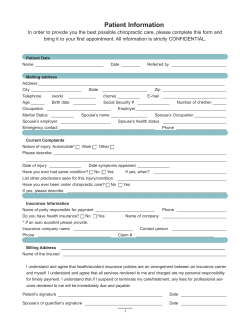
This manual is intended as a refresher summary and study... for experienced chiropractic assistants. It is not a...
CERTIFIED CHIROPRACTIC CLINICAL ASSISTANT Introduction NOTE: This manual is intended as a refresher summary and study aid for experienced chiropractic assistants. It is not a comprehensive text, and chiropractic assistants who lack practical experience should not consider it authoritative or the equivalent of formal, in-depth coursework. A statute was passed by the North Carolina General Assembly mandating that an employee of a chiropractic physician who performs clinical duties must be certified. The law defines who must be certified as follows: (a) "Chiropractic clinical assistant" means a nonlicensed employee of a chiropractic physician whose duties include (i) collecting general health data, such as the taking of an oral history or vital sign measurements, (ii) applying therapeutic procedures, such as thermal, sound, light and electrical modalities, and hydrotherapy, and (iii) monitoring prescribed rehabilitative activities. Nothing in this section shall be construed to allow a chiropractic clinical assistant to provide a chiropractic adjustment, manual therapy, nutritional instruction, counseling, or any other therapeutic service that requires individual licensure. The law goes on to set the requirements as follows: (b) Any person employed as a chiropractic clinical assistant shall obtain a certificate of competency from the State Board of Chiropractic Examiners (Board) within 120 days after the person begins employment. Certification shall not be required for employees whose duties are limited to administrative activities of a nonclinical nature. Except as otherwise provided in this section, it shall be unlawful for any person to practice as a chiropractic clinical assistant unless duly certified by the Board. (c) An applicant for certification under this section shall be (i) at least 18 years of age, (ii) a high school graduate or the equivalent, (iii) of good moral character, and (iv) able to demonstrate proficiency in the following subjects: (1) Basic anatomy. (2) Chiropractic philosophy and terminology. (3) Utilization of standard therapeutic modalities. (4) Contraindications and response to emergencies. (5) Jurisprudence and patient privacy protection. (d) If an applicant for certification is already certified or registered as a chiropractic clinical assistant in another state, the Board shall issue a certificate of competency upon evidence that the applicant is in good standing in the other state, provided the requirements for certification or registration in the other state are substantially similar to or more stringent than the requirements for certification in this State. (e) Any certificate issued under this section shall expire at the end of the calendar year unless renewed in a time and manner established by the Board. Applicants for initial certification or renewal of certification shall pay to the secretary of the Board a fee as prescribed and set by the Board, which fee shall not exceed fifty dollars ($50.00). (f) The Board may adopt rules pertaining to initial educational requirements, course approval, instructor credentials, examination of applicants, grandfathering, reciprocity, continuing education requirements, and the submission and processing of applications as are reasonably necessary to enforce this section." Page 2 Session Law 2013-290 House Bill 371 A Certified Chiropractic Clinical Assistant (CCCA) is an individual who has completed the required number of hours in a clinical setting to be exempted from the education hours and then passed a certification test, or one who has obtained the required education and then passed the certification exam given by the North Carolina Board of Chiropractic Examiners. This certification does not extend to radiographic procedures. A separate certification is required to be eligible to perform these duties. It also does not include manipulative therapy, manual therapy, nutritional instruction or any other service that requires licensure. Clinics may choose to utilize massage therapy as a service to patients. This type of body work is considered to be within the scope of practice for a licensed massage therapist. The chiropractic physician may perform this type of service on a patient but may not direct a chiropractic assistant (certified or not) with no other licensure to perform the service. A chiropractic assistant (CA) is an individual who performs administrative duties only and does not interact with any treatment performed on the patient. The North Carolina Board of Examiners is empowered to pass rules that will help to administer the law described above. As part of those rules, some chiropractic assistants may be certified as part of a “grandfather” process described as follows: Grandfathered Applicant - An employee of a chiropractic physician who has amassed a minimum of 500 hours of clinical employment by July 1, 2014. The employing physician must confirm the hours and state that he/she has performed on the job training for the chiropractic assistant. Reciprocity Applicant - An applicant who is already certified or registered in another state as a certified clinical assistant and the requirements are substantially similar or more stringent than the requirements in North Carolina. New Applicant - An applicant who has not amassed a minimum of 500 hours by July 1, 2014. Requirements for certification for a new applicant: Completion of an approved educational program consisting of a minimum of 24 hours. 2 1) 18 hours may be obtained online. 6 hours must be in-person didactic training. 2) Complete and submit an application, fee of $20.00 and an affidavit attesting to good moral character. When this has been received and processed, the applicant would be eligible for a competency examination and certification. These examinations shall be available at least 4 times per year. If there is a lapsed certification due to non-renewal and the lapse does not exceed 12 months, the certificate holder may obtain reinstatement by making up the continuing education and submitting the renewal fee. If the lapse is longer than 12 months, it would be necessary for the candidate to re-take and pass the proficiency examination for new applicants and pay a renewal fee. History Dr. Daniel D. Palmer, also known as D.D. Palmer, was the founder of chiropractic in 1895 when a man by the name of Harvey Lillard, who was an acquaintance of Dr. Palmer, became the very first chiropractic patient. Mr. Lillard had been deaf for approximately 17 years after having an injury in his cervical spine. Dr. Palmer performed an adjustment and Mr. Lillard’s hearing was restored. After the news spread regarding this new form of healthcare, other patients began to seek Dr. Palmer’s care. Palmer Chiropractic College was the first chiropractic college formed in 1897. D.D. Palmer had a son, Dr. B.J. Palmer, who continued with chiropractic after his father’s death. Other chiropractic colleges were then formed. Chiropractic is from Greek words meaning “done by hand”. A chiropractic physician may use their hands to perform a manipulation or various types instruments may also be used for this purpose. Chiropractic care does not involve the use drugs or surgery. Chiropractic treatment has very few risks or side effects. Chiropractic physicians may treat acute and chronic conditions. They examine patients, especially the spine, to determine the cause of the patient’s condition. The doctor of chiropractic will then make recommendations for correction, or prevention of future conditions. Chiropractic has repeatedly been shown to be more cost-effective for certain conditions while maintaining some of the highest patient satisfaction with outcomes. Depending on the severity of the complaint and after a thorough examination, the doctor may recommend a number of treatments which may include spinal manipulative therapy, physiological therapeutics, rehabilitative exercises, supports, nutrition and other procedures to accomplish correction. 3 Chiropractic Philosophy and Physiology The principle of chiropractic is that the body is designed to heal itself, up to the point of the limitation of matter. The system in the body that controls all other systems is the nervous system. The nervous system normally maintains a steady environment or “steady state” in the body. An example is the body shivering to generate heat when the nervous system perceives that the environmental temperature is cold. The nervous system is what “senses” the cold, and the nervous system tells the muscles to shiver until enough heat is generated. The body’s ability to maintain this steady state is called “homeostasis”. Homeostasis literally means – steady state. When the spine is in normal alignment and the nervous system is functioning properly, and if all other conditions necessary for health are present such as sleep and nutrition, then the body is allowed to maintain homeostasis in all areas and the person experiences health. Health can be defined as optimum physical, mental, and social well-being, not just the absence of disease. If the spine is misaligned or fails to function as designed, this can cause a poorly functioning nervous system resulting in nerve impairment and poor function of the same areas that are supplied or innervated by that nerve. The result is that the body cannot maintain homeostasis and therefore cannot achieve health. Interestingly, sometimes this can be the case but there are no symptoms or pain. Accidents, injuries, overexertion and poor posture are some of the most common reasons for misalignment. Some of the common terminology that refers to this spinal misalignment or loss of function in its various clinical presentations include: Subluxation Fixation Vertebral Subluxation Complex Joint Dysfunction Joint Immobility Spinal Manipulable Lesion You should adopt the language that is preferred by your employing doctor of chiropractic. The danger of this lesion is that it can cause: pain, spasm, swelling, degeneration (arthritis) and most importantly- nerve irritation and decreased health in the part of the body supplied by that nerve. The correction for the lesion described above i.e. subluxation is called an adjustment. An adjustment is given by hand or with an instrument to restore normal function to the joint, relieve interference to the nerves, and allow the body to maintain homeostasis and 4 therefore, health. Sometimes there is so much degeneration, tissue damage, or scarring that the body will NEVER be able to fully regain health. In that case the patient may be managed by the doctor of chiropractic to prevent additional damage and manage the symptoms, or the patient may have to be referred for other treatment such as drugs or surgery. ANATOMY Anatomy is the study of the body’s structure. Physiology is the study of the body’s function. Other Definitions: Anomaly - A marked deviation from the normal standard, especially as a result of congenital or hereditary defects. Nerve - A cordlike structure comprising a collection of nerve fibers which convey electrical impulses between the brain and some other region of the body. SPINAL ANATOMY AND CURVES Cervical Spine 1. The first seven spinal bones (called vertebrae) make up the cervical spine or neck. They are numbered one through seven from top to bottom. So the 4th bone from the top is referred to as 4th cervical or C4. 2. The skull sits on top of the cervical spine, infact it sits on top of C1 also known as the atlas. 3. There is no disc between the atlas (C1) and the second bone known as C2 or axis. 4. The normal curvature of the cervical spine is called a lordotic curve. This means it curves forward in the middle of the curve (remember “forward with the lord”) Clinical Note: A common x-ray finding of an injured or damaged cervical spine is a loss of, or actual reversal of the normal cervical curve. Thoracic Spine 1. These are the twelve vertebrae of the mid - back which articulate (form joints) with the ribs. They are numbered one through twelve from top to bottom. For example, the fourth thoracic vertebra is referred to as T4. 2. The normal curvature in this area is known as a kyphotic curve or backward curve. 3. The thoracic vertebra are the only ones with ribs. There are 12 pair of ribs, one pair for each of the twelve thoracic vertebra. 5 Clinical Note: Hyper-Kyphosis is an exaggerated kyphotic curvature in the thoracic region and is commonly known as “humpback”. Clinical Note: Normally if the spine is viewed from behind the patient, the spine should be straight. Scoliosis is when the spine grows with a curve to the right or left when viewed from behind. Lumbar Spine 1. There are the five vertebrae of the lower back. They are numbered one to five from top to bottom and the last, or bottom-most vertebra in the spine is L5. 2. The normal curve in this area is known as lordotic. It is a forward curvature just like the cervical curve. Clinical Note: Hyper-Lordosis is an exaggerated curvature in the lumbar region commonly known as “swayback”. Sacrum 1. This is a bone composed of 5 united/fused vertebrae situated below the lumbar spine. It is one solid bone soon after birth. When viewed from behind it looks like an upside down triangle. When viewed from the side, it has a kyphotic curve like the thoracic spine. 2. The sacrum sits under, and supports, the 24 moveable vertebra of the spine. Coccyx 1. Last bone of the vertebral column, commonly known as the tail bone. It too is composed of multiple small vertebra that were fused soon after birth into the bone we call the coccyx. Vertebral Disc ( also Intervertebral Disc) 1. These are the somewhat soft cushions between most of the spinal bones (vertebrae). They act as shock absorbing cushions and allow for flexibility. They consist of rings of ligament much like tree rings, around a center of gelatin-like material. Sometimes, the gelatin-like material oozes out of the disc and puts pressure on a nerve or the spinal cord. This is called a herniated or bulging disc. Clinical Note: A herniated disc or bulged disc is usually the result of some type of excessive strain of the disc. This can be gradual as in poor posture, or sudden as in an accident. Additional Skeletal Anatomy Please be familiar with some of the major bones as follows: 6 Occiput (the skull bone at the back of the head that sits on top of C1) Humerus (Upper arm bone) Radius and Ulna (Lower Arm bones) Femur (The longest bone in the body) Tibia (the larger of the two lower leg bones, called the “shin”) Fibula (Smaller and more outside/lateral) Cervical Spine –top 7 vertebra Thoracic Spine- 12 vertebra Lumbar SpineLast 5 moveable vertebra Sacrum Coccyx Lateral (Side) View Antero-Posterior View (AP View) 7 Bulging or Herniated Disc Spinous Process Disc (Intervertebral Disc) Vertebral Body Hole for Nerve (called a Foramen) NOTE: In this case the disc is bulging backward into the hole (foramen) where the nerve exits between the spinal bones (vertebra). Scoliosis on X-ray Ribs Thoracic Spine with abnormal curve into lumbar spine Pelvis Sacrum Hip Joint 8 The Nervous System The brain and Spinal cord are protected by the skull and vertebral column. The spinal nerves exit the spinal column between two vertebra through a hole called an intervertebral foramen. The nervous system controls ALL other systems and function of the body. 9 PHYSIOLOGICAL THERAPEUTIC MODALITIES (Also known as Physiotherapy) Physiological therapeutics can be defined as “Any physical agent applied to produce therapeutic changes to biologic tissues; includes but not limited to thermal, acoustic, light, mechanical, or electric energy.” They can be attended (by a doctor or assistant) OR non-attended (meaning the patient does not have anyone supervising the therapy). The primary intended responses are to exert changes on the human body through increased blood flow, heating of tissues, relaxing contracted tissues, or accelerating cell metabolism. This results in rehabilitation and restoration of function, provides a reduction in disability, improved activities of daily living, and improved function and health to the patient. The attending chiropractic physician must determine which modality is most appropriate for use. This determination is based upon the four (4) stages of healing. The 4 stages of healing include: a. Acute stage is often considered within the first 72 hours (3 days) following an injury. The acute stage of care is directed at reducing pain, spasm, edema or loss/reduction of function. b. Sub-acute stage of healing continues for an additional 1-3 weeks but tissue healing may continue for up to 12 weeks. Treatment during the sub-acute stage shall be for the continued control of pain, spasm and edema with the intent of improving range of motion more than what was observed in the acute stage. In this stage, the improvement in muscle strength, reduction in ligamentous instability, improved soft and hard tissue healing and continued progress in bodily function is to be noted. c. Chronic stage begins when the sub acute stage ends and may continue for an indefinite period of time if the condition is not previously resolved. Chronic stage treatment provides for additional mobility and function with further increased strength and range of motion. At this stage, there may not be a possibility of fully resolving the patient’s condition so the goal becomes to manage it while allowing the patient to live the most complete lifestyle possible. d. Chronic recurrent stage includes intermittent exacerbations and remissions requiring additional therapy. The chronic recurrent stage may occur from overuse, instability, poor nutrition, underlying disease, poor case management or a return to activity too soon. The goal in this stage would be to control pain, edema and spasm and maintain mobility and function so not to regress. The goal is to treat the patient for the acute exacerbation, then return them to supportive care for their chronic condition. Factors that affect the patient’s ability to heal include: 1. Age of patient 2. Underlying disease 10 3. 4. 5. 6. 7. 8. Nutritional deficiencies Mechanism of injury Degree of injury or illness Tissues involved in the injury or illness Patient’s current state of health or prior injuries or illnesses Compliance with doctor’s recommendations A modality is a type of electrical, thermal or mechanical energy that causes physiological changes. It is used to relieve pain, improve circulation, decrease swelling and reduce muscle spasm. Typical types of modalities include electrotherapy i.e. electrical muscle stimulation, thermotherapy i.e. ultrasound or heat/ice packs, mechanotherapy i.e.traction and others. ULTRASOUND Ultrasound is high frequency sound waves that produce a form of deep tissue vibration and heating. It is used for relief of pain and muscle spasm, promotes circulation and relaxes tight muscles and soft tissue. The doctor must determine several factors prior to performing ultrasound treatment in order to achieve the desired effects. The desired depth of penetration, intensity of treatment and whether the wave is continuous or pulsed should all be considered. The frequency of the application determines the depth of treatment. The ultrasound wave can be continuous or intermittent (pulsed). Continuous treatment means the ultrasound is always generating energy. This treatment produces deep heat. Pulsed ultrasound treatment means that sound waves are very quickly turning on and off. This treatment creates mainly non-thermal effects. The intensity determines how much heat is produced. The higher the intensity, the more heat the patient should feel. The intensity should never be at a higher level than where a warming sensation is felt, but never when pain or burning is reported by the patient. During ultrasound treatment, the sound head should never be lifted from the patient or it may damage the ultrasound machine. ALSO- during continuous ultrasound treatment, the ultrasound head SHOULD NEVER STOP MOVING . There must be continuous contact of the sound head against the patient’s skin. There is an exception to this and that is when ultrasound treatment is being used under water. In this situation, there should be a gap between the soundhead and the patient, but the gap should be filled with water. Ultrasound treatment is most commonly administered with a water-soluble gel. There 11 should be a sufficient amount of gel to allow good contact and ease when moving the sound head on the patient’s skin. The sound head should be moved in a slow circular motion with a small amount of pressure, but should never be held still. Common Indications for Use 1. Soft tissue injuries 2. Chronic connective tissue and joint dysfunction 3. Osteoarthritis 4. Bursitis 5. Tendonitis, bursitis, capsulitis 6. Nerve entrapments 7. Chronic sprains / strains 8. Muscle spasm Contraindications 1. Cancerous lesions 2. Pregnant uterus 3. Metal implants 4. Eyes, heart, reproductive organs 5. Over the spinal column / brain (never over the bony spine, safe to use to the sides of the spine) 6. Impaired circulation or sensation 7. Fractures 8. Tissue under therapy with radiation 9. Growing bones CRYOTHERAPY (Cold Therapy) This is the application of cold temperatures for the purpose of removing heat or altering temperature in the body or body tissue. Cryotherapy includes ice packs, vaso-coolant sprays, cold pack or compress, ice massage or other cooling devices. Altering temperatures in the body or body tissue is usually superficial and most of the time used in acute or sub-acute injuries for pain relief. It also reduces swelling, inflammation and muscle spasms. Sensations felt with the use of ice packs – initially cold sensation, then stinging, and eventually numbness. Patients can be given instructions on home care utilizing cold packs. The patient should be instructed on use. For instance, how long the ice packs should remain on the body before removing, how long to leave them off, and a schedule for reapplying. Patients should never be instructed to lie on an ice 12 pack. Contraindications of cryotherapy include: a. Impaired local circulation b. Areas of impaired sensation or circulation c. Raynauld’s symptoms d. Cyanosis (blue colored skin) e. Skin rashes or open wounds f. Utricaria (rash) Clinical Note: a. Do not use any type of cryotherapy over the skin for greater than one hour b. Watch for signs of frostbite (damaged skin due to freezing) When treating in a bath of cold solution, it is important for the patient to move the body part slowly and monitor the fingers/toes for aching sensation. Stop prior to this and remove from solution to allow normal room temperature to equalize it. When using direct application of ice, NEVER place directly onto skin. Place a paper towel, plastic barrier, or cool wet towel directly on the skin surface. An ice massage is an effective therapy for small treatment areas. Move the ice pack or cube slowly over the area for trigger points, muscle spasms and contusion. THERMOTHERAPY (Heat Therapy) Thermotherapy is the use of therapeutic heat which promotes circulation and relaxes tense muscles. This could include heating pads, hot compresses, hot water bottle, ultrasound, diathermy, whirlpool, sauna, infrared and others that would increase localized temperature. Effects of thermotherapy include: a. Decreased pain b. Decreased tense muscles c. Decreased inflammation in the chronic state d. Increased local circulation Contraindications of thermotherapy include: a. Reddening or burning of the area b. Skin rashes c. Increased swelling d. Increased pain e. Malignancy f. Areas where blood or fluid is pooled g. Pregnancy 13 When using any heat therapy, the following rules should be observed: a. Never heat over an area where there is already an open wound, burn, sunburn or rash b. Use caution putting heat over bony areas c. The skin should be clean, dry and free of grease, oil and dirt d. Check the area within 5 minutes after initiating treatment and then periodically during treatment. e. Discontinue if patient complains of burning, nausea, dizziness or other signs of distress f. Patient should never lie on heat packs Clinical Note: Moist heat vs. dry heat: Moist heat does not dry out tissues. It penetrates better and is useful in sub-acute and chronic conditions. Clinical Note: Hydrocollator packs (moist heat packs) provide superficial moist heat. They are usually kept in a stainless steel tank at about 150-170 degrees. They are placed into a cloth case prior to applying to patient. The body area should be clean and dry. The patient should be instructed to remove the pack if it becomes too hot. Doctor or therapist should check on the patient’s skin periodically. Thick towels can also be utilized with hydrocolators. ELECTROTHERAPY Electrotherapy includes high volt currents, low volt currents and the combination of both in either the alternating or direct currents. ELECTRIC STIMULATION Prior to beginning any type of therapy, the equipment should be checked for worn or damaged parts. In the case of electrical stimulation, the electrodes should be checked to verify there is no damage. The control should be in the “off” position prior to making contact with the patient. The machine should then be set to patient tolerance as all patients react differently to this type therapy. There may be some patients that have the opinion “the stronger, the better”. This is not accurate because if the therapy is too strong, it could decrease maximum benefit to the patient or even cause harm. Effects of electrotherapy include: a. Pain control b. increased range of motion c. increased blood supply d. muscle stimulation & re-education 14 e. lymph and venous drainage f. reduce muscle spasm g. reduce edema and swelling h. general tissue healing i. improved strength and endurance in muscle Contraindications of electrotherapy a. pacemakers or other implanted electrical devices b. malignancy (except pain control) c. rashes, open lesions and sunburn d. over the skull, eyes, uterus or throat e. thrombophlebitis f. advanced cardiovascular disease or other systemic disease g. seizure disorders Clinical Note: Iontophoresis is the use of ultrasound or electric current to drive a topical substance through the skin and into the body. The contraindications of iontophoresis are generally the same as those for ultrasound and electrotherapy. MECHANOTHERAPY Mechanotherapy includes active and passive exercises, pressure point therapy, massage, traction, supports, lifts, esthetics. TRACTION Traction is a pulling force to the spine to separate vertebra. Traction can be performed either manually or mechanically. It may be designed to relieve pressure on a swollen spinal segment, or it may be intended to restore motion to a section of the spine that has decreased mobility, as in intersegmental traction. Effects of mechanotherapy include: a. increased circulation b. decreased spasm c. improved lymphatic flow d. pain reduction e. increase range of motion f. decrease local edema (swelling) Contraindications include: a. Osteoporosis 15 b. c. d. e. f. g. h. Infection Tumor Pregnancy Hernia Circulatory disease Fracture Surgery Responsibilities of CCCA Each CCCA should become familiar with the privacy, safety, and procedures of the office. In addition, they should be trained on and become familiar with the specific modalities in the office prior to performing services with these machines. Utilization of modalities must be directed and supervised by the chiropractic physician. The applicable standard of care requires that a chiropractic physician be present in the clinic when a CCCA applies therapeutic modalities, but the doctor is not required to observe or oversee the application of the modality. The NC Board of Chiropractic Examiners requires that each clinical assistant possess knowledge of: 1. The application of physiological therapeutic modalities 2. How, when and why they are applied (Indications) 3. When to inform the doctor that changes have occurred in a patient 4. What risks and contraindications may be associated with the application of these modalities 5. Proper maintenance of the therapeutic devices and other products utilized 6. Recording of information regarding utilization of therapy performed by the assistant SEXUAL AND PERSONAL BOUNDARIES When you are at work, you should strive to maintain a professional attitude and demeanor, regardless of whether you are dealing with patients or co-workers. The hallmarks of 16 professionalism include the following: 1. Limit disclosures about your personal life. Your attention should be devoted to the patient’s health; talking about your own problems signals that you are not focusing fully on the patient. 2. Always be pleasant, but don’t encourage patients to become your friends. Don’t consider dating a patient while the patient is under active care. 3. To the extent possible without giving offense, don’t accept gifts from patients. 4. Do your best to protect the patients’ privacy by using sheets, gowns, shrouds, trenchcoats, canvas tarps and/or plywood panels to cover their bodies. 5. Don’t tell off-color jokes or make sexual innuendoes. Do your best to discourage patients from telling off-color jokes in your presence. 6. Don’t remark or comment upon: Anyone’s personal behavior The attractiveness of the patient’s body, or lack thereof Sex 7. Never touch a patient inappropriately. Limit your physical contact to doctor-ordered therapeutic procedures only. 8. Don’t gossip about other patients or your co-workers. DOCUMENTATION All documentation should be complete, accurate and legible. If another doctor is filling in for the main doctor, he/she should be able to look at the notes and get a complete picture of the patient. It is acceptable to utilize abbreviations but all should take care to use common abbreviations. Any usage of notations that are not considered common should have a key or explanation of the abbreviation. If hand written notes are made, they should be in ink and never in pencil. The daily notes should be in chronological order and treatment rendered should be signed by the individual performing that particular portion of the treatment. There should never be any erasures, blacked out portions or white-out used. If it becomes necessary to change or correct an entry, it should be drawn through with a single black line, corrected, and signed or initialed. 17 When documenting physiotherapy modalities, a CCCA should list what modality was used, the duration of the therapy, and any applicable setting. The documentation should then be signed. The accuracy of records and daily notes is important because these are considered legal documents when presented in court. Documentation on the initial intake form for patients should include but not limited to: Demographic information, birthday, age, M/F, marital status, spouse’s name Employer information and type of duties patient performs Health history Chief complaint followed by secondary complaints (if applicable) How long problem has existed When and how complaint began Previous treatment and by whom Current pain grade as expressed by patient Smoker or non smoker What worsens pain What relieves pain Does the pain radiate Type of pain (sharp, dull, etc.) Has the pain interfered with ADLs (Activities of Daily Living) Clinical Note: Subjective information is that which is reported by the patient i.e. patient report of symptoms. Objective information is that which is observed by the doctor i.e. limited range of motion. PROTECTING PATIENT PRIVACY Protecting the privacy rights of patients is one of the most basic legal duties imposed upon chiropractic clinics. Federal statutes such as HIPAA and HITECH, along with rules adopted by various regulatory agencies, describe a broad range of situations where privacy rights can be compromised. In order to comply with privacy laws, you and your co-workers should always observe the following protocols: 1. Protected Health Information (PHI) consists of treatment records, billing records, sign-in sheets and any other records containing patient identifiers such as name, address, place of employment, telephone number, email address or social security number. 2. In general, do not disclose a patient’s PHI to anyone other than the patient unless the patient has authorized you to make disclosure to a third person. The patient’s 18 authorization must be in writing and no more than six months old. However, there are exceptions to this rule. No patient authorization is required when: You send PHI to your clinic’s billing service or debt collection service; You send PHI to workers compensation carriers; You send PHI to a law enforcement agency at the agency’s request (the Board of Chiropractic Examiners is a law enforcement agency). You send PHI in response to a subpoena or court order. 3. Do not disclose PHI to a patient’s spouse or other family member or caregiver unless the patient authorizes the disclosure. 4. Each patient must sign a Notice of Privacy Rights that informs the patient how your clinic protects PHI. If your clinic sends out birthday cards or appointment reminders, make sure the Notice of Privacy Rights alerts patients to expect these types of communication. 5. Do not discuss PHI where non-employees might overhear your conversation. Examples of potential problem situations include: Telephone calls in the vicinity of patients Conversations over the intercom Conversations at the waiting room counter Conversations in the hallway when patients are entering or leaving treatment rooms. 6. Computers containing PHI must be password-protected. Computer monitors must be placed so only clinic personnel can view the screen. Before leaving a computer unattended, close any active file and bring up the log-on window. 7. If PHI is maintained on paper documents, you must protect against accidental disclosure to unauthorized persons. Insert charts in wall holders so that no PHI, including the patient’s name, can be read. Do not leave charts face-up at your workstation. Do not leave charts unattended at photocopiers or fax machines unless this equipment is located in a secure area that is inaccessible to non-employees. 8. One staff member should be designated the privacy protection officer, and that person should maintain a log of all disclosures of PHI, including the legal justification for making a disclosure, such as “authorized by the patient per attached release.” 9. When the clinic’s answering machine is on and unattended, the volume setting should be low so that messages left by patients cannot be overheard. 10. Patient sign-in sheets must be partially covered so that when presenting for an appointment, the patient cannot see who signed in ahead of him or her. 19 11. When not in use, patient records must be stored in locked cabinets or storage rooms. 12. Old charts and other records that contain PHI cannot be discarded as ordinary trash; they must be shredded or otherwise destroyed to prevent unauthorized disclosure. 13. Patients who are younger than 18 must have a parent or legal guardian sign all documents in their behalf, including authorizations to disclose PHI. Be certain that you know the relationship between a minor patient and anyone claiming to be the patient’s guardian. 14. If you suspect that a patient’s PHI has been disclosed inappropriately or otherwise compromised, report the breach to your employing physician immediately. Your physician may have a duty to notify affected patients or, in cases of large-scale breach, to regulatory authorities. 15. If a patient requests a copy of his or her records, the clinic must honor the request within 14 days. You are allowed to charge a copying fee as follows: $.75 per page for the first 25 pages, $ .50 per page for pages 26-100, $ .25 per page for each page over 100. The right of patients to have copies of their own records upon request is absolute and must be honored in every case, regardless of whether the patient has an unpaid balance. Emergency Procedures Heart Attack As with other parts of the body, the heart must have a supply of oxygen and nutrients. Two coronary arteries supply this oxygen to the heart muscle. If one of the arteries is blocked too long, the heart is not receiving the needed oxygen and heart tissue could die. Some heart attacks can last several hours, so it is important to seek help quickly. Some of the signs of a myocardial infarction (heart attack) are squeezing chest pain, shortness of breath, nausea, pain into the shoulder and back, cold sweats, vomiting, feeling faint and possibly breast and arm pain in women. There is a possibility the patient is suffering a heart attach without pain. If that is the case, there may be symptoms such as weakness, dizziness, pounding heart, shortness of breath, nausea or vomiting. If there are any of the signs of a possible heart attack, seek help. If in an office setting, notify the doctor and call 911. Stroke 20 When arteries that supply oxygen to the brain rupture or become blocked, it could lead to a stroke. Some signs of a stroke are paralysis of arms or legs or one side of the face, tingling, numbness, confusion, dizziness, double vision, slurred speech or weakness on one side of the body. Other emergencies that may be seen in a chiropractic office: Head trauma Suspected spinal injury Bleeding Cardiac arrest Stroke Convulsion or seizure Choking Heart attack Clinical staff should be trained in areas of emergencies and instructed what steps should be followed when one arises. Most of these will require emergency medical intervention. When in doubt, call 911. 21 TERMINOLOGY Abduction Away from the midline of the body Acute New, sudden Adduction Movement towards the center of the body Antalgic Leaning away from pain Anterior To the front Atlas First cervical vertebra Axis Second cervical vertebra Caudad Towards the feet Cephalic Towards the head Chronic Long standing Coccyx Last bone of the vertebral column Congenital Existing at or before birth Contralateral Opposite side Degeneration Deterioration which causes some degree of loss of function Distal Away from point of reference Extension Bending backward External rotation - Turning away from midline Flexion Act of bending forward Humerus Arm bone Inferior Beneath, lower Inflammation Tissue reaction producing symptoms of swelling, heat, redness Internal rotation Turning to midline Intervetebral disc - Fibro elastic cartilage between the vertebrae Ipsilateral On the same side Lateral To the side Lateral recumbent - Lying on side Mandible Jaw bone Medial Toward the mid line MUA Manipulation under anesthesia Objective Information observed by a provider Palmer Palm of the hand Plantar Sole of foot Posterior Back or behind Prone Lying face down Proximal Near the point of reference Scapula Shoulder bone Sprain Injury in which the ligaments are stretched or lacerated Sternum Chest bone Strain Over stretching or overexertion of a muscle Subjective Information a patient may tell a Dr. Subluxation Misalignment of a vertebra Superior Higher, above Supine Lying on back, face up Ventral Anterior Vertebra Bony segments forming the spine 22
© Copyright 2026