Partners in Health Update - April 2015
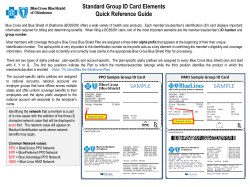
update SM April 2015 ICD-10: External testing update and tips for a successful conversion page 5 EDI web resources updated page 6 User guides and webinar now available for recent NaviNet® transaction changes page 16 Inside this edition Business Transformation ►►Business Transformation has been completed ICD-10 ►►Join us for the next What’s Up Wednesday call on April 15, 2015 ►►External testing update and tips for a successful conversion Billing ►►EDI web resources updated ►►Updated process for submitting an overpayment/refund request ●● Correction: Claim submission requirements when billing with place of service code 22 Medical ►►NaviNet to provide direct access link to CareCore’s provider Partners in Health UpdateSM is a publication of Independence Blue Cross and its affiliates (Independence), created to provide valuable information to the Independence-participating provider community. This publication may include notice of changes or clarifications to administrative policies and procedures that are related to the covered services you provide in accordance with your participating professional provider, hospital, or ancillary provider/ancillary facility contract with Independence. This publication is the primary method for communicating such general changes. Suggestions are welcome. Contact information: Provider Communications Independence Blue Cross 1901 Market Street 27th Floor Philadelphia, PA 19103 [email protected] portal ►►Medical and claim payment policy activity posted from February 21 – March 23, 2015 Quality Management ●● Highlighting HEDIS : Well-child visits in the first 15 months of life ® ►►Independence’s Medicare utilization remains within national standards ►►Improving lead testing among CHIP members NaviNet® ►►User guides and webinar now available for recent NaviNet transaction changes Health and Wellness ►►Know your terms ►►Free mobile health tool for your patients: CareCam app now available for diabetes and asthma self-management Models are used for illustrative purposes only. Some illustrations in this publication copyright 2015 www.dreamstime.com. All rights reserved. Independence Blue Cross offers products through its subsidiaries Independence Hospital Indemnity Plan, Keystone Health Plan East and QCC Insurance Company, and with Highmark Blue Shield — independent licensees of the Blue Cross and Blue Shield Association. This is not a statement of benefits. Benefits may vary based on state requirements, Benefits Program (HMO, PPO, etc.), and/or employer groups. Providers should call Provider Services for the member’s applicable benefits information. Members should be instructed to call the Customer Service telephone number on their ID card. The third-party websites mentioned in this publication are maintained by organizations over which Independence exercises no control, and accordingly, Independence disclaims any responsibility for the content, the accuracy of the information, and/or quality of products or services provided by or advertised in these third-party sites. URLs are presented for informational purposes only. Certain services/ treatments referred to in third-party sites may not be covered by all benefits plans. Members should refer to their benefits contract for complete details of the terms, limitations, and exclusions of their coverage. NaviNet is a registered trademark of NaviNet, Inc., an independent company. FutureScripts and FutureScripts Secure are independent companies that provide pharmacy benefits management services. CPT copyright 2014 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. For articles specific to your area of interest, look for the appropriate icon: Professional Facility Ancillary ►►Articles designated with a blue arrow include notice of changes or clarifications to administrative policies and procedures. Keystone Health Plan East, Personal Choice®, Keystone 65 HMO, and Personal Choice 65SM PPO have an accreditation status of Commendable from NCQA. BUSINESS TRANSFORMATION Business Transformation has been completed Independence is pleased to announce that the transition of our membership and claims processing to a new operating platform has been completed. As you know, Independence began this transition in November 2013. The new platform offers greater capabilities, increased flexibility in benefit design, and enhanced functionalities to improve the overall customer experience. This important transition included the following milestones: ●● Transition of X12 transactions. All trading partners send and receive transactions to/from the Highmark Gateway as of November 1, 2013. ●● FEP claims. Institutional claims processing for Federal Employee Program (FEP) members was migrated to the new platform on November 1, 2013. Professional claims processing for FEP members should continue to be submitted with Highmark as the payer. ●● Host claims. Claims processing for professional Host Medicare Advantage PPO (MA PPO) BlueCard® claims and institutional Host claims was migrated to the new platform on November 1, 2013. ●● Medicare Advantage HMO and PPO member claims. All Medicare Advantage HMO and PPO members were migrated to the new platform on January 1, 2015. ●● Commercial member claims. All commercial members have now been migrated to the new platform. This transition of commercial member claims happened over time, generally based on when the customer/member’s contract renewed. Important changes as a result of the transition Check member ID cards at every visit Because all members were issued a new member ID card upon migration, it is imperative that provider offices do the following: 1.Obtain a copy of the member’s current ID card at every visit to ensure that you submit the most up-to-date information to Independence. 2.Verify eligibility and benefits using NaviNet prior to rendering service. Below are some of the important changes that occurred as a result of our transition to the new platform. These changes affect the way you do business with Independence. ●● Member ID cards/numbers. As members were migrated to the new platform, they were issued a new member ID card with a new ID number and, in some cases, a new alpha prefix. The subscriber and all members covered under the subscriber’s policy share the same ID number. ●● Provider payment. Now that all members are migrated, you will receive a different format of the Statement of Remittance (SOR) – called the Provider Explanation of Benefits (professional) and Provider Remittance (facility). On the new format for facility claims, services have been combined and displayed April 2015 | Partners in Health UpdateSM on one line. Note: You will continue to receive an SOR for dates of service that occurred prior to the member’s migration to the new platform. In addition, 835 transactions generated on the new platform contain additional and updated information. Please refer to our Trading Partner Business Center at www.highmark.com/edi-ibc for more specific information. ●● Claims processing. Additional data elements are required to ensure proper claims processing on the new platform. For example, taxonomy codes are required on all claims submissions. Information regarding the specific data elements required can be found in the Independence Blue Cross HIPAA Transaction Standard Companion Guide, which is available at www.ibx.com/edi. ●● Provider Automated System. Now that all members have been migrated to the new platform, the Provider Automated System is no longer available for any functionality (e.g., eligibility, claims status, authorizations). Providers must use the NaviNet® web portal to retrieve this information. ●● NaviNet. Many changes have been implemented on Independence NaviNet Plan Central, including adding, removing, and enhancing transactions. For more specific information, please refer to the NaviNet Transaction Changes section of our Business Transformation site at www.ibx.com/pnc/businesstransformation. This section of our site contains user guides and webinars for the new or enhanced transactions. For more information For more information related to our Business Transformation, go to www.ibx.com/pnc/ businesstransformation. This site contains a communication archive as well as a frequently asked questions (FAQ) document. If you still have questions after reviewing the FAQ, email us at [email protected]. 3 www.ibx.com/providers ICD-10 Join us for the next What’s Up Wednesday call on April 15, 2015 What’s Up Wednesday is a monthly teleconference hosted by Pennsylvania’s Blue Plans to help prepare health care professionals for the ICD-10 transition on October 1, 2015. What’s Up Wednesday features special guest speakers and ICD-10 experts who will lead discussions to help you get ready for the compliance date. All providers, clearinghouses, information trading partners, and information networks are encouraged to participate. How to participate ●● No registration is required. Prior to the call, visit the What’s Up Wednesday web page at www.ibx.com/ providers/claims_and_billing/icd_10/whatsupweds.html to access and download the presentation materials. ●● On the day of the call, dial 1-800-882-3610 and enter pass code 5411307 when prompted. Please dial in five minutes prior to the start of the call. ICD-10 Will you be ready? Questions If you have specific ICD-10-related questions during the call, please email them to [email protected]. Call details Date: Wednesday, April 15, 2015 Time: 2 – 3 p.m. ET Phone number: 1-800-882-3610 Pass code: 5411307 April 2015 | Partners in Health UpdateSM 4 www.ibx.com/providers ICD-10 External testing update and tips for a successful conversion Independence has begun testing with large health systems, which include hospitals, physicians, and clearing houses. We will be communicating our testing experience and lessons learned to network providers to ensure a smooth transition to ICD-10 by October 1, 2015. Tips for a successful conversion Steps you can take to ensure a successful transition to ICD-10: 1. Make a plan ●● Identify which ICD-9 codes you use heavily. ●● Identify staff that need to be trained in medical coding and/or documentation. ●● Contact vendors to learn their transition plans, ICD-10 related costs to the practice, and resources available to the practice. ●● Contact the specialty societies or the Centers for Medicare & Medicaid Services (CMS) website for any resources available to the practice. 2. Get trained ●● Buy or download an ICD-10 diagnosis codebook. ●● Arrange and obtain documentation training for physicians and other clinicians. ●● Crosswalk common diagnosis codes to ICD-10 and identify new requirements or differences in essential documentation. ●● Sign up for key CMS webinars to increase understanding of the ICD-10 environment. 3. Update internal practice tools ●● Convert superbills to ICD-10. ●● Convert other materials to ICD-10, such as authorizations, orders, and referrals. ●● Identify current code-related claim denials and areas where ICD-10’s specificity in documentation and code assignment can address this. ●● Obtain payer medical polices with ICD-10 codes for comparison. 5. Test the process ●● ●● ●● ●● Perform testing on systems within the practice. Perform end-to-end testing, where available. Identify and correct issues encountered during testing. Educate staff on the impact of ICD-10 to payer edits, adjudication, and other claims elements to processes within the practice. 4. Work with vendors and payers ●● Arrange and implement ICD-10 software upgrades and training for staff on use of new software, either directly or via the vendor. ●● Identify electronic health records documentation templates and assess how they support ICD-10 specificity for claims submission and medical necessity. ●● Engage payers on any discrepancies and omissions in ICD-10 coding for medical policies. ●● Identify if payers anticipate any changes in processing and payments due to ICD-10. For the most up-to-date information, including updates on external testing, frequently asked questions, and dial-in information for the next What’s Up Wednesday call, please visit our dedicated ICD-10 web page at www.ibx.com/icd10 and be sure to read future editions of Partners in Health Update. April 2015 | Partners in Health UpdateSM 5 www.ibx.com/providers BILLING EDI web resources updated We recently updated our online resources for information related to electronic data interchange (EDI). Independence provider EDI page Now when you go to www.ibx.com/edi, you’ll see a brief overview and steps for getting started with EDI. On the right side of the page, you’ll see a blue box called EDI Resources, which contains the following for download and viewing: ●● frequently asked questions about EDI ●● payer ID grids (professional and facility) ●● companion guide The EDI web page is intended to provide a few key resources for submitting claims to Independence. It also contains a link to the Trading Partner Business Center, our online resource for tools and documentation related to conducting EDI business with Independence. continued on the next page April 2015 | Partners in Health UpdateSM 6 www.ibx.com/providers BILLING continued from the previous page Trading Partner Business Center The Trading Partner Business Center is available at www.highmark.com/edi-ibc. Launched in 2013, it was recently revamped to make it easier to use to find information and resources. The updated left-hand menu contains the following options: ●● Sign up. This link provides information for how to sign up as a trading partner to do business with Independence. ●● Update Trading Partners. The forms within this menu option are for requesting changes to a trading partner profile, including changes to provider affiliation, trading partner contact information, and trading partner set-up. ●● Resources. This page includes many tools to assist trading partners in doing business with Independence, including sample transactions, communication standards, and information about registration for electronic funds transfer (EFT). ●● News. Included within this option is information about scheduled system outages and a list of corporate holidays. If you have any questions related to EDI, please call Highmark EDI Operations at 1-800-992-0246. Highmark EDI Operations is available Monday through Friday, 8 a.m. to 5 p.m., ET. April 2015 | Partners in Health UpdateSM 7 www.ibx.com/providers BILLING Updated process for submitting an overpayment/refund request If your office receives an overpayment from Independence and you need to submit an adjustment to correct the overpayment, you can do so in one of the following ways. The NaviNet® web portal Participating providers with access to NaviNet should initiate an adjustment to correct an overpayment by selecting the Claim Inquiry and Maintenance transaction and then Claim Status Inquiry. From there you can enter one of the two appropriate search criteria options: ●● Billing Provider/Member ID/Date of Birth ●● Billing Provider/Member Last Name/First Name/Date of Birth Once the search is complete, you can find a link to Claim Investigation through the Claims Search Results and Claim Details screens. Through the Claim Investigation link you can submit the credit and/or retraction request, which will appear on a future Provider Explanation of Benefits (Provider EOB) or Provider Remittance. Overpayment/Refund Form Offices that are nonparticipating with Independence or not yet NaviNet-enabled can submit their adjustment request using the Overpayment/Refund Form, which is located at www.ibx.com/providerforms. Once the form has been completed, please mail it, along with a copy of the Provider EOB or Provider Remittance, to: Independence Claims Overpayment 1901 Market Street, 39th Floor Treasury Services – Misc. Cash Receipts Philadelphia, PA 19103-1480 Note: The submission address for the Overpayment/Refund Form recently changed. Please ensure you are using the most recent version of the form. If you have any questions regarding submitting an overpayment request, please contact Customer Service. April 2015 | Partners in Health UpdateSM 8 www.ibx.com/providers BILLING Correction: Claim submission requirements when billing with place of service code 22 This article contains corrections to the field requirements for electronically submitted claims that appeared in the March 2015 edition of Partners in Health Update. This article was also designated for both professional and facility provider types; however, it was intended for professional and ancillary providers. We apologize for any confusion this may have caused. When billing with place of service code 22, outpatient hospital, it is important to remember that you must complete all required fields in their entirety, specifically as it relates to the Servicing Facility field. It is important that the proper ZIP code is included to receive accurate payment. Required fields For claims submitted electronically: ●● Loop 2310C NM1 (Service Facility Location Name) —— N3 (Service Facility Location Address) —— N4 (Service Facility Location City, State, ZIP Code) —— REF (Service Facility Location Secondary Identification) For claims submitted on paper: ●● Box 32 (see image, right) Completing all required fields facilitates the submission of a Clean Claim as contractually required. For complete information on submitting claims electronically, refer to the EDI section of our website at www.ibx.com/edi. For complete information on submitting paper claims, please read the Claims Submission Toolkit for Proper Electronic and Paper Claims Submission available at www.ibx. com/providers/claims_and_billing/claims_ resources_guides.html. April 2015 | Partners in Health UpdateSM 9 www.ibx.com/providers MEDICAL NaviNet® to provide direct access link to CareCore’s provider portal As previously communicated, providers are required to obtain precertification through CareCore National, LLC (CareCore), an independent company, for non-emergent outpatient radiation therapy services for all commercial and Medicare Advantage HMO, POS, and PPO members. In addition, we will transition to the use of CareCore Radiation Therapy Utilization Management Criteria when reviewing requests for radiation therapy services starting May 1, 2015. For members under age 19, services requested will always be automatically approved; however, precertification through CareCore is still required to ensure accurate and timely claims payment. Effective May 1, 2015, the NaviNet web portal will offer direct access to CareCore’s provider portal to streamline the process of obtaining precertification. Providers can select CareCore from the Authorizations transaction and will be automatically redirected to CareCore’s provider portal without having to re-enter login credentials. Previous credentials used to access CareCore’s provider portal are no longer needed when going through NaviNet. Additional enhancements to NaviNet, including the ability to review finalized precertifications for radiation therapy services precertified by CareCore, will be announced via NaviNet Plan Central later this month. Precertification guidelines The criteria that will be used as the basis for reviewing precertification requests as of May 1, 2015, are available on CareCore’s website at https://www.carecorenational.com/benefits-management/radiation-therapy/radiation-therapytools-and-criteria.aspx. In addition, the following medical policies include a link to the criteria that CareCore will use to determine medical necessity for radiation therapy services as well as a complete list of procedure codes that require precertification: ●● Commercial: #09.00.56: Radiation Therapy Services; ●● Medicare Advantage: #MA09.020: Radiation Therapy Services. To view these policies, visit our Medical Policy Portal at www.ibx.com/medpolicy. Select Accept and Go to Medical Policy Online, and then select the Commercial or Medicare Advantage tab from the top of the page, depending on the version of the policy you’d like to view. Type the policy name or number in the Search field. Requesting precertification You can initiate precertification for non-emergent outpatient radiation therapy in one of the following ways: ●● NaviNet. Select CareCore from the Authorizations transaction. ●● Telephone. Call CareCore directly at 1-866-686-2649. Medical and claim payment policy activity posted from February 21 – March 23, 2015 Each month, new policy activity is posted to our Medical Policy Portal. Policy activity may include new, updated, reissued, or archived policies and coding updates. Included with this edition of Partners in Health Update is a supplementary listing of policy activity that occurred for our commercial and Medicare Advantage Benefits Programs from February 21 – March 23, 2015. April 2015 | Partners in Health UpdateSM10 For the most up-to-date information about medical and claim payment policy activity, go to www.ibx.com/ medpolicy and select Accept and Go to Medical Policy Online. Then select either the Commercial or Medicare Advantage tab from the top of the page, depending on the version of the policy you’d like to view. You can also get to our Medical Policy Portal through the NaviNet® web portal by selecting the Reference Tools transaction, then Medical Policy. www.ibx.com/providers QUALITY MANAGEMENT Highlighting HEDIS®: Well-child visits in the first 15 months of life This article series is a monthly tool to help physicians maximize patient health outcomes in accordance with NCQA’s* HEDIS®† measurements for high quality care on important dimensions of services. Go to www.ibx.com/providers/resources/hedis.html to view previously published Highlighting HEDIS® topics. If you have feedback or would like to request a topic, email us at [email protected]. HEDIS® definition Well-child visits in the first 15 months of life: The percentage of members who turned 15 months old during the measurement year and who had the following number of well-child visits with a primary care physician during their first 15 months of life: ●● no well-child visits ‡ ●● one well-child visit ●● two well-child visits Well-child visits in the first 15 ●● three well-child visits months of life is a performance ●● four well-child visits measure in the Quality Incentive ●● five well-child visits Payment System (QIPS) program for measurement year ●● six or more well-child visits 2015 for participating providers. QIPS alert Why this measure is important The American Academy of Pediatrics recommends six well-child visits in the first year of life: the first within the first month of life, and then again at around two, four, six, nine, and twelve months of age. These visits are of particular importance during the first year of life, when an infant undergoes substantial changes in abilities, physical growth, motor skills, hand-eye coordination, and social and emotional growth. Regular check-ups are one of the best ways to detect physical, developmental, behavioral, and emotional health problems. — NCQA, HEDIS 2015 V1 Plan performance The chart below compares the national average for six or more well-child visits in the first 15 months of life for commercial HMO/PPO plans vs. Independence’s rates over a four-year period. Commercial Year National Independence HMO PPO HMO PPO 2013 79.0% 76.9% 78.2% 83.6% 2012 78.2% 76.4% 76.2% 83.0% 2011 78.0% 76.1% 70.5% 61.2% 2010 76.3% 72.8% 76.1% 75.2% As the chart demonstrates, Independence performs below the national average for HMO and above the national average for PPO. The goal for Independence is to reach the national 90th percentile benchmark, which is currently at 89.8 percent and 86.9 percent for HMO and PPO plans, respectively. — Source: 2014 State of Health Care (NCQA) Quick tips for improvement 99Schedule the entire suite of visits with or at the conclusion of the first visit. 99Inform caregivers on the importance of well-child visits. 99Be proactive – make outreach calls to members who are not on track to complete the recommended six visits. *The National Committee for Quality Assurance (NCQA) is the most widely recognized accreditation program in the U.S. †The Healthcare Effectiveness Data and Information Set (HEDIS) is an NCQA tool used by more than 90 percent of U.S. health plans to measure performance on important dimensions of care. ‡ QIPS is a reimbursement system developed by Keystone Health Plan East for participating Pennsylvania primary care physicians that offers incentives for high-quality, accessible, and cost-effective care. April 2015 | Partners in Health UpdateSM11 www.ibx.com/providers QUALITY MANAGEMENT Independence’s Medicare utilization remains within national standards As part of Independence’s annual review process, we obtain data from the Healthcare Effectiveness Data and Information Set (HEDIS®) and Consumer Assessment of Healthcare Providers and Systems (CAHPS®) to help evaluate utilization for our Medicare Advantage HMO and PPO members. The results showed that utilization remains within national standards and members do not perceive significant barriers to getting appropriate care. HEDIS® data evaluation Independence used the data from HEDIS® to evaluate hospital discharges and the frequency rates of select cardiac procedures. Hospital utilization Hospital utilization comparisons of acute discharges per 1,000 (Table 1) show that Keystone 65 HMO and Personal Choice 65SM PPO rates continue to improve and remain within the relevant national 10th and 90th percentiles as the appropriate thresholds for over/under utilization. Comparison of HEDIS® rates for Keystone 65 HMO reports a point change from 2013 to 2014 of 2.71 but an overall downward trend for the last three measurement years; comparison of HEDIS® rates for Personal Choice 65SM PPO reports a point change of -20.01 from HEDIS® 2013 to 2014, with a downward trend over the last three measurement years. Table 1: Hospital utilization comparison acute discharges per 1,000 HEDIS® year Point change 2013 – 2014 R-squared Trending per 1000 members Within 2.71 71.42% Down Within -20.01 99.70% Down 2012 2013 2014 Rate Rate Rate Threshold Threshold status Keystone 65 HMO 346.31 286.89 289.60 170.83 – 334.11 Personal Choice 65 PPO 301.65 277.40 257.39 170.83 – 334.11 Use of services Independence also measured the frequency of selected procedure rates for cardiac angioplasty, cardiac catheterization, and coronary artery bypass graft (CABG). Based on a comparison of 2014 HEDIS® utilization rates with respect to established thresholds, utilization for use of services for these identified indicators fell within the established threshold for most age/gender cohorts. There were two cohorts that did not fall within national or regional thresholds and one cohort that fell above national, but within regional thresholds. These rates are measured according to age group and gender, and Independence recognizes the probability of unequal variance as an issue with the cardiac procedure rates. continued on the next page April 2015 | Partners in Health UpdateSM12 www.ibx.com/providers QUALITY MANAGEMENT continued from the previous page CAHPS data evaluation Independence used CAHPS data to evaluate composite care, including member perception of getting needed care in a timely manner and specialty care. Keystone 65 HMO The rates for Keystone 65 HMO members getting needed care during 2014 (Table 2) remains within the national average. The point difference for members with Keystone 65 HMO CAHPS from 2013 to 2014 reports a change of -0.09 for all indicators measured for this report and shows a downward trend over the last three reporting years (2012 – 2014). The plan recognizes the difficulty in obtaining care and continues to actively recruit health care providers within the region, including reaching out to network providers via the Clinical Quality Committee for input into barriers to care that the plan may influence. Table 2: CAHPS member satisfaction data — Keystone 65 HMO HEDIS® year Point change 2013 – 2014 R-squared Three-year trend Within -0.09 42.86% Down 3.53 Within -0.09 42.86% Down 3.29 Within -0.09 42.86% Down 2012 2013 2014 Rate Rate Rate National average Threshold status In the last six months, how often was it easy to get care, tests, or treatment you thought you needed? 3.64 3.67 3.58 3.57 In the last six months, how often was it easy to get appointments with a specialist? 3.61 3.64 3.55 Getting needed care composite 3.64 3.67 3.34 continued on the next page April 2015 | Partners in Health UpdateSM13 www.ibx.com/providers QUALITY MANAGEMENT continued from the previous page Personal Choice 65 PPO The rate for Personal Choice 65 PPO members during 2014 (Table 3) for obtaining needed care, tests, and treatment and overall care composite increased from CAHPS 2013 to 2014 and is significantly above the national average as reported by the Centers for Medicare & Medicaid Services. Personal Choice 65 PPO members are not required to identify a primary care physician, and many PPO members with chronic conditions use a specialist as their primary physician. However, based on member responses regarding the ease of care and care composite, there were no significant barriers to members receiving appropriate care noted. Table 3: CAHPS member satisfaction data — Personal Choice 65 PPO HEDIS® year 2014 Point change 2013 – 2014 R-squared Three-year trend 2012 2013 Rate Rate Rate National average Threshold status In the last six months, how often was it easy to get care, tests, or treatment you thought you needed? 3.61 3.64 3.73 3.57 Above* 0.09 92.31% Up In the last six months, how often was it easy to get appointments with a specialist? 3.61 3.61 3.52 3.53 Within -0.09 75.00% Down Getting needed care composite 3.61 3.61 3.37 3.29 Above* 0.03 75.00% Up *Threshold status significantly better/worse than the national average For more information To learn more about HEDIS®, go to www.ibx.com/providers/resources/hedis.html to view Highlighting HEDIS® articles that have been published in Partners in Health Update. These articles are educational resources for understanding HEDIS® measures. If you have feedback about the Highlighting HEDIS® series or topic requests, please email us at [email protected]. HEDIS is a registered trademark of the National Committee for Quality Assurance (NCQA). Used with permission. April 2015 | Partners in Health UpdateSM14 www.ibx.com/providers QUALITY MANAGEMENT Improving lead testing among CHIP members Last year, Independence reminded Keystone Health Plan East practitioners of the importance of testing children enrolled in the Pennsylvania Children’s Health Insurance Program (CHIP) for Elevated Blood Lead Level (EBLL). This year, we again would like to take the opportunity to remind your practice that some of our CHIP population may reside in homes that place them at risk for EBLL. As such, we’re providing you with an update on how your practice can identify CHIP members and continue to evaluate their need for testing. During 2013, the Pennsylvania Insurance Department reiterated to health plans the importance of increasing rates for lead testing among CHIP members. Independence shared with practitioners the Centers for Disease Control and Prevention’s (CDC) updated recommendation for prevention of lead poisoning and a new reference level of 5μg/dL to identify children and environments associated with lead-exposure hazards. In accordance with the Pennsylvania Insurance Department and Healthcare Effectiveness Data and Information Set (HEDIS®) specification, children who are enrolled in CHIP follow the same guidelines for lead testing as children who are enrolled in the Medicaid program; therefore, they should receive at least one lead capillary or venous blood test on or before their second birthday. Important update: Identifying CHIP members In December 2014, the parents and guardians of CHIP members received a new Keystone Health Plan East ID card with a new member ID number and instructions to begin using the new cards effective January 1, 2015. To ensure the records of CHIP members are updated and the children receive correct coverage, parents were instructed to use the new ID card each time their children receive medical services and when filling a prescription at the pharmacy. The new Independence member ID cards still include the identifying words “PA KIDS” written on the front, as shown in the sample CHIP ID card displayed below. L NaviNet® enhancements Enhancements are being made to the NaviNet web portal to give providers the ability to identify CHIP members through the PCP CAP Rosters transaction under ePayment. In the meantime, providers should continue to identify CHIP members by using their ID cards. In addition, a list of CHIP members will also be mailed to Keystone Health Plan East primary care physicians. Additional information about this enhancement will be provided in future editions of Partners in Health Update. To learn more about changes to NaviNet, we strongly encourage you to review the NaviNet Transaction Changes section of our Business Transformation site at www.ibx.com/pnc/businesstransformation, which includes User Guides and a complete archive of communications. continued on the next page April 2015 | Partners in Health UpdateSM15 www.ibx.com/providers QUALITY MANAGEMENT continued from the previous page What practices can do: Lead testing vs. screening Lead testing is described as one or more lead capillary or venous blood test for lead poisoning administered by a child’s second birthday. Lead screening is described as an assessment or questionnaire regarding a child’s health or living environment. While the terminologies are sometimes used interchangeably, lead screening is not the same as lead testing. Practitioners are asked to test children enrolled in the CHIP program between ages 9 to 12 months, again at 24 months, and thereafter based on risk. All CHIP members should be tested for EBLL regardless of risk level. A risk assessment should be performed starting at 6 months, then again at 9 and 18 months, then annually from ages 3 to 6 with testing as appropriate. Your personal recommendation has tremendous influence on the parents/guardians of your pediatric patients and their decision to seek lead testing information for their children. Therefore, we respectfully ask for your practice’s participation in ensuring that all CHIP members receive lead testing as appropriate. The following resources provide additional information regarding lead testing recommendations: ●● CDC: www.cdc.gov/nceh/lead/nlppw.htm ●● Philadelphia Department of Public Health: 215-685-2788 (Philadelphia residents) ●● National Lead Information Center: 1-800-424-LEAD (non-Philadelphia residents) ●● U.S. Environmental Protection Agency: www.epa.gov NAVINET® User guides and webinar now available for recent NaviNet transaction changes As previously communicated, significant changes were made in March to the NaviNet® web portal. We encourage you to review the new user guides and webinar listed below, which are posted in the NaviNet Transaction Changes section of our Business Transformation site at www.ibx.com/pnc/businesstransformation. ●● NaviNet Office Conversion Guide and webinar ●● Tiering Enhancement Guide ●● Allowance Inquiry Guide ●● Network Facility Inquiry Guide ●● Network Provider Inquiry Guide If you have questions after reviewing these resources, please call the eBusiness Hotline at 215-640-7410. Later this month, we will introduce a new transaction – Cash Management – that provides you with a weekly payment accumulation and summary of payments received for the current year. More information about this new transaction will be posted to Independence NaviNet Plan Central in the coming weeks. April 2015 | Partners in Health UpdateSM16 www.ibx.com/providers HEALTH AND WELLNESS Know your terms The National Institutes of Health (NIH) wants your expectant patients to be aware of the new full-term pregnancy definition and the importance of waiting for delivery until 39 weeks when possible. The following new terms reflect the latest research regarding gestational age: ●● Early term: 37 weeks through 38 weeks and six days ●● Full term: 39 weeks through 40 weeks and six days ●● Late term: 41 weeks through 41 weeks and six days ●● Post term: 42 weeks and beyond The NIH encourages providers to explain the critical development of the brain, lungs, and liver that babies experience between 37 and 39 weeks and to share the risks of elective delivery before full term. Expectant parents should also know that risks to both mother and baby are higher during this time period. As the American Congress of Obstetricians and Gynecologists (ACOG) and Independence have already encouraged, please do NOT schedule elective deliveries prior to 39 weeks gestation. Learn more by reviewing the ACOG and Society for Maternal-Fetal Medicine Committee Opinion #579 “Definition of Term Pregnancy” at http://www.acog.org/-/media/Committee-Opinions/Committee-on-Obstetric-Practice/co579.pdf. Free educational materials, developed by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and National Child and Maternal Health Education Program (NCMHEP) are available to help you share this important message with your expectant patients. To order these materials, go to www.nichd.nih.gov/ncmhep/terms/ordermaterials. Free mobile health tool for your patients: CareCam app now available for diabetes and asthma self-management As part of our ongoing commitment to help members improve their health, beginning April 1, 2015, Independence is offering a new chronic care management app to diabetic and asthmatic members through CareCam Health Systems (CCHS), an independent vHealthTM technology firm. The CareCam app can be downloaded by your Independence diabetic and asthmatic patients to their smartphone or tablet for free and is designed to help them comply with your recommended care plan between appointments. Trial participants viewed CareCam as a helpful coach and trusted source of condition-specific education and reported increased feelings of independence and accountability. CareCam also received positive feedback from physician focus group participants. April 2015 | Partners in Health UpdateSM17 The app helps your patients customize a daily schedule of health care activities, based around the recommendations you provide during visits. Patients receive reminders for late or missed activities and personalized feedback on their results. Patients can access condition-specific video education and summaries of past results to share with you during appointments. CareCam users can also invite friends or family members to follow their progress and provide support and encouragement. CareCam requires no action from physicians except to direct Independence diabetic and asthmatic patients to search “CareCam’’ in the Apple App Store or Google Play Store to download the app for free. Note: During registration some patients may be required to call CareCam to validate their eligibility. www.ibx.com/providers Important Resources Anti-Fraud and Corporate Compliance Hotline 1-866-282-2707 or www.ibx.com/antifraud Care Management and Coordination Baby BluePrints® 215-241-2198 / 1-800-598-BABY (2229)* Case Management 1-800-313-8628 Condition Management Program 1-800-313-8628 Credentialing Credentialing Violation Hotline 215-988-1413 or www.ibx.com/credentials Customer Service/Provider Services Provider Automated System 1-800-ASK-BLUE (1-800-275-2583) Provider Services user guide www.ibx.com/providerautomatedsystem Electronic Data Interchange (EDI) Highmark EDI Operations 1-800-992-0246 FutureScripts® (commercial pharmacy benefits) Prescription drug prior authorization 1-888-678-7012 Pharmacy website (formulary updates, prior authorization) www.ibx.com/rx FutureScripts® Secure (Medicare Part D pharmacy benefits) FutureScripts Secure Customer Service Formulary updates 1-888-678-7015 www.ibxmedicare.com NaviNet® web portal Independence eBusiness Hotline Registration 215-640-7410 www.navinet.net Other frequently used phone numbers and websites Independence Direct Ship Injectables Program (medical benefits) www.ibx.com/directship Medical Policy www.ibx.com/medpolicy Provider Supply Line 1-800-858-4728 or www.ibx.com/providersupplyline *Outside 215 area code Visit our Provider News Center: www.ibx.com/pnc Medical and claim payment policy activity Commercial business The following pages list the policy activity for commercial business that we have posted to our Medical Policy Portal from February 21 – March 23, 2015. For the most up-to-date information about medical and claim payment policy activity for commercial business, go to www.ibx.com/medpolicy, select Accept and Go to Medical Policy Online, and then select the Commercial tab. You can also view policy activity using the NaviNet® web portal by selecting the Reference Tools transaction, then Medical Policy. New policies The following commercial policies have been newly developed to communicate coverage and/or reimbursement positions, reporting requirements, and other processes and procedures for doing business with Independence. Policy # Title Notification date Effective date 00.01.61 Reimbursement for Components of Comprehensive Laboratory Panels February 4, 2015 March 6, 2015 05.00.76 Breast Pumps March 11, 2015 April 10, 2015 Updated policies The following commercial policies have been reviewed and updated to communicate current coverage and/or reimbursement positions, reporting requirements, and other procedures for doing business with Independence. Policy # Title Type of policy change Notification date Effective date 06.02.01f Lyme Disease: Diagnosis and Intravenous (IV) Antibiotic Treatment Coverage and/or Reimbursement Position; Medical Coding; General Description, Guidelines, or Informational Update January 26, 2015 07.02.09c Ambulatory Blood Pressure Monitoring (ABPM) Medical Necessity Criteria; Medical Coding; General Description, Guidelines, February 23, 2015 or Informational Update March 25, 2015 08.00.26s Botulinum Toxin Agents General Description, Guidelines, or Informational Update February 9, 2015 March 11, 2015 08.00.50m Rituximab (Rituxan ) Coverage and/or Reimbursement Position; Medical Necessity Criteria; Medical Coding; General Description, Guidelines, or Informational Update N/A March 11, 2015 08.00.79a Plerixafor Injection (Mozobil™) General Description, Guidelines, or Informational Update N/A March 11, 2015 08.01.10a Octreotide acetate (Sandostatin® LAR Depot) Medical Necessity Criteria; Medical Coding N/A February 25, 2015 09.00.02e Electron Beam Computed Tomography (EBCT) for Screening Evaluations General Description, Guidelines, or Informational Update N/A March 11, 2015 09.00.40d Screening for Vertebral Fracture with Dual-Energy X-ray Absorptiometry (DEXA/DXA) General Description, Guidelines, or Informational Update N/A March 11, 2015 09.00.42c Computer-Aided Detection (CAD) System for use with Chest Radiographs General Description, Guidelines, or Informational Update N/A March 11, 2015 ® February 21 – March 23, 2015 February 25, 2015 1 Policy # Title Type of policy change Notification date Effective date 09.00.49g Proton Beam Radiation Therapy Coverage and/or Reimbursement Position; Medical Necessity Criteria May 1, 2015 December 31, 2014 Revised March 4, 2015 11.01.02k Cochlear Implant Medical Necessity Criteria; Medical Coding; General Description, Guidelines, February 25, 2015 or Informational Update 11.01.06b Coverage and/or Reimbursement Bone-Anchored (Osseointegrated) Position; Medical Necessity Criteria; Hearing Aids and Implantable Middle General Description, Guidelines, or Ear Hearing Aids Informational Update 11.06.05c Endometrial Ablation 11.06.07c March 27, 2015 February 5, 2015 May 6, 2015 Coverage and/or Reimbursement Position; Medical Necessity Criteria; Medical Coding; General Description, Guidelines, or Informational Update N/A March 4, 2015 Ovarian and Internal Iliac Vein Embolization as Treatment for Pelvic Congestion Syndrome General Description, Guidelines, or Informational Update N/A March 18, 2015 11.08.17e Debridement of Mycotic and Symptomatic Non-Mycotic Hypertrophic Toe Nails Medical Necessity Criteria; Medical Coding; General Description, Guidelines, February 23, 2015 or Informational Update March 25, 2015 11.11.01g Evaluation and Treatment of Erectile Dysfunction (ED) Medical Necessity Criteria March 5, 2015 June 3, 2015 11.14.02j Trigger Point Injections Medical Coding N/A March 4, 2015 11.14.13f Extracorporeal Shock Wave Therapy (ESWT) for Musculoskeletal Conditions General Description, Guidelines, or Informational Update N/A February 25, 2015 11.15.22c Percutaneous Image-Guided Lumbar Decompression (PILD) for Spinal Stenosis General Description, Guidelines, or Informational Update; Medical Coding N/A February 25, 2015 11.15.24a Migraine Deactivation Surgery General Description, Guidelines, or Informational Update N/A March 11, 2015 11.17.06l Surgical and Minimally Invasive Treatments for Urinary Outlet Obstruction due to Benign Prostatic Hyperplasia (BPH) Coverage and/or Reimbursement Position; Medical Necessity Criteria March 9, 2015 April 8, 2015 12.01.01ab Experimental/Investigational Services Coverage and/or Reimbursement Position; Medical Coding March 2, 2015 April 1, 2015 Reissued policies The following commercial policies have been reviewed, and no substantive changes were made. Policy # Title Reissue effective date Reissue published date 05.00.04c Food and Drug Administration (FDA) Approval of Medical Devices March 4, 2015 March 4, 2015 05.00.62g Injectable Dermal Fillers March 4, 2015 March 5, 2015 07.00.01f Biofeedback Therapy March 4, 2015 March 4, 2015 07.03.14i Intraoperative Neurophysiological Monitoring (INM) March 18, 2015 March 19, 2015 07.10.06b Assisted Reproductive Technology for Infertility and Oocyte Cryopreservation March 4, 2015 March 4, 2015 07.11.01b Smell and Taste Dysfunction Testing March 18, 2015 March 19, 2015 07.13.08c Partial Coherence Interferometry March 4, 2015 March 4, 2015 09.00.51a Positron Emission Mammography (PEM) March 4, 2015 March 4, 2015 February 21 – March 23, 2015 2 Policy # Title Reissue effective date Reissue published date 10.04.01k Pulmonary Rehabilitation March 4, 2015 March 4, 2015 11.05.10b Reimbursement for a Presbyopia- or Astigmatism-Correcting Intraocular Lens March 4, 2015 March 4, 2015 11.14.03e Meniscal Allograft Transplantation March 18, 2015 March 19, 2015 11.15.13c Lysis of Epidural Adhesions March 4, 2015 March 4, 2015 11.15.19e Nucleoplasty March 4, 2015 March 4, 2015 11.16.03f Lung Volume Reduction Surgery March 4, 2015 March 4, 2015 Coding updates The following commercial policies have been reviewed and updated to add new and revised medical codes (e.g., ICD-9 and ICD-10 diagnosis codes; CPT® and HCPCS codes; revenue codes) and/or remove terminated medical codes. Policy # Title Effective date Published date 00.03.02s Diagnostic Radiology Services Included in Capitation January 1, 2015 February 6, 2015 Revised March 18, 2015 00.10.01u Services Paid Above Capitation for Health Maintenance Organization (HMO) Primary Care Physicians January 1, 2015 February 24, 2015 03.00.10l Modifiers LT/RT: Left Side/Right Side Procedures January 1, 2015 March 20, 2015 08.00.92m Coagulation Factors for Hemophilia April 1, 2015 March 20, 2015 09.00.32l Diagnostic and Therapeutic Radiopharmaceutical Agents January 1, 2015 March 20, 2015 11.00.10r Multiple Surgical Reduction Guidelines January 1, 2015 March 20, 2015 Archived policies Independence has determined that it is no longer necessary for the following commercial policies to remain active. Policy # Title Notification date Archive effective date 11.15.11b Treatment for Hyperhidrosis (Nonpharmacologic) March 11, 2015 April 10, 2015 11.17.07f Radiofrequency Micro-remodeling (by transurethral, transvaginal, or paraurethral approach) for Urinary Stress Incontinence February 11, 2015 March 13, 2015 Continue to the next page for information about Medicare Advantage policy activity. February 21 – March 23, 2015 3 Medical and claim payment policy activity Medicare Advantage business The following pages list the policy activity for Medicare Advantage business that we have posted to our Medical Policy Portal from February 21 – March 23, 2015. For the most up-to-date information about medical and claim payment policy activity for Medicare Advantage business, go to www.ibx.com/medpolicy, select Accept and Go to Medical Policy Online, and then select the Medicare Advantage tab. You can also view policy activity using the NaviNet® web portal by selecting the Reference Tools transaction, then Medical Policy. New policy The following Medicare Advantage policy has been newly developed to communicate coverage and/or reimbursement positions, reporting requirements, and other processes and procedures for doing business with Independence. Policy # Title Notification date Effective date MA01.006 Reimbursement for Components of Comprehensive Laboratory Panels February 4, 2015 March 6, 2015 Updated policies The following Medicare Advantage policies have been reviewed and updated to communicate current coverage and/or reimbursement positions, reporting requirements, and other procedures for doing business with Independence. Policy # Title Type of policy change Notification date Effective date MA00.005a Experimental/Investigational Services Coverage and/or Reimbursement Position; Medical Coding March 11, 2015 April 10, 2015 MA05.052a Canes and Crutches Medical Coding N/A March 18, 2015 MA06.006a Lyme Disease: Diagnosis and Intravenous (IV) Antibiotic Treatment Coverage and/or Reimbursement Position; Medical Coding; General Description, Guidelines, or Informational Update January 26, 2015 February 25, 2015 MA08.003a Enteral Nutritional Therapy Medical Necessity Criteria N/A March 11, 2015 MA08.017a Botulinulm Toxin Agents General Description, Guidelines, or Informational Update February 9, 2015 March 11, 2015 MA08.022a Rituximab (Rituxan ) Coverage and/or Reimbursement Position; Medical Necessity Criteria; Medical Coding; General Description, Guidelines, or Informational Update N/A March 11, 2015 MA08.039a Plerixafor Injection (Mozobil™) General Description, Guidelines, or Informational Update N/A March 11, 2015 MA08.065a Octreotide Acetate (Sandostatin® LAR Depot) Medical Necessity Criteria; Medical Coding N/A February 25, 2015 MA09.007a Proton Beam Therapy Coverage and/or Reimbursement Position; Medical Necessity Criteria February 12, 2015 May 1, 2015 Revised March 4, 2015 MA09.011a Electron Beam Computed Tomography (EBCT) for Screening Evaluations General Description, Guidelines, or Informational Update N/A March 11, 2015 MA09.013a Screening for Vertebral Fracture with Dual-Energy X-ray Absorptiometry (DEXA/DXA) General Description, Guidelines, or Informational Update N/A March 11, 2015 ® February 21 – March 23, 2015 4 Policy # Title Type of policy change Notification date Effective date MA09.014a Computer Aided Detection (CAD) System for use with Chest Radiographs General Description, Guidelines, or Informational Update N/A March 11, 2015 MA11.004a Surgical and Minimally Invasive Treatments for Urinary Outlet Obstruction due to Benign Prostatic Hyperplasia (BPH) Coverage and/or Reimbursement Position; Medical Coding March 9, 2015 April 8, 2015 MA11.014a Debridement of Mycotic and Symptomatic Non-Mycotic Hypertrophic Toe Nails Medical Necessity Criteria; Medical Coding; General Description, Guidelines, or Informational Update February 23, 2015 March 25, 2015 MA11.017a Trigger Point Injections Medical Coding N/A March 4, 2015 MA11.039a Cochlear Implantation Medical Necessity Criteria; Medical Coding; General Description, Guidelines, or Informational Update February 25, 2015 March 27, 2015 MA11.049a Bone-Anchored (Osseointegrated) Hearing Aids and Implantable Middle Ear Hearing Aids Coverage and/or Reimbursement Position; Medical Necessity Criteria; General Description, Guidelines, or Informational Update February 5, 2015 May 6, 2015 MA11.064a Implantable Miniature Telescope™ (IMT) for the Treatment of EndStage Age-Related Macular Degeneration (AMD) Medical Necessity Criteria January 15, 2015 April 15, 2015 MA11.065a Endometrial Ablation Coverage and/or Reimbursement Position; Medical Necessity Criteria; Medical Coding; General Description, Guidelines, or Informational Update N/A March 4, 2015 MA11.066a Ovarian and Internal Iliac Vein Embolization as Treatment for Pelvic Congestion Syndrome General Description, Guidelines, or Informational Update N/A March 18, 2015 MA11.079a Evaluation and Treatment of Erectile Dysfunction (ED) Medical Necessity Criteria March 5, 2015 June 3, 2015 MA11.087a Extracorporeal Shock Wave Therapy (ESWT) for Musculoskeletal Conditions General Description, Guidelines, or Informational Update N/A February 25, 2015 MA11.097a Percutaneous Image-Guided Lumbar Decompression (PILD) for Spinal Stenosis Medical Coding N/A February 25, 2015 Reissued policies The following Medicare Advantage policies have been reviewed, and no substantive changes were made. Policy # Title Reissue effective date Reissue published date MA05.021 Injectable Dermal Fillers March 4, 2015 March 5, 2015 MA05.040 Food and Drug Administration (FDA) Approval of Medical Devices March 4, 2015 March 4, 2015 MA07.010 Biofeedback Therapy March 4, 2015 March 4, 2015 MA07.021 Partial Coherence Interferometry March 4, 2015 March 4, 2015 MA07.043 Smell and Taste Dysfunction Testing March 18, 2015 March 19, 2015 MA07.051 Intraoperative Neurophysiological Testing March 18, 2015 March 19, 2015 MA08.001 Vedolizumab (Entyvio ) March 18, 2015 March 19, 2015 MA09.015 Positron Emission Mammography (PEM) March 4, 2015 March 5, 2015 MA10.001 Pulmonary Rehabilitation Services March 4, 2015 March 5, 2015 ® February 21 – March 23, 2015 5 Policy # Title Reissue effective date Reissue published date MA11.003 Lung Volume Reduction Surgery (LVRS) March 4, 2015 March 5, 2015 MA11.005 Deep Brain Stimulation (DBS) March 18, 2015 March 19, 2015 MA11.043 Reimbursement for a Presbyopia- or Astigmatism-Correcting Intraocular Lens March 4, 2015 March 5, 2015 MA11.053 Sterilization March 4, 2015 March 4, 2015 MA11.081 Meniscal Allograft Transplantation March 18, 2015 March 19, 2015 MA11.095 Lysis of Epidural Adhesions March 4, 2015 March 5, 2015 MA11.098 Migraine Deactivation Surgery March 4, 2015 March 5, 2015 MA11.101 Nucleoplasty March 4, 2015 March 5, 2015 Coding updates The following Medicare Advantage policies have been reviewed and updated to add new and revised medical codes (e.g., ICD-9 and ICD-10 diagnosis codes; CPT® and HCPCS codes; revenue codes) and/or remove terminated medical codes. Policy # Title Effective date Published date MA00.027a Diagnostic Radiology Services Included in Capitation January 2, 2015 February 6, 2015 Revised March 18, 2015 MA00.033a Services Paid Above Capitation for Health Maintenance Organization (HMO) Primary Care Physicians January 2, 2015 February 24, 2015 MA03.006a Modifiers LT/RT: Left Side/Right Side Procedures January 2, 2015 March 20, 2015 MA08.004b Coagulation Factors for Hemophilia April 1, 2015 March 20, 2015 MA09.009a Diagnostic and Therapeutic Radiopharmaceutical Agents January 2, 2015 March 20, 2015 MA11.032a Multiple Surgical Reduction Guidelines January 2, 2015 March 20, 2015 Archived policies Independence has determined that it is no longer necessary for the following Medicare Advantage policies to remain active. Policy # Title Notification date Archive effective date MA11.038 Radiofrequency Micro-remodeling (by transurethral, transvaginal, or paraurethral approach) for Urinary Stress Incontinence February 11, 2015 March 13, 2015 MA11.094 Treatment for Hyperhidrosis (Nonpharmacologic) March 11, 2015 April 10, 2015 NaviNet is a registered trademark of NaviNet, Inc., an independent company. CPT copyright 2014 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. February 21 – March 23, 2015 6
© Copyright 2026