What is “Cool” about Radiofrequency Ramsin Benyamin, MD
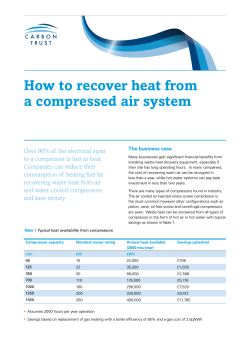
What is “Cool” about Radiofrequency Ramsin Benyamin, MD Disclaimer • • Founder/President/Medical Director, Millennium Pain Center, Illinois: Bloomington-Normal, Decatur, Peoria, Des Plaines, Libertyville, Evanston, Chicago Co-founder, Millennium Pain Management-Teknon Medical Center, Barcelona, Spain • • Clinical Assistant Professor of Surgery, College of Medicine, University of Illinois Adjunct Professor, Department of Biological Sciences, Illinois State University • • • • Past-President, American Society of Interventional Pain Physicians (ASIPP) President-Elect, American Society of Interventional Pain Physicians (ASIPP) Board of Directors, SIPMS Past-President, Illinois Society of Interventional Pain Physicians • • Board of Examiners, American Board of Interventional Pain Physicians (ABIPP) Member, Guidelines committee, ASIPP • • • • Associate Editor, “ Pain Physician” Editorial Board, “ Pain Practice” Editorial Board, “Journal of Opioid Management” Reviewer, “Neurosurgery”, “Neuromodulation”, “ Journal of Neuro-Interventional Surgery” Disclaimer • Clinical research/Teaching/lecture: Kimberly Clark Principle of Ionic Heating RF energy is applied Ions in surrounding tissue move creating friction1 Friction heats surrounding tissue Hot tissue heats probe or electrode by conduction Probe thermocouple located at the tip, reads tissue temperature 1. Organ LW. Appl Neurophysiol 1976;39:69-76. Independent Lesion Parameters • Electrode Shape: Lesion size is influenced by the length and gauge of the electrode2,3 • Lesion size increases with surface area Longer: longer Wider: wider 20 Ga. 10mm 18 Ga. 10mm 2. Bogduk N, Macintosh J, Marsland A. Neurosurgery 1987;20:529-35. 3. Alberts WW, Wright EW, Jr., Feinstein B, et al. J Neurosurg 1966;25:421-3. 20 Ga. 4 mm Internally Cooled Electrodes 5. Goldberg SN, Gazelle GS, Solbiati L, et al. Acad Radiol 1996;3:636-44. 6. Lorentzen T. Acad Radiol 1996;3:556-63. 7. Wittkamp FHM, Hauer RN, Robles de Medina EO. J Am Coll Cardiol 1988;11. Physics of Cooled RF Conventional RF Cooled RF Testing performed in chicken (37°C) for 3:00 at a set temperature of 70 °C. Electrode: 18 Gauge, 4mm active tip. Physics of Cooled RF • “3D” sphere • Increasing radius ‘r’by a factor of 2 increases volume ‘V’ by a factor of 8 according to V = 4/3πr3 Cooled vs. Non-Cooled RF Lesions Standard RF: Internally Cooled RF Probe V = ‘x’ mm3 4 mm V = 8‘x’ mm3 Internal cooling doubles the lesion radius and increases the lesion volume by a factor of 8 8 mm Thermal vs. Cooled RF Temperature 80° C Non-cooled Cooled 45° C r Distance Probe Conventional RF lesion size is limited by heat generated in the tissue adjacent to the electrode Cooling tissue adjacent to the electrode (via cooling the RF probe) increases radius of overall effective heating. Cooled RF Lesion Properties Cooled RF‐ 18Ga, 4mm Size and shape of cooled RF lesions are a function of: Electrode length/ geometry Set temperature Time (Duration) Coolant Flow Rate Coolant Temperature 40% 10 mm Testing performed in chicken (37°C) for 3:00 at a set temperature of 70 °C. Large Spherical, Forward Projecting Lesion Cooled RF Conventional RF Application to Discogenic Pain Cooled RF for Sacroiliac Joint Pain • Large Cooled-RF lesions are positioned in a lateral arc around each dorsal sacral aperture • Nine targets create a combined lesion volume adequate to compensate for known anatomical variations SInergy Cooled RF Lesioning pattern: 3 lesions created lateral to S1 & S2 foramina, 2 lesions lateral to the S3 foramen, and 1 lesion lateral to L5 dorsal ramus. SI Joint Pain – Patel RCT, Pain Medicine 2012 • Prospective Randomized, Double Blind, Placebo Controlled Clinical Trial (N = 51) • Randomized 2:1 • Criteria for cooled RF treatment – – – – – Chronic low back pain ≥ 6 months NRS between 4 & 8 on 10 cm scale Failed conservative therapy Signs/symptoms of SI-joint mediated pain ≥ 75% pain relief from dual SI lateral branch blocks • Follow up 9 months post treatment Patel, et al, Pain Med. 2012 Mar;13(3):38398. SI Joint Pain – Patel RCT (cont.) * p < 0.05 Patel, et al SI Joint Pain - Stelzer, Pain Med 2013 • Large, single-center, retrospective review (N = 126) • Criteria for cooled RF treatment – – – – Chronic low back pain ≥ 6 mo. & VAS ≥ 5 Signs/symptoms of SI-joint mediated pain Failed conservative therapy ≥ 50% pain relief from single SI joint injection • Follow up range 4-20 months Stelzer, et al. Pain Med. 2013 Jan;14(1):29-35. SInergy Cooled RF Lesioning pattern: 3 lesions created lateral to S1 & S2 foramina, 2 lesions lateral to the S3 foramen, and 1 lesion lateral to L5 SI Joint Pain (Stelzer cont.) KEY RESULTS 4-6 Months 6-12 Months > 12 months 50% Reduction in Pain 86% 71% 48% VAS 2 Point Reduction in Pain 92% 84% 74% QOL “Improved” or “Much Improved” 96% 93% 85% Stopped or Decreased Use of Opioids 100% 62% 67% Author Conclusions: • Results support use of cooled RF for patients who fail conservative treatment • Decreases in pain & medication usage may justify use in a broader population Stelzer, et al. Pain Med. 2013 Jan;14(1):29-35. SI Joint Pain – Cohen RCT, Anesth. 2008 • Prospective Randomized, Double Blind, Placebo Controlled Clinical Trial (N = 28) • Criteria for cooled RF treatment – – – – Chronic low back pain ≥ 6 mths Failed conservative therapy, including corticosteroid injections Signs/symptoms of SI-joint mediated pain ≥ 75% pain relief from single diagnostic SI joint injection • Randomized 1:1 • Follow up 6 months • % success defined as: – ≥ 50% reduction in NRS pain AND – A positive Global Perceived Effect (GPE) AND – A 10 point decrease in ODI (Oswestry Disability Index) OR – A 4 point decrease in ODI coupled with reduction in medication usage. Cohen, et al, Anesthesiology. 2008 August; 109(2): 279–288. SI Joint Pain – Cohen RCT (cont.) “The proportion of subjects who experienced a “positive outcome” was significantly higher in the denervation group than in the control group (p < 0.001). This success rate persisted at 3- and 6- month follow up visits” Author Conclusions: “Results support use of cooled RF for patients to treat presumptive Sacroiliac joint pain” Cohen, et al. SI Joint Pain Predictor – Cohen, Reg Anesth and Pain Med 2009 • Retrospective study (N = 77) • Focus of study was to identify factors associated with SI joint RF denervation outcomes. • Reviewed Conventional RF and Cooled RF • Outcome Measures: – Success = VAS Pain Score decrease > 50% for 6 months and positive Global Perceived Effect. – Follow up 6 months post procedure Cohen, et al, Reg Anesth and Pain Med . May/June 2009;Vol 34, number 3:206-214 SI Joint Pain Predictor – Cohen (cont.) Author Conclusions: “The use of Cooled, rather than Conventional RF, was associated with a higher percentage of positive outcomes.” “The only positive predictor of a successful outcome was the use of Cooled RF technology.” Cohen, et al. Conventional RF Current technology for lumbar neurotomy uses conventional RF. Lesions created are: Oval shape • Requires parallel trajectory Volume • Requires precise placement • May require multiple passes Cooled RF Lesions Cooled RF technology offers lesions with different set of characteristics: Spherical shape Distally projecting Large volume Approach angle independent 40 % 14 mm Cooled RF, 18Ga, 4mm Cooled RF for treatment of thoracic z -joint UPPER UPPER 12 mm MID MID 12 mm LOWER LOWER 12 mm Variable path Optimized lesion size Consistent ablation of thoracic z -joint MB Complex Anatomical Structures A sub group of patients may be more difficult to treat due to: Disordered anatomy: • Degenerative changes with age • Enlarged z-joint • Scoliosis • Obesity Modified anatomy: • Presence of surgical implants • Scar tissue formation in vicinity of joint Cooled RF – Coagulation zone Visual Image Infrared Image Red = Temp between 45 and 55 oC Yellow = Temp above 55 oC New Applications Are We Doing Too Many TKRs? Peter McCann, MD; Editorial 2012 • JAMA: Increase in 20 years: 161% in primary, 106% in revision TKR: aging, obesity • Actual per capita increase: tripled in 20 years • 5 Billion dollars a year • CMS: MR: surgery is reasonable/necessary • Overuse not substantiated • Welcomes transparency, independent analysis, peer review Efficacy of pulsed radiofrequency treatment on the saphenous nerve in patients with chronic knee pain Mert Akbasa,∗, Nurettin Lulecib, Kamer Derea, Emel Lulecic, Ugur Ozdemird and Huseyin Toman Journal of Back and Musculoskeletal Rehabilitation 2011 • • • • N: 115 patients PRF of infrapatellar branch of Saphenous nerve x8minutes Follow-up: 6 months WOMAC,VAS in rest, movement, flexion Patient response to different treatment Patient requiring second dose of PRF treatment after 3 months Patient requiring second dose of PRF treatment after 6 months Patient reporting > 50% decrease in VAS after 6 months Patient reporting satisfaction by WOMAC Score after 6 months (excellent or good) Number of patients (%) 0 (0%) 3 (2.6%) 115 (100%) 113 (98.2%) Radiofrequency treatment relieves chronic knee osteoarthritis pain: A double-blind randomized controlled trial Woo-Jong Choi a, Seung-Jun Hwang b, Jun-Gol Song a, Jeong-Gil Leem a, Yong-Up Kang c, Pyong-Hwan Park a, Jin-Woo Shin • • • • • • • • 38 patients randomized Kellgren-Lawrence grade: 2-4 Single diagnostic block: 2ml Lidocaine 2% SL, SM, IM geniculate nerves: 70c x 90s Periosteum @ junction of shaft & epicondyle Follow-up: 1, 4, 12 weeks VAS, GPE, Oxford knee score 59% had >50% relief Anteromedial view of the right knee joint. (A) The superior medial genicular nerve (1) runs down the upper part of the medial epicondyle (asterisk) of the femur with genicular vessels (2). The adductor magnus (3) which is inserted into the adductor tubercle on the medial condyle of the femur. (B) The inferior medial genicular nerve (1) passes the lower parts of the medial epicondyle (asterisk) of the tibia. The tibial collateral ligament (2) which is attached to the medial condyle of the tibia Percutaneous Radiofrequency Treatment for Refractory Anteromedial Pain of Osteoarthritic Knees Masahiko Ikeuchi, MD, PhD,* Takahiro Ushida, MD, PhD,*† Masashi Izumi, MD,* and Toshikazu Tani, MD, PhD Pain Medicine, 2011 • • • • • • RF(18) vs. nerve block(17) Kellgren-Lawrence: grade 3-4 3 weeks washout/abstinence Medial retinacular nerve, infrapatellar branch of saphenous RF: 70 x 90s repeat in 2weeks Follow-up: 6 months Articular innervation • Anteromedial joint: obturator nerve • Anterolateral joint: femoral nerve • Posterosuperior joint: sciatic nerve • Posteroinferior joint: nerves to quadratus femoris muscle • Posterolateral joint: superior gluteal nerve The sensory innervation of the hip joint - An anatomical study Surgical Radiologlc Anatomy Journal of Clinical Anatomy K. Birnbaum l, A. Prescher2, S. Hef31er1 and K.-D. Heller 1 © Springer-Verlag 1997 Percutaneous Radiofrequency Lesioning of Sensory Branches of the Obturator and Femoral Nerves for the Treatment of Hip Joint Pain Masahiko Kawaguchi, M.D., Keiji Hashizume, M.D., Toshio Iwata, M.D., and Hitoshi Furuya, M.D. Regional Anesthesia and Pain Medicine, 2001 • • • • • N: 14 patients Single diagnostic block: nerve/joint RF: obturator in 9, obturator and femoral in 5 VAS: 6.8 to 2.7 86% had %50 for 1-11 months Fig 3. Fluoroscopic image showing the Sluijter-M ehta cannulae for the radiofrequency lesioning of sensory branches of left obturator nerve. The tip of the cannula was located near the anteromedial aspect of the extraarticular portion of the hip joint, the site below the inferior junction of the pubis and the ischium, which appears teardrop in shape in the antero-posterior radiograph. After the injection of 2 mL mepivacaine, radiofrequency thermocoagulation was performed at 80°C for 90 seconds. Percutaneous Radiofrequency Lesioning of Sensory Branches of the Obturator and Femoral Nerves for the Treatment of Non-Operable Hip Pain Atif Malik, MD, Thomas Simopolous, MD, Mohamed Elkersh, MD, Musa Aner, MD, and Zahid H. Bajwa, MD Pain Physician, 2003 • Case series: 4 patients • Single diagnostic nerve block: 1ml Marcaine 0.25% • All 4 had reduction in VAS • 3 had improved function • 2 had reduction in pain meds Pulsed Radiofrequency Treatment of Articular Branches of the Obturator and Femoral Nerves for Management of Hip Joint Pain Hong Wu, MD, MS; John Groner, MD ; Pain Practice 2007 • Case report: 2 patients • Single diagnostic block: 0.5-1ml Lidocaine 1% • 50% pain relief & improved function: 3-4 months Percutaneous Radiofrequency Denervation in Patients With Contraindications for Total Hip Arthroplasty FABRIZIO RIVERA, MD; CARLO MARICONDA, MD; GIOVANNI ANNARATONE, MD ORTHOPEDICS , March 2012 N: 16 Single diagnostic block: Ropivacaine: 3ml Follow-up: 6 months Mean VAS: 9.52 to 6.35 Harris Hip Score: 28.64 to 43.88 Mean WOMAC (OA index): 75.70 to 63.70 8 patients: >50% relief at 6 months No side effects: 3 cases of hematoma In conclusion… “Learn from the mistakes of others. You can’t live long enough to make them all yourself.” Eleanor Roosevelt I have my faults, but being wrong ain't one of them. Jimmy Hoffa Thanks! [email protected]
© Copyright 2026