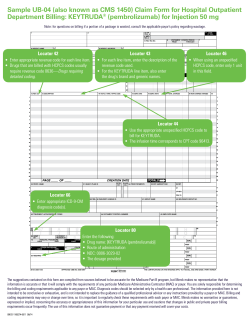
Provider Claims and Billing Manual Version Two Publication Date: July 2014
Provider Claims and Billing Manual Version Two Publication Date: July 2014 Claims and Billing Manual Table of Contents Claim Filing..................................................................................................................................... 1 Procedures for Claim Submission ............................................................................................... 1 Claim Submission Instructions .................................................................................................... 2 Claim Filing Deadlines ................................................................................................................ 3 Refunds for Improper Payment or Overpayment of Claims ........................................................ 3 Claim Form Field Requirements ..................................................................................................... 5 Required Fields (CMS-1500 Claim Form) .................................................................................. 5 EDI Mapping for CMS-1500..................................................................................................... 17 Required Fields (UB-04 Claim Forms) ..................................................................................... 23 EDI Mapping Table (UB-04) .................................................................................................... 40 Special Instructions and Examples for CMS-1500, UB-04 and EDI (837) Claims Submissions . 47 I. Supplemental Information ..................................................................................................... 47 A. CMS-1500 Paper Claims – Field 24: ............................................................................... 47 B. EDI – Field 24D (Professional): ...................................................................................... 47 C. EDI – Field 33b (Professional): ....................................................................................... 48 D. EDI – Field 45 and 51(Institutional):............................................................................... 48 E. Reporting NDC on CMS-1500 and UB-04 and EDI: ...................................................... 48 Common Causes of Claim Processing Delays, Rejections or Denials .......................................... 51 Electronic Data Interchange (EDI) for Medical and Hospital Claims ........................................... 54 Electronic Claims Submission (EDI) ............................................................................................ 55 Hardware/Software Requirements............................................................................................. 55 Contracting with Emdeon and Other Electronic Vendors ......................................................... 55 Contacting the EDI Technical Support Group .......................................................................... 55 Specific Data Record Requirements .......................................................................................... 56 Electronic Claim Flow Description ........................................................................................... 56 Invalid Electronic Claim Record Rejections/Denials ................................................................ 57 Plan Specific Electronic Edit Requirements.............................................................................. 57 Exclusions ................................................................................................................................. 57 Resubmitting Professional Corrected Claims ............................................................................ 59 Common Rejections .................................................................................................................. 59 Common Rejections, continued................................................................................................. 60 Supplemental Information ............................................................................................................. 61 Allergy Testing/Immunotherapy ............................................................................................... 61 Ambulatory Surgical Centers .................................................................................................... 61 Anesthesia ................................................................................................................................. 61 Behavioral Health ...................................................................................................................... 61 Claims and Billing Manual Chemotherapy ........................................................................................................................... 62 Child HealthCheck (EPSDT) Services ...................................................................................... 62 Dental Claims (DentaQuest)...................................................................................................... 63 Diabetes ..................................................................................................................................... 63 Durable Medical Equipment...................................................................................................... 63 Family Planning ........................................................................................................................ 63 Family Planning (non-obstetric) ................................................................................................ 63 Immunizations ........................................................................................................................... 64 Injectable Drugs ........................................................................................................................ 64 Maternity ................................................................................................................................... 64 Maternity Birthing Center (obstetric) ........................................................................................ 65 Maternity Delivery .................................................................................................................... 65 Maternity Fetal Bio-Physical Profile ......................................................................................... 65 Outpatient Hospital Services ..................................................................................................... 65 Pain Management ...................................................................................................................... 65 Pharmacy Coverage (PerformRx) ............................................................................................. 66 Physical/Occupational and Speech Therapies ........................................................................... 66 Transplants ................................................................................................................................ 66 Vision Care Exams .................................................................................................................... 66 Vision Claims (eyeQuest).......................................................................................................... 67 Weight Assessment and Counseling for Nutritional and Physical Activity (Child/Adolescent)67 Well Child Visits ....................................................................................................................... 67 Women’s Preventive Health Services ....................................................................................... 67 Electronic Billing Inquiries ........................................................................................................... 68 2013 HEDIS Billing Guidelines .................................................................................................... 69 Claims and Billing Manual Claim Filing Important: Procedures for Claim Submission AmeriHealth District of Columbia, hereinafter referred to as the ‘Plan’ or ‘AmeriHealth DC’ is required by state and federal regulations to capture specific data regarding services rendered to its members. All billing requirements must be adhered to by the provider in order to ensure timely processing of claims. When required data elements are missing or are invalid, claims will be rejected by AmeriHealth DC for correction and re-submission. Claims for billable services provided to AmeriHealth DC members must be submitted by the provider or an entity employed by the provider who performed the services. Claims filed with AmeriHealth DC are subject to the following procedures: Verification that all required fields are completed on the CMS-1500 or UB-04 forms. Verification that all diagnosis and procedure codes are valid for the date of service. Verification for electronic claims against 837 edits at Emdeon Verification of member eligibility for services under AmeriHealth DC during the time period in which services were provided. Verification that the services were provided by a participating provider or that an out-of-network provider has received authorization to provide services to the eligible member. Verification that an authorization or referral has been given for services that require prior authorization or referral by the Plan. Verification of whether there is Medicare coverage or any other thirdparty resources and, if so, verification that the Plan is the “payer of last resort” on all claims submitted to AmeriHealth DC Rejected Claims are defined as claims with invalid or missing required data elements, such as the provider tax identification number or member ID number, that are returned to the provider or EDI* source without registration in the claim processing system. Rejected claims are not registered in the claim processing system and can therefore be resubmitted as a new claim within 180 calendar days from the date of service or discharge. Denied Claims are registered in the claim processing system but do not meet requirements for payment under AmeriHealth DC guidelines. Denied claims must be resubmitted as corrected claims. Denied claims must be resubmitted as corrected claims within 365 days of the original date of service. Note: These requirements apply to claims submitted on paper or electronically. * For more information on EDI, review the section titled Electronic Data Interchange (EDI) for Medical and Hospital Claims in this document. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 1 Provider Services 202-408-2237 or 888-656-2383 Claims and Billing Manual Claim Submission Instructions Important: Submit claims to AmeriHealth DC via: Mail: Please submit paper claims to the appropriate address below: By Telephone: Provider Claim Services 202-408-2237 or 888-656-2383 (Select the appropriate prompt.) AmeriHealth DC/Medicaid Attn: Claims Processing Department P.O. Box 7342 London, KY 40742 On Paper: If you prefer to write, please be sure to stamp each claim “corrected” or “resubmission” and address the letter to the appropriate claims address, as listed on the left. OR AmeriHealth DC/Alliance Attn: Claims Processing Department P.O. Box 7354 London, KY 40742 Electronic: AmeriHealth DC participates with Emdeon. As long as you have the capability to send EDI claims to Emdeon, whether through direct submission or through another clearinghouse/vendor, you may submit claims electronically. Electronic claim submissions to AmeriHealth DC should follow the same process as other electronic commercial submissions. To initiate electronic claims: - Claim Adjustments Requests for adjustments may be submitted electronically, on paper, by telephone. Contact your practice management software vendor or EDI software vendor. Inform your vendor of AmeriHealth DC’s EDI Payer ID#: 77002. You may also contact Emdeon at 877-363-3666 or visit to www.emdeon.com for information on contracting for direct submission to Emdeon. AmeriHealth DC does not require Emdeon payer enrollment to submit EDI claims. Electronically: Use CLM05-3 to report claim adjustments electronically. Claim Disputes If a claim or a portion of a claim is denied for any reason or underpaid, the provider may dispute the claim within 60 days from the date of the denial or payment. Claim disputes must be submitted in writing, along with supporting documentation, to: AmeriHealth DC Attn: Claim Disputes P.O. Box 7358 London, KY 40742 Medical Appeals Any additional questions may be directed to the AmeriHealth DC EDI Technical Support Hotline by calling 888-656-2383 and selecting the appropriate prompts or by emailing to [email protected]. Administrative or medical appeals must be submitted in writing to: AmeriHealth DC Attn: Provider Appeals Department P.O. Box 7359 London, KY 40742 Note: AmeriHealth DC EDI Payer ID#: 77002 __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 2 Provider Services 202-408-2237 or 888-656-2383 Claims and Billing Manual Claim Filing Deadlines All original paper and electronic claims must be submitted to AmeriHealth DC within 180 calendar days from the date services were rendered (or the date of discharge for inpatient admissions).This applies to capitated and fee-for-service claims. Please allow for normal processing time before re-submitting a claim either through the EDI or paper process. This will reduce the possibility of your claim being rejected as a duplicate claim. Claims are not considered as received under timely filing guidelines if rejected for missing or invalid provider or member data. Note: Claims must be received by the EDI vendor by 9:00 p.m. in order to be transmitted to the Plan the next business day. Rejected claims are defined as claims with missing or invalid data elements, such as the provider tax identification number or member ID number, that are returned to the provider or EDI source without registration in the claim processing system. Rejected claims are not registered in the claim processing system and can be re-submitted as a new claim. Claims originally rejected for missing or invalid data elements must be re-submitted with all necessary and valid data within 180 calendar days from the date services were rendered (or the date of discharge for inpatient admissions). Denied claims are registered in the claim processing system but do not meet requirements for payment under AmeriHealth DC guidelines. They should be re-submitted as a corrected claim. Claims originally denied must be re-submitted as a corrected claim within 365 days of the original date of service. Claims with Explanation of Benefits (EOBs) from primary insurers, including Medicare, must be submitted within 180 days of the date on the primary insurer’s EOB. Please note, COB claims may be submitted electronically or on paper. Refunds for Improper Payment or Overpayment of Claims If a Plan provider identifies improper payment or overpayment of claims from AmeriHealth DC, Medicaid or Alliance programs, the improperly paid or overpaid funds must be returned to the Plan. Providers are required to return the identified funds to AmeriHealth DC by submitting a refund check directly to the appropriate claims processing department: AmeriHealth DC/Medicaid Attn: Provider Refunds P.O. Box 7342 London, KY 40742 AmeriHealth DC/Alliance Attn: Provider Refunds P.O. Box 7354 London, KY 40742 Note: Please include the member’s name and ID, date of service and claim ID. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 3 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 4 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements Claim Form Field Requirements The following charts describe the required fields that must be completed for the standard Centers for Medicare and Medicaid Services (CMS) CMS-1500 or UB-04 claim forms. If the field is required without exception, an “R” (Required) is noted in the “Required or Conditional” box. If completing the field is dependent upon certain circumstances, the requirement is listed as “C” (Conditional) and the relevant conditions are explained in the “Instructions and Comments” box. The CMS-1500 claim form must be completed for all professional medical services, and the UB-04 claim form must be completed for all facility claims. All claims must be submitted within the required filing deadline of 180 calendar days from the date services were rendered (or the date of discharge for inpatient admissions). Claims with Explanation of Benefits (EOBs) from primary insurers, including Medicare, must be submitted within 180 days of the date on the primary insurer’s EOB. Although the following examples of claim filing requirements refer to paper claim forms, claim data requirements apply to all claim submissions, regardless of the method of submission (electronic or paper). Required Fields (CMS-1500 Claim Form) CMS-1500 Claim Form Field # Field Description Instructions and Comments Required or Conditional* 1 Insurance Program Identification Check only the type of health coverage applicable to the claim. This field indicates the payer to whom the claim is being filed. R 1a Insured’s I.D. Number Enter the Member ID number as it appears on the AmeriHealth DC Member ID card. This number begins with a ‘7’ and is also known as the Medicaid ID number. For electronic submissions, this ID must be less than 17 alphanumeric characters. R (Enter the Member ID Number) 2 Patient’s Name (Last, First, Middle Enter the patient’s name as it appears on the member’s AmeriHealth DC Member Initial) ID card or enter the newborn’s name when the patient is a newborn. 3 Patient’s Birth Date/Sex MMDDYY / M or F R R Enter the patient’s birth date and select the appropriate gender. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 5 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # Field Description Instructions and Comments Required or Conditional* 4 Insured’s Name (Last, First, Middle Initial) Enter the patient’s name as it appears on the AmeriHealth DC Member ID card, or enter the newborn’s name when the patient is a newborn. R 5 Patient’s Address (Number, Street, Enter the patient’s complete address and telephone number. (Do not punctuate City, State, Zip) Telephone (with the address or telephone number.) Area Code) R 6 Patient Relationship To Insured 7 Insured’s Address (Number, Street, City, State, Zip Code) Telephone (with Area Code) 8 Reserved for NUCC use 9 Other Insured's Name (Last, First, Refers to someone other than the patient. Completion of fields 9a Middle Initial) through 9d is required if the patient is covered by another insurance plan. Enter the complete name of the insured. C 9a Other Insured's Policy Or Group # Required if # 9 is completed. C 9b Reserved for NUCC use To be determined. Not Required 9c Reserved for NUCC use To be determined. Not Required 9d Insurance Plan Name Or Program Name List AmeriHealth DC as the health plan. R 10 a,b,c Is Patient's Condition Related To: Indicate Yes or No for each category. Is condition related to: R Always indicate self. R R Not used. Not Required a) Employment b) Auto Accident (Including Place/State) c) Other Accident __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 6 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # 10d Field Description Claim Codes NUCC) Instructions and Comments (Designated Required or Conditional* by Enter new Condition Codes as appropriate. Available 2-digit Condition Codes include nine codes for abortion services and four codes for worker’s compensation. Please refer to NUCC for the complete list of codes. Examples include: AD – Abortion Performed due to a Life Endangering Physical Condition Caused by, Arising from or Exacerbated by the Pregnancy Itself W3 – Level 1 Appeal Insured's Policy Group Or FECA # Required when other insurance is available. Complete if more than one other Medical insurance is available, or if “yes” to 10 a, b, c. Enter the policy group or FECA number. C 11 C 11a Insured's Birth Date / Sex Same as # 3. Required if 11 is completed. C 11b Other Claim ID Enter the following qualifier and accompanying identifier to report the claim number assigned by the payer for worker’s compensation or property and casualty: Y4 – Property Casualty Claim Number C Enter qualifier to the left of the vertical, dotted line; identifier to the right of the vertical, dotted line. 11c Insurance Plan Name Or Program Name Enter name of the other insurance health plan. Required if 11 is completed. C 11d Is There Another Health Benefit Plan? Indicate Yes or No by checking the box. R If Yes, complete # 9 a-d. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 7 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # Field Description Instructions and Comments Required or Conditional* 12 Patient's Or Authorized Person's Signature Not required 13 Insured's Or Authorized Person's Signature Not required 14 Date Of Current Illness Injury, Pregnancy (LMP) MMDDYY or MMDDYYYY C Enter applicable 3-digit qualifier to right of vertical dotted line. Qualifiers include: • 431 – Onset of Current Symptoms or Illness • 484 – Last Menstrual Period (LMP) Use the LMP for pregnancy. Example: __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 8 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # 15 Field Description Instructions and Comments Required or Conditional* MMDDYY or MMDDYYYY Other Date C Enter applicable 3-digit qualifier between the left-hand set of vertical dotted lines. Qualifiers include: • • • • • • • • • 454 – Initial Treatment 304 – Latest Visit or Consultation 453 – Acute Manifestation of a Chronic Condition 439 – Accident 455 – Last X-Ray 471 – Prescription 090 – Report Start (Assumed Care Date) 091 – Report End (Relinquished Care Date) 444 – First Visit or Consultation Example: 16 Dates Patient Unable To Work In Current Occupation C __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 9 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # 17 Field Description Instructions and Comments Name Of Referring Physician Or Other Source Required or Conditional* Required if a provider other than the member’s primary care physician rendered invoiced services. Enter applicable 2-digit qualifier to left of vertical dotted line. If multiple providers are involved, enter one provider using the following priority order: 1. Referring Provider 2. Ordering Provider 3. Supervising Provider C Qualifiers include: • DN – Referring Provider • DK – Ordering Provider • DQ – Supervising Provider Example: 17a Other ID Number Of Referring Physician (AmeriHealth DC Provider ID#) 17b National Provider Identifier (NPI) Enter the AmeriHealth DC Provider ID Number for the referring physician. The qualifier indicating what the number represents is reported in the qualifier field to the immediate right of 17a. If the Other ID number is the AmeriHealth DC ID number, enter G2. If the Other ID number is another unique identifier, refer to the NUCC guidelines for the appropriate qualifier. C Enter the NPI number of the referring provider, ordering provider or other source. Required if #17 is completed. R __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 10 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # Field Description Instructions and Comments Required or Conditional* C 18 Hospitalization Dates Related To Current Services 19 Additional Claim Information (Designated by NUCC) Required when place of service is inpatient. MMDDYY (indicate from and to date). Enter additional claim information with identifying qualifiers as appropriate. For multiple items, enter three blank spaces before entering the next qualifier and data combination. 20 Outside Lab Optional C 21 Diagnosis Or Nature Of Illness Or Injury. (Relate To 24E) Enter the applicable ICD indicator to identify which version of ICD codes is being reported: R • • Not Required 9 - ICD-9-CM 0 - ICD-10-CM Enter the indicator between the vertical, dotted lines in the upper right-hand portion of the field. Enter the codes to identify the patient’s diagnosis and/or condition. List no more than 12 ICD diagnosis codes. Relate lines A – L to the lines of service in 24E by the letter of the line. Use the highest level of specificity. Do not provide narrative description in this field. Note: Claims with invalid diagnosis codes will be denied for payment. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 11 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # 22 23 24A Field Description Instructions and Comments Required or Conditional* Resubmission Code and/or Original For resubmissions or adjustments, enter the appropriate bill frequency code (7 or Ref. No. 8 – see below) left justified in the Submission Code section, and the Claim ID# of the original claim in the Original Ref. No. section of this field. Additionally, stamp “resubmitted” or “corrected” on the claim • 7 – Replacement of Prior Claim • 8 – Void/cancel of Prior Claim C Prior Authorization Number Enter the prior authorization number. Refer to the Provider Manual to determine if services rendered require an authorization. C Date(s) Of Service “From” date: MMDDYY. If the service was performed on one day there is no need to complete the “to” date. See page 43 for additional instructions on completing the shaded portion of field 24. R See page 43 for supplemental guidance on the shaded portions of fields 24 A – J. 24B Place Of Service Enter the CMS standard place of service code. “00” for place of service is not acceptable. R 24C EMG This is an emergency indicator field. Enter Y for “Yes” or leave blank for “No” in the bottom (unshaded area of the field). C 24D Procedures, Services Or Supplies CPT/HCPCS/ Modifier Enter the CPT or HCPCS code(s) and modifier (if applicable). Procedure codes (5 digits) and modifiers (2 digits) must be valid for date of service. R Note: Modifiers affecting reimbursement must be placed in the first modifier position. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 12 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # Field Description Instructions and Comments Required or Conditional* 24E Diagnosis Pointer Diagnosis Pointer - Indicate the associated diagnosis by referencing the pointers listed in field 21 (1, 2, 3, or 4). Note: AmeriHealth DC can accept up to eight (8) diagnosis pointers in this field. Diagnosis codes must be valid ICD codes for the date of service. R 24F Charges R 24G Days Or Units Enter charges. A value must be entered. Enter zero ($0.00) or actual charged amount. (This includes capitated services.) Enter quantity. Value entered must be greater than zero. (Field allows up to 3 digits.) 24H Child HealthCheck (EPSDT) Services In Shaded area of field: C R AV - Patient refused referral; S2 - Patient is currently under treatment for referred diagnostic or corrective health problems; NU - No referral given; or ST - Referral to another provider for diagnostic or corrective treatment. In unshaded area of field: “Y” for Yes – if service relates to a pregnancy or family planning “N” for No – if service does not relate to pregnancy or family planning __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 13 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # 24I Field Description Instructions and Comments Required or Conditional* If using NPI in field 24J, enter the qualifier “ZZ”. ID Qualifier R If using a DC Medicaid provider ID for an atypical provider, enter the qualifier “1D”. If the Other ID number is the AmeriHealth DC ID number, enter G2. If the Other ID number is another unique identifier, refer to the NUCC guidelines for the appropriate qualifier. 24J Rendering Provider ID NPI in the bottom (unshaded) portion. Enter the AmeriHealth DC Provider ID number in the top (shaded) portion. The individual rendering the service is reported in 24J. Enter the AmeriHealth DC ID number in the shaded area of the field or, if an atypical provider, enter the provider’s DC Medicaid ID number. Enter the NPI number in the unshaded area of the field. Physician or Supplier's Federal Tax ID number. Recommended R 25 Federal Tax ID Number SSN/EIN R 26 Patient's Account No. Enter the patient’s account number assigned by the provider R 27 Accept Assignment Yes or No must be checked.. R 28 Total Charge Enter the total of all charges listed on the claim. R 29 Amount Paid Required when another carrier is the primary payer. Enter the payment received from the primary payer prior to invoicing the Plan. Medicaid programs are always the payers of last resort. C 30 Reserved for NUCC Use To be determined. 31 Signature Of Physician Or Supplier Signature on file, signature stamp, Including Degrees Or Credentials / computer-generated or actual signature is acceptable. Date Not Required R __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 14 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # Instructions and Comments Required or Conditional* Name And Address Of Facility Where Services Were Rendered (If Other Than Home Or Office). Required. Enter the physical location. (P.O. Box #’s are not acceptable here.) R 32a. NPI number Required unless Rendering Provider is an Atypical Provider and is not required to have an NPI number. R 32b. Other ID# Enter the AmeriHealth DC Provider ID # (strongly recommended) R 32 Field Description (AmeriHealth DC issued Provider Identification Number) Enter the G2 qualifier followed by the DC Medicaid ID #. Required when the Rendering Provider is an Atypical Provider and does not have an NPI number. Enter the twodigit qualifier identifying the non-NPI number followed by the ID number. Do not enter a space, hyphen, or other separator between the qualifier and number. 33 33a. Billing Provider Info & Ph # Required – Identifies the provider that is requesting to be paid for the services rendered and should always be completed. Enter physical location; P.O. Boxes are not acceptable. R NPI number Required unless Rendering Provider is an Atypical Provider and is not required to have an NPI number. R __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 15 Provider Services 202-408-2237 or 888-656-2383 CMS-1500 Claim Form Field Requirements CMS-1500 Claim Form Field # 33b. Field Description Instructions and Comments Other ID# Enter the AmeriHealth DC Provider ID # (strongly recommended.) (AmeriHealth DC issued Provider Identification Number) Required or Conditional* R Required when the Billing Provider is an Atypical Provider and does not have an NPI number. For atypical providers that do not have an NPI, enter the G2 qualifier followed by the DC Medicaid ID #. Do not enter a space, hyphen, or other separator between the qualifier and number. If using NPI in field 33a, enter the taxonomy code in 33b and the qualifier “ZZ” in the box to the left. Note: *DC Medicaid provider numbers may only be used for atypical providers. Atypical providers are providers that do not meet the definition of healthcare provider under the Health Insurance Portability and Accountability Act (HIPAA); for example waiver providers, attendant care providers, chore services providers, respite care providers. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 16 Provider Services 202-408-2237 or 888-656-2383 Professional Claims EDI Mapping EDI Mapping for CMS-1500 CMS-1500 Claim Form EDI Mapping Field # 1 Field Description Instructions and Comments Insurance Program Identification Required or Conditional* 2000B, SBR09 = CI R Commercial Insurance 1a 2 3 Insured ID Number 2010BA/NM1 <Plan Name> Member’s identification number Use 2330A for COB Data R Patient’s Name (Last, First, Middle 2010BA/NM1 New Born (2010CA/NM1) Initial) 2010CA/NM1 2010CA/NM1 2010BA/DMG Patient’s Birth Date/Sex 2010CA/DMG - Newborn R R 2010BA/NM1 4 Insured’s Name (Last, First, Middle Initial) R 5 Patient’s Address (Number, Street, 2010CA/N3/N4 City, State, Zip) Telephone (Include Area Code) 6 Patient Relationship To Insured 7 Insured’s Address (Number, Street, 2010BA/N3/N4 City, State, Zip Code) Telephone (Include Area Code) 8 Reserved for NUCC Use 9 Other Insured's Name (Last, First, 2330A/NM1 Middle Initial) C 9a Other Insured's Policy Or Group # 2320/SBR C 9b Reserved for NUCC Use Not in IG NR 9c Reserved for NUCC Use Not in IG NR 9d Insurance Plan Name Or Program Name 2330 NM1 C R 2000C/PAT01 Blank R NR NR __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 17 Provider Services 202-408-2237 or 888-656-2383 Professional Claims EDI Mapping CMS-1500 Claim Form EDI Mapping Field # 10a,b,c 10d Field Description Instructions and Comments Required or Conditional* Is Patient's Condition Related To: 2300/CLM11 C Claim Codes (Designated by NUCC) Not in IG C 2300/PWK R 11 Insured's Policy Group Or FECA # 11a Insured's Birth Date / Sex 2010BA/DMG02 2010CA/DMG02 R 11b Other Claim ID Not in IG C 11c Insurance Plan Name Or Program Name 2000B/SBR04 C 11d Is There Another Health Benefit Plan? 2000B/SBR05 R 12 Patient's Or Authorized Person's Signature 2300CLM092320/OI04 C 13 Insured's Or Authorized Person's Signature 2300CLM08 14 Date Of Current Illness Injury, Pregnancy (LMP) 2300/DTP03 C 15 Other Date 2300 DTP C 16 Dates Patient Unable To Work In Current Occupation 2300/DTP03 NR 17 Name Of Referring Physician Or Other Source 2310A/NM1 C 17a Other ID Number Of Referring Physician (Plan Provider ID#) 2310A/REF02 C 17b National Provider Identifier (NPI) 2310A/NM109. C 2000B/SBR NR 2320/OI04 (Enter the referring provider’s NPI) __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 18 Provider Services 202-408-2237 or 888-656-2383 Professional Claims EDI Mapping CMS-1500 Claim Form EDI Mapping Field # Field Description Instructions and Comments Required or Conditional* 18 Hospitalization Dates Related To Current Services 2300/DTP 19 Additional Claim Information (Designated by NUCC) 2300/NTE01 NR 20 Outside Lab 2400/PS102 NR 21 Diagnosis Or Nature Of Illness Or Injury. (Relate To 24E) 2300, HIXX R 22 Resubmission Code and/or Original 2300/REF/Qualifier F8 Ref. NoUsed for Original Claim # 2300/REF/ Qualifier 9F Required when CLM05-3 (Claim Frequency Code) indicates this claim is a replacement or void to a previously adjudicated claim. 23 Prior Authorization Number 2300/REF/Qualifier G1 Referral Number 2300/REF/ Qualifier 9F Date(s) Of Service 2400/DTP R 24A C NR C See page 41 for supplemental guidance on the shaded portions of fields 24 A - J 24B Place Of Service 2400/SV105 R 24C EMG 2400/SV109 NR 24D Procedures, Services Or Supplies CPT/HCPCS Modifier 2400/SV1 C 24E Diagnosis Pointer 2400/SV1 R 24F Charges 2400/SV1 R 24G Days Or Units 2400/SV1 R 24H Child HealthCheck Services 2300/CRC03 C 24I ID Qualifier 2310B/REF01 R __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 19 Provider Services 202-408-2237 or 888-656-2383 Professional Claims EDI Mapping CMS-1500 Claim Form EDI Mapping Field # 24J Field Description Instructions and Comments Required or Conditional* 2310B/NM109 Rendering Provider ID R 2310B/REF02 25 Federal Tax ID Number SSN/EIN of Billing Provider 2010AA/REF R 26 Patient's Account No. 2300/CML01 R 27 Accept Assignment Not in IG 28 Total Charge Loop 2300/CLM R 29 Amount Paid 2320/AMT Qualifier D C NR COB data should be submitted as it was received from other payer 2320/AMT Qualifier EAF 30 Reserved for NUCC Use 31 Signature Of Physician Or Supplier Loop 2300/CLM06 Including Degrees Or Credentials / Date 32 Name And Address Of Facility Where Services Were Rendered (If Other Than Home Or Office). NOTE: Ambulance information should be sent as per 837 IG NR NR 2310C R 2310D/2310E 2300/CRC & CR1 32a. NPI number of Supervising Provider name 2310C/NM1 R 32b. Other ID# 2310C/REF01=G2 R (AmeriHealth DC issued Provider Identification Number) Strongly recommended __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 20 Provider Services 202-408-2237 or 888-656-2383 Professional Claims EDI Mapping CMS-1500 Claim Form EDI Mapping Field # 33 Field Description Instructions and Comments Required or Conditional* 2010AA/NM1 2010AA/N3 2010AA/N4 2010AA/PER Billing Provider Info & Ph # R Submission of Taxonomy is strongly 2000A/PRV recommended P.O. Box in the Billing Address will cause the claim to be rejected at the clearinghouse. P.O. Box may only be submitted with the Pay to Provider 33a. 2010AA NPI number R Required unless Rendering Provider is an Atypical Provider and is not required to have an NPI number. 33b. Other ID# AmeriHealth DC issued Provider Identification #) If Billing is also the Rendering Provider: C 2010BB/REF Enter the AmeriHealth DC Plan Provider ID # (strongly encouraged.) Strongly recommended Enter the G2 qualifier followed by the AmeriHealth DC Plan ID #. 2000A/PRV Required when the Rendering Provider is an Atypical Provider and does not have an NPI number. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 21 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 22 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements Required Fields (UB-04 Claim Forms) UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # 1 Field Description Unlabeled Field Billing Provider Name, Address and Telephone Number Instructions and Comments Service Location, no P.O. Boxes Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * R R R R Left justified Line a: Enter the complete provider name. Line b: Enter the complete address. Line c: City, State, and Zip Code (Zip Codes should include Zip + 4 for a total of 9 digits.) Line d: Enter the area code, telephone number. 2 Unlabeled Field Enter Remit Address Billing Provider’s Designated Pay-To Name and Address Billing Provider’s designated pay-to address. (Zip Codes should include Zip + 4 for a total of 9 digits.) Enter the AmeriHealth DC Facility Provider ID number. Left justified 3a Patient Control No. Provider's patient account/control number. R R 3b Medical/Health Record Number The number assigned to the patient’s medical/health record by the provider. C C __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 23 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # 4 Field Description Type Of Bill Instructions and Comments Enter the appropriate three or four -digit code. Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * R R First position is a leading zero – Do not include the leading zero on electronic claims. Second position indicates type of facility. Third position indicates type of care. Fourth position indicates billing sequence. 5 Fed. Tax No. Enter the number assigned by the federal government for tax reporting purposes. R R 6 Statement Covers Period From/Through Enter dates for the full ranges of services being invoiced. MMDDYY R R 7 Unlabeled Field No entry required 8a Patient Identifier Patient AmeriHealth DC ID is conditional if number is different from field 60. C C __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 24 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # 8b Field Description Patient Name Instructions and Comments Patient name is required. Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * R R R R R R Last name, first name, and middle initial. Enter the patient name as it appears on the AmeriHealth DC ID card. Use a comma or space to separate the last and first names. Titles (Mr., Mrs., etc.) should not be reported in this field. Prefix: No space should be left after the prefix of a name e.g., McKendrick. Hyphenated names: Both names should be capitalized and separated by a hyphen (no space). Suffix: A space should separate a last name and suffix. 9a-e Patient Address The mailing address of the patient 9a. Street Address 9b.City 9c. State 9d. ZIP Code 9e. Country Code (report if other than U.S.A.) 10 Patient Birth Date The date of birth of the patient. Right-justified; MMDDYYYY __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 25 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * The sex of the patient recorded at admission, outpatient service, or start of care. R R Admission Date The start date for this episode of care. For inpatient services, this is the date of admission. Rightjustified R R 13 Admission Hour The code referring to the hour during which the patient was admitted for inpatient or outpatient care. Left Justified R R 14 Admission Type A code indicating the priority of this admission/visit. R Not Required 15 Source of Referral for Admission or Visit A code indicating the source of the referral for this admission or visit. R Not Required 16 Discharge Hour Code indicating the discharge hour of the patient from inpatient care. R Not Required 17 Patient Discharge Status A code indicating the disposition or discharge status of the patient at the end of the service for the period covered on this bill, as reported in Field 6. R R 11 Patient Sex 12 Admission 12 – 15 12 __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 26 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * Condition Codes A code used to identify conditions or events relating to the bill that may affect processing. Please see NUCC Specifications Manual Instructions for condition codes and descriptions to complete fields 18 – 28. C C 29 Accident State The accident state field contains the two-digit state abbreviation where the accident occurred. Required when applicable. C C 30 Unlabeled Field Leave Blank. 18 - 28 31a,b – 34a,b Occurrence Codes and Dates Enter the appropriate occurrence code and date. Required when applicable. C C 35a,b – 36a,b Occurrence Span Codes And A code and the related dates that identify an event that Dates relates to the payment of the claim. Required when applicable. C C Reserved C C C C 37a,b 38 Leave Blank. Responsible Party Name and The name and address of the Address party responsible for the bill. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 27 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description 39a,b,c,d Value Codes and Amounts – 41a,b,c,d 42 Revenue Code Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * A code structure to relate amounts or values to identify data elements necessary to process this claim as qualified by the payer organization. Value Codes and amounts. If more than one value code applies, list in alphanumeric order. Required when applicable. Note: If value code is populated then value amount must also be populated and vice versa. Please see NUCC Specifications Manual Instructions for value codes and descriptions to complete fields 39 – 41. C C Codes that identify specific accommodation, ancillary service or unique billing calculations or arrangements. On the last line, enter 0001 for the total. Refer to the Uniform Billing Manual for a list of revenue codes. R R __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 28 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * 43 Revenue Description The standard abbreviated description of the related revenue code categories included on this bill. See NUBC instructions for Field 42 for description of each revenue code category. R R 44 HCPCS/Accommodation Rates 1. The Healthcare Common Procedure Coding system (HCPCS) applicable to ancillary service and outpatient bills. R R 2. The accommodation rate for inpatient bills. 45 Serv. Date Report line item dates of service for each revenue code or HCPCS code. R R 46 Serv. Units Report units of service. A quantitative measure of services rendered by revenue category or for the patient to include items such as number of accommodation days, miles, pints of blood, renal dialysis treatments, observation hours etc. R R __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 29 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * 47 Total Charges Total charges for the primary payer pertaining to the related revenue code for the current billing period as entered in the statement covers period. Total charges include both covered and non-covered charges. Report grand total of submitted charges at the bottom of this field to be associated with revenue code 001. Value entered must be greater than zero ($0.00). R R 48 Non-Covered Charges To reflect the non-covered charges for the destination payer as it pertains to the related revenue code. Required when Medicare is Primary. C C Not required Not required If there is more than one other private payer, lump all amounts together in Field 48 and attach each company’s EOB or RA. 49 Unlabeled Field __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 30 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * 50 Payer Enter the name for each payer being invoiced. When the patient has other coverage, list the payers as indicated below. Line A refers to the primary payer; Line B refers to the, secondary; and Line C refers to the tertiary. R R 51 AmeriHealth DC Identification Number The number used by the health plan to identify itself. AmeriHealth DC’s Payer ID is #77002 R R 52 Rel. Info Release of Information Certification Indicator. This field is required on Paper and Electronic Invoices. R R Line A refers to the primary payer; Line B refers to the secondary; and Line C refers to the tertiary. It is expected that the provider have all necessary release information on file. It is expected that all released invoices contain "Y". 53 Asg. Ben. Assignment of Benefits Certification Indicator is required." R R 54 Prior Payments The A, B, C indicators refer to the information in Field 50. C C __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 31 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * 55 Est. Amount Due Enter the estimated amount due (the difference between “Total Charges” and any deductions such as other coverage). C C 56 National Provider Identifier – Billing Provider The unique NPI identification number assigned to the provider submitting the bill; NPI is the national provider identifier. Required if the health care provider is a Covered Entity as defined in HIPAA Regulations. R R A unique identification number assigned to the provider submitting the bill to AmeriHealth DC. Complete if NPI is not mandated in Field 56. The UB-04 does not use a qualifier to specify the type of Other (Billing) Provider Identifier. Use this field to report other provider identifiers as assigned by the health plan listed in Field 50 A, B and C. C C 57 A,B,C Other (Billing) Provider Identifier AmeriHealth DC issued Provider Identification Number (strongly recommended) __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 32 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * 58 Insured's Name Information refers to the payers listed in field 50. In most cases this will be the patient name. When other coverage is available, the insured is indicated here. R R 59 Patient Rel Enter the patient’s relationship to insured. For Medicaid programs the patient is the insured. R R Enter the patient's Member ID exactly as it appears on the AmeriHealth DC Member ID patient's AmeriHealth DC ID Number card on line B or C. When other insurance is present, enter the AmeriHealth DC Member ID on line A. R R Use this field only when a patient has other insurance and group coverage applies. Do not use this field for individual coverage. C C Code 18: Self 60 Insured’s Unique Identifier 61 Group Name Line A refers to the primary payer; B, secondary; and C, tertiary. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 33 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * Use this field only when a patient has other insurance and group coverage applies. Do not use this field for individual coverage. Line A refers to the primary payer; B, secondary; and C, tertiary. Enter the AmeriHealth DC prior authorization number. Line A refers to the primary payer; B, secondary; and C, tertiary. Field 63A is required. C C R R DCN Document Control Number. New field. The control number assigned to the original bill by the health plan or the health plan’s fiscal agent as part of their internal control. Note: Resubmitted claims must contain the original claim ID. C C 65 Employer Name The name of the employer that provides health care coverage for the insured individual identified in field 58. Required when the employer of the insured is known to potentially be involved in paying this claim. C C 66 The qualifier that denotes the Diagnosis and Procedure Code Qualifier (ICD Version version of International Classification of Diseases (ICD) Indicator) reported. A value of 9 indicates ICD-9, a value of 0 indicates ICD-10. R R 62 Insurance Group No. 63 Treatment Authorization Codes 64 __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 34 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # 67 Field Description Prin. Diag. Cd. and Present on Admission (POA) Indicator 67 A - Q Other Diagnosis Codes 68 Unlabeled Field 69 Admitting Diagnosis Code Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * The ICD codes describing the principal diagnosis (i.e., the condition established after study to be chiefly responsible for causing the use of hospital services that exists at the time of services or develops subsequently to the service that has an effect on the length of stay. R R The ICD diagnoses codes corresponding to all conditions that coexist at the time of service, that develop subsequently, or that affect the treatment received and/or the length of stay. Exclude diagnoses that relate to an earlier episode which have no bearing on the current hospital service. C C The ICD diagnosis code describing the patient’s diagnosis at the time of admission as stated by the physician. Required for inpatient and outpatient admissions. R R __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 35 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments The ICD diagnosis codes describing the patient’s reason for visit at the time of outpatient registration. Required for all outpatient visits. Up to three ICD codes may be entered in fields A, B and C. 70 Patient’s Reason for Visit 71 Prospective Payment System No entry required (PPS) Code 72a-c 73 External Cause of Injury (ECI) Code The ICD diagnosis codes pertaining to external cause of injuries, poisoning, or adverse effect. External Cause of Injury “E” diagnosis codes should not be billed as primary and/or admitting diagnosis. Required if applicable. Unlabeled Field No entry required Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * C R C C C C __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 36 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # 74 Field Description Principal Procedure Code and Date Instructions and Comments The ICD code that identifies the principal procedure performed at the claim level during the period covered by this bill and the corresponding date. Inpatient facility – Surgical procedure code is required if the operating room was used. Other Procedure Codes and Dates C 75 Unlabeled Field C R R The ICD codes identifying all significant procedures other than the principal procedure and the dates (identified by code) on which the procedures were performed. C Inpatient facility – Surgical procedure code is required if the operating room was used. R Outpatient facility or Ambulatory Surgical Center – CPT, HCPCS or ICD code is required when a surgical procedure is performed. 33X 83X Required or Required or Conditional* Conditional * Outpatient Facility or Ambulatory Surgical Center – CPT, HCPCS or ICD code is required when a surgical procedure is performed. 74a-e Outpatient, Bill Types 13X, 23X, C R No entry required __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 37 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # Field Description Instructions and Comments Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * 76 Attending Provider Name and Identifiers NPI#/Qualifier/Other ID# Enter the NPI of the physician who has primary responsibility for the patient’s medical care or treatment in the upper line, and Enter the NPI number of the their name in the lower line, last attending physician name first. If the Attending Physician has another unique ID#, enter the appropriate Enter the AmeriHealth DC descriptive two-digit qualifier issued Provider ID number followed by the other ID#. Enter the last name and first Enter the two digit qualifier name of the Attending that identifies the Other ID Physician. number as the AmeriHealth DC issued Provider ID number R R 77 Operating Physician Name and Identifiers – NPI#/Qualifier/Other ID# Enter the NPI of the physician who performed surgery on the patient in the upper line, and their name in the lower line, last Enter the NPI number of the name first. If the operating physician who performed physician has another unique surgery ID#, enter the appropriate descriptive two-digit qualifier followed by the other ID#. Enter the AmeriHealth DC Enter the last name and first issued Provider ID number name of the Attending Physician. C C R R Enter the two digit qualifier that identifies the Other ID number as the AmeriHealth DC issued Provider ID number Required when a surgical procedure code is listed. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 38 Provider Services 202-408-2237 or 888-656-2383 UB-04 Claim Field Requirements UB-04 Claim Form Field Requirements Inpatient, Bill Types 11X, 12X, 18X, 21X, 22X, 32X Field # 78 – 79 80 Field Description Instructions and Comments Enter the NPI# of any physician, other than the attending physician, who has responsibility for the patient’s Enter the NPI number of medical care or treatment in the another attending physician upper line, and their name in the Enter the AmeriHealth DC lower line, last name first. If issued Provider ID number the other physician has another unique ID#, enter the Enter the two digit qualifier that identifies the Other ID appropriate descriptive twodigit qualifier followed by the number as the AmeriHealth other ID#. DC issued Provider ID number Other Provider (Individual) Names and Identifiers – NPI#/Qualifier/Other ID# Remarks Field 81CC,a-d Code-Code Field Outpatient, Bill Types 13X, 23X, 33X 83X Required or Required or Conditional* Conditional * C C Leave Blank C C To report additional codes related to Form Locator (overflow) or to report externally maintained codes approved by the NUBC for inclusion in the institutional data set. C C __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 39 Provider Services 202-408-2237 or 888-656-2383 Institutional Claims EDI Mapping EDI Mapping Table (UB-04) UB-04 Claim Form EDI Mapping Inpatient, Bill Outpatient, Types 11X, Bill Types 12X, 18X, 13X, 23X, 21X, 22X, 33X 83X 32X Field # 1 2 Field Description Instructions and Comments Unlabeled Field Billing Provider Name, Address and Telephone Number 2010AA/NM1 Submission of Taxonomy is strongly recommended 2000A Unlabeled Field Billing Provider’s Designated Pay-to Name and Address Required or Required or Conditional* Conditional* R R R R 201AA/N3 & N4 2010AB/N3 & N4 3a Patient Control No. 2300 CLM01 R R 3b Medical/Health Record Number 2300/REF C C R R Qualifier EA 4 Type Of Bill 5 Fed. Tax No. 2010AA R R 6 Statement Covers Period From/Through 2300/DTP R R CLM05 __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 40 Provider Services 202-408-2237 or 888-656-2383 Institutional Claims EDI Mapping UB-04 Claim Form EDI Mapping Inpatient, Bill Outpatient, Types 11X, Bill Types 12X, 18X, 13X, 23X, 21X, 22X, 33X 83X 32X Field # Field Description Instructions and Comments 7 Unlabeled Not in IG NR NR 8a Patient Identifier 2010BA C C 8b Patient Name 2010BA/NM1 2010CA/NM1 - Newborn R R Patient Address 2010BA R R 10 Patient Birth Date 2010BA/DMG 2010CA/DMG - Newborn R R 11 Patient Sex 2010BA/DMG 2010CA/DMG - Newborn R R 12 Admission 12 – 15 12 Admission Date 2300/DTP C C 13 Admission Hour 2300/DTP C C 14 Admission Type 2300/CL1 R Not Required 15 Source of Referral for Admission or Visit 2300/CL1 R Not Required 16 Discharge Hour (Date) 2300/DTP R C 17 Patient Discharge Status 2300/DTP R C 9a-e Required or Required or Conditional* Conditional* __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 41 Provider Services 202-408-2237 or 888-656-2383 Institutional Claims EDI Mapping UB-04 Claim Form EDI Mapping Inpatient, Bill Outpatient, Types 11X, Bill Types 12X, 18X, 13X, 23X, 21X, 22X, 33X 83X 32X Field # Field Description Instructions and Comments Required or Required or Conditional* Conditional* 18 - 28 Condition Codes HIXX where HI01= BG C C 29 Accident State 2300/REF C C 30 Unlabeled Field Not in IG NR NR 31a,b – 34a,b Occurrence Codes and Dates HIXX where H101 = BH C C 35a,b – 36a,b Occurrence Span Codes And HIXX where H101 = BI Dates C C Not in IG NR NR Responsible Party Name and Not in IG Address NR NR HIXX where H101 = BE C C 37a,b 38 Reserved 39a,b,c,d Value Codes and Amounts – 41a,b,c,d 42 Rev. Cd. 2400/SV2 R R 43 Revenue Description Not in IG NR NR 44 HCPCS/Accommodation Rates/HIPPS Rate Codes 2400/SV2 R R 45 Serv. Date 2400/DTP R R 46 Serv. Units 2400/SV2 R R 47 Total Charges 2300/CLM0 R R 48 Non-Covered Charges 2300/AMT01 C C NR NR COB data should be submitted as received by other payer 49 Unlabeled Field Not in IG __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 42 Provider Services 202-408-2237 or 888-656-2383 Institutional Claims EDI Mapping UB-04 Claim Form EDI Mapping Inpatient, Bill Outpatient, Types 11X, Bill Types 12X, 18X, 13X, 23X, 21X, 22X, 33X 83X 32X Field # 50 Field Description Instructions and Comments Payer 2010BB/ref Required or Required or Conditional* Conditional* R R Plan Payer ID 51 Health Plan Identification Number 2010BB R R 52 Rel. Info Not in IG NR NR 53 Asg. Ben. Not in IG NR NR 54 Prior Payments Not in IG NR NR 55 Est. Amount Due Not in IG NR NR 56 National Provider Identifier – Billing Provider 2010AA/NM1 R R 2010BB/REF C C R R 57 A,B,C Other (Billing) Provider Identifier 2310A/REF QUALIFIER G2 58 Insured's Name 2010BA/NM1 2010CA/NM1 - Newborn 59 P. Rel If 2000C/PAT01 R R 60 Insured’s Unique Identifier 2010BA/NM1 R R __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 43 Provider Services 202-408-2237 or 888-656-2383 Institutional Claims EDI Mapping UB-04 Claim Form EDI Mapping Inpatient, Bill Outpatient, Types 11X, Bill Types 12X, 18X, 13X, 23X, 21X, 22X, 33X 83X 32X Field # Field Description Instructions and Comments 61 Group Name 2000B/SBR 62 Insurance Group No. 63 64 C C Not in IG NR NR Treatment Authorization Codes Not in IG NR NR DCN 2300/REF02 where REF01= F8 (Original Reference number) C C NR NR Not Not Required Use for submission of original claim number for adjusted or voided claims Not in IG 65 Employer Name 66 Use ICD code qualifiers per Diagnosis and Procedure Code Qualifier (ICD Version IG Indicator) 67 Required or Required or Conditional* Conditional* Prin. Diag. Cd. and Present on Admission (POA) Indicator 67 A - Q Other Diagnosis Codes 2300/HIXX Required R R C C NR NR Qualifier BK 2300/HIXX Qualifier BF 68 Unlabeled Field Not in IG __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 44 Provider Services 202-408-2237 or 888-656-2383 Institutional Claims EDI Mapping UB-04 Claim Form EDI Mapping Field # 69 Field Description Instructions and Comments Admitting Diagnosis Code 2300/HIXX Inpatient, Bill Outpatient, Types 11X, Bill Types 12X, 18X, 13X, 23X, 21X, 22X, 33X 83X 32X Required or Required or Conditional* Conditional* C C C C R R C C NR NR C C C C NR NR R R Qualifier BJ 70 Patient’s Reason for Visit 2300/HIXX Qualifier PR 71 Prospective Payment System 2300/HIXX (PPS) Code Qualifier DR External Cause of Injury (ECI) Code 2300HIXX 73 Unlabeled Field Not in IG 74 Principal Procedure code and Date 2300/HIXX 72a-c 74a-e Qualifier BN Qualifier BR Other Procedure Codes and 2300/HIXX Dates Qualifier BQ 75 Unlabeled Field Not in IG 76 Attending Provider Name and Identifiers NPI#/Qualifier/Other ID# 2310A/NM1 2310/REF Qualifier G2 Enter the NPI number of the attending physician Attending Provider is required __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 45 Provider Services 202-408-2237 or 888-656-2383 Institutional Claims EDI Mapping UB-04 Claim Form EDI Mapping Inpatient, Bill Outpatient, Types 11X, Bill Types 12X, 18X 13X, 23X, 21X, 22X, 33X 83X 32X Field # 77 Field Description Instructions and Comments Required or Required or Conditional* Conditional* Operating Physician Name and Identifiers – NPI#/Qualifier/Other ID# 2310B/NM1 C C 2310C/NM1 C C 2300/NTE. Can leave blank C C NR NR Enter the NPI number of the physician who performed surgery 78 – 79 Other Provider (Individual) Names and Identifiers – NPI#/Qualifier/Other ID# Enter the NPI number of another attending physician 80 Remarks Field 81CC,a-d Code-Code Field Not in IG __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 46 Provider Services 202-408-2237 or 888-656-2383 Common Causes of Claim Processing Delays, Rejections or Denials Special Instructions and Examples for CMS-1500, UB-04 and EDI (837) Claims Submissions I. Supplemental Information A. CMS-1500 Paper Claims – Field 24: Important Note: All unspecified Procedure or HCPCS codes require a narrative description be reported in the shaded portion of field 24. The shaded area of lines 1 through 6 allow for the entry of 61 characters from the beginning of 24A to the end of 24G. The following are types of supplemental information that can be entered in the shaded lines of Item Number 24: Narrative description of unspecified codes National Drug Codes (NDC) for drugs (Only enter one NDC per EDI claim line.) Vendor Product Number – Health Industry Business Communications Council (HIBCC) Product Number Health Care Uniform Code Council – Global Trade Item Number (GTIN) formerly Universal Product Code (UPC) for products Contract rate The following qualifiers are to be used when reporting these services. N4 Narrative description of unspecified code (all miscellaneous fields require this section be reported) National Drug Codes VP Vendor Product Number Health Industry Business Communications Council (HIBCC) OZ Product Number Health Care Uniform Code Council – Global Trade Item Number (GTIN) CTR Contract rate ZZ To enter supplemental information, begin at 24A by entering the qualifier and then the information. Do not enter a space between the qualifier and the number/code/information. Do not enter hyphens or spaces within the number/code. More than one supplemental item can be reported in the shaded lines of Item Number 24. Enter the first qualifier and number/code/information at 24A. After the first item, enter three blank spaces and then the next qualifier and number/code/information. B. EDI – Field 24D (Professional): Details pertaining to Anesthesia Minutes, and corrected claims may be sent in Notes (NTE). Details sent in claim level NTE that will be included in claim processing (837): Please include L1, L2, etc. to show line numbers related to the details. Please include these letters AFTER those specified below: o Anesthesia Minutes need to begin with the letters ANES followed by the specific times o Corrected claims need to begin with the letters RPC followed by the details of the original claim (as per contract instructions) o DME Claims requiring specific instructions should begin with DME followed by specific details __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 47 Provider Services 202-408-2237 or 888-656-2383 Common Causes of Claim Processing Delays, Rejections or Denials C. EDI – Field 33b (Professional): Field 33b – Other ID# - Professional: 2310B loop, REF01=G2, REF02+ Plan’s Provider Network Number. Less than 17 Digits Alphanumeric. Field is strongly suggested. Note: do not send the provider on the 2400 loop. This loop is not used in determining the provider ID on the claim. D. EDI – Field 45 and 51(Institutional): Field 45 – Service Date must not be earlier than the claim statement date. Service Line Loop 2400, DTP*472 Claim statement date Loop 2300, DTP*434 Field 51 – Health Plan ID – the number used by the health plan to identify itself. AmeriHealth DC’s Health Plan EDI Payer ID# is 77002. EDI – Reporting DME DME Claims requiring specific instructions should begin with DME followed by specific details. Example: NTE* DME AEROSOL MASK, USED W/DME NEBULIZER Example: NTE*ADD* NO LIABILITY, PATIENT FELL AT HOME~ E. Reporting NDC on CMS-1500 and UB-04 and EDI: 1. NDC on CMS-1500 NDC should be entered in the shaded sections of item 24A through 24G To enter NDC information, begin at 24A by entering the qualifier N4 and then the 11 digit NDC information o Do not enter a space between the qualifier and the 11 digit NDC number o Enter the 11 digit NDC number in the 5-4-2 format (no hyphens) o Do not use 99999999999 for a compound medication, bill each drug as a separate line item with its appropriate NDC Enter the drug name and strength Enter the NDC quantity unit qualifier o F2 – International Unit o GR – Gram o ML – Milliliter o UN – Unit Enter the NDC quantity o Note: The NDC quantity is frequently different than the HCPC code quantity __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 48 Provider Services 202-408-2237 or 888-656-2383 Common Causes of Claim Processing Delays, Rejections or Denials Example of entering the identifier N4 and the NDC number on the CMS-1500 claim form: N4 qualifier NDC Unit Qualifier 11 digit NDC NDC Quantity 2. NDC on UB-04 NDC should be entered in Form Locator 43 in the Revenue Description Field Report the N4 qualifier in the first two (2) positions, left-justified o Do not enter spaces o Enter the 11 character NDC number in the 5-4-2 digit format (no hyphens) o Do not use 99999999999 for a compound medication, bill each drug as a separate line item with its appropriate NDC Immediately following the last digit of the NDC (no delimiter), enter the Unit of Measurement Qualifier o F2 – International Unit o GR – Gram o ML – Milliliter o UN – Unit Immediately following the Unit of Measure Qualifier, enter the unit quantity with a floating decimal for fractional units limited to 3 digits (to the right of the decimal) o Any unused spaces for the quantity are left blank Note that the decision to make all data elements left-justified was made to accommodate the largest quantity possible. The description field on the UB-04 is 24 characters in length. An example of the methodology is illustrated below. N 4 1 2 3 4 5 6 7 8 9 0 1 U N 1 2 4 5 . 5 6 7 3. NDC via EDI The NDC is used to report prescribed drugs and biologics when required by government regulation, or as deemed by the provider to enhance claim reporting/adjudication processes. EDI claims with NDC info should be reported in the LIN segment of Loop ID-2410. This segment is used to specify billing/reporting for drugs provided that may be part of the service(s) described in SV2. Please consult your EDI vendor if not submitting in X12 format for details on where to submit the NDC number to meet this specification. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 49 Provider Services 202-408-2237 or 888-656-2383 Common Causes of Claim Processing Delays, Rejections or Denials When LIN02 equals N4, LIN03 contains the NDC number. This number should be 11 digits sent in the 54-2 format with no hyphens. Submit one occurrence of the LIN segment per claim line. Claims requiring multiple NDC’s sent at claim line level should be submitted using CMS-1500 or UB-04 paper claim. When submitting NDC in the LIN segment, the CTP segment is required with 5010 HIPAA. This segment is to be submitted with the Unit of Measure and the Quantity. Federal Tax ID on UB-04: Federal Tax ID on UB-04 (Box# 5) will come from Loop 2010AA, REF02. Condition codes Condition codes (Box number 18 thru 29) will come from 2300 CRC01 – CRC07 Patient reason DX Patient reason DX (Box 70) qualifier will be PR qualifier from 2300, HI01. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 50 Provider Services 202-408-2237 or 888-656-2383 Common Causes of Claim Processing Delays, Rejections or Denials Common Causes of Claim Processing Delays, Rejections or Denials Authorization Number Invalid or Missing A valid authorization number must be included on the claim form for all services requiring prior authorization from AmeriHealth DC. Attending Physician ID Missing or Invalid – Inpatient claims must include the name of the physician who has primary responsibility for the patient's medical care or treatment, and the medical license number on the appropriate lines in field number 76 (Attending Physician ID) of the UB-04 claim form. A valid medical license number is formatted as two alpha, six numeric, and one alpha character (AANNNNNNA) OR two alpha and six numeric characters (AANNNNNN). An attending physician is required. Billed Charges Missing or Incomplete – A billed charge amount must be included for each service/procedure/supply on the claim form. Diagnosis Code Missing 4th or 5th Digit – Precise coding sequences must be used in order to accurately complete processing. Review the ICD-9-CM or ICD-10-CM manual for the 4th and 5th digit extensions. Look for the th or th symbols in the coding manual to determine when additional digits are required. Diagnosis, Procedure or Modifier Codes Invalid or Missing Coding from the most current coding manuals (ICD-9-CM, or ICD-10-C, CPT or HCPCS) is required in order to accurately complete processing. All applicable diagnosis, procedure and modifier fields must be completed. EOBs (Explanation of Benefits) from Primary Insurers Missing or Incomplete – A copy of the EOB from all third party insurers must be submitted with the original claim form for paper claims. Include pages with run dates, coding explanations and messages. AmeriHealth DC accepts EOBs via paper or electronic format (EDI). External Cause of Injury Codes – External Cause of Injury “E” diagnosis codes should not be billed as primary and/or admitting diagnosis. Future Claim Dates – Claims submitted for Medical Supplies or Services with future claim dates will be denied, for example, a claim submitted on October 1 for bandages that are delivered for October 1 through October 31 will deny for all days except October 1. Important: Include all primary and secondary diagnosis codes on the claim. Important: Missing or invalid data elements or incomplete claim forms will cause claim processing delays, inaccurate payments, rejections or denials. Important: Regardless of whether reimbursement is expected, the billed amount of the service must be documented on the claim. Missing charges will result in rejections or denials. Important: All billed codes must be complete and valid for the time period in which the service is rendered. Incomplete, discontinued, or invalid codes will result in claim rejections or denials. Important: State level HCPCS coding takes precedence over national level codes unless otherwise specified in individual provider contracts. Important: The services billed on the claim form should exactly match the services and charges detailed on the accompanying EOB. If the EOB charges appear different due to global coding requirements of the primary insurer, submit claim with the appropriate coding which matches the total charges on the EOB. Important: Child HealthCheck services may be submitted electronically or on paper. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 51 Provider Services 202-408-2237 or 888-656-2383 Common Causes of Claim Processing Delays, Rejections or Denials Handwritten Claims – Completely handwritten claims will be rejected. Legible handwritten claims are acceptable on resubmitted claims. (See Illegible Claim Information) Important: For claims with COB, the adjudication date of the other payer is required for EDI and paper claims Highlighted Claim Fields – (See Illegible Claim Information) Important: Submitting the original copy of the claim form will assist in assuring claim information is legible. Illegible Claim Information – Information on the claim form must be legible in order to avoid delays or inaccuracies in processing. Review billing processes to ensure that forms are typed or printed in black ink, that no fields are highlighted (this causes information to darken when scanned or filmed), and that spacing and alignment are appropriate. Handwritten information often causes delays or inaccuracies due to reduced clarity. Incomplete Forms – All required information must be included on the claim forms in order to ensure prompt and accurate processing. Member Name Missing – The name of the member must be present on the claim form and must match the information on file with the Plan. Member Plan Identification Number Missing or Invalid – Enter the patient’s Member ID exactly as it appears on the patient’s AmeriHealth DC Member ID card. The member’s AmeriHealth DC ID must be included on the claim form or electronic claim submitted for payment. Newborn Claim Information Missing or Invalid – Always include the first and last name of the mother and baby on the claim form. If the baby has not been named, insert “Baby Girl” or “Baby Boy” in front of the mother’s last name as the baby’s first name. Verify that the appropriate last name is recorded for the mother and baby. Payer or Other Insurer Information Missing or Incomplete – Include the name, address and policy number for all insurers covering the Plan member. Place of Service Code Missing or Invalid – A valid and appropriate two digit numeric code must be included on the claim form. Refer to CMS-1500 coding manuals for a complete list of place of service codes. Provider Name Missing – The name of the provider of service must be present on the claim form and must match the service provider name and TIN on file with the Plan. Important: The individual provider name and NPI number as opposed to the group NPI number must be indicated on the claim form. Important: Do not highlight any information on the claim form or accompanying documentation. Highlighted information will become illegible when scanned or filmed. Important: Do not attach notes to the face of the claim. This will obscure information on the claim form or may become separated from the claim prior to scanning. Important: Submit newborn’s facility bill for child at the time of delivery using the baby’s Medicaid ID. The newborn’s Medicaid ID is to be used on well babies, babies with extended stays (sick babies) past the mother’s stay and on all aftercare and professional bills. The facility or provider should obtain the newborn’s Medicaid ID via the eligibility verification system operated by DHCF before submitting the claim to AmeriHealth DC. Important: The claim for baby must include the baby’s date of birth as opposed to the mother’s date of birth. Important: On claims for twins or other multiple births, indicate the birth order in the patient name field e.g. Baby Girl Smith A, Baby Girl Smith B, etc. Important: Date of service and billed charges should exactly match the services and charges detailed on the accompanying EOB. If the EOB charges appear different due to global coding requirements of the primary insurer, submit claim with the appropriate coding which matches the total charges on the EOB. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 52 Provider Services 202-408-2237 or 888-656-2383 Common Causes of Claim Processing Delays, Rejections or Denials Provider NPI Number Missing or Invalid – The individual NPI and group NPI numbers for the service provider must be included on the claim form. Revenue Codes Missing or Invalid – Facility claims must include a valid four-digit numeric revenue code. Refer to UB-04 coding manuals for a complete list of revenue codes. Spanning Dates of Service Do Not Match the Listed Days/Units – Span-dating is only allowed for identical services provided on consecutive dates of service. Always enter the corresponding number of consecutive days in the days/unit field. Tax Identification Number (TIN) Missing or Invalid - The Tax ID number must be present and must match the service provider name and payment entity (vendor) on file with the Plan. Third Party Liability (TPL) Information Missing or Incomplete – Any information indicating a work related illness/injury, no fault, or other liability condition must be included on the claim form. Additionally, a copy of the primary insurer’s explanation of benefits (EOB) or applicable documentation must be forwarded along with the claim form. Type of Bill – A code indicating the specific type of bill (e.g., hospital inpatient, outpatient, adjustments, voids, etc). The first digit is a leading zero. Do not include the leading zero on electronic claims. Taxonomy –The provider’s taxonomy number is required if needed by the plan to determine the provider’s plan ID when using NPI only is not effective. Important: The individual service provider name and NPI number must be indicated on all claims, including claims from outpatient clinics. Using only the group NPI or billing entity name and number will result in rejections, denials, or inaccurate payments. Important: When the provider or facility has more than one NPI number, use the NPI number that matches the services submitted on the claim form. Imprecise use of NPI numbers results in inaccurate payments or denials. Important: When submitting electronically, the provider NPI number must be entered at the claim level as opposed to the claim line level. Failure to enter the provider NPI number at the claim level will result in rejection. Please review the rejection report from the EDI software vendor each day. Important: Claims without the provider signature will be rejected. The provider is responsible for re-submitting these claims within 180 calendar days from the date of service. See timely filing guidelines on page 3. Important: Claims without a tax identification number (TIN) will be rejected. The provider is responsible for re-submitting these claims within 180 calendar days from the date of service. See timely filing guidelines on page 3. Important: Any changes in a participating provider’s name, address, NPI number, or tax identification number(s) must be reported to AmeriHealth DC immediately. Contact Provider Services at 202-408-2237 or 888-656-2383 to assist in updating the AmeriHealth DC record. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 53 Provider Services 202-408-2237 or 888-656-2383 Electronic Data Interchange (EDI) Quick Tips Electronic Data Interchange (EDI) for Medical and Hospital Claims Electronic Data Interchange (EDI) allows faster, more efficient and cost-effective claim submission for providers. EDI, performed in accordance with nationally recognized standards, supports the health care industry’s efforts to reduce administrative costs. The benefits of billing electronically include: Reduction of overhead and administrative costs. EDI eliminates the need for paper claim submission. It has also been proven to reduce claim re-work (adjustments). Receipt of clearinghouse reports makes it easier to track the status of claims. Faster transaction time for claims submitted electronically. An EDI claim averages about 24 to 48 hours from the time it is sent to the time it is received. This enables providers to easily track their claims. Important: Please allow for normal processing time before resubmitting the claim either through EDI or paper claim. This will reduce the possibility of your claim being rejected as a duplicate claim. Important: In order to verify satisfactory receipt and acceptance of submitted records, please review both the Emdeon Acceptance report, and the R059 Plan Claim Status Report. Refer to the Claim Filing section for general claim submission guidelines. Validation of data elements on the claim form. By the time a claim is successfully received electronically, information needed for processing is present. This reduces the chance of data entry errors that occur when completing paper claim forms. Quicker claim completion. Claims that do not need additional investigation are generally processed quicker. Reports have shown that a large percentage of EDI claims are processed within 10 to 15 days of their receipt. All the same requirements for paper claim filing apply to electronic claim filing. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 54 Provider Services 202-408-2237 or 888-656-2383 Electronic Data Interchange (EDI) Quick Tips Electronic Claims Submission (EDI) The following sections describe the procedures for electronic submission for hospital and medical claims. Included are a high level description of claims and report process flows, information on unique electronic billing requirements, and various electronic submission exclusions. Hardware/Software Requirements There are many different products that can be used to bill electronically. As long as you have the capability to send EDI claims to Emdeon, whether through direct submission or through another clearinghouse/vendor, you can submit claims electronically. Contracting with Emdeon and Other Electronic Vendors If you are a provider interested in submitting claims electronically to the Plan but do not currently have Emdeon EDI capabilities, you can contact the Emdeon Provider Support Line at 877-363-3666. You may also choose to contract with another EDI clearinghouse or vendor who already has Emdeon capabilities. Contacting the EDI Technical Support Group Providers interested in sending claims electronically may contact the EDI Technical Support Group for information and assistance in beginning electronic submissions. Important: Emdeon is the largest clearinghouse for EDI Healthcare transactions in the world. It has the capability to accept electronic data from numerous providers in several standardized EDI formats and then forwards accepted information to carriers in an agreed upon format. Important: Contact AmeriHealth DC’s EDI Technical Support by calling 202408-2237 or 888-656-2383 and choosing the appropriate prompts. Or by e-mail at [email protected] Important: Providers using Emdeon or other clearinghouses and vendors are responsible for arranging to have rejection reports forwarded to the appropriate billing or open receivable departments. Important: The Payer ID for AmeriHealth DC is 77002 NOTE: Plan payer specific edits are described in Exhibit 99 at Emdeon. When ready to proceed: Read over the instructions within this booklet carefully, paying special attention to the information on exclusions, limitations, and especially, the rejection notification reports. Contact your EDI software vendor and/or Emdeon to inform them you wish to initiate electronic submissions to the Plan. Be prepared to inform the vendor of the Plan’s electronic payer identification number. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 55 Provider Services 202-408-2237 or 888-656-2383 Electronic Data Interchange (EDI) Quick Tips Specific Data Record Requirements Claims transmitted electronically must contain all the same data elements identified within the EDI Claim Filing sections of this booklet. EDI guidance for Professional Medical Services claims can be found beginning on page 13. EDI guidance for Facility Claims can be found beginning on page 36. Emdeon or any other EDI clearing-house or vendor may require additional data record requirements. Electronic Claim Flow Description In order to send claims electronically to the Plan, all EDI claims must first be forwarded to Emdeon. This can be completed via a direct submission or through another EDI clearinghouse or vendor. Once Emdeon receives the transmitted claims, the claim is validated for HIPAA compliance and the Plan’s Payer Edits as described in Exhibit 99 at Emdeon. Claims not meeting the requirements are immediately rejected and sent back to the sender via an Emdeon error report. The name of this report can vary based upon the provider’s contract with their intermediate EDI vendor or Emdeon. Accepted claims are passed to the Plan, and Emdeon returns an acceptance report to the sender immediately. Claims forwarded to the Plan by Emdeon are immediately validated against provider and member eligibility records. Claims that do not meet this requirement are rejected and sent back to Emdeon, which also forwards this rejection to its trading partner – the intermediate EDI vendor or provider. Claims passing eligibility requirements are accepted for claims processing. Claims are not considered as received under timely filing guidelines if rejected for missing or invalid provider or member data. Important: Rejected electronic claims may be resubmitted electronically once the error has been corrected. Important: Emdeon will produce an Acceptance report * and a R059 Plan Claim Status Report** for its trading partner whether that is the EDI vendor or provider. Providers using Emdeon or other clearinghouses and vendors are responsible for arranging to have these reports forwarded to the appropriate billing or open receivable departments. * An Acceptance report verifies acceptance of each claim at Emdeon. ** A R059 Plan Claim Status Report is a list of claims that passed Emdeon’s validation edits. However, when the claims were submitted to the Plan, they encountered provider or member eligibility edits. Important: Claims are not considered as received under timely filing guidelines if rejected for missing or invalid provider or member data. Timely filing Note: Your claims must be received by the EDI vendor by 9:00 p.m. in order to be transmitted to the Plan the next business day. Providers are responsible for verification of EDI claims receipts. Acknowledgements for accepted or rejected claims received from Emdeon or other contracted EDI software vendors, must be reviewed and validated against transmittal records daily. Because Emdeon returns acceptance reports directly to the sender, submitted claims not accepted by Emdeon are not transmitted to the Plan. If you would like assistance in resolving submission issues reflected on either the Acceptance or R059 Plan Claim Status reports, contact the Emdeon Provider Support Line at 1-800-8456592. If you need assistance in resolving submission issues identified on the R059 Plan Claim Status report, contact the AmeriHealth DC EDI Technical Support Hotline by calling 202-408-2237 or 888656-2383 and selecting the appropriate prompts or by e-mail at [email protected] __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 56 Provider Services 202-408-2237 or 888-656-2383 Electronic Data Interchange (EDI) Quick Tips Invalid Electronic Claim Record Rejections/Denials All claim records sent to the Plan must first pass Emdeon HIPAA edits and Plan specific edits prior to acceptance. Claim records that do not pass these edits are invalid and will be rejected without being recognized as received at the Plan. In these cases, the claim must be corrected and re-submitted within the required filing deadline of 180 calendar days from the date of service. It is important that you review the Acceptance or R059 Plan Claim Status reports received from Emdeon or your EDI software vendor in order to identify and re-submit these claims accurately. Plan Specific Electronic Edit Requirements The Plan currently has specific edits and guidelines for professional and institutional claims sent electronically: Member Number must be less than 17 AN Statement date must be not be earlier than the date of service Plan Provider ID is strongly encouraged Taxonomy ID is strongly encouraged Claim line may be zero for encounters Release of Information permits a Y or I Only one NDC number is permitted per claim line Claims for dates of service prior to May 1, 2013 will be rejected for incorrect payer ID. Exclusions Certain claims are excluded from electronic billing. These exclusions fall into two groups: These exclusions apply to inpatient and outpatient claim types. Important: Requests for adjustments may be submitted electronically, on paper or by telephone. By Telephone: Provider Claim Services 202-408-2237 or 888-656-2383 (Select the appropriate prompts.) On Paper: If you prefer to write, please be sure to stamp each claim submitted “corrected” or “resubmission” and address the letter to the appropriate claims address as listed on page 2. Important: Contact Emdeon Provider Support Line at 1-800-845-6592 Important: Claims submitted can only be verified using the Accept and/or Reject Reports. Contact your EDI software vendor or Emdeon to verify you receive the reports necessary to obtain this information. Important: When you receive the Rejection report from Emdeon or your EDI vendor, the plan does not receive a record of the rejected claim. Important: Plan expects claims to be submitted for the subscriber, including newborns. The use of the 2010CA loop should be limited. Excluded Claim Categories At this time, these claim records must be submitted on paper. Claim records requiring supportive documentation. Claim records for medical, administrative or claim appeals. Excluded Provider Categories Claims issued on behalf of the following providers must be submitted on paper. Providers not transmitting through Emdeon or providers sending to Vendors that are not transmitting (through Emdeon) NCPDP Claims __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 57 Provider Services 202-408-2237 or 888-656-2383 Electronic Data Interchange (EDI) Quick Tips Electronic Submission of Coordination of Benefits (COB) Claims COB data may be submitted via the 837 claim transactions. The claim must be adjudicated prior to submission to the plan(s), and the claim must contain payment details from the other carrier(s). COB information should be submitted to AmeriHealth DC as it was received from the other payer. If received at the line level, please submit the claim’s COB information at line level. If received at claim level, please submit the claim’s COB information at claim level. As an example, 837P COB claims are typically at the line level and 837I COB claims are typically at claim level. COB data must include the adjudication data from the other payer. AmeriHealth DC should not to be included as another payer for COB data. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 58 Provider Services 202-408-2237 or 888-656-2383 Common Rejections Resubmitting Professional Corrected Claims Providers using electronic data interchange (EDI) can submit “professional” corrected claims electronically rather than via paper to AmeriHealth DC. Please send the correct identifier on the CLM segment (CLM05-3 of 6, 7, or 8) and include the previous claim number in the 2300 loop, REF segment, using the F8 qualifier. You may also send the claim number in the claim level notes segment (2300n loop, NTE segment, ADD qualifier. RPC must be the first 3 characters of the NTE02 element). Remember to: Use frequency code “6” for replacement of a prior claim or frequency code “7” for adjustment of prior claims utilizing bill type in loop 2300, CLM05-03 (837P) Include the original claim number in Loop 2300, segment REF01=F8 and REF02=the original claim number; no dashes or spaces Do include the Plan’s claim number in order to submit your claim with the 6 or 7 Do use this indicator for claims that were previously processed (approved or denied) Do not use this indicator for claims that contained errors and were not processed (rejected upfront) Do not submit corrected claims electronically and via paper at the same time For more information, please contact the AmeriHealth DC EDI Hotline by calling 202-408-2237 or 888-656-2383 and selecting the appropriate prompts or by emailing to: [email protected]. Common Rejections Invalid Electronic Claim Records – Common Rejections from Emdeon Claims with missing or invalid batch level records Claim records with missing or invalid required fields Claim records with invalid (unlisted, discontinued, etc.) codes (CPT-4, HCPCS, ICD-9 or ICD-10, etc.) Claims without member numbers Important: Claims originally rejected for missing or invalid data elements must be corrected and re-submitted within 180 calendar days from the date of service. Rejected claims are not registered as received in the claim processing system. (Refer to the definitions of rejected and denied claims on page 1 and to the timely filing guidelines on page 3.) Important: Before resubmitting claims, check the status of your submitted claims by calling Provider Services or inquiring online at www.amerihealthdc.com. Important: Corrected Professional Claims may be sent in on paper via the CMS-1500 form or via EDI submission. If sending paper, please stamp each claim submitted “corrected” or “resubmission” and send all corrected or resubmitted claims to the appropriate mailing address as listed on page 2. Important: Corrected Institutional and Professional claims may be resubmitted electronically using the appropriate bill type to indicate that it is a corrected claim. Adjusted claims must be identified in the bill type. Invalid Electronic Claim Records – Common Rejections from the Plan (EDI Edits within the Claim System) Claims received with invalid provider numbers Claims received with invalid member numbers Claims received with invalid member date of birth o __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 59 Provider Services 202-408-2237 or 888-656-2383 Common Rejections Common Rejections, continued NPI Processing – The Plan’s Provider Number is determined from the NPI number using the following criteria: 1. Plan ID, Tax ID and NPI number 2. If no single match is found, the Service Location’s ZIP code is used 3. If no service location is include, the billing address ZIP code will be used 4. If no single match is found, the Taxonomy is used 5. If no single match is found, the claim is researched to determine the appropriate Plan Provider Number to use for claims processing. 6. If a Plan Provider ID is sent using the G2 qualifier, it is used as the provider on the claim. The legacy Plan ID is used as the primary ID on the claim 7. If you have submitted a claim, and you have not received a rejection report, but are unable to locate your claim via online inquiry, it is possible that your claim is in review by AmeriHealth DC. Please check with provider services and update you NPI data as needed. It is essential that the service location of the claim match the NPI information sent on the claim in order to have your claim processed effectively. Important: If you have not received a rejection for a claim, and the claim is not available via claim status inquiry, please contact Provider Services (Claims Unit). Resolution of the NPI data may be needed in order to avoid claim denials for invalid provider. Contact the Emdeon Provider Support Line at: 1-800-845-6592 Contact AmeriHealth DC EDI Technical Support by calling: 202-408-2237 or 888-656-2383 (and selecting the appropriate prompts) Important: Provider NPI number validation is not performed at Emdeon. Emdeon will reject claims for provider NPI only if the provider number fields are empty. Important: The Plan’s Provider ID is recommended as follows: 837P – Loop 2310B, REF*G2[PIN] 837I – Loop 2310A, REF*G2[PIN] __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 60 Provider Services 202-408-2237 or 888-656-2383 Appendix Supplemental Information Allergy Testing/Immunotherapy AmeriHealth DC reimburses complete service codes that allow for combined billing of preparation and injection. Provision of allergen preparation and injection services may be reimbursed together. Evaluation and management visit codes may be reimbursed in addition to allergen immunotherapy only if other identifiable services are provided and documented during the same visit. Preparation of single dose vials, procedure code 95144, may be reimbursed only when an allergist is preparing extract to be injected by another physician. Preparation of a multiple dose vial may be reimbursed only once per treatment cycle using procedure codes 95145-95170. Ambulatory Surgical Centers Ambulatory Surgical Centers (ASC) are required to bill on CMS-1500 or 837 Format. Multiple surgery deduction is paid at 100% of payment group rate for the primary procedure on line one, 50% of the payment group for the secondary procedure on line 2, 25% of the tertiary procedure on line 3, 25% for all subsequent procedures. Medicaid payment for a single bilateral procedure in one day is 150 percent of the payment group rate. It is billed on line 1 of the claim using modifier 50. Anesthesia Anesthesia claims must be submitted via the CMS-1500 or electronic equivalent with the following information in each line or loop: Item 24D/Loop 2400 – report the appropriate ASA procedure code and modifier (if applicable). Item 24F/Loop 2300 – report the actual charged amount. Item 24G/Loop 2400 – report the actual total anesthesia time in minutes. Fifteen (15) minute time increments will be used by the claims payment system to determine the payment from the actual total anesthesia time in minutes, as reported in 24G/Loop 2400. Behavioral Health Behavioral health providers will follow the same claim submission procedures as medical health care providers. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 61 Provider Services 202-408-2237 or 888-656-2383 Appendix Chemotherapy Effective July 1, 2013, AmeriHealth DC will require oncology providers to obtain prior authorization for chemo and/or any other specialty drugs, including injectables, from PerformRx via the process described below. 1. Select the appropriate prior authorization form, available online at www.amerihealthdc.com. [Hint: Click Providers at the top of the page and then click Forms on the left. Look for the specialty prior authorization forms under the heading “Pharmacy Authorization Forms.”] 2. Complete the appropriate form and fax to PerformRx at 855-811-9332. 3. Upon approval by PerformRx, the requested drug will be shipped to your practice within 48 hours. Please indicate the appropriate mailing address on the prior authorization form at the time of your request. 4. You may choose to either: o Use your private stock and replace it with the shipment from PerformRx; OR, o Schedule services around the delivery of the shipment from PerformRx. Child HealthCheck (EPSDT) Services All AmeriHealth District of Columbia PCPs are responsible to provide HealthCheck services to members from birth to age 21, according to the DC Medicaid HealthCheck Periodicity Schedule and the DC Medicaid Dental Periodicity Schedule. View the most recent Periodicity Schedules at www.dchealthcheck.net. Specific billing guidance for screenings is provided below. For additional information, please see “Immunizations,” “Well Child Visits” and “Weight Assessment and Counseling for Nutritional and Physical Activity.” Procedure Code(s) Service 99381 Initial Med Screen < age 1 99382 Initial Med Screen age 1 to 5 99383 Initial Med Screen age 6 to 12 99384 Initial Med Screen age 12 to 18 99385 Initial Med Screen age 18 to 20 99391 Periodic Med Screen < age 1 99392 Periodic Med Screen age 1 to 5 99393 Periodic Med Screen age 6 to 12 99394 Periodic Med Screen age 12 to 18 __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 62 Provider Services 202-408-2237 or 888-656-2383 Appendix 99395 Periodic Med Screen age 18 to 20 83655 Lead Screening in Children Dental Claims (DentaQuest) DentaQuest is the delegated manager of dental services covered by AmeriHealth DC. Please visit www.dentaquest.com for more information about how to bill for these services or contact their Provider Services department at 800-341-8478. Diabetes Please refer to the 2013 HEDIS guidelines provided at the back of this document. Durable Medical Equipment Claims for durable medical equipment will be submitted via the same claim submission procedures as other medical services. Family Planning Submit claims via CMS-1500, UB-04 or via 837 electronic format. AmeriHealth DC members may access family planning services through any family planning clinic or provider without a referral. Some services may require prior authorization. Certain services such as sterilizations and hysterectomy require the submission of a consent form with the claim. Family Planning (non-obstetric) Only one initial family planning visit per recipient per birth center can be reimbursed. Training on use of natural family planning methods is not reimbursable. Insertion or removal of Norplant is reimbursable in addition to a family planning initial or annual visit or an evaluation and management visit if all components of an evaluation and management visit are met and documented in addition to the Norplant services. Insertion of an IUD is reimbursable in addition to a family planning initial or annual visit or an evaluation and management visit if all components of an evaluation and management visit are met and documented in addition to the IUD service. Reimbursement for the IUD device is covered using the appropriate J-code or HCPCS procedure code, including J7300, J7302, J7306, and J7307. Procedure code 99070 is not an appropriate code and cannot be reimbursed for an IUD. Removal of an IUD is reimbursable when performed as a separate procedure. No visits can be reimbursed on the same day to the same provider. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 63 Provider Services 202-408-2237 or 888-656-2383 Appendix Family planning procedure codes are not reimbursable on the same date of service to the same recipient with any evaluation and management procedure codes. Immunizations Please refer to the 2013 HEDIS guidelines provided at the back of this document. Injectable Drugs All specialty drugs and injectables currently require prior authorization from PerformRx via the process described below: 1. Select the appropriate prior authorization form, available online at www.amerihealthdc.com. [Hint: Click Providers at the top of the page and then click Forms on the left. Look for the specialty prior authorization forms under the heading “Pharmacy Authorization Forms.”] 2. Complete the appropriate form and fax to PerformRx at 855-811-9332. 3. Upon approval by PerformRx, the requested drug will be shipped to your practice within 48 hours. Please indicate the appropriate mailing address on the prior authorization form at the time of your request. 4. You may choose to either: o Use your private stock and replace it with the shipment from PerformRx; OR, o Schedule services around the delivery of the shipment from PerformRx. Injectable medications are reimbursed by billing the appropriate A, J, Q, S or HCPCS procedure code when a provider purchases and administers the medication in the office. Providers must enter the National Drug Code (NDC) on the claim when billing for any injectable medication. All drugs billed are required to be submitted with NDC information and may be submitted via CMS-1500 or 837 electronic format. Refer to NDC instructions in Supplemental Information section on page 47. The NDC number and the HCPCS code for drug products are required on both the 837 format and the CMS-1500 for reimbursable medications. Claims submitted without NDC information and a valid HCPCS code will be denied. Maternity Conditions related to the prenatal period must be billed as prenatal visits. Services provided during the pregnancy that are not related to the pregnancy diagnosis code may be billed as evaluation and management visits with the appropriate non-pregnancy diagnosis code. Prenatal hospital visits in the obstetrical unit for a length of stay less than 24 hours are billed with the appropriate evaluation and management observation codes. The Prenatal Risk Screening should be offered at the first prenatal visit. The prenatal visit that includes completion of the Prenatal Risk Screening is reimbursed once per pregnancy by billing procedure code H1001, add modifier TG if the screening is completed during the first trimester. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 64 Provider Services 202-408-2237 or 888-656-2383 Appendix Prenatal visits must be billed using H1001 or other acceptable codes. Venipuncture, specimen handling and transportation, urinalysis and H&H are included in the prenatal visit reimbursement To prevent inappropriate claim denials, providers are advised to bill prenatal visits as they occur. Maternity Birthing Center (obstetric) The procedure code is H1000. Manual or automated urine, hemoglobin and hematocrit tests performed as part of an evaluation and management visit are not reimbursed in addition to the evaluation and management visit. The provider may not bill for them as separate procedures. Conditions related to the prenatal period must be billed as prenatal visits. Services provided during the pregnancy that are not related to the pregnancy diagnosis code may be billed as evaluation and management visits with the appropriate non-pregnancy diagnosis code. To prevent inappropriate claim denials, providers are advised to bill prenatal visits as they occur. The Prenatal Risk Screening should be offered at the first prenatal visit. The prenatal visit that includes completion of the Prenatal Risk Screening is reimbursed once per pregnancy by billing procedure code H1001, add modifier TG if the screening is completed during the first trimester. H1001 is included in the total number of prenatal visits. Do not bill H1001 with a modifier 22. This is not a valid modifier for this code. Maternity Delivery Delivery procedure codes 59410, 59515, 59614, and 59622 include immediate postpartum services within the delivery hospitalization. Deliveries of less than 20 full weeks gestation are billed using procedure codes 59820 or 59821, not a delivery procedure code. When there is a vaginal delivery followed by a cesarean section, the provider must bill both the procedure code for the vaginal delivery and the procedure code for the cesarean section with a modifier 22 on the same claim form. Maternity Fetal Bio-Physical Profile If more than two biophysical profiles are required, the additional biophysical profiles must be billed with a modifier 22. A report must be submitted with the claim that documents the medical necessity for the biophysical profile and the result of each component. Without all of these components and proper documentation, the claim will be denied. Outpatient Hospital Services For each outpatient hospital services, AmeriHealth DC will reimburse according to the individual provider contract rates. As a reminder, members should be referred to LabCorp for outpatient lab services. For more information on LabCorp, please visit www.labcorp.com or call 888-LABCORP. Pain Management Please note, anesthesiologists must also be credentialed to provide pain management services to members of AmeriHealth DC. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 65 Provider Services 202-408-2237 or 888-656-2383 Appendix Routine postoperative pain management, except for continuous epidural, is not reimbursable to the anesthesiologist. Pain management by epidural catheter on the days after the catheter insertion for obstetrical anesthesia may be reimbursed using procedure code 01996 with no time increments. Pharmacy Coverage (PerformRx) PerformRx is the delegated manager of pharmacy services covered by AmeriHealth DC for Medicaid members. For more information on the provision of pharmacy services, including our formulary, specialty and oral prior authorization forms, and pharmacy directory, please visit the provider area of our website at www.amerihealthdc.com. With the exception of oncology, specialty items are drop shipped via our specialty pharmacy program. For questions regarding pharmacy services or to submit a prior authorization request, contact PerformRx at: Provider Services (Medicaid): 888-602-3741 Prior Authorization Fax: 855-811-9332 Pharmacy services for AmeriHealth DC Alliance members are covered directly by the Department of Health Care Finance (DHCF) and fulfilled by its designated pharmacy network. The Alliance formulary and list of participating pharmacies may also be found on the provider area of our website at www.amerihealthdc.com. AmeriHealth DC will cover an emergency supply for Alliance members only when the pharmacies in their designated network are closed or the member is out of the network area. For questions regarding pharmacy services for Alliance members, contact PerformRx at: Provider Services (Alliance): 888-987-5821 Physical/Occupational and Speech Therapies Therapy services may be billed on a UB-04 or CMS-1500 claim form or via 837 electronic format. Transplants AmeriHealth DC covers pre-transplant work-ups, including evaluations, and post-transplant services after discharge from the transplant-related admission. The transplant and related inpatient services are covered by the District’s fee-for-service Medicaid program and must be billed to DC Medicaid. Vision Care Exams Medicaid does not reimburse both an evaluation and management visit and a general ophthalmological visit on the same day for the same member without a referral for the general ophthalmological visit. As a reminder, vision care is not a covered benefit for Alliance members. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 66 Provider Services 202-408-2237 or 888-656-2383 Appendix Vision Claims (eyeQuest) EyeQuest is the delegated manager of vision services covered by AmeriHealth DC. Please visit www.eyequest.com for more information about how to bill for these services. Or contact their Provider Services department at 800-341-8478. Weight Assessment and Counseling for Nutritional and Physical Activity (Child/Adolescent) Please refer to the 2013 HEDIS guidelines provided at the back of this document. Well Child Visits Please refer to the 2013 HEDIS guidelines provided at the back of this document. Women’s Preventive Health Services Please refer to the 2013 HEDIS guidelines provided at the back of this document. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 67 Provider Services 202-408-2237 or 888-656-2383 Appendix Electronic Billing Inquiries Please direct inquiries as follows: Action Contact If you would like to transmit claims electronically… Contact Emdeon at: 877-363-3666 If you have general EDI questions … Contact AmeriHealth DC EDI Technical Support by calling: 202-408-2237 or 888-656-2383 and selecting the appropriate prompts or by emailing: [email protected] If you have questions about specific claims transmissions or acceptance and R059 - Claim Status reports… Contact your EDI Software Vendor or call the Emdeon Provider Support Line at 866-496-2722 If you have questions about your R059 – Plan Claim Status (receipt or completion dates)… Contact Provider Claim Services by calling 202408-2237 or 888-656-2383 and selecting the appropriate prompts If you have questions about claims that are reported on the Remittance Advice…. Contact Provider Claim Services 202-408-2237 or 888-656-2383 and selecting the appropriate prompts If you need to know your provider NPI number… Contact Provider Services at: 202-408-2237 or 888-656-2383 If you would like to update provider, payee, NPI, UPIN, tax ID number or payment address information… For questions about changing or verifying provider information… Please Contact Provider Services: By Fax: 202-408-1277 By Telephone: 202-408-2237 or toll-free at 888-656-2383 If you would like information on the 835 Remittance Advice… Contact your EDI Vendor or call Emdeon at 877363-3666 Check the status of your claim… Review the status of your submitted claims by calling Provider Services or online at www.amerihealthdc.com Sign up for Electronic Funds Transfer Contact Emdeon at 866-506-2830, Option 1 __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 68 Provider Services 202-408-2237 or 888-656-2383 Appendix 2013 HEDIS Billing Guidelines Please note, the following information is reprinted with permission from the HEDIS 2013, Volume 2: Technical Specifications for Health Plans by the National Committee for Quality Assurance (NCQA). HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). To purchase copies of this publication, contact NCQA Customer Support at 888-275-7585 or www.ncqa.org/publications. EFFECTIVENESS OF CARE AND PREVENTION Measure/Coding Directions Adult BMI Assessment (ABA) (Code the visit+ BMI code) Requirement CPT Outpatient Visits 99201-99205, 99211-99215, 99217-99220, 9924199245 99341-99345, 99347-99350, 99385-99387, 99395-99397, 99401 BMI UB Revenue 051x, 0520-0523, 0526-0529, 0982, 0983 V85.0-V85.5 Measure/Coding Directions Requirement Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents (Code the visit+each appropriate component) Outpatient Visits-(Must be with a PMP or OBGYN) CPT BMI percentile Counseling for Nutrition ICD-9-CM Diag/Proc 99201-99205, 99211-99215, 99217-99220, 9924199245, 99341-99345, 99347-99350, 99381-99387, 99391-99397, 99401 V85.5x (use as secondary or greater diagnosis code) V65.3 (use as secondary or greater 97802-97804 diagnosis code) V65.41 (use as secondary or greater diagnosis code) Counseling for physical activity Childhood Immunization Status (CIS) When coding E&M and vaccine administration services on the same date you must append modifier 25 to E&M code effective 01/01/2013 ICD-9-CM Diag/Proc Requirement CPT ICD-9-CM Diag/Proc Dtap 90698, 90700, 90721, 90723 99.39 IPV 90698, 90713, 90723 99.41 MMR 90707, 90710 99.48 Measles and Rubella 90708 Measles 90705 Mumps 90704 Rubella 90706 HiB 90645-90648, 90698, 90721, 90748 Hepatitis B 90723, 90740, 90744, 90747, 90748 070.2, 070.3, V02.61 VZV 90710, 90716 052, 053 Pneumococcal conjugate 90669 HCPCS UB Revenue 051x, 0520-0523, 0526-0529, 0982, 0983 S9470, S9452, S9449 S9451 __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 69 Provider Services 202-408-2237 or 888-656-2383 Appendix Immunizations for Adolescents (IMA) When coding E&M and vaccine administration services on the same date you must append modifier 25 to E&M code effective 01/01/2013. Hepatitis A 90633 070.0, 070.1 Rotavirus (2 doses) 90681 Rotavirus (3 doses) 90680 Influenza 90655, 90657, 90661, 90662 Meningococcal 90733, 90734 Tdap 90715 Td 90714, 90718 Tetanus 90703 99.38 Diphtheria 90719 99.36 99.52 99.39 Human Papillomavirus Vaccine for Female Adolescents HPV 09649, 09650 When coding E&M and vaccine administration services on the same date you must append modifier 25 to E&M code effective 01/01/2013. Measure/Coding Directions Requirement CPT HCPCS UB Revenue Breast Cancer Screening (BCS) Mammography 77055-77057 G0202, G0204, G0206 0401, 0403 Cervical Cancer Screening 88141-88143, 88147, 88148, 88150, 8815288155, 88164-88167, 88174, 88175 G0123, G0124, G0141, G0143, G0147, G0148, Q0091 923 Chlamydia testing 87110, 87270, 87320, 87490-87492, 87810 Requirement CPT LOINC Lead Tests 83655 5671-3, 5674-7, 10368-9, 10912-4, 14807-2, 17052-2, 25459-9, 27129-6, 32325-3 Requirement CPT ICD-9-CM Diag UB Revenue Outpatient 99201-99205, 9921199215, 99217-99220, 99241-99245, 9938299385, 99392-99395, 99401-99404, 99411, 99412, 99420, 99429 462, 463, 034.0 051x, 0520-0523, 0526-0529, 0982, 0983 ICD-9-CM Diag/Proc UB Revenue 460, 465 051x, 0520-0523, 0526-0529, 0982, 0983 466 051x, 0520-0523, 0526-0529, 0982, 0983 Cervical Cancer Screening Chlamydia Screening in Women (CHL) Lead Screening for Children (LSC) Appropriate Testing for Children with Pharyngitis Appropriate Treatment for Children with Upper Respiratory Infection (URI) (Code the visit+URI associated diagnosis) Requirement Outpatient Visits CPT 99201-99205, 9921199215, 99217-99220, 99241-99245, 9938199385, 99391-99395, 99401-99404, 99411, 99412, 99420, 99429 Outpatient Visits 99201-99205, 9921199215, 99217-99220, 99241-99245, 99385, 99386, 99395, 99396, 99401-99404, 99411, 99412, 99420, 99429 Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis (AAB)(Code the visit + bronchitis associated diagnosis) __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 70 Provider Services 202-408-2237 or 888-656-2383 Appendix Use of Spirometry Testing in the Assessment and Diagnosis of COPD (SPR) (Code the visit + COPD associated diagnosis) Spirometry Testing 94010, 94014-94016, 94060, 94070, 94375, 94620 491, 492, 493.2, 496 051x, 0520-0523, 0526-0529, 0982, 0983 Outpatient Visits 99201-99205, 9921199215, 99217-99220, 99241-99245, 9934199345, 99347-99350, 99382-99386, 9939299396, 99401-99404, 99411, 99412, 99420, 99429 493.0, 493.1, 493.8, 493.9 051x, 0520-0523, 0526-0529, 0982, 0983 Use of Appropriate Medication for People with Asthma(ASM) (Code the visit + asthma associated diagnosis) Controlling High Blood Pressure (CBP) (Code the visit + hypertension associated diagnosis) Measure/Coding Directions Cholesterol Management for Patients with Cardiovascular Conditions (CMC) (Code the visit + each appropriate component) Requirement ICD-9-CM Diag/Proc Hypertension 401 Requirement CPT Outpatient Visits 99201-99205, 99211-99215, 99241-99245, 99384-99387, 99394-99397 Requirement CPT PCI ICD-9-CM Diag/Proc 00.66, 36.06, 36.07 92980, 92982, 92995 411, 413, 414.0, 414.2, 414.8, 414.9, 429.2, 433-434, 440.1, 440.2, 440.4, 444, 445 IVD Requirement CPT/CPT Category II LOINC LDL Screening 80061, 83700, 83701, 83704, 83721, 3048F, 3049F, 3050F 2089-1, 12773-8, 1357-7, 18261-8, 18262-6, 22748-8, 55440-2, 39469-2, 49132-4, 69419-0 Requirement CPT UB Revenue Outpatient 99201-99205, 99211-99215, 99217-99220, 9924199245, 99341-99345, 99347-99350, 99384-99387, 99394-99397, 99401-99404, 99411, 99412, 99420, 99429, 99455, 99456 051x, 0520-0523, 0526-0529, 0982, 0983 EFFECTIVENESS OF CARE-DIABETES Comprehensive Diabetes Care (CDC) (Code the visit + diabetes diagnosis+appropriate component) Requirement ICD-9-CM Diag/Proc Diabetes 250, 357.2, 362.0, 366.41, 648.0 Requirement CPT UB Revenue Outpatient Visits 99201-99205, 99211-99215, 99217-99220, 9924199245, 99341-99345, 99347-99350, 99384-99387, 99394-99397, 99401-99404, 99411, 99412, 99420, 99429, 99455, 99456 051x, 0520-0523, 0526-0529, 0982, 0983 __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 71 Provider Services 202-408-2237 or 888-656-2383 Appendix Requirement CPT/CPT Category II LOINC A1C test 83036, 83037, 3044F, 3045F, 3046F LDL-C screening 80061, 83700, 83701, 83704, 83721, 3048F, 3049F, 3050F 4548-4, 4549-2, 17856-6, 59261-8, 62388-4, 71875-9 2089-1, 12773-8, 13457-7, 18261-818262-6, 22748-8, 39469-2, 49132-4, 55440-2, 69419-0 Nephrophathy screening test 82042, 82043, 82044, 84156, 3060F, 3061F USE OF SERVICES-When coding E&M and vaccine administration services on the same date you must append modifier 25 to E&M code effective 01/01/2013. Measure/Coding Directions Requirement CPT ICD-9-CM Diag/Proc Well-Child Visits in the First 15 Months of Life (W15) Well-Child Visit 99381, 99382, 99391, 99392, 99461 V20.2, V20.3, V70.0, V70.3, V70.5, V70.6, V70.8, V70.9 Well-Child Visits in the Third, Fourth, Fifth, and Sixth Years of Life (W34) Well-Child Visit 99382, 99383, 99392, 99393 V20.2, V70.0, V70.3, V70.5, V70.6, V70.8, V70.9 Adolescent Well-Care Visits (AWC) Well-Child Visit 99383-99385, 9939399395 V20.2, V70.0, V70.3, V70.5, V70.6, V70.8, V70.9 ACCESS-AVAILABILITY OF CARE Prenatal and Postpartum Care (PPC) (One of these four options has to occur) Frequency of Prenatal Care (FPC) (One of these four options has to occur) Option 1: Any prenatal care visit to an OB practitioner, a midwife or family practitioner or other PMP with documentation of when prenatal care was initiated. Option 2: Any visit to an OB practitioner or midwife with one of the following: •Obstetric panel •Rubella antibody/titer with Rh incompatibility (ABO/Rh blood typing) •TORCH antibody panel •Ultrasound (echocardiography) of pregnant uterus •Pregnancy-related diagnosis code Option 3: Any visit to a family practitioner or other PMP with a pregnancy-related ICD-9 CM diagnosis code AND one of the following: •Obstetric panel •Rubella antibody/titer with Rh incompatibility (ABO/Rh blood typing) •TORCH antibody panel •Ultrasound (echocardiography) of pregnant uterus When using a visit to a family practitioner or other PMP, it is necessary to determine that prenatal care was rendered and the member was not merely diagnosed as pregnant and referred to another practitioner for prenatal care. Option 4: Any visit to a family practitioner or other PMP with diagnosis-based evidence of prenatal care in the form of a documented LMP or EDD with a completed obstetric history or risk assessment and counseling/education Postpartum Care (PPC) Postpartum visit to an OB/GYN practitioner or midwife, family practitioner, or other PMP on or between 21 and 56 days after delivery. Documentation in the medical record must include a note indicating the date when a postpartum visit occurred and one of the following. • Pelvic exam, or • Evaluation of weight, BP, breasts and abdomen, or – Notation of “breastfeeding” is acceptable for the “evaluation of breasts” component. • Notation of postpartum care, including, but not limited to: – Notation of “postpartum care,” “PP care,” “PP check,” “6-week check.” – A preprinted “Postpartum Care” form in which information was documented during the visit. __________________________________________________________________________________________ * Required (R) fields must be completed on all claims. Conditional (C) fields must be completed if the information applies to the situation or the service provided. Refer to the NUCC or NUBC Reference Manuals for additional information www.amerihealthdc.com 72 Provider Services 202-408-2237 or 888-656-2383
© Copyright 2026