Khurda district which comprise the state capital reported two malaria deaths in 2005, while the disease appears to be spreading in Sonepur district, official sources said. (Times of India 21/6/09) Swine flu couple shows signs of improvement (3) CHENNAI: The city’s first confirmed cases of swine flu, a couple in their 20s, are now quarantined at the Communicable Disease Hospital (CDH), Tondiarpet and are undergoing treatment. The couple, whose name has been withheld, reside in Vadapalani and had flown from New Jersey on June 13. “At that time, they did not have symptoms so they were sent home. But later on visited a private hospital in their locality. From there, they were referred to the state health department,’’ a senior corporation health official said. The 25-year-old woman, who is pregnant, had visited a private facility for a routine check-up along with her husband, health officials said. Doctors there had suspected the couple had swine flu and referred them to a city health officer.On June 18, the couple was placed under quarantine and their samplessent for testing, which came positive on Sunday. “They have already been given two days of tamiflu treatment. They will be given three more days of this and then discharged. As of now they are doing well,’’ said Director of Public Health Dr S Elango. The couple is on two doses of 75 mg tamiflu daily. Doctors at the CDH have been given masks and alcohol based sanitizers to prevent any cross infections. The State health department has also said that 200 corporation doctors have been given training on dealing with swine flu. In addition, private doctors have been sensitised on the subject through literature and continuing medical education programmes and have been asked to notify State health authorities if they suspect a case. As the virus does not thrive in the city’s climate, health authorities are reasonably confident it will not spread further. (Express Buzz 23/6/09) Campaign against Japanese encephalitis (3) Thiruvananthapuram: A high-level meeting of the District Task Force here on Monday finalised the action plan for a mass vaccination campaign against Japanese encephalitis from July 15 to August 5. Children from the age of one to 15 will be administered one dose of the vaccine. While children from one to three years of age will be vaccinated at health centres and hospitals, those from three to five years will be administered the vaccine at anganwadis and children aged five to 15 at schools. The campaign in the district is being taken up on directions from the Central and State governments. The meeting sought the help of the departments of Local Self-Government, Education, Social Welfare and Revenue as well as doctors, voluntary agencies and parent-teacher associations to make the campaign a success. It was also decided to launch an awareness programme for the campaign. Revenue Divisional Officer-in-charge K.T. Varghese presided over the meeting. District Medical Officer Dr. N. Sreedhar, Additional Director Dr. Kumari G. Prema, Deputy DMO Dr. Mema, District Reproductive and Child Health Officer Dr. Chandralekha Nair, professors from the Medical College Hospital, Corporation Health Officer Dr. Sreekumar and representatives of various departments and organisations participated in the meeting. (The Hindu 23/6/09) Improvement of maternal health a far cry (3) NEW DELHI, 30 JUNE: In spite of the government's claims that rural health is undergoing a massive change under its flagship programme, a survey by a federation of advocacy agencies today said the quality of healthcare is too bad in Orissa and women are dying in hospitals during child-births. “Earlier many women were dying at home during baby-birth and now they are facing the same situation at health centres,” said Mr Nabin Kumar Pati, co-chairman of the White Ribbon Alliance, India. A survey by the alliance that is a conglomerate of 1,500 organisations in 12 districts of Orissa found that implementation of safe motherhood policies and programmes have implementation problems. The findings revealed that 52 per cent of the Auxillary Nurse Midwife (ANM) have no weighing machines and 55 per cent don’t have blood pressure measuring instruments. ANMs play a key role in imparting health care to women and children in rural India. “Only 8.1 per cent of these health workers have stethoscopes available with them and this highlights the gap in supply of instruments and drugs,” Ms Aparajita Gogoi, national coordinator of the alliance, told reporters. Experts present on the occasion said eight years back the maternal mortality rate (MMR) in Orissa was 367 per 100,000 live births as against national average of 401. But now the state was much below the national average in controlling maternal mortality. “At present the MMR in Orissa is 303 as against a little above 254 in the national level,” White Ribbon Alliance's Orissa head Ashok Sahu said. India is one of the key contributors to the maternal deaths in the world with over 20 per cent of such deaths being reported from the country. Around 100,000 deaths occur in India from the causes related to pregnancy and child birth. Orissa, where 75,000 women deliver babies every year, 2,500 women lose their life. The survey conducted in districts like Angul, Bolangir, Boud, Dhenkanal, Jharsuguda, Kandhamal, Khurda, Koraput, Mayurbhanj, Nuapada, Sonepur and Sundergarh, found that 54 percent of the ANMs are administering life saving drugs and performing obstetric first aid in the absence of gynaecologists. Of the 24 FRUs (first referral units) the alliance interacted with, 14 were functional but six of them only have blood transfusion facilities available with them. ; PTI (Statesman 1/7/09) “Urgent need to stem maternal mortality” (3) NEW DELHI: “A quarter of the world’s maternal deaths occur in India and in some States the levels are alarming. Orissa is one such example with a maternal mortality rate of 303 per 100,000 live births and an infant mortality rate of 65 per 1,000 live births,” states the finding of the “Deliver Now for Women and Children” campaign. Addressing a press conference here on Tuesday, the White Ribbon Alliance for Safe Motherhood-India national coordinator Aparajita Gogoi said that of the many challenges before the Government, the urgent need to stem maternal mortality was crucial because it was largely preventable. “It was with this objective that the ‘Deliver Now for Women and Children’ campaign was launched nationally on April 11 last year with a focused initiative in Orissa. While the national maternal mortality rate is reducing, in Orissa it continues to plateau. Therefore, the campaign gave women a chance to make their voices heard on maternal and child health. Public hearings were organised in 12 districts, giving rural women an opportunity to share their experiences directly with local officials and decisionmakers.” Dr. Gogoi said maternal deaths in the country were much higher considering the fact that many expectant women deliver at home. “Maternal deaths are high in rural areas and urban slums”. (The Hindu 1/7/09) First suspected swine flu death in India (3) THIRUVANANTHAPURAM: In what is suspected to be the first swine flu death in India, a 51-year-old NRI hailing from Kerala's Kollam died at a private hospital in the district on Wednesday night. ``The man, identified as Stanely Pelis, had returned from the UK in early June. The end came around 9pm, just a couple of hours after he was admitted to the Holy Cross hospital,'' the state's director of health services K Shylaja said. A throat swab has been sent to the National Institute of Communicable Diseases in Delhi to identify if it was indeed the H1N1 virus, she added. Asked if Pelis had been quarantined on arrival, Shylaja said, ``He had landed at the Mumbai airport from UK. He then took a domestic flight to Thiruvananthapuram and disembarked at the domestic terminal here on June 12''. The screening by health authorities is done mainly at the international terminals and hence he may have passed through. ``He may have been screened at Mumbai, but then it is quite possible that he did not show any symptoms of the flu as the virus has a one week incubation period. Later after reaching home, he developed fever and consulted physicians who gave him medicines for common flu. But then it aggravated and finally on Wednesday, he had to be admitted,'' Shylaja explained. Meanwhile, two persons who deplaned at the Nedumbasseri International Airport in Kochi with symptoms of the influenza have been admitted to special wards and placed under observation. They were returning from Ireland and USA respectively. On Wednesday, the NICD had confirmed the presence of H1N1 in a 69-year-old woman hailing from Chenganoor in Alappuzha district, taking the number of swine flu affected in the state to four. She had arrived here from Canada. On June 28, the health directorate had for the first time since the outbreak of the pandemic confirmed three cases of swine flu in Kerala. This included a mother-son duo who had returned from London. The 24-year-old boy Tony, a house surgeon in UK, and his 53-year-old mother Mary had arrived at the Nedumbasseri International airport from London with symptoms of common flu. The third was Rukhiya, a 34-year-old hailing from Manjeri in Malappuram district. The Health department also announced that it was stepping up surveillance at international airports. (Times of India 3/7/09) Booster shot for public health (3) New Delhi, July 07, 2009: The UPA government emphasised its commitment to rural health by giving a bulk of the increased health funding to the National Rural Health Mission (NRHM) while ignoring the healthcare sector, which got none of the sops it had been asking for. The NRHM outlay rose 17 per cent to Rs 14,127 crore this year, up by Rs 2,057 crore from the 12,070 crore provided in the interim budget. It accounted for almost the entire increase in health outlay, which increased to Rs 19,380 crore from 16,534 crore in 2008-09. Launched in 2005 to make affordable healthcare accessible to the rural India, the NRHM is intended to bring down infant and maternal mortality, reduce the total fertility rate, reduce prevalence of certain widespread diseases and upgrade community health centers. “Increased funds for public health are always welcome but the government should have also strengthened disease prevention,” said Dr Shrinath Reddy, cardiologist, chairman, Public Health Foundation of India. “Taxes on tobacco products could have been increased.” “The budget was a non event for the healthcare sector,” said Shivinder Singh, managing director of Fortis Healthcare. “We expected the sector would be granted infrastructure status, which has not happened.” (Hindustan Times 7/7/09) Swine flu cases in Gujarat rise to five (3) Ahmedabad, July 12, 2009: Four suspected cases of swine flu in the city have turned out to be positive, taking the number of H1N1 virus infections reported from Gujarat to five, Health Department officials said on Sunday. Three girls and their caretaker who were part of All Friends Society (AFS) group which had returned from a year-long cultural-cum-educational exchange programme in the US on July 7 have tested positive. Reports of two girls testing positive of swine flu had come from Delhi's National Institute of Communicable Diseases (NICD) on Saturday, while the positive report of another girl and the caretaker came on Sunday, Principal Secretary (Health) Ravi Saxena told PTI. "Result of three girls from the group AFS and its caretaker isolated at the civil hospital are positive, according to NICD, New Delhi," Saxena said. One new case of suspected swine flu has been admitted to the civil hospital in Ahmedabad on Sunday by the Ahmedabad Municipal Corporation (AMC) health officials, he said, adding the person had not travelled to foreign country but had came in contact with one of the three girls. "Suspected swine flu case of a 40-year-old male has been admitted in isolation in the civil hospital by the AMC health officials on Sunday," he added. (Hindustan Times 12/7/09) Malaria claims 20 lives, thousands ill in Koraput (3) Jeypore, Jul 14 : The dreaded Malaria once again wreaked havoc in the tribal-dominated Koraput district claiming as many as 20 lives in the past one week. Official sources said nearly 3,000 Malaria cases were reported from different hospitals in Jeypore and Koraput sub-division for the past few days causing panic among the residents. According to the reports, the Malaria cases had become more rampant in Jeypore, Kotpad, Laxmipur, Dasmantpur, Borrigumma, Boipariguda, Kundra, Lamtaput and Nandapur pockets. Though the reports of Malaria cases were reported from villages close to Jeypore and Koraput government hospital areas, the tribals, living in the inaccessible pockets, have fallen victim to the disease due to lack of proper medical facilities. The district health administration had been organising meetings with field staff and other departments to combat Malaria in all the 228 panchayats in the district every year. Shockingly this year, the review meeting of Malaria prevention was not held as most of the districtlevel officials were engaged in combating naxal-related problems. The Vector Control Research Center, recently set up in Koraput to curb the Malaria menace, has enrolled over 1,000 cases of Malaria patients sending panic waves among the tribals. Every year, over 200 Malaria related deaths and 15,00,00 Malaria fever cases were recorded in 14 blocks and three urban bodies in the Koraput district. (New Kerala 14/7/09) Japanese Encephalitis toll at 105 (3) Gorakhpur, Jul 17 : The vector-borne deadly Japanese Encephalitis (JE) toll reached 105, following the death of two more children today. Officials sources said so far, 455 JE patients had reported at the Baba Raghav Das Medical College and other district hospitals in the division, of which 105, including 19 from Bihar and one from Nepal, had died. In the last 24 hours, five fresh JE cases had come to light. Almost 47 JE patients were still convalescing. JE patients mostly come from Gorakhpur, Maharajganj, Sant Kabirnagar, Deoria, Kushinagar, Basti, Siddharthnagar, Azamgarh, Gonda, Bahraich, Mau, Ballia and Balrampur districts of UP. Gorakhpur has the dubious distiction of being the JE epicentre in the region. The endemic afflicts eastern UP during monsoon every year and continues to take people under its jaws till the onset of winters. (New Kerala 17/7/09) Encephalitis claims 18 lives in Sivasagar (3) SIVASAGAR , July 18 – As many as 18 persons have died and scores of others have been affected by Japanese encephalitis and malaria in Sivasagar District so far even as the administration speeds up fogging, DDT spraying and medicated net distribution in 114 affected villages and in the towns. However there is no report of malarial death till now from any part of the district. Blood samples from over half a lakh people have been collected so far and 38 have tested to have been affected by malaria . It is to be noted that the scourge of malaria and Japanese enaphalitis was predominant in the border regions of the district adjoing Nagaland and Arunachal Pradesh Geleki, Bihubar, Abhayapore, Borhat , Kanubari , Halowating etc but gradually has spread to the semi urban and urban areas and there has been no effort to contain the increase of mosquitoes and other carriers. (Assam Tribune 18/7/09) 105 child malnutrition deaths from April-June in Melghat (3) AMRAVATI: The Melghat region of Vidarbha is presently a picture of despair and what sounds a discordant note is the cries of kid dying due of malnutrition. A total 105 infants have died between April and June 2009 in Melghat. Despite efforts by the government and non-government agencies and after spending a large amount of money, the infant deaths in this tribal region are unabated. Health department sources said that about 69 children are reported to be in stage IV of malnutrition in Chilkhaldhara and Dharni tehsils of Melghat region. Sources said over Rs 80 crore have been spent on various schemes implemented in the region but results are far from satisfactory. In 2007-08, till July 15,2007, 102 children died of malnutrition, the figure till July 15 2008 was 95. MLA Rajkumar Patel told TOI said that there are many schemes for tribal welfare but these do not reach them. Staff crunch in PHCs, sub district hospitals has hit the health care machinery. District administration officials however blame the lack of awareness and illiteracy among tribals as reasons for high child mortality rate. Health department sources said that tribals are unwilling to shed old beliefs and prefer that the women deliver at home only. Bandu Sane, president, Khoj, an NGO, told TOI that the administration is not sensitive towards the tribals problem. “Though it is mandatory to appoint pediatrician and gynaecologist in all 11 PHCs in Melghat on a permanent basis but only three pediatricians, one gynaecologist have been appointed and that too for only amonth. As per a GR children in stage III and IV of malnutrition should be admitted to hospitals, but this is not the case,” he alleged. ZP CEO Omprakash Bakoriya said, “Child marriage is rampant and as girls become mothers at a very young age. The infants are often weak making them vulnerable to various diseases. All infant deaths reported are not malnutrition deaths,” Bakoriya maintained. All 105 deaths of children in age group of 0-6 are not due to malnutrition but children fail pray to the various diseases like hypoglycemia, hypothermia, pneumonia, neonatal sepsis, premature babies etc, health department sources said. (Times of India 23/7/09) 1.5 lakh people affected from viral fever in North Kerala (3) Malappuram/Kozhikode, July 29 (ANI): Lakhs of people in five districts of Kerala, especially the northern regions, are suffering from viral fever mainly caused by mosquito bite during monsoon season. Buzz up! Nearly, ten people have died so far in these regions. According to the health reports, more than 1.5 lakh people in five regions are affected in just few days and the government is taking all necessary steps to check the spread of the disease.Special camps have been arranged and extra doctors have been deputed to these regions. The severely affected districts of Kerala are Malappuram, Kozhikode, Wayand, Kannur and Kasaragod. Many cases of Dengue fever, Chikunguniya, and Hepatitis have also been reported. The symptoms differ as per the region and the doctors say that this can be attributed as mosquito borne communicable diseases or viral fever with severe body pain. Dr. Abdul Samad, Superintendent of District Hospitalin Malapuram, said "after monsoon the number of people affected from fever is fast increasing specially in June and July. Compared to last month, 100 times increase has been reported, it is not a usual viral fever, the afflicted are showing symptoms of heavy pain and swelling with rashes." "We can attribute that its chikangunnya and like viral diseases which is spreading in these regions," he said. Till July 28, the number of patients had crossed 11 lakh starting from January this year. Hundreds of people afflicted with fever and acute joint pains, belong mostly from hilly hamlets and tribal areas throng in huge numbers to nearby hospitals for faster relief. Patients' complain of headache and joint pain and have not experienced such fever earlier. "Whole body in under severe pain. Many part of body have swollen and become red. I cannot stand and walk so my children helped me to the hospital. Doctor says that after medication it will be all right. I never experienced such pain," said Ansuma Bevi, a patient at the Malappuram Hospital. The district administration has moved into crisis management mode and has ordered to distribute free ration for families whose breadwinner have fallen sick. (ANI) (One India 29/7/09) One woman dies every 5 min during delivery in India: report (3) New Delhi Every five minutes, a woman dies in India while delivering a child. According to a report prepared by Centre for Reproductive Rights which was released on Saturday, the maternal mortality in the country is 301 per one lakh live births. "Every five minutes, roughly one maternal death occurs in India," the report said. UN Special Rapporteur on Health Anand Grover said that in most cases, such deaths "are avoidable" and called for empowerment of women at the grassroot level. "Maternal mortality rate in India has become unacceptable, which in most cases are avoidable. We, instead of empowering the civil society, must work for empowerment of women at the grassroot level," he said. Legal Advisor of Centre for Reproductive Rights, New York, Melisa Upreti said "it is a matter of shame for the government of India which has failed to provide basic nutrition and health care for women. In South Asia region, India, Pakistan and Bangladesh have refused to endorse the UN Resolution on Maternal Mortality," she said. Zameen Kaur of Human Rights Law Network claimed that out of the total maternal deaths, 25 per cent are from the Dalit community in the country. MP Sandeep Dikshit favoured closer interaction between NGOs and the government for a targeted approach to check the malaise. (Express India 1/8/09) Call for maternal health legislation (3) NEW DELHI: The Centre for Reproductive Rights has called upon the legal fraternity to seek accountability for human rights violation arising from maternal mortality. Collaborate with activists and public health experts to develop PIL claiming that the right to survive pregnancy and childbirth is a constitutionally protected right, a report “Maternal Mortality in India: Using International and Constitutional law to Promote Accountability and Change” has recommended. The Centre has sought court intervention to direct the legislative bodies to introduce comprehensive maternal health legislation based on human rights standards. The report released here on Saturday says that public interest petitions should be filed to seek court orders for immediate implementation of service guarantees for pregnant women under the National Rural Health Mission, elimination of provisions that makes maternal health care conditional on consent for sterilisation and denying benefits to certain categories of women. It says that there should be clarity of the purpose of monetary incentives for pregnant women and punishment for those who make informal demands for money from pregnant women. Citing instances where courts had intervened to give justice to victims, the report suggested that legislation should include official guarantees of maternal health services, including emergency obstetric care, enforceable standards for ensuring quality of care, patient’s right to privacy, confidentiality and informed decision making. Steps should also be taken to develop multi-pronged legal accountability strategies for addressing issues relating to maternal mortality like lack of access to contraceptives, unsafe abortion and child marriage by stringent implementation of the Medical Termination of Pregnancy Act and the Child Marriage Restraint Act. The report recommends engaging the National Commission for Women and the National Human Rights Commission for monitoring and accountability strategies. According to the National Family Health Survey-III, maternal mortality ratio had fallen from 400 deaths per 100,000 live births in 1997 to 301 deaths in 2006. (The Hindu 2/8/09) States not doing enough in health sector: Azad (3) New Delhi, August 04, 2009: Unhappy with the way the National Rural Health Mission has been implemented by states, Union Health Minister Ghulam Nabi Azad has said the flagship scheme was not going in the right direction and the state governments should equally "share the burden"."What I see is that the state governments think the government of India is giving money, why should we bother," Azad told PTI. According to Azad, this defeats the entire purpose of the NRHM. "We have to tell them that you also have to do your duty and put in extra money." Observing that states have started thinking of the Centre's NRHM scheme as "replacement" to their duties in the health sector, he said, "...whether it is going in the right direction...I do not feel so. "From our side we are doing enough," he said, adding that the states have not increased their budget in the health sector but instead decreased it. "I shall have to discuss with each state government. They will have to share the burden. We have said we will give money or extra doctors, infrastructure, primary health structures and other facilities. "We are not the replacement. It (health) is a state subject...We have come to add to you services not replace you," he said. The health minister said he would visit each state over the coming months to monitor the implementation of NRHM. Though some states are doing better in immunisation than others, Azad said almost all of them are lacking in health infrastructure. (Hindustan Times 4/8/09) First swine flu death in India (1) NEW DELHI: India on Monday reported its first death due to H1N1 flu infection, with a 14-year-old-girl from Pune succumbing to the deadly influenza virus. The girl, a student of class IX from St Anne’s High School first showed symptoms of H1N1 infection — sore throat, running nose and headache — on July 21. But a critical delay in being tested for H1N1 infection and being administered Tamiflu, because she was admitted in a private hospital instead of the stipulated government isolation ward meant for both suspected and confirmed H1N1 patients, may have been the cause of her death. Union health minister Ghulam Nabi Azad told TOI, “Had Tamiflu been administered in the beginning, the girl could have been saved. I advise people to go to government hospitals and get checked for H1N1 even if they have mild symptoms.’’ What’s bothering the Union health ministry is that the girl had attended school till July 23, raising serious fears that the virus may have jumped to other students and teachers in the school besides everybody she came in contact with from July 20-23. Shockingly, Lymette Wilson, the school’s physical education teacher said the state health department had not even informed the school that a student was found to be infected with H1N1. This is why the school hasn’t even started looking for similar H1N1 symptoms in other students till now. Wilson said, “Till yesterday, we were told it’s a lung infection.” The state health department on the other hand is upset with the National Institute of Virology for not informing them that a positive sample was sent to them by a private hospital. M S Devnikar, head of Pune’s joint coordination committee for containment of H1NI, told TOI, ‘‘Till today, we were not aware that a patient with symptoms of swine flu was admitted to a private hospital.” The school meanwhile will be shut on Tuesday as a mark of condolence on the girl’s death. However, it will open after that. India recorded its first H1N1 case in Hyderabad on May 16 and since then the virus has spread to almost 22 cities and towns across the country. Explaining the series of events that led to the death of the girl, Maharashtra’s health secretary Sharvari Gokhale told TOI, ‘‘On July 21, the girl first showed symptoms. She then consulted a general practitioner and kept attending school till July 23. Two days later, she reported high fever. She was then admitted to Jehangir hospital, a private nursing home on July 27. Her condition worsened following which she was shifted to the Intensive Care Unit and was put on a ventilator on July 29.’’ “On July 31, her throat and nose swab was sent to National Institute of Virology (Pune) which confirmed that she was infected with H1N1. The same day, almost 10 days after her symptoms first appeared, she was administered the first dose of Tamilfu, which obviously was too late,” Gokhale said. ‘‘Inspite of telling people day in and day out that in case they show symptoms of H1N1, they should immediately report only to stipulated government hospitals, the instructions are not followed. We are sending a team tomorrow to trace all contact cases in the school,’’ she added. India’s announcement of the death came soon after the first fatality due to the virus was reported from sub-Saharan Africa, the only region in the world that had not reported any deaths till Sunday night. The death in South Africa of a healthy student due to H1N1 infection on Monday means that the virus has now killed people in all regions of the world. The World Health Organisation declared the present outbreak as a H1N1 influenza epidemic on June 11. The virus has till now killed more than 800 people worldwide and is expected to hit 30% of the world population in its second wave, towards the end of the year when the cool climate would be perfect for the virus to propagate. Meanwhile the Union health ministry will soon chair a meeting to discuss the death. Union health secretary Naresh Dayal said that Tamiflu could be made available as an over-the-counter drug in select government hospitals and chemist shops only on prescription by a physician, soon. “NIV and NICD will evaluate what caused this death. We will do a thorough medical examination to see whether the girl had any underlying condition or was it the delay that caused the death. The pneumonia she contracted in the end became too serious and ended her life. Last three days she was so critical that she couldn’t even be moved from the private nursing home to a government hospital,” officials said. (Times of India 4/8/09) Pune, Satara districts notified under Epidemic Diseases Act (3) MUMBAI: Maharashtra Health Minister Rajendra Shingane said on Tuesday that the government had issued a show-cause notice to Jehangir Hospital in Pune, where the country’s first death due to swine flu occurred and Ruby Hall Clinic, which tested the 14-year-old girl’s throat swabs and found them to be negative for the swine flu virus. Dr. Shingane said action against them would be decided based on their reply. The Law Department was also being consulted. He declined to commit himself on the kind of action, saying only that “100 per cent action will be taken.” At a press conference, Dr. Shingane and Additional Chief Secretary (Public Health) Sharvaree Gokhale said the girl would have survived had she been admitted to a public hospital and given prompt treatment. They advised people who showed symptoms of swine flu to go to public hospitals and not seek treatment in private institutions. The government has notified Pune and Satara districts affected areas under the Epidemic Diseases Act 1897. This is an enabling provision allowing the State to take certain steps in the event of an epidemic. All the girl’s primary contacts, 78 in the nursing home and 27 personal, were advised home quarantine and preventive treatment. Instructions were given to keep the students of St. Anne’s, where the girl studied, under surveillance and watch out for symptoms of swine flu. The school has been closed. “It’s not our fault,” the Minister said. The girl was diagnosed with swine flu and treated nearly 11 days after the primary symptoms manifested. Timely treatment was vital. It was also not known how she contracted the virus. Dr. Shingane said that there was no reason to panic and if people showed symptoms, they should visit the nearest public hospital. The school should have also notified the public authorities, he said. “Don’t they read the newspapers,” wondered Ms. Gokhale. Chief Minister Ashok Chavan expressed his sorrow at the death of the girl. He said the State was capable of dealing with the disease and there was no need to panic.(The Hindu 5/8/09) Swine flu grips more people; death toll 17, Pune worst affected (3) Pune/New Delhi, Aug 12 : The Centre today launched full scale preventive steps against the spreading swine flu with directives to invoke Epidemic Act, if necessary, in different parts of the country to tackle the situation on a war-footing as five people died of the HINI virus within 12 hours in Pune, taking the nationwide toll to seventeen. In the wake of the growing number of cases in Maharashtra where 11 people have died of the dreaded disease, the government has shut down schools till Auguast 20 and closed down multiplexes and malls for three days from tomorrow. As a precautionary measure, organisers of religious festivities,incvluding popular "Dahi Handi"public shows on the occasion of the Lord Krishna Birth anniversary have scaled down the celebrations to avoid huge public assemblies. A 48-year-old man succumbed to the deadly H1N1 flu in the government-run Sassoon Hospital in Pune today-the 10th victim in the city and 17th in the country. Gautam Shelar, a driver by profession, who was kept in the isolation ward of the Hospital, was on ventilator since last Monday. He died at 1605 hrs. He was earlier admitted to a private hospital after he suffered fever and cough, district collector Chandrankant Dalvi told reporters here. Earlier, 50-year-old Nita Meghane, a resident of posh Kalyani Nagar who was undergoing medical treatment in the hospital since last five days, succumbed to the contagious virus at 1530 hrs. She was brought to the Sassoon Hospital on Tuesday and the same day her blood sample was sent to the National Institute of Virology (NIV), which tested positive for H1N1 on Wednesday. She was on ventilator since Thursday. Talking to UNI, Medical Superintendent of Sassoon Hospital Dr P S Pawar confirmed the death of 10th victim, saying ''our doctors tried to give all possible treatment but could not save their lives. Ten people have fallen victim so far to the dreaded H1N1 virus since the first death of 14-year-old girl Reeda Shaikh on August 3. Another victim, a 41-year-old man, Balu Kulund, also succumbed to the dreaded disease. He was admitted two days ago in critical condition and he had stopped responding to medicines since last night. Among the dead were 29-year-old Shrawani Deshpande, who died at Sassoon General Hospital early this morning and a doctor, Rupesh Prahlad Gangurde (28), succumbing at a civil hospital in Nashik. With this the nationwide toll of the pandemic has climbed to 17 with two deaths reported from Gujarat and one each from Kerala and Tamil Nadu. A report from Ahmednagar district said 13 people, including a student from Pune, are suspected to have acquired the virus and been admitted to the civil hospital. Their throat and nasal swabs have been sent to National Institute of Virology (NIV). The Centre today asked states to take steps to check sale of spurious Oseltamivir in markets and started the process of procuring 2 crore Tamiflu tablets from pharmaceutical companies. The Health Ministry held an emergency meeting of the State Drug Controllers informing them about the reports about availability of Tamiflu with some chemists in the open markets in Delhi and some other cities who are illegally selling them at exhorbitant prices and asked them to check whether these tablets were spurious. States have also been asked to take measures to prevent illegal sale of Oseltamivir in the open market as at present the drug is being made available free of cost in designated government hospitals, Joint Secretary in the ministry Vineet Chowdhury told mediapersons here. Regarding the reports about disappearance of masks from the markets, Mr Chowdhury said that N-95 masks are used by the doctors and para-medics involved in taking the sample of infected persons, testing and treating them and not being recommended for general public. He said that people should wear three layered surgical masks which are cheaply available in the markets. ''This is a public health emergency and crisis and we expect the citizens to cooperate,'' he said and added that strict action under the Epidemics Act would be taken against those involved in hoarding and illegal sale of Tamiflu tablets and such masks……….New Kerala 12/8/09) Infant, 75-year-old die in Pune; death toll climbs to 19 (3) Pune An eleven-month-old boy and a 75-year-old woman died here on Thursday, taking the toll in Pune, severely hit by the virus, to 12 and across the country to 19. The boy, Rutwik Kamle was admitted first to a private hospital and then shifted to government-run Sassoon Hospital Wednesday evening in a serious condition, official sources said. He died early this morning. Bharti Goyal, who was suffering from the viral infection, died in KEM Hospital here, they said. With this, the number of flu deaths here has risen to 12 and across the country to 19. Besides the Pune deaths, one person each has succumbed to the virus in Ahmedabad, Vadodara, Nashik, Chennai and Thiruvananthapuram and two in Mumbai. Ten people last night tested positive for swine flu in Gujarat, taking the total number of those afflicted by the disease countrywide to 1,203. While Pune remained the worst-hit area by the disease with 61 new cases being reported from the city, Gujarat's 10 new cases took the number of those infected to 27 in the state. "All test results that were pending have come and according to them, 10 more people, including three women, have tested positive for swine flu," Gujarat Principal Secretary Health Ravi Saxena said. The figures include five from Ahmedabad, four from Surat and one from Navsari, Saxena said. In Navsari, a 14-yearold boy has been infected by the virus. According to the available data, a total of 125 fresh cases have been reported, taking the total number of those afflicted to 1,203. Besides the western region, flu cases were reported from Mumbai (24), Kolkata (3), Bangalore (10), Shillong (1), Goa (1), Delhi (8) and Hyderabad (3). In Shillong, the 17-year-old male patient had travelled to the UK. In Bangalore, all of the 10 cases had contracted the virus in the country and had no foreign travel history. Goa also reported one indigenous case. All the eight patients in Delhi and three in Hyderabad had acquired the infection in India.(Express India 13/8/09) Swine flu toll touches 15 in Pune, India's toll 23 (3) Five people, including two septuagenarian women and an AIDS patient, today died of swine flu in Pune taking the death toll in Pune to 15 and India's toll to 23: 70-year-old Parubhai Shinde, hailing from Ganesh Nagar in Yerawada, was admitted to a hospital here four days back following high fever and other symptoms of swine flu and died late tonight, health officials said. Another senior citizen, Bharati Goyal, who was suffering from fever and breathlessness for the last four days, had been on ventilator when she died today of suspected swine flu, sources said. 37-year-old Archana Kolhe, who was shifted to government-run Sassoon Hospital on August 10 with fever and acute respiratory problems from a private hospital, succumbed to the flu in the afternoon, Pune Municipal Corporation Commissioner Mahesh Zagade told reporters. An eight-month-old boy, Swabhiman Kamble, died late last night in Sahyadri Hospital, a designated private hospital to treat flu patients, Zagade said, adding that reports of his throat swab samples are still awaited. 44-year-old HIV positive Prabhakar Wariager died late this evening of swine flu within hours of his admission to the Sassoon Hospital. Wairager, hailing from Watgaon village in the district, had earlier tested positive for the swine flu and admitted to the hospital in the afternoon, hospital sources said. (Mumbai Mirror 14/8/09) Concern over rising infant mortality rate (3) Srikakulam: The Hospital Development Committee at Narasannapeta near here, which met under the chairmanship of local MLA Dharmana Krishna Das, expressed concern over rising infant mortality rate due to poor level of awareness on sanitation, hygiene and importance of institutional deliveries among the rural population. Despite the government doing everything possible to encourage institutional deliveries to prevent of infant mortality, the rural people were still influenced by superstitions, which dissuade them from getting admitted in government hospital for safe delivery. The State government, under the Rural Health Mission, is giving an incentive of Rs.1,000 to pregnant women who come to government hospital for delivery and Rs.800 to those who go to private hospitals for delivery. Besides, it is keeping one 108 ambulance at the service of people of two mandals to enable them to get delivered under the supervision of a medical officer. The government is also spending a lot of money on monitoring the health of lactating women by offering them pre-natal and post-natal care through the ICDS projects. The anganwadi centres offer nutritious food to pregnant women. Asha Workers are paid Rs.150 as incentive for personally bringing a pregnant woman for delivery to the government hospital. Despite the government giving many incentives to pregnant women, they are still not opting for institutional delivery resulting in infant mortality. The women are rushing to the government hospital in an emergency situation, which involves high risk to the life of mother and the baby. Members of the development committee of Narsannapeta Government Hospital expressed grave concern over the four to five infant deaths reported in the hospital every month for the past four months. Though the hospital had little do to do with these deaths, the members felt that they should do everything possible to achieve cent per cent institutional deliveries to bring down infant mortality rate. District Medical Officer Praveen, noted social worker Tankala Babjee and other local body representatives participated.(The Hindu 15/8/09) New guidelines for swine flu patients (3) NEW DELHI: The Centre has issued revised guidelines for treatment of A(H1N1) influenza patients in the wake of a large number of people turning up at the hospitals for testing. All individuals seeking consultations for flu-like symptoms should now be screened at healthcare facilities, both government and private, or examined by a doctor. The patients have been categorised as follows: Category A: Patients with mild fever plus cough/sore throat with or without body ache, headache, diarrhoea and vomiting. They do not require Oseltamivir and should be treated for the symptoms mentioned above. The patients should be monitored for their progress and reassessed after 24 to 48 hours by the doctor. No testing of the patient for H1N1 is required. Patients should confine themselves at home and avoid mixing with the public and high risk members in the family. Category B: (i) In addition to all the signs and symptoms of Category A, if the patient has high grade fever and severe sore throat, he/she may require home isolation and Oseltamivir; (ii) In addition to all the signs and symptoms of Category A, individuals having one or more of the following high risk conditions shall be treated with Oseltamivir: children under five, pregnant women, those above 65 years, those with lung diseases, heart disease, liver disease, kidney disease, blood disorders, diabetes, neurological disorders, cancer and HIV/AIDS; Patients on long term cortisone therapy. No H1N1 tests are required for Category-B (i) and (ii). Such patients should confine themselves at home and avoid mixing with the public and high-risk members in the family. Category C: In addition to the symptoms of Categories A and B, if the patient has one or more of the following: breathlessness, chest pain, drowsiness, fall in blood pressure, sputum mixed with blood, bluish discolouration of nails; irritability among small children, refusal to accept feed; worsening of underlying chronic conditions. Such patients require testing, immediate hospitalisation and treatment. The guidelines were finalised after a five-hour meeting chaired by Health and Family Welfare Minister Ghulam Nabi Azad. These norms will be reviewed and revised from time to time as per the need and on the basis of spread of the disease. The meeting was attended by officials of the Ministry of Health and Family Welfare, Directorate-General of Health Services, and representatives and experts of private and public hospitals. During the meeting, various guidelines and protocols developed by the World Health Organisation, Geneva, the Centre for Disease Prevention and Control, Atlanta, United States, and the National Health Service, United Kingdom, were also discussed.(The Hindu 16/8/09) Swine flu: Another 11 cases reported, government gives updated guidelines (3) Eleven cases of H1N1 were reported on Sunday from the Capital. Ten of these patients have no known history of travel while three are schoolchildren. The eleventh patient is a 14-year-old boy who had travelled to UK. According to the authorities, the school children on home quarantine were called back to hospital after their results turned out to be positive. “Two of the children were called back, and they have been admitted to Malviya Hospital,” said a Delhi government spokesperson. The government, however, is expecting the number of patients needing hospitalisation to go down in the coming weeks, since the Centre has tweaked the treatment guidelines. As per the new guidelines, patients have been categorised as follows: Category A: Patients with mild fever accompanied by cough or sore throat with or without bodyache, headache, diarrhoea and vomiting, do not require Oseltamivir and should be treated for the symptoms mentioned above. The patients should be monitored for their progress and reassessed at 24 to 48 hours by the doctor. No testing of the patient for H1N1 is required. Patients should confine themselves at home and avoid mixing with the public and high-risk members in the family. Category B: (i) In addition to all the signs and symptoms of Category A, a patient who has high grade fever and severe sore throat, may require home isolation and Oseltamivir; (ii) In addition to all the signs and symptoms of Category A, individuals having one or more of the following high-risk conditions shall be treated with Oseltamivir: children under five, pregnant women, those above 65, those with lung diseases, heart disease, liver disease, kidney disease, blood disorders, diabetes, neurological disorders, cancer and HIV/AIDS; Patients on long term cortisone therapy.... contd.(Indian Express 17/8/09) Nine fresh cases recorded in State (3) CHENNAI: Nine fresh cases of A(H1N1) influenza were recorded in the State on Wednesday, according to Public Health officials. All the cases were from Chennai, and included two children. The patients were put on Tamiflu. The children were given special care by paediatricians. This takes the total number of positive cases to 129. The highlight on Wednesday was that two private hospitals in the city — Vijaya Hospital and Apollo Hospital — began to admit and treat patients. The drugs were dispatched from the Communicable Diseases Hospital by Corporation Health Authorities. “It is very good that the private sector is pitching in with the treatment efforts. Everyone should contribute, especially in a situation like this,” said V.K. Subburaj, Principal Secretary, Health. He says though the number of cases in Tamil Nadu is still low, a new problem has cropped up — a number of patients seem to be running away from hospitals. This had taken place in Coimbatore, Madurai and Chennai and public health officials had to hunt down these patients. “People should realise that running away untreated is good neither for them nor for the community. They take the virus into the community and spread it there. That is the situation we are trying to avoid,” he added. (The Hindu 20/8/09) Flu takes heavy toll of health care budget (3) BANGALORE: Less than six months into the Influenza A(H1N1) scare and the health ministry has already spent a whopping Rs 6.3 crore to combat it. So far, throat swabs of 12,604 patients have been tested in the country. According to health ministry officials, each test costs the government Rs 5,000 for the government -- that's Rs 6.3 crore for tests alone. This is half the annual budget of Karnataka for controlling tuberculosis, a disease that affects more than 63,000 new patients every year, and has a mortality rate of 8% every year in the state. According to health & family welfare department, director, Dr Usha Vasankar, the government spends Rs 8,000 per patient. "Each H1N1 flu patient requires 10 tablets of Tamiflu which cost around Rs 1,800. The other costs are for swab collection process (Rs 800), N-95 mask (Rs 120) and lab test for confirmation (Rs 5,000). So, it all adds up to about Rs 8,000 and currently, the state government is footing this bill for every suspected patient." As this is a new virus, the testing process is tedious and takes almost 4 hours per sample. While the Centre has supplied testing kits for 500 samples, the state governments had to procure additional kits to control the flu from spreading. In Karnataka, additional 1,500 testing kits were procured by the state government and each kit can test 100 samples. With treatment cost escalating and with disease spreading from metros to the remote districts, there is need for rapid preventive action, especially in six states -- Karnataka, Tamilnadu, Andhra Pradesh, Maharashtra, Manipur and Gujarat, where there is a high incidence of HIV/ AIDS and more than 50% of the patients are affected by tuberculosis. "As these patients are immuno-compromised with low CD4 count, they are under high-risk category and are prone to be affected by H1N1 flu. The number of HIV and TB cases being high in these state, precautionary measures should be taken," said Dr Sangeetha Kodkani, in-charge director of the state TB Demonstration Centre. Now, with several private laboratory and hospitals coming forward to conduct the lab test, than for disease confirmation itself will cost patient Rs 8,000 to Rs 10,000 in these private labs. Due to the escalating health bill, the health ministry is considering asking private hospitals to conduct screening as well as lab testing. If this comes into force, lab tests alone will cost the patient anywhere between Rs 8,000 to Rs 10,000. Health experts say: "As long as patients have a choice of government institute screening and testing freely, affordability will not be an issue. Apart from those returning from abroad, now the virus has begun to affect the middle and lower middle classes. Government patient care facility should continue, along with support from private hospital, as an option for those who can afford the treatment." (Times of India 23/8/09) 24 tribals die of diarrhea (3) Bhawanipatna, 24 Aug: At least 24 tribals have died due to diarrhoea in Orissa's Kalahandi district during the last fortnight, officials said today. While 13 people have died in five tribal villages under Bhawanipatna block, four hamlets under Lanjigarh block accounted for 11 deaths. The villages under Bhawanipatna block where the deaths were reported are: Panchbaheli (6), Jamchuan (3), Tengnabaheli (2) and Rukunibundel and Bundelguda (1 each).The affected villages under Lanjigarh block are: Ghatikundra (6), Tarangsel (3) and Talbora and Jalkrida (1 each). Kalahandi district collector, Mr RS Gopalan claimed that while the situation is under control in Lanjigarh block due to intensive measures taken by mobile health teams, the condition in Bhawanipatna block was “alarming”. Ten mobile health teams are being used to combat outbreak of the water-borne disease and doctors from different parts of the district have been deputed to the affected areas. Lamenting that people were resorting to rituals and crude methods to get cured instead of taking medicines, Mr Gopalan said that awareness through street plays has been launched.The district administration would pay Rs 200 from Rogikalyan Samiti to the volunteers who brought serious patients to primary health centres and hospitals for treatment, he said.(Statesman 25/8/09) Swine flu claims one more in Beed, Marathwada toll 6 (3) AURANGABAD: Swine flu claimed one more life in Beed on Saturday, taking the death toll in the district to two and in Marathwada to six. Earlier, two deaths were reported from Latur, one from Beed and one each from Jalna and Aurangabad. He was confirmed positive for the H1N1 virus on Sunday. According to S S Patil, deputy director of health services, Latur, the 32-year-old victim a resident of Khokarmoha in Beed district was initially treated at the Yashwantrao Chavan Memorial Hospital in Pimpri, Pune, from where he was shifted to the Beed civil hospital on August 27 with complaints of severe cold, cough, and breathlessness. "He was also an HIV positive patient," Patil said. After admission to the Beed hospital on August 27, his throat swab was sent for further examination to the National Institute of Virology (NIV), Pune. However he died a day before the throat swab report came. "The number of people examined for the H1N1 virus in Latur, Beed, Osmanabad and Nanded districts so far has reached 31,413 while the hospital authorities isolated 338 people. Swabs of 321 of those screened were sent for tests. The NIV sent back the reports of 250 patients, 50 of whom were found H1N1 positive", Patil pointed out. Right now, he said, only two positive H1N1 patients were being treated at the government hospital at Nanded and their condition was good. Aurangabad division comprising Aurangabad, Jalna, Parbhani and Hingoli has witnessed screening of 25,150 people so far, said Vikas Nikam, assistant director of health services. He said the number of positive patients in the division has increased to 22 while nine people are being treated at different government hospitals. But there was no cause for worry as their condition was good and improving. Till date, 233 swabs were sent to the NIV, of which 175 reports have been received. Nikam said that except two deaths in Jalna and Aurangabad, no fresh death due to the H1N1 virus was confirmed. (Times of India 1/9/09) WHO wants countries to focus on diarrhoea to reduce child deaths (3) Kathmandu, Sep 8 : WHO has expressed concern over 50 children under-five years dying every hour in South-East Asia due to diarrhoea, and asked countries to focus on the disease in their national health programme. Diarrhoea is a leading cause of child mortality in the region, second only to pneumonia, a WHO release said. ''Diarrhoea and acute respiratory infections are the biggest killers of children under five in South-East Asia. Diarrhoea is also seriously under reported in the region. There is a need to focus on diarrhoea and pneumonia in national health programs,'' WHO Regional Director for South-East Asia Samlee Plianbangchang told journalists at WHO's Regional Committee session in Kathmandu, Nepal today. In South-East Asia, the average incidence of acute diarrhoea among children under five years of age is around three episodes per child per year. In some South-East Asian countries, it could be as high as 12 episodes per child per year, he pointed out. Lack of safe water, sanitation, proper nutrition, essential health services and awareness about effective interventions make the poor, especially vulnerable to acute diarrhoeal diseases. Large outbreaks of acute watery diarrhoea and deaths in the South-East Asia Region in the recent past have affected both children and adults, he added. Simple, safe and relatively inexpensive interventions are available, which can greatly reduce the deaths due to diarrhoea in this Region. Exclusive breastfeeding up to six months of age, frequent hand-washing, nutritional interventions, timely immunisations and improved case management with early oral rehydration therapy and zinc at both community and facility levels. An adequate supply of safe water and improved sanitation as well as community, household and good personal hygiene practices can tangibly reduce the disease burden in this Region. Control of diarrhoea and acute respiratory infections requires an integrated and comprehensive approach for prevention and case management with full involvement of the community. The WHO Regional Office for South-East Asia is supporting countries in their efforts to control these diseases by developing a regional strategy, guidelines and protocols, and training materials. (New Kerala 8/9/09) 227: Record dengue cases in Pimpri-Chinchwad in one month (3) Even as the swine flu cases are rising in Pimpri-Chinchwad, dengue cases have emerged as the new threat. In August, the twin industrial township witnessed the highest number of 227 cases which was the highest for any month since the aedis egyptia virus began making its presence felt a few years back. Similarly, malaria cases have also seen a sharp rise with 110 cases registered last month. In July too both dengue and malaria cases where on a high. Both had registered over 100 cases, but the number of cases recorded in August surpasses the previous record. With maximum number of dengue cases last month, the total number of dengue cases since January up to August has reached 541 and malaria cases during the same period has reached 540. Pimple Saudagar, Pimple Nilakh and Wakad have been the three suburbs where maximum number of dengue cases have been recorded till last month. In August as well as this month, Indrayani Nagar has reportedly seen a large number of cases. According to local residents, at least 13 persons have been admitted to various hospitals, most of whom have reportedly recovered. PCMC medical officials said like Pimple Saudagar, Pimple Nilakh and Wakad, Indrayani Nagar area has also witnessed tremendous construction activity due to which there has been a rise in dengue cases. "There have been hardly any casaulties of dengue. All the patients of dengue who had turned critical have recovered," PCMC officials said. Patients affected by dengue in Pimpri-Chinchwad generally prefer private hospitals like Aditya Birla, Chinchwad, Niramya Hospital, Chinchwad and Lokmanya Hospital, Chinchwad and Nigdi. However, residents from Sangvi, Bhosari, Dighi and Dapodi prefer private hospitals in Pune. (Indian Express 8/9/09) Most deaths in young people are preventable: WHO study (3) Geneva, Sep 11 : Most of the 2.6 million deaths of young people each year are preventable, according to a new study supported by the World Health Organisation and released in Geneva Friday. The main causes of deaths in the 10-24 age group were road traffic accidents, complications during pregnancy and child birth, suicide, violence, HIV/AIDS and tuberculosis. The study, to be published in the Lancet, a medical journal, found that 97 percent of these deaths were taking place in low and middle-income countries. "Young people ... often fall through the cracks," said Daisy Mafubelu, WHO's expert for family and community health. She said it was important to improve their access to information and services "and help young people avoid risky behaviours that can lead to death".There are an estimated 1.8 billion people that fall into this age group, accounting for 30 percent of the world's population. Road traffic accidents could be avoided through more appropriate speed limits, strict enforcement of drunk-driving laws and by the use of helmets and safety belts, the WHO said. Moreover, young people need sex education, condoms and other contraceptives, the ability to perform safe abortions, access to antenatal and obstetric services and testing and care for HIV/AIDS. The study also led the researchers to conclude that suicide and other violence could be prevented through life-skills training and positive parental involvement in young people's lives. Furthermore, the WHO recommended that access to lethal means of all kinds, including guns and toxins, should be reduced, along with limiting the consumption of alcohol. There also needed to be better care and support for those exposed to child abuse, youth violence, and sexual assault, to help young people deal with the immediate and long-term consequences of these traumatic events. (New Kerala 11/9/09) Malaria spreads wings in Balangir, claims 38 (3) PATNAGARH: Three persons of a family died of malaria in village Chabripali of Bhanpur gram panchayat in Balangir district recently. Affected by malaria, now the sole bread winner of the tribal family Jimut Bariha (45) and his lone surviving seven-year-old son Ram Prasad have been admitted to Balangir district headquarters hospital. Reports said at least 121 villagers are affected by malaria with the death toll pegged at 38 in the district. This is despite implementation of numerous welfare and healthcare projects in the region. The schemes were aimed at making urban centric healthcare into rural centric health services with the participation of the community. It was only last year landless Jimut had returned home after working outside the State. And since then he had been doing odd jobs to eke out a living. But malnutrition and fever forced Jimut to remain confined to home. And it took a toll on the financial condition of the family which has resulted in hunger pangs. On September 6, his ten-month-old daughter and three-year-old son died within a span of 12 hours. Unable to bear the shock and having to go without food, his wife Bimala died on September 9. While the CDMO Dr. Purna Chandra Sahu has attributed the deaths to malaria, Jimut’s mother Minicha and father Champe Bariha besides ward member Jaibihari Bariha and villagers said the trio died of starvation. Although, sarpanch of Bhanpur gram panchayat Chudamani Nag had sent 10 kg rice to the household after the news of death reached him, it was too late and too little for the family which was rocked by three deaths within a span of 72 hours. Numerous welfare schemes and development projects to ensure food security in the district seem to have remained on paper only forcing people to undergo untold miseries. Villagers said while the deaths in the family of Jimut brought to the fore his plight and starvation, there is long list of such people who are going without work, food and healthcare. (Express Buzz 13/9/09) Over 67 pc victims of H1N1 had risk factors (3) PUNE: District collector Chandrakant Dalvi on Saturday said that of the 40 deaths reported in the district due to H1N1 influenza, 27 (67.5%) had risk factors like hypertension, diabetes, central nervous system (CNS) disorders and heart diseases. Five of them had a history of hypertension. He also said that delayed diagnosis and treatment were the key factors in some of the deaths. Dalvi appealed people who have either hypertension, diabetes, CNS disorders or heart diseases to take due care and approach screening centres in case of symptoms like coughing, sneezing and cold. "Four people who died had history of diabetes melitus and central nervous system (CNS) disorders while three others had history of heart diseases and obesity. Three patients were very old while two cases were of liver disorders," said Dalvi. Elaborating on delayed diagnosis and treatment, Dalvi said that if the patient does not show any signs of recovery even after 48 hours of showing flu-like symptoms, it is advisable to visit the screening centre for a second opinion. Dalvi said that all general practitioners will again be given instructions to refer H1N1 symptomatic cases to designated centres immediately. He informed that the state health department has conducted a training camp for general practitioners at each tehsil in the district. Dispelling fears of rapid spread of the virus in schools, Dalvi said there is no panic at the school level in the city as well as rural areas. All the schools and colleges in the rural areas have now been asked to screen students on a daily basis. The screening will be conducted by class teachers at the beginning of the class. He said, "No private laboratory in the city has been given permission to conduct tests for H1N1 influenza. According to instructions issued by the central government, the private laboratories in the city cannot conduct swab tests." (Times of India 14/9/09) Kalahandi battles malnutrition woes (3) BHAWANIPATNA: Tribals are more prone to infectious diseases due to malnutrition. An Indian Council of Medical Research (ICMR) bulletin said this in October 2003. In 2009 too this holds good in some of the tribal pockets of Kalahandi which are witnessing gastroenteritis and malaria in epidemic proportions. A senior doctor working in the field of epidemic control in the district preferring anonymity asked, ‘‘Can a patient sustain only by administration of IV-Fluid without supportive nutritional diet?’’ No is the answer as at least 20 patients died of infectious diseases after treatment. The food habit and cultivation pattern are such that tribals are deprived of nutritional diets. It is usually observed that here people’s food habit is quite different from coastal plains due to over dependence on forest and shifting cultivation in the absence of other sources of earning. They grow 13 different varieties of crops including ragi, kandul, kating, koshla and judunga through shifting cultivation which sustain them for three to four months after repaying debts to money-lenders. They also collect various tubers like keukanda, pitakanda, bhatkanda, kargikanda and mundikanda from the nearby forests. As during this period of the season, crops grown through shifting cultivation are not harvested, the food consumption is usually restricted to gruel made of ragi mixed with little rice and salt. This situation improves during winter as harvesting is completed by then. Against this background, introduction of NREGS held out hope with the expectation that the age-old food insecurity will be minimized. However, the scheme has failed depriving people of their purchasing power. Jobs to registered people in the district is poor and it’s abysmally poor in the inaccessible tribal pockets, according to data of District Rural Development Agency (DRDA). According to statistics, in the financial year 2008-2009, job cards were issued to 2,64,862 persons of which employment could be provided only to 82,051 persons generating 136,1818 mandays in the district. Only 736 families could get 100 days of mandatory work in the district. The scenario has not improved in current financial year too. According to the report, in 2009-10, 2,64,862 persons have registered themselves and among them so far 1,50.653 persons have been provided jobs generating 1,50,653 mandays. But only eight families have completed 100 days of work. The scenario is worse in inaccessible tribal pockets. The status of NREGS in the epidemic-hit tribal panchayats under Lanjigarh and Bhawanipatna blocks present a sorry picture. Jugsaipatna, Chancher and Sagada gram panchayats in Bhawanipatna block and Malijuang, Pahadpadar, Lakhbahali and Bengaon gram panchayats in Lanjigarh block are worst affected by the epidemic outbreak. According to DRDA statistics, in last fiscal job cards were issued to 818, 664, and 1439 persons in Jugsaipatna, Chancher and Sagada gram panchayats in Bhawanipatna block respectively of which 521, 136, and 931 persons were provided jobs in the respective gram panchayats. And among them only eight, zero and three families could get 100 days of work. During current financial year same numbers of job cards were issued and employment was offered to 118 persons of 67 households in Jugsaipatna gram panchayat generating 1517 mandays while 37 persons of 27 households of Chancher got employment generating 480 mandays and 159 persons of 101 households of Sagada gram panchayat got jobs generating 1389 mandays. Similarly in Malijuang, Pahadpadar and Lakhbahali Bengaon gram panchayats, which are epidemic affected, in Lanjigarh block persons provided work and mandays generated are very poor in current financial year. In the epidemic pockets of Bhawanipatna and Lanjigarh blocks the work availability under NREGS is hardly 10 to 15 days so far during current financial year. In several places workers engaged are not getting their wages for months for different reasons. In this context Bharat Thakur, chief executive of NGO Janakalyan Sanstha who is working in inaccessible pockets, expressing anguish said as the people are deprived of employment they have no purchasing power. In the absence of work, they have no way out but to entirely depend on forests giving rise to malnutrition problems, he reasoned. (Express Buzz 14/9/09) 40 p.c. children in tribal haadis in H.D. Kote taluk malnourished (3) H.D. Kote (Mysore district): Three-year-old Suma, daughter of Jayamma of Balle Haadi in H.D. Kote taluk, recently died of tuberculosis. Delay in providing medical treatment for the child because of the family’s superstitious beliefs is supposed to have caused the death. However, Director, Development through Education (DEED), Srikanth, says Suma was severely malnourished. Malnourishment in children is a common problem in over a hundred haadis (tribal settlements) in H.D. Kote taluk. Poverty, illiteracy, ignorance and failure of the public healthcare system have worsened the situation, says Somanna of the Budakattu Krishikara Sangha (BKS). The Government can provide some help by way of establishing anganwadis in these haadis for the benefit of children and pregnant women. In fact, there is provision for opening an anganwadi even if there are just 25 children in the area, but sadly the authorities concerned are not prepared to establish anganwadis in these haadis. Over 25 children of Kollegagowdanahalli Haadi, which is just 5 km from the taluk headquarters, recently fell ill. Tribal people, who are superstitious, did not take their children to hospital. However, because of the initiative of Basavaiah, a farm labourer, a doctor visited the Haadi. “However, after administering medicine to children once, the doctor did not make a second visit to the haadi. We cannot afford to go to private hospital,” says Basavaiah (60) who earns Rs. 30 a day. “Had there been an anganwadi in our haadi our children could have benefited from nutritious food that is provided and pregnant women also could have got nutrition supplement and medicines provided there. If the Government is ready to open a “mini-anganwadi”, I am prepared to donate my house,” he says. It is significant that tribal people are not even aware of the National Rural Employment Guarantee Act (NREGA) envisaged to enhance livelihood security by extending at least 100 days of guaranteed employment to people in rural areas. Most of the tribal people work in farms for as small a sum as Rs. 20 and Rs. 30. The situation is no different in Aanagatti Haadi, which is on the other side of State Highway. Besides the problem of malnourishment, there is drinking water shortage. At least 9 people live in each of the thatched huts in this haadi. “We have trek 2 km to Shiramalli to get drinking water. It is difficult to fetch water at night as there is no power connection to our haadi. Borewell water that we get is contaminated. Our repeated pleas to authorities to provide safe drinking water and power connection has not yielded any result,” says Rajamma (29). More than water and power connections, women in Aanagatti Haadi are worried about their malnourished children. Mr. Srikanth says that according to a survey, over 40 per cent of children in the tribal haadis in H.D. Kote taluk were malnourished. Many tribal women who do not take vitamin tablets during pregnancy give birth to malnourished children. And, child mortality rate in these haadis is very high, he adds……..(The Hindu 11/9/09) 113 swine flu cases reported (3) New Delhi, September 24, 2009: The national capital on Thursday reported 113 fresh cases of swine flu with the majority of them being children, Delhi Health Minister Kiran Walia said. "Of the 113 swine flu cases, 65 are children and all of them have been quarantined," she said. Walia said that till on Thursday, 2,275 cases were admitted and treated in designated government hospitals and of these 90 per cent have been discharged. Delhi has so far reported nine swine flu deaths. "The situation is under control and the government is doing its best in providing treatment to H1N1 patients. I advise people to visit the doctor at the earliest if any symptom of swine flu appears," she said. (Hindustan Times 24/9/09) China number two in world for rabies deaths: Govt (3) Beijing, September 28, 2009: China is second only to India worldwide in the number of people killed by rabies every year, the government has reported, making the disease one of the nation's biggest public health threats. "China is one of the countries most severely affected by rabies, and in recent years the number of annual reported deaths from rabies has averaged around 2,400," the health ministry said in a statement on its website. "It is only inferior in number to India, and gives us the world's second-place ranking." The statement, issued to coincide with World Rabies Day on Monday, said rabies was among the top three infectious diseases in China. According to the official Global Times newspaper, the other two serious diseases with high fatality rates are AIDS and tuberculosis. The ministry quoted the World Health Organization as saying that more than 55,000 people die from rabies -- a disease most often transmitted through animal bites -- every year, with 95 percent of the cases in Asia or Africa. (Hindustan Times 29/9/09) Malnutrition stalks Koraput children (3) KORAPUT: Two-year-old Brundabati weighs 6 kg, three less than normal. And, neither she nor her parents can be blamed for that. After all, poverty stalks them from close quarters. The family does not have enough to eat. "My husband works as a daily-wage labourer. But mostly he stays at home due to non-availability of work. The earnings are not enough to keep the family away from starvation and a nutritous diet is a far cry," said Brundabati's mother Bhagbati Kirsani of Koraput's Podaiguda village. Bhagbati has two other children. Similar is the case of four-year-old Mumu Sai Kirsani, who weighs only 9.5 kg when her weight should be 13 kg. Similarly, Kumita Badnaik, who is 29 months old weighs 7.5 kg, much lesser than her expected weight. Out of 59 children between 0 and five years at Podaiguda, 37 are in different stages of malnutrition. Five of them are severely malnourished. Malnutrition is common in tribal-dominated Koraput district and is particularly severe among children under three years of age. According to a survey, 25 per cent children in this age-group are in Grade II, III or IV of malnutrition. Sources said early marriages among tribals is a major reason behind the malnutrition problem. Majority of tribal girls marry early (between 10 and 14 years) and soon conceive. As a result, the health of these women as well as that of their children deteriorates. Apart from tribal's healthcare practices, absence of any supplementary diet, unhygienic living conditions, chronic diseases and apathetic attitude of officials concerned are also responsible for malnutrition among children. "The tragedy of persistent child malnutrition in the district reflects failure of health and nutrition delivery mechanisms. The government schemes to counter malnutrition have failed in the area. The apathy of the officials is also largely responsible for such cases. At present, over 2,000 children in the district are severely malnourished," alleged Sanjit Patnaik, a Koraput-based social activist. "Though they are supposed to provide cooked nutritious diet to these children at anganwadi centers, officials give away the nutritious Indiamix powder to parents to take it home and prepare it for their children which the tribals rarely do," he said. But district officials don't feel the situation is alarming. "Though we have not completely succeeded in arresting malnutrition, we are sensitive towards the problem. The situation has not deteriorated. Nutritious diet is provided to pregnant women and malnourished children at 1,560 anganwadi centers in the district. Severely malnourished children are referred to the nearest hospitals. Every month, malnourished children are weighed at the anganwadi centres and the villages mapped to show the nutritional status of each child and the village," said district social welfare officials. (Times of India 2/10/09) Climate change a major cause of child mortality: Study (3) NEW DELHI: Climate change, besides other factors like poverty, is one of the main causes of high child mortality in the world today, a study by an international charity Save the Children said Monday. Respondents in India and China, two of the 14 countries that the survey was carried out in, acknowledged the fact. More than 400,000 children die within 24 hours of their birth in India alone every year - the highest anywhere in the world, the study, released globally Monday, said. Globally nine million children die every year before the age of five -- that is one child every three seconds. Citing a number of explanations backing up their finding, the report said that climate change already affects 250 million people - half of them being children - in a year. "In the next 20 years, it is estimated that climate change and other factors will increase the number of people affected by disasters by more than 300 percent. Already climate change is affecting children's health and access to food and water," the report said. Change in climatic conditions, which cause floods and increasing temperatures, further cause child killer diseases like malaria and diarrhoea. "Malaria already kills 800,000 children under five each year. Rising temperatures will increase the geographical range and seasonality of the disease. In some areas where temperatures were previously low enough to keep malaria at bay - like the Kenyan highlands - the average temperature has increased so as to increase the risk of transmission," the report said. "If global temperatures increase by two degrees, an additional two-three million people will experience water stress, thus contributing to water borne diseases," it added. While poverty was cited as the main threat to children's lives in 14 countries that the survey was carried out in, including Australia, Canada, Britain and the US, only China cited climate change as the main reason while India also identified it as a major challenge. The study is part of Save the Children's 'Everyone' campaign to reduce child mortality. (Times of India 6/10/09) Study: 2 million babies and mothers die at birth (3) More than 2 million babies and mothers die worldwide each year from childbirth complications, outnumbering child deaths from malaria and HIV/AIDS, according to a study. The study, released Tuesday at the International Federation of Gynecology and Obstetrics world congress being held in Cape Town, also showed that such deaths could be easily avoided. "The world will continue to miss the unheard cry of the 230 babies who die every hour from childbirth complications," unless there is better planning and implementation of policies, according to the study. Some 1.02 million babies are stillborn and another 904,000 die soon after birth. By comparison, 820,000 children die from malaria and 208,000 die from HIV/AIDS worldwide. About 42 percent of the world's 536,000 maternal deaths also occur during childbirth, according to the study. Deaths in Africa and South Asia account for three-quarters of the maternal and infant deaths. The research was led by Save the Children, the Gates Foundation and Johns Hopkins University with investigators from a dozen countries. It was published in the October edition of the federation's journal. "The huge numbers hide multiple personal stories of loss," said Joy Lawn, who runs Save the Children's Saving Newborn Lives campaign. "Each death is a tragedy to a family — actually a double tragedy since almost all these deaths could be prevented." The report said that many of the deaths could be avoided with improvements in basic health care, and training for local health care workers to perform emergency cesarean sections and other lifesaving techniques. Lawn said she hoped that the study would be used by countries to ensure money was invested where it was needed. Poverty is one of the main causes of these deaths. In wealthier countries most women give birth with a skilled attendant while in poor countries, few women do. Most deaths also occur in remote rural areas where there are few doctors and nurses. Each year, 60 million of the world's 136 million births occur outside health facilities, and only one out of every five babies born in African hospitals are cared for by skilled staff. Lawn told The Associated Press that researchers were taken aback by the shocking figures and the lack of attention given to these mothers and their babies. "It is seen as women's business. Stillbirths don't count. Sometimes the deaths of women don't even count," she said. However, she said that developments in Malawi show some signs of encouragement. The country, located in southern Africa, has only three pediatricians for about 12 million people. Yet, 60 percent of births took place in a clinic or hospital, she said, adding that the majority of cesarean sections were performed not by doctors but by trained health workers. "They knew they didn't have a lot of money or people and so had to be strategic," she said. The authors of the research welcomed the $5.3 billion committed by world leaders to maternal and child care at last month's United Nations General Assembly.(Sify News 7/10/09) Diarrhoea kills 1.5 mn children annually: UN (3) Diarrhoea, which can be corrected through inexpensive and simple means, kills an estimated 1.5 million children each year, a UN study released on Wednesday showed. The number of children in the developing world dying of diarrhoea outpaces the combined youth fatalities from AIDS, malaria and measles, according to research done by the World Health Organisation (WHO) and the UN Children's Fund (Unicef). Ann Veneman, the head of Unicef said this was a "tragedy." "Inexpensive and effective treatments for diarrhoea exist, but in developing countries only 39 percent of children with diarrhoea receive the recommended treatment," Veneman said. A new vaccine was developed for Rotavirus, an organism responsible for more than 40 percent of all diarrhoea, but it remains out of reach in most of the developing world, the UN said. Well over two billion people globally do not have adequate sanitation facilities, UN figures have shown, while 88 percent of diarrhoeal deaths are attributable to unsafe water, inadequate sanitation and poor hygiene. "Access to clean water and good hygiene practices are extremely effective in preventing childhood diarrhoea," WHO and Unicef said jointly. Meanwhile, the UN was pushing forward Thursday a Global Hand-washing Day, the second time the international body was supporting such an initiative. The day "shines a spotlight on the importance of hand-washing with soap and water as one of the most effective and affordable health interventions," Unicef said ahead of the event, which is running under the slogan "clean hands save lives." In one example, the UN estimated that hand washing with soap can reduce the incidence of diarrhoeal disease by over 40 percent, though many in the world remained without access to the basic products required for this simple and inexpensive act.(Hindustan Times 16/10/09) Half of India's children malnourished, says NGO report (3) New Delhi, October 16, 2009: As the world observes World Food Day on Friday, India, with 47 percent of its children under the age of six malnourished, ranks below countries like Bangladesh and Nepal on the state of hunger, a report says. According to the report by ActionAid, an international NGO, India stood at the 22nd spot amongst a list of 51 countries, like Australia, Britain, the US, Nepal and Bangladesh. Anne Jellema, ActionAid's international policy director, talking about the report, said: "It is the role of the state and not the level of wealth, that determines progress on hunger." India's case showed a lot of contrasts. While the country ranked amongst the first three developing countries on the indicator for social protection, because of poor implementation over 30 million Indians have joined the ranks of hungry since mid-1990s, the study revealed. Babu Matthew, country director for ActionAid India, said: "The dark side of India's economic growth has been that the excluded social groups have been further marginalised, compounding their hunger, malnutrition and even leading to starvation deaths." Meanwhile, China has been able to cut numbers of its hungry people by 58 million in ten years through strong state support for small farmers, the report said. India ranks sixth among developing nations in terms of legal framework for addressing hunger and food rights. Brazil is ranked first under this parameter. The ActionAid report said that India has some of the best legislations for social protection amongst the developing nations on nutrition, free school meals, employment guarantee, and food subsidy for the poor and pension for vulnerable groups. However, talking about poor implementation of laws and schemes which results in them becoming futile for the common man, Amar Joyti Nayak, food rights head of the NGO, said: "Implementation remains a massive challenge in the absence of recognition of rights of the poor". "Entitlements have to be delivered on the ground by empowering the communities and enforced earnestly with greater political will by the government," he said. "In a year when poor are reeling under crop loss due to droughts and floods in India, focus must be on supporting agriculture, especially subsistence and women farmers," Nayak added. The report said that although the farm loan waiver enabled a boost in investment to agriculture in 2008, longer term interventions are required. Delay in payment of wages through the National Rural Employment Guarantee Act (NREGA) further ails those who have been already starving. Jellema said: "Massive and urgent support to poor farmers, and social welfare programmes for vulnerable groups, are needed to reverse growing global hunger. At the World Food Summit next month, donor countries need to announce an additional 23 billion dollars to support these measures." (Hindustan Times 16/10/09) Maternity Mortality Rate in State (3) The rate of maternal mortality in Madhya Pradesh is the highest in the country. Everyday nearly 25 expectant mothers die due to a host of reasons like ignorance, diseases related to pregnancy, poverty and ill-health. First there was news of high rate of child mortality in the State due to malnutrition. The Women and Child Welfare department of the state government did not conduct nutritional programmes for children properly and misused the fund allotted for it. According to a report of UNICEF, in one year 498 expectant mothers die within 48 hours in the state. Around 11 lakh infants take birth every year in the state. Less or more the same condition is in Orissa and Bihar. Women in rural areas do not get medical check-up and treatment facility in pre natal cases. Only 10-11 per cent expected mothers avail these facilities. Lack of roads and safe drinking water facilities in rural areas are the major reasons even after 62 years of independence. However, road and rural development activities are now taking place in the rural areas. Courts are being established in villages. It is definite that progress in rural areas would be seen with these village oriented programmes. The state government should connect all the villages with mobile hospitals through these schemes. Even after several efforts and endless speeches of the leaders, the government doctors are not ready to work in villages, hence it would be practicable that mobile hospitals could function if roads are constructed. Several developmental schemes have become a joke in India. Rajnarayan was Union Health Minister in PM Morarji Desai's Cabinet in the year 1977. He had a good physique. He had toured England and seeing mobile hospitals there he was much impressed. High quality mobile hospitals were also established in India then. Madhya Pradesh had also got some of them. How many of them were conducted in Madhya Pradesh it is not known. Chief Minister Shivraj Singh Chouhan should find out about these mobile hospitals and what happened to them. It might be possible that they got missed during investigation or once again the imported mobile hospitals from London have started. (Central Chronicle 16/10/09) Encephalitis claims two more lives in UP; toll mounts to 409 (3) Gorakhpur (UP): Two more children succumbed to encephalitis at BRD Medical College Hospital here, raising the death toll in the disease to 409 since January this year, a health official said today. Additional director, health, L P Rawat, said while two children died in the past two days, 49 fresh cases of suspected encephalitis were admitted to the hospital. Currently, 257 patients of the brain fever are under treatment at BRD hospital, while 33 others are admitted to various government hospitals in the region, he said. A total of 2428 patients suffering from Japanese Encephalitis and Acute Encephalitis Syndrome (AES) have been admitted to different hospitals this year, he added.(DNA 18/10/09) Malari kills 111 people in Mizoram this year (3) Aizawl: Malaria remains the main killer disease in Mizoram and has claimed at least 111 lives this year between January and August, state health department officials said here today. The officials attributed the high incidence of malaria in the state to long spell of drought and erratic monsoon rain. The health department urged the people to take preventive measures and also asked the public to make maximum use of the 1,283 Drug Distribution centres from where malarian drugs are distributed to the affected free of cost. (DNA 23/10/09) 12 cases of unnatural deaths will be re-opened (3) Mysore city police have decided to re-open 12 cases of ‘unnatural death’ of women reported in and around Mysore sub-urban bus stand in the last five years. This is, in the wake of Mohan Kumar’s arrest, who is accused of killing 19 women. Mysore City Police Commissioner Sunil Agarwal told Deccan Herald, after going through police records of suspicious death of women in the age group of 20-30 in lodges near bus stand, the FSL report had confirmed of one death due to cyanide. The cause of death of 11 other women had been attributed to poisoning, pesticide and tuberculosis by the FSL. The department was reexamining the records to see whether it corroborates with the statement of teacher-turned-serial killer Mohan Kumar. After the bodies were recovered from the toilets of bus stands, the police have closed the file with the permission of executive magistrate. The police commissioner said, if necessary, the bodies would be exhumed. Interestingly, there were no claimants for any body. As per procedure, after postmortem and collecting viscera, the unclaimed bodies are kept for sometime and then disposed of after certain time, by taking pictures of victims for record purpose. Even if they exhume now, the cause of the death could be ascertained thanks to latest technology. The services of police officers during whose period those deaths took place, would be utilised to get more information. The department would also reopen all those cases and convert those cases into murder from ‘unnatural death’, after collecting concrete evidence. Sunil pointed out that the accused’s statement was not tallying with that of police records being maintained by the police station concerned. The Mysore police, if needed, would move a body warrant in Dakshina Kannada court to secure the custody of Mohan Kumar, as majority of the cases had been reported in Mysore. A circle inspector attached to Lashkar police station attended a meeting in Mangalore on Saturday. The police would take suitable decision depending upon the outcome of the Mangalore’s meeting, he added. However, according to preliminary investigations, Mohan Kumar may have killed at least four women in Mysore, sources told Deccan Herald. The parents of two such victims, who were identified later, are also likely to be summoned for investigation, they added.(Deccan Herald 24/10/09) Rural women exposed to DDT likely to have boys with urogenital birth defects (3) Washington, Oct 24 : Rural women exposed to DDT-sprayed to reduce malaria-are likely to give birth to boys with urogenital birth defects (UGBD), say researchers. The research led by the University of Pretoria in South Africa showed that women who stayed at home in sprayed villages, rather than being a student or working, had 41 per cent more baby boys with UGBDs, such as missing testicles or problems with their urethra or penis. The authors suggest this is because they spent more time in homes where domestic DDT-based sprays are still commonly used to kill the mosquitos that cause malaria, even in areas where organised mass spraying no longer takes place. "If women are exposed to DDT, either through their diet or through the environment they live in, this can cause the chemical to build up in their body," said lead author Professor Riana Bornman from the University''s Department of Urology. "DDT can cross the placenta and be present in breast milk and studies have shown that the residual concentration in the baby''s umbilical cord are very similar to those in maternal blood. "It has been estimated that if DDT exposure were to cease completely, it would still take ten to 20 years for an individual who had been exposed to the chemical to be clear of it. “Our study was carried out on boys born between 2004 and 2006, five to nine years after official records showed that their mothers had been exposed to spraying. “Although most countries have now banned the use of DDT, certain endemic malarial areas still use indoor residual spraying with DDT to decrease the incidence and spread of the disease, which is caused by mosquitoes," Bornman added. The research team suggests that educating people living in the DDTsprayed communities about ways of protecting themselves from undue DDT exposure needs to be carried out as a matter of extreme urgency. "We are now carrying out further research to find out how indoor spraying using DDT-based products affects humans and how this risk can be reduced," said Bornman. The study appears online in UK-based urology journal BJUI. (New Kerala 24/10/09) Understand social inequalities to counter TB (3) PUNE: The failure of the tuberculosis (TB) control programme in India stems from the failure to interpret biomedical factors in the light of social inequalities. This is the reason why TB has remained one of the biggest causes of death for over 40 years, said research associate Sachin Atre from the Centre for Health Research and Development. Atre was speaking at a special session on tuberculosis organised by the Advocacy to Control Tuberculosis Internationally (ACTION) project, an international partnership of advocates working to mobilise resources to treat and prevent the spread of TB, on Sunday. Elaborating on the reasons governing the failure of TB control programme, Atre said, "Drug resistance is often attributed to a patient's non-compliance with the therapeutic regimen. Non-compliance, however, has many causes, such as poverty, gender discrimination, homelessness, and side effects of the anti-TB drugs themselves, and how they affect individuals in different settings," said Atre. "Functioning of the immune system is closely associated with a person's nutritional status. A poor nutritional status also affects drug absorption, resulting in sub-therapeutic serum drug levels, which may lead to non-response to drug therapy," said Abhay Kudale, general secretary of Maharashtra Association of Anthropological Sciences. (Times of India 26/10/09) MP becomes first state in India to top IMR for 6th time: Report (3) Bhopal: Madhya Pradesh has got the unenviable distinction of becoming the first state in the country to top the Infant Mortality Rate (IMR) for the sixth time in a row.Madhya Pradesh had replaced Orissa as the state with the highest IMR in the country about six years ago and since then, the former is keeping this stigma on its head. "Madhya Pradesh has the highest 70 IMR in the country in 2008 also even after it has decreased by two points in the state in comparison to 2007 when IMR was 72 at per thousand live births," says the latest bulletin of Sample Registration System (SRS) of the Registrar General of India. Orissa, which stands second in worst performing states in IMR in 2008 recorded 69 infant deaths and managed to keep the IMR below that of Madhya Pradesh consistently for the last six years. Kerala achieved the status of best performing states in IMR in 2008 where only 12 infant deaths were reported during the period followed by Tamil Nadu (31) and Maharashtra (33). The SRS bulletin also shows that Madhya Pradesh continues to be even worse in case of the female children and the IMR for girl children is 72 in the state as compared to 68 for boy children.(DNA 1/11/09) Rs 2,400 cr mega budget for battle with cancer (3) Mumbai: India will spend Rs 2,400 crore on cancer control during the 11th Five Year Plan, 10 times more than the allocation during the previous Plan period. Health Minister Ghulam Nabi Azad made the announcement on Sunday at the inauguration of the Mobile Outreach Project at Tata Memorial Cancer Hospital TMCH). The focus would be on community-based cancer control strategies, he said. Apart from the budget for the National Cancer Control Programme, Azad also announced a unique scheme for patients living below the poverty line (BPL) under the Health Minister’s Cancer Patient Fund. “The fund has been established by the government with seed money of Rs 100 crore and state governments are expected to contribute,” Azad said. “Up to Rs 1 lakh of a BPL patient’s treatment costs can be supported at any of our 27 regional cancer centres and 40 oncology wings in institutes under the National Cancer Control Programme, or at any public sector health facility.” (Indian Express 2/11/09) Action plan against child marriage in State (14) GUWAHATI, Nov 1 – The Law Research Institute, Eastern Region, Gauhati High Court, the Department of Social Welfare, Government of Assam and UNICEF have come forward to develop an action plan for prevention of child marriage in the State. Child marriage is prevalent in certain communities, particularly the minority community and the tea tribes despite the fact that rapid changes have swept across the State. Girls as young as 11 years of age are forced to leave school and married off, most often to men double their age. This problem has led to other problems like maternal mortality and infant mortality. The Law Research Institute has undertaken a study covering five districts, Kamrup, Darrang, Dhubri, Lakhimpur and Dibrugarh to assess the factors behind the early marriage of the girl child. The study will include Kamrup Metro also as young girls in the poverty pockets in the capital city are married off against their wishes. “Our objective is to study the reasons for the practice of child marriage,” said Dr Jeuti Barooah, director of the Law Research Institute. “We undertook our study since August this year and we are hopeful to complete our study very soon,” informed Dr Barooah. Disclosing some of the findings of the yet to be completed study, Dr Barooah said, “Poverty and illiteracy are the major reasons for the practice of child marriage,” adding that tradition too was a factor behind early marriage of the girl child. The study team has also stumbled upon some pre-conceived community notions that have encouraged child marriage. One such notion is that if girls are not married in tender age they will never get married. The communities practising child marriage lacked legal awareness, the study found. “A conservative mentality, male dominance and religion have hindered the growth of progressive thoughts in some communities which has caused miseries to the girl child,” observed Dr Barooah. (Assam Tribune 2/11/09) Every minute, a kid dies of pneumonia (3) BANGALORE: India looks indeed like a leading Third World country: malnourished children breathe polluted air and suffer from lack of nutrition and hygiene. It leads the world with 27% of the global pneumonia cases. Worse, every minute, a child dies of pneumonia in India, followed by Afghanistan, China, Pakistan and Bangladesh. Annually, two million children under five die from it, and pneumonia contributes to almost 20% of childhood mortality cases — more than AIDS, measles and malaria combined. So says WHO data published in the Lancet Journal in Sept. WHAT CAUSES PNEUMONIA? In India, the main culprit is malnourishment — here, 47% of the paediatric population suffers from low immune systems. “Lack of good nutrition, polluted air and poor hygiene are the main causes of pneumonia. Premature babies are at higher risk, so by improving maternal nutrition, low-birth premature babies can be prevented and by tackling malnourishment, improving immune system and controlling air pollution, pneumonia can be prevented. Better access to antibiotics can control mortality due to the disease,” said Dr H Paramesh, national president for respiratory disease chapter of the Indian Academy of Paediatrics. Environmental factors have increased a child’s susceptibility, especially among in homes, exposed to pollution caused by using biomass fuels for cooking and parental smoking habits. India accounts for 40% of worldwide childhood pneumonia cases, and among children who survive Hib meningitis, 30% suffer from disabilities. (Times of India 2/11/09) Goa has country’s lowest infant mortality rate (3) NEW DELHI, NOV 1: Goa has the country’s lowest infant mortality rate (IMR), at 10 deaths per thousand live births. Kerala’s IMR is 12, while Manipur’s is 14. The average IMR for the country as a whole has gone down marginally, from 55 per thousand live births to 53, over the last one year, say the latest figures released by the Registrar General of India (RGI). IMR is the number of deaths of infants under one year of age in any given year, per thousand live births. It is often used as an indicator of the level of health in a country. According to the United Nations, the current world infant mortality rate is 49.4. Other states, like Delhi (35), Maharashtra (33), Tamil Nadu (31) and West Bengal (35), as well as union territories Puducherry (25) and Chandigarh (28) are better than the world average, while states like Karnataka (45), Gujarat (50), Madhya Pradesh (70), Uttar Pradesh (67), Rajasthan (63), Orissa (69) and Assam (64), remain areas of concern. The IMR in urban areas was 36 in 2008 (compared to 37 in 2007). In rural areas it was 58 (61 in 2007), according to the report. The figures may seem unimpressive compared to the IMR in developed nations – it is 3.2 in Japan and 3 in Singapore – health ministry officials say the steady decline over the last three years is a positive sign. India hopes to reduce its IMR to 30 per thousand live births by 2012. (Herald 2/11/09) Malnutrition, a multifaceted problem: Stagg (3) Bhopal, Nov 3: There is a lot to be done on the delivery of services end. The state government is doing a good job, but delivery of services needs a lot of improvement. There are technical reasons why the state government denies malnutrition deaths. Almost half the high figures of child immortality deaths are from pneumonia and other diseases. Most of these deaths are indirectly related to malnutrition, but as doctors certify that the deaths are from pneumonia and other diseases, they are not recorded under malnutrition. DFID officials claimed. Department for International Development (DFID) of United Kingdom today suggested the Madhya Pradesh government to adopt Thaliand model in combating malnutrition problem in the state. The model has miraculously reduced malnutrition to half in Thailand, and thus could be adopted in Madhya Pradesh also, claimed the officials. ''Malnutrition is a global problem, particularly for the developing and poor countries. The problem does not related to food alone, but it includes multidimensional problem and it is a challenge before the countries to overcome the problem. Madhya Pradesh government has taken initiatives to cope with the problem,'' Mr Anderson told media here. Mr Anderson said DFID was spending Rs 2000 crore annually in India for poverty reduction purpose and in Mahdya Pradesh the organisation had spent Rs 300 cr per annum. He said DFID was providing financial assistance to the Madhya Pradesh government in the sectors like health, power sector, rural livelihoods project and urban services of the poor. The DFID team also visited several slums in the state capital to oversee the implementation of the projects and interacted with the people, he said. Talking about the national scenario, Mr Anderson said DFID was supporting programmes at the national level as well as in the five focussed states -- Bihar, Madhya Pradesh, Orissa, Andhra Pradesh and West Bengal - in India. He said DFID worked in partnership with the Centre and the state governments to achieve its national poverty reduction targ ets and internationally agreed Millennium Development Goals. ''Our programmes are focussed on creating an enabling environment for sustainable and equitable economic growth and to improve access to better quality services for poor people, particularly in health and education,'' Mr Andersorn asserted. A delegation of DFID, led by its Head Michael Anderson and British High Commissioner Richard Stagg, today met Chief Minister Shivraj Singh Chouhan and senior officials and apprised the progress of DFID's supported progammes in the state. Mr Anderson said during their interaction with Mr Chouhan they had shared their views on the issue and the DFID delegation informed the CM that the Thailand model to combat malnutrition was very effective and suggested the state government to adopt it to combat the menace. He said Mr Chouhan was excited about the proposal and agreed to accept it. Mr Stagg, who met state Chief Secretary Rakesh Sahni today, said that he had an elaborate talks on issues of energy area improvement, industrial scenario, education, health, nutritious diet, climate change and possibilites of cooperation of British government's International Development Department. He said that a meeting with state Urban Administration and Development Minister Babulal Gaur was very fruitful. The Minister apprised him abut the urban development programmes undertaken by the state government in several cities in the state. Mr stagg said UK's commitment to DFID was very strong and despite a sharp fall in GDP in the country, it did not slash its funds for DFID. (Central Chronicle 3/11/09) Corporation urged to screen women for cancer (3) CHENNAI: If the Chennai Corporation is able to provide every woman in the city at least one gynaecological screening, it will be adequate to detect and even prevent the top two cancers among women, V. Shanta, chairman, Cancer Institute (WIA), has said. She said every woman coming to the Corporation’s health centres must also be subjected to an examination of the gynaec tract. This would be useful to identify a number of cases of cervical cancer in pre-cancerous stages. In 1962, when over 9000 women were screened for cancer in four districts in a project she had participated in, 20 were found to have cancer, 18 of them in very early stage. On the other hand, she said, if one looked at hospital records, 75 per cent of the patients came with advanced disease. “We have to get the message out that cancer need not be fatal,” Dr. Shanta said. “Today we are curing one out of three patients and we have the potential of curing two out of three patients, when they come early enough,” she said, speaking at the National Cancer Awareness Day event at Cancer Institute for Corporation doctors. Cervical cancer and breast cancer are more common in women, both of which are detectable at the pre-cancerous stage, and thereby preventable, she said. Cervical cancer was more common among women in lower socioeconomic groups and triggered by chronic genital infections, inadequate postpartum care and lack of education about sexual hygiene. With men one of the prominent causes of cancer is tobacco use, Dr. Shanta said. Tobacco usage caused 40 per cent of the cancers in men with cancer of the mouth, food and wind pipe and the lungs topping the list. Getting rid of tobacco with seriously implemented antismoking legislations would cut down the numbers dramatically. S. Vincent, member-secretary, Tamil Nadu State Council for Science and Technology, suggested that the Institute consider setting up clubs in schools and colleges akin to the Red Ribbon Clubs, which disseminate information about HIV/AIDS. He complimented Cancer Institute for its efforts in pushing the ban on smoking in public places and its implementation. Dr. Vincent also urged the staff at the Institute to submit project proposals to the Council for funding. Charumathi, District Family Welfare Officer, Chennai Corporation, said that the civic body was paying a lot of attention to prevention and detection of cancer among women. E. Vidhubala, Tobacco Cessation Cell, Cancer Institute, spoke about reducing the health burden through tobacco cessation interventions. (The Hindu 8/11/09) Difference between men's and women's health (3) The World Health Organisation said on Monday women tend to receive poorer medical care than men. click here Following is a breakdown of the differences between male and female health in children, adolescents, adults and elderly people, according to the United Nations health agency's report: Infants and children -- Death rates and causes of death are similar among boys and girls until 9 years of age. -Pre-term birth, birth asphyxia and infections are the main causes of death in the first month of life, when mortality is the highest. Pneumonia, diarrhoea and malaria are the main causes of death during the first five years of life. -- Girls are more likely to suffer sexual violence than boys. Adolescents-- Teenaged girls are at risk of unsafe, unwanted and forced sexual activity that can make them vulnerable to HIV AIDS, other infections, unwanted pregnancy and unsafe abortion. -- Women catch sexually transmitted infections more easily than men for biological reasons and also due to lack of access to information as well as health services. -- Pregnancy-related complications are among the main causes of death among girls aged 15 to 19 in developing countries, with unsafe abortions accounting for a large number of such deaths. Adults-- Every year, about 500,000 women die from giving birth, almost all in developing countries. -- Poorer nations lack services to screen and treat cervical cancer, the second most common type of cancer among women. -- Women are more susceptible to depression and anxiety than men. Some 73 million women worldwide suffer a major depressive episode every year. Mental disorders following childbirth affect about 13% of women within a year of delivery. -- Women typically prepare most of the family food, and thus are most exposed to indoor smoke from burning solid fuels for cooking, a phenomenon most common in poor countries. The burden of chronic obstructive pulmonary disease, a lung ailment also related to smoking, is 50% higher among women than men. -- Women suffer far more fire-related injuries and deaths than men, with most related to cooking accidents and others the result of intimate partner violence. Burns are a leading cause of death among women aged 15 to 44 in Southeast Asia. Elderly -- Though often considered a "male" problem, heart attacks and stroke are the main killers of older women. Cardiovascular disease is often undiagnosed in women. -- Because they live an average of six to eight years longer than men, women represent a big proportion of all older people. Their main problems in older age, often untreated, include poor vision, hearing loss, arthritis, depression and dementia.(DNA 9/11/09) 5000 under-5 children die in India everyday: UNICEF (3) NEW DELHI: Despite a decrease in child mortality figures, 5,000 children under the age of five die in India everyday due to preventable. Within the under five mortality rate, the maximum 96 per cent of children who die belong to the Scheduled Tribes, 88 per cent to Scheduled Castes and 59 to general population. "It is early marriage and inadequate health care of women which adversely affects the survival of their children," said Karen Hulshoff, Country Representative of UNICEF in India said. The report says malnutrition rates in India continue to be very high. Though the percentage of malnourished children below the age of three has decreased from 52 per cent to 46 per cent, it is still way below the Millennium Development Goals (MDG). Forty seven per cent of women had deliveries with skilled health provider, it said. A majority 56 per cent women use contraceptives. Condom use was high at 61 per cent for women and 52 per cent for men, it said. Knowledge about HIV/AIDS has also increased. While 34 per cent of men are aware of AIDS, in women the corresponding figure was 24 per cent. Between 1990 and 2006, the use of improved sanitation in India has doubled. Reaching the MDG target remains a great challenge and requires accelerated efforts to outpace population growth, Hulshoff said. The report "State of the World's Children", says that the mother's level of education is one of the key factors in reducing child mortality. As far as under-five mortality rate was concerned, 95 per cent of the dead children were born to mothers who had no education. The child mortality rate decreased from 80 per cent to 53 per cent in 2008. The target to achieve the MDG was 40 per cent. School attendance rates are still dropping at secondary education levels, specially among girls. The school attendance rates were high in the age group of 6-10 years at 85 per cent for boys and 81 per cent for girls. While the school attendance rate for the general population is high at 84 per cent, it is 74 per cent for Scheduled Castes and 68 per cent for Scheduled tribes. Birth registration in India improved significantly from 58 per cent in 2001 to 69 per cent in 2008. There has also been a decline in the incidence of child marriage in India over the years. The proportion of women marrying before reaching the age of 18 in India though is still very high. (Times of India 20/11/09) PIL brings to fore poor health indicators in Gujarat (3) Ahmedabad: Gujarat high court has admitted a public interest litigation (PIL) with regard to the poor health indicators and gaps in health infrastructure in Gujarat. The PIL was filed by Dinesh Bagda, chairperson of village social justice committee and a resident of Amreli. The PIL draws attention to the poor health indicators and health infrastructure in general, and is concerned with various statistical aspects highlighted by the Health Review- Gujarat 2007-08 and other surveys and heath bulletin in particular. The Health Review-Gujarat 2007-2008 conducted by the Commissionerate, Health, Medical Services and Medical Education, Gujarat, has puts forward startling facts described as under: (I) Maternal Mortality Rate (MMR) -- it is 172/lakh live birth, it means approx 24,000 (as per 2001 census) pregnant women lost their life due to maternity related reasons, which is very high. It suggests that the reach of public health services to such women, even in time of emergency, is either not accessible or not preferred by most families. Similarly, the National Family Health Survey- III (2005-06), gives a disturbing picture of Maternal and Child health care in Gujarat. The health infrastructure in Gujarat as per the RHS Bulletin, March 2007, ministry of health & family welfare, government of India, discloses shortage of health personnel. The PIL states that there is a vacancy of ANMs in 89 sub-centres of Amreli district alone. There exists a linear chain of poor public health infrastructure, which discourages people to avail public health facilities/services, and which in turn leads to poor public health condition. The petitioner (Dinesh Bagda) has prepared certain data regarding the health condition of people in the state. The child mortality rate in the state is also very high. Around 1-20 children die within a year, while 1-16 children die before reaching five years of age. This apart, the infant mortality rate (IMR) in rural areas of Gujarat is 61 per cent higher than in urban areas of the state and girls face a higher mortality risk than boys. Similarly, the Ante-Natal Care (ANC) in the state is very poor; one in 8 women (13) delivers without ante-natal care. Of these 37 per cent belong to lower income group. Even when women receive ante natal care, they do not receive several other services needed to monitor their pregnancy. Gujarat is also one of the few stateswhere full vaccination coverage has declined in the past seven years. BCG and measles vaccines have increased marginally, but the coverage of three doses of DPT and Polio has dropped. In spite of the Pulse Polio Campaign, one third of the country's children still haven't received the recommended three doses of polio vaccine. (DNA 20/11/09) Gaps in labour management raises maternal mortality: study (3) CHENNAI: Gaps in the management of the third stage of labour, the period between the delivery of the baby and the delivery of the placenta, are raising the risk of maternal mortality in Tamil Nadu, according to a study. The study undertaken in eight villages as part of a Health and Population Innovation Fellowship granted by the Population Council, Delhi, found that the practice of the standard Active Management of Third Stage Labour (AMTSL) was very poor. And, where they were put into practice the measures did not adhere to guidelines, the study said. AMTSL is the primary intervention that could reduce by 50 per cent the incidence of Post Partum Haemorrhage which is the leading cause of maternal deaths. “The study generated enough evidence to show that the simple intervention was not accessible or available to women in a Government setting,” said Subha Sri, who authored it. In her remarks, Girija Vaidyanathan, Mission Director, National Rural Health Mission, said the Government had initiated AMTSL sensitisation programmes starting with nurses. Asha Oumachigui, former professor, department of O&G, JIPMER, Puducherry chaired the session. Earlier, R. Porkai Pandian, additional director of public health, released the study report. (The Hindu 23/11/09) Seven new dengue cases in Delhi, tally up to 1,094 (3) New Delhi: The national capital on Tuesday recorded seven new dengue cases, taking the total number of people affected by the mosquito-borne disease to 1,094, said a health department official. "There were seven new confirmed cases in the last 24 hours. The total number of dengue affected people is now 1,094," the health official stated. Until now, there have been two confirmed deaths because of dengue in the city - one of a 15-year-old boy and the other of a 9-year-old boy. Of the total cases, 1,081 were Delhi residents and 13 were from outside the city. According to the health department, the number of dengue cases will go down in the coming days since the carrier-mosquitoes causing the disease cannot breed in temperatures below 15 degrees celsius. (DNA 1/12/09) Dengue cases in Delhi rise to 1,118 (3) NEW DELHI: Delhi reported five new dengue cases on Friday, taking the tally of those affected by the mosquito-borne disease to 1,118, a health department official said. "On Friday, five new dengue cases were reported. The cumulative number of people affected by the disease is now 1,118," a senior health department official told IANS. Of the total affected, 14 patients are from outside Delhi. Three people have died due to the disease this year in Delhi. The third dengue death, of a 45-year-old man, was confirmed Wednesday by the health department. The earlier two deaths were of a 15-year-old and a nine-year-old boy. With the onset of winter, the health department is hoping that the number of dengue cases will drop since the breeding of the carrier mosquito cannot occur below 15 degrees Celsius. Last year, the national capital reported two dengue deaths and a total of 1,312 cases. (Times of India 4/12/09) Climate change will hit 175m kids every year’ (3) NEW DELHI: A new report suggests that 175 million children will be affected every year by frequent natural disasters caused due to climate change. Painting a grim future, a report by child rights NGO Save the Children said climate change was the biggest global health threat to children that could increase risk of deaths due to diarrhoea, malnutrition, malaria and other diseases because of reduced community access to clean water, nutritious food and hygienic surroundings. The report — ‘Feeling the Heat: Child Survival in a Changing Climate’ — links access to basic facilities with climate change. It said that 2 million children under 5 years of age die each year in India. Pointing out that this was the highest number anywhere in the world, the report said children were dying from a small number of preventable diseases, such as diarrhoea, malaria and pneumonia. “Climate change will make these conditions worse, placing children at greater risk, because it will reduce poor communities’ access to clean water, reduce their ability to grow nutritious food, increase food prices and allow malaria mosquitoes to spread,” the report said. The average number of natural disasters has increased from 200 a year to more than 400, and this is predicted to increase by as much as 320% in the next 20 years. The report said climate change disasters would also continue to increase malnutrition and certain diseases that often kill children. It estimated that malnutrition, which affects 178 million worldwide and is associated with up to 3.2 million child deaths each year, would affect 25 million more children by 2050. Already, one-third of all malnourished children live in India.Calling for world leaders to sign a deal at Copenhagen, Save the Children CEO Thomas Chandy said, “Climate change has put India at risk of not meeting the millennium development goals, and even taking several steps backwards from what has been accomplished to date. Children, who are not responsible for climate change, will be the ones who are hardest hit.” The report added that India lagged behind in its commitment to reducing under 5 mortality by 2015. Given present trends, India will not meet MDG 4 until 2020,five years after the promised date. “We fear that any progress India makes in reducing child mortality will be further slowed down by the effects of climate change,” Chandy said. (Times of India 7/12/09) NE states get $128.5 mn grant for AIDS, TB, malaria eradication (3) Imphal, December 08 2009: International aid agency Global Fund Tuesday announced a $128.5 million grant for India to fight AIDS, tuberculosis and malaria. The Geneva headquartered organisation said $38.1 million will go to malaria prevention and treatment efforts in the seven states in the northeast region - Arunachal Pradesh, Assam, Manipur, Meghalaya, Mizoram, Nagaland and Tripura. This includes efforts to achieve near universal coverage of long-lasting insecticide treated nets by 2015 in these areas. 'I am very pleased we are able to support India in its fight against the three diseases,' said Michel Kazatchkine, executive director of the Global Fund. 'I hope our collaboration continues and expands, helping India to reach the health-related Millennium Development Goals,' he added. Of the newly approved grants, $69.4 million will be provided for expanding care and treatment services for tuberculosis (TB), particularly for multi-drug resistant tuberculosis. India bears 21 percent of the global TB burden and has the highest estimated incidence of multi-drug resistant cases of any country. The Global Fund has also separately approved $18.6 million in a first of its kind multi-country HIV grant in South Asia for an initiative targeting gays and the transgender community. (E-PAO 8/12/09) Of still births, bad roads and malnutrition in Kokmar (3) KOKMAR (AMRAVATI DISTRICT): “The pain started in the afternoon,” says Sevanti Chimote. Still recovering from the harrowing experience of losing her baby, the young mother continues, “We called a jeep from Harisal and it arrived at 10 p.m.” Harisal may be only 26 km away, but a good part of the road, 16 km, is an extremely bad stretch. The drive, as a result, can take up to two hours. Ms. Chimote, who left at night on November 22, accompanied by her family, soon started bleeding. Doctors later said it was an ante-partum haemorrhage. She was given saline at the primary health centre in Harisal, but the bleeding did not stop. She had to be driven to Amravati, the nearest city in Maharashtra, a journey which takes up to three hours. Her five-year-old daughter plays around her, unmindful of the tragedy. Ms. Chimote was in hospital for three to four days and had to be given two bottles of blood. The doctors told her she was severely anaemic and that that was why she lost the baby, premature at seven months. On December 11, Health Minister Suresh Shetty suspended Amravati District Health Officer K.Z. Rathod for the substandard medicines and delivery kits in Melghat, which had ordinary razor blades instead of surgical blades. A CID inquiry has been ordered. But it not just the delivery kits; the overall health care in the region is substandard. There were three deaths due to diarrhoea in Kokmar in the Dharni taluk some time ago. One of them, Sonai Betekar (26), died at home after severe dehydration, and her son, one-and-halfyear-old Praveen, died a day later. The other casualty was a 12-year-old boy. The deaths of children in the area are purely due to negligence, says Dr. Ashish Satav of ‘Mahan,’ an NGO based in Dharni. According to official figures, from June to November 2009, as many as 325 children below the age of six have died in the Dharni and Chikhaldhara taluks, which comprise the Melghat region. In Dharni, 48 children died in August, 53 in September, and 42 in October. In November, of the total 36,264 children below age six in Melghat, only 13,604 were of normal weight. The rest are in various grades of malnutrition. Every year, at least 400 to 500 children below the age of six die in Melghat. Even in Kokmar, of the 55 children in the anganwadi, two are severely malnourished. The people get work in the nearby forest and repair the road themselves if it gets too bad. After years of demands, a State transport bus now has a service to the village, which is partially lit by solar power. The school has only one teacher who is overburdened. And it is closed most of the time as the teacher has to attend training or meetings. The people have demanded better roads, but no one has listened. In Chikhaldhara, the office of Fulmati Salame, the Child Development Project Officer, reflects the sorry state of affairs. There is no light, the telephone has been disconnected as the bill has not been paid, there is no vehicle for the staff, and some 25 villages don’t have money for the day care of severely malnourished children. Ms. Salame, the first post-graduate among the Korku adivasis, says the area continues to be plagued by low birth weight babies and severe malnutrition among the mothers as well, apart from infants. Dr. Satav points to a worsening of the health situation in Melghat. Referring to the still birth in Kokmar, he says that as per the norms of the Integrated Child Development Services, pregnant women have to be given 100 iron tablets apart from regular ante-natal check-ups. “How did they miss the fact that Sevanti was so anaemic?” he asks. “It was a fatal combination: the mother’s poor health, the bad roads and the delay in getting her medical aid, apart from the baby being premature that led to the still birth.”…… (The Hindu 14/12/09) Concern over growing number of cervical cancer cases (3) NEW DELHI: A panel of medical experts have expressed the need to tackle the growing number of women who are being diagnosed with cervical cancer in the country and advised an informed approach towards the new cervical cancer vaccine available in the India market. According to a study by eminent medical experts, world-wide five lakh women die every year, of which over lakh deaths occur in India alone. “This is the only cancer which can be prevented by vaccine and which if diagnosed in its very early stage may not be life-threatening. The cervical cancer vaccines should be given in three doses over a period of six month in the age group of 10 year to 45 years,” said Rockland Hospital senior gynaecologist Dr. Sheetal Agarwal. “Of course there is no way to know for sure if you’re going to get cervical cancer. Certain factors can make you more likely to get cervical cancer than another woman. These are called risk factors. However, just because you have one or more risk factors does not mean you will get cervical cancer. In fact, you can have all the risk factors and still not get cervical cancer. With cervical cancer, it is rare to get the disease if you have no known risk factors, but it is possible,” she added. It is estimated that three out of four people between the ages of 15 and 49 will get an HPV infection in their lifetime. Most people with HPV never know they are infected because the virus tends to go away on its own. “There are many types of this virus. Only a few high-risk types can cause cervical cancer. The only way to tell if you have a high-risk type of HPV is to be tested. About 15 types of HPV can lead to cervical cancer and HPV types 16 and 18 causes about 70 per cent of all cervical cancers,” said Dr. Agarwal. If high-risk types of HPV do not go away on their own, they may lead to cervical cancer. Infection with persistent high-risk HPV has been shown to cause virtually all cervical cancers. “Women get into the high-risk category by having sex with someone who has the virus. Protected sex helps but not always. If you smoke, you have a higher risk of getting cervical cancer. You are twice as likely to get cervical cancer as women who do not smoke. Women with an HIV infection also have a weakened immune system. If you have HIV, it is harder for you to get rid of a high-risk HPV infection. As a result you have a higher risk of developing cervical disease or cervical cancer,” said Dr. K. K. Pandey, head Oncology Department at Rockland Hospital. (The Hindu 14/12/09) World Health Organization to send swine flu vaccine to poor countries (3) LONDON: The World Health Organization plans to start shipping swine flu vaccine to Azerbaijan, Afghanistan and Mongolia in the next few weeks, flu chief Keiji Fukuda said on Thursday. Another 32 developing countries are in line to get the vaccine soon. The UN health agency has prioritized sending the shots to northern hemisphere countries first, which are being hit harder by swine flu than countries in the southern hemisphere. The agency had hoped to send the vaccine earlier, but the effort has been delayed by manufacturing problems and bureaucracy. When WHO declared swine flu to be a pandemic, or global outbreak, in June, it warned the virus could have a devastating impact in countries across Africa with high numbers of people with health problems like malnutrition, AIDS, and malaria. Most people who catch swine flu only have mild symptoms like a fever or cough and recover without needing medical treatment. WHO has a stockpile of about 180 million swine flu shots, donated by six drug makers and a dozen countries. Countries hoping to get swine flu vaccine from WHO must meet three conditions. They have to formally ask for it, agree to certain terms and conditions on how it will be used, and develop a national plan to make sure the right people -- like health workers and those with underlying health problems -- get it first. WHO is hoping to send enough swine flu vaccine to cover about 10 percent of populations in poor countries. Countries likely won't start vaccinating their populations until a few weeks after they receive the vaccine, but Fukuda said it wasn't too late to ship the vaccine -- even though swine flu appears to have peaked in several northern hemisphere countries, like Britain and the US ``This is a virus that we don't expect to suddenly disappear," Fukuda said, adding WHO expected the virus to keep circulating for the next few years. Fukuda said it was ``premature" to consider whether the pandemic might be on the decline, and that WHO would consult experts before making such a declaration. He said flu activity this year had peaked ``extraordinarily early" and warned there were still several months of winter to come. (Times of India 17/12/09) 119 die in Malaria attack this year in Mizoram (3) Aizawl, Dec 17 (PTI) An estimated 119 people died in Malaria outbreak in Mizoram between January and October this year as the disease turned out to be the biggest killer, state health department officials said today. The increase in number of deaths is due to the fact that malaria patients approached the hospitals and health centres too late, they said. Those who died were without any medical treatment for at least four days or more and the average hospitalisation period was just two and half days, the officials said. State vector-borne diseases control sources said that out of 1,51,631 blood samples tested, 8,426 people were found to be infected with the mosquito-borne disease. (PTI 17/12/09) Chikungunya, dengue impose $1.4 billion annual burden on nation (3) MADURAI: Two vector-borne diseases – chikungunya and dengue – impose a burden of $1.4 billion on the nation every year, according to a national-level study undertaken by the Indian Institute of Management-Ahmedabad through its Centre for Management of Health Services (CMHS). The findings will soon be published in the Dengue Bulletin of the World Health Organisation and this is the first time that the cost has been quantified through scientific evaluation, said S.S.Vasan, Visiting Research Fellow, the University of Oxford, here on Friday. Speaking to The Hindu, he said the $1.4 billion cost included treatment, wage loss, doctors’ fee, productivity impact, hospitalisation and expenses incurred by family members of affected persons who visit hospitals. The study was led by Dileep Mavalankar of the CMHS and the conclusions were arrived at early this year. It was also a multi-country study covering the U.S., U.K., Malaysia and other nations, said Dr. Vasan, who was one of the co-investigators of the project. He said the cost estimate for India took into account both reported and unreported cases. “The money people have been spending on mosquito coils and funds utilised by government for vector control activities like fogging were also included to arrive at the total cost for India.” Stating that the burden was immense for India because of the breakout of chikungunya and dengue every year, he said 90 per cent of the burden was shared by Tamil Nadu, Karnataka, Gujarat, Madhya Pradesh and Andhra Pradesh. Dr. Vasan, who is also the Chief Executive Officer and Director of Oxitec, a company that promotes technology/inventions made at Oxford University, was in the city to participate in the third conference on ‘Medical Arthropodology,’ organised by the Centre for Research in Medical Entomology (CRME), a laboratory of the Indian Council of Medical Research. Earlier, he delivered a lecture explaining the newly developed mathematical model to study flight/distance covered by mosquitoes and what terrain conditions that suited them most. “There are around 3,500 mosquito species and not all of them are our enemies. The mosquitoes that cause immense burden to us in cost and health factors must be studied scientifically,” Dr. Vasan observed. The two-day CRME conference is being attended by nearly 100 scientists/entomologists form various places and is focussed on the theme ‘Integrated Disease Vector Management-Operational Research.’ (The Hindu 19/12/09) xxxxxxx
© Copyright 2026