J M Arnold, J P Ribeiro and W S Colucci 1990;82:465-472
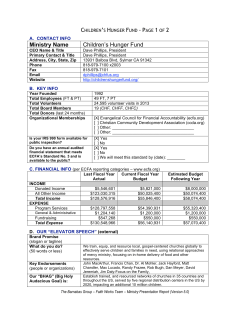
Muscle blood flow during forearm exercise in patients with severe heart failure. J M Arnold, J P Ribeiro and W S Colucci Circulation. 1990;82:465-472 doi: 10.1161/01.CIR.82.2.465 Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1990 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7322. Online ISSN: 1524-4539 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circ.ahajournals.org/content/82/2/465 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation is online at: http://circ.ahajournals.org//subscriptions/ Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014 465 Muscle Blood Flow During Forearm Exercise in Patients With Severe Heart Failure J. Malcolm 0. Arnold, MD, Jorge P. Ribeiro, MD, DSc, and Wilson S. Colucci, MD Muscle fatigue is a prominent symptom in patients with chronic heart failure (CHF). To determine whether it results from an intrinsic abnormality of vasodilating capacity of the vasculature in exercising muscle, we studied local forearm blood flow (FBF) during exercise in 13 patients with severe CHF and in eight normal untrained subjects of similar age. Intermittent forearm static exercise was performed by squeezing a hand dynamometer for 5 seconds, three times per minute, for 5 minutes at 15%, 30%, and 45% of maximum voluntary contraction. FBF was measured by mercury-in-rubber strain gauge venous plethysmography at baseline before exercise and during the last 3 minutes of each exercise stage. Exercise was repeated after 24 hours of intravenous administration of milrinone in the patients with CHF. FBF increased with forearm exercise in a reproducible manner during 24 hours in the normal subjects: rest, 2.54±0.23 (0 hours), 2.90±0.23, (24 hours); 15%, 7.25±0.92, 5.85±0.56; 30%17, 9.20±1.08, 10.05±0.85; 45%, 14.62±1.64, 13.85± 1.09 ml/100 mllmin;p=NS, 0 versus 24 hours. In patients with CHF, FBF was reduced at baseline compared with normal subjects (1.70±0.15 ml/100 ml/min, p<0.05), but no significant differences from normal subjects were observed during exercise (15%, 5.04+0.65; 30%, 7.64±0.99; 45%, 12.56+1.20 ml/100 mlmin). Peak exercise blood flow was correlated negatively with central venous pressure (r=-0.65, p<0.05) and positively with right ventricular ejection fraction (r=0.59, p<0.05). Twenty-four hours of intravenous milrinone administration did not significantly alter FBF during exercise. Similar results were seen for forearm vascular resistance and percent forearm oxygen extraction. The exercise protocol did not significantly increase cardiac output in CHF patients (n=4) (baseline, 3.93±0.77; 45%, 4.05±0.63 1/min; p=NS). Because FBF was not significantly reduced during submaximal forearm exercise in patients with severe CHF or improved by milrinone therapy, we conclude that 1) a reduction in vasodilator capacity is not limiting at submaximal work loads, and 2) an improvement in submaximal functional performance with milrinone may not be secondary to increased intrinsic vasodilation of muscle vasculature during exercise. Alternative explanations for muscle fatigue during whole-body exercise may include inadequate cardiac output response or abnormalities in muscle metabolism. (Circulation 1990;82:465-472) In patients with chronic heart failure (CHF), exercise capacity is usually limited by symptoms of dyspnea or fatigue. If the exercise is gradual rather than abrupt in its onset and severity, fatigue is more likely to result.' The specific cause of fatigue remains unclear, but decreases in nutritive blood flow,2,3 changes in muscle metabolism,45 and histological muscle fiber atrophy6 have been implicated. From the University of Western Ontario (J.M.O.A.), London, Ontario, and the Cardiovascular Division (J.P.R., W.S.C.), Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, Massachusetts. Supported in part by the Heart and Stroke Foundation of Ontario, grant AN 1006. J.M.O.A. is a PMAC Career Health Scientist. Address for correspondence: J. Malcolm 0. Arnold, MD, FRCP Edin, FRCPC, FACP, Cardiology Division, Victoria Hospital, 375 South Street, London, Ontario N6A 4G5, Canada. Received October 11, 1988; revision accepted March 20, 1990. Peripheral blood flow is reduced at rest in patients with CHF.78 During upright exercise, blood flow to an exercising limb remains reduced,2 but this could be due to either a reduction in cardiac output and arterial pressure or increased vascular tone. By studying forearm blood flow (FBF) during forearm exercise in patients with CHF, it should be possible to differentiate these two contributions. However, Zelis et a19 in a group of patients with severe rheumatic heart disease and fluid retention (New York Heart Association [NYHA] functional classes III and IV) found an inadequate arteriolar dilation during forearm exercise, whereas Wilson et al'0 suggested that vasodilation was not intrinsically impaired in patients with nonedematous CHF (NYHA classes II and III). Our present study was designed to address two issues: 1) Is blood flow to a single exercising forearm limb reduced in patients with severe CHF? 2) Does Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014 466 Circulation Vol 82, No 2, August 1990 TABLE 1. Characteristics of Study Patients With Chronic Heart Failure Duration of Evidence of NYHA LVEF RVEF symptoms peripheral Patient class (yr) (%) (%) edema (mo) 1 65 IV 7 25 60 None 2 43 IV 24 13 39 + + +/4 3 IV 72 16 18 36 + +/2 4 51 IV 15 NA 60 None 5 43 III 17 47 9 None 64 6 III 21 65 68 +14 7 32 IV 16 9 43 None 56 8 6 14 26 IV +/4 9 40 III 13 39 15 +/4 44 16 34 21 10 III None 8 11 69 55 11 IV +/4 9 70 15 12 IV 24 ++/ 10 53 35 15 13 IV None CHF, chronic heart failure; NYHA, New York Heart Association; LVEF, left ventricular ejection fraction; RVEF, right ventricular ejection fraction; CAD, coronary artery disease; DCM, dilated cardiomyopathy; NA, could not be Age Etiology of CHF CAD DCM CAD DCM CAD CAD DCM DCM DCM CAD CAD DCM CAD analyzed. milrinone, a new positive inotropic vasodilator that improves functional exercise capacity acutely,11,12 improve blood flow during exercise because of peripheral vasodilation? Methods Study Population We studied 13 patients with CHF (11 men and two women) who had a mean age of 54±4 years (range, 32 to 72 years) (Table 1). The etiology of CHF was coronary artery disease in seven and idiopathic dilated cardiomyopathy in six. All had severe left ventricular dysfunction with a mean left ventricular ejection fraction of 13.7±1.5% (range 6 to 24%) by radionuclide gated blood pool estimates. All patients had a documented clinical history of CHF (NYHA functional class III [n=4] or IV [n=9]), were receiving digoxin and diuretics, and had been clinically stable for at least 2 weeks. At the time of study, none had decompensated left ventricular failure. Eight normal subjects (seven men and one woman) of similar age (mean, 49±3 years; range, 38 to 66 years) served as our control group. All were untrained, drug-free subjects with a sedentary lifestyle and had no evidence of heart disease by clinical history, physical examination, electrocardiography, or chest radiography. The protocol was approved by the Human Subjects Review Committee of the institutions, and written, informed consent was obtained. Protocol CHF patients had been on a 2-g sodium diet and a stable dose of medications for at least 3 days before enrollment. All vasodilators were then withheld for at least 48 hours before study, and digoxin and diuretics were withheld on the morning of the study. A flow-directed triple lumen thermodilution catheter was inserted into the pulmonary artery through the right internal jugular vein on the first morning of the study in the CHF patients only. An intravenous catheter was inserted into an antecubital vein in the dominant arm of all subjects, and the tip was advanced 6 in. proximally to sample mixed venous blood draining the forearm. Maximum voluntary contraction of the dominant forearm was measured with a hand dynamometer (Jamar, Alimed, Boston, Mass.). Arterial pressure was measured in the opposite arm through an intra-arterial line in the CHF patients and with a semiautomated indirect recorder (Dinamap 845XT, Critikon, Tampa, Fla.) in the normal subjects. All studies were performed in a quiet, temperature-controlled environment (22-24° C) after an overnight fast. Patients and normal subjects were recumbent with head and shoulders comfortably supported. After 30 minutes of rest, baseline measurements of heart rate, blood pressure, cardiac output, pulmonary capillary wedge pressure, and FBF were obtained. FBF was measured with a mercuryin-Silastic rubber strain gauge applied around the dominant forearm, which was comfortably supported above the level of the heart.13 A wrist cuff was inflated to 200 mm Hg 1 minute before recordings to exclude hand blood flow.14 A venous occlusion pressure of 40 mm Hg was used in the upper arm cuff, and FBF was measured as the slope of the change in forearm volume. The venous cuff was inflated for 5-10 seconds for each flow measurement, then released. The mean of at least six flows was obtained at each measurement time. The mean of two sets of baseline flows was used as the control flow. After a stable hemodynamic baseline had been obtained, forearm exercise was commenced and consisted of repetitive contractions on the hand dynamometer maintained for 5 seconds and released for Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014 Amold et al Muscle Blood Flow During Forearm Exercise 15 seconds, similar to that described by Zelis et al.9 Exercise was performed for 5 minutes at 15%, 30%, and 45% of maximum voluntary contraction. All patients and normal subjects were able to complete the full protocol, but some required encouragement because of fatigue. No patients complained of painful muscles, although some normal subjects complained of discomfort in the hand during the last minute of exercise after inflation of the wrist cuff. Hemodynamics and FBF were measured during the last 3 minutes of each exercise stage, and FBF was measured during relaxation between contractions as described and validated by Longhurst et al.15 Oxygen saturation of mixed venous blood (Hemoximeter OSM2, Radiometer, Copenhagen) draining the exercising forearm was measured before and at the end of each exercise stage (immediately after the last flow measurement, during muscle relaxation). Arterial oxygen saturation was measured from the intra-arterial line in CHF patients and from a warmed earlobe capillary sample in the normal subjects. In five CHF patients, arterial samples were taken before exercise and at the end of each stage of exercise, but no significant change in oxygen saturation was observed with this forearm exercise protocol (rest, 95.5±0.9%; 15%, 94.7±1.2%; 30%, 94.1±1.3%; 45%, 95.0±0.7%). Therefore, in subsequent patients and normal subjects, arterial oxygen saturation was measured before exercise only. Normal subjects were restudied in an identical fashion 24 hours later. Intravenous and arterial lines were left in situ in the CHF patients who received a 48-hour intravenous infusion of milrinone (50 gg/kg during 10 minutes, 0.25 or 0.5 ,gg/kg/min for 6 hours, 0.5 ,ug/kg/min to 48 hours) during which repeat forearm exercise testing was performed at 24 hours. Plasma milrinone concentration between 24 and 48 hours of infusion was 166±18 ng/ml. The full hemodynamic effects of a 48-hour infusion of milrinone in these patients are reported elsewhere with the results of a multicenter trial.16 Neurohormones were assayed at rest in eight CHF patients. Plasma norepinephrine concentration was measured by a standard radioenzymatic technique17 and was 472±76 pg/ml. Plasma renin activity was measured by radioimmunoassayl8 and was 11.0±3.0 ng/ml/hr. Measured Variables Mean blood pressure was calculated as diastolic plus one third pulse pressure in the normal subjects and as the integrated intra-arterial pressure in patients with CHF. Forearm vascular resistance was calculated as mean blood pressure divided by FBF and is expressed in arbitrary units. Blood oxygen content was calculated as the product of hemoglobin concentration, 1.36 ml OJg of hemoglobin, and percent oxygen saturation. Oxygen extraction was calculated as the percent ratio of the arteriovenous oxygen difference and arterial oxygen content, and oxygen consumption (ml 01minm 100 ml) as the product of the arteriovenous oxygen difference and FBF divided by 100. Cardiac output was calculated 16 467 - 14 - 12 - (/~~~~~~~ E 6- 8 4- O L - ,- / 2- ReSt 15% 30% EXerCiSe 4596 FIGURE 1. Plot of forearmn blood flow (FBF) at rest and duting foreanm exercise in nonnal subjects stucdied on 2 consecutive days o, Day 1; *, day 2. p=NS day 1 vs. day 2. *p<.Ol FBF vs. preceding FBF on day 1. by thermodilution from the mean of at least three injections differing by less than 10%, and cardiac index was calculated as (I/min/M2). Pulmonary capillary wedge pressure was measured at end expiration. Systemic vascular resistance (dyne-*sec/cm5) was calculated as 80 multiplied by (mean blood pressure minus right atrial pressure) divided by cardiac output. Statistical Analysis Increases in FBF during exercise in normal subjects were compared by analysis of variance for repeated measures with contrasts performed with Tukey's method.19 Hemodynamic data at 0 and 24 hours were compared with paired t tests. A p value less than 0.05 was considered significant. Data from CHF patients before milrinone therapy were compared by unpaired t tests with normal subjects at day 1 and CHF patients after milrinone therapy at each level of exercise and p< 0.025 was considered significant. Linear regression was performed with the least-squares method. All values are expressed as mean-+SEM. Results To assess the reproducibility of the exercise protocol. the results from the normal subjects on the two consecutive days are shown in Figure 1. With each stage of exercise, there was a progressive increase in FBF, but no significant differences were seen between the FBFs of the two days at any level of exercise, confirming good reproducibility. Therefore, for clarity, the subsequent figures show only the normal results from day 1. To confirm that the forearm exercise protocol was p-rodcll-ingr local vascuilalr cagswithouit a change( Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014 iin Circulation Vol 82, No 2, August 1990 468 A B 16o Normals A CHF Pre MIL & CHF Post MIL 1412- FIGURE 2. Panel A: Forearm blood 60- flow (FBF) at rest and during forearm c ._ m c) 8- 40cr 0 E1 6- >c 30- 4- 20- 21 10- (I nu a 1 C 1.4- 60c x W E 1.0- E 0.8- g 40- C._ . D 1.2- 500 exercise in patients with chronic heart failure (CHF) studied before and after 24 hours of intravenous administration ofmilrinone (MIL). Panel B: Forearm vascular resistance (FVR) at rest and during forearm exercise in CHF patients studied before and after 24 hours of intravenous MIL. Panel C: Percent forearm oxygen extraction at rest and during forearm exercise in CHF patients studied before and after 24 hours of intravenous MIL. Panel D: Forearm oxygen consumption at rest and during forearm exercise in CHF patients studied before and after 24 hours of intravenous MIL. o, Normal subjects (day 1); A, pre-MIL; A, postMIL. *p<0.01, **p<0.001 vs. preMIL. Exercise is expressed as percentage of maximum voluntary contraction. 50- E10- m ' cEO 6-i 30- ( CV 20- (M 10v (l 0 oE 0.4- 0.2,. Rest U 1 15% 30% Exercise 45% . 1 Rest central pump function, hemodynamics were measured before and at peak forearm exercise before milrinone therapy in 12 CHF patients. Forearm exercise in CHF patients resulted in no significant changes in heart rate (89±3 and 90±3 beats/min), mean blood pressure (75 ±3 and 77±3 mm Hg), pulmonary artery diastolic pressure (27±3 and 28±2 mm Hg), right atrial pressure (10±2 and 10±2 mm Hg), or cardiac output (3.93±0.77 and 4.05±0.63 1/min, n=4). In normal subjects, the protocol did not increase heart rate (65 ±4 and 69±4 beats/min), and mean blood pressure tended to increase slightly (rest, 94±4; 15%, 97+4; 30%, 102±3; 45%, 107±3 mm Hg;p=0.06). FBF responses to forearm exercise in the CHF patients are shown in Figure 2A. Before milrinone therapy, FBF was reduced at rest in the CHF patients compared with the normal subjects (p<0.05); however, FBF progressively increased with exercise and was not significantly different from that in normal subjects. After milrinone therapy, FBF was significantly increased at rest, but exercise blood flow was not altered. Similar changes were seen with forearm vascular resistance (Figure 2B) and percent forearm oxygen extraction (Figure 2C), which were both increased at rest in patients with CHF. Milrinone therapy decreased forearm vascular resistance and percent oxygen extraction at rest but did not alter either variable from that seen in normal subjects at each stage of exercise. Indeed, because forearm vascular resistance was higher at rest in patients with l 15% 30% Exercise 45I% CHF than in normal subjects, yet the same at peak exercise, the reduction in forearm vascular resistance achieved during forearm exercise by patients with CHF (41.1+4.0 units) tended to be greater than that in normal subjects (31.4±3.5 units), although it did not reach statistical significance. Forearm oxygen consumption (Figure 2D) was normal in CHF patients at rest and was not altered by milrinone at rest or during exercise. Because the control group completed more physical work than the CHF group, the results are also shown in Figure 3 as the force developed with each contraction. This illustrates that the points for the control group have moved to the right and that differences from the CHF group are further reduced for FBF, forearm vascular resistance, and oxygen consumption. Percent forearm oxygen extraction remains increased in the CHF group to maintain normal oxygen consumption because hemoglobin was lower in the CHF patients (12.4 +0.5 versus 14.3+0.4 g%, p<O.Ol). FBF during exercise at 45% of maximum voluntary contraction was found to correlate negatively with resting central venous pressure and positively with resting right ventricular ejection fraction (Figure 4). No correlation was seen between exercise blood flow and resting plasma norepinephrine levels or plasma renin activity. At rest, milrinone significantly improved cardiac index (2.92±0.28 at 24 hours versus 2.12±0.25 Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014 Amold et al Muscle Blood Flow During Forearm Exercise A 469 B 6050- 1.2 - 40- *E >. 30- LL M 4- 20- 2- 10- 0- U .* C l l l A D 60- 50- o 40x 3020h10nv-.- l 10 l 20 l 30 l 40 40 30 20 Kg Kg FIGURE 3. Panel A: Forearm blood flow (FBF) at rest and during forearm exercise in patients with chronic heart failure (CHF) studied before and after 24 hours of intravenous administration of milrinone (MIL). Panel B: Forearm vascular resistance (FVR) at rest and duringforearm exercise in CHFpatients studied before and after 24 hours of intravenous MIL. Panel C: Percent forearm oxygen extraction at rest and during forearm exercise in CHF patients studied before and after 24 hours of intravenous MIL. Panel D: Forearm oxygen consumption at rest and during forearm exercise in CHF patients studied before and after 24 hours of intravenous MIL. o, Normal subjects (day 1); A, pre-MIL; A, post-MIL. *p<0.01, * *p<0. 001 vs. pre-MIL. Exercise is expressed as force developed (kg) with each contraction. Rest 1/min/m2 preinfusion, p<0.005) with a reduction in systemic vascular resistance (1,061 + 110 at 24 hours versus 1,382±143 preinfusion, p<0.01). Milrinone therapy tended to reduce pulmonary capillary wedge pressure (20.4± 1.4 versus 23.7± 1.8 mm Hg) and right atrial pressure (7.0±+1.3 versus 8.4±1.9 mm Hg), with small increases in mean blood pressure (72.1±2.5 versus 70.9±3.9 mm Hg) and heart rate (90.2±3.4 versus 86.1±3.0 beats/min), but these changes were not significant. Discussion Using a reproducible protocol of forearm exercise that did not cause significant central hemodynamic changes in patients with severe CHF, we showed no difference between CHF patients and normal subjects of similar age in the ability of their forearm vasculature to dilate and increase blood flow during exercise. This occurred even though their exercise functional capacity by clinical assessment was significantly reduced and suggests that the development of fatigue during exercise may not primarily result from an intrinsic defect in the vasodilating capacity of the muscle vasculature. This conclusion is supported by the observation that milrinone, a drug known to improve exercise capacity acutely in patients with CHF, although producing vasodilation at rest, did not improve vasodilation during forearm exercise. The protocol used in this study required exercise to 45% of maximum voluntary contraction for 5 minutes, and the end point was not chosen to be maximum symptom-limited exercise capacity. However, all patients and normal subjects complained of fatigue during the protocol, and submaximal exercise may be more relevant to a patient's performance of activities of daily living than maximal exercise. The protocol was designed to be similar to that described by Zelis et al,9 except that we adjusted the strength of contraction to allow for different muscle mass in individual patients. If the present results are considered as force developed, then the patients with CHF generated less force but had a similar vasodilation to normal subjects, further supporting the conclusion that the ability of their forearm muscle vasculature to dilate was not impaired. Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014 470 Circulation Vol 82, No 2, August 1990 24- r= -0.65 p<0.05 20- Qc 0 >'g16- i 8- UIDO 12- 0 0 0Z El~~~~~~ 0 8~~~~~~~~~~~~~~~~~~~~1 IL- 4a l X 4 8 12 16 24 20 CVP mmHg 24- 20f _E 16ae E g 12L L ?- E 8r = p< 4- 0.59 0.05 ut e 0 20 40 RVEF % 60 FIGURE 4. Plots of correlation ofpeak forearm blood flow (FBF) during forearm exercise at 45% of maximum voluntary contraction (MVC) with central venous pressure (CVP) and right ventricular ejection fraction (RVEF) in patients with chronic heart failure. This type of forearm exercise increased local muscle blood flow but did not increase cardiac output in the CHF patients. This represents an approximate 10 ml/min increase in FBF per 100 ml forearm volume. If the average forearm volume is 1,000 ml, then cardiac output would have been expected to increase 100 ml/min or 0.1 1/min. This is less than the measurement error of the thermodilution technique, and therefore, we cannot confirm whether the local increase in FBF resulted from a true central increase or merely a redistribution of cardiac output. Despite similar protocols, our conclusions differ from those of Zelis et a19 and may reflect the subset of patients they studied, all of whom had rheumatic heart disease and clinical evidence of right ventricular decompensation with fluid retention. Diuresis alone in these circumstances improves vasodilator reserve capacity.20 We did find a correlation between peak exercise blood flow and right ventricular dysfunction, as reflected by central venous pressure and right ventricular ejection fraction. This is of interest because right atrial pressure is known to negatively correlate with survival,2' and right ventricular rather than left ventricular ejection fraction correlates with upright exercise capacity in CHF.22 Although increased central venous pressure could be associated with increased tissue sodium and water retention and a decrease in vasodilator capacity, in an experimental animal model of heart failure induced by rapid atrial pacing, modest increases in mean right atrial pressure with evidence of some fluid retention and increased muscle water content were not associated with a decrease in peripheral arterial vasodilation.23 The degree of fluid retention was variable among the animals, and the investigators did not report a correlation between degree of fluid retention or central venous pressure and vasodilator capacity. Thus, it remains possible that the decrease in exercise blood flow seen by Zelis et a19 reflected local tissue edema secondary to the very high venous pressures present in their patients.24,25 Severe heart failure is also associated with neurohormonal activation,26,27 and plasma norepinephrine has been shown to correlate positively with right atrial pressure.28 This neurohormonal activation could be a further independent influence on vasodilator capacity, although we found no association with plasma norepinephrine levels or plasma renin activity in our patients. Another consideration is that venous plethysmography assumes the veins are empty at rest. With high right atrial pressures, this may not be so, and thus, further small increments in forearm volume during intermittent venous occlusion may be operating on a flattened portion of the venous pressurevolume curve,29 thus underestimating forearm blood flow. However, significant flattening of the curve does not occur until pressures higher than 20 mm Hg, and this elevation of right atrial pressure was present in only one of our patients. Our results support the observations of Wilson et al,10 who studied a group of nonedematous patients with less severe clinical heart failure (NYHA classes II and III) than our population, but they used a different protocol of forearm exercise. Blood flow responses in the forearm30 and biochemical alterations within the muscle31 can be dependent on the exercise protocol used. However, Wilson et al10 also found increases in blood flow to be similar between normal subjects and patients, suggesting that the reduced vasodilation seen by Zelis et a19 is more likely to be due to the edematous condition of the patients they studied rather than to differences in exercise protocol. In addition, our observations on the effects of milrinone further support the conclusion that improvements in exercise capacity of patients with compensated severe heart failure may not be mediated through alterations in the intrinsic vasodilator capacity of muscle blood vessels. Our results differ from those of LeJemtel et al,3 who compared one-leg with two-leg maximal bicycle exercise and concluded that the ability of the muscle vasculature to vasodilate is impaired in patients with CHF. However, oxygen uptake was significantly increased in their model, and thus, changes in cardiac output could have influenced their measurements of blood flow. Sullivan et a132 also studied leg blood flow Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014 Amold et al Muscle Blood Flow During Forearm Exercise during maximal upright bicycle exercise and found evidence of reduced perfusion at rest and during exercise. Because nonleg blood flow and arterial pressure were preferentially maintained during exercise at the expense of leg hypoperfusion, they concluded that a reflex-mediated peripheral vasoconstriction may occur in the exercising limb in the setting of an inadequate cardiac output response. Our findings complement the results of this study, because we studied a small muscle mass, without a change in cardiac output, and found no intrinsic abnormality in vasodilator capacity with exercise. Improved functional capacity after vasodilator therapy in CHF could occur through other mechanisms such as increased cardiac output. During whole-body upright exercise, this could maintain muscle perfusion and perhaps performance. Thus, our results are not inconsistent with previous observations during upright exercise that blood flow to exercising skeletal muscle is reduced in CHF2 and improved by long-term administration of drugs such as captopril that increase maximum oxygen uptake.33 Muscle fatigue and decreased performance may also involve alterations in skeletal muscle metabolism with increased phosphocreatine depletion and low pH.455Two studies in patients with heart failure have suggested that these changes do not appear to be secondary to impaired blood flow or muscle atrophy.34'35 Also, of interest, in a rat model of myocardial infarction and acute heart failure, milrinone preferentially increased blood flow to oxidative rather than glycolytic working muscle during maximal treadmill exercise.36 Hence, although total FBF was not increased in our patients, milrinone may improve the distribution between oxidative and glycolytic muscle fibers. If oxidative muscle fibers were to have better resistance to fatigue compared with glycolytic fibers, then this would be clinically helpful. In summary, we found no impairment in the ability of the local vasculature to dilate during submaximal, intermittent forearm static exercise in patients with compensated severe CHF despite the presence of mild-to-moderate peripheral edema in some patients. Milrinone did not further increase exercise forearm blood flow. We conclude that impairment of functional exercise capacity in patients with CHF is unlikely to be due primarily to an intrinsic vasodilator abnormality of muscle blood vessels. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. Acknowledgments We acknowledge the expert help of Diane Gauthier, BSc, RN, Gail Burton, RN, Gordon Marchiori, PhD, and the excellent secretarial assistance of Paula Hugin and Dale Arts. References 1. Lipkin DP, Canepa-Anson R, Stephens MR, Poole-Wilson PA: Factors determining symptoms in heart failure: Comparison of fast and slow exercise tests. BrHeartJ 1986;55:439-445 2. Wilson JR, Martin JL, Schwartz D, Ferraro N: Exercise intolerance in patients with chronic heart failure: Role of 20. 21. 22. 471 impaired nutritive flow to skeletal muscle. Circulation 1984; 69:1079-1087 LeJemtel TH, Maskin CS, Lucido D, Chadwick BJ: Failure to augment maximal limb flow in response to one-leg versus two-leg exercise in patients with severe heart failure. Circulation 1986;74:245-251 Wilson JR, Fink L, Maris J, Ferraro N, Power-Vanwart J, Eleff S, Chance B: Evaluation of energy metabolism in skeletal muscle of patients with heart failure with gated phosphorus-31 nuclear magnetic resonance. Circulation 1985;71:57-62 Massie B, Conway M, Yonge R, Frostick S, Sleight P, Ledingham J, Radda G, Rajagopalan B: 31P nuclear magnetic resonance evidence of abnormal skeletal muscle metabolism in patients with congestive heart failure. Am J Cardiol 1987; 60:309-315 Lipkin DP, Jones DA, Round JM, Poole-Wilson PA: Abnormalities of skeletal muscle in patients with chronic heart failure. Int J Cardiol 1988;18:187-195 Zelis R, Flaim SF: Alterations in vasomotor tone in congestive heart failure. Prog Cardiovasc Dis 1982;24:437-459 Leithe ME, Margorien RD, Hermiller JB, Unverferth DV, Leier CV: Relationship between central hemodynamics and regional blood flow in normal subjects and in patients with congestive heart failure. Circulation 1984;69:57-64 Zelis R, Longhurst J, Capone RJ, Mason DT: A comparison of regional blood flow and oxygen utilization during dynamic forearm exercise in normal subjects and patients with congestive heart failure. Circulation 1974;50:137-143 Wilson JR, Wiener DH, Fink LI, Ferraro N: Vasodilatory behavior of skeletal muscle arterioles in patients with nonedematous chronic heart failure. Circulation 1986;74:775-779 White HD, Ribeiro JP, Hartley LH, Colucci WS: Immediate effects of milrinone on metabolic and sympathetic responses to exercise in severe congestive heart failure. Am J Cardiol 1985;56:93-98 Timmis AD, Smyth P, Jewitt DE: Milrinone in heart failure: Effects on exercise hemodynamics during short term treatment. Br Heart J 1985;54:42-47 Whitney RJ: The measurement of volume changes in human limbs. J Physiol (Lond) 1953;121:1 Kerslake DM: The effect of the application of an arterial occlusion cuff to the wrist on the blood flow in the human forearm. J Physiol (Lond) 1949;108:451 Longhurst J, Capone RJ, Mason DT, Zelis R: Comparison of blood flow measured by plethysmograph and flowmeter during steady state forearm exercise. Circulation 1974;49:535-540 Anderson JL, Baim DS, Fein SA, Goldstein RA, LeJemtel TH, Likoff MJ: Efficacy and safety of sustained (48 hour) intravenous infusions of milrinone in patients with severe congestive heart failure: A multicentre study. J Am Coll Cardiol 1987;9:711-722 Peuler JD, Johnson GA: Simultaneous single isotope radioenzymatic assay of plasma norepinephrine, epinephrine and dopamine. Life Sci 1977;21:625-635 Emanuel RL, Cain JP, Williams GH: Double antibody radioimmunoassay of renin and angiotensin II in human peripheral plasma. J Lab Clin Med 1973;81:632-640 Winer BJ: Statistical Principles and Experimental Design. New York, McGraw-Hill Book Co, 1971 Sinoway L, Minotti J, Musch T, Goldner D, Davis D, Leaman D, Zelis R: Enhanced metabolic vasodilation secondary to diuretic therapy in decompensated congestive heart failure secondary to coronary artery disease. Am J Cardiol 1987; 60:107-111 Creager MA, Faxon DP, Halperin JL, Melidossian CD, McCabe CH, Schick EG, Ryan TJ: Determinants of clinical response and survival in patients with congestive heart failure treated with captopril. Am Heart J 1982;104:1147-1154 Baker BJ, Wilen MM, Boyd CM, Dinh HA, Franciosa JA: Relation of right ventricular ejection fraction to exercise capacity in chronic left ventricular failure. Am J Cardiol 1984;54:596-599 Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014 472 Circulation Vol 82, No 2, August 1990 23. Wilson JR, Lanoce V, Frey MJ, Ferraro N: Effect on peripheral arterioles of chronic fluid and sodium retention in heart failure. J Am Coll Cardiol 1988;12:202-208 24. Zelis R, Lee G, Mason DT: Influence of experimental edema on metabolically determined blood flow. Circ Res 1974; 34:482-490 25. Zelis R, Capone R, Mansour E, Field JM: The effects of short term venous congestion on forearm venous volume and reactive hyperemia blood flow in human subjects. Circulation 1978;57:1001-1003 26. Thomas JA, Marks BH: Plasma norepinephrine in congestive heart failure. Am J Cardiol 1978;41:233-243 27. Dzau VJ, Colucci WS, Hollenberg NK, Williams GH: Relation to the renin-angiotensin-aldosterone system to clinical state in congestive heart failure. Circulation 1981;63:645-651 28. Levine TB, Francis GS, Goldsmith SR, Simon AB, Cohn JN: Activity of the sympathetic nervous system and reninangiotensin system assessed by plasma hormone levels and their relationship to hemodynamic abnormalities in congestive heart failure. Am J Cardiol 1982;49:1659-1666 29. Wood JE: Factors of basic importance to the study of veins as capacitance vessels, in The Veins, Normal and Abnormal Function. Little, Brown & Co, Boston, 1965 30. Haslam RW, Cobb RB: Adaptations of forearm circulation to varied intensities and sets of heavy exercise. Med Sci Sports Exer 1983;15:349-354 31. Vollestad NK, Sejersted OM: Biochemical correlates of fatigue: A brief review. Eur JAppl Physiol 1988;57:336-347 32. Sullivan MJ, Knight JD, Higginbotham MB, Cobb FR: Relation between central and peripheral hemodynamics during exercise in patients with chronic heart failure. Circulation 1989;80:769-781 33. Mancini DM, Davis L, Wexler JP, Chadwick B, LeJemtel TH: Dependence of enhanced maximal exercise performance on increased peak skeletal muscle perfusion during long-term captopril therapy in heart failure. J Am Coll Cardiol 1987; 10:845-850 34. Wiener DH, Fink LI, Maris J, Jones RA, Chance B, Wilson JR: Abnormal skeletal muscle bioenergetics during exercise in patients with heart failure: Role of reduced muscle blood flow. Circulation 1986;73:1127-1136 35. Massie B, Conway M, Yonge R, Frostick S, Ledingham J, Sleight P, Radda G, Rajagopalan B: Skeletal muscle metabolism in patients with congestive heart failure: Relation to clinical severity and blood flow. Circulation 1987;76:1009-1019 36. Drexler H, Faude F, Hoing S, Just H: Blood flow distribution within skeletal muscle during exercise in the presence of chronic heart failure: Effect of milrinone. Circulation 1987; 76:1344-1352 KEY WORDS * heart failure * exercise, forearm * blood flow, muscle * milrinone Downloaded from http://circ.ahajournals.org/ by guest on September 11, 2014
© Copyright 2026