What is a Gastroscopy? Preparing patients for their procedure(s) in the GI/ Endoscopy Units
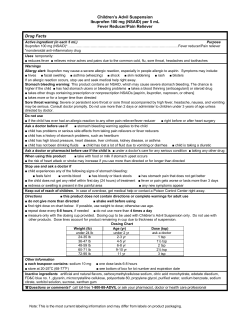
Preparing patients for their procedure(s) in the GI/ Endoscopy Units What is a Gastroscopy? A gastroscopy is a test in which a gastroscope (a long flexible tube) is passed through the mouth and down the back of the throat into the upper digestive tract. It allows the physician to examine the lining of the esophagus, stomach and duodenum (the first portion of the small intestine). It has its own lens and light source and the image is projected onto a video monitor. IT IS VERY IMPORTANT TO ENSURE YOUR PATIENT IS PROPERLY PREPARED FOR THE TEST THAT IS ORDERED What to tell your patients to expect FOR GASTROSCOPY •Ensure patient is NPO •Ensure any bloodwork that is ordered is completed •Document prep (NPO) and any pre meds given as ordered •Notify GI unit of any changes in patient’s patient s condition or if patient has not been NPO •Leave dentures on unit in marked container •Notify GI unit if patient is on ISOLATION and type •Ensure a patent IV/SL is in place. If your patient has a PICC or Central line only, please ensure that they have a saline solution infusing that may be used for medications. Why is it done? This test allows the gastroenterologist to diagnose a condition and prescribe or recommend a treatment. It can evaluate and treat problems such as: •Ulcers or growths in the esophagus, stomach or intestine •Narrowing in the esophagus or other areas of the upper digestive system •Abdominal pain, heartburn or persistent nausea and/or vomiting •Enlarged E l d bl blood d vessels l iin the h esophagus h or stomach h •Celiac disease (can’t digest gluten and wheat products) •Difficulty swallowing Gastroscopy can also be used to: •Remove small objects such as coins, bones, and food from the esophagus and stomach •Obtain samples to look at under the microscope •Treat bleeding in the esophagus, stomach, or small intestine •They will be asked to lie on their left side. •A mouth guard will be placed between their teeth.(This prevents damage to the patients teeth and the endoscope). • They will receive sedation through the IV line. Their throat may or may not be sprayed with a topical anaesthetic to numb itit.(This (This is physician dependent) •A flexible tube, called a gastroscope, will be inserted into their mouth. This tube will not interfere with their breathing. The tube will pass over the back of their tongue and is then passed down the esophagus (“food pipe”) down to the stomach. •Air is used to inflate the areas to allow the doctor to see the area better. They may have some bloating, feel pressure in their abdomen or feel a need to burp. The procedure takes from 5-20 minutes. Did you know? • 70 % of ulcers are found in the duodenum. Why is that? Answer: NSAIDS are one of the leading causes of ulcers and typically those ulcers develop in the duodenum. The stomach defends itself from hydrochloric acid and pepsin by creating a mucus coating. • What is the name of the primary bacterium that causes ulcers? Answer: Helicobacter pylori (H. pylori). H. pylori is a spiral-shaped bacterium found in the stomach. Unlike other bacterium, H. pylori is able to twist through the layer of mucous that protects the stomach cavity. 1 What is a Colonoscopy? What are the possible risks? What you should watch for when patients return to the unit. A Gastroscopy is a safe procedure, however it carries a very small risk of complications, including: •Bleeding – watch for S&S of GI bleeding – vomiting blood, tachycardia, cool extremities, syncope (change in postural BP), unexplained confusion A colonoscopy is a procedure that allows the doctor to see and examine the lining of the lower gastrointestinal tract. This includes the rectum and the large colon (also known as the large intestine or large bowel) using a flexible tube called a colonoscope. •Perforation – watch for severe epigastric/chest pain with movement, nausea and vomiting, or fever and/or chills vomiting chills. Observe upper chest area for signs of subcutaneous emphysema. It is easily palpable if present…..snap, crackle, pop feel. •Aspiration-from fluid or foods getting into their lungs – watch for coughing, SOB, increased chest wheeziness •Possible complications from the sedation received -watch for decreased LOC over a prolonged time, decreased respirations, decreased pulse, decreased BP, inability to rouse after approximately 1 hour – IF your patient received a reversal agent, watch out for re-sedation. Important You should check your patients’ vital signs and LOC upon return to the unit and within an hour post and as indicated. Be aware of any significant changes in vital signs or patient condition either from pre procedure state or upon return to unit post procedure. IT IS VERY IMPORTANT TO ENSURE YOUR PATIENT IS PROPERLY PREPARED FOR THE TEST THAT IS ORDERED FOR COLONOSCOPY •Ensure patient receives all of the ordered prep (ie: Colyte) and is on clear fluids only the day before the test. •Ensure the physician/GI unit is notified if the patient is not tolerating the prep so further orders can be given. •Patient should be passing clear/colorless liquid or clear yellow liquid if prep was effective-a small amount of sediment is fine as long as you can see the bottom of the toilet---if prep is ineffective notify GI unit well in advance of sending the patient for the test ineffective, test. •Document the prep given and results from the prep. •Ensure any bloodwork that is ordered is completed. ie INR •Notify GI unit of any changes in patient’s condition. •Ensure a patent IV/SL is in place. If your patient has a PICC or Central line only, please ensure that they have a saline solution infusing that may be used for medications. The most important thing that you can do to ensure the success of your patients colonoscopy is to make sure they are properly prepared for the test. The colon must be cleaned out to allow for clear examination of the bowel wall and detection of any abnormalities. Excellent bowel preparation results in a clean colon that allows the test to be done quickly and easily. A poor bowel preparation increases the risk of missing significant lesions, such as cancers or polyps, and may result in the test needing to be repeated. What to tell your patients to expect •They will lie on their left side for the procedure but may be repositioned during the test. •They will be given sedation through their intravenous to help them relax. • Many patients will fall asleep during the procedure and may not remember many of the details of what happened during the test. test •A flexible tube, called a colonoscope, will be lubricated and inserted into the rectum. •Air is used to inflate the colon to allow the doctor to see the area better. This may cause them some abdominal cramping and/or the urge to have a bowel movement. The procedure takes about 15-45 minutes to complete. Why is it done? Crohn’s disease versus Ulcerative Colitis This test allows the gastroenterologist to diagnose a condition and prescribe or recommend a treatment. Biopsies can be obtained to look at under the microscope if deemed necessary from symptoms or visualization of abnormalities. It can evaluate and treat problems such as: Crohn’s disease Ulcerative Colitis Usual lesion site Primarily the ileum, but can affect any portion of the GI tract from mouth to anus. Affects the large intestine only •change change of bowel pattern such as diarrhea or constipation constipation, pencil thin stool stool,etc etc Type of lesions Intermittent granulomatous skip l i lesions with healthy tissue in i hh l h i i between(cobblestone appearance). Continuous ulcerative and exudating l i lesions •abdominal pain Tissue involvement • screening for polyps or cancer (polyps can be removed and/or biopsies taken if found) May involve all layers of the Intestinal wall Mucosal layer only, unless disease is very severe Rectal bleeding Unusual unless colon is involved Commonly seen •bleeding or determine cause of unexplained anemia Fistulas and abscesses Common Rare •Crohn’s disease or Ulcerative colitis(Inflammatory Bowel Disease) Cancer development Uncommon Fairly common with long‐ standing disease. (Surveillance Colonoscopies with biopsies are required to monitor) •Narrowing in the colon 2 What are the possible risks? What you should watch for when patients return to the unit. A colonoscopy is a safe procedure but potential risks or complications are involved: Bleeding – watch out for S&S of GI bleeding – passing blood rectally, tachycardia, cool extremities, syncope (change in postural BP), unexplained confusion Perforation – watch for severe abdominal pain with movement, nausea and vomiting or fever and/or chills Infection – watch for fever and/or chills Possible complications from the sedation received – watch for decreased LOC over a prolonged time, decreased respirations, decreased pulse, decreased BP, inability to rouse after approximately 1 hour – IF your patient received a reversal agent, watch out for re-sedation. What is an ERCP? An ERCP is a procedure which allows the doctor to examine the gallbladder, pancreas and the ducts that carry bile and pancreatic juices to the duodenum (first part of the small bowel) During an ERCP(endoscopic retrograde cholangiopancreatography) a catheter is advanced through the endoscope and inserted into the pancreatic or biliary ducts. A contrast agent is injected into these ducts and X X-rays rays are taken to evaluate their caliber, length and course. Narrowing, stones, and tumors in the ducts can be identified in the X-rays. Important You should check your patients’ vital signs and LOC upon return to the unit and within an hour post or as indicated. Be aware of any significant changes in vital signs or patient condition either from pre procedure or from initial assessment upon return post test. •Encourage patients to pass air after the test to relieve any abdominal distension and/or cramping. IT IS VERY IMPORTANT TO ENSURE YOUR PATIENT IS PROPERLY PREPARED FOR THE TEST THAT IS ORDERED FOR ERCPs •Ensure patient is NPO •Ensure any bloodwork that is ordered is completed– usually an INR is needed – call GI unit if result is abnormal. •Document prep (NPO) and any premeds given as ordered •Notify GI unit of any changes in patient’s condition or if patient has not been NPO •Leave dentures on unit in marked container •Ensure a patent IV/SL is in place. If your patient has a PICC or Central line only, please ensure that they have a saline solution infusing that may be used for medications. What to tell your patients to expect •They will lie on an X-ray table on their abdomen unless otherwise instructed. •They will be given medication through the intravenous to help them relax. Most patients fall asleep during the procedure and don’t remember details of what happened. •A flexible tube, called a duodenoscope will be passed through their mouth, into their stomach, and down into their duodenum. This tube does not interfere with breathing. •Air Air is used to inflate the stomach and duodenum to allow the doctor to see the area better. You may feel bloating and/or pressure in your abdomen or feel a need to burp. •If there is anything that appears abnormal, the doctor can take biopsies or brushings or do therapeutic interventions through the scope. •They may have a slight sore throat for 1-2 days after. Warm, salt water rinses or throat lozenges may be used to lessen the discomfort. •They may have bloating, abdominal cramping, and soft bowel movements because of the air and the dye that was injected. It is strongly recommended that they expel the air to relieve discomfort. •They may feel light-headed or drowsy due to the effects of the medication. The procedure can take from about 15-60 minutes to complete. Why is it done? This test allows the doctor to diagnose a patient’s condition and prescribe a treatment. An ERCP may be done to evaluate problems such as: •jaundice (yellow – tinged skin and/or eyes) •abdominal pain/recurrent pancreatitis •abnormal liver function tests •stones, tumors, or narrowings And can also be done to: •remove gallstones from the bile duct (tube that drains the liver) •relieve blockage at the bottom end of the bile duct •remove stones from the pancreas •place stents – plastic tubes – temporary or metal tubes – permanent •obtain biopsies or brushings for microscopic examination •dilate (stretch) strictures (narrowings) of the ducts •treat leaks in the duct that were caused from trauma or surgery What are the possible risks of having an ERCP & what you should watch for when your patients return to the unit Bleeding – watch out for S&S of GI bleeding – vomiting blood, tachycardia, cool extremities, syncope (change in postural BP), unexplained confusion Perforation – (hole or tear) – watch out for severe chest or epigastric pain with movement, nausea and vomiting, or fever and/or chills Pancreatitis – epigastric pain, nausea and vomiting and abnormal liver enzymes Allergic reaction to X-ray dye or the medication used to relax the duodenum – watch out for rash, hives, sign of anaphylaxis Infection – new ne onset of increased temperat temperature, re rigors and/or chills Allergic reaction or breathing problems caused by the medication used for sedation – watch out for decreased LOC over a prolonged time, decreased respirations, decreased pulse, decreased BP, inability to rouse after approximately 1 hour –IF your patient received a reversal agent, watch out for resedation. Important •You should check your patients vital signs and LOC upon return to the unit and within an hour post or as indicated. Be aware of any significant changes in vital signs or patient condition either from pre procedure or from initial assessment upon return post test. •Encourage patients to burp, pass gas, or change position to aide in relieving bloating and /or cramping. Once awake enough, ambulation also helps with passing air. 3 COMMON MEDICATIONS YOU SEE ORDERED ON THE UNIT FOR PATIENTS WITH GI ISSUES Medications continued…… COLYTE/GOLYTELY is used for bowel evacuation before a GI examination. 4 Litres must be consumed as ordered – maintain hydration by oral fluids (if patient isn’t NPO) or with IV therapy as ordered. Cramping, nausea and vomiting and bloating are not unusual – treat as needed OCTREOTIDE is often ordered to treat variceal bleeding. It causes vasoconstriction in the blood vessels thereby reducing portal vessel pressures in bleeding varices. It is usually ordered as a bolus then continuous infusion. PANTOLOC is a proton pump inhibitor – is used for treatment of ulcers and decreasing acid reflux – IV form is often used to treat acute upper GI bleeds. It is usually ordered as a bolus then continuous infusion. SOLUMEDROL is a corticosteroid used for treatment of ulcerative colitis or Crohns disease. It is usually given IV and dose is dependent on severity of pt’s condition. More common adverse effects include acne, fluid and electrolyte imbalance, blood sugar variations, increased appetite and weight gain. Antibiotics may be ordered pre GI procedure for certain pre existing patient conditions or new conditions. •ERCP patients who are jaundiced almost always have IV antibiotics pre procedure. procedure •Erythromycin may be ordered 1-2 hours pre procedure as it is known to help clean out the stomach of blood allowing better visualization during the test. PREDNISONE is a corticosteroid used for treatment of ulcerative colitis or Crohns disease. It can be ordered either orally or intravenously. Dose and route is dependent on severity of pt’s condition. Dosage must be tapered to discontinue. More common adverse effects include acne, fluid and electrolyte imbalance, blood sugar variations, increased appetite and weight gain. DRUGS COMMONLY GIVEN IN THE GI UNIT FENTANYL– used for procedural sedation/analgesic for endoscopic procedures to decrease procedural discomfort. Watch out for respiratory depression, apnea, chest wall rigidity, and bradycardia. VERSED– is a short acting benzodiazepine sedative/hypnotic used for endoscopic procedures to decrease anxiety and recall of procedure. Watch out for respiratory depression and arrest.(Drug Half-life 1-4 hours) DIAZEMULS - is a long acting benzodiazepine sedative/hypnotic used for endoscopic procedures to decrease anxiety and recall of procedure. Watch out for respiratory depression and arrest.(Drug Half-life 21-37 hours) GLUCAGON – may be used to decrease motility of the stomach, duodenum, small bowel and colon during GI exams (used most often in ERCPs). Watch for blood sugar changes mainly hyperglycemia. NARCAN – is a reversal agent for narcotic depression. Watch for re-sedation. ANEXATE – is a reversal agent for benzodiazepines. Watch for re-sedation. Watch for seizures in patients who frequently take benzodiazepines. Gastrointestinal bleeding Gastrointestinal (GI) bleeding is responsible for 1% to 2% of all hospital admissions. •Bleeding can be either acute or chronic. •The source can be upper or lower, overt or occult. •The patient can be either hemodynamically stable or unstable on presentation. UPPER GI BLEED • can be in esophagus due to varices, esophagitis, cancer or Mallory Weiss tear • can be in stomach due to ulcer, gastritis or cancer • can be in duodenum due to ulcer or Aortoenteric fistula • can be due to coagulopathy Signs and Symptoms: In general, patient presents with melena and/or coffee ground emesis. They may have chest pain, anemia, fatigue, decreased O2 sat, abdominal distention, and have a change in vital signs (increased pulse, decreased BP, and postural changes). GI Bleeding continued Your Nursing Assessment questions should include: •Is there a prior history of GI bleeding (60% rebleed from the same site)? • Does the patient have any co morbidity diseases (peptic ulcer disease, pancreatitis, cirrhosis, cancer)? • Is the patient taking any medications (especially nonsteroidal anti‐inflammatory Is the patient taking any medications (especially nonsteroidal anti inflammatory agents)? •Does the patient use recreational drugs, cigarettes, or alcohol? •What is the character of the pain? Peptic ulcer pain is epigastric, gnawing, rhythmic, and dull. GI cancers are associated with vague epigastric pain, dysphagia, or weight loss. •Was there an history of excessive retching (Mallory–Weiss tear)? LOWER GI BLEED • can be in small bowel due to diverticulum, Crohns, Aorto enteric fistula, vascular problems, or neoplasm • can be in colon due to diverticulum, angiodysplasia, inflammatory bowel disease, ischemic gut, infection, or neoplasm • can be perianal d due e to hemorrhoids hemorrhoids, fist fistula la or a fiss fissure re • can be due to coagulopathy Signs and Symptoms: In general, presents with fresh blood per rectum. They may have chest pain, anemia, fatigue, decreased O2 sat, abdominal distention, and have a change in vital signs (increased pulse, decreased BP, and postural changes). 4 Your Nursing Assessment questions should include: •How old is the patient? Age is an important feature in discriminating the source of lower GI bleeding. A/ Patients aged less than 50 years usually bleed from infectious causes, anorectal disease, or inflammatory bowel disease. B/For patients aged more than 50 years, diverticulosis, angiodysplasia, cancer, and ischemia are most common and ischemia are most common . •Are there any associated symptoms? A/Diverticular disease presents as painless, high volume bleeding. B/Angiodysplasia and cancer present with symptoms of chronic blood loss (fatigue, dyspnea on exertion, positive fecal occult blood). C/Inflammatory bowel disease presents with bloody diarrhea, cramping, weight loss, and fever. A prior history of inflammatory bowel disease, cancer, or radiation to the abdomen is also important. Important to Note MANAGEMENT OF GI BLEEDS CONTACT ADMITTING PHYSICIAN For non-variceal UGI Bleed – PPIs (oral vs IV depending on pt stability) to reduce AS ORDERED: the bleeding and risk of rebleeding. • O2 therapy to maintain O2 sats For variceal UGI Bleed – Octreotide • large bore IVs • administer IV fluids/boluses (reduces blood flow and portal pressure) or • crossmatch vasopressin (potent vasoconstrictor that • keep NPO • GI consult – then prep for procedure as decreases blood flow and portal pressure) –if not actively bleeding, may be treated ordered • correct coagulopathy with beta blockers • bloodwork – CBC,e’lytes,Creatinine, For both Upper and Lower GI bleeds BUN, PTT,INR,LFTs treatment may include blood •Administer blood products/FFPs products/FFPs (to correct coagulopathy). •Administer medications A THERAPEUTIC ENDOSCOPY MAY BE NECESSARY The End! •Both upper and lower GI BLEEDS should be managed with maintaining ABCs and volume resusutation. •BE PREPARED – A STABLE GI BLEED MAY SUDDENLY BECOME UNSTABLE Keep a close eye on their condition and monitor the trend of UNSTABLE. their vitals. •DO ACCURATE AND TIMELY DOCUMENTATION If you wish to view a procedure to familiarize yourself with GI tests, please contact your clinical nurse educator to have this arranged . 5
© Copyright 2026