What is the Health Care Independence Program?
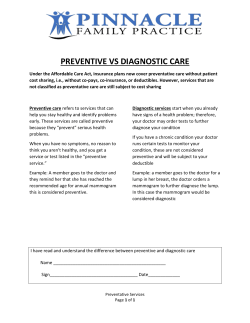
What is the Health Care Independence Program? The Health Care Independence Program pays for private health insurance for certain lowincome adults in Arkansas. Low-income adults who need insurance can apply online at access.arkansas.gov, www.arhealthconnector.org, or at one of the Department of Human Services’ (DHS) county offices. Eligible adults will be offered a choice of private insurance plans that best meets their needs. Who pays my premiums? There is no cost to beneficiaries for monthly health insurance premiums. For the first three years, the federal Medicaid program will pay the full premiums. After that, the federal and state Medicaid programs will share the costs of the premiums. The state program will pay a small portion of the costs every year until 2012, when it will pay 10 percent and the federal government will pay the rest. Who qualifies for coverage? Adults ages 19 through 64 with no dependent children and whose incomes are below 138 percent of the poverty level; OR parents ages 19 through 64 whose household income is between 17 and 138 percent of poverty. How do I sign up? To sign up, you must first fill out an application, which can be found at access.arkansas.gov, www.arhealthconnector.org or at your local DHS office. For a list of all county offices, click here. If you qualify for the Health Care Independence Program, you will then be sent to this website to answer a short questionnaire and then shop for a plan that is right for you. How much does the program cost me? The monthly private insurance premiums are paid for by the government so you will have no monthly premium costs. Depending on your income, you may have to pay a co-pay for certain appointments, prescriptions and other medical services. What if I have a pre-existing condition? Pre-existing conditions cannot and will not be held against you. As long as you meet the qualifications noted above, you will be given coverage, regardless of your medical history. Then why do I have to answer health questions? The health questions help us determine whether the Health Care Independence Program is the right program for you. In some instances, people with more serious health issues can receive coverage for a more comprehensive set of services through the traditional Medicaid program. Can’t I just pick a plan at arhealthconnector.org? Though the health insurance plans offered there are essentially the same, people eligible for the Healthcare Independence Program must shop for their private insurance plans here at www.insureark.org. What types of plans are available to me? Plans that cover Essential Health Benefits, which are: Outpatient services Emergency services Hospitalization Maternity and newborn care Mental health and substance abuse disorder services, including behavioral health treatment Prescription drugs Rehabilitative and habilitative services and devices Laboratory services Preventive and wellness services and chronic disease management Pediatric services, including dental and vision care What happens if I’m eligible, but don’t select a plan? The state will automatically assign you a plan after 12 days without a selection. But don’t worry, you can change plans up to 30 days after the auto-assignment has been made. What do I do if I have more questions? If you have any more questions, please call: For questions related to insurance carriers: Arkansas Insurance Department 855-283-3483 For questions related to the use of this website: Hewlett Packard call center 855-550-3974 For Medicaid eligibility questions: Division of County Operations call center 855-372-1084 Will the government tell me what doctor to go to or whether I can get a service? No. You will have private insurance. The insurance company will have a list of doctors that are in your network as well as what services are covered. All plans will cover the minimum services mentioned above. What are preventive benefits and how are they covered? Preventive benefits are designed to keep people healthy by providing screening for early detection of certain health conditions or helping to prevent illnesses. Many preventive services are required to be included in your policy with no out-of-pocket costs to you (meaning no deductibles, co-payments and coinsurance). Some of these covered preventive services are: ◦Colorectal cancer screenings, including polyp removal for individuals over age 50 ◦Immunizations and vaccines for adults and children ◦Counseling to help adults stop smoking ◦Well-woman checkups, as well as mammograms and cervical cancer screenings ◦Well-baby and well-child exams ◦Cholesterol screening How do I find out what drugs are covered by a plan? Health plans maintain lists of what drugs are covered and which are covered at the lowest costs. These lists are called formularies. You should review the formularies in any plan you select to make sure they meet your prescription drug needs. You need to call the health plan directly for help with this.
© Copyright 2026