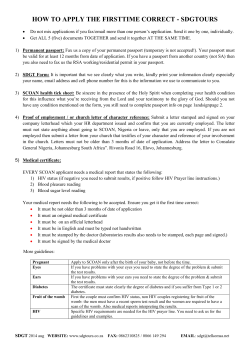
– Chapter 5 Communicable Disease Control Manual
Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 1 TABLE OF CONTENTS DEFINITIONS 3 SECTION I: OVERVIEW AND INDICATIONS FOR POC HIV TESTING .................... 8 1.0 BACKGROUND ........................................................................................................ 8 2.0 PURPOSE8 3.0 EPIDEMIOLOGY OF HIV INFECTION IN B.C. ......................................................... 8 4.0 POLICY FRAMEWORK ............................................................................................ 9 5.0 COMPARISON OF POC & STANDARD HIV TESTING ............................................ 9 6.0 POTENTIAL BENEFITS OF POC HIV TESTING .................................................... 10 7.0 POTENTIAL HARMS OF POC HIV TESTING ........................................................ 10 8.0 GENERAL REQUIREMENTS ................................................................................. 11 9.0 INDICATIONS FOR POC HIV TESTING ................................................................. 11 SECTION II: PERFORMING THE TEST .................................................................... 14 1.0 KEY INFORMATION ABOUT POC HIV TESTING ................................................. 14 2.0 CONDUCTING THE INSTI™ HIV TEST.................................................................. 15 3.0 INTERPRETING THE TEST RESULTS .................................................................. 18 4.0 FOLLOW-UP TESTING .......................................................................................... 20 SECTION III: QUALITY ASSURANCE ....................................................................... 24 1.0 OVERVIEW ............................................................................................................. 24 2.0 TRAINING 25 3.0 USING QUALITY CONTROL SAMPLES ................................................................ 27 4.0 PERFORMING A QUALITY CONTROL TEST........................................................ 30 5.0 PROGRAM REPORTS AND DOCUMENTATION .................................................. 32 6.0 PURCHASING AND INVENTORY CONTROL ....................................................... 35 7.0 OUTREACH AND MOBILE SITES ......................................................................... 37 SECTION IV: NON-REGULATED AND ALLIED HEALTH CARE PROVIDERS (NRACP) FRAMEWORK ....................................................................................................... 39 1.0 PURPOSE 39 2.0 ADVISORY COMMITTEE(S)................................................................................... 41 3.0 RESOURCES AND INFRASTRUCTURE ............................................................... 42 4.0 COMMUNITY READINESS AND MOBILIZATION ................................................. 42 5.0 LINKAGES TO CARE, TREATMENT AND SUPPORT .......................................... 43 6.0 TRAINING AND COMPETENCIES ......................................................................... 43 7.0 KEY MANAGEMENT CONSIDERATIONS ............................................................. 44 8.0 ACCOUNTABILITY AND SUPERVISION OF NRACPs ......................................... 45 REFERENCES ................................................................................................................. 47 APPENDICES 50 APPENDIX I — Summary of Test Properties ..................................................................... 51 APPENDIX II — Roles and Responsibilities ...................................................................... 52 APPENDIX III — Daily Log of Client POC Test Results ..................................................... 60 Suggested Citation: BC Centre for Disease Control. Point of Care HIV Test Guidelines for Health Care Settings, May 2014, Communicable Disease Control Manual, Chapter 5. BC Centre for Disease Control, 2014. Available from: http://www.bccdc.ca/dis-cond/comm-manual/CDManualChap5.htm. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 2 APPENDIX IV — Fax Template Form................................................................................ 61 APPENDIX V — Direct Observation Checklist for POC HIV Testing .................................. 62 APPENDIX VI — Training Completion Requirements for Nurses, Physicians, NursePractitioners ...................................................................................................................... 64 APPENDIX VII — Training Competencies for Nurses, Physicians, Nurse-Practitioners ..... 65 APPENDIX VIII — Quality Control Log .............................................................................. 66 APPENDIX IX — Monthly Summary Report ...................................................................... 67 APPENDIX X — Incident Summary Form .......................................................................... 68 APPENDIX XI — Temperature Monitoring Log .................................................................. 69 APPENDIX XII — Practice Guidance for Allied Health – Regulated Health Care Providers 70 APPENDIX XIII — Sample Letter for Colleges................................................................... 71 APPENDIX XIV — Recommended Base-Line Qualification for NRACP HIV POC Testers 73 APPENDIX XV — Competencies for Non-regulated and Allied Health Care Providers ...... 74 APPENDIX XVI — HIV Testing Education for Non-regulated and Allied Health Care Providers .......................................................................................................................................... 77 APPENDIX XVII — Checklist for New NRACP Sites ......................................................... 80 Contact Information for the BC Point of Care HIV Test Program: Phone: 604-707-5635 FAX: 604-707-2603 Webpage for Resources: http://www.bccdc.ca/SexualHealth/Programs/ProvincialPointofCareHIVTestingProgram/d efault.htm Suggested Citation: BC Centre for Disease Control. Point of Care HIV Test Guidelines for Health Care Settings, May 2014, Communicable Disease Control Manual, Chapter 5. BC Centre for Disease Control, 2014. Available from: http://www.bccdc.ca/dis-cond/comm-manual/CDManualChap5.htm. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 3 DEFINITIONS Acute HIV infection: The first 4-6 weeks after infection is a period when a person often has a high viral load and there is a greater likelihood of transmitting HIV to others compared with individuals in later stages of HIV infection. Individuals with acute HIV infection may test falsely negative on HIV tests if they are tested within the window period. Community Health Representative (CHR) Health care providers or “care providers” (PHAC, 2013) working in First Nations communities but employed by an external agency or the health authority. Confirmatory Test Venous blood sample sent to the laboratory to confirm a reactive HIV POC test result. The standard laboratory HIV Test Algorithm is applied to the sample. The resultant laboratory report is compared to the POC test result. Discordant results are flagged, and actions taken are recorded in the client history. Confirmatory results are reported in the HIV POC Program Monthly Report as one of: True Positive – POC and lab both reactive False Positive – POC reactive, lab – non-reactive Preliminary Positive – Confirmatory test NOT DONE Controls Each INSTI test kit membrane contains an internal/IgG control that should create a blue dot for each test. This indicates that enough sample and reagents were added so that if HIV antibodies are present in the sample, they should turn the “test dot” blue. Quality Control (QC) materials are external controls that are used to test the test system (test kits, tester and light) when the test system may have been challenged, and assurance is needed that test results are accurate. They test specifically for HIV negative, anti-HIV-1 and anti-HIV-2. The positive controls are intentionally weak to simulate an early infection (low antibody levels) – a critical point that all testers must be able to see. False Negative: DEFINITIONS A false negative result is reported when the POC test fails to detect a HIV infection. Since the BC Program does not include parallel blood testing with POC, such findings are discovered only when standard HIV laboratory tests are run and reported back to the test site. The most common reason for not detecting HIV is because the client is in early acute phase, and has not produced antibodies at sufficient levels that they can react with Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 4 the test material, and be detected by the tester. Underlying medical conditions that affect antibody production, long-term antiretroviral therapy and HIV-1 group N subtype infections may also result in a false negative result. False Positive: A false positive result is reported when the result for confirmatory testing is “not indicative of HIV infection”, but the POC result was reactive or indeterminate. Such results occur more commonly if there is a low prevalence of HIV infection in the population being testing (i.e. general population). Factors that may cause a false positive include recent viral infection, recent vaccination for viral infections, underlying immune conditions, cross-reacting antibodies of other origins. Since there is only 1 POC manufacturer in Canada, subsequent HIV testing should be by standard laboratory testing. Health care provider: (As per the Health Professions Act) An individual from a profession in which he or she exercises knowledge, skill, and judgment in, or provides a service related to, the preservation or improvement of the health of individuals, or the treatment or care of individuals who are injured, sick, disabled, or infirm. See Non-regulated Care Provider, Regulated Allied Health Care Professional, Community Health Representative. High HIV transmission activities: Activities that are associated with increased transmission or acquisition of HIV include: unprotected vaginal or anal sex; sex with an HIV infected person; sharing injection –drug-useequipment; sharing unprotected insertive sex toys; and acquisition of other sexually transmitted infections. High prevalence populations: Groups that have a higher incidence and prevalence of HIV infection in B.C. include men who have sex with men (MSM), people who use injection drugs, Aboriginal persons, incarcerated populations, sex workers and their clients. Lot number: The lot number is the 6-digit number which appears on the label on the outside of each box of 24 test kits. When discussing a box of test kits, only the lot number on the outside of the box is to be used. Non-Regulated Care Providers (NRCPs): Care providers who are not regulated by a regulatory body / College falling under the Health Professions Act (BC Laws 1996). This may include community outreach workers, community health workers, peers, care aids and non-regulated counselors, etc. DEFINITIONS Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 5 Point of Care (POC) HIV test KIT The supplies provided by the manufacturer to do one HIV test by Point of Care. These supplies include fingerpoke supplies, 1 test membrane, 1 each of solutions 1, 2, 3. Point of Care (POC) HIV test: POC HIV tests (or rapid HIV tests) are screening tests for antibodies for HIV. These tests are licensed by Health Canada for use by health care providers in clinical or laboratory settings, typically providing results within minutes. Point of Care HIV Test Site: Location supported by and meeting the expectations of the BC Point of Care HIV Test Program and the geographic Health Authority within which the site is found. Such sites are provided with publically-funded resources and support to provide HIV tests by Point of Care to clients in their communities. Point of Care Site Lead: The individual with the overall responsibility for ensuring that: the quality and technical aspects of POC HIV testing are conducted at each site; the ordering of test kits and supplies is completed; and the monthly reporting and ongoing training and competencies of staff are maintained. Point of Care HIV Test, Invalid result: An invalid interpretation is made when the IgG/control dot does not turn blue, or cannot be seen against the background. This result indicates that there is a problem either with the testing process, the control material, or the testing device. Often this is the result of an insufficient blood sample. Another POC test should be attempted on the client, correcting the original problem. If this repeats a second time, send a venous sample for laboratory HIV testing, and run QC to ensure the test kits are accurate. Point of Care HIV Test, Indeterminate result: A test result where there is only a blue ring around the test dot area, rather than a full blue dot, as is expected if the reaction is reactive. Treat as if the result is reactive, and counsel based on the results of the confirmatory test. Indeterminate results may be an indication of early HIV infection or may be a false positive. Point of Care HIV Test, Non-reactive result: If a client’s point of care HIV test is non-reactive (negative), it is considered a final result and further testing is not required. For clients that may have a higher likelihood of being acutely infected with HIV and may be in the window period, standard HIV testing should also be offered (as standard testing has a higher sensitivity for detection of acute HIV infection). DEFINITIONS Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 6 Point of Care HIV Test, Reactive result: If a client’s POC HIV test result is reactive, it is considered a “preliminary positive”. A venous blood sample must be collected for confirmatory testing by standard HIV testing. All reactive results are reported to the local Medical Health Officer or Designated Nurse. Preliminary Positive A reactive POC result is considered to be preliminary positive, is reported to the MHO or Designated Nurse, and is confirmed by standard HIV laboratory testing. A final result is reported as “preliminary positive” if the result has NOT been confirmed by standard HIV laboratory tests. Proficiency Test (PT) A high-level Quality Assurance activity that involves a group of testing sites performing the same test on the same unknown samples(s). Results are analyzed for all results and the resultant report compares the site performance to the group. Quality assurance (QA): All planned and systematic activities implemented within the quality system that can be demonstrated to provide confidence that a product or service will fulfill the requirements for quality. Quality control (QC): The activities undertaken to verify the accuracy of a test result or the operational techniques and activities used to fulfill requirements for quality. Quality control materials (also referred to as quality control samples or “triplet”) are to be tested to ensure each lot of POC HIV test kits is reacting and performing as expected, and to assess that a tester can see the colour reaction of a weak positive, under the test environment lighting levels. QC “Triplet”: The set of vials needed to complete one QC test. The set consists of 1 HIV-negative, 1 HIV-1 positive and 1 HIV-2 positive vial. All 3 vials must be tested at the same time to assess performance of the test kit, tester and testing environment. Regulated allied health care professionals: Professionals for whom HIV testing does not traditionally lie within scope of professional practice (e.g., non-physician, nonregistered nurse). This may include dentists, pharmacists, chiropractors, physiotherapists, massage therapists, occupational therapists, dietitians, social workers, etc. DEFINITIONS Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 7 Standard HIV test: Standard HIV testing requires collection of a venipuncture sample for laboratory-based testing, which is a two-step protocol combining screening (i.e., enzyme-linked immunoassay, EIA) and confirmatory (i.e., Western Blot) testing. The result of standard HIV testing is considered final. Turnaround time for test results is typically within one week. Test Results See Point of Care Test Definitions, Confirmatory Test, False Positive, False Negative, Preliminary Positive Tester Individual who does HIV POC tests. This person is aligned with a HIV POC site, and meets site, Health Authority and Provincial Program training and competence requirements. Trauma Informed Care Trauma Informed Practice Interpersonal trauma will be defined as experiences involving disruption in trusted relationships as the result of violence, abuse, war or other forms of political oppression, or forced uprooting and dislocation from one’s family, community, heritage, and/or culture. True Positive: A true positive result is reported based on confirmation of a POC reactive or indeterminate result by standard HIV laboratory test results. Voluntary HIV testing: A confidential process that allows a person to discuss HIV acquisition and transmission with his or her health care provider, to decide whether to be tested, and to receive follow-up support upon receiving test results. Voluntary HIV Testing includes both provider- and client-initiated testing. Window period: The time between infection with HIV and the detection of HIV by a diagnostic test. The window period may vary between different HIV test products or protocols. DEFINITIONS Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 8 SECTION I: 1.0 OVERVIEW AND INDICATIONS FOR POC HIV TESTING BACKGROUND Point of care (POC) HIV tests (also known as “rapid” HIV tests) are screening tests for HIV antibodies which can be performed on-site while the client waits, and provide results within minutes. If reactive, the result is preliminary only and needs to be confirmed using standard serology. In Canada, one POC HIV test product has been licensed for use in health care settings: the INSTI™ HIV-1/HIV-2 Rapid Antibody Test (bioLytical Laboratories; hereafter referred to as the INSTI™ HIV Test). For more detailed information about this product, please refer to Appendix I – Summary of Test Properties. In August 2010, the B.C. Centre for Disease Control (BCCDC), an agency under the Provincial Health Services Authority (PHSA) was asked by the B.C. Ministry of Health to introduce a centralized, province-wide HIV point of care (POC) testing, distribution, and quality assurance program. This program is funded through a provincial program, Seek and Treat for the Optimal Prevention of HIV/AIDS (STOP HIV/AIDS). Through this program, BCCDC supplies POC HIV test kits to the regional and First Nations health authorities, to support HIV testing at designated POC testing sites. 2.0 PURPOSE The purpose of this manual is to provide guidance regarding the implementation and use of POC HIV testing in B.C. for approved sites in order to maximize the quality of POC HIV testing both within each site implementing POC HIV testing and for the province overall. This manual outlines guidelines for programs or sites adopting POC HIV testing. Included in this manual are recommendations and procedures for the appropriate use of POC HIV test kits; and quality assurance components required for use with POC HIV test kits, such as staff training, documentation, purchasing and inventory control. This manual does not address pre- and post-test discussions surrounding POC HIV testing; these are separate guidelines located in Chapter 5 of the Communicable Disease Control Manual and can be found at www.bccdc.ca. These guidelines are broadly applicable to any site in B.C. offering POC HIV testing. Some sections, such as purchasing and inventory control, and reports and documentation, are specific to sites receiving POC HIV test kits through the provincial program. 3.0 EPIDEMIOLOGY OF HIV INFECTION IN B.C. The number of HIV tests performed in B.C. continues to increase. In 2013, 258,964 HIV tests (venal blood draw) were conducted. Of the 258,964, 19% (n=49179) were prenatal. In addition, 10,254 POC tests were performed in 2013. The highest number of new positive HIV test results is reported in men who have sex with men (MSM), heterosexual populations, and people who use injection drugs (IDU). Aboriginal persons SECTION I: OVERVIEW AND INDICATIONS FOR POC HIV TESTING Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 9 are over-represented among new positive HIV tests, particularly Aboriginal females. For the most recent data on recent trends in new positive HIV tests in B.C., please see the Annual Surveillance Reports (at http://www.bccdc.ca). The Public Health Agency of Canada (PHAC) estimates that in B.C. in 2008, there were between 280-540 incident HIV infections (of which 50% were MSM, 25% were IDU, and 21% were heterosexual from non-endemic countries). The prevalence of HIV in B.C. was estimated at 11,400 persons (range 9,300–13,500 persons), of which 50% were MSM, 25% were IDU, and 25% were heterosexual. Nationally, an estimated 26% of HIV positive persons are unaware of their infection. 4.0 POLICY FRAMEWORK Common objectives among HIV-related strategies in B.C. are the prevention of new HIV infections, reducing the number of HIV positive individuals who are unaware of their HIV status, and linkage of HIV positive individuals to care, treatment, and support services. Expansion and increased availability of HIV testing is one strategy identified in B.C. at provincial and health authority levels to help achieve these objectives, and is a critical component of the STOP HIV/AIDS Program. Expansion of testing is considered one component of comprehensive HIV-related services, generally with emphasis on regional populations with a higher prevalence of HIV infection, and as a means of connecting people with HIV to appropriate care and support. Expansion of testing into rural and remote communities has also been identified as a priority. Other common themes include the importance of pre- and post-test discussions, and integration of HIV testing with testing for Hepatitis C (HCV) and other sexually transmitted infections. Testing to prevent perinatal transmission of HIV, and to a lesser extent occupational transmission of HIV, is also identified. National strategies endorse HIV testing accompanied by pre and post-test discussions as an effective early intervention (by linkage to care) and an effective prevention strategy (by supporting the reduction of transmission in individuals with positive HIV tests). Three key elements must accompany HIV testing. Testing must be: confidential, accompanied by pre- and post-test discussions, and conducted with informed consent. 5.0 COMPARISON OF POC & STANDARD HIV TESTING The INSTI™ HIV Test has similar sensitivity and specificity compared to standard HIV screening tests (Sensitivity, Specificity > 99%). While a non-reactive (negative) result is considered final (unless the person is tested early during the phase of acute infection and is in the window period), false reactive (positive) results can occur. False reactive results are more likely in a setting with a low prevalence of HIV (e.g., a setting where the population being tested for HIV has a low risk of infection). SECTION I: OVERVIEW AND INDICATIONS FOR POC HIV TESTING Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 10 With standard HIV testing, confirmatory testing immediately follows positive screening tests in the lab and the result returned to the patient is final. With a reactive POC HIV test, the result is conveyed to the client as a preliminary result, and collection of a blood sample by venipuncture for confirmatory testing is required in order to provide the client with a final result at a later date. With standard HIV testing, a follow-up visit is required for receipt of results. The same applies to POC HIV testing if the result is preliminary reactive; however, if the POC HIV test is non-reactive, a follow-up visit is not required (if the client is outside of the window period). An individual with a non-reactive POC HIV test may be in the window period (i.e., prior to the development of a strong antibody response). Standard HIV screening tests are more sensitive than the INSTI™ HIV Test for detecting acute HIV infection, due to window period differences (see page 18 for more information). Typically, testers find POC HIV tests to be easy to use. Unlike machine-read results for standard HIV testing, interpretation of POC HIV tests is subjective. Inter-reader variability in test interpretation is low, although variability may be greater in early HIV infection when a reactive result may be faint and difficult to see. Unlike standard HIV testing, the tester and site administering the POC HIV test assumes the responsibility for quality assurance activities to ensure that the test is carried out correctly. With standard HIV testing, positive HIV results are reported to public health for partner notification through a routine, established surveillance system. With POC HIV testing, all reactive POC HIV test results are to be reported to Medical Health Officer or Designated Nurse by the tester/site. 6.0 7.0 POTENTIAL BENEFITS OF POC HIV TESTING POC HIV testing is highly acceptable to, and preferred by, many clients presenting for testing as well as testers. Use of POC HIV testing may increase uptake and volume of HIV testing. Individuals undergoing POC HIV testing will receive their POC test result, particularly if they are HIV negative. Receipt of a final HIV positive result may not differ from standard testing, although individuals may be more likely to return for receipt of confirmatory test results. The rapid turnaround time associated with POC HIV testing can guide urgent decisionmaking to prevent transmission of HIV infection or to improve patient care. POC HIV testing may be a viable testing option for individuals where venipuncture is difficult or has been unsuccessful. POTENTIAL HARMS OF POC HIV TESTING SECTION I: OVERVIEW AND INDICATIONS FOR POC HIV TESTING Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 11 8.0 POC HIV testing may lead to decreased uptake of testing for other infections (e.g., Hepatitis C, syphilis). As POC HIV testing is not laboratory-based or automated, there may be greater potential for user error or other site-specific factors to influence the quality of testing. Increased incidence of subsequent sexually transmitted infections has been reported in clients getting a POC HIV test in comparison to clients testing through standard protocols, possibly due to dis-inhibition on receipt of a non-reactive test result or compression of preand post-test discussions into a single visit. With POC HIV testing there may be missed opportunities for partner discussion and referral (and prevention of further HIV transmission) if clients are lost to follow-up after receipt of a reactive result without confirmatory testing. GENERAL REQUIREMENTS The following are general requirements for locations adopting POC HIV testing. Detailed information is found in Appendix II (Roles and Responsibilities). A Readiness Checklist is available on the Provincial Program webpage. 9.0 POC HIV testing is confidential, accompanied by pre and post-test discussions, and conducted with informed consent. Testing is conducted by providers who have been trained to deliver HIV pre- and post-test discussions and how to use POC test kits. Recommended quality assurance measures are in place (e.g., training/competence, documentation, monitoring of test outcome, use of quality control test kits, etc). Where feasible, clients presenting for HIV testing should be offered a choice of standard or POC HIV testing. Clients are encouraged to test for other infections as appropriate (e.g., HCV, syphilis). Capacity exists within the testing framework to provide additional support to clients and providers at the time of a reactive POC HIV test and to facilitate standard confirmatory HIV testing. Providers have knowledge of local care pathways and community resources available to clients who test positive for HIV. Reactive POC test results are reported to the local Medical Health Officer or Designated Nurse by the tester/site. INDICATIONS FOR POC HIV TESTING This section provides guidance regarding the appropriate use of POC HIV testing in B.C. In particular, this section suggests clinical scenarios and voluntary HIV testing settings where POC HIV testing is most indicated. These indications are based on the current epidemiology of HIV transmission in B.C., current policy frameworks for HIV testing, and a review of the evidence of impact and use of POC HIV testing. Information on expansion to Non-regulated or Allied Health Providers as testers can be found in Section IV, but Sections I to III apply to all sites and testers. 9.1 Clinical Scenarios Where There is an Urgent Need to Determine HIV Status SECTION I: OVERVIEW AND INDICATIONS FOR POC HIV TESTING Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 12 As with standard HIV testing, providers need to use best practice judgment based on the history of risk exposure, potential for acute or early infection, and knowledge of the POC HIV test window period when acting on the result of POC HIV tests. 9.1.1 Pregnant women near term or in labour with undocumented HIV status or ongoing risk of HIV infection in pregnancy The risk of transmission from a mother with HIV infection to her infant is substantially reduced if antiretroviral medications are administered to the mother during pregnancy, labour or delivery or to the infant shortly after birth. POC HIV testing of women near term or in labour with undocumented HIV status or ongoing risk of HIV infection provides an enhanced opportunity for rapid identification of HIV infection and initiation of antiretroviral therapy to reduce the risk of HIV transmission to the newborn.i 9.1.2 Testing of the source individual during blood and body fluid exposures Knowledge of the HIV status of source individuals during the evaluation of blood and body fluid exposures can guide decision-making regarding the administration of postexposure prophylaxis. POC HIV testing of source individuals reduces the time to result availability and may avoid unnecessary post-exposure prophylaxis and anxiety in the exposed person.ii 9.1.3 Clinical diagnosis of acutely ill patients Patients may present for emergency care where rapid knowledge of HIV status may improve quality of care by guiding further diagnostic workup or treatment (e.g., patients with a clinical presentation compatible with opportunistic infections). 9.2 HIV Testing Settings There are no set criteria for determining whether POC HIV testing should be offered in a specific HIV testing setting (broadly defined to include clinics, outreach programs, needle exchanges, etc). Rather, sites should be determined by Regional Health Authorities and First Nations communities according to local priorities for expanding and engaging populations in HIV testing, and with consideration at a regional level of sites where the potential benefits of POC HIV testing outweigh the potential harms (section 6.0, 7.0 above). A further consideration is whether voluntary testing settings have the infrastructure and resources required to adopt POC HIV testing (section 8.0 above; Appendix II). Examples of voluntary HIV testing settings where POC HIV testing is expected to have the most benefit include: i Refer to Oak Tree Clinic, B.C. Women’s Hospital and Health Centre for guidelines regarding HIV testing and management in pregnancy (www.bcwomens.ca/Services/HealthServices/OakTreeClinic/default.htm) ii Refer to BCCDC guideline “Blood and Body Fluid Exposure Management (March 2010)” in the CD Control Manual (www.bccdc.ca) SECTION I: OVERVIEW AND INDICATIONS FOR POC HIV TESTING Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 13 9.2.1 Settings accessed by populations where the prevalence of undiagnosed HIV is expected to be higher Compared to sites in the region offering standard HIV testing, POC HIV testing may lead to increased uptake and volume of HIV testing. Use in these settings where the client population is known or suspected to have a higher prevalence of undiagnosed HIV may contribute to reducing the proportion of HIV positive individuals who are unaware of their HIV status. 9.2.2 Settings accessed by populations where not returning for test results is common among those tested Receipt of a positive HIV result has been demonstrated to lead to a reduction in risk behaviour. POC HIV testing has been demonstrated to improve the receipt of final test results. In settings where a high proportion of clients are tested and do not return to find out their test results, POC HIV testing may be of benefit, particularly where failure to return is common among HIV positive individuals. 9.2.3 Settings accessed by populations where provision of a POC HIV test result will improve public health follow-up or connection to HIV clinical care For example, presentation for medical care, admission to facilities, or other services may provide opportunities to engage individuals in testing. However, as the tester may not be the patient’s primary health care provider, and rapid patient turnover within facilities is common, receipt of test results, follow-up by public health of positive results, and connection to HIV care may be difficult. In such settings, POC HIV testing with immediate identification of individuals with reactive HIV results may improve follow-up and connection to care. 9.2.4 Settings accessed by populations with low rates of testing where POC HIV testing may lead to increase uptake of testing The convenience and ease of testing due to rapidity of result, and requirement for a single visit (if negative) may be appealing and lead to increased test uptake. This must be balanced by the increased cost of this test and by the expectation of increased numbers of false positive results in a no-or low-risk population. POC may reduce the fear of confidentiality breach that may occur in small, remote or isolated communities. SECTION I: OVERVIEW AND INDICATIONS FOR POC HIV TESTING Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 14 SECTION II: PERFORMING THE TEST 1.0 KEY INFORMATION ABOUT POC HIV TESTING The INSTI™ HIV Test is used to screen for HIV antibodies in whole blood. POC HIV testing is confidential, accompanied by pre and post-test discussions, and conducted with informed consent. Guidelines for pre- and post-test discussions to accompany POC HIV testing are located in Chapter 5 of the Communicable Disease Manual (www.bccdc.ca). Where feasible, clients should be offered a choice of standard or POC HIV testing. Clients should also be encouraged to test for other infections such as syphilis or Hepatitis C as appropriate. Providers should have knowledge of local care pathways and community resources available to individuals who test positive for HIV. Quality Control testing of POC HIV test kits should be conducted according to recommendations (see Section III — Quality Assurance) prior to offering POC HIV testing. Any indication that POC HIV test kits are not performing properly should be reported to the POC Site Lead, the Provincial POC HIV Testing Program and the manufacturer. All test results and other relevant information such as lot number and expiry date, should be documented (see Section III — Quality Assurance). If a client’s POC HIV test result is: reactive This result is considered to be a “preliminary positive”. A venous blood sample must be collected to confirm the POC HIV test result for confirmatory testing by standard HIV testing. All reactive results are to be reported to the local Medical Health Officer or Designated Nurse and a plan should be made with the client to return for the confirmatory result. non-reactive This result is considered a final result and further testing is not required. For clients who may have a higher likelihood of being acutely infected with HIV and may be in the window period, standard HIV testing should also be offered (standard testing has a higher sensitivity for detection of acute HIV infection). Invalid This result cannot be reported. The test should be repeated with a fresh sample using a new membrane unit, kit components, and support materials. If the client has a second invalid result, standard HIV testing should be performed, Quality Control materials should be tested, and the POC Site Lead notified. Indeterminate A venous blood sample must be drawn and forwarded to a laboratory for HIV standard testing. SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 15 2.0 CONDUCTING THE INSTI™ HIV TEST 2.1 Test Schematic CENTREWELL TEST MEMBRANE 2.2 Flow Diagram for HIV POC Testing During a Client Visit Provide pre test discussion Perform the POC test Read test result Yes Negative Test (non-reactive) Positive Test (reactive) Indeterminate Test Invalid Test Post test discussion No Window period? Repeat with new sample and test kit Yes Provide post test discussion Client visit concluded Complete requisition and draw venous blood Schedule follow up appointment Wait for test result Provide post test discussion SECTION II: PERFORMING THE TEST No Second test valid? Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 16 2.3 Procedure for Conducting the INSTI ™ Test Prior to conducting the POC HIV test, check that the POC HIV test kits have not expired, and that quality control testing has been done as per the guidelines in Section III 3.0. Prepare for testing. 1. Wash or sanitize hands. 2. Prepare a testing area by disinfecting a non-porous level surface with an approved disinfectant. Note: Alternately a new, clean, blue pad may be utilized to contain the testing materials. 3. Gather the following materials: INSTI™ HIV Test kit, which contains: HIV test membrane each of reagent solutions 1, 2 and 3 alcohol swab single-use lancet single-use pipette capable of dispensing 50 uL gloves gauze or cotton ball for post-puncture wound coverage biohazard sharps/waste container 4. Select the finger to use for obtaining the blood sample. Note: Avoid using the index finger or thumb because these two fingers are usually more calloused than the other three fingers. Similarly, avoid the tip of the finger. 5. Massage and/or warm the selected finger to allow blood to flow to the surface. 6. Open alcohol swab and the Solution 1 vial (do not discard the lid). 7. Open the pouch containing the membrane unit. 8. Remove the test membrane from the pouch without touching the centre well. Position the test membrane on the level surface with the tab down (facing you). Note: If the centre well is touched, the HIV antigen molecules will be torn from the membrane and the test will not perform correctly. 9. Collect finger prick Put on gloves. 10. Wipe selected warmed finger thoroughly with alcohol swab and position hand at waist level or lower. Allow alcohol to dry before proceeding. SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 17 blood 11. Twist off the protective cap from the lancet and then pull the cap straight off. 12. Position the lancet device against the finger. Holding lancet body, press the lancet firmly against the finger. 13. Dispose the lancet directly into a sharps container. 14. Hold the pipette horizontally and touch the tip of the blood drop to the tip of the pipette. Note: The pipette will fill by capillary action; do not squeeze the pipette during filling. 15. Fill the pipette to the fill line to obtain the required amount. Note: It is very important to draw the correct amount of blood. If the puncture site does not yield a sufficient amount, a separate second puncture using a new lancet and pipette is required. 16. Place gauze over the puncture site and ask the client to hold it against the puncture site and to elevate the hand. 17. Transfer the blood from the pipette into the sample diluent (Solution 1) vial by squeezing the bulb of the pipette to dispense the blood into the vial (figure A). Note: If the blood does not expel from the pipette, hold the pipette vertically and slide a finger over the vent hole and squeeze the pipette bulb (figure B). SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 18 18. Dispose the pipette in a biohazard waste container. 19. Recap the vial (Solution 1 + sample), mix by turning upside down a few times. Note: Do not shake vigorously. Complete each of the following steps immediately. Testing – Using solutions 1, 2, 3 20. Carefully pour the entire contents of the Solution 1 vial into the membrane well. Note: If most of the solution has gone into the well but some has dripped on the side of the vial, continue the test. If the control dot appears the test can be interpreted. The test is built to ensure sufficient sample has been added when the control dot appears. 21. Wait until the solution is absorbed by the membrane (takes only a few seconds). 22. Mix the Colour Developer (Solution 2 vial) by slowly turning the vial upside down several times. Note: This solution should appear evenly suspended prior to adding to the membrane. 23. Open and add the entire contents of the colour developer (Solution 2) to the centre of the membrane unit. Wait until the solution is absorbed by the membrane (takes approximately 20 seconds). 24. Open and add the clarifying reagent (Solution 3 vial) to the centre of the membrane unit. Interpret the results 25. Read the result immediately and record the result. Clean up. 26. Discard the test membrane in a biohazard waste container. Note: If more than 5 minutes have passed since adding the clarifying solution (solution 3) the result is invalid. 27. Remove and discard gloves. 28. Decontaminate the work area with an approved disinfectant. 3.0 INTERPRETING THE TEST RESULTS 3.1 Procedure 1. Review the flowchart in Section II 2.2 (Flow Diagram for HIV POC Testing during a Client Visit) for information on interpreting the test result. 2. Read the test with the tab in the lower position from the membrane. 3. Interpret the test according to the instructions in the table on page 15. 4. Interpret the test and convey the result to the client. 5. Record the test result as per instructions in Section III, 5.1. SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 19 3.2 Table: Interpretation of HIV Point of Care Test Results (INSTI™) Result If the membrane shows: Interpretation: Next Steps: Non-reactive (negative) Only one blue dot at the top (farthest from the plastic tab): Test is valid Result is final. Antibodies to HIV-1 and HIV-2 have not been detected If client has signs or symptoms of acute HIV infection, blood sample should be drawn and sent for standard HIV testing. Test is valid A venous sample must be drawn and sent for standard HIV testing (to confirm the result and to rule out the possibility of a false positive result). Reactive (preliminary positive) Two blue dots appear, one above the other (one dot may be darker than the other). Antibodies to HIV-1 or HIV-2 have been detected Report reactive result to local Medical Health Officer, or Designated Nurse. Indeterminate One blue dot at the top. Faint background ring appears on the lower test dot. Invalid No blue dot at the top of the membrane; or blue specks appear; or there is a uniform blue colour across the membrane. Test is valid Antibodies to HIV-1 or HIV-2 may have been detected Test is invalid Something may be wrong with the test kit or the testing process A venous sample should be drawn and sent for standard HIV testing. Treat as a reactive result. Repeat with a fresh sample and new test kit making sure that sufficient sample has been collected for testing. If the second test is also invalid, a venous sample should be drawn and sent for standard HIV testing. Report invalid resultsX2 to POC Site Lead, and Program Lead. Use quality control samples to make sure that the test is operating properly. SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 20 3.3 3.4 Notes and Limitations The control dot may be darker or lighter than the lower, client/test dot. When there is a problem reading the test (e.g., shadows or rings), then two individuals should read the test, if possible. The names of both people reading the test(s) should be documented. Remember that results read more than 5 minutes after the addition of solution 3 are considered to be “invalid”. When more than 60uL of blood is used, the flow through the membrane may be slowed and produce a uniform blue colour across the entire membrane (an invalid result). It is extremely important to use the supplied capillary pipette to add the sample to solution 1. A client in the window period may have a false non-reactive test result. Clients who are more likely to be in the acute phase of HIV infection (i.e., have high likelihood of HIV infection) should be encouraged to have blood drawn for standard HIV testing at the same visit. A test that is performed using an insufficient sample, performed incorrectly or where a defective device is used, will give an invalid result and testing should be repeated. If the second POC HIV test performed is also invalid, quality control samples should be used to determine if the test kits are performing correctly. Notify the POC Site Lead and the Program after two consecutive invalid results. Venous blood samples should be drawn and sent to BCCDC for standard laboratory HIV testing. False non-reactive (negative) or invalid test results may be obtained from clients with hypogammaglobulinemia conditions (e.g., multiple myeloma), patients receiving HAART, and patients with elevated hemoglobin. Patients receiving HAART should not require POC testing. For patients with hypogammaglobulinemia, RNA or HIV antigen/antibody testing may be required. The INSTI™ HIV test has not been validated for detection of antibodies to HIV-1 Group N sub-group. Further Information Please contact the Provincial POC HIV Testing Program for further information about the test, interpretation of test results, or troubleshooting. 4.0 FOLLOW-UP TESTING It is essential to confirm all reactive or indeterminate POC HIV test results with standard laboratory HIV testing. In addition, a confirmatory lab sample should be drawn and sent for testing if a test results in two consecutive invalid results. Clinical judgment remains important in HIV testing. If you receive a “not indicative of HIV infection” or indeterminate standard HIV test result for a client who you consider to have a high likelihood of having an HIV infection, you may contact a medical or clinical virologist at the PHSA Laboratory to review the case and to determine if additional tests are indicated. Individuals (regardless of POC HIV test result) should be advised to get tested for other infections via standard blood testing where appropriate (i.e., syphilis, hepatitis B, hepatitis C). As with standard HIV testing, if the serology done to confirm a reactive POC results in a true positive result, a second blood test is recommended to confirm the diagnosis. This will help to SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 21 eliminate the low possibility of error that might result from sample handling errors such as mislabeling of submitted samples. Repeat testing is particularly recommended when the client’s history suggests a low risk for exposure to HIV or the client does not undergo subsequent viral load testing or connect with HIV primary care follow-up. 4.1 Procedure for Follow-Up Testing Samples can be collected on-site and transported directly to BCCDC Provincial Health Microbiology and Reference Laboratory for follow-up testing, or indirectly via another laboratory. Testing is most often done by the BCCDC lab, but may be referred to another site, based on Health Authority or site processes. Detailed instructions and quick reference guides for confirmatory testing are available on the Provincial HIV POC website. Contact the Provincial HIV Point of Care Program, if needed. General Instructions for All Collection Methods: 1. A laboratory requisition must be completed according to established procedure (BCCDC serology requisition or other), indicating whether HIV testing is to be reported nominally or non-nominally. Ask the client before including POC test results on the requisition. 2. If samples are collected off-site, then samples will be drawn and sent for testing, based on the Health Authority HIV testing practices. It is preferred if samples can be sent to the BCCDC lab, but may not occur. 3. If samples are collected on-site, then draw 1 gold top and 1 EDTA (purple) top tube. See the appropriate Guide to Lab Servicesiii for current information. All blood samples drawn and sent for testing must have 2 unique identifiers. Information used on the sample and requisition must match. Arrange for the sample to be transported to BCCDC Provincial Health Microbiology and Reference Laboratory for testing, per established process. 4. When the result of standard laboratory HIV testing is received, record the result in the client chart and on the Daily Log of Client POC Test Results (Appendix IV). Recording the result on the client log assists the person who completes the Monthly Inventory Log. For clients with an initial reactive or indeterminate POC HIV test result, record one of the following: iii Refer to PHSA Laboratories Guide to Programs and Services (http://www.phsa.ca/NR/rdonlyres/D632D3568E8F-4917-BC3D-463EB5F8A14B/0/GuidetoProgramServices.pdf ) SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 22 If standard lab test (confirmatory) result is Then record the following in client history and on Client Test Log: Indicative of HIV infection (positive) Not indicative of HIV infection (negative) Not done True Positive (TP) False Positive (FP) Preliminary Positive (PP) Include an explanation/investigation of, or reason for, discordant/differing results in the client record and on the client test log. 5. Notify the client of their confirmatory test result per site policy. Additional Steps for Testing Sites Sending Samples DIRECTLY to BCCDC Provincial Health Microbiology and Reference Laboratory: Write “STAT” on the upper right corner of the BCCDC requisition, and on any outer packaging, such as a paper bag or cooler. (This alerts the staff who sort samples and run the tests that this sample goes first, or to open this container first and send the STAT sample quickly to the lab.) If you collect and send a sample directly to BCCDC Lab, then write the POC result in the Comments section of the BCCDC Serology requisition. Note: This information will facilitate tracking of test results and may assist BCCDC Laboratory in determining the appropriate standard HIV tests to perform. If blood is to be collected or tested elsewhere, then discuss the addition of POC test results on the requisition with the client, as it may be perceived as a confidentiality breach if this information is put on the requisition. Complete the FAX template and send to BCCDC to alert them that a sample is coming (See Appendix III). This triggers a process in the lab so that they follow-up if the sample does not arrive when expected. Writing the POC result on the FAX preserves confidentiality as well as providing additional information to the lab staff. 4.2 Ruling Out Acute HIV Infection Some clients may be more likely to have an acute HIV infection; for example, individuals with symptoms of HIV seroconversion, or individuals who are likely to have ongoing or recent exposure to HIV. For these individuals, following a non-reactive POC HIV test, it is recommended to submit a blood sample for standard HIV testing. SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 23 A standard HIV test can detect HIV antibodies as early as 2-3 weeks after infection; POC HIV testing may take a little longer but can detect HIV antibodies as early as 3-4 weeks after infection. For both POC and standard testing, approximately 95% of people will have a reactive HIV test by 6 weeks after infection (>99% by three months). Standard HIV laboratory screening tests are more sensitive than the INSTI™ HIV Test, due to window period differences. In the event that a reactive POC HIV test is followed by a negative standard laboratory test, further testing can be requested by the clinician. If a recent high-risk exposure has occurred, or acute HIV infection (seroconversion) is suspected, indicate “query acute HIV” on the test requisition, provided the client agrees. SECTION II: PERFORMING THE TEST Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 24 SECTION III: QUALITY ASSURANCE Non-Regulated or Allied Health Care Providers: Information in this section applies to all sites, and testers. Specific information for NRACP is found in Section IV. Specific Competency and Training Program examples are found as Appendix documents. 1.0 OVERVIEW The objective of quality assurance activities is to ensure the delivery of a high quality, accurate and efficient POC HIV testing process, and to detect/prevent potential errors before they affect client results. Quality assurance activities must be practiced to ensure that test results are accurate and as reliable as possible, and to ensure confidence in the testing program and testers. For this reason, the overall responsibility for the quality and technical aspects of each site’s POC HIV testing should be assigned to one individual (the “POC Site Lead”). In B.C., quality assurance is a shared responsibility between testers, the POC Site Lead, the Provincial POC HIV testing program, the Health Authority, the PHSA Laboratory, and the POC HIV test manufacturer (bioLytical). While test sites (including hospital wards, clinics, outreach programs or other care settings) are not subject to laboratory accreditation standards, the quality assurance activities described in this section are based on the manufacturer’s recommendations and follow the same principles as those found in the Accreditation Canada Standards for Point of Care Tests (March 2012). 1.1 Reporting Concerns Regarding the Quality of POC HIV Tests Testers may be the first to suspect issues with the quality of POC HIV test kits, and/or controls. Potential indications that POC HIV tests may not be performing as expected include: Increases in the number of clients with invalid, indeterminate, or false positive results. Incorrect POC HIV test results with the use of quality control samples. Any concerns of this nature, including the lot number of the implicated POC HIV test kit or quality control test should be reported to: POC Site Lead; and Provincial POC HIV Testing Program Tel: 604-707-5635 Fax: 604707-2603 These reports will be investigated to determine if the issue may be related to an expected variation or impaired quality of the POC HIV test kit or quality control samples, or to staff performance (e.g., incorrect procedure). SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 25 2.0 TRAINING The most important part of the program is to ensure that all HIV POC testers are well-trained and can confidently perform and interpret the test. Records of training, competency and proficiency assessments should be maintained and be consistent with existing practice standards at each site. 2.1 Initial Training for POC HIV Testing Core HIV education and POC HIV testing training sessions are held regularly by BCCDC and health authority trainers. Training needs and appropriate mode of delivery are discussed as part of a new site set-up. For more information, contact the Provincial POC HIV Testing Program. Each site/Health Authority must define what additional observations or assessments, beyond the initial training sessions, must be met before a new tester is approved to offer POC HIV testing at that site. Training for POC HIV testing may include a combination of education offered by BCCDC and by the POC Site Lead as follows: BCCDC or Regional Health Authorities Pre- and Post-Test HIV discussion (as needed). Completion of one 2–3 hour training program on the use of test kits and quality assurance activities. POC Site Lead Demonstration of competencies (see Appendix V –Direct Observation Checklist and Appendix VII- Training Completion Requirements). HIV POCT online training modules are available through the PHSA Learning Hub. HIV Education (pre/Post Counselling) is also available online through the BCCDC Learning Hub. Training addresses POC HIV testing competencies for testers (please refer to the table in Appendix VI —Training Competencies). Once training has been completed, each trainee should independently demonstrate, at a minimum, the competencies described in Appendix VII —Training Completion Requirements, in the presence of their POC Site Lead. 2.2 Continuing Education and Ensuring Ongoing Competency for Testers Continuing education and ongoing competency assessment can be done by a variety of methods and should be scheduled by the POC Site Lead for testers depending on their level of experience with POC testing. SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 26 Competence assessment is usually done with new testers, and should be repeated at six months, then yearly as an ongoing assessment. Competence may be assessed more often for low-volume test sites (< 5 diagnostic tests/month). Competence should include assessments of counselling skills as well as use of the Point of Care Test. Possible ways to provide continuing education related to POC and to ensure ongoing competency for testers are listed below: 1. Interaction with Testers Informal assessments can be done whenever the POC Site Lead is at the site, participating in, or observing, daily activities. 2. Review of daily log of client POC test results (Appendix IV) and Quality Control Log (Appendix IX) It is recommended that the POC Site Lead review these documents at a minimum of once a month as an opportunity to assess how testers are performing and provide follow up as necessary. This can be done at the same time as information is gathered to complete the Monthly Inventory Report. 2.3 3. Direct observation of tester It is recommended that refresher training occur whenever there is a problem or issue identified or on a regular basis for staff, especially those who do not perform POC HIV tests regularly (see Appendix V – Direct Observation Checklist). 4. Regular reviews with testers in a meeting setting Discussions with testers in a meeting setting can facilitate sharing of experiences with test kit usage and allow the POC Site Lead to gauge competency and comfort levels of testers and discuss learning needs. 5. Investigation of errors This is an opportunity to assess how testers are performing based on the findings of an error or nearmiss event. These investigations are also an opportunity to discuss testing and to review documents. 6. Proficiency Testing: See below. Proficiency Testing Proficiency Testing (PT) is a higher-level Quality Assurance activity that is conducted two to three times per year when an external provider sends unknown testing materials to all testing sites. Each site is expected to test the unknown materials and enter their results into an online database. Once all the results have been entered, each site will be able to compare SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 27 themselves to other sites (note: names of other sites participating in the PT program will not be visible to other users) and identify if there are concerns with testing at their site. Participation in a PT program is an expectation for each site participating in the provincial POC HIV testing program. It is an important tool that can be used by the site and the provincial program to verify the accuracy and reliability of POC HIV testing results in order to protect patient safety. PT differs from Quality Control (QC) testing as it should assess the entire testing process, involves the testing of unknown samples and anonymously compares the performance of all sites participating in the program. The provincial POC HIV testing program will contract the services necessary for PT with an external provider on behalf of sites affiliated with the provincial program. Costs for PT are assumed by the provincial POC HIV testing program. The provincial program will be able to see the results from participating sites, but the identity of individual testers will not be included in the results database. 3.0 USING QUALITY CONTROL SAMPLES Quality Control (QC) samples are produced by the manufacturer (bioLytical). QC checks the stability and function of the test kit, the tester’s eyes and the lighting conditions in which the test is run. Since the result is a visual colour, it is critical that each tester is able to detect a weak reactive result and to distinguish between a nonreactive and a weak reactive result in the lighting conditions of the test environment. Each box of QC samples contains 36 vials, consisting of an equal number of: anti-HIV-1 positive control, anti-HIV-2 positive control and HIV negative control. Each vial should be sufficient to conduct to 4-5 tests (144-180 tests total/ box). The samples are shipped at ambient temperature and should be frozen on receipt by the site. The materials will last up to one year if they remain frozen at -20ºC. Once thawed, they last 28 days when refrigerated at 2-8ºC. Samples are warmed to room temperature (approximately five minutes) and mixed before use. QC samples are made from human sera and should be treated as a biohazard risk, albeit, a low risk. Sites should follow biosafety rules regarding storage, handling and disposal of QC samples. Quality control samples should be stored in a freezer in the plastic container in which they are shipped and enclosed in a biohazard bag. Once thawed, vials can be stored in a refrigerator in a labeled, leak-proof container. When used on a regular basis, QC samples provide assurance that the HIV test results being given to clients are valid and accurate, and can be used to fulfill competence needs. 3.1 Frequency of Use SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 28 It is a Provincial Program expectation that all sites will test QC samples per manufacturer’s recommendations, but at a minimum of once per month. If QC fails, the accuracy of results since the last QC success is in doubt. Sites must balance how often QC samples are tested with the number of clients who would have to be retested in the event of a problem with the test kits. For sites doing few tests per month (0-25), the once per month minimum is reasonable as the number of clients that would need to be retested is minimal. For sites that do many (25 or more) tests per month, regular use of QC samples may be increased (e.g. once per week). 3.2 Indications for Use of QC Samples The manufacturer recommends that QC be run at the following times: for newly trained testers prior to actually using the POC HIV test kit on clients when a site receives a new shipment of POC HIV test kits when there is a change in test kit lot number when a site receives a new shipment of quality controls (usually once per year) if the temperature of the storage or testing area falls outside of the manufacturer’s specified temperature range (less than 15°C or greater than 30°C) when two consecutive invalid results occur with the same client Indications for when to run QC samples are included at the bottom of the QC Log (Appendix VIII). It is recommended that the reason for testing should be included on the log to aid the identification of potential opportunities for improvement. When QC samples do not provide the expected results and it has been determined that there is a problem with the test kits, or QC failures are unresolved, none of the tests used since the last time QC samples were used with correct results can be considered valid. Contact the Provincial POC HIV Testing Program immediately as client retests, or a product recall, may be required. 3.3 Overview of the Use of QC QC assesses the test, the tester’s eyes and the light conditions under which testing is done. When testing QC samples, use one set of controls “triplet” (one each of anti-HIV-1 positive control, anti-HIV-2 positive control and negative control) and a separate pipette for each of the three controls for a total of three POC HIV test kits and 3 QC pipettes. Ideally, a different tester does QC testing each time, or, at a minimum, the same tester should not always be conducting the QC testing, so that all testers are comfortable with the process, and testing is done even in the absence of the “assigned QC tester”. The positive control samples are intentionally weak positives to simulate a critical point in early infection, where antibody levels of the client may be barely high enough to be detected by the test kit. It is critical that all testers are able to see this weak reaction, using the light conditions under which client tests are done. When performing QC testing, it is recommended that sites rotate testers each time QC is done, or follow a “View or Do” model for quality control. The “View or Do” model encourages SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 29 those performing QC testing to show the results to their colleagues so that as many test kit users as possible have the opportunity to see what reactive and non-reactive results look like. Using this technique reminds a larger number of testers of the weak positive, without using a large number of test kits. Contact the Provincial POC HIV Testing Program for suggestions as to how this may be done at a site. 3.4 Quality Control Failure When the QC results seen on the test membrane do not agree with the expected result, QC is determined to have “failed” and an investigation into what caused the problem is necessary. This event should be reported in the site’s error/accident/corrective action reporting system. In the event of a QC failure, record the QC result and inform the POC Site Lead as soon as possible. Client POC HIV testing must be stopped immediately, until the cause of the failure is found and corrected. It is important to review the testing environment for factors that could have caused the QC failure. Do not continue to use QC samples until you get a “correct result”. It is a good practice to start an investigation by excluding more-common errors such as mix-up of control materials, reagents, pipettes and missed steps in the use of QC. Other important areas to investigate are: recent changes to the test or testing environment QC storage conditions QC expiry date/contamination pipette used for testing 3.5 Suggested Actions if QC Fails: FIRST – assess why the failure occurred, then repeat use of QC samples from the SAME vial if the assessment suggests a procedural error. If QC fails again: repeat test using a FRESH vial taken from the freezer If QC fails again: repeat test using a test kit from a newly opened box with the newly opened QC vial. if QC fails again there may be a problem with the test kit lot. STOP CLIENT TESTING. Notify the POC Site Lead and the BCCDC POC HIV Program Lead IMMEDIATELY. When QC samples do not provide the expected results and it has been determined that there is a problem with the test kits, or QC failures are unresolved, none of the tests used since the last time QC samples were used with correct results can be considered valid. SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 30 This means that all clients tested since the last use of QC samples with correct results will need to be called back and retested (unless a confirmatory test was ordered). A recall of the test kit or control products may be indicated. 4.0 PERFORMING A QUALITY CONTROL TEST 4.1 Quality Control (QC) Test Procedure (Using INSTI™ HIV POC Test Kit) Preparation Prepare test membrane Mix samples 1. Remove one HIV-1 positive, one HIV-2 positive and one negative QC vial from fridge or freezer and bring to room temperature (approximately 5 minutes). 2. Document the QC test information (lot number, expiry date) on the appropriate log. Note: vials expire 28 days after thawing if stored in the refrigerator. 3. Wash or sanitize hands. 4. Prepare a testing area by disinfecting a non-porous level surface with an approved disinfectant. Note: Alternately a new, clean blue pad may be utilized to contain the testing materials. 5. Gather the following materials: three INSTI™ HIV Test kits (one for each of the positives and negative control) three quality control pipettes gloves biohazardous sharps/waste container 6. Open one pouch containing the first membrane unit. 7. Remove the test membrane from the pouch without touching the centre well. Position the test membrane on the level surface with the tab down (facing you). Note: If the centre well is touched, the HIV antigen molecules will be torn from the membrane and the test will not perform correctly. 8. Label the membrane with the type of control (i.e., HIV negative, HIV-1 positive, HIV-2 positive) using a black or blue marking pen and place the membrane on a level surface. 9. Put on gloves. Note: All control samples should be handled as if capable of transmitting infectious diseases. 10. Gently agitate the 3 QC sample vials by inverting, or flicking, a few times. Tap the bottoms of the vials a few times on a hard surface to bring all the material from the cap back into the body of the vial. Pipette a sample 11. Unscrew the cap of the negative QC sample, and retain it. Unscrew the cap of solution 1, and retain it. SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 31 Hold both opened bottles in one hand. 12. Squeeze the bulb of the QC pipette very gently to push a small amount of air out of the pipette (do not use the capillary pipette). Hold the pipette vertically above the QC vial, lower the pipette into the vial, and then slightly release the pressure on the bulb to aspirate the QC sample from the vial. Fill the pipette just to the neck of the bulb. If you pull up sample into the bulb, squeeze gently to push excess volume out, retaining sample only in the “straight part” of the pipette. Solution 1 13. Move the pipette with sample above the opened solution 1 vial. Squeeze the bulb of the pipette to dispense the sample into solution 1. 14. Discard the pipette in a biohazard sharps/waste container. Recap the QC vial. 15. Recap . the solution 1 vial, mix by inverting the vial a few times. Carefully pour the entire contents of the solution 1 vial into the membrane well. Wait until the solution is absorbed by the membrane (takes only a few seconds). Note: If most of the solution has gone into the well but some has dripped on the side of the vial, continue the test. If the control dot appears the test can be interpreted. The test is built to ensure sufficient sample has been added when the control dot appears. Solution 2 16. Mix the color developer (solution 2 vial) by slowly turning the vial upside down several times. Note: This solution should appear evenly suspended prior to adding to the membrane. Open and add the entire contents of solution 2 to the centre of the membrane unit. Wait until the solution is absorbed by the membrane (takes approximately 20 seconds). Solution 3 17. Mix, open, and add the clarifying solution (solution 3 vial) to the centre of the membrane unit. Wait until the solution is absorbed by the membrane (takes approximately 20 seconds). Record results 18. Read the result immediately and record the result. Note: If more than 5 minutes have passed since adding the clarifying solution the result is considered invalid. SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 32 19. Discard the test membrane into a biohazard sharps/waste container. Repeat for HIV-1 control 20. Open and label a new membrane and repeat from step 11 with the second quality control (HIV-1). Repeat for HIV-2 control 21. Open and label a new membrane and repeat from step 11 with the third quality control (HIV-2). Clean up 22. Remove and discard gloves. 23. Decontaminate the work area with an approved disinfectant. 24. Check that the lids are tight on all QC vials. Place in labeled container with the expiry date (28 days after thaw) and store in refrigerator. 5.0 PROGRAM REPORTS AND DOCUMENTATION Managing the whole POC HIV testing process is critical to its success. It is recommended that testing sites develop and maintain standard operating procedures related to POC HIV testing, which are based on these guidelines and consistent with existing practice standards. These procedures should be reviewed per needs for each tester group; variant instructions for non-regulated or allied health professionals should be highlighted as necessary. Testing sites should retain all POC HIV test records according to their agency’s policy on retention of clinical records (or a minimum of two years if no such policy exists). This section outlines the minimum information that needs to be collected for the client, for quality control testing, and for monthly summary reporting. This information may be recorded and retrieved in a variety of different formats depending on the testing site (e.g., electronic charts, paper charts, testing logs). Templates of tools for this documentation are provided in the appendices of this document. Templates and modifiable versions are available on the Program webpage. ONLY the monthly summary report form is sent to the Provincial POC HIV Testing program. Other documents may be used by the site and the Provincial POC HIV Testing Program for troubleshooting, in the event of a recall, or in the event of a critical incident such as a quality control or a proficiency testing failure. 5.1 Documentation of Test Results for POC HIV Tests If information is manually written, it is recommended that it be as legible as possible. SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 33 For each client undergoing POC HIV testing, the following minimum information should be documented in the client chart and Client Test Log: Date of POC HIV test Client identifying information including contact information (2 unique identifiers are needed). Sites using electronic record-keeping may be able to use a chart number as identification on the test log. This enables rapid recovery of records should a recall occur. Tester Identification POC HIV test lot number and expiry date (found on the outside of the box of 24 kits) POC HIV test result (i.e., reactive, non-reactive, invalid, indeterminate) Whether a venipuncture for HIV serology was collected (or requisition for HIV serology given, if sample collection not available on site) Standard HIV serology result (i.e., reactive, non-reactive, invalid, indeterminate) Final classification of a reactive POC HIV test: o Preliminary positive (i.e., no standard serology performed, lost to follow-up) o True positive (i.e., standard serology is reactive) o False positive (i.e., standard serology is non-reactive) Testing sites are required to establish processes to: Monitor that clients with a reactive POC HIV test result have standard HIV serology performed, and that these results are received and reviewed by the site and with the client. Follow up when standard HIV serology and POC HIV test results are not the same. Rapidly identify all clients tested with a POC HIV test from a specific lot number, or that have a specific type of POC HIV test result (e.g. non-reactive, reactive, invalid) in case of a quality issue requiring investigation or re-testing. Extract information on key POC HIV test program indicators for reporting on a monthly basis (see section 5.2 below). While some testing sites may be able to use existing clinical information systems to meet the above requirements, an alternate approach is to establish a testing log. This testing log should be maintained in a central location and be completed for all POC HIV tests conducted at the testing site, and can be reviewed as required to meet the above requirements. A testing log template is provided in Appendix III — Daily Log of Client POC Test Results. 5.2 POC HIV Test Monthly Summary Reports In order to maintain an appropriate regional and provincial supply of POC HIV test kits, and to monitor the performance of POC HIV test kits at regional and provincial levels, testing sites are required to provide a monthly summary report to the Provincial POC HIV Testing Program which includes the following information: The number of POC HIV test kits (and their expiry dates), in inventory at the start and end of the month The number of clients tested by POC HIV test kits: o Number of clients with non-reactive POC HIV test results SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 34 o Number of clients with reactive POC HIV test results (total number, and numbers with final result being true positive, false positive or preliminary positive, based on standard serologic testing) o Number of clients with invalid POC HIV test results o Number of clients with indeterminate POC HIV test results The number of POC HIV test kits used for quality control testing The number of POC HIV test kits used for training and proficiency testing The number of test kits wasted The number of test kits expired and discarded This information is to be sent to the appropriate regional health authority contact person(s) and the Provincial POC HIV Testing Program by the end of the first week of the subsequent month. A template of a reporting form for this purpose is provided at Appendix IX — Monthly Summary Report. 5.3 Documentation of Quality Control Results Testing sites are required to document the results of all quality control tests performed, including: The type of quality control material (e.g., negative, HIV-1 positive, HIV-2 positive) Quality control lot number and expiry date on vial POC HIV test lot number (on the box of 24 test kits) POC HIV test result (reactive, non-reactive, invalid) If the result is invalid, then the log should show that QC was retested and passed. Inclusion of the reason (or probable reason) for the invalid result is good practice. This documentation should be maintained in a central place (often kept with the test kits) and reviewed monthly by the POC Site Lead to ensure that quality control testing is performed at the recommended frequency (see 3.0 above). It is recommended that a separate QC Log be kept and that the reason to run QC be included in the record. This makes it easier for the person gathering information for the Monthly Inventory Report to assess if an opportunity exists for improvement, or for preventive action, or if QC is being run at an appropriate level. 5.4 Incident Reporting Any incident involving POC HIV testing at a testing site should be reported to the POC Site Lead, according to local practice standards. The purpose of incident reporting is to be able to monitor and document unexpected or unintended outcomes so that a problem can be identified and corrected before client results are affected. Examples of incidents include: Unexpected results using quality control samples Inaccurate interpretation of POC HIV test results Temperature where test kits stored is higher or lower than requirements Use of expired test kits, or expired quality control materials SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 35 Testing sites may have established methods for incident reporting that can be used in these situations. Alternately, an incident log can be maintained to document all POC HIV testrelated incidents, which can be periodically reviewed by the POC Site Lead (see template in Appendix X). The POC Site Lead may determine that additional support and training may be required, and are recommended to contact the Provincial POC HIV Testing Program Lead in this regard. 6.0 PURCHASING AND INVENTORY CONTROL 6.1 INSTI™ HIV Test Kits Under the Provincial POC HIV Testing Program, the Provincial Program Manager arranges for the purchase of POC HIV test kits for participating Health Authorities and First Nations sites in B.C. Costs for these POC HIV test kits are paid from the Provincial Program budget; orders are placed on a quarterly basis up to an approved allotment. Through the Provincial POC HIV Testing Program, test kits are ordered in boxes of 24 (i.e., supplies to conduct 24 POC HIV tests). Individually packaged POC HIV test kits are not purchased through the provincial program. Regional and First Nations Health Authorities who require more POC HIV test kits than their allotment will be required to purchase these test kits independently. All questions regarding ordering POC HIV test kits can be directed to the Provincial POC HIV Testing Program. 6.2 Quality Control Materials and Other Supplies Costs for Quality control samples and related supplies are paid from the Provincial Program budget and ordered through the Provincial POC HIV Testing Program as required by each participating site. Other testing supplies such as extra lancets, quality control storage materials and temperature monitors can be ordered through the Provincial POC HIV Testing Program. 6.3 Inventory Control POC HIV test kits are shipped to participating sites designated by the Regional or First Nations Health Authority. It is the responsibility of each site/Health Authority or First Nations Health Authority to reconcile the number of test kits received against the number of tests performed. When test kits and quality control samples are received, it is recommended that each site notify the Provincial POC HIV Testing Program of the following: Number of POC HIV tests or quality control samples received. Lot number and expiry dates of test kits and quality control samples. Status of supplies (i.e. any damage). Note: POC HIV Kits come in boxes of 24 and each has a lot number and expiry date on the outside of the box. While the separate components of the test kits each have their own lot numbers, only the lot number and expiry date on the outside of the box needs to be recorded. SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 36 Unsuitable supplies include those that are expired, improperly stored, or damaged. Contact the Provincial POC HIV Testing Program to request pick-up/return/disposal of unsuitable supplies. Please refer to the Returning Unsuitable Supplies table in section 6.4. 6.4 Returning Unsuitable Supplies Determine the supply destination according to the table below. If supply involves: Expired INSTI™ HIV Test kits or quality control samples Improperly stored INSTI™ HIV test kit or quality control samples Action: Notify the Provincial POC HIV Testing Program with number and consult to prevent recurrence. Note: Kits may be transferred to a high use location prior to expiry through the Provincial POC HIV Testing Program. Quarantine the materials at the correct storage temperature while an investigation is underway. Report incident to the POC Site Lead and Provincial POC HIV Testing Program. Consider this as an opportunity to determine why this occurred and to prevent reoccurrence. Defective materials in kits or quality control samples Report incident to the POC Site Lead and the Provincial POC HIV Testing Program. Save the original material(s) in the event it needs to be sent to the Provincial POC HIV Testing Program. Improperly shipped/received or damaged materials Report incident to POC Site Lead. Contact the Provincial POC HIV Testing Program for instructions on how to proceed. Recalled INSTI™ HIV Test kits or quality control samples Quarantine affected supplies. Report incident to POC Site Lead and Provincial POC HIV Testing Program. Complete recall form and fax to Provincial POC HIV Testing Program. Follow Provincial POC HIV Testing Program instructions for return or disposal. 6.5 Monitoring Storage Temperature of INSTI™ HIV Test Kits Temperature monitoring is required to ensure that the INSTI™ HIV Test kits are stored between 15 °C and 30°C. A temperature monitor that measures maximum and minimum SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 37 temperatures over a given period of time should be stored with the POC HIV test kits, and a temperature monitoring log should be maintained (a sample temperature monitoring log is provided in Appendix XI). If the temperature monitor indicates that the ambient temperature has increased or decreased outside of the specified range, test kits should be moved to an alternate location for storage and the POC Site Lead should be notified. If test kits have been kept outside of the recommended temperature range (15 – 30°C) overnight or for extended periods in unmonitored locations/spaces, it is recommended that kits be quarantined, moved to a temperature monitored area, quality control samples used and the incident reported to the POC Site Lead. After using the quality controls and receiving valid results, the kits may be used for client testing. 7.0 OUTREACH AND MOBILE SITES The quality assurance recommendations in this section (i.e., use of quality control samples, training, documentation) apply equally to outreach and mobile sites. For these sites, the following should be considered. 7.1 Transporting / Storing Supplies Quality assurance requirements must be maintained wherever kits are stored (e.g., temperature monitoring). Kits should not be stored overnight or for extended periods in unmonitored locations/spaces (e.g., vehicles). 7.2 Testing Space A flat level surface must be available for testing staff to conduct the test on to avoid spillage (i.e., flat, level surface such as a carrying case and clipboard). The surface must be able to be decontaminated with a bleach solution or alternative method of maintaining a clean work surface that is not capable of transmitting infectious substances. 7.3 Waste Disposal Mobile sites must have biohazard waste disposal capability (i.e., biohazard waste or sharps containers). 7.4 Venipuncture Capability Outreach and mobile sites should either: a) be equipped and staffed to provide clients with venipuncture to obtain a sample for standard HIV laboratory testing if the POC HIV result is reactive, indeterminate or invalid, and/or if the client may have acute or early HIV infection. SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 38 b) establish a procedure to ensure that a venipuncture sample is collected (e.g., accompany clients to a nearby laboratory with a completed requisition for HIV testing). SECTION III: QUALITY ASSURANCE Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 39 SECTION IV: NON-REGULATED AND ALLIED HEALTH CARE PROVIDERS (NRACP) FRAMEWORK 1.0 PURPOSE This section is meant to provide additional support for sites involving non-regulated and allied health care providers (NRACPs) in POC HIV testing. Current evidence supports including non-regulated and allied health care providers as testers, showing that providers such as dentists, pharmacists, social workers, licensed practical nurses, counsellors, community members or “peers”, and community health workers (CHRs - in BC’s First Nations communities) are appropriate for the tester role. In some cases, NRACP may be more appropriate for and effective at engaging with people from high prevalence populations or communities. Although this Framework is primarily intended for non-regulated care providers, sites with regulated professionals with limited medical experience or HIV knowledge may wish to use it as a reference as well. Please refer to the recommendations for Regulated Care Providers. Regulated health care professionals with medical experience (physicians, nurse practitioners, nurses) should continue to use the existing Guidelines and are out of scope of this section. This Framework includes the following consideration and recommendations related to NRACPs and POC HIV testing: Definition of non-regulated care providers and allied health regulated professionals Framework components Key Management Considerations Recommendations for NRACP supervision Also included are tools to support training and implementation of NRACPs at POC HIV testing sites: Practice Guidance for Regulated Professional and Template for a letter of introduction for Professional Colleges (Appendix XII and XIII) Baseline qualifications for NRACP POC testers (Appendix XIV) Key competencies for NRACP POC testers (Appendix XV) Training Curriculum Outline (Appendix XVI) POC Policies and Procedures This framework is intended to outline considerations and provide recommendations specific to NRACPs performing POC HIV testing. It does not provide guidelines for POC HIV testing policies and procedures such as test performance and Quality Assurance (QA). For additional information on Policies and Procedures for performing POC testing and QA including provincial standards of practice for POC testing, please refer to sections II and III of this document. SECTION IV: NRACP FRAMEWORK Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 40 1.1 Definitions Non-regulated and Allied Health Care Providers For the purposes of this framework, other care providers who may potentially perform POC HIV testing fall into two additional categories: Regulated allied health care professionals for whom HIV testing does not traditionally lie within scope of professional practice (e.g., non-physician, non-registered nurse) (This may include dentists, pharmacists, chiropractors, physiotherapists, massage therapists, occupational therapists, dietitians, social workers, etc.). Please see Appendix XII for guidance related to POC HIV testing for regulated health care professionals. Non-Regulated Care Providers (NRCPs) who are not regulated by a regulatory body / College falling under the Health Professions Act (BC Laws 1996). (This may include community outreach workers, community health workers, peers, care aids and non-regulated counselors, etc.) 1.2 POC HIV Testing Settings with NRACP As stated in Section I 9.2, there are no set criteria for determining whether or not POC HIV testing should be offered in a specific setting. Sites considering the adoption of POC testing with NRACPs should be determined by Regional Health Authorities and First Nations communities according to local priorities for expanding and engaging populations in HIV testing. Factors such as cost/benefit and the infrastructure and resources available to support this type of expansion should be considered. Sites for NRACP POC testers could potentially include both community and acute care. 1.3 NRACP Framework Components SECTION IV: NRACP FRAMEWORK Provincial & Regional Laboratories Non-Profit & Private Services First Nations Health Provincial & Regional Public Health Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 41 Community & Client-Centered HIV/AIDS Services This Framework illustrates the basis for best practice in POC HIV testing by NRACP, the foundation of which is a strong commitment to community and client-centered HIV/AIDS health services, supported by stakeholders including provincial and regional public health and laboratories, First Nations Health services, and non-profit and private health services. With inter-sectorial support and buy-in, POC HIV testing among NRACPs can be realized through establishing and maintaining the components in the following sections. 2.0 ADVISORY COMMITTEE(S) A provincial advisory committee, consisting of management and community representatives involved in HIV testing, developed and approved this NRACP framework, created decisionsupport tools, and gathered information on the successes and challenges of implementation of POC HIV testing among NRACPs. A provincial HIV POCT Advisory/Accountability Committee will respond to practice concerns and will continue to create, inform, and revise policies related to the implementation of this framework, and other issues germane to the practice of HIV POC testing in the province. The committee consists of at least one key decision maker from each health authority who will have the authority to regulate POC testing supplies and designate new POC testing sites in consultation with the Provincial HIV POCT Program. SECTION IV: NRACP FRAMEWORK Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 42 3.0 RESOURCES AND INFRASTRUCTURE Resources and infrastructure needs related to NRACPs performing POC will depend on whether or not the setting is already a POC HIV testing site. For CURRENT HIV POC test sites: changes may need to be made regarding time required to perform client tests and quality control, and staffing changes to support new policies and procedures related to training, QC, supervision, and support of NRACP POC testers. Resources should also include codes of conduct and methods of redress for patients as well as NRACP POC tester supervision by a qualified medical staff experienced in POC testing. Testing and Quality Control materials may be self-procured by an organization directly from the manufacturer, or they may be supplied through the provincial or a regional affiliate program. Irrespective of who pays for test kits and Quality Control materials, for all sites, additional clinical materials (gloves, bandaids, sharps containers, etc) will need to be supplied and may affect the site’s operational budget. A site lead should be appointed to be in charge of inventory management, monitoring utilization of test kits, including documentation requirements (see Section III 5.0). As outlined in other sections, POC HIV tests should be: performed in a confidential setting accompanied by pre-test discussion include informed consent, post-test counselling and enable referral to primary care and supports Adequate infrastructure must include adequate private consulting spaces and lockable storage for medical records. Additional resources may be needed to assist community-based organizations in infection control, safe disposal of medical supplies, to conduct Quality Control (QC) tests (e.g., a freezer) and to provide follow-up counselling, support, and an established link to primary care and support services (See Appendix XVII for checklist). Follow-up testing recommendations are described in Section II 4.0 and include sending a confirmatory sample to the laboratory. Ideally NRACPs should have the capacity to complete confirmatory blood testing on site or create a clearly defined pathway to refer clients for a confirmatory test. 4.0 COMMUNITY READINESS AND MOBILIZATION Strategies are needed to increase access to and uptake of HIV testing for marginalized groups, particularly through innovative approaches such as offering POC testing at mobile clinics, harm reduction programs or outreach. NRACPs may be well-situated in communities to provide POC HIV testing linked to these services. Inclusion of NRACPs and members of client populations as testers and in the development of NRACP POC HIV testing program SECTION IV: NRACP FRAMEWORK Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 43 development, monitoring, and evaluation will help to ensure that the most appropriate and acceptable practices are followed. Marginalized communities in the province, especially rural, remote and many First Nations communities may face additional barriers to implementing POC HIV testing. They require culturally appropriate and safe supports to engage with the communities and to enable them to offer HIV POC testing in a manner that ensures confidentiality, increases awareness while reducing stigma, and connects HIV-positive clients to care available both in and outside of their communities. Linking to other programs and resources such as Chee Mamuk’s provincial HIV education programs is an essential step to assessing community readiness and mobilizing communities to offer and access HIV testing. Non-regulated care providers such as Community Health Representatives (CHRs) who have close ties to communities are well placed for providing culturally safe POC HIV testing, prevention, and linkage to care. 5.0 LINKAGES TO CARE, TREATMENT AND SUPPORT All HIV POC test providers should have knowledge of local care pathways and community resources available to individuals who test positive for HIV, as well as prevention services such as harm reduction supplies and services, for those testing HIV negative. Whenever possible, clients testing newly positive should be immediately linked to an appropriate HIV care provider in or near their community. Where possible, a partnership should be developed with a local clinic for further STI screening and reproductive services as well as support for new HIV positives. As part of new site implementation, each site is expected to contact clinics, laboratories, and the local public health unit to define this support for testers. Testers are expected to follow these defined linkages to support and care for their clients. 6.0 TRAINING AND COMPETENCIES As outlined in Section III 2.0, POC HIV tests should be performed by well-trained testers who can confidently provide and interpret this screen. Records of training, competency and proficiency assessment should be maintained and be consistent with standards of practice set forth by professional colleges and/or employers. NRACP training sessions should be made available through the BCCDC and regional health authorities. See Appendix XVI for sample modules titled “HIV Testing Education for non-regulated and allied health care providers.” There are no specific national or provincial requirements concerning who can perform a HIV POC test in BC. However, having qualified, trained staff to manage and perform POC tests, along with QA activities, is one of the most important factors for ensuring accurate and reliable results. Training for POC HIV testing is outlined in detail in Section III 2.0. Key aspects include qualifications, training, and competency assessment. See Appendix XIV for recommended baseline qualifications for NRACP POC testers which include various attitudes, knowledge, and skills. SECTION IV: NRACP FRAMEWORK Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 44 Similarly to regulated providers, pre and post HIV test discussion training is a prerequisite to POC HIV testing training. All NRACP trainings should include completion of a training program tailored to the NRACPs knowledge level as well as the demonstration of the ability to perform the POC and quality control tests correctly. In addition to the POC skills training, NRACPs may require special training and supervision regarding: informed consent and confidentiality HIV infection pathology care pathways healthcare ethics stigma and criminalization infection control and biosafety laboratory procedures Transport of Dangerous Goods (TDG) health records and documentation Training can be provided by BCCDC, by the regional health authority or by a combination of both. Training is crucial to ensure quality POC HIV testing. NRACP should be fully trained in performing the tasks and responsibilities associated with POC testing. The key components to include in training for NRACP POC testers are based on the core competencies outlined in Appendix XV. Training needs to be ongoing and linked to performance monitoring. Trained testers should be able to competently demonstrate use of the POC test kit and QC materials. Continuing education and ensuring ongoing competency for testers and activity examples are outlined in Section III 2.2. These activities are determined by the employers and can be done using a variety of methods. Assessments may be thorough without being complicated or time-intensive. 7.0 KEY MANAGEMENT CONSIDERATIONS When assessing the expansion or introduction of NRACP HIV POC testers, management / employer of the organization should be guided by expectations of these guidelines, and the following considerations: Who would be your local or regional medical contact for providing practice support to your NRACP POC testers (i.e. a physician, NP or RN)? Have you connected with the Provincial HIV POC Program to request inclusion in the provincial program for supplies? Has your request been authorized by your health authority liaison who will be accountable for your program? (Contact the Provincial HIV POC Program for more information.) Is your organization linked to your regional public health services and are there mechanisms for reporting HIV POC screening results and connecting clients for public health follow-up should they be HIV-positive? What program tools are available to support NRACPs in their work with clients? SECTION IV: NRACP FRAMEWORK Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 45 What professionals or partner organizations can the NRACP liaise with in order to get a confirmatory blood sample drawn on-site or a lab test ordered (e.g. physician, nurse practitioner, registered nurse, phlebotomist) should it be needed? What trainings (including pre-post HIV test discussion and HIV POC training) are available in your region and how would you support your staff to be trained and to receive ongoing support and assessment? What kind of accountability mechanism exists in your organization for unregulated care providers in the absence of professional regulatory bodies that govern health care professionals? Does the professional regulatory body of allied health regulated professionals (SW, pharmacists, etc.) support the practice of HIV POC testing? This may require special approval from their registrar for a pilot. (See appendix) Does your organization have a department of professional practice that supports this initiative? Does your organization have insurance for the testers in the event of any liability issues arising for POC HIV testing with NRACPs? Do you require any additional insurance? If testers are volunteers rather than employees within an organization, do they have insurance coverage under the employer or another source? This framework recommends that POC HIV testing be assigned by the Health Authority / employer to a regulated or non-regulated care provider by outlining it as a task that is within the role description and training of the tester as defined by the employer / supervisor and is integrated into their formal job description where possible. If registered health professionals such as physicians, nurse practitioners or registered nurses are present in the healthcare setting, it is recommended that employers develop formal processes to share responsibility for quality of care between these professionals and other care providers. An employer may choose to request that these professionals delegate or assign POC HIV testing whereby the physician or registered nurse/ NP maintains primary responsibility for the POC testing as a task. Please note that it is outside an LPN’s practice to designate such tasks. Please refer to Professional Standards and Guidelines for Delegation of Medical Acts according to the College of Physicians and Surgeons of British Columbia and the College of Registered Nurses of British Columbia’s Practice Support; Assigning and Delegating to NonRegulated Care Providers. For LPN practice please refer to the College of Licensed Practical Nurses website for LPN scope of practice information (contact information is in the Reference Section). 8.0 ACCOUNTABILITY AND SUPERVISION OF NRACPs To be included in the provincial POC program each health authority must designate a physician or nurse leader (e.g., MHO, Practice Lead for a Health Authority) as a liaison for POC testing to join the advisory council and authorize new sites in their region in consultation with the provincial HIV POC Program. This Health Authority person/team may provide practice support and opportunities for continuing education and assessment of NRACP POC SECTION IV: NRACP FRAMEWORK Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 46 testers in the community. Although organizations (e.g., Health Authority, NGO, etc) have legal and ethical responsibility for their employees who provide POC HIV testing as a part of their job, regional supports are crucial to maintaining clinical confidence and competence of testers. SECTION IV: NRACP FRAMEWORK Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 47 REFERENCES Accreditation Canada Point of Care Testing Standards March 1, 2012 BCCDC. BCCDC HIV Testing Training Videos. 2012. Available at: http://phsa.mediasite.com/mediasite/Catalog/Full/ae4cef7b1abf40a2aa647137536c00c121 BCCDC. Starting POC at Your Site. Available at: http://www.bccdc.ca/SexualHealth/Programs/ProvincialPointofCareHIVTestingProgram/Starti ngPOCHIVTest.htm BCCDC. Point of Care Site Resources. Available at: http://www.bccdc.ca/SexualHealth/Programs/ProvincialPointofCareHIVTestingProgram/POC SiteResources.htm#ProgTemp BioLytical.com website. (Accessed March, 2014). Available at: www.biolytical.com BC Laws. Health Professions Act. 1996. (Accessed March 2014).Available at: http://www.bclaws.ca/Recon/document/ID/freeside/00_96183_01 BC Office of the Provincial Public Health Officer. HIV Testing Guidelines for the Province of British Columbia. May 2014. British Columbia HIV Prevalence and Incidence Estimates used to Construct the 2008 National HIV Estimates: Updated December 7, 2009. Surveillance and Risk Assessment Division, Centre for Infectious Disease Prevention and Control (CIDPC), Public Health Agency of Canada. Burdge DR, Money DM, Forbes JC, Walmsley SL, Smaill FM, Boucher M, et al. Canadian consensus guidelines for the management of pregnant HIV-positive women and their offspring. Canadian Medical Association Journal (online), 1-14. 24-6-2003. Canadian Aboriginal AIDS Network (2012). Assessing community readiness and implementing risk reduction strategies. Available at: http://caan.ca/wpcontent/uploads/2012/05/CR-manual-eng.pdf Chansonneuve, D. (2007). Reclaiming Connections: Understanding Residential School Trauma among Aboriginal People. Ottawa, ON: Aboriginal Healing Foundation CLSI. A Quality System Model for Health Care; Approved Guideline. CLSI document HS01A2 Clinical Laboratory Standards Institute, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2002. CLSI. Quality Practices in Noninstrumented Point-of-Care Testing: An Instructional Manual and Resources for Health Care Workers; Approved Guideline. CLSI document POCT08-A. Wayne, PA: Clinical and Laboratory Standards Institute; 2010. College of Licensed Practical Nurses of British Columbia. Scope of Practice for Licensed Practical Nurses: Standards, Limits and Conditions. (Accessed April 2014) Available at: REFERENCES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 48 https://www.clpnbc.org/Documents/Practice-Support-Documents/Scope-of-PracticeONLINE.aspx College of Physicians and Surgeons of British Columbia. Delegation of a Medical Act. Professional Standards and Guidelines. (Accessed April 2014) Available at: https://www.cpsbc.ca/files/pdf/PSG-Delegation-of-a-Medical-Act.pdf College of Registered Nurses of British Columbia’s. Practice Support; Assigning and Delegating to Non-Regulated Care Providers. (Accessed April 2014) Available at: https://www.crnbc.ca/Standards/Lists/StandardResources/98AssigningDelegatingUCPs.pdf Cook D, Gilbert M, DiFrancesco L, Krajden M. Detection of early sero-conversion HIV infection using the INSTI™ HIV-1 Antibody Point of Care Test. The Open AIDS Journal, 2010; 4:176-179. Expert Working Group on Canadian Guidelines for Sexually Transmitted Infections. Canadian Guidelines on Sexually Transmitted Infections 2006 Edition. Public Health Agency of Canada 2006. Gilbert M. Impact and use of point of care HIV testing: a public health evidence paper. BC Centre for Disease Control; 2010. Available at: www.bccdc.ca under "Statistics and Reports". Hadland, S.E., Marshall, B.D.L., Kerr, T., Qi, J., Montaner, J.S., Wood, E. (2011). Suicide and history of childhood trauma among street youth. Journal of Affective Disorders, 136(2012), 377-380. Harris, M., & Fallot, R., D. (2001). Using Trauma Theory to Design Service Systems. San Francisco, CA: Jossey Bass Health Professions Act, Government of British Columbia, 2007. Hopper, E.K., Bassuk, E.L., Olivet, J. (2010). Shelter from the storm: Trauma-informed care in homelessness services settings. The Open Health Services and Policy Journal, 3, 80-100. INSTI™ test kit Manufacturer’s insert. INSTI™ HIV-1/HIV-2 Antibody test kit. bioLytical Laboratories Inc. Richmond B.C. 50-1028I. ©2012. INSTI™ HIV-1 Test controls. bioLytical Laboratories Inc. Richmond B.C. Product # 80-1037. 50-1045N. ©2013. Pearce, M.E., Christian, W.M., Patterson, K., Norris, K., Moniruzzaman, A., Craib, K.J.P., et al. (2008). The Cedar Project: Historical trauma, sexual abuse and HIV risk among young Aboriginal people who use injection and non-injection drugs in two Canadian cities. Social Science & Medicine, 66, 2185–2194 Peer Testing Project (VCH). Available at: http://www.catie.ca/en/pc/program/peer-testingproject. 2011 REFERENCES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 49 PHSA Laboratories, Central Processing and Receiving Laboratory. Mel Krajden. Unpublished data. 2014. PHSA Laboratories Guide to Programs and Services, BCCDC Public Health Microbiology & Reference Laboratory. April 2014. Available at: http://www.phsa.ca/NR/rdonlyres/D632D3568E8F-4917-BC3D-463EB5F8A14B/0/GuidetoProgramServices.pdf PHS Community Services Society. Peer HIV Testing. CATIE. Available at: http://www.catie.ca/en/pc/program/peer-testing-project PHSA Laboratories, Quality Manual. Vancouver, B.C. Version 2.00. February 2014. Plested BA, Jumper-Thurman P, Edwards RW. Community Readiness Manual and Community Readiness Toolkit. 2009. Available at: http://www.nccr.colostate.edu/order.html Policies, Procedure and Quality Assurance for Point of Care HIV Testing in Ontario. Ontario Ministry of Health, Aids Bureau. Sept 2008. Public Health Agency of Canada (2013). Human immunodeficiency virus HIV Screening and Testing Guide. Available at: http://www.phac-aspc.gc.ca/aids-sida/guide/hivstg-vihgddeng.php#a WHO Curriculum – Rapid HIV Tests: Guidelines for use in HIV testing and counselling services in resource-constrained settings, 2004. Available at: http://applications.emro.who.int/aiecf/web28.pdf WHO HIV Rapid Test Training Curriculum. 2010. Available at: http://www.who.int/diagnostics_laboratory/documents/guidance/hivrttraining_overview/en/ REFERENCES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 50 APPENDICES Many of the following Appendix documents are available on the Provincial Program webpage as PDF or customizable documents. Please download from the webpage rather than using versions found in the Guidelines. Link to Provincial Program webpage: http://www.bccdc.ca/SexualHealth/Programs/ProvincialPointofCareHIVTestingProgram/POC SiteResources.htm#ProgTemp Appendix documents applicable to all readers include: Appendix I to Appendix XI Appendix documents specific for Non-regulated or Allied Health Care Providers: Appendix XII to Appendix XVII APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 51 APPENDIX I — Summary of Test Properties INSTI™ HIV-1 / HIV-2 Antibody Test Kit Supplier: bioLytical Laboratories Inc. License Issue Date (Class IV Medical Device): October 25, 2005 COMPONENTS: INSTI membrane unit contains HIV-1 (gp41) and HIV-2 (gp36) recombinant proteins (which capture HIV-1 and HIV-2 specific antibodies), and a procedural control (protein-A treated spot) which detects the presence of IgG antibodies normally present in blood and blood components SAMPLE TYPE: Fingerstick blood, EDTA-treated whole blood or plasma, serum. VALIDATION FOR USE: Validated for HIV-1, HIV-2 antibodies. Not validated for detection of antibodies to HIV-1 N subtype. TEST PERFORMANCE: Fingerstick whole blood ♥ : Sensitivity Specificity Sensitivity 99.6% [95% CI 98.9-99.9%], Specificity 99.7% [95% CI 99.4-99.8%] Positive Fingerstick whole blood: PPV varies according to HIV prevalence. Predictive HIV Prevalence PPV Value (PPV) 0.1% (1 in 1000) 12.5% 0.2% (1 in 500) 22.2% 1.0% (1 in 100) 58.9% 10.0% (1 in 10) 94.0% Low Antibody Performance equivalent to standard HIV testing protocols using Titer commercial low titer performance panels. Window When compared to standard HIV testing on 25 established commercial period seroconversion panels the INSTI™ HIV Test was reactive: at the same time (14/25, 56%) or up to eight days later than standard testing (9/25, 36%). In the remaining two panels (8%), the INSTI™ HIV Test was not reactive by the last bleed in the seroconversion panel. The sensitivity of the INSTI™ HIV Test for detection of acute HIV infection is 69.4% [95% CI 54.6%-81.8%]. PRECAUTIONS: False negative or invalid test results may be obtained in clients with severe hypogammaglobulinemia conditions (e.g., multiple myeloma), patients receiving HAART, and patients with elevated hemoglobin. STORAGE: Storage temperature 15-30 °C, shelf-life 12 months. EXTERNAL QUALITY CONTROL: In place (August 2007) ♥ See product insert for sensitivity and specificity using other sample types. APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 52 APPENDIX II — Roles and Responsibilities This document summarizes the roles and responsibilities of the Tester, the Health Authority/Site, the BCCDC Provincial POC Program and service providers such as bioLytical and the proficiency testing service provider. Collaboration of all of these groups is critical to the success of a POC HIV testing program. The BCCDC Provincial Point of Care Testing program has created the Point of Care Guidelines for Health Care Settings; sites/Health Authorities are responsible for adapting and implementing these guidelines to meet their specific needs and operational policies/procedures. Activity Tester (approved by site and/or Health Authority) Testing Process APPENDICES Provide pre and post discussions, including informed consent, to clients according to established process and procedures. Perform client testing and interpret results according to established procedures. Deliver test results to client according to established procedures. Obtain venous blood sample for confirmatory testing as applicable and arrange for follow up with client regarding confirmatory test results. Record usage and results of each test kit on client testing log used at site (including those used for quality controls, wasted, training etc.) Follow site policies regarding confidentiality of records. Report concerns/problems with the test kit performance to POC site lead and provincial program manager as applicable. Site /Health Authority* Provincial Program These items may be the responsibility of the Health Authority or site and is to be determined at a regional level. Allocate sufficient clinic, material and human resources to implement, operate, review and maintain the use of POC HIV testing within each site. Ensure necessary equipment available for testing (i.e. gloves, sharps containers, Band-Aids). Report all reactive results to Medical Health Officer according to established regional procedures for communicable disease reporting. Collaborate with testers to ensure appropriate implementation of POC HIV testing. Report concerns/problems with the test kit performance to provincial POC HIV Service Provider: bioLytical (manufacturer of INSTI test kit) Prepare, maintain and report budget status and requirements to the appropriate committees and management teams. Provide monthly summaries of POC test kit usage by Health Authority and provincially to the appropriate committees and management teams. Provide data regarding test kit usage to Health Authority/Site as requested. Provide support to sites performing POC HIV testing including training, procurement, distribution and trouble shooting. Follow up with sites on abnormal results (i.e. invalid, indeterminate, false negative, false positive). Report concerns/problems with the test kit performance to appropriate BCCDC managers and to bioLytical. Provide advice regarding usage and specifications of test kit. Follow up on concerns/problems related to test kit performance and provide direction on the use of kits. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 53 Activity Tester (approved by site and/or Health Authority) Participate in the evaluation of the POC HIV testing program. Site /Health Authority* Provincial Program These items may be the responsibility of the Health Authority or site and is to be determined at a regional level. testing program manager. Participate in the evaluation of the POC HIV testing program. (manufacturer of INSTI test kit) APPENDICES Service Provider: bioLytical Collaborate with testers, Health Authority/site to ensure optimal implementation of POC HIV testing at site, health authority and provincial levels. Disseminate product information and feedback to Health Authorities/Sites if concerns have been raised and subsequently addressed by bioLytical. Evaluate the POC HIV testing program and report findings from the evaluation to the appropriate committees and management teams. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 54 Activity Tester Site /Health Authority* (approved by site and/or Health Authority) Training Competency Continuing education/ refresher training Participate in POC as well as HIV pre and post test discussion training programs. Successfully complete competency assessment before testing clients in collaboration with POC site lead. Participate in periodic refresher training and continuing education. Participate in additional training as identified during Site Approval Process. These items may be the responsibility of the Health Authority or site and is to be determined at a regional level. APPENDICES Provincial Program Schedule staff training in collaboration with provincial program. Verify that trained staff members have successfully completed competency assessment before testing clients. Retain training and competency records for all staff (tracked, filed and retained for 10 years). Schedule periodic refresher training and continuing education for testers. Identify additional non-HIV training requirements. Verify new testers have completed all HIV and nonHIV training/competency requirements. Service Provider: bioLytical (manufacturer of INSTI test kit) Develop training materials such as presentations, checklists etc. Coordinate, participate and deliver content for training as requested by and in collaboration with Health Authorities/sites. Develop continuing education materials and coordinate continuing education sessions in collaboration with Health Authority/Site as needed. Cooperate with appropriate trainers in the development and presentation of associated nonHIV training materials. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 55 Activity Tester (approved by site and/or Health Authority) Quality Control Samples Store and use quality control samples according to manufacturer’s instructions. Use quality control samples as per provincial program guidelines. Record quality control sample results and notify POC site lead of any unexpected results. Contact POC site lead/provincial program manager if quality control samples fail to give the result expected. Site /Health Authority* These items may be the responsibility of the Health Authority or site and is to be determined at a regional level. APPENDICES Provincial Program Order quality control samples through the provincial POC HIV testing program. Assume responsibility for integrity of quality control samples in health authority/site. Ensure quality control samples are stored as per manufacturer’s instructions and contact provincial POC HIV Testing Program if there is a concern with storage. Review POC HIV test kit usage log sheets and take corrective action as required. Contact provincial POC HIV testing program in the event of a problem with quality control samples. Service Provider: bioLytical (manufacturer of INSTI quality control samples) Purchase quality control samples for sites. Provide guidance around the use of quality control samples and training. Act as a resource for quality control sample problems/concerns. Contact the manufacturer as needed. Manufacture and ship quality control samples. Respond to any issues related to quality control samples. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 56 Activity Tester Site /Health Authority* (approved by site and/or Health Authority) Provincial Program These items may be the responsibility of the Health Authority or site and is to be determined at a regional level. Inventory Track test kit usage on daily log of client POC test results, and Quality Control Log. Report when kit inventory is low or close to expiration date to POC site lead. Store test kits and materials as indicated in provincial guidelines. Evaluate testing site needs for each upcoming order cycle. Collaborate with provincial POC HIV Testing Program to order test kits and required supply inventory. Assume responsibility for test kits at site/in health authority. Forward testing Monthly Summary Report (see Appendix IX) to provincial POC HIV testing program. Participate in kit redistribution to optimize utilization and eliminate wastage in such instances as kits being near expiration date. (manufacturer of INSTI test kit) APPENDICES Service Provider: bioLytical Initiate renewal of contract with kit vendor. Order test kits on behalf of sites and organize distribution and delivery. Verify Certificate of Analysis for each lot number received. Retain the original Certificate of Analysis for each kit lot number and provide a copy to testing sites on request. Verify performance of new lot. Verify ongoing performance of each lot. Order and distribute supplies such as quality controls, extra lancets, pipets and temperature monitors. Disseminate information regarding inventory changes to sites in a timely manner. Coordinate redistribution of limited date kits in collaboration with Health Authorities/sites to enhance utilization. Inform the POC HIV Program of any product updates or changes related to test kits, quality controls samples or other associated testing materials in a timely manner. Supply test kits and quality control samples with the maximum expiry date possible. Provide the Certificate of Analysis for each kit lot with each shipment Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 57 Activity Tester (approved by site and/or Health Authority) Storage of INSTI Test Kits Documentation and Reference Material APPENDICES Site /Health Authority* Provincial Program These items may be the responsibility of the Health Authority or site and is to be determined at a regional level. Service Provider: bioLytical (manufacturer of INSTI test kit) Complete daily temperature logs for all areas where test kits are stored, and notify POC site lead of any temperature outside the accepted range. Move stock as needed if temperature goes out of range. Run QC to ensure kits are acceptable for client use if temperature ranges are exceeded. Ensure temperature logs are maintained regularly for all areas where test kits are stored and take corrective action as required. Assume responsibility for storage of test kit materials and supplies. Provide sites with temperature monitors as needed or recalibrate existing monitors as scheduled. Complete and retain all documentation as outlined in the provincial program guidelines, and/or per site/HA requirements. Use most recent version of provincial program guidelines and manufacturer’s instructions. Provide feedback to provincial program on suggestions for new documents, or revisions of current documents. Maintain all documentation as required. Review Client and QC logs at least monthly Ensure the most recent version of provincial program guidelines and manufacturer’s instructions are being used by testers. Liaise with testers and Health Authority/Site supervisors to update documents and reference materials as required. Notify provincial program regarding changes to product documents. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 58 Activity Tester Site /Health Authority* (approved by site and/or Health Authority) Risk Management Report abnormal/unexpected errors/outcomes to the POC site lead. These items may be the responsibility of the Health Authority or site and is to be determined at a regional level. Recall Process APPENDICES Respond to recall alert messages from Provincial Program. Review current stock for recalled product. Quarantine recalled product and follow instructions from Site Lead and contact Provincial Program Manager regarding outcomes. Re-test clients as recommended by Provincial Program Manager. Provincial Program Service Provider: bioLytical (manufacturer of INSTI test kit) Retain and store clients log sheets in case of need to communicate problem with test kit to clients. Investigate unexpected outcomes, record actions and ensure implementation of corrective actions. Report abnormal/unexpected results to the provincial POC HIV testing program. Ensure recalled product has been identified and quarantined for all sites Communicate with sites, Provincial Program and bioLytical throughout entire process. Lead process for client retesting as necessary. Retain all documents related to the recall event Discuss abnormal/unexpected results with Health Authority/site supervisors. Report to advisory and steering committees as required. Relay information on changes or problems with test kits to all sites as applicable. Report abnormal/unexpected results to appropriate BCCDC management and to bioLytical as applicable. Facilitate communication between POC Site Leads/sites and bioLytical. Determine if client retest is needed and facilitate process as needed Respond to any concerns regarding kit performance and provides guidance as to how to proceed. Initiate recall process. Liaise with Provincial Program Manager throughout the recall process. Provide clear instructions of expectations to Provincial Program and sites. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 59 Activity Proficiency Testing Tester Site /Health Authority* (approved by site and/or Health Authority) These items may be the responsibility of the Health Authority or site and is to be determined at a regional level. Participate in proficiency testing as requested. Work with provincial program to enroll sites in proficiency testing program. Schedule staff participation in proficiency testing events. Review proficiency testing results with staff, and follow up concerns accordingly. Maintain proficiency testing records. Provincial Program Service Provider: bioLytical (manufacturer of INSTI test kit) APPENDICES Service Provider: Proficiency Testing provider Initiate and manage contract with proficiency testing provider on behalf of the sites. Act as the contact for sites if concerns or questions arise. Analyze provincial proficiency testing data results in aggregate form and report on results as part of the Provincial POC HIV Testing program evaluation. Offer support/assistance (i.e. training) for those sites that discover errors as a result of their participation in the proficiency testing program. Manufacture and distribute the proficiency testing materials to sites. Respond to issues regarding shipments or testing schedule. Analyze data from all participating sites. Create and distribute reports to participating sites. Respond to any proficiency testing issues related to kit performance. Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 60 APPENDIX III — Daily Log of Client POC Test Results Testing site: ________________________________ POC Test Lot Number (on Box): ______________________ Reviewer’s signature: ________________________________ Expiry Date (on Box): ______________________ Date of Test Tester Initials dd/mm/yyyy Client Identifier 1* (ie Name, Chart Number, DOB) Client Identifier 2* POC Test Result Reactive Non-reactive Invalid Indeterminate HIV Serology Collected or Requested (Yes, No) HIV Serology Result Reactive Non-reactive Indeterminate Not Done Reactive POC Test Final Result TP – True Pos FP – False Pos Notes / Comments (# of test kits left) PP – Prelim Pos^ * A minimum of two client identifiers is recommended for accuracy of client information. Where electronic client records are used, the chart number can be used here if two identifiers are in the client record. ^ In this context, Preliminary Positive refers to individuals having a reactive POC test result but are lost to follow-up and confirmatory serology was not performed. APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 61 APPENDIX IV — Fax Template Form APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 62 APPENDIX V — Direct Observation Checklist for POC HIV Testing Test Provider: ________________ Observer: ________________ Did the test provider: 1. Check to ensure Quality Control has been performed according to requirements prior to testing the client sample? 2. Obtain informed consent for the test? 3. Offer standard laboratory HIV testing or POC testing to the client? 4. Record the client and test information on the testing log sheet? 5. Record or check the lot number and expiry date of the test kit? 6. Provide a clean area on which to perform testing? 7. Wash/sanitize hands prior to starting the testing process? 8. Remove the membrane from the pouch without touching the centre well? 9. Wear gloves to perform the test? 10. Wipe client’s selected finger thoroughly with alcohol swab prior to puncture? 11. Dispose of the used lancet directly into a sharps container? 12. Fill the pipette to the fill line to obtain the required amount of blood? 13. Transfer the blood in the pipette into the solution 1 vial by squeezing the bulb of the pipette to dispense the blood into the vial? 14. Dispose of the used pipette directly into a biohazard waste container? 15. Mix the blood in solution 1 vial by gentle inversion? 16. Test the sample within 5 minutes of mixing blood with solution 1? 17. Mix solution 2 by gently turning it upside down and ensuring contents mixed? 18. Add the entire contents of solution 2 to the centre of the membrane unit and allow time to absorb? 19. Add the entire contents of solution 3 to the centre of the membrane unit and allow time to absorb? APPENDICES YES NO Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 63 Did the test provider: YES NO 20. Read the result within 5 minutes of adding the clarifying solution (solution 3)? 21. Remove and dispose of gloves into biohazard waste container? 22. Record the result on the testing log sheet? 23. Discuss and advise testing for HIV using venous blood collection for clients who tested negative with POC test but may be in the window period? 24. Draw venous blood when POC test was reactive, invalid (a second time), indeterminate or if an acute HIV infection is suspected? 25. Label the venous blood in the presence of the client with all required identifiers? 26. Complete the laboratory requisition as required? 27. Provide client an opportunity to express degree of satisfaction with the testing process (via web link card or printed survey)? Number of test kits used under observation: _________ Observer: _____________________________ Date: _________________ Follow-up issues identified? YES _____ NO ______ Comments: __________________________________________________________________________ __________________________________________________________________________ __________________________________________________________________________ Review of direct observation by trainer/assessor The test provider has demonstrated competence YES _____ NO ______ Observer: _____________________________ Date: _________________ Note that it is recommended that POC HIV Testing competencies are reviewed once per year. APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 64 APPENDIX VI — Training Completion Requirements for Nurses, Physicians, NursePractitioners The following completion requirements specifically pertain to the use of the POC HIV test. It is expected that learners attending POC training have knowledge of the following prerequisites: HIV Pre- and Post-Test discussions Legal and professional requirements and practice standards for obtaining informed consent Legal and professional requirements and practice standards for maintaining confidentiality To successfully complete the POC HIV testing training, the learner must attend a two- to threehour POC testing workshop and at completion of the training workshop independently demonstrate at minimum the following competencies: POC HIV Testing Initial Testing and Quality Assurance Training — Competencies Trainer Initials 1. Demonstrate the appropriate use and interpretation of the POC HIV test. 2. Demonstrate the procedures for using quality control samples. 3. Demonstrate a client-centered approach when obtaining informed consent, for maintaining confidentiality, and when providing client education. 4. Demonstrate a client-centered approach when interpreting and providing the POC test result and when discussing next steps and follow-up. 5. Demonstrate how and when to report POC test results. 6. Describe potential errors and measures to reduce errors related to use of the POC test kit and quality control materials. 7. Describe follow-up and referral process for confirmed HIV positive standard lab tests. By signing below, the learner and trainer are declaring that the learner has competently, ethically, and safely demonstrated the above completion requirements. It is recommended that POC HIV Testing competencies are reviewed once per year. Learner Name: Learner Signature: Trainer Name: Trainer Signature: Date: Completed form to be retained by the POC Site Lead. APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 65 APPENDIX VII — Training Competencies for Nurses, Physicians, Nurse-Practitioners Core POC HIV Test Provider Competencies Knowledge of: legislation, confidentiality, and informed consent related to HIV testing HIV infection and window period and the impact on testing HIV diagnostic tests and appropriate use how to implement and sustain quality assurance activities education and communication techniques documentation and reporting requirements Skill in: obtaining informed consent describing the diagnostic test options available using POC test kit and running quality controls collecting POC test sample interpreting test results and providing appropriate followup and determining next steps based on results collecting or referral for collection of venous sample providing appropriate client education collecting and documenting data for surveillance, reporting, and case management APPENDICES Judgment regarding: choosing the appropriate HIV diagnostic product (i.e. standard or POC testing) client follow-up and referral based on HIV test results referring clients to appropriate services (i.e. treatment, counseling) Attitude that: respects client’s choices and beliefs demonstrates self awareness of own beliefs, values, and practice limitations demonstrates sensitivity regarding impact of HIV diagnosis, reporting, and partner notification respects and supports the adherence to quality assurance activities Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 66 APPENDIX VIII — Quality Control Log Testing site: ______________________________ Date of Quality Control Tester Initials dd/mm/yyyy 1. 3. 5. 7. Quality Control Material Quality Control Lot Number POC Test Lot Number (Negative, Positive HIV-1 Positive HIV-2) (On Vial) (On Box) Receive new shipment New tester, before they start testing Change to new lot number Temperature out of range (below 15C or above 30C) APPENDICES POC Test Result Reactive Non-reactive Invalid POC Test performs as expected (Yes, No) Notes / Comments Reason for testing (from numbers below) 2. Invalid client result X 2 4. At regular intervals - monthly 6. Trouble-shooting Site Lead Review Initial Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 67 APPENDIX IX — Monthly Summary Report APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 68 APPENDIX X — Incident Summary Form APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 69 APPENDIX XI — Temperature Monitoring Log Room Temperature Log for INSTI Kit Storage Site: Day Month: Notify POC Site Lead when temperature is: less than 15 0 C more than 30 0 C Time # Kits hh:mm Monitor Record Temp Acceptable? 0 C Minimum Maximum Yes/No 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 Reviewed by: Comments: APPENDICES Review Date: Initials Year: Not Acceptable? Actions Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 70 APPENDIX XII — Practice Guidance for Allied Health – Regulated Health Care Providers Regulated health care providers interested in including Point of Care HIV testing in their professionals practice are recommended to follow these steps prior to initiating training and beginning POC testing: Contact your professional college to find out if Point of Care testing has already been approved as part of your scope of practice. If your professional college is unfamiliar with Point of Care HIV testing or unclear about whether or not it could be part of your scope of practice, refer them to the letter of introduction of the BCCDC below and contact the provincial POC HIV testing program (BCCDC) for additional informational and supportive resources to provide to your professional college. Once POC HIV testing has been approved as part of your scope of practice, begin the steps to implementing it within your practice and health care setting. Definition of Allied Health: provide diagnostic, therapeutic, and rehabilitative health services. These fields encompass all professions in health care with the exception of Medicine and Nursing and may or may not be regulated. The Canadian Association of Allied Health Programs (www.caahp.ca) recognizes the following allied health programs: Anaesthesia Technology, Biomedical Engineering Technology , Cardiac Sciences, Dental Sciences, Electro-neurosciences , Emergency/ Paramedic, Environmental Health, Food & Nutrition, Health Information Sciences, Medical Imaging Sciences, Medical Laboratory Sciences, Ophthalmic Sciences, Pharmaceutic Sciences, Radiation Therapy, Rehabilitation Sciences, Respiratory Therapy, Traditional Chinese Medicine Definition of regulated health care provider: There are 26 regulated health professions in British Columbia, of which 25 are self-regulating professions governed by 22 regulatory colleges under the Health Professions Act. Social workers are a self-regulating profession governed by a regulatory college under the Social Workers Act. A list of regulated professionals is available here: http://www.health.gov.bc.ca/professional-regulation/index.html#redirect_notice_display_301 Chiropractic, Dental Hygiene , Dental Technology, Dentistry, Denturism, Dietetics, Emergency Medical Assisting, Massage Therapy, Medicine, Midwifery, Naturopathic Medicine, Nursing (Licensed Practical), Nursing (Registered), Nursing (Registered Psychiatric), Occupational Therapy, Opticianry, Optometry, Pharmacy, Physical Therapy, Podiatric Medicine, Psychology, Speech and Hearing Health Professions, Traditional Chinese Medicine and Acupuncture, Social Work APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 71 APPENDIX XIII — Sample Letter for Colleges Dear Colleagues, This letter is meant to provide Professional Colleges in BC with information to introduce and assist College Staff in decision-making regarding Point of Care (POC) HIV Testing’s inclusion in scope of their professional practice. HIV testing has traditionally been done through venous blood draws and therefore has been performed primarily by medical staff including physicians, nurses, and medical laboratory technicians. It follows then that these professionals were the first in BC to implement POC HIV testing as part of their practices. However, given the simplicity of the finger poke screening procedure of HIV Point of Care Testing, diverse groups of professionals and community workers are capable of performing and interpreting this POC HIV screening test. POC HIV testing is widespread and performed by various groups of regulated and nonregulated providers throughout Canada and globally. Point of Care HIV Testing is relatively new as a practice in BC with the introduction of BC’s Provincial HIV Point of Care HIV Testing Program in 2011. Several professional Colleges that fall under the BC Professions Act have begun or completed the process of review and inclusion of POC HIV testing into their professional practice. The Provincial Point of Care HIV Testing Background Please refer to the BCCDC’s website and POC page for further information and to link to the Point of Care HIV Test Guidelines for Health Care Settings at www.bccdc.ca/POC. Point of Care (POC) HIV tests (also known as “rapid” HIV tests) are HIV antibody screening tests which can be performed on-site while the client waits, and provide results within minutes. In August 2010, the BC Centre for Disease Control (BCCDC) was asked by the Ministry of Health to introduce a Provincial POC HIV Testing Program to oversee centralized, province-wide HIV point of care testing, distribution, and quality assurance program funded through the provincial pilot project, Seek and Treat for the Optimal Prevention of HIV/AIDS (STOP HIV/AIDS). As a result, POC HIV testing has been used in all Health Authorities in British Columbia. The BCCDC has published provincial practice guidelines: Point of Care HIV Test Guidelines for Health Care Settings. The INSTI HIV-1/HIV-2 Rapid Antibody Test is the only POC HIV test product licensed for use in health care settings. Please refer to the manufacturer’s website for further product and quality information at http://www.biolyticalcanada.com/ Recommended Testing Sites: POC HIV Testing is recommended for use in voluntary HIV testing settings accessed by a) high prevalence populations b) where not returning for test results is common, or c) where provision of a POC HIV test result will improve public health follow-up or connection to HIV clinical care. It is also recommended in clinical scenarios where there is an urgent need to determine HIV status (i.e. pregnant women near-term or in labour with undocumented HIV status, testing of source individual during blood and fluid exposures, or clinical diagnosis of acutely ill patients). Roles and Responsibilities: APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 72 Shared roles and responsibilities between Health Authorities, First Nations health agencies and BCCDC facilitate the appropriate use of POC HIV testing in communities by designating appropriate healthcare sites for offering POC HIV testing, providing professionals with POC HIV testing training and guidelines and by participating in the monitoring and evaluation of POC HIV testing in the province. Contact Information For more information about POC HIV testing’s fit with professional scope of practice and/or to arrange a meeting, please contact: Provincial Point of Care HIV Testing Program 655 West 12th Avenue Vancouver, BC, V5Z 4R4 Phone: 604.707.5635 Fax: 604.707.2603 Email: [email protected] Website: www.bccdc.ca/POC APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 73 APPENDIX XIV — Recommended Base-Line Qualification for NRACP HIV POC Testers These qualifications can be used as part of NRACP POC tester job postings or descriptions in order to facilitate the engagement of qualified candidates into these positions. Attitudes: Accepting and respectful of diversity, demonstrating a positive, non-judgmental attitude toward people from various social groups and life paths. Culturally aware and competent (regarding both socio and ethno-cultural considerations) Curious and flexible (willing to change). Can work collaboratively within systems (to provide broad access to care). Able to separate own values and morals from those of others. Demonstrates a caring attitude toward others. Altruistic – able to provide person-centered care. Knowledge Literacy – is able to read and write at a basic level. Numeracy – can work with numbers to the extent required to conduct POC testing. Basic knowledge (experience a definite asset) of issues faced by populations vulnerable to HIV. (i.e. Addictions, men who have sex with other men, sexual diversity etc.) Knowledge of community resources (both health care and social services systems). Understands privacy considerations and can demonstrate a sensitivity to issues related to confidentiality. Understands trauma informed care, and factors that contribute to person’s vulnerability. Integrates this knowledge into developing approaches to care. Skills Basic communications skills – ability to listen, process and respond appropriately. Interpersonal skills – able to give and take to resolve conflict. APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 74 APPENDIX XV — Competencies for Non-regulated and Allied Health Care Providers These key competencies are meant to frame and inform the design of training sessions and ongoing assessment of competencies for NRACP POC testers. Please see Appendix XVI for an example of training curriculum components. Conducts HIV Test Informed Consent Documentation Testing Environment Confidentiality Social Context Boundaries PersonCentered Care Competencies for NonRegulated Care Providers Self Care The attitudes, knowledge, skills and judgment (“competencies”) for non-regulated and allied health care providers (NRACP) to conduct HIV testing were identified by a literature review and community-based care-givers in focus groups conducted in three separate regions of British Columbia. These competencies are grouped here with the standards of practice identified by the same groups. In this document the person conducting the test is referred to as the “provider” or “NRACP”, and the person receiving the test is referred to as the “person”. Standard 1 –Person-centered Care: i. Builds and sustains person-centered relationships as the focus of approach to HIV testing. Advocates that the interests of the person are at the forefront of their agency’s approach to HIV testing service delivery. ii. Demonstrates compassion and respect in the care provided to all people from diverse backgrounds by providing care that is free bias and prejudice. APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 75 iii. Demonstrates trust by collaborating with the person to make decisions related to his or her care. Facilitates opportunities for the person to test in an environment that best suits his or her needs. iv. Assures that the language and approach is clear, understandable, and acceptable to the person who is receiving care. v. Understands trauma informed care, and factors that contribute to person’s vulnerability. Integrates this knowledge into developing approaches to care. Standard 2 –Boundaries: i. Does not allow his or her personal or private interests to interfere with providing care. ii. Recognizes and challenges any situation in which the person’s dignity or rights are interfered with by the power imbalance that exists between service providers and person. iii. Recognizes when conflicts interfere with providing care, and takes measures to protect the person. (E.g. removing him or herself from situations that are ethically uncertain and refers the person to another provider.) iv. Assures that all physical contact is for therapeutic purposes, and is helpful to, and desired by the person v. Reports unsafe, harmful or unethical practice of other providers. Standard 3 –Confidentiality: i. Applies current best practices to protect the private and personal information about the person. ii. Understands and informs the person of the limits to confidentiality as laid out in law and the ethical standards, policies and practices of their organization. iii. Challenges people and situations where the person’s private information is not being protected, and reports situations where the person’s confidentiality is persistently being breached. Standard 4 - Conducts HIV Test: i. Demonstrates skill using available HIV test kits. ii. Assures that the person understands HIV, how it is transmitted, and the nature and limitations of the test that is being used. iii. Addresses any questions and concerns the person might have, and determines if the person is ready to test. iv. Assures supports are in place in the event of a positive diagnosis. v. Understands that reportable disease follow-up is part of HIV testing, and collaborates with the communicable disease team to report and manage new HIV positive results. Standard 5 – Informed consent: i. Clearly states the purpose and process of HIV testing to the person so that the person is able to fully understand and agree to be tested. ii. Assures that the person receives adequate information to agree to, or decline testing. iii. Assures that consent is voluntarily given, and does not coerce the person to agree to test if that is not the person’s will. APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 76 iv. iv. v. Understands that consent can be withdrawn at any time, and accepts the person’s right to change his or her mind about testing. Bases the person’s capacity to give informed consent solely on their ability to demonstrate their understanding the test and services that are being provided. Understands that people with chronic mental health challenges or those who use alcohol and drugs may still be capable of providing informed consent. Obtains a signed consent form to transmit confidential information. Standard 6 – Documentation: i. Accurately records discussions, decisions, actions, plans and referrals regarding the person’s care and status, and signs all documents related to the person’s care. ii. Documents the person’s statement of voluntarily consenting to test. iii. Collaborates with the communicable disease team from the Health Authority about how documentation related to new HIV positive results and follow-up will be coordinated and recorded. Standard 7 – Testing Environment: i. Offers HIV testing only when education, monitoring, and evaluation systems are in place to assure the competent delivery of HIV testing services. ii. Assures the person has access to the necessary follow-up services, including arranging for the person to have a laboratory HIV test to confirm a point of care positive test result. iii. Advocates for a process whereby ethical dilemmas can be resolved within the workplace. iv. Employs multiple and creative approaches to delivering care that provides the person with minimum barrier services. Collaborates with other agencies to reduce restrictions to access to safe and culturally attuned services. Standard 8 – Social Context: i. Determines the local circumstances surrounding populations at risk for HIV within their specific community. ii. Assesses and responds to the community’s level of readiness and willingness to respond to issues related to delivering HIV testing services. iii. Works with individuals and groups from the community to develop services that are acceptable within the community setting, and address the needs of the people who are at risk for HIV. iv. Employs knowledge of socially-based contributors to vulnerability for acquiring HIV (such as stigma, discrimination, poverty, and homelessness) in community development. Provides education and support to the community to increase the level of knowledge related to HIV risk and service needs. Standard 9 – Self Care: i. Employs external and self-care measures to deal with the emotional stress of providing HIV testing services. ii. Advocates for adequate support services for HIV test providers. APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 77 APPENDIX XVI — HIV Testing Education for Non-regulated and Allied Health Care Providers Module I: HIV in Canada and BC, standards for HIV testing, population approaches to HIV testing and prevention and guiding principles when working with individuals HIV In Canada and British Columbia How knowledge, engagement , relationship building and assessment contribute to effective testing, prevention and support efforts Population & Public Health Approaches to HIV Testing Working with Individuals o Benchmarks for informed consent o Person Centred Care – What does this look like? o Effective communication – include demonstrating of communication skills o Confidential Care, the limitations of confidentiality and the consequences for breaches of confidentiality o Culturally competent care o Include the cultural competence course o Boundaries - Establishing and maintaining Client/provider boundaries – steps to take when boundaries become blurred o Ethics and HIV testing o Documentation Module 2: The Virus –HIV as a pathogen and a disease, the impact of HIV at the cellular, individual and population levels What is HIV HIV Transmission HIV and the Immune System o HIV Replication o The Course of HIV Infection o Progression of HIV - Untreated o Progression of HIV - Treated Treatment and Prevention Module 3: Individual and population issues which impact vulnerability to HIV Who is Getting HIV in BC HIV Rates per Health Authority Working with Individuals who have increased vulnerability to HIV APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 78 Module 4: HIV Tests – The characteristics of the POC test and the lab test Characteristics of HIV Tests o http://www.bccdclearning.ca/moodle/mod/book/view.php?id=1449&chapterid=1141 Window periods of the POC and Lab tests o Biological Markers Standard Lab Tests as a confirmation of the POC test False Positive Results Module 5: Provider responsibilities prior to testing. Prior to HIV testing Assessing and responding to person’s knowledge of HIV and HIV testing Describing the different POC test results Discussing benefits as well as possible personal challenges of knowing HIV status Assessing a persons readiness to test Supporting the person who is vulnerable and decides not to test for HIV Discussing a person’s support network Next steps if negative or preliminarily positive Module 6: Performing HIV POC Tests – This module will train the person in use of the POC test kit including the quality control issues which accompany its use. http://www.bccdclearning.ca/moodle/mod/book/view.php?id=1493&chapterid=1255POC Provincial Training Program Module 7: Discussing POC results. Introduces HIV reporting, the legal implications of HIV non-disclosure and the benefits of clinical follow up when HIV positive The POC test result is negative o How to discuss the result o Responding in a person centered way o Consideration of window period o Community referrals The POC test result is indeterminate or invalid o How to discuss the result o Next Steps The POC test result is reactive o How to discuss the result APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 79 o Responding in a person centered way o Pathway for confirmatory testing o Prevention messaging while waiting for results – protecting partners o Community referrals The BC HIV reporting process o How to report a preliminary positive POC result – nominal / non nominal Talking with HIV positive persons about their partners o How to talk with newly diagnosed persons about informing partners. o How public health nurses can assist with partner notification. o Is partner notification mandatory or voluntary? o What is the role of the testing provider around discussing disclosure and non disclosure of HIV status? o Provider next steps around non disclosure if another person may be being exposed. Where to find current legal information about disclosure Module 8: Possible impacts of providing HIV testing on an individual provider Exceptional issues which could occur when testing peers – guest speaker from the HIV community Recognizing personal provider stress –self care Debriefing when working on a team Lines of team communication Ethical challenges in HIV testing Module 9: Clinical Practice – An opportunity to demonstrate understanding of HIV testing guidelines, skills performing POC HIV testing and interpreting results. Participant will be aware of ongoing competency requirements established by employer Preceptored Practice Observing an expert performing POC testing Observation of practice by an expert – giving both negative and preliminary positive results Evaluation Certification of completion Ongoing competency requirements APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 80 APPENDIX XVII — Checklist for New NRACP Sites Implementation Checklist for NRACP HIV Testing Sites 1. Initial Engagement - Review the following: Rationale for additional HIV testing Context of the clinical program Leadership and operational roles Will site be supported by BC POC HIV Test Program or test independently? 2. Site Preparation Who will fill leader and operational roles for implementation? o Use Roles and Responsibilities Appendix II Client volumes – how many clients are served per year? Training and Go live dates o Training should be as close to go live as possible. o Modify Curriculum o What content needs to be customized? 3. On‐Site readiness Confidential and appropriate space for client testing? Safe and secure client record storage? Plan for disposal of hazardous waste? Infection control plan? 3a. Confirmatory Lab testing What process does the site currently follow to refer or conduct HIV tests? Reporting reactive results – who to contact and what support does the client need? Who will order confirmatory HIV tests? 3b. Reporting POC testing How are POC tests results/usage reported? How is usage of POC tests reported to BCCDC? What is the POC recall process – who leads this at this site? How are POC test kits and supplies ordered? Who does this? 4. Client Support Materials Client information brochure about HIV testing Posters for clinic rooms and waiting area HIV POC Support Materials HIV POC instructions What to do with a reactive result? Lab vs. HIV POC testing guide BCCDC HIV POC Testing guidelines Testing frequency recommendations (M. Gilbert) Referral resources for HIV primary care and supports APPENDICES Communicable Disease Control Manual – Chapter 5 Point of Care HIV Test Guidelines for Health Care Settings May 2014 Page 81 5. Training What training is needed? How will the training be provided? How will competence be assessed? By whom? How often? o Schedule staff for POC training (online or in-person options) o HIV Pre‐Post test counselling o On site shoulder to shoulder training for new testers o Review POC test mechanics o How to record POC tests on the testing log o Reporting reactive results to MHO/Designated Nurse o Support strategies for clients with reactive test results o How to order HIV POC materials o How to dispose of test materials safely o Infection control procedures o Sample collection and transport procedures o Review plan for storage of client records o Other needs 6. Check‐in Identify any barriers to testing Identify any successes Identify any problems in operational processes Address problems identified Share testing level progress (# tests administered) APPENDICES
© Copyright 2026