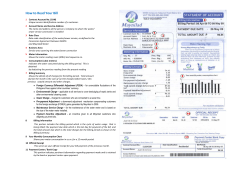
Manual hospital for Participating Hospitals, Ancillary Facilities, and Ancillary Providers
hospital Manual for Participating Hospitals, Ancillary Facilities, and Ancillary Providers Independence Blue Cross offers products directly, through its subsidiaries Keystone Health Plan East and QCC Insurance Company, and with Highmark Blue Shield — independent licensees of the Blue Cross and Blue Shield Association. Table of Contents Hospital Manual 1 Introduction .......................................................................................................... 1.i 2 General Information ............................................................................................. 2.i 3 Administrative Procedures .................................................................................. 3.i 4 BlueCard® .............................................................................................................. 4.i 5 Fraud, Waste, and Abuse ..................................................................................... 5.i 6 Medical Policy ....................................................................................................... 6.i 7 Billing & Reimbursement for Hospital Services ................................................ 7.i 8 Billing & Reimbursement for Ancillary Services ............................................... 8.i 9 Care Management and Coordination ................................................................. 9.i 10 Behavioral Health .............................................................................................. 10.i 11 Quality Management .......................................................................................... 11.i 12 Disclaimer Information ...................................................................................... 12.1 7/1/2014 i Introduction Hospital Manual 1 Table of Contents Who is “Plan”? .......................................................................................................................1.1 Navigating through the Hospital Manual ..............................................................................1.1 Keyword search function ....................................................................................................................... 1.1 Table of Contents .................................................................................................................................. 1.1 Reference links ...................................................................................................................................... 1.1 Hyperlinked websites ............................................................................................................................ 1.2 Definitions ..............................................................................................................................1.2 7/1/2014 1.i Introduction Hospital Manual 1 The Hospital Manual for Participating Hospitals, Ancillary Facilities, and Ancillary Providers (Hospital Manual) is part of your Hospital, Ancillary Facility, or Ancillary Provider Agreement (Agreement), as applicable, with Independence Blue Cross and its Affiliates (collectively referred to as “IBC” or “Plan” throughout this Hospital Manual). This manual supplements the terms of your contract and is updated regularly to provide you with pertinent policies, procedures, and administrative functions relevant to the Covered Services your facility provides to our Members. The Hospital Manual is one of several communication vehicles that enables us to offer timely, pertinent information to you. We will provide your facility with regular updates through the following resources: Partners in Health UpdateSM: Our monthly newsletter that includes news and announcements on various topics such as administrative processes, medical policies, and other important information. The NaviNet® web portal: An online gateway that allows real-time transactions between IBC and its Providers. Provider Bulletins: Valuable resources that provide information about policies and procedures that are essential to Participating Providers. Website: www.ibx.com/providers. Who is “Plan”? As used herein, the term “Plan” refers to Independence Blue Cross and its managed care subsidiaries and Affiliates, including, but not limited to, Keystone Health Plan East and QCC Insurance Company. Refer to the Administrative Procedures section of this manual for a complete list of products. Navigating through the Hospital Manual This Hospital Manual has been published in the Adobe Acrobat® Portable Document Format (PDF). The PDF offers time-saving, Web-like functionality that makes locating information quick and easy. For optimal performance, we suggest that you visit the Adobe® website at www.adobe.com/downloads and download the latest edition of Adobe Reader® at no cost. A brief overview of some of the time-saving enhancements is listed below. Keyword search function Every word in the Hospital Manual can be found by conducting a keyword search. There are several simple ways to start a search. Each of the following methods will produce the same results: Choose Edit and then Search from the main menu drop-down. Press CTRL + F. Type directly into the “Find” field that may already appear on your toolbar. Right-click your mouse, and choose Search. Table of Contents A hyperlinked Table of Contents is provided at the beginning of each section. Just click on a topic of interest, and you will be taken directly to that section. Reference links For your ease of reading and navigation, many sections of the Hospital Manual refer to a particular page or section within the manual where additional information is located. These reference links are displayed in green. Whenever you come across one of these reference links, simply click the green text to view the page or section indicated. 7/1/2014 1.1 Introduction Hospital Manual 1 Example: Refer to the General Information section for additional contact information. Hyperlinked websites All websites mentioned in the Hospital Manual are hyperlinked. If the Hospital Manual refers to a website — either an IBC or third-party website — you can click the italicized web address, and the website will open in your Web browser. All links are current as of the date indicated at the bottom of each section. Note: You must have an Internet connection to view these sites. Definitions All capitalized terms in this manual shall have the meaning set forth in either your Agreement or the Member’s benefits plan, as applicable. A Payor is an entity which, pursuant to a Benefit Program Agreement with IBC, funds, administers, offers, or arranges to provide Covered Services and which has agreed to act as Payor in accordance with IBC’s Agreements with its Participating Providers. IBC itself is a Payor in certain circumstances. With respect to a self-insured plan covering the employees of one or more employers, the Payor is the employer. IBC is not a guarantor of payment for other Payors. In the event a Benefit Program Agreement with a self-insured Payor is terminated, for any reason, including, but not limited to, the failure of such Payor to fund its self-insured plan in accordance with the terms of the Benefit Program Agreement, IBC shall update its electronic Member eligibility database as soon as reasonably possible, to reflect the nonMember status of such self-insured plan’s employees. In accordance with your Agreement with IBC, the Hospital may directly bill individuals who are not or were not Members on the date of service. Notwithstanding anything to the contrary in your Agreement with IBC, Hospital may also directly bill Members of such self-insured plans for services, which are denied by IBC, or for any amounts owed, when a self-insured Payor fails to fund its self-funded plan in accordance with the terms of the Benefit Agreement. 7/1/2014 1.2 General Information Hospital Manual 2 Table of Contents Attention: Transition to a New Operating Platform in Progress .........................................2.1 Contact information ...............................................................................................................2.1 Important telephone numbers ................................................................................................................ 2.1 Claims mailing addresses ...................................................................................................................... 2.3 Appeals mailing addresses .................................................................................................................... 2.3 Network Coordinators ...........................................................................................................2.3 Network Coordinator Locator Tool ....................................................................................................... 2.4 Provider Services ...................................................................................................................2.4 Provider Communications.....................................................................................................2.4 ibx.com/providers .................................................................................................................................. 2.4 Provider News Center............................................................................................................................ 2.5 NaviNet Plan Central ............................................................................................................................. 2.5 Provider Supply Line .............................................................................................................2.6 Cost and quality transparency tools ....................................................................................2.6 7/1/2014 2.i General Information Hospital Manual 2 Attention: Transition to a New Operating Platform in Progress As of November 1, 2013, and continuing through mid-2015, IBC is transitioning its membership to a new operating platform (new platform) in stages, generally based on when the customer/Member’s contract renews. During this transition, we will be working with you in a dual claims-processing environment until all of our membership is migrated to the new platform. In other words, as Members are migrated, their claims will be processed on the new platform; however, we will continue to process claims on the current IBC platform for Members who have not yet been migrated. Throughout this section of the manual, there may be information that is noted as being applicable only for migrated or non-migrated Members. Please take note of these instances as you review this information. Visit our Business Transformation site at www.ibx.com/pnc/businesstransformation for the most up-to-date information about our transition to the new platform. A Frequently Asked Questions document and communication archive are available on this site for your reference. Contact information Important telephone numbers Within Philadelphia area Outside Philadelphia area ® AIM Specialty Health (AIM) Call for CT/CTA, MRI/MRA, PET, and Nuclear Cardiology Precertification requests Anti-Fraud and Corporate Compliance Hotline Baby BluePrints 1-800-ASK-BLUE 1-866-282-2707 ® Perinatal case management Nurse on call 24 hours a day 1-800-598-BABY [2229] 215-241-2198 Credentialing Credentialing violation hotline Credentialing and re-credentialing inquiries 215-988-1413 [email protected] Customer Service Keystone Health Plan East HMO/POS Hours: Mon. – Fri., 8 a.m. – 6 p.m. 1-800-ASK-BLUE ® Personal Choice PPO Hours: Mon. – Fri., 8 a.m. – 6 p.m. Federal Employee Program (FEP) Hours: Mon. – Fri., 8 a.m. – 5 p.m. Keystone 65 HMO/POS Hours: 8 a.m. – 8 p.m., 7 days a week (on weekends and holidays from February 15 through September 30, your call may be sent to voicemail) 7/1/2014 215-241-4400 215-241-2365 1-800-645-3965 2.1 General Information Hospital Manual 2 Within Philadelphia area Outside Philadelphia area 215-561-4877 1-888-718-3333 SM Personal Choice 65 PPO Hours: 8 a.m. – 8 p.m., 7 days a week (on weekends and holidays from February 15 through September 30, your call may be sent to voicemail) MedigapSecurity and Security 65 ® Hours: 8 a.m. – 8 p.m., 7 days a week (on weekends and holidays from February 15 through September 30, your call may be sent to voicemail) 1-888-926-1212 TTY/TDD Language assistance services are offered through the AT&T Language Line for Members who have difficulty communicating because of an inability to speak or understand English. Highmark EDI Operations Hours: Mon. – Fri., 8 a.m. –5 p.m. ® FutureScripts (Pharmacy Benefits) Hours: Mon. – Fri., 8 a.m. – 6 p.m. ® FutureScripts Secure (Medicare Part D) Hours: Mon. – Fri., 8 a.m. – 6 p.m. Blood Glucose Meter Hotline Health Coaching Case management HMO/PPO (Medicare Advantage and Commercial) Hours: Mon. – Fri., 8 a.m. – 5 p.m. Condition management Hours: 24 hours a day, 7 days a week 215-241-2944 1-888-857-4816 1-800-922-0246 1-888-678-7012 Toll-free fax: 1-888-671-5285 1-888-678-7015 1-888-678-7012 1-800-ASK-BLUE Independence Administrators 1-888-356-7899 Independence Blue Cross and Highmark Blue Shield Caring Foundation 1-800-464-5437 Keystone First Hours: Mon. – Fri., 8 a.m. – 5 p.m. Nurse on call 24 hours a day 1-800-521-6007 Mental Health/Substance Abuse Magellan Behavioral Health, Inc. Customer Service/Precertification For Keystone Health Plan East Members with Caring Foundation benefits Hours: 24 hours a day, 7 days a week NaviNet 1-800-688-1911 1-800-294-0800 ® NaviNet Customer Care (technical issues) eBusiness Hotline (portal registration and questions) 1-888-482-8057 215-640-7410 Preapproval/Precertification* Hours: Mon. – Fri., 8 a.m. – 5 p.m. 7/1/2014 1-800-ASK-BLUE 2.2 General Information Hospital Manual Within Philadelphia area 2 Outside Philadelphia area Provider Automated System* Authorization services are available Monday through Saturday, 5 a.m. to 11 p.m., and Sunday, 9 a.m. to 11 p.m. Provider Supply Line 1-800-ASK-BLUE www.ibx.com/providerautomatedsystem 1-800-858-4728 www.ibx.com/providersupplyline *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, you will no longer be able to use the Provider Automated System for that Member. This includes all functionality, such as eligibility, claims status, and Preapproval. You must use the NaviNet web portal to perform these tasks. Claims mailing addresses For a complete list of claims submission addresses, refer to the facility payer ID grid at www.ibx.com/edi. There, claims submission information is broken out by alpha prefix/product name. The following are other claims-related addresses: Indemnity Independence Blue Cross 1901 Market Street IBC Operations Support Philadelphia, PA 19103-1480 Attn: SG1 Outer County Claims – Lehigh, Lancaster, Northamption, and Berks County PA Provider Claims P.O. Box 69303 Harrisburg, PA 17106-9303 Appeals mailing addresses Facility Appeals (Inpatient appeals for Hospitals) P.O. Box 13985 Philadelphia, PA 19101-3985 ER services appeals Claims Medical Review – ER Review Independence Blue Cross 1901 Market Street Philadelphia, PA 19103-1480 Outpatient appeals (except ER) Provider Appeals P.O. Box 41453 Philadelphia, PA 19101-1453 Payment review for lack of Preapproval Facility Payment Review P.O. Box 13985 Philadelphia, PA 19101-3985 Network Coordinators Network Coordinators play a critical role in educating our network Providers and their office staff on policies, procedures, and specific billing processes. Network Coordinators also serve as a liaison for the Provider’s office and may promote or suggest workflow solutions. In an effort to build and sustain a strong working relationship with you, Network Coordinators will contact you regularly to: resolve issues review clinical and claim payment policies discuss new policy implementation explain new products and programs investigate and assist in resolution of inquiries 7/1/2014 2.3 General Information Hospital Manual 2 Note: Network Coordinators cannot revise claims submissions or change Provider data. We encourage you to contact your Network Coordinator for help in making day-to-day office operations run as smoothly as possible and help you work efficiently and effectively with us. Network Coordinator Locator Tool The Network Coordinator Locator Tool identifies your Network Coordinator, his or her direct telephone number, fax number, manager, and the Medical Director who supports your facility. Inquiries can also be submitted directly to your coordinator through this tool. To use the Network Coordinator Locator Tool, go to www.ibx.com/providers and select Contact Us from the “Providers” drop-down menu. When you open the tool, you will be prompted to enter either your IBC corporate ID number or your tax ID number. Your Network Coordinator’s contact information will be displayed. If you receive an error message, or if your Network Coordinator’s information is unavailable, contact Customer Service for assistance. Provider Services Provider Services serves as a valuable resource to you in addition to your Network Coordinator. The role of Provider Services is to: service Provider telephone inquiries in an accurate and timely manner; educate Providers and facilitate effective communications between Providers and Independence Blue Cross (IBC) responding to telephone inquiries in a timely and accurate way; educate Providers about self-service utilization; assist Providers in the identification and resolution of claim inquiries. To reach Provider Services, call Customer Service at 1-800-ASK-BLUE and follow the voice prompts. Provider Communications To access the most current and updated information regarding IBC and our policies, procedures, and processes, refer to our monthly newsletter, Partners in Health UpdateSM, our website at www.ibx.com/providers, the Provider News Center, NaviNet Plan Central, and this Hospital Manual. These resources are designed to work in unison to provide your facility with timely informational updates. To receive email updates that provide you with the latest information, including Partners in Health Update and news alerts, simply complete our email address submission form at www.ibx.com/ providers/email. Allow up to two weeks for us to process your request, and remember to add IBC ([email protected]) to your email address book. We respect your privacy and will not make your email address available to third parties. For more information about our privacy policy, go to www.ibx.com/privacy. ibx.com/providers Find important information and resources, such as forms, bulletins, and billing guidelines, specific to our Provider network. Simply place your cursor over the “Providers” tab along the top, and choose from the drop-down menu that appears. Information in this menu is broken out as follows: Communications Business Transformation Policies and Guidelines Claims and Billing Tools and Resources 7/1/2014 2.4 General Information Hospital Manual 2 Pharmacy Information Resources for Patient Management Contact Us Provider News Center The Provider News Center is our Provider-dedicated website, located at www.ibx.com/pnc, which features up-to-date news and information of interest to Providers and the health care community. The site has a user-friendly interface that allows you to easily navigate the latest news and information of interest to you and your facility: Latest News. All Provider news published within the previous month is listed on the home page. Spotlight. Promotional banners located along the top of the website highlight important news. Dedicated News. The home page features dedicated sections for important topics (e.g., ICD-10) with significant impact to our Participating Providers. Sortability & Searchability. All news is grouped into convenient categories (such as Billing & Reimbursement, NaviNet®, and Products) and broken out by Provider type (Professional, Facility, or Ancillary) so you can quickly find news that’s relevant to you and your office staff. You can also conduct keyword searches to pinpoint specific content. Additionally, the Provider News Center includes a Quick Links section that gives easy access to our traditional IBC resources, such as Inside IPP (the Inter-plan programs publication), IBC forms, the IBC Medical Policy portal, NaviNet, and our annually published Provider publication indices. Business Transformation As of November 1, 2013, IBC has begun our transition to a new operating platform. During this transition, we are working with you in a dual claims-processing environment until all of our membership is migrated to the new platform. In other words, as Members are migrated, their claims will be processed on the new platform; however, we will continue to process claims on the current IBC platform for Members who have not yet been migrated. To assist you in understanding this transition, we have a created a dedicated Business Transformation section on our Provider News Center. The Business Transformation site is a source of news, information, and resources (including a Frequently Asked Questions document and complete communication archive) related to this ongoing process. We encourage you to frequently visit the Business Transformation site at www.ibx.com/pnc/businesstransformation. NaviNet Plan Central In addition to fast, secure, and HIPAA-compliant access to Provider and Member information and real-time transactions, NaviNet-enabled Providers have access to a valuable source of information on our NaviNet Plan Central page. This page contains important tools and resources, including: the latest Provider news and announcements; the most current version of our publications and Hospital Manual; information about upcoming Business Transformation and ICD-10 changes; helpful documents, including user guides, frequently asked questions, enrollment forms for our Medicare Advantage plans, and health and wellness tools; contact information. 7/1/2014 2.5 General Information Hospital Manual 2 Provider Supply Line To replenish office supplies such as the Hospital Manual, allergy stickers, and directories, call the tollfree Provider Supply Line at 1-800-858-4728 or use the online request form available at www.ibx.com/providersupplyline. Have the following information ready so your order can be processed in an error-free, timely manner: NPI number facility name facility address facility telephone number Orders are normally shipped within 24 hours and should arrive at your facility within 3 – 5 business days. Note: Calls to the Provider Supply Line should be for supply requests only. All other inquiries should be directed to Customer Service at 1-800-ASK-BLUE or your Network Coordinator. Supply orders will not be accepted through Customer Service. The IBX App We encourage our Members and Providers to download our free smartphone app, which is available for both iPhone and Android phones. With frequently updated and improved features, the IBX App gives Members easy, 24/7 access to health care coverage. The Doctor’s Visit Assistant allows the user to: fax or email a copy of their ID card; check the status of Referrals and claims; view their health history and prescribed medications; record notes and upload photos of symptoms. The IBX App also offers expanded Provider search capabilities and other ways for users to manage their health on the go. Users of the IBX App can easily find doctors, hospitals, pharmacies, urgent care centers, and Patient-Centered Medical Homes; access benefit information; and track deductibles and spending account balances. Cost and quality transparency tools IBC offers cost and quality transparency tools for Participating Providers and commercial and Medicare Advantage HMO and PPO Members, including those who carry an Independence Administrators ID card. These tools were designed to assist IBC Members in becoming more informed consumers and managing their health benefits. These tools are also relevant to Providers, as they strive to become more accountable for the cost and quality of care being delivered. The following tools and features are available: Find a Doctor tool. Our easy-to-use tool assists Members in their online search for Participating Physicians, specialists, hospitals, and other health care Providers. Patient Experience Review. Users of the Find a Doctor tool can search for a Physician or facility and view Member-submitted ratings and reviews. Members who log on to ibxpress.com or MyIBXTPA.com, our secure Member websites, can enter ratings and write reviews about their experiences with participating Physicians. Migrated Members can enter ratings and reviews for network facilities. A comprehensive process is in place to moderate all submitted reviews for 7/1/2014 2.6 General Information Hospital Manual 2 inappropriate content or language and to verify that the Member had a visit with the Provider. Non-Members and Providers can read the reviews but cannot write them. ® Hospital Comparison Tool. Through an agreement with WebMD , an independent company, the Hospital Advisor tool provides hospital quality and safety information. Both Providers and Members can research and compare hospitals based on procedure/diagnosis and location and can review details on process and outcomes results. The search results can also be customized according to which measure (e.g., volume, mortality, complications, and length-of-stay) are most important to the user. Members can access the tool through our secure Member website, www.ibxpress.com. Providers can access the Hospital Advisor through NaviNet by selecting Reference Tools from the Plan Transactions menu and then selecting Provider Directory. ® Blue Distinction Centers . These facilities are selected by the Blue Cross and Blue Shield Association through a rigorous evaluation of clinical data that provides insight into the facility’s structures, processes, and outcomes of care. Through the Blue Distinction Center designation, consumers can identify facilities that have demonstrated experience in certain services, meet rigorous quality standards, and consistently demonstrate positive quality results. Cost Estimator. This feature allows Members to receive estimated cost information for nearly 150 inpatient, outpatient, and diagnostic procedures performed at our network hospitals, ASCs, and other diagnostic facilities. The Cost Estimator provides Members with the tools and information to estimate their out-of-pocket costs. Hospital Quality Measures. IBC continues to promote and encourage Members to access publicly available hospital quality data, such as information published at www.phcqa.org and information made available through third-party data sources on IBC’s websites. 7/1/2014 2.7 Administrative Procedures Hospital Manual 3 Table of Contents Attention: Transition to a New Operating Platform in Progress .........................................3.1 Rendering services ................................................................................................................3.1 Member eligibility ................................................................................................................... 3.1 Copayments ............................................................................................................................. 3.2 Hospital Referrals .................................................................................................................... 3.4 Member consent for financial responsibility ........................................................................... 3.4 Product offerings ...................................................................................................................3.4 Traditional ................................................................................................................................ 3.5 Personal Choice® — Preferred Provider Organization ............................................................ 3.5 Keystone Health Plan East — HMO ....................................................................................... 3.5 Flex Copay Series .................................................................................................................... 3.6 Flex Deductible Series ............................................................................................................. 3.6 Preapproval guidelines..........................................................................................................3.6 The NaviNet® web portal ........................................................................................................3.6 iEXCHANGE® ..........................................................................................................................3.7 Provider Automated System .................................................................................................3.8 Submitting claims ..................................................................................................................3.8 Electronic Data Interchange claims submission ...................................................................... 3.9 Claims submission requirements ............................................................................................. 3.9 Clean Claim ............................................................................................................................. 3.9 Coordination of Benefits/Other Party Liability ..................................................................... 3.10 HIPAA 5010 and ICD-10 ...................................................................................................... 3.11 Medicare Advantage PPO claims processing ........................................................................ 3.11 Overpayments ........................................................................................................................ 3.11 Updating your Provider information ...................................................................................3.12 7/1/2014 3.1 Administrative Procedures Hospital Manual 3 Attention: Transition to a New Operating Platform in Progress As of November 1, 2013, and continuing through mid-2015, IBC is transitioning its membership to a new operating platform (new platform) in stages, generally based on when the customer/Member’s contract renews. During this transition, we will be working with you in a dual claims-processing environment until all of our membership is migrated to the new platform. In other words, as Members are migrated, their claims will be processed on the new platform; however, we will continue to process claims on the current IBC platform for Members who have not yet been migrated. Throughout this section of the manual, there may be information that is noted as being applicable only for migrated or non-migrated Members. Please take note of these instances as you review this information. Visit our Business Transformation site at www.ibx.com/pnc/businesstransformation for the most up-to-date information about our transition to the new platform. A Frequently Asked Questions document and communication archive are available on this site for your reference. Rendering services Be sure to verify Member eligibility and cost-sharing amounts (i.e., Copayments, Coinsurance, and Deductibles) each time a Member is seen. Member eligibility It is extremely important to properly identify the Member’s type of coverage. All Member ID cards carry important information such as name, ID number, alpha prefix, and coverage type. The information on the card may vary based on the Member’s plan. Eligibility is not a guarantee of payment. In some instances, the Member’s coverage may have been terminated. How to check eligibility Always check the Member’s ID card before providing service. If a Member is unable to produce his or her ID card, ask the Member for a copy of his or her Enrollment/Change Form or temporary insurance information printed from www.ibxpress.com, our secure Member website. This form is issued to Members as temporary identification until the actual ID card is received and may be accepted as proof of coverage. The temporary ID card is valid for a maximum of ten calendar days from the print date. Participating facilities are required to use either the NaviNet® web portal or the Provider Automated System* for all Member eligibility inquiries. A guide and webinar are available for guidance on where to obtain Member eligibility and claims status information through NaviNet. You can find these materials at www.ibx.com/ pnc/businesstransformation in the NaviNet Transaction Changes section. If we are unable to verify eligibility, we will not be responsible for payment of any Emergency or nonemergency services. *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, you will no longer be able to use the Provider Automated System for that Member. This includes all functionality, such as eligibility, claims status, and Preapproval. You must use NaviNet to perform these tasks. 7/1/2014 3.1 Administrative Procedures Hospital Manual 3 Notice of Medicare Advantage HMO and PPO non-coverage All skilled nursing facilities, home health agencies, and comprehensive outpatient rehabilitation facilities must provide advance notice of Medicare coverage termination to Medicare Advantage HMO and PPO enrollees no later than two days before coverage of their services will end. However, if services are expected to be less than two days, the Notice of Medicare Non-Coverage (NOMNC) should be delivered upon admission. If there is a span of longer than two days between services, the NOMNC should be issued on the next to last time services are provided. In addition to providing the date when coverage of services will end, the NOMNC also describes the patient’s options if he or she wants to appeal the decision or would like more information. Visit the Centers for Medicare & Medicaid Services (CMS) website at www.cms.hhs.gov for more information on this process. Copayments Members are responsible for making all applicable Copayments. The Copayment amounts vary according to the Member’s type of coverage and benefits plan. For NaviNet-enabled Providers, Copayments are listed on the Eligibility Details screen when using the Eligibility and Benefits Inquiry transaction. IBC routinely audits the claims we adjudicate to ensure they are paid accurately and in accordance with the Member’s benefit plan. Audits include, but are not limited to, ensuring appropriate application of costsharing. Urgent care services Urgent care services are available for urgent medical issues that do not require the advanced medical services of the emergency room/department (ER) when a Member’s Physician is unavailable. Generally, urgent care is categorized as medically necessary treatment for a sudden illness or accidental injury that requires prompt medical attention, but is not life-threatening and is not an emergency medical condition, when a Member's Primary Physician is unavailable. Urgent care services are available at approved urgent care centers and retail health clinics. Copayment information for urgent care services is available on NaviNet. Only Providers who are specifically credentialed and contracted with IBC as an urgent care Provider can charge an urgent care Copayment for urgent care services. If you have questions related to the urgent care benefit, contact Customer Service at 1-800-ASK-BLUE. Out-of-pocket maximums Commercial HMO, POS, and PPO Members. As required by Health Care Reform, Members should not be charged any cost-sharing (i.e., Copayments, Coinsurance, and Deductibles) once their annual limit has been met. These limits are based on the Member's benefit plan but may not exceed $6,350.00 for an individual, and $12,700.00 for a family. To verify if Members have reached their out-of-pocket maximum, Providers should use the Eligibility and Benefits Inquiry transaction on NaviNet. Medicare Advantage HMO and PPO Members.CMS has mandated a maximum out-of-pocket (MOOP) limit for all Medicare enrollees. The MOOP will establish an annual limit on total enrollee cost-sharing liability (e.g., Deductibles, Copayments, Coinsurance) for Medicare Part A and B services. Its dollar amount will be established annually by CMS but will not change during the course of the calendar year. Once Medicare Advantage HMO and PPO Members reach their MOOP limit, they will have no liability for the remainder of the calendar year for Medicare Part A and B claims. 7/1/2014 3.2 Administrative Procedures Hospital Manual 3 Use NaviNet to check all Medicare Advantage HMO and PPO Members’ benefits as they relate to cost-sharing for every office visit or procedure. Copayments relative to allowed amount for Managed Care products When the Copayment is greater than the allowable amount, only the allowable amount should be collected from the Member. In the event that the Copayment is collected and the facility subsequently determines that the allowed amount is less than the Copayment, the difference between the allowable amount and the Copayment for the service must be refunded to the Member. Please verify the Member’s specific benefits plan to determine all applicable Copayments. Keystone HMO Proactive Members For Members with coverage through Keystone HMO Proactive, our tiered provider network plan, continue to use the Eligibility and Benefits Inquiry transaction on NaviNet to verify your patients’ Copayment amount for their office visit. This transaction will display the appropriate cost-sharing amounts for all three benefit tiers. Therefore you will need to know your benefit tier placement to determine the appropriate amount to collect from the Keystone HMO Proactive Member. Medicare-eligible Members IBC coordinates benefits for commercial Members who are Medicare-eligible, have not enrolled in Medicare Parts A or B, and for whom Medicare would be the primary payer. If a Member is eligible to enroll in Medicare Parts A or B but has not done so, IBC will pay as the secondary payer for services covered under an IBC commercial group Benefits Program (e.g., Personal Choice®, Keystone Health Plan East), even if the Member does not enroll for, pay applicable premiums for, maintain, claim, or receive Medicare Part A or B benefits. This affects any Member who is Medicare-eligible and for whom Medicare would be the primary payer. It is important that you routinely ask your Medicare-eligible Members to show their Medicare ID cards. If you have identified a Member who is eligible to enroll in Medicare Parts A and B, but has not done so, you may collect the amount under ―Member Responsibility‖ on the Statement of Remittance (SOR)†, which includes any cost-sharing plus the amount Medicare would have paid as the primary payer. Preventive drugs Under the Patient Protection and Affordable Care Act, certain preventive services are offered to commercial Members at no cost-sharing. As a result, three classes of drugs (including all strengths/dosages) that are currently covered under the IBC pharmacy benefit with a prescription are now considered preventive for certain ages and genders: Drug class Gender Ages Folic acid (prescriptions with 0.4 – 0.8 mg) Women only All ages All Children ages 6 months through 1 year All Children ages 6 months through 6 years Men Women 45 – 79 55 – 79 Iron supplements Oral fluoride Aspirin to prevent cardiovascular disease 7/1/2014 3.3 Administrative Procedures Hospital Manual Breast cancer chemotherapy prevention Women All ages Tobacco interventions All Adults who use tobacco products Vitamin D supplements All 65 and older 3 Therefore, these drugs will be covered at a $0 Copayment for the genders and ages indicated above. Note: These changes do not apply to Special CareSM, CHIP, or Medicare Advantage HMO and PPO Members. Hospital Referrals When a Member is referred for a surgical procedure or hospital admission, the Primary Care Physician (PCP) needs to issue only one Referral to the specialist or attending/admitting Physician. This Referral will cover all facility-based (i.e., hospital, ambulatory surgical center [ASC]) services provided by the specialist or attending/admitting Physician for the treatment of the Member’s condition. The Referral is valid for 90 days from the date it was issued. The admitting Physician should obtain the required Preapproval. Any pre-admission testing and hospital-based Physician services (e.g., anesthesia) will be covered under the hospital or surgical Preapproval. Note: Certain products have specialized Referral requirements and/or benefits exemptions. Member consent for financial responsibility The Member Consent for Financial Responsibility form is used when a Member does not have a required Referral for nonemergency services or elects to have services performed that are not covered under his or her benefits plan. By signing this form, the Member agrees to pay for noncovered services specified on the form. The form must be completed and signed before services are performed. The form is available on our website at www.ibx.com/providerforms, or Providers may use their own. This form does not supersede the terms of your Agreement, and you may not bill Members for services for which you are contractually prohibited. Medicare Advantage HMO and PPO Members Providers must give Keystone 65 HMO and Personal Choice 65SM PPO Members written notice that noncovered/excluded services are not covered and that the Member will be responsible for payment before services are provided. If the Provider does not give written notice of noncovered/excluded services to the Member, then he or she is required to hold the Member harmless. Product offerings Providers are required to use NaviNet or the Provider Automated System* to obtain Member eligibility information. Providers should call Customer Service for specific product information. The following grids outline the products offered through IBC to assist you in quickly identifying our Members. For a complete list of alpha prefixes that correspond to these products, refer to our payer ID grids at www.ibx.com/edi. 7/1/2014 3.4 Administrative Procedures Hospital Manual 3 Traditional Traditional Blue Cross Hospitalization (Indemnity) Comprehensive Major Medical (CMM) Major Medical Security 65 ® 65 Special Special Care SM MedigapSecurity Personal Choice® — Preferred Provider Organization † ® Personal Choice PPO ® Personal Choice PPO Platinum Personal Choice PPO Gold Personal Choice PPO Silver/Silver Reserve Personal Choice PPO Bronze/Bronze Reserve Personal Choice PPO Catastrophic Personal Choice 65 SM PPO‡ Federal Employees Program (FEP) Keystone Health Plan East — HMO Keystone Health Plan East HMO Keystone HMO Platinum Keystone HMO Gold/Gold Proactive Keystone HMO Silver/Silver Proactive Keystone HMO Bronze Keystone Point-of-Service (KPOS) Keystone 65 Preferred HMO Keystone 65 Select HMO Children’s Health Insurance Program (CHIP) 7/1/2014 3.5 Administrative Procedures Hospital Manual 3 Flex Copay Series Product Keystone Health Plan East HMO Keystone POS Keystone Direct POS Personal Choice PPO Flex Deductible Series Product Keystone Health Plan East HMO Keystone Direct POS ® † Personal Choice PPO *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, you will no longer be able to use the Provider Automated System for that Member. This includes all functionality, such as eligibility, claims status, and Preapproval. You must use NaviNet to perform these tasks. † Some national customers and large local customers use group-specific alpha prefixes. Please refer to the payer ID grids available at www.ibx.com/edi. ‡ Personal Choice 65 PPO is available in Philadelphia and Bucks counties only. Preapproval guidelines Preapproval is required for certain services prior to services being performed. Examples of these services include planned or elective inpatient admissions and select outpatient procedures. Refer to the Care Management and Coordination section of this manual for more information on Preapproval requirements. Preapproval requirements are available on our website at www.ibx.com/preapproval. Note: Preapproval is not required for Emergency Services. The NaviNet® web portal NaviNet, a HIPAA-compliant, Web-based connectivity solution offered by NaviNet, Inc., an independent company, is a fast and efficient way to interact with us to streamline various administrative tasks associated with your IBC patients’ health care. By providing a gateway to IBC’s back-end systems, NaviNet enables you to submit and receive information electronically with increased speed, efficiency, and accuracy. The portal also supports HIPAA-compliant transactions. All Participating Providers, facilities, Magellan-contracted Providers, and billing agencies that support Provider organizations are required to have NaviNet access and must complete the following tasks using NaviNet. Detailed guides and webinars are available for many transactions in the NaviNet Transaction Changes section of our Business Transformation site at www.ibx.com/pnc/ businesstransformation. 7/1/2014 3.6 Administrative Procedures Hospital Manual 3 Eligibility and claims status. All participating Providers and facilities are required to use NaviNet (or call the Provider Automated System*) to verify Member eligibility and check claims status information. The claim detail provided includes specific information such as check date and number, service codes, paid amount, and Member responsibility. † Authorizations. All participating Providers and facilities must use NaviNet in order to initiate authorizations, including ones for medical/surgical procedures, chemotherapy/infusion therapy, durable medical equipment (DME), Emergency hospital admission notification, home health (dietitian, home health aide, occupational therapy, physical therapy, skilled nursing, social work, speech therapy), home infusion, and outpatient speech therapy. Requests for medical/surgical procedures can be made up to six months in advance on NaviNet, and in most cases, requests for Medically Necessary care are authorized immediately. NaviNet submissions that result in a pended status can take up to two business days to be completed. These may include requests for additional clinical information as well as requests that may result in a duplication of services. If the authorization remains pended beyond two business days, or if the authorization request is urgent, call 1-800-ASK-BLUE for assistance. Claim adjustment. Providers who call Customer Service to question a claim payment or to request a claim adjustment will be directed to submit the request via NaviNet using the Claim Investigation transaction. *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, you will no longer be able to use the Provider Automated System for that Member. This includes all functionality, such as eligibility, claims status, and Preapproval. You must use NaviNet to perform these tasks. † This information does not apply to Providers contracted with Magellan Behavioral Health, Inc. (Magellan). Magellancontracted Providers should contact their Magellan Network Coordinator at 1-800-866-4108 for authorizations. If you are a current NaviNet user and need technical assistance, contact NaviNet at 1-888-482-8057 or our eBusiness Provider Hotline at 215-640-7410. If you are not NaviNet-enabled, go to www.navinet.net and select Sign Up from the top right. Interactive training demos are also available to all users on NaviNet. Simply select Customer Support from the top navigation menu, and then select Customer Care. NaviNet for out-of-area claims Using the transactions within the BlueExchange® Out of Area option in the Plan Transactions menu, Providers can review claims status, view eligibility and benefits information, and make Referral/authorization submissions for out-of-area Members. Also available is the BlueCard COB Questionnaire, which should be completed by all out-of-area Members prior to rendering service to streamline claims processing and expedite payment to Providers. Providers can also obtain information regarding the Home Plans’ medical policy and Preapproval requirements using the Medical Policy/ PreCert Inquiry transaction, just by entering the alpha prefix of the out-of-area Member. Detailed guides and webinars are available for several BlueExchange transactions in the NaviNet Transaction Changes section of our Business Transformation site at www.ibx.com/pnc/ businesstransformation. iEXCHANGE® Independence Administrators, which offers third-party administration services to self-funded health plans based in the Philadelphia region and has plan Members throughout the U.S., provides you with an additional online service called iEXCHANGE, a MEDecision product. iEXCHANGE supports the direct 7/1/2014 3.7 Administrative Procedures Hospital Manual 3 submission and processing of health care transactions, including inpatient and outpatient authorizations, treatment updates, concurrent reviews, and extensions. This online service is offered through AmeriHealth Administrators, an independent company that provides medical management services for Independence Administrators. Certain services require precertification to ensure that your patients receive the benefits available to them through their health benefits plan. With just a click of a mouse, you can log into iEXCHANGE, complete the precertification process, and review treatment updates. Available transactions: inpatient requests and extensions other requests and extensions (outpatient and ASC) treatment searches treatment updates Member searches After registering, you can also access iEXCHANGE through NaviNet for Independence Administrators plan Members. For more information or to get iEXCHANGE for your facility, visit www.ibxtpa.com/providers or contact the iEXCHANGE help desk at Independence Administrators by calling 1-888-444-4617. Provider Automated System* Providers can use the Provider Automated System, our speech-enabled, automated phone service, to retrieve Member eligibility information for HMO, POS, and PPO Members, inquire about Referrals, and receive authorization status updates. The Provider Automated System is accessible 24/7 at 1-800-ASK-BLUE. A guide that contains step-by-step instructions on how to use all of the menu prompts available through Customer Service, including transactions in the Provider Automated System is available at www.ibx.com/providerautomatedsystem. Note: For behavioral health services, Providers should still call the number on the Member’s ID card under Mental Health/Substance Abuse. *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, you will no longer be able to use the Provider Automated System for that Member. This includes all functionality, such as eligibility, claims status, and Preapproval. You must use NaviNet to perform these tasks. Submitting claims This section contains general information about claims submission for hospital, ancillary facility, and ancillary Providers. For more detailed information about claims submission for specific services, please refer to either the Billing & Reimbursement for Hospital Services or the Billing & Reimbursement for Ancillary Services section of this manual, as appropriate. Be sure to visit our website at www.ibx.com/edi for information on claims submission and billing and tools related to these activities. This site makes it easy to find important claims-related information and provides access to electronic billing guidelines, HIPAA Transaction Standard Companion Guides, payer ID grids, and claim form requirements. 7/1/2014 3.8 Administrative Procedures Hospital Manual 3 Participating Providers must submit all claims for IBC Members to IBC If you are a Participating Provider with IBC submitting claims for IBC commercial HMO, POS, and PPO and Medicare Advantage HMO and PPO Members, you must submit the claim directly to IBC. This requirement applies both to Providers in the IBC five-county service area (i.e., Bucks, Chester, Delaware, Montgomery, and Philadelphia) and Providers located in contiguous counties (i.e., counties that surround the IBC five-county service area). Claims for IBC Members may not be submitted to a local plan if the Provider is contracted with IBC. For example, an IBC-Participating Provider located in Camden County, New Jersey (i.e., a contiguous county) should not submit a claim to Horizon Blue Cross Blue Shield of New Jersey for an IBC Member. Rather, he or she should submit the claim directly to IBC. If an IBC-Participating Provider attempts to submit a claim to their local plan for an IBC Member, the claim will be denied. No payment will be issued by IBC until the claim is correctly submitted to IBC. Electronic Data Interchange claims submission Electronic Data Interchange (EDI) claims submission is the most effective way to submit your claims. EDI claims submission reduces payor rejections and administrative concerns and increases the speed of claims payment by submitting HMO, PPO, and POS claims electronically. If you are in need of EDI support for IBC claims, Highmark EDI Operations is your first point of contact. Highmark EDI Operations is available at 1-800-992-0246, Monday through Friday from 8 a.m. to 5 p.m., ET. Additional EDI billing information can be viewed online at www.ibx.com/edi. Claims submission requirements For Providers who bill electronically, refer to the claims submission requirements found in the Companion Guides at www.ibx.com/edi. IBC recommends that you share our electronic billing requirements and updates with your billing vendor. For Providers who bill on paper, please refer to the following: UB-04 claim form. Facility Providers who bill on paper should use a UB-04 claim form. A description of how to complete a paper UB-04 claim form can be found at www.ibx.com/pdfs/ providers/npi/ub04_form.pdf. CMS-1500 claim form. The CMS-1500 claim form should only be used by ancillary Providers, such as home infusion, DME, ambulance, and private duty nursing. For more information on submitting CMS-1500 claim forms, refer to Claims submission toolkit for proper electronic and paper claims submissions, available at www.ibx.com/pdfs/providers/claims_and_billing/npi/ claims_submission_toolkit.pdf. Failure to use the correct claim form for the services being billed will result in the claim being returned to you or claim denial. Clean Claim A Clean Claim is a claim for payment for a Covered Service provided to an eligible Member on the date of service, accepted by IBC’s EDI system as complete and accurately submitted, and consistent with the Clean Claim definition set forth in applicable federal or State laws and regulations. The following information is generally required for a Clean Claim: patient’s full name patient’s date of birth valid Member ID number, including prefix 7/1/2014 3.9 Administrative Procedures Hospital Manual 3 statement “from” and “to” dates diagnosis codes facility bill type revenue codes procedure codes (e.g., CPT® at the line level for Outpatient claims, ICD-9-CM at the claim level for Inpatient claims) charge information and units service Provider’s name, address, and National Provider Identifier (NPI) Provider’s TIN For proper claims processing, please ensure that your billing NPI is affiliated with the entity that submits your electronic claims (e.g., your clearinghouse vendor). If your billing NPI is not affiliated with the submitter, claims for migrated Members will not be accepted for processing and will reject. Missing or incomplete information will result in a claim being returned to you. Claims denied due to missing or incomplete information must be corrected and resubmitted within the time frame specified in your Agreement with IBC in order to be eligible for payment. Coordination of Benefits/Other Party Liability Where IBC is determined to be the secondary payor, IBC will reimburse for any remaining balance, not paid by the primary carrier, only up to and including its own fee schedule or contracted rate, excluding applicable Deductibles, Copayments, and Coinsurance. If the primary carrier paid more than IBC would have paid had it been the primary carrier, no additional payment will be made, and the Member may not be billed. As a result, the total of the primary carrier’s payment plus any balance paid by IBC will never exceed the contracted rate of payment. Motor vehicle accident All claims, up to the appropriate auto benefits amount related to the motor vehicle accident (MVA), are coordinated with the auto insurance carrier. To expedite payment, the Provider should bill the auto insurance carrier first. When the auto insurance carrier sends notice that the applicable auto benefits have been exhausted, the Provider should submit an exhaust letter with each claim form that is submitted to ensure prompt payment and to avoid a timely filing denial. Members should not be billed or be required to pay before MVA-related services are rendered. Workers’ compensation If a claim is related to a workers’ compensation accident, the Provider must bill the workers’ compensation carrier first and conditionally bill IBC to avoid a timely filing denial. If the workers’ compensation carrier denies the claim, the Provider should submit the bill to IBC with a copy of the denial letter attached to the claim. To expedite payment, include the following information when filing a workers’ compensation claim: Member’s name Member’s ID number date of accident name and address of workers’ compensation carrier 7/1/2014 3.10 Administrative Procedures Hospital Manual 3 Submitting COB information Facilities can submit Coordination of Benefits (COB) information electronically for facility services using the applicable 837I format. For instructions on how to bill electronically, visit www.ibx.com/edi. Submitting COB information electronically eliminates the need for paper claims submissions. Claims submitted electronically are processed faster and have a significantly higher “first pass” adjudication rate, which translates into a faster payment. COB for dependents IBC processes COB claims for dependents of Members with different coverage plans according to the “birthday rule.” If both parents have family coverage with two different health plans, the parent whose birthday falls nearest to January 1 is the primary insurance carrier. Example: If the mother’s birthday is January 30 and the father’s birthday is March 1, the mother’s plan is primary. Exceptions to the “birthday rule” may apply under certain conditions, including but not limited to, where required by divorce decree, child custody, or other court order. HIPAA 5010 and ICD-10 HIPAA 5010. The U.S. Department of Health and Human Services stipulates that any health care entity that submits electronic health care transactions, such as claims submissions, eligibility, and remittance advice, must comply with the X12 Version 5010 standards. HIPAA 5010 Companion Guides are available at www.ibx.com/ediforms to assist you in submitting HIPAA 5010-compliant transactions. ICD-10. CMS has delayed the compliance date for the International Classification of Diseases, 10th Edition (ICD-10) diagnosis and procedure codes to no sooner than October 1, 2015. All covered entities will be required to comply with ICD-10 by the final effective date determined by CMS. Visit www.cms.gov/icd10 for more information about the delay. Medicare Advantage PPO claims processing IBC will process BCBSA plan Medicare Advantage enrollee claims for covered professional, facility, and ancillary services (ambulance, DME, and home infusion) in the five-county service area in accordance with your contracted rates. Overpayments If you identify an erroneous overpayment when reviewing your Statement of Remittance (SOR)* and reconciling it against a Member account, log on to NaviNet, select Claim Inquiry and Maintenance from the Plan Transactions menu, and then Claim Status Inquiry. Once the claim is accessed, you can link to Claim Investigation to request a claim retraction through the claims adjudication process. Through this preferred and expedited process, credits and/or retractions will automatically appear on a future SOR*. Occasionally we identify erroneous overpayments, in which case you will receive instructions either in a letter highlighting the specific overpayment or listed on your A/R statement. Follow the specific instructions noted in the letter and/or statement. *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, Providers will no longer receive the current SOR. Facility Providers will receive what will be called the Provider Remittance. Once all Members are migrated in 2015, you will only receive the new Provider Remittance. 7/1/2014 3.11 Administrative Procedures Hospital Manual 3 Updating your Provider information Accurate data files allow us to continue to provide you with important information on billing, claims, changes or additions to policies, and announcements of administrative processes. You are required to submit any changes to your information in writing. This request should be sent directly to the Senior Vice President of Contracting and the Legal Department at the following addresses. Independence Blue Cross Attn: Senior Vice President of Contracting 1901 Market Street, 27th Floor Philadelphia, PA 19103 Independence Blue Cross Attn: Deputy General Counsel, Managed Care 1901 Market Street, 43rd Floor Philadelphia, PA 19103 Note: Thirty days’ advance notice is required for processing. 7/1/2014 3.12 BlueCard® Hospital Manual 4 Table of Contents Overview .................................................................................................................................4.1 About BlueCard......................................................................................................................4.1 Benefit coverage plans excluded from BlueCard ........................................................................... 4.1 Inside IPP............................................................................................................................................. 4.1 Identifying BCBSA Plan enrollees ........................................................................................4.1 Enrollees in the United States ........................................................................................................... 4.1 International enrollees ........................................................................................................................ 4.2 Verifying eligibility and obtaining Preapproval ....................................................................4.3 BlueExchange® ......................................................................................................................4.4 COB Questionnaire ............................................................................................................................ 4.4 Filing BlueCard claims ..........................................................................................................4.5 Claims process flow ........................................................................................................................... 4.5 Claim status inquiries ......................................................................................................................... 4.5 Other Party Liability (OPL) ..................................................................................................... 4.6 Requests for medical records ...............................................................................................4.6 Medical record request guidelines .................................................................................................... 4.6 7/1/2014 4.i BlueCard® Hospital Manual 4 Overview This section of the manual contains information about BlueCard, including a description of the program, resources to help facilitate communication between the Member’s Home and the Host Plan, and requirements and tips for submitting BlueCard claims for out-of-area Members. Out-of-area Members are Members of other Blue Cross and Blue Shield plans who travel or live in the IBC five-county service area, which includes Philadelphia, Bucks, Montgomery, Chester, and Delaware counties. About BlueCard BlueCard is a national program through the Blue Cross and Blue Shield Association (BCBSA), an association of independent Blue Cross and Blue Shield plans, that enables enrollees of one commercial BCBSA plan to obtain health care service benefits while traveling or living in another BCBSA plan’s service area. The program links participating health care Providers with the various BCBSA plans across the country and in more than 200 countries and territories worldwide through a single electronic network for claims processing and reimbursement. As a participating facility or ancillary facility Provider, you are expected to render services to HMO and PPO patients, or patients with traditional hospitalization coverage who (1) are enrolled in Blue Cross® and Blue Shield® plans other than those offered by IBC and (2) who travel or live in the IBC five-county service area (Bucks, Chester, Delaware, Montgomery, and Philadelphia) and present to your facility for treatment. These members are subject to eligibility verification and applicable Preapproval requirements. Benefit coverage plans excluded from BlueCard The following benefit plans are excluded from the BlueCard program: stand-alone dental prescription drugs Federal Employee Program (FEP) all Medicare Advantage plans Inside IPP Inside IPP, an inter-program publication, is a quarterly newsletter intended to increase awareness of and satisfaction with the BlueCard program. It highlights BlueCard-specific initiatives and plans for improvement. The latest edition can be found at www.ibx.com/insideipp, where you can also find a complete archive of past editions. Identifying BCBSA Plan enrollees Enrollees in the United States ID cards for out-of-area enrollees may include: an image of a suitcase with “PPO” in it an image of a blank suitcase The main identifier on ID cards for out-of-area enrollees is the alpha prefix. The three-character alpha prefix at the beginning of the Member ID number is the key element used to identify and correctly route claims to the appropriate BCBSA plan. The alpha prefix identifies the BCBSA plan or national account to which the enrollee belongs and is critical for confirming an enrollee’s membership and coverage. 7/1/2014 4.1 BlueCard® Hospital Manual 4 Prior to providing services to enrollees of other BCBSA plans, be sure to follow these procedures: Ask the enrollee for the most current ID card each time services are rendered. Since new ID cards may be issued to enrollees throughout the year, this will ensure that you have the most up-to-date information in the patient’s file. Make copies of the front and the back of the ID card, and pass this key information on to your billing staff. ID numbers must be reported exactly as shown on the ID card and must not be changed or altered. Do not add or omit any characters from the ID number. You may remove spaces if the suffix is separated from the ID number by a space on the ID card. A correctly reported ID number includes the alpha prefix and all subsequent characters, up to 17 positions total. This means that you may see cards with ID numbers between three and 14 numbers/letters following the alpha prefix. To ensure accurate claims processing, it is critical to capture all ID card data. If the information is not captured correctly, you may experience a delay with claims processing. Note: FEP enrollees will have the letter “R” in front of their ID number instead of an alpha prefix. These Members are excluded from the BlueCard Program. International enrollees BlueCard involves claims for Members of Blue Plans in the 50 United States and the District of Columbia. It also includes claims for Blue Plan Members of international Licensees such as: Triple-S Salud* (Blue Cross Blue Shield of Puerto Rico) Blue Cross Blue Shield of the U.S. Virgin Islands* Blue Cross Blue Shield of Panama* Blue Cross Blue Shield of Uruguay* GeoBlueSM* – the Blue International Solutions Licensee located in Malvern, PA, which provides coverage for students and expatriates of other nations while they are in the United States *Independent licensee of the Blue Cross and Blue Shield Association. Members enrolled with a foreign Licensee can access Provider networks of Blue Licensees in the United States, as well as the networks of other foreign Licensees. These Members carry a Blue ID card with an alpha prefix that has been assigned to the specific international Licensee. The claims submission process is the same as with any other BlueCard claim. Host claims for these service areas should be sent to IBC for processing. Please treat these Members the same as domestic Blue Plan Members, and do not collect any payment from them beyond their cost-sharing amounts. Note: The Canadian Association of Blue Cross Plans and its enrollees are separate and distinct from the BCBSA and its enrollees in the United States. Claims for enrollees of the Canadian Blue Cross Plans are not processed through the BlueCard Program. Please follow the instructions on the enrollee’s ID card when servicing the Canadian Association of Blue Cross Plan enrollees. These plans include the following: Alberta Blue Cross Atlantic Blue Cross Care Manitoba Blue Cross Pacific Blue Cross Quebec Blue Cross Saskatchewan Blue Cross 7/1/2014 4.2 BlueCard® Hospital Manual 4 Verifying eligibility and obtaining Preapproval Verifying eligibility To verify eligibility and coverage information for enrollees from other BCBSA plans, please do one of the following: Log on to IBC’s BlueExchange® via the NaviNet® web portal. Select the BlueExchange Out of Area option from the Plan Transactions menu, and then select Eligibility and Benefits Inquiry. Enter all required fields for the search. You will receive real-time responses to your BlueExchange eligibility requests Monday through Saturday, from 5 a.m. to 10 p.m. ET, and on Sundays, from 9 a.m. to 9 p.m. ET. Submit a HIPAA 270 transaction (eligibility request) electronically to IBC. You will receive real-time responses to your eligibility requests for out-of-area enrollees Monday through Saturday, from 7 a.m. to 1 a.m. ET the next day. Call the BlueCard Eligibility® line at 1-800-676-BLUE. – English- and Spanish-speaking phone operators are available to assist you. – Keep in mind that Blue Plans are located throughout the country and may operate on a different time schedule than IBC. You may be transferred to a voice response system linked to customer enrollment and benefits. – The BlueCard Eligibility line is for eligibility, benefits, and Preapproval/Referral authorization inquiries only. Obtaining Preapproval Remind enrollees of the following regarding obtaining Preapproval: Outpatient services. Out-of-area Members are responsible for obtaining Preapproval from their Home Blue Plan when required for outpatient services. You may also contact the out-of-area enrollee’s plan on the enrollee’s behalf. Inpatient services. For inpatient services, Providers will be responsible for obtaining Preapproval from the Member’s Home Plan for out-of-area Members. The out-of-area Member will be held harmless. Failure to obtain Preapproval for inpatient facility services for out-of-area Members will result in a denied claim. To avoid claim denials, be sure to Preapprove the inpatient stay and check that additional days are authorized before an out-of-area Member is discharged. If there are denied days within an approved inpatient stay, the Provider will be financially liable for the denied days and the Member will be held harmless. In diagnosis related group (DRG)/case rate situations, when the length of an inpatient stay extends beyond the Preapproved length of stay, any additional days must be Preapproved by the last day of the originally Preapproved days. You can contact the Plan in one of the following ways: Call the BlueCard Eligibility line at 1-800-676-BLUE and ask to be transferred to the utilization review area. Submit a HIPAA 278 transaction (referral/authorization request) electronically to IBC. Log on to NaviNet, select the BlueExchange Out of Area option from the Plan Transactions menu, and then select Referral/Auth Submission (HIPAA 278 transaction). If you require assistance with any of the BlueExchange transactions, refer to the User Guides on the NaviNet Customer Care web page for more information. 7/1/2014 4.3 BlueCard® Hospital Manual 4 BlueExchange® BlueExchange is an electronic solution that provides HIPAA compliance for inter-Plan transactions and allows for electronic communication between the Provider and the out-of-area Member’s Home Plan. You can access BlueExchange through NaviNet by selecting the BlueExchange Out of Area option from the Plan Transactions menu, and then Eligibility and Benefits Inquiry. You can also access BlueExchange through trading partners that support eligibility and benefit requests. Using BlueExchange, you can perform the following transactions: Claims Status Inquiry. This transaction allows Providers to acquire up-to-date claims status information for out-of-area Members for whom a claim has been submitted from a local Provider’s office. Eligibility and Benefits Inquiry. This transaction allows Providers to submit inquiries on out-of-area Members in real time. Providers can also use procedure codes as part of the criteria when searching for a Member’s benefits information. Referral/Auth Submission. This transaction allows Providers to submit referral and authorization requests for out-of-area Members. All BlueExchange transaction requests submitted by the Provider performing the inquiry or submission are routed from NaviNet to the Member’s Home Plan. The Member’s Home Plan then transmits the requested Member information through NaviNet. Medical Policy/PreCert Inquiry. Using the Medical Policy Router, you can be routed to the Home Plan’s website that contains medical policies and general Preapproval requirements. This transition happens seamlessly based on the alpha prefix of the Plan, and it gives Providers easy access to medical policy and Preapproval requirements. To view medical policy and Preapproval requirements for out-of-area Blue Members, select Medical Policy/PreCert Inquiry from the BlueExchange Out of Area option in the Plan Transactions menu. To conduct a search, select Medical Policy or Pre-Certification from the drop-down menu under “Type of Inquiry.” Simply enter the alpha prefix noted on the Member’s ID card, and select Submit. If you have any questions regarding the information, please contact the out-of-area Member’s Home Plan. If you require assistance with any of the BlueExchange transactions, refer to the User Guides on the NaviNet Customer Care web page for more information. COB Questionnaire Coordination of benefits (COB) refers to how the Blue system ensures that its Members receive full benefits and prevents double payment for services if they have coverage from two or more sources. All out-of-area Blue Cross and/or Blue Shield Members should complete the COB Questionnaire prior to services being rendered for the following reasons: streamlined claims processing; expedited payment to Providers; reduction in the number of denials related to COB; ability for employer groups to finalize out-of-area claims for their employees. Instructions for completing the questionnaire The questionnaire is available on our website at www.ibx.com/providers/claims_and_billing/ bluecard.html or through NaviNet by selecting BlueCard COB Questionnaire from the BlueExchange Out of Area option in the Plan Transactions menu. 7/1/2014 4.4 BlueCard® Hospital Manual 4 Business Office staff should complete the first two fields of the questionnaire: Provider name and NPI. Then the out-of-area Member should complete the remaining sections of the questionnaire before services are rendered. Immediately process the completed questionnaire by following the instructions on the form. Note: The COB Questionnaire should not be used for local IBC Members or FEP Members. Filing BlueCard claims When you provide hospital/ancillary facility services to an out-of-area BCBSA Plan enrollee, the claim is considered a facility BlueCard claim. Facility BlueCard claims must be submitted to IBC. IBC is the BlueCard processor for facility services and will be your point of contact for claims-related questions. To send claims to IBC electronically, use the 837I HIPAA transaction. The list of available ISA and GS codes to use can be found at www.ibx.com/edi. For claim submission addresses to submit paper claims, refer to the payer ID grids at www.ibx.com/edi. Claims process flow Below is an example of how a facility BlueCard claim flows through the BlueCard Program for processing: An enrollee of another Blue Plan receives services from an IBC-Participating Facility in the IBC five-county service area. The facility submits the claim to IBC (i.e., the local Blue Plan). IBC recognizes the BlueCard enrollee and transmits the claim to the enrollee’s Home Plan. The Home Plan adjudicates the claim according to the enrollee’s benefits plan. The Home Plan issues an Explanation of Benefits to the enrollee. The Home Plan transmits the claims processing results to IBC. IBC issues a Statement of Remittance* and payment to the Participating Facility Provider. Verify the enrollee’s cost-sharing amount and collect any applicable Copayment at the time of service. Indicate on the claim any payment you collected from the enrollee. For details, consult the appropriate companion guide at www.highmark.com/edi-ibc. Do not send duplicate claims. Sending another claim or having your billing agency resubmit a claim automatically will slow down the claims payment process and creates confusion for the enrollee. If outof-area enrollees contact you, advise them to contact their Home Blue Plan and refer them to their ID card for a customer service number. The Home Plan should not contact you directly regarding claims issues, but if someone from the Home Plan contacts you, refer him or her to IBC. *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, Providers will no longer receive the current SOR. Facility Providers will receive what will be called the Provider Remittance. Once all Members are migrated in 2015, you will only receive the new Provider Remittance. Claim status inquiries IBC is your single point of contact for all BlueCard facility claim inquiries. Claim status inquiries can be done by: Phone. For HMO and PPO facility claims and Traditional Hospitalization claims, call IBC at 1-800-ASK-BLUE. Hours of operation are from 8 a.m. to 5 p.m., ET, Monday through Friday. Electronically. Send a HIPAA 276 transaction claim status inquiry transaction to IBC, or log on to IBC NaviNet Plan Central and submit a HIPAA 276. NaviNet. Log on to NaviNet, select the BlueExchange Out of Area option from the Plan Transactions menu, and then select Referral/Auth Submission (HIPAA 278 transaction). 7/1/2014 4.5 BlueCard® Hospital Manual 4 Other Party Liability (OPL) In cases where there is more than one payer and a Blue Cross Blue Shield Plan is a primary payer, submit OPL information with the Blue Cross and/or Blue Shield claim. Upon receipt, we will electronically route the claim to the Member’s Blue Plan. The Member’s Plan then processes the claim and approves payment, and we will reimburse you for services. Requests for medical records A medical record documents a Member’s medical treatment, past and current health status, and treatment plans for future health care. Requesting these records is a significant operating component in successfully resolving BlueCard claims issues. There are several reasons why a Home Plan may request medical records from the Host Plan – IBC, in this case. For example, when a claim results in an appeal, medical records may be required to finalize the claim. A Home Plan may request multiple records at a time. Upon receipt of the request from the Home Plan, IBC validates the request and assures there is not a duplicate request on file. A letter is then mailed to the Provider indicating the type of records required and indicates the address where the medical records should be returned. When we receive medical records from a Provider, they are sent to the Home Plan for review, and a determination is made on how to proceed with the processing of the claim. When a Host Plan Provider receives a request for medical records, it is very important that the records be sent in a timely manner to ensure that the Provider is reimbursed and the services rendered to the out-ofarea Member are covered appropriately. To expedite the handling for these medical record requests, please adhere to the following tips and guidelines: Submit by fax or email for the quickest processing. Only the medical records that have been requested should be sent. Unsolicited medical records cannot be forwarded to another plan by IBC. Host Plan medical records can be sent in any of the following ways: Fax. Medical records can be securely faxed to 215-238-7915. Email. Medical records can be emailed to [email protected]. Mail. If you do not have access to fax or email, you can send medical records by mail on a CD or in hardcopy. Please mail the medical records to: Host Medical Records Department 1901 Market Street SG1 Philadelphia, PA 19103-1480 Medical record request guidelines It is important that Providers are aware of the guidelines that support the medical records request process. Please review the following: Medical records should be stored in a secure manner accessible to authorized personnel only, with Protected Health Information (PHI) safe against unauthorized or inadvertent disclosure. Office staff should receive periodic training about the protection and confidentiality of Member PHI. Medical records should be safeguarded against loss or destruction. Medical records should be maintained according to state requirements and in accordance with the terms of your Provider Agreement. 7/1/2014 4.6 BlueCard® Hospital Manual 4 Subject to applicable State or federal confidentiality or privacy laws, IBC or its designated representatives, or designated representatives of local, State, and federal regulatory agencies that have jurisdiction over IBC, must be allowed access to Provider records on request at the Provider’s place of business during normal business hours to inspect, review, and copy those records at no cost to the plan. When requested by IBC or its designated representatives, or designated representatives of local, State, or federal regulatory agencies, Providers must produce copies of any such records and permit access to the original medical records for comparison purposes within the requested time frame. If requested, the Provider will submit to examination under oath regarding the medical records. The initial request for medical records will be generated from the Member’s Home Plan through BlueSquared®, a Web-based application that facilitates Inter-Plan business processes in real time. 7/1/2014 4.7 Fraud, Waste, and Abuse Hospital Manual 5 Table of Contents Corporate and Financial Investigations Department ...........................................................5.1 CFID Support ........................................................................................................................................ 5.1 Financial Investigations ......................................................................................................................... 5.1 Audits .................................................................................................................................................... 5.1 Production of records and examination under oath............................................................5.3 Documentation requirements for DME services ................................................................................... 5.3 Report fraud, waste, and abuse ............................................................................................5.3 7/1/2014 5.i Fraud, Waste, and Abuse Hospital Manual 5 Corporate and Financial Investigations Department The Corporate and Financial Investigations Department (CFID) is responsible for the prevention, detection, and investigation of all potential areas of fraud, waste, and abuse against IBC. The CFID is also responsible for conducting audits of Providers and pharmaceutical-related services. It identifies, selects, and audits Providers for inaccurately paid claims. In addition, the CFID seeks financial recoveries of overpaid claims and submits these claims for correct adjudication. The CFID is comprised of the following: CFID Support Financial Investigations Professional Provider Audits Facility Provider Audits Ancillary Provider Audits Pharmacy Audits CFID Support CFID Support uses data-mining software to proactively identify aberrant claims, billing patterns, and trends across all IBC lines of business. CFID Support gathers and evaluates information from a variety of sources to support CFID: STAR and STAR Sentinel – sophisticated software data-mining tools that analyze all categories of claims received, Provider demographics, and Member benefits – are primary sources of audit and investigation identification and selection. Members and Providers can confidentially report concerns through the toll-free hotline, 1-866-282-2707, and our website, www.ibx.com/antifraud. Leads are received from internal business areas, as well as external law enforcement agencies, regulatory authorities, and industry specialists. Financial Investigations Financial Investigations evaluates all allegations of fraud, waste, and abuse involving Providers, Members, vendors, associates, and others. They use a wide array of investigative tools to: identify and investigate fraudulent and abusive activities; make referrals to federal, State, and local law enforcement for criminal and/or civil prosecution; make referrals to regulatory authorities for violations of professional licensure; recover losses related to fraud and abuse; employ prevention techniques to decrease and eliminate future losses; make recommendations to terminate Providers for cause from the IBC network. Audits Facility Provider Audits The Agreement between your facility and IBC includes language that allows IBC the right to audit medical and financial records related to Covered Services provided to our Members and the records related to the billing and payment for services rendered. Ancillary and facility Provider audits are conducted by IBC staff, which consists of registered nurses, medical coders, and claims experts, or by an independent audit firm engaged by IBC. 7/1/2014 5.1 Fraud, Waste, and Abuse Hospital Manual 5 Using sophisticated data-mining software tools, the CFID analyzes claims and compares them to Member enrollment data and overall Provider information. Any trends, patterns, or aberrant billing practices are selected for an in-depth audit or investigation. Audits may include: DRG validation audits to ensure that submitted claims are coded properly and remitted appropriately; outpatient fee schedule coding audits to ensure that CPT®/HCPCS codes are properly submitted to reflect the services rendered and that remittance is consistent with policies and contracts; outpatient observation audits to ensure that services rendered accurately match services billed; outpatient critical-care audits to assure accurate coding of outpatient critical-care emergency room/department visits. Process In order to conduct a facility Provider audit, IBC takes the following steps: 1. Reviews prepayment and post-payment claims. 2. Reviews billing and/or medical records, if necessary, for audit process. 3. Notifies Provider in advance of an onsite audit. 4. Notifies Provider of specific purpose and scope (subject to change) of audit. 5. Gives the Provider a draft report of the audit findings. 6. Communicates, in writing, the final audit results to the Provider. 7. Conducts Provider credit balance audits, such as access to current credit balance reports, and aged accounts receivable trial balances, for any account where IBC made payment as primary, secondary, or tertiary Payor. 8. Requires the Provider to repay any overpaid claims. 9. Gives Providers a two-level review process of audit findings; this must be requested in writing. Ancillary Provider Audits The purpose of ancillary Provider audits is to determine the appropriateness of ancillary claims submitted by durable medical equipment (DME) Providers and home infusion Providers (HIP) for services rendered to IBC Members. Audits compare information from an ancillary Provider’s claim with the ancillary Provider’s medical documentation. Ancillary billing audits determine whether all medical items or services appear on the bill and/or whether the ancillary Provider’s documentation substantiates the charge. Through routine and ad hoc audits, ancillary audits identify patterns of potential fraud, waste, and abuse with support of the Financial Investigations team. IBC contracts with external audit firms to conduct field audits of Providers to compare service provisions and billing with your contract Agreement. Audit procedures are followed across all lines of company business. Routine and ad hoc desk and field audits are performed by ancillary audit staff on claims submitted by DME Providers and HIPs to identify the following: billing inaccuracies; unbundling of charges; inappropriate HCPCS and CPT coding; processing errors leading to overpayments; audits of high-dollar medications administered in the home setting to assure the accuracy of claims billed; DME audits to ensure that claims accurately reflect services rendered; medication compounding audits to ensure that necessary and appropriate compounding and billing are done only when commercially prepared mixtures are unavailable. 7/1/2014 5.2 Fraud, Waste, and Abuse Hospital Manual 5 In addition, a comparison of service provisions and claims in accordance with ancillary Provider contract Agreements is performed. Providers are afforded a two-level review process of audit findings. Ancillary auditors and analysts will serve as first-level reviewers familiar with billing practices, coding, medical terminology, and medical record charting. The scope of an ancillary Provider audit includes any ancillary Provider, regardless of contracting status, that renders and bills for services to IBC Members. Prepayment or post-payment audits may be performed and will vary based on Provider and type of service billed for the Member. Production of records and examination under oath When requested by IBC or designated representatives of federal, State, or local law enforcement and/or regulatory agencies, Providers shall produce copies of all medical/financial records requested within 30 days. Providers will permit access to the original medical/financial records for comparison purposes within the requested time frames and, if requested, shall submit to examination under oath regarding the same. If a Provider fails or refuses to produce copies and/or permit access to the original medical records within 30 days as requested, in addition to other remedies, IBC reserves the right to require Selective Medical Review before claims are processed for payment to verify that claims submissions are eligible for coverage under the applicable benefits plan. Documentation requirements for DME services IBC’s DME documentation requirements are consistent with the Centers for Medicare & Medicaid Services documentation requirements, which underscore the importance of securing and retaining documentation. If required documentation is not available on file to support a claim at the time of an audit or record request, IBC may seek repayment from the DME supplier for claims not properly documented. Documentation requirements for DME include the following: Before submitting a claim to IBC, the DME supplier must have on file a timely, appropriate, and complete order for each billed prescription order item that is signed and dated by the Member’s servicing Provider. Proof of delivery is required in the medical record and must include a contemporaneously prepared delivery confirmation or Member’s receipt of supplies and equipment. If delivered by a commercial carrier, the medical record documentation must include a copy of delivery confirmation. If delivered by the DME supplier/Provider, the medical record documentation must include a copy of delivery confirmation that is signed by the Member or caregiver. All documentation must be prepared at the same time as delivery and be available to IBC upon request. The DME supplier must monitor the quantity of accessories and consumable supplies that a Member is actually using and contact the Member regarding replenishment of supplies no sooner than approximately seven days prior to the delivery/shipping date. Dated documentation of this Member contact is required in his or her medical record. Delivery of the supplies should be done no sooner than approximately five days before the Member would exhaust his or her on-hand supply. Report fraud, waste, and abuse If you suspect health care fraud, waste, or abuse against IBC, we urge you to report it. All reports are confidential. You are not required to provide your name, address, or other identifying information. You have three options for submitting your report: 7/1/2014 5.3 Fraud, Waste, and Abuse Hospital Manual 5 1. Submit the Online Fraud, Waste & Abuse Tip Referral Form electronically at www.ibx.com/anti-fraud. 2. Call the confidential anti-fraud and corporate compliance toll-free hotline at 1-866-282-2707. 3. Write a description of your complaint, enclose copies of supporting documentation, and mail it to: Independence Blue Cross Corporate and Financial Investigations Department 1901 Market Street Philadelphia, PA 19103 7/1/2014 5.4 Medical Policy and Claim Payment Policy Hospital Manual 6 Table of Contents Claim Payment Policy Department .......................................................................................6.1 CPPD’s role within IBC .......................................................................................................... 6.1 Access to policies ..................................................................................................................6.2 BlueExchange® Out of Area ................................................................................................... 6.2 6/1/2013 6.0 Medical Policy and Claim Payment Policy Hospital Manual 6 Claim Payment Policy Department The goal of the Claim Payment Policy Department (CPPD) is to facilitate Member access to health care that is clinically appropriate, effective, and of high quality as determined by a critical analysis of scientific literature, current community practice, and the involvement of practitioners in policy development. CPPD’s role within IBC CPPD works with various areas in the company to determine, verify, and publish coverage decisions for services through policy development, maintenance, and revision. Coordination of policy implementation and ensuring accurate claims processing are also part of this process. Specific functions of the CPPD include the following: determine coverage positions for medical products or services through technology evaluation, new policy development, and revisions to existing policies; develop claim payment policy to communicate: – IBC’s coverage and reimbursement position on a specific topic or service; – the criteria for coverage and reimbursement; – the process for reporting specific services. monitor and evaluate medical and claim payment policies for clinical/administrative accuracy in accordance with National Committee for Quality Assurance (NCQA) guidelines, or more frequently when changes in technology have occurred; support medical code activities as well as establish and maintain the development and documentation of coverage positions for Current Procedural Terminology (CPT®) and Healthcare Common Procedure Coding System (HCPCS) medical codes; facilitate clinical review of Quality Management initiatives/programs through the medical policy committee; meet regulatory requirements related to technology assessment and medical policy to achieve accreditation (by NCQA, among others); comply with governmental policies (e.g., Medicare), legislative mandates, etc.; communicate medical and claim payment policy determinations to Participating Providers through newsletters, direct mail, and our website; research and communicate responses to inquiries regarding policies, Medical Necessity issues, new and emerging technologies, reimbursement issues, and coding; make medical and claim payment policies available on our website; coordinate the consistent application of medical and claim payment policies; provide routine review and revision activity to update policy information as new data is received; educate IBC associates regarding policy and supporting documents; serve as content owner of procedure code-to-procedure code edits and edit rationale disclosure; offer support of procedure code-to-procedure code editing software for accuracy of claims processing; develop ongoing review to ensure utilization in the most appropriate and cost-effective setting for the member and the plan, for the delivery of injectables. 6/1/2013 6.1 Medical Policy and Claim Payment Policy Hospital Manual 6 Access to policies Providers can view our medical and claim payment policies online at www.ibx.com/medpolicy. The policies are available to assist Providers in administering and understanding the benefit provisions. Notifications are posted online prior to the effective dates of the policies. Notifications are listed by the intended effective dates, so you can become familiar with them in advance. To read policy notifications, follow these instructions: 1. Visit www.ibx.com/medpolicy. 2. Select Accept and Go to Medical Policy Online. 3. Select Policy Notifications. You can also view policy notifications using the NaviNet® web portal by selecting Reference Tools from the Plan Transactions menu, and then Medical Policy. Notifications are posted frequently, so it’s important to check the site often. BlueExchange® Out of Area The BlueExchange Out of Area transaction on NaviNet offers a menu option that gives you access to information regarding the medical policy of a Member’s Home plan. To find this information: 1. Select BlueExchange Out of Area from the Plan Transactions menu. 2. Select Medical Policy/PreCert Inquiry. Follow these steps to conduct a search: 1. Select Medical Policy from the drop-down menu under “Type of Inquiry.” 2. Enter the Member ID alpha prefix noted on the insurance ID card. 3. Select Submit. The information displayed is provided by the Member’s Home plan. Questions pertaining to the information displayed should be directed to the Member’s Home plan. 6/1/2013 6.2 Billing & Reimbursement for Hospital Services Hospital Manual 7 Table of Contents Attention: Transition to a New Operating Platform in Progress .........................................7.1 Overview .................................................................................................................................7.1 General billing guidelines......................................................................................................7.1 Electronic billing (837I) ........................................................................................................................ 7.1 Paper billing........................................................................................................................................... 7.2 Inpatient Services ..................................................................................................................7.2 Inpatient claims ..................................................................................................................................... 7.2 Maternity admissions............................................................................................................................. 7.5 Per case reimbursed admissions only .................................................................................................... 7.5 Outpatient Services ...............................................................................................................7.6 Cardiology ............................................................................................................................................. 7.6 Diabetic education ................................................................................................................................. 7.6 Emergency services ............................................................................................................................... 7.7 Laboratory services ............................................................................................................................... 7.8 Observation services .............................................................................................................................. 7.8 Outpatient surgery ................................................................................................................................. 7.8 Outpatient implantable devices ........................................................................................................... 7.12 Radiology services............................................................................................................................... 7.13 Short-term rehabilitation therapy services ........................................................................................... 7.14 Sleep study (neurology) ....................................................................................................................... 7.14 Additional billing information .............................................................................................7.15 Revenue codes requiring HCPCS/CPT codes ..................................................................................... 7.15 Not separately payable (NSP) procedures ........................................................................................... 7.15 Coding discrepancies ........................................................................................................................... 7.15 Billing requirements for Providers contracted under Ambulatory Payment Classification (APC) ..... 7.15 Billing for physician and advanced practice nurse services ................................................................ 7.16 Professional office-based services in an outpatient setting ................................................................. 7.16 Coordination of Benefits/Other Party Liability ................................................................................... 7.16 7/1/2014 7.i Billing & Reimbursement for Hospital Services Hospital Manual 7 Attention: Transition to a New Operating Platform in Progress As of November 1, 2013, and continuing through mid-2015, IBC is transitioning its membership to a new operating platform (new platform) in stages, generally based on when the customer/Member’s contract renews. During this transition, we will be working with you in a dual claims-processing environment until all of our membership is migrated to the new platform. In other words, as Members are migrated, their claims will be processed on the new platform; however, we will continue to process claims on the current IBC platform for Members who have not yet been migrated. Throughout this section of the manual, there may be information that is noted as being applicable only for migrated or non-migrated Members. Please take note of these instances as you review this information. Visit our Business Transformation site at www.ibx.com/pnc/businesstransformation for the most up-to-date information about our transition to the new platform. A Frequently Asked Questions document and communication archive are available on this site for your reference. Overview The purpose of this section is to describe the specific billing and Preapproval requirements for services rendered in the hospital setting and to supplement the claims submission information in the Administrative Procedures section. Many of the services in this section of the manual require Preapproval. A list of current Preapproval requirements is available online at www.ibx.com/preapproval. These requirements are subject to change. Any additional requirements specific to a certain type of service are listed under that service category. General billing guidelines Electronic billing (837I) National Association of Insurance Commissioners (NAIC) codes All claims submitted electronically must be submitted with the NAIC codes for the line of business identification. Please view the appropriate payer ID document at www.ibx.com/edi for a complete list of the NAIC-assigned codes. When billing through Electronic Data Interchange (EDI), claims may be submitted through a vendor that you are contracted with or directly to Independence Blue Cross (IBC) through your own computer system. Claims are submitted in batches and may be sent daily or weekly, depending on your claims volume. If you submit claims electronically, you will continue to receive the unsolicited 277 (U277) for notification of both rejected and accepted non-migrated claims and a 277CA for migrated claims. The error description on the U277 and 277CA will aid you in correcting and resending files to ensure an expedited remittance. For submission instructions, please refer to the appropriate Companion Guide at www.ibx.com/ediforms. If you have questions about an electronic claims submission, please contact Highmark EDI Operations at 1-800-992-0246. 7/1/2014 7.1 Billing & Reimbursement for Hospital Services Hospital Manual 7 Paper billing If you must submit a claim on paper, you will need to use the CMS-1500 or UB-04 claim form, as specified in the remainder of this section based on the type of service you provide. Inpatient Services The purpose of this section is to communicate specific billing requirements and reimbursement policies for inpatient hospital services. Hospitals will be reimbursed for inpatient services according to the terms of their Agreement. To the extent that any of the requirements or policies in this section conflict with the Agreement, the terms of the Agreement shall govern. Interim billing. Inpatient claims submitted with bill types 112 (Interim – first claim), 113 (Interim – continuing claim), and 114 (Interim – last claim) and/or a discharge status indicating that the Member is still inpatient will be denied on your Statement of Remittance (SOR) for non-migrated Members, and rejected on the 277CA for migrated Members. You will be advised to submit the bill when the Member is discharged. Long-term care hospitals, physical rehabilitation hospitals, and skilled nursing facilities are excluded from this directive and may continue to bill with a patient status of 30. Inpatient claims Preapproval Preapproval is required for certain services prior to services being performed, including elective inpatient admissions. For detailed information on Preapproval, please refer to the Care Management and Coordination section of this manual. Inpatient day An inpatient day is an admission period that begins at midnight on the day of admission and ends 24 hours later. The midnight-to-midnight method is to be used in reporting inpatient days even if the hospital uses a different definition for other purposes. Any part of an inpatient day, including the day of admission, counts as an inpatient day. The day of discharge is not counted as an inpatient day. Inpatient services Inpatient services are Covered Services that are diagnostic, therapeutic, or surgical and pursuant to an admission. Reimbursement for inpatient services includes, but is not limited to: ancillary services anesthesia care appliances and equipment diagnostic services medication and supplies nursing care radiology recovery room services room and board surgical procedures (including implantable devices, blood, and blood products) therapeutic items (drugs and biologicals) The reimbursement rates for inpatient acute admissions are inclusive of all services provided to the Member during the admission. The rate of payment is determined by the effective date of a Member’s inpatient admission and applies for the length of the admission; therefore, any rate change under the contract during the Member’s stay will not apply. 7/1/2014 7.2 Billing & Reimbursement for Hospital Services Hospital Manual 7 Outpatient services included in reimbursement for inpatient services Outpatient services rendered during an inpatient admission. IBC’s hospital inpatient reimbursement includes payment for all services provided (1) during the inpatient stay, (2) on the day of the admission, and (3) on the day of discharge. There is no additional payment for services billed on an outpatient basis. Charges for outpatient services rendered to the Member during the inpatient stay, on the day of the admission, and on the day of the discharge must be reported on the inpatient claim. If a hospital submits a separate claim for outpatient services that were, or should have been, reported on the Member’s inpatient claim, the outpatient claim is subject to retrospective review through a Provider audit. Outpatient services rendered prior to an inpatient admission (preadmission). Outpatient procedures, such as preadmission services and other services related to the admission, can be before the date of the inpatient admission, but they are not separately reimbursable. Charges for outpatient services not related to the admission may be billed separately. Preadmission services include: – Preoperative examinations. Services billed with a diagnosis code for preoperative examinations are not separately reimbursable. – Preadmission diagnostic services. IBC’s acute care hospital inpatient reimbursement includes payment for preadmission diagnostic services, and charges for preadmission diagnostic services must be included on the inpatient claim. Diagnostic services provided to a Member within three days prior to and including the date of the Member’s admission are deemed to be inpatient services and included in the inpatient payment. For example, if a Member is admitted on a Wednesday, outpatient services provided by the hospital on Sunday, Monday, Tuesday, or Wednesday are included in the inpatient reimbursement. Diagnostic services include the following revenue/procedure codes*: o 0254: Drugs incident to other diagnostic services o 0255: Drugs incident to radiology o 030X: Laboratory o 031X: Laboratory pathological o 032X: Radiology diagnostic o 0341, 0343: Nuclear medicine, diagnostic/diagnostic radiopharmaceutical o 035X: Computed tomography (CT) scan o 0371: Anesthesia incident to radiology o 0372: Anesthesia incident to other diagnostic services o 040X: Other imaging services o 046X: Pulmonary function o 0471: Audiology diagnostic o 0482: Cardiology, stress test o 0483: Cardiology, echocardiology o 053X: Osteopathic services o 061X: Magnetic resonance technology (MRT) o 062X: Medical/surgical supplies, incident to radiology or other diagnostic services o 073X: Electrocardiogram (EKG/ECG) o 074X: Electroencephalogram (EEG) o 0918: Testing, behavioral health o 092X: Other diagnostic services * The list of diagnostic services may be revised periodically to reflect current revenue and/or procedure codes. 7/1/2014 7.3 Billing & Reimbursement for Hospital Services Hospital Manual – 7 Other preadmission services. Non-diagnostic outpatient services that are related to a Member’s hospital admission during the three days immediately preceding and including the date of the Member’s admission are deemed to be inpatient services and are included in the inpatient payment. Non-diagnostic services are defined as being related to the admission when there is a match between the principal diagnosis codes (first three digits) assigned for both the preadmission services and the inpatient stay. Inpatient hospice care Reimbursement is made directly to the contracted hospice agency for the provision of inpatient hospice care. The contracted hospice agency is responsible for reimbursing the hospital for the provision of general inpatient hospice care. Present on admission (POA) indicator All acute care hospitals are required to follow instructions from the Centers for Medicare & Medicaid Services (CMS) regarding the identification of the POA indicator for all diagnosis codes for inpatient claims. Claims submitted without a valid POA indicator will be rejected. Consistent with the CMS requirements for POA indicators, the following facility types are exempt: critical access hospitals long-term care hospitals cancer hospitals children’s inpatient facilities inpatient rehabilitation facilities psychiatric hospitals Member enrollment during an admission IBC payment responsibility varies depending on the Member’s coverage, as summarized below: Commercial HMO and PPO Members. IBC is required to cover the admission from the Member’s enrollment date in an IBC plan. If a Member enrolls in a Commercial plan from another Commercial HMO plan, the previous plan should cover the Member’s entire admission. Medicare Advantage HMO and PPO Members. Original Medicare covers the Member through to the discharge date. If the Member’s benefits plan or regulations conflict with these provisions, actual payments may vary. Member termination during an admission IBC payment responsibility varies depending on Member coverage and Provider payment methodology, as summarized below: Line of business Payment methodology Commercial HMO and Medicare Advantage HMO/PPO Commercial PPO Per diem Pays to the discharge date Pays to the last covered day Per case Pays the entire case rate Pays the entire case rate Percent of charge Pays to the discharge date Pays to the last covered day If the Member’s benefits plan or regulations conflict with these provisions, actual payments may vary. 7/1/2014 7.4 Billing & Reimbursement for Hospital Services Hospital Manual 7 Maternity admissions Reimbursement for maternity admissions is inclusive of the mother and newborn days while the mother is inpatient. Neonatal intensive care unit (NICU) and transitional nursery days are paid separately regardless of mother’s status as inpatient. Normal delivery claims. When billing newborn baby charges (e.g., revenue code 0170, 0171, 0172, or 0179) the maternity charges for mother and baby must be submitted as separate claims — one for the mom and one for the baby. Providers will receive two separate remittances. Detained baby claims. If the baby remains hospitalized after the mother is discharged (i.e., detained baby), a new admission with its own Preapproval is required. The detained baby’s admission date is the same date as the mother’s discharge date. A separate claim for the detained baby’s admission is required. For Members with Federal Employee Program (FEP) coverage. In those cases where the baby requires a higher level of care and is considered sick while the mother is still hospitalized, a separate admission for the baby is needed. The baby’s admission requires its own Preapproval. The baby’s claim is to be billed using either revenue code 0173 or 0174, and the admission date is the same as the Preapproval date. *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, Providers will no longer receive the current SOR. Facility Providers will receive what will be called the Provider Remittance. Once all Members are migrated in 2015, you will only receive the new Provider Remittance. Per case reimbursed admissions only All inpatient days that are reimbursed under a diagnosis-related group (DRG) and/or per-case payment rate are subject to Medical Necessity review, which may include concurrent review and/or retrospective review. Admissions that have been preapproved will not be retrospectively denied for Medical Necessity unless the Preapproval was based on erroneous information or misinformation provided by the hospital. Readmissions Readmissions are subject to the Inpatient Hospital Readmission policy, which applies to hospitals and health systems paid per case or per admission for inpatient hospital stays. For additional information on readmissions, please refer to our medical policies at www.ibx.com/medpolicy. Ungroupable or invalid DRG Claims that are ungroupable or group to an invalid DRG will be denied payment. Claims may be resubmitted by the hospital with corrected data. Version DRG versus rate effective date Unless otherwise specified in the contract, the grouper version used will be based on the contracted version in effect on the date of admission. For all hospitals, the CMS Pricer adjustment factor applied to the DRG pricing will be based on the date of admission. Per-diem reimbursed admissions only All inpatient days that are reimbursed under a per diem payment rate are subject to a concurrent review of Medical Necessity. In the event the hospital fails to provide timely medical information necessary for concurrent review as requested by IBC, inpatient days not reviewed concurrently will be reviewed retrospectively for Medical Necessity. Admissions that have been concurrently reviewed will not be retrospectively denied for Medical Necessity unless the concurrent review was based on erroneous information or misinformation provided by the hospital. 7/1/2014 7.5 Billing & Reimbursement for Hospital Services Hospital Manual 7 Revenue code groupings Per diem reimbursement shall be based on bed-type in accordance with the following crosswalk. To the extent that any of the following revenue codes conflict with the Agreement, the terms of the Agreement shall govern. Group Revenue codes Medical/surgical 0110, 0111, 0112, 0117, 0120, 0121, 0122, 0127, 0130-0132, 0134, 0137, 0140-0142, 0150-0152, 0157, 0206, 0214 Medical/surgical/pediatric 0113, 0123, 0133, 0143, 0153 Intensive care 0200-0203, 0207-0213, 0219 Sub-acute 0159, 0190-0194, 0199 Maternity/NICU 0170-0174, 0179 General rehab (non-behavioral health) 0118, 0128, 0138, 0148, 0158 Behavioral health 0114, 0116, 0118, 0124, 0126, 0128, 0134, 0136, 0138, 0144, 0146, 0148, 0154, 0156, 0158, 0204 Outpatient Services The purpose of this section is to communicate specific billing requirements and reimbursement policies for outpatient hospital services. All services are reimbursed in accordance with IBC’s medical policies, which can be found at www.ibx.com/medpolicy. Hospitals will be reimbursed for outpatient services according to the terms of their Agreement. To the extent any of the below requirements or policies conflict with the Agreement, the terms of the Agreement shall govern. Please refer to the current Correlation Edits for Outpatient Claims, which is updated and distributed each quarter, when determining which revenue codes and HCPCS and/or CPT® codes to use for billing. Cardiology The technical components for outpatient cardiology services are paid at the hospital’s contracted outpatient rate, with the exception of the following EKG procedure codes: 93000, 93005. These procedure codes are paid as a global reimbursement for technical and professional service components for HMO Members, and the hospital is responsible for reimbursing the Physician for their professional services. Diabetic education Outpatient diabetic education is a covered benefit for eligible Members who have been diagnosed as having diabetes mellitus and have a written Physician order to attend an outpatient diabetic education program. In order for a participating hospital’s program to be eligible as an approved outpatient diabetic education program in the IBC network, the program must be certified by the American Diabetes Association (ADA) and specifically referenced in the Agreement. When billing for diabetic education, use revenue code 0942, include the HCPCS and/or CPT code(s), the number of units, and a diabetic diagnosis on the UB-04 claim form. For billing and reimbursement purposes, one unit is equal to one visit (individual or group session). 7/1/2014 7.6 Billing & Reimbursement for Hospital Services Hospital Manual 7 Emergency services Reimbursement rates for emergency services are inclusive of all services provided to the Member during the visit, including the professional component of laboratory and radiology for all managed care Benefits Programs. Fee schedule payments for Traditional (Indemnity) Members apply only for facility services. How to bill for emergency services Whenever one of the revenue codes in the 045X series is present, the UB-04 admitting diagnosis and the Member’s reason for the visit are required fields for outpatient claims. Please report one diagnosis code describing the Member’s stated reason for seeking care. Emergency room/department (ER) claims that do not have the required information completed will not be processed. Critical care Critical care in the ER is to be billed with procedure code 99291 (i.e., critical care). Please note that procedure code 99292 is not separately reimbursable. When ER level-of-service procedure codes are billed with 99291, the claim will be paid at the lower level of service. Follow-up care Routine (non-emergent) follow-up care provided in the ER setting by a Participating Provider is not a covered benefit and is not eligible for a separate ER visit payment. Claims billed for routine (nonemergent) follow-up care provided in the ER setting that contain a routine follow-up diagnosis code will be automatically denied. When follow-up care provided in the ER setting is denied as a noncovered service, commercial Members may be billed for such noncovered services. In order to bill Members for these services, you must provide the Member with prior written notice indicating that follow-up care in the ER setting is not covered and that they will be financially responsible for any follow-up care given in the ER setting. Inpatient admissions If the ER visit results in an inpatient admission, the date the Physician wrote the order becomes the date of admission. The ER charges should be included on the inpatient claim, and no separate ER claim should be filed. Surgical procedures If an ER visit includes surgery performed in a fully equipped and staffed operating room, the facility will receive fee schedule reimbursement for the ER and for the surgery. Otherwise, the surgical services are included in the reimbursement for the ER visit. The surgery should be billed using the appropriate surgery revenue and HCPCS and/or CPT codes. When surgical services are performed in the ER and not a fully equipped operating room, those surgical services should be reported with the applicable ER revenue codes. Reimbursement for ER services when billed with surgical services Services billed together Services reimbursed* Revenue code requirements Surgical services performed in the operating room and emergency services performed in the ER Both ER services and surgical services are reimbursed Surgical services reported with 36x, 481, 49x, or 790; ER services reported with 45x Surgical services and emergency services performed in the ER ER services are reimbursed Surgical services reported with 45x; ER services reported with 45x *Fee schedule reimbursement for these services includes all services provided during the visit, including the professional component of laboratory and radiology. 7/1/2014 7.7 Billing & Reimbursement for Hospital Services Hospital Manual 7 Observation services If an ER visit includes observation services, observation services may be eligible for separate reimbursement at the hospital’s contracted rate. For additional information on observation services, please refer to our medical policies at www.ibx.com/medpolicy. Laboratory services Members are required to obtain a Physician order for laboratory services. Reimbursement for laboratory services is a global (i.e., technical and professional component) payment for services rendered. Payment is made directly to the facility according to the hospital’s contracted rates (if there is no separate designated [capitated] laboratory agreement). Capitated laboratory services Laboratory services for HMO/POS Members are generally provided by the designated Provider under the Capitated Laboratory Program. A complete listing of the services included in this program can be found at www.ibx.com/medpolicy. Laboratory services that are excluded from capitation are paid at the hospital’s contracted rate. STAT laboratory services for HMO/POS Members If an HMO/POS Member receives STAT laboratory services from their capitated laboratory Provider, these services are included in the capitated laboratory payment and are not separately reimbursed. However, if the HMO/POS Member is not at their capitated site for STAT laboratory services, payment for the STAT testing will be reimbursed according to the hospital contracted rates. A Referral is not required for any STAT laboratory services. For additional information on STAT laboratory services, please refer to our medical policies at www.ibx.com/medpolicy. Observation services Observation services are considered an outpatient service, and involve the use of a bed and periodic monitoring by the facility’s nursing or other ancillary staff in order to evaluate and treat an individual’s condition or determine the need for a possible inpatient admission. For further details on observation services, including billing requirements and reimbursement, please refer to our medical policies at www.ibx.com/medpolicy. Outpatient surgery Outpatient surgery reimbursement represents an all-inclusive payment for all facility Covered Services provided during and related to the surgical procedure. The all-inclusive payment includes services/items provided in conjunction with surgical procedures but excludes certain implantable devices. Please refer to the Outpatient Implantable Devices section for more information. All services related to the outpatient surgery should be billed on the same claim. Surgeries performed on multiple dates should be billed on separate claims for each surgical date of service and include all of the services related to each surgery. Do not bill multiple surgical dates of service on the same claim. Outpatient surgical procedures are assigned a surgical category, which determines the level of reimbursement. Surgical procedures not listed on the Outpatient Fee Schedule are individually reviewed for payment consideration when performed in a hospital outpatient setting. Services included in reimbursement for outpatient surgery Outpatient services rendered prior to an outpatient surgical procedure. Outpatient procedures, such as preadmission diagnostic services and other services related to the surgical procedure, can occur before the date of the surgical procedure but are not separately reimbursable. 7/1/2014 7.8 Billing & Reimbursement for Hospital Services Hospital Manual 7 Preoperative examinations. Services billed with a diagnosis code for preoperative examinations are not separately reimbursable. Preadmission diagnostic services. Reimbursement for outpatient surgical procedures includes payment for preadmission diagnostic services. Charges for preadmission diagnostic services must be included on the surgical claim. Diagnostic services provided to a Member within 30 days prior to and including the date of the Member’s surgery are included in the surgical procedure payment. Diagnostic services include the following revenue/procedure codes*: – 0254: Drugs incident to other diagnostic services – 0255: Drugs incident to radiology – 030X: Laboratory – 031X: Laboratory pathological – 032X: Radiology diagnostic – 0341, 0343: Nuclear medicine, diagnostic/diagnostic radiopharmaceutical – 035X: Computed topography (CT) scan – 0371: Anesthesia incident to radiology – 0372: Anesthesia incident to other diagnostic services – 040X: Other imaging services – 046X: Pulmonary function – 0471: Audiology diagnostic – 0482: Cardiology, stress test – 0483: Cardiology, echocardiology – 053X: Osteopathic services – 061X: Magnetic resonance technology (MRT) – 062X: Medical/surgical supplies, incident to radiology or other diagnostic services – 073X: Electrocardiogram (EKG/ECG) – 074X: Electroencephalogram (EEG) – 0918: Testing, behavioral health – 092X: Other diagnostic services *The list of diagnostic services may be revised periodically to reflect current revenue and/or procedure codes. Observation services. When Outpatient surgical claims are paid according to the fee schedule, there is no additional reimbursement for observation room services. For more information regarding observation services, please refer to our medical policies at www.ibx.com/medpolicy. Multiple surgical procedures When multiple outpatient surgical procedures are performed during the same date of service, Providers may bill multiple outpatient surgical procedures with multiple surgical revenue codes. IBC will reimburse the primary procedure at 100 percent of the contracted rate and each eligible secondary procedure at 50 percent of the contracted rate. The primary service on each claim will be determined based on the highestallowable contracted rate. When a claim has multiple procedures with the same highest-allowable contracted rate, the first listed procedure with the highest allowable will be reimbursed as primary, all other eligible procedures will be reimbursed as secondary. Example 1 Rev Procedure code code Contracted rate Status Reimbursement 0360 23130 $100 x 2.5 = $250 Primary (highest allowable) 100% of contracted rate 0369 23156 $50 x 2.5 = $125 Secondary 50% of contracted rate 7/1/2014 7.9 Billing & Reimbursement for Hospital Services Hospital Manual 7 Example 2 Rev code Procedure code Contracted rate Status Reimbursement 0481 92937 $200 x 2.0 = $400 Primary (highest allowable) 100% of contracted rate 0481 92938 $200 x 2.0 = $400 Secondary 50% of contracted rate 0360 93505 $80 x 2.5 = $200 Secondary 50% of contracted rate Incidental procedures Services identified as incidental procedures (IP) on the Outpatient Fee Schedule may or may not be eligible for reimbursement. When multiple surgical procedures are performed on the same date of service, procedures identified as IP are considered incidental to the primary procedure and are not eligible for additional reimbursement. However, payment for an IP is made when that procedure is the only surgical procedure performed or when it is the primary procedure for the episode of care. Example 1 (IP with additional surgical procedures) Revenue code Procedure code IP Reimbursement 0361 24366 N/A 100% of contracted rate 0361 24000 IP No reimbursement 0361 28476 N/A 50% of contracted rate Example 2 (IP as primary surgical procedure) Revenue code Procedure code IP Reimbursement 0360 58672 IP 100% of contracted rate Example 3 (IP as primary and secondary surgical procedures) Revenue code Procedure code IP Reimbursement 0360 29836 IP 100% of contracted rate 0360 29830 IP No reimbursement Members may not be balance-billed for any incidental procedure that is not reimbursed by IBC. Surgical procedures not found on the Outpatient Fee Schedule Surgical procedures not listed on the Outpatient Fee Schedule are individually reviewed for payment consideration when performed in a hospital outpatient setting. IBC may also request medical records to help determine a reimbursement rate or to ensure that the procedure code reported accurately represents the surgery performed. If medical records are requested, IBC will make a determination regarding reimbursement once the documentation is received. Variations before and after surgery Preapproval by IBC is based on the code for the procedure planned, but the code assigned for billing after the procedure may be different. Assuming the codes are reasonably related, this is not a barrier for payment; however, an updated Preapproval may be required. Cancelled surgeries Currently, three types of outpatient cancelled surgery scenarios are eligible for reimbursement. In order for these claims to be processed correctly, certain coding and billing criteria must be met. Claims 7/1/2014 7.10 Billing & Reimbursement for Hospital Services Hospital Manual 7 submitted that do not meet these criteria will be returned to the facility for correction. Please note the criteria for each of the following scenarios when coding and billing your claims. Scenario 1: Patient receives preoperative services, but surgery is cancelled. Example: The patient has preadmission testing for intended cataract surgery but subsequently develops a cold and the surgery is cancelled. Coding and billing requirements: Report the principal diagnosis code, which is the reason for the surgery. Report the secondary diagnosis with the appropriate diagnosis code(s) indicating cancelled surgery. Report the HCPCS and/or CPT code(s) for the preoperative services, indicating procedures performed and the date(s) of service. Submit the claim through the standard channels — no medical record review is required. Reimbursement: The hospital will be reimbursed for preoperative services according to its Agreement. Scenario 2: Planned surgery is stopped before the entire procedure is completed. Example: The patient has planned a laparoscopic adhesiolysis. Surgery proceeds as far as the insertion of the laparoscope when the patient develops an arrhythmia and the surgery is stopped. Coding and billing requirements: Report the principal diagnosis code, which is the reason for the surgery. There is no need to use a diagnosis code indicating cancelled surgery. Code the procedure to the extent it was completed. In this example, the diagnostic laparoscopy code would be used to describe the insertion of the scope. Submit the claim through the standard channels — no medical record review is required. Reimbursement: The hospital will be reimbursed to the extent that the procedure was performed (e.g., diagnostic laparoscopy) according to its Agreement. Scenario 3: Patient was admitted to same day surgery/short procedure unit, but surgery was cancelled before it began. Example: Some services related to the intended procedure have been rendered. For example, the patient is in the operating room. When anesthesia has been induced, the patient’s blood pressure drops and the procedure is cancelled. Coding and billing requirements: Report the principal diagnosis code, which is the reason for the surgery. Report the secondary diagnosis with the appropriate code indicating cancelled surgery. Report the HCPCS and/or CPT code for the intended procedure with the correct revenue code for outpatient surgery. Submit the claim to your Network Coordinator with medical records for the encounter and the reasons for the cancellation. Claims submitted without this required information will not be considered for payment. Reimbursement: The hospital/facility may be reimbursed for surgical procedures cancelled for reasons beyond the hospital’s control. The hospital will be reimbursed at the minor surgery rate (surgical category M) for fee schedule claims or according to their Agreement for all other claims. The procedure will not be reimbursed if the cancellation is due to administrative reasons (e.g., equipment failure, staffing problems). 7/1/2014 7.11 Billing & Reimbursement for Hospital Services Hospital Manual 7 Outpatient implantable devices If the hospital is contracted under the hospital Outpatient Surgery Fee Schedule, specific implantable devices are eligible for additional reimbursement. These select approved implantable devices, listed and updated periodically through Provider bulletins, are reimbursed separately at the hospital’s invoice cost. Please refer to the Outpatient Implantable Device List. How to bill implantable devices Submit the claim electronically through standard channels. Bill the implant using revenue code 0275 or 0278, as appropriate. Charges must also be assigned to implants. These devices will be reimbursed separately at the Provider’s cost, as documented on the manufacturer’s invoice (shipping and sales tax excluded). The implant revenue code and charges must be billed on the initial claim submission. They will not be added when the request for implant reimbursement is submitted. After the base claim is paid, submit the following documentation via fax to Facility Payment at 215-238-7088: operative report implant record implant manufacturer’s invoice (not purchase order) Note: The purchase order is not acceptable in lieu of the manufacturer’s invoice. It may be submitted in addition to the manufacturer’s invoice to clarify a date discrepancy. Also, a manufacturer’s invoice received with handwritten amounts will not be considered acceptable documentation. Generally, we will not accept an invoice with a date greater than the date of surgery as applicable documentation. However, it may be your hospital’s billing practice to request a device with a purchase order, receive the device and use it during surgery, and then be billed by the manufacturer after the actual surgery date. If this is the case, include both the invoice and purchase order for documentation, and specify that this is your hospital’s practice. For certain implants that are purchased on consignment or ordered in bulk (e.g., drug-eluting stents), a representative copy of the manufacturer’s invoice that reflects the cost per unit, units per order (e.g., pack, case, box), and model number and/or clear description of the implantable device will be considered acceptable documentation. We will also require that the patient-specific serial number of the implantable device be recorded in the implant record. To facilitate processing, include a cover sheet that contains a summary of the required information, including: Member name Member ID number Member claim number implant type invoice amount A sample form is available for your use at www.ibx.com/providerforms. Implant record The implant record is required to verify the model and serial number of the implantable device. This information can be found on the implant labels that are attached to the implant record. The facility should place these labels on the operative report, purchase order, or on one of the following: cardiac catheterization report implantable device registration form intra-operative nursing record 7/1/2014 7.12 Billing & Reimbursement for Hospital Services Hospital Manual 7 medical device or issue tracking form operative notes progress notes You may submit one of these forms in lieu of the implant record as long as they include the implant label, indicating the implant’s model and serial number, and a brief description of the device. With the exception of radioactive seeds, implantable devices include implant labels from the manufacturer. Implant requests received without all required documentation will not be considered for reimbursement. Please note that originally submitted requests for implant payments will be processed in accordance with the timely filing provisions of your Agreement. Reimbursement exceptions The following are examples of circumstances where implantable devices are not eligible for reimbursement: The base surgery claim has been denied or has not yet been paid. The type of device is not specified on approved listing. There is insufficient documentation. IBC is not the primary payer. Radiology services Radiology services are reimbursed in accordance with IBC’s medical policies, which are available at www.ibx.com/medpolicy. Members are required to obtain a Physician order and/or a Referral to receive radiology services. Additionally, there are certain high-technology diagnostic services that require Preapproval, and IBC has delegated this responsibility to AIM Specialty Health® (AIM). For additional information on high technology diagnostic services, please refer to our medical policies at www.ibx.com/medpolicy. Payment will be made directly to the facility according to the hospital’s contracted rates. Reimbursement for radiology services is a global (i.e., technical and professional component) payment. Please refer to the current Correlation Edits for Outpatient Claims document, which is updated and distributed each quarter, when determining which revenue codes and HCPCS and/or CPT codes to use for billing. Outpatient hospital services For HMO Members, hospitals that are not the Member’s designated radiology site may perform and be reimbursed for the services listed in the following chart. If the hospital is the designated radiology site for the Member, the covered services listed are included in the capitation payment and no additional payment will be made. 7/1/2014 7.13 Billing & Reimbursement for Hospital Services Hospital Manual Reason for ultrasound 7 Place of service Procedure codes Diagnosis codes High-risk pregnancy Outpatient hospital 76801, 76802, 76805, 76810, 76811, 76812, 76815, 76816, 76817, 76818, 76819, 76820, 76821 V23.0-V23.9 Rule out ectopic pregnancy Outpatient hospital 76815, 76817, 76830, 76856, 76857 633.00-633.91, 761.0, 761.4, 635.70-635.92 V61.70 First-trimester screening Outpatient hospital 76801, 76802 When billed in conjunction with 76813 or 76814 V28.3 Capitated services Radiology services for HMO/POS Members are generally provided by the designated Participating Provider under the Capitated Diagnostic Radiology Program. A complete listing of the services included in this program can be found at www.ibx.com/medpolicy. Radiology services that are excluded from capitation are paid at the hospital’s contracted rate. Interventional radiology Interventional radiology (IR) involves procedures with both a surgical and radiological component. In addition to a surgical revenue code and correlated surgical procedure code, claims also should be submitted with a radiology revenue code and correlated radiology procedure code. The surgical procedure code is reimbursed and includes the radiology services. Short-term rehabilitation therapy services Short-term rehabilitation therapy services are reimbursed in accordance with IBC’s medical policies, which can be found at www.ibx.com/medpolicy. Payment will be made directly to the facility according to the hospital’s contracted rates. Please refer to the current Correlation Edits for Outpatient Claims document, which is updated and distributed each quarter, when determining which revenue codes and HCPCS and/or CPT codes to use for billing. Capitated services Physical therapy and occupational therapy services for HMO/POS Members are generally provided by the designated Participating Provider under the Capitated Outpatient Short-Term Rehab Program. A complete listing of the services included in this program can be found at www.ibx.com/medpolicy. Therapy services that are excluded from capitation are paid at the hospital’s contracted rate. Sleep study (neurology) In order for a participating hospital’s sleep study program to be eligible as an approved sleep study program for IBC’s network, the program must be accredited by the Joint Commission or the American Association of Sleep Medicine, as specifically referred to in your Agreement. For hospital billing, sleep study is part of the neurology fee schedule and should be billed using neurological revenue codes. 7/1/2014 7.14 Billing & Reimbursement for Hospital Services Hospital Manual 7 Additional billing information Revenue codes requiring HCPCS/CPT codes When billing one of the revenue codes listed below, a corresponding HCPCS/CPT code must be reported on the claim line. Revenue code series Revenue codes 02xx 0250-0256, 0258-0261, 0269, 0274-0275, 0278, 0280, 0289-0294, 0299 03xx 0300-0312, 0314, 0319-0324, 0329-0333, 0335, 0339-0344, 0349-0352, 03590362, 0367, 0369, 0374, 0380-0387, 0389-0381, 0399 04xx 0400-0404, 0409-0410, 0412-0413, 0419-0424, 0429-0434, 0439-0444, 04490452, 0456, 0459-0460, 0469-0472, 0479-0483, 0489-0490, 0499 05xx 0510-0517, 0519, 0530-0531, 0539 06xx 0610-0612, 0614-0616, 0618-0619, 0621-0623, 0631-0637 07xx 0700, 0720-0723, 0729-0732, 0739-0740, 0750, 0760-0762, 0769, 0771, 0790 08xx 0820-0825, 0829-0835, 0839-0845, 0849-0855, 0859-0861, 0880-0881, 0889 09xx 0901, 0903, 0914-0918, 0920-0925, 0929, 0940-0949, 0951-0952 Not separately payable (NSP) procedures When multiple procedures are billed, no additional payment is made to hospitals for procedures identified as NSP on the Outpatient Fee Schedule. Services identified as NSP are an inherent part of another procedure and therefore are considered packaged services/items for which no separate payment is made. Members may not be balance-billed for any NSP procedure that is not reimbursed by IBC. Coding discrepancies Any coding discrepancies should be reported using the NaviNet® web portal. In the Plan Transactions menu, select Claim Inquiry and Maintenance, then Claim Status Inquiry. Claims in a finalized status will offer a link to Claim Investigation where you can note any discrepancies. Billing requirements for Providers contracted under Ambulatory Payment Classification (APC) The billing requirements for products reimbursed under APCs are as follows: Correlation requirements. The Correlation Edits for Outpatient Claims document will continue to be applied to all claims submitted, including claims submitted for APC reimbursement. Please be sure to use the most recently published correlations edits table. Integrated Outpatient Code Editor (IOCE). The IOCE identifies billing errors and indicates what actions to take to rectify a claim, as well as performs the calculations to determine composite rate payments where applicable. All claims submitted will be processed through the IOCE, so any errors will need to be addressed accordingly to ensure that an acceptable claim is received and available for adjudication. Modifiers. All modifiers required in accordance with billing guidelines from the CMS will be in effect. In order to receive the correct level of reimbursement, all claims submitted should contain the appropriate modifiers for the services rendered. Implantable items The Outpatient Implantable Device Reimbursement List does not apply to APC reimbursement. The reimbursement for implantable items is included in the appropriate surgical procedure and is not paid separately. Please follow CMS billing requirements for modifiers and code combinations for implants. 7/1/2014 7.15 Billing & Reimbursement for Hospital Services Hospital Manual 7 Billing for physician and advanced practice nurse services Physician and advanced practice nurse services may not be billed by a facility using a UB-04 claim form or 837I transaction. These services must be billed by the Physician or advanced practice nurse using his or her NPI on a CMS-1500 claim form or through an 837P transaction. Professional office-based services in an outpatient setting When a professional Participating Provider performs a service that is considered an office-based service (e.g., office visit, outpatient consultation, professional interpretation and report) in an office-based setting (e.g., clinic, treatment room) located in a hospital facility or hospital affiliate-owned site, the facility is not eligible to receive reimbursement for these services or for any services included in the payment to the professional Participating Provider. However, according to their contract, the facility is eligible to receive reimbursement for any ancillary Covered Services (e.g., laboratory test, radiologic study) related to the office visit or consultation. For additional information about these services, please refer to our medical policies at www.ibx.com/medpolicy. Coordination of Benefits/Other Party Liability All claims should clearly indicate if the claim is the result of an accident, such as a motor vehicle accident, or related to employment. Refer to the General Information section of this manual for more details. The claim should be submitted to the appropriate primary insurance carrier and should include all services rendered during the admission or date of service. To ensure that timely filing standards are met, these types of claims should also be submitted to IBC with the appropriate indicator, in the event that the primary insurer denies responsibility for the claim. 7/1/2014 7.16 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Table of Contents Overview .................................................................................................................................8.1 General billing guidelines......................................................................................................8.1 Electronic billing (837P or 837I) ........................................................................................................... 8.1 Paper billing........................................................................................................................................... 8.1 Billing guidelines by type of service ....................................................................................8.1 Ambulance services ............................................................................................................................... 8.1 Ambulatory surgical center services...................................................................................................... 8.2 Birthing centers ..................................................................................................................................... 8.4 Dialysis centers...................................................................................................................................... 8.4 Durable medical equipment ................................................................................................................... 8.5 Home health........................................................................................................................................... 8.6 Hospice .................................................................................................................................................. 8.9 Independent laboratory .......................................................................................................................... 8.9 Lithotripsy centers ................................................................................................................................. 8.9 Skilled nursing facility ........................................................................................................................ 8.10 7/1/2014 8.i Billing & Reimbursement for Ancillary Services Hospital Manual 8 Overview The purpose of this section is to describe the specific billing and Preapproval requirements for services rendered by ancillary facility and ancillary professional Providers and to supplement the General Information and Administrative Procedures sections. Many of the services in this section of the manual require Preapproval. A list of current Preapproval requirements by product is available online at www.ibx.com/preapproval. These requirements vary by benefits plan and are subject to change. Any additional requirements specific to a certain type of service are listed under that service category. General billing guidelines Electronic billing (837P or 837I) National Association of Insurance Commissioners (NAIC) codes All claims submitted electronically must be submitted with the NAIC codes for the line of business identification. Please view the appropriate payer ID document at www.ibx.com/edi for a complete list of the NAIC-assigned codes. When billing electronically, claims may be submitted through a vendor that you are contracted with or directly to Independence Blue Cross (IBC) through your own computer system. Claims are submitted in batches and may be sent daily or weekly, depending on your claims volume. Once claims are submitted through Electronic Data Interchange (EDI), you will receive a Functional Acknowledgement (FA) report/U277 from your contracting vendor or directly from IBC. The FA/U277 will identify those claims that were accepted for processing, as well as those that could not be forwarded for processing and the corresponding reason. For electronic submission instructions, please refer to the appropriate Companion Guide at www.ibx.com/ ediforms. If your facility is not operational on EDI for all products, please contact the EDI support group at 215-241-2305. Paper billing If you must submit a claim on paper, you will need to use the CMS-1500 or UB-04 form, as specified in the remainder of this section based on the type of service you provide. Billing guidelines by type of service Ambulance services Preapproval requirements Preapproval is required for all non-emergent ambulance transport, except for transport from one acute-care setting to another (billed with HH modifier). Transfers from a medical facility to a mental health facility by ambulance must be Preapproved by Magellan Behavioral Health, Inc., an independent company. Billing information Participating ambulance Providers must submit claims using the 837P (electronic) or CMS-1500 form (paper). Please also note the following billing requirements specific to ambulance Participating Providers: The National Provider Identifier (NPI) assigned to your organization must appear on every claim. 7/1/2014 8.1 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Only those services specified in your Agreement will be reimbursed. Ambulance Providers must include ZIP code information on all ambulance service claims: – Electronic claims. If you bill electronically via HIPAA 5010, please include both the pick-up and drop-off ZIP codes in the appropriate fields. – Paper claims. If you bill claims on paper, please include the pick-up ZIP code in box 23 of the CMS-1500 form. The ZIP code is the only data element that should be included in that field. Ambulatory surgical center services Preapproval requirements Preapproval is based on the HCPCS and/or CPT® codes for the planned procedure. If there is a change to the planned procedure, the HCPCS and/or CPT codes on the claim may be different from the code originally reported. Assuming the codes are reasonably related, this is not a barrier for payment. Significant discrepancies may be questioned prior to payment. Billing information Participating ambulatory surgical centers (ASC) must submit claims using the 837I (electronic) or UB-04 form (paper). Please also note the following billing requirements specific to ASCs: The NPI assigned to your organization must appear on every claim in field locator 56. Preapproval authorization numbers, if applicable, should appear in field locator 63. To expedite processing, do not submit claims until all charges are identified and included on the claim. The correct bill type, 83X, must be used. If the bill type does not correspond with your Provider type, the claim will be rejected and returned to you. A “no-pay” bill must also be sent to the fiscal intermediary for Keystone 65 HMO or Personal Choice 65SM PPO Members. Inclusions and exclusions ASC Surgery Fee Schedule reimbursements are made on a per-service basis only for those services included on the fee schedule, unless listed separately on the fee schedule. Sequencing Claims with multiple surgical procedures are processed in the order in which they appear on the claim. Be sure to bill the procedure with the highest allowable (primary) procedure first. IBC does not reorder the claim lines; however, some clearinghouses use software that changes the order, thus affecting the processing by IBC. Payment for multiple surgical procedures When multiple surgical procedures are performed during the same date of service, the highest allowable (primary) procedure is paid at 100 percent of the fee schedule rate, and the remaining procedures are paid at 50 percent of the fee schedule rate. 7/1/2014 8.2 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Revenue codes ASCs should use the following revenue codes for surgery claims: 0360, 0361, or 0490. The same revenue code should be used for each procedure. When Providers bill with different revenue codes, there is no additional reimbursement. Examples: Revenue code CPT 0360 ® Status Percent 23410 Highest allowable (primary) 100% 0360 36530 Second highest allowable 50% 0360 11402 Second highest allowable 50% Revenue code CPT Status Percent 0490 67105 Highest allowable (primary) 100% 0360 67105 No reimbursement – Charges for procedures All billed procedures must have corresponding charges. IBC cannot accept procedures with a $0.00 charge. If your system rolls up all charges to the first procedure, be sure to drop down a nominal (e.g., $1.00) amount to the other procedures. Example: Revenue code CPT Charges Status Percent 0490 36530 $1810.00 Highest allowable (primary) 100% 0490 11402 $1.00 Second highest allowable 50% Incidental procedures When multiple procedures are billed, no additional payment is made for procedures that are considered incidental to the highest allowable (primary) procedure. The Member may not be balance-billed for incidental procedures (IP). IPs are marked with an “IP” on the ASC Surgery Fee Schedule. Payment for an IP is made when that procedure is the only one performed or when it is the highest allowable (primary) procedure for the episode of care. When multiple procedures are performed and all are incidental, only the IP that is the highest allowable (primary) procedure is reimbursed. Example: Revenue code CPT Incidental Status Percent 0360 29877 IP Highest Allowable (Primary) 100% 0360 29880 IP Second highest allowable 0360 11402 0360 58120 Second highest allowable IP 50% Second highest allowable Note: Updates are made periodically to the ASC Surgery Fee Schedule. 7/1/2014 8.3 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Birthing centers Participating birthing centers must submit claims using the 837I (electronic) or UB-04 form (paper). Please also note the following billing requirements specific to birthing centers: The NPI assigned to your organization must appear on every claim in field locator 56. To expedite processing, do not submit claims until all charges are identified and included on the claim. A charge amount must appear in the total charge field for each line item. Lines with zero dollar charges will not be accepted. The amount billed must be greater than zero. The correct bill type, 84X, must be used. If the bill type does not correspond with your Provider type, the claim will be rejected and returned. Dialysis centers Billing information Participating dialysis centers must submit claims using the 837I (electronic) or UB-04 form (paper). Please also note the following billing requirements specific to dialysis centers: The NPI assigned to your organization must appear on every claim in field locator 56. To expedite processing, do not submit claims until all charges are identified and included on the claim. The correct bill type, 72X, must be used. If the bill type does not correspond with your Participating Provider type, the claim will be rejected and returned to you. A charge amount must appear in the total charge field for each line item. Lines with zero dollar charges will not be accepted. The amount billed must be greater than zero. All bills must be submitted on a monthly basis. Referrals for HMO Members are not required. In order to ensure correct claim payment, please use the following revenue codes when billing for services rendered in accordance with your Agreement: Revenue code (UB-04 field locator 42) UB-04 description (field locator 43) 0821 Hemodialysis 0825 Hemodialysis with training 0829 Home dialysis training and treatment 0831 Peritoneal dialysis 0835 Peritoneal dialysis with training 0841 CAPD dialysis 0845 CAPD dialysis with training 0851 CCPD dialysis 0855 CCPD dialysis with training Billing procedures The following requirements for submitting claims to IBC for renal dialysis services are based on Medicare’s billing instructions (National Uniform Billing Committee/HCFA). In order for your claims to be accepted and processed by IBC, the billing requirements defined below must be used. 7/1/2014 8.4 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Note: Follow the coding guidelines in the current UB-04 and ICD-9-CM/CPT manuals when reporting all services. HCPCS/CPT codes: HCPCS/CPT codes are required when reporting services in the following series of revenue codes: 30X 31X 32X 73X 92X 82X 3X 84X 85X 636 Notice of Medicare coverage Upon enrollment of any IBC Member, participating dialysis centers must submit to IBC a copy of the Medicare HCFA-2728 form that is sent to the Renal Networks. These forms are needed to facilitate our Member reconciliation efforts with the Centers for Medicare & Medicaid Services (CMS) and to ensure appropriate coordination of benefits. Please submit forms for IBC Members covered under all products referenced in this manual to: Independence Blue Cross 27th floor 1901 Market Street Philadelphia, PA 19103-1480 Please refer to the General Information section of this manual for claims information. Durable medical equipment Preapproval requirements Purchased durable medical equipment (DME): Preapproval is required for purchased DME costing $500 or more per line item (except diabetic supplies, unit dose medications for nebulizers, and ostomy supplies). Rental DME: Preapproval is required for all DME rentals (with the exception of oxygen), regardless of price. Preapproval is required for the repair and/or replacement of DME and prosthetic devices. Billing information Participating DME Providers must submit claims using the 837P (electronic) or CMS-1500 form (paper). Please also note the following billing requirements specific to DME Providers: The NPI assigned to your organization must appear on every claim. The “from” and “to” dates of care must be provided. A Certificate of Medical Necessity is not required for billing but must be kept on file with the patient’s chart to be made available upon request. The claim form must show a written description for any miscellaneous billed service that has not been defined or priced. Note: Subject to state-specific mandates. 7/1/2014 8.5 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Home health All home health services, unless noted otherwise, require timely Preapproval. Participating home health Providers must submit claims using the 837I (electronic) or UB-04 form (paper). Please also note the following billing requirements specific to Participating home health Providers: Whether you bill via EDI or on paper, you must complete those fields that are identified as required on the UB-04 Data Field Requirements. The NPI assigned to your organization must appear on every claim in field locator 56. The reported service dates must fall within the reported “statement from” and “statement through” dates. The revenue codes listed in this section should be used to bill home health services. The correct bill type, 32X, must be used. If the bill type does not correspond with your Participating Provider type, the claim will be rejected and returned to you. Be sure that all the required form fields are completed. Be sure that all the Member information is correct (e.g., date of birth, relation-to-insured code). COVERED SERVICES Revenue code Description 0421 Physical therapy, visit charge 0431 Occupational therapy, visit charge 0441 Speech therapy, visit charge 0551 Skilled nursing, visit charge 0561 Medical social worker, visit charge 0571 Home health aide (hourly rate) 0590 Nutrition consultation, visit charge – benefit only for Managed Care benefit programs; not for Traditional (Indemnity) IBC. Mother’s Option® Please note the following requirements specific to claims for Mother’s Option: The NPI assigned to your organization must appear on every claim in field locator 56. Preapproval is not required for the Mother’s Option well-mom/baby home care visit, provided that the visit(s) comply with the Mother’s Option guidelines. The claim should be billed with the mother as the patient, never the baby. If additional visits for the baby are needed, Preapproval should be obtained and the service should be billed under your home health Participating Provider number. Timely Preapproval is required for all phototherapy services. A separate authorization should be obtained for the skilled nursing visit and for the rental of the Wallaby® blanket. Phototherapy claims must always be billed with the baby as the patient. The revenue codes listed in this section should be used to bill Mother’s Option services. The reported service dates must fall within the reported “statement from” and “statement through” dates. The correct bill type, 32X, must be used. If the bill type does not correspond with your Participating Provider type, the claim will be rejected and returned to you. 7/1/2014 8.6 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Be sure that all the required fields are filled in. Be sure that all the Member information is correct (e.g., date of birth, relation-to-insured code). For more information, please see the Care Management and Coordination section of this manual. Note: Self-funded groups are not required to follow any state mandates, including Pennsylvania Act-85. Please verify that a baby has been added to a policy prior to billing phototherapy or standard home care services. MOTHER’S OPTION ® Revenue code Description 0551 Well-mom/baby, visit charge 0291 Phototherapy (Wallaby rental), daily charge COVERED DIAGNOSES Diagnosis code When reporting service V24.2, 650 Well-mom/baby visit 774.6 Phototherapy (Wallaby rental) Perinatal/Baby BluePrints® Please note the following requirements specific to claims for Mother’s Option: The NPI assigned to your organization must appear on every claim in field locator 56. The reported service dates must fall within the reported “statement from” and “statement through” dates. The revenue codes listed in this section should be used to bill perinatal services. The correct bill type, 32X, must be used. If the bill type does not correspond with your Provider type, the claim will be rejected and returned to you. Be sure that all the required form fields are completed. Be sure that all the Member information is correct (e.g., date of birth, relation-to-insured code). COVERED SERVICES Revenue code Description 0551 Skilled nursing, visit charge 0561 Medical social worker, visit charge 0571 Home health aide, hourly charge 0589 Fetal non-stress test, visit charge 0590 Nutrition consultation, visit charge 7/1/2014 8.7 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Home infusion therapy Participating home infusion Providers must submit claims using the 837P (electronic) or CMS-1500 form (paper). Please also note the following billing requirements specific to home infusion Providers: Claims must be submitted biweekly or monthly. The NPI assigned to your organization must appear on every claim. The start and end dates of care must be provided. Only those services specified in your Agreement will be reimbursed. When more than one antibiotic therapy is administered, it must be reported with the correct approval number assigned for each therapy. When reporting hydration therapy, only one rate shall be reimbursable on a per-day basis, regardless of volume used. The line maintenance services are reported only when a Member is not receiving active therapy. National Drug Code (NDC) numbers are used for determining the average wholesale price (AWP) of the drug component. The AWP is determined using First DataBank pricing. When billing for a drug used in conjunction with infusion therapy, you must use the NDC number of the dispensed drug and the number of units dispensed. Each NDC number must appear on a separate line of the claim form. All drug claims will require the submission of an accompanying 11-digit NDC. This includes claims for hemophilia Factor products that are currently submitted with specific J codes. The NDC must be submitted using the 5-4-2 format when billing with hyphens (e.g., 12345-1234-12). NDC numbers without hyphens (12345678911) will also be accepted. Please do not include spaces, decimals, or other characters in the 11-digit string, or the claim will be returned for correction prior to processing. Private duty nursing Private duty nursing (PDN) is defined as medically appropriate, complex skilled nursing care in the individual’s private residence by a registered nurse or a licensed practical (vocational) nurse. The purpose of PDN is to provide continuous monitoring and observation of a Member who requires frequent skilled nursing care on an hourly basis. In addition, PDN may assist in the transition of care from a more acute setting to home and teaches competent caregivers the assumption of this care when the condition of the Member is stabilized. Please review the medical policy, which is available at www.ibx.com/medpolicy, for more information about Medical Necessity requirements and how PDN differs from a skilled nursing visit. Participating PDN Providers must submit claims using the 837P (electronic) or CMS-1500 form (paper). Please also note the following billing requirements specific to PDN Providers: The NPI assigned to your organization must appear on every claim. The procedure codes listed in this section must be used in order to ensure proper claims payment. Since Preapproval is required for the reported service, please complete field locator number 23 on the CMS-1500 form. COVERED SERVICES Procedure code Description S9123 Registered nurse, per hour S9124 Licensed practical nurse, per hour 7/1/2014 8.8 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Hospice Preapproval requirements All inpatient hospice services require timely Preapproval; however, there is no Preapproval requirement for home hospice services (revenue code 0651). Billing information Participating hospice Providers must submit claims using the 837I (electronic) or UB-04 form (paper). Please also note the following billing requirements specific to hospice Providers: The NPI assigned to your organization must appear on every claim in field locator 56. The reported service dates must fall within the reported “statement from” and “statement through” dates. The revenue codes listed in this section should be used to bill hospice services. The correct bill type, 81X, must be used. If the bill type does not correspond with your Provider type, the claim will be rejected and returned to you. Be sure that all the required form fields are completed. Be sure that all Member information is correct (e.g., date of birth, relation-to-insured code). COVERED SERVICES Revenue code Description 0651 Home hospice care, visit charge 0652 Continuous care home hospice (per hour) 0655 Respite care hospice (per day) 0656 Inpatient hospice care (per day) Independent laboratory Participating independent laboratory Providers must submit claims using the 837P (electronic) or CMS1500 form (paper). Please also note the following billing requirements specific to independent laboratory Participating Providers: The NPI assigned to your organization must appear on every claim. Only those service codes specified in your Agreement will be reimbursed. Lithotripsy centers Participating lithotripsy centers must submit claims using the 837I (electronic) or UB-04 form (paper). Please also note the following billing requirements specific to lithotripsy centers: The NPI assigned to your organization must appear on every claim in field locator 56. The reported service dates must fall within the reported “statement from” and “statement through” dates. The correct revenue code assigned by IBC (0790) must be reported in order to ensure proper claim payment. The correct bill type, 83X, must be used. If the bill type does not correspond with your Provider type, the claim will be rejected and returned to you. 7/1/2014 8.9 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Skilled nursing facility Billing information Participating skilled nursing facilities (SNF) must submit claims using the 837I (electronic) or UB-04 form (paper). Please also note the following billing requirements specific to SNFs: Preapproval numbers, when applicable, should appear in box 63 The NPI assigned to your organization must appear on every claim in field locator 56. To expedite processing, do not submit claims until all charges are identified and included on the claim. A charge amount must appear in the total charge field for each line item. Lines with zero dollar charges will not be accepted. The amount billed must be greater than zero. Miscellaneous HCPCS/CPT codes (codes ending in “99”) are not acceptable. In order to assure correct claims payment, utilize the following revenue codes when billing for services rendered: Revenue code Description 0121 Days after Medicare/65 Special 0130, 0150 Basic SNF – Freestanding or hospital-based 0120, 0191 Subacute medical 0129, 0199 Subacute medical – high-cost IV drug* 0118, 0128, 0190, 0192 Subacute rehab 0206, 0193 Ventilator dependent-chronic care 0200, 0194 Ventilator dependent-active weaning *High-cost IV drug is when the cost of the drug is greater than $100 AWP. Managed care products The facility’s per diem rate is all-inclusive for Members at a skilled or subacute level of care. Facilities are responsible for paying any subcontracted Provider who furnishes ancillary services to inpatient Members. This includes, but is not limited to, the following: routine diagnostic lab tests and processing venipuncture DME (except for those items set forth under the exceptions noted below) enteral feedings medical/surgical supplies parenteral hydration therapy pharmaceuticals, including IV therapies physical, occupational and/or speech therapy, including supplies to support these services routine radiology services performed onsite at the SNF The services itemized below should be Preapproved by an IBC-Participating Provider who will bill and be reimbursed directly for the service. 7/1/2014 8.10 Billing & Reimbursement for Ancillary Services Hospital Manual 8 The following items are excluded under the per diem rates. DME: – customized orthotics/prosthetics – low air loss specialty beds/mattresses and Clinitron/air fluidized beds consistent with CMS Group II and III requirements – bariatric beds – wound vac devices and supplies Other services: – Physician services – MRIs, CAT scans, Doppler studies – emergent transportation – dialysis services – blood and blood products Referrals for HMO Members in long-term care/custodial-care nursing homes A Referral is required for ancillary services or for consultation with a specialist for Members residing in long-term care (LTC) or nursing homes. In such cases, Preapproval is not required. We have established LTC panels for our PCPs who provide care in LTC participating facilities. The LTC panels do not have designated ancillary services (e.g., laboratory, physical therapy, radiology, or podiatry). The completion of a Referral is required for any ancillary service for an LTC panel Member. In addition, a Referral is required for any specialist Physician consultation and/or follow-up for an LTC panel Member. LTC panel PCPs must issue Referrals for any professional service or consultation for an LTC panel custodial nursing home Member. Examples of services that required Referrals include specialist, podiatry, physical therapy, and radiology. Participating Providers should submit Referrals in advance of the service being provided using the NaviNet® web portal or the Provider Automated System. Consultants and ancillary Participating Providers are encouraged to provide Referral information with the claim to assist in processing. Preapproval is required only for inpatient admission for hospital care, SNF care, short procedure unit cases, or outpatient surgi-center procedures. During an approved skilled nursing care admission, it is not necessary for the attending Physician to issue a Referral. All Participating Providers giving care to the Member should use our inpatient skilled nursing care authorization number for claims during dates of service within the skilled nursing inpatient stay. Note: Certain products have specialized Referral and Preapproval requirements and/or benefits exemptions. Podiatry services for HMO members only in SNFs The HMO podiatric benefit is intended to cover services required to treat significant structural and/or inflammatory pathologic conditions of the foot — not to provide routine foot care to all Members. Routine foot care is a covered benefit only for Members with diabetes or peripheral vascular disease. The SNF Preapproval will allow claims to pay to any HMO network podiatrist who treats a Member receiving skilled or subacute care. If special circumstances require the use of a podiatrist outside of the HMO network, the PCP must contact the Care Management and Coordination department for Preapproval. 7/1/2014 8.11 Billing & Reimbursement for Ancillary Services Hospital Manual 8 Part B therapy services SNFs that provide outpatient physical, occupational, or speech therapy services will be reimbursed separately only for Medicare Advantage HMO and PPO Members who reside at the facility at a custodial level of care. 7/1/2014 8.12 Care Management and Coordination Hospital Manual 9 Table of Contents Overview .................................................................................................................................9.1 Utilization review process and criteria .................................................................................9.1 Utilization review overview .................................................................................................................. 9.1 Selective medical review ....................................................................................................................... 9.2 Post approval audit ................................................................................................................9.3 Delegation of utilization review activities and criteria .......................................................................... 9.3 Clinical criteria, guidelines, and resources ............................................................................................ 9.3 Important definitions .............................................................................................................9.5 “Medically Necessary” or “Medical Necessity”.................................................................................... 9.5 Experimental/investigational ................................................................................................................. 9.5 Preapproval/Precertification review .....................................................................................9.6 Certain surgical procedures ................................................................................................................... 9.7 Medications ........................................................................................................................................... 9.7 Admission review ..................................................................................................................9.8 Concurrent review .................................................................................................................9.9 Obstetrical admissions..........................................................................................................9.9 Penalties for lack of Preapproval/Precertification ...............................................................9.9 Retrospective review of inpatient stays ...............................................................................9.9 Retrospective review of outpatient services ......................................................................9.10 Nonemergency ambulance transport .................................................................................9.10 Discharge planning coordination .......................................................................................9.10 Termination of benefits .......................................................................................................9.11 Denial procedures ................................................................................................................9.11 Delays in service ..................................................................................................................9.12 Decreased levels of care (skilled/subacute vs. acute days) .............................................9.12 Member decision days .........................................................................................................9.12 Observation status...............................................................................................................9.12 Transfers within and between inpatient facilities ..............................................................9.13 Transfers within the same facility ....................................................................................................... 9.13 Transfers between facilities ................................................................................................................. 9.13 Reconsideration and hospital appeals processes.............................................................9.14 7/1/2014 9.i Care Management and Coordination Hospital Manual 9 Peer-to-Peer Reconsideration process ................................................................................................. 9.14 Appeals for lack of Medical Necessity ................................................................................................ 9.14 Appeals for cosmetic or experimental/investigational services........................................................... 9.15 ER services appeals ............................................................................................................................. 9.15 Outpatient payment disputes (except ER) ........................................................................................... 9.16 Timely submission of Medicare Advantage HMO and PPO Member’s medical records .9.16 Continuity-of-care ................................................................................................................9.17 Baby BluePrints® maternity program .................................................................................9.17 Postpartum program – Mother’s Option® ............................................................................................ 9.17 Baby BluePrints postpartum services .................................................................................................. 9.18 Preapproval/Precertification for home phototherapy........................................................................... 9.19 7/1/2014 9.ii Care Management and Coordination Hospital Manual 9 Overview The Care Management and Coordination (CMC) department is comprised of health care professionals whose objective is to support and facilitate the delivery of quality health care services to our Members. This is accomplished through several activities, including Preapproval/Precertification of elective health care services, medical review, facilitation of discharge plans, and case management. All capitalized terms in this section shall have the meaning set forth in either your Provider Agreement or the Member’s benefits plan, as applicable. Utilization review process and criteria Utilization review overview Utilization review is the process of determining whether a given service is eligible for coverage or claim payment under the terms of a Member’s benefits plan and/or a network Provider’s contract. In order for a health care service to be covered or payable, it must 1) be listed as included in the benefits plan, 2) be Medically Necessary, and 3) not be specifically excluded from coverage. The vast majority of IBC benefits plans exclude coverage for services considered experimental/investigational and those considered primarily cosmetic in nature. To assist us in making coverage determinations for certain requested health care services, we apply established IBC medical policies and medical guidelines based on clinical evidence to determine the Medical Necessity of the requested services and the appropriate setting (e.g., office, inpatient, outpatient) for Covered Services requested by a Member’s health care Provider. When a Covered Service can be administered in various settings, Providers should request Preapproval/Precertification, as required by the applicable benefits plan, to provide the Covered Services in the most appropriate and cost-effective setting for the Member’s current medical needs and condition. IBC’s Preapproval/Precertificationreview will be based on the clinical documentation from the requesting health care Provider. It is not practical to verify Medical Necessity for all Covered Services. Therefore, certain procedures may be automatically approved by IBC, based on the following: the generally accepted Medical Necessity of the procedure itself; the diagnosis reported; an agreement with the Provider performing the procedure. For example, certain services provided in an emergency room (ER) are automatically approved by IBC. The approval is based on the procedure having met Emergency criteria, including the severity of the diagnosis reported (e.g., rule out myocardial infarction or major trauma). Other requested services, such as certain elective inpatient or outpatient services, may be reviewed on a case-by-case basis where the specific procedure and setting are considered. Utilization reviews generally are categorized based on the timing of the review and the service for which a determination is requested. Preapproval/Precertification review. When a review is required before a service is performed, it is a Preapproval/Precertification review. Admission review. Initial review of the Medical Necessity of an Emergency admission. Concurrent review. Reviews occurring during a hospital stay or when services are already being provided are concurrent reviews. 7/1/2014 9.1 Care Management and Coordination Hospital Manual 9 Retrospective/Post-service review. Those reviews occurring after services have been performed are either retrospective or post-service reviews. IBC follows applicable State and federal standards for the time frames in which such reviews are to be performed and for when coverage or payment determinations are issued and communicated. Pennsylvania law requires that initial preservice, concurrent, and retrospective utilization review (UR) decisions of managed care plans be communicated verbally and confirmed in writing to the enrollee and the requesting health care Provider within specific time frames. We ask that our Participating Providers inform Members of our initial UR decisions upon their receipt of the communication from IBC. Providers should document that they provided this verbal notification. IBC provides written notification of determinations to Providers and Members within the required time frames. Note: For retrospective determinations, in situations where the Member is held harmless from financial responsibility for the service, Providers are not required to notify the Member in this way. Generally, when a requested service requires utilization review to determine Medical Necessity, nurses perform the initial case review and evaluation for coverage approval. Only an IBC Medical Director may deny coverage for a procedure based on Medical Necessity. The nurses review applicable policies and procedures in the benefits plan, taking into consideration the individual Member’s condition and applying sound professional judgment. Evidence-based clinical protocols are applied to specific procedures. When the clinical criteria are not met, the service request is referred to an IBC Medical Director for further review and coverage or payment determination. Independent medical consultants, who are board certified in the relevant medical specialty as required by the particular case under review, may also be engaged to conduct a clinical review. If coverage for a service is denied based on lack of Medical Necessity, written notification is sent to the requesting Provider and Member notifying them of the denial and their due process appeal rights in accordance with applicable law. IBC’s utilization review program encourages peer-to-peer discussion regarding coverage decisions based on Medical Necessity by giving Physicians direct access to IBC Medical Directors to discuss coverage determinations. The nurses, IBC Medical Directors, other professional Providers, and independent medical consultants who perform utilization review services are not compensated or given incentives based on their coverage review decisions. It is our policy that all utilization review decisions are based on the appropriateness of health care services and supplies, in accordance with the benefits available under the Member’s coverage, our definition of Medical Necessity, and applicable medical policies. IBC Medical Directors and nurses are salaried; contracted external Physicians and other professional consultants are compensated on the basis of the number of cases reviewed, regardless of the coverage determination. There are no financial incentives that would encourage utilization review decisions that result in under-utilization. Selective medical review In addition to the foregoing requirement, IBC reserves the right, under our Utilization and Quality Management Programs, to perform a medical review prior to, during, or following the performance of certain Covered Services (selective medical review) that are otherwise not subject to reviews as previously described. In addition, we reserve the right to waive medical review for certain Covered Services for certain Providers, if we determine that those Providers have an established record of meeting the utilization and/or quality management standards for these Covered Services. 7/1/2014 9.2 Care Management and Coordination Hospital Manual 9 Providers are notified in advance when we are planning on performing selective medical review, Members may not be penalized when required selective medical review results in a determination that a service is not Medically Necessary. Post approval audit IBC reserves the right to perform an audit of medical records for services that have been approved and claims were adjudicated, to assure that information given at the time of the utilization review was accurate. This audit may be delegated to an external medical review company Hospitals will be notified in advance of these audits, and will be asked to submit medical records. If a discrepancy is found between the medical record and the information provided at the time of the initial medical review, inpatient reimbursement may be retracted and hospitals may bill for appropriate outpatient charges such as observation. Hospitals may appeal these determinations based on instructions provided at time of the adverse decision. Delegation of utilization review activities and criteria In certain instances, IBC has delegated utilization review activities to entities with an expertise in medical management of a specific membership population (such as neonates/premature infants) or type of benefits (such as mental health/substance abuse). A formal delegation and oversight process is established in accordance with applicable law and with nationally recognized utilization review and quality assurance accreditation body standards. In such cases, the delegate’s utilization review criteria are generally adopted by IBC for use by the delegated entity. Self-insured plans In addition to the above, self-insured plans and/or Payors may delegate utilization review and criteria activities to third parties with expertise, with respect to their members and in accordance with the terms of the self-funded or Payors benefit program agreement with IBC. Clinical criteria, guidelines, and resources The following guidelines, clinical criteria, and other resources are used to help make Medical Necessity and appropriateness coverage decisions: InterQual®. The InterQual clinical decision-support criteria model is based on the evaluation of intensity of service and severity of illness. Covered Services for which InterQual criteria may be applied include, but are not limited to, the following: – inpatient hospitalizations – inpatient rehabilitation – long-term, acute care facility admissions – observation – skilled nursing facility (SNF) – some elective-surgery settings for inpatient and outpatient procedures – home health care In addition, we apply acute-care guidelines for Emergency admissions. Admissions that do not meet acute intensity of services and severity of illness guidelines are reviewed by an IBC Medical Director, and coverage or payment is denied if guidelines are not met. Observation services do not require Preapproval/Precertification but are subject, at IBC’s discretion, to InterQual criteria for Medical Necessity, which requires that the treatment and/or procedures include at least six hours of observation. 7/1/2014 9.3 Care Management and Coordination Hospital Manual 9 Note that medical records may be required to complete a review to determine coverage or payment in many situations including, but not limited to, a Medical Necessity review or cosmetic review. When submitting a written request for utilization review, be sure to attach the request letter to the medical records, and submit records as instructed. Electronic versions of medical records are acceptable and encouraged. Medical records that arrive attached to a request letter require less research and are forwarded to the appropriate team for review. We may conduct focused evaluations of the Medical Necessity requests for the use of an inpatient setting for certain elective surgical procedures. Examples include, but are not limited to, cardiac catheterizations, laproscopic cholecystectomies, tonsillectomies, adenoidectomies, hernia repairs, and battery and generator changes. Providers must submit clinical documentation when it is believed that the outpatient setting would not be appropriate and inpatient admission is necessary. Procedures performed during Emergency admissions must also meet guidelines from InterQual regarding acute admission. Centers for Medicare & Medicaid Services (CMS) guidelines. CMS adopts and publishes a set of guidelines for coverage of services by Medicare (for Medicare Advantage HMO and PPO Members). CMS guidelines are also used to help determine coverage for durable medical equipment (DME) services for all products. CMS and InterQual guidelines consider elective diagnostic coronary angiography and percutaneous coronary intervention (i.e., balloon angioplasty, brachytherapy, and stents) as outpatient procedures, unless the Provider submits clinical documentation that inpatient admission is required. Such documentation should include the presence of major cormorbidities, altered physiologic status, and/or the need for intensive monitoring for at least 24 hours following the procedure. IBC medical policies. IBC internally develops a set of policies that document the coverage and conditions for certain medical/surgical procedures and ancillary services that are considered Medically Necessary. IBC medical policies may be applicable for Covered Services including, but not limited to, the following: – DME – infusion therapy, including certain chemotherapy agents – nonemergency ambulance transports – review of potential cosmetic procedures and obesity surgery – review of potential experimental or investigational services – speech therapy Non-certification decisions. The criteria used to make non-certification decisions is stated in the letters to the Members and Providers, along with instructions on how to request specific guidelines. Providers may request the specific guidelines or criteria used to make specific utilization management determinations by faxing a request to 215-761-9529 or submitting a request to: Request for InterQual Criteria Care Management and Coordination Department 1901 Market Street, 30th Floor Philadelphia, PA 19103 7/1/2014 9.4 Care Management and Coordination Hospital Manual 9 Important definitions “Medically Necessary” or “Medical Necessity” “Medically Necessary” or “Medical Necessity” shall mean health care services that a Physician, exercising prudent clinical judgment, would provide to a patient for the purpose of preventing, evaluating, diagnosing, or treating an illness, injury, or disease of its symptoms, and that are: (a) in accordance with generally accepted standards of medical practice; (b) clinically appropriate, in terms of type, frequency, extent, site, and duration, and considered effective for the patient’s illness, injury, or disease; and (c) not primarily for the convenience of the patient, Physician, or other health care Provider, and not more costly than an alternative service or sequence of services at least as likely to produce equivalent therapeutic or diagnostic results as to the diagnosis or treatment of that patient’s illness, injury, or disease. For these purposes, “generally accepted standards of medical practice” means standards that are based on credible scientific evidence published in peer-reviewed medical literature generally recognized by the relevant medical community, Physician Specialty Society recommendations, and the views of Physicians practicing in relevant clinical areas and any other relevant factor. Experimental/investigational Experimental/investigational services: A drug, biological product, device, medical treatment, or procedure that meets any of the following criteria: is the subject of ongoing phase I or phase II clinical trials; is the research, experimental study, or investigational arm of ongoing phase III clinical trials, or is otherwise under a systematic, intensive investigation to determine its maximum tolerated dose, toxicity, safety, efficacy, or efficacy compared with a standard means of treatment or diagnosis; is not of proven benefit for the particular diagnosis or treatment of the covered person’s particular condition; is not generally recognized by the medical community, as clearly demonstrated by Reliable Evidence*, as effective and appropriate for the particular diagnosis or treatment of a covered person’s particular condition; is generally recognized by either the Reliable Evidence* or the medical community that additional study on its safety and efficacy for the particular diagnosis or treatment of a covered person’s particular condition is recommended. A drug is not considered experimental/investigational if it has received final approval by the U.S. Food and Drug Administration (FDA) to market for the particular diagnosis or condition. Any other approval granted as an interim step in the FDA regulatory process (e.g., an investigational new drug exemption — as defined by the FDA), is not sufficient. Once FDA approval has been granted for a particular diagnosis or condition, use of the drug for another diagnosis or condition shall require that one or more of the following established referenced compendia recognize the usage as appropriate medical treatment: American Hospital Formulary Service (AHFS) Drug Information U.S. Pharmacopeia (USP) – National Formulary Any drug that the FDA has determined to be contraindicated for the specific treatment for which the drug has been prescribed will be considered experimental/investigational. A biological product, device, medical and/or behavioral health treatment, or procedure is not considered experimental/investigational if it meets all of the Reliable Evidence* criteria listed below: 7/1/2014 9.5 Care Management and Coordination Hospital Manual 9 Reliable Evidence exists that the biological product, device, medical and/or behavioral health treatment, or procedure has a definite positive effect on health outcomes. Reliable Evidence exists that over time the biological product, device, medical and/or behavioral health treatment, or procedure leads to improvement in health outcomes (i.e., the beneficial effects outweigh any harmful effects). Reliable Evidence clearly demonstrates that the biological product, device, medical and/or behavioral health treatment, or procedure is at least as effective in improving health outcomes as established technology, or is usable in appropriate clinical contexts in which established technology is not employable. Reliable Evidence clearly demonstrates that improvement in health outcomes, as defined above, is possible in standard conditions of medical practice, outside clinical investigative settings. Reliable Evidence shows that the prevailing opinion among experts, regarding the biological product, device, medical and/or behavioral health treatment or procedure, is that studies or clinical trials have determined its maximum tolerated dose, its toxicity, its safety, its efficacy, or its efficacy as compared with a standard means of treatment for a particular diagnosis. *Reliable Evidence is defined as any of the following: Reports and articles in the authoritative medical and scientific literature; the written protocol used by the treating facility or the protocols of another facility studying substantially the same drug, biological product, device, medical and/or behavioral health treatment, or procedure; or the written, informed consent used by the treating facility or by another facility studying substantially the same drug, biological product, device, medical and/or behavioral health treatment, or procedure. Preapproval/Precertification review For services requiring Preapproval/Precertification, facilities are encouraged to contact IBC at least five business days prior to the scheduled date of the procedure to ensure documentation of timely Preapproval/Precertification. Preapproval/Precertification can be requested through the NaviNet® web portal or by calling the Provider Automated System* at 1-800-ASK-BLUE, Monday through Friday, 8 a.m. to 5 p.m. Providers with NaviNet access are expected to use NaviNet to initiate requests for Preapproval/Precertification. Providers may also obtain the status of an authorization through NaviNet. *As of November 1, 2013, and continuing through mid-2015, IBC is in the process of migrating its membership to a new operating platform. Once a Member has been migrated to the new platform, you will no longer be able to use the Provider Automated System for that Member. This includes all functionality, such as eligibility, claims status, and Preapproval/Precertification.. You must use NaviNet to perform these tasks. After business hours, a nurse is on call to assist with inquiries regarding urgent services and discharge planning needs or to help direct Members or Providers to appropriate settings. The after-hours on-call nurse can be reached by calling 1-800-ASK-BLUE. The CMC department will evaluate your request and will notify your office once a decision has been reached for those cases that require clinical review. You will be provided with a Preapproval/Precertification reference number based on the determination of your request. Failure to obtain Preapproval/Precertification may result in Provider penalties or denials of payment regardless of Medical Necessity. At the time of Preapproval/Precertification review, the following information will be requested: name, address, and phone number of Subscriber relationship to Subscriber name, address, and phone number of the Subscriber relationship to the Subscriber 7/1/2014 9.6 Care Management and Coordination Hospital Manual 9 Member ID number group number Physician name and phone number facility name diagnosis and planned procedure codes indications for admission: signs, symptoms, and results of diagnostic tests past treatment date of admission or service current functional level (SNF and rehabilitation only) estimated length of stay (SNF and rehabilitation only) short- and long-term goals (SNF and rehabilitation only) discharge plan (SNF and rehabilitation only) If the required Preapproval/Precertification is not requested and the Member is already admitted, the facility should contact IBC following admission by using NaviNet to initiate approval of the admission. If IBC approves the admission, the day of the admission review will be considered the first day of admission, and all prior inpatient days of the admission will be denied. Certain products have specialized Referral and Preapproval/Precertification requirements. Visit www.ibx.com/preapproval to view a list of current services and drugs, including without limitation infusion drugs, that require Preapproval/Precertification. Note: These requirements vary by benefits plan and are subject to change. Certain surgical procedures The following procedures are generally performed on an outpatient basis when elective, and not urgent or emergent: thyroidectomy — partial or total parathyroidectomy recurrent hernia temporomandibular joint (TMJ) arthroplasty and discectomy arthroscopy (shoulder, elbow, wrist) open reduction internal fixation of uncomplicated wrist or finger fractures We ask that Providers perform these procedures as outpatient; however, if you feel there are medical reasons that would justify an inpatient stay, IBC will review these upon request and approve the inpatient setting if medically appropriate. If we approve these procedures as inpatient and the patient goes home the same day, we will reimburse these procedures as outpatient. You may direct your review requests to the Precertification Department by calling 1-800-ASK-BLUE and saying Authorizations. Note: None of the procedures listed above require Preapproval/Precertification if performed in the outpatient setting. Medications For all drugs covered under the medical benefit that require Preapproval/Precertification, Providers will be required to report Member demographics, such as height and weight. 7/1/2014 9.7 Care Management and Coordination Hospital Manual 9 Certain drugs that require adherence to Dosing and Frequency Guidelines will be reviewed during Preapproval/Precertification. Dosing and Frequency Guidelines are included in the medical policies for such drugs, which are available at www.ibx.com/medpolicy. Dosing and Frequency Guidelines help IBC verify that our Members’ drug regimens are in accordance with national prescribing standards. These guidelines are based on current FDA approval, drug compendia (e.g., American Hospital Formulary Service Drug Information®, Micromedex®), industrystandard dosing templates, drug manufacturers’ guidelines, published peer-reviewed literature, and pharmacy and medical consultant review. Requests for coverage outside these guidelines require documentation (i.e., published peer-reviewed literature) to support the request. Note: Infusion drugs that are newly approved by the FDA during the term of a facility contract are considered new technology and will be subject to Preapproval/Precertification requirements, pending notification by IBC. Use NaviNet to verify individual Member benefits. Providers may submit authorization requests for services rendered by an infusion therapy Provider, a prosthetics Provider, or a DME Provider. Providers must submit authorization requests for services rendered by a home health Provider, including skilled nursing, physical therapy, speech therapy, occupational therapy, home health aide, social work, and dietitian. Admission review Admission review is the initial review of the circumstances surrounding an Emergency admission to determine whether coverage for inpatient services will be granted. The review examines the severity of the Member’s condition based on patient presentation and diagnostic study results, as well as the treatment provided, and whether the patient’s condition is such that it symptoms are unlikely to resolve within 24 hours. Admissions to rule out seriously acute conditions should be considered for observation level of care. Hospitals are required to notify IBC using NaviNet of all Emergency admissions within two business days of admission. Within two business days of notice, hospitals must provide clinical information to IBC, by which IBC will make a determination to approve the inpatient stay. Clinical information can be provided by phone, fax, or secure email. Failure to provide supporting clinical information after notice of admission will result in the claim remaining “pended.” No reimbursement will be made until clinical information is provided to IBC and medical review is completed. Upon review of all available information, the IBC care coordinator may determine that inpatient criteria are not met. A Medical Director will then review the clinical information and may authorize or deny the inpatient admission. A determination will be rendered within one business day of receipt of all clinical information. The status of admission review determinations can be found on NaviNet. Denial of inpatient admission is followed up with a letter describing the rationale for the denial and the Provider’s appeal rights. Under diagnosis related group (DRG) reimbursement, hospitals may be asked to provide IBC with requested clinical updates for Members who remain inpatient at the following checkpoints: 5 days, 10 days, 17 days, and weekly thereafter. The clinical updates will assist in making appropriate discharge planning arrangements and case management referrals. 7/1/2014 9.8 Care Management and Coordination Hospital Manual 9 Concurrent review Concurrent review is the review of continued stay in the hospital after an admission is determined to be Medically Necessary. Concurrent review is performed when reimbursement is based on a per-diem arrangement. After initial admission review, the hospital is required to initiate concurrent review on or before the last covered day. The information can be provided by phone, fax, or secure email and must include: current medical information for the days being reviewed treatment plan current progress on goals a discharge plan update If all pertinent information is provided and the days are Medically Necessary utilizing InterQual criteria, the approval will be verbally communicated to the hospital contact at the time of the review. If sufficient information is not available, the case will be pended until the necessary information is obtained from the hospital. If the IBC care coordinator is unable to approve additional days, the case will be referred to an IBC Medical Director for Physician review. The Medical Director will review all information and render a determination within one business day. Throughout the concurrent review process, the care coordinator is continually assessing the potential for discharge needs and communicating with the Physician and hospital Discharge Planning department to facilitate discharge as appropriate. Obstetrical admissions Preapproval/Precertification and notification of maternity admissions for routine deliveries is not required. However, obstetricians are encouraged to remind their IBC Members to self-enroll into the Baby BluePrints® prenatal care management program by calling 1-800-598-BABY. Penalties for lack of Preapproval/Precertification It is the network Provider’s responsibility to obtain Preapproval/Precertification for the services listed at www.ibx.com/preapproval. If Preapproval/Precertification is not obtained when required under the Member’s benefits, neither the Member nor IBC will be responsible for payment. Members are held harmless from financial penalties if the network Provider does not obtain prior approval. Retrospective review of inpatient stays Authorization is required for an inpatient stay; however, under limited circumstances and by request, the CMC team may extend review of a case after services have been provided in order to determine coverage or eligibility for payment. This retrospective (or post-service) review is not a guarantee of payment. These limited circumstances include: when a hospital/facility is unaware of a Member’s insurance coverage at the initiation of service. In this scenario, it is the responsibility of the hospital/facility to obtain authorization as soon as that information is obtained. if the hospital/facility discovers that a patient is an eligible IBC Member after he or she is discharged, but he or she was incorrectly classified under different insurance coverage. In this case, the hospital/facility must provide CMC with the admission “face sheet.” if the Member is discharged prior to medical review being completed. 7/1/2014 9.9 Care Management and Coordination Hospital Manual 9 If you are not certain whether authorization for an inpatient stay was obtained, please use NaviNet to verify the status of the authorization request prior to submitting a claim. To request a retrospective review, please adhere to the following processes: For Emergency admissions. If you find that notification of an Emergency admission was not given by the hospital to CMC, you can request a retrospective review through NaviNet for up to a year after the date of service. To do so, select ER Admission Notification from the Authorizations option in the Plan Transactions menu. For elective admissions. If you find that authorization was not obtained for an elective admission, you can initiate a review by calling 1-800-ASK-BLUE Monday through Friday, 8 a.m. to 6 p.m., and following the voice prompts. Note: Please do not send paper copies of the Member’s complete medical record for an admission where authorization was not previously obtained. Medical records only need to be submitted in select cases and upon request. Once our CMC team has been notified of the request for retrospective review, we will contact the hospital/facility to request clinical information. In the case of hospitals/facilities for which we have remote access to medical records, we will attempt to obtain the clinical information on our own. Review of the case and notification of the determination will be made no later than 30 days from when we receive all supporting information that is necessary to perform the review. If the hospital/facility fails to supply clinical information for retrospective review, we may issue an administrative denial for payment. Please also note the following: We will base our determination of Medical Necessity on the information that was available to the hospital/facility at the time of admission. The hospital/facility may not bill a Member for services that are determined not to be Medically Necessary during the retrospective review process. Retrospective review of outpatient services Similar to the circumstances regarding the retrospective review of inpatient stays, CMC may extend review of outpatient care that had required Preapproval/Precertification after services were provided in order to determine coverage or eligibility for payment. Please refer to the previous section for information about when this applies and the process to be followed. Nonemergency ambulance transport Nonemergency medical ambulance transport services require Preapproval/Precertification when such a transport meets all of the following criteria: It is a benefit as outlined in the Member contract. It is a means to obtain covered treatment or services. It meets medical policy associated with transport origin, destination, and Medical Necessity. Visit www.ibx.com/medpolicy to view our Nonemergency Ambulance Transport Services policy. Discharge planning coordination Discharge planning is the process by which IBC care coordinators, after consultation with the Member, his or her family, the treating Physician, and the hospital care manager, do the following: 7/1/2014 9.10 Care Management and Coordination Hospital Manual 9 assess the Member’s anticipated post-discharge problems and needs; assist with creating a plan to address those needs; coordinate the delivery of Member care. Discharge planning may occur by telephone or onsite at the hospital. All requests for placement in an alternative level of care setting/facility (such as acute or subacute rehab or SNF) will be reviewed for Medical Necessity. Hospitals must provide the requested information to CMC to determine whether placement is appropriate according to InterQual guidelines. When appropriate, alternative services (such as home health care and outpatient physical therapy) will be discussed with the Member or his or her family, the attending Physician, and the hospital discharge planner or social worker. Once alternative placement is authorized, the approval letter is sent to the Member, the hospital, and the attending Physician. If the request does not meet the criteria, the case is referred to an IBC Medical Director for review and determination. Termination of benefits Termination of benefits (TOB) may occur when a Member chooses to remain in the hospital following a determination that inpatient acute care is no longer Medically Necessary in that setting. Upon TOB, the Member is financially responsible for care received following the administration of the TOB notice. The following criteria define the circumstances under which IBC considers TOB to be appropriate. The patient must meet discharge criteria in all circumstances. The attending Physician orders a discharge or documents that the Member is no longer at acute hospital level of care, but the Member or responsible party refuses available alternative settings. The Member or responsible party has refused to cooperate with discharge planning. The Member or responsible party has shown continued noncompliance with the hospital plan of care. Members may not be held financially responsible for denials unless the above criteria are met. Disagreements with determinations made by IBC are to be resolved through the Hospital Provider Appeals Process. Denial procedures All cases that do not satisfy the relevant Medical Necessity criteria are referred to and reviewed by an IBC Medical Director for a determination. If the service is determined to be covered, IBC staff will inform the Provider who submitted the request. If the Medical Director determines that the information provided by the attending Physician is insufficient to determine Medical Necessity, the case will be pended until the required information is received. The attending Physician will be notified as soon as possible, but not more than 24 hours later, of the specific additional information required. Written confirmation of the request for additional information will be sent within two business days to the hospital, Member, and vendor, as appropriate. If the request involves urgent care, the hospital, Member, and/or vendor, will have two calendar days to submit the required information. For non-urgent (elective) care, the information must be submitted within 45 calendar days of the request for additional information for commercial plans, and within 28 days for Medicare Advantage HMO and 7/1/2014 9.11 Care Management and Coordination Hospital Manual 9 PPO plans. If the information is not submitted in the applicable time frame, the request may be denied and the information regarding an appeal process will be included in the denial letter. All determinations are communicated verbally, and written confirmation is sent to the attending Physician, hospital, Primary Care Physician, and Member, as applicable. The clinical review criteria applied in rendering an adverse coverage or payment determination are available free of charge and will be furnished upon request. All adverse determination (denial) notifications include contractual basis and the clinical rationale for the denial, as well as how to initiate an appeal. Delays in service Under per diem reimbursement, when there is a delay in providing Medically Necessary treatment to a Member due to a non-medical reason, such as hospital scheduling issues, and such delay lengthens the hospital stay, the days resulting from the delay will be denied for payment. Decreased levels of care (skilled/subacute vs. acute days) For Members at facilities paid under per diem arrangements who are no longer at an acute level of care, reimbursement to a hospital at a skilled rate, in accordance with its Agreement, will be appropriate when all of the following circumstances apply: The Member no longer requires acute hospital services but still has inpatient skilled needs. Placement in a skilled or subacute facility is problematic and/or delayed for reasons beyond the hospital’s or IBC’s control. The need for a skilled rate is of limited duration (generally fewer than seven days). A skilled rate will not be used for Members who would otherwise require long-term SNF placement. The skilled rate will not be used on a retrospective basis when the hospital has received a denial of days. If the facility is not contracted for a skilled rate and the Member is no longer receiving services at an acute level, the days may be denied after review by an IBC Medical Director. In these denied cases, the Hospital Provider Appeals Process will apply. Member decision days A Member decision day is defined as: “A day in which the Member is making a decision as to whether he or she will have a certain treatment or procedure, thereby causing a delay in said procedure or treatment.” Under per diem reimbursement, decision days that are not otherwise Medically Necessary will be denied as a delay in service. Requests for exceptions to this procedure will be presented to the IBC Medical Director by the review nurse. The Medical Director will consider the circumstances and possibly contact the attending Physician to learn more about this situation prior to rendering a determination. Observation status Observation status is an outpatient service that does not require authorization. It should be considered if a patient does not meet InterQual acute care criteria and one or more of following apply: Diagnosis, treatment, stabilization, and discharge can be reasonably expected within 24 hours. Treatment and/or procedures will require more than six hours observation. The clinical condition is changing and a discharge decision is expected within 24 hours. 7/1/2014 9.12 Care Management and Coordination Hospital Manual 9 It is unsafe for the patient to return home or a caregiver is unavailable (arrangements need to be made for a safe and appropriate discharge setting such as SAC/SNF, home care, etc.). Symptoms are unresponsive to at least four hours ER treatment. There is a psychiatric crisis intervention or stabilization with observation every 15 minutes. Observation status does not require a physical “stay” in an observation unit and does not apply to ER observation of less than six hours. IBC uses the InterQual level of care guidelines to determine Medical Necessity and reserves the right to retrospectively audit claims where there has been billing for observation status to assure that appropriate guidelines have been met. If a Member has received observation services and is subsequently admitted, the date of the admission becomes the date that observation began. Observation services that result in an admission are subject to CMC review for Medical Necessity. Any questions about the status or review of a Member who has received services should be discussed with the CMC coordinator or supervisor. For billing information, please refer to the Billing & Reimbursement for Hospital Services section of this manual. Transfers within and between inpatient facilities Members may be transferred within or between inpatient facilities for a variety of reasons. Some common reasons for transfers are: transfer to a specialized facility or unit inside or outside the current facility; transfer because the current facility is unable to provide necessary treatment for the Member; transfer because the Member’s primary or regular Physician is at another facility; transfer due to Member or family request; transfer to an in-network facility from an out-of-network facility. Transfers within the same facility All nonemergency transfers within an acute care facility to a psychiatric, rehabilitation, or long-term acute care unit within the same facility must be Preapproved/Precertified with CMC or Magellan Behavioral Health, Inc., as appropriate. All Emergency transfers within a facility from a psychiatric or rehabilitation unit to an acute care unit within the same facility do not need to be Preapproved/Precertified, but the facility must notify CMC or Magellan Behavioral Health, Inc., if applicable. Transfers between facilities When a Member requires transfer to another facility for a service unavailable at the admitting facility and the Member returns to the admitting facility the same day (i.e., no overnight stay at the second facility) no Preapproval/Precertification or review of the transfer is required. When services do require an overnight stay at the accepting facility, the day of transfer is considered the day of discharge from the transferring facility and the day of admission to the accepting facility. If the admission is nonemergent, the second facility must Preapprove/Precertify the new admission; if the admission is emergent, the facility must notify CMC or Magellan Behavioral Health, Inc. 7/1/2014 9.13 Care Management and Coordination Hospital Manual 9 Reconsideration and hospital appeals processes Peer-to-Peer Reconsideration process In the event that an adverse determination (denial) is issued without discussion between an attending/ordering Physician and an IBC Medical Director, the requesting Provider (including attending/ordering Physician or hospital medical director) may request a Peer-to-Peer Reconsideration with an IBC Medical Director. Peer-to-Peer Reconsideration is an optional, informal process designed to encourage dialogue between the requesting Provider and IBC’s Medical Directors and may be requested by an attending/ordering Physician for a Preapproval/Precertification, concurrent, or post-service review denial based on Medical Necessity. For concurrent review denials, the process should be initiated prior to a Member’s discharge from the hospital; however, hospitals have up to two business days from the date the Member is discharged to initiate the process. For Preapproval/Precertification denials, the process should be initiated after the hospital has received notification of the denial but before the service is actually rendered. To initiate the process, the attending physician, ordering physician, hospital Utilization Management department physicians, or their designated physician representative (e.g., hospital medical director) may contact an IBC Medical Director through email or by calling the Physician Referral Line at 1-888-814-2244, or at 215-241-0494 within Philadelphia. The Physician Referral Line is available Monday through Friday from 8:30 a.m. to 5 p.m. The requesting Physician has the option to submit additional documentation in support of the request. This will typically include pertinent parts of the medical record (usually progress notes and orders) and a written rationale to explain why the requested service or settings are Medically Necessary, based on medical judgment and InterQual criteria. The request for Peer-to-Peer Reconsideration will be responded to within one business day of receipt. The Peer-to-Peer Reconsideration discussions are heard at prescheduled meetings via telephone twice a week. At that time, the Physician will be provided with the opportunity to present additional supporting documentation to support his or her position. For concurrent review denials, the Peer-to-Peer Reconsideration decision will be completed within ten business days of the Member’s discharge date. For Preapproval/Precertification and Post-Service denials, the decision will be completed within ten days following the request. A decision to overturn all, or a portion of, the initial adverse determination will be communicated in writing to the hospital. If the Peer-to-Peer Reconsideration decision is to uphold all or a portion of the original denial/adverse determination, the hospital may initiate the applicable Appeal for Lack of Medical Necessity process for services that were denied post-service or concurrently as not Medically Necessary. Appeals for lack of Medical Necessity Where all or part of an admission or outpatient service at an eligible facility is denied for failure to meet Medical Necessity criteria, the IBC Member is held harmless and cannot be billed for the denied day(s) or service(s). The facility may appeal such denial of payment for lack of Medical Necessity through the process detailed below. This process is the exclusive means of resolving such disputes. Appeals for lack of Medical Necessity and payment reviews for lack of Preapproval/Precertification may not be pursued through the Member grievance or Member appeal processes. Inpatient appeals for acute care hospitals, long-term acute facilities for vent weaning, and inpatient SNFs The facility must submit the appeal in writing within 180 calendar days of the adverse determination notice (received during the Utilization Review process or facility Peer-to-Peer Reconsideration decision). 7/1/2014 9.14 Care Management and Coordination Hospital Manual 9 The written appeal request must contain the entire medical record for the case being appealed. Inpatient appeals for denials due to Medical Necessity should be mailed to the following address: Facility Appeals P.O. Box 13985 Philadelphia, PA 19101 Inpatient appeals are reviewed by an external, independent, licensed Physician who is of the same or similar specialty that typically manages the care under review and who was not involved in the initial adverse determination or facility Peer-to-Peer Reconsideration decision. The decision to uphold or overturn all, or a portion of, the adverse determination is communicated in writing to the facility within 30 calendar days of IBC’s receipt of the written appeal request and the complete medical record. The written determination of the appeal will include the rationale for the determination where all, or a portion of, the adverse determination is upheld. This decision is final and binding. Outpatient appeals for acute care hospitals, freestanding ambulatory surgical centers, and sleep centers The facility must submit the appeal in writing within 180 calendar days of the adverse determination notice (initial adverse determination, facility Peer-to-Peer Reconsideration decision, or claim processing date noted on the Statement of Remittance). The written appeal request must contain the entire medical record for the case being appealed. Outpatient appeals for denials due to Medical Necessity should be mailed to the following address: Facility Appeals P.O. Box 13985 Philadelphia, PA 19101 Outpatient appeals are reviewed by an external, independent, licensed hysician of the same or similar specialty that typically manages the care under review and who was not involved in the initial adverse determination or facility Peer-to-Peer Reconsideration decision, if applicable. The decision to uphold or overturn all, or a portion of, the adverse determination is communicated, in writing, to the facility within 30 calendar days of IBC’s receipt of the written appeal request and the complete medical record. The written determination of the appeal will include the rationale for the determination where all, or a portion of, the adverse determination is upheld. This decision is final and binding. Appeals for cosmetic or experimental/investigational services To appeal a denial for cosmetic or experimental/investigational services, hospitals should send their request, along with the appropriate Member authorization and any applicable supporting documentation, to the following address: Member Appeals P.O. Box 41820 Philadelphia, PA 19101 ER services appeals ER claims that do not meet IBC’s criteria for Emergency are automatically processed at the lowest ER payment rate in the fee schedule or as otherwise provided in the Agreement. To appeal an ER determination, please complete an ER Review Form, attach the Member’s medical record, and submit to: 7/1/2014 9.15 Care Management and Coordination Hospital Manual 9 Claims Medical Review – Emergency Room Review Independence Blue Cross 1901 Market Street Philadelphia, PA 19103-1480 Outpatient payment disputes (except ER) To dispute a payment denial of an Outpatient service claim, including denials for failure to obtain Preapproval/Precertification, case rate, or bundling, hospitals should send their request for payment review, with any applicable supporting documentation, to the following address: Provider Disputes P.O. Box 7930 Philadelphia, PA 19101 Hospitals will be notified of the determination in writing within 45 calendar days of IBC’s receipt of the dispute. Payment disputes receive one non-clinical reconsideration review and are not eligible for appeal. Timely submission of Medicare Advantage HMO and PPO Member’s medical records As part of the federally mandated Medicare Advantage and Grievances process, IBC is required to obtain a Member’s medical record in order to make a determination of coverage. Should we uphold our determination, we are required to forward the Member’s appeal file, which includes medical records, to an independent review entity (IRE). IREs are contracted with CMS to perform second-level independent reviews of Medicare Advantage Members’ appeals. Upon our request, and in accordance with your Hospital, Ancillary Facility, or Ancillary Provider Agreement, you must provide copies of a Medicare Advantage HMO or PPO Member’s medical records to us as required. Further, Providers must submit medical records to us in a timely manner. Receiving timely medical records enables us to submit them to an IRE and ensure compliance with mandated appeal deadlines. CMS requires that both IBC and the IRE make their determinations within 72 hours for an expedited appeal and within 30 days for a standard appeal. If a Member requests an expedited review, we will immediately send a request to the Provider for medical records. We must receive the records within 24 hours for an expedited appeal and within ten days for a standard appeal. If an appeal is sent to an IRE, the IRE may request additional records, which are required to be sent under the same time frames as previously stated. Other reasons that IBC may require the timely submission of medical records include: facilitating the delivery of appropriate health care services to Medicare Advantage HMO and PPO Members; assisting with utilization review decisions, including those related to care management programs, quality management, grievances (as discussed in this section of the manual), claims adjudication, and other administrative programs; complying with applicable State and federal laws and accrediting body requirements (e.g., National Committee for Quality Assurance); facilitating the sharing of such records among health care Providers directly involved with the Member’s care. 7/1/2014 9.16 Care Management and Coordination Hospital Manual 9 Continuity-of-care If a Provider’s contract is discontinued, the Member may continue an ongoing course of treatment in a facility setting for a transitional period that will be the lesser of the current period of active treatment, or up to 90 calendar days for Members undergoing active treatment for a chronic or acute medical condition. In the case of a Member in the second or third trimester of pregnancy, this period extends through postpartum care related to the delivery. The continuity-of-care period may be extended by IBC when clinically appropriate. Coverage of Covered Services provided during the continuity-of-care period is contingent upon the Provider’s agreement to comply with the terms and conditions applicable to IBC Participating Providers prior to providing services for this time period. If IBC initiates termination of a Provider with cause, we will not be responsible for coverage of health care services provided by the terminated Provider to the Member following the date of termination. Notification will be provided to our Members, and arrangements will be made to facilitate transfer to another Participating Provider. Baby BluePrints® maternity program Our Baby BluePrints maternity program is designed to educate all pregnant IBC Members about pregnancy and preparing for parenthood. The program also helps to identify expectant mothers who may be at risk for complications during their pregnancy and to assist in improving the quality of care to pregnant women and newborns. If any risk factors are detected, our OB nurse Health Coaches provide telephone support to our Members and their Physician or midwife to help coordinate their benefits and provide information they need for the healthiest delivery possible. Note: Some value-added services covered under this program are enhancements to the standard Member benefits and are therefore subject to change at any time upon notice. Postpartum program – Mother’s Option® All Members who have an uncomplicated pregnancy and delivery have the option of choosing a shorter length of stay in the hospital. In order to support a smooth and safe transition home, home care visits are available per the following guidelines: Uncomplicated vaginal delivery If discharged within the first 24 hours following an uncomplicated vaginal delivery, two home health visits are available if desired by the Member. These visits do not require Preapproval/Precertification but should be arranged by a hospital discharge planner with one of the Mother’s Option home care Providers. The first visit should occur within 48 hours of discharge. The second visit should occur within five days of discharge. If discharged within the first 48 hours following an uncomplicated vaginal delivery, one home health visit is available if desired by the Member. This visit does not require Preapproval/Precertification but should be arranged by a hospital discharge planner with one of the Mother’s Option home care Providers. This visit should occur within 48 hours of discharge. Uncomplicated cesarean delivery If discharged within the first 96 hours following an uncomplicated cesarean delivery, one home health visit is available if desired by the Member. This visit does not require Preapproval/Precertification but should be arranged by a hospital discharge planner with one of the Mother’s Option home care Providers and should occur within 48 hours of discharge. 7/1/2014 9.17 Care Management and Coordination Hospital Manual 9 Standard length of stay Managed care HMO/PPO Members. When the hospital stay is longer than 48 hours (vaginal) or 96 hours (cesarean), one home health visit is available if desired by the Member or Provider. This visit does not require Preapproval/Precertification but should be arranged by a hospital discharge planner with one of the Mother’s Option home care Providers. These visits must occur within five days of discharge. Additional home health visits that are Medically Necessary beyond the described Mother’s Option visits, must be Preapproved/Precertified by calling the Perinatal Case Management department at 1-800-598-BABY or 215-241-2198 within Philadelphia. SM Special Care or Comprehensive Major Medical Members. Members who opt for discharge less than 48 hours after vaginal delivery and less than 96 hours after cesarean delivery are eligible for one home care visit under their home health benefits. Preapproval/Precertification for this visit can be done by calling the Perinatal Case Management department as noted above. Baby BluePrints postpartum services Postpartum care Postpartum home skilled nursing visits beyond those provided through Mother’s Option are approved when Medically Necessary. These visits must be Preapproved/Precertified through Baby BluePrints or by calling 1-800-ASK-BLUE. Lactation support programs and breast pump reimbursement through Healthy LifestylesSM Lactation support services include information about valuable community resources, educational websites, or certified lactation consultants. Members may self-refer to any International Board Certified Lactation Consultant (IBCLC) and receive a $100 reimbursement through our Healthy Lifestyles program.* Members may submit a receipt listing the date of the visit and the consultant’s IBCLC certification number within 90 days after delivery. Health Coaches are available for initial breast feeding support by telephone. Additionally, they will be able to evaluate the need for further assistance (e.g., community resources, lactation consultant, or OB Provider). Managed care Members who obtain a manual/mini-electric breast pump at pharmacies or baby supply stores may submit their receipt to Healthy Lifestyles for reimbursement up to $50 within 90 days after delivery.* Hospital-grade pumps are covered under the following circumstances and when supplied by an innetwork Provider: – detained premature newborn – infants with feeding problems that interfere with breastfeeding (e.g., cleft palate/lip). *This program is only available for non-migrated Members. As Members are migrated to our new operating platform, they will have access to a new suite of Healthy Lifestyles programs, called Healthy Lifestyles SM Solutions. Please note that many of the same popular programs that currently fall under the Healthy Lifestyles umbrella will still be offered; however, this specific reimbursement will no longer be offered. Breast pump coverage under Health Care Reform Members can purchase one portable manual or electric breast pump, plus supplies, per pregnancy from a participating, in-network DME Provider with no Member cost-sharing. 7/1/2014 9.18 Care Management and Coordination Hospital Manual 9 Note: The rental of hospital-grade breast pumps requires approval for Medical Necessity. Rentals are available at no cost-sharing only for those Members who require the use of a hospital-grade pump. If approval is obtained for Medical Necessity, Member cost-sharing will not be applied when the Member rents the breast pump from an in-network DME Provider. Lactation support and counseling under Health Care Reform Lactation support and counseling, by a trained Provider during pregnancy and/or in the postpartum periods, is currently covered during an inpatient maternity stay as part of an inpatient admission, the postpartum Mother’s Option visit, and through the OB postpartum visit and/or pediatrician well-baby visit. Note: Lactation consultants are not a recognized Provider type by Pennsylvania Blue Shield and therefore are not directly contracted by the Plan. Preapproval/Precertification for home phototherapy Preapproval/Precertification through Baby BluePrints is required when ordering home phototherapy to treat jaundiced newborns. Skilled nursing visits must also be Preapproved/Precertified. 7/1/2014 9.19 10 00 Table of Contents Overview ...............................................................................................................................0 10.1 Behavioral Health Hospital Manual Emergency admissions .......................................................................................................10.1 Member eligibility, precertification, and claims submission ............................................10.1 HMO/referred (in-network) POS Members ............................................................................ 10.1 PPO Members.................................................................................................................................... 10.2 FEP PPO Members ........................................................................................................................... 10.2 Traditional (Indemnity) Members .................................................................................................. 10.3 Autism coverage ..................................................................................................................10.3 6/1/2013 10.i 10 00 Overview 0 Magellan Behavioral Health, Inc. (Magellan) is an independent managed care behavioral health care Behavioral Health Hospital Manual company contracted by Independence Blue Cross (IBC) to manage the behavioral health and substance abuse benefits for the majority of our Members with HMO, POS, PPO, Federal Employee Program (FEP), and Traditional (Indemnity) coverage. Magellan develops, contracts with, and services its own network of behavioral health Providers and facilities. Members are not capitated to a specific behavioral health site. However, for a Member to receive the highest level of benefits, behavioral health services must be provided by Magellan providers. Note: Magellan is available 24 hours a day, 7 days a week, at 1-800-688-1911. Emergency admissions Precertification (authorization) for Emergency admissions is not required. When a Member is admitted as an inpatient through the emergency room/department, the hospital is required to notify Magellan within 48 hours or on the next business day. Member eligibility, precertification, and claims submission Providers are encouraged to verify Member benefits and eligibility by calling Magellan at 1-800-688-1911. The contact information is also located on the Member’s ID card. FEP Member eligibility can be verified by contacting FEP Customer Service at 215-241-4400. Residential Treatment Centers (RTCs) are no longer treated as covered Providers. Changes have been put into place to discontinue Preferred Behavioral Health/Substance Abuse benefits for inpatient facility claims submitted by RTCs unless they are provided and approved under the case management process. This applies to both the Standard and Basic Option for claims incurred on or after January 1, 2011, with a type of bill equal to 086X or have a revenue code equal to 1001 or 1002. Precertification and continuing authorizations are not required for routine and medication management outpatient behavioral health services under most IBC benefits plans. However, precertification is required for substance and alcohol abuse services, behavioral health inpatient services, Partial Hospitalization Programs, and Intensive Outpatient Programs. Members must call Magellan once an appointment has been made to ensure that the precertification process is properly initiated. HMO/referred (in-network) POS Members In order for HMO/referred (in-network) POS Members to receive in-network behavioral health and substance abuse benefits, they must use a Magellan HMO/referred (in-network) POS Provider. Benefits vary based on plan type and employer group. Not all employer groups use Magellan for behavioral health benefits. Providers are encouraged to verify benefits and eligibility by contacting Magellan. Members can select any participating Magellan HMO/referred (in-network) POS network Provider. All HMO/referred (in-network) POS inpatient, nonemergency admissions, Partial Hospitalization Programs/Intensive Outpatient Programs, and behavioral health and substance abuse services must be Preapproved. To Preapprove an admission or Partial Hospitalization Program/Intensive Outpatient Program, please contact Magellan. 6/1/2013 10.1 10 00 Claims submission Behavioral health and substance abuse claims for HMO/referred (in-network) POS Members who have 0 Magellan as their behavioral health Provider must be submitted to: Behavioral Health Hospital Manual Magellan Behavioral Health, Inc. P.O. Box 1958 Maryland Heights, MO 63043-1958 For electronic claims submission, use Payer ID 01260. PPO Members In order for the majority of Members with PPO coverage to receive in-network behavioral health and substance abuse benefits, they must use the Magellan PPO Provider network. Benefits vary based on plan type and employer group. Providers are encouraged to verify Member benefits and eligibility by contacting Magellan. All PPO inpatient, and Partial Hospitalization Programs/Intensive Outpatient Programs for behavioral health and substance abuse services must be precertified by calling Magellan. Claims submission Claims for PPO Members should be sent to: Personal Choice® claims P.O. Box 69352 Harrisburg, PA 17106-9352 For electronic claims submission, use Payer ID 54704. FEP PPO Members In order for Members with FEP PPO coverage to receive in-network behavioral health and substance abuse benefits, they must obtain precertification for inpatient services. Members must use the Magellan PPO facility Provider network to receive in-network behavioral health and substance abuse benefits. Benefits vary based on FEP plan type. All inpatient services must be Preapproved by calling Magellan. Benefits and eligibility can be verified by contacting FEP Customer Service at 215-241-4400. Claims submission Facility claims for FEP Members should be sent to: Federal Employee Program (FEP) Independence Blue Cross Attn: FEP 1500 SG/Front End 1901 Market Street Philadelphia, PA 19103-1480 For electronic claims submission, use Payer ID 54704. 6/1/2013 10.2 10 00 Traditional (Indemnity) Members Magellan also manages the behavioral health and substance abuse benefits for Traditional Members. 0 Almost all inpatient and Partial Hospitalization Programs/Intensive Outpatient Programs for behavioral Behavioral Health Hospital Manual health and substance abuse services must be Preapproved. To Preapprove an admission or Partial Hospitalization Program/Intensive Outpatient Program service, call Magellan. Claims submission Please submit behavioral health and substance abuse claims to: Independence Blue Cross (Indemnity) 1901 Market Street Operations Support, SG1 Philadelphia, PA 19103-1480 Autism coverage The diagnosis and treatment of autism spectrum disorders (ASD) are covered for eligible commercial Members. Before you provide care related to ASD, be sure to verify Member eligibility through the NaviNet® web portal or the Provider Automated System. Covered Services include, but are not limited to, Medically Necessary occupational, physical, speech, and psychological therapy, as described in a comprehensive treatment plan, and behavioral interventions based on the principles of applied behavioral analysis (ABA), as described in a treatment plan. Covered Services are subject to Medical Necessity review, the Copayment, Deductible, and Coinsurance provisions of the Member’s benefits plan, and any applicable Referral or prescription requirements. Covered Services with a primary diagnosis of ASD are not subject to limits of the number of Provider treatments. Treatment for ASD is not covered when provided by or through a school or camp, whether or not as part of an individualized education program. Refer to Medical Policy #07.03.07: Evaluation and Management of Autism Spectrum Disorders (ASD), which is available at www.ibx.com/medpolicy, for specific coverage information regarding the diagnosis and treatment of ASD. Note that our Medical Policy is consistent with applicable State mandates. 6/1/2013 10.3 Quality Management Hospital Manual 11 Table of Contents QM Program activities .........................................................................................................11.1 Member safety activities...................................................................................................................... 11.1 Monitoring of continuity and coordination of care.............................................................................. 11.1 Quality improvement ........................................................................................................................... 11.2 Hospital responsibilities ...................................................................................................................... 11.2 Confidentiality of information ............................................................................................................. 11.3 Blue Distinction Centers for Specialty Care® .....................................................................11.3 5/1/2014 11.i Quality Management Hospital Manual 11 QM Program activities Through our Quality Management (QM) Program, we monitor, evaluate, and act to improve the quality and safety of clinical care and the quality of service provided to Members by Participating Practitioners/ Providers and by delegates across our HMO/POS, and PPO Medicare Advantage product lines. We identify meaningful clinical and service issues that are likely to impact enrolled Members and establish performance indicators, goals, and benchmarks that correspond to topics falling within the scope of the QM Program. The mechanisms used to identify meaningful clinical and service issues include, but are not limited to: the results of analysis of demographics, claims, and other data to identify high-volume, high-risk, and problem-prone services and acute and chronic conditions; the results of data from internal performance monitoring activities and satisfaction survey results; data from complaints and Member appeals and direct input from Members, practitioners/Providers, and IBC staff. Through ongoing review of performance data with respect to established goals, benchmarks, and formal annual evaluations of the effectiveness of the QM Program, IBC confirms that existing clinical quality, safety, and service improvement initiatives remain appropriate and identifies new topics for inclusion in the program. Member safety activities The QM department leads Plan-wide activities that promote and support Providers and Members in increasing Member safety initiatives and reducing medical/medication errors. These activities include: communicating information on Member safety and preventing medical/medication errors through Member and Provider mailings and newsletters; supporting regulatory agency standards; implementing initiatives that pertain to quality of care, Member safety, and medical/medication errors. The Member Safety Program supports the Partnership for Patient Care, a regional collaborative that promotes best practices and evidence-based medicine to improve the safety and quality of health care at network hospitals. The program uses a regional, strategic, and cohesive approach and an interactive forum to facilitate hospitals’ efforts to more rapidly implement best practices. Monitoring of continuity and coordination of care Our goal is for Members to receive seamless, continuous, and appropriate care. On an annual basis, we collect data about coordination of care across settings or transitions in care. Data is collected related to the coordination between medical and behavioral health care. A quantitative and causal analysis of data is conducted to facilitate the identification of improvement opportunities. Based on the results of the analysis, we identify opportunities to improve continuity and/or coordination of care and implement appropriate initiatives to address opportunities for improvement. Examples of different settings include: outpatient facilities inpatient facilities surgery centers nursing homes 5/1/2014 11.1 Quality Management Hospital Manual 11 Examples of the type of data collected to improve coordination of care and promote collaboration between medical and behavioral health care include: exchange of information; appropriate diagnosis, treatment, and Referral of behavioral health disorders commonly seen in primary care; appropriate use of psychopharmacological medications; management of treatment access and follow-up for Members with co-existing medical and behavioral health disorders; primary and secondary preventive behavioral health programs. Examples of transitions in care include: changes in the management of care between practitioners (e.g., enrollment or disenrollment in disease management programs); changes in which different practitioners become active or inactive in providing care for a Member. Examples of the type of data collected to promote the identification of improvement opportunities and facilitate the design and implementation of improvement initiatives include: discharge planning data; surveys of practitioners regarding communication and coordination issues; case management data. QM works with the Care Management and Coordination department to monitor the coordination of the care of Members when they move from one setting to another, such as when they are discharged from a hospital. Without coordination, such transitions often result in poor quality care and risks to patient safety. Quality improvement Information about our Quality Improvement Program is available to our Providers and Members upon request. This information includes a description of our Quality Improvement Program and a report on our progress in meeting our goals. For more information, Providers may contact Customer Service at 1-800-ASK-BLUE. Members can contact Customer Service at the number listed on their ID card. Hospital responsibilities Hospitals contracted with IBC are required to comply with IBC’s QM Program. Hospitals have the responsibility to: ensure that all necessary authorizations are obtained prior to rendering services; be available and accessible 24 hours per day, 7 days per week; notify the Primary Care Physician (PCP)/family practitioner of follow-up care for services performed in the Emergency department; notify the PCP/family practitioner of follow-up care for services performed after a hospital stay; maintain Member confidentiality and comply with HIPAA* regulations; respect Member rights and responsibilities; comply with QM Program initiatives and any related policies and procedures; comply with QM requirements, including, but not limited to, the following: – cooperate with the onsite medical review process and provide medical records when requested for clinical and/or service outcome measures; – respond to investigations of Member complaints regarding quality of care and services; 5/1/2014 11.2 Quality Management Hospital Manual – 11 cooperate with the development of corrective action plans when measurements identify opportunities for improvement or as a result of a quality of care inquiry. *HIPAA, the Health Insurance Portability and Accountability Act, was enacted by the U.S. Congress in 1996, and became effective July 1, 1997. This act is a grouping of regulations that work to combat waste, fraud, and abuse in health care delivery and health insurance. The intention of HIPAA is also to improve the effectiveness and efficiency of the health care system; portability and continuity of health insurance coverage in the group and individual markets; and the ability to provide consequences to those that do not apply with the regulations explicitly stated within the Act. Confidentiality of information Protected Health Information (PHI) is protected against unauthorized or inadvertent disclosure. Medical records are safeguarded against loss or destruction and are maintained according to State requirements. At a minimum, medical records must be maintained for at least 11 years or age of majority plus 6 years, whichever is longer. Medical records are stored in a secure manner that allows access by authorized personnel only. Staff receives periodic training in Member information confidentiality. For complete information on IBC’s QM Program, including Member rights and responsibilities, please visit www.ibx.com/qualitymanagement. Blue Distinction Centers for Specialty Care® Blue Distinction® was created by the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans, to give consumers more information to make informed health care decisions and to work with Providers to improve health care quality outcomes and affordability. Associated with Blue Distinction are the Blue Distinction Centers for complex and rare cancers, bariatric surgery, cardiac care, and transplants. All of the Centers must offer specific, evidence-based criteria on Provider qualifications, best practices, and outcomes. For more information about the Blue Distinction Centers for Specialty Care, visit www.bcbs.com/bluedistinction. 5/1/2014 11.3 Disclaimer Information Hospital Manual 12 16 The third-party websites mentioned throughout this manual are maintained by organizations over which Independence Blue Cross (IBC) exercises no control, and accordingly, IBC disclaims any responsibility for the content, the accuracy of the information, and/or quality of products or services provided by or advertised in these third-party sites. URLs are presented for informational purposes only. Certain services/treatments referred to in third-party sites may not be covered by all benefits plans. Members should refer to their benefits contract for complete details of the terms, limitations, and exclusions of their coverage. Magellan Behavioral Health, Inc., an independent company, manages mental health and substance abuse benefits for most IBC members. CPT copyright 2012 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. NaviNet® is a registered trademark of NaviNet, Inc., an independent company. WebMD® is an independent company offering online health information and wellness education to Independence Blue Cross members. The Blue Cross and Blue Shield names and symbols, BlueCard, BlueExchange, Blue Distinction, Blue Distinction Centers for Specialty Care, and Baby BluePrints are registered marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans. Independence Blue Cross offers products directly, through its subsidiaries Keystone Health Plan East and QCC Insurance Company, and with Highmark Blue Shield – independent licensees of the Blue Cross and Blue Shield Association. 6/1/2013 12.1
© Copyright 2026