Antibiotic guide Update: 22/03/2006
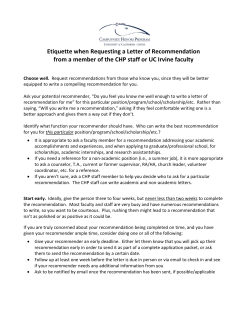
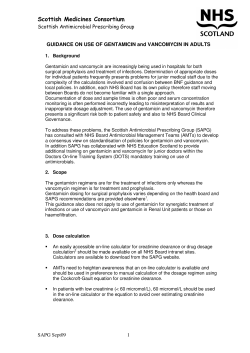
Antibiotic guide Update: 22/03/2006 Category ABCDE- III III - Definition Strength of recommendation Good evidence to support a recommendation for use Moderate evidence to support a recommendation for use Poor evidence to support a recommendation for or against use Moderate evidence to support a recommendation against use Good evidence to support a recommendation against use Quality of evidence Evidence from at least one properly randomized, controlled trial Evidence from at least one well-designed clinical trial without randomization, from cohort or casecontrolled analytic studies (preferably from more than one center), from multiple time-series studies, or from dramatic results in uncontrolled experiments Evidence from opinions of respected authorities, based on clinical experience, descriptive studies, or reports of expert committees Reference: Clin Infect Dis 1994 ;18 :421 o o o o o 1.1. Meningitis, meningo-encephalitis, brain abscess 1.1.1. Community acquired purulent meningitis (non HIV) 1.1.2. Community acquired non purulent meningitis (non HIV) 1.1.3. Méningo-encephalitis 1.1.4. Brain abscess 1.2. Urinary tract infections 1.2.1. Acute urethritis 1.2.2. Acute prostatitis 1.2.3. Chronic bacterial prostatitis 1.2.4. Pyelonephritis 1.3. Digestive infections 1.3.1. Acute infectious diarrhea 1.3.2. Mild community acquired peritonitis 1.3.3. Severe community acquired peritonitis 1.3.4. Cholecystitis, cholangitis 1.3.5. Liver abscess 1.4. Skin and soft tissue infections 1.4.1. Gangrene, necrotizing fasciitis, severe cellulitis in diabetes mellitus patients 1.4.2. Superficial cellulitis, non complicated erysipelas (facial excluded) 1.4.3. Facial cellulitis 1.5. Various infections 1.5.1. Community acquired septic shock (unknown origin, non neutropenic) 1.5.2. Septic arthritis 1.5.3. Bites (cat, dog, human) 1.5.4. Venous catheter associated lymphangitis without bacteremia 1.5.5. Peripheral and central venous catheter associated bacteremia 1.6. HEENT 1.6.1. Pharyngitis 1.6.2. Acute otitis media: first episode 1.6.3. Acute otitis media: treatment failure at day-3 1.6.4. Acute sinusitis 1.7. Respiratory infections 1.7.1. Community acquired pneumonia: PORT severity index 1.7.2. Community acquired pneumonia (Class I and II, non associated pleural effusion) 1.7.3. Community acquired pneumonia (Class III to V, and any class with associated pleural effusion) 1.7.4. acute bacterial exacerbation of chronic bronchitis o o o o 1.8. Gynecologic infections 1.8.1. Non suppurated primitive salpingitis 1.8.2. Suppurated primitive salpingitis 1.9. Endocarditis 1.9.1. Enterococcus spp., Streptococcus spp., HACEK and blood culture negative endocarditis 1.9.2. Endocarditis: other 1.9.3. Methicillin susceptible Staphylococcus aureus endocarditis 1.10. Vascular infections 1.10.1. Vascular graft infections (vascular graft removed) 1.10.2. Vascular graft infections (vascular graft not removed) 1.11. Diabetic foot infections 1.11.1. Without associated osteomyelitis 1.11.2. With associated polymicrobial osteomyelitis and no sepsis 1.11.3. With associated polymicrobial osteomyelitis and sepsis 1.11.4. With associated monomicrobial osteomyelitis o o 1.1. Meningitis, meningo-encephalitis, brain abscess • • • • Community acquired purulent meningitis (non HIV) Community acquired non purulent meningitis (non HIV) Méningo-encephalitis Brain abscess 1.1.1. Community acquired purulent meningitis Etiologic agents: Streptococcus pneumoniae, Neisseria meningitidis, Listeria, Haemophilus influenzae Empiric treatment for all Community acquired purulent meningitis (non HIV) Treatment Route and dosage Ceftriaxone Amoxicillin 2g X2/d IV 2g X6/d IV 15 mg/Kg, then 60 mg/Kg/d IV continuous. Vancomycin Target levels: 30 µg/ml Strength of recommendation A A Quality of evidence III III A III Duration Streptococcus pneumoniae Treatment Stop amoxicillin Route and dosage Strength of recommendation Quality of evidence Duration AND CARRY ON Ceftriaxone Vancomycin. (stop if susceptible to ceftriaxone)) 2g X2/d A III 60 mg/Kg/d continuous.. Target levels: 30 µg/ml A III 10 to 14 days Neisseria meningitidis Treatment Route and dosage Strength of recommendation Quality of evidence Duration Stop Amoxicillin AND CARRY ON Ceftriaxon 2g X2/d IV A II 7 days Listeria Treatment Stop ceftriaxone vancomycin AND START Amoxicillin Gentamicin Route and dosage Strength of recommendation Quality of evidence 2g X6/d IV 4,5mg/Kg/d IV A A II II Duration and 21 days References: 1. Sanford guide to antimicrobial therapy 2004 2. Johns Hopkins University Division of Infectious Diseases antibiotic guide 1.1.2. Community acquired non purulent meningitis (non HIV) Etiologic agents: Entérovirus, Listeria, leptospira Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Amoxicilline (Clamoxyl®) 2g X6/j IV B III 7 days Alternative treatment : (proven penicillin allergy) Treatment Route and dosage Strength of recommendation Quality of evidence Duration Triméthoprim/sulfaméthoxazole 15 à 20 mg/Kg/d IV (triméthoprim) in 3 or 4 injection/d B III 7 days Enterovirus Treatment Route and dosage Strength of recommendation Quality of evidence Duration Stop antibiotics Human herpes virus Treatment Route and dosage Strength of recommendation Quality of evidence Duration Stop antibiotics and start Acyclovir 10 mg/KgX3/d IV 14 à 21 days 1.1.3. Meningo-encephalitis Etiologic agents: Herpes simplex, Listeria monocytogenes, Mycobacterium tuberculosis, Varicella zoster virus Treatment Treatment Amoxicillin Acyclovir Rifampin Isoniazid Ethambutol Route and dosage Strength of recommendation Quality of evidence 2gX6/d IV 10 mg/KgX3/d IV 10 mg/Kg/d oral or IV B* III* 5 mg/Kg/d oral or IV 20 mg/Kg/d oral or IV Duration 21 days 21 days 1 year 1 year 2 months Pyrazinamide (Pirilène®) 30 mg/Kg/j per os 2 months * our recommandation 1.1.4. Brain abscess Etiologic agents: Steptocoques, Bacteroides, enterobacteria Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Ceftriaxone 2gX2/d IV B II 6 to 12 weeks* Metronidazole 7,5 mg/KgX4/d IV B II 6 to 12 weeks* * Duration of Treatment not codified. Depend on CT Scan and/or MRI References: 1. Sanford guide to antimicrobial therapy 2004 2. Johns Hopkins University Division of Infectious Diseases antibiotic guide 3. Clin Infect Dis. 1993;17:857-63. 1.2. Urinary tract infections • • • • Acute urethritis Acute prostatitis Chronic bacterial prostatitis Pyelonephritis 1.2.1. Acute urethritis Etiologic agents: Neisseria gonorhoeae, Chlamydia trachomatis, Ureaplasma urealyticum, Trichomonas vaginalis Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Ceftriaxone 500 mg IM A II One injection Azithromycin 1g oral A II Single dose Reference 1. CDC 1998 STD treatment Guidelines ( MMWR 1998 ; 47 : 49-52) 1.2.2. Acute prostatitis Etiologic agents: E coli , Proteus spp, Klebsiella spp , Enterococcus spp, S aureus, N. gonorrhoeae , C trachomatis Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Ofloxacin 200 mgx2/d oral B III 28 days References: 1. Sanford guide for antimicrobial therapy 2004 Rev Med Int 2002 ;23 :999-1005 1.2.3. Chronic bacterial prostatitis Etiologic agents : E coli , Proteus spp, Klebsiella spp , Enterococcus spp, S aureus Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Ofloxacin 200 mg x 2 / d oral B III 28 days Alternative treatment Route and dosage 1 DS tabletX2/d Triméthoprim/sulfaméthoxazole DS oral Treatment Strength of recommendation Quality of evidence Duration B III 28 days Reference: 1. Sanford guide for antimicrobial therapy 2004 Rev Med Int 2002 ;23 :999-1005 1.2.4. Pyelonephritis Etiologic agents : Enterobacteria, enterococcus Treatment Must be adapted to antimicrobial susceptibility Treatment Route and dosage Strength of recommendationQuality of evidence Duration Escherichia coli : ciprofloxacin 500 mgX2/d oral 14 days Entérococcus : amoxicillin 1 grX3/d oral 14 days Empiric treatment waiting antimicrobial susceptibility Treatment Route and dosage Strength of recommendation Quality of evidence Duration Ciprofloxacin 500 mgX2/d day Alternative empiric treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Ceftriaxon 2 g/d IM or IV 1.3. Digestive infections • • • Acute infectious diarrhea Mild community acquired peritonitis Severe community acquired peritonitis • • Cholecystis, cholangitis Liver abscess 1.3.1. Acute infectious diarrhea Etiologic agents: Viruses, Salmonella sp, Shigella, Campylobacter jejuni, E. coli, staphylococcus, amibiasis Treatment Treatment Route and dosage Moderate diarrhoea (less than 6 episodes per day and no fever) Symptomatic treatment Severe diarrheoa (more than 6 episodes per 500 mgX2/d day, fever) Ciprofloxacin Alternative treatment Strength of recommendation Quality of evidence A I A II Duration 3 to 5 days Treatment Triméthoprim/sulfaméthoxazole Route and dosage 1 DS tabletX2/d Strength of recommendation B Quality of evidence II Duration 3 to 5 days References: 1. J Infect Dis. 1993 Nov;168(5):1304-7. Arch Intern Med. 1990 Mar;150(3):541-6. 2. Sanford guide to antimicrobial therapy 2004 3. Johns Hopkins University Division of Infectious Diseases antibiotic guide 1.3.2. Mild community acquired peritonitis Etiologic agents: Enterobacteria, pneumocoque, entérocoque, anaérobies Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Amoxicillin/clavulanate 1 gX3/d oral or IV B III 10 days Gentamicin 160 mg/d IV B III 3 days 1.3.3. Severe community acquired peritonitis Etiologic agents: Entérobactéries, pneumocoque, entérocoque, anaérobies, P. aeruginosa, BGN Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Piperacillin/tazobactam 4 gX3/d IV B III 10 days Gentamicin 160 mg/d IV B III 3 days 1.3.4. Cholecystitis, cholangitis Etiologic agents : Enterobacteria, entérocoques, bacteroides, clostridium Treatment Treatment Ceftriaxone Metronidazole Route and dosage Strength of recommendation Quality of evidence Duration 2 g/d IV B III Cholecystitis : 24 to 48 hours after surgery or 3 to 5 days after surgery if delayed surgery 500 mgX4/d oral or IV B III Cholangitis : 7 to 10 days 1.3.5. Liver abscess Etiologic agents: Enterobacteria, Bacteroides, entérococcus, Entamoeba hystolytica Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration* Ceftriaxone 2 g/d IV B III 1 to 4 months Metronidazole 500 mgX4/d oral B III 1 to 4 months *If confirmed amebiasis, then treat with Metronidazole alone for 10 days Reference: 1. Sanford guide to antimicrobial therapy 2004 1.4. Skin and soft tissues infections • • • 1.4.1. • Gangrene, necrotizing fasciitis, severe cellulitis in diabetes mellitus patients Superficial cellulitis, non complicated erysipelas (facial excluded) Facial cellulitis Gangrene, necrotizing fasciitis, severe cellulitis in diabetes mellitus patients Etiologic agents: Clostridium perfringens, Clostridium sp., group A, C and G Streptococcus , gram negative rods Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Pipéracillin/tazobactam 4 gX3/d IV B III 10 to 28 days If associated septic shock Treatment Route and dosage Strength of recommendation Quality of evidence Duration Pipéracillin/tazobactam 4 gX3/d IV B III 10 to 28 days Gentamicin 160 mg/d IV B III 3 days References: 1. Sanford guide to antimicrobial therapy 2004 2. Johns Hopkins University Division of Infectious Diseases antibiotic guide 1.4.2. • Superficial cellulitis, non complicated erysipelas (facial excluded) Etiologic agents: group A, B, C and G Streptococcus, Staphylococcus aureus Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Amoxicillin/clavulanat 1gX3/d oral B II 3 days after recovery. Not more than 10 days References: 1. J Int Med Res. 1991;19(6):433-45. 2. Eur J Clin Microbiol Infect Dis. 1991;10(10):880-4. Alternative treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Azithromycin 500 mg on day-1, then 250 mg/d B II 5 days References: 1. Cutis. 1984;34(6):567-70 2. Antimicrob Agents Chemother. 1983;24(6):856-9. 3. Antimicrob Agents Chemother. 1983;24(5):679-81. 1.4.3. Facial cellulitis Etiologic agents: Staphylococcus aureus, group A Streptococcus Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Oxacillin 2gX6/d IV B III 3 days after recovery. Alternative treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Vancomycin 2 g/d IV B III 3 days after recovery. References: 1. Sanford guide to antimicrobial therapy 2004 2. Johns Hopkins University Division of Infectious Diseases antibiotic guide 1.5. Various infections • • • • 1.5.1. • Community acquired septic shock (unknown origin, non neutropenic) Septic arthritis Bites (cat, dog, human)Venous catheter associated lymphangitis without bacteremia) Peripheral and central venous catheter associated bacteremia Community acquired septic shock (unknown origin, non neutropenic) Etiologic agents: gram negative rods, gram positive, other (Klebsiella sp. and staphylococcus aureus) Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Pipéracilline/tazobactam 4 gX3/d IV B III Non codified Vancomycin 2 g/j IV B III Alternative treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Imipenem 1 gX3/d IV B III Non codified Vancomycin 2 g/d IV B III References: 1. Sanford guide to antimicrobial therapy 2004 2. Johns Hopkins University Division of Infectious Diseases antibiotic guide 1.5.2. Septic arthritis Etiologic agents: S. aureus, streptococcus, haemophilus sp., Neisseria gonorrheae, other Treatment Treatment Adapted to susceptibility Route and dosage Strength of recommendation Quality of evidence antimicrobial Empiric treatment waiting for antimicrobial susceptibility Treatment Route and dosage Strength of recommendation Quality of evidence Duration Vancomycin 2 g/d IV B III 1.5.3. Bites (cat, dog, human Comment: 1. Role of antimicrobial treatment debated in case of small bite at early stage (< 9 hours) Duration 14 to 28 days 2. Check tetanus vaccination 3. Evaluate HIV risk in case of human bite 4. Evaluate rabies risk Etiologic agents: Pasteurella multocida, Bacteroides spp., Capnocytiphaga, S. aureus Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Amoxicillin/clavulanate 1 gX3/d oral B II 10 days References: 1. Sanford guide to antimicrobial therapy 2004 2. Pediatr Emerg Care. 1992;8:194-9 3. Am J Emerg Med. 2004;22:10-3 4. Arch Emerg Med. 1989;6:251-6 1.5.4. Venous catheter associated lymphangitis without bacteremia Treatment Remove catheter • 3 blood culture • No antibiotic if negative blood cultures References: 1. Clin Infect Dis 2001 ;32 :1249-72 • 1.5.5. Peripheral and central venous catheter associated bacteremia Treatment: • Remove catheter • 3 blood cultures • Antimicrobial treatment adapted to antimicrobial susceptibility (initial blood culture). Start treatment after the third blood culture • If 3 negative blood cultures, then stop antibiotics • If ay least 1 positive blood culture, then carry on antimicrobial treatment for 14 days • Search for metastatic localization (transoesop^hageal echocardiography, CT Scan of the thorax and abdomen, vertebram MRI if pain). Then treatment duration is 6 weeks * Duration du Treatment : 14 jour si bactériémie simple. 6 semaines en cas de localisation septique secondaire References: 1. Clin Infect Dis 2001 ;32 :1249-72 1.6. HEENT • • • • Pharyngitis Acute otitis media: first episode Acute otitis media: treatment failure at day-3 Acute sinusitis 1.6.1. Pharyngitis Etiologic agents: • Viruses ( Rhinovirus, coronavirus..) +++++ • Group A Streptococcus, Anaerobes, Neisseria gonorrhoeae, Corynebacterium diptheriae, other Treat only confirmed group A Streptococcus pharyngitis Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Pénicillin V 1 million UI X 3 / d oral A II 10 days Alternative treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Azithromycin 500 mg/d oral (1 daily dose) A II 3 Days References: 1. Clin Infect Dis 2002 ;35 :113-125 1.6.2. Acute otitis media Etiologic agents : Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Viruses Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration If no antimicrobial treatment in the 1gX3/d oral previous month: Amoxicillin If antimicrobial treatment in the previous 2gX3/d oral month : Amoxicillin B II 10 days B II 10 days Alternative treatment Treatment Azithromycin Route and dosage Strength of recommendation Quality of evidence Duration 500 mg at day-1, then 250 mg/d B II 5 days oral References: 1. Ann Otol Rhinol Laryngol Suppl. 2000;183:1-12. 2. Pediatr Infect Dis J. 2000;19(2):95-104 3. Pediatr Infect Dis J. 1996;15(Suppl 9):4-9. 1.6.3. Acute otitis media: treatment failure at day-3 Etiologic agents: Streptococcus pneumoniae Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Ceftriaxone 2g/d IM B III 3 days References: 1. Pediatr Infect Dis J. 1998;17(10):963-8 2. Sanford guide to antimicrobial therapy 2004 3. Johns Hopkins University Division of Infectious Diseases antibiotic guide 1.6.4. Acute sinusitis Etiologic agents: • Bcteria: 0,2 to 10% o H. influenzae, S. pneumoniae, group A streptococcus, M. catarrhalis, S. aureus, anaerobes • allergy or viruses : 90 à 99% o Coronavirus, Parainfluenza virus, Rhinovirus Treatment Treatment Route and dosage Symptomatic treatment Persistent symptoms at day-7 or severe initial presentation (major pain, fever > 38°C): Amoxicillin/ 1gX3/d oral clavulanate Strength of recommendation A Quality of evidence I B III Duration 7 days 10 days Alternative treatment (proven penicillin allergy) Treatment Route and dosage Strength of recommendation Quality of evidence Duration Azithromycin 500 mg day-1, then 250 mg / d oral B I 5 days References: 1. 2. 3. 4. Arch Intern Med. 2003 Aug 11-25;163(15):1793-8 (non intérêt amoxicilline/clavulanate d emblée) Antimicrob Agents Chemother. 2003;47(9):2770-4 Sanford guide to antimicrobial therapy 2004 Johns Hopkins University Division of Infectious Diseases antibiotic guide 1.7. Respiratory infections • • • • 1.7.1. • Community acquired pneumonia: PORT severity index Community acquired pneumonia (Class I and II, not associated with pleural effusion) Community acquired pneumonia (Class III to V, and any class with associated pleural effusion) Acute bacterial exacerbation of chronic bronchitis Community acquired pneumonia: PORT severity index PORT severity index Patient characteristics Demographic factor male Points assigned No. Of years of age Female No. Of years of age - 10 Nursing home resident +10 Comorbid illness Neoplastic disease +30 Liver disease +20 Congestive heart failure +10 Cerebrovascular disease +10 Renal disease +10 Physical examination findings Altered mental status +20 Respiratory rate > 30 breaths/min +20 Systolic blood pressure < 90 mm Hg +20 Temperature < 35°C or > 40°C +15 Puls > 125 beats/min +10 Laboratory or radiographic findings Arterial PH < 7,35 +30 Blood urea nitrogen > 30 mg/dL +20 Sodium < 130 mEq/l +20 Glucose > 250 mg/dL +10 Hematocrit < 30% +10 Arterial partial pressure of oxygen < 60 mm Hg +10 Pleural effusion +10 Score Class Points Class I 0,1% Class II > 70 Class III 71 à 90 Class IV 91 à 130 Class V 131 1.7.2. • Mortality note age < 50 years, non of the 5 comorbid conditions (see table), normal or only mild deranged vital signs, and normal mental status 0,6% à 0,7% 0,9% à 2,8% 8,2% à 9,3% 27% à 31% Community acquired pneumonia (Class I and II, not associated with pleural effusion) Etiologic agents: S pneumoniae, Mycoplasma pneumoniae, Chlamydia pneumoniae, Coxiella burnetii ( H influenza, Moraxella catarrhalis) Treatment Treatment Telithromycin 1.7.3. • Route and dosage Strength of recommendation Quality of evidence Duration 800 mg/d oral B II 3 to 5 days apyrexia Community acquired pneumonia (Class III to V, and any class with associated pleural effusion) Etiologic agents: S pneumoniae, Mycoplasma pneumloniae, Chlamydia pneumoniae, Coxiella burnetii ( H influenza, Moraxella catarrhalis) Treatment Treatment Azithromycin Ceftriaxone Change azithromycin to erythromycin if oral route impossible Route and dosage 500 mg/d at day-1, then 250 mg/d oral 2 g/d IV 1gX3/j IV Strength of recommendation Quality of evidence B II B II Duration If alcoholism, coma, psychotropic treatment, neurological conditions (suspected aspiration pneumonia), ad to the previous treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Metronidazole 500 mgX3/d oral or IV B III *Duration: 3 to 5 days after apyrexia or 3 weeks if associated pleural effusion References: 1. Clin Infect Dis 2003 ; 37 : 1405-33 1.7.4. • Acute bacterial exacerbation of chronic bronchitis Etiologic agents Viruses, S pneumoniae, H influenza, Moraxella catharrhalis. Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Amoxicillin 1g X 3 / d oral B III 7 days Alternative treatment Treatment Telithromycin Route and dosage Strength of recommendation Quality of evidence Duration 800 mg/d oral B III 7days Treatment recommandation: • Bronchitis in patients with no underlying conditions: no antibiotics • Acute bacterial exacerbation of chronic bronchitis without obstructive syndrome: no antibiotics • Acute bacterial exacerbation of chronic bronchitis without obstructive syndrome in case of persistent fever > 38°C after 3 days: start antibiotics • Acute bacterial exacerbation of chronic bronchitis with obstructive syndrome: start antibiotics 1.8. Gynecologic infections • • 1.8.1. • Non suppurated primitive salpingitis Suppurated primitive salpingitis Non suppurated primitive salpingitis Etiologic agents: Neisseria gonohorroeae, Chlamydia, Bacteroides, enterobacteria, streptococcus Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration Ofloxacin 400 mgX2/d oral B III 14 days Metronidazole 500 mgX2/d oral B III 14 days Alternative treatment Treatment Route and dosage Strength of recommendation Ceftriaxone Doxycycline 1 g IM 100 mgX2/d oral B B Quality of evidence III III Duration 1 injection 14 days References: 1. Sanford guide to antimicrobial therapy 2004 2. MMWR 1998;47:79-86 1.8.2. • Suppurated primitive salpingitis Etiologic agents : Neisseria gonohorroeae, Chlamydia, Bacteroides, enterobacteria, streptococcus Treatment Treatment Clindamycin Route and dosage Strength of recommendation Quality of evidence Duration 900 mgX3/d IV B III 24 hours after apyrexia 4,5 mg/Kg/d IV or IM 24 hours after apyrexia, change 100 mgX2/d treatment to : Doxycycline oral Gentamicin B III 24 hours after apyrexia B III 14 days References: 1. Sanford guide to antimicrobial therapy 2004 2. MMWR 1998;47:79-86 1.9. Endocarditis • • • 1.9.1. • Enterococcus spp., Streptococcus spp., HACEK and blood culture negative endocarditis Endocarditis: other Methicillin susceptible Staphylococcus aureus endocarditis Enterococcus spp., Streptococcus spp., HACEK and blood culture negative endocarditis Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration* Amoxicillin 2 grX6/d IV B III Gentamicin 3 mg/Kg/d IV B III *Duration: • • • • • • Pénicillin G susceptible Sterptococcus (CMI < 0.1) and non complicated native cardiac valves: 2 weeks of combination therapy Streptococcus (Pénicillin G: 0.1 < CMI < 0.5): 2 weeks of combination therapy, then 2 weeks amoxicillin IV alone. Streptococcus (Penicillin G: CMI > 0.5, Enterococcus: 6 weeks of combination therapy Complicated streptococcus endocarditis and/or prosthetic cardiac valves: 2 weeks of combination therapy, then 4 weeks amoxicillin IV alone. Blood culture negative endocarditis: 3 weeks of combination therapy, then 3 weeks amoxicillin IV alone HACEK: 4 weeks of combination therapy 1.9.2. Endocarditis: other Coagulase negative Staphylococcus, methicillin resistant Staphylococcus aureus, enterococcus (Penicillin G CMI > 16 µg/ml), blood culture negative pacemaker-related endocarditis, post-operative endocarditis (< 12 months), right-sided endocarditis, nosocomial endocarditis Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration* Vancomycin 30 mg/Kg/d B III Gentamicin 3 mg/Kg/d IV B III *Duration: • • Staphylococcus and blood culture negative endocarditis: 7 days of combination therapy, then 5 weeks vancomycin IV for native valves; 2 weeks of combination therapy, then 4 weeks vancomycin IV for prosthetic valves and pacemakers. Enterococcus : 6 weeks of combination therapy. 1.9.3. Methicillin susceptible Staphylococcus aureus endocarditis Treatment Treatment Route and dosage Strength of recommendation Quality of evidence Duration* cloxacillin 2 grX6/d IV B III Gentamicin 3 mg/Kg/d IV B III *Duration: • 7 days of combination therapy, then 5 weeks cloxacillin alone for native valves; 2 weeks of combination therapy, then 5 weeks cloxacillin alone for prosthetic valves. 1.10. Vascular infections • • 1.10.1. • Vascular graft infections (vascular graft removed) Vascular graft infections (vascular graft not removed) Vascular graft infections (vascular graft removed) Methicillin susceptible Staphylococcus aureus Treatment Route and dosage Strength of recommendation Quality of evidence Duration* oxacillin 2 grX6/d IV B III Methicillin-resistant Staphylococcus aureus, coagulase-negative Staphylococcus, infection of lower limb vascular graft (unknown etiologic agent) Treatment Route and dosage Strength of recommendation Quality of evidence Duration* Vancomycin 2 g/d IVSE B III Enterococcus and Streptococcus Treatment Route and dosage Strength of recommendation Quality of evidence Duration* Amoxicillin 2 grX6/d IV B III Gram-negative rods and intra abdominal vascular graft (unknown etiologic agent) Treatment Route and dosage Strength of recommendation Quality of evidence Duration* Ticarcillin/clavulanate 5 grX3/d IV B III Pseudomonas spp. Treatment Route and dosage Strength of recommendation Quality of evidence Duration* ceftazidime 1 grX3/d IV B III gentamicin 160 mg/d IV B III ciprofloxacin 500 mgX3/d oral B III Fungi Treatment amphotericin B flucytosine IN CASE OF RENAL FAILURE Change amphotericin B to liposomal amphotericin B Route and dosage Strength of recommendation Quality of evidence B III B III B III 1 mg/Kg/d IV (in 12 hours) 100 mg/Kg/d IV 3 mg/Kg/j IV *Duration: 1 week after vascular graft removal 1.10.2. • Vascular graft infections (vascular graft not removed) Susceptible Staphylococcus aureus and coagulase-negative staphylococcus Treatment Route and dosage Strength of recommendation Quality of evidence Duration* Rifampin 300 mgX3/d oral B III ofloxacin 200 mgX2/d oral Duration* Resistant Staphylococcus aureus and coagulase-negative staphylococcus Route and dosage Strength of recommendation Quality of evidence IF POSSIBLE Rifampin Fusidic acid IF NOT 300 mgX3/D oral 2 tabletsX2/d oral B B III III triméthoprim/sulfaméthoxazole 2 DS tabletsX3/d oral B III 600 mgX3/d oral B III 2 g/d IV B III Treatment OR clindamycin OR Vancomycin Pseudomonas aeruginosa Duration* Treatment Route and dosage Strength of recommendation Quality of evidence Duration ceftazidime 1 grX3/d IV B III ciprofloxacin 500 mgX3/d oral B III 3 weeks gentamicin 160 mg/d IV B III THEN ciprofloxacin 500 mgX3/d oral B III 3 weeks ceftazidime 1 grX3/d IV B III THEN ciprofloxacin 500 mgX3/d oral B III 4 months 1/2 Enterobacteria Treatment Route and dosage Strength of recommendation Quality of evidence triméthoprim/sulfaméthoxazole 2 DS tablets X3/d oral B III Duration* Enterococcus and Streptococcus Treatment Route and dosage Strength of recommendation Quality of evidence Duration* amoxicillin 2 grX3/d oral B III Unknown etiologic agent Treatment triméthoprim/sulfaméthoxazole clindamycin Route and dosage 2 DS tabletsX3/d oral 600 mgX3/d oral *Duration: 6 months 1.11. Diabetic foot infections Strength of recommendation Quality of evidence B III B III Duration* Without associated osteomyelitis With associated polymicrobial osteomyelitis and no sepsis With associated polymicrobial osteomyelitis and sepsis With associated monomicrobial osteomyelitis • • • • 1.11.1. • Without associated osteomyelitis Treatment Treatment triméthoprim/sulfaméthoxazole clindamycin 1.11.2. • Route and dosage 1 DS tabletX3/d oral 600 mgX3/d oral Strength of recommendation Quality of evidence Duration B III 3 weeks B III 3 weeks With associated polymicrobial osteomyelitis and no sepsis Treatment Treatment triméthoprim/sulfaméthoxazole clindamycin 1.11.3. • Route and dosage 1 DS tabletX3/d oral 600 mgX3/d oral Strength of recommendation Quality of evidence Duration B III 6 weeks B III 6 weeks With associated polymicrobial osteomyelitis and sepsis Treatment Treatment Ticarcillin/clavulanate THEN triméthoprim/sulfaméthoxazole clindamycin Route and dosage 5 gX3/d IV 1 DS tabletX3/d oral 600 mgX3/d oral Strength of recommendation B Quality of evidence III B III 6 weeks B III 6 weeks Duration 10 days 1.11.4. • With associated monomicrobial osteomyelitis Treatment Treatment Adapted to antimicrobial susceptibility Route and dosage Strength of recommendation Quality of evidence Duration 6 weeks
© Copyright 2026