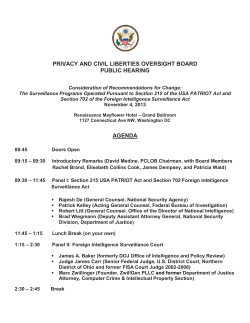
Building a Public Health Community of Practice APC Training Conference
Building a Public Health Community of Practice How to Take Biosurveillance to the Next Level and Reap its Broad Benefits APC Training Conference February 19, 2008 Prepared and presented by: Bill Stephens, MS, APC Manager Dean Lampman, MBA, Regional Surveillance Coordinator Kay Sanyal-Mukherji, MPH, Workforce Development Specialist 1 Agenda Topic: 1. 2. 3. 4. 5. 6. 7. 8. 9. Pre-test Communities of public health practice overview Biosurveillance fundamentals and best practices Health partnerships applied: response protocols Break Interactive group session 1 Interactive group session 2 Discussion of group sessions / conclusion Post-test Time: 10 25 25 30 15 15 15 20 10 2 Pre-test 3 Learning objectives: At the end of this session, participants will be able to: • Describe three functional areas of biosurveillance where syndromic surveillance applies and clinician-only input is insufficient. • Identify the primary purposes of biosurveillance and how it can benefit public health and other stakeholders in a public health community of practice. • List and apply several key decision-making criteria contained in biosurveillance system response protocols that are used to evaluate and respond to public health threats. 4 The context for public health information systems: • Healthcare in the U.S. ‘under fire’ for a variety of reasons: – Poor quality of care, errors resulting in more deaths annually than highway accidents, breast cancer or AIDS – Presence of disparities in access to care and in health outcomes – National disasters, terrorism or infectious disease public health threats – Rapidly increasing costs of healthcare • One response: American Health Information Community (AHIC) – – – – Federally chartered 9-13-05 Advisory committee Provides input to HHS Goal is to achieve common interoperability framework for health IT with input from a broad range of stakeholders on achieving widespread adoption – Work performed by four workgroups: • Population Health and Clinical Care Connections – Biosurveillance Data Steering Group • Consumer Empowerment • Chronic Care • Electronic Health Records 5 Context for public health information systems continued: • 12-06: Pandemic and All-Hazards Preparedness Act (PAHPA) – Broad implications for HHS’s preparedness and response activities – New Assistant Secretary for Preparedness and Response (ASPR) – Establish quadrennial National Health Security Strategy and support new programs (e.g., advanced development of medical countermeasures) • 11-07: Homeland Security Presidential Directive 21 (HSPD-21) – Establish biosurveillance capability for early warning of a biological attack or disease outbreak w/ ongoing “near real-time” updates – Formulate “comprehensive plan for promoting community public health and medical preparedness to help those building resilient communities” – Develop “disaster medical capability that can immediately re-orient and coordinate resources within all sectors to satisfy community needs” – Foster medical countermeasure stockpiling and distribution so that communities can “distribute and dispense countermeasures” in 48 hours 6 AHIC: It’s different … and powerful “Why is this group different than any of the hundreds of others who regularly gather under different banners and acronyms for the same purpose? Spoken bluntly, the answer is market power. Around this table sits representatives of the federal and state agencies that pay for and regulate a major piece of the $1.7 trillion dollars a year spent on health care in America.” Dr. Michael O. Leavitt Secretary, DHHS 7 AHIC’s key objective: Creating a robust health IT environment that brings together: • Public Health Information • Electronic Health Records (EHR) • Personal Health Records (PHR) • Open source, open standards for data and security /privacy • Interoperable Health Information Exchanges (HIE) 8 AHIC priorities and use case roadmap The AHIC MDS enables achievement of the requirements in the biosurveillance use case. 9 HIEs will link public health and clinical care entities: • Population Health and Clinical Care Connections Workgroup recommendations include: -- 1.0: Develop a business case for data information exchange between public health and clinical care as well as develop a communications plan to improve the understanding of the need for this exchange -- 1.3: Support the establishment of a proof-of-concept demonstrating the added value of sharing data from clinical care to public health through health information exchanges. -- 1.4: Develop a plan to encourage the integration of state funded public health surveillance programs and health information exchanges. • Harmonized biosurveillance use case defined to provide input to HITSP standards including: – A framework or “functional area matrix” for public health and healthcare – Biosurveillance data standards via a Minimum Data Set (MDS) – Lab reporting standards for EHR and public health 10 Why focus on the biosurveillance use case? • Primarily, it provides the baseline for the broadest possible response to recommendation 1.0 from the PHCCC workgroup • Secondarily, it integrates data requirements (MDS) across the functional areas matrix (FAM) in which public health and healthcare generally will share information in the “brave new world” of health information exchanges. – Open source software and industry standards are making it work: “Linux had Apache; healthcare gets Mirth. Our "killer app" has arrived...” - Ron Sweeny, Academic Medical Imaging - Western Michigan 11 What is biosurveillance? The BDSG adopted ASTHO’s definition of biosurveillance in fall 2006: Biosurveillance is often referred to as syndromic surveillance; however the ability to detect events early requires a broader set of information than that of syndromes. While there’s no single agreed-upon definition, there’s agreement that such “biosurveillance” systems need to take advantage of integrated data from multiple sources including public health information as well as electronic health information not traditionally monitored by public health. 12 What is biosurveillance? Biosurveillance systems must leverage two major surveillance methods: o Well-established public health surveillance methods and sources used for the tracking, monitoring, and reporting of health-related information, such as epidemiologic investigations of infectious disease outbreaks or environmental conditions are needed to ensure a broad coverage of data sources, to use as baselines comparisons, and to support the accuracy and reliability of the biosurveillance findings. o Early event detection and situational awareness - the use of an automated system to evaluate case and suspected case reporting along with statistical surveillance and data visualization of pre-diagnostic and diagnostic data to support the earliest possible detection of events that may signal a public health emergency - are essential components for near real-time detection of natural or man-made health events. 13 Functional areas for health information Early event detection: 1. Secondary use of clinical care and other health-related data for early identification of public health events 2. Reportable disease case reporting from clinical care via the Web and 24/7 call reporting systems with triage of disease urgency 3. Situational awareness of the size, location, and spread of a health event using secondary use data and case reporting 4. Disease data exchange using HL7-specific implementation guides 5. Detection algorithms to determine and visualize deviation from normal disease patterns Outbreak management: 1. Case investigation and management 2. Exposure contact tracing 3. Exposure source investigation and linking of cases and contacts to exposure sources 4. Data collection, packaging, and shipment of clinical and environmental specimens 5. Integration with early event detection and countermeasure administration capabilities 6. Linking laboratory test results with clinical case data 7. Flexibility to support agent-specific and emerging requirements while adhering to standard terminology and data relationships Connecting laboratory systems: 1. Standard HL7 message formats and terminology standards for specimen receipt and laboratory result reporting 2. Receipt and management of specimen and sample data 3. Monitoring of testing activity to project load distribution during a large-scale event Source: Office of the National Coordinator, Health IT 14 Functional areas for health information (cont’d) Countermeasure and response administration: 1. Support and track administration of vaccinations and prophylaxes 2. Support apportionment and allocation for limited supplies 3. Traceability to drug lot, vaccinator, or clinic 4. Adverse events monitoring 5. Follow-up of patients (e.g., vaccine "take" response evaluation) 6. Isolation and quarantine monitoring and tracking 7. Links to distribution vehicles (such as commercial distribution channels and the Strategic National Stockpile to provide traceability between distributed and administered products 8. Integration with immunization and disease registries Partner communications and alerting: 1. Rapid distribution of health alerts and communications to public health workers, primary care physicians, public health laboratory workers, the public, etc. 2. Multiple channels of distribution: e-mail, pagers, voicemail, and/or automated faxing 3. Selective distribution based on the urgency and sensitivity of the message 4. Collaborative communications (Web boards, threaded discussions, and Web conferencing) among a defined set of involved public health professionals 15 Functional areas for health information (cont’d) Cross-functional components: 1. Secure message transport: ensuring messages are received and read only by intended audiences 2. Public health directory: for consistent, uniform management of people, roles, organizations, organization types, and jurisdictions when exchanging information 3. Recipient addressing: identifying appropriate recipient lists for information exchange 4. Terminology standards: adhering to standard vocabulary lists and structures 5. System security and availability: protecting systems from sabotage or failure, and protecting data from corruption or unauthorized access 6. Privacy: protecting patients and organizations from fraudulent or unauthorized use of their information 16 Functional areas where syndromic surveillance applies: • Early event detection • Outbreak management • Partner communication and alerting And where clinician input alone is insufficient because: • The scale of these tasks exceeds clinicians’ capabilities • Clinicians are not properly trained for these tasks • Early detection requires no significant time lag, which is common in clinical confirmation (e.g., for lab tests) – Support for these claims and more reasons presented in next section … 17 What is a community of public heath practice? • People and organizations working together who may share resources in an effective, efficient way – working towards separate but related solutions. • Partners: – Hospitals and physicians – Schools, school-based clinics and daycares – EMS providers, law enforcement and other first responders – Long-term care facilities and mental health care providers – Public information officers and the media – Academics, vendors, subject-matter experts, where applicable – Insurance companies 18 What is a community of public heath practice? (con’t.) • Resources and practices: – Surveillance data and systems • And their accompanying response protocols – Networks/grids, IT assets and solutions, including: • Applications • Databases • Forums – Medical facilities and laboratories – Governance models – RHIOs, HIEs 19 20 21 Current North Central Texas Surveillance Communications Model: “A Loose Federation” Hospitals ----------------------THR Baylor HCA Tenet Others Hospital Council ----------------------Serves hospitals Provides reports Leads exercises Maintains EM Systems Local Public Health -----------------------Dallas County Collin County Denton County Wichita County State Public Health -----------------------Region 2/3 Office (Arlington, TX) Regional EPI Group ICPs and ICP Committees APC / TCPH ---------------------Maintains HIE and supporting tools Federal Public Health -----------------------CDC (Atlanta, GA) Leads collaboration, but cannot set policy beyond Tarrant County Comments: Legend: = required reporting relationship = voluntary reporting relationship = some required & some voluntary reporting Strength: The model works. Collaboration is occurring. Each participant maintains a high degree of control over their own event alert response protocols. Weakness: The model lacks formal HIE governance. The high degree of autonomy of each participant limits the ability of the region to quickly develop a consistent response protocol. Gaps may exist22 that are difficult to pinpoint and also challenging to overcome. Communities of public health practice overview What questions may we answer at this point? 23 Agenda Topic: 1. 2. 3. 4. 5. 6. 7. 8. 9. Pre-test Communities of public health practice overview Biosurveillance fundamentals and best practices Health partnerships applied: response protocols Break Interactive group session 1 Interactive group session 2 Discussion of group sessions / conclusion Post-test Time: 10 25 25 30 15 15 15 20 10 24 Syndromic surveillance definition, purpose: • Syndromic surveillance has been defined as "the timely collection, analysis, and investigation of healthrelated data that precede diagnosis." • Syndromic surveillance is used to: – Trace disease patterns over time – Describe patterns of disease in geographic locations and demographics at any time – Detect changes in community health status, especially for the early detection of outbreaks – Reduce morbidity and mortality (improve health status) 25 Is early detection important? With a pandemic possible, it seems vital! “Any community that fails to prepare, with the expectation that the federal government (or for that matter, the state government) will be able to step forward and come to their rescue at the final hour, will be tragically wrong -- not because we will lack a collective wallet, but because there is no way that you can respond to every hometown in America at the same time.” 1918 Pandemic: Worst epidemic ever 20 to 40 million deaths -- HHS Secretary Leavitt, April 20, 2006 26 Isn’t clinician input enough? “Where’s Doctor Smith?” Definitely not! For many reasons … • Automated surveillance doesn’t sleep, doesn’t get bored, doesn’t play golf, and is good at the math • Many physicians are not trained in “He’s seeing patient Green.” infectious disease or public health • Systems that rely on human input have poor compliance rates – Even if a disease is detected that is legally required to be reported, studies show that < 10% of such cases are actually reported • Timely clinical detection is unlikely for CDC Category A agents – Incorrect clinician diagnosis rate: > 50%; incorrect response rate: 75% – Most pathogens require tests typically not on hand or routinely ordered – The best case, anthrax, may show positive from a routine test in 18 hours See handout: “Challenges to Rapid Clinical Detection of Select Agents,” by Dr. David Siegrist, 6-26-06 27 Biosurveillance transcends early event detection: Situational awareness requires deep data in a window of opportunity: • • • • Initial detection (identify event rapidly) Quantification (how many are ill?) Localization (where is this happening?) Investigation (demographics, etiology, conveyance, travel histories, etc.) • Subsequent detection (identify more cases) • Outbreak management (confirm, track cases) • Countermeasures (isolation, vaccination) • Target (illness, deaths recede) 28 Biosurveillance transcends early event detection: Situational awareness requires broad data across outbreak health cycle: • Exposure occurs, but feels fine initially • Headache, fever (pharmacies) • Develops cough (call hotline) • • • • Sees provider (care visit, absent) Calls ambulance, admitted (EMS / ED) Critical, ICU, lab tests (diagnosed) Expires (reported) 29 Infectious disease outbreak health cycle: 30 Partner participation benefits: • Early awareness is preparedness – Consider potential for pandemic, bioterrorism, etc. • Supports infection control goals – Shows community patterns (MRSA) • Enhances image of provider • Fosters collaboration with others and public health on health problem solving • Chance to influence project directions • When open systems apply, low or no cost • Likely ancillary IT / operational benefits 31 How partners share data with public health: • Sign data use agreement (aka contract) with ‘HIPAA’ coverage for data elements (AHIC MDS) to be shared – Contract can be amended if data elements change • Assess network connections and transfer methods, which are typically VPN and HL7, but can vary • Identify and link to interfaces (often done w/ interface engine) • Send test files, work out mapping issues • Total project time varies, but usually can be accurately estimated and isn’t “huge.” “It’s not rocket science!” 32 Biosurveillance’s scope of work (per CDC) • Purpose is to: – Establish near real-time electronic nationwide public health situational awareness capability via interoperable network of systems (e.g., NHIN) – Share data to enhance rapid response to, and management of, potentially catastrophic infectious disease outbreaks and other public health emergencies. • Requires simultaneous provision of data to all levels of public health • Successful HIEs (aka public health community of practice) must: – Standardize information storage and messaging formats – Resolve varying local, state, and federal regulations – Address privacy concerns – Accurately identify patients 33 Biosurveillance’s scope of work (continued): Activities to be addressed: 1. Minimum Data Set (MDS) for biosurveillance Evaluate availability and usefulness for situational awareness 2. Interoperability standards 3. Bidirectional communication 4. Data quality and accessibility 5. Data evaluation and assessment to detect, characterize and track a public health threat 6. Evidence of effectiveness, costs and scalability 34 AHIC MDS: Gold standard MDS = 58 elements Facility data • 1-5 = Base data • 6-23 = Daily data 10 Patient data (24-33) Patient data 23 Facility data Clinical data (34-43) Clinical data Lab data (44-58) Lab data 15 Facility (23) = 40% Other (35) = 60% 10 MDS = situational awareness, anything < only offers early warning BioSense seeks MDS inputs, CDC seeks to validate MDS’ utility 35 = TBD (possible threat?) = TBD schools = targeted in ’08 = existing Evolving Case Study: North Texas 36 52 data feeds, 120+ users The starting point was hospitals 37 ESSENCE application’s impact: • • • • • User view allows collaboration with public health – Has proven valuable for hospital ICPs, others • One of several systems used for N. Texas surveillance • Differs from RODS in how it generates, sends alerts Offers good slicing, dicing capabilities for analysis Used by Dallas County to identify heat emergencies Offers physician data, school absenteeism modules Continuously enhanced to address user feedback “ESSENCE let’s us view what’s happening in our multihospital system. We can monitor in real time patients being seen and admitted, an impossible task otherwise. It’s user friendly, and best of all, it’s at no cost to us.” -- Judy Prescott, Manager, Epidemiology, Baylor University Medical Center 38 EpiAgent enhances local situational awareness: • EpiAgent is a PHIN-compliant next-generation surveillance tool from General Biodefense • A clinical event monitor, it applies a case-based analytical model and offers rule-based analysis of clinical data (e.g. MDS) • Can automatically detect individual instances of targeted items: – Anthrax (existing rules) – Varicella, aka chicken pox (existing rules) – MRSA (future rules) • Cases found can send alerts automatically to authorized users – Authorized users can include hospitals and public health • Ideal complement to syndromic surveillance systems, which have proven effective with case counts of 100, 500, 1,000 and 5,000 A key expansion point is hospitals 39 Next steps for participating hospitals: • Support provision of more data for situational awareness – This applies regardless of the phasing of any MDS project • Champion project to share AHIC MDS data – Keep staff and management aware of the benefits • Encourage system use, identify areas for improvement • Improve data quality (pursue standards of data entry) – Make staff aware they’re feeding an analytical system • Improve data analysis and response (apply protocols) – Be available when called on by public health staff We’re making it easy by asking for test data! EpiAgent demo can open the treasure chest! 40 Contact presenters for demo 41 LEFR system key features: • Portal uses audible alerting to prompt agency monitors when new notifications are posted • Color coding of notifications conveys relative urgency of events • Supporting text is concise, action oriented; brevity avoids scrolling • ‘Show more’ links provide details; complete event history accessible • Users can also add their comments to notifications or send their own messages (not tied to a notification) 42 Contact presenters for demo 43 Data Flow Within School Health Surveillance System Data entry form on open source portal (DNN) XML DB on open source portal Open source ETL tool (Mirth) Royalty-free ESSENCE DB at TCPH Royalty free ESSENCE application Efficient, affordable, replicable method 44 Users click on their choices among a series of images with large to small geographic coverage 45 Users can click on the next or previous links to see other images in the series and click the close link to return the main maps page. 46 This page provides access to flu prevention resources school nurses can use. More resources or topics could be added. 47 Biosurveillance fundamentals and best practices What questions may we answer at this point? 48 Agenda Topic: 1. 2. 3. 4. 5. 6. 7. 8. 9. Pre-test Communities of public health practice overview Biosurveillance fundamentals and best practices Health partnerships applied: response protocols Break Interactive group session 1 Interactive group session 2 Discussion of group sessions / conclusion Post-test Time: 10 25 25 30 15 15 15 20 10 49 Why response protocols matter: • Clear guidelines needed to review and summarize large amounts of data, daily • Approaches or steps to review data and analyze the importance of anomalies in data • Prompt inquiries that need to be completed in hours or days, depending on estimated degree of urgency – Example: Phone consultation with physician at a hospital • Essential for determining relative value of different approaches in outbreak detection in each system • Provides information useful to determine efficiency of system in detecting outbreaks in the initial stages 50 Why response protocols matter: • They can help maximize the functionality and value of a surveillance system • A standard framework can help distinguish statistical anomalies from more important public health events • Can translate to time and cost savings for PH in: – Investigating alerts – Systems development, maintenance and upgrades 51 Response protocols framework: • • • • Anomaly detection Anomaly characterization Validation of anomaly Assessing public health significance of findings • Other factors of importance 52 Anomaly detection: • Systems use statistical algorithm to determine if actual case counts exceed expected counts for syndromes • Helps epidemiologists spot suspicious disease clusters • Healthcare providers send information on unusual disease clusters and incidence that system can evaluate • Detection should occur at multiple levels to discover anomalies that may be missed in a single jurisdiction 53 Anomaly detection: • Check quality and completeness of data: – Onset of exposure, symptoms, behavior – Timeliness, capture of data – Completion of data processing – Application of pattern recognition – Sufficient records available – Generation of automated alert 54 Anomaly characterization: • Anomaly should be described fully w/ respect to person, place, and time (descriptive epidemiology) • Use geographic and demographic information • Clinical data should be evaluated and summarized • More information may be needed to fully characterize 55 Anomaly characterization: Key questions to explore: • How widespread is the pattern? • Are similar patterns found elsewhere? • How many days has anomaly lasted? • Has geographical spread changed over time? • Does anomaly affect certain demographics? 56 Anomaly validation: Anomalies: expected or unusual? • • • • • • Seasonal or temporal (e.g. ILI) Environmental causes Disease trends Corroborate data sources Holiday, day-of-week effects Same pattern prior year? BioSense protocol: (protocol continued on next slide) 57 Assessing public health significance of findings: Public health significance? • Extent of variance from usual frequency distribution • Atypical from known patterns • Magnitude, continuity of increase given syndrome group • Sustained for multiple days? 58 Other factors of importance: • Unique attributes of the data stream to assess: – Lag time between occurrence of an event and time it is available to the system for detection of anomaly – Clinical value of the data • One data stream or source may be chosen as primary indicator of change and other data sources as secondary • Compare anomaly w/ other surveillance systems 59 Considerations in drafting response protocols: • Most tasks in response protocols overlap • Concept similar to early stages of outbreak investigation • Procedures for response protocols will vary based on: – Surveillance system the protocol supports – Jurisdiction in which it operates – Agency preferences • Communication of findings and response should be: – Consistent for anomalies/events of similar nature/importance – Easily and routinely monitored – Shared across all levels and jurisdictions 60 Constraints in drafting response protocols: Variables that effect the design of a common protocol: • • • • • • • • Agency size Experience Training Degree of risk Time pressures Data quality (lag time) Jurisdiction Department level 61 Agency protocol #1: Tarrant County • Factors that constitute a concern: – Unusual epidemiology – High number of excess cases – Multiple sites with excess – Sustained increase • Detection of anomaly that is of concern: – Consultation with chief epidemiologist – Review medical records and/or follow-up with patients – Lab testing – Consultation with key public health officials – Send alerts to health providers – Outbreak confirmed; outbreak investigation 62 Agency protocol #2: CDC BioSense Protocol steps: • Identify anomalies • Prioritize anomaly list • Characterize anomaly • Make a decision • Determine action 63 Sample protocol usage scenario #1: Bubba’s unhappy campers Background: – Clinician in Weatherford, TX notices several of her patients coming in with common symptoms – 43 patients presented at hospital with diarrhea, nausea, vomiting, and some with fever – No final diagnosis, but she suspects something Action: – She contacts director of LHD with information – Sanitarian is director of LHD – LHD does not have staff or surveillance system to investigate 64 Sample protocol usage scenario #1: Bubba’s unhappy campers • Sanitarian contacts regional health department • RHD queries ESSENCE to analyze chief complaints – Finds similar counts with symptoms under the GI (gastrointestinal) syndrome – MAP portal in ESSENCE is based on GIS technology – Counts high in Weatherford only, not nearby areas 65 66 Sample protocol usage scenario #1: Bubba’s unhappy campers • Investigators check ESSENCE data against OTC sales – Increase in sales of Pepto-Bismol and similar products • Investigators note that there’s unusual health event occurring in the Weatherford area hospital 67 Sample protocol usage scenario #1: Bubba’s unhappy campers • Epidemiologists from RHD sent to work with clinician to investigate • Clinician reveals that some patients have returned with fevers • Epis review medical charts and order lab tests 68 Sample protocol usage scenario #1: Bubba’s unhappy campers • Epis, sanitarian interview all patients – Finding: all ate at same place (Bubba’s Chicken Shack) on same day – All ate the daily fried chicken special • Sanitarian investigates – Finding: food was contaminated • Restaurant shut down for investigation 69 Sample protocol usage scenario #1: Bubba’s unhappy campers • Tests come back positive for Campylobacter – Bacterium spread through contamination, especially through undercooked poultry – Can cause chronic diarrhea • PH director at RHD sees a need for intervention and issues a media release 70 Sample protocol usage scenario #1: Bubba’s unhappy campers • LHD and RHD issue a public health alert and media statement • Few additional victims come forward • All victims are given effective antibiotics 71 Sample protocol usage scenario #1: Bubba’s unhappy campers • Bubba self-medicates at his favorite watering hole • Quite late the next day, Bubba’s hurting again, so he takes still more meds 72 Sample protocol usage scenario #2: What to ask & say if the anthraxswer is blowin’ in the wind 73 Sample protocol usage scenario #2: What to ask & say if the anthraxswer is blowin’ in the wind • Background: • While monitoring the LE/FR Surveillance System in May, 2007, the Arlington (Texas) Police Department a notices yellow advisory involving increased respiratory complaints • Advisory concentrated in their location and adjacent locations • Advisory issued by Tarrant County Public Health, which cited significant increase in respiratory problems • Advisory indicates that the precise cause of the problems is being investigated and more information will be forthcoming 74 Sample protocol usage scenario #2: What to ask & say if the anthraxswer is blowin’ in the wind Action: • LHD contacts Police Department to indicate that public health is aware of the situation and is investigating • Public health’s LE/FR system advisory notification indicates: – The respiratory problem is significant and widespread in the county – For officer’s safety, and with bioterrorism a possibility not yet ruled out, it’s time to don PPE (i.e., N95 masks) – Same message goes to other agencies that may enter into affected areas • Police Department sends message to all agency users in system • Police Department alerts other community stakeholders (its partners) that lack LE/FR; warns them to take preventive action 75 76 Sample protocol usage scenario #2: What to ask & say if the anthraxswer is blowin’ in the wind • Tarrant County Public Health continues to investigate • Queries respiratory complaints in highlighted regions – Findings: similar clusters in that area • Compares data to last year’s data – same time period – Determines counts are higher than previous year • Compare against other data sources – Similar rise in OTC sales of respiratory medication • Time period is not typical for respiratory problems 77 Sample protocol usage scenario #2: What to ask & say if the anthraxswer is blowin’ in the wind • Other factors examined: – Weather reports • Pollen counts have been extremely high for most of the month • Counts are exceedingly high throughout last week of the month – Lab data from care givers • Anthrax not indicated MAY 2007 78 Sample protocol usage scenario #2: What to ask & say if the anthraxswer is blowin’ in the wind • The respiratory problems were due to allergies • Local Health Authority determines no threat – Alert precautions to front-line personnel lifted – Stakeholders in community of practice are briefed 79 Sample protocol usage scenario #3: Saved by the school bell • Background: – October 2007 in school Web portal – School nurse notices that many students are absent or coming into office with common symptoms – Symptoms of sneezing, coughing, runny nose, and fever consistent with flu 80 Sample protocol usage scenario #3: Saved by the school bell Action: • Nurses enter absenteeism data • LHD makes use of school portal to communicate w/ school nurses – LHD surveillance lead asks nurses to send flu resources home w/ students • Nurses report similar findings • LHD investigates w/ ESSENCE using school and other health data 81 Sample protocol usage scenario #3: Saved by the school bell • ESSENCE has ER data • Using both sources, they query chief complaints and limit age to those in elementary school • Map portal shows zip codes with the significant clusters 82 Sample protocol usage scenario #3: Saved by the school bell • The original school was found in the zip code with a significantly large cluster – Adjacent areas showing small clusters • LHD target zip codes with large clusters for samples • Through local physician offices, LHD obtains lab results for several samples chosen – Lab tests reveal FLU 83 Sample protocol usage scenario #3: Saved by the school bell • LHD sent messages to all schools telling them to take preventive action • Original school installs new antibiotic scrubbing solution to mitigate the spread – Other schools follow suit • Health Authority calls for broadened flu shot distribution • Flu shots distributed in areas that show most signs of flu 84 Health partnerships applied: response protocols What questions may we answer at this point? 85 Agenda Topic: 1. 2. 3. 4. 5. 6. 7. 8. 9. Pre-test Communities of public health practice overview Biosurveillance fundamentals and best practices Health partnerships applied: response protocols Break Interactive group session 1 Interactive group session 2 Discussion of group sessions / conclusion Post-test Time: 10 25 25 30 15 15 15 20 10 86 Agenda Topic: 1. 2. 3. 4. 5. 6. 7. 8. 9. Pre-test Communities of public health practice overview Biosurveillance fundamentals and best practices Health partnerships applied: response protocols Break Interactive group session 1 Interactive group session 2 Discussion of group sessions / conclusion Post-test Time: 10 25 25 30 15 15 15 20 10 87 Interactive group session 1 88 Agenda Topic: 1. 2. 3. 4. 5. 6. 7. 8. 9. Pre-test Communities of public health practice overview Biosurveillance fundamentals and best practices Health partnerships applied: response protocols Break Interactive group session 1 Interactive group session 2 Discussion of group sessions / conclusion Post-test Time: 10 25 25 30 15 15 15 20 10 89 Interactive group session 2 90 Agenda Topic: 1. 2. 3. 4. 5. 6. 7. 8. 9. Pre-test Communities of public health practice overview Biosurveillance fundamentals and best practices Health partnerships applied: response protocols Break Interactive group session 1 Interactive group session 2 Discussion of group sessions / conclusion Post-test Time: 10 25 25 30 15 15 15 20 10 91 Discussion of interactive group sessions 92 Key points from interactive group session 1 • Participants’ response protocols should have included these investigative steps: – Detected anomaly – Pursued more information to characterize and validate threat – Assessed significance by examining disease trends – Examined other factors of importance – In this case, following all of the above steps would have shown the serious nature of this threat 93 Key points from interactive group session 1 • Participants’ response protocols and efforts to communicate (internal & external) should have: – Followed agency, jurisdictional and corporate standard operating procedures or guidelines – Made effective use of all communications channels – Called for precautionary measures w/out panic – Responded to the possibility of bioterrorism 94 Key points from interactive group session 2 • Salmonella outbreak caused by food items not handled in sanitary manner. Plan 1 critiques should have noted: – Good: Conducting interviews and investigation revealed specific number of victims affected – Good: Focus is on the victims, not the school staff – Good: Case control study is excellent investigative tool that’s designed to isolate possible causes (a necessary item) and supplements the findings from the laboratory tests – Good: Identifying cause of problems allows for remediation – Bad: There did not seem to be any effort to communicate with the school or public during the investigatory process 95 Key points from interactive group session 2 • Plan 2 critiques should have noted: – Good: There was an effort to communicate with the school and public during investigatory process, though this could be bad if the communication is poor and causes undue panic – Good: Lab testing is useful method of investigation – Bad: Investigation focused on school officials, not victims – Bad: Focus changed to new victims coming forward, not the original ones who were affected – Bad: Ending investigation solely on the basis of lab results from new victims (who potentially are not suffering from same problems or causes as the original ones) does not identify or address cause of problems w/ the original victims 96 In conclusion … • • • • • • • Clinician-only input is insufficient for several reasons Biosurveillance systems have broad, major benefits Response protocols apply key decision-making criteria General guidelines are helpful, may not be sufficient Actual responses may occur in various forms, ways A public health community of practice engages many Response protocols require effective communication “It takes a village public health community of practice.” 97 In conclusion … • • • • • • • Staff experience key factor in readiness, protocol development LHD should always assess community-level health problems Usually, LHDs will lead community health problem solving Not all health problems turn out to be what they first look like Findings and response should be shared broadly and promptly Health status should be monitored at various granularity levels One plan does not fit all 98 References and resources to learn more: • These handouts are part of your conference materials: – – – – – – AHIC MDS and preconditions Copy of these slides and full scenarios upon which exercises were based “Challenges to Rapid Clinical Detection of Select Agents” (D. Siegrist) List of references and resources with active hyperlinks “Region Has ‘Radar’ for Outbreaks” (Fort Worth Star-Telegram) “Syndromic Surveillance on the Epidemiologist’s Desktop: Making Sense of Much Data” (K. Hurt-Mullen et al) – Tarrant County Public Health and CDC BioSense response protocols – Tarrant County syndromic surveillance efficacy test report (Siegrist et al) • Contact information for presenters: Presenter: Title: E-mail: Phone: Bill Stephens, MS APC Manager [email protected] (817) 321-4730 Dean Lampman, MBA Regional Surveillance Coordinator [email protected] (817) 321-5365 Kay Sanyal-Mukherji, MPH Workforce Development Specialist [email protected] (817) 321-5310 99 You can also request our forthcoming CD: • All handouts on prior slide and: Building a Public Health Community of Practice A Compendium of Biosurveillance Resources – – – – Surveillance implementation guide More on LE/FR and school portals A report on the NEDSS program More TBD? Give us your input! • Methods to order: – Sign up sheet here – E-mail request later 100 References and resources to learn more: • • Book: “Handbook of Biosurveillance,” M. Wagner et al., Elsevier, May, 2006. Details: www.elsevier.com/wps/find/bookdescription.cws_home/707451/description Useful Websites and pages: – American Health Information Community: www.hhs.gov/healthit/community/background/ – CDC Biosense: www.cdc.gov/biosense/ and CDC PHIN: www.cdc.gov/phin/ – CDC syndromic surveillance resources: www.cdc.gov/epo/dphsi/syndromic.htm – Johns Hopkins Applied Physics Lab (ESSENCE developer): www.jhuapl.edu/ – HIMSS HIT Dashboard: www.hitdashboard.com/ – HIPAA and decision tool: www.hipaa.org and www.hhs.gov/ocr/hipaa/decisiontool/ – Health Level 7: www.hl7.org/ – Homeland Security Presidential Directive 21: www.fas.org/irp/offdocs/nspd/hspd-21.htm – Mirth project (open source HL7 interface engine): www.mirthproject.org/ – Office of the National Coordinator: www.hhs.gov/healthit/onc/mission/ – PAHPA: www.hhs.gov/aspr/conference/pahpa/2007/pahpa-progress-report-102907.pdf – Regenstrief Institute: www.regenstrief.org/ – University of Pittsburgh’s RODS Lab (RODS developer): https://www.rods.pitt.edu/site/ – Southwest Center for Advanced Public Health Practice (APC): www.texasapc.net – Tarrant County Public Health: www.tarrantcounty.com/eHealth/site/default.asp 101 Post-test 102 Agenda Topic: 1. 2. 3. 4. 5. 6. 7. 8. 9. Time: Pre-test Communities of public health practice overview Biosurveillance fundamentals and best practices Health partnerships applied: response protocols Break Interactive group session 1 Interactive group session 2 Discussion of group sessions / conclusion Post-test 10 25 25 30 15 15 15 20 10 Thank you for your attention and participation! i 103
© Copyright 2026