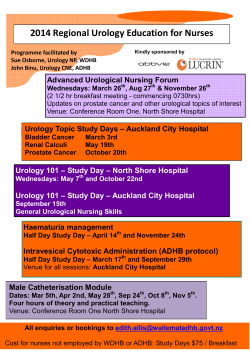
European Urology Today
European Urology Today Official newsletter of the European Association of Urology 1-7 28th Annual EAU Congress Hemorrhagic cystitis Including list of award winners Challenges in treatment 9 Prof. Maurizio Brausi Vol. 25 No.2 - March/May 2013 Neobladder and continent urinary diversion 16 Expert’s view Prof. Richard Hautmann More collaborative links, practical use of research findings Recurring messages in Milan: Collaboration and using research discoveries By Joel Vega Closer links across urological specialties and medical disciplines and the practical use of recent research findings in everyday clinical practice are among the recurring messages given by experts, opinion leaders and speakers during the 28th Annual EAU Congress held in Milan, Italy. “This meeting does not only connect us as urologists but also provide the venue for us to achieve more and work closely across disciplines, specialities and borders. Together, we can make progress,” said EAU Secretary General Prof. Per-Anders Abrahamsson (SE) in his welcome remarks at the opening ceremony held last March 15 in Milan, Italy. Abrahamsson not only noted the EAU’s role as a representative organisation but also its capacity to expand the reach of urology to other disciplines and the crucial function it performs to promote scientific research and professional development. The Scientific Programme of the five-day congress reflected the EAU’s aim to provide a fitting venue for urologists in and outside Europe, their partners from other medical disciplines and the industry to effectively collaborate for research and clinical work. With the first day presenting the views of urological associations from around the world at the Urology Beyond Europe, and the meeting of prostate cancer experts at the Conference on Prostate Cancer Prevention, the congress emphasised quality scientific presentations that aim to carefully examine controversies, debates and other issues in urooncology and urological diseases. A case discussion on male urinary incontinence Urology Award to Prof. Urs Studer (CH) (See inside pages for a complete list of awardees). In prostate cancer research, experts said the immediate need is for a direct or practical application of research discoveries in genetic markers. “Researchers understand that it is difficult to translate even excellent basic research to the clinical lab. And even when that research gets to the clinical lab, the complexity and the costs of a test can limit its use because today healthcare costs are going up very rapidly,” said Dr. Harry Rittenhouse (USA), who spoke on urinary PCA3 a t the prostate cancer prevention meeting. Core urology issues With four plenary sessions held during the congress, participants have a comprehensive view of urological issues ranging from core urology topics, urooncology, reconstructive, andrology, stones, female to At the opening ceremony the EAU honoured its paediatric urology, to name a few. The first session pioneering members and opinion leaders and examined paediatric urology and the ageing patient awarded promising young urologists. Among the top with speakers providing key messages on the benefits honours given were the Willy Gregoir Medal to Prof. and drawbacks of surgery for hypospadias, the use of Clement Claude Abbou (FR) and the EAU Innovators in artificial mesh implants in women with incontinence, “Quality is the major goal. We cover more topics every year, but you have to do that without losing sight of the quality,” said Prof. Arnulf Stenzl (DE), Chairman of the Scientific Congress Office in an earlier interview. insights in treating vesicoureteral reflux (VUR) and the value of providing personalised management for ageing patients with co-morbidities and functional problems. possible screening as long as they know the benefits and drawbacks of screening tests. Tom Hudson (IE) of the patient’s group Europa Uomo presented the patient’s view. Insights on the optimal treatment for upper urinary tract cancers were presented and discussed in Plenary Session 2 with topics such as the benefit of lymphadenectomy, the pros and cons of organsparing approaches and the role of endoscopic treatment, among other issues. Meanwhile, the session on the third day tackled lower urinary tract management with speakers examining urodynamic assessment in current practice, a lively case discussion on surgical options for male urinary incontinence and practical therapies for LUTS. “My appeal to all physicians is for us to understand each other. Please don’t use language that we don’t understand since what we need is a simple and clear explanation, which is of crucial importance,” Hudson said. “We appreciate your fantastic efforts to find cure and treatment, but cut the confusion if I may put it bluntly,” he said referring to the continuing debate on PSA screening, particularly in the US. The latest data on PDE5 inhibitors, beta-3 agonists, botuliniumA toxin, and combination therapies were presented and speakers emphasised the role of urologists to take the lead. “Urologists need to maintain control over this complex and multifaceted condition,” said Prof. Chris Chapple (GB), as he noted that more research is needed despite the radical changes in the medical treatment of LUTS in recent years. At the joint EORTC-ESUR Section Meeting “The EAU, the patients group Europa Uomo and the ERSPC all presented perspectives which added more nuance to the (PCa screening) debate…” Section Meetings Aside from the plenary sessions, seven Section Meetings were held with the day-long live surgeries attracting a full attendance. Ten live surgeries were transmitted to the congress auditorium with running commentary by the operating doctors, and annotated by moderators in the session hall. The closing plenary brought to the fore new insights in much debated topics such as prostate cancer screening and treating metastatic and castration resistant prostate cancer (PCa). Also presented were the EAU’s new guidelines on ethics of live surgery and a preview report by the prostate cancer prevention consensus group. Sixteen Thematic Sessions were also held over two days and covered various topics in urology such as minimal invasive surgery, urological cancers, surgical complications, neurourology, challenging cases to pain management, to name a few. The EAU’s view on PCa screening through PSA testing was presented by Abrahamsson who noted the importance of not denying well-informed men a At the closing session, Abrahamsson invited the audience to Stockholm for the 29th Annual EAU Congress to be held from April 11 to 15, 2014. Next year’s congress will be the third to be held in Sweden after the well-attended congresses in 1999 and 2009. Post-congress reflections Picking up what occurs below the radar is equally crucial At the 28th Annual EAU Congress in Milan, the Scientific Congress Office has again presented a programme whose format, coverage and contents reflected the intense and careful preparations which are necessary for a high quality international meeting. With around 13,000 participants, including the more than 10,000 delegates to the EAU/EAUN congresses, the session halls were filled to capacity during the live surgeries, the International Conference on Prostate Cancer Prevention and the Plenary and Thematic Sessions. Earnest discussions marked the seven Section Meetings, the abstract sessions, and the Urology Beyond Europe which offered the perspectives of colleagues from outside the region. Certainly, we can say that we do not only have an international reach in terms of coverage, but also presented current views and trends in various regions. The international meeting on prostate cancer prevention, for instance, showed the dynamics of offering an international platform where manifold viewpoints are carefully examined. In Plenary Session 4, Keith Parsons of the Guidelines Office, presented the EAU policy for live surgery, touching on ethical issues and safety guidelines which is a first in the urological community. In the same session we heard the key messages on recurring topics and controversies such as the PCa screening debate. The EAU, the patients group Europa Uomo and the ERSPC all presented perspectives which added more nuance to the debate than ever before. Thus, the overarching theme is one that many will agree on: for us to offer optimal care we need to effectively collaborate within and outside urology. Moreover, to fully benefit from the discoveries of research we have to find the practical uses of these findings in everyday clinical practice. Chris Chapple led a session on lower urinary tract management, March/May 2013 Prof. Manfred Wirth Editor-in-Chief emphasising the importance of a concerted effort from both medical scientists and the industry to work together on clinical trials and research breakthroughs. At the General Assembly Meeting, we have also confirmed that for the EAU to further advance we need to strengthen the formal ties with our medical and non-medical partners. The danger for organisations is to evolve into monolithic systems, with a tendency to ‘macro-manage’ processes whose very nature are often local or circumscribed. We are aware that some of the developments with the most significant impact often occur in small moments or increments, taking place just below the radar. Our organisation aims to precisely detect these seemingly mundane but steady gains by keeping our ears close to the ground. We encourage you to give your comments by logging in to the EAU website and use the email form and send us your suggestions for improvement. In this issue you will find, as customary after the annual congress, the summary reports of some of the highlights discussed in Milan. There are photos, opinion articles and the regular editorial departments. For those who have missed the congress, it will not be possible to report all the messages, but with this edition you will have a bird’s eye view of the manifold issues that impact on urology. The annual congress is not merely a gathering of like-minded individuals nor is it a place to heighten old scores and scientific disputes. Rather, our congress serves as a direct link to ideas, to the potentially crucial and to what may occur under the radar, and whose value remains to be weighted in the days ahead. European Urology Today 1 Highlight Session 1: Prostate disease What is new in BPH assessment and treatment Dr. Aurélien Descazeaud Limoges Academic Hospital Dept. of Urology Limoges (FR) aurelien. descazeaud@ chu-limoges.fr Prostate disease includes benign and malignant disease. As prostate cancer was extensively covered in other highlight sessions, this article focuses on benign prostate hyperplasia (BPH). What are the key messages on BPH evaluation and treatment to take home from the 2013 EAU meeting? Although almost all abstracts selected contained interesting data, we apologise to the authors who are not cited here due to space constraints. How to evaluate bladder outlet obstruction (BOO)? The question is still unresolved. In men with acute urinary retention, lower age, large drained volume, and severe pain were independent predictive factors of BOO (Rom et al., #991). Suzuki et al. (#998) suggested combining several values obtained from transrectal ultrasonography to predict BOO, including transition zone index, intravesical prostatic protrusion, and resistive index. Similarly, Ciudin and coll. (#993) considered that the joint measurements of bladder wall thickness, middle lobe protrusion, and prostate volume might replace urodynamics in the evaluation of BOO. Several studies attempted to determine predictive factors of successful therapy in BPH. High BMI was associated with failure of surgical treatment (Wilder et al., #989). In addition, patients with predominant nocturia were less likely to improve their symptoms following medical or surgical treatment of BPH (Cäkir et al., #407). In a 22-million population-based analysis including 34,000 patients operated by TURP, smaller resected prostate weight could be at higher risk of continual medication or reoperation (Lin et al., #515). The use of 5 Alpha reductase inhibitors (5ARI) is still debated. First, in the COMBAT study, combination therapy resulted in improvements in nocturia compared with monotherapies (Reardon et al., #1095). Association of 5ARI and tadalafil was evaluated in two studies, and showed that the association was safe and efficient in both lower urinary tract symptoms (LUTS) and erectile dysfunction (Park et al., #1092; Hauk et al., #1096). In a randomised study including 142 patients, Pastore et al. (#517) found that dutasteride for six weeks before transurethral resection of the prostate reduced surgical bleeding. Finally, statin use was associated with a mild prostate volume reduction only in patients not taking 5ARI (Cho et al., #409). Several studies assessed the role of antimuscarinics therapy in BPH. Combination therapy with tamsulosin OCAS (oral controlled absorption system) formulation plus solifenacin was found to offer significant improvements in IPSS quality of life index versus tamsulosin OCAS alone in men with LUTS related to BPH who had both voiding and storage symptoms (Napier et al., #1089). Liao & coll. (#1090) evaluated first-line antimuscarinic monotherapy in patients with enlarged prostates. Four parameters were found predictive of successful treatment including: • Predominant storage symptoms • No elevated post-void residual volume • Higher maximum urinary flow rate (Qmax). • Smaller prostate volume In Gotoh’study (#404), combination therapy of imidafenacin and tamsulosin in patients with overactive bladder related to BPH had greater improvements in OAB symptoms and in nocturia compared to those treated by tamsulosin alone. European Urology Today Editor-in-Chief Prof. M. Wirth, Dresden (DE) Section Editors Dr. A. Cestari, Milan (IT) Mr. Ph. Cornford, Liverpool (GB) Prof. O. Hakenberg, Rostock (DE) Prof. P. Meria, Paris (FR) Prof. J. Rassweiler, Heilbronn (DE) Prof. O. Reich, Munich (DE) Prof. Th. Roumeguère, Brussels (BE) J.L. Vasquez, Frederiksberg (DK) Regarding lasers, Netsch & coll. (#636) reported an interesting series of 56 patients under oral anticoagulation including aspirin, clopidogrel and coumadin, who were treated by thulium laser for BPH. Five patients required early reoperation, and four received blood transfusion. This highlights the fact that BPH on OA patients is at high bleeding risk, even using laser treatment. In another study, 120 & 180 watt Greenlight ® lasers were compared. The later system reduced mean operative time from 80 min. to 53 min. and was safe (Hueber et al., #638). Some experimental techniques were reported this year. First, mirabegron, a novel Beta3 adreno receptor agonist might be efficacious on storage symptoms in patients already treated by alpha blocker therapy (Ogura et al., #1091). According to phase 2 studies, NX1207, a pro-apoptotic protein delivered by intraprostatic injection, might be safe and effective in the treatment of LUTS related to BPH; a phase-3 study is ongoing in the United States (Gemmell et al., #626). Meditate ® is a temporary implantable nitinol device which was tested in 19 BPH patients. This might provide effective BOO relief (Porpiglia et al., #630). The Urolift ® device, which is transurethraly implanted into the prostate might also be effective in BPH patients. This can be placed under local anaesthesia (Amend et al., #629). Campos Pinheiro and colleagues (#628) reported a series of 365 consecutive patients treated by prostatic artery embolisation for LUTS related to BPH. This outpatient technique might be particularly effective in patients with prostate larger than 100 ml. The authors reported one case of bladder wall ischemia. Summary highlights The following are the summary conclusions: • Predominance of obstructive symptoms, high prostate volume, low Qmax and the use of several ultrasonography parameters might help identify patients with BOO; • Preliminary studies showed that the association of 5ARI and tadalafil might be safe and efficient; • Antimuscarinics agents, alone or in association might be useful in BPH, especially in patients in whom LUTS might not be only prostate related; • The 180 watt Greenlight ® laser appears to be faster than the 120 watt version; • BPH surgery in oral anticoagulation patients remains at high-risk, even using laser devices; and • Finally, some emerging techniques might be promising, but are still experimental. Fig. 1: Urolift ® device (Amend et al., #629) Impressions from Special Guest Editor Prof. F. Montorsi, Milan (IT) Founding Editor Prof. F. Debruyne, Nijmegen (NL) Editorial Team H. Lurvink, Arnhem (NL) E. Starkova, Arnhem (NL) J. Vega, Arnhem (NL) L. Keizer, Arnhem (NL) EUT Editorial Office PO Box 30016 6803 AA Arnhem The Netherlands T +31 (0)26 389 0680 F +31 (0)26 389 0674 [email protected] Disclaimer No part of European Urology Today (EUT) may be reproduced without written permission from the Communication Office of the European Association of Urology (EAU). The comments of the reviewers are their own and not necessarily endorsed by the EAU or the Editorial Board. The EAU does not accept liability for the consequences of inaccurate statements or data. Despite of utmost care the EAU and their Communication Office cannot accept responsibility for errors or omissions. 2 European Urology Today March/May 2013 Highlight Session 1: Reconstruction Reconstruction urology is an evolving field with new aspects emerging Asst. Prof. Cristian Surcel Fundeni Clinical Institute Dept. of Urology Bucharest (RO) [email protected] At the 28th Annual EAU Congress many thoughtprovoking abstracts were presented on reconstruction and which addressed various aspects, ranging from stem cells to robotic urinary diversions. Unfortunately not all authors are included in this article, since less than 5% of the papers will be discussed in this short review. The selection of papers was done according to their clinical relevance, number of patients included in the study, reproducibility of results and, of course, and their innovative or pioneering approach. This year in Milan, 51 abstracts regarding various aspects of reconstruction were accepted, as seen in Table 1. Tissue engineering was a very hot topic in this year’s congress, accounting for more than 30% of the abstracts on reconstruction. Roelofs et al. (#870) investigated whether neurological damage can be prevented and skin regeneration can be improved, by covering an experimental spina bifida lesion on fetal lambs with a growth factor loaded scaffold (VEGF and FGF-2). They showed that suturing or gluing the scaffold on the spina bifida lesion can improve the neurological outcome and significantly diminish the urinary leakage. For the surgical treatment of long and complicated urethral strictures, bioartificial matrix-stabilized urothelium offers an innovative therapeutic option for urethral reconstruction. Collagen matrices increase the stability of cell-based implants and promote cell viability and proliferation of urothelial cells. Vaegler et al. (#248) investigated various stabilization strategies of tissue-engineered urothelium. Collagen Cell Carrier (CCC) seeded with autologous urothelial cells was implanted in mini-pigs after induction of a urethral stricture. The seeded CCC displayed excellent stability characteristics and suturability when manipulated and the urothelium-matrix transplants integrated properly into the host tissue without any sign of visible inflammation. Transplantation of mesenchymal stem cells can be Table 1: Overview of selected abstracts on reconstruction used for the regeneration of the damaged cells of corpora cavernosa. Song et al. (#325) examined the differentiation of human mesenchymal stem cells cultivated on the surface of nanofibrous meshes (nano-hMSCs) into neuron-like cells and their capacity to recover the erectile function using their transplantation around the injured cavernous nerve (CN) of rats. They prove that Nano-hMSCs differentiated into neuron-like cells and their transplantation on damaged corpora cavernous improves the erectile function of the rats with cavernous nerve injury. Bladder neck sclerosis is a severe complication of transurethral resection of the prostate (TURP) with an increasing incidence in the laser/vaporization era. Endoscopic resection or incision of bladder neck is usually successful in management of such cases, but, in some patients, even repeated endoscopic procedures fail to resolve the sclerosis. Sayedahmed et al. (#867) performed a retrospective evaluation of 17 patients who underwent a modified Y-V plasty of the bladder neck post TUR-P. Difference to the standard Y/V-plasty was a T-shaped incision of the anterior bladder wall. With this technique two vascularised flaps were created, which offer the possibility to reconstruct a wide bladder neck and also, the anterior prostatic urethra. They evaluated Q max, residual urine volume, questionnaires (IPSS, SF-8 and ICIQ-SF) to all patients before and after the Y-V plasty. After a mean follow-up of 39.2 months, the mean Q max increased from 2.3 ml/s to 19.3 ml/s and 94.1% of patients reported satisfactory micturation with significant improvement of quality of life. In conclusion, the Y-V Plasty of the bladder neck sclerosis after TURP and failed endoscopic treatment represents a viable option with a high success rate. Stricture recurrence after urethroplasty with buccal mucosal graft (BMG) represents a challenge for reconstructive surgeons. Pandey et al. (#790) addressed this issue in a prospective study and concluded that a short-length bridging at the transplantation site can be treated successfully with urethrotomy or dilatation in more than 50% of cases. Buccal mucosa graft can be used once more for long recurrent strictures, but the success rates are less than after primary reconstruction. Milan section: More collaborative links, practical use of research findings. . . . . . . . . . . . . . . . . . . . . . 1 Post-congress reflections . . . . . . . . . . . . . . . . 1 Highlight Session 1: Prostate disease . . . . . . . 2 Highlight Session 1: Reconstruction . . . . . . . . 3 Highlight Session 2: Andrology. . . . . . . . . . . . 4 Highlight Session 2: Oncology. . . . . . . . . . . . . 4 Overview of prizes and awards. . . . . . . . . . 5-7 Ten questions: John Wickham. . . . . . . . . . . . . 8 London hosts 3rd ESGURS-ESAU meeting. . . . 8 Sexual Medicine takes a step forward with qualifying exam. . . . . . . . . . . . . . . . . . . 9 Hemorrhagic cystitis: Etiology and treatment. . . . . . . . . . . . . . . . . . . . . . . . . 9-10 Robot-assisted radical cystectomy (RARC) with total intracorporeal diversion with an ileal neobladder is a challenging procedure in urology, demanding high levels of experience. Tyritzis et al. (#1035) presented the largest single center series to date of this operation, focusing on complications and oncological outcomes. Between 2002 and 2012, a total of 67 RARC with intracorporal Studer neobladder were performed. Despite their short mean follow-up time of 27months, they showed good oncological outcomes, but the mean operating time, complication rates (immediate and late), median hospitalization time remained significantly high. Clinical Challenge. . . . . . . . . . . . . . . . . . . . . . 11 The authors concluded that after 10 years of RARC with total intracorporeal urinary diversion, the technique is still under refinement. Centers need to standardise all the steps of the operation in an effort to decrease complication rates and to optimise oncological outcomes. Live surgical events: Skills or thrills?. . . . . . . 18 To conclude, reconstruction urology is an evolving field. Every year, new aspects come to light and challenge current clinical practices. I congratulate and encourage all the authors who have submitted their work and to continue with their efforts. Key articles from international medical journals. . . . . . . . . . . . . . . . . . . . . . . . . . 12-13 EBU section: EBU Certification Programme Prague. . . . . . 14 Coimbra’s Residency Training gains EBU certification . . . . . . . . . . . . . . . . . . . . . . . . . 14 ERUS 10th Anniversary Meeting. . . . . . . . . . 15 Neobladder and continent cutaneous diversion after RC. . . . . . . . . . . . . . . . . . . . . 16 USANZ Trainee Week . . . . . . . . . . . . . . . . . . 17 ESU section: European Urology Forum 2013 . . . . . . . . . . . 19 Optimising management of non-muscle invasive TCC. . . . . . . . . . . . . . . . . . . . . . . . . 20 YUO section: Creating a network of professional contacts. . Endourology fellowship in Pakistan . . . . . . . A call for active support. . . . . . . . . . . . . . . . Milan Congress: Clockwork efficiency. . . . . . Residents’ Day: Tips and challenges. . . . . . . 22 22 23 23 23 EULIS section: Open stone surgery in 2013. . . . . . . . . . . . . . 24 Endourology course in Torino, Italy . . . . . . . 24 See you next year in Stockholm! History Office section: Remembering Arthur Barth (1858-1927) . . . . 25 28th Annual EAU Congress Book reviews. . . . . . . . . . . . . . . . . . . . . . . . 26 2nd EULIS Meeting: Towards personalised management . . . . . . . . . . . . . . . . . . . . . . . . 27 Delegates per country Canadian Tour 2012 . . . . . . . . . . . . . . . . . . . 28 ESUT’s dynamic presence in Milan. . . . . . . . 29 Congress calendar 2013/2014 . . . . . . . . . 30-31 Who’s Who in Urology. . . . . . . . . . . . . . . . . 32 EU-ACME section: Win a free registration to Stockholm in 2014!. 32 EU-ACME MCQ 2012 winners . . . . . . . . . . . . 32 Obituary: Mirja Ruutu. . . . . . . . . . . . . . . . . . 33 The red colour corresponds to the number of delegates per country (the more intense the colour, the larger the representation) 3,292 4,997 1,186 216 Total delegates EAU 9,691 March/May 2013 Mont Blanc Senior Visiting Scholarship Programme . . . . . . . . . . . . . . . . . . . . . . . . . 34 Accrual Workshop MAGNOLIA trial. . . . . . . . 36 EAU 2012 Registrations per category EAU members Non EAU members Residents EAU member Residents non EAU member Between bench and clinic. . . . . . . . . . . . . . . 34 Nurses EAUN member Nurses non EAUN member Total delegates EAUN 186 219 405 Total delegates EAU/EAUN Congress10,096 Exhibitors2,349 Press173 Accompanying Persons 270 Total participants 12,888 Prostate and kidney dilemmas. . . . . . . . . . . 36 www.reviews. . . . . . . . . . . . . . . . . . . . . . . . 37 Tübingen hosts joint meeting. . . . . . . . . . . . 37 EAUN section: Overview report: 14th International EAUN Meeting. . . . . . . . . . . . . . . . . . . . . . . . . . . . 38 EAUN Fellowship addresses patient safety. . 39 A forward-looking urology practice . . . . . . . 39 European Urology Today 3 Monday, 18 March, Highlight Session 2: Andrology Sessions examine basic science and clinical aspects within andrology Dr. Mikkel Fode Herlev Hospital Dept. of Urology Herlev (DK) mikkelfode@ gmail.com The 28th Annual EAU Congress presented many high quality andrology abstracts, and it is a privilege for me to highlight some of the studies which focused on basic science in male infertility and sexual dysfunction as well as the clinical aspects of men’s sexual health. Two major aspects regarding male infertility were discussed, namely epigenetics and lifestyle factors. Epigenetics relates to molecular modifications of DNA and one aspect that has been shown to be of importance is the replacement of histones by protamine late in the spermatogenesis. An abstract by Rogenhofer et al. (#27) investigated ejaculated semen from 306 men from infertile couples and 32 healthy controls. Here, an abnormal ratio of protamine 1: protamine 2 predicted fertilization rates with artificial reproductive techniques, with the most aberrant ratios leading to the worst results. Larger studies are underway to further illuminate this issue. Regarding lifestyle issues and fertility, two studies by Bechara et al. (#29) and Silva et al. (#30) showed morphological testicular changes and reduced sperm concentration in hypertensive rats and rats fed with a diet of saturated fat, respectively. Interestingly, these changes were ameliorated by enalapril in hypertensive rats and no adverse effects were seen when saturated fats were replaced by unsaturated fats. In men’s health, Zacharakis et al. (#129) compared the results of early implantation of a penile prosthesis after priapism and late implantation several months after the incident. The study described an increased ease of dilation of the corpora in the early treatment group and a reduced need for revision surgery. Furthermore, there was no penile shortening in the early implantation group compared to 40% in the late implantation group. The authors recommended that implants are implanted as quickly as possible if a case of refractory ischemic priapism has lasted beyond 48 hours. Another study (Appel et al., #131) reported on low intensity extracorporeal shock-wave therapy (ESWT). The authors evaluated results up to eight months after treatment in 155 patients from previous trials. More than 50% of patients still had clinically significant improvements in erectile function compared to baseline at this point. The effect was best in patients with mild to moderate ED. A lengthy discussion after the presentation underlined that ESWT is still a controversial treatment but it is clear that evidence continues to accumulate. The final ED topic is the concept of penile rehabilitation after radical prostatectomies, which also led to some discussion at the conference. Unfortunately, 16 years after our Milan host, Prof. Francesco Montorsi, published the first paper on the topic, there is still no conclusive evidence regarding the optimal treatment protocol. This was illustrated in a questionnaire study by Bannowsky et al. (#127), which showed that 262 German urologists used no less than 39 different rehabilitation protocols. Another hot topic in andrology is late onset hypogonadism. At the EAU meeting we saw an observational study of 850 hypogonadal men who were treated with testosterone injections for up to five years (Yassin et al., #207). The mean BMI dropped an impressive 7.4 points which is more than generally seen in such studies. It is important to note that it was an observational study not controlled for lifestyle modifications. However, it does illustrate some of the potential benefits of testosterone treatment. At the other end of the spectrum are the potential harms, and although this has recently been intensely questioned, the main concern remains prostate cancer. Arguments are heated on both sides but the fact remains that high quality studies are lacking regarding safety and harm. from previous non-randomized trials and they indicate that varicocelectomies are relevant in the treatment of hypogonadism whenever the two conditions co-exist. The congress presented a number of very interesting studies regarding regenerative medicine and premature ejaculation. A study by Castiglione et al. (#324) represented the first attempt to treat active Peyronie’s disease in a rat model with adipose To address the concerns, a large group of much esteemed colleagues have initiated a multicenter study tissue-derived stem cells. The stem cell treatment was shown to prevent penile fibrotic changes and to (n=999) designed specifically to investigate the improve erections (Figure 1). The full study was development of prostate cancer with long-term published in the March edition of European Urology testosterone use. An abstract by Rosen et al. (#211) and the group is conducting further studies to provided a very nice characterization of the investigate whether stem cells may be of benefit in the participants. However, the real value of the study will chronic phase of the disease. become evident in the next few years when longitudinal and prospectively collected data on the effects of testosterone treatment are published. Another study by La Croce et al. (#328) concerned premature ejaculation. This very innovative study Another testosterone-related study completely confirmed the presence of an endocannabinoidregulatory enzyme called “fatty acid amide hydrolase” bypassed these safety discussions by attempting to treat the cause of the hypogonadism. In the study by in ephithelial cells of both animal and human seminal Afoko et al. (#212), the authors managed to randomize vesicles. Interestingly, inhibition of this enzyme-delayed 59 middle aged patients with varicoceles and apomorphine induced ejaculation in rats by almost 15 symptoms of hypogonadism to varicocelectomy or minutes from about five to around 20 minutes. This observation. In the no-treatment group, the means that the research group might have found a new testosterone levels remained low while the mean target for the treatment of premature ejaculation, which value increased from 6.3 nmol/L to 10.8 nmol/L in the has never been explored before. The effects could have treatment group over 18 months. In addition, patients been mediated at a local level, which means that such a treatment could be without significant side effects on reported an improvement of their hypogonadal the central nervous system. symptoms. The results are in accordance with those As can be expected many high quality abstracts are not highlighted here and I regret that it is not possible to include or cite more studies. However, full presentations from the conference are available at http://www.eaumilan2013.org/. Figure 1: Stem cells prevented fibrosis and preserved erectile function in a rat model of active Peyronie’s disease Monday, 18 March, Highlight Session 2: Oncology New insights in CRPC, penile cancer and nephron-sparing surgery Prof. Axel S. Merseburger Clinic for Urology and Urologic Oncology Medical School Hannover (DE) Merseburger.axel@ mh-hannover.de Urologic oncology was again a topic that drew a lot of attention, and the highest percentage of the 1182 abstracts was on topics that directly or indirectly covered urologic oncology. With this high number of submitted abstracts, it is thus impossible to cover all important investigations. In this short review, I have chosen the studies which are of interest and have an immediate clinical impact: segemental ureterectomy provides oncologic and renal functional outcomes similar to radical nephroureterectomy. No significant difference in cancer-specific survival was reported in this matched-pair analysis. However, the renal function was not superior in the organ preserved group (RNU 10.6 ml/min. vs. SNU 6.6 ml/min. p = 0.174) which might be due to confounders such as previous intrarenal surgery, ureter stents, etc. (Figure 1). They also demonstrated that although the use of abiraterone can potentially lead to an accumulation of precursor hormones, its anti-androgenic properties may stop precursor hormone-induced androgen receptor (AR) activation. High concentrations of androgen precursors can drive CRPC growth through direct activation of overexpressed AR and not necessarily via the result of intra-tumoural CYP17metabolism. European Study (ZEUS) which showed no difference in the incidence of bone metastases between the Zometa group and control arm. Patients were randomised between standard treatment plus Zometa® 4 mg infusions every three months for a total of 48 months. No difference in survival was shown after a median follow-up of 50 months. Zoledronic acid was expected to show its potential in preventing hormone therapy-induced bone loss. Rink et al. (#813) have assessed the median time from radical nephroureterectomy to disease recurrence. This was reported to be 12 months in the cohort of 547 assessed patients, while the median time from disease recurrence to tumour-specific death was 10 months. This suggests that CRPC may not rely solely on de novo androgen synthesis. We show that abiraterone, a CYP17A1-blocking drug that has recently been approved in the treatment of CRPC, possesses an additional anti-androgenic property and can block androgen precursor-induced AR-activation at higher concentrations than what is needed for CYP17A1 specific inhibition. The study won the first prize for best abstract in oncology at the 28th Annual EAU Congress. Below are the general conclusions: Volpe et al. (#174) reported on the first data of the Italian prospective active surveillance (AS) trial in small renal masses. Of the 32 included patients no progression to metastasis or tumour-specific death occurred. The authors concluded that AS might be an option in selected elderly and/or comorbid patients. Sooriakumaran et al. (#824) aimed to compare such outcomes in a Swedish cohort treated from 1996 onwards in their large observational study. 34,515 Djajadiningrat et al. (#392) have demonstrated men were treated for prostate cancer throughout contemporary five-year cancer-specific survival (CSS) Sweden with either surgery (n = 21,533) or of penile squamous cell carcinoma patients treated at Rouffilange et al. (#96) examined the indications of partial nephrectomy (PN) within the limits of technical radiotherapy (n = 12,982) as their first treatment our institution and compared this with previous feasibility. The group assessed the morbidity, option and form the study cohort. Radiotherapy cohorts stratified by treatment periods. The main change was the introduction of dynamic sentinel node mortality, oncological and functional results of PN for patients generally had higher Gleason sums and the treatment of renal tumours greater than 7 cm. PN clinical stages, were older, and had higher PSA than biopsy (DSNB) in 1994. Despite less surgery on the is feasible for tumours over 7 cms but has a global patients that underwent surgery (p < 0.0001 for all regional nodes, improvement of five-year CSS has complication rate of 31%. Additionally, this comparisons). Survival outcomes favored surgery, and been seen in cN0 patients. This is probably due to investigation found an association of a high local for locally advanced/metastatic patients treatment detection of microscopic disease by DSNB. The recurrence rate of 23.5% despite negative surgical results were similar. The only cohort in which authors concluded that penile preserving therapies radiotherapy had superior prostate-cancer-mortality margins. are increasingly performed, without jeopardizing outcomes was those aged 65-74 with non-localised survival. Moll et al. (#824) reported that anti-androgenic disease. properties of the drug abiraterone may provide an Klatte et al. (#575) have shown in their retrospective Finally, Wirth presented during the closing and fourth additional mechanism of action in blocking tumour multicenter study (OSS-UTUC) that for the growth of castration resistant prostate cancer (CRPC). plenary session the initial study results of the Zometa management of ureteral urothelial carcinoma, • The AR remains the most important target in the treatment of CRPC; • Nephron-sparing surgery in large renal lesion is feasible, hence recurrence rates are high; • Dynamic sentinel node biopsy (DSNB) in penile cancer has resulted in less surgery on the regional nodes and improvement of five-year CSS; • No difference in survival was shown for Zoledronic vs. placebo; and • Surgery was superior compared to radiotherapy with regards to survival in localised prostate cancer. Figure 1: Cancer-specific survival in the study of Klatte et al. (#575) 28th Annual EAU Congress 4 European Urology Today March/May 2013 Overview of prizes and awards at the 28th Annual EAU Congress EAU Willy Gregoir Medal 2013 Opening Ceremony C-C. Abbou, Créteil, France - Handed out by P-A. Abrahamsson EAU Frans Debruyne Life Time Achievement Award 2013 J. Breza, Bratislava, Slovakia - Handed out by P-A. Abrahamsson Friday, 15 March EAU Crystal Matula Award 2013 P. Boström, Turku, Finland Supported by an unrestricted educational grant from LABORIE - From left to right: P. Boström, R. Laborie (LABORIE) and P-A. Abrahamsson EAU Hans Marberger Award 2013 J. Rassweiler, Heilbronn, Germany Supported by an unrestricted educational grant from KARL STORZ GMBH & CO.KG - From left to right: J. Rassweiler, P-A. Abrahamsson and S. Storz (KARL STORZ GMBH & CO.KG) EAU Innovators in Urology Award 2013 U. Studer, Berne, Switzerland - Handed out by P-A. Abrahamsson New EAU Honorary Members EAU Prostate Cancer Research Award 2013 I. Ahmad, Glasgow, United Kingdom Supported by an unrestricted educational grant from the FRITZ H. SCHRÖDER FOUNDATION - From left to right: I. Ahmad, F.H. Schröder (FRITZ H. SCHRÖDER FOUNDATION) and P-A. Abrahamsson P. Rigatti, Milan, Italy - Handed out by P-A. Abrahamsson I. Sinescu, Bucharest, Romania - Handed out by P-A. Abrahamsson R. Umbas, Jakarta, Indonesia - Handed out by P-A. Abrahamsson Prize for the Best Paper published on Clinical Research in the Urological Literature in 2012 Prize for the Best Paper published on Fundamental Research in the Urological Literature in 2012 E. Martens, S. Jalava, N. Dits, G. Van Leenders, S. Møller, J. Trapman, C. Bangma, T. Litman, T. Visakorpi, G. Jenster (Rotterdam, The Netherlands; Tampere, Finland; Vedbeak, Denmark) For the paper: “Diagnostic and prognostic signatures from the small non-coding RNA transcriptome in prostate cancer.” Oncogene 2012;31:978-991. – doi: 10.1038/onc.2011.304 - Handed out by P-A. Abrahamsson Prize for the Best Scientific Paper published in European Urology in 2012 R. Rosenblatt, A. Sherif, E. Rintala, R. Wahlqvist, A. Ullén, S. Nilsson, P-U. Malmström, The Nordic Urothelial Cancer Group (Katrineholm, Stockholm, Uppsala, Sweden; Helsinki, Finland; Oslo, Norway) For the paper: “Pathologic downstaging is a surrogate marker for efficacy and increased survival following neoadjuvant chemotherapy and radical cystectomy for muscle-invasive urothelial bladder cancer.” European Urology 2012;61(6):1229-1238. Supported by an unrestricted educational grant from ELSEVIER - From left to right: A. Sherif who accepted the award on behalf of R. Rosenblatt, F. Montorsi and J. Catto S. Shariat, M. Rink, B. Ehdaie, E. Xylinas, M. Babjuk, A. Merseburger, R. Svatek, E. Cha, S. Tagawa, H. Fajkovic, G. Novara, P. Karakiewicz, Q-D. Trinh, S. Daneshmand, Y. Lotan, W. Kassouf, H-M. Fritsche, F. Chun, G. Sonpavde, A. Joual, D. Scherr, M. Gonen (New York, San Antonio, Los Angeles, Dallas, Houston, United States of America; Hamburg, Hanover, Regensburg, Germany; Paris, France; Prague, Czech Republic; Padua, Italy; Montreal, Canada; Casablanca, Morocco) For the paper: “Pathologic nodal staging score for bladder cancer: A decision tool for adjuvant therapy after radical cystectomy.” Eur Urol 2013 Feb;63(2):371-8. doi: 10.1016/j.eururo.2012.06.008. Epub 2012 Jun 16. - Handed out by P-A. Abrahamsson Prize for the Best Scientific Paper published on Fundamental Research in European Urology by a young urologist in 2012 R. Kandimalla, A. Van Tilborg, L. Kompier, D. Stumpel, R. Stam, C. Bangma, E. Zwarthoff (Rotterdam, The Netherlands) For the paper: “Genome-wide analysis of CpG island methylation in bladder cancer identified TBX2, TBX3, GATA2, and ZIC4 as pTa-specific prognostic markers.” European Urology 2012;61(6):1245-1256. Supported by an unrestricted educational grant from ELSEVIER - From left to right: E. Zwarthoff who accepted the award on behalf of R. Kandimalla, F. Montorsi and J. Catto Award Gallery Friday, 15 March Prize for the Best Scientific Paper published on Clinical Research in European Urology by a young urologist in 2012 M. Rink, B. Ehdaie, E. Cha, D. Green, P. Karakiewicz, M. Babjuk, V. Margulis, J. Raman, R. Svatek, H. Fajkovic, R. Lee, G. Novara, J. Hansen, S. Daneshmand, Y. Lotan, W. Kassouf, H-M. Fritsche, A. Pycha, M. Fisch, D. Scherr, S. Shariat (New York, Dallas, Hershey, San Antonio, Los Angeles, Houston, United States of America; Hamburg, Regensburg, Germany; Montreal, Canada; Prague, Czech Republic; St. Poelten, Austria; Padua, Bolzano, Italy) Bladder Cancer Research Consortium (BCRC) and Upper Tract Urothelial Carcinoma Collaboration (UTUCC) For the paper: “Stage-specific impact of tumor location on oncologic outcomes in patients with upper and lower tract urothelial carcinoma following radical surgery.” European Urology 2012;62(4):677-684. - From left to right: M. Rink, F. Montorsi and J. Catto The European Urology Platinum Award 2013 From left to right: W. Artibani, C. Pierce, H. Van Poppel, C. Schulman, J. Roelofswaard, P-A. Abrahamsson, M. Wirth, M. Schlief, F. Montorsi and J. Catto 28th Annual EAU Congress March/May 2013 European Urology Today 5 Overview of prizes and awards at the 28th Annual First Prize for the Best Abstract (Oncology) J. Moll, R. Van Soest, J. Kumagai, R. Graeser, I. Hickson, G. Jenster, W. Van Weerden (Rotterdam, The Netherlands; Beerse, Belgium) For the abstract: “824 Abiraterone is able to block AR activation induced by accumulating levels of precursor hormones resulting from CYP17A1 inhibition.” - Handed out by A. Stenzl First Prize for the Best Abstract (Non-Oncology) M. Lanz, C. Birchall, A. Ali, K. Walton, C. Townes, L. Lim, S. Roushias, P. Aldridge, R. Pickard, J. Hall (Newcastle Upon Tyne, United Kingdom) For the abstract: “623 Bacterial motility and NF-kB activation by clinical isolates from urinary tract infections.” - Handed out by A. Stenzl Second Prize for the Best Abstract (Oncology) Award Gallery P. Sooriakumaran, L. Haendler, T. Nyberg, I. Heus, M. Olsson, S. Carlsson, M. Roobol, P. Wiklund (Stockholm, Sweden; Rotterdam, The Netherlands) For the abstract: “912 Comparative oncologic effectiveness of radical prostatectomy and radiotherapy in prostate cancer: An analysis of mortality outcomes in 34,515 patients treated with up to 15 years follow-up.” - Handed out by A. Stenzl Friday, 15 March Second Prize for the Best Abstract (Non-Oncology) K. Filipski, K. Deckmann, T. Bschleipfer, G. Krasteva-Christ, T. Papadakis, A. Rafiq, M. Wolff, I. Ibanez-Tallon, B. Schütz, E. Weihe, W. Kummer (Giessen, Berlin, Marburg, Germany) For the abstract: “62 A new cell in the urogenital tract - cholinergic chemosensory brush cells are sentinels of the urethra.” - Handed out by A. Stenzl Third Prize for the Best Abstract (Oncology) H. Uemura, T. Kimura, K. Yoshimura, T. Minami, M. Nozawa, T. Nakagawa, H. Fujimoto, S. Egawa, A. Yamada, K. Itoh (Osaka, Tokyo, Fukuoka, Japan) For the abstract: “98 Combination therapy of peptide vaccines and dexamethasone for hemotherapy naïve castration resistant prostate cancer - a randomized phase-2 study.” - Handed out by A. Stenzl Third Prize for the Best Abstract (Non-Oncology) Y. Song, H. Lee, J. An, J. Yun, J. Kim, S. Doo, W. Yang, S. Kim (Seoul, South Korea) For the abstract: “325 Repair of erectile dysfunction using transplantation of human mesenchymal stem cells cultivated on the surface of nanofibrous meshes in rats with cavernous nerve injury.” - Handed out by A. Stenzl to J. Yun who accepted the award on behalf of Y. Song First Video Prize Video Award Session O. Ukimura, A. De Castro Abreu, M. Nakamoto, S. Shoji, S. Leslie, A. Berger, A. Goh, M. Desai, M. Aron, I. Gill (Los Angeles, United States of America) For the video: “V79 Novel surgical tile-pro navigation with 3D prostate cancer model during robot-assisted radical prostatectomy.” - From left to right: P.A. Geavlete, O. Ukimura and A. Messas Monday, 18 March Second Video Prize Third Video Prize A. Rao, R. Gray, H. Motiwala, M. Laniado, O. Karim (Wexham, United Kingdom) For the video: “V78 Sequential occlusion angiography using contrast enhanced ultrasound scan (CEUS) demonstrating the avascular plane of Brodel: An adjunct to a novel technique of zero-ischaemia robot-assisted partial nephrectomy.” - From left to right: P.A. Geavlete, O. Karim, who accepted the award on behalf of A. Rao, and A. Messas Section Awards Saturday, 16 March S. Crouzet, Lyon, France For the video: “V77 Alternative solution to current MIS robotic system.” - From left to right: P.A. Geavlete, S. Crouzet and A. Messas Best Booth Award 2013 Millennium: The TAKEDA Oncology Company - From left to right: P-A. Abrahamsson, V. Kemp, C. Kruhl, J. Vachon, R. Cacioppo and L. Khoury (Millennium: The TAKEDA Oncology Company) ESUI Vision Award 2013 F.E. Lecouvet, Brussels, Belgium For the paper: “Can whole-body magnetic resonance imaging with diffusion-weighted imaging replace Tc 99m bone scanning and computed tomography for single-step detection of metastases in patients with high-risk prostate cancer.” Supported by an unrestricted educational grant from HITACHI MEDICAL SYSTEMS EUROPE / HITACHI ALOKA MEDICAL - From left to right: J. Walz, B. Dowell (HITACHI MEDICAL SYSTEMS EUROPE / HITACHI ALOKA MEDICAL) and F.E. Lecouvet 28th Annual EAU Congress 6 European Urology Today March/May 2013 EAU Congress ESRU Campbell’s Challenge First Prize for the Best Abstract by a resident The winner of the Campbell’s Challenge is J. Roth, Klagenfurt, Austria - Handed out by T. Esen Residents Day Saturday, 16 March Second Prize for the Best Abstract by a resident F. Castiglione, P. Hedlund, F. Van Der Aa, T. Bivalacqua, M. Albersen (Milan, Italy; Leuven, Belgium; Baltimore, United States of America) For the paper: “324 Intratunical injection of human adipose tissue-derived stem cells prevents fibrosis and is associated with improved erectile function in a rat model of Peyronie’s disease.” - From left to right: F. Castiglione, M. Albersen and T. Esen G. Shaw, D. Lewis, J. Boren, A. Ramos-Montoya, D. Soloviev, R. Bielik, K. Brindle, D. Neal (Cambridge, United Kingdom) For the paper: “833 Monitoring the effects of therapeutic fatty acid synthase inhibition in prostate cancer using 11C acetate PET.” - Handed out by T. Esen Third Prize for the Best Abstract by a resident A. Ingels, A. Thong, M. Saar, M. Valta, R. Nolley, J. Santos, H. Zhao, D. Peehl (Stanford, United States of America) For the paper: “975 Pre-clinical trial of a new dual mTOR inhibitor: INK128 for renal cell carcinoma.” - A. Ingels Resident’s Corner Awards - Awards for the two Best Scientific Papers published in European Urology by a resident in the year 2012 T. Hambrock, C. Hoeks, C. Hulsbergen-Van De Kaa, T. Scheenen, J. Fütterer, S. Bouwense, I. Van Oort, F. Schröder, H. Huisman, J. Barentsz (Nijmegen, Rotterdam, The Netherlands) For the paper: “Prospective assessment of prostate cancer aggressiveness using 3-T diffusion-weighted magnetic resonance imaging–guided biopsies versus a systematic 10-core transrectal ultrasound prostate biopsy cohort” European Urology;61(1):177-184. - From left to right: F. Montorsi, I. Van Oort who accepted the award on behalf of T. Hambrock, T. Esen and J. Catto E. Cha, L-A. Tirsar, C. Schwentner, P. Christos, C. Mian, J. Hennenlotter, T. Martini, A. Stenzl, A. Pycha, S. Shariat, B. Schmitz-Dräger (New York, United States of America; Nürnberg, Tübingen, Germany; Bolzano, Italy) For the paper: “Immunocytology is a strong predictor of bladder cancer presence in patients with painless hematuria: a multicentre study.” European Urology 2012;61(1):185-192. - From left to right: F. Montorsi, E. Cha, T. Esen and J. Catto EUSP Best Scholar Award 2013 EUSP Session L.F. Arenas Da Silva, Mullheim an der Ruhr, Germany For his report: “Urethral Reconstruction using tissue engineering techniques.” - From left to right: P. Mulders, V. Mirone, L. Arenas Da Silva, L. Martínez Piñeiro First Prize for the Best EAUN Poster Presentation B. Bonfils, M. Højgaard, J. Meinung, M. Kelsen, G. Lam Wrist (Herlev, Denmark) For the poster: “Patient comfort during intravesical chemotherapy - a randomized trial comparing two methods of instillation.” - Handed out by K. Fitzpatrick Monday, 18 March Second Prize for the Best EAUN Poster Presentation N. Raue, C. Hitschler, B. Domurath (Bad Wildungen, Germany) For the poster: “Importance of ultrasound determination of the urinary bladder volume for care in patients with spinal cord injury (SCI) who practise catheterization.” - Handed out by K. Fitzpatrick Second Prize for the Best EAUN Poster Presentation A. Ungricht, M. Widmer, T. Makris, N. Schölly, M. Walter, T.M. Kessler (Zurich, Switzerland) For the poster: “Urodynamics in spinal cord injury patients: Be aware of autonomic dysreflexia.” - Handed out by K. Fitzpatrick Prize for the Best EAUN Nursing Research Project EAUN Meeting Monday, 18 March E. Grainger, R. Knudsen, L. Aarvig, B. Thoft Jensen (Århus, Denmark) For the Project Plan: “Optimizing the implementation of fast-track nephrectomy pathways.” - Handed out by K. Fitzpatrick 28th Annual EAU Congress March/May 2013 European Urology Today 7 • What project are you working on now? Staying alive as long as possible to defeat the insurance company (laughs). Seriously, I finished (in 2012) writing a paper for the British Medical Journal about medicine and bureaucracy, and the impact on medical decisions. • What’s the first operation you ever did? Appendectomy- as a student. The first thing that strikes you is when you make the first incision and the amount of pressure you make. I fiddled around and just made a little scratch. • If you were not a urologist, what would you be? I would still be a surgeon. I would hate sitting in an office looking at the computer or fiddling with paper. • What’s the last great book you have read? The Letters of P.G. Wodehouse. Quite fun, that would entertain you. • What’s the last thing that surprised you? To reach this age when nothing surprises you. In general, anything a politician would do now would not surprise me. • Do you collect anything? I collect and restore old cars. It takes up a lot of space. Luckily I got a bit of land. The oldest one is a 1954 Morris Minor. The most recent is a Lotus 1981. The great excitement of driving an old car is that you never know what’s going to break down. • What’s your favorite hour in a day and why? When I go to bed and read. • What would you be doing in your free time? I’m being run by my wife (laughs hard). • What question you haven’t found an answer yet? Oh, good lord… It boils down to small particle physics, what is controlling all these. I don’t have any particular religious beliefs but I’d like to know where it’s all going to go. • What is your biggest fear? TEN QUESTIONS Interview by Joel Vega (Long pause) Having a heart attack, probably that’s my biggest fear. Age: 85 Specialty: Urology City/Neighbourhood: Dorking, south London, United Kingdom Recent Awards: EAU Innovators in Urology Award 2012 JOHN WICKHAM London hosts 3rd ESGURS-ESAU Experts to tackle challenges with insightful strategies http://esgurs-esau.uroweb.org With the goal to closely examine challenging issues in reconstructive urology and andrology, and provide practical approaches to many problematic cases, the EAU Section of Genito-Urinary Reconstructive Surgeons (ESGURS) and the EAU Section of Andrological Urology (ESAU) will hold its 3rd Joint ESGURS-ESAU meeting in London in September. 3rd Joint Meeting of the EAU Section of GenitoUrinary Reconstructive Surgeons (ESGURS) and the EAU Section of Andrological Urology (ESAU) The ESGURS sessions on the first day will also feature live surgeries on slings versus sphincter for incontinence cases, to be followed by a series of lectures and video presentations that will closely look into pelvic fracture urethral reconstruction, renal trauma management, iatrogenic ureteric trauma management and treatment approaches of degloving genital injury. The two-day meeting from September 13 to 14 will present live surgeries by many of Europe’s leading reconstructive and andrological specialists, instructive lectures and video presentations and a series of debates that will examine key issues in both fields. The ESAU session, on the other hand, will focus on managing infertility which will cover topics such as ejaculatory disturbances and duct obstruction, vasovasostomy, varicocele therapy, sperm retrieval and epididymovasostomy. “The use of minimal invasive techniques, which are currently used in the field of reconstructive urology, will be featured and how it impact on treatment outcomes. Update lectures, video presentations to show the latest techniques and live surgery to be performed by the leading experts will also be held,” according to the organisers. The second and last day will open with live surgeries on penile and urethral reconstruction for lichen sclerosus (BXO), and a follow-up surgical session on penile implants. Two blocks of debates will be featured by both the ESGURS and the ESAU, with the aim to highlight practical issues and clarify key points in much-debated controversies. The live surgery sessions, which will be conducted in accordance with the recently issued EAU Guidelines on ethical live surgeries, will be directly transmitted from the operating theatres of the UCLH Education Centre in London to the meeting rooms. Moderated commentary and interactive audience feedback will guide the programme to further prompt insightful discussions. The ESGURS debates will tackle the following topics: management of bladder neck contractures after prostate cancer treatment, with focus on either reconstruction versus endoscopic procedures; full length anterior strictures, i.e. interval dilatation versus reconstruction; among other topics. Meanwhile, the ESAU debate series will examine a range of management strategies, such as managing The organisers, led by Professors Anthony Mundy chronic scrotal pain, management of priapism with (UK), Serdar Deger (ESGURS chairman) and Wolfgang focus on shunts as compared with early implants; a Weidner (ESAU chairman), said the meeting’s third discussion on prostate cancer topics (penile edition promises to be one of the most comprehensive rehabilitation post therapy and testosterone and PCa) joint meetings of both sections. mechanical therapy for Peyronie’s Disease and micropenis. Right on the first day, and following an update lecture on managing ejaculatory dysfunction, two live “For this much anticipated event, we look forward to surgeries are scheduled to demonstrate techniques in an in-depth and insightful meeting that will provide urethroplasty and another session on grafting all participants not only with a comprehensive techniques as compared with Nesbit for Peyronie’s update, but also a new look or examination of current Disease. management strategies. (By Joel Vega) 8 European Urology Today 13-14 September 2013, London, United Kingdom EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations Call for case reports and videos deadline 1 July 2013 European Association of Urology March/May 2013 Sexual Medicine takes a step forward with qualifying exam Everything you want to know about sex but are afraid to ask your patients Dr. Dr. Stefan Buntrock Chief of Urology Klinik am Kurpark Bad Wildungen (DE) The reason why it is so difficult for both doctors and patients to talk about intimate topics is simple: it is taboo. Only a minority of us have been brought up with a proper education about sex, by our parents or at school. Medical school did not prepare us how to talk to patients about sex and neither did we get any training during residency. Sexual symptoms are not uncommon problems which are irrelevant for diagnostic purposes or the successful treatment of a disease. On the one hand they can indicate or are linked to serious underlying causes like cardiovascular disease. As stated by other authors, “A man with ED and no cardiac symptoms is a cardiac (or vascular) patient until proven otherwise.” problem. PDE-5 inhibitors might temporarily restore erectile function but what if the partner does not accept them? What if she gets the impression that his attraction to her is based on a pharmacological reaction? There is a saying that “talk is cheap”, but when it comes to sexual medicine, the oral intervention targeted at the couple is indispensable. stefan.buntrock@ klinik-am-kurpark.de So between us and our patients is a sort of tacit understanding: if you don’t start talking about it, I certainly won’t. No wonder, a recent survey among 366 general practitioners in northern Germany revealed that only 19% of the patients have their sexual history taken routinely1. Conversely, the incidence and prevalence of sexual health problems is high. On the other hand, sexual symptoms can be due to personal and interpersonal crises, resulting in significant reductions of individual quality of life. Sometimes, and particularly in cancer, damage to one’s sexual function is unavoidable. It is therefore important to first address sexual issues before surgical procedures which may have a detrimental effect on sexual life. But even if the tumour can be resected, health might be more difficult to restore. This is because health has something to do with how we feel about ourselves. Any physician should be able to take a sexual history, provide basic information and deal with misconceptions a couple may have about sex. Psychosexual treatment methods, on the other hand, belong in the hands of the specially-trained expert. December 5, 2012 was a historic date. For the first time, the Multidisciplinary Joint Committee of Sexual Medicine (MJCSM) conducted a qualification examination in the field of sexual medicine. I was one of the 341 participants from 54 nations who took the opportunity to become a Fellow of the European Committee of Sexual Medicine (FECSM). The examination was intended for physicians who work in the field. But the more interesting question is: why should anybody not work in this area of medicine? Sexual problems result from an abundance of causes and could be encountered frequently in daily practice if only doctors would dare to ask. Some basic knowledge and skills in sexual medicine should therefore be mandatory for any one practicing medicine. Nevertheless, many of us feel quite uneasy with the subject and don’t address it when talking to patients. “As social beings we need emotional warmth, acceptance, the need to feel close to others and be socially secure. Sexual function serves this purpose.” Evidence suggests that roughly one third of the male and nearly half of the female adult population suffer from sexual problems.2,3 Less than 25% seek medical help.4 Urologists are specialists of the genito-urinary tract, and they should be comfortable in discussing sexual function in clinical settings. We all have basic needs that go beyond water, food, clothing and shelter. As social beings we need emotional warmth, acceptance, the need to feel close to others and be socially secure. Sexual function serves this purpose. It is a multi-layered phenomenon that involves complex dimensions such as relationship, lust and reproduction. And besides the fragile interplay between body and mind, sexual function usually involves other people which make things even more complicated. Unfortunately, we don’t have a pill yet to solve the Sex has been and will always play a central role in our lives. But with the complex interplay between body and mind, sexual dysfunction is common. Thus, there is a need for more doctors to specialise in this area, and establishing a qualification examination in sexual medicine is a major step to a higher level of medical care. References 1. Cedzich DA and Bosinski HA. Sexuologie 2010; 17: 135-47. 2. Lewis RW, Fugl-Meyer KS, Bosch R et al. J Sex Med 2004; 1(1): 35-39. 3. Mercer CH, Fenton KA, Johnson AM et al. BMJ 2003; 327: 426-27. 4. Moreira ED, Brock G, Glasser DB et al. Int J Clin Pract 2005; 59: 6-16. 5. Jackson G, Rosen RC, Kloner RA, et al. J Sex Med 2006; 3: 28-36. Hemorrhagic cystitis: Etiology and treatment Treatment of hemorrhagic cystitis is difficult with therapies described in literature Prof. Maurizio Brausi Chairman of Urology AUSL Modena Modena (IT) [email protected] Hemorrhagic cystitis is a diffuse inflammatory condition of the urinary bladder due to an infectious or noninfectious etiology resulting in bleeding from the bladder mucosa (definition)1. Causes The most common cause of hemorrhagic cystitis is bacterial infection. Escherichia Coli, Staphylococcus saprophyticus, Proteus Mirabilis, and Klebsiella are the most common organisms involved2. Fungal infections can also cause hemorrhagic cystitis. The most common organisms are Candida Albicans, Cryptococccus neoformans, Aspergillus fumigastus and Torulopsis glabrata. Finally, Schistosoma hematobium and Echinococcus granulosus may also be implicated. Nonoxynol-9, ether, allopurinol, methaqualone, methenamine mandelate, gentian violet and intravesical instillation of drugs for the treatment of Non-Muscle Invasive Bladder Cancer (NMIBC) like Epirubicin, thiotepa, MMC, Gemcitabine and Bacillus Calmette-Guerin are the most involved agents. Therapy includes: immediate bladder irrigation. Oxybutynin, hydrocortisone, dymethyl sulfoxide and intravesical 50cc of 1% lidocaine with 100 mg of hydrocortisone for alleviating symptoms6. “Occupational exposure to chemical substances, aniline, a costituent of dyes, and toluidine, found in pesticides and shoes polish, can cause hemorrhagic cystitis.” Chemotherapeutic drugs Cyclophosphamide and ifosfamide (syntetic analogues) used in many chemotherapeutic protocols are the most important agents cuasing hemorrhagic cystitis. Urinary tract symptoms such as frequency, urgency, nocturia and dysuria are very common. Microscopic hematuria occurs in seven to 53% of patients while gross hematuria in 0.6 to 15%7. Chronic and recurrent hemorrhagic cystitis often arises Phosphoramide mustard, the active antineoplastic after radiotherapy and chemotherapy for the treatment metabolite and acrolein are toxic to the urothelium8. The prolonged exposure of the bladder urothelium to of pelvic tumours (prostate, bladder, rectal and gynaecological cancers) and should be considered as acrolein may determine edema of the bladder complications of the treatment. Infections are less mucosa, vascular dilatation and increased capillary common causes of chronic hemorrhagic cystitis exept fragility resulting in hemorrage. This complication can occur in 2 to 40% of patients treated with in immunocompromised patients. cyclophosphamide. The onset of hematuria usually Paediatric and immunocompromised patients are occurs within 48 hours of treatment9-10. susceptible to develop viral hemorrhagic cystitis. The BK polioma virus, adenovirus type 7,11,34 and 35, Other systemic chemotherapeutic agents: Busulphan Cytomegalovirus, JC virus and Herpes virus have been (alkyl sulfonate compound used for leukemia) can implicated3-4. Polyoma virus is the most common cause hemorrhagic cystitis in 16% of patients, Danazol cause in a paediatric population and can cause (semi syntetic anabolic steroid) in 19% of patients hemorrhagic cystitis in 5.7% to 7.7% bone marrow with hereditary angioedema. Hematuria occurs after transplant recipients. The onset is from one to four a long interval and is related to dose. Tiaprofenic months after transplantation5. acid, temozolomide and 9-nitrocamptothecin (topoisomerase I inhibitor)11. Finally penicillin and its Systemic diseases synthetic derivatives like methicillin, carbenicillin, Hemorrhagic cystitis can occur in patients with ticarcillin, piperacillin and penicillin G can cause amyloidosis, rheumatoid artritis and Crohn’s disease. hemorrhagic cystitis through an immunological mechanism1. Drugs Occupational exposure to chemical substances, aniline, Topical agents can provoke a direct irritation of the a costituent of dyes, and toluidine, found in pesticides bladder mucosa. and shoes polish, can cause hemorrhagic cystitis. Also chlorodimeform with its metabolite 2-methylaniline Expert views (aniline derivative) commonly used on cotton plants March/May 2013 and fruit trees can cause hemorrhagic cystitis. The hematuria usually is self-limiting once the exposure to the agent is eliminated.12 Radiotherapy Radiation cystitis is a late complication of radiotherapy for prostate, bladder, rectal and gynaecological cancers treated conservatively. It occurs at least after 90 days after the initiation of RT but it may occur also after 10 years of treatment13. The frequency is about 10-20% of patients treated with external beam radiation develop bladder-related complications14. Among the histological features is a progressive obliterative endoarteritis that leads to ischemia of the bladder mucosa. Then, the mucosa ulcerates and bleeds. Neovascularity forms in the damaged areas causing the typical vascular blush seen at cystoscopy. The newly-formed vessels are more fragile. In case of bladder distension of minor trauma or any mucosal irritation bleeding is possible. Acute episodes usually stop in 12-18 months in most of these patients14. Late radiations injuries are irreversible and progressive. The time interval between the treatment and development of delayed symtoms is inversely proportional to the dose received15. The pathophysiology of late radiation damage includes cellular depletion, fibrosis and obliterative endoarteritis16. The fibrosis decreases the bladder capacity and patients complain of urgency, frequency and dysuria. In some cases incontinence may develop1. Grading of hemorrhagic cystitis A grading system for severity of hemorrhagic cystitis has been proposed by Droller17: 0. 1. 2. 3. 4. No symptoms of bladder irritability or hemorrgae Microscopic hematuria Macroscopic hematuria Macroscopic hematuria with small clots Massive macroscopic hematuria requiring instrumentation for clots evacuation and/or causing urinary obstruction The most important step in these patients is to determine the cause of hematuria. If the cause is not obvious a work-up with urine cytology, upper urinary tract imaging and cystoscopy should be performed. The patients medications should be reviewed and anticoagulants stopped. Laboratory evaluation with hemoglobin, complete blood count, blood urea, serum creatinine, coagulation profile and urine culture should be done1. Treatment of bacterial, fungal and viral hemorrhagic cystitis Bacterial and fungal hemorrhagic cystitis are usually cured with the appropriate antibiotic and antifungal therapy according to cultures. In case of viral cystitis, cidofovir is the drug of choice in immunosupressed patients1. Treatment of drug-induced hemorrhagic cystitis In case of drug-induced cystitis, immediate bladder irrigation is indicated. Oxybutynin, hydrocortisone, dymethyl sulfoxide and intravesical 50cc of 1% lidocaine with 100 mg of hydrocortisone help in alleviating symptoms5. Drugs should be stopped and in some cases, when possible, treatments delayed (chemo therapy or BCG instillation for bladder cancer). Exposure to chemicals like aniline or other agents should be eliminated. Usually hematuria is selflimiting in these cases. Treatment of hemorrhagic cystitis due to chemotherapeutic agents Stopping the drug or reducing the dose is the primary treatment. Hydration and forced diuresis is helpful to reduce the toxicity profile of the drugs. Continuous bladder irrigation (CBI) decreases the duration of exposure of the urothelium to acroelin, reducing toxicity. The drug sodium 2-mercaptoethane sulfonate (mesna) iv in three doses can prevent cystitis by ifosfamide and cyclophosphamide. Mesna is rapidly excreted by the urinary tract; the sulphydryl group complexes with the terminal methyl group of acrolein forming a non toxic thioether7. An initial dose equivalent to 20% of the ifosfamide dose is given 15 minutes before the drug, followed by the same doses four and eight hours later. The role of mesna in preventing hemoragic cystitis after cyclophosphamide is controversial. Two randomised controlled studies comparing mesna and hyperidratation or CBI showed no difference on the incidence of hematuria18-19. A study comparing combination of hyperbaric oxygen with mesna showed 93% urothelial protection vs 33% in the non-treated group. Since cyclophosphamide may produce bladder cancer (transitional cell carcinoma) in 2 to 5.5 % of patients7, mesna may reduce the risk20. Treatment of hemorrhagic cystitis due to radiation Prevention with accurate tailoring of radiation field limiting the dose to the bladder is the most important approach. New technologies like cyberknife can help in this. Continued on page 10 European Urology Today 9 Continued from page 9 Radiation-induced hemorrhagic cystitis is very difficult to treat because of the ischemic nature of the disease. Oral agents like steroids, Vitamin E, trypsin and orgotein have been used without success1. the sensory nerves of the bladder. A preliminary cystoscopy for clots evacuation and fulguration of bleeding vessels should be perfomed. The skin of the perineum must be protected with petroleum jelly. A 18F Foley catheter is introduced and 1-2% formalin under gravity is instilled into the bladder and kept for 15 minutes. About 10-30% of patients may not respond to low dose and may require a second instillation with high dose (4-10%)37. Hyperbaric oxygen (HBO) therapy has been extensively used and investigated. HBO involves the inhalation of 100% oxygen pressurized to 1.4 -3.0 atm in sessions of 60-120 minutes. These conditions stimulate angiogenesis, fibroblast proliferation and collagen “If the cause is not obvious a workformation21. Bevers reported the results of a up with urine cytology, upper urinary prospective study on 40 patients treated with 20 sessions of HBO for 90 minutes. The response rate after tract imaging and cystoscopy should three months was 92.5%, while after 23 months the be performed.” recurrence of hematuria was 12% per year22. Chong 23 confirmed these results . The drawbacks of HBO are risk of tumour growth (enhanced angiogenesis) and the high costs (10,000-15,000 US dollars per patient) Embolisation Super selective embolization with microcatheters of Hyaluronic acid at a dose of 40 mg/ml solution for 30 vesical arteries has been described by MacIvor et al. minutes, weekly, used as a preventive measure for with a success rate of 22-25%. Side effects include radiation cystitis determines a reduction of baldder gluteal pain (occlusion of the superior gluteal artery)38. complications by 33%. Shao et al reported the results of a study comparing intrvesical hyaluronic acid Surgery instillation vs HBO in 36 patients with radiationVarious surgeical procedures have been suggested. induced hemorrhagic cystitis. No side effects after HA Placement of bilateral nephrostomy tubes under US were seen. The improvement rate showed no statistical and occlusion of the ureteral orifices39, urinary difference between the two groups. Decrease of diversions, ligation of hypogastric artery and finally frequency was significant in both groups but persisted cystectomy have been described. Stillwell reported the in time (12 months) only in HA group. The improvement need of cystectomy in 5% of patients with intractable in the visual analogic scale remained significant in hemorrhagic cystitis from cyclophosphamide10. both groups at 18 months24. Conclusions WF-10-the formulation of terachlorodecaoxygen iv, a Treatment of hemorrhagic cystitis is difficult. A variety novel healing agent with immune effect (inhibition of of therapies have been described. However, due to the chronic inflammatory process) determined a complete rarity of this complication, large studies are lacking. response rate of 74-88% in patiens with RC from RT for Radiation-induced cystitis is more commonly seen by cervical cancers25. urologists because of the extensive use of radiotherapy for the treatment of locally advanced prostate cancer Treatment of intractable bladder hemorrhage and bladder cancer in some countries. HBO seems the The first step is to insert a three-way catheter to therapy of choice even if expensive. Surgery should be decompress the bladder, to evacuate clots and start considered as the last step for the treatment of this saline irrigation. In some cases cystoscopic complication. examination is needed. The bladder should be carefully evaluated and every single site of bleeding References fulgurate. In patients who do not respond to this 1. Manikandan R, Kumar S, Lalgudi D et al: Hemorragic treatment further therapies are needed cystitis: a challenge to the urologist. Indian J Urol Medical therapies Conjugated estrogens have been employed for the treatment of viral and radiation-induced cystitis with success rates from 60 to 86%26. Sodium pentosan polysulfates protects the surface of the bladder mucosa and can reduce the inflammatory response of the urothelium. One to eight weeks are needed to reduce the degree of hematuria27. Instillation therapy E-aminocaproic acid inhibits fibrinolosis by preventing the activation of plasminogen to plasmin. It is given orally, parenterally or intravesically by continuous bladder irrigation. The maximum recommended dosage in 24 hour is 30 mg. Sigh et al reported a response rate of 92% in 37 cases. The major disadvantage is the clots formation in the bladder. Patients should be clot-free before treatment. Alum (aluminium ammonium sulphate or aluminium potassium sulphate) irrigation causes protein precipitation, vasoconstriction and decreased capillary permeability28. The standard dose is 50 mg alum in a liter of sterile water via CBI 250 ml/h. Complete resolution of hematuria was achieved in 60-100% of patients in three to seven days29. Toxicity is minimal. In children and in patients with renal failure microcytic anemia, osteomalacia, dementia, encephalopaty, metabolic acidosis have been described30-31. Silver nitrate Instillations cause a chemical coagulation and eschar at the bleeding sites. It is instilled in the bladder as a solution at a concentration of 0.5 -1% kept for 10-20 minutes. Reflux should be excluded before instillation as renal failure due to precipitation and obstruction of upper tract has been described32. Prostaglandin E1, E2 and F2 alfa have a cytoprotective effect by regulating mucus production33. They can also cause a contraction of the blood vessels in the mucosa and submucosa via membrane stabilization. Another action is the determination of platelets aggregation. Side effects such as bladder spasm has been reported in 78% of patients34-35. Formalin (40% formaldehyde) is the most effective hemostatic agent used intravesically. Formalin rapidly fixes the bladder mucosa through a process involving protein cross-linking36. Reflux should be ruled out before instillation. Formalin must be instilled under general or spinal anesthesia since it is caustic to 10 European Urology Today Clin Oncol 1991;9:2016-20. 19. Vose JM, Reed EC, et al. Mesna compared with continuous bladder irrigation as uroprotection during high-dose chemotherapy and transplantation: A randomized trial. J Clin Oncol 1993;11:1306-10. 20.Cannon J, Linke CA, et al. Cyclophosphamide associated carcinoma of urothelium: Modalities for prevention. Urology 1991;38:413-6. 21. Marx RE, Ehler WJ, et al. Relationship of oxygen dose to angiogenesis induction in irradiated tissue. Am J Surg 1990;160:519-. 22.Bevers RF, Bakker DJ, et al. Hyperbaric oxygen treatment for haemorrhagic cystitis. Lancet 1995;346:803-5. 23. Chong KT, Hampson NB, et al. Early hyperbaric oxygen theraphy improves outcome for radiation induced haemorrhagic cystitis. Urology 2005;65:649-53. 24.Shao Y. et al. Comparison of intravesical hyaluronic acid instillation and hyperbaric oxygen in the treatment of radiation-induced hemorrhagic cystitis. BJUI. Volume 109, Issue 5, pages 691–694, March 2012 25.Veerasarn V, Boonnuch W, et al. A phase II study to evaluate WF 10 in patients with late haemorrhagic radiation cystitis and proctitis. Gynecol Oncol 2006;100:179-84. 26.Heath JA, Mishra S, et al. Estrogen as treatment of haemorrhagic cystitis in children and adolescents undergoing bone marrow transplantation. Bone Marrow Transplant 2006;37:523-6. 27. Hampson S, Woodhouse C. Sodium pentosanpolysulphate in the management of haemorrhagic cystitis: Experience with 14 patients. Eur Urol 1994;25:40-2. 28.Arrizabalaga M, Extramiana J, et al. Treatment of massive hematuria with aluminum salts. Br J Urol 1987;60:223-6. 29.Choong SK, Walkden M, et al. The management of intractable hematuria. BJU 2000;86:951-9. 30.Perazella M, Brown E. Acute aluminum toxicity and alum bladder irrigation in patients with renal failure. Am J Kidney Dis 1993;21:44-6. 31. Bogris SL, Johal NS, et al. Is it safe to use aluminum in the treatment of pediatric hemorrhagic cystitis? A case discussion of aluminum intoxication and review of the literature. J Pediatr Hematol Oncol 2009;31:285-8. 32.Ragavaiah NV, Soloway MS. Anuria following silver nitrate irrigations for intractable bladder haemorrhage. J Urol 1977;118:681-2. 33. Jeremy JY, Mikhailidis DP, et al. The rat urinary bladder produces prostacyclin as well as other prostaglandins. Prostaglandins Leukot Med 1984;16:235-48. 34.Levine LA, Krane DM. Evaluation of carboprost tromethamine in the treatment of cyclophosphamideinduced haemorrhagic cystitis. Cancer 1990;66:242-5. 35.Laszlo D, Bosi A, et al. Prostaglandin E2 bladder instillation for the treatment of hemorrhagic cystitis after allogeneic bone marrow transplantation. Haematologica 1995;80:421-5. 36.De Vries CR, Freiha FS. Hemorrhagic cystitis: A review. J Urol 1990;143:1-9. 37. Vicente J, Rios G, et al. Intravesical formalin for the treatment of massive hemorrhagic cystitis: Retrospective review of 25 cases. Eur Urol 1990;18:204-6. 38.McIvor J, Williams G, et al. Control of severe haemorrhage by therapeutic embolisation. Clin Radiol 1982;33:561-7. 39.Gonzalez CM, Case JR, et al. Glutaraldehyde cross-linked collagen occlusion of the ureteral orifices with percutaneous nephrostomy: A minimally invasive option of refractory hemorrhagic cystitis. J Urol 2001;166:977-8. 11-15 April 2014 2010;26:159-166. 2. Krane DM, Levine LA. Hemorrhagic cystitis. AUA Update Series 1992; XI: Lesson 31. 3. Erard V, Storer B, et al. BK virus infection in haematopoietic stem cell transplant receipents: Frequency, risk factors and association with post engraftment haemorrhagic cystitis. Clin Infect Dis 2004;39:1861-5. 4. Hofland CA, Eron LJ, et al. Haemorrhagic adenovirus cystitis after renal transplantation. Transplant Proc 2004;36:3025-7. 5. Dropulic LK, Jones RJ. Polyomavirus BK infection in blood and marrow transplant recipients. Bone Marrow Transplantation 2008;41:11-8. 6. Mayersak JS, Viviano CJ. Transurethral insertion of vaginal contraceptive suppository into the urinary bladder. Wis Med J 1994; 93:13-5. 7. Talar-Williams C, Hijazi YM, et al. Cyclophosphamideinduced cystitis and bladder cancer in patients with Wegener’s granulomatosis. Ann Intern Med 1996;124: 477-84. 8. Schoenike SE, Dana WJ. Ifosfamide and mesna. Clin Pharm 1990;9:179-91. 9. Cox PJ. Cyclophosphamide cystitis. Identification of acrolein as the causative agent. Biochem Pharmacol 1979;28:2045-9. 10. Stillwell TJ, Benson RC Jr. Cyclophosphamide- induced hemorrhagic cystitis. A review of 100 patients. Cancer 1988;61:451-7. 11. Islam R, Issacson BJ, et al. Hemorrhagic cystitis as an unexpected adverse reaction to temozolomide: Case report. Am J Clin Oncol 2002;25:513-4. 12. Folland DS, Kimbourgh RD, et al. Acute hemorrhagic cystitis. Industrial exposure to the pesticide chlordimeform. JAMA 1991;116:1052-5. 13. Cox JD, Stetz J, et al. Toxicity criteria of the Radiation Therapy Oncology (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341-6. 14. Corman JM, McClure D, et al. Treatment of radiation induced hemorrhagic cystitis with hyperbaric oxygen. J Urol 2003;169:2200-2. 15. Oration JP. Complications following radiation therapy in carcinoma cervix and their treatment. Am J Obstet Gynecol 1964;88:854-66. 16. Pasquier D, Hoelscher T, et al. Hyperbaric oxygen therapy in the treatment of radio-induced lesions in normal tissue: A literature review. Radiother Oncol 2004;72:1-13. 17. Droller MJ, Saral R, et al. Prevention of cyclophosphamide- induced hemorrhagic cystitis. Urology 1982;20:256-8. 18. Shepard JD, Pringle LE, et al. Mesna versus hyperhydration for the prevention of cyclophosphamide induced hemorrhagic cystitis in bone marrow transplantation. J SEPTEMBER 8–12, 2013 www.siucongress.org Featuring the ICUD Consultations on Upper Tract Urothelial Carcinoma Congenital Anomalies in Children 3006_SIU2013_EUT_Vancouver_JAN_b.indd 1 Client: SIU 2013 Description: Vancouver Docket number: 23-3006 13-01-15 10:36 AM March/May 2013 File Size: Trim Size: 100 % 133,4 mm X 194,3 mm Clinical challenge Prof. Oliver Hakenberg Section editor Rostock (DE) Case study No. 33 The Clinical challenge section presents interesting or difficult clinical problems which in a subsequent issue of EUT will be discussed by experts from different European countries as to how they would manage the problem. Oliver.Hakenberg@ med.uni-rostock.de This 64-year-old lady presented with the incidental finding of presumably neoplastic lesion of the right kidney (fig. 1). Pre-operative staging, however, showed pulmonary hilar lesions on the left side (fig. 2) which were considered to be neoplastic as well. A transbronchial biopsy of the hilar lesion was done and histology was assessed as being compatible with renal cell carcinoma. Readers are encouraged to provide interesting and challenging cases for discussion at [email protected] Case study No. 32 This 27-year-old university student was referred to our department by an office urologist initially with a testicular tumour in stage III (embryonal carcinoma). He had been surgically treated by left radical orchidectomy in December 2011. After complete staging which showed multiple pulmonary, large hepatic and retroperitoneal lymph node disease, he underwent three courses of PIE chemotherapy (cisplatin, ifosfamide, etoposide) with full dosage and re-staging after the second cycle which showed good response in all sites. He underwent retroperitoneal lymphadenectomy in March 2012 with removal of all residual retroperitoneal disease; the histology of the nodes removed showed necrosis and a small area of mature teratoma. At surgery, the hepatic lesions had also been biopsied showing necrosis (figure 1). Following this, the patient received two more courses of PIE chemotherapy. Re-staging showed shrinkage of all remaining lesions. One of the larger pulmonary lesions was surgically removed Fig. 2: CT scan of April 2012 showing the large of pulmonary lesion which was surgically removed Fig. 1: CT scan of March 2012 showing hepatic metastases in May 2012 (figure 2) with histology also showing necrosis only. The only marker which had been elevated was HCG which had normalized after the first three courses of chemotherapy. In October 2012, the office urologist informed us that the patient was well but the HCG had increased to 27 U/l (normal range up to 4 U/l). Re-staging was initiated which showed further regression of the remaining known lesions. Within three weeks, however, HCG had increased to 3000 U/l and the patient was referred to us again. He was admitted one week later and on admission HCG was 9000 U/L. Another staging including a PET/CT reported reduction in size of all known lesions, no new lesions and some new metabolic activity in projection to the pleura. Fig. 1: CT scan of the abdomen Discussion points: 1. Are other diagnostic tests useful? 2. What treatment options are available? 3. What is the prognosis? Case provided by O. Hakenberg, Dept. of Urology, Rostock University, Germany. [email protected] A chance of cure with removal of all residual masses and chemotherapy Comments by Prof. Dr. Walter Albrecht Mistelbach (AT) chemotherapy (PEI/VIP or TIP or VeIP) will result in long-term remission of about 50%. Initially this young man has been a case of stage III nonseminomatous germ cell tumour belonging to the poor prognosis group according to the IGCCCG staging system. The five-year survival rate is not more than 50%. EAU guidelines are recommending four cycles of PEB chemotherapy (cisplatin, etoposide, bleomycin) followed by complete resection of all metastatic sites within four to six weeks as standard therapy. In case of necrosis and/or teratoma no further treatment is needed. In case of relapse, four cycles of cisplatin-combination Instead of this the patient only received three cycles of PEI, followed by retroperitoneal lymphadenectomy. Histological workup showed necrosis and mature teratoma, as did the biopsies of the liver metastases and one surgically removed pulmonary lesion. Obviously, further surgery has been calculated to be risky; therefore two more cycles of PEI have been administered showing shrinkage of all remaining lesions together with normalisation of HCG. the more myelotoxic regimen? It may be speculated that bleomycin has been avoided because of an unreported impairment of lung function. Why was retroperitoneal lymphadenectomy performed already after the third instead of the fourth cycle of chemotherapy leading to a delay of further cycles? Fig. 2: Pulmonary CT scan Discussion points: 1. Are other diagnostic tests useful? 2. What treatment options are available? 3. What should be done? As dramatic increase of HCG has been documented, it may be recommended to also check the brain and bones for metastases. As there may be some vital cancer cells especially in the liver, an attempt to remove all residual lesions should be made now followed by second-line chemotherapy. Case provided by O. Hakenberg, Dept. of Urology, Rostock University, Germany. [email protected] Five months later a dramatic increase of HCG up to 9000 U/l occurred but restaging showed further reduction of all known lesions. Nevertheless the five-year survival rate of approximately 50% may be further compromised by the probably insufficient preoperative cisplatin dose and the incomplete resection of all lesions Some questions arise: why was PEI chosen as a first-line chemotherapy instead of BEP although being after chemotherapy. Case Study No. 31 continued This patient had initially been treated by PIE chemotherapy in view of a history of bronchial asthma and because the treating urologist wanted to avoid bleomycinerelated pulmonary toxicity. Retroperitoneal lymphadenectomy was performed after only three cycles of chemotherapy instead of four. However, all removed and biopsied lesions showed necrosis with only one retroperitoneal node also showing a small amount of mature teratoma. Surgical removal of all lesions was never an option as there were too many especially in both lungs. In view of the fact, that preoperative chemotherapy had been insufficient it was considered necessary to add two more cycles of PIE which had shown efficacy before. Following this, the patient developed recurrence after six months. European Urology Today - Manuscript Submission European Urology Today, the EAU newsletter is published five times each year. Its main role is to function as the European Association of Urology’s bulletin, as a platform for the EAU to present their meetings, the various sections and offices, as well as discuss general issues of interest to their members. Another important objective is to have a platform that allows for the inclusion of a range of scientific papers which are considered of interest to a large readership. Editorial Policy Manuscripts are submitted with the explicit understanding that the decision to include material will be made by the Editor-in-Chief in conjunction with his Section Editors. All authors have read and approved the manuscript subject to submission. It is the author’s responsibility to obtain permission to reproduce any parts of other publications (i.e., tables, figures). Precise reference to the original work must be given in the legends. Statements in articles or opinions expressed by any contributor in any article are not the responsibility of the editors or the publisher. The publisher is not responsible for the loss of manuscripts through circumstances beyond their control. The publisher will commit itself to make judicious use of the article in accordance with the aims and objectives of the association and make the article available to medical professionals at no cost. August/September 2011 March/May 2013 Manuscript Submission Manuscripts and questions regarding manuscript submission may be directed to: European Association of Urology European Urology Today Editorial Office P.O. Box 30016 6803 AA Arnhem, The Netherlands Telephone: +31 (0)26 389 0680 E-mail: [email protected] Submission of an article signifies the author’s consent to transfer copyright to the EAU, publisher of European Urology Today. All authors are kindly requested to submit a photograph of themselves (and their co-authors). Case Submission Interesting and challenging cases are published and discussed in the Clinical Challenge section. Please submit your case for consideration to the EUT Editorial Office. Submission platforms All material is to be submitted in English, as Word file, TXT files for text and JPG, TIFF, PPT for illustrations. All illustrations must be a minimum of 300 dpi to meet printing quality. For files over 10 MB an upload server is available. Word count for authors is available on our website (Publications, European Urology Today) and on request at the EUT Editorial Office. Proofs Young Urologists/Resident Corner Accepted manuscripts will be copy-edited to bring them into conformity with the journal’s style. Unless otherwise indicated, proofs are sent in PDF format via e-mail to the corresponding author. Proofs must be returned within the deadline specified by the publisher. This section is reserved for articles of which the first author is a resident in training. All material is to be submitted for consideration to the section editor responsible for this section, Dr. Christian Ruf, [email protected] Types of Articles Original articles Original articles may be solicited by the editorial board or submitted to the editorial board for consideration. In case of doubt, authors are encouraged to check with the editorial board describing the content of their article before submission. Maximum word count for original articles is approximately 2,000 words, exclusive of references and illustrations. In case authors provide large reference files, the editor-in-chief may decide to either limit the total number of references included in the print, or make references available on request through [email protected]. Effects and Actions: International Meeting Reports Maximum word count for submitted articles is approximately 2,000, exclusive of references and illustrations. All material is to be submitted initially to the EUT Editorial Office, [email protected] Reports (General - Accredited/ Certified Centres – etc) General reports and papers on interesting developments/urology departments/accreditation etc. may be submitted for consideration to the Editor-in-Chief. Illustrations are welcome. Word count for reports are approximately 900/1,000 words. Reviews of books, journals and new media The patient was then restarted on PIE chemotherapy as re-staging had shown further shrinkage of all lesions. This led to an HCG-response which was, however, comparatively slow. After two cycles, TIP chemotherapy was started together with stem cell harvesting. TIP led to a further marked reduction of HCG but again the kinetics were not considered adequate. Therefore, high-dose chemotherapy was started which the patient is currently undergoing. Books, journals and new media to be considered for review may be sent to the EUT Editorial Office. Letters to the editor Authors are welcome to submit letters to the editor. The text of letters should be limited to 500 words. Letters to the editor will be published as space permits. Information All queries on manuscript submission should be directed to the EUT Editorial Office at [email protected]. European Urology Today 21 European Urology Today 11 Key articles from international medical journals Prof. Oliver Reich Section editor Munich (DE) quartile compared with 2,000 cases prevented by a similar effort in the lowest PRS quartile (Padditive = 1 × 10-4). Thus, the potential impact of eliminating smoking on the number of bladder cancer cases prevented is obviously larger for individuals at higher than at lower genetic risk. Oliver.Reich@ klinikummuenchen.de The findings have implications for targeted prevention strategies should genetic analysis become widely available and will undoubtedly serve as a basis for cost-benefit analysis for competing political intentions regarding health care, tobacco industries and tax revenues. Insulin-like growth factor receptor-binding protein 5 identified as a promising marker in urothelial carcinoma In an exemplary way the authors of this study systematically searched for and identified a new marker for urothelial cancer. They assessed the published transcriptome of urinary bladder urothelial cancer and identified insulin-like growth factorbinding protein-5 (IGFBP-5) as the most significantly up-regulated gene associated with the regulation of cell growth. IGFBP-5 is one of the binding proteins that regulate insulin-like growth factors (IGFs). By immunohistochemistry the IGFBP-5 expression status and its associations with clinicopathological features and survival in 340 cases of upper urinary tract urothelial carcinoma (UUT) and 295 cases of urothelial bladder cancer (UBC) were evaluated. Additionally, western blot analysis was performed to evaluate IGFBP-5 protein expression in human urothelial cell lines. IGFBP-5 overexpression was significantly associated with advanced pT stage (p < 0.001), higher histological grade (UUT, p < 0.001; UBC, p = 0.035), lymph node metastasis (UUT, p = 0.006; UBC, p = 0.004), vascular invasion (UUT, p < 0.001; UBC, p = 0.003), perineural invasion (UUT, p = 0.034; UBC, p = 0.021) and frequent mitosis (UUT, p < 0.001; UBC, p = 0.023). IGFBP-5 overexpression independently predicted poor disease-specific survival and metastasis-free survival in both groups of patients. Western blot analysis showed IGFBP-5 protein overexpressed in human urothelial cancer cell lines. The authors demonstrated convincingly that IGFBP-5 plays an important role in tumour progression in urothelial carcinoma and that its overexpression is associated with advanced tumour stage and signifies poorer clinical outcome. Source: IGFBP-5 overexpression as a poor prognostic factor in patients with urothelial carcinomas of upper urinary tracts and urinary bladder. Liang PI, Wang YH, Wu TF, Wu WR, Liao AC, Shen KH, Hsing CH, Shiue YL, Huang HY, Hsu HP, Chen LT, Lin CY, Tai C, Wu JY, Li CF. Cancer Res. 2013 Mar 27. [Epub ahead of print] Cigarette smoking and genetic susceptibility: 6.2% life-time risk The main environmental risk factor for bladder cancer today is cigarette smoking; however, genetic susceptibility is of great importance. This paper gives a detailed analysis of the risk of developing bladder cancer in a smoking population. The analyses included up to 3,942 cases and 5,680 controls of European background in seven studies. The authors tested for multiplicative and additive interactions between smoking and 12 susceptibility loci, individually and combined as a polygenic risk score (PRS). Thirty-year absolute risks and risk differences by levels of the PRS were estimated for U.S. males aged 50 years. Six of 12 variants showed significant additive gene-environment interactions, most notably NAT2 (p = 7 × 10-4) and UGT1A6 (p = 8 × 10-4). The 30-year absolute risk of bladder cancer in U.S. males was 6.2% for all current smokers (range 2.9% to 9.9%). Risk difference estimates indicated that 8,200 cases would be prevented if elimination of smoking occurred in 100,000 men in the upper PRS Key articles 12 death donors older than 60 years compared with brain-death donors of the same age group. Prolonged cold ischaemic time (> 24 hrs. vs. < 12 hrs.) was not associated with decreased graft survival for all decreased-donor kidneys, but was associated with poorer graft survival for kidneys from circulatorydeath donors than for those from brain-death donors (HR 2.36, [CI 1.39-4.02, p = 0.004]). This study shows that there is no difference in the effect of donor age between kidneys from circulatorydeath and brain-death donors and this will help reassure clinicians when considering potential kidneys Source: Common Genetic Polymorphisms Modify offered for transplantation. However, the finding that increasing cold storage times is associated with the Effect of Smoking on Absolute Risk of inferior transplant outcomes for kidneys from Bladder Cancer. Garcia-Closas M, Rothman N, Figueroa JD, Prokunina-Olsson L, Han SS, Baris circulatory death donors will need to inform the future development of the UK national allocation policy. D, Jacobs EJ, Malats N, De Vivo I, Albanes D, Purdue MP, Sharma S, Fu YP, Kogevinas M, Wang Z, Tang W, Tardón A, Serra C, Carrato A, García-Closas R, Lloreta J, Johnson A, Schwenn M, Karagas MR, Schned A, Andriole G Jr, Grubb R 3rd, Black A, Gapstur SM, Thun M, Diver WR, Weinstein SJ, Virtamo J, Hunter DJ, Caporaso N, Landi MT, Hutchinson A, Burdett L, Jacobs KB, Yeager M, Fraumeni JF Jr, Chanock SJ, Silverman DT, Chatterjee N. Cancer Res; 73(7); 1-10, 2012 Circulatory-death donor kidneys don’t tolerate the cold Transplantation is the preferred treatment for end-stage kidney disease but there is a severe shortage of decreased-donor kidneys. In the UK, this has led to an increasing use of kidneys from circulatory-death donors. Unlike those donated after brain death these incur substantial warm ischemic injury before and during procurement, which results in poor function immediately after transplantation. However, emerging evidence shows they provide satisfactory graft function at least in the medium term (five years). Source: Effect of donor age and cold storage time on outcome in recipients of kidneys donated after circulatory death in the UK: a cohort study. Summers DM, Johnson RJ, Hudson A, Collett D, Watson CJ, Bradley JA. Lancet 2013; 381: 727-34. SEER analysis shows no progress in bladder cancer survival since 1973 The purpose of the analysis was to examine the overall and stage-specific age-adjusted incidence, five-year survival and mortality rates of bladder cancer in the United States, between 1973 and 2009. For this end, a total of 148,315 bladder cancer patients were identified in the Surveillance, Epidemiology and End Results database (SEER) between years 1973 and 2009. Incidence, mortality, and five-year cancerspecific survival rates were calculated. Temporal trends were quantified using the estimated annual percentage change (EAPC) and linear regression models. All analyses were stratified according to disease stage and further examined according to sex, race, and age groups. For results, the authors report an increase in the incidence rate of bladder cancer from 21.0 to 25.5/100,000 personyears between 1973 and 2009. This has led to greater acceptance at least when donors are less than 60 years. It is therefore of increasing importance to understand if kidneys from circulatory-death donors aged older than 60 years fare any worse than kidneys from brain-death donors. In addition, as kidneys are allocated on a national Stage-specific analyses revealed an increase incidence basis, it is important to understand any extra risks this for localised stage from 15.4 to 20.2 (EAPC: +0.5%, p poses kidneys from circulatory-death donors. < 0.001) and distant stage from 0.5 to 0.8 (EAPC: +0.7%, p = 0.001). During the period examined, This paper, using data from the UK transplant registry, stage-specific five-year survival rates increased for all includes all adult recipients of deceased-donor renal stages, except for that of distant (metastatic) disease. transplants between 1.1.05 and 1.11.10. Recipients No significant changes in mortality were recorded were excluded from the main analysis if they had among localised (EAPC: _0.2%, p = 0.1) and regional received a previous renal transplant. All-cause graft stage (EAPC: _0.1%, p = 0.5). failure was taken as time from transplantation to graft nephrectomy or return to dialysis, or death of the An increase in mortality rates was observed among patient with a functioning graft. Delayed graft function distant stage (EAPC: +1.0%, p = 0.005). Significant was defined as the need for dialysis within the first variations in incidence and mortality were recorded seven days after transplantation. Graft function was when estimates were stratified according to sex, race, measured from the estimated glomerular filtration and age groups. rate (eGFR). Overall, statistically significant changes were observed, although all were minor. The authors noted This study shows that there is no that little or no change in bladder cancer outcomes difference in the effect of donor age has been achieved during the period studied. between kidneys from circulatorydeath and brain-death donors… 6490 decreased-donor kidney transplants were done at 23 centres. Primary non-function was higher in recipients of kidneys from circulatory-death donors than in recipients of kidney from brain death donors (4% vs. 3% p = 0.04) as was delayed graft function (49% vs. 24% [HR 3.08, p < 0.0001]). Three-year graft survival showed no difference between circulatorydeath (n = 1768) and brain-death (n = 4127) groups (HR 1.14, [CI 0.95-1.36, p = 0.16]). Graft function was marginally lower at 12 months after transplantation in recipients of circulatory-death donor kidneys compared with recipients of brain-death donor kidneys (eGFR 48 ml/min per 1.73 m2 vs. 50 ml/min per 1.73 m2 p = 0.01). Donor age older than 60 years (compared with < 40 years) was associated with an increased risk of graft loss for all decreased-donor kidneys (HR 2.35, [CI 1.85-3.00, p < 0.001]) but there was no increased risk of graft loss for circulatory- Source: Incidence, survival and mortality rates of stage-specific bladder cancer in United States: A trend analysis. Firas Abdollah, Giorgio Gandaglia, Rodolphe Thuret, Jan Schmitges, Zhe Tian, Claudio Jeldres, Niccolo Maria Passoni, Alberto Briganti, Shahrokh F. Shariat, Paul Perrotte, Francesco Montorsi, Pierre I. Karakiewicz, Maxine Sun. mortality (CSM) rate and other-cause mortality (OCM) rate for patients with newly diagnosed bladder cancer. All patients (n = 3281) identified from a population-based cancer registry diagnosed between 1994 and 2009 were identified, with a median follow-up interval of 48 months (IQ range 18.1–98.7). Competing risk analysis was performed within patient groups and outcomes compared using Gray’s test. At five years after diagnosis, 1,246 (40%) patients had died, (19%) from bladder cancer and 629 (19%) from other causes. The five-year cancer-specific mortality rate varied between 1% and 59%, and OCM rate between 6% and 90% and this depended primarily on the tumour type and patient age. Cancer-specific mortality was highest in the oldest patient groups: few elderly patients received radical treatment for invasive cancer (52% vs 12% for patients < 60 vs. > 80 years, respectively). Female patients with high-risk non-muscle-invasive bladder cancer had worse cancer-specific mortality than equivalent males (Gray’s p < 0.01) although the rate of BCG usage was not different. The authors thus showed that effective treatment is probably underused in the elderly accounting for their higher cancer-specific mortality. Also, gender-specific differences seem to exist certainly in outcomes if not in management. These data must be taken into account by clinicians and obviously management should be adjusted. Source: Competing mortality in patients diagnosed with bladder cancer: evidence of undertreatment in the elderly and female patients. A P Noon, P C Albertsen, F Thomas, D J Rosario and J W F Catto. British Journal of Cancer advance online publication 12 March 2013; doi: 10.1038/bjc.2013.106 Two-weekly versus threeweekly docetaxel to treat castration-resistant advanced prostate cancer: a randomised, phase 3 trial Docetaxel administered every three weeks is a standard treatment for castration-resistant advanced prostate cancer. The authors of this study hypothesised that two-weekly administration of docetaxel would be better tolerated than threeweekly docetaxel in patients with castration-resistant advanced prostate cancer, and initiated a prospective, multicentre, randomised, phase 3 study to compare efficacy and safety. Eligible patients had advanced prostate cancer (metastasis, a prostate-specific-antigen test result of more than 10·0 ng/mL, and WHO performance status score of 0—2), had received no chemotherapy (except with estramustine), had undergone surgical or chemical castration, and had been referred to a treatment centre in Finland, Ireland, or Sweden. Enrolment and treatment were done between March 1, 2004, and May 31, 2009. Randomisation was done centrally and stratified by centre and WHO performance status score of 0—1 vs 2. Patients were assigned 75 mg/m2 docetaxel intravenously on day 1 of a three-week cycle, or 50 mg/m2 docetaxel intravenously on days 1 and 15 of a four-week cycle. 10 mg oral prednisolone was administered daily to all patients. The primary endpoint was time to treatment failure (TTTF). Data in the per-protocol population was assessed. The study is registered with ClinicalTrials.gov, number NCT00255606. 177 patients were randomly assigned to the twoweekly docetaxel group and 184 to the three-weekly Cancer Epidemiology (2013), http://dx.doi.org/10.1016/j. group. 170 patients in the two-weekly group and 176 in the three-weekly group were included in the canep.2013.02.002 analysis. The two-weekly administration was associated with significantly longer TTTF than the three-weekly administration (5·6 months, 95% CI Effective treatment for 5·0—6·2 vs 4·9 months, 4·5—5·4; hazard ratio 1·3, 95% bladder cancer underused in CI 1·1—1·6, p=0·014). Grade 3—4 adverse events occurred more frequently in the three-weekly than in females and in the elderly the two-weekly administration group, including neutropenia (93 [53%] vs 61 [36%]), leucopenia (51 [29%] vs 22 [13%]), and febrile neutropenia (25 [14%] In contrast to a SEER database analysis, this smaller vs six [4%]). Neutropenic infections were reported population-based study investigates cancer-specific and competing mortality risks in bladder cancer. Thus, more frequently in patients who received docetaxel every three weeks (43 [24%] vs 11 [6%], p=0·002). the authors determined the bladder cancer-specific EAU EU-ACME Office European Urology Today March/May 2013 Prof. Oliver Hakenberg Section editor Rostock (DE) Oliver.Hakenberg@ med.uni-rostock.de Women’s Health; ClinicalTrials.gov number, NCT01166438. Source: Anticholinergic therapy vs. OnabotulinumtoxinA for urgency urinary incontinence. Anthony G. Visco, Linda Brubaker, Holly E. Richter, Ingrid Nygaard, Marie Fidela R. Paraiso, Shawn A. Menefee, Joseph Schaffer, Jerry Lowder, Salil Khandwala, Larry Sirls, Cathie Spino, Tracy L. Nolen, Dennis Wallace, and Susan F. Meikle, for the Pelvic Floor Disorders Network. N Engl J Med 2012; 367:1803-1813November 8, 2012; The authors concluded that administration of DOI: 10.1056/NEJMoa1208872 docetaxel every two weeks seems to be well tolerated in patients with castration-resistant advanced prostate cancer and could be a useful option when threeBone density testing among weekly single-dose administration is unlikely to be prostate cancer survivorstolerated. does it happen? Funding: Sanofi. Source: Two-weekly versus three-weekly docetaxel to treat castration-resistant advanced prostate cancer: a randomised, phase 3 trial. Pirkko-Liisa Kellokumpu-Lehtinen, Ulrika Harmenberg, Timo Joensuu, Ray McDermott, Petteri Hervonen, Claes Ginman, Marjaana Luukkaa, Paul Nyandoto, Akseli Hemminki, Sten Nilsson, John McCaffrey, Raija Asola, Taina Turpeenniemi-Hujanen, Fredrik Laestadius, Tiina Tasmuth, Katinka Sandberg, Maccon Keane, Ilari Lehtinen, Tiina Luukkaala, Heikki Joensuu, for the PROSTY study. The Lancet Oncology, Volume 14, Issue 2, Pages 117 - 124, February 2013. doi:10.1016/S1470-2045(12)70537-5 Anticholinergic therapy vs. OnabotulinumtoxinA for urgency urinary incontinence Anticholinergic medications and onabotulinumtoxinA are used to treat urgency urinary incontinence, but data directly comparing the two types of therapy are needed. Most patients with prostate cancer become long-term survivors of the disease and so awareness of the late complications of therapy is important. Androgendeprivation therapy (ADT) is the most frequently used systemic therapy with up to 50% of men receiving ADT during the course of their disease. It improves overall survival when given as an adjuvant therapy for men with high-risk tumours undergoing radiotherapy and improves quality of life for men with metastatic cancer. Since 2008 guidelines of the National Comprehensive Cancer Network have recommended routine bone density testing before and during treatment to characterise the risk of fracture. In addition, the American College of Physicians 2008 guidelines recommend bone density testing among men receiving treatment with ADT. However, singleinstitution data to date shows low rates of testing. This paper presents data on bone density testing in a large population based cohort of older men with prostate cancer in the USA who received ADT for at least one year. March/May 2013 However, a recent modelling study suggested that bone density testing to guide treatment with bisphosphonates in men who are receiving ADT for localised prostate cancer is a cost-effective approach to this aspect of survivorship care. Thus, as efforts to improve the delivery of cost-effective preventive care increase, measuring and incentivising the use of bone density testing for this population may be an effective strategy. Source: Bone density testing among prostate cancer survivors treated with androgendeprivation therapy. Morgans AK, Smith MR, O’Malley AJ, Keating NL. Cancer 2013; 119: 863-70. Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer The authors of this EORTC trial report on the long-term results of immediate postoperative irradiation versus a wait-and-see policy in patients with prostate cancer extending beyond the prostate, aimed to confirm whether previously reported progression-free survival was sustained. This randomised, phase 3, controlled trial recruited patients aged 75 years or younger with untreated cT0—3 prostate cancer (WHO performance status 0 or 1) from 37 institutions across Europe. Eligible patients were randomly assigned centrally (1:1) to postoperative irradiation (60 Gy of conventional irradiation to the surgical bed for six weeks) or to a The SEER/Medicare data was used for this analysis. wait-and-see policy until biochemical progression 136,066 men with local or regional prostate cancer (increase in prostate-specific antigen >0·2 μg/L diagnosed from 2001 and 2007 and aged > 66 years at confirmed twice at least two weeks apart). The diagnosis who were enrolled with Medicare for a year investigators analysed the primary endpoint, before diagnosis and at least six months after biochemical progression-free survival, by intention to diagnosis. Men with metastatic disease were not treat (two-sided test for difference at α=0.05, adjusted for one interim analysis) and did exploratory included as done density scan is unreliable in bone analyses of heterogeneity of effect. The trial is with secondary deposits; moreover, guidelines registered with ClinicalTrials.gov, number recommend bisphosphonate therapy for metastatic NCT00002511. disease. The authors performed a double-blind, doubleplacebo–controlled, randomised trial involving women with idiopathic urgency urinary incontinence who had five or more episodes of urgency urinary incontinence per three-day period, as recorded in a diary. For a six-month period, participants were randomly assigned to daily oral anticholinergic medication (solifenacin, 5 mg initially, with possible …a recent modelling study escalation to 10 mg and, if necessary, subsequent switch to trospium XR, 60 mg) plus one intradetrusor suggested that bone density injection of saline or one intradetrusor injection of 100 testing to guide treatment with U of onabotulinumtoxinA plus daily oral placebo. The primary outcome was the reduction from baseline in bisphosphonates in men who are mean episodes of urgency urinary incontinence per receiving ADT for localised prostate day over the six-month period, as recorded in three-day diaries submitted monthly. Secondary cancer is a cost-effective approach. outcomes included complete resolution of urgency urinary incontinence, quality of life, use of catheters, and adverse events. Of these 29,860 men were identified who had received ADT continuously for at least a year. Receipt Of 249 women who underwent randomization, 247 of bone density testing was assessed from six months were treated, and 241 had data available for the before diagnosis to one year after the initiation of primary outcome analyses. The mean reduction in ADT. Demographic data was collected along with data episodes of urgency urinary incontinence per day over on who was treating the patient in an attempt to the course of six months, from a baseline average of identify factors associated with testing. 5.0 per day, was 3.4 in the anticholinergic group and 3.3 in the onabotulinumtoxinA group (P=0.81). Overall 10.2% of men underwent bone density testing Complete resolution of urgency urinary incontinence during the study period. Bone density testing was reported by 13% and 27% of the women, increased over time (14.5% of men who initiated ADT respectively (P=0.003). Quality of life improved in both in 2007-2008 vs. 6% of men who initiated ADT in 2001-2002; odds ratio for 2007-2008 vs. 2001-2002, groups, without significant between-group 2.29; 95% CI, 1.83-2.85). differences. The anticholinergic group had a higher rate of dry mouth (46% vs. 31%, P=0.02) but lower Men aged over 85 years were less likely to undergo rates of catheter use at two months (0% vs. 5%, testing when compared with men less than 70 years P=0.01) and urinary tract infections (13% vs. 33%, but there was no difference among the other age P<0.001). groups. Black men were less likely than white men to undergo testing (OR, 0.72; 95% CI, 0.61-0.86), and The authors concluded that oral anticholinergic men who were not black or Hispanic had higher rates therapy and onabotulinumtoxinA by injection were associated with similar reductions in the frequency of of testing than white men (OR, 1.39; 95% CI, 1.13-1.71). Men living in areas with higher educational daily episodes of urgency urinary incontinence. The group receiving onabotulinumtoxinA was less likely to attainment were more likely to undergo bone density testing than those living in areas with the lowest have dry mouth and more likely to have complete education levels (p < 0.001). Men who visited a resolution of urgency urinary incontinence but had higher rates of transient urinary retention and urinary medical oncologist and/or a primary care provider in addition to a urologist had higher odds of testing than tract infections. men who only consulted a urologist (p < 0.001). Funding: Eunice Kennedy Shriver National Institute of Evidence about the adverse effects of ADT on Child Health and Human Development and the skeletal health has been available for almost a decade National Institutes of Health Office of Research on Key articles but this appears to have little effect on clinical practice. Perhaps because the data available is based upon bone mineral density rather than fracture prevention, and therefore is not believed to be clinically relevant. It would be interesting to understand bisphosphonate usage alongside screening as it is possible men are receiving treatment without bone density testing. A total of 1,005 patients were randomly assigned to a wait-and-see policy (n=503) or postoperative irradiation (n=502) and were followed up for a median of 10·6 years (range two months to 16·6 years). Postoperative irradiation significantly improved biochemical progression-free survival compared with the wait-and-see policy (198 [39·4%] of 502 patients in postoperative irradiation group vs 311 [61·8%] of 503 patients in wait-and-see group had biochemical or clinical progression or died; HR 0·49 [95% CI 0·41—0·59]; p<0·0001). Late adverse effects (any type of any grade) were more frequent in the postoperative irradiation group than in the wait-andsee group (10 year cumulative incidence 70·8% [66·6—75·0] vs 59·7% [55·3—64·1]; p=0.001). Results at median follow-up of 10·6 years showed that conventional postoperative irradiation significantly improves biochemical progression-free survival and local control compared with a wait-andsee policy, supporting results at five-year follow-up; however, improvements in clinical progression-free survival were not maintained. Exploratory analyses suggest that postoperative irradiation might improve clinical progression-free survival in patients younger than 70 years and in those with positive surgical margins, but could have a detrimental effect in patients aged 70 years or older. Funding: Ligue Nationale contre le Cancer (Comité de l’Isère, Grenoble, France) and the European Organisation for Research and Treatment of Cancer (EORTC) Charitable Trust. Source: Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: long-term results of a randomised controlled trial (EORTC trial 22911). Michel Bolla, Hein van Poppel, Bertrand Tombal, Kris Vekemans, Luigi Da Pozzo, Theo M de Reijke, Antony Verbaeys, Jean-François Bosset, Roland van Velthoven, Marc Colombel, Cees van de Beek, Paul Verhagen, Alphonsus van den Bergh, Cora Mr Philip Cornford Section editor Liverpool (GB) Philip.Cornford@ rlbuht.nhs.uk Sternberg, Thomas Gasser, Geertjan van Tienhoven, Pierre Scalliet, Karin Haustermans, Laurence Collette, for the European Organisation for Research and Treatment of Cancer, Radiation Oncology and Genito-Urinary Groups. The Lancet, Volume 380, Issue 9858, Pages 2018 - 2027, 8 December 2012. doi:10.1016/S0140-6736(12)61253-7 PSA testing causes stress The European Randomized Study of Screening for Prostate Cancer noted that 75% of men with an elevated PSA have a negative biopsy. Clearly such false positive results led to unnecessary invasive procedures but evidence suggests it also causes increased utilisation of health care resources and decreased adherence to further screening. In women a false positive mammogram has been shown to be associated with a reduced quality of life and feelings of anxiety that lasted for at least a year. In this study qualitative methods were used to obtain descriptions of the long-term emotional consequences for men who had an elevated PSA and one or more negative biopsies. Data presented was acquired between March 2009 and May 2010 in New Jersey and is a subset (16) of a larger study (64) looking at men’s decisions regarding prostate cancer screening. In this group all men had a positive screening test and one or more negative biopsies. Interviews were recorded and lasted 30-90 minutes. The interview guide was developed using Andersen’s Behavior Model of Health service as the conceptual framework. The data obtained was analysed by a team containing two family physicians and two sociologists using iterative cycles of readings and reflection. As for most men, elevated PSA led to a cascade of biopsies and further PSA tests, as there is no consensus about how often biopsies should be repeated. All subjects not unsurprisingly experienced transient anxiety while waiting for the results of their prostate biopsies. This anxiety occurred with every biopsy, not just the first one. In addition it was possible to identify three persistent emotional responses. The attitude and recommendation of the urologist was influential in how men responded to false positive screening tests. a)Increased fear of cancer (5) appeared to be associated with the urologist emphasising the lack of certainty of a negative biopsy. Indeed one man was so worried he wanted a prophylactic prostatectomy. There was also frustration with uncertainties of PSA screening. b)Relief with increased vigilance (7). The most common outcome after a negative biopsy was to request more frequent screening. c)Relief with less worry about elevated PSA (4). More common in men who had had multiple biopsies and when the urologist reassured men about their persistently elevated PSA. This study reported significant emotional consequences that persisted for up to 24 years after the initial biopsy. As for most men, elevated PSA led to a cascade of biopsies and further PSA tests, as there is no consensus about how often biopsies should be repeated. This results in increased fear of cancer or increased vigilance about prostate cancer. This data suggests we need to develop evidencebased guidelines about further testing after a negative prostate biopsy. Source: Emotional consequences of persistently elevated PSA with negative prostate biopsies. Scott JG, Shaw EK, Friedman A, Ferrante JM American Journal of Cancer Prevention 2013; 1: 4-8. EAU EU-ACME Office European Urology Today 13 EBU Certification Programme Urology department in Prague receives EBU approval Prof. Marek Babjuk Charles University 2nd Medical Faculty Prague (CS) Marek.Babjuk@ fnmotol.cz Prof. Ladislav Jarolim Charles University 2nd Medical Faculty Prague (CS) ladislav.jarolim@ lfmotol.cuni.cz Founded in 1984, the urological department of the University Hospital Motol has enjoyed since 1996 the status of University Clinic at the 2nd Faculty of Medicine of Charles University in Prague. With more than 2,400 beds and over 80,000 admissions per year, Hospital Motol is considered the largest in Czech Republic and one of the biggest in central Europe. Associate Professor Ivan Kawaciuk led the department since its establishment until his retirement in 2009. Kawaciuk is succeeded by the author, with Prof. Ladislav Jarolim as deputy chairman. The medical staff is composed of 13 certified urologists, four residents and an internal medicine specialist. Five junior urologists have recently passed the European Board of Examinations and were accorded the FEBU title. The department has 36 adult patient beds including a six-bed intensive care unit, four day care beds and around 3,700 admissions per year. Urology procedures are performed in two operating rooms. With full-day surgical services, more than 1,600 patients are treated surgically every year. With our training goals, our centre focuses on patients for major urological procedures. For example, every year 50 cystectomies, 160 radical prostatectomies (open or laparoscopic), more than 120 kidney cancer procedures (mostly laparoscopic), and 10 retroperitoneal lymph node dissections in testis cancer, among other procedures, are performed. At the outpatient department we annually treat 9,000 general urology patients (UTI, LUTS etc.), 9,500 patients with urinary stone disease, 13,000 oncological patients, 2,500 patients with andrological problems and erectile dysfunction, and 2,000 patients with functional urology diseases. The outpatient clinic has facilities to perform intravesical instillation, systemic chemotherapy, cystoscopies, prostate biopsies or urodynamics. We also collaborate with other departments in the hospital such as radiology, clinical oncology, spinal unit etc. The department provides a full range urological practice except for kidney transplantations and ESWL. Paediatric urology is partially performed in cooperation with the hospital’s department of paediatric surgery. Our main focus is on onco-urology. During the last three years teams were designated for each onco-urological sub-specialty, each concentrating on implementing new procedures, evaluation of results and research activities. The bladder cancer team conducts research in non-invasive detection and prognostic factors, investigates new imaging methods (NBI, PDD) and the surgical treatment of locally advanced disease. The renal cancer team addresses new tissue and serum markers and the improvement of minimally-invasive treatment modalities. In 2010, the Centre for Research and Treatment of Prostate Cancer was founded with broad activities in radical surgery and basic and clinical research, including defining and using new prognostic markers and treatment modalities like immunotherapy. For potential projects, tissue banking was initiated. Other activities include reconstructive urology, surgical operations for incontinence, BPH treatment, EBU Certified Centres treatment of urolithiasis including endoscopic surgery and metabolic counselling, treatment of congenital defects (in cooperation with paediatric urologists) and andrology. Another unique activity includes services and surgical procedures dealing with transsexualism. Over 300 operated cases (mostly male to female) where performed in the last 12 years. The chairmen surrounded by the staff of the urological department The resident training programme was established based on the requirements of the Czech postgraduate education system. The teaching programme employs a systematic training in all urological subtopics, while at the same time providing an individualised approach in mentoring residents. In general, training is clinically oriented. Every resident has a personal written training programme, which specifies individual schedule and time periods spent on each subtopic. Currently, there are four residents in training. Urology Training in the Czech Republic • takes five years; this includes four months in Surgery, two months in Internal medicine, one month in Gynaecology, two months in Intensive care and at least one month in Paediatric urology • During the first year of the training period residents focus on General urology including ward rounds of operated patients and outpatient department. • After one year residents start to rotate in the following sub-specialties: Onco-urology, Reconstructive urology, Female/functional and Neuro-urology, Paediatric urology, Endoscopy and laparoscopy, and Andrology. • During particular sub-specialization courses, residents assist and perform surgery in the specific field, study and discuss relevant literature and clinical papers. Every subspecialization is guided by one or two staff members, specialized in the relevant topic. A personal tutor assigned to each resident-in-training is responsible for fulfilling all points in the teaching programme. Special attention is paid on the training of skills in urological interventions and surgery. Residents maintain an individual logbook with a given number of performed and assisted operations and invasive diagnostic procedures. Residents participate in regular teaching rounds under the guidance of staff members, regular clinical conferences, pathology, radiology, oncology and other multidisciplinary conferences. The level of knowledge and achieved skills are evaluated every six months by the personal tutor and yearly by the head of the department. An important tool is the EBU In-Service Assessment. Trainees participate in all available educational courses and seminars. Presentation skills are trained during monthly scientific meetings. Each resident is requested to prepare and present at least one lecture, every year, on a given topic. From the third residency year, residents start to present results of their research activities during the annual meeting of the national society and, if possible, in international meetings. From their second year, residents are included in research groups and are obliged to write at least two articles in a peer-reviewed journal during their training. Due to the success of the training system, the efficient facilities and the range of academic activities in clinical work, basic research and publications, the urology department applied for EBU certification. The EBU certification, granted for a period of five years in October 2012, has led to the critical appraisal of our training programme. Coimbra’s Residency Training gains EBU certification A commitment to high quality standards Dr. Paulo Dinis Dept of Urology and Renal Transplantation University Hospital of Coimbra Coimbra (PT) Portugal is also above the European average in terms of the number of transplants, with 45.7 renal transplants/million inhabitant per year. The University Hospital of Coimbra, an academic hospital located in Portugal’s central region, serves a population of over 500,000, and has been building a respectable reputation in healthcare, education and research. [email protected] Dr. Frederico Furriel Dept of Urology and Renal Transplantation University Hospital of Coimbra Coimbra (PT) [email protected] On July 20, 1969 when Neil Armstrong became the first man to set foot on the moon, history was also being written in Portugal. On the same day, in Coimbra, a team lead by Linhares Furtado performed the first renal transplant in the country despite the obstacles and the novelty of transplantation medicine. Forty years later, the Department of Urology, where this milestone happened, is now considered as one of Europe’s leading renal transplantation centres. EBU Certified Centres 14 European Urology Today The Department of Urology and Renal Transplantation employs 12 urologists and 10 residents in urology. Its two in-patient wards have a 53-bed capacity, one for patients afflicted with various urological diseases, while the other one is dedicated to renal transplantation. Besides renal transplantation, the department is also a centre of expertise in other urological specialties such as medical and surgical oncology and laparoscopy. Urological care in all other areas, such as endourology, andrology, neurourology and reconstructive urology, is also provided and maintained with high international standards. international meetings, • publish articles • annually take part in the EBU In-Service Assessment. The Portuguese residency training programme in Urology • takes six years; including one year in General Surgery, • two months in Paediatric Surgery and • four months in other specialties, such as Pathology, Radiology, Gynaecology, Vascular Surgery or Plastic Surgery, depending on the residents’ choice. • The programme includes a plan, defining the knowledge and surgical goals for each year of the residency. There are regular multidisciplinary meetings such as “Morbidity & Mortality” meetings and Campbell Every year, approximately 2,000 patients are admitted review sessions. Residents keep an updated logbook to the in-patient facilities, with an estimated 24,000 of their practice and, at the end of each year, all medical appointments made. The department has two residents write a detailed report on their surgical and well-equipped surgical theatres, enabling the surgical scientific activities which they also publicly discuss treatment of over 1,200 patients every year. Outwith the staff. patient surgery is also preformed once every week. Many of the facilities required for modern urology Moreover, during their final residency year residents practice are available such as urodynamics, flexible are encouraged to: cystoscopy ESWL, 3-Tesla MRI, CT, PET-CT scan. • attend the EUREP (European Urology Residents Education Programme) course and At the department, staff and residents are committed • take the written part of the FEBU exam. to maintain a friendly and cooperative atmosphere, enhancing intellectual stimulation in both medical The EBU has granted full certification of the Residency and surgical training. Residents are encouraged to: Training Programme for the first time in 2003. The • take active participation in national and programme was certified for a second term of five The staff of the Urology and Renal Transplant Department in Coimbra years in October 2012. This is a mark of excellence and a commitment to maintain high residency training standards. Furthermore, the application itself presents a valuable opportunity to gain external feedback, which is always helpful when continuous improvement is required. We are confident that other urology departments in Portugal will also apply for EBU certification in the near future, as we are strongly committed to maintain quality standards in Portuguese urological training and practice. Recently, a reform in the healthcare system led to the merger of our hospital with another tertiary care unit, creating the largest urology department in the country. With this recent development we expect further improvements in patient care, staff training, and research. March/May 2013 A chance to join the ... International Academic Exchange Programme Chinese Urological Association (CUA) in collaboration with the European Association of Urology (EAU) 2013 Chinese Tour The CUA/EAU International Exchange Programme will send Chinese faculty to Europe and European faculty to China. The programme aims to promote international exchange of urological medical skills, expertise and knowledge. To date one Chinese and two European tours have been organised and each of those proved extremely successful. Therefore the European Association of Urology (EAU) and the Chinese Urological Association are pleased to announce the 2013 Chinese Tour! For 2013 the CUA/EAU International Exchange Programme will provide grants to enable four EAU members (3 junior and 1 senior faculty member) to participate in the Chinese Tour. The tour should take place from October 1 – 20, 2013 starting with visits to different urological centres in China, culminating with participation at the CUA Annual Meeting to be held in Beijing (October 16 – 19, 2013). Eligibility criteria • Less than 42 years of age • Minimum academic rank of assistant professor • Letter from the departmental chairman of the applicant’s commitment to academic medicine • Membership of the EAU • Availability to travel from October 1 - 20, 2013 Information and application forms For all further information and programme application forms, please visit www.uroweb.org, and select International Relations, CUA-EAU or contact the EAU Central Office, T +31 (0)26 389 0680, F +31 (0)26 389 0674, E: [email protected]. EAU Central Office, Attn. Secretariat, P.O. Box 30016, 6803 AA Arnhem, The Netherlands ERUS 10th Anniversary Meeting Stockholm to host annual meeting in September Dr. Magnus Annerstedt Herlev Hospital Dept. of Urology Herlev (DK) magnus.annerstedt@ me.com recent EAU congress in Milan which were wellattended. Our Junior ERUS section also attracts young urologists interested in robotic urology. They have their own programme at the annual congress and a separate working group within the ERUS. We highly encourage our young colleagues to actively take part in different working groups to develop the necessary skills. The Stockholm meeting will present 10 live surgeries including standard procedures, prostate, kidney and bladder, as well as new indications in high-definition (HD) and 3D by renowned international experts in robotic surgery. These will be complemented by The EAU Robotic Urology Section (ERUS), formerly a non-affiliated society, will hold in Stockholm, Sweden state-of-the-art lectures, workshops and roundtable the 10th anniversary of its yearly congress. It all discussions on the latest developments. started back in 2004 in Paris with about 50 participants, and since then the ERUS Congress has The venue will be in central Stockholm at the Stockholm Waterfront Congress Centre, which is grown steadily with last year’s meeting in Paris attracting over 700 participants. For the second time located near the city’s major attractions. With its stunning architecture, meeting participants will not in its history, Stockholm will host the ERUS meeting on September 3 to 5, 2013. only benefit from this very exciting meeting but will also have the opportunity to explore Stockholm at the best time of the year in early September. With its ambitious plans, ERUS aims to be the scientific platform for every urologist interested in the ERUS exerts efforts to present high quality robotic latest development in urological robotic science and practice with the ultimate goal of improving the level surgery by international experts with interactive of patient care. Currently, the section has several moderation to prompt discussions and careful examination of these procedures. All live surgery will projects in the pipeline. comply with the EAU’s new ethical guidelines. Within the working group of science there are several New devices from the industry will also be on display plans such as designing new studies and securing data collection. A lot of effort is done to achieve and in the exhibit section. On the opening day, a junior maintain a high level of surgical science within ERUS meeting will be held to educate and inspire the robotic urology, while incorporating traditional open next generation of minimally invasive surgeons, followed by courses on individual robotic procedures surgery as a core expertise or comparison for skills as well as a separate overview of current robotic acquisition. urologic surgery. A day-long course for nurses will Thus, we are proud to present a robotic master course also be part of the programme to provide tips on and curriculum to establish and standardise robotic surgical support and peri-operative patient care. We look forward to see you in Stockholm! education and training in an efficient and safe way. E-learning, master classes and fellowships are all part of this programme. For instance, we have Check our website for more details at www.erus2013.com. organised hands-on training courses during the March/May 2013 www.erus2013.com EAU Robotic Urology Section Congress (ERUS’13) 3-5 September 2013, Stockholm, Sweden EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations European Association of Urology European Urology Today 15 Neobladder and continent cutaneous diversion after RC An update on continent urinary diversion Prof. Richard E. Hautmann University of Ulm Ulm (DE) richard.hautmann@ uni-ulm.de Prof. Joachim W. Thüroff Dept. of Urology Johannes GutenbergUniversity Mainz Mainz (DE) joachim.thueroff@ unimedizin-mainz.de leakage may occur. A rapid increase in reservoir capacity following surgery allows daytime continence to be achieved. Night-time continence is established less quickly. During sleep, a detrusor-sphincter reflex normally increases outlet pressure as the bladder wall stretches during filling; this reflex is lost after cystectomy. As the reservoir fills at night, additional outlet contraction is not recruited, and when the rise in reservoir pressure exceeds outlet pressure, incontinence occurs. Men achieve self-assessed continence by day and by night in 92% and 76% of cases, respectively. Attempted nerve sparing improves daytime continence, which worsens with increasing age.3 Urinary tract infection also worsens continence, and an unexpected deterioration of continence should prompt exclusion of infection and residual urine or mucus collection.4 A clinical urinary tract infection is uncommon. Upper urinary tract safety: Voiding with a neobladder cannot produce reflux, which has been confirmed scintigraphically. Long-term upper tract outcomes are excellent. As few as 2.7% of patients develop ureteroileal strictures if a direct end-to-side anastomosis is used. The use of stents in the ureteroileal anastomosis improves outcomes.5 Up to half of patients who develop a short ureteroileal stricture can be successfully managed endourologically. The use of an antireflux nipple valve was associated with a worse outcome than a dynamic isoperistaltic afferent tubular segment.3 Urinary retention is more common in women undergoing a neobladder. Such retention may occur early but often appears after a year or more of good neobladder function and emptying. In the Ulm series of 116 women, the rate of retention increased steadily over time to approximately 50% by five years.3 The etiology has been debated, but most authors believe it is due to a kink in the urethra-pouch anastomosis as the full pouch falls posteriorly during the Valsalva maneuver.3 This can be documented on a lateral straining cystogram. Other suggested etiologies include autonomic denervation of the urethra or random reinnervation resulting in an inability to relax the sphincter.3 Since the first description of this potentially undesirable late complication, authors have suggested modifications in surgical technique to try to prevent this problem and have presented data to suggest improved outcomes. However, all are consecutive series, and because the complication may appear late, such reports may be biased by shorter follow-up in the “new” group. unsuitable, a nipple valve is established and fixed to the ileocecal valve and the reservoir wall with staples. The serous-lined extramural Valve/T-Pouch: The principle of the Valve/T-Pouch is the creation of a serous-lined trough in which a tapered ileal segment is placed. Two articles described the use of this technique in Europe. As correctly stated by the authors of this report, “construction of the pouch is sophisticated.” This is the main drawback of the technique and represents a serious obstacle to general acceptance.3 Stone formation is a common phenomenon after continent cutaneous reconstruction. Its etiology is multifactorial including residual urine, chronic bacteriuria, mucus, and staples.3 Although an incidence as high as 44% has been reported, most reports indicate rates of 5-20%.3 The risk of a perforation/rupture complication is higher after continent cutaneous diversion than after a neobladder because the former lacks a pop-off mechanism.8 Other important aspects: Bacterial colonisation after Nevertheless, some attempts to fill the posterior continent cutaneous diversion is more prevalent than pelvis and re-establish anterior and superior fixation after orthotopic reconstruction, but clinically of the bladder seems to be warranted. Treatment of symptomatic infections are rare. retention is intermittent catheterisation. a-Blockers are not effective. Transurethral resection of a urethral fold and open reduction of the pouch size with Summary anterior fixation to the abdominal wall have also • Surgical morbidity following continent been described. Every woman undergoing urinary diversion is significant and, when In these patients, the construction of a neobladder allows the elimination of a stoma and preservation of neobladder reconstruction should be advised that strict reporting guidelines are incorporated, it intermittent catheterisation may be required for is higher than previously published. Accurate body image without compromising cancer control. When involvement of the lower urinary tract by Postoperative management: Of paramount importance adequate emptying, and she must be willing and able reporting of postoperative complications after tumour prohibits the use of a neobladder, a continent is the active postoperative management and regular to learn how to perform it. Many women who are dry radical cystectomy is essential for counselling cutaneous reservoir may still offer some advantages but require self-catheterisation seem quite satisfied patients, combined modality treatment long-term follow-up of patients with a neobladder. with the diversion. over an ileal conduit. For patients who are not The key issues are achieving a capacity of 400-500 planning, clinical trial design, and assessment of surgical success. candidates for either type of continent diversion, the ml, residual-free voiding of sterile urine, and the Sexual function and quality of life: Only a few studies ileal loop remains a time honored option. treatment of any outlet obstruction.3 have examined the postoperative sexual function of • It is inappropriate to ask for direct women undergoing radical cystectomy and urinary comparisons of neobladder versus conduit. Radical cystectomy remains the best treatment option “Men achieve self-assessed for patients with invasive bladder cancer. Nevertheless, diversion. Results suggest that sexual dysfunction is These are different patient populations, and it continence by day and by night is incorrect to assume that patients are two major problems remain. First: Population-based common and may be potentially improved by studies indicate poor utilisation of radical cystectomy preserving the uterus when possible and preserving equally suitable for a neobladder and in 92% and 76% of cases, the autonomic nerves lateral to the vagina.3 counduit. A prospective randomised trial of a of less than 40% of patients needing it.1 Second, just respectively.” 15-20% of radical cystectomy patients received some neobladder versus conduit is unlikely. form of continent urinary diversion.2 Continent cutaneous urinary diversion Minimally invasive surgery: There is increasing interest Numerous techniques of continent cutaneous urinary • Urinary diversion into bowel segments is not inherently damaging to the kidneys. However, Radical cystectomy and urinary diversion are the most in laparoscopic and robotic cystectomy, with either diversion have been described but some of these difficult open, laparoscopic, or robotic procedures in intracorporeal or extracorporeal formation of conduit appeared only once in the literature, indicating they any form of obstruction, if left untreated, is were associated with technical problems, high detrimental. Infection is also a contributing urology, more so if the urinary diversion is performed or neobladder.3 Whether reports with intermediate factor. In general, renal function after totally intracorporeally. We update the follow-up suggesting equivalent oncologic outcome complication rates, and suboptimal functional results. diversion into continent detubularised Today, only a handful of methods are in use, and in recommendations of the ICUD-EAU International will be confirmed remains to be determined. But reservoirs is superior to ileal conduit Consultation on Bladder Cancer/Continent Urinary there are advantages in terms of blood loss, general, they are the second choice after neobladder diversion. However, the literature is Diversion 2012.3 transfusion rates, postoperative pain, and return of for patients undergoing radical cystectomy. insufficient to recommend one form of bowel function. In most reported series, cases were diversion over another. The main indication for continent cutaneous diversion Male neobladder highly selected. is when urethral removal is deemed necessary due to Age and motivation: There is no age cut-off. Some • There remains a long-term risk of renal patients >70 years request the simpler conduit Female neobladder a high risk of recurrence of urothelial carcinoma. This Age alone is not a criterion for offering a neobladder.3 risk can be estimated based on the pathology report deterioration, which is often asymptomatic, because the postoperative course is less arduous and from the preoperative transurethral resection biopsies and thus close follow-up is necessary for all incontinence is not an issue. Patient motivation is the The impact of age on outcomes with a neobladder patients who have undergone urinary most important factor when considering the suitability has not been fully determined in women. Women >75 of the prostate. Such biopsies should be taken from the bladder neck to the verumontanum on both sides for a neobladder. The extent of pelvic disease has little years of age are at higher risk of incontinence, but diversion to identify correctable causes early. bearing on the appropriateness of a neobladder. If some of them will have excellent neobladder function. before cystectomy. Relying on frozen sections of the Those with renal pathology prior to surgery urethra obtained during surgery may be dangerous seem to be at greatest risk of postoperative pelvic recurrence develops, it does usually not have a because of the risk of a false-negative report from the significant impact on the function of a neobladder. Patient selection: Prior to the wide adoption of a renal deterioration. Early intervention for Although prostatic involvement by urothelial cancer is neobladder for women, it was necessary to show it was pathologist. physical obstruction often results in a frequent a neobladder can still be performed if the safe to preserve the urethra during the cystectomy.3 sustained improvement in renal function. distal prostatic urethra is cancer-free.3 Only bladder neck involvement and anterior vaginal Patients who have undergone continent “It is standard to require a negative wall invasion predicted urethral involvement, although cutaneous diversion or a neobladder do not frozen section of the urethral Surgical technique: Nerve-sparing cystectomy does not 50% of those with a bladder neck tumour had no seem to be at increased risk of secondary just increase the chance of maintaining erectile tumour in the urethra.3 It is standard to require a malignancy. margin prior to proceeding with a function. In men with a neobladder who had an negative frozen section of the urethral margin prior to neobladder in women.3” attempted nerve-sparing operation, night-time • Any form of urinary diversion has its specific proceeding with a neobladder in women.3 Pre existing continence was better than in those who did not. A incontinence is a relative contraindication for women problems. In experienced hands and with neobladder must be a low-pressure reservoir of considering a neobladder. A woman with stress urinary Knowledge about the status of the urethra/prostate regular long-term follow-up, serious adequate capacity (allowing a socially acceptable incontinence may be willing to continue to wear pads enables the surgeon to inform the patient complications can be avoided and excellent voiding interval without urinary leakage) and must rather than deal with a stoma, or she may be preoperatively definitively about the type of the long-term results can be achieved. In this empty to completion. If this is so, the upper tract will considered for a sling or Burch procedure at the time of diversion to be recommended. Urothelial cell context, surgeons must continue to refine be preserved and metabolic disturbance will be carcinoma located in the urethra or involving the diversion with planned self-catheterisation. their surgical technique of radical cystectomy minimal. Ileum should be used whenever possible. prostatic ducts or stroma is the main indication for and urinary diversion to provide the utmost Detubularisation and a spherical shape ensure that a Anatomic basis of the preservation of continence in urethrectomy. Some patients may prefer a continent safety for the patient.3 neobladder has low pressure and maximum volume women: The neobladder was introduced as an option diversion to a neobladder because of the risk of urine for the length of bowel used. for women in the 1990s. Prior to that, it was generally leakage after a neobladder. • Evidence suggests an association between believed that the primary continence mechanism in surgical volume and outcome in radical Continence is achieved when outlet pressure exceeds women was located in the bladder neck.3 However, it Antirefluxing ureteric anastomosis is required in cystectomy; the challenge of optimum care reservoir pressure. This requires preservation of the was ultimately recognised that the urethra alone continent cutaneous diversion because the efficient for elderly patients with comorbidities is best sphincter and construction of a low-pressure reservoir could provide continence if the sphincter mechanism outlet mechanism can allow high intra-reservoir mastered at high-volume hospitals by by doubly folding detubularised ileum to achieve the was preserved. pressures. Different types of inlet, pouch, and outlet high-volume surgeons. Preoperative patient final reservoir volume of 450-500 ml. The reservoir have been combined. The stoma is usually placed in information, patient selection, surgical has initially a volume of around 150 ml. Stretching the Complications: Most of the early and late complications the umbilicus, where it remains invisible. techniques, and careful postoperative reservoir is achieved by delaying voiding when the of women undergoing radical cystectomy and follow-up are the cornerstones to achieve patient feels the urge to void is irresistible, and that neobladder are identical to those of men and are The ileal nipple valve was used in the first Mainz good long-term results.3 managed in a similar fashion.3 Two complications are pouch,6 later the submucosally tunnelled different in women: pouch-vaginal fistula and urinary catheterisable appendix was introduced. Today, the Expert views retention. appendix is the first choice, but if it is missing or Continued on page 17 Indications and patient selection criteria have significantly changed over the past two decades. At high-volume hospitals, orthotopic reconstruction has become the procedure of choice for urinary diversion in both men and women undergoing radical cystectomy. 16 European Urology Today March/May 2013 Apply for your EAU membership online! Would you like to receive all the benefits of EAU membership, but have no time for tedious paperwork? www.uroweb.org Continued from page 16 Becoming a member is now fast and easy! Figure 1: Neobladder in a female patient A Suspensory ligaments, H Urethra, M Neobladder mesentery, R Rectum, S Symphysis pubis, V Vagina. References 1. Goossens-Laan CA, Visser O, Hulshof MC, et al. Survival after treatment for carcinoma invading bladder muscle: a Dutch population-based study on the impact of hospital volume. BJU Int. 2012;110:226-32. 2. Gore JL, Litwin MS. Urologic Diseases in America Project. Quality of care in bladder cancer: trends in urinary diversion following radical cystectomy. World J Urol 2009;27:45-50. 3. Hautmann RE, Abol-Enein H, Davidsson T, Gudjonsson S, Hautmann SH, Holm HV, Lee ChT, Liedberg F, Madersbacher S, Manoharan M, Mansson W, Mills RD, Penson DF, Skinner EC, Stein R, Studer UE, Thueroff JW, Turner WH, Volkmer BG, Xu A. ICUD-EAU International Consultation on Bladder Cancer 2012: Urinary Diversion. Eur Urol 2013;63:67-80. 4. Zehnder P, Dhar N, Thurairaja R, Ochsner K, Studer UE. Effect of urinary tract infeczion on reservoir function in patients with ileal bladder substitute. J Urol 2009;181:25459. 5. Studer UE, Burkhard FC, Schumacher M, et al. Twenty years experience with an ileal orthotopic low pressure bladder substitute-lessons to be learned. J Urol 2006;176:582-6. 6. Thueroff JW, Alken P, Riedmiller H, Engelmann U, Jacobi GH, Hohenfelner R. The Mainz pouch (mixed augmentation ileum and cecum) for bladder augmentation and continent diversion. J Urol 1986;136:17-26. 7. Thueroff JW, Alken P, riedmiller H, Jacobi GH, Hohenfellner R. 100 cases of Mainz pouch: continuing experience and evolution. J Urol 1988;140:283-8. 8. Mansson W, Bakke A, Bergman B, et al. Perforation of continent urinary reservoirs. Scandinavian experience. Scand J Urol Nephrol 1997;31:529-32. Go to www.uroweb.org and click EAU membership to apply online. It will only take you a couple of minutes to submit your application, the rest - is for you to enjoy! USANZ Trainee Week Young urologists benefit from comprehensive, quality training Dr. Martina Wolfgang General Hospital St. Pölten Dept of Urology St. Pölten (AT) martina.wolfgang@ stpoelten.lknoe.at Board of Surgical Education and Training and the Council of the RACS. USANZ collaborates with the RACS as an agent of the College, administers the training programme in Australia and manages the Board in Urology, otherwise known as the Training, Accreditation and Education Committee (TA&E Committee). Education and training The SET Programme in urology is designed to improve the quality and efficiency of surgical education and From November 18 to 22 last year the annual Trainee training. It starts with two years (SET 1+2) of general The openness and friendliness of the Australian and New Week of the Urological Society of Australia & New Zealand trainees made the international participants feel surgical skills, followed by three years (SET 3-5) of Zealand (USANZ) took place in Melbourne and welcome advanced clinical urology training and ends with the Geelong in Victoria, Australia. This programme is a Senior level, respectively a minimum time of six component of the SET (Surgical Education and years. Training) Programme and is compulsory for all background including important studies is important Australian and New Zealand SET (2-5) trainees. The Trainee Week, which is held in a different in preparing for the exam, thus most of them are well Australian state each year or in New Zealand, started prepared. Approximately 90 trainees from across Australia and with practice examinations (Practice Vivas and Written New Zealand and – as part of a reciprocal Examination). All SET4 trainees undertook the oral During the next four days an intensive programme is arrangement with international associations – six exams and were examined by a SET5 trainee together scheduled with a series of excellently presented trainees from the European Association of Urology with a urological consultant. I was fortunate to lectures, case discussions in small groups, trainee (EAU), the Urological Association of Asia (UAA), the observe these exams with the SET3 trainees and the presentations and a very informative lesson about British Association of Urological Surgeons (BAUS) and other international registrars. exam performance from an examiner’s as well as a the Canadian Urological Association (CUA) attended psychologist’s point of view. the meeting. There are four oral exams; Anatomy and Operative Surgery, Pathology, Structure Oral and Clinical I was surprised of the active role the SET4 and After successfully completing the FEBU Written exam Investigation and Management. These exams are especially SET5 trainees had in the programme. September 2012, I was selected and invited by the designed to help the trainees prepare for the final During the lecture series, the trainees also presented EAU to register for this programme and I felt very Fellowship Examination. Trainees learn the style of alternating with urologists, and also led the small honoured and curious of this unexpected possibility to exam questions and how to think and answer in a group case discussions and, as previously mentioned, learn more about the Australian Trainee Programme structured way. I got the impression that all of the acted as examiners in the oral exam. For me, it and also the Australian people and culture. trainees had a solid basic knowledge of urology, seemed that most of the trainees know each other, including anatomy and pathology. Furthermore, perhaps because of the Trainee Weeks they have Organisational background trainees know that knowledge of the scientific attended before, or due to the fact that all trainees USANZ, the official and professional body for have to rotate for their working place/ hospital (and urological surgeons in Australia and New Zealand, is in the majority of cases also the town), annually. committed to clinical excellence, education, promotion of research and the dissemination of The Australian and New Zealand SET trainees enjoy a information on urological topics. On the other hand, good reputation in international urology and this the Royal Australasian College of Surgeons (RACS) is could be attributed to their training as previously the principal body for the training and education of described. Changing residence every year impacts surgeons in both countries. Accreditation is given by one’s private life and for me, as a European, this is the Australian Medical Council and the Medical hard to imagine. But otherwise this system offers the Council of New Zealand to the RACS which sets the possibility to a consistent quality in education and standards for education and training. training and a fair competition to all trainees. Furthermore, the trainees learn to accept new The Board in Urology of the RACS has oversight for responsibilities and perform with confidence. An intensive programme is scheduled which includes a series the conduct of the training programme in urology across Australia and New Zealand, and reports to the of excellently presented lectures Compared with Austria, in Australia there seem to be March/May 2013 no influence of a ‘’settled (or conservative) urology’, which could explain why there’s a greater focus on surgical (operative) education during the resident years. It’s also advantageous that, with the beginning of the fifth year, the SET trainees are allowed and encouraged to take their ‘’Final Clinical Examination.’’ This enables them to concentrate on the operative or surgical part during the last two years of training. Social programme The social programme included the Welcome BBC, a dinner with the major sponsors and the Final Dinner. The international participants were warmly welcomed and introduced on the first day by Richard Grills, Deputy Chair & Board of Urology Member and the extraordinary Mrs. Deborah Klein, who is responsible for organising the Trainee Week. Whenever there were queries or a problem before or during the meeting, Deborah was always there to provide help. The openness and friendliness of the Australian trainees also helped the international participants to feel welcome and I guess everybody made new friendships and returned home with new ideas. It is also an amazing thing for me to realise that one can travel to ‘’the other end of the world’’ and come to meet people who also previously worked with ones colleagues. All these contacts can perhaps lead to professional cooperation or the chance to work abroad. It was my first time to visit Australia and I regretted that I didn’t have enough time to arrange for a longer stay. It would have been interesting to also visit an Australian department of urology or see more of this fascinating country. But it won’t surely be the last time that I will visit Australia. The skyline of Melbourne European Urology Today 17 Live surgical events: Skills or thrills? EAU policy on live surgery presented in Milan Mr. Keith Parsons Chairman EAU Guidelines Office Liverpool (GB) parsons_keith@ hotmail.com One of the most successful features of any EAU Congress is the live surgical sessions, so it is timely to discuss the EAU position on live surgery. As in all surgery, things may occasionally go wrong. In relation to live surgery, however, it is hard to find out whether they ever do or whether the live surgery event itself was contributory. Certainly an extensive literature trawl failed to find any authoritative articles revealing such information. Nevertheless, there is sufficient anxiety about live surgical events for a number of international organisations only to allow them to take place under strict regulatory control and for several to ban them altogether. Why might an organisation be keen, therefore, to continue to organise live surgical events? Intuitively it is felt to enhance surgical training, to accelerate the dissemination of advances in surgery, to promote the adoption of innovation, and to improve the quality of care, not least by the audience being able to observe the very best surgeons performing particular procedures. There is, however, no firm evidence to support or refute these suppositions. The EAU distinguishes between two types of live surgery: • ‘Live surgery’ is any surgical procedure conducted in real time, and observed for educational purposes. That may of course be in any surgical department, and part of general training. • A ‘live surgical event’ is any surgical procedure organised for a dedicated audience and conducted in real time and observed for educational purposes. These days the latter might involve a number of extra people in the operating room, including camera men and technicians, all present to make sure that images can be projected in real time to an auditorium and for there to be interaction between the audience and the operating team. the attraction may be the thrill that something might go wrong. It is rather more likely that the audience wants to see, not only how an expert surgeon avoids problems, but if they are encountered, how they are dealt with. Faced with a keenness to preserve live surgery events, and in the light of the anxiety about them, the EAU Executive Board established an ‘Ethics of Live Surgery Panel’ charged with the responsibility of investigating the whole issue and producing a policy on live surgery for the association. The Panel (Table 1) comprised members from all the EAU Sections who use live surgery and other experts with extensive knowledge about it. The first step was an extensive literature search, with no time limit, of all the main data bases. The result was 306 articles which, using a Prisma Flow chart, was culled to 81 papers which were circulated to the panel members. From review of the information, 102 questions on all aspects of live surgery were put to the panel members in an internet survey. They included questions on the pros and cons of live surgery versus video recordings (34); patient safety (27); ethical aspects (13); regulatory considerations (12), and the remaining 11 questions dealt with general aspects of live surgery and the role of clinicians and organisations. From the polled answers, the definitions above were determined. On 15% of other issues there was 100% agreement. The outstanding issues and principles were then explored further during an internet e-consensus conference using the Delphi process. The Delphi process is a method for structuring group communication so that the process is effective in allowing a group of individuals, as a whole, to deal with a complex problem. How it works is that a question is posed and anonymous votes are cast. At the end of the round, each panel member can see the cumulative results of all the panel member’s votes and reflect upon them. This is then followed by re-iterative rounds, where an individual’s vote in the next round is informed by knowledge of the group’s results of previous rounds. In this way, a consensus, if it is to be found, can be drawn together. In the e-consensus conference, which had 3 rounds, a consensus level of 80% was used. Thirty-three questions were put and a consensus was achieved in 70% of the issues. Table 1: EAU Ethics of Live Surgery Panel Screenshot Consensus-finding software 2.The over-riding principle is that patient safety must take priority over all other considerations in the conduct of live surgery 3.All EAU endorsed live surgical events must be organised by a specifically identified local organising committee with a designated director 4.This committee will report to, and act under the auspices of the EAU Live Surgery Committee who will authorise the event, ensure compliance with requirements, and establish and maintain a database of all EAU live surgical events A draft policy statement and a series of supporting documents were then written, which embodied all the issues where greater than 80% agreement was found on the internet survey and where there was a formulated consensus from the e-consensus conference. These draft documents were then discussed and finalised at a one-day Panel Symposium which ratified the policy and the supporting documents. The supporting documents include a definition of the local live surgery event committee and its requirement to appoint a director who will liaise with the EAU Live Surgery Committee (EAU-LSC) (Table 2). Application for an event must be made to this committee using a live surgery procedure checklist, available online. Within that application is the requirement that a defined Code of Conduct must be adhered to and a structured process in organising the event must be followed. Table 2: EAU Live Surgery Committee (EAU-LSC) W. Artibani EAU Executive Committee, Chairman K. Parsons Guidelines Office A. Stenzl Scientific Congress Office J. van Moorselaar ESU L. Martinez-Piñeiro Section Office Th. Pieuchaud ERUS T. Knoll EULIS J. Heesakkers ESFFU J. Rassweiler ESUT L. Denis Patient representative A consent form addendum, specific for live surgery, must be signed by the patient. Translations of it are available. Mr. Parsons presents the new EAU policy on live surgery at the 28th Annual EAU Congress in Milan Finally, there must be a commitment in advance that all outcomes and any complications must be reported to the EAU-LSC, using the standard EAU approved reporting complications pro-forma as agreed by the appropriate guideline. The benefits of this new policy are numerous. The patient’s safety will be paramount, and they will have clear information about the event, and meet the surgeon involved the day before. There will be an advocate to safeguard their interest. The organising centre will have a clear framework within which to plan and execute the event. The surgeon(s) responsibilities will be explicit, and there will be no surprises on the day of surgery, having been able to review patient data well in advance. The surgeons will have the chance to ensure that all their preferences are met and any requirements are available in the operating room. The audience will have informed moderators, and be able to participate in a structured dialogue via a moderator in the operating room with the surgical team. The EAU has the opportunity to acquire prospectively audited information about all aspects of live surgery, and will be able to determine its safety with authority. Finally, there will be a cumulative database compiled affording further research opportunities, particularly in the area of the educational value, and benefits of live surgery. In this way, the gap in the evidence base about live surgery, and whether it does achieve it aims, will be filled. EAU Executive Committee ESUT External consultant ESOU ERUS ESGURS Expert Expert ESUT ESFFU SPO EULIS EAU Section Office Editor-in-Chief Eur Urol ESU ERUS ESU EAU Guidelines Office ERUS ESUT ESUT ESUT EAU Scientific Office ESU ERUS = EAU Robotic Urology section, ESFFU = EAU Section of Female and Functional Urology, ESGURS = EAU Section of Reconstructive Urology Surgeons, ESOU = EAU Section of Oncological Urology, EULIS = EAU Section of Urolithiasis, ESU = European School of Urology, ESUT = EAU Section of Uro-Technology, SPO = EAU Strategy Planning Office 18 1. The EAU endorses the use of live surgery as a technique for the dissemination of surgical knowledge, and does so provided that it is organised within a clearly defined regulatory framework A new feature of the policy is the appointment of a patient’s advocate who will be a local senior urological surgeon, not involved in the organising of the event, but who will be in the operating room with the sole responsibility of looking after the patient’s best interest and who has the authority to terminate the live surgery if deemed necessary. Live surgical events at EAU Congresses are always extremely popular and it is sometimes claimed that W. Artibani C. Abbou R. Boscolo M. Brausi B. Challacombe S. Deger V. Ficarra G. Guazzoni B. Guillonneau J. Heesakkers D. Jacqmin T. Knoll L. Martinez-Piñeiro F. Montorsi J. Van Moorselaar A. Mottrie J. Palou Redorta K. Parsons Th. Piechaud A. Rane J. Rassweiler J. De La Rosette A. Stenzl R. Van Velthoven The EAU policy on Live Surgery: European Urology Today Ethics of Live Surgery Panel gathered for the Panel Symposium in Munich March/May 2013 European Urology Forum 2013 http://esudavos.uroweb.org Davos meeting features challenging insights The 22nd Annual EAU Winter Forum, chaired by Professors Chris Chapple and Joan Palou and held from February 2 to 5, 2013 in Davos, Switzerland proved to be an outstanding success with 200 attendees. The busy academic programme was supported by a distinguished faculty of experts composed of: P. Abrams, Bristol (GB), C. Abbou, (FR), W. Artibani, Verona (IT), W. Aulitzky, Vienna (AT), D. Castro Diaz, Sante Cruz de Tenerife (ES), C.R. Chapple, Sheffield (UK). F.M.J. Debruyne, Arnhem (NL), C. Evans, Sacramento (USA), P. Mulders, Nijmegen (NL), J.M. Nijman, Groningen (NL), J. Palou, Barcelona (ES), A. Patel, London (GB), J. Rassweiler, Heilbronn (DE), C. Stief, Munich (DE), H.G. Van Der Poel, Amsterdam (NL), and M. Wirth, Dresden (DE). The meeting opened with the popular session on ‘What is New in Urology…’ which covered topics such as andrology and erectile dysfunction, targeted therapy for uro-oncology, endourology, laparoscopy, Botulinum toxin in urology, imaging prostate cancer, bladder cancer, paediatric urology and robotics. Key note lectures reviewed the contemporary management of non-invasive bladder cancer, the role of ablation therapy for organ-confined prostate cancer, upper tract ureteroscopy: where do we stand in 2013?, the impact of beta three agonists for overactive bladder, quality assurance in urology, advances in medical uro-oncology, contemporary practice for bladder cancer, managing infertility and the management of early stage prostate cancer, among others. Hands- on-training in ureterenoscopy and transurethral resection were supervised by a faculty comprised of A. Breda, Barcelona (ES), J-T, Klein Heilbronn (DE), C.M. Scoffone, Turin (IT), O. Traxer Paris (FR). Hands-on training on URS and TUR are supported by an unrestricted educational grant from Karl Storz GmbH & Co.KG European Urology Forum 2014 Other sessions included Interactive case study sessions on paediatric and functional urology and tips and tricks for urethroplasty, upper tract endoscopy and radical cystectomy. Another important and much valued aspect of the meeting, and which has now become an essential part of the programme, is the “Challenge the Experts Forum” where a superb faculty of young experts pitted their knowledge and wits against the faculty. The young challengers presented three lectures each on topics of their choice and are challenged on these presentations by the faculty and the audience. Superb presentations were given by the young academic faculty, namely M. Binbay (TR), C. Gingu (RO), L. Peri Cusi (ES), M. Roupret (FR) and A. Salonia (IT). Challenge the experts 1-4 February 2014, Davos, Switzerland EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations Frans Debruyne, founding organiser of the Winter Forum, chaired and moderated the competition and brought to the sessions his unmistakeable incisive style and with an intellect that guarantees the success of this competition. In this hard fought contest with very high standards, M. Roupret (Paris, FR) triumphed and won the first prize. Between the morning and evening academic sessions, participants also had access to the extensive EAU Video Library of surgical procedures. Participants highly appreciated the scientific programme and despite the intensive scientific sessions, the location and meeting venue provided ample opportunities for relaxation and sports. The substantial and stable number of regular attendees demonstrates the success of this annual meeting, with familiar faces attending year after year for their regular updates and continuing medical education (CME). We welcome and hope to see you next year from February 1 to 4, 2014! European Association of Urology Prof. Chris Chapple - Course director Prof. Joan Palou - Course director European School of Urology Activities 2013-2014 Organised courses at National Urological Society meetings December May 4 17 31 ESU organised course on Place and role of lymphadenectomy in urologic cancers at the time of the national congress of the Romanian Association of Urology ESU organised course on Pushing back the boundaries in CRPC and UTI at the time of the national congress of the Estonian Urological Association Bucharest (RO) Tartu (EE) June 13 22 September 6 ESU organised course on Update in non-muscle invasive bladder cancer T1G3 and nephron sparing surgery at the time of the national congress of the Polish Urological Association Jachranka (PL) ESU organised course on Prostate cancer at the time of the national congress of the Hungarian Association Urology ESU organised course on Female urology; fundamentals of stress incontinence and prolapse at the time of the national congress of the Czech Urological Society ESU organised course on at the time of the national congress of the Jordanian Association of Urological Surgeons ESU organised course on Localised prostate cancer at the time of the national congress of the Turkish Urological Association ESU organised course on Update in urooncology at the time of the national congress of the Scientific Society of Urologists of Uzbekistan ESU organised course on Update and evolving investigation in urology at the time of the national congress of the Russian Society of Urology ESU organised course on Lasers and endoscopes in urology: What an urologist should know at the time of the national congress of the French Association of Urology Eger (HU) Salzburg (AT) 15-17 6th ESU Masterclass on Female and functional reconstructive urology, in collaboration with the EAU Section of Female and Functional Urology (ESFFU) Berlin (DE) November ESU Medical oncology course on Genitourinary Cancer (MOGUC) Marseille (FR) Residents course September Carlsbad (CZ) Amman (JO) 13-18 11th European Urology Residents Education Programme (EUREP) Prague (CZ) Combined EAU/ESU meetings July Antalya (TR) Tashkent (UZ) 12-13 Chinese Urology Education Programme (CUEP) Beijing (CN) CUA-EAU programme on LUTS and Oncology Beijing (CN) October 15-16 Moscow (RU) February 2014 1-4 European Urology Forum 2014 – Challenge the experts Davos (CH) Paris (FR) ESU Office T +31 (0)26 389 0680 F +31 (0)26 389 0684 [email protected] www.uroweb.org March/May 2013 ESU – Weill Cornell Masterclass in General urology November 14 November 1 4 7 22 July Teaching course October 26 31 31 Masterclasses 7-13 ESU organised course on Interventional therapy for BPO - Surgical treatment for BPO at the time of the national congress of the Slovak Urological Association Trnava (SK) ESU organised course on at the time of the national congress of the Belarusian Association of Urology Minsk (BY) ESU organised course on Paediatric urology for the adult urologist: A practical update at the time of the national congress of the Egyptian Association of Urology Sharm el-Sheikh (EG) ESU courses are accredited within the programme by the EBU with 1 credit per hour European Urology Today 19 Optimising management of non-muscle invasive TCC ESUT-ESOU Expert Meeting in Davos Prof. Thorsten Bach Asklepios Hospital Harburg Dept. of Urology Hamburg (DE) t.bach@ asklepios.com Professors Jens Rassweiler (Heilbronn, DE) and Mauricio Brausi (Modena, IT) organised the second meeting of the EAU Section of Urotechnology (ESUT) and the EAU Section of Oncological Urology (ESOU) in Davos on February 2 this year in Davos, Switzerland. Around 40 participants including urologists, researchers and industry representatives participated in this all-day meeting on strategies to optimise the diagnosis and treatment of non-muscle invasive urothelial cancer. The meeting focused on all possible aspects of dealing with transitional cell carcinoma (TCC), including up-to-date diagnosis and future options to improve cancer detection as well as surgical treatment options, comparing standard treatments with new approaches and discussing future developments. Furthermore, postoperative treatment concepts, in particular the role of instillation therapy was discussed and critically reviewed by the expert participants. Diagnostics and imaging Concerning diagnostics and imaging, photodynamic diagnosis (PDD) using Hexvix™ has become standard of care, leading not only to increased detection rate and decreased rates of residual tumour, but also to a decreased recurrence rate as Prof. Stenzl (Tübingen, DE) pointed out. Despite this promising improvement, other diagnostic options are pushing the frontiers. While PDD is only available in the bladder, digital imaging techniques like NBI (Narrow Band Imaging, Olympus) or SPIES (Storz Professional Image Enhancement System, K. Storz) [Fig. 1] offers improved cancer detection not only in the bladder, but also in the upper urinary tract. An exciting diagnostic option was presented by Prof. De la Rosette (Amsterdam, NL). He showed the initial results from OCT (Optical Coherence Tomography) [Fig. 2], which enables the assessment of tumour extension and infiltration depth, especially of upper urinary tract tumours with high sensitivity and specificity. Treatment Transurethral resection of the bladder remains the reference standard for the surgical treatment and staging of bladder cancer. In the light of well-known limitations, like tumour slicing throughout the resection and incomplete primary resection, it is necessary to stress the importance of correctly performing bladder tumour resection, including the necessity to obtain a specimen of the muscular layer to allow correct staging. Bipolar resection of bladder tumour - but also vaporisation of the tumour with resection only of the tumour base - is gaining higher acceptance and was advocated as standard approach by Professors Janetschek (Innsbruck, AT) and Rischmann (Toulouse, FR). Fig. 1: SPIES for enhanced tumour detection (Courtesy K. Storz, Germany). BCG maintenance therapy plays an important role in intermediate- and high-risk non-muscle invasive TCC. In intermediate-risk tumours one year of maintenance therapy seems to be sufficient, while high-risk tumour patients should be kept on maintenance for three years, to achieve the best possible outcome, as shown by Prof. Chlosta (PL). In terms of effectiveness, data supports a superiority of Fig. 2: OCT in Upper Urinary Tract TCC (Courtesy J. de la Rosette, Connaught-strain over Tice and pre-existing The Netherlands) immunisation may be beneficial. Finally, optimising strategies for instillation therapy were discussed and preliminary data of the potential benefits of En-bloc resection of bladder tumours provides thermochemotherapy were presented by Mr. Eshel complete resection, or even enucleation of the (Tel Aviv, IL), who proposed improved outcome with tumour, without tumour fragmentation and the high-flow heated chemotherapy (MMC at 47°) and potential risk of tumour cell dispersal and seems even prolonged disease-free intervals using prepossible for tumour sizes up to 3 cm in diameter TUR-B chemotherapy instillation. [Fig. 3]. Various devices, including water-jet, laser as well as mono- and bipolar hooks are used within The participants had a comprehensive and productive clinical trials to evaluate the clinical efficacy. However, ESUT/ESOU meeting, examining crucial aspects of the although the experimental data seems very modern management and future trends in nonpromising, clinical data is insufficient so far and the muscle invasive TCC. results of on-going trials need to be awaited, before any evaluation of these techniques will be possible. “Gathering a group of experts from different fields in this focused, open and unbiased meeting makes possible for us to identify the prospects and directions of modern disease management,” said “...OCT (Optical Coherence Rassweiler. Tomography), which enables the assessment of tumour extension and infiltration depth, especially of upper urinary tract tumours...” Instillation therapy Early instillation chemotherapy should be standard of care in all singular low-risk tumours to reduce re-implantation of tumour cells, while the effect seems negligible in patients with multiple, recurrent or large and high-grade tumours. Fig. 3: En bloc laser enucleation of papillary tumour of the bladder (Courtesy T.R.W. Herrmann, Germany) http://seem.uroweb.org ESU Medical Oncology course on Genitourinary Cancer (MOGUC) at the occasion of the 5th EMUC Place Date Chair Marseille, France 14 November 2013 J. Palou, Barcelona (ES) H. Van Poppel, Leuven (BE) 08.00 Genitourinary cancer: urologist and oncologist J. Palou, Barcelona (ES) H. Van Poppel, Leuven (BE) 11.45 Testis cancer: chemotherapy according to histology and stage G. Kramer, Vienna (AT) S. Osanto, Leiden (NL) 08.05 Pre knowledge test 12.15 Lunch 08.30 Kidney cancer: surgery or targeted therapy in local recurrence and metastatic disease. Why, which and when. M. Kuczyk, Hanover (DE) 13.15 Testis cancer: cases in daily practice G. Kramer, Vienna (AT) S. Osanto, Leiden (NL) 09.00 09.30 Kidney cancer and metastatic disease: evaluation and sequential treatment. New advents in immunotherapy. B. Escudier, Villejuif (FR) Interactive case discussion M. Kuczyk, Hanover (DE) B. Escudier, Villejuif (FR) 10.00 Break 10.15 Prostate cancer: concepts and daily management in metastatic disease. Hormonal therapy N. Mottet, Saint Etienne (FR) 10.45 11.15 Prostate cancer: drugs available in the last years. When and why? And the vaccines? Let´s be clear S. Chowdhury, London (GB) Interactive clinical case discussion S. Chowdhury, London (GB) N. Mottet, Saint Etienne (FR) EAU 9th South Eastern European Meeting (SEEM) 1-3 November 2013, Thessaloniki, Greece EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations 13.45 Bone therapy: mechanism of action, useful, when and in which GU tumours? K. Miller, Berlin (DE) 14.15 Interactive case discussion K. Miller, Berlin (DE) 14.45 Break 15.00 Bladder cancer: what it is the advised combination therapy and when. Unmet medical needs in bladder cancer. J. Bellmunt, Barcelona (ES) F. Witjes, Nijmegen (NL) 15.30 Interactive case discussion J. Bellmunt, Barcelona (ES) F. Witjes, Nijmegen (NL) Call for Abstracts 16.00 Post knowledge test deadline 1 August 2013 16.30 Close For more information please go to www.uroweb.org European Association of Urology 20 European Urology Today March/May 2013 ESU - Weill Cornell Masterclass in General urology EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations For more information please contact the EAU Education Office at [email protected] or go to http://esusalzburg.uroweb.org 7-13 July 2013, Salzburg, Austria Sunday, 7 July 2013 Arrival at Schloss Arenberg, check-in and registration 18.00 – 19.00 19.00 – 19.30 19.30 – 20.30 Faculty meeting Welcome reception Dinner 11.30 Adrenal surgery: Why and when? 12.30 Lunch 14.00 OMI/AAF Presentation 14.15 Tips and tricks: Vasectomy, varicocelectomy Monday, 8 July 2013 08.00 Pre Seminar test 09.00 Urethral surgery: Basic principles 10.00 Coffee break 10.30 Urethral surgery update: Technique and results 11.30 Erectile dysfunction update 12.30 Lunch 14.00 Testosterone replacement: Benefits, risks, and therapeutic options C.R. Chapple, Sheffield (GB) C.R. Chapple, Sheffield (GB) M. Remzi, Vienna (AT) P. Schlegel, New York (US) W. Aulitzky, Vienna (AT) 15.30 – 17.00 Cases by participants P. Schlegel, New York (US) J. Walz, Marseille (FR) 08.00 09.00 15.00 – 17.00 Cases by participants 08.00 Infertility update: Advanced therapy and new insights P. Schlegel, New York (US) 09.00 Varicoceles: Action, indications and surgical repair - current status 10.00 Coffee break 10.30 Adrenal gland: Physiopathology and diagnostic tests P. Schlegel, New York (US) J. Walz, Marseille (FR) European Uroradiology of the kidney masses: computed tomography (CT), magnetic resonance imaging (MRI), nuclear scintigraphy, ultrasound: Why and when in the diagnosis and follow up? Treatment of localised renal cell carcinoma: Technical aspects of open partial nephrectomy, role of minimally invasive techniques. role and extent of lymph node dissection in renal cancer H. Van Poppel, Leuven (BE) 10.00 Coffee break 10.30 Surgery for advanced and metastatic renal cancer S.F. Shariat, Vienna (AT) 11.30 Systemic therapy for advanced and metastatic renal cancer S. Tagawa, New York (US) 12.30 10.00 Coffee break 10.30 Penile cancer management of the primary and the nodes 11.30 Laparoscopic surgery: Tips and tricks and its use for testicular cancer J. Walz, Marseille (FR) 15-20 participants others: free afternoon Thursday, 11 July 2013 08.00 Association Testicular cancer: Treatment stage by stage S.F. Shariat, Vienna (AT) of Urology 12.30 Friday, 12 July 2013 08.00 09.00 Peyronie’s disease: New concepts in management 10.00 Coffee break 10:30 Ejaculatory dysfunction W. Aulitzky, Vienna (AT) 11:30 16.30 Coffee break 08.00 - 10.00 17.00 - 18.00 Module 5 - Female urinary retention and bladder emptying disorders Coffee break 10.30 - 12.30 Module 2 - OAB and mixed incontinence 12.30 - 13.00 Cases by participants 13.00 - 14.00 Lunch break 14.00 - 15.30 Module 3 - Female reconstructive surgery F. Burkhard, Berne (CH) E. Costantini, Perugia (IT) D. De Ridder, Leuven (BE) Urethral diverticula Urethral reconstruction Vesicovaginal fistula Ureteric fistula Radiation fistula and injuries 15.30 - 16.30 D. Castro Diaz, Santa Cruz De Tenerife (ES) C.R. Chapple, Sheffield (GB) CIC management Neuromodulation Module 4 - Imaging of the lut and gu tract F. Burkhard, Berne (CH) E. Costantini, Perugia (IT) J.P.F.A. Heesakkers, Nijmegen (NL) X-ray techniques MRI Ultrasound High risk prostate cancer in 2013: an update H. Van Poppel, Leuven (BE) 12.30 Lunch 14.00-17.00 Cases by participants 17.00 Post Seminar test 18.00 Farewell reception 19.00 Graduation dinner + selection 4 candidates cases W. Aulitzky, Vienna (AT) D. Paduch, New York (US) H. Van Poppel, Leuven (BE) Saturday, 13 July 2013 Farewell breakfast and departure EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations For more information please contact the EAU Education Office at [email protected] or go to Definitions, diagnostics, prevalence Conservative management Male slings Artificial sphincters Complication management 17.00 - 18.00 Saturday, 16 November 2013 08.00 - 09.00 Module 6 - Female sexual function E. Costantini, Perugia (IT) Hormonal changes Sexual abuse Dyspareunia C. R. Chapple, Sheffield (GB) J.P.F.A. Heesakkers, Nijmegen (NL) Definitions, diagnostics, classification Clinical decision making Conservative and medication management Refractory OAB (Btx and neuromodulation, augmentation) D. Paduch, New York (US) http://esuberlin.uroweb.org Friday, 15 November 2013 10.00 Sexually transmitted diseases: A 2013 update D. Paduch, New York (US) 15-17 November 2013, Berlin, Germany Definitions, diagnostics, classification and decision making Conservative treatment (EAU guidelines) Surgical management (EAU guidelines) Complication management Lunch break 15-20 participants others: free afternoon In collaboration with the EAU Section of Female and Functional Urology (ESFFU) D. De Ridder, Leuven (BE) A. Vaze, Mumbai (IN) W. Aulitzky, Vienna (AT) C.R. Chapple, Sheffield (GB) G. Janetschek, Salzburg (AT) D. Paduch, New York (US) M. Remzi, Vienna (AT) P. Schlegel, New York (US) S.F. Shariat, Vienna (AT) S. Tagawa, New York (US) H. Van Poppel, Leuven (BE) J. Walz, Marseille (FR) 14.00 – 17.00 Hands-on training laparoscopy 6th ESU Masterclass on Female and functional reconstructive urology Module 1 - Stress incontinence Faculty G. Janetschek, Salzburg (AT) Lunch 14.00 – 17.00 Hands-on training laparoscopy Role and indications for chemotherapy for testicular cancer S. Tagawa, New York (US) J. Walz, Marseille (FR) P. Schlegel, New York (US) Tuesday, 9 July 2013 09.00 Wednesday, 10 July 2013 W. Aulitzky, Vienna (AT) C.R. Chapple, Sheffield (GB) W. Aulitzky, Vienna (AT) P. Schlegel, New York (US) M. Remzi, Vienna (AT) 09.00 - 11.00 08.00 - 10.00 Coffee break 10.30 - 13.00 Module 8 - Bowel K. Matzel, Erlangen (DE) Anal incontinence Constipation 13.00 - 14.00 Lunch break 14.00 - 15.00 Cases by participants 15.00 - 17.00 Module 9 - Male incontinence D. Castro Diaz, Santa Cruz De Tenerife (ES) D. De Ridder, Leuven (BE) J.P.F.A. Heesakkers, Nijmegen (NL) Module 11 - Neurogenic bladder D. Castro Diaz, Santa Cruz De Tenerife (ES) J.P.F.A. Heesakkers, Nijmegen (NL) Neuroanatomy related to type of bladder dysfunction Conservative management Surgical management Urodynamic follow-up of patients with neurogenic bladder Complication management (chronic UTI, stones, renal failure, deteriorating hand function) E. Costantini, Perugia (IT) D. De Ridder, Leuven (BE) A. Vaze, Mumbai (IN) 11.00 - 11.30 D. Castro Diaz, Santa Cruz De Tenerife (ES) Diagnosis, classification Prophylaxis EAU guidelines F. Burkhard, Berne (CH) D. Castro Diaz, Santa Cruz De Tenerife (ES) C.R. Chapple, Sheffield (GB) E. Costantini, Perugia (IT) D. De Ridder, Leuven (BE) J.P.F.A. Heesakkers, Nijmegen (NL) K. Matzel, Erlangen (DE) A. Vaze, Mumbai (IN) Sunday, 17 November 2013 Module 7 - Pelvic organ prolapse Anatomy and clinical examination and classification (POP-Q) Vaginal prolapse repair Abdominal/laparoscopic/robotic prolapse repair Mesh or no mesh Complications: classification and management The frail and elderly Module 10 - UTI Faculty 10.00 - 10.30 Coffee break 10.30 - 11.30 Module 12 - Chronic pelvic pain F. Burkhard, Berne (CH) Definitions, prevalence, etiologies EAU guidelines on assessment and treatment algorithm 11.30 - 12.30 Module 13 - Diversion surgery for functional reasons F. Burkhard, Berne (CH) D. De Ridder, Leuven (BE) Decision making Surgical techniques (Bricker, neo-bladder, Monti-Yang, Mitrofanoff) Complication management 12.30 This Masterclass is accredited within EU-ACME programme by EBU with credit points Adjournment European Association of Urology March/May 2013 European Urology Today 21 Young Urologists/Residents Corner Creating a network of professional contacts Danish resident gives high approval mark to Residents Day Dr. Pernille Skjold Kingo Dept. of Urology Århus University Hospital Århus (DK) pernille.skjold@ stofanet.dk As in previous years, the Young Urologists Office (YUO) in collaboration with the European Society of Residents in Urology (ESRU) organised a special session for young urologists, and presented a day-long programme that featured many excellent and inspiring lectures by urology experts. The main topic focused on how to prepare young urologists after residency training with a special emphasis on building up surgical skills, and the need to be actively involved in national and international research projects. A. Mottrie, (Aalst, BE) lectured on robot-assisted laparoscopy for young trainees, while B.S.E.P Van Cleynenbreugel, (Leuven, BE) presented a video session on basic laparoscopic skills. Both presentations provided a very good insight on how, when and where the training of these techniques could be undertaken. They also stressed the importance for young urologists to master the basic skills needed in the work-up of diagnosing urological diseases such as prostate cancer. L.N. Türkeri (Istanbul, TR) gave a very thorough and useful presentation on how to perform a TRUS- guided prostate biopsy. Meanwhile, O. Traxer (Paris, FR) explained how to perform a good PCNL and when to choose the mini-perc and the standard nephrectoscope. ESRU’s former chairman M.E. Silay (Istanbul, TR) gave an overview of the trends in paediatric urology, and noted that due to improvements and development of smaller and better laparoscopic and endourologic equipment during the last decade this has led to a great change in the treatment regimens for paediatric patients. He said many of the paediatric procedures that used to be performed by open procedure are now more commonly performed by either laparoscopy or endoscopy. F.M.E. Wagenlehner (Gieβen, DE) thoroughly discussed the different antibiotics and resistant patterns, and stressed the fact that with the use of many antibiotics, organisms are becoming more and more resistant, and as a consequence patients no longer respond to treatment, and in worst case scenarios can even lead to urosepsis. One of his take home messages is to check the resistant pattern if a patient don’t respond to the prescribed antibiotic instead of simply prolonging the treatment with the same antibiotic. He also urged urologists to use antibiotics wisely and include it in their treatment strategy only when indicated. of the main causes of this phenomenon is due to couples who decide to have a family at a later age. gave the participants the opportunity to actively interact with the experts. Career choices Another topic discussed was making the choice for a primarily academic or clinical career after residency training. An interesting debate on the subject was presented by S. Al Hayek (Cambridge, GB) and E.B. Cornel (Hengelo, NL), and both presenters made convincing arguments. In the end, young urologists have to decide for themselves, whilst taking into careful consideration the opportunities and drawbacks in either the academic or clinical practice. The programme ended with the Nightmare Case session, with three challenging cases presented by young urologists. All cases were very informative, well presented and prompted a good discussion regarding diagnosis, treatment and identifying potential complications. The social programme included a dinner which provided the opportunity for the residents to get to know each other in a more relaxed setting. The Residents Day met my expectations, and served very well its aim to provide a platform for young urologists to share experiences and network with colleagues from other countries. The speakers’ messages reiterate the need to work hard, practising and refining one’s skills and engaging in innovative research work. Overall, this annual event is highly informative and I thank the organisers for a very productive and memorable day. As a follow-up to the debate on career choices, A.G. Van der Heijden (Njimegen, NL), G. Godoy (Houston, Texas, US), H. Fajkovic (St. Pötten, AT) and S.Larre (Reims, FR) shared their experiences, advice and tips on how to secure a scholarship or fellowship, and how they manage to achieve their career aims through networking and continued efforts for self-improvement and skills training. Their presentations were very inspiring that one feels encouraged to immediately apply and get started. Andrologist J.O.R. Sonksen (Herlev, DK) presented a diagnostic approach and clinical work-up for the infertile couple. Even though these cases are referred to experts in specialised centres, the young urologist needs to know this kind of patient so they can give the right diagnosis and prescribe the proper treatment for Other highlights were a discussion on the residency the couple. Interestingly, 8% of all children born curriculum, the Campbell Quiz session and the nowadays are conceived through IVI-D or IVI-H. One presentation from the EAU Guidelines Office which Dr. Timothy Oedekoven (DE) presenting a Nightmare Case Endourology fellowship in Pakistan The Indus Hospital Initiative Dr. Andreas Bourdoumis Endourology and Stone Services Barts Health NHS Trust London (GB) bourdoua@ hotmail.com After completing my training in general urology at the 2nd Department of Urology at Sismanogleio General Hospital of the University of Athens, Greece, I was lucky to be appointed as endourology fellow at the Royal London Hospital in London, UK. Shortly after the start of this two-year EBU-accredited fellowship I participated in a charity mission to Pakistan. This project, called “The Indus Hospital Initiative” was initiated by my programme director Mr. Noor Buchholz and aims to bring together a team of urologists which, using their own finances and free time, travel to the Indus Hospital in Karachi to support local urologists. I consider it a challenge to join a group of experts who are travelling to a potentially unstable region. Nevertheless, the opportunity was indeed unique and presented an opportunity for me to further improve my skills in advance endourologic procedures. Dr. Christian Bach Dept of Urology Southmead Hospital Bristol (GB) Christian.Bach@ bartsandthelondon. nhs.uk knowledge transfer. This goal is essential since the local urologists-in-training have very little opportunities to travel abroad due to financial and political circumstances. Conducting operations with the local urologists proved to be highly productive as we demonstrated techniques such as supine PCNL and the “Barts flank free modified supine position.” We could also learn from the highly-skilled local urologist who showed their own technique in prone PCNL using an upper pole puncture and which has the advantage of clearing even staghorn stones with only one access. A total of 11 PCNL and several other urological procedures were performed during our stay in Karachi. Our team consisted of Mr. Noor Buchholz, director of the Royal London Endourology and Stone Services, Mr. Islam Junaid, consultant urological and transplant surgeon, Mr. Christian Bach, former senior endourology fellow in the Royal London Hospital and currently fellow in robotics at the Southmead Hospital in Bristol. To cover the academic aspect, the director of the Indus Hospital, Dr. Zafar Zaidi organised a urolithiasis symposium with a faculty consisting of our own team and local experts. Important topics included basic science of stone formation, metabolic aspects, prevention, modern treatment modalities as well as future perspectives. Around 50 participants from Karachi attended this very successful meeting. There were also participants from the neighbouring cities of Hyderabad and Bahawalpur and one delegate even traveled more than 500 km by car from Larkana city! The mission would focus on sharing our expertise as doctors from a high-volume stone unit and tertiary referral centre. The programme would include mentoring local urologists both theoretically and in the operating room thereby creating a platform for But the most impressive, in my view, was our visit to the Indus Hospital itself which was made possible due to the commitment and perseverance of a small group of idealists in a country still facing political turmoil. 22 European Urology Today A charity institution, Indus Hospital is entirely a Dornier Sigma ultrasound guided lithotripsy unit financed with donations and was envisioned by Dr. and in the very busy outpatient section up to a Abdul Bari Khan, Dr. Zafar Zaidi, Dr. Amin Chinoy and hundred patients per day come for consultation. Dr. Akhtar Aziz Khan as a tertiary care centre to provide quality care for the less privileged. It took “...deeply impressed by the more than 10 years from the original conception to the achievements of the hospital’s four laying of the hospital’s foundations. The first patients were admitted in July 2007 and the first surgical pioneers...” operation took place in the following month. The founders of Indus Hospital planned to establish a modern university hospital of 1,200 beds, with Located in the Korangi area, in the southern part of medical, nursing and research schools on site and the the city, the 150-bed hospital prides itself to be the first truly eco-friendly hospital in the region. We were improvements will all be entirely funded by donations and non-profit fund raising. It may seem an amazed how few disposables were used and how impossible task, but one only has to hear Zaidi’s view quick and efficient everything was organised. It has six operating theatres for adult and paediatric surgical regarding the project: If 100,000 people were committed to offer 1,000 Pakistani rupees (about 10 procedures, including trauma and orthopaedics, general surgery, cardiothoracic surgery, urology, ENT, euros) every month for a five-year period, the whole project would be completed within that time frame, ophthalmology and dental services. It also offers a and a sustainable endowment would be created to six-bed ITU and dedicated endoscopy and support the infrastructure plans and pay the daily angiography suites. functional expenses. And indeed, there is already a very supportive, mainly Pakistani community of The urology department is staffed by two consultant supporters in the country itself. Overseas the project urologists, Dr. Zafar Zaidi and Dr. Zaheer Alam, one associate specialist and five residents. The department offers a great opportunity for Pakistani expatriates to support the home country in an effective and occupies an entire floor with 36 beds. The workload sustainable way. consists mainly of stone surgery, transurethral operations, upper tract laparoscopic and reconstructive surgery. A dedicated urologist operates The trip was truly an unforgettable experience for me and also a great learning opportunity from a medical and human perspective, giving me a sense of fulfillment and accomplishment due to its altruistic goals. I am deeply impressed by the achievements of the hospital’s four pioneers and I am also looking forward to return to Karachi in the future, knowing that Dr. Buchholz and Dr. Zaidi plan to establish a charity project. From right: Mr Bourdoumis, Mr Buchholz, Dr Alam, Dr Zaidi, Mr Junaid and senior resident Dr Abdul Hafeez Qureshi during a retroperitoneoscopic nephrectomy More significantly, this charity hospital would not exist without the help of many and I strongly encourage anyone to support this fantastic project. Visit their website at: http://indushospital.org.pk for more information or contact Dr. Zaidi directly by writing to [email protected]. March/May 2013 Young Urologists/Residents Corner A call for active support Organisers of Residents’ Day look for more input from young urologists Dr. Guillermo Martinez ESRU Secretary Member of the Young Urologists Office Koper (SI) esrusecretary@ gmail.com “Don’t ask what Residents and Young Urologists Day can do for you...” I presume readers would know not only the reference of the statement above, but also what to add and complete this sentence. And that is why we have decided to get you involved in deciding what should next year’s’ Special Session offer. But first of all, let us recall the Residents Day meeting held a few months ago. During the 28th Annual EAU Congress in Milan, and also in previous congresses, the Young Urologists and Residents Day Special Session took place on Saturday, March 16. Organised by the Young Urologists Office together with ESRU, it was one of the most visited sessions in the congress with more than 500 participants scanned and a nearly full session hall throughout the day. The meeting featured an excellent line-up of speakers and a carefully prepared programme, precisely tailored to what we believe would cater to the needs of young urologists and residents. various urological specialties. For this session we are grateful to have the direct support of the European Board of Urology (EBU) and the EAU, a collaboration which demonstrates the continued joint effort by everyone to understand how urological training in Europe is being performed. Moreover, these efforts attempt to come up with a common European urological curriculum that will serve as a reference or basis of what is to be accomplished during training. By presenting the perspective of our more senior colleagues who have all gone through the various phases of training and education and are now successful specialists, participants can receive insights and have an overview on future prospects, tips on whether to pursue an academic or non-academic career and scholarship opportunities, among other key topics. The latter is particularly important for novice urologists and the speakers certainly provided helpful suggestions and effective approaches on how to secure and benefit from fellowships and the essential preparation needed for a career changing experience. The session also examined challenges and future prospects, with a panel discussing issues such as employment, migratory and labour trends and how the current European economic landscape impact on healthcare issues. In another session we have addressed the issue of training and what is expected from a trainee in terms of knowledge and skills that are required in the Moreover, a wonderful evidence-based session was also held, with excellent speakers discussing the latest evidence in endourology, biopsy techniques, As in 2012, we also had a presentation from the EAU Guidelines Office with an update on evidence analysis, including a live demonstration of the innovative Internet-based update system. Several young urologists and residents have been trained by the EAU Guidelines Office to create teams for evidence analysis. Milan Congress: Clockwork efficiency Italian resident experiences congress for the first time Dr. Giulio Patruno University ‘Tor Vergata’ of Rome Dept. of Urology Rome (IT) g.patruno@ gmail.com Benvenuti! (Welcome) is one of the first words that tourists learn when travelling in Italy. ‘Benvenuti a Milano!’ said Prof. Francesco Montorsi during the opening ceremony as he formally welcomed more than 13,000 participants from all over the world who came to Milan. As a junior resident, this year’s congress has been more than just a meeting. The event was my first European congress and brought me for the first time to Milan, Italy’s second biggest city and the country’s economic and financial hub. Here Piazza Affari (as the stock exchange is nicknamed) operates 24 hours a day with thousands of bankers crowding Milan’s busy streets. The congress was impressive and the efficient organisation was reflected in the timely arrival of shuttle buses that picked up the delegates from the closest metro station. At the congress venue everything ran with clockwork precision, from the welcome, registration, information to the friendly staff members. My fellow Italian ESRU National Communication Officer (NCO), Dr. Gianluca Salerno and I attended the ESRU Board meeting on Friday afternoon before we proceeded to the opening ceremony which featured an opera performance from La Scala. After the ceremony, and following Milanese tradition, aperitivi was served. Saturday was the Resident’s Day, which gave me an opportunity to look into the experiences of residents in other European countries. Excellent reports and great lectures covered many key urology topics, ranging from surgical to medical treatment strategies, from paediatric to functional urology, to name a few. Big questions faced by residents were also examined such as career planning, clinical practice vis-à-vis an academe-based profession, and scholarship opportunities. More than 400 participants attended and this year the Campbell’s Quiz challenged many of the residents, with an Austrian resident beating other participants for the top prize. In the evening, the Resident’s Dinner March/May 2013 took place at the Il Gattopardo Cafè, with free drinks and clubbing late into the night. The evening gave us a needed break, allowing us to get to know our colleagues better in an informal and relaxed atmosphere. Learning opportunities The next two days, although hectic, offered many learning opportunities such as training sessions, symposia and courses. Hands-on training with simulators gave us an opportunity to perform new and more complicated surgical procedures. Being well trained on simulators provides the benefit of lower risks when doing actual operations and also shortens the so-called learning curve. On Monday, the European Urological Scholarship Programme (EUSP) session gave a comprehensive overview of the scholarships and training available to residents, and Prof. Mirone offered helpful and detailed information, and showed how a scholarship can play a crucial role in one’s career development. I also met old and new colleagues and friends from all over Europe, and the exhibition hall served as a convenient meeting point. At the EAU booth, we picked up copies of the handy pocket version of the 2013 Guidelines and other publications. The ESRU booth was also located near the EAU’s, and residents got the chance to receive detailed information about the association and their activities. At the final plenary session, the role of PSA screening, risk and benefits were extensively discussed, including both the European and American perspectives. Prof. Per-Anders Abrahamsson concluded his lecture by emphasizing that men who consider PSA screening should be aware of the risks and benefits of the procedure. Outside the congress, we had the chance to see a little of Milan. At the Gallery Vittorio Emanuele II, right in the centre of Milan’s fashionable district near Via Montenapoleone, the bag and shoe stores have been quite popular among our female colleagues! In the Last but not least, we had our annual Campbell’s Quiz Session. This year one extremely well-prepared participant won the latest edition of Campbell’s Urology, surely a well-deserved prize. For residents, how would you complete or finish the opening statement in this article? What can you do for next year’s Special Session? It’s plain and simple: just let us know what you would like to discuss or be taken up for next year. Help us understand or alert us whether we are on the right track or if we need to focus on something that we have missed. To achieve this, the ESRU together with the Young Urologists Office will conduct a survey among our network of national representatives. The survey questionnaire should reach you within the next couple of months. Please do support us and send your feedback. The ESRU and the Young Urologists Office would like to thank everyone who contributed to the success of this year’s Residents and Young Urologists Day. We look forward to see you next year. With your active support we hope to organise and present in 2014 an even better programme in Stockholm, Sweden. Residents’ Day: Tips and challenges I have attended the AUA Meeting before, but it was my first time to attend the EAU Congress. Comparing these congresses I realised that they have the same impact, coverage and influence. The Resident’s Dinner presents a chance to get to know residents from other countries In the case of the EAU Congress this year, Milan in Italy as a venue was an ideal choice with its historical legacy, accessible location and efficient transport systems. At the congress, I attended the Residents’ Day, certainly an important meeting particularly to urology residents like me. Attendance to this meeting was high and the session hall was full during the plenary meetings. Gallery there is a “urological” curiosity. At the central mosaic of the Gallery’s floor, a bull from Turin’s coat-of-arms is depicted. According to tradition, it will bring good luck if a person puts his right heel on the bull’s genitals and turns three times. The Residents’ Day programme featured lectures and talks about a career in urology, opportunities for fellowships and research grants in European and American clinics, tips on how to develop and improve one’s research projects and clinical practice, and how to secure other career or professional opportunities. Testimonials As the ESRU-NCO from the host country I have asked some Italian colleagues for their comments of the congress. Dr. Marco Casilio, a young andrologist from the Hospital Villa Tiberia in Rome said: “I really appreciated the Video Sessions and attended most of the sessions at the eURO Auditorium. In particular, I really liked the videos on robot-assisted surgeries.” In my view this kind of meeting, with its emphasis on professional skills and properly identifying the various challenges and prospects in our specialty is important as it has an influence on the development and growth of urology as a specialty. With the globalised world that we live in today it is certainly important to examine and consider various viewpoints and opinions. Dr. Eugenia Fragalà (Catania, Sicily), said: “The congress was an amazing experience and many video sessions were extremely interesting. It was great to watch the best urologists doing live operations. At the EAU congress, I found only the best!” Another topic discussed during the meeting was the current challenges and obstacles faced by residents, the prospects that we have and how to resolve the issues on education, training and career development. A traditional feature in the programme was the Campbell Team Challenge Quiz session which I find very informative and enjoyable. “I liked hands-on courses and I attended “Laparoscopy for Beginners,” said Dr. Valerio Iacovelli, a resident from Rome. “The practical approach gave trainees the right trips and tricks on surgical procedures, and the relaxed mentoring of our tutors is also very helpful.” Dr. Marilena Gubbiotti, a resident from Perugia, appreciated the high quality scientific programme. “The five days were wonderful and are very helpful for the growth of young urologists like us. With the participation of the world best experts, we can only benefit from this experience.” The ESRU board at work infertility, functional urology, paediatric urology to urological infections, among other topics. I can only agree with my colleagues as the congress has been an exciting and rewarding experience. It served as a window to European and international urological practice, and a great opportunity to directly hear from the experts their views on key issues. After the break, sessions focused on various urological issues such as an update on guidelines analysis. The presentation of former ESRU president, M. S. Sılay on paediatric endourology was not only well-illustrated with humorous pictures but also impressive. During the Nightmare Session interesting clinical problems that have perplexed residents were discussed with the invited experts. The programme closed with the awarding ceremony. Overall, I am glad that I had the chance to attend and be part of this very well organised Annual EAU Congress and the Residents’ Day, and I hope that I can again take part in future meetings. Dr. Fatih Elbir, Istanbul (TR) European Urology Today 23 Open stone surgery in 2013 With more expertise on minimally invasive procedures, open surgery for stones is declining Mr. Hammad Ather Associate Professor Aga Khan University Karachi Karachi ( PK) hammad.ather@ aku.edu Mr. Noor Buchholz EULIS board member London (GB) nb@londonurology consultant.com to encrusted stent including obstruction and infection. Forgotten stents can often become encrusted1 involving not only the two coils but sometimes the whole length of the stent. The best therapy is prevention. We described the use of an automated computerised system to track overdue stents which was able to decrease the number of overdue stents dramatically from 12.5 to 1.2% within one year since the start of the programme2. Matlaga and Assimos3 looked at the trend of open surgery at Wake Forest University in North Carolina, United States. They observed that between 1998 to 2002, of 986 procedures performed for the purpose of stone removal, only 0.7% were open surgical procedures, compared with the earlier reported rate of 4.1% in 893 procedures. The two most frequent indications for open intervention in the two aforementioned series3,4 were failed endourological interventions and anatomical abnormalities precluding endourological surgery. “Urolithiasis is a highly recurrent disease. Approximately 50% of patients will form another stone in five to seven years...” between 1987 and 1995 to 8% between 1996 and 1998. However, the remaining indications for open ureterolithotomy include failure of less invasive modalities, the presence of medical/ anatomical abnormalities, a concomitant open procedure, and the presence of large impacted calculi for which patients prefer to avoid multiple procedures. Introduction of shock wave lithotripsy (SWL), percutaneous nephrolithotomy (PCNL), semi rigid ureteroscopy (URS) and retrograde intra renal surgery (RIRS), and laparoscopy all have drastically reduced the need for open surgery. Indications of open surgery are currently restricted to complex stones, failed endourological treatment and anatomical abnormalities. However, in a well-equipped endourological centre with appropriate expertise almost all urinary tract stones can be dealt with in a minimally invasive fashion avoiding open surgery nowadays. References Ather et al.5 have looked at the need for open surgery for ureteral stones in a developing country and noted The management of urolithiasis has seen a paradigm that with recent advances in endourology the shift. Open surgery was the predominant modality up indications for open surgery have decreased considerably, from 26% between 1989 and 1995 to to the 1980’s. Today, it is hardly done any more in a 8% between 1996 and 1998. However, the remaining well-equipped endourological unit. indications for open ureterolithotomy include failure of less invasive modalities, the presence of medical/ Current indications of open surgery are limited and anatomical abnormalities, a concomitant open are becoming increasingly more limited with procedure, and the presence of large impacted calculi advances in endourology and laparoscopy. These indications include complex stone burden, anatomical for which patients prefer to avoid multiple procedures. abnormalities precluding endourological interventions, and as a salvage procedure following failed endourological interventions. “Besides costs, patient compliance is Renal stones Complex renal stones are considered as a possible indication for open surgery. Complexity of renal stones can be defined based on stone- and patientrelated factors. However, its definition is highly relative and widely surgeon- and centre-dependent. The stone related factors include stone-burden, -distribution and calyceal anatomy. Patient-related factors include body habitus (in particular spinal deformities), co-morbidities, use of anticoagulants and bleeding diathesis, and patient compliance. Indication of open surgery is heavily dependant on the availability of endourological armamentarium and expertise. Cost is another important consideration, as minimally invasive surgery (MIS) may require multiple procedures and numerous disposables. Besides costs, patient compliance is another important factor in choosing MIS for complex renal stones. Urolithiasis is a highly recurrent disease. Approximately 50% of patients will form another stone in five to seven years following their first stone episode8. The treatment of recurrent large burden renal stones with a history of previous open surgery is particularly challenging due to the altered retroperitoneal anatomy. Gupta and colleagues noted that patients undergoing PCNL with a past history of renal stone surgery may need more attempts to access the pelvi-caliceal system and have some difficulty in tract dilatation because of retroperitoneal scarring. However, overall morbidity and efficacy was the same in both, patients with or without previous open stone surgery9. another important factor in choosing MIS for complex renal stones.” In our experience, even in a developing country scenario, the indications for open surgical intervention for renal stones have decreased dramatically6. The rates of open surgical intervention for renal stones in 2010, 2011, and 2012 were 4.5, 3.7 and 3.9%, respectively. This is not only due to advances and easier availability of endourological techniques, but also to increasing awareness and desire of the patients for less invasive procedures. Interestingly, the increasing trend in MIS does not result from evidence-based direct comparisons. There are no good head-to-head trials comparing various endourological interventions and open surgery. Recently Barack and colleagues7 compared open surgery and PNL for pediatric renal stones. They noted Another relative indication for open surgical intervention may include neglected, heavily encrusted that PNL has superiority over open surgery with stents. Patients can present with complications related regards to in-patient stay, transfusion, and rate of stenting. However, the stone free rate 91% for PCNL and 85% for open surgery were not statistically EAU Section of Urolithiasis (EULIS) significant different (p = 0.318). The 2011 EAU Guidelines provide a comprehensive list of indication for open surgery. Complex stone burden is the foremost indication for open stone surgery. However, complex stone burden remains a poorly defined term as complexity may result from stone burden, intra-calyceal distribution, calyceal anatomy, renal anatomy and concomitant abnormalities like UPJO. Another determining factor is the availability of endourological armamentarium and the level of expertise. Ureteral stones As far as ureteral stones are concerned, optimal treatment modalities for large proximal ureteral stones are controversial, and include SWL, ureteroscopic stone fragmentation, PCNL, laparoscopic ureterolithotomy and open surgery. There has been some good quality evidence. A recently reported small RCT from Brazil9 compared SWL, ureteroscopy and laparoscopic ureterolithotomy and noted that large proximal ureteral stones often require multiple procedures to achieve stone-free status. Laparoscopic ureterolithotomy, as compared with SWL or ureteroscopy, may achieve higher stone-free rates and fewer re-treatments, but is associated with more postoperative pain, a longer procedure time and hospital stay. Almeida and colleagues10 in a prospective non-randomised trial compared open and laparoscopic ureterolithotomy and noted that laparoscopy offered significant advantages over open ureterolithotomy, resulting in improved analgesia and shorter hospital stay, with similar complication rates The rate of open surgery for ureteral stone has not only declined in the west but also in developing countries. As mentioned above, Ather et al.5 reported a reduction in the number of open operations performed in their hospital in Pakistan from 26% 1. Vanderbrink BA, Rastinehad AR, Ost MC, Smith AD. Encrusted urinary stents: evaluation and endourologic management. J Endourol 2008;22(5):905-12. 2. Ather MH, Talati J, Biyabani R. Physician responsibility for removal of implants: the case for a computerized program for tracking overdue double-J stents. Tech Urol 2000;6(3):189-92. 3. Matlaga BR, Assimos DG. Changing indications of open stone surgery. Urology. 2002;59(4):490-3. 4. Assimos DG, Boyce WH, Harrison LH, McCullough DL, Kroovand RL, Sweat KR. The role of open stone surgery since extracorporeal shock wave lithotripsy. J Urol 1989;142:263-7. 5. Ather MH, Paryani J, Memon A, Sulaiman MN. A 10-year experience of managing ureteric calculi: changing trends towards endourological intervention - is there a role for open surgery? BJU International 2001;88:173-177. 6. Ather MH. Open surgery for stones in 2012. Experts in Stone Disease conference (ESD 2012), Dubai, UAE, 13-16th Dec 2012. 7. Bayrak O, Seckiner I, Erturhan S, Duzgun I, Yagci F. Comparative analyses of percutaneous nephrolithotomy versus open surgery in pediatric urinary stone disease. Pediatr Surg Int 2012;28:1025–1029. 8. Pramar MS. Kidney stones. BMJ 2004;328(7453):1420-4. 9. Gupta R, Gupta A, Singh G, Suri A, Mohan SK, Gupta CL. PCNL--A comparative study in nonoperated and in previously operated (open nephrolithotomy/ pyelolithotomy) patients--a single-surgeon experience. Int Braz J Urol 2011;37(6):739-44. 10. Lopes Neto AC, Korkes F, Silva JL 2nd, Amarante RD, Mattos MH, Tobias-Machado M, Pompeo AC. Prospective randomized study of treatment of large proximal ureteral stones: extracorporeal shock wave lithotripsy versus ureterolithotripsy versus laparoscopy. J Urol 2012;187(1):164-8. 11. Almeida GL, Heldwein FL, Graziotin TM, Schmitt CS, Telöken C. Prospective trial comparing laparoscopy and open surgery for management of impacted ureteral stones. Actas Urol Esp 2009;3(10):1108-14. Endourology course in Torino, Italy Enthusiastic response to EULIS-ESUT sponsored training Dr. Cesare Marco Scoffone Cottolengo Hospital Urology Unit Turin (IT) [email protected] The second edition of the Technology and Training in Endourology Course directed and organised by the author together with Drs. Cecilia Maria Cracco and Fabiola Liberale, took place from 8 to 10 November last year at the Cottolengo Hospital of Turin, Italy. urologists participated in this training which aimed to provide a dynamic exchange of endourological tips and tricks, define the various steps of minimally invasive procedures and deepen their knowledge of technologies that we regularly employ to optimise clinical results. The format of the course, conceived by the author and which was successfully implemented in 2011, included live surgeries performed by both selected experts and young urologists under tutorship. This year the procedures were Endoscopic Combined IntraRenal Surgery (ECIRS), Retrograde IntraRenal Surgery (also with digital instruments), bipolar TURB and TURP, HoLEP, vapoenucleation with Green Laser and ThuLEP. The quality of audio-visual transmission of both retrograde and antegrade endoscopic images, This initiative was created in 2011 under the together with fluoroscopy, ultrasound and sponsorship of the Italian Society of Urology (SIU), the environmental shots, was outstanding, thanks to the Italian Society of Endourology (IEA), and the European complete optic fiber wiring of the urologic operating Association of Urology (EAU) sections EULIS and ESUT. room, and the efficient work of the technicians. The A very practical and interactive course, 70 young active contribution of session moderators who provided insightful comments yielded informative and enlightening perspectives regarding the various steps EAU Section of Urolithiasis (EULIS) of the procedures. 24 European Urology Today Besides the live surgeries, the programme included roundtable discussions and focused commentaries, which this year covered a wide range of topics, such as the following: the pre-operative cooperation between urologists and radiologists, laboratory and endoscopic diagnosis of urolithiasis, prevention of recurrences, endoscopic approach in children, irrigation systems and the risk of high intrarenal pressures, pros and cons of all therapeutic approaches for urolithiasis, physical principles of lasers, training issues, technical issues on the various approaches in the treatment of LUTS, providing assistance or the use of flexible instruments, the between the audience and experts was stimulating various steps of RIRS (access, irrigation, lithotripsy, extraction of stone fragments, final stenting) and legal and for three days the session hall was full aspects regarding informed consent. throughout the meeting. Not only was the atmosphere friendly and relaxed, participants said they felt free to The faculty included well-known endourologists from ask and convey their point of view. all over Europe such as Olivier Traxer (Paris, FR), Thomas Knoll (Sindelfingen, DE), Alberto Breda Overall, we had a very positive and successful (Barcelona, ES), Palle Osther (Fredericia, DK), Technology and Training in Endourology Course, and Fernando Gomez Sancha (Madrid, ES) as well as we believe that all the participants -- both young and Italian experts Antonio Frattini, Guido Giusti, Agostino veteran urologists- experts) were not only satisfied Meneghini, Emanuele Montanari and many others. with the sharing of knowledge and experience, but All the invited speakers gave original presentations also benefitted from the new ideas that will inspire which elicited insightful comments. The discussion them to face the challenges in endourology. March/May 2013 Remembering Arthur Barth (1858-1927) Towering achievements of a modest man Dr. Thaddaeus Zajaczkowski Member History Office Muelheim an der Ruhr (DE) th.zajaczkowski@ gmx.de In those days, it was an object of modernity, made up of 16 pavilions. The complex also included the offices of the hospital administration, accounts department, mortuary, operating suites, nurses’ home, boilerroom, and accommodation for doctors, office workers and staff. The entire complex consists of 26 buildings and occupies an area of 157,572 m2, when it was handed over for use in 1911 (Figure 1). After World War I, in 1921, a start was made to gradually expand the hospital. In response to the enormous demand, a 200-bed Skin and Venereal Prof. Arthur Barth, the first director of the Diseases Department was constructed. In 1927 the Department of Surgery at the then newly-erected Institute of Radiodiagnostics and Radiotherapy Municipal Hospital in Danzig, died 86 years ago on Therapy was established, and in 1933, in addition to May 7, 1927 in Schwerin, Germany. the Central Laboratory, an Orthopaedic and Rehabilitation Department was opened in the Surgical Prof. Barth was a distinguished surgeon. From 1896 Unit. In 1934, the Municipal Hospital had rooms for to 1911 he worked as Senior Registrar in the surgical 1,160 patients, including 320 beds for surgical department of the “old” municipal hospital, while patients. from 1911 until 1924 he was Director of Clinical Surgery In the centre of this complex stood the two-storey in the newly-built Municipal Hospital. He primarily operating block. On the upper floor there was a small focused on surgery of the genitourinary system. operating theatre and preparation room, together with a septic procedure room and preparation room. The beginning of the hospital service in Gdansk (Danzig) is closely connected with the arrival of the During the inter-war period the facility was the most Teutonic Knights in 1308. The earliest institution to be advanced institution in the Northern Province of mentioned in historical records is the Hospital of the Prussia. Doctors employed there, for the most part Holy Ghost in Gdansk, built in 1310-1311. Run by the high-level specialists, used to go abroad to perform Knights Hospitaller until 1382, it was primarily operations and give lectures. reserved for the treatment of sick pilgrims, travellers, and paupers. The passing of the centuries saw the As the long-serving director of the surgical gradual development of Danzig’s hospital service. department in the old municipal hospital (1896-1911), Prof. Arthur Barth contributed enormously to the Danzig’s surgical traditions date back to the 15th building and development of the – in those days century, when the earliest hospitals were run as – modern buildings and surgical facilities. His vast poorhouses or shelters for the homeless. The first surgical experience, gained at modern hospitals in hospitals that could be compared to the hospitals of other German cities was exploited for this purpose. today were created at the turn of the 15th and 16th At the same time, adapting building plans to local centuries in the area around present-day Dyrekcyjna conditions helped create a practical and modern, Street (Am Olivaer Tor). Initially, it housed smallpox hospital complex. patients, which is why it was called a smallpox house In 1935, based around the Municipal Hospital and the or lazaretto. It became the actual Municipal Hospital in the 17th century. At that time it had 15 wards and an other hospitals of the free City of Danzig, the Academy operating room. In 1755 it acquired its own pharmacy. of Practical Medicine was opened, which in 1940 was transformed into a full medical academy, its name later changed to Medizinische Akademie Danzig (MAD). In the 19th century, the Municipal Hospital treated between 600 and 700 patients annually. It served the Early years city until 1911, when a modern municipal hospital Barth was born on 20 February 1858 in Untergreißlau, complex came into use in April of that year, later to become a centre of academic service. It was not until near Weißenfels (state (district) of Saxony-Anhalt). His father was a long-serving general practitioner in the 19th century, with the city’s growing population, Naumburg. After selling his practice, he took up scientific development and medical advances that farming on his family estate. It was there, too, that three modern hospitals were built in Danzig: the Arthur spent his carefree childhood years. He received Hospital of Obstetrics and Gynaecology (1819), the his primary education at home. His teachers were his Holy Virgin Hospital (1852), and the Evangelical governess, a primary school teacher, and his father. Hospital run by the Deaconess Sisters (1857). Later, from 1868 to 1870, he attended secondary school in Weisßenfels. In 1877 he completed the Danzig’s new Municipal Hospital complex From 1907 to 1911 a new, 850-bed Municipal Hospital seven-year course of studies at the elite National School in Pforta. (Figure 2) was erected, and was officially opened in April 1911. The facility was handed over for use, complete with its administrative, financial and technical services. In the early days, the surgical department and the department of internal medicine formed the core of the new hospital complex. The hospital was fully capable of meeting the modern healthcare requirements of those times. Located at Danzig-Langfuhr, Delbrückallee (now GdanskWrzeszcz, Debinki), it had excellent connections with the rest of the city and was easily accessible to patients and their families. Fig. 1: Scheme of the Municipal Hospital in Danzig EAU History office March/May 2013 clinic of the Augusta Hospital in Berlin (under Prof. Ernst Küster, 1839-1930). From 1 May 1884 until 1 September 1885 he worked as an assistant in the Department of Surgery at the Municipal Hospital in Danzig (the Senior Registrar was Dr. Georg Wilhelm Braun, 1836-1895). From 1885 to 1890 he was an assistant in the Department of Surgery at Augusta Hospital in Berlin. When Prof. Küster was appointed Director of the Surgical Clinic at the University of Marburg, Barth soon followed his former Chief, and on 1 November 1890 he started work as principal assistant in the Surgical Clinic at Marburg, becoming Deputy Head of Department in 1891. In 1892, he qualified as Assistant Lecturer on the strength of his paper titled “On histological changes occurring during the treatment of renal lesions, and behaviour of the renal parenchyma.” His experimental-clinical dissertation based on his activities at the University of Marburg, concerned the assessment of treatments for kidney lesions (1892). In 1896 he was appointed Associate Professor. Chief of the surgery department In 1896, Barth took over from Dr Wilhelm Baum as director of the “old” Gdansk Municipal Hospital in Zaspa (Sandgrube). Barth was largely instrumental in the creation and development of the Municipal Hospital Complex in Danzig. Among the distinguished names involved in the establishment and development of the modern Municipal Hospital in Danzig was its first director, surgeon, academic and author, Prof. Barth. He was an outstanding specialist in osteoarticular surgery and maxillary surgery as well as of the abdominal cavity and urology, but his primary speciality was renal surgery. He played a significant part in the planning and execution of the modern Municipal Hospital complex in Danzig. Construction began in 1907 and was completed in 1911. Barth became director of the Surgical Clinic in the newly-built municipal hospital (Figure 3). His academic works touched upon many areas of surgery. Barth’s Magdeburg days, in the closing decade of the 19th century, produced some of his most highly appreciated research studies of global significance, among other things about the artificial production of bone tissue grafts in cases of joint degeneration and bone transplantation. Like many surgeons at a time when new departments were moving away from surgical medicine, Barth carried out urological operations and published more than 30 outstanding works in urology. Of special significance were his publications on subjects as diverse as the treatment of renal lesions (doctoral thesis), renal section, purulent kidney disease, horseshoe kidneys, hypertrophy and atrophy of the prostate gland, renal tuberculosis, renal abscesses and urolithiasis, as well as his many publications relating to other systems and disorders. These include inflammation of the pancreas, gastric and duodenal ulcers, cancer of the larynx, inflammation of the paranasal sinuses, and neoplasmas of the oral cavity. His activities as a surgeon were valued not just in Danzig; his fame extended beyond West Prussia, and as far as Pomerania. As a long-serving, versatile professor of surgery he made a significant contribution to the development of modern surgery. He took part in World War I on Polish territory and in France as Surgeon-General and as a consultant and surgeon to the 17th Army Corps. He received the Iron Cross 2nd Class and 1st Class, and in 1916 he was awarded the noble title of “Secret Medical Adviser” (Geheimen Medizinal-Rath). Co-founder of the German Urological Society Barth was a member of the German Society of Surgeons (DGCH), and regularly attended their congresses. He delivered many papers and was a lively participant in discussions. He was also co-founder of the German Urological Society (DGU) in 1907. In 1909, at the 2nd DGU Congress in Berlin, he delivered the supplementary paper entitled: “Suppurative, non-tubercular inflammation of the kidneys,”. He also took part in conventions organised by the German Urological Society, personally delivering urological papers. His assistants were equally enthusiastic participants at German urological congresses. In 1911, at the 3rd DGU Congress in Vienna, Barth was elected fellow of the German Urological Society. Fig. 3: Prof. Arthur Barth, in Danzig Barth travelled abroad, presenting papers on various surgical and urological topics. He was a very busy clinician and academic and published dozens of clinical research studies and countless case reports. Some of his published works were – and still are to this day – often cited in Germany as well as in world literature. Final years In 1924, Barth fell victim to influenza, which was complicated by inflammation of the heart muscle. On 1 November 1924, after spending 30 years of his life in Danzig, at his own request, he was retired from and went to live in Schwerin. There, he was active in the local Medical Association and devoted his time to writing, including writing an autobiography. He died on 7 May 1927 in Schwerin. In accordance with his last wishes, he was buried in Danzig in the He was proud of his family – his wife Charlotte, the cemetery next to the Municipal Hospital, in the daughter of Senator Friedrich Nebelthau from Bremen Delbrückallee (now, Debinki Street). Today, the and his five handsome and successful children. cemetery no longer exists. Pioneering director His years in Danzig as hospital head were for Prof. Barth the crowning achievement in his busy life. He recorded successes in every area of his professional career: academic, administrative, as well as social. He was also both valued and respected as a top-class surgeon by his many patients of every social standing in Danzig and surrounding areas. With the outbreak of World War I, his once harmonious family life came quickly to an end. His two sons were drafted into the army and sent off to Fig. 2: Barth as a pupil at the classical secondary school the front. His wife fell ill, while his son Helmut was killed in battle. The war found him, too, serving at the front, where he was forced to serve as a consultant He then went on to study medicine in the medical surgeon, employed by the German High Command. departments at Jena, Marburg, and Berlin. He The loss of the war and its consequences for completed his medical studies in 1882 in Jena. That Germany, as well as worries and concerns for the same year he received his doctorate at Jena on the future, took a toll on his health. In 1924, heart strength of his dissertation titled: “On the relationship troubles, myocardial damage following influenza with between the diameter of pelvic narrowing and the pelvic complications, finally forced him to abandon his inlet”. He completed a one-year obstetrics course at career as a surgeon. the Institute of Obstetrics in Dresden and Vienna. Scientific activity Surgical training Barth was an outstanding specialist in full surgery He gained his specialisation and surgical experience and had dozens of published works to his name on in countless departments and clinics across Germany, that subject. He was primarily concerned with surgery always under the guidance of eminent surgeons. In of the genitourinary system, particularly renal and 1883-1884 he worked as a volunteer in the surgical prostate surgery. In 1928, Prof. Alexander von Lichtenberg in his welcome address to the 8th Congress of the German Urological Society in Berlin had this to say about Barth’s death: “Prof. Arthur Barth, Surgical Senior Registrar in Danzig, died at the age of 70. He was a man whose brilliant work inspired many to take up renal surgery”. Arthur Barth was a man with many positive characteristics: irreproachable character, a love for everything of beauty, simplicity and humility, and a dislike for showing off. He never put himself on a pedestal. The words “he always proved himself a greater man than he pretended to be” suit him perfectly. This could be the reason why, despite his many and great professional achievements in such historically difficult times – Word War I and revolution – his name has remained largely unknown. Or was it, perhaps, because at that time Danzig was not an academic centre of medicine? European Urology Today 25 Book reviews Prof. Paul Meria Section Editor Paris (FR) paul.meria@ sls.aphp.fr Active Surveillance for Localized Prostate Cancer PSA-based prostate cancer detection led to a significant increase of incidence during the past 20 years. Consequently, many indolent cancers were discovered, with some of the cases being considered as “overdiagnosed.” Publication Edition Binding Pages Illustrations Price Website : Nov. 2012 : 1st : Hard cover : 208 : 33, 22 in colour : 148,35 euro : www.springer.com Klein and Jones, with the support of 50 experts, wrote an updated and expanded third version of their excellent textbook. They added new chapters and dealt with some controversial aspects and new concepts in diagnosis and treatment. European and Canadian experiences of AS were presented and the authors pointed out their encouraging results and the need to perform further studies for refining patient’s selection for AS. Diet, physical activity and their potential benefits were also considered such as the psycho-social aspects of patients submitted to AS. The authors concluded with an economical study demonstrating a reduction of costly treatments in patients undergoing AS and, looking to the future, considered AS as the next standard for patients with low-risk prostate cancer. This excellent overview dedicated to AS fills a lack in the literature. We can agree with the authors who consider AS as the future standard for selected patients. For these reasons this textbook can be recommended to all physicians involved in prostate cancer management. Editor ISBN E-book Publisher : L. Klotz : 978-1-61779-911-2 : 978-1-61779-912-9 : Humana Press Book reviews 26 European Urology Today Handbook of Clinical Gender Medicine Gender medicine encompasses sex differences, either genetic-biological or phenotypic, but goes beyond these to include the broader social, cultural and normative factors that affect health. Male and female reproductive systems are different but the concept of gender medicine considers the notion that no differences exist in terms of social and biological determinants related to health and disease. Gender is a social science, since sex is a biological one. The concept of gender medicine was developed at Karolinska Institute, in Stockholm, Sweden, 12 years ago. An international working group was created in 2008 and obtained funding from Pfizer Inc. to support the development of the book, which aims to change the vision of the medical approach of gender medicine. The introduction dealt with general considerations about gender matters, followed by a section addressing social and biological determinants in health and disease. One chapter of this section focused on ambiguous genitalia, a difficult paediatric problem. Prostate cancer remains the most important topic in urology based on the high number of annual publications. Indeed, many advances were observed during the past 10 years and a timely update remains useful for all practitioners. Hereditary cancers were described in detail, including predisposing genetic factors. Recent and substantial progresses were made in this field and the authors The corollary was frequently a case of reviewed various loci involved in prostate cancer “overtreatment,” with functional consequences for the development and aggressiveness. The relation patients and financial implication for medical care between cancer and chronic prostate inflammation organisations. The concept of active surveillance (AS) was discussed in a well-documented chapter. was developed by Klotz, with the aim of limiting the risk of overtreatment in patients with low-risk cancers, while providing timely radical treatment for those requiring it. Currently, this concept is supported by an increasing number of urologists. The key or crucial role of AS is its function to revise the strategy in case of cancer aggressiveness, and the authors focused on various triggers for radical treatment; the role of multiparametric MRI in diagnosis and monitoring was clearly demonstrated, although the frequency of imaging remains unclear. A special technique for PSA kinetics assessment was also described, allowing rational decision-making. Men’s health is a relatively recent topic strongly related to urology. Actually, most urologists are already involved in the management of specific problems that impact on men’s quality of life such as erectile disorders, ageing, lower urinary tract symptoms or infectious diseases. Management of Prostate Cancer Epidemiology and risk factors were described in a comprehensive introductory chapter, followed by an update on PSA and its current use. Future prospects on blood and urinary biomarkers were described, some of them either already available or still undergoing further assessment. The rationale and clinical implications of screening were described and some recommendations were given for clinical practise. Klotz and about 30 co-authors provided in this textbook a comprehensive amount of updated information about AS. After a recap on the issue of “overdiagnosis” and “overtreatment,” the authors focused on the selection of patients suitable for AS, since the challenge remains on how to provide a reliable distinction between significant and insignificant cancers (the so-called ‘tigers and pussycats,’ as described by Boccon Gibod in a 1996 editorial article). The authors also described tissue and serum biomarkers and their role in predicting high-risk disease. Urological Men’s Health Editor Shoskes and more than 30 co-authors aimed to write a textbook covering the bothersome aspects of urological conditions and their consequences on men’s health. The opening chapter dealt with preventive health evaluation in men, and examined general points and non-urologic problems such as diabetes, hypertension or immunisations. Specific chapters covered various topics, focusing on urogenital disorders. Erectile dysfunction was described, including the physiologic and practical aspects in the assessment of endothelial function. Peyronie’s disease was also described such as the surgical management of erectile dysfunction. The controversies on prostate cancer screening were discussed, focusing on PSA test and its current usefulness. Chronic pelvic pain syndrome and recurrent urinary tract infections, two conditions that seriously impair quality of life, were described in depth, including the practical aspects of their management. The following chapters were dedicated to various medical specialities, including neurology, pain management, cardiology and related topics, cancer, rheumatisms and musculoskeletal conditions, metabolic diseases and transsexualism. A short section was dedicated to urology and dealt with lower urinary tract symptoms and BPH, sexual dysfunction in men and women, and chronic kidney diseases. Peculiar aspects of geriatrics were discussed in the final section, which was dedicated to the social and biological determinants of health in ageing people. Undoubtedly, this original and unique textbook collected a considerable amount of information in a recently developed topic. It opens a new perspective in the approach of biology and gender understanding and serves as a guide for clinical work in various medical specialities. BPH and lower urinary tract symptoms, which represent more than a third of consultations in urology, were taken up including the medical and surgical aspects, as well as overactive bladder and urinary incontinence. The hormonal problems related to male ageing were also described, with a chapter focused on localised prostate cancer. Other problems such as chronic pain and psychosocial factors were discussed in the final chapters. This textbook provides the reader with an original and useful approach to men’s health and will be of interest to many physicians, whether they are urologists or general practitioners. The role of hormones and obesity in prostate cancer development were described and the authors focused on chemoprevention based on dietary factors and 5 alpha-reductase inhibitors. Editor ISBN E-book Publisher Publication The authors pointed out the importance of prostate Edition biopsy procedures and described various techniques Binding and their respective indications. Clinical nomogrammes Pages were considered in a special chapter, including Illustrations descriptions of their usefulness and current limits. Price Website A richly illustrated and comprehensive chapter was dedicated to the pathologic evaluation of prostate cancer specimens. A substantial part of the book dealt with the treatments of localised, locally advanced and metastatic disease. The new concepts, such as active surveillance, were discussed, although there are still some remaining concerns on this topic. A chapter focused on the management of postoperative incontinence. The aspects of castration-resistant cancers were considered, including secondary hormonal therapies, cytotoxic therapies and new developments available in the future. This textbook presents an inclusive coverage of practical information and can be recommended for all urologists and oncologists, either certified or still in training. Editors ISBN E-book Publisher Publication Edition Binding Pages Illustrations Price Website : E. Klein, J.S. Jones : 978-1-60761-258-2 : 978-1-60761-259-9 : Humana Press : Nov. 2012 : 3rd : Hard cover : 428 : 37, 11 in colour : 158,95 euro : www.springer.com Editors ISBN E-book Publisher Publication Edition Binding Pages Illustrations Price Website : D.A. Shokes : 978-1-61779-899-3 : 978-1-61779-900-6 : Humana Press : 2012 : 1st : Hard cover : 215 : 38, 25 in colour : 148,35 euro : www.springer.com : K. Schenck-Gustafsson, P.R. DeCola, D. Pfaff, D.S. Pisetsky : 978-3-8055-9929-0 : 987-3-8055-9930-6 : S. Karger : 2012 : 1st : Soft cover : 522 : 62 fig., 4 in colour, 63 tables : 51,00 euro : www.karger.com Make fewer passes, use fewer products, and reduce costs. Flexor Parallel ® ™ R A P I D R E L E A S E ™ U R E T E R A L A C C E S S S H E AT H MEDICAL www.cookmedical.com © COOK 2012 URO-BEMEAADV-FLPEUT1-EN-201212 March/May 2013 21st Meeting of the EAU Section of Urological Research (ESUR) EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations For more information please contact Congress Consultants at [email protected] or go to http://esur.uroweb.org 25-27 September 2013, Dresden, Germany In collaboration with the 65th Congress of the DGU (Deutschen Gesellschaft für Urologie e.V.) ESUR Board Tentative Scientific Programme Wednesday, 25 September 2013 ESUR Opening Systemic therapy in metastatic RCC: Delay, start, stop? A. Schrader, Ulm (DE) Friday 27 September 2013 ESUR/DGU Forum: Significant prostate cancer Prof. Z. Culig, ESUR Chairman Prof. K. Junker, Meeting President Mechanisms of resistance: What is different? Role of the immune system in urology Chemoresistance in urological tumours Lectures by: Lectures by: Oral session Oral session ESUR poster session ESUR/DGU poster session Poster session ESUR/DGU Opening DGU/ESUR ESUR/DGU Forum: Perspectives in advanced bladder carcinoma: From bedside to bench (ESUR/DGU) Hot topics in urological pathology Extended lymph node dissection in bladder cancer: Do we have evidence for therapeutic benefit? A. Hartmann, Regensburg (DE) H. Moch, Zurich (CH) G. Van Leenders, Rotterdam (NL) T. Blankenstein, Berlin (DE) A. Griffioen, Amsterdam (NL) E. Nossner, Munich (DE) Thursday, 26 September 2013 ESUR/DGU Forum: Renal cell carcinoma: Clinical controversies and scientific perspectives (ESUR) Should preoperative biopsy become mandatory for all renal tumours <3cm? T. Steiner, Erfurt (DE) Biomarkers for individual diagnostics and therapy: What is possible today? E. Oosterwijk, Nijmegen (NL) R. Pili, Buffalo (US) Rising PSA under hormonal treatment in M0 disease – treat or wait? B. Wullich, Erlangen (DE) Sequence therapy for advanced prostate cancer O. Cuvillier, Toulouse (FR) B. Mellado, Barcelona (ES) M. Puhr, Innsbruck (AT) K. Miller, Berlin (DE) Translation of scientific advancement into new therapies for prostate cancer H. Leung, Glasgow (GB) J. Lehman, Kiel (DE) J. Gschwend, Munich (DE) Mechanisms of therapy resistance Lectures by: Oral session J. Catto, Sheffield (GB) Pooled retrospective cystectomy series – reliable source for evidence based medicine? Z. Culig, Innsbruck (AT) - Chairman Y. Allory, Creteil (FR) A. Bjartell, Malmö (SE) G. Jenster, Rotterdam (NL) K. Junker, Homburg (DE) M. Knowles, Leeds (GB) M. Mancini, Padova (IT) Faculty T. Blankenstein, Berlin (DE) M. Brausi, Modena (IT) J. Catto, Sheffield (GB) O. Cuvillier, Toulouse (FR) A. Griffioen, Amsterdam (NL) J. Gschwend, Munich (DE) A. Hartmann, Regensburg (DE) J. Lehman, Kiel (DE) H. Leung, Glasgow (GB) B. Mellado, Barcelona (ES) K. Miller, Berlin (DE) H. Moch, Zurich (CH) E. Nossner, Munich (DE) C-H. Ohlmann, Homburg/Saar (DE) E. Oosterwijk, Nijmegen (NL) R. Pili, Buffalo (US) M. Puhr, Innsbruck (AT) J. Rahnenfuhrer, Dortmund (DE) A. Schrader, Ulm (DE) T. Steiner, Erfurt (DE) G. Van Leenders, Rotterdam (NL) A. Vlahou, Athens (GR) B. Wullich, Erlangen (DE) C-H. Ohlmann, Homburg/Saar (DE) J. Rahnenfuhrer, Dortmund (DE) ESOU lecture: Future therapeutic options in advanced bladder cancer M. Brausi, Modena (IT) Lecture by: A. Vlahou, Athens (GR) ESUR poster session European Association of Urology 2nd EULIS Meeting: Towards personalised management Prof. P. Osther: “Treatment of urolithiasis is challenging, unique and rewarding at the same time” On 5-7 September 2013, the EAU Section of Urolithiasis (EULIS) will convene for the second time at their dedicated meeting, this time in Copenhagen, Denmark. After their successful pilot in 2011, the section is compiling a very intensive and interactive programme, featuring sessions of various formats. The EULIS chairman, Prof. Palle Osther, answered several questions about the upcoming meeting and the most pressing developments in the field of urinary stones. Palle Osther: Previously most of our knowledge on the pathophysiology of stone formation was based on whole urine studies, and saturation theories were the talk-of-the-town. Recent research looks more at the initial steps of stone formation as a microenvironmental process occurring in different parts of the nephron, and at the meeting urinary saturation controversially will be discussed as casual or causal in stone disease in a pro-and-con debate. What has changed in the field of urolithiasis since the last EULIS meeting? Which new developments will be addressed this time? Furthermore, shifting trends in the endourological management of large renal stones will be undoubtedly heavily debated – PCNL versus flexible ureteroscopy, conventional PCNL versus mini-PCNL, micro-PCNL, ultra-mini PCNL. At present these minimal invasive therapies are fighting to prove their eligibility. Palle Osther: The incidence and prevalence of urolithiasis are steadily increasing throughout Europe. In the last ten years stone prevalence has increased by 30% in industrialised countries. At EULIS, we strongly believe that increasing awareness of the kidney stone disease is needed both from the perspective of the doctors and the society in order to provide the best care to this huge population of patients. This was also reflected in the recent EAU Patient Information initiative launched with materials on kidney and ureteral stones. At the 2013 edition of the EULIS meeting in Copenhagen, we will focus on trends in the field of stone disease, both with regard to its epidemiological aspects, basic research and pathophysiology as well as medical and surgical management. Surely, I am looking forward to some very interesting and inspiring debates. These different modalities also will be addressed in live-surgery sessions, and I am sure this will add to our common knowledge database on tips-and-tricks in everyday stone management. The programme includes a large section on stents and the role of metal in stents – this is a very specialist topic, how can it be of use and interest to practising urologists? Palle Osther: That’s right. The meeting will include a pre-congress workshop on ureteral stenting. Recently, For instance, we will debate why ureteroscopic much debate has been on when to stent and when management in some areas of Europe is now the not to stent. On one hand the possibility to use stents dominant treatment scenario, whereas in others SWL has been revolutionised and is now a vital part of is still preferred for the majority of patients. modern endourology. On the other hand, these stents Furthermore, new knowledge on the role of Randall’s may have undesirable side-effects, such as irritative plaques on the pathogenesis of calcium bladder symptoms and sexual dysfunction, which nephrolithiasis and the link between the metabolic means that the decision of placing a stent should be syndrome and uric acid and calcium nephrolithiasis based on specific indications rather than as a routine will be discussed intensively. Hopefully this will add to procedure. our knowledge in order to provide better means for preventing stone formation. Different stents have been manufactured to overcome potential side-effects, including metal stents. The Which topics, do you expect to raise a lot of discussion– workshop will deal with overall stent issues such as why? How are they dealt with within the programme? indications for stent placement, durability and March/May 2013 problems with incrustations as well the role of metal stenting. format of the session with the topics that need to be covered? Also the workshop will include live stent insertions transmitted from the OR of Rigshospitalet in Copenhagen. In this way the participants will get both state-of-the-art scientific knowledge on stents in urology as well as tips and tricks regarding placement procedures of the different stents and on how to deal with complications. Palle Osther: At an international meeting on stone disease a huge format of scientific and educational activities are mandatory. That is why we will have a large variety of sessions, including state-of-art lectures, pro-and-con debates, poster-sessions, hands-on-training courses and live surgery sessions. Only in this way we will be able to appropriately confront the complexity of basic research and practical clinical management of the great varieties of stone diseases. At the meeting workshops on SWL, URS, PCNL as well as medical and dietary management of kidney stones will be offered as well. World-renowned experts from both Europe and overseas will be conducting these workshops, and the participants will have the opportunity to meet urologists who have become legends for their outstanding work in urolithiasis. Stones are different – urinary tracts are different – patients are different. The variability of stone disease is tremendous. That is what makes treatment of urolithiasis so challenging, unique and rewarding at the same time. There is also going to be a discussion on how to train an academic stone doctor – why is this discussion relevant The strategy on how to manage stone disease should and what do you expect to draw from it? be based on a thorough individual assessment including history, stone burden, composition and Palle Osther: At our EULIS workshops all around the structure, metabolic abnormalities, anatomy of world throughout the years we have seen different collecting system and the patient in general, patient’s health care systems with different standards with physical condition and co-morbidity, patient’s mental regard to offered treatment modalities as well as and social conditions, kidney function, bleeding training possibilities. These events have created a disorders and medication, symptoms and last but not global fruitful and friendly atmosphere in the least patient’s expectations and preferences. Also, the urolithiasis community – we are so to speak sisters physician’s preferences, his or her skills and and brothers in stone. possibilities affect treatment decision. This very open forum allows us to take what is best from different areas of the world, and gives us an optimal basis for discussions on how to train an academic stone doctor. These ties enable us to take into consideration the best available knowledge and local treatment opportunities, thereby creating the foundation of evidence-based medicine in the stone field - tracking down the best external evidence with which to answer our clinical questions. I strongly believe that this meeting, with all its formats will help up on our way towards personalised management of urolithiasis, which is the only way to go. The event will certainly achieve what it set out to do, help the participants to ‘bridge the gap between basic science and clinical practice in urolithiasis’. There is a large variety of formats at the meeting – from workshops and state-of-the art lectures, to live surgery and hands-on training sessions. How do you match the Visit the official website of the EULIS meeting for more information and to register: http://eulis2013.uroweb.org Abstract submission for 2nd EULIS is now open and will close on 6 May 2013. European Urology Today 27 Canadian Urological Association (CUA) Canadian Tour 2012 Academic Exchange Programme CUA-EAU Academic Exchange Programme: sharing insights and best practices Dr. A. Erdem Canda, Dr. Roman Sosnowski, Dr. Peter Nyiradi, Prof. Rolf Ackermann Patients sometimes would travel up to two days or more to receive specialised care. Thus, the Internetbased ‘TeleHealth Alberta’ is a dynamic communications system allowing multi-media interactions between a local health facility located somewhere and the physician based in central Edmonton. The system enables the exchange of crucial information regarding the patients’ health condition and complaints, including the option for a video transmission of the attending physician’s examination, such as showing the malformation of external genitalia as demonstrated in a recent case. The Canadian Urological Association (CUA) European Association of Urology (EAU) Academic Exchange Programme offered the opportunity to four European urologists to visit leading urology institutions in Canada and examine the best practices of these institutions. We earlier reported on the visits to Halifax and Montreal (EUT issue Aug. 2012) and Toronto and Vancouver (EUT issue Oct. 2012). The tour, which further brought the participants to Calgary, Edmonton and Banff, also allowed both European visitors and their Canadian hosts to exchange insights on the clinical challenges they encounter in everyday clinical practice. The following article provides details of the third part of the tour: Calgary The exciting invitation by Drs. Bryce Weber, Stephen Pautler and Walid Farhat to participate in the 5th Annual Course on Basic and Advanced Urology Laparoscopic Skills in Calgary enabled us to get practical skills in dry and wet lab training at the Clinical Skills Building of the Faculty of Veterinary Medicine. Photo 4: Wet lab, Laparoscopic Urology Course, Calgary. Picture 10: Prof. Ackermann’s speech during CUA Meeting in During a tour conducted by Prof. Ronald Moore of the Banff, Canada. multidisciplinary research facilities, we realised that the Medical Faculty and the Department of Urology at the University of Alberta in Edmonton also pursue a structure which allows uncomplicated interactions among medical scientists from various disciplines. Prof. Moore also briefed us on the exciting aspects of his investigations in photodynamic research. A sightseeing tour of the University of Alberta’s extensive campus grounds gave us a view of many impressive new buildings. Later in the day, CUA president Prof. Chetner invited us to a wonderful dinner at the Royal Mayfair Golf Club by Prof. Chetner, together with the members of the department (Photo 7). Photo 5: Downtown, City of Calgary. Picture 11: Dr. Canda’s presentation during the Pediatric Urology Meeting in Banff. we enjoyed a short tour of Calgary’s downtown area, where we saw iconic places and districts that reminded us that the city hosted the 1988 Olympic Winter Games (Photo 5). Photo 1: Dry lab, Laparoscopic Urology Course, Calgary. We very much enjoyed this special opportunity of a practical training provided by our Canadian colleagues and supported by highly skilled laparoscopic urologists. The course consisted of three parts. The first included lectures with attractive video presentations of laparoscopic and robotic procedures, while in the second part we had the chance to exercise our skills using training boxes and simulators in a dry lab (Photo 1). But the most important and even more exciting part of the course consisted of the hands-on training in the wet lab (Photos 2-4). We performed laparoscopic partial nephrectomy, pyeloplasty and nephrectomy using the latest devices, instruments and haemostatic materials under the enthusiastic guidance of the instructors (Photos 2-4). Edmonton Arriving in Edmonton on a sunny Sunday afternoon, we all felt that we would need some physical exercise in order to prepare for another full clinical and scientific programme scheduled the following day. A bicycle ride along the beautiful North Sascatchuan River was certainly the right activity since it gave us the first impressions of Edmonton. Dr. Niels Jacobson welcomed us at the University of Alberta Hospital and guided us right into the operating room where we watched him perform a robotic assisted radical prostatectomy, a procedure he executed with a high level of competence. Following the surgery, we had a meeting with Dr. Peter Metcalfe, a paediatric urologist and third-generation member of a very prominent family of urologists who played a key role in developing the department (Photo 6). We also learned from Metcalfe that paediatric urology is further boosting its research activities despite the clinical challenges they face. collaboration between Canadian and European urologists could be further intensified through multi-institutional studies (Photo 11). Picture 8: Dr. Howard Evans behind performing a case of laparoscopic radical nephrectomy, Department of Urology, The University of Alberta. The next day’s case presentations and tour of the outpatient facilities were followed by observing an open radical cystectomy and subsequent urinary diversion with ileal conduit. Later that day, we also observed a case of laparoscopic radical nephrectomy (Photo 8) and had the chance to visit the operating rooms and the clinics at the Grey Nuns Community Hospital (Photo 9). Moreover, the course demonstrated the efforts of Canadian urologists to further advance their already high-level of competence. Despite a tight programme Picture 12: Presentation of glass sculptures engraved with dates of our visit given by Prof. Michael Chetner, President of the CUA, Banff. Picture 9: Dr. Keith Rourke, visiting the operating room at the Grey Nuns Community Hospital, Edmonton. Picture 6: Dr. Peter Metcalfe, Divison of Pediatric Urology, The University of Alberta. Photo 2: Wet lab, Laparoscopic Urology Course, Calgary. Photo 3: Wet lab, Laparoscopic Urology Course, Calgary. 28 European Urology Today At CUA’s Annual Banquet, we did not only expressed our sincere gratitude to our hosts but also took the opportunity to present to our hosts, and on behalf of the EAU, commemorative plates to mark this exceptional exchange programme. We also received from CUA president Prof. Chetner glass sculptures engraved with the dates of our visit (Photo 12). During the banquet Prof. Yves Fradet from Montreal received the prestigious Award of The Canadian Urological Association, with Prof. Lawrence Klotz giving an impressive and very elegant introduction of Prof. Fradet and his carreer. Metcalfe also showed how big the area is which covers the Yukon, the Northwest Territories and the Hudson Bay, with its small population, and where no local specialised medical services are available. Picture 7: Dinner with the Faculty, Department of Urology, The University of Alberta. The full and insighful programme carefully prepared by our Edmonton hosts gave us a true and realistic insight into the comprehensive scope of their activities. They made our stay in Edmonton not only highly informative but also socially fulfilling. An invitation by Prof. Gerald Todd, department chairman, to the Faculty Club of the University of Alberta was another highlight of the visit, and showed the hospitality of our hosts. We left Edmonton with fond memories, thankful for the friendliness we have experienced. Banff In Banff, our last destination, we attended the 67th Annual Meeting of the Canadian Urological Association. Prof. Rolf Ackermann, our senior mentor, spoke during this year’s annual conference of the Canadian Urological Society at Banff Springs Conference Center (Photo 10). Dr. Canda participated at the Pediatric Urologists of Canada (PUC) that was held during the annual CUA conference. He presented a research project where he noted how the The Banff meeting also gave us many opportunities to again meet our Canadian urological colleagues who hosted us during our visits at the Academic Urological Institutions and Departments in Halifax, Montreal, Toronto, Vancouver, Edmonton and Calgary. Our thanks to all contributors from the CUA and the EAU for giving us this excellent opportunity. And to Dr. Keith Rourke of the Division of Urology, University of Alberta who took us to Lake Louise, one of Banff’s beautiful locations (Photo 13). Picture 13: Visit to Lake Louise with Dr. Keith Rourke, Edmonton. March/May 2013 ESUT’s dynamic presence in Milan Well-attended live surgery sessions attest to quality content Dr. Ioannis Georgiopoulos Fellow in Endourology Dept. of Urology University of Patras Patras (GR) [email protected] Associate Prof. Evangelos Liatsikos Section Editor ESUT Patras (GR) [email protected] The EAU Section of Uro-Technology (ESUT) conveyed a remarkable impression at 28th Annual EAU Congress in Milan, by hosting a series of live surgeries, hands-on-courses and presentations. By showcasing the latest advances in urological technology, ESUT’s aim was to highlight groundbreaking surgical innovations in European urology. For more than a decade, ESUT-sponsored live surgeries have been among the most attended sessions of the annual congress. Jointly organised with EULIS (EAU Section of Urolithiasis) and ERUS (EAU Section of Robotic Surgery in Urology), this year’s “What is new in endourology, laparoscopy and robotics” session, held on Saturday, April 16, was once again very popular. performed an innovative LESS robotic pyeloplasty, while Prof. Stolzenburg demonstrated the use of 3D technology in retroperitoneal laparoscopic partial nephrectomy. Meanwhile, Prof. Tunc (Ankara, TR) performed an extremely rapid laparoscopic nephrectomy with a direct upper pole access technique, which was followed by the standard technique for robotic partial nephrectomy expertly demonstrated by Prof. A. Mottrie. Advanced stone surgery techniques were then highlighted, with Prof. Traxer demonstrating his flexible ureteroscopic management of stones in caliceal diverticula and Dr. Breda and Giusti collaborating to perform supine PCNL and flexible ureteroscopy. Finally, a pre-recorded video of a laparoscopic pudendal nerve decompression performed by Prof. Erdogru of Istanbul was screened. Moderated sessions The second session moderated by Professors Artibani, Dasgupta, Laguna and Skolarikos began with a difficult robotic radical prostatectomy case performed by Prof. Wiklund in a patient with advanced disease. Professors Alcaraz and Ribal (Barcelona, ES) then showed the possibility of NOTES nephrectomy using 3D vision through a flexible transvaginal camera. This was followed by Greenlight PVP surgery performed by Professors Bachmann (Basel, CH) and Tubaro (Rome, IT). Prof. Piechaud then presented the technique for extended robotic lymphadenectomy in prostate cancer. The session moved on to innovations in bladder imaging, with a presentation of Narrow Band Imaging (NBI) and Photo Dynamic Diagnosis (PDD) through digital cystoscopy by Prof. Malavaud (Toulouse, FR). A novel imaging, SPIES (Storz Professional Image Enhancement System), which provides higher detail through modification of color contrast was showcased by Prof. Lapini, in combination with PDD for a bipolar-resection of bladder tumours. Hands-on laparoscopy course These courses are always very popular and, since space is limited, are often sold-out even before the start of the congress. A variety of courses in minimally invasive surgical techniques was available again this year and eagerly awaited by participants. Basic laparoscopic courses were offered, with experienced tutors demonstrating basic techniques in pelvi-trainers. More advanced laparoscopic surgeons could take courses in LESS techniques, where the details of single-site surgery were explored in greater depth. For the endoscopic treatment of BPH, a course on bipolar TURP was presented, and trainees refined their skills using a simulator in complex cases. Greenlight prostate vaporization courses were also available, and participants can choose either basic or advanced skills lessons. A virtual reality model replicated the surgical experience for trainees, and sessions were enriched with surgical videos and tips from the expert tutors. For the management of urolithiasis, courses in endourology and ureterorenoscopy were available. Trainees also had the opportunity to become familiar with the wide range of equipment used (baskets, wires, lasers, etc), and to perform flexible ureteroscopy and lithotripsy in models. A course in robotic surgery was also offered, and reservations were needed due to very limited slots. The course took trainees through the basics of robotic surgery, from the efficient use of the console, drills for improving hand-eye coordination to finishing the standard steps of robotic surgery. Members of the ESUT were also actively involved in ESU courses and presentations. These two to three-hour long courses are a great opportunity for participants to become acquainted with specific details of a technique or the management of a specific entity. ESUT members were responsible for some of the more popular courses, including a flexible ureterorenoscopy course by Prof. Traxer, a PCNL course by Professors Liatsikos and Knoll, a robotic prostatectomy course by Prof. Piechaud and a NOTES and mini-laparoscopy course by Prof. Rane. More advanced surgeons had the opportunity to participate in the laparoscopic and robotic cystectomy course with Professors Rassweiler and Van Velthoven. In summary, ESUT’s participation in this year’s annual EAU congress focused on the exciting developments in uro-technology. We look forward to next year’s congress in Stockholm for us to provide another opportunity to bring the future of urology closer to the present. Upcoming ESUT affiliated events The third and final surgical session included an interesting mix of upper and lower tract techniques, and was moderated by Professors. De la Rosette, Michel, Burchardt and Annerstedt. A quick and practical BPH treatment, Urolift, was demonstrated by Professors Sievert and Woo, with the case completed in 10 minutes. In other BPH cases, Prof. Carmignani (Milan, IT) performed a TULEP technique, while Prof. Pfitzenmaier (Bielefeld, DE) performed a prostate vaporisation. Live surgery session The audience was treated to the best in current surgical techniques by internationally renowned experts, and had the opportunity to participate in a lively debate with the surgeons and moderators. The session began with an introduction by ESUT Chairman Prof. J. Rassweiler who noted the close collaboration among the participating surgeons and the outstanding facilities of the Department of Urology at San Raffaele Turro Hospital, and at the Vita Salute San Raffaele University. Dr. Andras Hoznek then presented follow-up details on last year’s live surgery patients, in accordance with the new EAU policy on surgical ethics in live surgery. This critically important innovation was reviewed by Prof. Artibani, in advance of Prof. Keith Parson’s full presentation of the new policy during the final plenary session. Prof. Liatsikos (Patras, GR) then demonstrated his technique for single-site laparoscopic nephrectomy using 3D vision assistance. Near the end of the session, two interesting pre-recorded videos were shown, with a novel robotic-assisted flexible ureteroscopic system presented by Prof. Saglam (Ankara, TR) and Prof. Janetschek’s video of a pelvic lymphadenectomy assisted by ICG (Indocyanine Green dye). Concluding the very successful meeting, closing remarks were given by Prof. van Velthoven. World Congress of Endourology 2013 in New Orleans, USA The Society of Endourology is the premier organisation whose aim is to share, teach, and report the latest state-of-the-art developments in endourology, laparoscopy, robotics, percutaneous surgery and minimally invasive surgery. For the 31st Annual World Congress of Endourology & SWL (WCE) scheduled on October 22 to 26, 2013 in New Orleans, our scientific theme will focus on state-of-the-art advances in biomedical imaging for pre-surgical planning, intraoperative navigation and improvement of outcomes. International experts in this exciting and innovative field will cover emerging technologies on image-guided surgery such as: Moderated by Professors Rassweiler, Abbou, Wiklund and Knoll, the initial surgical session began with interventions in the upper urinary tract, with the procedures transmitted via the massive screens of the eURO auditorium. Prof. Guazzoni (Milan, IT) • Molecular Imaging to Decrease Positive Surgical Margins; • Nanotechnology and Urology; • Optical Biopsy of Urothelial Carcinoma Using Confocal Endomicroscopy; • Image fusion of MR and Ultrasound for Prostate Biopsy; • Critical Analysis of Focal Therapies for Prostate Cancer; and • Other specialty lectures from world-renowned speakers Hands-on ureteroscopy course Visit our website (www.wce2013.com) for further information Members of the audience use 3D glasses in some live surgery sessions EAU Section of Uro-Technology March/May 2013 An important aspect of ESUT’s efforts in promoting technological advances is the education and training of younger urologists. ESUT (in collaboration with EULIS and ERUS) actively participates in hands-oncourses organised by the European School of Urology. Instructional courses WCE2013 will also feature an expanded number of morning instructional courses, featuring international experts sharing their experiences, tips and tricks, management of complications including: • Practical Management of Stones: Prophylaxis & Medical Management • BPH and Incontinence • Ablation of Small Renal Mass: Current Status • Management of Complications After Laparoscopy & Robotics • Robotic Prostatectomy: Step-by-Step Technique • Endourological Treatment of Upper Urinary Tract Tumor • Stents: What’s New • Percutaneous Surgery: Supine and Prone Approaches, Access Technique (Fluoroscopy vs. Ultrasound) • Imaging and Uro-Radiology • Robotic/Lap Partial Nephrectomy • NOTES & LESS in Urology: What Can We Do Now? • Robotic Assistant: Help Me, Don’t Hurt Me • Ureteroscopy: Rigid and Flexible Techniques Submit your abstracts for WCE 2013 The abstract submission site is now open. The Make plans now to join us October 22 - 26, 2013, in deadline for poster and video abstracts is June 3, 2013. New Orleans, Louisiana, for WCE2013. We look forward to seeing you there! Submit your abstracts now at www.wce2013.com! European Urology Today 29 Congress calendar 2013/2014 May 15-16: Cambridge, United Kingdom Flexible and rigid ureteroscopy workshop Contact: Stephanie Taylor E-mail:[email protected] Website:www.camurology.org.uk 15-18: Bucharest, Romania National Congress of the Romanian Association of Urology Contact: Dr Radu Constantiniu E-mail:[email protected] 17: ESU organised course on Place and role of lymphadenectomy in urologic cancers at the time of the national congress of the Romanian Association of Urology Contact:ESU 16-17: Cambridge, United Kingdom International Multidisciplinary workshop on Prostate Multiparametric MRI Reading (ESU) & MRI-targeted Transperinal Prostate Biopsies Contact: Stephanie Taylor E-mail:[email protected] Website:http://www.camurology.org.uk/ teaching/courses/prostatemultiparametric-mri-reading-andmri-targeted-transperineal-prostatebiospsies-may-2013/ 16-17: Athens, Greece Prostate Cancer Translational Research Conference Contact: Prostate Cancer 2013 Secretariat E-mail:[email protected] Website:http://www.prostatecancer2013.com 16-18: Osijek, Croatia Symposium 10th Osijek Urological Days and 3rd Osijek Nephrology Days Contact: Dr. Hrvoje Kuveždic E-mail:[email protected] Website:www.urologija.kbco.hr 17-19: Athens, Greece 33rd Athenian Urology Days Contact: ERASMUS S.A. E-mail:[email protected] Website:www.athenianurologydays.gr 18-21: Istanbul, Turkey 50th ERA-EDTA Congress Contact: ERA-EDTA Congress Office E-mail:[email protected] Website:http://www.era-edta2013.org/ 19-23: Milan, Italy Symposium on biomarkers of prostate cancer Contact: Dr Cathie Sturgeon E-mail:[email protected] Website:www.milan2013.org/index.php 24-25: Jastrzebia Góra, Poland 6th Pomeranian Uro-Oncology Conference Contact: Elzbieta Senkus-Konefka - Medical University of Gdansk E-mail:[email protected] Website:www.uro-onko.pl 28-1 Jun: Dublin, Ireland 38th Annual Meeting of the International Urogynecological Association Contact: IUGA Office E-mail:[email protected] Website:http://www.iuga.org/ 29-31: Amsterdam-Noordwijk, The Netherlands 6th International Symposium on Focal Therapy and Imaging in Prostate & Kidney Cancer Contact: ERASMUS SA E-mail:[email protected] Website:www.focaltherapy.org 30-31: Lisbon, Portugal 14th Practical Course Prostate Ultrasound and Biopsy - 5th International Workshop on Prostate Biopsy Contact: Ana Pais E-mail:[email protected] Website:http://www.admedic.pt/ficheiros/ congressos/programa1362148778.pdf 30 European Urology Today 30-1 Jun: Amsterdam, The Netherlands 1st World Congress on Abdominal and Pelvic Pain Contact:CongresLink E-mail:[email protected] Website:www.pelvicpain-meeting.com 31: Tartu, Estonia 8th Baltic Urological Conference Contact: Estonian Society of Urologists E-mail:[email protected] 31: ESU organised course on Pushing back the boundaries in CRPC and UTI at the time of the national congress of the Estonian Urological Association Contact:ESU 31-4 Jun: Hong Kong, China World Congress of Nephrology ISN, HKSN and APSN Contact:ISN E-mail:[email protected] Website:http://www.wcn2013.org/ 31-4 Jun: Chicago (IL), USA Annual Meeting of the American Society of Clinical Oncology (ASCO) E-mail:[email protected] Website:http://events.jspargo.com/asco13/public/ enter.aspx June 4-5: London, United Kingdom Advanced Applied Female Pelvic Anatomy and Surgery (Cadaveric course) Contact: RCS Education E-mail:[email protected] Website: http://www.rcseng.ac.uk/courses/coursesearch/course.2007-05-31.6426708897 4-5: Bristol, United Kingdom 2nd Young Urology Meeting Contact: Young Urology Meeting E-mail:[email protected] Website:www.young-urology.org 5-8: Murnau, Germany 26th Annual Meeting of the German-speaking medical Society for Paraplegia (DMGP) 2013 Contact: Conventus Congressmanagement & Marketing GmbH E-mail:[email protected] Website:www.dmgp-kongress.de 6-7: Tirol, Austria Minimally Invasive Percutaneous Stone Therapy Clinical Workshop (MIP) Contact: Dept. of Urology and Andrology E-mail:[email protected] 6-8: Lisbon, Portugal 6th EAU Leading Lights in Urology (LLU) followed by the Young Academic Urologists Meeting (YAUM) Contact:EAU E-mail:[email protected] Website:http://leadinglights.uroweb.org/ 6-8: Cologne, Germany Brachytherapy for Prostate Cancer Course Contact:ESTRO E-mail:[email protected] Website:http://www.estro-events.org/Pages/ defaulthome.aspx 7-8: Paris, France Third Teaching Course on Prostate MRI Contact: F. Cornud, D. Portalez E-mail:[email protected] Website:www.prostatemricourse.com 7-9: Ankara, Turkey 2nd Ankara Robotic Urology Symposium & Course Contact: A. Erdem Canda, MD E-mail:[email protected] Website:www.robotictimes.org 12-14: Trnava, Slovakia 20th Annual Conference of the Slovak Society of Urology Contact: Tatiana Ivancikova, Tajpan s.r.o. E-mail:[email protected] Worldwide, continually updated urological meeting calendar at 13: ESU organised course on Interventional therapy for BPO - Surgical treatment for BPO at the time of the national congress of the Slovak Urological Association Contact:ESU 12-14: Marseille, France Global Congress on Prostate Cancer 2013 Contact:e-hims E-mail:[email protected] Website:www.e-hims.com 14-16: Izmir, Turkey 1st International Uroanatomy Congress Contact: International Young Urologists Association (IYUA) E-mail:[email protected] Website:www.uroanatomy.org 17-20: Manchester, United Kingdom Annual Meeting of The British Association of Urological Surgeons (BAUS) Contact:BAUS E-mail:[email protected] Website:www.baus.org.uk 21-22: Minsk, Belarus National congress of the Belarussian Association of Urology Contact: Prof. Viachaslau Vshchula E-mail:[email protected] 22: ESU organised course at the time of the national congress of the Belarussian Association of Urology Contact:ESU 23-25: London, United Kingdom 6th Hamlyn Symposium on Medical Robotics Contact: The Hamlyn Centre E-mail:[email protected] Website:www.hamlyn-robotics.org/ 22-25: Niagara Falls (ON), Canada 68th Annual meeting of the Canadian Urological Association Contact:CUA E-mail:[email protected] Website:www.cua.org/ 26-28: Paris, France 3rd International Meeting “Challenges in Endourology and Functional Urology” Contact: ERASMUS SA E-mail:[email protected] Website:www.challenges-endourology.com 26-28: Malmö, Sweden Prostate Cancer Translation Research in Europe (PCTRE) Contact: Congress Consultants Email:[email protected] Website:http://pctre2013.uroweb.org July 5-6: Athens, Greece Clinical Topics in Urology “Lithiasis from A TO Z” Contact: ERASMUS S.A. E-mail:[email protected] Website:www.CTUcongress.org 4-5: Tirol, Austria Minimally Invasive Percutaneous Stone Therapy Clinical Workshop (MIP) Contact: Dept. of Urology and Andrology E-mail:[email protected] www.uroweb.org August 6-10: Melbourne, Australia Prostate Cancer World Congress Website:www.prostatecancercongress.org.au E-mail:[email protected] 26-30: Barcelona, Spain Annual Meeting of the International Continence Society Contact: ICS Office E-mail:[email protected] Web:http://www.icsoffice.org/Events/ ViewEvent.aspx?EventID=180 September 3-5: Stockholm, Sweden ERUS’13 - EAU Robotic Urology Section Congress on Latest Developments in Robotic Surgery Contact: e-HIMS bvba E-mail:[email protected] Website:www.erus2013.com 5-7: Copenhagen, Denmark 2nd Meeting of the EAU Section of Urolithiasis (EULIS) Contact: Congress Consultants B.V. E-mail:[email protected] Website:http://eulis.uroweb.org 5-7: Jachranka, Poland 43rd National Congress of the Polish Urological Association Contact: PTU E-Mail:[email protected] Web:www.pturol.org.pl 6: ESU organised course Update in non-muscle invasive bladder cancer T1G3 and nephron sparing surgery at the time of the 43rd National Congress of the Polish Urological Association Contact:ESU 8-12: Vancouver, Canada 33rd Congress of the Société Internationale d’Urologie (SIU) Contact: SIU Central Office E-mail:[email protected] Website:www.siu-urology.org/ 10: Birmingham, United Kingdom Dragon’s Den’ Urology SaPhonelite Meeting, “New Horizons in Non-invasive bladder cancer” Contact: Centre for Professional Development E-mail:[email protected] Website:http://www.birmingham.ac.uk/facilities/ mds-cpd/conferences/urological-cancertrends/saPhonelite-meeting/ saPhonelite-meeting.aspx 11: Birmingham, United Kingdom Current Trends in Urological Cancer, 10th Annual Symposium Contact: Centre for Professional Development E-mail:[email protected] Website:http://www.birmingham.ac.uk/facilities/ mds-cpd/conferences/urological-cancertrends/index.aspx 12-13: Tirol, Austria Minimally Invasive Percutaneous Stone Therapy Clinical Workshop (MIP) Contact: Dept. of Urology and Andrology E-mail:[email protected] 13-14: London, United Kingdom ESU - Weill Cornell Masterclass in General urology Contact:ESU E-mail:[email protected] Website:http://esusalzburg.uroweb.org 3rd Joint Meeting of the EAU Section of GenitoUrinary Reconstructive Surgeons (ESGURS) and the EAU Section of Andrological Urology (ESAU) Contact: Congress Consultants B.V. E-mail:[email protected] Website:http://esgurs-esau.uroweb.org/ 12-13: Beijing, China 13-18: Prague, Czech Republic Chinese Urology Education Programme (CUEP) Contact: European School of Urology (ESU) and Chinese School of Urology (CSU) E-mail:[email protected] Website:www.uroweb.org 11th European Urology Residents Education Programme (EUREP) Contact: Congress Consultants B.V. E-mail:[email protected] Website:http://eurep.uroweb.org/ 7-13: Salzburg, Austria March/May 2013 Congress calendar 2013/2014 Worldwide, continually updated urological meeting calendar at 19-22: Istanbul, Turkey 16-19: Beijing, China 6-8: Moscow, Russia 20th European Symposium on Urogenital Radiology (ESUR 2013) Contact: Organization Secretariat E-mail:[email protected] Website:http://www.esur2013.org/en/default.asp 20th Annual meeting of the Chinese Urological Association (CUA 2013) Contact: Ms. Betty Zhou E-mail:[email protected] Website:www.cuan.cn National Congress of the Russian Society of Urology Contact:[email protected] 23-27: Countries all over Europe 16-17: London, United Kingdom Urology Week 2013 Contact: European Association of Urology Email:[email protected] Website:www.urologyweek.org 25-27: Dresden, Germany 21st Meeting of the EAU Section of Urological Research (ESUR) In collaboration with the 65th DGU Congress Contact: Congress Consultants B.V. E-mail:[email protected] Website:http://esur.uroweb.org 25-28: Dresden, Germany 65th Congress of der German Society of Urology (DGU) Contact:DGU E-mail:[email protected] Website:www.dgu-kongress.de/index. php?id=571&L=2 26-27: Amsterdam, The Netherlands 2nd International State-of-the-Art in Uro-Oncology Conference on Prostate and Kidney Cancers Contact:EUOG Email:[email protected] Website:http://euog.org/ 27-1 Oct.: Amsterdam, The Netherlands 17th ECCO - 38th ESMO - 32nd ESTRO European Cancer Congress Contact:ECCO Email:[email protected] Website:http://www.ecco-org.eu 30-1: London, United Kingdom Understanding Urodynamics Course Contact: Royal College of Obstetricians and Gynaecologists E-mail:[email protected] Website:http://www.rcog.org.uk/events/ understanding-urodynamics-0 October 2-4: Moscow, Russia VIII Congress of the Russian Association of Oncological Urology Contact: Kamolov Bakhodur E-mail:[email protected] Website:www.roou.ru 2-5: Lima, Peru Congreso CAU Peru 2013 Contact: Sociedad Peruana de Urología Email:[email protected] Website:www.cauperu2013.com/ 4-6: Prague, Czech Republic 13th Central European Meeting (CEM) Contact: Congress Consultants B.V E-mail:[email protected] Website:http://cem.uroweb.org 5-8: Riccione, Italy 86th Annual Meeting of the Società Italiana di Urologia (SIU) Contact: Società Italiana di Urologia (SIU) E-mail:[email protected] Website:www.siu.it 10-12: Tübingen, Germany 1st Joint Section Meeting of Female and Functional Urology (ESFFU), Genito-Urinary Reconstructive Surgeons (ESGURS) and Oncological Urology (ESOU) Contact: Congress Consultants B.V. E-mail: [email protected] Website:http://esffu-esgurs-esou.uroweb.org 15-16: Beijing, China CUA-EAU Programme on LUTS and Oncology Contact: European School of Urology (ESU) and Chinese School of Urology (CSU) E-mail:[email protected] Website:www.uroweb.org March/May 2013 Annual Scientific Update in Urogynaecology Contact: Royal College of Obstetricians and Gynaecologists E-mail:[email protected] Website:http://www.rcog.org.uk/events/annualscientific-update-urogynaecology-0 16-19: Umag, Croatia 5th Congress of the Croatian Society of Urology with International Participation Contact: Jelena Krmic Website:www.5hrvatskikongresHUD2013.org 22-26: New Orleans (LA), USA 31st World Congress of Endourology and SWL Contact: Endourological Society E-mail:[email protected] Website:www.wce2013.com 24-26: Eger, Hungary National congress of the Hungarian Association Urology Contact: Dr. Tóth György E-mail:[email protected] 26: ESU organised course on Prostate cancer at the time of the national congress of the Hungarian Association Urology Contact:ESU 30-1 Nov: Carlsbad, Czech Republic National congress of the Czech Urological Society Contact: Dr. Milan Hora E-mail:[email protected] 31: ESU organised course on Female urology; fundamentals of stress incontinence and prolapse at the time of the national congress of the Czech Urological Society Contact:ESU 30-3 Nov.: Antalya, Turkey National Congress of the Turkish Association of Urology Contact:TAU E-mail:[email protected] Website:www.uroturk.org.tr 1: ESU organised course on Localised prostate cancer at the time of the national congress of the Turkish Urological Association Contact:ESU 31-2 Nov: Amman, Jordan 8th international conference of the Jordanian Association of Urological Surgeons (JAUS) Contact: Dr. Khaldoun Gharaibeh E-Mail:[email protected] 31: ESU organised course at the time of the national congress of the Jordanian Association of Urological Surgeons Contact:ESU November 1-3: Thessaloniki, Greece 9th South Eastern European Meeting (SEEM) Contact: Congress Consultants B.V. E-mail:[email protected] Website:http://seem.uroweb.org/ 4: Tashkent, Uzbekistan National congress of the Scientific Society of Urologists of Uzbekistan Contact:SSUU E-mail:[email protected] 4: ESU organised course on Updates on urooncology at the time of the national congress of the Scientific Society of Urologists of Uzbekistan Contact:ESU 7: ESU organised course on Update and evolving investigation in urology at the time of the national congress of the Russian Society of Urology Contact:ESU 6-10: Antalya, Turkey 11th Urooncology Congress Contact: Association of Urooncology, Turkey Contact: Serenas Tourism Congress Organization Co. E-mail: [email protected] [email protected] Website:www.urooncologycongress.org 8-9: Strasbourg, France Annual symposium Robotic Assisted Microsurgical & Endoscopic Society (RAMSES) Contact:RAMSES E-mail:[email protected] Website:WWW.ROBOTICMICROSURGEONS.ORG 15-17: Marseille, France 5th Multidisciplinary Meeting on Urological Cancers Embracing Excellence in Prostate, Bladder and Kidney Cancer Contact: EAU, ESMO and ESTRO E-mail:[email protected] Website:www.emuc2013.org 14: ESU Medical oncology course on Genitourinary Cancer (MOGUC) Contact:ESU 15-17: Berlin, Germany 6th ESU Masterclass on Female and functional reconstructive urology, in collaboration with the EAU Section of Female and Functional Urology (ESFFU) Contact:ESU E-mail:[email protected] Website:www.uroweb.org 20-23: Paris, France 107th National Congress of the French Association of Urology Contact: Colloquium-AFU 2013 Email:[email protected] Website:http://www.urofrance.org/congres-etformations.html 22: ESU organised course on Lasers and endoscopes in urology: “What an urologist should know” at the time of the national congress of the French Association of Urology Contact:ESU 21-22: Tirol, Austria Clinical Workshop Program 2013 - Laparoscopic Partial Nephrectomy & Single Incision Triangular Umbilical Surgery Contact: Dept. of Urology and Andrology E-mail:[email protected] 29: Kazan, Russia Conference of the Russian Association of Oncological Urology in the Volga federal district Contact: Russian Association of Oncological Urology E-mail:[email protected] Website:www.roou.ru www.uroweb.org January 2014 17-19: Prague, Czech Republic 11th Meeting of the EAU Section of Oncological Urology (ESOU) Contact: Congress Consultants B.V. E-mail:[email protected] Website:http://esou.uroweb.org February 2014 1-4: Davos, Switzerland European Urology Forum 2014 - Challenge the experts Contact:ESU April 2013 11-15: Stockholm, Sweden 29th Annual EAU Congress Contact: Congress Consultants B.V. E-mail:[email protected] Website:www.eaustockholm2014.org May 2013 30-3 June: Chicago, USA American Society of Clinical Oncology (ASCO) Annual Meeting 2014 Contact:ASCO E-mail:[email protected] Website:www.asco.org/portal/site/ascov2 June 2013 21-24: St. Johns (NL), Canada 69th Annual meeting of the Canadian Urological Association Contact:CUA E-mail:[email protected] Website:www.cua.org/ October 2013 1-4: Dusseldorf, Germany 66th Congress of der German Society of Urology (DGU) Contact:DGU E-mail:[email protected] Website:www.dgu.de/ 12-16: Glasgow, Scotland 34th Congress of the Société Internationale d’Urologie (SIU) Contact: SIU Central Office E-mail:[email protected] Website:www.siu-urology.org/ December 2013 5-9: Kish Island, Iran 12th Asian Congress of Urology (ACU) Contact: Urological Association of Asia and Iranian Urological Association Email:[email protected] Website:www.12thacu2014.org December 2-6: Sharm el-Sheikh, Egypt National congress of the Egyptian Association of Urology Contact: Prof. Eissa - EUA President E-mail:[email protected] 4: ESU organised course on paediatric urology for the adult urologist: A practical update at the time of the national congress of the Egyptian Association of Urology Contact:ESU 6-7: Tirol, Austria Minimally Invasive Percutaneous Stone Therapy Clinical Workshop (MIP) Contact: Dept. of Urology and Andrology E-mail:[email protected] For more elaborate information on all EAU meetings please contact Congress Consultants or consult the EAU website: Phone: +31 (0)26 389 1751 Fax: +31 (0)26 389 1752 Website:www.uroweb.org For more elaborate information on all ESU courses please contact the European School of Urology or consult the EAU website: Phone: +31 (0)26 389 0680 Fax: +31 (0)26 389 0684 E-mail:[email protected] Website:www.uroweb.org European Urology Today 31 Who’s Who in Urology Notification: Promoting your meetings The EAU executive is pleased to help promote any scientific meetings. However, due to the large number of requests we are receiving, we have been forced to set up some rules and regulations related to the circulation of promotional material. Jan Breza Gabriel Haas Raja Khauli Chairman, Department of Urology, Slovak Medical University Bratislava, Slovakia; Professor and Chairman, Department of Urology, Comenius University School of Medicine, Bratislava; ViceChancellor (2003-2010); Slovak Medical University; Visiting Associate Professor (1991-1993), Department of Urology, University of California, San Francisco, USA; Awarded, Frans Debruyne Lifetime Achievement, EAU (2013); Honorary Member (2009), European Association of Urology; Awarded (2008) Jessenius Award, Slovak Academy of Science; Awarded (2003) Slovak Medical Association – Gold Medal; Author of more than 190 international medical publications. Medical Director (2009-Present) of Urology, Astellas Global Development; Professor and Chairman (1995-2007), Department of Urology at SUNY Upstate Medical University, Syracuse, New York, USA; Honorary Member, Peruvian and Hungarian Urological Associations. Former President, Hungarian Medical Association of America and of the Northeastern Section of the American Urological Association; Author of over 170 scientific papers and book chapters; Former Editor, Canadian Journal of Urology. Professor of Surgery, and Head, Division of Urology, American University of Beirut Medical Center; Adjunct Professor of Urology, University of Massachusetts Medical Center, Worcester, Massachusetts, USA; Residency in urology, University of Maryland and the Cleveland Clinic Foundation; Elected President (2006), Arab Association of Urology; Chairman (2012) Examination Committee of the Arab Board of Urology; Member (2013), EAU Regional Board; Elected President, Urological Society for Transplantation and Renal Surgery (USTRS); Author of more 160 peer reviewed manuscripts and 11 book chapters. Europe Official 9 newsletter Adolesc ent an Uro log of the European urology Special needs of creation adolescen of ts a stronger require Prof. Jean-Jacque the adolescen s Wyndaele t urology Associatio 27th An 31 nual EA Sustained U Cong research work res n of Urolo gy Active surveill A word ance for of low-risk cancer andwarning: Active patient surveillan the risk ce on prostate s of overdiagn Bangma osis y Toda y Vol. 24 Prof. Chris No.2 - March/May 9th ESOU 35 2012 800 participanMeeting ts gather on latest in Hamburg developm ents in urologica for update l cancers Further investmen and urology’s ts in innovative colleague s stronger discipline said Prof. and specialists ties with research studies s from other Hidehiro other medical that was remain one of Japanese Kakizaki discipline the key, reiterated Urologica who s,” overarchi five-day l Associatio co-chaired the ng themes Chris Chapple. 27th Annualby opinion leaders n session This year February returned throughou EAU Congress the Japanese with Prof. 24 to 28 t the nearly in full force held from in Paris, France. a year after with more than delegation Experts prevented the Fukushim 150 participan who strategies lectured and Vienna. many from attending a calamity which ts, spoke during the the 2011 significant congress on optimal treatment congress were one in managem gains made in The in reporting saying medical ent in recent that ICUD-EAU and sessions healthcar of the Committe e if innovative years can only surgical closely working lead to better (5th ICI) International Consultati es of the studies held in the and the with other pursued. on on first two specialists crucial role of the need for a days also Incontinence balanced are consistent fields such demonstr approach the rising ated ly related “This annual in other urologica Lower Urinaryincidence of congress together incontinen l the most Tract Symptom and pursuing provides evidence ce and highly attended research session the goals that for meetings, s (LUTS). One of of groundbr working expert collated the treatment insights that will the reporting eaking groups on consensus findings for patients help us the strong identify is only of various effective imaging, fistulas, a range of issues General links we now have,”possible if we from epidemio pharmaco syndrome maintain Per-Ande logy to bladder , among logy, rs Abrahams said EAU Secretary ceremony other incontinen . pain son during ce topics. the opening Focus on uro-onco With eight logy plus the EAU Section Meetings Profs. Radziszews first plenary held on ki and Chapple cancer, participan session which tackledFebruary 25 (3rd and ts had a variety of 4th from bladder full-day specialise left) chair agenda transmiss the second d topics and a wide Atala as he ions to choose plenary rooms located of surgeries session complex listed various obstacles on functional conducted from. Live work involved were presentedin Paris, Aalst urology in scaffolds, in creating such as the (BE) and six operating avoiding by (ESUT), biological tumour all-cause a feat that the EAU Section Mannheim (DE) construction formation and prostate of stable of Uro-Techn previous exceeded added: “Surgery blood vessels. and the congresse ESUT’s cancer mortality, in cooperati s. The day-long programm ology The last-day did not observatio ” said Wilt. es in reduce plenary session, presented on with the ERUS, He cancer. A n in men with low mortality more session conducted developments examined potential PSA or than bladder complex surgical EULIS and ESIU, Prof. Freddie in prostate exist in the latest and kidney procedure men with mortality benefi low risk prostate Hamdy givingcancer (PCa) research. surgeries. s in prostate, personali t from higher PSA disease.” sed the keynote With and possibly surgery may At the plenary PCa, Professortreatment for remarks high risk session s Timothy low and intermedi on Professor provided on managing The concludin s Wilt updates ate in-depth Manfred Wirth bladder g part of PCa, respective on the PIVOTand Lars Holmberg risk late-break and cancer discussion the last ing and SPCG4 ly. either medical s, highlightiJames Catto led Mason and developments session focused studies ng the or surgical on Fritz Schröder with Professor on neoadjuva the extent approach suitability of s Malcolm updating es (dependin patient’s and aggressiveness the audience screening nt hormone therapy response of the disease) g on data, respective have seen and prostate to the selected on ly. cancer treatment and quality of an improvement Key . “We in life,” messages on the benefi said Prof. Arnulftechnique, capacity • Degarelix from Mason ts of cystectom and Stenzl and Schröder standard is goserelin ‘non-inferior’ despite y, considerein his lecture were: the emergenc therapies plus bicalutam to the combinat d volume . e of newer as the gold ide at reducing ion of in patients medical dependen with prostate Catto noted t PCa (Mason). advanced hormoneLive transmissio issues, a the critique on • The Phase fact radical surgery ns of prostate, conducted that chemo-raunderscored 111b CS30 bladder in due offered by and kidney organised 6 operating rooms better control trial revealed of patients, diation offers Nicholas James to QoL surgeries by ESUT that degarelix symptoms who said benefits of lower in cooperationin 3 different countries, deserves and pointed out to certain Session urinary hesitancy (LUTS) such as with EULIS, were a re-evalua participant that types frequency tract in urination. ERUS and s view the 3D glasses tion in the bladder-preservatio , urgency ESIU ESUT live (Mason). light of Right on and The need surgeries recent data. n • The two-year the first with for sustained day, the EAU theme in with 11 other the joint meetings 21% reductionupdate on the the second research efforts associatio urology ESRPC study regional organised ns with Profs. plenary session was a recurring “In men with of 1% comparedon PCa mortality by underlinin showed programm for the Urology and internatio on Chapple during the localised prostate a rate, or nal with the Beyond (Schröder and Piotr functional g an increase consultati e demonstrated Europe interim identifying the crucial role ); and Radziszew compared early PSA era, radical cancer detected study of the on researche to observatio 2009 Particular among various need for closer prostatect treatment the most effective rs can play ski • Early ly urology n did not . omy PCa diagnosis and medicalin uro-oncology groups. emerging Prof. Karl-Dietrich medical or surgical in significantly where the known prospects treatment has defi Sievert examined reduce cancers newer options nite benefi , saying for prostate new diagnostic are overdiagn disadvantages, in pharmaco that current trends countries emerging, practition and kidney current osis (Schröder such as a ts, alongside such as use high rate therapy ers from ). Japan, Latin-Ame aside from point to On biomarkeof antimuscarinics of diverse rican countries,Iran, India, the and r research, vital to maintain the Arab PDE-5 outcomes to name and in the coming Sievert expects inhibitors. effective a and outside more collaborat few, said it is years as urology. new data concrete ive work Technolog within come in. ical “Our participat New technologadvances ion here y learning and were reflects the attendant discussed from the importan if we expand each other. in the fourth-da myriad topics such our views We can only move t role of y plenary challenges nephrolith as the optimal to consider session forward use those of ureterend otomy, new optical of percutaneous with our oscopy, systems benefits and the in use of AUA lecture of simulation shock wave lithotripsy on regenerat in surgical training. Anthony Atala, director ive medicine The Regenera tive Medicine, of the Wake given by Prof. in tissue showcase Forest Institute engineeri for cells to create ng, particular d the current efforts ly the use biological kidney, of stem substitute heart, liver s for the and many other organs. bladder, “There are March/Ma still challenge y 2012 resolve s several issues in ahead…we still tissue engineeri need to ng,” said and mult i-dis By Joel Vega s: Collab ciplinary orative work is crucial links are essential , say opin ion 28th Ann www.eaum ual EAU ilan2013.org Congres leaders s Europea n Urology Today 1 All EAU related meetings (Section Offices either full members or partners) and national societies meetings with which we have a special alliance, may be promoted by e-mail (e-mail newsletter or separate e-mail communication), in addition to the other available channels. All other urological meetings may be included in our Uroweb and Urosource congress calendar as well as in the European Urology Today congress calendar. Please feel free to contact us ([email protected]) in case there are any queries or remarks related to this notice. “Who’s Who in Urology,” is an informative listing of decision-makers, leading researchers, faculty heads, industry representatives, medical scientists and other active professionals in urology. This series reflect not only the milestones achieved in urology but also show urology’s multifaceted network and interdisciplinary nature. Win a free registration to Stockholm in 2014! EU-ACME members, join the MCQ quiz published in European Urology To increase awareness regarding the significant and growing role of online Continuing Medical Education (CME) and promote its benefits, the EU-ACME office introduced in 2009 an exciting initiative amongst its members. From all EU-ACME members who participated, the three highest scoring participants who topped the MCQ quizzes published in the journals of the EU-ACME Office European Urology will be entitled to a free registration for the Annual EAU Congress. The EU-ACME committee believes that this knowledgebased competition would encourage the best and the most talented to participate. Hence, this exciting initiative was continued for 2014. 29th Annual EAU Congress to be held in Stockholm from April 11 to 15, 2014. From January 1 up to December 31, 2013, interested EU-ACME members will have to answer multiple questions published in European Urology. For details, visit: www.eu-acme.org/europeanurology Participants who answered the most questions correctly will be awarded with free registration for the Winners will be formally notified in early January next year, and their names published in the February 2014 issue of this newsletter. Good luck to all! Credit Registry Reports electronically! EU-ACME members may generate and print Credit Registry Reports online. If you do not wish to receive hard copy of the CRR please log in to your online account and check the box “I will generate and print my CRR online. I do not wish to receive a copy by regular mail”. www.eu-acme.org EU-ACME MCQ 2012 winners MCQ initiative draws enthusiastic response From the period January 1 to December 31 last year, EU-ACME members answered multiple questions published in European Urology. Participants who answered the most questions correctly were awarded with free registration for the 28th Annual EAU Congress in Milan held in March this year. The 2012 winners are: 1. Dr. Jose Angel Cuesta Alcala, Spain (CME-110604) 2. Mr. Mark Saxby, United Kingdom (CME-000243) 3. Mr. Franz-Josef Schattka, Ireland (CME-110659) EU-ACME committee chairman Prof. R. Nijman congratulated all the winners for their successful participation in our online CME-programme! EU-ACME Office 32 European Urology Today March/May 2013 Mirja Ruutu http://esou.uroweb.org Loving mother and dedicated urologist 11th Meeting of the EAU Section of Oncological Urology (ESOU) 1943-2013 17-19 January 2014, Prague, Czech Republic EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations Prof. Mirja Ruutu passed away last January 20 in Helsinki at the age of 69 years. She suffered from gastric cancer for three years. Mirja Ruutu, or Miitu as we knew her, had a great career as a urologist, teacher and professor at Helsinki University Hospital and University of Helsinki. She was qualified as general surgeon in 1977, urology in 1979, obtained her doctorate in 1985 and became docent in 1987. She worked as a consultant of urology in the Surgical Hospital until 1994 when she moved to the Meilahti Hospital. Mirja Ruutu was elected professor of urology in 2002. European Association of Urology UROLOGY WEEK 2013 Mirja had a high academic profile in Finnish and Scandinavian urological communities, and with the European School of Urology and the European Board of Urology. She was the first Fellow of the European Board of Urology (FEBU) in Finland in 1996. For many years she was involved in different collaboration groups and had administrative responsibilities in the Scandinavian Association of Urology. She was nominated Honorary Member of several international societies. Mirja´s many scientific interests included urethral strictures, biocompatibility and toxicity of catheters, impotence, prostate and renal cancers and interstitial cystitis. She was the most popular opponent in doctoral dissertations in Finland during the last years. In 2002 Mirja was elected as Urologist of the Year. Although Mirja officially retired in January 2008, she worked as a researcher at our institution until last December 2012. Mirja´s main hobbies were horses and dogs. She leaves a husband and three children. By Prof. Kimmo Taari European Urological Scholarship Programme (EUSP) Do not forget to submit your online applications for Short Visit, Clinical Visit, Visiting Professor Programme, Scholarship and Clinical Research Fellowship before the next deadline of 1 September 2013! For more information and application, please contact the EUSP Office – [email protected] or check our website http://www.uroweb.org/education/scholarship/ Urology Week is an initiative of the European Association of Urology, which brings together national urological societies, urology experts and patient groups with Cut the cord. the aim to build awareness of prostate conditions among the general public. Every year, various educational and media events take place during this week throughout Europe. VueLite ™ LED LIGHT SOURCE If you would like to organise an event in your country or find out more, please visit: www.urologyweek.org European Association of Urology MEDICAL www.cookmedical.com © COOK 2012 March/May 2013 URO-BEMEAADV-EUTVUE-EN-201212 European Urology Today 33 Between bench and clinic Mont Blanc Senior Visiting Scholarship Programme PCTRE: Two-way communication On 27-28 June 2013, the Swedish city of Malmö will host the 2nd Meeting on Prostate Cancer Translational Research in Europe. This meeting is truly unique as it fosters the vital cooperation between basic research and practice, offering multiple opportunities for researchers and practising urologists alike. According to Prof. Anders Bjartell, the meeting’s local organiser, the main issue in translational research today is the establishment of a bi-directional communication between laboratories and clinical departments. The PCTRE meeting is perfectly geared to tackle this issue. “At this meeting we make sure that the questions from the clinic are answered from the bench and vice versa,” explained Prof. Peter Mulders, chairman of the EAU Research Foundation which co-organises this event. “We will also be giving an overview of everything that is currently going on in European research on prostate cancer: many European programmes will be presented there, last updates will be given.” “Because of the interaction between researcher and practitioners on the floor, the delegates will be hearing a very balanced discussion on the what might be the next step in the treatment of prostate cancer.” Dresden hosts visiting Chinese scholars This translational meeting provides a unique opportunity for researchers to understand how discoveries can be implemented in a clinical setting, whereas practising urologists will get first-hand insights into the challenges and ambitions of today’s PCa research. Prof. Gang Zhu Beijing Hospital Dept. of Urology Beijing (CN) “A wide range of research topics will be addressed, including genomics, animal models, stem cells, imaging and drug development,” stressed Prof. Bjartell. “Additionally, we will discuss a very pressing issue of networking and funding of large-scale research projects.” zhugang2000@ gmail.com “It is of utmost importance that we address the commercialisation of important discoveries and how clinical trials should be designed for a successful outcome. We also need to understand how newly developed advanced methods can be integrated in research projects.” The scientific programme of this event will include a number of highly interactive sessions, among others dedicated to omics in personalised medicine, non-coding RNAs in prostate cancer, the integration of biomarkers into clinical utility and prostate cancer imaging in the next decade. This meeting is also a unique opportunity for young experts to profile their work and make a step forward in the European research community. The organisers invite all researchers active in this field to submit their abstracts for presentation at this meeting. Visit the official website of the PCTRE Meeting: http://pctre2013.uroweb.org Dresden, Germany hosted the second “Mont Blanc” Senior Visiting Scholarship Programme on Urogenital Tumours from March 10 to 14 this year with the successful participation of a group of Chinese urologists. Jointly sponsored by the Chinese Urological Association (CUA) and the European Association of Urology (EAU) the programme, named after the highest peak on mainland Europe, has chosen Dresden to offer the Chinese participants the opportunity of learning advanced expertise and techniques through surgical procedure observation, interactions and academic exchanges. Seven Chinese doctors from various cities in China participated in this year’s programme, namely: Gang Zhu and Tongwen Ou (Beijing); Guoqing Ding (Zhejiang); Zhiquan Hu (Wuhan); Quanlin Li (Dalian), Yonghui Chen (Shanghai) and Yuchun Zhu (Sichuan). Ms. Ren Yang, executive director of the Chinese School of Urology, accompanied the participants led by Prof. Gang Zhu. The visiting scholars spent three days with their German colleagues and joined various activities such as surgical procedures, visiting facilities, ward rounds, multi-disciplinary meetings and oncological consultations at the Urological Department of Carl Prostate Cancer Translational Research in Europe (PCTRE) Session 1: Omics in personalized medicine Chairs: G. Jenster, Rotterdam (NL) O. Kallioniemi, Helsinki (FI) 08.40 – 08.55 Advances in technology and informatics drive personalised cancer medicine O. Kallioniemi, Helsinki (FI) Sequencing cancer genomes: From research to future diagnostics M. Rubin, New York (US) Analysis of prostate cancer by next-gen sequencing J. Weischenfeldt, Heidelberg (DE) Germline genetic profiles – implications for targeted screening R. Eeles, London (GB) Panel discussion G. Jenster, Rotterdam (NL) O. Kallioniemi, Helsinki (FI) 09.35 – 09.55 09.55 – 10.10 10.10 – 10.40 Break and poster viewing 10.40 – 12.00 Session 2: Non-coding RNAs in prostate cancer Chairs: T. Visakorpi, Tampere (FI) J. Catto, Sheffield (GB) 10.40 – 11.00 11.00 – 11.15 11.15 – 11.30 11.30 – 11.45 European Urology Today All of the participants have wonderful memories of the visit and we are certainly inspired and committed to share with our Chinese colleagues the knowledge and experience we have gained. For more information please contact Congress Consultants at [email protected] or go to miRNAs: implications for personalized medicine N. Zaffaroni, Milan (IT) The therapeutic implications of miR-34c in PCa Y. Ceder, Malmö (SE) Why are snoRNAs and tRNAs differentially expressed in prostate cancer? E. Martens-Uzunova, Rotterdam (NL) Novel lncRNAs in CRPC T. Visakorpi, Tampere (FI) 11.45 – 12.00 Panel discussion T. Visakorpi, Tampere (FI) J. Catto, Sheffield (GB) 12.00 – 13.00 Lunch and poster viewing 13.00 – 14.20 Session 3: Integrating biomarkers into clinical utility Chairs: J. Schalken, Nijmegen (NL) W. Watson, Dublin (IR) 13.00 – 13.25 Prostate cancer biomarkers – addressing the clincial question E. Steyerberg, Rotterdam (NL) The long and winding road of the biomarker regulatory approval process J. Schalken, Nijmegen (NL) The Movember Global Action Plan on prostate cancer biomarkers C. Nelson, Brisbane (AU) Panel discussion on ‘What are the bottlenecks of biomarker clinical utility’ C. Bangma, Rotterdam (NL) H. Lilja, New York (US) 13.25 – 13.40 13.40 – 14.00 14.00 – 14.20 14.20 – 15.00 Break and poster viewing 15.00 – 16.30 Session 4: Funding or prostate cancer research in Europe Chairs: P-A. Abrahamsson, Malmö (SE) C. Bangma, Rotterdam (NL) 15.00 – 15.10 15.10 – 15.25 15.25 – 15.40 15.40 – 15.55 European 15.55 – 16.10 Association 16.10 – 16.30 of Urology 34 Welcome and introduction A. Bjartell, Malmö (SE) P-A. Abrahamsson, Malmö (SE) P. Mulders, Nijmegen (NL) 08.40 – 10.10 09.15 – 09.35 One of the social highlights was the awarding ceremony when Prof. Zhu was granted by Prof. Wirth, on behalf of the EAU, an EAU collar badge in recognition of his contribution to the CUA-EAU collaboration. http://pctre2013.uroweb.org Thursday, 27 June 2013 08.55 – 09.15 During the knowledge exchange session, our German colleagues presented their studies on siRNA-mediated inhibition of antiapoptotic genes in bladder cancer cells, new drugs for overactive bladder, ultrasound and MRI fusion technique for prostate biopsy and the surgical management of vena cava thrombi in advanced kidney cancer. The author shared his experiences and techniques in the use of LESS surgery in urology and treatment options for localised prostate cancer such as comparing radical prostatectomy against active surveillance. On the other hand, Prof. Yuchu Zhu reported on evidencebased medicine results in Chinese urology. Clearly, through this bilateral exchange we can efficiently share our respective insights and actual clinical experience. EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations 27-28 June 2013, Malmö, Sweden 08.30 – 08.40 Gustav Carus Hospital, Dresden University of Technology, Germany. Headed by Prof. Manfred Wirth, the Department of Urology of the Carl Gustav Carus Hospital is considered as one of Germany’s largest urological centers and has comprehensive knowledge and experience in treating urogenital tumours. Our group was impressed by the standardized quality medical care provided by the urological team. Moreover, the multi-disciplinary meetings also convinced us that close collaboration among the specialties of urology, oncology and radiology can vastly improve the delivery of optimal service to cancer patients. Overview of prostate cancer research funded by the European Commission E. Schenk, Rotterdam (NL) Cancer research funding in Horizon 2020 M. Griethuysen, Rotterdam (NL) European public-private partnerships: Current experiences and the future R. Graeser, Beerse (BE) Role for patient organisations in Horizon 2020 T. Hudson, Dublin (IR) Movember in Europe P. Villanti, Melborne (AU) Panel discussion P. Mulders, Nijmegen (NL) 16.30 – 17.45 Poster session Chairs: S. Fuessel, Dresden (DE) W. Watson, Dublin (IR) 12.10 – 13.10 Lunch and poster viewing 13.10 – 14.25 Session 7: Drug development from bench to bed Chairs: Z. Culig, Innsbruck (AT) I. Mills, Oslo (NO) 13.10 – 13.30 Androgen ablation and combination therapies in prostate cancer: New targets P. Rocchi, Marseille (FR) A dark side of the androgen ablation therapy: cofactors and oncogenes up-regulated during androgen ablation F. Santer, Innsbruck (AT) Immuno-therapy for prostate cancer TBC Panel discussion Z. Culig, Innsbruck (AT) I. Mills, Oslo (NO) Friday, 28 June 2013 08.30 – 10.00 08.30 – 08.55 08.55 – 09.10 09.10 – 09.25 09.25 – 09.40 09.40 – 10.00 Session 5: Stem cells and animal models Chairs: N. Maitland, York (GB) C. Robson, Newcastleupon-Tyne (GB) Mechanisms regulating prostate cancer stem cells M. Ousset, Brussels (BE) Alternatives to animal models to study prostate stem cells R. Heer, Newcastle-upon-Tyne (GB) Understanding the complexity of prostate cancer initiating cells: Implications for therapy A. Collins, York (GB) Tumorigenesis and metastasis of urological malignancies, a cancer stem cell perspective G. Van Der Horst, Leiden (NL) Panel discussion N. Maitland, York (GB) C. Robson, Newcastle-uponTyne (GB) 10.00 – 10.30 Break and poster viewing 10.30 – 12.10 Session 6: Prostate cancer imaging in the next decade Chairs: A. Bjartell, Malmö (SE) W. Van Weerden, Rotterdam (NL) 10.30 – 10.45 The Webmicroscope J. Lundin, Helsinki (FI) Fast Path EU Project W. Gallagher, Dublin (IR) Prostate cancer imaging from animals to humans D. Ulmert, Malmö (SE) Diagnostic imaging of prostate cancer R. Reiter, Los Angeles (US) Panel discussion A. Bjartell, Malmö (SE) W. Van Weerden, Rotterdam (NL) 10.45 – 11.00 11.00 – 11.20 11.20 – 11.50 11.50 – 12.10 13.30 – 13.50 13.50 – 14.10 14.10 – 14.25 14.25 – 14.30 Closure A. Bjartell, Malmö (SE) P-A. Abrahamsson, Malmö (SE) P. Mulders, Nijmegen (NL) Organising committee Prof. P-A. Abrahamsson, Malmö (SE) Prof. C. Bangma, Rotterdam (NL) Prof. A. Bjartell, Malmö (SE) Prof. Z. Culig, Innsbruck (AT) Dr. S. Fuessel, Dresden (DE) Prof. F. Hamdy, Oxford (GB) Dr. G. Jenster, Rotterdam (NL) Prof. O. Kallioniemi, Helsinki (FI) Dr. H. Lilja, New York (US) Prof. N. Maitland, York (GB) Dr. I. Mills, Oslo (NO) Prof. P. Mulders, Nijmegen (NL) Prof. C. Robson, Newcastle upon Tyne (GB) Prof. J. Schalken, Nijmegen (NL) Dr. E. Schenk, Rotterdam (NL) Prof. T. Visakorpi, Tampere (FI) Prof. W. Watson, Dublin (IE) March/May 2013 2nd Meeting of the EAU Section of Urolithiasis (EULIS) EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations For more information please contact Congress Consultants at [email protected] or go to http://eulis.uroweb.org 5-7 September 2013, Copenhagen, Denmark Wednesday 4 September 2013 SWL - Who needs a stent? H-G. Tiselius, Stockholm (SW) Prolonged stenting in stone patients: what are the problems? N. Buchholz, London (UK) 1st International EULIS pre-conference symposium on metal stenting of the ureter Copenhagen University Hospital Rigshospitalet 08.30 - 17.00 Live Surgery Moderators: N. Buchholz, London (UK) M. Holm, Copenhagen (DK) 08.30 - 08.50 08.50 - 09.50 09.50 - 10.10 10.10 - 10.35 The role of metal in the world of stents M. Holm, Copenhagen (DK) LIVE insertion Allium stent Physics of metal in stents made easy The Allium stent 10.35 - 10.50 Coffee break 10.50 - 11.50 Live insertion Resonance stent E. Liatsikos, Patras (GR) 11.50 – 12.15 The Uventa stent 12.15 - 13.00 Lunch break 13.00 - 14.00 14.00 - 14.25 LIVE insertion Uventa stent The Memokath stent N. Buchholz, London (UK) The Resonance stent E. Liatsikos, Patras (GR) LIVE insertion Memokath stent N. Buchholz, London (UK) Encrustation models and shock wave treatment of encrusted metal stents 14.25 - 14.45 14.45 - 15.45 15.45 - 16.05 16.05 - 16.25 Coffee break 16.25 - 16.45 Ureter stents – What does the future hold? N. Buchholz, London (UK) Farewell - M. Holm, Copenhagen (DK) 16.45 - 17.00 14.00 - 15.30 15.30 - 16.00 Coffee break 16.00 - 17.30 Poster Session 4: Inhibitors and promoters / pathphysiology upper urinary tract / genetics Chairs: H. Jung, Fredericia (DK) D. Kok, Rotterdam (NL) Macromolecules and stones - what do we know? D. Kok, Rotterdam (NL) Genetic basis of macromolecular modifications and their role in stone formation S. Khan, Gainesville (US) 16.00 - 17.30 Opening - P. Osther, Frederica (DK) 08.35 - 10.35 Keynote lectures 1 Chairs: K. H. Andreassen, Frederica (DK) P. Osther, Frederica (DK) Formation of Randall’s plaques and their involvement in stone formation S. Khan, Gainesville (US) Trends in PCNL - What have we learned from the CROES study? J. de la Rosette, Amsterdam (NL) Modern management of stones in children K. Sarica, Istanbul (TR) Retention and growth of urinary stones: Insights from imaging J. Williams, Indianapolis (US) Case discussion: Nightmare session Chair: T. Knoll, Sindelfingen (DE) Panel: N. Buchholz, London (UK) C. Chaussy, Regensburg (DE) B. Hess, Zürich (CH) T. Knoll, Sindelfingen (DE) J. Reis-Santos, Lisbon (PT) 10.35 - 11.00 Coffee break 11.00 - 13.00 Update on stone disease 1 Chairs: H-G. Tiselius, Stockholm (SE) A. Trinchieri, Milan (IT) Update on stone surgery 1 Chairs: H. Ather, Karachi (PK) A. Hoznek, Paris (FR) Friday, 6 September 2013 08.30 - 17.00 G. Guisti, Milan (IT) C. Scoffone, Turin (IT) RIRS for large stone Surgeon: O. Traxer, Paris (FR) Prone vs. Supine vs. Lateral PCNL: Status quo and perspectives A. Papatsoris, Athens (GR) Mini-PCNL Surgeon: T. Knoll, Sindelfengen (DE) Supine PCNL with ultrasound-guided puncture Surgeon: T.B.C. IPAD assisted percutaneous access to the kidney Fact or fiction? T.B.C. Debate: Maxi, mini, ulta-mini, micro PCNL - The smaller, the better? Mini-PCNL S. Lahme, Pforzheim (DE) Ultra-mini PCNL J. Desai, Ahmedabad (IN) Pediatric stone therapy: Arguments for endoscopy and against SWL M. Straub, Munich (DE) RIRS Surgeon: K. Andreassen, Frederica (DK) Semirigid URS using Backstop Surgeon: G. Guisti, Milan (IT) Expanding the indications for RIRS A. Breda, Barcelona (ES) Avoiding complications in URS M. Brehmer, Stockholm (SE) Baskets, wires, energy sources. What should be in the OR? 08.30 - 10.30 13.00 - 14.00 Lunch break 14.00 - 15.30 Poster Session 2: Stones & metabolism Chairs: J. Galan, Alicante (ES) J. Williams, Indianapolis (US) 10.30 - 11.00 Coffee break 11.00 - 13.00 Update on stone disease 2 Chairs: B. Hess, Zurich (CH) J.A. Meneses, Belo Horizonte (BR) Nephron pathophysiology in calcium nephrolithiasis R. Unwin, London (UK) Improving patient compliance to life style advice C. Bach, London (UK) Does the economic crisis affect incidence of urolithiasis? J. Reis-Santos, Lisbon (PT) EAU patient information Project T. Bach, Hamburg (DE) Impact of metaphylaxis on renal function in active kidney stone formers J.A. Meneses, Belo Horizonte (BR) Gender aspects in the treatment of urolithiasis C. Seitz, Vienna (AT) Dietary acid load and renal stone formation A. Trinchieri, Milan (IT) Cardiovascular disease and kidney stones T.B.C. 14.00 - 15.30 Poster Session 3: SWL/ stents Chairs: C. Chaussy, Regensburg (DE) M. Holm, Copenhagen (DK) European Association of Urology March/May 2013 Update on SWL Chairs: K.H. Andreassen, Frederica (DK) M. Hanna, London (UK) SWL - Is it possible to go any further C. Chaussy, Regensburg (DE) H-G. Tiselius, Stockholm (SE) Inversion, hydration and diuresis during SWL - Does it improve outcome? H. Ather, Karachi (PK) Renal haematoma after SWL H-M. Fritsche, Regensburg (DE) Pain management during SWL M. Hanna, London (UK) Predicting stone fragmentation in SWL using imaging J. Williams, Indianapolis (US) SWL - How to avoid complications M. Alomar, Riyahd (SA) First European experience with the XininEisenmenger lithotripter J. Rassweiler, Heilbronn (DE) Poster Session 1: Paediatric Urolithiasis / experimental Urolithiasis Chair: B. Hoppe, Cologne (DE) Primary hyperoxaluria - Anything new? B. Hoppe, Cologne (DE) Experimental models in urolithiasis S. Khan, Gainesville (US) 14.00 - 15.30 13.00 - 14.00 Poster session 7: Basic research Chairs: H-G. Tiselius, Stockholm (SE) J. Williams, Indianapolis (US) Clinical implications of physcochemistry in stone formation D. Kok, Rotterdam (NL) Role of calcium phosphate in calcium oxalate crystallization H-G. Tiselius, Stockholm (SE) 14.00 - 15.30 HOT workshop 3: SWL - Frederiksberg Hospital Chairs: C. Chaussy, Regensburg (DE) H-M. Fritsche, Regensburg (DE) How to improve outcome in SWL C. Chaussy, Regensburg (DE) Complications of SWL H-M. Fritsche, Regensburg (DE) SWL in children T.B.C. Practical demonstrations of positioning and stone targeting 15.30 - 16.00 Coffee Break 15.30 - 17.30 Poster Session 8: Imaging & pain management Chairs: O. Graumann, Fredericia (DK) K. Venborg Pedersen, Fredericia (DK) Sub-plenary session: Live surgery Chairs: A. Ng, Hong Kong (HK) B. Turna, Izmir (TR) ECIRS Surgeons: The wonder of ECIRS C. Scoffone, Turin (IT) RIRS compared to PCNL A. Skolarikos, Athens (GR) Can we prevent complications in URS P. Geavlete, Bucharest (RO) Endourology in upper urinary tract stenosis N. Buchholz, London (UK) RIRS: What can expect in the future? O. Traxer, Paris (FR) Management of stones in pregnancy 11.00 - 13.00 HOT workshop 2 - SWL - Herlev Hospital Chairs: S. Osther, Fredericia (DK) H-G. Tiselius, Stockholm (SE) Poster session 6: Metaphylaxis in stone formers Chairs: R. Siener, Bonn (DE) F. Keeley, Bristol (UK) Evidence based medicine: Efficacy of stone prevention K. Sarica, Istanbul (TR) How realistic is metabolic stone management in developing countries? H. Ather, Karachi (PK) Poster Session 5: PCNL/ URS I Chairs: S. Lahme, Pforzheim (DE) I. Saltirov,Sofia (BL) How to improve outcome in SWL H-G. Tiselius, Stockholm (SE) Imaging in SWL S. Osther, Frederica (DK) Pain management during SWL T.B.C. Complications of SWL K. Andreassen, Frederica (DK) Practical demonstrations of positioning and stone targeting Are we facing a new era in metabolics? Impact of endoscopic findings on recurrence prevention M. Straub, Munich (DE) Alkali citrate - a panacea for medical treatment of all kidney stones? B. Hess, Zürich (CH) Dietary renal acid load and emerging welfare pathologies T.B.C. When to suspect a genetic disorder in a patient with renal stones - and why? G. Gambaro, Rome (IT) Dietary factors and life style R. Siener, Bonn (DE) An update and practical guide to renal stone management W. Robertson, London (UK) 11.00 - 13.00 14.00 - 15.30 Refining indications for PCNL T. Knoll, Sindelfingen (DE) Management of complications in PCNL S. Lahme, Pforzheim (DE) 16.00 - 17.30 Update on stone management Chairs: J. Reis-Santos, Lisbon (PT) R. Swartz, Örebro (SE) Post-Ureteroscopic Lesions M. Schönthaler, Freiburg (DE) Mechanical pushing and pulling forces during URS Ø. Ulvik, Bønes (NO) Compliance to prophylaxis in remal stone formers can we do better? A. Trinchieri, Lecco (IT) What does the urologist ask the nephrologist N. Buchholz, London (UK) What does the nephrologist ask the urologist? G. Gambaro, Rome (IT) Outcome of stone treatment: What is the most suitable definition of stone free S. Lahme, Pforzheim (DE) HOT workshop 1 - URS & laser Chairs: R. Swartz, Örebro (SE) O. Traxer, Paris (FR) Which scope? A. Papatsoris, Athens (GR) How to improve RIRS outcome: Update on laser settings and irrigation O. Traxer, Paris (FR) Complications of URS P. Geavlete, Bucharest (RO) Hands-on model training Thursday, 5 September 2013 08.30 - 08.35 14.00 - 15.30 Imaging in pediatric urolithiasis T.B.C. Upper urinary tract pain management K. Venborg Pedersen, Fredericia (DK) 15.30 - 17.30 Poster Session 9: Stones in animals / Clinical therapy in humans / Guidelines Chairs: T. Bach, Hamburg (DE) C. Türk, Vienna, (AT) What’s new in the EAU Urolithiasis guidelines C. Türk, Vienna, (AT) Lessons learnt from animals W. Robertson, London (UK) 16.00 - 17.30 Workshop 4: Non-surgical stone treatment Chairs: G. Gambaro, Rome (IT) B. Hess, Zürich (CH) Dietary management of urolithiasis: What are the evidence? R. Siener, Bonn (DE) Medical management: What are the evidence? B. Hess, Zürich (CH) Chronic kidney disease and urolithiasis G. Gambaro, Rome (IT) Patient education D. Kok, Rotterdam (NL) Case discussions Saturday, 7 September 2013 08.30 - 09.10 Keynote lectures 2 Chairs: D. Kok, Rotterdam (NL) P. Osther, Fredericia (DK) K. Sarica, Istanbul (TR) 08.30 - 09.10 Debate: Urinary saturation in stone disease: Casual or Causal? Casual: W. Robertson, London (UK) Causal: H-G. Tiselius, Stockholm (SE) 09.10 - 10.10 Race, Urolithiasis and Diversity Chairs: H. Ather, Karachi (PK) N. Buchholz, London (UK) B. Hess, Zürich (CH) Diversity in stone composition T. Knoll, Sindelfingen (DE) Diversity in lithogenic risk factors G. Gambaro, Rome (IT) Diversity in Stone Mangement Strategies P. Alken, Mannheim (DE) 08.30 - 10.30 HOT workshop 5: PCNL Chairs: M. Brehmer, Stockholm (SE) E. Liatsikos, Patras (GR) Positioning in PCNL C. Scoffone, Turin (IT) Imaging and access M. Brehmer, Stockholm (SE) Stone fragmentation E. Liatsikos, Patras (GR) Future aspects of PCNL A. Hoznek, Creteil (FR) Hands-on model work 10.30 - 10.40 Best published paper lecture 10.40 - 11.05 Souvenir session 11.05 - 12.30 ESD 2014/ EULIS 2015 N. Buchholz, London (UK) J. Galan, Alicante (ES) 12.30 - 13.00 Presentation of new chairman and farewell Lunch break European Urology Today 35 Accrual Workshop MAGNOLIA trial Interactive, case-based learning activities to boost recruitment Dr. Wim Witjes Scientific and Clinical Research Director EAU Research Foundation, Arnhem, The Netherlands [email protected] Dr. Raymond Schipper Clinical Project Manager EAU Research Foundation, Arnhem, The Netherlands trial is challenging, involving different disciplines (urology, oncology, radiology and pathology) and is targeted at a complex patient population. The workshop was designed for investigators and their research staff to discuss the recruitment challenges and exchange ideas how to efficiently organize, identify and manage patients for the study. The three-hour programme started with updates on the study status and recruitment strategies. Two presentations by Prof. Colombel (Lyon, FR) and Dr. Peter Goebell (Erlangen, DE) provided the audience with strong arguments to give priority to the MAGNOLIA study instead of neo-adjuvant chemotherapy and adjuvant chemotherapy. Prof. Llorente (Alcorcon, ES) and Prof. Colombo (Milan, IT) presented and discussed patient cases to identify the appropriate patients based on the trial’s inclusion and exclusion criteria and highlighted the importance of a coordinator who oversees all study activities and can initiate and accelerate study procedures within the participating hospital. In the second part of the workshop the participants were split in groups to discuss a particular theme (ICF procedures, Screen Failures, Pathology). These sessions yielded important information on the challenges that sites are facing to recruit patients and the possible actions that can be undertaken to enhance accrual. patients and their family was considered crucial. Furthermore, the use of the TUR material would definitely improve the quality of the samples and the number of samples available for the MAGE-A3 expression. The output of the discussions will be compiled in a report that will be sent to all MAGNOLIA sites. The meeting participants enthusiastically commented on the workshop and said that the programme was informative and interesting. Similar meetings will also be organised on a national level in the future. For making this first Accrual Workshop very inspiring and successful, the EAU-RF thanks all speakers and participants! There was a consensus about the need to have a shortened set of information for the patients like a patient leaflet and to add an inclusion/exclusion checklist to the first ICF. In addition to the actions on the ICFs, an optimal collaboration between the study For more information on the MAGNOLIA study please staff and the patients to answer all questions from the visit the website: http://magnolia.uroweb.org r.schipper@ uroweb.org The EAU Research Foundation (EAU-RF) held its first Accrual Workshop for the MAGNOLIA study last March 16 in Milan, Italy, coinciding with the 28th Annual EAU congress. The meeting generated a high level of interest and was well attended by 55 delegates from 37 sites of all participating countries (Germany, France, Spain, Italy, The Netherlands, Poland, Czech Republic, Romania, Ukraine, Russia) including PI’s, sub-investigators, research coordinators, research nurses and pathologists. The MAGNOLIA study is a double-blinded phase II trial in which the safety and efficacy of antigen specific cancer immunotherapy with recMAGE-A3 + AS15 in patients with muscle invasive bladder cancer after radical cystectomy is evaluated. The MAGNOLIA EAU Research Foundation Group photo of the participants of the MAGNOLIA Accrual Workshop in Milan Prostate and kidney dilemmas EMUC2013 Amsterdam to host 2nd International Conference Current controversies, challenging treatment dilemmas and recent developments on prostate and kidney cancers will be the focus of the 2nd International State-of-the-Art Conference on Prostate and Kidney Cancers. To be held in Amsterdam from 26 and 27 September, the two-day conference will gather some of the world’s leading experts on prostate and kidney cancers to the Dutch capital to carefully examine current treatment strategies, best practices and prospects for optimal management. “The two-day conference will provide a clinicallybased overview of the current therapeutic dilemmas with an emphasis on the opportunities for multidisciplinary management. Topics are current controversies, recent developments in the field, and complex cases, in addition to the cutting edge research and the latest developments,” said the Scientific Committee of the European Uro-Oncology Group. The meeting will not only enable clinicians to stay up-to-date with new information on daily clinical practice, but the meeting will also provide a comprehensive and concise insight into the state-of-theart approach to treating prostate and kidney cancers. “There will be interactive discussions to engage the participants, and programme will appeal to the practicing physician and scientists in many ways,” said Prof. Susanne Osanto (NL), who leads the organising committee. 36 European Urology Today Moreover, specialists such as medical oncologists will have an opportunity to meet recognized experts who will provide updates on both the scientific and clinical aspects of genito-urinary cancers. “We aim that these updates will have an immediate impact on clinical practice or current research efforts,” added Osanto. Some of the topics to be discussed are optimal treatment of localized renal cell carcinoma (RCC), metastatic RCC, surgery in oligometastatic RCC, localized prostate cancer (PCa), treatment of oligometastatic disease, metastatic PCa, contemporary approaches, and clinical metastases and response assessment issues in clinical trials To be held at the InterContinental Amstel Hotel Amsterdam, EACCME accreditation will be requested for 12 points. Further information and queries can be sent to [email protected] or access the website at http://euog.org/ 5th European Multidisciplinary Meeting on Urological Cancers Embracing Excellence in Treatment of Prostate, Bladder and Kidney Cancer From guidelines to personalised medicine 15-17 November 2013, Marseille, France Abstract deadline: 8 July 2013 www.emuc2013.org Organised by March/May 2013 www.reviews Dr. Andrea Cestari Section Editor Milan (IT) journal articles in urology right to your desktop, smartphone, or tablet. The content available on PracticeUpdate has already been vetted by the top minds in urology and filtered to match the specific areas of interest to the reader or user.Registering is very easy and free of charge and it is worthwile to have a log-in account for easy access. [email protected] www.ehealthcareers.com/ www.practiceupdate.com/ urology As practising urologists, we are all aware how challenging it can be to know what really matters to our practice, particularly with the volume of constantly evolving information that are available in the web. The new “PracticeUpdate” website created by Elsevier is a valuable new online tool that provides access to information of great interest to urologists, and presented in a very convenient and attractive manner. As you go through the pages of this website, one realises that there’s no need to waste time skimming journal articles, jumping from site to site in order to stay on top of what’s happening in urology. PracticeUpdate does all the work for you. It delivers the latest, most pertinent news, developments and Are you planning to look for a job in the United States? Or are you searching for a fellowship programme as well? This website will be probably of help. eHealthCareers.com brings you the latest urology jobs straight from the pages of The Journal of Urology . Once registered, and when you set up job alerts from this website, you’ll see or receive alerts only on the jobs you’re interested in. After you provide information on specialty and location, the website will send an alert when a matching job gets posted. Moreover, it is possible to directly scroll for detailed information on a particular job or position posted on this website. The website also features videos, articles and provides an accelerated job search. Users can also post their resumes, and prospective employers are also featured to highlight their services and vacancies. Certainly, for a one-stop website focused on a comprehensive job search ehealthcareers is a helpful and convenient tool to have in your desktop. http://cem.uroweb.org EAU 13th Central European Meeting (CEM) 4-6 October 2013, Prague, Czech Republic EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations Call for Abstracts deadline 1 August 2013 European Association of Urology www.reviews Tübingen hosts joint meeting Section offices pool efforts for an in-depth meeting http://esffu-esgurs-esou.uroweb.org By Joel Vega 2nd Joint Section Meeting of ESFFU, ESGURS and ESOU Three frontline EAU section offices have pooled efforts to organise and hold an in-depth meeting that will tackle the challenges and issues in andrology, onco-urology functional, female and reconstructive urology, marking the second time of close collaboration among these specialities. and male incontinence, surgical treatment of prostate and bladder cancers, surgical troubleshooting in neobladder complications and medical strategies for incontinence. Live surgeries will also be scheduled during the meeting with moderated sessions that will demonstrate surgical procedures such as radical cystectomy and prostatectomy, surgical options for Tübingen, Germany will host from October 10 to 12 this male and female incontinence, anterior and posterior year the 2nd Joint Section Meeting of the EAU Section of urethroplasties, and troubleshooting procedures in Female and Functional Urology (ESFFU), EAU Section of male slings, rectourethral fistulas and parastomal hernias, to name a few. Genitourinary Reconstructive Surgeons (ESGURS) and the EAU Section of Oncological Urology (ESOU). Prof. John Heesakkers, ESFFU chairman, said the “...how various specialties attempt meeting will not only shed practical insights on issues encountered by specialists on female to achieve optimal follow-up care, various and functional urology, but will also look into the impact of these procedures on diagnosis, disease prevent complications and other progression, complications, and medical options. management issues...” “Not only do we aim to present the insights and perspectives of veteran specialists, but also intend to promote a closer collaboration among young and expert practitioners. This meeting is an ideal platform for them to exchange best practices that will inform their treatment strategies,” said the organisers. With Prof. Karl-Dietrich Sievert leading local organisers, the meeting will present a scientific programme focusing on recent advances and how various surgical and medical strategies impact on the aim of urologists to provide optimal medical care. “Best practices will be presented and examined, and how various specialties attempt to achieve optimal follow-up care, prevent complications and other management issues will be thoroughly discussed and examined by an expert faculty, while opening the discussion to participants,” said Sievert. Among the issues and topics to be discussed are urethroplasty techniques, surgical options for female March/May 2013 EAU Section of Female and Functional Urology (ESFFU) EAU Section of Genito-Urinary Reconstructive Surgeons (ESGURS) EAU Section of Oncological Urology (ESOU) 10-12 October 2013, Tübingen, Germany EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations “Opinion leaders will demonstrate new techniques and look into the controversial issues ranging from surgical treatment for prostate and bladder cancers, prospects and current trends in managing incontinence, surgical troubleshooting procedures to medical options,” said Heesakkers. The organisers said one advantage of holding joint meetings with other specialities is that actual clinical challenges can be discussed in a more thorough manner, with the various opinions of experienced specialists adding depth to the discussion. A technical exhibit will also be concurrently held with the three-day event to provide an overview of new technologies used in the diagnosis and treatment of various urological diseases. The organisers also invite participants to join the abstract sessions and submit the results of their research studies. Deadline for abstract submission will be on July 9, 2013, with the final selection or outcome of the abstract review available by August. European Association of Urology European Urology Today 37 Overview report: 14th International EAUN Meeting Milan meeting draws enthusiastic approval from urology nurses The three-day 14th International EAUN Meeting in Milan last March gathered around 400 participants for a varied scientific programme that covers a range of topics including controversies in post-operative procedures to specialised nursing care of patients with urological cancers and bladder dysfunction. practice, which was very interesting to work on,” said Beije and Van Der Scheer. “We tried to inform our urology colleagues as much as possible about our patient. Presenting the case was an opportunity to share knowledge with our colleagues from other countries and to find out if we are on the right track.“ The case deals with complicated ostomy and wound care after cystectomy and Bricker deviation (with complex co-morbidity). “We don’t often see such big problems with such a good result, although together with our patients we face challenging issues every day,” they added. Ms. Dora Mair presenting at the Bladder dysfunction session Pros and cons regarding prostate cancer screening was one of the issues discussed with a panel of prostate cancer experts from Europe sharing their views on the controversial subject. Both nurses also said that they learned from the case the importance of good communication and documentation of nursing problems and interventions. “A colleague asked what we could have done differently. Our answer was that the nursing discharge document should not be open to multiple interpretations,” Beije said. “Although we thought the information we gave the patient was clear (text, European nurses visit the hospital San Raffaele Turro The revamped EAUN booth drew much attention Willem De Blok, a Dutch nurse, explained indications and preparations for cystoscopy, legal aspects, experiences of nurses practising cystoscopies, and discussed some clinical cases. The chief of the nursing department of urology gave a presentation, and mentioned that in their clinic there are two wards for urologic patients: one for the uninsured patients and another for those with insurance. The ward for patients with insurance is a VIP ward with spacious rooms and with a second bed for a family member, a large bathroom and a little lounge. A representative of Olympus Europe Holding GmbH, She also discussed the new clinical routine for robotic prostatectomy surgery, and mentioned the following points regarding the new routine: 1. No bowel washout day before operation but only a little enema in the evening and morning prior to the operation. The patient can eat normally the evening before, and in most cases the patient can also have meals after the operation; 2. No epidural painkillers or opiates after the operation; and 3. Mobilisation in bed on the day of the operation and a few hours out of bed the day after the operation. “Both nurses also said that they learned from the case the importance of good communication and documentation of nursing problems and interventions.” Roderick Van Den Bergh (NL) presented the pro-view on PSA screening while Klaus Brasso (DK) provided the opposing opinion. The presentations were later followed by a panel discussion with Brasso, Karen Flynn Thomas (IE) and Erik Van Muilekom (NL) as members. Moderated by Van Den Bergh, the panel carefully examined the benefits of early detection, while weighing its drawbacks in some groups of patients. The results of the new clinical routine for robotic prostatectomy Jury members Jerome Marley, Veronika Geng and Michael Borre watch the presentation of a research plan in the Research Plan Competition session photos), it led to problems. Sometimes, (whenever possible) bedside teaching could be a solution.” “The truth probably lies somewhere in the middle,” said Van Den Bergh. He added: “PSA screening at a population level reduces PCa mortality by 21 to 29%, while at the same time PSA screening results in a large over-diagnosis of 50%.” Comments from the audience also indicated that patients’ views must be carefully considered as some patients prefer active treatment from doctors over so-called watchful waiting strategies. Video abstract session The video abstract session “Inside the body: Surgery in Motion,” a new feature in the EAUN programme also received high praise in post-meeting surveys. Several participants remarked that this session was very interesting and instructional and should definitely be repeated in Stockholm. Presenting a difficult case Two Dutch nurses, Marjette Beije and Alice Van Der Scheer from the Netherlands Cancer Institute (NL), presented a difficult case in the session “Nursing solutions in difficult cases & case discussions” this year and enthusiastically shared their experience. “In Milan, we presented a difficult case from our daily From left: Particpants Enzo Federico (IT) and Maria Russo (IT) with cystoscopy trainer Carmen Sommers (NL) 38 European Urology Today Sven Boettjer, presented the history and development of the equipment and the technical aspects, and introduced the scopes and the five stations that are They added that the difficult case presentation made used. In small groups, the participants performed them more aware of the role of their skills, their several tasks with various scopes. Although nurses interventions and its impact on the treatment. “Did are not likely to perform tumour resections in actual we overlook something or are there other aspects that practice, the bladder models proved very convenient could have been improved? For us it was a great and popular during the demonstrations. With the kind opportunity to examine these issues by participating help of Lisette Van De Bilt and Carmen Sommers, in Milan.” nurse practitioners (NL), the team assisted and mentored the 23 participants. They also noted that it was a challenge to present the case in English within the given time (10 minutes) A follow-up evaluation showed that the course itself, with an international audience as they were the content and the way the course was presented prompted to get straight to the main questions, which were well-appreciated. Participants commented that a actually helped to get a clear look of the main different timeslot and the use of video recordings of problems. cystoscopies of anomalies can further improve the course. Cystoscopy course: positive feedback One of the main goals of the EAUN is to fill in gaps in Overall, and with the participants giving a positive nursing education. The EAUN board considered a response, the EAUN Board is considering to again cystoscopy course for nurses as one of the needs and offer the course in next year’s programme in the course in Milan served as a test for offering an Stockholm, Sweden. Obviously, the support of the accredited course. In some countries patients are ESU and Olympus is very crucial and hopefully we will provided with a cystoscopy in a nurse-led clinic, and again collaborate with them next year. in the US, the UK, Scandinavia and the Netherlands, especially trained nurses are familiar with performing Visit to the San Raffaele Hospital cystoscopies independently. This is certainly not the Some nurses also visited the local San Raffaele and case in all countries, and as far as the EAUN is San Raffaele Turro hospitals to get an impression of concerned this need also not be the goal. urology nursing practice in Italy. Cel Vandewinkel from Belgium reported: “I and about 20 other nurses There is no doubt that nurses who run nurse-led from different countries had the luck to visit the San cystoscopy clinics are well-trained since most nurses Raffaele Hospital in Milan established 150 years ago, are trained on the job and have had their training and which used to be a psychiatric hospital. directly from the urologists in actual clinical practice. Often their training is based on the so-called “do one-see one-teach one principle.” Trained nurses recommend that offering good theoretical education should be the basis, alongside a hands-on training session. In Milan, nurses who do not perform cystoscopies themselves also proved to be interested to participate in such courses. Frank d’Ancona, a Dutch urologist, introduced the course with a lecture on anatomy and physiology of the bladder, embryology, anatomy and anomalies and pathology of the urological system. Lawrence Urodynamic examination room in the Urology department Drudge-Coates, clinical nurse specialist (UK) and Free mobilisation Gas canalisation Stool canalisation Pain VNS scale Presence of postoperative nausea Discharge after: Conventional 51h. 43h. 94h. 3,65 After clinical path 29.5h 29.5h. 88h. 1,85 13,5% 5 to 6 days 23%* 3 to 4 days *there is no compromise about the use of anesthetic medication The participants also visited the rooms where lithotripsy, cystography, changing the DJ or nephrostomy catheter and prostate biopsy and urodynamic examinations take place. The urological polyclinic was also equipped with a cardiologic consultation room with equipment for cardiac echo, cardiac effort test, etc. “On behalf of all the nurses who visited the hospital, I thank the nursing staff and the head nurses of the urology department for the very fine welcome we had in San Raffaele,” said Vandewinkel. New EAUN booth This year’s EAUN meeting also featured a revamped booth, which gave both members and non-members the opportunity to inquire about membership inquiries, future activities or simply have a meeting place. Nurses’ dinner A special nurses’ dinner with music and an informal atmosphere formed part of the social programme. However, some were unable to attend since they were unaware that registration for this event always takes place online together with the meeting registration, and is not automatically included in the registration. All in all this year’s EAUN meeting was a success in terms of attendance and quality of the programme, and many of the participants said they look forward to another instructive and insightful meeting in Stockholm. Next year’s meeting The meeting in 2014 will take place from 12 to 14 April 2014, in Stockholm, Sweden. This year’s abstract deadline will again be on the 1st of December (2013). More information on the submission of a Difficult Case or a Research Plan can be found on page 40 of this newsletter. The congress website www.eaustockholm2014. org/15th-eaun-meeting/ with more information will be available soon. We are looking forward to your submissions! March/May 2013 EAUN Fellowship addresses patient safety Berne University Hospital hosts short-term visit Kaija Tylli Registered Nurse Helsinki University Hospital Helsinki (FI) comparing practice and procedures to those of a hospital operating in a completely different environment. As a renowned Swiss hospital, the Berne University Hospital provided an ideal setting for this comparative work. [email protected] Host institution Berne University Hospital was founded in 1354. It is named Inselspital and it provides highly specialised medical care and has an international reputation of being equipped with high-technology and engaging in excellent scientific research. The hospital employs over 7,100 people (Inselspital, 2012). Helsinki University Hospital (HUCH) provides highspecialised medical care for more than a million people within the Helsinki region. The coordination of the service provision is divided between four departments: Department of Medicine, Department of Surgery, Department of Gynecology and Pediatrics, and Department of Psychiatry. The 17 HUCH hospitals form part of Helsinki and Uusimaa Hospital District (HUS). HUCH hospitals serve as training centers and provide excellent facilities for both national and international research projects. As of last year, the number of employees for the whole HUS organisation totalled to around 21,322. Inselspital has committed itself to a continuing and long-term investment in nursing development and research, and the strategy is to focus on Evidence Based Practice (EBP) for at least the last 10 years. (Willener, 2006). The Department of Nursing Development and Research has developed several standards and strategies of different nursing interventions for the whole organisation, and every clinic has adapted them to their own speciality. All patient education material is produced here. (Hirter, Shaha, 2013). (39 beds), operating theatres, Intermediate Care Unit (five beds) and a stone treatment centre (eight beds). The Department of Urology has a Clinical Nurse Specialist (CNS) who cooperates with the Department of Nursing Development and Research and is responsible for nursing development and nursing quality within the clinic. The CNS has also been part of research groups of the clinic. (Willener, 2013). The Clinical Nurse Specialist organises education in the clinic regarding current topics twice every month. To share knowledge of experienced nurses with their younger colleagues, additional short sessions (20 minutes) are organised in the ward. (Willener, 2013). “The Department of Nursing Development and Research has developed several standards and strategies of different nursing interventions for the whole organisation.” effectively identify and implement relevant procedures, every organisation needs dedicated staff that has proper resources. One possible way to support the implementation of evidence based nursing practices is to have a separate department for this. It provides a solid support for clinical work. Once proper nursing practices have been identified, their implementation in the daily work needs an ongoing effort. Ideally, every clinic should have dedicated staff for this type of work. The staff, e.g. a Clinical Nurse Specialist (CNS), is important for all aspects of nursing development and nursing quality. The CNS is an important link between research and development and the daily nursing practice: from selecting the development topic to implementing and evaluating it. The CNS could be used for nursing consultancy or as a visionary of the future. The latest strategies, evidence based nursing practices and guidelines should be easy to find in the daily practice. An up-to-date and structured Intranet is one way of providing this important source. It serves both the newcomers and the experienced nurses. It is also important to have a continuing discussion about clinical topics. These routine sessions will aid both the newcomers and the experienced nurses, and the goal of this developing work is that the nursing practices will be solid and safe. Before my visit to Berne I was in contact with the very kind and experienced CNS Mrs Rita Willener, who arranged me a versatile programme in the Department of Urology. Mrs. Willener founded the Swiss Association of Urology Nurses while being an EAUN board member. The above is supported by our own survey results. She has really done a remarkable career. (Tylli & Koskinen, 2012). Here one finding was that newcomers found it difficult to get sufficient proper Improving patient safety information needed for decision-making in nursing. I found my visit to Berne very rewarding and I learned much about patient safety. In the following I list the Even if patient safety thinking belongs to everyone in All in all the team in Clinic of Urology consists of one main points that I found during this project. the organisation, it is important to have a separate The Department of Urology in Inselspital (Fig. 1) is professor of urology, 18 urologists, six senior residents internationally renowned for its surgical techniques in unit for this. With is a systematic reporting and (residents in urology), around three junior residents evaluation system of adverse events and near-misses treating bladder and prostate cancers. The Department A clear relationship has been demonstrated between (residents in surgery), and 84 nurses, Last year, 2,392 of Urology consists of an Outpatient Clinic, two wards inadequate nurse staffing and increase in e.g. in place, patient safety can be improved. elective urologic surgical operations were done in mortality rates, urinary tract infections, pressure ulcers addition to about 250 emergency operations. and length of hospital stay. There are studies showing Acknowledgement (Matikainen, 2012). the improvement in quality of care and increase in job This visit was made possible with a grant of the satisfaction following the implementation of the European Association of Urology Nurses Fellowship mandated ratios. (Berry & Curry, 2012). My aim with this Fellowship short term visit is to Programme. improve the current patient safety culture and bring concrete improvement proposals to daily practice and Evidence based nursing is a type of evidence based Note: healthcare. It involves identifying reliable research procedures. This work greatly benefited from The references and an extended version of this article results and implementing them in nursing practices. are available on request at [email protected]. Figure 1: Clinic of Urology (Anna-Seiler Haus) at Berne The aim is to provide the highest quality of patient Please mention title, author and EUT edition March/ European Association of Urology Nurses University Hospital. care in the most cost-effective way. In order to May 2013 in your email. I work in the Clinic of Urology as a registered nurse. The Clinic of Urology covers the entire range of adult urology, from diagnose to high-specialised medical care and follow-up. The clinic consists of two Outpatient Clinics (in Meilahti Hospital and in Peijas Hospital), three wards (48 beds), operating theatres and a stone treatment center. I work mainly in the urodynamic laboratory. The Department of Risk Management organises patient safety education for all of the clinics in Inselspital, and there is a systematic reporting and evaluation system of adverse events. The reports are mostly concerned with medication. There is a system of emergency notifications if an acute defect is noticed with products or operation modes. These notifications are immediately transmitted to the Intranet. (Paula, 2013). A forward-looking urology practice Report from Tauranga, New Zealand Pene Meiklejohn Manager, Urotech Limited Tauranga (NZ) [email protected] Tauranga City, located in the Bay of Plenty region on the east coast of northern New Zealand, is one of the country’s top holiday destinations, boasting one of the sunniest climates and many beautiful beaches. Tauranga is New Zealand’s sixth largest city with an urban population of 122,000 encompassing 168 square kilometers. Around 17.4 % of the population is over 65 and the Bay of Plenty region has an estimated population of 214,910. The management of the urological health budget is unique in this region. Venturo is a joint venture partnership providing elective urological services for the Bay of Plenty. The joint venture partners are the Bay of Plenty District Health Board and Urology Bay of Plenty. Urology Bay of Plenty, in essence, is composed of the four urology doctors in Tauranga. The clinicians believed that they could provide a better and timelier service if they managed the budget and deliver the service in a different format compared to the previous system. European Association of Urology Nurses March/May 2013 The concept is based on outcome rather than output and all appropriate referrals were seen and treated within a set timeframe and with very few exceptions. Some of the factors that set Venturo apart from other hospital-managed services are the categories of referrals that are seen and treated within a fixed timeframe of two months for a First Specialist Assessment (FSA) and six months for elective surgery. To demonstrate the efficiency, in 2011 there were 877 surgical urology procedures performed at the public hospital wherein the urology team has three full day lists per week. Obviously a dedicated and efficient theatre team is available. The venture is now in its 18th year and has been at the forefront of health delivery innovation. A neighbouring region, Waikato, adopted this model soon after its development. The founding urologists of Venturo, Peter Gilling and Mark Fraundorfer, are internationally renowned for their innovation, use of technology and clinical research. This culture has been maintained with the recruitment of urologists such as Andre Westenberg and Liam Wilson. Pioneering strategy The pioneering nature of their business strategy is also evident in their medical accomplishments and opportunities. Tauranga has been the birth place of numerous surgical procedures including the invention of Holmium Laser Enucleation of the Prostate (HOLEP) for BPH. Tauranga was the first in the world to use Holmium for surgery, modifying and developing techniques and equipment to suit the HOLEP procedure. The first ever laparoscopic pubo-vaginal sling was also performed here. Other NZ first’s include laparoscopic prostatectomy, laparoscopic nephrectomy, renal cryotherapy, prostate cryotherapy, robotic prostatectomy and prostate aqua ablation. The idea of using ultrasound for performing TRUS biopsy came from Tauranga. Prior to ultrasound, the needle guide was manually employed by the doctor, meaning it was finger rather than ultrasound guided. Tauranga Urology Research Limited (TURL) was established in 1992 by Gilling and Fraundorfer and has experience in Phase I (first time ever in humans) to Phase IV (variation to the license of an approved drug etc) trials. The trials are single or multi-centre, pilot and / or multinational studies and include pharmaceutical and device studies. TURL employs a manager and three part-time research nurses. Current studies include metastatic prostate cancer, overactive bladder, robotic prostatectomy, BPH, bladder cancer and post-prostatectomy stress incontinence. A current project is a Phase I study for BPH. “...The first ever laparoscopic pubo-vaginal sling...” There are two hospitals in Tauranga, one public and the other privately owned. The private hospital (Grace) is owned and managed by Norfolk Southern Cross Ltd, a partnership between two private hospitals. Grace Hospital, which opened in 2007, has six modern operating theatres, 50 inpatient beds and a separate day-stay facility performing around 6,500 procedures per year. 30% of the Da Vinci robotic prostatectomies that are performed at Grace are for patients living out of the region. 70% of all Brachytherapy Implants are also for out-of-region patients. The publicly owned Tauranga Hospital has 349 beds including 224 beds which are available for medical and surgical patients (including critical care and coronary care). Tauranga Hospital has eight operating theatres. A committed partnership There is a strong and committed relationship between the urologists and nurses as we work together to develop new techniques and procedures. The teamwork also involves frequent development of care plans, pathways, procedural setups and patient information booklets for procedures that have never been performed. The urology nurses are appreciated and encouraged to establish in-service and study groups; funding is available for study and conference leave and communication between the doctors and nurses are informal and friendly. Generally, ‘Team Tauranga’ has a strong representation at NZ Urology Nurse Conferences. Tauranga has hosted the annual National Urology Nurses conference several times in the past decade with the most recent in 2009 when 120 delegates attended. These conferences are always a great opportunity to showcase a region, network with colleagues, establish friendships and be updated of developments in other centres. Currently three of the eight New Zealand Urology Nurses Society (NZUNS) committee members are from this region, and I serve as secretary and have been in the committee for five years. For me and many of my colleagues, urology work in Tauranga is exciting, interesting, rewarding and challenging. Come and visit us! European Urology Today 39 Join our search for Nursing Solutions in Difficult Cases If you are among those who encounter atypical cases in daily practice and have found your own solutions, we would like to invite you to take a few photos and write a standard protocol. You can download a form with a list of standard questions. The form should include a description of the problem, the nursing intervention provided, the material you have chosen to help the patient and the final results. Please note: Difficult Cases that have not been (completely) solved may also be submitted! Call for Cases Share your expertise Together with the EAUN you will share and pass on this knowledge to other nurses. The cases will be evaluated by an international expert jury. The 10 most interesting cases are presented by the authors and discussed with the audience in a special session at the 15th International EAUN Meeting in Stockholm. The EAUN will place the material on their website as a unique opportunity to learn from each other. All submissions that meet the criteria will be published on the EAUN website and in European Urology Today. Some of the Submission Criteria and Rules • TheauthorsandpresenterofthisDifficultCasemustberegisterednurses • Thetopicselectedmustbeofrelevancetourologynursinginterventionsin Difficult Cases • Thecaseisillustratedwithphotosoftheproblemandthesolution(ifany), preferably 2-5 photos • ThesolutiondescribedinthisDifficultCaseisyourownsolutionanda nursing intervention • Thecaseispresentedinacompletedsubmissionformaccompaniedbya written patient consent • WheninvitedtopresenttheDifficultCaseinStockholmyouwillpresentthe case using the EAUN Difficult Cases slides All criteria can be found at the Stockholm website: www.eaustockholm2014.org/15th-eaun-meeting How to apply • PleasecheckthespecialpageonDifficultCasesubmissionatthecongress website for full details. • For more information you can contact the EAUN Office at [email protected] Submission deadline: 1 December 2013 Nursing Solutions in Difficult Cases Join our search for the best nursing solutions! We are looking forward to your contributions! European Association of Urology Nurses Nursing research may bring the most amazing results With the EAUN’s commitment to support innovative work, we invite you to submit a research project proposal for the EAUN Nursing Research Competition. During the 15th International EAUN Meeting in Stockholm (12-14 April 2014), all projects of the nominees will be discussed in a scientific session, enabling all participants to learn through feedback and discussions. A winner, chosen from the six final nominees selected by a jury, will receive € 2,500 to (partly) fund the research project. The 10 best cases will be granted a free registration for the 15th International EAUN Meeting in Stockholm, 12-14 April 2014 Call for Research Projects Eligible participants have to comply with the following: • Onlyregisterednursescansubmitaresearchproject • Theprojecthasnotstartedatthetimeofsubmission • Theresearchandthepresentationhavetobedonebyanurse • Thetopicselectedmustbeofrelevancetourologicnursing • Theresultsoftheprize-winningresearchprojectwillbepublishedin EuropeanUrologyTodayandontheEAUNwebsiteandthewinneris invited to submit an abstract for the next International EAUN Meeting. Consider the following guidelines before you start writing your research protocol: • Isyourresearchquestionclearandwhydoesitmatter? • Howwillyouaddressthisquestion?(i.e.whatmethodswillyouuse?) • Howimportantisthisactivitytourologicnursing? • Areyourresearchmethodsappropriate? All criteria can be found at the Stockholm congress website (from 1 May 2013): www.eaustockholm2014.org/15th-eaun-meeting How to apply • Please check the congress website www.eaustockholm2014.org for full details. • [email protected] Submission deadline: 1 December 2013 We hope that you will not miss this opportunity. Remember, nursing research small or large can still change the urological world! EAUN Nursing Research Competition € 2,500 grant to be awarded at the 15th International EAUN Meeting in Stockholm, 12-14 April 2014 40 European Urology Today March/May 2013
© Copyright 2026