4/26/2013 Why does volume matter? Euvolemia: Hypovolemia
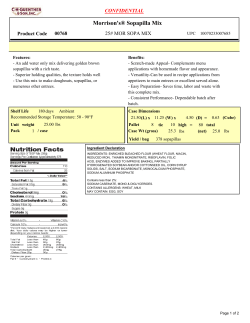
4/26/2013 Anne Diroll, RN, CNN Why does volume matter? California Dialysis Council Long Beach, CA April 2013 Place photo here Euvolemia: Confronting an Old Challenge Hypovolemia Normovolemia Hypervolemia •Sepsis •Overfiltration •Ascites •N/V •Bleeding •Optimal balance •Regulated by normal kidney •Underfiltration •DW underestimated Organ Dysfunction Adverse Outcomes “The cornerstone of critical thinking is the ability to ask questions.” Organ Dysfunction Adverse Outcomes Dennis Bartels in Scientific American, March, 2013 Adapted from: Prowle JR et al. (2009). Fluid balance and acute kidney injury, Nat. Rev. Nephrol. 6, 107-115. doi:10.1038/nrneph.2009.213 Condition for Coverage Correlation Grids V Tag ‘manage the patient’s volume status’ V504 Patient Assessment § 494.80 BP/fluid management needs V Tag V543 Interdialytic BP & weight gain Target weight Symptoms Value – Euvolemic & BP 130/80 § 494.90(a)(1) Plan of Care § 494.90 Manage BP and volume status Management of volume status Euvolemic and BP 130/80 under the “Patient plan of care” condition V507 Anemia V547 Volume Bleeding Infection ESA hypo-response www.cms.gov/Regulations-and-Guidance/Legislation/CFCsAndCoPs Achieve and sustain Hgb/Hct Hgb on ESAs 10-12 g/dL Hgb off ESAs >10 g/dL Adapted from: Centers for Medicare & Medicaid Services – Version 1.3 4-Compartment Fluid Model CV Mortality Rates are High Intravascular Volume 5L Intracellular Volume 28L Dialysate Extracellular Volume 11L Period prevalent dialysis patients; unadjusted Adapted from Ahmad, S. (1999). Fluid Movements in relation to ultrafiltration. In M. Knowles (Ed.), Manual of clinical dialysis (p. 32). London: Science Press Ltd. USRDS 2011 Annual Data Report, Figure 4.3 (Volume 2) 1 4/26/2013 Hospitalization Effects of Fluid Overload 12 days / patient year Increased fluid LV work LV hypertrophy & myocardial fibrosis RISKS SCD IHD Heart Failure Adapted from: Glassock, RJ, Pecoits-Filho, R. & Barberato, SH. Left ventricular mass in chronic kidney disease and ESRD, Clin J Am Soc Nephrol 4: S79-S91, 2009. doi:10.2215/CJN.04860709 USRDS 2012 Annual Data Report, Figure 3.2 (Volume 2) Factors Affecting HTN in Renal Failure Essential Hypertension Na+/K+ ATPase inhibitors Volume-Dependent Hypertension in Hemodialysis ReninAngiotensinAldosterone Volume excess Parathyroid hormone/Ca2+ Endothelin, NO, etc. MI Arrhythmias Sympathetic activity Hypertension 85-90% HTN is volume dependent Erythropoetin Therapeutic Interventions • Prudent diet • Volume reduction • Achieve dry weight • Low sodium bath • Ultrafiltration Toxin(s) Adapted from Ahmad, S. (1999). Pathogenic factors contributing to hypertension in renal failure. In M. Knowles (Ed.), Manual of clinical dialysis (p. 112). London: Science Press Ltd. Mailloux, LU, Bellucci, AG, Napolitano, B & Mossey, RT. (1994). The contribution of hypertension to dialysis patient outcomes. ASAIO Journal. 40(2):130-137. Antihypertensives: Hypertension & Hypotension - The Vicious Cycle – 1994 Anemia: Achieving & Sustaining Hgb/Hct Predialysis hypertension • Hypervolemia dilutes Hgb AND Hct • Current ESA therapy does not account for volume • Hypervolemia increases inflammation • Inflammation contributes to ESA resistance Interdialytic weight gain Dry weight never achieved Minimal weight loss LVH on ECHO? Antihypertensive drugs 33% Normotension Volume repletion Dialysis-induced hypotension (autonomic and/or V. dysfunction?) Adapted from: Mailloux, LU, Bellucci, AG, Napolitano, B & Mossey, RT. (1994). The contribution of hypertension to dialysis patient outcomes. ASAIO Journal. 40(2): p.134. Reyes-Bahamonde J, Raimann JG, Thijssen S, Levin NW, & Kotanko P. (2013) Fluid Overload and Inflammation—A Vicious Cycle. Seminars in Dialysis Vol 26, No 1 (January–February) pp. 16–39 DOI: 10.1111/sdi.12024 Pecoits-Filho, R et al. (2004). Impact of residual renal function on volume status in chronic renal failure. Blood Purif. 22(3):285-92. Amgen Package insert. 2 4/26/2013 Increased Hospitalizations 14.3% of Medicare patients hospitalized are for fluid-related diagnosis Costs • Heart failure was the primary diagnosis in 83% of episodes, fluid overload in 11%, and pulmonary edema in 6% ¾ of deaths and hospitalizations in dialysis patients can be linked to sudden death or CHF, which • 25,291 patients (14.3%) of prevalent Medicare patients experienced 41,699 care episodes over ~2 years • Average cost was $6,372 per episode; total costs were approximately $266 million are left ventricular in origin Arneson, TJ, Liu, J, Qiu, Y, Gilbertson, DT, Foley, RN, Collins, AJ. Hospital treatment for fluid overload in the medicare hemodialysis population. Clin J Am Soc Nephrol. 2010 Jun;5(6):1054-63 Glassock, RJ, Pecoits-Filho, R. & Barberato, SH. (2009). Left ventricular mass in chronic kidney disease and ESRD, Clin J Am Soc Nephrol 4: S79-S91. doi:10.2215/CJN.04860709 Physiological Effects of Fluid Deficit Arneson, TJ, Liu, J, Qiu, Y, Gilbertson, DT, Foley, RN, Collins, AJ. (2010). Hospital treatment for fluid overload in the medicare hemodialysis population. Clin J Am Soc Nephrol. 5(6):1054-63 Causes of Death in Prevalent Dialysis Patients, 2008-2010 • Access Complications • Myocardial Stunning/Cardiac Ischemia • Stroke risk/leukoaraiosis • Loss of residual renal function • Hypotension/Hypertension • Cramping/Nausea/Vomiting • top causes of early sign-offs • leads to decreased adequacy McIntyre, CW. (2009). Effects of hemodialysis on cardiac function. Kidney Int. 76(4):371-375. Stevens, LA, Viswanathan G, Weiner, DE. (2010). CKD and ESRD in the Elderly: Current Prevalence, Future Projections, and Clinical Significance. Adv Chronic Kidney Dis. July ; 17(4): 293–301. doi:10.1053/j.ackd.2010.03.010 Brewster, UC, Perazella, MA. (2004). Cardiorenal effects of the renin-angiotensin-aldosterone system. Hospital Physician. Jun;40:11-20. Rocco, MV & Burkart, JM. (1993). Prevalence of missed treatments and early sign-offs in hemodialysis patients. JASN. Nov:4(5):1178-1183. Myocardial Stunning and Ischemia Increased Troponins Silent ST Depression • cTn1 rose significantly when measured 44 h. after dialysis sessions complicated by IDH • Elevated levels predict mortality • Subclinical ischemia • W/O plaque rupture • First reported in 1989 • Reported as 15-40% occurrence USRDS 2012 Annual Data Report, Figure 4.1 (Volume 2) Loss of Residual Renal Function hypovolemia ↑ BP & ↑ pulse renin Intradialytic Hypotension (20-30% occurrence) vasoconstriction angiotensin I UF Rate Loss of Contractile Function Cardiac Remodeling • Dialysis-induced myocardial stunning associated with increased rate of intradialytic and post dialytic ventricular arrhythmias • LVH (75% of pts on dialysis) • Reduced arterial compliance • Impaired microcirculation aldosterone A.C.E. angiotensin II Guyton & Hall, Textbook of Medical Physiology, 10th ed, 2000. McIntyre, CW. (2009). Effects of hemodialysis on cardiac function. Kidney Int. 76(4):371-375 Brewster & Perazella: Cardiorenal Effects of the Renin-Angiotensin-Aldosterone System,Hospital Physician, June 2004, pp. 11-20. 3 4/26/2013 “The presence of Residual Renal Function is protective against mortality. Specifically, the presence of Residual Renal Function, even at a low level, is associated with a lower mortality risk in hemodialysis patients.” Dallas QI, 2012 – Goals of Therapy • ECV control using assistive technology • Normalized ECV • Prevent intradialytic hypotension and cardiac stunning through controlled ultrafiltration Shemin D, Bostom AG, Laliberty P, Dworkin LD. (2001). Residual Renal Function and mortality risk in hemodialysis patients. Am J kidney Dis. Jul;38(1):85-90. Tools to Improve Safe Fluid Removal • Reduce volume-related hospitalizations Parker, T.F. et al. A quality initiative: Reducing rates of hospitalizations by objectively monitoring volume removal. Nephrology News and Issues. 2013 Mar;27(3): 30-36 Quality Initiative Protocol: Assess Two Techniques to Control ECV Education Only Group • Education • Eight (8) facilities Education and Intervention Group • Seven (7) facilities • Educational program for physicians, staff, and patients • Show necessity for volume control • Oxygen saturation • Control intradialytic ECV to gain optimal volume removal and prevent symptoms • Salt restriction • Assistive Technology • Clinical assessment of dry weight Sinha, AD (2011). Why assistive Technology is needed for probing of dry weight. Blood Purification, 31: 197-202. DOI: 10.1159/000321840 • Establishment of normalized ECV using assistive technology Parker, T.F. et al. A quality initiative: Reducing rates of hospitalizations by objectively monitoring volume removal. Nephrology News and Issues. 2013 Mar;27(3): 30-36 Implications of current trend toward prescribing high dialysate sodium in HD Education • Fluid assessment and the importance of proper fluid management • All Physicians, Dieticians, RNs • Extra Tx for fluid removal prn • 4-hour Tx time • Update Med lists • Dialysate T 36° C • Max UFR of 13 mL/Kg/hour • • • No sodium modeling Dialysate sodium 138 mEq/L Focused review of sodium content in food HYPERNATRIC DIALYSATE Decreased sodium removal Increased serum sodium Volume overload Increased thirst Hypertension LVH, CHF, Stroke, Death Santos, SFF & Peixoto, AJ. (2008). Revisiting the Dialysate Sodium Prescription as a Tool for Better Blood Pressure and Interdialytic Weight Gain Management in Hemodialysis Patients. Clin J Am Soc Nephrol. Doi:10.2215/CJN.03360807 4 4/26/2013 Dialysate Sodium & Sodium Gradient Thirst • 1,084 clinically stable HD patients • Dialysate sodium 136-149 mEq/L • Mean pre-HD plasma Na+ 136.7 (+/- 2.9 mEq/L) • 83% patients dialyzed against a positive Na+ gradient • Mean Na+ gradient 4.6 (+/- 4.4mEq/L) • Plasma Na+ increased in 91% patients • Post-HD thirst directly correlated with sodium gradient • Mean post-HD Na+ 141.3 (+/- 2.5mEq/L) Mendoza JM, Sun S, Chertow GM, Moran J, Doss S, Schiller B: Mendoza JM, Sun S, Chertow GM, Moran J, Doss S, Schiller B: Dialysate sodium and sodium gradient in maintenance hemodialysis: a neglected sodium restriction approach? Dialysate sodium and sodium gradient in maintenance hemodialysis: a neglected sodium restriction approach? Nephrol Dial Transplant (2011) 26: 1281-1287 doi: 10.1093/ndt/gfq807 Nephrol Dial Transplant (2011) 26: 1281-1287 doi: 10.1093/ndt/gfq807 Sodium Burden Education + Assistive Technology Mendoza JM, Sun S, Chertow GM, Moran J, Doss S, Schiller B: Dialysate sodium and sodium gradient in maintenance hemodialysis: a neglected sodium restriction approach? • < 3% per hour volume reduction = increase UF goal by 200 mL per Tx • 3 - 8% per hour volume reduction (not to exceed 15% total) = No change • > 8% per hour volume reduction = decrease UF goal • Oxygen supplementation for SaO2 of < 90% or SvO2 of < 60% • Refill Assessment: If refill is present, add 200 mL to UF goal next Tx Nephrol Dial Transplant (2011) 26: 1281-1287 doi: 10.1093/ndt/gfq807 Blood Pressure Mosaic Octagon of Blood Pressure BP = Cardiac Output X Peripheral Vascular Resistance Hypervolemia = BP or BP Hypovolemia = BP or BP Smith & Kampine: Circulatory Physiology - the essentials 3rd edition Williams & Wilkins 199. Sinha AD, Agarwal R: The Pitfalls of the Clinical Examination in Assessing Volume Status. Seminars in Dialysis-2009 DOI: 10.1111/j/1525-139X/2009/0087641.x Brewster & Perazella: Cardiorenal Effects of the Renin-Angiotensin-Aldosterone System, Hospital Physician, June 2004, pp. 11-20. Diroll A, Hlebovy D: Inverse relationship between blood volume and blood pressure. Nephrol Nursing J 30:460-461, 2003. Adapted from Page, I.H., Circ Res 34:133, 1974 5 4/26/2013 Hypoxia Definition Interventions to Prevent Hypotension Non Dialysisbased Dialysis-based Daily HD Thermoregulation O2 Therapy/Hypoxia Avoidance Dialysate Na of 138 mEq/L pH/Bicarb Slower UFR “An inadequate supply of oxygen to tissues is called tissue hypoxia” Dietary Na Reduction Diabetes Control West, JB (1985). Gas transport to the periphery. In TM Tracy (Ed.), Respiratory physiology‐the essentials. p. 83. Baltimore, MD: Williams & Wilkins Glennie, JA. (2013) Architecture student. UT, Austin,TX. Art used with permission McIntyre, CW. (2009). Effects of hemodialysis on cardiac function. Kidney Int. 76(4):371375 Ahmad, S. (1999). Complications of hemodialysis. In M. Knowles (Ed.), Manual of clinical dialysis (p. 35). London: Science Press Ltd. Incidence Hypoxia Causes • Hypoxemia occurs in nearly 90% of patients during hemodialysis, may contribute to intradialytic hypotension, nausea, and muscle cramps HYPOXIC • Pulmonary • Hypoventilation • Pleural effusion present in 28% of pre-dialysis chest radiographs ANEMIC • ↓ Hemoglobin = hypoxemia • Dilutional d/t hypervolemia • Soft tissue calcification was identified in 79% of patients on hemodialysis – heart, lungs, stomach CIRCULATORY • ↓ Cardiac Output • Hypovolemia HISTOTOXIC • Sepsis • Toxic Substances • Functional pulmonary changes • Sleep apnea 60% ESRD patients, contributing to arrhythmias and pulmonary HTN Gheuens, E.O., Daelemans, R., & De Broe, M.E. (2000). Pulmonary problems in hemodialysis and peritoneal dialysis. In N. Lameire & R.L. Mehta (Eds.), Complications of dialysis (pp. 485-491). New York, NY: Marcel Dekker, Inc. Guyton, AC & Hall, JE (2000). Respiratory insufficiency – pathophysiology, diagnosis, oxygen therapy. In A Norwitz (Ed.), Textbook of medical physiology (pp. 490-491). Philadelphia, PA: Saunders. West, JB (1985). Gas transport to the periphery. In TM Tracy (Ed.), Respiratory physiology-the essentials (p. 83). Baltimore, MD: Williams & Wilkins. Case Study Hypoxia Anemia Vasodilation CP Complications Volume Overload Hypotension Saline Bolus ↓ UFR Thorn, C.E., Kyte, H., Slaff, D.W. & Shore, A.C. (2011). An association between vasomotion and oxygen extraction. American Journal of Physiology Heart and Circulatory Physiology, 301(2): H442-H449. Gheuens, EO et al (2000). Pulmonary problems in hemodialysis and peritoneal dialysis. In N. Lameire & R.L. Mehta (Eds.), Complications of dialysis (pp. 485-491). NY, NY: Marcel Dekker, Inc. Diroll, DD (2013). Oxygen as an adjunct to treat intra-dialytic hypotension during hemodialysis. Manuscript submitted for publication. Monitor-Guided Interventions Elapsed Time Blood Pressure Pulse BV ∆ Oxygen Saturation Intervention 0:00 112/63 61 0.0% 82.3% HD commenced 0:30 86/46 62 -2.0% 85% O2 @ 2L per nasal cannula 0:40 97/51 62 -0.5% (refill) 94% UF Goal increased from 3.0L to 4.9L 1:00 108/51 65 -1.5% 94% 1:15 118/56 66 -2.0% 94% 1:30 140/72 69 -2.0% 95% 2:00 136/78 70 -2.5% 94% 2:30 125/64 71 -4.5% 90% 3:00 137/74 71 -5.0% 93% 3:30 125/68 72 -7.3% 92% -7.3% 93% 4:00 HD ended Diroll, DD (2013). Oxygen as an adjunct to treat intra-dialytic hypotension during hemodialysis. Manuscript submitted for publication. 6 4/26/2013 Fluid-Related Hospitalizations Hospitalized days (per 1000 treatments) All-Cause Hospitalizations Hospitalized days (per patientyear) Hospitalizations (per 1000 treatments) Hospitalizations (per patientyear) Before After Before After Before After Before After Education & Assistive Technology 1.02 0.53 0.16 0.08 4.17 1.83 0.65 0.29 Education Only 0.99 1.04 0.15 0.16 4.5 5.54 0.70 0.86 Parker, T.F. et al. A quality initiative: Reducing rates of hospitalizations by objectively monitoring volume removal. Nephrology News and Issues. 2013 Mar;27(3): 30-36 Hospitalized days (per 1000 treatments) Hospitalized days (per patientyear) Hospitalizations (per 1000 treatments) Hospitalizations (per patientyear) Before After Before After Before After Before After Education & Assistive Technology 13.87 10.45 2.16 1.63 72.68 64.26 11.34 10.03 Education 11.09 10.68 1.73 1.67 66.35 66.38 10.35 10.35 Parker, T.F. et al. A quality initiative: Reducing rates of hospitalizations by objectively monitoring volume removal. Nephrology News and Issues. 2013 Mar;27(3): 30-36 Conclusion Results • Results suggest substantial reduction in ECV-related hospitalizations using objective monitoring of ECV removal and attainment of “normalized ECV” versus education only intervention • Statistically significant for all-cause hospitalizations • Approaching statistical significance for fluid-related events and fluid-related hospitalized days • Conventional education and assessment of “dry weight”, in this study, does not appear to be effective Parker, T.F. et al. A quality initiative: Reducing rates of hospitalizations by objectively monitoring volume removal. Nephrology News and Issues. 2013 Mar;27(3): 30-36 Adequacy: Include Blood Volume Reduction URR = pre BUN – post BUN post BUN 1. Move from a Kt/V model to a Kt/V + volume removal prescriptive model 2. Contemporary management, which is dependent on a clinically derived estimate of dry weight, leads to both an overestimation and underestimation of dry weight 3. Future work should focus on the impact of uremic toxin clearance and volume control as critical components of the measurement of dose of dialysis Parker, T.F. et al. A quality initiative: Reducing rates of hospitalizations by objectively monitoring volume removal. Nephrology News and Issues. 2013 Mar;27(3): 30-36 Jaeger & Mehta: Assessment of dry weight in hemodialysis. JASN, 10:392-403, 1999 Ahmad, S. (1999). Dose of hemodialysis. In M. Knowles (Ed.), Manual of clinical dialysis (p. 52). London: Science Press Ltd. Target BVR 1Steep BVR = post Hct 3-hour run, total BVR = 4.8 to 10.8% 4-hour run, total BVR = 6.4 to 14.4% Improvements: Target ≥ 65% post Hct – pre Hct slope = BVR 1.6% to 3.6% per hour Examples: x 100 2BP reduction 1higher albumin level 1higher Hgb x 100 1Flat Target ≥ ??? Leypoldt, JK, Cheung, AK, Steuer, RR, Harris, DH, & Conis, JM. Determination of circulating blood volume by continuously monitoring hematocrit during hemodialysis. JASN. 1995; 6:214-219. Boyle, A & Sobotka, PA. Redefining the therapeutic objective in decompensated heart failure: hemoconcentration as a surrogate for plasma refill rate. Journal of Cardiac Failure. 2006; 12(4) 247-249. slope = BVR 0.3% to 1.1% per hour 1.72 higher hazard of mortality 1Agarwal, R. Hypervolemia is associated with increased mortality among hemodialysis patients. Hypertension. 2010 Jul; DOI: 10.1161/HYPERTENSIONAHA.110.154815 2Sinha, AD, Light, RP, & Agarwal, R. Relative plasma volume monitoring during hemodialysis aids the assessment of dry weight. Hypertension. 2009 Dec. DOI:10.1161/HYPERTENSIONAHA.109.143974 7
© Copyright 2026