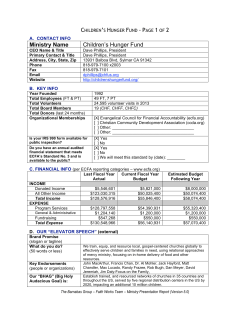
Current strategies for the prehospital care of congestive heart failure Continuing Education
Continuing Education Current strategies for the prehospital care of congestive heart failure by Bryan E. Bledsoe, DO, FACEP OBJECTIVES Upon completion of this article, the reader should be able to: • Define congestive heart failure • Distinguish between right heart failure and left heart failure • Distinguish between congestive heart failure and cardiogenic shock • Define cardiac output and stroke volume. • Define preload and afterload • Describe the mechanisms the body uses to maintain adequate cardiac output • Describe Starling’s Law of the Heart. • Discuss the function of BNP • List factors that can lead to CHF • Describe pulmonary edema • List signs and symptoms of CHF detailing which are primarily due to right heart failure and which are primarily due to left heart failure • Discuss treatment strategies for CHF in the prehospital setting • Describe CPAP and discuss its role in prehospital care • Detail pharmacologic therapy for CHF and acute pulmonary edema • State the reason for not administering nitrates to persons who have recently taken erectile dysfunction medications photo by Kenny Navarro INTRODUCTION Congestive heart failure (CHF) is a frequently encountered emergency in prehospital care. CHF occurs when the heart becomes an ineffective pump. More than three million Americans have CHF and 400,000 new cases are identified each year. With CHF, despite failure of the heart to pump effectively, it is still able to meet the metabolic demands of the body. When the heart cannot meet the metabolic demands of the body, the condition is referred to as cardiogenic shock. The difference between these two conditions is important to understand. CHF is often classified as right heart failure or left heart failure depending on the ventricle involved. With right heart failure, the right ventricle becomes ineffective as a forward pump and fluid accumulates on the systemic circulation. With left heart failure, the left ventricle becomes ineffective as a forward pump and fluid accumulates in the pulmonary 32 Texas EMS Magazine July/August 2008 circulation. In most patients there is a combination of right heart failure and left heart failure (biventricular failure). In fact, the most common cause of right ventricular failure is left ventricular failure. CHF can also be classified as forward or backward heart failure. Backward failure results from elevated systemic venous pressure and primarily involves the right ventricle. Forward heart failure is due to reduced forward flow into the aorta and systemic arterial circulation. We typically classify CHF as either acute or chronic. Acute CHF develops relatively rapidly. Chronic CHF is that which develops over a longer period of time. Treatment strategies differ based upon whether CHF is acute or chronic. PATHOPHYSIOLOGY The heart is a highly effective pump. In a normal person, the heart beats approximately 100,000 times a day, which is 35 million times a year or 2.5 million times in a lifetime. The circulatory system is a closed system. That means that the blood can only pump out what is delivered to it. It also means that the right ventricle and left ventricle normally pump the same amount of blood with each contraction. The amount of blood pumped by the heart in one minute is called the cardiac output (CO). CO can be defined as follows: Cardiac Output (CO) = Stroke Volume (SV) × Pulse Rate. The stroke volume (SV) is the amount of blood pumped by the heart with each beat. The pulse rate is the number of times the heart beats per minute. Thus, the amount of blood the heart pumps is affected by the SV and the pulse rate. To increase CO, the body can increase the heart rate or the SV. To decrease CO, the body can decrease the heart rate or SV. Heart rate is controlled by the brain. There are several factors affecting stroke volume. First, the heart can only pump out the amount of blood it receives from the venous system. This is called the preload. If the preload is decreased, there is less blood for the heart to pump and cardiac output falls. The most common reason for a decreased preload is inadequate fluid in the circulatory system (e.g., dehydration, blood loss, spinal injury, anaphylaxis). The strength of the ventricular contraction varies based upon several conditions. For example, the more the ventricle is stretched, the stronger will be the subsequent contraction. This phenomenon is referred to as Starling’s Law of the Heart. The most common cause of ventricular stretch is increased preload. Thus, as more blood is forced into the ventricle and the more it is stretched, the greater will be the force of the subsequent contraction. There are various factors and substances that increase the strength of the ventricular contraction. These include such things as the hormones epinephrine and norepinephrine. These hormones are released by the adrenal medulla glands in response to stress (sympathetic stimulation). In addition, it has been recently discovered that the heart secretes hormones. These hormones are referred to as natriuretic peptides. Thus far, two peptides have been identified: • Atrial natriuretic peptide (ANP) is manufactured, stored, and released by atrial muscle cells in response to such things as atrial dilation and sympathetic stimulation. It primarily causes a reduction in blood volume resulting in decreased central venous pressure (CVP), cardiac output, and blood pressure. • Brain natriuretic peptide (BNP) was initially discovered in the brain. However, it is principally secreted by the ventricles of the heart in response to excessive stretching of heart muscle cells. It causes a reduction in blood volume resulting in decreased CVP, cardiac output and blood pressure. BNP levels are elevated in congestive heart failure (CHF) and have become a marker for the presence of CHF. BNP (marketed as nesiritide) can be administered as a treatment for acute decompensated CHF. Thus, in times of increased demand, various hormones, such as epinephrine, norepinephrine and others are increased to stimulate increased cardiac contraction (inotropy). When the heart starts to fail, natriuretic peptides and other hormones are Continuing Education July/August 2008 Texas EMS Magazine 33 Continuing Education released to increase cardiac contractile strength. The final factor to affect stroke volume is afterload. Afterload is the pressure in the systemic arterial system that the heart must overcome before blood moves forward. Thus, the greater the afterload, the less will be the stroke volume. In adults, preload, cardiac contractile force and afterload can impact stroke volume. Children, on the other hand, have very little capacity to change their stroke volume. Instead, they rely on changes in heart rate (chronotropy) to regulate their cardiac output. As discussed earlier, CHF occurs when the heart becomes ineffective as a forward pump. There are various causes of this. First, the heart muscle itself can become damaged through myocardial infarction. When a part of the heart is infarcted, the affected muscle dies and is replaced by scar tissue. Scar tissue cannot contract. When enough of the ventricular mass is affected, CHF occurs. When a large percentage of the ventricular mass is affected (usually > 40%), cardiogenic shock develops. Other factors can adversely affect the ability of the heart to contract. Damage can occur from various chemicals such as prolonged exposure to alcohol or cocaine. Several of the cancer chemotherapy agents (e.g., adriomycin) are known to impair cardiac function. While the causes of CHF can be numerous, most, in fact are due to hypertension and infarcts. SIGNS AND SYMPTOMS The signs and symptoms of CHF can range from subtle to overt. Generally, signs and symptoms suggest which side of the heart is involved. If the right ventricle fails, blood will accumulate and pressures 34 Texas EMS Magazine July/August 2008 will increase in the venous system. This causes edema of the legs and feet (pre-sacral area in bed-bound patients), distension of the jugular veins, engorgement and enlargement of the liver, and weight gain (due to water gain). Generally, the pulse rate will be increased to help compensate for the fall in CO. Failure of the left ventricle causes accumulation of fluid in the pulmonary system (pulmonary edema). Pulmonary edema is the accumulation of fluids in the spaces in the lungs outside of the blood vessels. This results in dyspnea, the inability to breathe while lying flat (orthopnea), and abnormal lung sounds (crackles or rales) from fluid accumulation. As more of the lungs are affected, hypoxemia will develop and the patient will develop altered mental status (e.g., agitation, confusion). If untreated, this may progress to coma and death. Often times, CHF is detected before it becomes severe and treated. Various medications are used and these tend to be quite effective. Initially, a diuretic is prescribed to help promote the elimination of water through the kidneys. Usually, furosemide (Lasix) or a similar loop diuretic is used. In addition, many patients are started on digoxin (Lanoxin). Digoxin is a cardiac glycoside that increases the strength of the cardiac contraction. Most patients are also placed on a blood pressure medication to counter some of the other body systems involved in the development of CHF. Most importantly, patients are instructed to maintain a careful diet. An increased intake of sodium or a similar substance can worsen the patient’s condition. People will have various levels of chronic CHF. These are best described by the New York Heart Association’s grading Continuing Education system (see table). NEW YORK HEART Acute CHF can ASSOCIATION SYMPTOMS develop in patients who CLASS have chronic CHF or in patients who have never No limitation of physical activity. Ordinary physical I had it. Pulmonary edema activity does not cause undue fatigue, palpitation, or (MILD) associated with CHF dyspnea (shortness of breath). can occur so quickly that Slight limitation of physical activity. Comfortable it is often called flash II at rest, but ordinary physical activity results in fatigue, pulmonary edema. With (MILD) palpitation, or dyspnea. acute CHF and pulmonary edema, patients can Marked limitation of physical activity. Comfortable III rapidly become hypoxic at rest, but less than ordinary activity causes fatigue, (MODERATE) and deteriorate. Thus, it is palpitation, or dyspnea. essential that prehospital Unable to carry out any physical activity without personnel identify the IV discomfort. Symptoms of cardiac insufficiency at rest. problem early and provide (SEVERE) If any physical activity is undertaken, discomfort is the necessary treatment. increased. The signs and Table 1. New York Heart Association CHF Functional Classifications symptoms of CHF can vary based upon which Suggestive Medications: side of the heart is principally involved. • Digoxin (Lanoxin) As mentioned previously, most • Furosemide (Lasix) patients will have some combination • Bumetanide (Bumex) of biventricular failure and will exhibit • ACE inhibitor (Vasotec, Zestril) mixed signs and symptoms. Signs and • Warfarin (Coumadin) symptoms of CHF include: (particularly with atrial Historical findings: fibrillation) • Anxiety • Long-acting nitrates (Isordil) • Weakness • Home oxygen • Lightheadedness Physical Examination Findings: • Malaise • Tachycardia (highly correlated • Nausea with CHF) • Dyspnea at rest • Peripheral edema (highly • Dyspnea on exertion correlated with CHF) • Orthopnea (inability to breathe • Jugular venous distension lying down) (highly correlated with CHF) • Paroxysmal nocturnal dyspnea • Tachypnea (spells of dyspnea at night) • Rales, crackles • Cough • Diaphoresis Past Medical History: The various findings seen in • CHF congestive heart failure all point to • Hypertension failure of the heart as an effective • Angina pectoris forward pump. As CHF worsens, • Alcohol abuse oxygen delivery to essential tissues, • Valvular heart disease such as the brain, declines and • Prior myocardial infarction July/August 2008 Texas EMS Magazine 35 Continuing Education the patient becomes symptomatic exhibiting confusion, malaise and agitation. When oxygen delivery begins to fall, the condition is emergent. Prehospital treatment strategies should be directed at correcting hypoxemia and then administering medications to improve cardiac output. PREHOSPITAL TREATMENT Over the last few years, there have been significant changes in the way CHF and acute pulmonary edema are treated. For years, the mainstay of CHF and acute pulmonary edema were morphine and a diuretic. Now, these agents are contraindicated. For example, in a Cleveland study, the administration of morphine to patients with acute decompensated CHF resulted in an increased need for mechanical ventilation, longer hospitalization, more ICU admissions, and higher mortality.1 Furosemide (Lasix), a potent diuretic, has been widely used in the treatment of CHF and acute pulmonary edema despite limited studies on its effectiveness. Studies have associated diuretic therapy for acute CHF with short-term adverse clinical outcomes, particularly at high doses, raising concerns for its toxicity.2 Some harmful effects of furosemide have been identified. Furthermore, most CHF patients are already taking furosemide and bolus administration seems to have little effect.3 Current strategies in the prehospital treatment of CHF and acute pulmonary edema include correction of hypoxemia and administration of medications to improve cardiac output. As soon as patient contact is made, EMS personnel should immediately begin the administration of 100 percent oxygen via a non-rebreather mask. This 36 Texas EMS Magazine July/August 2008 will maximize oxygen concentration and fully saturate circulating hemoglobin. After the mask is placed, monitors should be applied (e.g., 12-lead ECG, pulse oximetry, capnography, noninvasive blood pressure). A saline lock should be started. If IV access is not readily attainable, and the patient is in extremis, consider placing an intraosseous (IO) needle. For patients who have moderate to severe pulmonary edema, noninvasive ventilations should be started. In the prehospital setting this is best performed with continuous-positive airway pressure (CPAP). CPAP increases airway pressures and is effective in treating hypoxemia and pulmonary edema. CPAP is probably the single most important change in CHF treatment developed over the last few decades. It decreases the need for endotracheal intubation and is highly effective.4 CPAP is easy to administer and can be performed by EMT-Basics with appropriate training. The pharmacologic treatment of CHF and acute pulmonary edema primarily involves the use of nitrates. Nitrates, the most common of which is nitroglycerin (NTG), are vasodilators—primarily venous. NTG reduces myocardial work. Current strategies in the management of CHF call for more aggressive dosing of NTG. In fact, hypertensive patients with CHF (systolic blood pressure > 180 mm Hg) should generally receive three tablets or sprays of 0.4 mg NTG initially. CHF patients with a systolic blood pressure between140-180 mm Hg should receive two tablets or sprays of 0.4 mg NTG initially. Normotensive patients (systolic blood pressure between 90-140 mm Hg) should receive one tablet or spray of 0.4 mg NTG. Nitroglycerin should be repeated every 3-5 minutes if the systolic blood pressure remains greater than 100 mm Hg. ALS personnel should consider using intravenous NTG if allowed by local protocols. IV NTG is more predictable and effective. Topical NTG should only be used as a last resort (patient on CPAP who does not tolerate sublingual NTG). Absorption of NTG in the paste form is often unreliable and unpredictable in the emergency setting. Nitrates should not be used in patients who have taken one of the erectile dysfunction (ED) drugs. Generally, you should avoid the administration of NTG if the patient has taken sudenafil (Viagra) or vardenafil (Levitra) in the prior 24 hours or tadalafil (Cialis) in the prior 48 hours. Fatal hypotension has been reported when NTG has been administered to patients taking ED medications. Following aggressive NTG therapy, a second vasodilator is often added. The most commonly used are the angiotensin-converting enzyme (ACE) inhibitors. These include enalopril (Vasotec) and captopril (Capoten). Enalopril can be given intravenously. There is probably still a limited role for the loop diuretics such as furosemide (Lasix) in patients who have normotensive CHF and are already taking oral diuretics. The administration of BNP, marketed as nesitiride (Natrecor), can help improve cardiac output. While commonly used in the hospital setting, it is not frequently used in the prehospital setting. Studies on the effectiveness of nesitiride are mixed— but certain patients seem to benefit from administration. Patients who remain anxious after the correction of hypoxemia might benefit from a small dose of a benzodiazepine such as diazepam (Valium), midazolam (Versed), or lorazepam (Ativan). These drugs are anxiolytics and more effective on anxiety than morphine and do not have the adverse vascular effects. Patients with cardiogenic shock (systolic blood pressure less than 90 mm Hg) should receive pressor support (dobutamine or dopamine) and transport. Remember these patients may also be suffering acute coronary syndrome (ACS). They should receive aspirin and be transported, if possible, to a hospital with invasive cardiology capabilities. Continuing Education FUTURE STRATEGIES As we better understand the pathophysiology of CHF, we will develop strategies and treatments to help correct the problem. The development of CPAP has been one of the most significant improvements in CHF treatment in decades. Many patients who were previously intubated and placed on a ventilator are now being managed without intubation by CPAP. Many states and medical directors have started to allow basic EMTs, with additional training, to use CPAP and nitrates. Because CHF treatment is time-dependent, starting appropriate treatment early can save lives. Unfortunately, many hospitals do not have simple CPAP devices (although ventilators can be used in a CPAP mode). The transition to CPAP is best performed as a system (EMS and hospitals acquiring and introducing the device at the same time). That will assure that patients started on CPAP in the field can continue the same care in the hospital. Summary This discussion has been an July/August 2008 Texas EMS Magazine 37 Continuing Education overview of the current treatment of CHF. There has been a significant shift in strategy in regard to the management of CHF and pulmonary edema. Morphine should not be used and furosemide (Lasix) should be used judiciously. The mainstay of therapy should be nitrates and CPAP. This can be supplemented with other vasodilators such as ACE inhibitors.5 This presentation has been for educational purposes only. EMS personnel should always follow local protocols in regard to actual patient care issues. References 1. Peacock WF, Hollander JE, Diercks DB, Lopatin EF, Fonarow G, Emerman CL. Morphine and outcomes in acute 38 Texas EMS Magazine July/August 2008 decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008;4:205-209. 2. Cotter G., Metzkor E., Kaluski E., Faigenberg Z., Miller R., Simovitz A., Shaham O., Marghitay D., Koren M., Blatt A., et al: Randomised trial of high-dose isosorbide dinitrate plus low-dose furosemide versus high-dose furosemide plus low-dose isosorbide dinitrate in severe pulmonary edema. Lancet. 1998;351:389-393. 3. Hoffman JR, Reynolds S. Comparison of nitroglycerin, morphine and furosemide in treatment of presumed prehospital pulmonary edema. Chest. 1987; 92:586-93. 4. Hubble MW, Richards ME, Jarvis R, Millikan T, Young D. Effectiveness of prehospital continuous positive airway pressure in the management of acute pulmonary edema. Prehosp Emerg Care. 2006;10:430-9. 5. Bledsoe BE, Porter RS, Cherry RA. Paramedic Care: Principles and Practices, Third Edition. Upper Saddle River, NJ: Brady/ Pearson Education, 2009. CHF Treatment Algorithm HIGH-CONCENTRATION OXYGEN Continuing Education PLACE MONITORS DETERMINE BLOOD PRESSURE SBP > 100 SBP 90-100 SBP < 90 IV/IO IV/IO UNSTABLE TACHYCARDIA/ BRADYCARDIA? YES SBP > 180 SBP 140-180 SBP 100-140 3 TABS OR SPRAYS NTG*† 2 TABS OR SPRAYS NTG*† 1 TAB OR SPRAY NTG*† TREAT DYSRHYTHMIA PER PROTOCOL NO NON-INVASIVE VENTILATION (CPAP) CONSIDER DOPAMINE OR DOBUTAMINE NTG REPEATED EVERY 3-5 MINUTES IF SBP > 100 CONSIDER IV NTG CONSIDER ACE INHIBITOR CONSIDER NESITIRIDE CONSIDER BENZODIAZEPINE IF ANXIETY PERSISTS ONCE HYPOXEMIA IMPROVED TRANSPORT * - Dose = 0.4 mg sublingually † - Do not administer if patient has taken Levitra, Viagra or Cialis on last 24 hours. July/August 2008 Texas EMS Magazine 39
© Copyright 2026