Left Behind: Unintentionally Retained Surgically Placed Foreign Bodies and How Pictorial Review
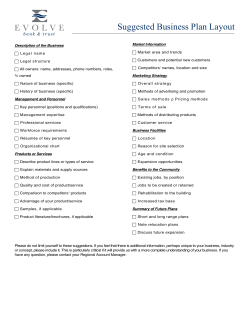
AJR Integrative Imaging LIFELONG LEARNING FOR RADIOLOGY Left Behind: Unintentionally Retained Surgically Placed Foreign Bodies and How to Reduce Their Incidence—Pictorial Review Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Gilbert Whang1, Greg T. Mogel, Jerome Tsai, Suzanne L. Palmer Objective Unintentionally retained surgically placed foreign bodies have been associated with increased morbidity and mortality, as well as increased costs and medicolegal consequences. This article reviews some of the most commonly retained surgical devices and provides a structured approach to intraoperative image acquisition and interpretation. By increasing the awareness of surgically placed foreign bodies, our goal is to reduce the incidence of and the complications associated with this difficult clinical problem. Conclusion Despite various systems and safeguards available, unintentionally retained surgically placed foreign bodies remain difficult to eliminate completely. Developing a standardized approach to the request, “intraoperative film, rule out foreign body,” is essential to reduce the adverse outcomes associated with this problem. Introduction Surgery often requires the placement of foreign material inside the human body. Many systems and safeguards are applied in the operating room (OR) to ensure that no material is left behind unintentionally after closure, but none is foolproof. Retained foreign bodies (RFBs), such as surgical sponges or gossypibomas (gossybium, Latin for cotton; and boma, Swahili for place of concealment), remain a clinically significant problem. Although the exact incidence is unknown, it has been reported to occur between one in 100 and one in 7,000 procedures [1, 2]. Approximately 1,500 cases of RFB occur annually in the United States [1]. RFBs undergo two types of foreign body reaction [3]: The first is an aseptic fibrinous response, resulting in formation of a granuloma, which can then undergo calcification and decomposition. This response is usually clinically silent and only incidentally discovered. The second is an inflammatory reaction, resulting in an abscess. In the body’s attempt to expel RFBs, fistulization, perforation of viscera, and bowel obstruction have been shown to occur [1, 3–5]. An analysis of medical malpractice claims by Gawande et al. [1] showed that the sequelae are serious, requiring reoperation in 69% of cases for removal of RFBs or management of the resulting complications. Twenty-two percent of the cases resulted in small-bowel fistulas, obstruction, or visceral perforation. One fatality was recorded. Less typical sequelae have been reported as well. Kester and Hassien [6] described a pulmonary embolism caused by pieces of a migrating surgical sponge. RFBs are also a cause of misdiagnosis. Because of the heterogeneous appearances on different imaging techniques, RFBs can mimic new primary tumors, recurrent tumors, and postsurgical collections [7–10]. The remnants of a decomposed surgical sponge have even masqueraded as an intrathoracic mass associated with bronchiectasis [11]. The lay public has often focused on this problem and the associated medicolegal implications [12]. Kaiser et al. [13] detailed claims from the files of a Massachusetts insurance company over a 7-year period, including total indemnity payments of more than $2 million and defense fees approaching $600,000. Gawande et al. [1] presented claims from 47 cases resulting in an average of more than $50,000 in costs for compensation and defense expenses. Finally, the Centers for Medicaid and Medicare Services have begun denying reimbursement for any costs associated with delayed retrieval of surgical equipment or the complications arising therefrom [14]. Many RFBs are detected soon after surgery: a mean of 21 days to detection, with 26% remaining undetected for 60 days or more [1]. Rappaport and Haynes [15] noted that 40% of gossypibomas are discovered within 1 year and that 50% are identified 5 years or more after surgery. One of the oldest known cases of an RFB is in the neurosurgical literature and is a retained surgical sponge after laminectomy. The time from retention to discovery was approximately 40 years [16]. Given all of the above, the radiologist is frequently confronted with the request, “rule out foreign body.” Interpretation of imaging studies (often, intraoperative radiographs) can be surprisingly complex for several reasons. For example, many surgical devices are intentionally placed and the reasons for ordering the study may vary dramatically (e.g., standard operating procedure vs incorrect count). Regardless, the radiologist must be prepared to confidently, Keywords: complications of surgery, foreign bodies, gossypiboma, iatrogenic injury, retained surgical sponges DOI:10.2214/AJR.09.7153 Received January 19, 2009; accepted after revision June 11, 2009. All authors: Department of Radiology, USC University Hospital, 1500 San Pablo St., 2nd Floor Imaging, Los Angeles, CA 90033. Address correspondence to G. Whang ([email protected]). 1 AJR 2009;193:S79–S89 0361–803X/09/1936–S79 © American Roentgen Ray Society AJR:193, December 2009 S79 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Whang et al. Fig. 1—67-year-old woman after aortic valve replacement. A, Clinical indication: missing sponge. Retained sponge was not seen on intraoperative chest radiograph (hard-copy image). B, Clinical indication: atypical chest pain, postoperative radiograph. Portable chest radiograph (hard-copy image) showed curvilinear radiographic density in right upper quadrant (arrow); follow-up abdominal film was recommended. C, Clinical indication: radiograph of kidneys, ureters, bladder to rule out foreign body. Intraoperative portable abdominal radiograph shows retained surgical sponge (arrow) overlying right upper quadrant (hard-copy image). D, Axial unenhanced CT image obtained 1 year later shows retained surgical sponge (oval) in right cardiophrenic region. A B C D and often quickly, render an interpretation that can dramatically alter the patient’s course. In this article, we seek to provide strategies and show, through cases, how best to navigate this important aspect of medical imaging. Predisposing Factors A number of factors have been proposed to explain the occurrence of unintentionally retained foreign bodies. Although the literature reflects some disagreement as to the relative risk of each, these risks can be broken down into two main categories. The first category is procedure-related risks, those applicable to a specific patient population or type of surgery. Procedure-related risks include the urgency of the procedure; multiple, complex, or lengthy procedures; and cases involving obese patients. The second category is process-related risks, reflecting the practices and culture of the surgical team. Processrelated risk factors are most commonly related to personnel changes during the surgical procedure, less-than-strict adherence to preoperative and postoperative device counts, and inconsistent policies regarding the use of intraoperative imaging. Kaiser et al. [13] reviewed approximately 10,000 malpractice claims over a 7-year period and identified 67 claims (0.67%) involving 40 patients with RFBs. Those authors S80 found that the factors resulting in retention included falsely correct device counts, or no device count at all, and falsely negative intraoperative radiography reports. The false-negative radiography reports were thought to be secondary to poor-quality images, intentionally placed medical devices on the image, and miscommunication of the true indication for the study. Gawande et al. [1] showed that retention of a foreign body was nine times as likely when an operation was performed on an emergency basis and four times as likely when the operation involved an unexpected change in procedure. Another conclusion was that patients with RFBs had significantly higher body mass indexes. A more recent study by Lincourt et al. [17] showed that foreign body retention increases with the complexity and duration of the surgical procedure and when the device counts are incorrect. Contrary to Gawande et al. [1], they did not find that increased body mass index, emergency surgery, or unexpected changes in operative procedure were predictors for RFBs. Unfortunately, it is difficult to pin down statistically significant risk factors because of the limitations of the studies published to date. The limitations of these studies include AJR:193, December 2009 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Retained Surgical Foreign Bodies A B C D E Fig. 2—55-year-old morbidly obese man after liver transplantation. A, Clinical indication: rule out foreign body. Intraoperative abdominal radiograph showed no radiopaque foreign body (hard-copy image). Image is underexposed because of large body habitus. B, Clinical indication: male after liver transplantation. Axial unenhanced CT image shows increased-density material adjacent to inferior vena cava (arrow). C, Sonogram shows echogenic structure producing acoustic shadowing (oval) adjacent to liver, which is the typical appearance of retained sponge on ultrasound. Excess abdominal fat or gas can interfere with localization by ultrasound. D, Intraoperative fluoroscopic image shows retained surgical sponges (arrow). E, Coronal unenhanced CT image shows retained surgical sponges (arrow). methods of data collection, variable reporting of medical errors, and unpredictable claims and suits. Medical errors, whether committed by the surgery team or the radiology team, contribute to the occurrence of RFBs. The following clinical cases highlight some of the problems that can occur in everyday practice. Clinical Scenarios Case 1 A 67-year-old woman underwent aortic valve replacement surgery. The intraoperative sponge count was incorrect, and a portable chest radiograph was obtained (Fig. 1A). A surgical progress note stated that the film was negative for RFBs. A follow-up portable chest radiograph (Fig. 1B) was reported as showing a curvilinear density overlying the right upper quadrant, of unclear cause; an abdominal radiograph was recommended. On postoperative day 2, a portable abdominal radiograph was obtained (Fig. 1C). The radiologist reported an irregular opacity in the right upper quadrant that was suspicious for an RFB. The radiology report noted that “the referring service was aware of the findings.” No further abdominal imaging was requested before discharge. No action was taken by the referring service. The sponge was found 1 AJR:193, December 2009 year later on a CT scan obtained for nonspecific upper abdominal pain (Fig. 1D). The sponge was surgically removed. The core problems identified were, first, inadequate intraoperative surveillance radiography because of poor radiographic technique. The first portable chest radiograph was never officially reported by a radiologist; it is uncertain whether the intraoperative film was ever presented to a radiologist for interpretation because no supporting documentation was found. At our institution, the surgeon decides when intraoperative images are necessary and whether they should be shown to a radiologist immediately. If the surgeon is comfortable viewing and interpreting the image in the given surgical setting, he or she may not request an immediate reading, and the image will be sent to the work list for routine reporting. If the surgeon requests an immediate reading, a radiologist is available either in house or on call 24 hours a day. The surgeon is responsible for directing the radiology technologist, deciding whether the area included in the image and the quality of the image are adequate. If an immediate reading is requested, the radiologist has the obligation to recommend repeat imaging or alternative imaging techniques if necessary. The second problem was failure to fully document and communicate the radiographic findings. A suspicious density was S81 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Whang et al. A B Fig. 3—68-year-old man after exploratory laparotomy, duodenostomy, and duodenal ulcer oversew. A, Clinical indication: rule out foreign body or retained surgical sponge. Intraoperative portable abdominal radiograph did not show retained sponge (hard-copy image). B, Postoperative day 2 portable abdominal radiograph shows retained laparotomy pad (oval) overlying pelvis (hard-copy image). A B Fig. 4—87-year-old man after aortic valve replacement. A, Because surgical sponge count was noted as correct, radiopaque sponge marker (arrow) was interpreted as normal postoperative finding (hard-copy image). B, Axial unenhanced CT image shows retained surgical sponge (arrow) in right pleural space. S82 AJR:193, December 2009 Retained Surgical Foreign Bodies Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Fig. 5—51-year-old man after low anterior resection. A, Scout film for CT scan. No radiopaque markers are seen. B, Axial contrast-enhanced CT image shows heterogeneous 10 × 9 × 12 cm soft-tissue mass (arrow) containing gas and fluid. A identified on the second portable chest radiograph and the portable abdominal radiograph obtained on postoperative day 2. The radiologist reported that this finding was communicated to the surgical service; however, the documentation of this contact was incomplete. The finding was not followed up by the surgical service. Because the name of the physician who was notified was not included in the report, the contact could not be confirmed and the finding was lost to follow-up. Case 2 A 55-year-old morbidly obese man underwent cadaveric donor liver transplantation. Two 4 × 4 surgical sponges were unaccounted for, and an intraoperative portable abdominal radiograph was obtained (Fig. 2A). The examination was reported as limited because of increased body habitus and poor technique. No RFBs were identified. The patient’s hospital course was complicated by recurrent febrile episodes. On postoperative day 18, unenhanced CT of the abdomen and pelvis was requested to evaluate for the cause of the persistent fevers and was interpreted as showing postoperative changes consistent with liver transplantation and no evidence of an abscess (Fig. 2B). The patient was discharged on postoperative day 21 but was readmitted on postoperative day 22 for nausea and nonbilious vomiting. An abdominal ultrasound showed a shadowing structure adjacent to the inferior vena cava anastomosis (Fig. 2C) and monophasic hepatic venous waveforms, consistent with venous outflow obstruction. The ultrasound correlated with the prior CT scan, and the reviewing radiologist became suspicious for an RFB. The attending surgeon was AJR:193, December 2009 B notified, and the patient underwent exploratory laparotomy. An intraoperative fluoroscopic image (Fig. 2D) on the day of exploratory laparotomy (postoperative day 26) confirmed the presence of radiopaque material in the right upper quadrant. Two surgical sponges directly posterior to the patient’s intrahepatic inferior vena cava were removed. Two core problems were identified. The first was inadequate intraoperative radiography because of the patient’s body habitus. The same standard technique for intraoperative imaging is used whether the RFB is a sponge or a needle. The patient’s estimated weight is used to adjust the kVp and mAs. An extra 5 kVp is added to account for the increased distance between the patient and the film cartridge. The x-ray source is set at the greatest distance to preserve the sterile field. Most portable units have a maximum kVp of 90 and maximum mAs of 320. Because of these limitations, adequate images may be impossible to obtain in the morbidly obese patient. In this case, many attempts were made without success to improve the quality of the image. The second problem was failure of the surgical service to communicate a persistently inaccurate sponge count, leading to failure of image interpretation. Two surgical sponges were left unaccounted for despite a thorough search of the OR. Had the radiologist been aware of this high suspicion, intraoperative fluoroscopy would have been recommended; if that was not helpful, immediate abdominal CT would be recommended for further evaluation. Because the radiologist’s index of suspicion was low, the radiodense material seen on the CT scan on postoperative day 18 was interpreted as intentionally placed surgical material. S83 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Whang et al. Case 3 A 68-year-old man underwent exploratory laparotomy, duodenostomy, and duodenal ulcer oversew for gastrointestinal bleeding. The intraoperative sponge count was incorrect, and a portable abdominal radiograph (Fig. 3A) was obtained. The clinical indication was “rule out foreign body/retained surgical sponge.” No retained sponge was seen, but other intended radiopaque tubes and drains were noted. A second portable abdominal radiograph was obtained 90 minutes later with the same clinical history. Clinical suspicion for a retained surgical sponge was high, but no retained foreign body was located. A portable abdominal radiograph obtained on postoperative day 2 (Fig. 3B) clearly showed a retained foreign body overlying the right side of the pelvis. The attending surgeon was subsequently notified and the sponge was removed. The core problem identified was inadequate intraoperative surveillance radiography because of incomplete examination. The retained laparotomy pad was not identified on the radiograph because it was not within the field of view. It is the surgeon who directs the radiology technologist in the OR. The areas included in the image are approved by the surgeon before presentation to the interpreting radiologist. In this case, the intraoperative study was initially interpreted by the surgeon and placed in the routine work list. No immediate reading was requested. Case 4 An 87-year-old man underwent aortic valve repair. The intraoperative sponge count was correct; therefore, no intraoperative imaging was performed. During the hospital course, a portable chest radiograph was obtained (Fig. 4A). The study was interpreted as showing surgical change in the right hemithorax after valve replacement. Subsequent portable chest radiographs were performed on postoperative day 5 to further evaluate the portable chest radiographic findings, and a retained sponge was located in to the right lateral pleural space (Fig. 4B). The attending surgeon was notified immediately, and the foreign body was removed 2 days later. The core problem identified was failure of the surgical service to communicate an inaccurate sponge count as the result of a counting error, leading to a failure of image interpretation. A correct count does not preclude the possibility of a retained surgical device; intraoperative counts can be incorrect [2]. Therefore, all nonbiologic devices seen on the radiograph must be scrutinized. Even though there was no clinical suspicion for an RFB, the appearance of a typical curvilinear density should have alerted the radiologist to the possibility of a retained sponge. Case 5 A 51-year-old man with rectal cancer underwent a low anterior resection. The intraoperative course was noteworthy for arterial bleeding after transection of the sigmoid mesentery. No details of sponge or instrument counts were given in S84 the operative report, and no intraoperative imaging was performed. CT was performed 7 weeks after surgery as a new baseline examination before chemotherapy. A scout film (Fig. 5A) showed right hip arthroplasty hardware and surgical clips. Contrast-enhanced CT of the abdomen and pelvis (Fig. 5B) showed a 10 × 9 × 12-cm soft-tissue structure with heterogeneous components, including gas and fluid. The case was discussed with the referring surgeon; because the differential diagnosis included abscess, encapsulated hematoma or phlegmon, and foreign body reaction, the patient underwent exploratory laparotomy. A large subfascial fluid collection containing a surgical towel was found. The core problem identified was failure of the surgical service to communicate an inaccurate towel count. There were no details of an incorrect sponge, towel, or instrument count, and after removal the surgical towel was found to have no radiopaque markers. This RFB would not have been seen on any intraoperative radiograph. Case 6 A 69-year-old cirrhotic man underwent liver transplantation. The operative report made no mention of an incorrect count or intraoperative complications. No intraoperative radiograph was requested. On postoperative day 1, a portable chest radiograph showed expected postoperative changes (Fig. 6A). Abdominal ultrasound showed the liver transplant and small postoperative fluid collections. The patient’s postoperative course was unremarkable. Unenhanced surveillance chest CT performed 5 months later showed a curvilinear radiopaque structure situated between the left lobe of the liver and the stomach (Fig. 6B). This finding of retained surgical sponge was relayed to the referring transplant surgeon, and it was removed surgically. MRI of the abdomen, performed the same day as CT, showed a 2.5-cm mass between the stomach and the liver (Figs. 6C and 6D). The core problem identified was failure of the surgical service to communicate an inaccurate sponge count, or failure of the surgical service to perform a count, leading to failure of perception. The surgical sponge was not detected on radiologic studies until it was looked for retrospectively, with adjustments in window settings (Fig. 6E). This could not have been done without computed radiography. The radiologist must remember to use window settings as a tool to increase the conspicuity of RFBs, especially in a suboptimal computed radiography or digital radiography image. Hard-copy images are difficult to manipulate; even if the image is scanned into a workstation, digital manipulation is limited. Case 7 A 55-year-old man underwent liver transplantation. Abdominal ultrasound on postoperative day 11 showed a 5-cm fluid collection posterior to the liver transplant, with internal echogenic material, that was consistent with gas (Fig. 7A). The referring service was alerted to the possibility of a AJR:193, December 2009 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Retained Surgical Foreign Bodies A B C D Fig. 6—69-year-old man after liver transplantation. A, This portable chest radiograph was read as normal postoperative changes, including multiple upper abdominal surgical clips and coils (computed radiography image). B, Axial unenhanced CT image shows retained surgical sponge between liver and stomach (arrow). C and D, Axial T2-weighted spin-echo (C) and T1-weighted gradient-echo (D) MR images show mass (arrow) between stomach and liver. Interestingly, metallic threads on surgical sponge did not cause susceptibility artifact on gradient-echo sequences. E, Resetting window of soft copy of initial portable chest radiograph increases ability to detect radiopaque foreign body (arrow). Even in retrospect, this sponge was difficult to detect with extreme window settings. AJR:193, December 2009 E S85 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Whang et al. focal abscess. On postoperative day 12, contrast-enhanced CT of the abdomen was performed for further evaluation. The collection of fluid and gas was noted between the liver and the inferior vena cava. It had the appearance of hemostatic packing material (Fig. 7B). This was confirmed at surgical evacuation of the retrohepatic abscess. The core problem identified was that there are mimics of unintentionally retained foreign bodies. The RFB in this case was intentionally placed for hemostasis. Postoperative imaging showed a suspicious fluid collection, which at surgical evacuation was confirmed to be superinfected, absorbable hemostatic material. Typically, absorbable hemostatic material has fairly uniform airlike radiolucency [10, 18]. Sterile gas bubbles can be seen and may persist as long as 6 months after surgical intervention. Discussion Surgery inherently involves the placement of foreign material inside the human body. Therefore, the risk of such material being left behind can never be fully eliminated. Medical imaging, among many other practices and procedures, can serve to mitigate this risk and reduce the morbidity, mortality, and medicolegal consequences associated with RFBs. Universal precautionary measures, such as the practice of counting surgical sponges, needles, and instruments are undertaken to decrease the likelihood of retaining surgical devices. The Association of periOperative Registered Nurses (AORN) Practices Committee presents detailed guidelines and best practices for avoiding retained surgical devices [19]. Some of these include using only sponges that can be detected at radiography and performing counts of sponges, needles, and instruments numerous times before, during, and after the procedure. When counts are incorrect, routine surgical exploration is undertaken, and radiographs of the pertinent surgical cavity should be obtained. The radiologist’s role is to locate suspected RFBs and to ensure proper communication of the findings in a clinically relevant time. Several aspects of the interaction make this task complex. At our institution, not all intraoperative images are interpreted immediately by a radiologist. The surgeon must request an immediate reading; otherwise, the study is sent to the routine work list and reported after the patient has left the OR. In these cases, it is the surgeon who controls the image quality and content. A radiologist is available 24 hours a day for immediate interpretations if necessary. The seven clinical cases presented here highlight some common problems that can cause delay in the diagnosis of unintentional RFBs. Case 1 presents an example of failure to fully document and communicate the radiographic findings. It is unknown why the initial intraoperative hard-copy radiograph was not officially read, or whether it was reviewed by a radiologist at the time of the study. With the advent of computed radiography, digital radiography, and PACS, these lost films are nearly a thing of the past. The radiologist reported the possibility of a retained sponge on the patient’s portable abdominal radiograph and second portable chest radiograph; however, there was inadequate documentation of direct communication to the referring service. Without proper documentation, there is no way to confirm that the critical information was adequately conveyed to the surgeons. To facilitate communication at our institution, imaging orders to search for unaccounted surgical sponges or devices are accompanied by a request form (Fig. 8) that details suspected RFB, the type of operation performed, and the surgical site. Using this information, the radiologist can evaluate the study more critically to confirm that the radiology technologist obtained the appropriate images, with the pa- A B Fig. 7—55-year-old cirrhotic man after liver transplantation. A, Longitudinal sonogram shows 5-cm fluid collection posterior to liver with internal echogenic material, consistent with gas. B, Axial contrast-enhanced CT image shows collection (arrow) of air and fluid between liver and inferior vena cava. S86 AJR:193, December 2009 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Retained Surgical Foreign Bodies tient properly positioned and with the region of interest in the field of view. If necessary, additional radiographs should be requested. Clear documentation of the encounter is mandatory and should include the full name of the informed clinician as well as the date and time of notification. If the findings are not dictated immediately, the radiologist must also make a note in the PACS system. Cases 1–3 are examples of inadequate intraoperative surveillance radiography because of image acquisition (poor technique or incomplete inclusion of surgical field) or patient body habitus. The primary technique for the imaging diagnosis of RFB is conventional radiography, and when performed appropriately, its immediate availability is invaluable to referring surgeons and interpreting radiologists. Intraoperative films are technically difficult to acquire, partly because of the portable nature of the examination, the requirement of maintaining a sterile field, and the presence of multiple intentionally placed surgical devices in the field of interest. Radiologists must be well versed in the radiographic appearance of common surgical devices and must have a high index of suspicion that any device may be unintentionally retained. Any technical problems encountered and the areas of the body imaged should be commented on in the radiology report. If an immediate reading is requested, the imaging findings should be communicated directly to the surgeon before he or she leaves the OR. Multiple radiographs may be needed for full coverage. The radiologist should clearly state in the final report how many images were obtained. If an RFB cannot be excluded on the intraoperative study, an appropriate alternative technique, if available, should be recommended. Intraoperative fluoroscopy may be used to further evaluate a specific area or density seen on the portable radiographs. Fluoroscopy can be especially helpful in distinguishing a retained surgical needle from an intentionally placed surgical clip. In patients with many surgical clips, distinguishing a small needle may be impossible; therefore, if the surgical needle is not found fluoroscopically, the patient’s incision is closed and no further imaging is requested. If a high incidence of suspicion for an RFB remains, unenhanced CT should be considered. Retained sponges on CT typically are seen as soft-tissue-density masses with a whorled texture or spongiform pattern because of air trapping within the synthetic fibers of the sponge (Fig. 9A). A rim-enhancing wall or calcified rim may be seen as well [20, 21]. The scout image should be examined for unexpected findings that are not readily apparent on the obtained sequences (Fig. 9B). MRI does not reliably show foreign bodies because of the lack of signal given off by inert objects. A retained surgical sponge may appear as a soft-tissue-signal-intensity collection or mass with a well-defined capsule and a complex mixed signal pattern [18] (Figs. 6C and 6D). Cases 2–6 present the failure of the surgical service to count correctly or to communicate an inaccurate sponge AJR:193, December 2009 count, leading to failure of perception or interpretation of RFBs. The radiologist must remember that an unintended RFB may be found even when the intraoperative counts are correct. The first postoperative portable chest radiograph in case 4 showed multiple well-visualized surgical devices, one of which was unintentional (Fig. 4A). Failure to recognize its appearance on radiographs could have been a result of unfamiliarity with its appearance (Fig. 10). Adjusting window settings of the portable chest radiograph in case 6 was the only way to detect the subdiaphragmatic RFB (Fig. 6E). This is only possible if the image is on PACS. Surgical sponges are not inherently radiopaque. Bariumimpregnated threads were introduced in the United States in 1933 [22]. Today, radiopaque markers are interwoven into surgical sponges or are in an attached string or tail. Occasionally, distortion of the surgical sponges in vivo will alter the normal appearance of radiopaque markers, decreasing conspicuity of an RFB (Fig. 2B). In such instances, multiplanar reformatted CT can visualize the findings in different angles and planes (Fig. 2E). Volume-rendered images may also aid the surgeon in presurgical planning [23]. Fig. 8—Example of information form to be filled out by operating room personnel (scrub/circulating nurses) at time of intraoperative radiologic examination. S87 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Whang et al. A B Fig. 9—Status postexploratory laparotomy in a 26-year-old man. A, Axial contrast-enhanced CT image shows soft-tissue-density mass with gas and high-density material (arrow). B, Scout image for CT scan of abdomen and pelvis clearly shows radiopaque marker (arrow). Retained bullets (arrowheads) are also seen. Surgical sponge was subsequently removed. A B Fig. 10—Representative surgical devices. A, Photograph shows representative devices on surgical tray. B, Radiograph of same objects as in A. S88 AJR:193, December 2009 Downloaded from www.ajronline.org by 176.9.124.142 on 09/16/14 from IP address 176.9.124.142. Copyright ARRS. For personal use only; all rights reserved Retained Surgical Foreign Bodies Radiofrequency identification is a promising new technology that might significantly reduce the occurrence of RFBs. Surgical devices such as sponges are tagged with radiofrequency identification chips, and a handheld wand device is used to detect tagged RFBs intraoperatively [24]. The first Food and Drug Administration–approved radiofrequency identification system, the SMARTSPONGE system, was recently introduced by ClearCount Medical Solutions, Inc. The radiologist’s role in the standardized approach to the request to “rule out foreign body” involves image acquisition, image interpretation, and proper communication with the referring clinician [25]. Failure in one or more of these areas may result in delayed diagnosis, resulting in increased morbidity and mortality. Options B, C, and D are not the best responses. Conclusion Unintentional RFBs are not common, but when a case occurs the risk of increased morbidity, mortality, and medico legal complications is increased. The departments of surgery and radiology must work together to help prevent these occurrences. Radiologists should have a high index of suspicion for RFBs when examining all postoperative patients, whether the surgery was recent or distant. All nonbiologic objects must be accounted for when imaging studies are interpreted. Therefore, the radiologist should be familiar with the radiographic appearances of these surgical devices and be prepared to use all necessary tools, especially window- and level-setting changes of radiographs. Proper communication between the radiologist and surgeon is extremely important, including timely telephone calls and appropriate documentation in the radiology report. Through the development and implementation of a standardized approach to the request to “rule out foreign body,” the incidence of unintentional RFBs can be reduced. Acknowledgments I would like to thank Suzanne Palmer and Greg Mogel for their continued support and guidance in my career devlopment. My thanks also to D. Randall Radin for contribution of a clinical case for this manuscript. References 1. Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner MJ. Risk factors for retained instruments and sponges after surgery. N Engl J Med 2003; 348:229–235 2. Egorova NN, Moskowitz A, Gelijns A, et al. Managing the prevention of retained surgical instruments: what is the value of counting? Ann Surg 2008; 247:13–18 3. Dux M, Ganten M, Lubienski A, Grenacher L. Retained surgical sponge with migration into the duodenum and persistent duodenal fistula. Eur Radiol 2002; 12:S74–S77 4. Robinson KB, Levin EJ. Erosion of retained surgical sponges into the intestine. AJR 1966; 96:339–343 5. Gonzalez-Ojeda A, Rodriguez-Alcantar DA, Arenas-Marquez H, et al. Retained foreign bodies following intra-abdominal surgery. Hepatogastroenterology 1999; 46:808–812 6. Kester NL, Hassien JD. Pulmonary embolism caused by a surgical sponge. AJR 1992; 158:757–759 7. Hoeffner EG, Soulen RL, Christensen CW. Gelatin sponge mimicking a pelvic neoplasm on MR imaging. AJR 1991; 157:1227–1228 8. Okten AI, Adam M, Gezercan Y. Textiloma: a case of foreign body mimicking a spinal mass. Eur Spine J 2006; 15:S626–S629 9. Dane C, Yayla M, Dane B. A foreign body (gossypiboma) in pregnancy: first report of a case. Gynecol Surg 2006; 3:130–131 10.Sandrasegaran K, Lall C, Rajesh A, Maglinte DT. Distinguishing gelatin bioabsorbable sponge and postoperative abdominal abscess on CT. AJR 2005; 184:475–480 11. Suwatanapongched T, Boonkasem S, Sathianpitayakul E, Leelachaikul P. Intrathoracic gossypiboma: radiographic and CT findings. Br J Radiol 2005; 78:851–853 12. Burton S. The biggest mistake of their lives. The New York Times, March 16, 2003 13.Kaiser CW, Friedman S, Spurling KP, Slowick T, Kaiser HA. The retained surgical sponge. Ann Surg 1996; 224:79–84 14.Sack K. Medicare won’t pay for medical errors. The New York Times, October 1, 2008 15.Rappaport W, Haynes K. The retained surgical sponge following intra-abdominal surgery. Arch Surg 1990; 125:405–407 16.Stoll A. Retained surgical sponge 40 years after laminectomy. Surg Neurol 1988; 30:235–236 17.Lincourt AE, Harrell A, Cristiano J, Sechrist C, Kercher K, Heniford BT. Retained foreign bodies after surgery. J Surg Res 2007; 138:170–174 18.O’Connor AR, Coakley FV, Meng MV, Eberhardt S. Imaging of retained surgical sponges in the abdomen and pelvis. AJR 2003; 180:481–489 19.[No authors indicated]. Recommended practices for sponge, sharps, and instrument counts. AORN J 2006; 83:418–433 20.Kokubo T, Itai Y, Ohtomo K, Yoshikawa K, Iio M, Atomi Y. Retained surgical sponges: CT and ultrasound appearance. Radiology 1987; 165:415–418 21.Kalovidouris A, Kehagias D, Moulopoulos L, Gouliamos A, Pentea S, Vlahos L. Abdominal retained surgical sponges: CT appearance. Eur Radiol 1999; 9:1407–1410 22.Hyslop JW, Maull KI. Natural history of a retained surgical sponge. South Med J 1982; 75:657–660 23.Ariz C, Horton KM, Fishman EK. 3D CT evaluation of retained foreign bodies. Emerg Radiol 2004; 11:95–99 24.Macario A, Morris D, Morris S. Initial clinical evaluation of a handheld device for detecting retained surgical gauze sponges using radiofrequency identification technology. Arch Surg 2006; 141:659–662 25.Tsai J, Whang G, Mogel GT, Palmer SL. “Rule out foreign body”: how to routinely find missing surgical devices through optimization of image acquisition, protocol standardization and physician communication. AJR 2008; 190 [American Roentgen Ray Society 108th Annual Meeting Abstract Book suppl]:201 F O R YO U R I N F O R M AT I O N The reader’s attention is directed to the Self-Assessment Module for this article, which appears on the preceding pages. AJR:193, December 2009 S89
© Copyright 2026